Molecular and Cellular Biology of Plasminogen Activation
Molecular and Cellular Biology of Plasminogen Activation
Molecular and Cellular Biology of Plasminogen Activation
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
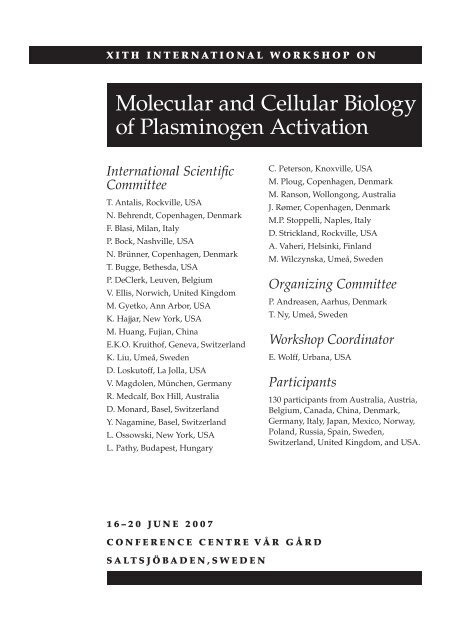
X I t h I n t e r n a t I o n a l w o r k S h o p o n<br />
<strong>Molecular</strong> <strong>and</strong> <strong>Cellular</strong> <strong>Biology</strong><br />
<strong>of</strong> <strong>Plasminogen</strong> <strong>Activation</strong><br />
International Scientific<br />
Committee<br />
T. Antalis, Rockville, USA<br />
N. Behrendt, Copenhagen, Denmark<br />
F. Blasi, Milan, Italy<br />
P. Bock, Nashville, USA<br />
N. Brünner, Copenhagen, Denmark<br />
T. Bugge, Bethesda, USA<br />
P. DeClerk, Leuven, Belgium<br />
V. Ellis, Norwich, United Kingdom<br />
M. Gyetko, Ann Arbor, USA<br />
K. Hajjar, New York, USA<br />
M. Huang, Fujian, China<br />
E.K.O. Kruith<strong>of</strong>, Geneva, Switzerl<strong>and</strong><br />
K. Liu, Umeå, Sweden<br />
D. Loskut<strong>of</strong>f, La Jolla, USA<br />
V. Magdolen, München, Germany<br />
R. Medcalf, Box Hill, Australia<br />
D. Monard, Basel, Switzerl<strong>and</strong><br />
Y. Nagamine, Basel, Switzerl<strong>and</strong><br />
L. Ossowski, New York, USA<br />
L. Pathy, Budapest, Hungary<br />
16–20 June 2007<br />
C. Peterson, Knoxville, USA<br />
M. Ploug, Copenhagen, Denmark<br />
M. Ranson, Wollongong, Australia<br />
J. Rømer, Copenhagen, Denmark<br />
M.P. Stoppelli, Naples, Italy<br />
D. Strickl<strong>and</strong>, Rockville, USA<br />
A. Vaheri, Helsinki, Finl<strong>and</strong><br />
M. Wilczynska, Umeå, Sweden<br />
Organizing Committee<br />
P. Andreasen, Aarhus, Denmark<br />
T. Ny, Umeå, Sweden<br />
Workshop Coordinator<br />
E. Wolff, Urbana, USA<br />
Participants<br />
ConferenCe Centre Vår Gård<br />
SaltSJöbaden,Sweden<br />
130 participants from Australia, Austria,<br />
Belgium, Canada, China, Denmark,<br />
Germany, Italy, Japan, Mexico, Norway,<br />
Pol<strong>and</strong>, Russia, Spain, Sweden,<br />
Switzerl<strong>and</strong>, United Kingdom, <strong>and</strong> USA.
ii X I t h I n t e r n a t i o n a l W o r k s h o p o n
The XIth International Workshop on <strong>Molecular</strong><br />
<strong>and</strong> <strong>Cellular</strong> <strong>Biology</strong> <strong>of</strong> <strong>Plasminogen</strong> <strong>Activation</strong><br />
is sponsored by<br />
Nobel Committee for Chemistry<br />
Swedish Cancer Society<br />
Swedish Research Council<br />
American Diagnostica Inc.<br />
The organizing committee would like to thank the organizers <strong>of</strong> the<br />
previous International Workshops <strong>of</strong> <strong>Plasminogen</strong> <strong>Activation</strong> for<br />
generously contributing unspent funds.<br />
<strong>Molecular</strong> & <strong>Cellular</strong> <strong>Biology</strong> <strong>of</strong> <strong>Plasminogen</strong> <strong>Activation</strong> iii
Housing Grant Recipients<br />
Nina Ahlskog, Umeå, Sweden<br />
Daniela Alfano, Naples, Italy<br />
Lisbeth Andersen, Aarhus, Denmark<br />
Annapaola Andolfo, Milan, Italy<br />
Esther Ardite, Barcelona, Spain<br />
Rashna Balsara, Notre Dame, USA<br />
Nathalie Beaufort, Munich, Germany<br />
Julie Bødker, Aarhus, Denmark<br />
Patrick Brunner, Vienna, Austria<br />
Katharaina Bruno, Chicago, USA<br />
Blake Cochran, Wollongong, Australia<br />
David Croucher, Sydney, Australia<br />
Angels Diaz-Ramos, Barcelona, Spain<br />
Daniel Dupont, Aarhus, Denmark<br />
Monika Ehnman, Stockholm, Sweden<br />
Monika Ehart, Vienna, Austria<br />
Paola Franco, Naples, Italy<br />
Yongzhi Guo, Umeå, Sweden<br />
Peter Hägglöf, Cambridge, United Kingdom<br />
Jakob Harslund, Frederiksberg, Denmark<br />
Emir Henic, Lund, Sweden<br />
Karin Hultman, Gothenburg, Sweden<br />
Benedikte Jacobsen, Copenhagen, Denmark<br />
Lotte Jensen, Frederiksberg, Denmark<br />
Anna Juncker-Jensen, Copenhagen, Denmark<br />
Jodi Lee, Wollongong, Australia<br />
Shih-Hon Li, Urbana, USA<br />
Anna Lillis, Baltimore, USA<br />
Sergei Lobov, Wollongong, Australia<br />
Immacolata Longanesi Cattani, Naples, Italy<br />
Ida Katrine Lund, Copenhagen, Denmark<br />
Chris Madsen, Milan, Italy<br />
Rajani Maiya, New York, USA<br />
Lester Meissenheimer, Leuven, Belgium<br />
Judit Mihaly, Vienna, Austria<br />
Evelyn Nieves-Li, Urbana, USA<br />
Bjorn Olausson, Umeå, Sweden<br />
Mohan Pabba, Umeå, Sweden<br />
Justin Paul, New York, USA<br />
Valentina Pirazzoli, Milan, Italy<br />
Boris Pliyev, Moscow, Russia<br />
Gerald Prager, Vienna, Austria<br />
Patrycja Przygodzka, Umeå, Sweden<br />
Tomasz Przygodzki, Umeå, Sweden<br />
Aless<strong>and</strong>ro Salvi, Brescia, Italy<br />
Morten Rasch, Copenhagen, Denmark<br />
Birgitte Rønø, Copenhagen, Denmark<br />
Gian Maria Sarra Ferraris, Milan, Italy<br />
Rima Sulniute, Umeå, Sweden<br />
Berta Vidal, Barcelona, Spain<br />
Patrik Wahlberg, Umeå, Sweden<br />
Ying Wei, San Francisco, USA<br />
Malgorzata Wygrecka, Giessen, Germany<br />
Wendy Xolalpa, Mexico, Mexico<br />
Aiwu Zhou, New York, USA<br />
iv X I t h I n t e r n a t i o n a l W o r k s h o p o n
Table <strong>of</strong> Contents<br />
Saturday, 16 June 2007 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .2<br />
Sunday, 17 June 2007 ..............................................................2<br />
Session 1—Vitronectin <strong>and</strong> the <strong>Plasminogen</strong> <strong>Activation</strong> System ............................2<br />
Session 2—Proteases, Inhibitors, Receptors, <strong>and</strong> Substrates in Vascular <strong>Biology</strong> . . . . . . . . . . . . . .3<br />
Session 3—Cell Signalling Upstream <strong>and</strong> Downstream <strong>of</strong> the<br />
<strong>Plasminogen</strong> <strong>Activation</strong> System . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .3<br />
Monday, 18 June 2007 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .4<br />
Session 4—Proteases, Inhibitors, Receptors, <strong>and</strong> Substrates in Neurobiology<br />
<strong>and</strong> Neuronal Pathology ..............................................................4<br />
Session 5—Proteases, Inhibitors, Receptors, <strong>and</strong> Substrates in Normal Development ..........5<br />
Session 6—The <strong>Plasminogen</strong> <strong>Activation</strong> System <strong>and</strong> Programmed Cell Death ................5<br />
Tuesday, 19 June 2007 .............................................................6<br />
Session 7—Proteases, Inhibitors, Receptors, <strong>and</strong><br />
Substrates in Tissue Repair <strong>and</strong> Tissue Remodelling ......................................6<br />
Session 8—Proteases, Inhibitors, Receptors, <strong>and</strong><br />
Substrates in Inflammation <strong>and</strong> Infectious Diseases . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .6<br />
Wednesday, 20 June 2007 ..........................................................7<br />
Session 9—Proteases, Inhibitors, Receptors, <strong>and</strong> Substrates in Cancer .......................7<br />
Session 10—Proteases, Inhibitors, <strong>and</strong> Receptors as Therapeutic Targets <strong>and</strong><br />
Therapeutic Proteins . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .7<br />
Poster Presentations ................................................................9<br />
Abstracts for Oral Presentations ...................................................13<br />
Abstracts for Poster Presentations . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .63<br />
Author Index . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .129<br />
Attendee List .....................................................................132<br />
<strong>Molecular</strong> & <strong>Cellular</strong> <strong>Biology</strong> <strong>of</strong> <strong>Plasminogen</strong> <strong>Activation</strong> 1
Saturday, 16 June 2007<br />
14:00–18:00 Registration<br />
17:30–17:40 Welcome <strong>and</strong> Meeting Overview<br />
Peter Andreasen <strong>and</strong> Tor Ny<br />
17:40–18:25 Popular lecture: “Carl Linnaeus—The man who gave all <strong>of</strong> us our names”<br />
Anna Rask-Andersen<br />
18:30–20:00 Dinner<br />
20:15–21:00 Lecture: “Control <strong>of</strong> invasive growth by plasminogen-related growth factors<br />
