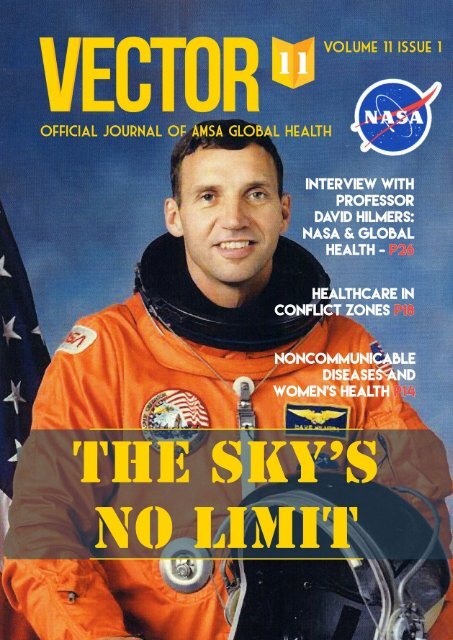
Vector Volume 11 Issue 1 - 2017
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
1
Advisory Board<br />
The Advisory Board, established in <strong>2017</strong>, consists of academic mentors who provide guidance for the<br />
present and future direction of <strong>Vector</strong>.<br />
Dr Claudia Turner<br />
Consultant paediatrician and clinician scientist with the University of Oxford & Chief Executive Officer of<br />
Angkor Hospital for Children.<br />
Professor David Hilmers<br />
Professor in the Departments of Internal Medicine and Pediatrics, the Center for Global Initiatives, and<br />
the Center for Space Medicine at the Baylor College of Medicine<br />
Associate Professor Nicodemus Tedla<br />
Associate Professor at the University of New South Wales School of Medical Sciences<br />
Dr Nick Walsh<br />
Medical Doctor (RACP) & Regional Advisor for Viral Hepatitis at the Pan American Health Organization<br />
/ World Health Organization Regional Office for the Americas<br />
<strong>2017</strong> <strong>Vector</strong> Committee<br />
Editor-in-chief<br />
Carrie Lee carrie.lee@amsa.org.au<br />
Associate Editors<br />
Kryollos Hanna Sophie Lim Koshy Matthew Nic Mattock Aidan Tan<br />
Ash Wilson-Smith Sophie Worsfold Danica Xie<br />
Publication Designer<br />
Lucy Yang<br />
Design and layout<br />
© <strong>2017</strong>, <strong>Vector</strong><br />
Australian Medical Students’ Association Ltd, 42 Macquarie Street, Barton ACT 2600<br />
vector@globalhealth.amsa.org.au<br />
vector.amsa.org.au<br />
Content<br />
© <strong>2017</strong>, The Authors<br />
Cover designs by Lucy Yang (University of New South Wales)<br />
<strong>Vector</strong> Journal is the official student-run journal of AMSA Global Health.<br />
Responsibility for article content rests with the respective authors. Any views contained within articles are those of the<br />
authors and do not necessarily reflect the views of the <strong>Vector</strong> Journal or the Australian Medical Students’ Association.<br />
i
Contents<br />
Editor’s Note: The Sky’s No Limit 1<br />
Commentary<br />
Rise of Trump/Fall of Health 2<br />
Owen Burton<br />
Anti-vaccination: Separating Fact from Fiction 5<br />
Elissa Zhang<br />
Climate Change and <strong>Vector</strong>-Borne Disease in Kiribati 8<br />
Erica Longhurst<br />
Features<br />
Humanity Lost? <strong>11</strong><br />
Patrick Walker<br />
Redefining Women’s Health: A Noncommunicable Diseases Perspective 14<br />
Charlotte O’Leary<br />
Healthcare in Conflict Zones 18<br />
Michael Wu<br />
Surgery: Luxury or Necessity? 22<br />
Maryam Ali Khan (Pakistan), Zineb Bentounsi (Morocco), Nayan Bhindi (Australia), Helena Franco (Australia), Tebian<br />
Hassanein Ahmed Ali (Sudan), Katayoun Seyedmadani (Grenada/USA), Ruby Vassar (Grenada), Dominique Vervoort<br />
(Belgium)<br />
Beyond the Horizon and Back Again: Interview with Professor David Hilmers 26<br />
Ashley Wilson-Smith<br />
Reviews<br />
PrEP-related health promotion for Aboriginal and Torres Strait Islander Gay and Bisexual Men 29<br />
Alec Hope<br />
Mental Illness Following Disasters in Low Income Countries 32<br />
Rose Brazilek<br />
Factors that Contribute to the Reduced Rates of Cervical Cancer Screening in<br />
Australian Migrant Women - a Literature Review 36<br />
Archana Nagendiram<br />
Medical Electives in Resource-poor Settings: Are We Doing More Harm Than Good? 40<br />
Gabrielle Georgiou<br />
Conference reports<br />
IFMSA - 5 letters with one big mission! Australian Medical Students attend the IFMSA 66th<br />
General Assembly in Montenegro 44<br />
Aysha Abu-sharifa, Stormie de Groot, Julie Graham, Justine Thomson<br />
Changing Climate, Changing Perspectives: iDEA Conference Report 47<br />
Isobelle Woodruff<br />
ii
Editor’s Note: The Sky’s No Limit<br />
Of the many things that come to mind when one thinks<br />
about global health, an astronaut is probably not high on the<br />
list. The front cover of this first issue of <strong>Vector</strong> for <strong>2017</strong> is<br />
not what we would conventionally expect of a global health<br />
journal. And yet, that is precisely the message that this issue<br />
conveys – the limitless diversity that global health has come<br />
to represent. We are living in an increasingly globalised world,<br />
with greater wealth and inequality we have ever encountered.<br />
We have made remarkable progress over the past few<br />
decades on the frontier of global health, including increased<br />
vaccination and access to treatment for diseases such as<br />
HIV. However, the agenda is now shifting to focus on new and<br />
emerging challenges.<br />
Undoubtedly, healthcare in a global context is intrinsically<br />
connected to the political, social and cultural phenomena<br />
that define today’s world. The rise to power of the United<br />
States President Donald Trump raises serious questions<br />
and concerns about the future of global health, with his<br />
controversial approaches and perspectives towards climate<br />
change, refugees and migrants, as well as sexual and<br />
reproductive health. Owen Burton (p 2) provides a thoughtprovoking<br />
commentary on these issues, and urges Australia<br />
to consider our future potential role in leading an alternative<br />
direction rather than following the direction set by the US.<br />
War and conflict, political stability and human rights<br />
also intersect with global health issues, as we see with the<br />
distressing increase in targeted attacks on health care<br />
facilities, Michael Wu (p 18) offers an insightful perspective<br />
into the situation of medical neutrality in conflict zones. In<br />
addition to man-made crises, natural disasters also pose a<br />
threat to human health and health care systems, with mental<br />
health implications a particular concern deserving attention,<br />
as discussed by Rose Brazilek (p 32).<br />
Climate change is the greatest challenge we are facing<br />
in the global health arena. Personal experiences and<br />
commentary are provided by Erica Longhurst (p 8).<br />
Noncommunicable diseases (NCDs) account for a<br />
substantial proportion of the global burden of disease. We<br />
are reminded by Charlotte O’Leary (p 14) that we need<br />
to question and redefine the approach we take towards<br />
this issue, to ensure that women’s health is not limited to<br />
reproductive health concerns, but a holistic approach over<br />
the entire life course, including addressing the risk factors<br />
and burden of NCDs specific to women and girls.<br />
Yet whilst our focus often turns to issues “abroad”, there<br />
is much to be addressed in global health on a local level.<br />
Health promotion amongst key populations in Australia is a<br />
particular topic of interest. A comprehensive review article by<br />
Alec Hope (p 29) describes issues regarding the promotion<br />
of HIV pre-exposure prophylaxis amongst Aboriginal gay and<br />
bisexual men in Australia. Migrant women in Australia also<br />
have lower rates of cervical cancer screening; the factors<br />
and interventions to address this issue are explored in a<br />
review article by Archana Nargendiram (p 36).<br />
The recent health policy “No Jab No Play / No Jab No<br />
Pay” also raises the issue of vaccination scepticism and<br />
conscientious objection, a concerning phenomenon in<br />
Australia as well as worldwide. A commentary by Elissa<br />
Zhang (p 5) provides an interesting overview of historical<br />
events like the Cutter Incident (involving the polio vaccine)<br />
and common concerns held by ‘anti-vaxxers’.<br />
With so much happening in global health, it is<br />
understandable for the general public, and particularly young<br />
people, to feel disenfranchised or disempowered. We even<br />
become desensitised and apathetic to the problems; such as<br />
conflict, mass displacement and natural disasters; that we<br />
are constantly exposed to in the media. Patrick Walker calls<br />
on us to remember the human side to the tragedies that we<br />
see, but also to promote tolerance and understanding with<br />
people who hold different views to our own (p <strong>11</strong>).<br />
An interview by Ashley Wilson-Smith with NASA astronaut,<br />
paediatrician and internist Professor David Hilmers (p 26)<br />
provides a window into his vast experiences in resourcepoor<br />
settings, including recently in the Ebola crisis, and the<br />
interview reinforces that global health is not always what we<br />
expect it to be. Professor Hilmers is also one of our Advisory<br />
Board members, a new initiative aimed at strengthening the<br />
academic standard and longevity of <strong>Vector</strong> Journal.<br />
There is a growing community of medical students who<br />
share a passion for global health. (Indeed, they are attending<br />
conferences around the world, including at Doctors for the<br />
Environment Australia (Belle Woody, p47) and with the IFMSA<br />
in Montenegro (p44)!) Unlike other medical specialities that<br />
have a clear career pathway, global health is a blank canvass.<br />
It is hard to define, and that lends a huge amount of potential<br />
– global health can be anything that you want it to be. There<br />
is “no limit” in that sense!<br />
I believe that the contents of this issue speak to the<br />
diversity of global health. Not only does it bring attention<br />
to some of the greatest challenges, it also celebrates the<br />
developments in research, collaboration and policies that<br />
pave the way towards new and creative solutions. We hope<br />
this issue engages you, inspires you, and challenges your<br />
ideas and assumptions about global health. I am incredibly<br />
grateful to the <strong>Vector</strong> Committee, to all of our authors and<br />
contributors, to the Advisory Board, AMSA Global Health and<br />
many other supporters.<br />
Dear Reader, let <strong>Vector</strong> be a platform for you to launch<br />
beyond the horizon into global health.<br />
Carrie Lee, <strong>Vector</strong> Editor-in-Chief <strong>2017</strong><br />
Correspondance: carie.lee@amsa.org.au<br />
1
Rise of Trump/Fall of Health<br />
[Commentary]<br />
Owen Burton<br />
Owen Burton holds degrees of Bachelor of Biomedical Science (Griffith University)<br />
and Masters of Orthoptics (University of Technology, Sydney)<br />
As Donald Trump took the stage declaring<br />
victory as the 45th President of the United<br />
States and the Leader of the Free World, I had<br />
a sudden chilling realisation. This man, who<br />
has spent his entire life ignoring or actively<br />
working against the dangers of climate change,<br />
progressive social policy and a centralised<br />
state control healthcare system, now sits at<br />
the head of the American government, which<br />
sets the trends in policy and action in the<br />
Western world.<br />
His often-repeated goal during campaigning<br />
was to “repeal and replace” Obamacare by<br />
relaxing legislation which prevents exploitation<br />
of the injured by private<br />
insurance interests, and<br />
removing funding for vital<br />
infrastructure in hospitals and<br />
speciality clinics, as well as<br />
sexual health and Planned<br />
Parenthood programmes.<br />
Although he has, so far, been<br />
unsuccessful in repealing<br />
Obamacare, he has not given up his crusade<br />
against basic healthcare provisions.<br />
Under Trump’s direct guidance, Tom Price,<br />
head of the Department of Health and Human<br />
Resources, continues to reduce requirements<br />
for insurance companies to provide essential<br />
benefits, and works towards completely<br />
dismantling systems related to women’s or<br />
sexual health. Such a removal of support and<br />
shift away from women is concerning, as it<br />
appears to indicate the return of deep-seated<br />
sexism within governmental institutions which<br />
sets an example for the wider society.<br />
These cuts will jeopardise the health<br />
of the world’s most at-risk individuals<br />
by removing access to education<br />
and preventative measures against<br />
sexually transmitted diseases, as well<br />
as all facets of maternal healthcare.<br />
While Trump has proven time and time<br />
again that he has little regard for females, this<br />
blatant attack seems like an extreme first step.<br />
People have been protesting the numerous<br />
unconstitutional and unethical executive<br />
orders streaming from the desk of the White<br />
House through large organised protests, rallies<br />
at offices of local governmental officials<br />
and online petitions. It is vital, however, that<br />
this momentum does not weaken: accepting<br />
this situation as the new ‘normal’ cannot be<br />
allowed to happen. Having to fight constantly<br />
is exhausting but essential. Without significant<br />
resistance, it is likely that Trump will be able<br />
push many of these bills through a Republicandominated<br />
congress and into<br />
law.<br />
Trump’s executive order to<br />
freeze funding and support for<br />
global aid serves to reinstate<br />
and expand Reagan’s 1984<br />
ban on United States (US)<br />
foreign aid. All $9.5 billion<br />
USD of American global health funding will<br />
be restricted from being available to any nongovernment<br />
organisations providing or even<br />
discussing abortion with patients.[1, 2] These<br />
cuts will jeopardise the health of the world’s<br />
most at-risk individuals by removing access to<br />
education and preventative measures against<br />
sexually transmitted diseases, as well as all<br />
facets of maternal healthcare. The World<br />
Health Organization estimated that a total of<br />
225 million women in developing countries<br />
were not using contraception, mainly due to<br />
lack of access and education.[3] With the<br />
implementation of this gag, it is expected that<br />
these numbers will rise significantly.<br />
2
Trump has made it clear that he is committed<br />
to the promises he made going into the<br />
election – promises which have the potential to<br />
jeopardise global health. The next step is likely<br />
to be severe cuts or the removal of foreign aid<br />
funding entirely, as Trump has expressed on<br />
Slashing America’s global aid<br />
support will only result in detriment for<br />
those people already suffering from<br />
the consequences of poor support<br />
for health services; a rise in disease,<br />
poverty and death are to be expected<br />
if this policy is to be implemented.<br />
multiple occasions that he has no intention of<br />
being “president to the world”. By internalising<br />
focus, Trump aims to disconnect America from<br />
the rest of the world – a process that has<br />
started with reduction and removal of aid and<br />
is predicted to continue with taxing of overseas<br />
goods.<br />
The impact this will have on global health<br />
programs is not to be underestimated. Slashing<br />
America’s global aid support will only result in<br />
detriment for those people already suffering<br />
from the consequences of poor support for<br />
health services; a rise in disease, poverty and<br />
death are to be expected if this policy is to be<br />
implemented.<br />
and taking a strong stand on healthcare and<br />
foreign aid, Australia could become a rally point<br />
for other nations – a model for them to work by<br />
and therefore improve the lives of millions of<br />
people who have already, and will be, affected<br />
by the rise of Trump.<br />
Acknowledgements<br />
None<br />
Conflict of Interest<br />
None declared<br />
Correspondence<br />
oburton101@gmail.com<br />
References<br />
1. Filipovic J. The Global Gag Rule: America’s Deadly<br />
Export. Foreign Policy. <strong>2017</strong> March; 20.<br />
2. Office of the Press Secretary, White House.<br />
White House. [Online].; <strong>2017</strong> [cited <strong>2017</strong> May 10.<br />
Available from: https://www.whitehouse.gov/the-pressoffice/<strong>2017</strong>/01/23/presidential-memorandum-regardingmexico-city-policy.<br />
3. Singh S, Darroch J, Ashford L. Adding It Up:<br />
The Costs and Benefits of Investing in Sexual and<br />
Reproductive Health 2014. Guttmacher Institute; 2014.<br />
Australia has an opportunity, and a<br />
responsibility here to intervene. As a country<br />
with the wealth and resources to help, we would<br />
be passively condoning Trump’s gag policy if<br />
we do not aim to lessen its blow on developing<br />
nations. By increasing our international aid<br />
and presence, as well as encouraging other<br />
countries to do so, we can hopefully avoid the<br />
rise of neoliberalist nationalism we have seen<br />
in America, and help prevent its consequences<br />
to global health.<br />
Most importantly, Australia needs to stand<br />
up against America on this issue. It is time for<br />
Australia to take the lead. By changing direction<br />
3
4
Anti-vaccination: Separating Fact<br />
from Fiction<br />
[Commentary]<br />
Elissa Zhang<br />
Elissa is a 4th year medical student at UNSW. She currently conducts research<br />
on parental attitudes towards vaccine policies and media portrayals of vaccine<br />
safety at the UNSW School of Public Health and Community Medicine.<br />
Vaccines are indubitably one of the great<br />
successes of public health, on par with clean<br />
water and basic sanitation. They have saved<br />
millions of lives, and even eradicated infectious<br />
diseases such as smallpox.[1]<br />
Yet, regardless of these achievements, the<br />
legitimacy and safety of vaccinations are still<br />
questioned. Earlier this year Australian One<br />
Nation Senator Pauline Hanson urged parents to<br />
take a non-existent “vaccine-reaction test”,[2]<br />
and United States (US) President Donald Trump<br />
called for a commission into vaccine safety.<br />
[3] Furthermore, the recent implementation<br />
of stricter childhood vaccination policies (No<br />
Reasons behind vaccination hesitancy<br />
For as long as vaccines have been around,<br />
there have been those who oppose them.<br />
Vaccine opposition began in early 1800s in<br />
Europe with the first vaccination mandates.<br />
Scientists, doctors, and members of the public<br />
questioned the scientific basis of vaccines,<br />
even citing that they would disturb with God’s<br />
“natural control over the balance between<br />
the blessed and the damned”.[5] The modern<br />
manifestation of vaccine objection is<br />
simply another iteration of this longstanding<br />
phenomenon..<br />
Jab No Pay; No Jab No Play) in Australia has<br />
raised contentious ethical issues regarding<br />
consent and balancing medical paternalism<br />
and parental autonomy in the provision of<br />
healthcare to children.[4]<br />
Ironically, the great success of vaccinations<br />
in dramatically reducing, and even eradicating<br />
disease is contributing to their own downfall.<br />
As diseases like measles and polio are no<br />
longer endemic in Australia, parents no longer<br />
directly face the harms of these highly virulent<br />
and contagious diseases. Consequently, they<br />
5
may perceive the risks from vaccinations to be<br />
greater than the likelihood of contracting the<br />
very diseases they prevent.[5]<br />
In fact, surveys of Australian parents show<br />
that the primary reason for vaccine hesitancy<br />
or objection is concerns about their safety[6]<br />
and a third of parents believe children are<br />
over-vaccinated. Newer vaccines, like the<br />
HPV vaccine, can be perceived to have<br />
a lower risk-benefit ratio, as they protect<br />
against diseases that are less prevalent or<br />
virulent. Older vaccines also face doubts, as<br />
the diseases they prevent are less common<br />
or even eliminated in the Australia, such as<br />
measles. Furthermore, concerns about adverse<br />
reactions to vaccination are growing. This could<br />
be attributed to the fact that such reactions<br />
are perceived to be more common than the<br />
diseases that they prevent.<br />
Common misconceptions regarding vaccines<br />
Rare but severe adverse reactions to<br />
some vaccinations attract great public<br />
interest, and give rise to misconceptions or<br />
over-estimations regarding their harms. For<br />
instance, the 1955 Cutter Incident in the USA<br />
involved administration of 380,000 doses of<br />
incompletely inactivated polio vaccinations to<br />
healthy children, which resulted in 40,000 cases<br />
of abortive polio (a minor form that does not<br />
involve the central nervous system), 51 cases<br />
of permanent paralysis and five deaths. It also<br />
started a polio epidemic, leaving even more<br />
people in the community affected.[7]<br />
This event severely undermined public<br />
confidence in the safety of vaccinations, even<br />
after it prompted the instigation much safer<br />
and stricter regulation of vaccines.[7] Incidents<br />
such as this undermine trust in vaccine safety,<br />
and these fears must be addressed in the<br />
community.<br />
Commonly, anti-vaxxers also claim that while<br />
they are not against vaccinations themselves,<br />
they oppose the adjuvants and preservatives<br />
that are potentially harmful, like thiomersal.<br />
However, studies have not been able to identify<br />
any harmful effects related to thiomersal, and<br />
even so, it was removed from all Australian<br />
childhood vaccines.[8]<br />
One of the most infamous controversies<br />
surrounding vaccine safety was Andrew<br />
Wakefield’s retracted 1998 paper that linked<br />
the Measles, Mumps and Rubella (MMR)<br />
vaccine to autism and bowel disease. His study<br />
was severely flawed, involving a sample of only<br />
12 children, and Wakefield was deregistered<br />
and discredited. In comparison, a Danish<br />
retrospective cohort study investigated over<br />
500,000 children who received the MMR vaccine<br />
and proved that there was no association<br />
between the vaccine and autism.[9] Despite<br />
this, many of the general public still believe in<br />
the association between the MMR vaccine and<br />
autism as a consequence of Wakefield’s study.<br />
Vaccine objection in the context of Australian<br />
vaccination policies<br />
As of January 2016, the nationwide legislation<br />
called “No Jab No Pay” has been put into<br />
effect, removing conscientious objection from<br />
exemption criteria to immunisation requirements<br />
for Centrelink childcare payments worth up to<br />
$19,000. A press release by then Prime Minister<br />
Tony Abbott and Health Minister Scott Morrison<br />
stated that “the choice made by families not<br />
to immunise their children is not supported by<br />
public policy or medical research nor should<br />
such action be supported by taxpayers in the<br />
form of child care payments”.[10]<br />
In contrast, public health experts believe that<br />
this policy is may be misplaced in its aims to<br />
reduce conscientious objection to vaccination,<br />
rather than addressing the more prominent<br />
barriers of access to services, logistical<br />
issues, and missed vaccination opportunities.<br />
[<strong>11</strong>] A policy such as this could also threaten<br />
the validity of a patient’s informed consent,<br />
which is outlined in the Australian Immunisation<br />
Handbook as being “given voluntarily in the<br />
absence of undue pressure, coercion or<br />
manipulation”.[12] This has generated a fresh<br />
6
debate into the ethics of mandating vaccines<br />
through paternalistic policy.<br />
Conflict of Interest<br />
None declared<br />
Statistics released in July 2016 show that<br />
following the implementation of this policy,<br />
148,000 incompletely vaccinated children had<br />
caught up, including 5,738 children of parents<br />
with previous conscientious objections.[13]<br />
Implications as medical professionals<br />
Public attitudes towards<br />
vaccinations are complex, as<br />
they are affected by a wide<br />
range of sources, including the<br />
media, personal experiences,<br />
and health providers. A<br />
variety of strategies should<br />
be implemented to influence<br />
such attitudes. For instance,<br />
willingness to vaccinate could<br />
be encouraged by focusing on improving<br />
awareness of the risks of vaccine preventable<br />
diseases, rather than discrediting or refuting<br />
myths about vaccine dangers. An intervention<br />
based on this strategy showed that higher risk<br />
perception of diseases resulted in an increased<br />
willingness to vaccinate.[14] It was also shown<br />
that rates of conscientious objection were<br />
reduced in areas with more administrative<br />
barriers to obtaining one.<br />
As future health professionals, we need<br />
to develop skills to practise evidence-based<br />
medicine. We need to be able to formulate our<br />
opinions based on verified facts, before helping<br />
parents to make informed decisions about<br />
vaccinations. We too can also be influenced by<br />
the vast amount of facts and misinformation<br />
disseminated about vaccinations in the media.<br />
Thus, it is our responsibility to stay up-to-date<br />
with the latest literature and separate fact from<br />
fiction, in order to provide the best care for our<br />
patients.<br />
Acknowledgements<br />
Supervisor Prof. Raina MacIntyre, UNSW<br />
r.macintyre@unsw.edu.au<br />
Correspondence<br />
elissa.j.zhang@gmail.com<br />
References<br />
As of January 2016, the<br />
nationwide legislation called “No<br />
Jab No Pay” has been put into<br />
effect, removing conscientious<br />
objection from exemption criteria<br />
to immunisation requirements for<br />
Centrelink childcare payments<br />
worth up to $19,000.<br />
1. Greenwood B. The contribution of vaccination to<br />
global health: past, present and future. Philos Trans<br />
R Soc Lond B Biol Sci. 2014;369(1645):20130433.<br />
Available from: https://www.ncbi.nlm.nih.gov/pmc/<br />
articles/PMC4024226/ DOI: 10.1098/<br />
rstb.2013.0433<br />
2. Australian Broadcasting<br />
Corporation. Pauline Hanson joins<br />
Insiders [Internet]. Sydney NSW:<br />
Australian Broadcasting Corporation;<br />
<strong>2017</strong> [cited <strong>2017</strong> May 29]. Available<br />
from: http://www.abc.net.au/insiders/<br />
content/2016/s4630647.htm<br />
3. Wadman M. Robert F. Kenndey Jr.<br />
says a ‘vaccine safety’ commission<br />
is still in the works. Science [Internet].<br />
<strong>2017</strong> Feb [cited <strong>2017</strong> May 29]. Available from: http://<br />
www.sciencemag.org/news/<strong>2017</strong>/02/robert-f-kennedy-jrsays-vaccine-safety-commission-still-works<br />
4. National Centre for Immunisation Research &<br />
Surveillance [Internet]. Westmead NSW: NCIRS; 2016. No<br />
jab no play, no jab no pay policies; 2016 [cited <strong>2017</strong> May<br />
29]; [all screens]. Available from: http://www.ncirs.edu.<br />
au/consumer-resources/no-jab-no-play-no-jab-no-paypolicies/<br />
5. Bond L, Nolan T. Making sense of perceptions of<br />