(HGF <strong>and</strong> MSP)”<br />
Paolo Michieli <strong>and</strong> Paolo Comoglio<br />
Sunday, 17 June 2007<br />
7:00–8:30 Breakfast<br />
X I t h I n t e r n a t I o n a l w o r k S h o p o n<br />
<strong>Molecular</strong> <strong>and</strong> <strong>Cellular</strong> <strong>Biology</strong><br />
<strong>of</strong> <strong>Plasminogen</strong> <strong>Activation</strong><br />
8:30–10:15 Session 1—Vitronectin <strong>and</strong> the <strong>Plasminogen</strong> <strong>Activation</strong> System<br />
Session Chairs: Michael Ploug <strong>and</strong> Mingdong Huang<br />
8:30–8:35 Introduction by Session Chairs<br />
8:35–8:55 001 • Defining the Native Disulfide Topology in the SMB Domain <strong>of</strong> Human<br />
Vitronectin • Li X, Zou G, Yuan W, Lu W*<br />
8:55–9:15 002 • The Vitronectin Binding Site on the Urokinase Receptor Comprises Residues<br />
from Both Domain I <strong>and</strong> the Flanking Interdomain Linker Region • Gårdsvoll H <strong>and</strong><br />
Ploug M*<br />
9:15–9:35 003 • uPAR-induced Cell Adhesion <strong>and</strong> Migration: Vitronectin Provides the Key •<br />
Madsen CD*, Sarra Ferraris GM, Andolfo A, Cunningham O, Sidenius N<br />
9:35–9:55 004 • Interactions between PAI-1 <strong>and</strong> Vitronectin: Two Proteins, Two Sites, <strong>and</strong> Two<br />
Phases • Schar CR, Jensen JK, Blouse GE, Minor KH, Andreasen PA, Peterson CB*<br />
9:55–10:15 005 • How Does Vitronectin Accelerate PAI-1’s Protease Inhibition? • Zhou A* <strong>and</strong><br />
Wei Z<br />
Relevant Posters—051–056<br />
2 X I t h I n t e r n a t i o n a l W o r k s h o p o n
10:15–10:35 Break<br />
10:35–12:20 Session 2—Proteases, Inhibitors, Receptors, <strong>and</strong> Substrates in Vascular <strong>Biology</strong><br />
Session Chairs: Marie Ranson <strong>and</strong> Thomas Bugge<br />
10:35–10:40 Introduction by Session Chairs<br />
10:40–11:00 006 • The Interaction between Tissue-type <strong>Plasminogen</strong> Activator <strong>and</strong> the Low<br />
Density Lipoprotein Receptor-Related Protein Induces <strong>Activation</strong> <strong>of</strong> the NF-kB<br />
Pathway during Cerebral Ischemia • Yepes M*, Brotzge XH, Polavarapu R<br />
11:00–11:20 007 • Unique Secretory Dynamics <strong>of</strong> Tissue <strong>Plasminogen</strong> Activator (tPA) Is<br />
Beneficial to Maintain Fibrinolytic Activity on Cell Surface • Suzuki Y*, Ihara H,<br />
Mogami H, Urano T<br />
11:20–11:40 008 • The Macrophage Low-Density Lipoprotein Receptor Related Protein (LRP)<br />
Modulates Murine Lipoprotein Metabolism • Lillis AP*, Mikhailenko I, Robinson S,<br />
Migliorini M, Battey F, Pizzo SV, Strickl<strong>and</strong> DK<br />
11:40–12:00 009 • Annexin 2 Mediates <strong>Plasminogen</strong>-Dependent Recruitment <strong>of</strong> Neovascular<br />
Mural Cells in Lymphoma Angiogenesis • Ling Q, Ruan J, Yan L, Sui G-Z, Deora AB,<br />
Church S, Cohen-Gould L, Rafii S, Lyden D, Hajjar KA*<br />
12:00–12:20 010 • <strong>Activation</strong> <strong>of</strong> Latent PDGF-CC by Tissue <strong>Plasminogen</strong> Activator Impairs<br />
Blood Brain Barrier Integrity during Ischemic Stroke • Su EJ, Fredriksson L,<br />
Geyer M, Folestad E, Cale J, Mann K, Gao Y, Pietras K, Andreé J, Yepes M, Strickl<strong>and</strong> DK,<br />
Betsholtz C, Eriksson U, Lawrence DA*<br />
12:20–12:30 Group photo<br />
Relevant Posters—057–060<br />
12:30–15:00 Lunch <strong>and</strong> free time<br />
15:00–17:30 Poster Session A—Posters 051–084<br />
17:30–19:00 Dinner<br />
19:00–21:10 Session 3—Cell Signalling Upstream <strong>and</strong> Downstream <strong>of</strong> the <strong>Plasminogen</strong><br />
<strong>Activation</strong> System<br />
Session Chairs: Francesco Blasi <strong>and</strong> Egbert K.O. Kruith<strong>of</strong><br />
19:00–19:05 Introduction by Session Chairs<br />
19:05–19:25 011 • <strong>Plasminogen</strong> Activator Inhibitor-1 Gene Regulation: Cross Talk between<br />
Hypoxia <strong>and</strong> Insulin Signalling • Flugel D <strong>and</strong> Kietzmann T*<br />
19:25–19:45 012 • Role <strong>of</strong> Rho GTPases <strong>and</strong> p38 MAP Kinase in the Regulation <strong>of</strong> t-PA <strong>and</strong><br />
PAI-1 Expression in Cultured Human Endothelial Cells • Fish RJ*, Dunoyer-Geindre<br />
S, Kruith<strong>of</strong> EKO<br />
19:45–20:05 013 • Urokinase Receptor/a5b1 Integrin Interaction <strong>and</strong> Signaling in Cancer Cells •<br />
Wei Y*, Tang CH, Kim Y, Robillard L, Kugler MC, Hill M, Brumwell A, Chapman HA<br />
20:05–20:10 Break<br />
<strong>Molecular</strong> & <strong>Cellular</strong> <strong>Biology</strong> <strong>of</strong> <strong>Plasminogen</strong> <strong>Activation</strong> 3
20:10–20:30 014 • Activated Human Neutrophils Rapidly Release the Chemotactically Active<br />
D2D3 Form <strong>of</strong> the Urokinase-type <strong>Plasminogen</strong> Activator Receptor (uPAR/CD87) •<br />
Pliyev BK* <strong>and</strong> Tkachuk VA<br />
20:30–20:50 015 • PDGF-DD Bioavailability Is Regulated by the uPA/uPAR System:<br />
Implications for Tumor Growth • Ehnman M*, Li H, Fredriksson L, Eriksson U<br />
20:50–21:10 064 • Detection <strong>and</strong> Prevention <strong>of</strong> Hepatic Fibrosis Targeting Proteolytic TGF-b<br />
<strong>Activation</strong> Reaction • Kojima S<br />
Relevant Posters—061–076<br />
Monday, 18 June 2007<br />
7:00–8:30 Breakfast<br />
8:30–11:00 Session 4—Proteases, Inhibitors, Receptors, <strong>and</strong> Substrates in Neurobiology <strong>and</strong><br />
Neuronal Pathology<br />
Session Chairs: Denis Monard <strong>and</strong> Dan Lawrence<br />
8:30–8:35 Introduction by Session Chairs<br />
8:35–8:55 017 • A Novel Neuronal Death Pathway Triggered By Excess Tissue <strong>Plasminogen</strong><br />
Activator • Li J*, Snyder EY, Sidman RL<br />
8:55–9:15 018 • The Inhibitor <strong>of</strong> Serine Proteases Protease Nexin-1 <strong>and</strong> its Receptor LRP<br />
Modulate SHH Signalling during Cerebellar Development • Vaillant C, Michos O,<br />
Orolicki S, Brellier F, Taieb S, Moreno E, Té H, Zeller R, Monard D*<br />
9:15–9:35 019 • Fibrin Deposition Accelerates Neurovascular Damage <strong>and</strong><br />
Neuroinflammation in Mouse Models <strong>of</strong> Alzheimer’s Disease • Paul J* <strong>and</strong><br />
Strickl<strong>and</strong> S<br />
9:35–9:55 020 • Anxiety-like Behavior <strong>and</strong> Impaired Fear Extinction in Mice with Altered<br />
Control <strong>of</strong> Extracellular Brain Proteolytic Activity • Meins M*, Herry C, Moreno E,<br />
Fischer C, Lüthi A, Monard D<br />
9:55–10:00 Break<br />
10:00–10:20 021 • Tissue <strong>Plasminogen</strong> Activator Is Co-Packaged <strong>and</strong> Co-Transported to<br />
Synaptic Sites with a Key Neuromodulator Associated with Synaptic Plasticity •<br />
Lochner JE*, Spangler E, Schuttner LC, Scalettar BA<br />
10:20–10:40 022 • Tissue <strong>Plasminogen</strong> Activator Modulates <strong>Cellular</strong> <strong>and</strong> Behavioral Response to<br />
Cocaine • Maiya R*, Zhou Y, Norris EH, Kreek MJ, Strickl<strong>and</strong> S<br />
10:40–11:00 023 • Characterisation <strong>of</strong> the Pathway <strong>of</strong> Polymerisation <strong>of</strong> Wildtype Neuroserpin<br />
<strong>and</strong> the Ser49Pro Mutant that Underlies the Dementia FENIB • Hägglöf P*,<br />
Belorgey D, Karlsson-Li S, Sharp LK, Lomas DA<br />
Relevant Poster—077<br />
4 X I t h I n t e r n a t i o n a l W o r k s h o p o n
11:00–11:20 Break<br />
11:20–12:25 Session 5—Proteases, Inhibitors, Receptors, <strong>and</strong> Substrates in Normal<br />
Development<br />
Session Chairs: Kui Liu <strong>and</strong> Leif Lund<br />
11:20–11:25 Introduction by Session Chairs<br />
11:25–11:45 024 • Matriptase Is an Essential Inhibitory Target for Hepatocyte Growth Factor<br />
Activator Inhibitor-1 during both Embryonic Development <strong>and</strong> Postnatal Life •<br />
Szabo R*, Molinolo A, List K, Bugge TH<br />
11:45–12:05 025 • Mice with very low Matriptase Are Viable <strong>and</strong> Phenocopy Human Autosomal<br />
Ichthyosis with Hypotrichosis Syndrome • List K*, Currie B, Scharschmidt T, Szabo R,<br />
Molinolo A, Shireman J, Segre J, Bugge TH<br />
12:05–12:25 026 • Role <strong>of</strong> Urokinase-Receptor in Hematopoietic Stem Cell Trafficking •<br />