risk of diseases and vaccinations: a qualitative study<br />
combining models of health beliefs, decision-making and<br />
risk perception. BMC Public Health. 20<strong>11</strong>;<strong>11</strong>:943.<br />
6. Rhodes A. Vaccination: perspectives of Australian<br />
parents [Internet]. Melbourne VIC: The Royal Children’s<br />
Hospital Melbourne; <strong>2017</strong> [cited <strong>2017</strong> May 29]. 6 p.<br />
Available from: https://www.childhealthpoll.org.au/wpcontent/uploads/2015/10/ACHP-Poll6_Detailed-report_<br />
FINAL.pdf<br />
7. Offit PA. The Cutter incident, 50 years later. N Engl J<br />
Med. 2005;352(14):14<strong>11</strong>-2.<br />
8. National Centre for Immunisation Research &<br />
Surveillance. Thiomersal FactSheet [Internet]. Westmead<br />
NSW: NCIRS; 2009 [cited <strong>2017</strong> May 29]. 5 p. Available<br />
from: http://www.ncirs.edu.au/assets/provider_resources/<br />
fact-sheets/thiomersal-fact-sheet.pdf<br />
9. Madsen KM, Hviid A, Vestergaard M, Schendel D,<br />
Wohlfahrt J, Thorsen P, et al. A population-based study of<br />
measles, mumps, and rubella vaccination and autism. N<br />
Engl J Med. 2002;347(19):1477-82.<br />
10. Abbott T, Morrison S. No jab – no play and no pay<br />
for child care [Internet]. Canberra ACT: Parliament of<br />
Australia; 2015. 2 p. Available from: http://parlinfo.aph.<br />
gov.au/parlInfo/search/display/display.<br />
7
Climate Change and <strong>Vector</strong>-Borne<br />
Disease in Kiribati<br />
[Commentary]<br />
Erica Longhurst<br />
Erica Longhurst is a third year medical student at the University of New South Wales, passionate<br />
about environmental health, and who is a big fan of the great outdoors! Her loves are travelling<br />
and learning about people. She is studying in Griffith NSW this year, on clinical placement with my<br />
uni. She’s also super passionate about everything that’s in this edition of <strong>Vector</strong>!<br />
In February 2016, I went on a New Colombo<br />
Plan-sponsored climate change research trip<br />
to Kiribati, a nation of low-lying atolls in the<br />
Pacific Ocean. The islands of Kiribati are on<br />
the equator halfway between Australia and<br />
Hawaii. One of the most important things<br />
that I learnt was how being sustainable is<br />
not that difficult at all, and that the people of<br />
Kiribati are absolute professionals at living in<br />
harmony with their environment. We travelled<br />
to Kiribati to research the social, economic<br />
and environmental effects of climate change.<br />
However, this trip also taught us much about<br />
ourselves and the society that we live in,<br />
Australia. It was an opportunity to see how<br />
those who contribute nothing to global pollution<br />
are suffering from the effects of climate<br />
change.<br />
There is a large focus in the international<br />
community on the environmental implications of<br />
climate change. Whilst this is highly significant,<br />
the impact of climate change on the health of<br />
local communities also needs to be brought to<br />
attention. When I think of this impact on local<br />
people, Kiribati is the first place that comes<br />
to mind. Climate change is responsible for<br />
an array of health issues, primarily the rise<br />
in communicable diseases as a result of the<br />
climate change-induced El Nino Southern<br />
Oscillation (ENSO) effect.[1] <strong>Vector</strong>-borne<br />
diseases such as malaria and dengue fever<br />
are particularly relevant. Increase in average<br />
global temperatures due to raised levels of<br />
greenhouse gases essentially accommodate<br />
these epidemics.[2] Without firstly responding<br />
to the health issues that these populations<br />
face as a result of climate change, many of the<br />
other issues cannot be addressed. In Kiribati,<br />
it is crucial to take measures to avoid future<br />
health consequences such as communicable<br />
diseases, as these people are so susceptible<br />
to the effects of climate change.<br />
8
The people of Kiribati are said to be the<br />
most vulnerable to the implications of climate<br />
change because of the close proximity of<br />
the inhabitants to the coastal regions of their<br />
islands. The ENSO effect is characterised by<br />
irregular warming of the eastern equatorial<br />
Pacific Ocean, and is responsible for raising<br />
average temperatures and inducing higher<br />
rainfall in the Asia Pacific region. Kiribati itself<br />
is only two metres above sea level, and so<br />
faces challenges in this domain. This is a very<br />
significant issue for cooler regions where there<br />
is limited experience or resistance to vectorborne<br />
infectious diseases.[3]<br />
<strong>Vector</strong>-borne diseases have many factors at<br />
play, such as host resistance, the environment,<br />
urbanisation and the pathogens themselves.<br />
The severity and prevalence of vector-borne<br />
diseases depends heavily on the climate, and<br />
thus directly correlates with the ENSO climate<br />
cycles. Temperature, rainfall and humidity<br />
are especially important concerns for vectorborne<br />
diseases.[4] According to the ‘The Sting<br />
of Climate Change’ report, ‘warmer conditions<br />
allow the mosquitoes and the malaria parasite<br />
itself to develop and grow more quickly, while<br />
wetter conditions let mosquitoes live longer and<br />
breed more prolifically’.[5] There is an overall<br />
increase in the potential for disease transmission<br />
due to the change in the ecology of vectors. This<br />
is characterised by quicker mosquito breeding<br />
cycle (thus, higher concentrations), increased<br />
biting rates, and shortened pathogen incubation<br />
periods.[6] If rainfall is excessive, pooled water<br />
can form, which creates breeding sites for<br />
mosquito larvae. There are many factors that<br />
operate in these scenarios, and so there is no<br />
one direct link between climate and mosquito<br />
populations.<br />
For both dengue and malaria, some of the<br />
most effective control measures to reduce<br />
the burden are long-lasting insecticidal bednets,<br />
indoor residual spraying with insecticides,<br />
seasonal malaria chemo-prevention,<br />
intermittent preventive treatment for infants and<br />
during pregnancy, prompt diagnostic testing,<br />
and treatment of confirmed cases with effective<br />
anti-malarial medicines.[7] These measures<br />
have dramatically lowered malaria disease<br />
burden in many Pacific Islander settings over<br />
the years. Thus, prevention is limited to vectorcontrol<br />
measures, which are very difficult to<br />
monitor.<br />
Visiting Kiribati gave me insight into the reality<br />
of climate change and its current impacts<br />
on health. It is clear that there is a distinct<br />
connection between climate change and<br />
vector-borne diseases. This poses particular<br />
challenges for developing nations where<br />
consequences of climate change are most<br />
pronounced. My experiences in Kiribati showed<br />
us raw, personal stories, and we strongly believe<br />
it is imperative to take action immediately.<br />
Acknowledgements<br />
None<br />
Conflict of Interest<br />
None declared<br />
Correspondence<br />
e.longhurst1012@gmail.com<br />
References<br />
1. Reiter P. Climate change and mosquito-borne<br />
disease. Environmental health perspectives; 20<strong>11</strong>. 141 p.<br />
121<br />
2. Ebi KL, Lewis ND, Corvalan C. Climate variability<br />
and change and their potential health effects in small<br />
island states: information for adaptation planning in the<br />
health sector. Environmental Health Perspectives; 2006,<br />
1957-1963 p.<br />
3. Haines A, McMichael AJ, Epstein PR. Environment<br />
and health: 2. Global climate change and health.<br />
Canadian Medical Association Journal; 2006, 729-734 p.<br />
4. Woodruff R, Whetton P, Hennessy K, Nicholls N,<br />
Hales S, Woodward A, Kjellstrom, T, Human health and<br />
climate change in Oceania: a risk assessment. Canberra:<br />
Commonwealth Department of Health and Ageing; 2003.<br />
5. Perry M. Malaria and dengue the sting in<br />
climate change. Reuters; 2008. Available from:<br />
http://www.reuters.com/article/us-climate-diseaseidUSTRE4AJ2RQ2008<strong>11</strong>20<br />
6. Bezirtzoglou C, Dekas K, Charvalos E. Climate<br />
changes, environment and infection: Facts, scenarios<br />
and growing awareness from the public health community<br />
within Europe. Anaerobe; 20<strong>11</strong>, 2 p.<br />
7. Githeko AK, Lindsay SW, Confalonieri UE, Patz JA.<br />
Climate change and vector-borne diseases: a regional<br />
analysis. Bulletin of the World Health Organization; 2000.<br />
<strong>11</strong>36-<strong>11</strong>47 p.<br />
9
REFUGEE AND ASYLUM SEEKER UPDATE<br />
MARCH <strong>2017</strong><br />
I MPORTANT UPDATE<br />
• The Immigration Department reduced the deadline asylum seekers must apply for protection visas from 1 year to<br />
60 days. 1<br />
• Affects thousands of asylum seekers. 1<br />
• Those who don’t make the deadline may have their claim overturned giving them no right to work or medicare 1<br />
• These applications are up to 60 pages long with complex medical terms in English, requiring legal advice for<br />
completion, overloading already saturated legal services 1<br />
• IHMS, contracted to provide primary health care +<br />
mental health services on Manus Island and Nauru has<br />
been found to be not registered by the PNG<br />
medical board. 2<br />
- Therefore, 103 staff working at the centre<br />
have been employed illegally. 2<br />
• Recent Dengue outbreak on Nauru (late Feb). 3<br />
Infecting 70 people on Nauru including 10 refugee and<br />
asylum seekers.<br />
- Unconfirmed reports up to 8 asylum seeker<br />
medevaced to Australia mainland for<br />
treatment. 3<br />
• Young male asylum seeker on Manus Island flown to<br />
Australia for treatment 9th Feb following long<br />
standing series of doctors referring the man to get a<br />
pacemaker since August 2016. 4<br />
- The man collapsed Feb 1 and was finally<br />
transferred. This is another example, just like<br />
that of Faysal Ahmed, of complaints being<br />
ignored for a long time 4<br />
• Amnesty International released a<br />
report labelling Australia’s offshore detention<br />
policy as inhuman and abusive 5<br />
o<br />
o<br />
Highlights governments refusal to<br />
honour offer from NZ to resettle 150<br />
refugees and asylum seekers 5<br />
Treatment of these people involves<br />
systematic neglect and cruelty<br />
designed to inflict suffering 5<br />
1<br />
Hart, C. (<strong>2017</strong>, February 26). Asylum seekers’ applications doomed to fail after visa deadline changes, says refugee support service. ABC news. Retrieved from<br />
www.abc.net.au/news/<strong>2017</strong>-02-26/asylum-seekers-issued-with-new-deadline-for-visa-applications/8304766<br />
2<br />
Armstrong, K. (<strong>2017</strong>, March 3). Manus Island health provider ‘operating illegally for three years’: report. SBS news. Retrieved from<br />
http://www.sbs.com.au/news/article/<strong>2017</strong>/03/02/manus-island-health-provider-operating-illegally-three-years-report<br />
3<br />
Riman, I. (<strong>2017</strong>, February 28). A physical attack and a Dengue-fever outbreak cause fear among Nauru detainees. SBS news. Retrieved from<br />
http://www.sbs.com.au/yourlanguage/arabic/en/article/<strong>2017</strong>/02/28/physical-attack-and-dengue-fever-outbreak-cause-fear-among-nauru-detainees<br />
4<br />
Booth, A. (<strong>2017</strong>, February 12). Manus Island asylum seeker with cardiac condition flown to Australia. SBS news. Retrieved from<br />
http://www.sbs.com.au/news/article/<strong>2017</strong>/02/17/manus-island-asylum-seeker-cardiac-condition-flown-australia<br />
5<br />
Jama, H. (<strong>2017</strong>, February 23). Amnesty critical of Australia’s asylum seeker policy. SBS news. Retrieved from<br />
http://www.sbs.com.au/yourlanguage/somali/en/content/amnesty-critical-australias-asylum-seeker-policy<br />
6<br />
Feng, L. (<strong>2017</strong>, March 8). Hungary toughens laws on asylum seekers again. SBS news. Retrieved from:<br />
http://www.sbs.com.au/news/article/<strong>2017</strong>/03/08/hungary-toughens-laws-asylum-seekers-again<br />
7<br />
Picture: Deacon, L. (<strong>2017</strong>, February 10). Migrants entering Hungary to be detained in shipping containers on border. Retrieved from<br />
http://www.breitbart.com/london/<strong>2017</strong>/02/10/migrants-entering-hungary-detained-shipping-containers-border/<br />
10
Humanity Lost?<br />
[Feature article]<br />
This article was originally published in the Doctus Project (February <strong>2017</strong>)<br />
Patrick Walker<br />
Patrick is a medical student at Monash University, and the Editor in Chief of non-profit health<br />
journalism organisation the Doctus Project. He is also the Global Health Policy Officer for the<br />
Australian Medical Students’ Association, attended the World Health Assembly recently in<br />
Geneva, and late last year completed a policy internship at the Grattan Institute. Health-wise, his<br />
interests lie mainly in global health and health policy, and outside of the classroom (or hospital)<br />
he’s either reading a novel, writing about something new, or sitting at the piano crunching out a<br />
tune or two. This year he is completing a Bachelor of Medical Science (Hons) with the Centre<br />
for International Child Health and the Royal Children’s Hospital, looking at oxygen systems and<br />
provision of care in low-resource settings. Looking forward, perhaps this line of work might form the<br />
basis of a career, though there’s plenty of time for that to change.<br />
‘We started the revolution holding roses.<br />
Hoping for support from the international<br />
community. Years passed. The roses turned<br />
into guns. But the hope for support continues.<br />
Still, neither roses nor hope helped.’<br />
- Abdulazez Dukhan, Syrian refugee<br />
Trump, with a simple and powerful message:<br />
he wanted to be heard. He wasn’t asking for an<br />
end to the conflict in his ‘beloved Syria’. He was<br />
simply asking for the West – and its perceived<br />
leader, Trump – to acknowledge the human<br />
side of the war. He was asking for humanity in<br />
the West’s response to his story.<br />
Abdulazez Dukhan is one of 4.5 million<br />
people who have fled Syria since the current<br />
conflict began in 20<strong>11</strong>. He is one of the<br />
countless people whose lives have been<br />
destroyed beyond recognition; one of the<br />
countless people forced to leave everything<br />
behind, in search of a safe place to live.<br />
In January, Abdulazez penned a moving<br />
letter to the new American president, Donald<br />
‘Your words matter for us,’ he writes. ‘You<br />
might be able to change our future ‘Dear future<br />
president, we hope that someone can hear our<br />
words. We hope that you do.’<br />
Sadly, his plea has largely fallen on deaf<br />
ears.<br />
<strong>11</strong>
Just two weeks after Dukhan’s letter was<br />
published by Al Jazeera, Trump signed an<br />
executive order banning people from seven<br />
predominantly Muslim countries, including Syria,<br />
from entering the United States (US) for 90<br />
days. The order also placed a blanket ban on<br />
all refugees for 120 days, and Syrian refugees<br />
indefinitely.<br />
of the highest number of forcibly displaced<br />
persons since World War II and unfathomable<br />
atrocities occurring throughout the Middle<br />
East, northern Africa and many other parts of<br />
the world. For many people – most notably the<br />
young and highly educated – these events were<br />
taken to be a clear marker of racism and an<br />
unwillingness to accept difference.<br />
But they were also each the result of a free,<br />
democratic vote. They reflected the view of the<br />
majority. Further, to pass them off as simply<br />
racist, or a blip in the global political agenda,<br />
would be naive and counter-productive.<br />
The ban is currently suspended thanks to a<br />
federal judge temporarily blocking the executive<br />
order, but Trump’s message can be heard loud<br />
and clear. His response to the Syrian War and<br />
the current refugee crisis is to look the other<br />
way; to close the doors to those most in need<br />
of help.<br />
When I first watched the video of Abdulazez<br />
Dukhan’s letter to Trump, I was brought to tears.<br />
Dukhan’s poignant words brought the horrors he<br />
had endured suddenly to life. For a moment, I felt<br />
I was able to gain a tiny glimpse into the harsh<br />
reality of life for the millions of Syrians living in<br />
a conflict zone.<br />
Perhaps this should not come as too much of<br />
a surprise. Trump’s protectionism and stance on<br />
immigration are neither novel nor unexpected.<br />
Rather, they can be viewed as a symptom of<br />
a broader rise in nationalism, in response to a<br />
global refugee crisis that continues to worsen.<br />
2016 was a year of many things, but<br />
prominent among them were nationalism,<br />
division, and an increasingly powerful global<br />
Right. Brexit and the rise of an assortment of<br />
right-wing parties defined politics in Europe.<br />
Across the Atlantic, Trump was elected to the<br />
Oval Office on a fervent anti-establishment and<br />
pro-US, protectionist agenda. Back home in<br />
Australia, we saw the re-emergence of Pauline<br />
Hanson and her far-right, anti-immigration One<br />
Nation party.<br />
All these events occurred in the context<br />
This visceral response is by no means<br />
unusual or unexpected. It is the same as the<br />
West’s response to the ‘boy in the ambulance’<br />
12
(five year-old Omran Daqneesh, injured by a<br />
blast in Aleppo in August last year) or to horrific<br />
images of the dead body of three year-old Aylan<br />
Kurdi washed up on a Turkish shore.<br />
It is human nature to feel outrage at injustice<br />
when it is put in front of us. It is not, however,<br />
human nature to react the same way to atrocities<br />
removed from one’s own existence and social<br />
or political sphere. Without these images and<br />
videos that become – for better or for worse –<br />
perverse icons of death and destruction, it is all<br />
too easy for us to simply turn away.<br />
This tendency means we often lose sight of<br />
the human side of tragic events to which we find<br />
ourselves unable to relate. This is exactly what<br />
we have seen in our politicians and our leaders.<br />
And it is in many cases exactly what we have<br />
seen in ourselves. Instead of compassion and<br />
unity, we have responded to horrors such as<br />
those going on in Syria with disaffection and, at<br />
times, apathy. Instead of reaching out to those in<br />
need, we have instead turned inwards, creating<br />
division and, on the other end, despair.<br />
The unprecedented political phenomenon of<br />
2016 is perhaps best encapsulated by social<br />
psychologist Jonathan Haidt. In a remarkably<br />
insightful and prescient essay entitled ‘When<br />
and why nationalism beats globalism’, Haidt<br />
unpacks the rise in nationalism we have seen<br />
in the past year, and tries to answer the simple<br />
question: ‘What on earth is going on in the<br />
Western democracies?’<br />
By resisting change and immigration, Haidt<br />
argues that nationalists are not, as many<br />
believe, being selfish or somehow morally<br />
inferior to those embracing change. Far from<br />
it. Rather than inciting discrimination, he writes,<br />
they are working to preserve their nation and<br />
culture. The division between nations that can<br />
arise from this attitude is a by-product, rather<br />
than an intended consequence.<br />
The way to tackle this, then, is not to label<br />
nationalist or anti-immigration sentiment as<br />
‘racism pure and simple’. As Haidt notes, ‘If we<br />
want to understand the recent rise of right-wing<br />
populist movements, then ‘racism’ can’t be the<br />
stopping point; it must be the beginning of the<br />
inquiry.’<br />
Rather than labelling the majorities who<br />
voted for Brexit, Trump or Hanson as racist or<br />
ignorant, we as a society need to understand<br />
their motives, and why they have turned to the<br />
Right for answers. We need to understand why<br />
so many of us are seemingly willing to turn a<br />
blind eye to horrors occurring outside of our<br />
immediate vicinity. We need to understand why<br />
we have lost compassion in our response to the<br />
plight of Syria.<br />
<strong>2017</strong> can be different from the division we<br />
saw in 2016, but only if we resist the urge to vilify<br />
the ‘Other’, regardless of who that ‘Other’ is – a<br />
Muslim refugee, a status quo conservative, a<br />
member of the educated elite, or a right-wing<br />
authoritarian.<br />
Instead, creating a space of mutual<br />
understanding between people of differing<br />
opinions may help bridge the gap that has<br />
formed between the Right and the Left; the<br />
Nationalists and the Globalists; the Educated<br />
and the Uneducated; the East and the West.<br />
By doing this, we will start on the path towards<br />
finding an adequate response to Dukhan’s<br />
plea to Trump. And, somewhere along the way,<br />
maybe we will find that humanity that seems to<br />
have gone missing.<br />
Photo credit<br />
Abdulazez Dukhan<br />
Acknowledgements<br />
Doctus Project<br />
Conflict of Interest<br />
None declared<br />
Correspondence<br />
patrick.walker@amsa.org.au<br />
13
Redefining Women’s Health:<br />
A Noncommunicable Diseases Perspective<br />
[Feature Article]<br />
Charlotte O’Leary<br />
Charlotte has completed 4 years of medical school at Monash University. She is currently undertaking<br />
a Bachelor of Medical Science (Honours) at the Uehiro Centre for Practical Ethics at the University of<br />
Oxford. Charlotte undertook a 3-month internship at the World Health Organization in early <strong>2017</strong> in the<br />
Global Coordination Mechanism for the prevention and control of noncommunicable diseases (NCDs).<br />
Noncommunicable diseases (NCDs) –<br />
mainly cardiovascular diseases, cancers,<br />
chronic respiratory diseases and diabetes –<br />
represent a major challenge for sustainable<br />
development in the twenty-first century. In 2015,<br />
NCDs were responsible for 39.5 million (70%)<br />
of the world’s deaths, with more than 40% (16<br />
million) dying prematurely, or before the age of<br />
70.[1] NCDs affect people of all ages in high,<br />
middle and low-income countries. In particular,<br />
women and girls face unique challenges in<br />
the growing NCD epidemic<br />
due to pervasive gender<br />
inequality, disempowerment and<br />
discrimination. Without specific<br />
attention to the needs of women<br />
and adolescent girls, the impact<br />
of NCDs threatens to unravel the<br />
fragile health gains made over<br />
the past decades and undermine future efforts<br />
to ensure gender equity and healthy lives for all.<br />
The problem<br />
Gender inequality and NCDs<br />
NCDs have been the<br />
leading causes of death<br />
among women globally for the<br />
past three decades, and now,<br />
NCDs account for nearly 65%<br />
of female deaths worldwide.<br />
Nearly two thirds of illiterate people in the<br />
world are women, and this ratio has remained<br />
unchanged for two decades.[2] Consequently,<br />
women have had fewer opportunities to improve<br />
their health literacy and equip themselves with<br />
transferable skills that will enable them to be<br />
advocates for their own health.<br />
Women face unique challenges accessing<br />
healthcare due to their lower socioeconomic,<br />
political and legal status compared<br />
to men. The critical importance of<br />
prevention and early diagnosis of<br />
NCDs requires regular contact with<br />
the healthcare system. In some<br />
cultures, the health of a woman<br />
is often seen as secondary to the<br />
health of a man, and she may be<br />
denied access to healthcare when resources<br />
are limited. Even when given the choice,<br />
women are more likely than men to invest their<br />
money in the health of their children and other<br />
family members, rather than prioritising their<br />
own health.<br />
NCDs have been the leading causes of<br />
death among women globally for the past three<br />
decades, and now, NCDs account for nearly<br />
65% of female deaths worldwide. Pervasive<br />
gender inequality particularly affects the health<br />
of women and girls, influencing their ability to<br />
improve their health literacy, access healthcare<br />
services, achieve economic empowerment<br />
and financial security and live with NCDs free<br />
from stigma and discrimination.<br />
Many women may experience financial<br />
vulnerability due to high out-of-pocket<br />
healthcare costs. Lower access to formal paid<br />
employment may deny women the social and<br />
financial securities required to insure them<br />
against poor health.<br />
Additionally, women are too frequently<br />
viewed as commodities, and women living<br />
with a chronic disease may face alienation<br />
14
and discrimination. This is often due to the<br />
emphasis in certain social or cultural settings<br />
on a woman’s suitability for marriage and<br />
childbearing, which may be affected by chronic<br />
diseases.<br />
The caring burden<br />
Beyond their personal experiences with<br />
NCDs, women are indirectly affected by the<br />
increase in the burden of chronic diseases due<br />
to their traditional role as carers in families and<br />
communities. In a survey of 10,000 women from<br />
around the world, half the women were caring<br />
for a family member with an NCD, with one in five<br />
realising their own economic opportunities were<br />
diminished as a result.[3] Another study from the<br />
United States revealed that women make 80%<br />
of the health care decisions for their families,<br />
yet often go without health care coverage<br />
themselves.[4] Caregiving responsibilities can<br />
threaten or disrupt the education of adolescent<br />
girls, and often impacts women in their most<br />
productive years. Paid work decreases<br />
because of the burden of caring for people<br />
living with NCDs and reduces the economic<br />
contribution of women. This loss of productivity<br />
is felt by the whole society. The large amount of<br />
unpaid work undertaken by women in the family<br />
and community at all levels of society is highly<br />
under-appreciated.<br />
Vulnerability to NCD risk factors<br />
Women are uniquely vulnerable to the four<br />
major risk factors for NCDs, namely physical<br />
inactivity, poor nutrition, tobacco use and<br />
excessive alcohol intake. Improved social<br />
status and economic empowerment has<br />
contributed to an alarming increase in cigarette<br />
smoking amongst women and girls. The World<br />