Montuori N, Selleri C, Ricci P, Visconte V,Carriero MV, Rotoli B, Rossi G, Ragno P*<br />
Relevant Posters—078–084<br />
12:25–17:30 Lunch <strong>and</strong> Free Time<br />
17:30–18:30 Dinner<br />
18:30–20:15 Session 6—The <strong>Plasminogen</strong> <strong>Activation</strong> System <strong>and</strong> Programmed Cell Death<br />
Session Chairs: Patrizia Stoppelli <strong>and</strong> Bernd Binder<br />
18:30–18:35 Introduction by Session Chairs<br />
18:35–18:55 027 • <strong>Plasminogen</strong> Activator Inhibitor-1, PAI-1, Regulates the Akt Survival Pathway<br />
• Rømer MU, Larsen L, Offenberg H, Brünner N, Lademann U*<br />
18:55–19:15 028 • A Host <strong>Plasminogen</strong> Activator Inhibitor-1 Deficiency Promotes Proliferation<br />
<strong>and</strong> Resistance to Apoptosis by <strong>Activation</strong> <strong>of</strong> the PI3-K/Akt Pathway in Endothelial<br />
Cells • Balsara RD*, Castellino FJ, Ploplis VA<br />
19:15–19:35 029 • Bomapin Is a Redox-Regulated Serpin which Stabilizes Retinoblastoma<br />
Protein during Apoptosis <strong>and</strong> Increases Proliferation <strong>of</strong> Leukemia Cells •<br />
Przygodzka P, Olausson B, Tengel Y, Larsson G, Wilczynska M*<br />
19:35–19:55 030 • Hepsin as a Cell Survival Factor • Qiu D, Owen K, Edwards DR, Ellis V*<br />
19:55–20:15 031 • Urokinase (uPA) Protects Endothelial Cell against Apoptosis by Upregulating<br />
the X-Linked Inhibitor <strong>of</strong> Apoptosis Protein (XIAP) •Prager GW*, Koschelnick Y,<br />
Mihaly J, Brunner P, Binder BR<br />
Relevant Posters—085–087<br />
<strong>Molecular</strong> & <strong>Cellular</strong> <strong>Biology</strong> <strong>of</strong> <strong>Plasminogen</strong> <strong>Activation</strong> 5
Tuesday, 19 June 2007<br />
7:00–8:30 Breakfast<br />
8:30–9:55 Session 7—Proteases, Inhibitors, Receptors, <strong>and</strong> Substrates in Tissue Repair <strong>and</strong><br />
Tissue Remodelling<br />
Session Chairs: Katherine Hajjar <strong>and</strong> Dudley Strickl<strong>and</strong><br />
8:30–8:35 Introduction by Session Chairs<br />
8:35–8:55 032 • Pro-fibrinolytic Effects <strong>of</strong> Metalloproteinases during Skin Wound Healing in<br />
the Absence <strong>of</strong> <strong>Plasminogen</strong> • Lund LR*, Green KA, Almholt K, Ploug M, Bugge TH,<br />
Rømer J<br />
8:55–9:15 033 • Complementary Roles <strong>of</strong> Intracellular <strong>and</strong> Pericellular Collagen Degradation<br />
Pathways in Mesenchymal Cell Survival <strong>and</strong> Proliferation • Wagenaar-Miller RA,<br />
Engelholm LH, Gavard J, Yamada S, Gutkind JS, Behrendt N, Holmbeck K, Bugge TH*<br />
9:15–9:35 034 • Interplay between MMPs <strong>and</strong> the Endocytic Collagen Receptor, uPARAP/<br />
Endo180, in Collagen Degradation • Behrendt N*, Madsen DH, Ingvarsen S, Hillig T,<br />
Wagenaar-Miller R, Kjøller L, Gårdsvoll H, Høyer-Hansen G, Bugge TH, Engelholm LH<br />
9:35–9:55 035 • The Urokinase Receptor Ko Mice Have Reduced Keratinocytes Proliferation<br />
<strong>and</strong> Migration during Wound Healing <strong>and</strong> Are Protected in a Skin Carcinogenesis<br />
Protocol • D’Alessio S, Mazzieri, R, Gerasi L, Blasi F*<br />
9:55–10:15 Break<br />
Relevant Poster—088<br />
10:15–12:00 Session 8—Proteases, Inhibitors, Receptors, <strong>and</strong> Substrates in Inflammation <strong>and</strong><br />
Infectious Diseases<br />
Session Chairs: Toni Antalis <strong>and</strong> Vincent Ellis<br />
10:15–10:20 Introduction by Session Chairs<br />
10:20–10:40 036 • Distinct Roles <strong>of</strong> Plasmin in Staphylococcus aureus-induced Sepsis <strong>and</strong><br />
Infection Models • Guo Y*, Li J, Hagström E, Ny T<br />
10:40–11:00 037 • Proteolytic <strong>Activation</strong> <strong>of</strong> the Human Urokinase/Plasmin System by<br />
Staphylococcus aureus • Beaufort N*, Wojciechowski P, Sommerh<strong>of</strong>f CP, Schmitt M,<br />
Potempa J, Magdolen V<br />
11:00–11:20 038 • The Maintenance <strong>of</strong> High Affinity <strong>Plasminogen</strong> Binding by PAM Variants<br />
from Group A Streptococci Is Mediated by Conserved Arg <strong>and</strong> His Residues in Both<br />
the A1 <strong>and</strong> A2 Repeat Domains • Ranson M*, S<strong>and</strong>erson-Smith ML, Walker MJ, Fu Q,<br />
Castellino FJ, Prorok M<br />
11:20–11:40 039 • <strong>Plasminogen</strong> Activator Inhibitor-1 (PAI-1) Is an Inhibitor <strong>of</strong> Factor VII-<br />
Activating Protease in Patients with Acute Respiratory Distress Syndrome •<br />
Wygrecka M*, Morty RE, Markart P, Kanse SM, Andreasen PA, Wind T, Guenther A,<br />
Preissner KT<br />
6 X I t h I n t e r n a t i o n a l W o r k s h o p o n
11:40–12:00 040 • Improved Muscle Regeneration in PAI-1-deficient Mice Is Associated with an<br />
Enhanced Inflammatory Response <strong>and</strong> Reduced Fibrin Deposition after Injury •<br />
Ardite E*, Vidal B, Jardí M, González B, Muñoz-Cánoves P<br />
Relevant Posters—089–095<br />
12:00–12:20 Presentation <strong>of</strong> the 2009 <strong>Plasminogen</strong> <strong>Activation</strong> Meeting<br />
12:20–14:30 Lunch <strong>and</strong> Free Time<br />
14:30–17:00 Poster Session B—Posters 085–116<br />
17:00 Reception <strong>and</strong> Gala Banquet <strong>and</strong> Boat Trip<br />
Wednesday, 20 June 2007<br />
7:00–8:30 Breakfast<br />
8:30–9:55 Session 9—Proteases, Inhibitors, Receptors, <strong>and</strong> Substrates in Cancer<br />
Session Chairs: Keld Danø <strong>and</strong> Thomas Kietzmann<br />
8:30–8:35 Introduction by Session Chairs<br />
8:35–8:55 041 • Invasion <strong>and</strong> Metastasis <strong>of</strong> Carcinoma Cells Is Prevented by Urokinase-<br />
Derived Antagonists <strong>of</strong> avb5 Integrin <strong>Activation</strong> • Franco P, Vocca I, Alfano D,<br />
Votta G, Carriero MV, Estrada Y, Netti PA, Ossowski L, Stoppelli MP*<br />
8:55–9:15 042 • Urokinase Receptor/Integrin Interactions in Lung Tumor Development •<br />
Tang CH, Hill M, Kim Y, Wei Y, Chapman HA*<br />
9:15–9:35 043 • uPA <strong>and</strong> uPAR Expressing Stromal Cells Accompany the Transition to<br />
Invasive Breast Cancer • Nielsen BS*, Rank F, Illemann M, Lund LR, Danø K<br />
9:35–9:55 044 • Generation <strong>of</strong> the Malignant Phenotype in HT-1080 Tumor Cells by<br />
PAI-1 Involves Modulation <strong>of</strong> Proteasomal Activity <strong>and</strong> Phosphatases • Mihaly J*,<br />
Carroll VA, Breuss JM, Prager GW, Binder BR<br />
9:55–10:15 Break<br />
Relevant Posters—096–106<br />
10:15–12: 20 Session 10—Proteases, Inhibitors, <strong>and</strong> Receptors as Therapeutic Targets <strong>and</strong><br />
Therapeutic Proteins<br />
Session Chairs: Gunilla Høyer-Hansen <strong>and</strong> Ann Gils<br />
10:15–10:20 Introduction by Session Chairs<br />
10:20–10:40 045 • PEGylated DX-1000: Pharmacokinetics, Anti-Tumor <strong>and</strong> Anti-Metastatic<br />
Effects <strong>of</strong> a Specific Plasmin Inhibitor • Devy L*, Rabbani SA, Stochl M, Ruskowski M,<br />
Mackie I, Naa L, Toews M, van Gool R, Chen J, Ley A, Ladner RC, Dransfield DT,<br />
Henderikx P<br />
<strong>Molecular</strong> & <strong>Cellular</strong> <strong>Biology</strong> <strong>of</strong> <strong>Plasminogen</strong> <strong>Activation</strong> 7
10:40–11:00 046 • Cytotoxic Potential <strong>of</strong> a Novel uPA-activity Dependent <strong>and</strong> EGF Receptor<br />
Targeting Pro-drug • Rønø B*, Kim GB, Liu S, Kristjansen PEG, Neville DM, Leppla SH,<br />
Bugge TH, Rømer J<br />
11:00–11:20 047 • Inhibition <strong>of</strong> Mouse uPA Activity by Mouse Monoclonal Antibodies in vitro<br />
<strong>and</strong> in vivo • Lund IK*, Jögi A, Behrendt N, Ploug M, Gårdsvoll H, Lund LR, Rømer J,<br />
Høyer-Hansen G<br />
11:20–11:40 048 • Crystal Structure <strong>of</strong> Human Urokinase Complexed with a Cyclic Peptidyl<br />
Inhibitor, uPAin-1 • Zhao G, Yuan C, Bian C, Wind T, Andreasen PA, Huang M*<br />
11:40–12:00 049 • Discovery <strong>of</strong> a Novel Zymogen Targeting Inhibitor <strong>of</strong> Urokinase-type<br />
<strong>Plasminogen</strong> Activator: Evidence for Structural Flexibility <strong>of</strong> the Protease Domain •<br />
Blouse GE, Bøtkjær KA, Deryugina EI, Kjelgaard S, Byszuk O, Mortensen KK, Quigley JP,<br />