Health Organization (WHO) estimates that the<br />
proportion of female smokers will rise from 12%<br />
in 2010 to 20% in 2025. Deaths attributable<br />
to tobacco use amongst women are also<br />
projected to increase from 1.5 to 2.5 million from<br />
2004 to 2030.[5] Women’s increasing social and<br />
economic status, especially in low and middleincome<br />
countries, has made them a prime target<br />
for the tobacco industry. This is especially true<br />
in Asia where regulation of tobacco advertising<br />
is lacking. Aside from the immoral promotion of<br />
health-harming products, the objectification of<br />
women is entrenched in tobacco advertising.<br />
Women’s bodies are exploited for the sale of<br />
cigarettes to men, whilst simultaneously and<br />
paradoxically, a message of health and beauty<br />
through tobacco consumption is conveyed to<br />
women and girls.[5]<br />
A similar trend is seen in alcohol consumption,<br />
with female alcohol consumption now rivalling<br />
male consumption, closing a historic divide.<br />
[6] Women and girls around the world are less<br />
likely to be physically active than boys and men<br />
due to sociocultural, economic and physical<br />
limitations imposed on them. In many cultures,<br />
women are largely responsible for food<br />
preparation. As a consequence, women often<br />
eat least and last in the family, compromising<br />
their nutrition. Additionally, inhalation of indoor<br />
cooking fuels is a well-known risk factor for<br />
chronic respiratory disorders, and this risk is<br />
borne disproportionately by women.[7] The list<br />
goes on.<br />
The way forward<br />
So how might we move forward at this<br />
critical time to ensure that we are effectively<br />
addressing the unique needs of women in<br />
the NCD epidemic? This problem is evidently<br />
complex and multifaceted. Presented here are<br />
some possible approaches, to firstly broaden<br />
our understanding of women’s health to include<br />
NCDs, and secondly to ensure that women are<br />
empowered and engaged in their own health.<br />
Defining women’s health<br />
One important step forward is to adopt a<br />
broader and more holistic definition of women’s<br />
health. Historically, the field of women’s<br />
health has focused on reproductive health,<br />
and consequently, considerable gains have<br />
been made in reducing maternal and newborn<br />
mortality and morbidity. While these gains are<br />
positive and important, it is equally important<br />
that the definition of women’s health not be<br />
confined to reproductive health. As Norton et al.<br />
15
posit in Women’s Health: A New Global Agenda,<br />
the currently narrow approach to women’s<br />
health firstly limits opportunities to effectively<br />
improve the health of the maximum number of<br />
women, and secondly, discriminates against<br />
women who do not have children.[8]<br />
In recent years, many international advocacy<br />
efforts have thus been made to expand this<br />
definition, and encompass a more holistic view<br />
of the health challenges faced by women. Such<br />
focus areas include, but are not limited to: the<br />
burden of NCDs in women, including mental<br />
health; the caring roles of women; and sexual<br />
and interpersonal violence. Additionally, the<br />
health of women must be considered across<br />
the whole life course. A reproductive focus<br />
risks excluding pre-adolescent girls<br />
and older women, all of whom face<br />
unique challenges in navigating<br />
their health in a climate of gender<br />
inequity. Indeed, women who have<br />
been through menopause have<br />
substantially increased risk of<br />
NCDs. Thus a focus on older women<br />
should be an integral of a life course<br />
approach to women’s health.<br />
Integrating NCDs into other health programs<br />
There are great opportunities to capitalise on<br />
existing healthcare services to better address<br />
the needs of women in the NCD epidemic. There<br />
is enormous opportunity to expand existing<br />
reproductive, communicable disease (such<br />
as HIV and tuberculosis) and sexual health<br />
services to incorporate NCDs. In particular,<br />
maternal and reproductive healthcare services<br />
are targeted at women, allowing healthcare<br />
to be delivered in an environment that is<br />
acceptable to, and accessible by, women and<br />
adolescent girls. Given the unique challenges<br />
faced by women in the NCD epidemic, these<br />
existing services can be broadened to include<br />
health promotion activities around NCD risk<br />
factors, early diagnosis and screening services<br />
(including breast and cervical cancer screening)<br />
and referral and treatment services. This will<br />
ensure that women are empowered to improve<br />
the health of themselves, their families and<br />
The impact of educating<br />
women has multigenerational<br />
effects due to their central<br />
position in the community, so<br />
improving women’s engagement<br />
with health promotion is a high<br />
yield intervention.<br />
communities. One such approach might be<br />
to follow up women with gestational diabetes<br />
after birth and to provide screening checks and<br />
education around good nutrition for mothers<br />
and children in order to prevent the development<br />
of diabetes. There is growing evidence for the<br />
feasibility and effectiveness of health system<br />
integration to prevent and control NCDs. [9,10]<br />
Women in medical research<br />
There is scope for the broader scientific and<br />
research community to ensure that women are<br />
equally represented in medical research. It is<br />
increasingly apparent that NCDs do not affect<br />
men and women equally. Women who smoke<br />
have a 25% greater relative risk of ischaemic<br />
heart disease than men who<br />
smoke.[<strong>11</strong>] Women suffer<br />
worse cardiovascular disease<br />
as a consequence of type 2<br />
diabetes than men,[12] and<br />
women with type 1 diabetes<br />
have a roughly 40% greater risk<br />
of all-cause mortality than men.<br />
[13] However, taking a focused<br />
biomedical approach is not<br />
sufficient to address the burden of NCDs in<br />
women. Medical research must also consider<br />
the social and cultural effects of gender<br />
inequity in order to fully appreciate the health<br />
outcomes of women with NCDs. Increasing<br />
attention to gender-disaggregated of research<br />
data has been recognised in the Sustainable<br />
Development Goals as an important tool for<br />
discovering these important gender disparities<br />
in illness.[14]<br />
Engaging women at every level<br />
Lastly, increasing female participation in<br />
decision-making will ensure the challenges<br />
faced by women are reflected in policies<br />
for health and sustainable development.<br />
Participation happens at every level. In local<br />
communities, women are attuned to the needs of<br />
other people, and as evident above, make many<br />
of the health related decisions in the community.<br />
There is a huge opportunity to harness their<br />
strength and knowledge to be a driving force<br />
16
for the prevention of NCDs. The impact of<br />
educating women has multigenerational effects<br />
due to their central position in the community,<br />
so improving women’s engagement with health<br />
promotion is a high yield intervention. There must<br />
be a concerted global effort to remove barriers<br />
to female participation in politics and high-level<br />
decision-making. Until this is achieved, it will<br />
be challenging to ensure that the multifaceted<br />
effects of gender inequity are accounted for in<br />
national and international policy.<br />
Conclusion<br />
Noncommunicable diseases are one of the<br />
biggest threats to health in an increasingly<br />
globalised world. Addressing gender inequity<br />
will be a necessary component of the solution.<br />
The health of women concerns everyone, and is<br />
far more than an economic, political or cultural<br />
issue. Ultimately, ensuring every woman and<br />
girl has the right to access the utmost level of<br />
health and wellbeing is an issue of human rights<br />
and justice.<br />
Acknowledgements<br />
None<br />
Conflict of Interest<br />
None declared<br />
Correspondence<br />
charlotte.a.oleary@gmail.com<br />
2014;25(4):1507-13.<br />
5. World Health Organization. Gender, women, and<br />
the tobacco epidemic. World Health Organization; 2010.<br />
6. Slade T, Chapman C, Swift W, et al Birth cohort<br />
trends in the global epidemiology of alcohol use and<br />
alcohol-related harms in men and women: systematic<br />
review and metaregression BMJ Open 2016;6:e0<strong>11</strong>827.<br />
doi: 10.<strong>11</strong>36/bmjopen-2016-0<strong>11</strong>827<br />
7. World Health Organization. Household air pollution<br />
and health [Internet]. Geneva: World Health Organization.<br />
<strong>2017</strong> [cited 27 May <strong>2017</strong>]. Available from: http://www.who.<br />
int/mediacentre/factsheets/fs292/en/<br />
8. Peters SA, Woodward M, Jha V, Kennedy S, Norton<br />
R. Women’s health: a new global agenda. BMJ Global<br />
Health. 2016 Nov 1;1(3):e000080.<br />
9. Chamie G, Kwarisiima D, Clark TD, Kabami J, Jain<br />
V, Geng E, Petersen ML, Thirumurthy H, Kamya MR, Havlir<br />
DV, Charlebois ED. Leveraging rapid community-based<br />
HIV testing campaigns for non-communicable diseases<br />
in rural Uganda. PloS one. 2012 Aug 20;7(8):e43400.<br />
10. Janssens B, Van Damme W, Raleigh B, Gupta J,<br />
Khem S, Soy Ty K, Vun MC, Ford N, Zachariah R. Offering<br />
integrated care for HIV/AIDS, diabetes and hypertension<br />
within chronic disease clinics in Cambodia. Bulletin of the<br />
World Health Organization. 2007 Nov;85(<strong>11</strong>):880-5.<br />
<strong>11</strong>. Huxley RR, Woodward M. Cigarette smoking as a<br />
risk factor for coronary heart disease in women compared<br />
with men: a systematic review and meta-analysis of<br />
prospective cohort studies<br />
12. Woodward M, Peters SA, Huxley RR . Diabetes and<br />
the female disadvantage. Women’s Health (Lond Engl).<br />
2015; <strong>11</strong>: 833-839.<br />
13. Huxley RR, Peters SA, Mishra GD, Woodward M.<br />
Risk of all-cause mortality and vascular events in women<br />
versus men with type 1 diabetes: a systematic review and<br />
meta-analysis. The Lancet Diabetes & Endocrinology.<br />
2015 Mar 31;3(3):198-206.<br />
14. United Nations. Transforming our world: the 2030<br />
Agenda for Sustainable Development. Geneva: United<br />
Nations. 25 Sept 2015.<br />
References<br />
1. World Health Organization. NCD mortality and<br />
morbidity [Internet]. Geneva: World Health Organization.<br />
<strong>2017</strong> [cited 27 May <strong>2017</strong>]. Available from: http://www.who.<br />
int/gho/ncd/mortality_morbidity/en/<br />
2. The World’s Women 2015. 2015. United Nations<br />
Statistics Division [Internet]. Accessed from: https://<br />
unstats.un.org/unsd/gender/chapter3/chapter3.html<br />
3. Insights from 10,000 women on the impact of<br />
NCDs [Internet]. Arogya World. 2014. Accessed from:<br />
http://arogyaworld.org/wp-content/uploads/2014/12/<br />
Arogya-Full-Report-For-Web.pdf<br />
4. Matoff-Stepp S, Applebaum B, Pooler J, Kavanagh<br />
E. Women as health care decision-makers: Implications<br />
for health care coverage in the United States.<br />
Journal of health care for the poor and underserved.<br />
17
Healthcare in Conflict Zones<br />
[Feature Article]<br />
Michael Wu<br />
Michael Wu graduated with a B.Pharm from the University of Sydney in 2012 with a major<br />
from the Clinical Excellence Commission focusing on IV to Oral Switch Therapy. Since then, my<br />
passions have grown from Infectious Diseases to just about everything. It’s a problem. I’d like to<br />
work all over the world at some stage, whether in Trauma or Ophthalmology.<br />
Introduction<br />
Medical neutrality in war-ravaged areas<br />
is the cornerstone of healthcare provision in<br />
conflict zones. However, weaponisation of<br />
healthcare – the deliberate destruction or<br />
removal of access to healthcare as a means<br />
of hamstringing opponents – has emerged as<br />
a concerning and common practice in modern<br />
military engagements. Medical neutrality was<br />
formalised in 1864 with the inception of the First<br />
Geneva Convention, which sought to establish<br />
a permanent ‘neutral’ agency that would deliver<br />
medical aid and services to sick and wounded<br />
combatants.[1] There was consensus amongst<br />
governments that armed conflict, no matter<br />
how violent, must maintain some semblance<br />
of compassion and humanity. This recognition<br />
was at the core of the message the Geneva<br />
Convention sent; that a line must be drawn<br />
in war and conflict. Recent years have seen<br />
military forces and governments ignore this<br />
sentiment, with clear violations of the Geneva<br />
Convention, from deliberate bombings and<br />
executions of doctors, nurses, pharmacists,<br />
medical students, and pharmacy students<br />
in Syria and Somalia, for example. Indeed, it<br />
would appear that many countries are either<br />
implicated in, or turn a blind eye to, atrocities<br />
resulting from violations of the Geneva<br />
Convention.<br />
Dr Kathleen Thomas has experienced<br />
this degeneration in the standard of warfare<br />
first-hand. Her story has become a landmark<br />
in this field. As an Australian doctor, she was<br />
responsible for an Intensive Care Unit at a<br />
Medecins Sans Frontieres (MSF) hospital in<br />
Kunduz, Afghanistan, when it was bombed by<br />
an American AC130 gunship in October, 2015.<br />
MSF had released the GPS coordinates of their<br />
hospital to American forces in the region days<br />
prior; their location was known. Repeated air<br />
strikes resulted in 42 fatalities, including 12<br />
staff, 24 patients and 4 caretakers, with dozens<br />
more wounded. MSF maintains that the attack<br />
was deliberate and has called for independent<br />
investigations by multiple bodies.[2] One must<br />
question why American forces, or indeed<br />
any government, would condone the attack<br />
of healthcare facilities. Similarly, however,<br />
it is important to realise that from a military<br />
perspective, this weaponisation of healthcare<br />
makes sense: it removes a valuable resource<br />
to guerrilla forces, that of neutral healthcare.<br />
Healthcare and conflict in Syria<br />
Syria is now the most dangerous nation in<br />
the world according to the Global Peace Index.<br />
[3] The Syrian civil war has left much of the<br />
country’s population displaced since beginning<br />
in 20<strong>11</strong>. As early as March that year, the country<br />
saw its first documented execution of a doctor.<br />
Subsequently, the attrition of healthcare in<br />
Syria has been the result of direct and violent<br />
attacks on health workers, as well as a mass<br />
exodus of health workers fleeing persecution.<br />
These direct attacks are mostly carried out by<br />
pro-government forces, and have manifested<br />
as “attacks on health facilities, executions,<br />
imprisonment or threat of imprisonment,<br />
unlawful disappearance (i.e. kidnapping),<br />
abduction, and torture sometimes leading to<br />
18
death” [4]. According to data from Physicians<br />
for Human Rights, 796 health workers were<br />
killed between March 20<strong>11</strong> and December<br />
2016. Of these deaths, shelling and bombing<br />
accounted for just over<br />
half (55%), followed by<br />
shooting (23%), torture<br />
(13%), and execution<br />
(8%).[5] In addition to<br />
health worker fatalities,<br />
military forces have also<br />
targeted health facilities.<br />
This escalated in late September 2015, when<br />
Russia intervened militarily to provide support<br />
for the Syrian government, with 2016 data<br />
showing an 89% increase in verified attacks<br />
on healthcare facilities. The Syrian Network<br />
for Human Rights documented “289 attacks on<br />
medical facilities, ambulances and Syrian Arab<br />
Red Crescent bases, 96% of which were by<br />
Syrian or Russian forces”.[6] In contrast to the<br />
attacks in Afghanistan, such as that of the MSF<br />
Hospital in Kunduz, these documented attacks<br />
became so blatant that the United Nations (UN)<br />
Security Council condemned them in Resolution<br />
2286 on May 2016.[7]<br />
In 2009, Syria had 29,927<br />
doctors,[8] a figure that has fallen<br />
by 15,000 due to persecution and<br />
war, as reported by Physicians for<br />
Human Rights in 2015.[9]<br />
In 2009, Syria had 29,927 doctors,[8] a figure<br />
that has fallen by 15,000 due to persecution<br />
and war, as reported by Physicians for Human<br />
Rights in 2015.[9] This vacuum of physicians<br />
has led to the development of gaps<br />
and deficits in the skills and numbers of<br />
healthcare personnel available to serve<br />
the civilian population, which is already<br />
under duress from open conflict and<br />
aerial bombings. However, a deeper look<br />
at this gap reveals a disparity between<br />
government controlled areas and nongovernment<br />
controlled areas. In 2015, the<br />
non-government controlled region of Eastern<br />
Aleppo had a doctor-to-patient ratio of 1:7000;<br />
just 5 years prior, the ratio was 1:800. Research<br />
from The Syrian Centre for Policy Research has<br />
demonstrated a gross disparity in healthcare<br />
cover, with 31% of Syrians living in areas with<br />
insufficient health workers and 27% living<br />
in areas with a complete absence of health<br />
workers.[4]<br />
Many medical students in Syria have<br />
abandoned their studies, either because there<br />
are no longer doctors to teach them, or because<br />
there is such an urgent need to replace missing<br />
health workers that students are required to<br />
provide care. This has amplified the<br />
potential for suboptimal outcomes,<br />
with inexperienced doctors and<br />
medical students forced to practice<br />
outside of their scope of proficiency,<br />
increasing the risk of complications<br />
for patients. Indeed, surgical<br />
complications and infections have<br />
become more common, potentially reflecting<br />
shortcomings in medical training.[4]<br />
Responses to healthcare weaponisation<br />
In the face of these atrocities, what is there<br />
to do? In keeping with observations regarding<br />
healthcare in conflict zones, particularly in the<br />
context of healthcare weaponisation, health<br />
policy released by The Lancet and American<br />
University of Beirut (AUB) Commission<br />
has explored priorities for maintaining and<br />
promoting healthcare despite the challenges<br />
of conflict. Strengthening accountability with<br />
respect to the protection of health workers has<br />
been noted as the key priority in combating the<br />
surge in violence towards health workers and<br />
facilities. Multiple nations and key advocates,<br />
such as the UN Secretary General and the UN<br />
Strengthening accountability<br />
with respect to the protection of<br />
health workers has been noted as<br />
the key priority in combating the<br />
surge in violence towards health<br />
workers and facilities.<br />
High Commissioner of<br />
Human Rights, have<br />
supported and referred<br />
numerous war crimes<br />
from the Syrian conflict<br />
to the International<br />
Criminal Court. These<br />
attempts have been<br />
obstructed by Russia and China, two of the five<br />
permanent members of the UN Security Council.<br />
Indeed, the UN Security Council has issued<br />
multiple resolutions demanding humanitarian<br />
access and condemning chemical warfare, the<br />
latter of which is particularly pertinent given<br />
recent chemical attacks in Syria. However,<br />
these resolutions have resounded emptily<br />
due to political and diplomatic obstruction.<br />
Fouad et al., publishing under the Lancet/AUB<br />
Commission, suggest that responsibility falls<br />
to the civic society and medical community<br />
19
to bring governments and warring factions<br />
to account, and to end war crimes against<br />
both health workers and civilians. Groups in<br />
the Netherlands, Belgium, Spain, France, and<br />
Sweden have already had some success in<br />
bringing the agenda of health workers in conflict<br />
zones to peace negotiations.[4]<br />
Other recommendations include supporting<br />
health workers in conflict zones with resources,<br />
and reinforcing their capacity to deliver a wide<br />
range of services beyond trauma management.<br />
The Syrian conflict has highlighted the shortand<br />
long-term complexities of healthcare in<br />
conflict zones, and it is not feasible to allow<br />
other domains of care, such as maternal and<br />
neonatal care, to suffer as a consequence<br />
of conflict, or to allow vaccine-preventable<br />
endemics to resurge, as has happened in<br />
Nigeria.<br />
Institutions, including<br />
military organisations,<br />
should actively encourage<br />
and promote the concept<br />
of medical neutrality, and<br />
work to minimise disruption<br />
to healthcare services.<br />
It must also be realised<br />
that promoting global solidarity with health<br />
workers will help to develop an environment<br />
within which protection in times of conflict is<br />
more readily achieved. Initiatives such as the<br />
Safeguarding Health in Conflict Coalition and<br />
the Red Cross’ Health Care in Danger Project<br />
should be developed further to prevent targeting<br />
of health workers, or at least to facilitate early<br />
mobilisation and response to violence against<br />
health workers and facilities.<br />
Finally, but perhaps most importantly,<br />
more research on health workers in conflict<br />
is required, with an emphasis on developing<br />
understanding across multiple nations and<br />
conflict zones, given the heterogeneity in<br />
warfare and its effects on healthcare. Such<br />
data will allow governments and organisations<br />
to draw precedence for future conflicts, and will<br />
lend weight to arguments advocating for the<br />
protection of health workers and the civilian<br />
populations they serve.<br />
Conclusion<br />
Finally, but perhaps most importantly,<br />
more research on health workers in<br />
conflict is required, with an emphasis<br />
on developing understanding across<br />
multiple nations and conflict zones,<br />
given the heterogeneity in warfare and<br />
its effects on healthcare.<br />
Fighting against this paradigm shift away<br />
from medical neutrality is an arduous and<br />
daunting task. Even with strong backing from<br />
top UN position holders and many governments,<br />
offending parties still roam free of retribution<br />
and accountability. Despite feeling like a<br />
David vs. Goliath battle, the fate of healthcare<br />
in conflict relies upon the empathic and<br />
moral consideration of medical neutrality, a<br />
responsibility which belongs to every health<br />
worker, medical student, and civilian.<br />
“The standard you walk past is the standard<br />
that you accept” – General David John Hurley<br />
(AC).<br />
References<br />
Acknowledgements<br />
None<br />
Conflict of Interest<br />
None declared<br />
Correspondance<br />
miwu5665@uni.sydney.edu.au<br />
1. Shaw M. Geneva Conventions. In: Encyclopaedia<br />
Britannica [Internet]. Chicago: Encyclopaedia Britannica<br />
Inc; 2004. Available from: https://www.britannica.com/<br />
event/Geneva-Conventions. (Accessed March 30th<br />
<strong>2017</strong>)<br />
2. Thomas K. What was lost in the Kunduz Hospital<br />
Attack [Internet]. Medecins Sans Frontieres; 2016.<br />
Available from: https://www.msf.org.au/article/storiespatients-staff/what-was-lost-kunduz-hospital-attack.<br />
(Accessed March 30th <strong>2017</strong>)<br />
3. Institute for Economics & Peace. Global Peace<br />
Index 2016 Report. IEP Report 39. 2016. Available from:<br />
http://visionofhumanity.org/app/uploads/<strong>2017</strong>/02/GPI-<br />
2016-Report_2.pdf. (Accessed March 30th <strong>2017</strong>)<br />
4. Fouad F, Sparrow A, Tarakji A, Alameddine M,<br />
El-Jardali F, Coutts A, et al. Health workers and the<br />
weaponisation of health care in Syria: a preliminary<br />
inquiry for The Lancet –American University of Beirut<br />
Commission on Syria. Lancet. <strong>2017</strong>. DOI: http://dx.doi.<br />
org/10.1016/ S0140-6736(17)30741-9<br />
5. Anatomy of a Crisis: A Map of Attacks on Health<br />
Care in Syria [Internet]. Physicians for Human Rights.<br />
Available from: https://s3.amazonaws.com/PHR_syria_<br />
20
map/findings.pdf (Accessed 30th March, <strong>2017</strong>).<br />
6. Reports on vital facilities attacked August 2014<br />
through December 2016 [Internet]. Syrian Network for<br />
Human Rights. Available from: http://sn4hr.org/blog/<br />
category/report/monthly-reports/vital-facilities-monthlyreports/<br />
(Accessed 30th March <strong>2017</strong>)<br />
7. United Nations. Security Council adopts resolution<br />
2286 (2016), strongly condemning attacks against<br />
medical facilities, personnel in conflict situations<br />
[Internet]. 2016. Available from: https://www.un.org/press/<br />
en/2016/sc12347.doc.htm (Accessed 30th March <strong>2017</strong>)<br />
8. Annual Report, 2009. Ministry of Health Syria;<br />
2009. Available from: http://www.moh.gov.sy/Default.<br />
aspx?tabid=251&language=en-US (Accessed 30th<br />
March, <strong>2017</strong>)<br />
9. Kupferman S. Syria’s neighbors must let doctors<br />
practice [Internet]. Physicians for Human Rights. 2016.<br />
Available from: http://physiciansforhumanrights.org/<br />
press/press-releases/syrias-neighbors-must-letdoctors-practice.html<br />
(Accessed 30th March 6, <strong>2017</strong>)<br />
21
Surgery: Luxury or Necessity?<br />
[Feature Article]<br />
Maryam Ali Khan (Pakistan), Zineb Bentounsi (Morocco), Nayan Bhindi (Australia),<br />
Helena Franco (Australia), Tebian Hassanein Ahmed Ali (Sudan),<br />
Katayoun Seyedmadani (Grenada/USA), Ruby Vassar (Grenada), Dominique<br />
Vervoort (Belgium) -InciSioN international team members<br />
InciSioN, the International Student Surgical Network, is a student-led organisation of<br />
medical students and young doctors from around the globe with one shared passion,<br />
Global Surgery. InciSioN embodies the aim of educating about, advocating for, and<br />
performing research in Global Surgery. Among the 33 members of InciSioN, we share 23<br />
countries spanning over 12 time zones, in 5 continents, and speak over 15 languages.<br />
The seminal report published by the Lancet<br />
Commission on Global Surgery (LCoGS) in<br />
April 2015 highlighted that an estimated 5<br />
billion people continue to lack access to<br />
safe and affordable surgical and anaesthetic<br />
care when required.[1] Often, surgical care is<br />