Andreasen PA*<br />
12:00–12:20 050 • A Novel Type <strong>of</strong> Agent Blocking the Association <strong>of</strong> uPA to its Receptor<br />
uPAR: uPA-binding Aptamers • Dupont DM*, Madsen JB, Kjems J, Andreasen PA<br />
Relevant Posters—107–116<br />
12:20 Lunch <strong>and</strong> departure<br />
8 X I t h I n t e r n a t i o n a l W o r k s h o p o n
Poster Presentations<br />
• Poster numbers 51–84 will be<br />
displayed from Saturday evening<br />
through Monday morning.<br />
• Presenters <strong>of</strong> poster numbers 51–84<br />
will present in Poster Session A on<br />
Sunday, 17 June from 15:00–17:30.<br />
• Poster numbers 85–116 will be<br />
displayed from Monday afternoon<br />
through Wednesday morning.<br />
• Presenters <strong>of</strong> poster numbers 85–116<br />
will present in Poster Session B on<br />
Tuesday, 19 June from 14:30–17:00.<br />
• Presenters should be present at their<br />
posters during the first 2 hours <strong>of</strong> the<br />
poster session.<br />
051 • Identification <strong>and</strong> Analysis <strong>of</strong> the Vn<br />
Binding Site in Mouse uPAR • Pirazzoli V*,<br />
Andolfo AP, Madsen CD, Sidenius N<br />
052 • Novel uPAR Binding Site in Vitronectin<br />
• Andolfo A* <strong>and</strong> Sidenius N<br />
053 • Dissecting Serpin-protease Reaction<br />
Pathways by the Use <strong>of</strong> Monoclonal<br />
Antibodies • Bødker JS*, Blouse GE,<br />
Dupont DM, Andreasen PA<br />
054 • PAI-1-vitronectin Interactions Involve<br />
an Extended Binding Surface <strong>and</strong> Mutual<br />
Conformational Rearrangements • Blouse GE,<br />
Peterson CB, Dupont DM, Ploug M, Gårdsvoll H,<br />
Schar CR, Perron MJ, Minor KH, Shore JD,<br />
Andreasen PA*<br />
055 • Intact (non-cleavable) Cell-surface<br />
u-PAR Accelerates Clearance <strong>of</strong><br />
tcu-PA:PAI-1:u-PAR Complexes <strong>and</strong><br />
Subsequent Re-surfacing <strong>of</strong> Intact <strong>and</strong><br />
Functional u-PAR • Nieves-Li EC* <strong>and</strong><br />
Manch<strong>and</strong>a N<br />
056 • The Central b-sheet <strong>of</strong> PAI-1<br />
Demonstrates Two Dynamically Distinct<br />
Regions • Li S*, Lawrence DA, Schwartz BS<br />
057 • Regulation <strong>of</strong> Cancer Cell Plasmin<br />
Generation by Annexin A2-S100A10<br />
Heterotetramer (AIIt) • Waisman DM*<br />
058 • <strong>Plasminogen</strong> Activator Inhibitor Type 2<br />
Binds to S100A10 in Annexin 2 Heterotetramer<br />
<strong>and</strong> Prevents Annexin 2-dependent Plasmin<br />
In-site Formation by Inhibiting tPA • Lobov S*,<br />
Croucher D, Ranson M<br />
059 • Underst<strong>and</strong>ing the Structural Basis<br />
<strong>of</strong> the Differential-Receptor-Mediated<br />
Endocytosis Mechanisms <strong>of</strong> PAI-1 <strong>and</strong> PAI-2<br />
in Cancer • Cochran BJ*, Lobov S, Croucher D,<br />
Ranson M<br />
060 • A Low-glycemic-index Diet Reduces<br />
Plasma PAI-1 Activity in Overweight Women<br />
• Jensen L*, Krog-Mikkelsen I, Sloth B, Flint A,<br />
Astrup A, Raben A, Tholstrup T, Brünner N<br />
061 • Urokinase Receptor-independent<br />
Signalling <strong>of</strong> the Urokinase-type <strong>Plasminogen</strong><br />
Activator via Phosporylation <strong>of</strong> STAT1 • Ehart<br />
M* <strong>and</strong> Binder BR<br />
062 • Urokinase Receptor Promotes Neo-<br />
Angiogenesis through its Ser88-Arg-Ser-Arg-<br />
Tyr92 Chemotactic Sequence • Longanesi-<br />
Cattani I*, Bifulco K, Cantelmo AR, Di Carluccio<br />
G, Spina R, Liguori E, Stoppelli MP, Carriero MV<br />
063 • The Density Enhanced Phosphatase 1<br />
(DEP-1) Down-Modulates Urokinase Receptor<br />
(uPAR) Surface Expression in Confluent<br />
Endothelial Cells • Brunner PM*, Heier PC,<br />
Prager GW, Mihaly J, Priglinger U, Binder BR<br />
064 • Detection <strong>and</strong> Prevention <strong>of</strong> Hepatic<br />
Fibrosis Targeting Proteolytic TGF-b<br />
<strong>Activation</strong> Reaction • Kojima S*<br />
<strong>Molecular</strong> & <strong>Cellular</strong> <strong>Biology</strong> <strong>of</strong> <strong>Plasminogen</strong> <strong>Activation</strong> 9
065 • Domain 1 <strong>of</strong> uPAR Is Required for its<br />
Morphological <strong>and</strong> Functional b2 Integrinmediated<br />
Connection with Actin Cytoskeleton<br />
in Human Endothelial Cells • Del Rosso M*,<br />
Fibbi G, Margheri F, Serratì S, Pucci M,<br />
Manetti M, Ibba-Manneschi L<br />
066 • The uPA/uPAR/Vn Pathway <strong>of</strong><br />
Signaling to MAPK-activation • Sarra<br />
Ferraris GM*, Madsen C, Sidenius N<br />
067 • Regulation <strong>of</strong> tPA <strong>and</strong> PAI-1 Gene<br />
Expression in Astrocytes • Hultman K*,<br />
Tjärnlund-Wolf A, Blomstr<strong>and</strong> F, Nilsson M,<br />
Medcalf R, Jern C<br />
068 • Identification <strong>of</strong> a Mitotic Epitope in the<br />
Domain 2 <strong>of</strong> the Urokinase Receptor (uPAR)<br />
• Degryse B*, Eden G, Arnaudova R, Furlan F,<br />
Blasi F<br />
069 • Vitronectin Inhibits <strong>Plasminogen</strong><br />
Activator Inhibitor-1 (PAI-1)-Induced<br />
Chemotaxis by Blocking PAI-1 Binding to<br />
the LDL Receptor-Related Protein • Neels JG,<br />
Kamikubo Y, Degryse B*<br />
070 • Estradiol Inhibits EGF-induced Cell<br />
Migration <strong>and</strong> uPAR Expression in Estrogen<br />
Receptor-a Negative, GPR30 Positive Ovarian<br />
Cancer Cells • Henic E*, Noskova V, Høyer-<br />
Hansen G, Hansson S, Casslén B<br />
071 • Methylation <strong>of</strong> the PAI-1 Gene in Oral<br />
Squamous Cell Carcinomas <strong>and</strong> Normal Oral<br />
Mucosa • Gao S, Krogdahl A, Sørensen JA,<br />
Dabelsteen E, Andreasen PA*<br />
072 • Urokinase Signaling through Its<br />
Receptor Promotes Invasiveness <strong>and</strong><br />
Metastasis <strong>of</strong> Pancreatic Cancer Cells •<br />
Xue A*, Xue M, Jackson C, Song E, Allen BJ,<br />
Smith RC<br />
073 • Tissue <strong>Plasminogen</strong> Activator Induces<br />
Cell Proliferation in Pancreatic Cancer by<br />
a Non-catalytic Mechanism that Requires<br />
ERK1/2 <strong>Activation</strong> through Epidermal<br />
Growth Factor Receptor <strong>and</strong> Annexin A2 •<br />
Ortiz-Zapater E, Peiró S, Roda O, Corominas JM ,<br />
Aguilar S, Ampurdanés C, Real FX, Navarro P*<br />
074 • Modulation <strong>of</strong> Lung Carcinoma Cell<br />
Lines <strong>and</strong> Primary Cultures Migration by<br />
uPA-Derived <strong>and</strong> EGFR Inhibitors • Franco P*,<br />
Mancini A, Votta G, Caputi M, Stoppelli MP<br />
075 • A Novel Role <strong>of</strong> Ku80 in Regulation<br />
<strong>of</strong> PAI-1 Gene Expression in Migrating<br />
Endothelial Cells Induced by Thymosin b4<br />
• Bednarek R*, Boncela J, Smolarczyk K,<br />
Cierniewski CS<br />
076 • Signaling Pathway Involved in<br />
Inhibition <strong>of</strong> PAI-1 Expression by CNP in<br />
Endothelial Cells • Jerczynska H*, Cierniewski<br />
CS, Pawlowska Z<br />
077 • Interaction <strong>of</strong> Alzheimer’s Amyloid<br />
b-peptide (Ab) 1-40 with PAI-2 • Pabba M*,<br />
Przygodzki T, Malisauskas M, Ol<strong>of</strong>sson A,<br />
Morozova-Roche L, Wilczynska M, Ny T<br />
078 • The Subcellular Itinerary <strong>of</strong> Hepatocyte<br />
Growth Factor Activator Inhibitor-1 in MDCK<br />
Cells • Godiksen S, Selzer-Plon J, Pedersen EDK,<br />
Borger Rasmussen H, Bugge TH, Vogel LK*<br />
079 • Evidence for a Matriptase-Prostasin<br />
(CAP1/PRSS8) Serine Protease Zymogen-<br />
Cascade-Regulating Epithelial Differentiation<br />
• List K*, Netzel-Arnett S, Currie B, Szabo R,<br />
Molinolo A, Antalis TM, Bugge TH<br />
080 • The <strong>Plasminogen</strong> <strong>Activation</strong> System<br />
in Monocytic Cell Differentiation <strong>and</strong><br />
Proliferation: Potential Target for <strong>Plasminogen</strong><br />
<strong>Activation</strong> Inhibitor Type- 2-Based<br />
Therapeutics • Lee JA*, Croucher DR, Ranson M<br />
081 • Identification <strong>and</strong> Localization <strong>of</strong><br />
Novel Serine Proteases in the Mouse Ovary •<br />
Wahlberg P*, Nyl<strong>and</strong>er Å, Kui L, Ny T<br />
082 • Alpha-enolase/<strong>Plasminogen</strong> Binding Is<br />
Required during Myogenesis in vitro <strong>and</strong> in<br />
vivo • Diaz-Ramos A*, Llorens A, Luque T,<br />
López-Alemany R<br />