associated with costly procedures and stateof-the-art<br />
equipment. While that might be true<br />
for a subset of procedures, there are many<br />
lifesaving procedures that are considered<br />
basic public health needs and can be<br />
performed cost-effectively with a simpler set<br />
of equipment. Through domains of research,<br />
education and advocacy, the relatively recent<br />
movement of Global Surgery endeavours to<br />
address and alleviate these vast disparities in<br />
surgical equity, particularly in low and middleincome<br />
countries (LMICs). Here, we would like<br />
to evaluate surgical care on a global scale<br />
from a basic public health standpoint.<br />
Basic surgical care and safe surgery<br />
Surgery is defined by the World Health<br />
Organization (WHO) as “any procedure<br />
occurring in the operating room involving the<br />
incision, excision, manipulation or suturing of<br />
tissue that usually requires regional or general<br />
anaesthesia or profound sedation to control<br />
pain”.[2] Surgery is rendered across all disease<br />
categories, and is an indispensable component<br />
of health care. Essential surgical care is a<br />
distinct concept, meaning surgery necessary<br />
to prevent imminent death or disability. Without<br />
access to essential surgical care, readily<br />
treatable diseases can pose serious threats to<br />
health.<br />
Safe surgery involves avoiding complications<br />
or adverse events that can arise before,<br />
during and after surgical procedures. Thus,<br />
safety measures are implemented before<br />
anaesthesia, before incision, during surgery<br />
and in the provision of post-operative care.<br />
The WHO estimates that every year almost<br />
7 million surgical patients suffer significant<br />
complications, most commonly including<br />
infection, bleeding and various complications of<br />
anaesthesia. More than half of these adverse<br />
events are preventable. In view of this, the WHO<br />
has implemented Guidelines for Safe Surgery<br />
(2009) to define core safety standards, with 10<br />
essential objectives that can be implemented<br />
in any country and any surgical setting. These<br />
serve to reinforce the standardisation of safe<br />
practices, particularly in developing countries.<br />
Cost of basic surgical care<br />
Access to safe anaesthesia and surgery,<br />
or lack thereof, has a considerable economic<br />
impact on both patients and society.<br />
22
Without sufficient public funding or health<br />
insurance, access to surgical services depends<br />
on the ability of patients and their family to pay.<br />
[3] High death rates for surgically treatable<br />
conditions in LMICs are often due the financial<br />
barriers of accessing surgical care. Thus<br />
affordability, and not necessarily availability, of<br />
treatment is a major focus.<br />
Surgically treatable causes of disease<br />
account for 28-32% of the global burden of<br />
disease; yet five billion people do not have<br />
access to the surgical care they need.[4] There<br />
is a common misconception that surgical<br />
treatment of these conditions is expensive and<br />
not cost-effective. Beyond the<br />
incredible impact certain basic<br />
surgeries, including caesarean<br />
sections and hernia repairs, can<br />
have on an individual’s quality of<br />
life, their overall monetary cost<br />
over time is comparable to other<br />
global health initiatives.<br />
The cost per DALY averted for basic surgeries<br />
is low in LMICs, in both small and large hospitals.<br />
Examples include emergency caesarean<br />
sections ($18 USD), elective inguinal hernia<br />
repair ($12.88 USD), and cleft lip repair ($15.44<br />
USD).[5] In contrast, other widely implemented<br />
public health initiatives can cost much more:<br />
oral rehydration therapy can cost over $1,000<br />
USD per DALY averted, and HIV HAART therapy<br />
can cost over $900 USD per DALY averted.[5]<br />
Beyond economic measures, lack of access<br />
to treatment of surgically treatable diseases<br />
has a major impact on the lives of patients, their<br />
families, and their communities. A condition as<br />
easily addressed as a strangulated hernia can<br />
be life-threatening to an otherwise healthy adult.<br />
Such a loss of life or work productivity can have<br />
devastating impacts not only on the patient, but<br />
also on those who financially depend on them.<br />
Surgery in low and middle income countries<br />
In the past, the impact of surgical diseases<br />
has been vastly underestimated by global<br />
Surgically treatable causes<br />
of disease account for 28-<br />
32% of the global burden of<br />
disease; yet five billion people<br />
do not have access to the<br />
surgical care they need.[4]<br />
health experts, leading to its absence in the<br />
Sustainable Development Goals (SDGs).<br />
However, since the establishment of the LCoGS<br />
in 2015, there has been a shift in this paradigm.<br />
With 16.9 million annual deaths (32.9% of all<br />
deaths) attributed to surgical conditions, the<br />
total burden far outweighs that of tuberculosis<br />
(TB), HIV/AIDS and malaria combined.[4] This<br />
is because easily treatable surgical diseases<br />
such as open fractures and obstructed labour<br />
cause significant morbidity and mortality due to<br />
lack of access to safe surgical care.<br />
The LCoGS sheds light on the startling<br />
paucity of surgeries performed in LMICs. It<br />
found that a disproportionately<br />
low number of surgeries are<br />
performed in LMICs compared<br />
to the population size. A third of<br />
the world’s poorest population<br />
resides in LMICs, and yet only<br />
6% of all surgical procedures<br />
worldwide are performed in<br />
these countries.[4] An additional<br />
143 million surgical procedures are required<br />
annually to overcome this present need.<br />
Failure to address such basic health and<br />
surgical needs can potentially endanger the<br />
economic progress of these countries. This<br />
is particularly pertinent given the growing<br />
population and problem of uneven healthcare<br />
access in LMICs. Each year, 33 million individuals<br />
worldwide face immense expenditures due to<br />
out-of-pocket payment of medical and surgical<br />
costs, which can push them into poverty.[4] The<br />
LCoGS found that workforce losses attributable<br />
to surgical conditions reduce GDP growth by up<br />
to 2%, particularly affecting growing nations. If<br />
no further is taken to address surgical needs in<br />
LMICs, it is estimated that the global economic<br />
loss in terms of international GDP could soar up<br />
to $12.3 trillion USD from 2015 to 2030.[4]<br />
These figures are alarming, and it is of<br />
utmost importance to recognise that these are<br />
not merely numbers and statistics, but that they<br />
represent real people affected every day. What<br />
must be stressed is that although the costs of<br />
23
providing surgery are high, investing in surgical<br />
services in LMICs is affordable, saves lives,<br />
and promotes economic growth.[4] To improve<br />
the current conditions, there is a great need<br />
to gather data, identify gaps in data regarding<br />
surgical access, funding and resources, and<br />
monitor progress.<br />
Global surgery in action<br />
Advocacy in recent years has demonstrated<br />
new potential for advancements in global surgery.<br />
Since its establishment in 2015, the LCoGS has<br />
been ground-breaking in demonstrating the<br />
many opportunities for improvements in global<br />
health and global surgery over the next 15 years<br />
and beyond.<br />
Progress has also been made in surgical<br />
safety. For instance, the sustained use of<br />
the “WHO Surgical Safety Checklist” led to<br />
continued improvements in surgical processes<br />
and reductions in 30-day surgical complications<br />
in Moldova, a LMIC, almost 2 years after<br />
its implementation.[6] Such improvements<br />
were seen despite the absence of continued<br />
oversight by the research team, demonstrating<br />
the important role that local leaders play in<br />
the success of quality improvement initiatives,<br />
especially in resource-limited settings.<br />
Moreover, opportunities to address health<br />
inequity and reset the global health agenda<br />
have arisen. These include global commitments<br />
to achieve Universal Health Coverage and the<br />
establishment of the Sustainable Development<br />
Goals. Realisation of the various goals to end<br />
poverty, ensure health for all, and promote<br />
sustainable economic growth, will be more<br />
achievable by ensuring delivery of safe,<br />
affordable and timely surgical care.[1]<br />
However, more improvements can still<br />
be made to further the provision of surgery<br />
worldwide. Currently, a global fund for surgery<br />
does not exist, and only a few foundations<br />
are willing to support surgery. Indeed, it took<br />
decades of advocacy to demonstrate the huge<br />
disease burden of other global health issues<br />
such as HIV/AIDs, tuberculosis and malaria,<br />
and then to develop funding mechanisms for<br />
them. With surgeons and leaders in global<br />
health advocating for patients in LMICs, we can<br />
hope to push for financial support in the coming<br />
years in order to improve the infrastructure and<br />
access to safe surgical care.<br />
In order to improve training and facilitate<br />
sharing of resources, there should also be further<br />
collaboration between hospitals in high income<br />
countries and LMICs (“twinning programs”).<br />
[3] However, donor hospitals, surgeons, and all<br />
those involved in efforts to redistribute surgical<br />
supplies need to exercise due diligence by<br />
ensuring that their partner institutions, including<br />
hospitals, clinics and medical schools, commit<br />
to reaching the poorest populations. Additionally,<br />
it is important to integrate vertical surgical<br />
programs into broader efforts to improve public<br />
health. In doing so, several important questions<br />
need to be raised: how effectively are the<br />
partner institutions providing care? Are they<br />
meeting broader goals of public health and<br />
global health equity?[3,7,8]<br />
Finally, professional interest groups starting<br />
at the level of medical students and residents<br />
can foster interest and educate others about<br />
surgery in a global healthcare setting. One<br />
such entity is the International Student Surgical<br />
Network (InciSioN). This international team of<br />
medical students and young doctors, began as<br />
a small working group within the International<br />
Federation of Medical Student Associations<br />
(IFMSA) in 2014. Since its initiation, members of<br />
InciSioN have been passionately active in global<br />
surgery research, advocacy and education.<br />
Conclusion<br />
Considering the significant economic and<br />
disease burden of lack of access to safe<br />
surgical care, surgery is truly a necessity and<br />
not a luxury. Put simply, essential surgical care<br />
should be made accessible and available<br />
to everyone in the public sector. Whilst the<br />
challenges are huge, progress in global surgery<br />
can be made with patience, determination and<br />
24
devotion to the cause. There is much hope that,<br />
through international movements led by various<br />
organisations, and with involvement of medical<br />
students, doctors, and leaders in global health,<br />
the landscape of safe surgical care will change.<br />
As members of InciSioN international team, we<br />
dream of a world where no life is lost due to lack<br />
of access to safe surgery and anaesthesia.<br />
References<br />
1. Lancet Commission on Global Surgery. Global<br />
surgery 2030 report overview [Internet]. 2015. Available<br />
from: https://www.surgeons.org/media/21831010/<br />
Lancet-Commission-Policy-Briefs.pdf<br />
2. World Health Organization. WHO guidelines for<br />
safe surgery 2009 [Internet]. World Health Organisation;<br />
2009. Available from: http://apps.who.int/iris/<br />
bitstream/10665/44185/1/9789241598552_eng.pdf<br />
3. Farmer PE, Kim JY. Surgery and global health: a<br />
view from beyond the OR. World J Surg [Internet]. 2008<br />
Mar [cited <strong>2017</strong> May 28];32(4):533-536. Available from:<br />
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2267857/<br />
pdf/ DOI: 10.1007/s00268-008-9525-9<br />
4. Meara, JG, Leather AJM, Hagander L, Alkire BC,<br />
Alonso N, Ameh EA et al. Global surgery 2030: evidence<br />
and solutions for achieving health, welfare, and economic<br />
development. Lancet [Internet]. 2015 Apr [cited <strong>2017</strong> May<br />
28];386:569-624. Available from: http://www.thelancet.<br />
com/pdfs/journals/lancet/PIIS0140-6736(15)60160-X.<br />
pdf DOI: 10.1016/S0140-6736(15)60160-X<br />
5. Grimes, CE, Henry JA, Maraka J, Mkandawire NC,<br />
Cotton M. Cost-effectiveness of surgery in low- and<br />
middle-income countries: a systematic review. World J<br />
Surg [Internet]. 2013 Oct [cited <strong>2017</strong> May 28];38:252-<br />
263. Available from: http://www.brighamandwomens.<br />
org/Research/labs/CenterforSurgeryandPublicHealth/<br />
Documents/AGSF/2014/December/Grimes%20<br />
CE%20CE%20of%20Surgery%20in%20LMICs%20<br />
systematic%20review%20WJS%202014.pdf DOI:<br />
10.1007/s00268-013-2243-y<br />
6. Kim RY, Kwakye G, Kwok AC, Baltaga R, Ciobanu G,<br />
Merry AF et al. Sustainability and long-term effectiveness<br />
of the WHO surgical safety checklist combined with pulse<br />
oximetry in a resource-limited setting. JAMA Surg [Internet].<br />
2015 Mar [cited <strong>2017</strong> May 28];150(5):473-479. Available<br />
from: http://jamanetwork.com/journals/jamasurgery/<br />
fullarticle/2207940 DOI: 10.1001/jamasurg.2014.3848.<br />
7. Walton DA, Farmer PE, Lambert W, Leandre F,<br />
Koenig SP, Mukherjee JS. Integrated HIV prevention and<br />
care strengthens primary health care: lessons from rural<br />
Haiti. J Public Health Policy. 2004;25(2):137-158.<br />
8. Farmer P. From “marvelous momentum” to health<br />
care for all. Foreign Affairs. 2007 Mar;86(2):155-161.<br />
25
Beyond the horizon and back again<br />
Interview with Professor David Hilmers<br />
[Feature Article]<br />
Ashley Wilson-Smith<br />
Prelude<br />
The globalisation of medicine, particularly<br />
within the last 50 years, has presented both<br />
students and practitioners with an exciting -<br />
yet staggering - amount of career and lifestyle<br />
pathways. Be it working with Medecins Sans<br />
Frontieres (MSF) in Africa; coordinating a WHO<br />
response to a new, virulent disease; or servicing<br />
rural-remote populations in outback Australia;<br />
the variety of work within medicine is nothing<br />
short of astounding.<br />
Early life and background<br />
Speaking with Professor David Hilmers of<br />
the Baylor College of Medicine, this becomes<br />
abundantly clear. With rich and varied<br />
occupational and academic experience,<br />
Hilmers’ pathway into medicine is as fascinating<br />
as his career has been since graduation. After<br />
growing up in a small town in Iowa, Hilmers<br />
moved from undergraduate study to flight<br />
school, the United States Marines – during the<br />
Vietnam War, no less – and eventually graduate<br />
school. Here, he studied electrical engineering<br />
and mathematics, giving him a tremendous<br />
grounding in scientific practice. Whilst he<br />
expressed a desire to practice medicine<br />
from as early as childhood, Hilmers was<br />
serendipitously given opportunities that initially<br />
drove him more towards working with N.A.S.A<br />
than working in medicine, as astounding as<br />
that may seem. Contextually, the United States<br />
space program was still maturing following<br />
the peak of the Cold War, with Hilmers’ career<br />
progression perfectly aligning with the 1980’s<br />
selection period.<br />
In space on IML-1 just before starting medical school<br />
Moving into N.A.S.A (and eventually,<br />
medicine)<br />
Whilst stationed in Japan on his third tour<br />
overseas, Hilmers heard that the Marines were<br />
offering forward candidates for consideration<br />
to the astronaut program. Given that his<br />
background was textbook in terms of the<br />
desired skillsets - flight/military experience,<br />
engineering and mathematics - he placed<br />
himself forward. One level after another, he<br />
cleared selection and eventually found himself<br />
as an astronaut-in-training, something which<br />
he considered entirely surprising. After a period<br />
of intense long-term preparation, training and<br />
eventually four on-orbit expeditions later,<br />
Hilmers decided that it was finally time to study<br />
medicine. Whilst it would have been incredible<br />
to hear more about this journey to N.A.S.A,<br />
it is his work following his time in space that<br />
really exemplifies the multifaceted nature of<br />
medicine and global health.<br />
26
Medical career and global health research<br />
experience<br />
After graduation and specialisation in<br />
Medicine/Paediatrics at the Baylor College of<br />
Medicine, Houston, Hilmers’ career branched out<br />
across all realms of medicine. Encompassing<br />
on-the- ground experience in disease outbreak<br />
areas, applying his engineering knowledge within<br />
a medical context, working with large soft-drink<br />
distributors (Coca Cola) and then finally more<br />
traditional faculty and hospital work, Hilmers’<br />
practice has been anything but conventional.<br />
Discussing all he has done in retrospect, he<br />
did find it amusing that his background mirrors<br />
his life outlook; a “little bit of variety” being his<br />
exact words.<br />
The Smart Pod<br />
A notable outcome following Hilmers’<br />
return from Liberia, however, was his ensuing<br />
attachment to a research team who were in<br />
the process of developing a rapidly deployable<br />
‘Emergency Smart Pod’ [1]. This pod is an on-site,<br />
versatile management centre and laboratory,<br />
with revolutionary potential with regards to<br />
disease outbreak and disaster response. Given<br />
his background, Hilmers was able to provide<br />
highly practical, ongoing advice; this came in the<br />
form of refining and redesigning early iterations,<br />
and increasing functionality and practicality.<br />
The pod, as it stands now, is a feat of modern<br />
science and engineering; touting high-tech<br />
computer systems with language and literacy<br />
programs, screening facilities, crowd control<br />
and Ebola-level handling capabilities. Hilmers<br />
humorously likened it to a space module. The<br />
pods are similar to shipping containers in size,<br />
but far lighter and more durable. In fact, they are<br />
built entirely from recyclable materials that can<br />
withstand extremes both hot and cold, and can<br />
be integrated with one another should the need<br />
arise. Clearly, the ability to treat, screen and<br />
mitigate disaster on-site will strengthen frontline<br />
medical workers domestically and abroad.<br />
Coca Cola and micronutrient deficiencies<br />
AIDS patient in Romania<br />
Starting his global health journey by touring<br />
overseas to Africa with the Baylor AIDS initiative,<br />
Hilmers subsequently went on to see AIDSravaged<br />
Eastern Europe post-collapse of the<br />
Soviet Union, and more recently was the Chief<br />
Physician of an Ebola treatment unit in Liberia<br />
during the outbreak. Whilst acknowledging<br />
the saddening reality of AIDS treatment and<br />
outcomes in the early days, Hilmers remarked<br />
that the experience was immensely educational<br />
and worthwhile. Indeed, it inspired him to<br />
continue his work with AIDS sufferers in local<br />
Houston.<br />
In terms of more typical research, Hilmers<br />
has been involved in a number of studies on<br />
health inequalities, with some interesting pieces<br />
focussing on effective delivery of micronutrients<br />
to nutrient-deficient communities. This work<br />
interestingly includes working with Coca Cola,<br />
given their not-so-surprising ability to source<br />
fresh, clean water for their drinks in even the<br />
most remote locations. The importance of this<br />
becomes clear with a bit of thought; considering<br />
Coca Cola’s highly efficient sourcing and<br />
distribution system, there is an opportunity to<br />
integrate fortified beverages into their product<br />
line. This has enabled access to otherwise<br />
inaccessible communities overseas, and<br />
disadvantaged communities domestically. This<br />
was notable, given the medical community’s<br />
overwhelming condemnation of Coca Cola’s<br />
27
soft-drinks in day-to-day practice. It’s a case<br />
that speaks to the astounding intricacy of global<br />
health work, and the manner with which problems<br />
can be solved in the most unconventional of<br />
ways.<br />
Life experience and medicine - how does<br />
everything relate?<br />
One of the things that became apparent<br />
to me regarding Hilmers’ work is an ability<br />
to extract the positive attributes needed in<br />
previous work, and apply them to his current<br />
setting. He credits his military training with giving<br />
him a “coolness under fire”, his engineering<br />
and mathematics background with a logical<br />
thought process, and finally his N.A.S.A flight<br />
experience with a systematic, step-by-step<br />
approach to problem solving - all experiences<br />
that have shown themselves to be invaluable.<br />
Therein lies a lesson for all students: take on<br />
board every opportunity to grow your skillset,<br />
as it will lend itself in ways that may not yet<br />
seem apparent This is, in fact, one of Hilmers’<br />
central advocacy arguments for continued<br />
work on the International Space Station,<br />
that space exploration and experimentation<br />
confers benefits to medical practice that are<br />
not foreseeable, and vice versa. For example,<br />
treatments that are developed to deal with the<br />
marked muscle atrophy, bone loss and vision<br />
impairment associated with long-term space<br />
travel, can then be applied to everyday medical<br />
practice.<br />
Going forward - individual practitioners and<br />
the profession<br />
So, what advice did Hilmers have for future<br />
medical practitioners as we move into our<br />
practicing years? Principally, it is important to<br />
work in a practice or organisation that allows<br />
you to follow your passion. Be that working solely<br />
within the W.H.O or Medecins Sans Frontieres,<br />
or perhaps academia with concurrent research<br />
and clinical duties, there is a balance that every<br />
person needs to figure out for themselves.<br />
Indeed, Australia is unique in the tremendous<br />
scope of medical opportunities available.<br />
Depending on your location, you can experience<br />
tropical disease in the far north states, noncommunicable<br />
disease in the mid-states, and<br />
the reality of disadvantaged communities<br />
in rural-remote locations. This does beg the<br />
question as to whether global health lends<br />
itself more to international health, as it seems<br />
to be viewed traditionally, or universal well-being<br />
within your own context or circumstance. There<br />
are no borders, rules or regulations as to what<br />
constitutes “global health”, only the limits of our<br />
imagination and creativity. Regardless, if you<br />
want to work in global health, the first step is<br />
finding an area of medicine you have a burning<br />
passion for – the rest will follow as natural<br />
sequelae.<br />
Ebola protective gear<br />
As the mid-century approaches, the threat<br />
of climate change, antibiotic resistance and<br />
the management of ethical conundrums – such<br />
as gene editing and healthcare equity – are<br />
all very real problems that our generation will<br />
have to face. It was saddening to hear Hilmers<br />
recall scenes of polluted, diverted or dammed<br />
lakes from space, of burning forests and haze<br />
hovering over cities, but that is the reality we<br />
live in. It does, therefore, imply that we hold at<br />
least part of the solution to the problems we<br />
face. In what form the specific solution will<br />
take, however, only time can tell. It is, however,<br />
abundantly clear that in going forward we<br />
should learn from leaders like Professor David<br />
Hilmers, whose experience is entirely unique<br />
and profound.<br />
28
PrEP-related health promotion for<br />
Aboriginal and Torres Strait Islander<br />
gay and bisexual men<br />
[Review]<br />
Alec Hope<br />
Alec is a 4th year medical student at the University of New South Wales who is conducting qualitative research into the health<br />
promotion of PrEP to Aboriginal and Torres Strait Islander gay and bisexual men. Alec’s research interests include immunology,<br />
sexual health, and health inequality. He is looking forward to completing his last two years of medical school in Wagga Wagga.<br />
Abstract<br />
Aboriginal and Torres Strait Islander peoples experience significantly poorer health<br />
compared to the general Australian population. This health inequality is highlighted in<br />
comparisons between Indigenous and non-Indigenous sexual health. Pre-exposure<br />
prophylaxis (PrEP) is a new HIV prevention technology that protects gay and bisexual<br />
men. Social, economic, cultural and historical barriers may exist that prevent Aboriginal<br />
and Torres Strait Islander gay and bisexual men from accessing PrEP, and therefore widen<br />
the sexual health inequality that already exists.<br />
Introduction<br />
Aboriginal and Torres Strait Islander (hereafter<br />
‘Indigenous’) peoples living in Australia have significantly<br />
poorer health than non-Indigenous Australians,[1] inextricably<br />
linked to a history of disempowerment and oppression through<br />
colonialism.[2, 3] Indigenous Australians are often identified<br />
as a priority population for public health interventions due to<br />
their generally lower health status.[4] Discrepancies between<br />
Indigenous and non-Indigenous sexual health have been recontextualised<br />
as a human rights issue to draw awareness<br />
and urgency to the matter of inequity of sexual health<br />
between Indigenous and non-Indigenous Australians.[5]<br />
HIV and Indigenous Australians<br />
Human immunodeficiency virus (HIV) is a retroviral<br />
infection that is both blood-borne and sexually transmissible.<br />
HIV exhibits epidemiological differences between Indigenous<br />
and non-Indigenous Australians. Sexual contact between<br />
men is responsible for 75% of HIV notifications for non-<br />
Indigenous Australians, compared to only<br />
51% of HIV notifications amongst Indigenous peoples.<br />
[6] Twenty-one percent of Indigenous HIV notifications are<br />
attributable to injecting drug use and 16% to heterosexual<br />
contact.[6,7] Worryingly, since 20<strong>11</strong>, the age-standardised<br />
rate of Indigenous HIV notifications has been steadily rising<br />
despite nationwide slowing of HIV notifications in the general<br />
population.[8] In 2015, the age-standardised rate of new HIV<br />
notifications in Indigenous people was more than double<br />
that of non-Indigenous people (6.8 per 100,000 vs 3.1 per<br />
100,000).[6]<br />
Men who have sex with men (MSM) are at elevated risk<br />
of becoming infected with HIV compared to the general<br />
population. It is unclear how many Indigenous Australians<br />
identify as gay or bisexual, and many Indigenous MSM may<br />
not identify as gay or bisexual, sometimes due to stigma.[9] A<br />
survey of Indigenous youth aged 16 to 29 found 6% of male<br />
respondents identified as gay, 2% as bisexual, and a small<br />
but significant number as transgender.[10]<br />
Indigenous gay and bisexual men (GBM) and other MSM<br />
may be at increased risk of contracting HIV compared to<br />
non-Indigenous GBM. Indigenous peoples experience higher<br />
rates of sexually transmitted infections (STIs), namely<br />
gonorrhoea and chlamydia, particularly in remote areas.<br />
[6] The presence of an STI predisposes individuals to HIV<br />
infection.[7] Furthermore, Indigenous GBM report higher rates<br />
of risky sexual behaviours compared to non-Indigenous<br />
GBM.[<strong>11</strong>, 12] Rates of unprotected anal intercourse with<br />
casual partners are higher in Indigenous GBM compared<br />
to non-Indigenous, a known risk factor for HIV infection.<br />
[13] Likewise, illicit drug use before or during group sex<br />
was reported at higher rates in Indigenous GBM compared<br />
to non-Indigenous GBM.[<strong>11</strong>, 14] Coupled with the worrying<br />
epidemiological pattern of HIV notifications among injecting<br />
drug users and heterosexual people, these elevated rates<br />
of risk factors among Indigenous people could increase the<br />
risk of HIV transmission for Australia’s Indigenous peoples.<br />
[<strong>11</strong>] Indeed, steady increases in Indigenous HIV notifications<br />
and an elevated age-standardised rate of Indigenous HIV<br />
notifications are causes for concern (Figure 1).[6]<br />
A pill a day to prevent HIV<br />
Antiretroviral (ARV) medications have been used since<br />
the 1990s as an effective treatment for HIV. More recently,<br />
at-risk individuals have used ARVs as an effective HIV<br />
29
prevention method.[15] At-risk individuals can take one pill<br />
daily containing two antiretroviral medications, preventing<br />
replication of the virus within the body so that viral exposure<br />
is not seroconverted, thus preventing HIV infection.[16]<br />
Randomised control trials have found that ARVs taken as<br />
pre-exposure prophylaxis (PrEP) can prevent 40-99% of HIV<br />
infections when taken more than four times a week.[17-21]<br />
PrEP implementation trials are currently being run in New<br />
South Wales, Queensland, Victoria, South Australia, and<br />
the Australian Capital Territory. These trials are supported<br />
and funded by state health departments, allowing free or<br />
heavily discounted access to expensive drugs that cannot<br />
be accessed as PrEP via the Australian Pharmaceutical<br />
Benefits Scheme (PBS).[22]<br />
In New South Wales, the Kirby Institute runs the Expanded<br />
PrEP Implementation in Communities (EPIC) trial in<br />
conjunction with NSW Health. After a year of recruitment, over<br />
5000 at-risk individuals have been enrolled and given access<br />
to PrEP. Most of these participants are GBM, identified as<br />
being at high risk of HIV exposure.[13] This represents a major<br />
expansion from a small pilot study to a large demonstration<br />
trial.<br />
Are Indigenous gay and bisexual men accessing PrEP?<br />
Studies in the United States (US) have found that identified<br />
priority populations, including Black (African-American) men<br />
who have sex with men, may have difficulty in accessing PrEP<br />
compared to the general population. This may be due to lack<br />
of awareness about PrEP,[23] stigma,[24] poor healthcare<br />
coverage,[3] or lack of culturally-appropriate services<br />
providing access.[25] Indeed, Black men who have sex with<br />
men in the US were successfully recruited, engaged and<br />
retained in PrEP programs that employed “culturally-tailored<br />
techniques”.[26]<br />
Research shows that in order to target interventions<br />
like PrEP to Indigenous communities, culturally-appropriate<br />
services owned and governed by the community are in the<br />
best position to deliver positive health outcomes.[27-29]<br />
Likewise, health promotion materials should be designed and<br />
produced by the community for the community, and should<br />
avoid blocks of text and overly technical terminology.[30]<br />
Therefore, Aboriginal community-controlled health services<br />
(ACCHSs) may be best placed to help promote and educate<br />
PrEP to at-risk members of the community, facilitating<br />
referral to specialised sexual health clinics for assessment<br />
and preventative methods that may or may not include<br />
PrEP. ACCHSs provide holistic care, and are well equipped<br />
to focus on prevention and primary healthcare.[31] ACCHSs<br />
are considered manifestations of self-determination and<br />
autonomy for Indigenous communities.[29, 32]<br />
Self-determination in Indigenous Australian health<br />
services<br />
The United Nations has identified ACCHSs as best<br />
practice models of self-determination,[29] and the United<br />
Nations Declaration on the Rights of Indigenous Peoples<br />
advocates for the right of all peoples, especially Indigenous,<br />
to be able to “freely determine their political status and freely<br />
pursue their economic, social and cultural development”.<br />
[33] However, self-determination in healthcare alone cannot<br />
improve health outcomes. Secure, long-term funding coupled<br />
with equitable partnerships between Aboriginal communitycontrolled<br />
and mainstream health services is required to<br />
address the gap between Indigenous and non-Indigenous<br />
health.[29, 32] Facilitating community empowerment reduces<br />
the rates of HIV and STIs in female sex workers (FSWs)<br />
in low- and middle-income countries.[34, 35] Community<br />
empowerment in Australian FSWs during the initial years of<br />
the HIV epidemic was essential in enshrining effective HIV<br />
prevention focused on universal condom use among FSWs.<br />
[36] This case study could be applicable to the Indigenous<br />
population, and similar community empowerment in the<br />
form of well-funded ACCHSs may allow the gap between<br />
Indigenous and non-Indigenous health.<br />
Furthermore, Aboriginal Sexual Health Workers administer<br />
culturally-appropriate health services throughout Australia,<br />
increasing the involvement of Indigenous people in the<br />
healthcare workforce.[28, 37] However, Indigenous peoples<br />
need to be consulted and involved in the decision-making<br />
process and not just in the delivery of health services.[38, 39]<br />
Conclusion<br />
PrEP is touted as a crucial part of the HIV eradication<br />
strategy throughout the world. However, efforts to prevent HIV<br />
transmission may be hampered by a failure to engage priority<br />
populations, including Aboriginal and Torres Strait Islander<br />
Australians. PrEP implementation projects such as EPIC need<br />
to ensure adequate coverage of at-risk Indigenous peoples<br />
through culturally-appropriate health promotion and security<br />
of access to medication. This would be facilitated through<br />
the involvement of Indigenous Australians in the decisionmaking<br />
process. Further research will explore PrEP-related<br />
health promotion to Indigenous peoples and communities,<br />
and attempt to identify any gaps or facilitators.<br />
Figure 1. The age-standardised rate<br />
of new HIV notifications by Indigenous<br />
status.[8]<br />
30
Acknowledgements<br />
Dr Bridget Haire, The Kirby Institute<br />
b.haire@unsw.edu.au<br />
Conflict of Interest<br />
None declared<br />
Correspondence<br />
alecjulianhope@gmail.com<br />
References<br />
1. Commonwealth of Australia. Closing the Gap Prime Minister’s Report<br />
<strong>2017</strong>. Canberra: Department of the Prime Minister and Cabinet; <strong>2017</strong>.<br />
2. Anderson I. Indigenous Australia and health rights. Journal of Law<br />
and Medicine. 2008;15(6).<br />
3. Zambas SI, Wright J. Impact of colonialism on Māori and<br />
Aboriginal healthcare access: a discussion paper. Contemporary Nurse.<br />
2016;52(4):398-409.<br />
4. Australian Government. National Aboriginal and Torres Strait Islander<br />
Health Plan 2013-2023. Australia: Commonwealth of Australia; 2013.<br />
5. Thompson SC, Greville HS, Param R. Beyond policy and planning to<br />
practice: getting sexual health on the agenda in Aboriginal communities in<br />
Western Australia. Aust New Zealand Health Policy. 2008;5(1):3.<br />
6. The Kirby Institute. Bloodborne viral and sexually transmitted<br />
infections in Aboriginal and Torres Strait Islander people: Annual Surveillance<br />
Report 2016. Sydney: The Kirby Institute; 2016.<br />
7. Ward J, Costello-Czok M, Willis J, Saunders M, Shannon C. So far,<br />
so good: Maintenance of prevention is required to stem HIV incidence in<br />
aboriginal and torres strait islander communities in Australia. AIDS Education<br />
and Prevention. 2014;26(3):267-79.<br />
8. Institute TK. HIV, viral hepatitis and sexually transmissible infections<br />
in Australia<br />
Annual Surveillance Report 2016. UNSW Australia, Sydney NSW 2052:<br />
The Kirby Institute; 2016.<br />
9. Australian Federation of AIDS Organisations. National Indigenous<br />
Gay and Transgender Consultation Report. 1998.<br />
10. Ward J, Bryant J, Wand H, Pitts M, Smith A, Delaney-Thiele D, et al.<br />
Sexual Health and relationships in young Aboriginal and Torres Strait Islander<br />
people: Results from the first national study assessing knowledge, risk<br />
practices and health service use in relation to sexually transmitted infections<br />
and blood borne viruses. Alice Springs: Baker IDI Heart & Diabetes Institute;<br />
2014.<br />
<strong>11</strong>. Lea T, Costello M, Mao L, Prestage G, Zablotska I, Ward J, et al.<br />
Elevated reporting of unprotected anal intercourse and injecting drug use<br />
but no difference in HIV prevalence among Indigenous Australian men who<br />
have sex with men compared with their Anglo-Australian peers. Sex Health.<br />
2013;10(2):146-55.<br />
12. Lawrence CG, Rawstorne P, Hull P, Grulich AE, Cameron S, Prestage<br />
GP. Risk behaviour among Aboriginal and Torres Strait Islander gay men:<br />
Comparisons with other gay men in Australia. Sex Health. 2006;3(3):163-7.<br />
13. Cooper D, Grulich A. Impact of the rapid expansion of pre-exposure<br />
prophylaxis (PrEP) on HIV incidence, in a setting with high HIV testing and<br />
antiretroviral treatment coverage, to achieve the virtual elimination of HIV<br />
transmission by 2020: a NSW HIV Strategy implementation project. The<br />
University of New South Wales: The Kirby Institute; 2016.<br />
14. Lawrence CG, Rawstorne P, Hull P, Grulich AE, Cameron S, Prestage<br />
GP. Risk behaviour among Aboriginal and Torres Strait Islander gay men:<br />
Comparisons with other gay men in Australia. Sexual Health. 2006;3(3):163-<br />
7.<br />
15. Therapeutic Goods Administration of Australia. Public Summary for<br />
Australian Register of Therapeutic Goods #107072 (Truvada). Australia:<br />
Therapeutic Goods Administration of Australia; 2016.<br />
16. Therapeutic Goods Administration of Australia. Truvada Product<br />
Information V.15. Australia: Therapeutic Goods Administration of Australia;<br />
2016.<br />
17. Grant RM, Lama JR, Anderson PL, McMahan V, Liu AY, Vargas L, et<br />
al. Preexposure Chemoprophylaxis for HIV Prevention in Men Who Have Sex<br />
with Men. N Engl J Med. 2010;363(27):2587-99.<br />
18. Eisingerich AB, Wheelock A, Gomez GB, Garnett GP, Dybul MR,<br />
Piot PK. Attitudes and Acceptance of Oral and Parenteral HIV Preexposure<br />
Prophylaxis among Potential User Groups: A Multinational Study. PLoS One.<br />
2012;7(1):e28238.<br />
19. Thigpen MC, Kebaabetswe PM, Paxton LA, Smith DK, Rose CE,<br />
Segolodi TM, et al. Antiretroviral Preexposure Prophylaxis for Heterosexual<br />
HIV Transmission in Botswana. New England Journal of Medicine.<br />
2012;367(5):423-34.<br />
20. Molina J-M, Capitant C, Spire B, Pialoux G, Cotte L, Charreau I, et al.<br />
On-Demand Preexposure Prophylaxis in Men at High Risk for HIV-1 Infection.<br />
New England Journal of Medicine. 2015;373(23):2237-46.<br />
21. McCormack S, Dunn DT, Desai M, Dolling DI, Gafos M, Gilson R, et<br />
al. Pre-exposure prophylaxis to prevent the acquisition of HIV-1 infection<br />
(PROUD): effectiveness results from the pilot phase of a pragmatic openlabel<br />
randomised trial. The Lancet. 2015;387(10013):53-60.<br />
22. Winsor B. Three ways to get PrEP in Australia. SBS Sexuality<br />
[Internet]. <strong>2017</strong>. Available from: http://www.sbs.com.au/topics/sexuality/<br />
agenda/article/2016/08/30/three-ways-get-prep-australia.<br />
23. Brooks RA, Landovitz RJ, Regan R, Lee SJ, Allen VC, Jr. Perceptions<br />
of and intentions to adopt HIV pre-exposure prophylaxis among black men<br />
who have sex with men in Los Angeles. Int J STD AIDS. 2015;26(14):1040-8.<br />
24. Miller M, Serner M, Wagner M. Sexual diversity among black men<br />
who have sex with men in an inner-city community. Journal of Urban Health.<br />
2005;82(1):i26-i34.<br />
25. Cairns G. US PrEP study achieves high levels of engagement<br />
and adherence among black men who have sex with men AIDSMap2016<br />
[Available from: http://www.aidsmap.com/print/US-PrEP-study-achieveshigh-levels-of-engagement-and-adherence-among-black-men-who-havesex-with-men/page/3080023/.<br />
26. Hucks-Ortiz C. Successful Engagement of Black MSM into a Culturally<br />
Relevant Clinical Trial for PrEP. 2016 International Aids Conference; 20 July<br />
2016; Durban, South Africa: HIV Prevention Trials Network; 2016.<br />
27. Ward J, McGregor S, Guy RJ, Rumbold AR, Garton L, Silver BJ, et al.<br />
STI in remote communities: Improved and enhanced primary health care<br />
(STRIVE) study protocol: A cluster randomised controlled trial comparing<br />
‘usual practice’ STI care to enhanced care in remote primary health care<br />
services in Australia. BMC Infectious Diseases. 2013;13(1).<br />
28. Thomas DP, Heller RF, Hunt JM. Clinical consultations in an Aboriginal<br />
community-controlled health service. A comparison with general practice.<br />
Australian and New Zealand Journal of Public Health. 1998;22(1):86-91.<br />
29. Mazel O. Self-determination and the right to health: Australian<br />
aboriginal community controlled health services. Human Rights Law Review.<br />
2016;16(2):323-55.<br />
30. Hill PS, Murphy GJ. Cultural identification in Aboriginal and Torres<br />
Strait Islander AIDS education. Australian Journal of Public Health.<br />
1992;16(2):150-7.<br />
31. Ward J, Akre SP, Kaldor JM. Guarding against an HIV epidemic within<br />
an Aboriginal community and cultural framework; lessons from NSW. N S W<br />
Public Health Bull. 2010;21(3-4):78-82.<br />
32. Taylor J, Dollard J, Weetra C, Wilkinson D. Contemporary<br />
management issues for Aboriginal Community Controlled Health Services.<br />
Australian health review : a publication of the Australian Hospital Association.<br />
2001;24(3):125-32.<br />
33. International Covenant on Civil and Political Rights, (1966).<br />
34. Blanchard AK, Mohan HL, Shahmanesh M, Prakash R, Isac S, Ramesh<br />
BM, et al. Community mobilization, empowerment and HIV prevention among<br />
female sex workers in south India. BMC Public Health. 2013;13(1):234.<br />
35. Kerrigan D, Kennedy CE, Morgan-Thomas R, Reza-Paul S, Mwangi<br />
P, Win KT, et al. A community empowerment approach to the HIV response<br />
among sex workers: effectiveness, challenges, and considerations for<br />
implementation and scale-up. The Lancet. 2015;385(9963):172-85.<br />
36. Bates J, Berg R. Sex Workers as Safe Sex Advocates: Sex Workers<br />
Protect Both Themselves and the Wider Community From HIV. AIDS<br />
Education and Prevention. 2014;26(3):191-201.<br />
37. Davidson PM, MacIsaac A, Cameron J, Jeremy R, Mahar L, Anderson<br />
I. Problems, Solutions and Actions: Addressing Barriers in Acute Hospital<br />
Care for Indigenous Australians and New Zealanders. Heart, Lung and<br />
Circulation. 2012;21(10):639-43.<br />
38. Anderson I, Davis G. The hard conversation: Indigenous voices on<br />
public policy. Meanjin. 2016;75(2):68-82.<br />
39. Lock MJ, Thomas DP, Anderson IP, Pattison P. Indigenous<br />
participation in an informal national Indigenous health policy network.<br />
Australian Health Review. 20<strong>11</strong>;35(3):309-15.<br />
31
Mental illness following disasters in<br />
Low Income Countries<br />
[Review]<br />
Rose Brazilek<br />
Rose Brazilek is a PhD candidate studying through the Australian Centre for Blood Disease<br />
at the Alfred Hospital. She has a keen interest in translational medical research and blood<br />
disorders. In the future, she hopes to specialise in haematology with a special interest in<br />
thrombosis and haemostasis.<br />
Abstract<br />
Disasters test the capacity of health infrastructure to act in a well-coordinated and adaptable manner, due to the unique<br />
nature of each event. While immediate provision of healthcare focuses on the physical consequences, the long term mental<br />
health ramifications of such events are often forgotten, and services are ill-equipped to deal with the mental illnesses<br />
arising from them. The inherent challenges to the public health response are compounded by the limitations experienced<br />
by Low to Middle Income Countries (LMIC). These countries may lack the fiscal resources to fund such interventions and<br />
have unstable socio-political environments, which may further complicate disaster response. It is by consideration of these<br />
limitations, risk factors specific to such countries, and cultural sensitivity then that effective, long-standing mental health<br />
interventions can be implemented. This paper will review the predisposing factors to mental illness development following<br />
disaster, particularly in respect to at-risk subpopulations, the impact of socio-political climate and low GDP on disaster<br />
response, and the development of effective, culturally-specific interventions. The intersection between low national GDP<br />
and poor mental health infrastructure often translates to poorer mental health outcomes following disaster. Women,<br />
people of low educational status and low income are especially predisposed to development of mental illness. Common<br />
mental health disorders include Post Traumatic Stress Disorder, depression and anxiety<br />
Introduction<br />
In Low and Middle Income Countries (LMIC), mental<br />
health care considerations of disaster survivors have taken<br />
a proverbial back seat, as the establishment of basic needs<br />
take priority.[1] Unfortunately, overwhelming evidence of<br />
causality between natural disasters and mental health issues<br />
has confirmed that provision of culture-specific mental<br />
health care is an integral part of the public health response<br />
following massive loss of life and injury to minimise longterm<br />
recovery ramifications, and a lack of these services<br />
negatively impacts survivors.[2]<br />
Psychosocial and mental health support programmes<br />
are increasingly being recognised as a crucial component<br />
of the humanitarian response to disasters.[3] However,<br />
disaster response coordination is notoriously complicated<br />
with numerous factors to consider, and lack of funding<br />
and resources in low income countries further limits health<br />
responses.[4] This paper will examine the predisposing<br />
factors to the development of mental illness in those affected<br />
by disaster in LMIC, and suggests potential preventative<br />
actions.<br />
Common mental health disorders arising from disasters<br />
Poor mental health in the immediate aftermath following<br />
disasters is to be expected in most survivors, the degree<br />
of suffering is affected by the nature of the experience,<br />
support networks, coping skills and the community response.<br />
[4] This suffering includes distress –situations in which the<br />
individual feels anger, fear, sadness or shame – emotional<br />
dysregulation, or emotional numbing, however these typically<br />
resolve without long-term consequences.[5] It is when they<br />
are sustained, and impact on daily functioning, that they<br />
are defined as a ‘mental illness’. The most common of<br />
these are the anxiety disorders, particularly Post Traumatic<br />
Stress Disorder (PTSD), in which the individual experiences<br />
heightened arousal, avoidance of triggers, and flashback<br />
episodes.[5] Other mood disorders commonly experienced<br />
include abnormal grief reactions and depression.<br />
Due to the decreased utilisation of health services,<br />
particularly mental health services around the world and<br />
especially in Low to Middle Income Countries (LMIC),<br />
individuals may attempt to self-medicate with alcohol<br />
and other substances.[4] This may lead to substance use<br />
disorders as a way to deal with stressors, by avoiding or<br />
displacing difficult emotions associated with disasters. This<br />
is especially common in patients with a history of substance<br />
use disorder in remission, as relapse is common following<br />
stressful events.<br />
Somatisation disorders also show increased incidence<br />
following disasters; a way for survivors to express emotional<br />
distress.[2] They are more likely to occur in individuals<br />
with other concurrent mental health diagnoses, such as<br />
PTSD. Various cultures approach emotional distress as<br />
irrational, and thus there are a number of culture-specific<br />
disorders that manifest in this way.[3] These include Latah,<br />
32
a condition originating in Southeast Asia in which individuals<br />
have an abnormal startle reaction; Koro, significant anxiety<br />
surrounding recession of genitalia; or Susto, a cultural<br />
variation of panic attacks originating in Latin America.[6]<br />
Knowledge and sensitivity surrounding these diagnoses<br />
may dramatically increase utilisation and efficacy of mental<br />
health programs in disaster areas.<br />
Predisposing factors to mental health disorder diagnosis<br />
There is a complex interplay between social dynamics<br />
and mental health diagnoses, and alteration for cultural<br />
context is an important consideration for any mental health<br />
intervention to be effective. Disasters have the potential to<br />
have a greater impact than initially considered because of<br />
the fear regarding the loss of long-held traditions that define<br />
the culture and community of those affected.[7]<br />
Gender<br />
Of people impacted by disaster in LMIC, females have<br />
been shown to have a higher overall likelihood of developing<br />
mental health disorders, particularly depression.[8, 9]<br />
Recognition of the specific cultural challenges that females<br />
face following a disaster may reduce the impact of events<br />
on their recovery. Females in LMIC often occupy roles of<br />
household responsibility, and women may therefore feel guilty<br />
regarding their lack of ability to tend to basic domestic tasks.<br />
Practical consideration may also mitigate some impact of<br />
the trauma; though shelters often offer gender-segregated<br />
areas, nursing mothers may be reluctant to feed in public<br />
spaces. Women may suffer additional mental strain or sexual<br />
harassment if they are obliged to use public toilet services,<br />
or if they are seen in wet clothing in traditionally modest<br />
countries. These considerations must be kept in mind for<br />
established relief facilities to be effective, particularly in the<br />
case of foreign aid provision.<br />
Low income<br />
The correlation between low income in LMIC and increased<br />
propensity towards poor mental health may be explained<br />
by the ‘reserve capacity model’.[5] This model states that<br />
as individuals have increasing background worries – for<br />
instance uncertainty regarding income and food shortages<br />
– their capacity to deal with additional stressors, as in the<br />
case of disaster, diminishes accordingly. It is well established<br />
that those of low Socio-Economic Status (SES) have poorer<br />
mental health, and often have the least access to services,<br />
either because lack of funding or locational difficulties.[10]<br />
Recognising low SES as a risk factor for the development<br />
of mental illness following disaster may allow more targeted<br />
relief efforts to be initiated.<br />
Formal education<br />
Education and financial stability may also influence<br />
recovery and disease development.[10] One of the key<br />
areas preventing development of LMIC is the lack of<br />
formal education of its citizens. This may also influence<br />
coping capacity following a disaster. On a practical level,<br />
educated individuals have an increased ability to cope<br />
with documentation demands, applications and resource<br />
seeking. This accordingly reduces the stress and impact<br />
of coping following disasters. Similarly, financial status may<br />
impact individuals at every stage of disasters. Those with<br />
lower incomes may have poorer quality of life and less safe<br />
dwellings, and are thus most predisposed to damage in the<br />
event of disasters.[<strong>11</strong>] Additionally, poor financial reserves<br />
may make it difficult to repair houses, and thus affects<br />
post-disaster recovery as well as the reserve capacity of<br />
individuals.<br />
At-risk subpopulations<br />
Children<br />
Children are amongst the most vulnerable groups to<br />
disasters.[12] Negative long-term effects on paediatric<br />
wellbeing include increased incidence of PTSD, depression,<br />
and life dissatisfaction. Children may lose one or both parents<br />
due to disasters, potentially leaving them without a primary<br />
caregiver in areas with inadequate infrastructure such as<br />
education to meet their needs.<br />
Such events have been showed to have a deleterious<br />
impact on school performance, particularly in young males.<br />
[13] In countries where education level has a direct correlation<br />
with lifetime health quality, lack of access to education may<br />
drastically alter an individual’s life course, as well as the<br />
overall poverty level of the affected country. Schools, if still<br />
operational, may provide invaluable facilities for mental<br />