083 • The Serpinb8 Is Alternatively Spliced<br />
to the Known Long Form <strong>and</strong> a Novel Short<br />
Form • Olausson B*, Przygodzka P, Dahl L,<br />
Carlsson L, Wilczynska M<br />
10 X I t h I n t e r n a t i o n a l W o r k s h o p o n
084 • Characterization <strong>of</strong> a Combined PAI-1<br />
<strong>and</strong> TIMP-1 Gene-deficient Mouse Model •<br />
Harslund J*, Nielsen OL, Brünner N, Offenberg H<br />
085 • Dual Role <strong>of</strong> the uPA/uPAR System in<br />
Apoptosis <strong>of</strong> Mesangial Cells <strong>and</strong> Diabetic<br />
Nephropathy • Tkachuk N, Tkachuk S*, Kiyan J,<br />
Shushakova N, Haller H, Dumler I<br />
086 • Phenotypic Consequences <strong>of</strong><br />
<strong>Plasminogen</strong> Activator Inhibitor-1 Gene<br />
Ablation on STAT1 <strong>Activation</strong> <strong>and</strong> Cell Cycle<br />
Progression in Proliferating Endothelial<br />
Cells • Balsara RD*, Morin SJ, Meyer CA,<br />
Castellino FJ, Ploplis VA<br />
087 • Urokinase <strong>and</strong> its Receptor as Novel<br />
C-Myc Target Genes Affecting Cell Migration<br />
<strong>and</strong> Apoptosis • Alfano D*, Iaccarino I,<br />
Stoppelli MP<br />
088 • Effect <strong>of</strong> <strong>Plasminogen</strong> on Cell Migration<br />
Using an in vitro Wound Model • Sulniute R*,<br />
Li J, Ny T<br />
089 • uPA, but not its Receptor uPAR, Is<br />
Necessary for Experimentally-induced <strong>and</strong><br />
Pathological Muscle Regeneration • Vidal B*,<br />
Serrano AL, Jardí M, Suelves M, Muñoz-<br />
Cánoves P<br />
090 • Urokinase-type <strong>Plasminogen</strong> Activator<br />
Deficiency Strongly Attenuates Ischemia<br />
Reperfusion Injury <strong>and</strong> Acute Kidney<br />
Allograft Rejection • Gueler F, Rong S,<br />
Mengel M, Park J-K, Kirsch T, Haller H,<br />
Dumler I, Shushakova N*<br />
091 • a1-antitrypsin Polymerization Studies<br />
using Gas-phase Electrophoretic Mobility<br />
<strong>Molecular</strong> Analysis (GEMMA) • Przygodzki T*,<br />
Mallya M, Phillips RL, Belorgey D, Hägglöf P,<br />
Lomas DA, Ny T<br />
092 • The <strong>Plasminogen</strong> Interaction <strong>of</strong><br />
Antigen 85B Protein from Mycobacterium<br />
Tuberculosis: Role <strong>of</strong> Lys89 • Xolalpa W*,<br />
Vallecillo AJ, Rosales L, Ruiz BH, Espitia C<br />
093 • <strong>Plasminogen</strong> as a Factor in Innate<br />
Immunity • Ahlskog N*, Guo Y, Ny T<br />
094 • The Inflammatory Cytokine Oncostatin<br />
M Induces <strong>Plasminogen</strong> Activator Inhibitor-<br />
1 in Human Vascular Smooth Muscle Cells<br />
in vitro via PI3 kinase <strong>and</strong> MAP-kinase<br />
Dependent Pathways • Demyanets S, Kaun C,<br />
Rychli K, Rega G, Pfaffenberger S, Maurer G,<br />
Huber K, Wojta J*<br />
095 • Crohn’s Disease but not Chronic<br />
Ulcerative Colitis Induces the Expression<br />
<strong>of</strong> PAI-1 in Enteric Neurons • Laerum OD*,<br />
Illemann M, Skarstein A, Helgel<strong>and</strong> L, Øvrebø K,<br />
Danø K, Nielsen BS<br />
096 • The Effect <strong>of</strong> Matrix Metalloprotease<br />
3 Deficiency in Spontaneous Metastasis •<br />
Juncker-Jensen A*, Rømer J, Almholt K<br />
097 • Tumor Cell Expression <strong>of</strong> C4.4A, a<br />
Structural Homologue <strong>of</strong> the Urokinase<br />
Receptor, Correlates with Poor Prognosis<br />
in Non-Small Cell Lung Cancer • Skov BG,<br />
Hansen LV, Ploug M, Pappot H*<br />
098 • Urokinase Receptor Splice Variant<br />
uPAR-del4/5 <strong>and</strong> rab31 mRNA Expression<br />
in Breast Cancer • Magdolen V*, Kotzsch M,<br />
Sieuwerts A, Grosser M, Meye A, Smid M,<br />
Schmitt M, Luther T, Foekens JA<br />
099 • PN-1, a Serine Protease Inhibitor,<br />
Increases MMP-9 Activity in Breast Cancer<br />
Cell Line • Fayard B* <strong>and</strong> Monard D<br />
100 • Cleavage <strong>of</strong> uPAR: Mechanism <strong>and</strong><br />
Prognostic Significance • Høyer-Hansen G*,<br />
Almasi CE, Pappot H<br />
101 • Expression <strong>of</strong> Urokinase Receptor<br />
(uPAR) <strong>and</strong> <strong>Plasminogen</strong> Activator<br />
Inhibitor-1 (PAI-1) in Human Colon Cancer<br />
<strong>and</strong> their Matched Liver Metastases •<br />
Illemann M*, Bird N, Majeed A, Laerum OD,<br />
Lund LR, Danø K, Nielsen BS<br />
102 • A Structural Basis for Differential Cell<br />
Signaling Initiated by PAI-1 <strong>and</strong><br />
PAI-2: Implications for Metastatic Potential •<br />
Croucher D*, Saunders D, Ranson M<br />
<strong>Molecular</strong> & <strong>Cellular</strong> <strong>Biology</strong> <strong>of</strong> <strong>Plasminogen</strong> <strong>Activation</strong> 11
103 • Thrombin Induces Tumor Invasion<br />
through the Induction <strong>and</strong> Association <strong>of</strong><br />
Matrix Metalloproteinase-9 <strong>and</strong> b-1 Integrin<br />
on the Cell Surface • Bruno K*, Radjabi R,<br />
Sawada K, Montag A, Kossiak<strong>of</strong>f A, Lengyel E<br />
104 • Overexpression <strong>of</strong> Protease Nexin-1<br />
mRNA in Oral Squamous Cell Carcinomas •<br />
Gao S, Krogdahl A, Sørensen JA, Dabelsteen E,<br />
Andreasen PA*<br />
105 • The Matrix Metalloprotease (MMP)<br />
Inhibitor Galardin Increases Collagen<br />
Deposition <strong>and</strong> Reduces Spontaneous<br />
Metastasis in the MMTV-PymT Transgenic<br />
Breast Cancer Model • Almholt K*, Lærum OD,<br />
Lund LR, Danø K, Johnsen M, Rømer J<br />
106 • Proteomics <strong>of</strong> uPAR Protein: Protein<br />
Interactions in Cancer Metastasis • Saldanha R,<br />
Molloy M, Xu N, Baker MS*<br />
107 • A New Tagging System for Production<br />
<strong>of</strong> Recombinant Proteins in Drosophila<br />
S2 Cells Using the Third Domain <strong>of</strong> the<br />
Urokinase Receptor • Gårdsvoll H*, Hansen LV,<br />
Jørgensen TJD, Ploug M<br />
108 • Photoaffinity Labeling <strong>of</strong> uPAR with<br />
Cyclic Peptides • Jacobsen B*, Gårdsvoll H,<br />
Barkholt V, Østergaard S, Ploug M<br />
109 • In Vivo Inhibition <strong>of</strong> the Murine<br />
uPA-uPAR Interaction using Monoclonal<br />
Antibodies Raised in uPAR Deficient Mice •<br />
Rasch MG*, Pass J, Jögi A, Rønø B, Gårdsvoll H,<br />
Lund LR, Høyer-Hansen G, Lund IK<br />
110 • RNA Interference for Urokinase-<br />
Targeting Limits Growth <strong>of</strong> Hepatocellular<br />
Carcinoma Xenografts in Nude Mice •<br />
Salvi A*, Arici B, Barlati S, De Petro G<br />
111 • Potent <strong>and</strong> Broad Anti-tumor Activity<br />
<strong>of</strong> an Engineered Matrix Metalloproteinaseactivated<br />
Anthrax Lethal Toxin that Targets<br />
Tumor Vasculature • Liu S, Wang H,<br />
Currie BM, Molinolo A, Leung HJ, Moayeri M,<br />
Alfano RW, Frankel AE, Leppla SH, Bugge TH*<br />
112 • Elucidation <strong>of</strong> the Epitope <strong>of</strong> MA-<br />
31C9, a Non-inhibitory Anti-human PAI-1<br />
Antibody • Meissenheimer LM*, Dewilde M,<br />
Compernolle G, Declerck PJ, Gils A<br />
113 • Residues outside the Epitope Determine<br />
the Function <strong>of</strong> MA-159M12, an Inhibitory<br />
Anti-rat PAI-1 Antibody • Meissenheimer LM*,<br />
Compernolle G, Declerck PJ, Gils A<br />
114 • Conformational Probes <strong>and</strong> Activity<br />
Regulators <strong>of</strong> <strong>Plasminogen</strong> Activator<br />
Inhibitor-1, Isolated from Phage-displayed<br />
Disulphide Bridge-constrained Peptide<br />
Libraries • Dupont DM, Jensen JK, Mathiasen L,<br />
Blouse GE, Wind T, Andreasen PA*<br />
115 • Urokinase-type <strong>Plasminogen</strong> Activatorinhibiting<br />
Cyclic Peptides Demonstrate New<br />
Modalities for Inhibition <strong>of</strong> Serine Proteases •<br />
Andersen LM*, Wind T, Hansen HD, Blouse GE,<br />
Christensen A, Jensen JK, Malmendal A,<br />
Nielsen NC, Andreasen PA<br />
116 • In vivo Treatment with Monoclonal<br />
Antibodies against Mouse Urokinase-type<br />
<strong>Plasminogen</strong> Activator in Cancer Models •<br />
Jögi A*, Lund IK, Høyer-Hansen G, Lund LR,<br />
Danø K, Rømer J<br />
12 X I t h I n t e r n a t i o n a l W o r k s h o p o n
Abstracts for Oral Presentations<br />
i001i<br />
Defining the Native Disulfide Topology in the SMB Domain <strong>of</strong><br />
Human Vitronectin<br />
Li X, Zou G, Yuan W, Lu W*<br />