health support for students following natural disaster events<br />
in LMIC. Schools provide a relatively stable environment for<br />
observation and continued support, and they may bring a<br />
sense of normalcy back to areas ravaged by disaster.[14]<br />
Aid workers<br />
A specific challenge is to assess and care for the first<br />
responders and aid workers who assist in relief work following<br />
a disaster. All rescue workers have a higher risk of chronic<br />
distress following exposure to an incident; although several<br />
elements, such as years of experience, perceived locus of<br />
control and social support; may mitigate development of<br />
disease.[15] These factors are important as responders<br />
are often foreign aid workers, operating without existing<br />
infrastructure and in unfamiliar environments devoid of a<br />
support network. Though they are often briefed beforehand<br />
and may receive training to prevent long-term mental health<br />
consequences, such workers are often volunteers with<br />
minimal experience. There is also some degree of stoicism<br />
amongst these volunteers, as their degree of suffering is<br />
judged to be far less than that of the people they are assisting.<br />
Specific considerations in LMIC<br />
The impact of disasters in LMIC appears to be far greater,<br />
in part due to the fragility of their existing infrastructure, and<br />
the lack of significant financial reserves to rebuild and support<br />
affected communities.[3] It is expected that encroaching<br />
urbanisation and industrialisation of developing counties will<br />
33
increase the incidence of disasters – both man-made and<br />
natural – and that developing countries will be most affected<br />
in terms of number and severity. It has been shown that the<br />
risk of PTSD also rises proportionate to increase in severity<br />
and frequency of such events.[15]<br />
Several factors worsen the impact of disasters. Houses<br />
are often of inferior build quality, which reduces the ability<br />
to withstand severe forces.[7] Slums and communities<br />
experiencing poverty are also likely to be built in disasterprone<br />
areas such as flood plains because their inhabitants<br />
are unable to obtain property in safer areas.<br />
In the immediate aftermath of these events, LMIC may<br />
struggle to adequately treat the problems of their citizens<br />
due to limited training and capacity of healthcare and<br />
aid professionals.[10] The World Health Organization has<br />
recognised the role of unskilled aid workers in assessing<br />
mental health conditions and have devised a framework to<br />
use in these circumstances.[16] Untrained or poorly-organised<br />
humanitarian aid and destruction of primary infrastructure<br />
may also constitute secondary stressors following natural<br />
disasters and may compound the initial trauma of the<br />
event. Improper, or lack of, information dissemination may<br />
lead to anxiety and depression about food distribution, with<br />
negatively impacts on community wellbeing.[3]<br />
Determinants of effectiveness of public health responses<br />
One of the difficulties surrounding mental health disaster<br />
response is the changeable nature of the assistance<br />
required. Systems required in the immediate aftermath to aid<br />
those dealing with loss, physical impairment and adaptation<br />
to a different way of life are vastly different as some people<br />
return to their original occupations and homes.[3] Pre-disaster<br />
planning should involve a multidisciplinary team of healthcare<br />
professionals, infrastructure experts and politicians to create<br />
lasting policies that are effective and easily implemented.<br />
Disparities in the availability, accessibility and quality of<br />
mental healthcare due to ethnicity are well-documented. This<br />
may be due to language barriers, fears regarding insurance<br />
and monetary constraints, geographical difficulties<br />
(especially in rural communities), mental health stigma and<br />
lack of education.[7] Addressing these barriers may increase<br />
uptake of such services and reduce the incidence of mental<br />
health-related decrease in quality of life for those most at<br />
risk.<br />
Solutions include the validation and normalisation of<br />
distress reactions, so individuals feel they are experiencing<br />
legitimate reactions, rather than moments of weakness.<br />
[7] It is important to recognise the role of communities and<br />
to establish programs which value interdependence rather<br />
than independence in such situations. Promoting community<br />
action and initiatives will increase community resilience and<br />
realisation of the true impact of shared events.<br />
Cultural competence and sensitivity in foreign aid workers<br />
is essential to effective integration of support services,<br />
as well as the recognition that cultural competence is an<br />
ongoing learning process rather than an end-state.[16] It<br />
is important to identify the causes of potential stigma and<br />
mistrust in order to properly engage minorities in healthcare.<br />
Rituals and traditions from the cultures of those affected may<br />
also be utilised and integrated into care solutions, thus using<br />
innovative interventions to circumvent such difficulties. Finally,<br />
it is critical that aid workers and all stakeholders advocate,<br />
facilitate and conduct research into the incidence of mental<br />
illness and effective treatment solutions for mental illness in<br />
affected populations to increase efficacy of interventions in<br />
the future.[1]<br />
Disaster-derived mental illness: a contemporary<br />
perspective<br />
Disasters today are often man-made, as in the case of<br />
conflict. There is scarce research into the impact of such<br />
political conflict in LMIC. Of the research exists, it has been<br />
shown that women and people with a past history of mental<br />
illness have the greatest risk of developing mental disorders<br />
post-event.[17] Higher levels of constant political terror –<br />
measured on a scale that stratified countries according<br />
to the frequency of politically-motivated crises – directly<br />
correlated with higher rates of PTSD and depression.[18]<br />
Resource limitation directly impacts on the quality and<br />
quantity of care provided because LMIC must allocate fiscal<br />
resources frugally. They often chose to apportion money<br />
only to the most severely-affected populations, where the<br />
greatest benefit would be attained. This, in addition to the<br />
deterioration of healthcare services in wartime, culminates<br />
in a dearth of services for all but the most severely affected.<br />
The current global political climate, with the rise of<br />
nationalism and the unprecedented numbers of people<br />
displaced by conflict worldwide, also raise a number of<br />
considerations with respect to disaster preparedness.<br />
[19] There are more people displaced by conflict than ever<br />
before, seeking relocation in countries with greater stability<br />
and economic opportunity. The mental health of refugees<br />
is also influenced by the circumstances in the country of<br />
their resettlement. For example, a study of Latino and Asian<br />
refugees arriving in America found that those who experienced<br />
discrimination, unemployment or who experienced uncertainty<br />
due to unpredictable health insurance had lower self-rated<br />
mental health.[19] These post-settlement factors had a<br />
greater impact on their mental health than pre-settlement<br />
trauma, including war-related trauma.[19] This reflects the<br />
detrimental effect of hostile attitudes from the host country<br />
towards displaced individuals, and should be considered in<br />
the provision of mental health services for these affected<br />
communities.<br />
The impact of political instability on disaster responses<br />
in LMIC was also demonstrated following the earthquake in<br />
Nepal’s Gorkha region. Nepal has a GDP of only $20 billion<br />
USD, and an extremely limited capacity to fund disaster<br />
relief operations. Political instability and slow constitutional<br />
development following abolition of the region’s monarchy has<br />
prevented ratification of rigorous governance surrounding<br />
disaster prevention efforts, such as building codes, which<br />
may have reduced the impact of such an event.<br />
34
Conclusion<br />
Considerations regarding the provision of mental health<br />
support to people in LMIC following disasters rely on a complex<br />
interplay between existing culture, socio-political climate<br />
and financial constraints hindering relief and prevention<br />
efforts. This review has identified that potential avenues for<br />
improvement of mental health services in disaster responses<br />
include: identification of most at-risk subpopulations<br />
including low SES; active integration of cultural sensitivity in<br />
in the provision of mental health support; and measures to<br />
address barriers in uptake of care. Though further research<br />
is needed into the impacts of disaster in LMIC, governments<br />
must actively engage in policy development before these<br />
events occur and learn from previous experiences to protect<br />
their citizens from long-term mental health implications of<br />
disasters.<br />
14. Thapa K. Mental Health in Post-Earthquake Nepal. Nepal Journal of<br />
Epidemiology.5(4):520-1.<br />
15. Marmar CR, Weiss DS, Metzler TJ, Delucchi KL, Best SR, Wentworth<br />
KA. Longitudinal Course and Predictors of Continuing Distress Following<br />
Critical Incident Exposure in Emergency Services Personnel. The Journal of<br />
Nervous and Mental Disease.187(1):15-22.<br />
16. Zhang Y, Baik SH. Race/Ethnicity, disability, and medication<br />
adherence among medicare beneficiaries with heart failure. Journal of<br />
general internal medicine. 2014;29(4):602-7.<br />
17. Ostadtaghizadeh A, Soleimani SV, Ardalan A. Health Consequences<br />
and Management of Explosive Events. Health in Emergencies and Disasters<br />
Quarterly.1(2):71-8.<br />
18. Charlson FJ SZ, Degenhardt L, Chey T, Silove D, Marnane C. Conflict<br />
in Libya on Population Mental Health: PTSD and Depression Prevalence and<br />
Mental Health Service Requirements. PLoS ONE.7(7):e40593.<br />
19. Kim I. Beyond Trauma: Post-resettlement Factors and Mental Health<br />
Outcomes Among Latino and Asian Refugees in the United States. Journal<br />
of Immigrant and Minority Health.18(4):740-8.<br />
Acknowledgements<br />
None<br />
Conflict of Interest<br />
None declared<br />
Correspondence<br />
rose.brazilek1@monash.edu<br />
References<br />
1. Galea S, Brewin CR, Gruber M, Jones RT, King DW, King LA, et al.<br />
Exposure to hurricane-related stressors and mental illness after Hurricane<br />
Katrina. Archives of general psychiatry. 2007;64(12):1427-34.<br />
2. Treatment CfSA. Trauma-Informed Care in Behavioral Health<br />
Services. 2014. US.<br />
3. McFarlane AC, Williams R. Mental health services required after<br />
disasters: learning from the lasting effects of disasters. Depression research<br />
and treatment.1:970194.<br />
4. Norris FH, Friedman MJ, Watson PJ. 60,000 disaster victims speak:<br />
Part II. Summary and implications of the disaster mental health research.<br />
Psychiatry: Interpersonal and biological processes. 2002;65(3):240-60.<br />
5. Gallo LC, Bogart LM, Vranceanu AM, Matthews KA. Socioeconomic<br />
status, resources, psychological experiences, and emotional responses:<br />
a test of the reserve capacity model. Journal of personality and social<br />
psychology.88(2):386-99.<br />
6. Fergusson DM, Horwood LJ, Boden JM, Mulder RT. Impact of a major<br />
disaster on the mental health of a well-studied cohort. JAMA psychiatry.<br />
2014;71(9):1025-31.<br />
7. Norris FH, Alegria M. Mental health care for ethnic minority individuals<br />
and communities in the aftermath of disasters and mass violence. CNS<br />
spectrums. 2005;10(2):132-40.<br />
8. Kar N, Bastia BK. Post-traumatic stress disorder, depression and<br />
generalised anxiety disorder in adolescents after a natural disaster: a<br />
study of comorbidity. Clinical Practice and Epidemiology in Mental Health.<br />
2006;2(1):1-7.<br />
9. Nahar N, Blomstedt Y, Wu B, Kandarina I, Trisnantoro L, Kinsman<br />
J. Increasing the provision of mental health care for vulnerable, disasteraffected<br />
people in Bangladesh. BMC public health.14:708.<br />
10. Lima BR, Pai S, Santacruz H, Lozano J. Psychiatric disorders among<br />
poor victims following a major disaster: Armero, Colombia. J Nerv Ment<br />
Dis.179(7):420-7.<br />
<strong>11</strong>. Sathyanarayana Rao TS. Managing Impact of Natural Disasters :<br />
Some Mental Health <strong>Issue</strong>s. Indian Journal of Psychiatry.46(4):289-92.<br />
12. Catani C, Jacob N, Schauer E, Kohila M, Neuner F. Family violence,<br />
war, and natural disasters: A study of the effect of extreme stress on<br />
children’s mental health in Sri Lanka. BMC Psychiatry. 2008;8(1):1-10.<br />
13. Kar N, Jagadisha, Murali N. Post-traumatic stress disorder in children<br />
following disaster. Kerala Journal of Psychiatry. 2001;16.<br />
35
Factors that contribute to the reduced rates<br />
of cervical cancer screening in Australian<br />
migrant women - a literature review<br />
[Review]<br />
Archana Nagendiram<br />
Archana is a fourth year medical student from James Cook University with interests in<br />
global health and women’s health.<br />
Abstract<br />
AIM: This literature review presents factors that have led to decreased cervical cancer screening rates in Australian<br />
migrant women. It also evaluates past interventions that have been implemented to solve this issue in screening.<br />
METHODS: A wide range of peer reviewed articles from databases such as CINAHL and SCOPUS were analysed to<br />
determine factors that have led to migrant women having a lower cervical cancer screening rate in comparison to<br />
the general Australian population. This review also analysed the reference lists from these articles.<br />
RESULTS: The factors that have led to this reduction in screening rates include cultural differences, limited acculturation,<br />
modesty, and logistical issues. Specific cultural issues such as female genital mutilation and the use of Ayurvedic<br />
medicine in certain ethnic groups may also contribute. There have been interventions aimed at increasing screening<br />
rates, including ethnic media campaigns and education of health professionals, such as doctors and nurses who<br />
work in these communities. However, their effectiveness is uncertain due to a lack of evaluation after implementation.<br />
CONCLUSION: Whilst research has provided a basic understanding of the reasons that have contributed to<br />
the difference in screening between these two populations, there have been insufficient strategies applied to<br />
remedy it. Moreover, there has been inadequate appraisal of current interventions and discussion of the cultural<br />
appropriateness of current programs.<br />
Introduction<br />
This year, the Australian government has renewed the<br />
National Cervical Cancer Screening Program (NCSP) to<br />
incorporate updated screening protocols in accordance<br />
to new research. Hence, it is important to assess the value<br />
of the previous screening protocols in underscreened<br />
populations such as Australia’s migrant women. From 2012-<br />
2013, 58.2% of the target population partook in the NCSP<br />
and since the introduction of organised cervical cancer<br />
screening in Australia, cervical cancer mortality has fallen<br />
by 44% (95% CI 0.51-0.62).[1,2,3] Whilst migrant women<br />
have benefited from screening, the results have not been<br />
as favourable in comparison to the general population. The<br />
incidence of cervical cancer is higher in migrant women from<br />
countries with higher incidence of cervical cancer, including<br />
Sub-Saharan Africa, Central America, South East Asia and<br />
Melanesia.[1]<br />
Consequently, this paper will examine relevant literature<br />
since the current NCSP’s introduction in 1991. It will analyse<br />
the factors that have caused lower screening rates in<br />
migrants, at the level of both the individual and the health<br />
system. It will also analyse past and future interventions that<br />
may reduce these disparities evident in the rates of cervical<br />
cancer screening in Australian migrant women.<br />
Methods<br />
This literature review used various online databases to<br />
source information. It concentrated on articles that surveyed<br />
Australian migrant women, however some larger international<br />
studies were also used to provide global context. CINAHL<br />
was searched with keywords “cervical cancer AND migrant<br />
women”, and SCOPUS was searched with the key words<br />
“cervical cancer AND migrant AND Australia”. Only peer<br />
reviewed journal articles were used, and opinion papers were<br />
excluded in the search. Relevant articles since 1991 were<br />
analysed, from the implementation of the NCSP in Australia.<br />
Additionally, reference lists of relevant articles were examined<br />
using similar inclusion criteria.<br />
What is a pap smear?<br />
Pap smears are the recommended primary screening tool<br />
for cervical cancer by the NCSP. During the procedure, the<br />
doctor collects a cytological sample from the ectocervical<br />
and endocervical canal of the uterus, which is then analysed to<br />
see if any pre-cancerous or cancerous changes are present.<br />
If a cytological abnormality is identified, the patient will then<br />
be referred for colposcopy.[4] Pap smears are routinely<br />
used in general practice and account for approximately 1.7<br />
of 100 consultations.[5] Disease incidence and burden is<br />
reduced in Australia through organised screening for cervical<br />
36
cancer. A key strategy lies in general practitioners instigating<br />
accessible screening, recall systems and opportunistic<br />
screening in their practice.[6]<br />
Factors that prevent regular screening<br />
Lack of Knowledge<br />
Prior to living in Australia, many migrant women from<br />
developing countries had never heard of cervical cancer<br />
screening or understood the risk factors associated with the<br />
disease.[7] This is the result of a lack of organised screening<br />
programs in countries such as Ghana and Vietnam, as their<br />
health systems lack the appropriate human resources and<br />
infrastructure to support such programs.[8,9,10] Hence,<br />
Australian general practitioners are key in providing health<br />
education to new migrant women about the NCSP. A<br />
qualitative study of 21 West African women in Australia<br />
showed that they became informed about pap smears via<br />
public health campaigns and from antenatal care during<br />
pregnancy in Australia. After this initial point of contact, they<br />
had their first pap smear after their pregnancy and then<br />
received reminders every two years.[8] Although migrant<br />
women of reproductive age were educated through these<br />
campaigns, post-menopausal women who have a greater<br />
risk of cancer with age were neglected.[<strong>11</strong>]<br />
Even with health education on cervical cancer, it appears<br />
that migrant women still have a misconstrued understanding<br />
about the NCSP or why they require a pap smear.[8,12]<br />
The surveyed West African migrant women believed that<br />
they did not require a pap smear without a family history of<br />
cervical cancer.[8] Thai and Chinese migrant women also<br />
had misconceptions about the risk factors of cervical cancer<br />
which included promiscuous behaviour, karma or having a<br />
sexual partner who had unhygienic genitalia.[7,13] Some<br />
Chinese migrant women did not understand the role of pap<br />
smears as a screening tool and none of the surveyed women<br />
were aware of the role of Human Papillomavirus (HPV)<br />
in cervical cancer.[7] Furthermore, these migrant women<br />
believed they did not require a pap smear as they were<br />
asymptomatic, had no family history and only had one sexual<br />
partner.[7,8]<br />
Cultural Factors<br />
Language is a common barrier for women from non-English<br />
speaking backgrounds (NESB). Migrant women have a strong<br />
preference to see a doctor who speaks their native language,<br />
regardless of their English proficiency, as it allows for clearer<br />
articulation of their concerns, particularly regarding intimate<br />
procedures.[7] However, a study of migrant women from NESB<br />
portrayed that 75.1% of the surveyed women would prefer<br />
female health providers to male practitioners to conduct their<br />
pap smear, and only 36.4% would travel a large distance<br />
to see a doctor who spoke their own language.[14] Another<br />
study of Thai immigrant women analysed that 61% would<br />
prefer a female general practitioner to perform the pap smear<br />
due to embarrassment.[13] This implied that modesty was<br />
important to migrant women from a NESB, especially as the<br />
newer migrant population often were from very conservative<br />
cultures in the discussion of sexual and reproductive health<br />
is surrounded by stigma.[8] Additionally, cultural beliefs about<br />
maintaining purity may also affect cervical cancer screening,<br />
with Assyrian migrants believing that unmarried women<br />
should not have pap smears as premarital sex is prohibited.<br />
[15] Throughout the literature, it appears that migrant women<br />
feel vulnerable and embarrassed during their pap smears<br />
and would ideally prefer a female doctor who spoke their<br />
language to assist them.[7,8,12]<br />
Moreover, there are factors that are culturally specific, such<br />
as female genital mutilation (FGM) and the use of Ayurvedic<br />
medicine. Approximately 130 million females worldwide have<br />
experienced FGM, mainly in Asia, the Middle East and Africa.<br />
[16] Migrant women with FGM may not wish to undergo pap<br />
smears due to pain, both physical and psychological, and<br />
the reminder of the initial traumatic experience.[8] Ayurvedic<br />
medicine is practised throughout Asia. A study of Thai women<br />
in Brisbane showed these women saw a variety of alternative<br />
medical practitioners; including naturopaths, chiropractors,<br />
herbalists and traditional Chinese healers; both in Australia<br />
and Thailand.[13] As these women would often rely on these<br />
traditional methods for medical care, they were less likely<br />
to present to their general practitioner for ailments and thus<br />
have a reduced chance of undertaking opportunistic cervical<br />
cancer screening.<br />
Finally, the time since migration to Australia is directly<br />
proportional to a woman’s probability of having regular pap<br />
smears.[7] As acculturation occurs, the individuals becomes<br />
more integrated into the Australian community and start to<br />
adopt health preventative behaviours.[13] Single migrants or<br />
those who are married to other migrants took the longest time<br />
to adjust to the health system. On the other hand, migrants<br />
who married an Australian or had a catalytic health event,<br />
such as the birth of a child, had a faster trajectory to health<br />
acculturation.[12]<br />
Other Factors<br />
Various factors further contribute to the lower participation<br />
of migrant women in cervical cancer screening. Several<br />
migrant women from Asia and the Middle East hold a fatalistic<br />
view of health and believe that screening is superfluous, as<br />
they have no control over their destiny.[19] Migrant women<br />
from Yugoslavian and West African communities describe<br />
their fear of their results and do not wish to start looking for<br />
problems that did not exist.[8,20] Similar to women in the<br />
general population, Chinese Australian women describe how<br />
previous negative experiences have deterred them from<br />
having regular pap smears.[7] Additionally, they may simply<br />
forget or have logistical barriers that prevent regular pap<br />
smears, such as lack of transportation or childcare.[7,20]<br />
Interventions<br />
From 2002 to 20<strong>11</strong>, the Australian Research Council<br />
(ARC) spent 7.8% of their funding for people-related research<br />
on the migrant population; insufficient considering migrants<br />
comprise over a quarter of the Australian population.<br />
[21,22] Moreover, the lack of funding for migrant research<br />
37
does not allow for the provision of strongly evidencebased<br />
interventions into migrant health, especially as data<br />
is not available as to the amount of ARC funding allocated<br />
specifically to cervical cancer screening.[22] Nonetheless,<br />
using available Australian data supplemented with some<br />
international publications, the following conclusions can be<br />
drawn about the effectiveness of past interventions and<br />
discussion of what is required for future success.<br />
Educational Campaigns<br />
Migrant women state that they largely receive information<br />
about cervical cancer from health professionals and public<br />
media campaigns. Therefore, the lack of awareness about<br />
pap smears must be targeted in both health and community<br />
settings; through general practice, migrant resource centres<br />
and community centres.[8] General practitioners play a key role<br />
in advocating for cervical cancer screening in consultations<br />
and through reminder letters, as migrant women who have<br />
never had a pap smear may not be comfortable asking for<br />
the test.[7,8,23] Similarly, the use of nurses in community,<br />
refugees health, women’s health, and child and family health<br />
is key in facilitating discussions regarding cancer screening<br />
amongst the migrant population.[8]<br />
The Ethnic Communities Council of Queensland (ECCG)<br />
created the Pilot Cancer Screening Education Program<br />
(PCSEP) which identified cervical cancer screening levels in<br />
various migrant populations before and after their program.<br />
In this program, 76% of participants participated in cervical<br />
cancer screening and this increased to 91% after the PCSEP.<br />
[24] Yet as this result was not statistically significant, we<br />
cannot confirm that this target program would be successful<br />
in increasing cervical cancer screening rates in migrant<br />
populations.<br />
Cultural Sensitivity<br />
As cultural factors play a key role in the decreased<br />
screening rate amongst migrant women, it is essential for<br />
Australian doctors to undertake cultural sensitivity training.<br />
This may improve understanding of factors affecting women<br />
from certain cultures such as modesty and fatalistic views of<br />
health.[7] This will allow health practitioners to appropriately<br />
tailor their consultations and the way that they promote<br />
cervical cancer screening with their migrant patients.<br />
There may also be reduced rates of cancer screening<br />
referrals from migrant doctors to patients of their own<br />
nationality. A study of Korean American doctors showed<br />
that there were reduced referral rates of colorectal cancer<br />
screening for their Korean patients. This was because they<br />
understood the cultural sensitivities surrounding cancer<br />
screening and perceived that compliance would be lower<br />
amongst their Korean patients.[25] It is key for doctors<br />
providing carer to patients of the same nationality to undergo<br />
training in cancer screening. The significance of bilingual<br />
health practitioners cannot be underestimated, as migrants<br />
prefer to see practitioners of the same nationality.[7,23] In<br />
the Vietnamese community, information sessions for bilingual<br />
practitioners about cervical cancer has been documented,<br />
but the effectiveness of this intervention has not been<br />
assessed.[23]<br />
Use of ethnic media<br />
Previous interventions have used ethnic media as a health<br />
promotion strategy to increase cervical cancer screening in<br />
various migrant populations.[23,26] Between 1991 and 1994,<br />
Pap Test Victoria conducted three sets of interventions in<br />
ethnic media outlets for over 12 migrant groups including<br />
Vietnamese, Chinese, Arabic and Turkish populations.<br />
During these interventions, the respective ethnic media<br />
outlets conducted live interviews, paid announcements and<br />
competitions with prizes. These three interventions led to an<br />
increase in screening compliance by 6.7% (95% CI 4.4-9.2).<br />
[26] As ethnic media can be utilised for health promotion and<br />
appears to be an effective method of increasing screening<br />
uptake, funding should be allocated for a nationwide ethnic<br />
media campaign on cervical screening.<br />
Conclusion<br />
Lower rates of cervical cancer screening in migrant<br />
women is a multifaceted issue. Factors contributing to these<br />
lower rates include lack of knowledge, cultural differences,<br />
limited acculturation and logistical issues. While research has<br />
been undertaken to understand the cause of the decreased<br />
participation of migrant women in regular pap smears, there<br />
have not been sufficient evidence-based interventions to<br />
address the issue. Although the government has redesigned<br />
the NCSP to reflect current medical research, there has<br />
been little evaluation of the cultural appropriateness of the<br />
current NCSP and the effectiveness of previous interventions<br />
to increase participation amongst the migrant population.<br />
The renewal of the NCSP should parallel the increased<br />
number of research projects that occurred during its initial<br />
implementation, as this is necessary to provide updated<br />
information on cervical cancer screening to migrant<br />
women. This will then allow for the application of evidencebased<br />
interventions to increase pap smear rates in this<br />
underscreened population.<br />
Acknowledgements<br />
None<br />
Conflict of Interest<br />
None declared<br />
References<br />
1. Aminisani N, Armstrong BK, Egger S, Canfell K. Impact of<br />
organised cervical cancer screening on cervical cancer incidence and<br />
mortality in migrant women in Asutralia. BMC Cancer. 2012;12(1):491-501.<br />
2. Australian Institute of Health and Welfare. Cerivcal screening in<br />
Australia 2012-2013. [Internet]. 2015 [updated 2015 May 1; cited <strong>2017</strong><br />
May 20]. Available from: http://www.aihw.gov.au/WorkArea/DownloadAsset.<br />
aspx?id=60129550872.<br />
3. Simonella L, Canfell K. The impact of a two- versus three-yearly<br />
cervical screening interval recommendation on cervical cancer incidence<br />
and mortality: an analysis of trends in Australia, New Zealand, and England.<br />
Cancer Causes Control. 2013;24(9):1727-1736. doi: 10.1007/s10552-013-<br />
0250-9.<br />
4. Shader RI. The PAP test and the pap smear. Clin Ther.<br />
38
2015;37(1):1-3. doi: 10.1016/j.clinthera.2014.12.002.<br />
5. Australian Institute of Health and Welfare. General practice<br />
activity in 2009-10. [Internet]. 2010 [updated 2010 Dec 8;cited <strong>2017</strong> May 5].<br />
Available from: http://www.aihw.gov.au/publication-detail/?id=6442472433.<br />
6. Munro A, Pavicic H, Leung Y, Westoby V, Steel N, Semmens J et al.<br />
The role of general practitioners in the continued success of the National<br />
Cervical Screening Program. Aust Fam Physician. 2014;43(5):293-296.<br />
7. Kwok C, White K, Roydhouse JK. Chinese-Australian women’s<br />
knowledge, facilitators and barriers related to cervical cancer screening:<br />
a qualitative study. J Immigr Minor Health. 20<strong>11</strong>;13(6):1076-1083. doi:<br />
10.1007/s10903-0<strong>11</strong>-9491-4.<br />
8. Ogunsiji O, Wilkes L, Peters K, Jackson D. Knowledge, attitudes<br />
and usage of cancer screening among West African migrant women. J Clin<br />
Nurs. 2013;22(7-8):1026-1033. doi: 10.<strong>11</strong><strong>11</strong>/jocn.12063.<br />
9. Sankaranarayanan R, Nessa A, Esmy PO, Dangou JM. Visual<br />
inspection methods for cervical cancer prevention. Best Pract Res Clin<br />
Obstet Gynaecol. 2012;26(2):221-232. doi: 10.1016/j.bpobgyn.20<strong>11</strong>.08.003.<br />
10. Lesjak M, Hua M, Ward J. Cervical screening among immiagrant<br />
VIetnamese women seen in general practice: current rates, predictors<br />
and potential recruitment strategies. Aust NZ J Public Health. 1999; 23(2):<br />
168-173.<br />
<strong>11</strong>. White MC, Holman DM, Boehm JE, Peipins LA, Grossman M,<br />
Henley SJ. Age and cancer risk: a potentially modifiable relationship. Am J<br />
Prev Med. 2014;46(3 Suppl 1):S7-15. doi: 10.1016/j.amepre.2013.10.029.<br />
12. Terry D, Ali M, Le Q. Asian migrants’ lived experience and<br />
acculturation to Western health care in rural Tasmania. Aust J Rural Health.<br />
20<strong>11</strong>;19(6):318-323. doi: 10.<strong>11</strong><strong>11</strong>/j.1440-1584.20<strong>11</strong>.01229.x.<br />
13. Jirojwong S, Manderson L. Beliefs and Behaviors About<br />
Pap and Breast Self-Examination Among Thai Immigrant Women in<br />
Brisbane, Australia. Women & Health. 2001;33(3-4):53-73. doi: 10.1300/<br />
J013v33n03_04.<br />
14. Henderson S, Kendall E, See L. The effectiveness of culturally<br />
appropriate interventions to manage or prevent chronic disease in culturally<br />
and linguistically diverse communities: a systematic literature review.<br />
Health Soc Care Community. 20<strong>11</strong>;19(3):225-249. doi: 10.<strong>11</strong><strong>11</strong>/j.1365-<br />
2524.2010.00972.x.<br />
15. Ussher JM, Rhyder-Obid M, Perz J, Rae M, Wong TWK, Newman<br />
P. Purity, Privacy and Procreation: Constructions and Experiences of Sexual<br />
and Reproductive Health in Assyrian and Karen Women Living in Australia.<br />
Sexuality & Culture. 2012;16(4):467-485. doi: 10.1007/s12<strong>11</strong>9-012-9133-6.<br />
16. Allen B, Oshikanlu R. Female Genital Mutilation: A practical guide<br />
for health visitors and school nurses. Community Pract. 2015;88(12):30-33.<br />
17. Taylor RJ, Mamoon HA, MOrrell SL, Wain GV. Cervical Screening<br />
in Migrants to Australia. Aust NZ J Public Health. 2001; 25(1): 55-61.<br />
18. Wain G, Morrell S, Taylor R, Mamoon H, Bodkin N. Variation<br />
in cervical cancer screening by region, socio-economic, migrant and<br />
Indigenous status in women in New South Wales. Gynecol. Oncol. 2001;<br />
41(3): 320-325.<br />
19. Aminisani N, Armstrong BK, Canfell K. Cervical cancer screening<br />
in Middle Eastern and Asian migrants to Australia: a record linkage study.<br />
Cancer Epidemiol. 2012;36(6):e394-400. doi: 10.1016/j.canep.2012.08.009.<br />
20. Fernbach M. Exploration of factors linked with high cervical<br />
cancer rates in women from the former Yugoslavia in Victoria, Australia.<br />
Ethn Health. 2002;7(3):209-220. doi: 10.1080/1355785022000042033.<br />
21. ABS. 3412.0 - Migration, Australia (2013-2014). website. http://<br />
www.abs.gov.au/ausstats/abs@.nsf/mf/3412.0. Published 2015.<br />
22. Renzaho A, Polonsky M, Mellor D, Cyril S. Addressing migrationrelated<br />
social and health inequalities in Australia: call for research funding<br />
priorities to recognise the needs of migrant populations. Aust Health Rev.<br />
Jul 13 2015. doi: 10.1071/AH14132.<br />
23. Cheek J, Fuller J, Gilchrist S, Maddock A, Ballantyne A.<br />
Vietnamese women and pap smears: issues in promotion. Aust NZ J Public<br />
Health. 1999.<br />
24. Cullerton K, Gallegos D, Ashley E, et al. Cancer screening<br />
education: can it change knowledge and attitudes among culturally and<br />
linguistically diverse communities in Queensland, Australia? Health Promot<br />
J Austr. Jun 29 2016. doi: 10.1071/HE15<strong>11</strong>6.<br />
25. Jo AM, Maxwell AE, Rick AJ, Cha J, Bastani R. Why are Korean<br />
American physicians reluctant to recommend colorectal cancer screening<br />
to Korean American patients? Exploratory interview findings. J Immigr Minor<br />
Health. Aug 2009;<strong>11</strong>(4):302-309. doi: 10.1007/s10903-008-9165-z.<br />
26. Mitchell H, Hirst S, Mitchell JA, Staples M, Torcello N. Effect of<br />
ethnic media on cervical cancer screening rates. Aust N Z J Public Health.<br />
1997; 21(2). 265-267.<br />
39
Medical electives in resource-poor settings:<br />
Are we doing more harm than good?<br />
[Review]<br />
Gabrielle Georgiou<br />
Gabrielle is a final-year medical student (VI) at the University of New South<br />
Wales. She has a particular interest in global health and medical education.<br />
Abstract<br />
Medical students from around the world desire ever-increasing global health experiences and education,<br />
particularly from international medical electives. However, while elective experiences offer a number of<br />
potential benefits for students and sending institutions alike, recent evidence suggests that significant<br />
practical, social and ethical challenges may result, specifically in resource-poor settings. Ideally, there<br />
should be an opportunity for students to engage with elements of a global health program or some form<br />
of pre-departure training prior to undertaking a medical elective, with the aim being to engage with social<br />
determinants of health, and aspects of service learning. Furthermore, additional research is required to<br />
ensure that medical electives do not detract in any way from the pursuit of global health equity and the<br />
provision of care in these locations.<br />
Introduction<br />
Interest in international medical electives is burgeoning,<br />
with medical students from around the world desiring global<br />
health content in their curricula,[1] and greater discovery<br />
traversing international socio-cultural borders.[2-8] In the<br />
United States, for example, of ninety-six medical schools<br />
surveyed, 87% reported availability of international clinical<br />
electives, 45% offered preclinical research abroad, and<br />
61% offered international opportunities over school holidays.<br />
[9] Here in Australia, international health is often explored in<br />
medical schools through compulsory elective terms, which<br />
typically occur over a period of 6-8 weeks and may take<br />
place in developing countries.[1]<br />
Medical electives may involve experiences in developing<br />
nations with pronounced inequities in health and socioeconomic<br />
development.[1, 10] Such electives have been<br />
described in the literature with various terms - from<br />
‘international medical experiences’, ‘global health programs’,<br />
‘medical electives’, and ‘global health experiences’, to the<br />
use of other, more controversial definitions, such as “medical<br />
voluntourism”, “fly-by medical care”, or “duffel-bag medicine”.<br />
[6] While elective experiences offer potential benefits for<br />
medical students and sending institutions alike, recent<br />
evidence suggests the potential for significant practical and<br />
ethical challenges, exacerbating global health inequities.[2-4,<br />
7, 8, <strong>11</strong>-14]<br />
Motivations<br />
Certain factors appear to influence student involvement<br />
in medical electives. These include altruistic intent, curiosity,<br />
having a sense of adventure and hopes of language<br />
development, as well as the allure of the opportunity to<br />
experience medical practice outside the scope of one’s<br />
normal hospital and community setting.[15] Other benefits<br />
which may result from experiencing a medical elective include<br />
the prospect of improving clinical skills, enabling personal<br />
transformation,[12] increasing tropical medicine knowledge,<br />
gaining cross-cultural competency, and improving overall<br />
confidence, independence and resourcefulness levels.[5]<br />
Benefits<br />
Electives may offer an ideal setting for students to engage<br />
with preventative health measures that are utilised around<br />
the world.[9] Students can develop a greater understanding<br />
of effective resource management and public health<br />
strategy implementation, improve their awareness of the<br />
social determinants of health, and improve their competency<br />
as global health advocates.[5] There is also evidence that<br />
students’ increase their willingness to assist underserved<br />
populations and levels of social responsibility when they<br />
experience medicine in another country, particularly in the<br />
developing world.[9, 16]<br />
International medical experiences are also said to<br />
facilitate the process of service learning- that is, a structured<br />
learning style incorporating community service, experiential<br />
learning, as well as adequate preparation and reflection.[9,<br />
17] Consciousness-raising, self-efficacy, and networking<br />
capability, are three notable outcomes which may be<br />
facilitated by this service learning style.[14]<br />
Institutions hosting medical students may also benefit<br />
through improved international partnerships, promoting<br />
40
a potential workforce of international health workers in<br />
the future, reciprocal training opportunities for local staff<br />
and students to work abroad, equipment donation, and/or<br />
potential financial compensation.[5]<br />
Concerns<br />
Nonetheless, medical electives have the potential to<br />
cause serious ethical breaches, particularly those resulting<br />
from a medical student practising medicine beyond their<br />
level of competency.[4] There have been growing concerns<br />
that students are utilising elective opportunities to practise<br />
skills, enhance their resumes, and to travel to ‘exotic’ places,<br />
which can result in vulnerable communities serving as a<br />
means for students to merely fulfill selfish ends, as opposed<br />
to students serving to address the needs of the community.<br />
[7, 14, 16] Some have argued that electives in resource-poor<br />
settings are being used as a glorified form of tourism, with<br />
no known sustainable benefits for the receiving community.<br />
[13] Furthermore, any form of pre-departure training or global<br />
health education as a pre-requisite for such an elective is<br />
often missing, limited, or narrow in focus.[15]<br />
For the student specifically, there may be health risks<br />
involved, substantial costs assumed, the potential for<br />
cultural shock, and the likelihood of experiencing ethicallychallenging<br />
situations, which may include pressure to exceed<br />
the student’s role, and also perform procedures without<br />
adequate supervision.[5] There may be uncertainty about<br />
how best to contribute, working beyond the student’s scope<br />
of practice, navigating through unknown medical cultures,<br />
and leaving a subsequent gap in care provision when the<br />
student returns home. There are various other issues which<br />
may result, including failure to obtain truly informed consent<br />
due to language, cultural or other barriers, lack of adequate<br />
medical knowledge, and a lack of cultural awareness, which<br />
can all potentially lead to patient harm.[5]<br />
In the case of elective work in Honduras, for example,<br />
medical tourism is considered harmful, entrenching<br />
paternalism and inequitable relationships.[14] It is argued that<br />
while educational and social benefits may potentially occur,<br />
they are not natural consequences of these international<br />
experiences, but instead, examples of practical outcomes<br />
which must be nurtured and developed through significant<br />
education, reflection, and long-term relationship building.[14]<br />
Recommendations<br />
Healthcare practitioners may provide effective input<br />
during a short-term medical elective only if they have<br />
adequate knowledge, skills and ethical preparation prior to<br />
their departure.[18] There must be a shift in focus from the illprepared<br />
student who faces significant ethical dilemmas in<br />
global health on an international medical elective, to greater<br />
provision of support by teachers and institutions, prior to such<br />
an experience, given they ultimately have a responsibility to<br />
provide global health training and awareness of potential<br />
challenges.[4, 15, 19, 20]<br />
Students should be given pre-departure training, which<br />
may involve reflecting upon potential ethical challenges<br />
and discussing issues regarding resource shortages and<br />
other cultural or professional differences.[17] There should<br />
be an opportunity for students to engage with elements of a<br />
global health program prior to their undertaking of a medical<br />
elective, with the deliberate aim being to engage with social<br />
determinants of health.[7, 12, 13, 15] This may encourage<br />
students to question social inequities and shift the experience<br />
of a medical elective into a period of transformative learning.<br />
[19] This may in turn contribute to social change within the<br />
medical realm - which is a vital need for improving global<br />
health.[15]<br />
Further, student-led groups, databases and/or forums<br />
could be utilised to facilitate conversation, mentoring<br />
opportunities, and more personalised pre-departure training.<br />
Discussion amongst students who have been on an elective<br />
previously may allow for reflection upon these experiences<br />
and any challenges faced, as well as the sharing of<br />
knowledge with future cohorts who have not yet undertaken<br />
their placements.<br />
A global health curriculum would ideally examine ethical<br />
issues associated with working with vulnerable populations,<br />
and incorporate potential health and personal safety<br />
challenges associated with working in resource-poor<br />
environments.[3, 4, 20, 21] Experiential data suggests that<br />
ethical dilemmas are often part of medical electives and<br />
that, in most cases, medical students are not adequately<br />
trained to negotiate their way through ethically-troublesome<br />
situations.[19] There is a clear necessity for training so<br />
that students are able to recognise when to ‘say no’ during<br />
such experiences, and are able to learn from challenging<br />
situations.[3, 4, 16]<br />
The Working Group on Ethics Guidelines for Global<br />
Health Training (WEIGHT) has developed a set of guidelines<br />
regarding ethical issues and best practice for global health<br />
training. It simultaneously encourages efforts to continuously<br />
assess and evaluate the potential benefits and harms of<br />
programs being undertaken worldwide.[2] Trainees must<br />
understand their personal responsibility during a global<br />
health experience, to ensure it is a primarily positive one, and<br />
to recognise that their actions and behaviours can have farreaching<br />
long-term implications.[2]<br />
Evidence suggests that one of the most effective ways<br />
of teaching skills relating to global health - such as ethical<br />
and cultural competency - is through service learning.[17]<br />
Service learning incorporation relies on increased academic<br />
programming, fostering sustainable hospital partnerships,<br />
and encouraging mentorship and reflection for students<br />
involved, prior to, during and after their elective experiences.<br />
[21] Reflecting on the purpose of their volunteer experience,<br />
as well as their capacities and goals, will inform a more<br />
culturally-appropriate provision of care abroad, and will<br />
allow the student to recognise that good intentions alone<br />
are not necessarily sufficient preparation or justification for<br />
volunteering or working overseas.[20] Thus, the application<br />
of a simulation-based approach to global health ethics<br />
education prior to an elective may be useful in dealing with<br />
41
the tensions which exist between service learning and the<br />
respect of patient rights and well-being.[17]<br />
Social justice-oriented approaches to service learning,<br />
coupled with active critical reflection, also serve viable<br />
pedagogical approaches for learning the health advocate<br />
role.[10] This means that students should be able to better<br />
recognise and address relevant ethical and professional<br />
issues, with a greater understanding and appreciation<br />
of altruism, social justice, autonomy, and integrity as a<br />
result.[10] When a student does undertake an elective in a<br />
developing country, such experience leads to higher levels<br />
of community health knowledge on return, a greater sense<br />
of what it means to be vulnerable, a heightened awareness<br />
of the social determinants of health, and an appreciation<br />
of the importance of socially responsible approaches for<br />
community engagement and health advocacy.[10]<br />
Another important consideration is to enable bi-directional<br />
flow of medical students through formal partnerships between<br />
university institutions. This can facilitate more positive<br />
elective experiences through sustainable relationships and<br />
effective involvement in medical care, as well as encouraging<br />
an international medical workforce in the future.[5] Along<br />
with fostering such connections, skills building in crosscultural<br />
effectiveness, long-term sustainability planning, and<br />
local capacity building may help to produce more effective<br />
overseas opportunities with meaningful outcomes.[7]<br />
Discussion<br />
Overall, there is a clear need for individuals who wish to<br />
undertake medical electives in the future to reflect upon<br />
ethical and best practice guidelines prior to departure,[2] and<br />
to subsequently decide whether the experience is right for<br />
them.[12] It would also be of benefit to engage in conversation<br />
with previous cohorts about their elective experiences,<br />
enabling a baseline understanding of any challenges that lie<br />
ahead. Pre-departure, students should aim to gain as much<br />
contextual knowledge as possible in relation to their host<br />
country, including the language, the specific local needs,<br />
the details of the participating institution and the work being<br />
carried out. Students must recognise the possible ethical<br />
consequences of the work being done, and appreciate the<br />
potential impact they might have during such an experience.<br />
[12, 16]<br />
By incorporating a greater emphasis on learning and on<br />
reflection prior to, during, and after an international medical<br />
elective experience, students will be better placed to question<br />
their values, assumptions, and beliefs to help mitigate<br />
the potential harms which their placement may cause.<br />
[15] Students must actively question themselves and their<br />
surroundings, consider the ways in which healthcare is being<br />
delivered, and engage with potential ethical dilemmas and<br />
broader social, political and economic concerns underlying<br />
their medical provision, without necessarily being engaged<br />
in the direct provision of medical care.[<strong>11</strong>] Indeed, practising<br />
beyond one’s capabilities as a medical student is central<br />
to the potential harm which may result during an overseas<br />
elective in a resource-poor environment, particularly when<br />
this is coupled with a lack of adequate supervision.<br />
Education and planning are essential in minimising harm<br />
to host communities. It is necessary to have well-defined<br />
objectives and structured clinical experiences in place for<br />
students while abroad, which may be promoted by institutions<br />
and educators through mandatory global health education to<br />
ensure medical electives are carried out to the highest ethical<br />
standards.[8, 19] At all stages, electives must be completed<br />
in a way that acknowledges any underlying power balances,<br />
ethical challenges, and resource differentials to provide<br />
community-led efforts which are focused on sustainable<br />
development and community health gains.[7]<br />
There is an undeniable need for more global health<br />
Global Health Programs Abroad<br />
1. University of Saskatchewan, Canada: the ‘Making the Links’ program provides an opportunity for<br />
undergraduate medical students to participate in a local student-led inner-city clinic, a Northern Aboriginal<br />
community health initiative and a long-standing service-learning project in Mozambique over two years. This<br />
includes the provision of a supplementary clinical curriculum, guided and facilitated reflections, as well as a<br />
complementary global health course and language courses.[15]<br />
2. University of British Columbia, Canada: ‘First, Do No Harm: Global Health Initiatives, Ethics and Social<br />
Responsibility’ is a piloted series of interactive workshops.[16] Participants analyse case studies exploring<br />
different ethical dilemmas. Results have indicated that this approach to learning and reflection is necessary<br />
before participating in a global health initiative, and that problem-based learning is effective in teaching<br />
students to engage in the process of identifying and addressing ethical issues.[16]<br />
3. University of Arizona, United States: a four-week immersion program undertaken by students prior to an<br />
overseas placement covers a range of international health topics.<br />
42
education to be incorporated into the curriculum for medical<br />
students around the world, with rubrics containing detailed<br />
expectations and outcomes that are applicable to global<br />
health experiences.[21] Educators have a responsibility<br />
to their students to facilitate the development of skills in<br />
cultural competency, compassion, and public health, as well<br />
as encouraging them to understand the potential ethical<br />
challenges they may encounter.[9]<br />
Additional qualitative research is required to ensure that<br />
the expectations, attitudes, and experiences of healthcare<br />