Institute <strong>of</strong> Human Virology, University <strong>of</strong> Maryl<strong>and</strong> School <strong>of</strong> Medicine, Baltimore, Maryl<strong>and</strong>, USA<br />
Presenting author e-mail: luw@umbi.umd.edu<br />
The N-terminal 44 amino acid residues <strong>of</strong> the human plasma glycoprotein vitronectin, known as<br />
the somatomedin B (SMB) domain, mediates the interaction between vitronectin <strong>and</strong> plasminogen<br />
activator inhibitor 1 (PAI-1) in a variety <strong>of</strong> important biological processes. Several laboratories<br />
have published conflicting reports on the native disulfide topology in the SMB domain with no<br />
consensus reached thus far. Using native chemical ligation <strong>and</strong> orthogonal protection <strong>of</strong> selected<br />
Cys residues, we chemically synthesized three topological analogs <strong>of</strong> SMB with predefined<br />
disulfide connectivities corresponding to those previously published. In addition, we oxidatively<br />
folded a fully reduced SMB in aqueous solution, <strong>and</strong> prepared, by CNBr cleavage, the N-terminal<br />
segment <strong>of</strong> 51 amino acid residues <strong>of</strong> intact vitronectin purified from human blood. Biochemical<br />
<strong>and</strong> functional characterizations allowed us to conclude that (1) only the Cys5-Cys21, Cys9-Cys39,<br />
Cys19-Cys32 <strong>and</strong> Cys25-Cys31 connectivity is present in native vitronectin; (2) only the native<br />
disulfide connectivity is functional; (3) the native disulfide pairings can be readily formed during<br />
spontaneous (oxidative) folding <strong>of</strong> the SMB domain in vitro. Our results unequivocally define the<br />
native disulfide topology in the SMB domain <strong>of</strong> human vitronectin, <strong>and</strong> provide important clues<br />
as to how the controversy arose in the first place.<br />
<strong>Molecular</strong> & <strong>Cellular</strong> <strong>Biology</strong> <strong>of</strong> <strong>Plasminogen</strong> <strong>Activation</strong> 13
i002i<br />
The Vitronectin-Binding Site on the Urokinase Receptor<br />
Comprises Residues from Both Domain I <strong>and</strong> the Flanking Interdomain<br />
Linker Region<br />
Gårdsvoll H <strong>and</strong> Ploug M*<br />
Finsen Laboratory, Rigshospitalet, Copenhagen, Denmark<br />
Presenting author e-mail: m-ploug@finsenlab.dk<br />
The urokinase-type plasminogen activator receptor (uPAR) has been implicated as a modulator<br />
<strong>of</strong> several biochemical processes that are active during tumor invasion <strong>and</strong> metastasis e.g.<br />
extracellular proteolysis, cell adhesion <strong>and</strong> cell motility. The structural basis for the high-affinity<br />
interaction between the urokinase-type plasminogen activator (uPA) <strong>and</strong> uPAR, which focuses<br />
cell surface associated plasminogen activation in vivo, is now thoroughly characterized by sitedirected<br />
mutagenesis studies <strong>and</strong> X-ray crystallography. In contrast, the structural basis for the<br />
interaction between uPAR <strong>and</strong> the extracellular matrix protein vitronectin, which is involved<br />
in the regulation <strong>of</strong> cell adhesion <strong>and</strong> motility, remains to be clarified. In the present study, we<br />
have identified the functional epitope on uPAR that is responsible for its interaction with the<br />
full-length, extended form <strong>of</strong> vitronectin using a comprehensive alanine-scanning library <strong>of</strong><br />
purified single-site uPAR mutants (244 positions tested). Interestingly, the 5 residues identified<br />
as ‘’hot spots’’ for vitronectin binding form a contiguous epitope comprising two exposed loops<br />
connecting the central 4-str<strong>and</strong>ed b-sheet in uPAR domain I (Trp32, Arg58 <strong>and</strong> Ile63) as well<br />
as a proximal region <strong>of</strong> the flexible linker peptide connecting uPAR domains I <strong>and</strong> II (Arg91<br />
<strong>and</strong> Tyr92). This binding topology provides the molecular basis for the observation that uPAR<br />
can form a ternary complex with uPA <strong>and</strong> vitronectin. We also show that the affinity for the<br />
small SMB domain <strong>of</strong> vitronectin is increased approximately 4-fold for uPAR-uPA complexes as<br />
compared to unoccupied uPAR.<br />
14 X I t h I n t e r n a t i o n a l W o r k s h o p o n
i003i<br />
uPAR-induced Cell Adhesion <strong>and</strong> Migration:<br />
Vitronectin Provides the Key<br />
Madsen CD* 1 , Sarra Ferraris GM1 , Andolfo A1 , Cunningham O1 1, 2<br />
, Sidenius N<br />
1 The FIRC Institute <strong>of</strong> <strong>Molecular</strong> Oncology (IFOM), Milan, Italy;<br />
2 <strong>Molecular</strong> Genetics Unit, DIBIT, Università Vita-Salute San Raffaele, Milan, Italy<br />
Presenting author e-mail: chris.madsen@ifom-ieo-campus.it<br />
Expression <strong>of</strong> the GPI-anchored membrane receptor uPAR induces pr<strong>of</strong>ound changes in cell<br />
adhesion <strong>and</strong> migration, <strong>and</strong> its expression correlates with the malignant phenotype <strong>of</strong> cancers. To<br />
identify the key molecular interactions essential for uPAR function in these processes; we carried<br />
out a complete functional alanine-scan <strong>of</strong> uPAR in HEK293 cells. Of the 255 mutant receptors<br />
characterized, 34 failed to induce changes in cell adhesion, cell morphology accompanied by<br />
actin-rearrangement <strong>and</strong> focal adhesion turn-over, <strong>and</strong> cell migration. Remarkably, the molecular<br />
defect <strong>of</strong> all <strong>of</strong> these mutants was a specific reduction in integrin-independent cell binding to the<br />
somatomedin-B domain <strong>of</strong> the extracellular matrix component, vitronectin. In order to mimic the<br />
membrane-ECM interaction induced by uPAR-Vn, we generated a GPI-anchored plasminogen<br />
activator inhibitor-1 (PAI-1). This, like uPAR, binds specifically <strong>and</strong> with high affinity to the SMB<br />
domain <strong>of</strong> Vn but shares no other similarity with uPAR. Surprisingly, the chimeric PAI-1/GPI<br />
recapitulated the biological effects <strong>of</strong> uPAR expression. A direct uPAR-Vn interaction is thus both<br />
required <strong>and</strong> sufficient to initiate downstream signalling leading to changes in cell morphology<br />
<strong>and</strong> migration. Together these data demonstrate a novel mechanism by which a cell adhesion<br />
molecule lacking inherent signalling capability evokes complex cellular responses, independently<br />
<strong>of</strong> lateral interactions with signalling receptors, by modulating the contact between the cell <strong>and</strong><br />
the matrix. The importance <strong>of</strong> the uPAR/Vn-interaction was not cell-type specific as all mutants<br />
identified were subsequently confirmed in CHO cells. Finally we have mapped the direct<br />
vitronectin binding epitope (W32, R58, I63, R91, Y92) <strong>of</strong> uPAR.<br />
<strong>Molecular</strong> & <strong>Cellular</strong> <strong>Biology</strong> <strong>of</strong> <strong>Plasminogen</strong> <strong>Activation</strong> 15
i004i<br />
Interactions between PAI-1 <strong>and</strong> Vitronectin: Two Proteins,<br />
Two Sites, <strong>and</strong> Two Phases<br />
Schar CR 1 , Jensen JK 2 , Blouse GE 2 , Minor KH 1 , Andreasen PA 2 , Peterson CB* 1<br />
1Department <strong>of</strong> Biochemistry, <strong>Cellular</strong>, <strong>and</strong> <strong>Molecular</strong> <strong>Biology</strong>, University <strong>of</strong> Tennessee, Knoxville,<br />
Tennessee, USA;<br />
2Laboratory <strong>of</strong> <strong>Cellular</strong> Protein Science, Department <strong>of</strong> <strong>Molecular</strong> <strong>and</strong> Structural <strong>Biology</strong>, University <strong>of</strong><br />
Aarhus, Aarhus, Denmark<br />
Presenting author e-mail: cbpeters@utk.edu<br />
We have generated a mutant form <strong>of</strong> vitronectin that lacks the well-characterized N-terminal<br />
somatomedin B domain, known to house the primary high-affinity site for binding <strong>of</strong> PAI-1 to<br />
vitronectin. Residual binding <strong>of</strong> PAI-1 to this deletion mutant <strong>of</strong> vitronectin is observed. Also, we<br />