institutions accepting elective students are clearly<br />
understood. Recognising the benefits and concerns of<br />
elective programs in resource-poor settings in greater depth<br />
will ensure that electives do not detract in any way from the<br />
pursuit of global health equity and the provision of care in<br />
these locations.[6]<br />
Acknowledgements<br />
None<br />
13. Snyder J, Dharamsi S, Crooks VA. Fly-by medical care: conceptualizing<br />
the global and local social responsibilities of medical tourists and physician<br />
voluntourists. Globalization and health. 20<strong>11</strong>;7(1):1.<br />
14. McLennan S. Medical voluntourism in Honduras: ‘Helping’ the poor?<br />
Progress in Development Studies. 2014;14(2):163-79.<br />
15. Hanson L, Harms S, Plamondon K. Undergraduate International<br />
Medical Electives: Some Ethical and Pedagogical Considerations. Journal of<br />
Studies in International Education. 20<strong>11</strong>;15(2):171-85.<br />
16. Dharamsi S, OseiTwum JA, Whiteman M. Socially responsible<br />
approaches to international electives and global health outreach. Medical<br />
education. 20<strong>11</strong>;45(5):530-1.<br />
17. Logar T, Le P, Harrison JD, Glass M. Teaching Corner: “First Do<br />
No Harm”: Teaching Global Health Ethics to Medical Trainees Through<br />
Experiential Learning. Journal of Bioethical Inquiry. 2015;12(1):69-78.<br />
18. Asgary R, Junck E. New trends of short-term humanitarian medical<br />
volunteerism: professional and ethical considerations. Journal of medical<br />
ethics. 2013;39(10):625-31.<br />
19. Petrosoniak A, McCarthy A, Varpio L. International health electives:<br />
thematic results of student and professional interviews. Medical Education.<br />
2010;44(7):683-9.<br />
20. McCall D, Iltis AS, editors. Health Care Voluntourism: Addressing<br />
Ethical Concerns of Undergraduate Student Participation in Global Health<br />
Volunteer Work2014: Springer.<br />
21. Stoltenberg M, Rumas N, Parsi K. Global health and service learning:<br />
lessons learned at US medical schools. Medical education online. 2012;17.<br />
Conflict of Interest<br />
None declared<br />
Correspondence<br />
gabbygeorgiou@gmail.com<br />
References<br />
1. Fox GJ, Thompson JE, Bourke VC, Moloney G. Medical students,<br />
medical schools and international health. Medical Journal of Australia.<br />
2007;187(9):536.<br />
2. Crump JA, Sugarman J, the Working Group on Ethics Guidelines for<br />
Global Health T. Ethics and Best Practice Guidelines for Training Experiences<br />
in Global Health. The American Journal of Tropical Medicine and Hygiene.<br />
2010;83(6):<strong>11</strong>78-82.<br />
3. Banatvala N, Doyal L. Knowing when to say” no” on the student<br />
elective; students going on electives abroad need clinical guidelines. British<br />
Medical Journal. 1998;316(7142):1404-6.<br />
4. Shah S, Wu T. The medical student global health experience:<br />
professionalism and ethical implications. Journal of medical ethics.<br />
2008;34(5):375-8.<br />
5. Bozinoff N, Dorman KP, Kerr D, Roebbelen E, Rogers E, Hunter A, et<br />
al. Toward reciprocity: host supervisor perspectives on international medical<br />
electives. Medical education. 2014;48(4):397-404.<br />
6. DeCamp M, Enumah S, O’Neill D, Sugarman J. Perceptions of a<br />
short-term medical programme in the Dominican Republic: voices of care<br />
recipients. Global public health. 2014;9(4):4<strong>11</strong>-25.<br />
7. Melby MK, Loh LC, Evert J, Prater C, Lin H, Khan OA. Beyond Medical<br />
“Missions” to Impact-Driven Short-Term Experiences in Global Health<br />
(STEGHs): Ethical Principles to Optimize Community Benefit and Learner<br />
Experience. Academic Medicine. 9000;Publish Ahead of Print.<br />
8. Ketheeswaran P. Good intentions with unknown consequences:<br />
understanding short term medical missions: SCHOOL OF MEDICINE Thesis<br />
GOOD INTENTIONS WITH UNKNOWN CONSEQUENCES: UNDERSTANDING<br />
SHORT TERM MEDICAL MISSIONS by PAVINARMATHA KETHEESWARAN<br />
BS, University of Florida; 2015.<br />
9. Ackerman LK. The Ethics of Short-Term International Health<br />
Electives in Developing Countries. Annals of Behavioral Science and Medical<br />
Education. 2015;16(2):40-3.<br />
10. Dharamsi S, Richards M, Louie D, Murray D, Berland A, Whitfield M,<br />
et al. Enhancing medical students’ conceptions of the CanMEDS Health<br />
Advocate Role through international service-learning and critical reflection:<br />
A phenomenological study. Medical Teacher. 2010;32(12):977-82.<br />
<strong>11</strong>. Wallace LJ. Does Pre-Medical ‘Voluntourism’Improve the Health of<br />
Communities Abroad? Journal of Global Health Perspectives. 2012;1:1-5.<br />
12. Citrin DM. “Paul Farmer Made Me Do It”: A Qualitative Study of Short-<br />
Term Medical Volunteer Work in Remote Nepal: University of Washington;<br />
20<strong>11</strong>.<br />
43
IFMSA - 5 letters with one big mission!<br />
Australian Medical Students attend the IFMSA<br />
66th General Assembly in Montenegro<br />
[Conference report]<br />
Aysha Abu-sharifa (University of Notre Dame Fremantle), Stormie de Groot<br />
(University of New England), Julie Graham (James Cook University), Justine<br />
Thomson (University of Wollongong)<br />
The International Federation of Medical<br />
Students Associations, or IFMSA, was founded<br />
in 1951 in response to the overwhelming global<br />
challenges following World War II. Committed<br />
to the ideals of the Alma Ata Declaration<br />
and “Health for All” (2007), the founders<br />
believed that medical students should not<br />
be passive bystanders, but rather, use their<br />
ability to create lasting and meaningful change<br />
through collaboration and innovation. Today,<br />
the organisation represents over 1.3 million<br />
medical students from over 122 countries<br />
worldwide, with the Australian Medical<br />
Students’ Association (AMSA) having been part<br />
of the organisation for many years.<br />
The IFMSA is involved in a wide range of<br />
global health advocacy, public health, primary<br />
health and clinical health projects. This<br />
encompasses training arms, medical student<br />
exchange programs and collaborative public<br />
health projects. There are several standing<br />
committees working within specific areas of<br />
global health, including Public Health (SCOPH),<br />
Sexual and Reproductive Health (SCORA),<br />
Medical Education (SCOME), Human Rights<br />
and Peace (SCORP) and Professional and<br />
Research Exchanges (SCOPE/SCORE).<br />
The IFMSA is also divided into regions which<br />
allow for effective collaboration across<br />
geographically similar areas, such as the Asia<br />
Pacific Region, of which AMSA is a member. The<br />
IFMSA offers the opportunity for all Australian<br />
medical students, through AMSA, to be involved<br />
in student activities on an international scale.<br />
Most recently, AMSA sent a team of 14<br />
Australian delegates to attend the IFMSA’s 66th<br />
General Assembly (GA) in Budva, Montenegro,<br />
from March 2-8, <strong>2017</strong>. The team was led by<br />
Julie Graham, AMSA Global Health’s Vice Chair<br />
International and acting IFMSA Australian<br />
President, along with Liz Bennett, AMSA Global<br />
Health’s Chair. The General Assembly is likened<br />
to an international version of an AMSA Council<br />
in which policies are discussed and debated,<br />
changes to operational processes are made,<br />
new member states are voted in and prepared<br />
statements are read. Most of these processes<br />
take place in plenary sessions, where Julie and<br />
Liz represented Australia on issues relating to<br />
medical education and general global health.<br />
Charlotte O’Leary presents youth declaration on<br />
NCDs<br />
Along with the plenary sessions, each<br />
standing committee also conducts their own<br />
parallel SCORA sessions for members. The<br />
Australian members were divided between<br />
many of these half-day standing sessions,<br />
which allowed the Australian team members<br />
to think about being part of the global health<br />
community and how IFMSA projects could open<br />
many doors on this level. Other key components<br />
of the program include joint sessions between<br />
standing committees, National Member<br />
Organisation meetings and plenaries, where<br />
delegates participate as guests to support and<br />
advise the delegation leaders.<br />
44
This year’s GA was marked by several<br />
significant achievements by the Australian<br />
team. Most notably Australian student<br />
Charlotte O’Leary was responsible for the Non-<br />
Communicable Disease (NCD) Youth Caucus,<br />
which lead to the creation and adoption by the<br />
IFMSA of the “Budva Youth Declaration: A Call<br />
to Action on Non-communicable Diseases”.<br />
Charlotte has just completed a 3-month<br />
internship at the World Health Organization<br />
(WHO) in Geneva and was appointed by the<br />
IFMSA to organise and moderate the NCDthemed<br />
events. AMSA Global Health Chair,<br />
Liz Bennett, was also one of the panellists<br />
amongst many prestigious speakers and<br />
discussed the linkage between nutrition, food<br />
systems, and NCDs. The Youth Caucus formed<br />
the key components of the themed events on<br />
NCDs. It was opened at the IFMSA GA opening<br />
ceremony by Dr Bente Mikkelsen, Head of the<br />
WHO Commission on NCDs, and was followed<br />
by two panel discussions.<br />
Prerna Diksha<br />
AMSA was also represented at the IFMSA<br />
GA Activities Fair, where over 150 projects<br />
worldwide were featured and discussed with<br />
delegates. Three Australian projects were<br />
presented, including Project Burans, presented<br />
by Prerna Diksha of Melbourne University,<br />
Crossing Borders, a National Project of AMSA<br />
Global Health, presented by Aysha Abu-sharifa,<br />
and AMSA’s Newcastle NewGHC presented<br />
by Adelaide Pratt (Logistics Convenor, AMSA<br />
2016 Newcastle Global Health Conference).<br />
Project Burans is a philanthropic mental health<br />
initiative of the Emmanuel Hospital Association,<br />
the largest non-governmental provider of<br />
healthcare in India. It won second place for<br />
founder Prerna Diksha and other members of<br />
Melbourne University, out of almost 150 other<br />
entries!<br />
Participation in both policy writing and<br />
review represents a significant opportunity for<br />
involvement in any IFMSA GA. Julie Graham,<br />
delegation leader, was a member of the Policy<br />
commission team for the IFMSA Rural Health<br />
Policy, along with 2 other international team<br />
members. This policy received input from<br />
around the world prior to the GA, including<br />
ample suggestions from Australian medical<br />
students. The Rural Health Policy was one of<br />
12 propositions that were successfully passed<br />
during the plenary policy session.<br />
The Pre GA provides a great opportunity to<br />
work with and get to know a smaller proportion<br />
of students attending the GA. Medical science<br />
student, Stormie de Groot attended a Pre-GA<br />
workshop, “Transforming Our World by 2030:<br />
Reaching the Sustainable Development Goals<br />
(SDGs)”, which focused on how and why the<br />
SDGs were developed, their purpose, and how<br />
medical students could work towards achieving<br />
them.<br />
“It was insightful and humbling to<br />
see the work that was already being<br />
achieved by National Medical student<br />
Organisations (NMOs) around the world,<br />
amongst various social, cultural and<br />
political contexts. Overall, it challenged<br />
all of us to adopt the SDG framework<br />
into our existing AMSA Global Health<br />
Projects and beyond through our AMSA<br />
Sustainable Development Policy (2016).”<br />
-Stormie de Groot, University of New England.<br />
The activities of the Sexual and Reproductive<br />
Health stream within the IFMSA represent<br />
a key area for involvement for Australian<br />
medical students, many of whom are engaged,<br />
interested and skilled in this field. Justine<br />
Thomson, Education Officer for AMSA Global<br />
45
Health, was involved in presenting a session<br />
within the SCORA streams on Comprehensive<br />
Sexuality Education.<br />
“As a health and physical education<br />
teacher prior to medical school, I enjoyed<br />
the opportunity to take part in the General<br />
Assembly and share my knowledge in<br />
[sexual health]. My experiences within the<br />
general SCORA sessions were excellent<br />
and the guest speakers were highlights,<br />
particularly Dr Lale Say from the<br />
Department of Reproductive Health and<br />
Research, WHO, speaking on Female<br />
Genital Mutilation, and new guidelines in<br />
this space.”<br />
-Justine Thomson, University of Wollongong.<br />
Dr Elijah Painsil, from the Yale School of<br />
Medicine, also presented a keynote address<br />
around the challenges of children and<br />
adolescents living with HIV.<br />
In addition to the significant academic<br />
opportunities, the IFMSA General Assembly<br />
allowed the Australian team members to<br />
grow and develop on a personal level through<br />
their interactions with other delegates. It<br />
was not hard for the team to truly believe the<br />
foundational philosophy of the IFMSA: that with<br />
collaboration and partnership, it is possible<br />
to have an impact on health challenges of<br />
the world. For delegation member Aysha<br />
Abu-sharifa, the highlight was the personal<br />
interactions with other delegates, and being<br />
challenged by various cultural perspectives on<br />
polarising issues. The Human Rights and Peace<br />
stream offered insights into human rights law<br />
versus humanitarian law, health inequalities in<br />
an intersectional context, and the effects of<br />
discrimination on the paediatric population.<br />
“[Another] highlight this year was the Activities<br />
Fair where projects ranged from medical<br />
students mentoring orphans in Baghdad, to signlanguage<br />
proficiency training for healthcare<br />
workers in Athens, to the advocacy of nondiscriminatory<br />
health care for sex workers in the<br />
Netherlands.” Aysha Abu-sharifa, University of<br />
Notre Dame Freemantle.<br />
The March General Assembly in Montenegro<br />
was an encouraging reminder of the need for<br />
global collaboration from Australian medical<br />
students. This year’s delegates agreed that<br />
not only is there a lot to learn from like-minded<br />
students, but there is also a great deal to<br />
contribute. The IFMSA conference is only one<br />
of the many platforms in which individuals can<br />
get involved.<br />
Act now:<br />
• Join the mailing lists of the IFMSA to learn<br />
about all the great opportunities (www.ifmsa.<br />
org)<br />
• Email julie.graham@amsa.org.au to found<br />
out more about getting involved with AMSA’s<br />
international opportunities, including IFMSA<br />
exchanges.<br />
Photo credit<br />
Jasper Lin & Jessica Yang<br />
Acknowledgements<br />
None<br />
Conflict of Interest<br />
None declared<br />
Correspondence<br />
julie.graham@amsa.org.au<br />
References:<br />
1. Baum F. Classics in Social Medicine; Health for<br />
All Now! Reviving the spirit of Alma Ata in the twenty first<br />
century: An Introduction to the Alma Ata declaration.<br />
Social Medicine. 2007;2(1):34-41.<br />
Upcoming events:<br />
1. IFMSA August General Assembly in Tanzania:<br />
Pre GA 28 July-1 August; GA 1-7 August; Post GA<br />
7-10 August<br />
2. IFMSA Asia Pacific Regional Meeting (APRM)<br />
in Japan: Pre- September 15-17; APRM September<br />
17-21<br />
46
Changing Climate, Changing Perspectives:<br />
iDEA Conference Report<br />
[Conference report]<br />
Isobelle Woodruff<br />
Isobelle is a third year Doctor of Medicine student at UNDS, currently completing her<br />
clinical years in Melbourne. She is also the AMSA Code Green Co-National Project<br />
Manager and is passionate about empowering people to mitigate the health effects of<br />
climate change. Her other areas of interest include mental health and wellbeing, nutrition<br />
and behavioural change strategies.<br />
The iDEA conference is an annual national<br />
conference of Doctors for the Environment<br />
Australia (DEA). Run over two days with over 35<br />
world-renowned speakers; engaging breakout<br />
workshops; and entertaining social nights<br />
with gourmet, ethically-sourced food; iDEA<br />
is the centrepiece of environmental health<br />
education and inspiration. iDEA unites medical<br />
professionals and students from around<br />
Australia “with one common goal – to address<br />
the human health impacts of the environment<br />
and climate change”,[1] with a <strong>2017</strong> theme of<br />
“Global Problems, Local Solutions”.<br />
effects of climate change; droughts, bushfires,<br />
allergies, asthma”. Similarly, Dr Simon Judkins,<br />
President-Elect of the Australian College of<br />
Emergency Medicine, asserted that “climate<br />
change means that we are seeing bigger<br />
and more frequent large scale disasters, and<br />
emergency physicians are front and centre<br />
when it comes to responding to those events”.<br />
Global Problems<br />
Throughout the weekend, I was reminded of<br />
why our changing climate is indeed “the biggest<br />
global health threat of the 21st century”,[2]<br />
affecting health both directly and indirectly.<br />
The widely cited 2009 paper “A Commission<br />
on Climate Change” in The Lancet outlines<br />
the direct effects of climate change to be,<br />
namely; increased heat stress, floods, drought<br />
and increased frequency of intense storms.[2]<br />
In a panel of College Presidents at iDEA17,<br />
Dr Bastian Seidel, President of the Royal<br />
Australian College of General Practitioners,<br />
outlined the direct impacts of climate change<br />
on human health through referencing his<br />
everyday experiences as a general practitioner;<br />
“General Practitioners (GPs) are true climate<br />
change witnesses. As a GP in Southern<br />
Tasmania, there is not a single day that<br />
patients don’t come in and tell me about the<br />
L to R: Dr Scot Ma (ANZCA), Prof John Middleton (UK<br />
FPH), Dr Simon Judkins (ACEM), Dr Bastian Seidel (RACGP),<br />
Dr Kym Jenkins (RANZCP)<br />
In addition to the direct impacts of climate<br />
change on human health, there are also<br />
subtler, insidious, indirect effects. Some of<br />
these include air pollution, the spread of<br />
vector-borne diseases, food insecurity and<br />
under-nutrition, displacement and an increase<br />
in mental illness.[2] Dr Helen Szoke, CEO of<br />
Oxfam, directed our attention to the recent<br />
WHO report on pollution and child health, a<br />
landmark study which found that more than 1<br />
in 4 deaths of children under 5 years of age<br />
are attributed to unhealthy environments.<br />
Additionally, climate change could drive 122<br />
47
million more people into extreme poverty by<br />
2030 through its impact on increasing vectorborne<br />
diseases, food insecurity, increasing the<br />
number of climate refugees and respiratory<br />
disease through air pollution.[3]<br />
Dr Alessandro Demaio, Medical Doctor for<br />
the World Health Organization (WHO) and cofounder<br />
of NCD-Free, addressed the connection<br />
between obesity and climate change. This is a<br />
potentially hidden link, but one not to be ignored:<br />
if food waste were a country, it would be the<br />
third largest CO2 emitter.[4] He emphasised<br />
the importance of collaboration on global<br />
issues such as obesity and climate change,<br />
“when it comes to NCDs and climate change,<br />
opportunities for co-mitigation are profound and<br />
unprecedented. Inaction cannot be an option.”<br />
He urged us to think laterally on<br />
the topic – both issues have<br />
similar causes and solutions,<br />
so how can we address them<br />
together through lobbying, policy<br />
change and targeted public<br />
health strategies?<br />
Local Solutions<br />
In the face of impending “climate chaos”,<br />
as it was colloquially referred to throughout<br />
the conference, it is easy to feel overwhelmed<br />
by the reality of climate change. Despite this,<br />
the speakers provided messages of hope and<br />
inspired action and empowerment through local<br />
solutions.<br />
Coming from a refreshingly non-medical<br />
perspective, Tim Buckley, one of Australia’s top<br />
financial energy analysts, provided an overview<br />
of the progress our neighbours in India and<br />
China are making in the renewable energy<br />
market [5]. He outlined the importance of<br />
knowing your audience – the motivation behind<br />
these nations’ transition to renewables wasn’t<br />
for health reasons, but economic reasons in<br />
India (considering renewables cost 80% of<br />
what it costs to import fuel) and populationdriven<br />
air quality concerns in China. Buckley<br />
highlighted the financial stability and success<br />
What makes climate change so<br />
difficult to comprehend is the lack<br />
of a clear, single perpetrator; it<br />
doesn’t have a face.<br />
these nations have had since leading the way in<br />
renewables and why it makes economic sense<br />
for Australia to follow suit.[6] Focusing the light<br />
on Australian shores, Dr Roger Dargaville from<br />
the Melbourne Energy Institute outlined the<br />
need for robust policy and strategic direction for<br />
the Australian energy market, if we are to move<br />
towards renewables and avoid further energy<br />
demand issues like the recent South Australian<br />
energy crises.<br />
Changing Perspectives and Summary<br />
I took away a bigger picture of how we<br />
conceptualise climate change, and left thinking<br />
that we need to change our perspective to<br />
achieve true change. What makes climate<br />
change so difficult to comprehend is the lack<br />
of a clear, single perpetrator;<br />
it doesn’t have a face. Without<br />
oversimplifying complex issues,<br />
it is clear that, for example, when<br />
we want to blame someone for<br />
the obesity epidemic we think<br />
of big corporate companies like<br />
Coco Cola or McDonalds. When we want to<br />
blame someone for displaced people and mass<br />
migrations, we think of war and governments.<br />
With climate change, it isn’t as easy to play<br />
the blame game. We can’t easily point the finger<br />
at someone or something and say “this is the<br />
reason why; this is the cause”. Because we can’t<br />
readily shift the blame onto something easily<br />
identifiable, it makes the issue less tangible<br />
and more challenging to connect with. There is<br />
nowhere to direct the anger and frustration at<br />
the catastrophic changes we are seeing around<br />
us, the natural response is to either disconnect<br />
with the issue, or to feel overwhelmed with<br />
despair and subsequently be driven to inaction.<br />
In truth, we should be pointing the finger at<br />
is ourselves. As was made abundantly clear<br />
at the conference and in countless articles<br />
and reviews presented by the wider scientific<br />
community, the evidence overwhelmingly<br />
indicates that climate change is largely human<br />
driven, and thus we must take responsibility.[7]<br />
48
Yes, we are a large part of the cause. But if<br />
I learned anything over the weekend, it is that<br />
we can also drive the solution. In the words of<br />
Dr Helen Szoke, “the mission that you sign up<br />
to when you become a doctor means that you<br />
have a responsibility to assist humanity climate<br />
change is a big part of that.” There needs to be<br />
a shift of focus from the negative outcomes of<br />
climate change, towards the positive ways we<br />
as doctors, we have an obligation to talk and<br />
act on climate change”.<br />
Photo credit<br />
Mack Lee<br />
Acknowledgements<br />
None<br />
Conflict of Interest<br />
None declared<br />
Correspondence<br />
isobelle.woodruff@amsa.org.au<br />
References<br />
iDEA17 delegates<br />
can address it. We need to stop seeing it as<br />
an issue and start seeing it as a potential for<br />
change and act in the infinite ways the speakers<br />
outlined at iDEA. While it is the biggest threat to<br />
our species and planet, climate change could<br />
also be “the greatest global health opportunity<br />
of the 21st century”.[8]<br />
The evening before the conference<br />
commenced, I was honored to hear from human<br />
rights lawyer Julian Burnside AO QC, who<br />
eloquently stated; “to remain silent is as much<br />
a political act as to speak out”. This simple idea<br />
is as applicable to climate change and human<br />
health as ever; the health impacts of climate<br />
change are direct and indirect, immediate and<br />
long term, both overt and subtle. We must have<br />
a global perspective on the issue, but also the<br />
willingness to act locally to create sustainable<br />
and tangible change to protect the health of our<br />
planet and our people. It is our responsibility as<br />
informed, ethically-minded health professionals<br />
to act now. In the words of Dr Stephen Parnis, ex-<br />
AMA Vice President “prevention and mitigation<br />
is always better than reaction and recovery –<br />
1. Doctors for the Environment Australia. iDEA17 Conference<br />
DEA<strong>2017</strong> [Available from: https://www.dea.org.au/<br />
idea<strong>2017</strong>/.<br />
2. The Lancet. A Commission on climate change. The<br />
Lancet. 2009;373(9676):1659.<br />
3. Inheriting a sustainable world? Atlas on children’s<br />
health and the environment. Geneva: World Health<br />
Organisation, <strong>2017</strong>.<br />
4. Food and Agriculture Organization of the United<br />
Nations. Food wastage footprint; impacts on natural<br />
resources (summary report). Natural Resources<br />
Management and Environment Department, United<br />
Nations, 2013.<br />
5. Buckley T. IEEFA Update: China Is Now Three Years<br />
Past Coal. IEEFA, <strong>2017</strong> Feburary 28, <strong>2017</strong>. Report No.<br />
6. Tan JAMH. Economics: Manufacture renewables to<br />
build energy security. Nature. 2014;513(7517).<br />
7. McMichael AJ. Globalization, Climate Change, and<br />
Human Health. The New England Journal of Medicine.<br />
2013;386:1335-43.<br />
8. Nick Watts et al. Health and climate change:<br />
policy responses to protect public health. The Lancet.<br />
2015;386(10006):1861 - 914.<br />
49
<strong>Vector</strong> <strong>Volume</strong> <strong>11</strong> <strong>Issue</strong> 2<br />
Submission Callouts July-August <strong>2017</strong><br />
Felt inspired by the articles in this issue? Have your own research/<br />
commentary/ feature/ report to share? We want to hear from you!<br />
Follow our Facebook page ‘<strong>Vector</strong> Journal’ and check out our<br />
website vector.amsa.org.au to stay in the loop<br />
50
Cover image reproduced with<br />
permission from Dr Hilmers<br />
51