have used a large battery <strong>of</strong> mutant forms <strong>of</strong> PAI-1 to evaluate the specific interactions required<br />
for binding. With these reagents, the second binding site for vitronectin on PAI-1 was mapped<br />
to a region around helix D rich in charged amino acids. We have used kinetic <strong>and</strong> equilibrium<br />
measurements with surface plasmon resonance to study PAI-1 to full-length <strong>and</strong> the truncated<br />
mutant <strong>of</strong> vitronectin that is missing the somatomedin B domain. Clearly, the interaction <strong>of</strong><br />
vitronectin <strong>and</strong> PAI-1 at the second site is weaker than the primary interaction between the<br />
somatomedin B domain <strong>and</strong> the flexible joint region that lies between helices D, E <strong>and</strong> F on<br />
PAI-1. Most notably, the <strong>of</strong>f rate for binding is much faster, comparable to that for latent PAI-1<br />
dissociation from vitronectin. Interestingly, latent PAI-1 binds nearly as well at the second site<br />
as does active PAI-1, consistent with less dramatic structural changes in the helix D region upon<br />
conversion to the latent structure compared to those that occur with expansion <strong>of</strong> the central beta<br />
sheet that affect the primary binding site interactions with the somatomedin B domain. These<br />
characteristic features <strong>of</strong> binding at the two sites are consistent with FRET experiments <strong>and</strong><br />
stopped-flow fluorescence measurements that reveal biphasic binding between vitronectin <strong>and</strong><br />
PAI-1.<br />
16 X I t h I n t e r n a t i o n a l W o r k s h o p o n
i005i<br />
How Does Vitronectin Accelerate PAI-1’s Protease Inhibition?<br />
Zhou A* <strong>and</strong> Wei Z<br />
Department <strong>of</strong> Haematology, University <strong>of</strong> Cambridge, CIMR, Cambridge, United Kingdom<br />
Presenting author e-mail: awz20@cam.ac.uk<br />
Vitronectin binds <strong>and</strong> stabilises PAI-1’s activity through its somatomedin B (SMB) domain.<br />
Vitronectin can also accelerate PAI-1’s protease (thrombin <strong>and</strong> activated protein C) inhibition<br />
by more than 100-fold. To investigate the mechanism underlying this acceleration, firstly we<br />
prepared SMB domain alone <strong>and</strong> various SMB containing fragments <strong>of</strong> vitronectin. Kinetics<br />
studies showed that these fragments <strong>of</strong> vitronectin, like urea-treated vitronectin, had little effect<br />
on PAI-1’s protease inhibition. Secondly cross-linking experiment with inactive thrombin variant<br />
(S195A) showed that thrombin could only be cross-linked to native VN (not urea-treated VN) in<br />
the presence <strong>of</strong> active PAI-1. Thirdly, mutagenasis studies <strong>of</strong> thrombin showed that substitution<br />
<strong>of</strong> the surface exposed residue Asp100 with Arg attenuated vitronectin PAI-1’s inhibition<br />
<strong>of</strong> thrombin by more than 50%, while other mutations <strong>of</strong> thrombin such as Glu97Arg <strong>and</strong><br />
Asp178Arg etc had no effect. Altogether, these data indicate that native vitronectin has a cryptic<br />
thrombin binding site, which is exposed upon PAI-1 binding (likely masked in urea treated VN)<br />
<strong>and</strong> interacts with thrombin surface near Asp100, <strong>and</strong> vitronectin accelerates PAI-1’s protease<br />
inhibition by bridging PAI-1 <strong>and</strong> thrombin together.<br />
<strong>Molecular</strong> & <strong>Cellular</strong> <strong>Biology</strong> <strong>of</strong> <strong>Plasminogen</strong> <strong>Activation</strong> 17
i006i<br />
The Interaction between Tissue-type <strong>Plasminogen</strong> Activator <strong>and</strong><br />
the Low Density Lipoprotein Receptor-Related Protein Induces<br />
<strong>Activation</strong> <strong>of</strong> the NF-kB Pathway during Cerebral Ischemia<br />
Yepes M*, Brotzge XH, Polavarapu R<br />
Department <strong>of</strong> Neurology <strong>and</strong> Center for Neurodegenerative Disease, Emory University School <strong>of</strong><br />
Medicine, Atlanta, Georgia, USA<br />
Presenting author e-mail: myepes@emory.edu<br />
We previously demonstrated that the interaction between tPA <strong>and</strong> the low density lipoprotein<br />
receptor-related protein (LRP) following middle cerebral artery occlusion (MCAO) increases<br />
the permeability <strong>of</strong> the blood brain barrier (BBB). Here we studied the relation between tPA <strong>and</strong><br />
NF-kB activation following MCAO. Wild-type (WT), tPA (tPA–/–), <strong>and</strong> plasminogen (Plg–/–)<br />
deficient mice underwent MCAO <strong>and</strong> analysis <strong>of</strong> NF-kB activation by immunohistochemistry,<br />
Western blot (p65-phosphorylation) <strong>and</strong> electrophoretic mobility shift assay (EMSA). We observed<br />
a rapid activation <strong>of</strong> NF-kB in WT <strong>and</strong> Plg–/– mice that was abolished in tPA–/– animals. The<br />
effect <strong>of</strong> MCAO on LRP expression was studied by immunohistochemistry <strong>and</strong> quantitative<br />
real-time PCR (qRT-PCR). We found that MCAO induces a rapid increase in LRP expression<br />
in WT mice that is significantly attenuated in tPA–/– mice. Treatment <strong>of</strong> WT mice with either<br />
the receptor associated protein (RAP) or anti-LRP antibodies inhibited MCAO-induced NF-kB<br />
activation. The intracerebral injection <strong>of</strong> tPA into tPA–/– mice following MCAO resulted in NF-kB<br />
activation that was not observed when tPA was co-administered with either RAP or LRP-blocking<br />
antibodies. Immunohistochemistry <strong>and</strong> qRT-PCR demonstrated an increase in the expression <strong>of</strong><br />
inducible nitric oxide synthase (NF-kB-dependent gene) in the ischemic area in WT mice that<br />
was attenuated in tPA–/– mice <strong>and</strong> in WT animals treated with RAP or anti-LRP antibodies.<br />
We conclude that during cerebral ischemia tPA has a plasminogen-independent ‘’cytokine-like’’<br />
function <strong>and</strong> that the interaction between tPA <strong>and</strong> LRP results in NF-kB pathway activation <strong>and</strong><br />
induction <strong>of</strong> NF-kB-dependent genes with known effect on cell death <strong>and</strong> BBB permeability.<br />
18 X I t h I n t e r n a t i o n a l W o r k s h o p o n
i007i<br />
Unique Secretory Dynamics <strong>of</strong> Tissue <strong>Plasminogen</strong> Activator (tPA)<br />
Is Beneficial to Maintain Fibrinolytic Activity on Cell Surface<br />
Suzuki Y*, Ihara H, Mogami H, Urano T<br />
Department <strong>of</strong> Physiology, Hamamatsu University School <strong>of</strong> Medicine, Hamamatsu, Japan<br />
Presenting author e-mail: seigan@hama-med.ac.jp<br />
Introduction: Vascular endothelial cells (VECs) express <strong>and</strong> secrete various anti-thrombotic<br />
molecules to keep the vascular patency. tPA, the primary fibrinolytic enzyme in vasculature, is<br />
one <strong>of</strong> them. After secretion as an active form, tPA initiates fibrinolysis both on VECs <strong>and</strong> in blood<br />
where its specific inhibitor <strong>of</strong> PAI-1 exists. Here, we analyzed the dynamics <strong>of</strong> tPA secretion from<br />
the containing granules <strong>and</strong> its modulation by PAI-1 using total internal reflection fluorescence<br />
microscopy (TIRF-M). Method: An established cell-line <strong>of</strong> VECs was cultured <strong>and</strong> transfected<br />
with green fluorescent protein (GFP)-tagged either wild type tPA, tPA (S478A)(Ser478 at active<br />
center is replaced by Ala, no ability to complex with PAI-1) or tPA (catalytic domain; CD)(deleted<br />
in finger-, EGF-like-, kringle1- <strong>and</strong> 2- domains). The exocytotic dynamics <strong>of</strong> these tPAs-GFP near<br />
the plasma membrane (PM) were analyzed by TIRF-M. Results: (1) tPA-GFP showed unique<br />
dynamics <strong>of</strong> slow disappearance from PM after opening <strong>of</strong> its containing granules (fluorescence<br />
half life: TF1/2=10sec). (2) Supplemented PAI-1 shortened TF1/2 <strong>and</strong> increased tPA-PAI-1<br />
complex but not free tPA in supernatant. TF1/2 <strong>of</strong> tPA(S478A)-GFP was slower than tPA-GFP,<br />
indicating that the complex formation with PAI-1 is essential for rapid dissociation <strong>of</strong> tPA from<br />
the opened granular membrane. (3) TF1/2 <strong>of</strong> tPA(CD)-GFP was faster than tPA-GFP, indicating<br />
that FEK domains are responsible for slow disappearance. Conclusion: tPA has unique, slow<br />
secretory dynamics which is beneficial to maintain fibrinolytic activity on VECs. PAI-1 facilitates<br />
tPA dissociation <strong>and</strong> suppresses fibrinolytic activity on VECs.<br />
<strong>Molecular</strong> & <strong>Cellular</strong> <strong>Biology</strong> <strong>of</strong> <strong>Plasminogen</strong> <strong>Activation</strong> 19
i008i<br />
The Macrophage Low-density Lipoprotein-Receptor-Related<br />
Protein (LRP) Modulates Murine Lipoprotein Metabolism<br />
Lillis AP* 1,2 , Mikhailenko I 1 , Robinson S 1 , Migliorini M 1 , Battey F 1 , Pizzo SV 2 , Strickl<strong>and</strong> DK 1<br />
1Center for Vascular <strong>and</strong> Inflammatory Diseases, University <strong>of</strong> Maryl<strong>and</strong> School <strong>of</strong> Medicine, Baltimore,<br />
Maryl<strong>and</strong>, USA;<br />
2 Department <strong>of</strong> Pathology, Duke University Medical Center, Durham, North Carolina, USA<br />
Presenting author e-mail: alillis@som.umaryl<strong>and</strong>.edu<br />
Very low-density lipoproteins (VLDL) <strong>and</strong> chylomicrons transport cholesterol <strong>and</strong> triglycerides<br />
(TG) to muscle, adipose <strong>and</strong> other extra-hepatic tissues. Lipoprotein lipase selectively removes<br />
<strong>and</strong> hydrolyzes TGs, transferring free fatty acids to these tissues. The resulting remnant<br />
lipoproteins bind to two members <strong>of</strong> the low-density lipoprotein receptor (LDLR) family, LDLR<br />
itself <strong>and</strong> the LDLR-related protein (LRP). LRP is a large endocytic receptor that recognizes more<br />
than 30 different lig<strong>and</strong>s. Accumulating evidence supports a role for hepatic LRP in the clearance<br />
<strong>of</strong> remnant lipoproteins. However, LRP is also abundant in resident liver macrophages (Kupffer<br />
cells) which reside in the sinusoids <strong>of</strong> the liver in close proximity to the space between endothelial<br />
cells <strong>and</strong> hepatocytes where lipoprotein remnants are sequestered <strong>and</strong> modified before being<br />
recognized by LRP <strong>and</strong> the LDL receptor. To investigate a possible role <strong>of</strong> macrophage LRP in<br />
remnant lipoprotein metabolism, we developed tissue-specific knockouts using the LoxP/Cremediated<br />
recombination system on mice genetically deficient in the LDLR. By crossing mice<br />
carrying loxP-tagged LRP with a LysMCre transgenic mouse line expressing the Cre recombinase<br />
at the mouse M lysozyme locus, we have generated LDLR-deficient mice in which the LRP gene<br />
is also selectively <strong>and</strong> efficiently deleted in macrophages (macLRP- mice). After placing macLRP-<br />
mice (<strong>and</strong> their sibling controls which are deficient in LDLR but express LRP normally) on a high<br />
fat, high cholesterol (Western) diet for 3 weeks, we observed elevated serum triglycerides (5.0 vs<br />
2.8 mg/ml, p
i009i<br />
Annexin 2 Mediates <strong>Plasminogen</strong>-Dependent Recruitment <strong>of</strong><br />
Neovascular Mural Cells in Lymphoma Angiogenesis<br />
Ling Q 1 , Ruan J 2 , Yan L 1 , Sui G-Z 1 , Deora AB 1 , Church S 2 , Cohen-Gould L 1 , Rafii S 2 , Lyden D 3 ,<br />
Hajjar KA* 1<br />
Departments <strong>of</strong> 1 Cell <strong>and</strong> Developmental <strong>Biology</strong>, 2 Medicine, 3 Pediatrics, Weill Cornell Medical College,<br />
New York, New York, USA<br />
Presenting author e-mail: khajjar@med.cornell.edu<br />
Malignant tumor progression depends upon the development <strong>of</strong> tumor-associated blood vessels,<br />
either via co-option <strong>of</strong> nearby host vascular cells, or through recruitment <strong>of</strong> marrow-derived<br />
progenitor cells. Annexin 2 (A2) is a cell surface co-receptor for plasminogen (Plg) <strong>and</strong> tPA that<br />
augments the catalytic efficiency <strong>of</strong> Plg activation. We showed previously that A2–/– mice display<br />
impaired growth factor-induced postnatal angiogenesis in the corneal pocket, oxygen-induced<br />
retinopathy, <strong>and</strong> Matrigel plug assays. Here, we examined neovascularization <strong>of</strong> experimental<br />
lymphoma in mice with fibrinolytic deficiency states. For EL4, a T cell lymphoma, <strong>and</strong> B6RV2, a<br />
B cell lymphpma, tumor growth was rapid in wildtype <strong>and</strong> tPA–/– mice, but severely retarded<br />
in both A2–/– <strong>and</strong> Plg–/– mice. Immunohistochemical staining <strong>of</strong> EL4 tissue on day 8 revealed<br />
reduced vascular density, frequent intravascular fibrin thrombi, <strong>and</strong> dilated microvessels in<br />
A2–/–, but not A2+/+, mice. Electron microscopy <strong>and</strong> immun<strong>of</strong>luorescence revealed a paucity<br />
<strong>of</strong> pericytes <strong>and</strong> secondary dropout <strong>of</strong> endothelial cells within A2–/– tumor microvessels. Flow<br />
cytometric analysis <strong>of</strong> circulating marrow-derived progenitor cells showed reduced populations<br />
<strong>of</strong> VEGFR1+/CD11b+ hematopoietic precursor cells in A2–/– versus A2+/+ tumor-bearing mice.<br />
In lethally irradiated A2–/– mice, tumor growth was rescued completely upon engraftment<br />
with A2+/+ marrow. Transplantation <strong>of</strong> green fluorescent protein (GFP)-positive bone marrow<br />
led to the recruitment <strong>of</strong> abundant GFP+/CD11b+/CD68+ cells to locations surrounding<br />
tumor neovessels. In addition, transplantation <strong>of</strong> normal marrow restored the investment <strong>of</strong><br />
tumor microvessels with a-smooth muscle actin-positive pericytes. These data indicate that A2<br />
contributes critically to tumor angiogenesis in experimental lymphoma, by enabling recruitment<br />
<strong>of</strong> A2+ myelomonocytic cells that instruct pericyte recruitment <strong>and</strong> neovascular stabilization.<br />
<strong>Molecular</strong> & <strong>Cellular</strong> <strong>Biology</strong> <strong>of</strong> <strong>Plasminogen</strong> <strong>Activation</strong> 21
i010i<br />
<strong>Activation</strong> <strong>of</strong> Latent PDGF-CC by Tissue <strong>Plasminogen</strong> Activator<br />
Impairs Blood Brain Barrier Integrity during Ischemic Stroke<br />
Su EJ 1 , Fredriksson L 2 , Geyer M 1 , Folestad E 2 , Cale J 1 , Mann K 1 , Gao Y 3 , Pietras K 2 , Andreé J 4 , Yepes M 5 ,<br />
Strickl<strong>and</strong> D 3 , Betsholtz C 4 , Eriksson U 2 , Lawrence DA* 1<br />
1Department <strong>of</strong> Internal Medicine, Division <strong>of</strong> Cardiovascular Medicine, University <strong>of</strong> Michigan<br />
Medical School, Ann Arbor, Michigan, USA;<br />
2 Ludwig Institute for Cancer Research, Stockholm Branch, Karolinska Institutet, Stockholm, Sweden;<br />
3Center for Vascular <strong>and</strong> Inflammatory Disease <strong>and</strong> Departments <strong>of</strong> Surgery <strong>and</strong> Physiology, School <strong>of</strong><br />
Medicine, University <strong>of</strong> Maryl<strong>and</strong>, Baltimore, Maryl<strong>and</strong>, USA;<br />
4Laboratory <strong>of</strong> Vascular <strong>Biology</strong>, Division <strong>of</strong> Matrix <strong>Biology</strong>, Department <strong>of</strong> Medical Biochemistry <strong>and</strong><br />
Biophysics, Karolinska Institutet, Stockholm, Sweden;<br />
5Department <strong>of</strong> Neurology <strong>and</strong> Center for Neurodegenerative Disease, Emory University School <strong>of</strong><br />
Medicine, Atlanta, Georgia, USA<br />
Presenting author e-mail: dlawrenc@umich.edu<br />
The current treatment for ischemic stroke, intravenous tPA, only benefits a limited number <strong>of</strong><br />
patients. This is due in part to the requirement that tPA be administered within 3 hours <strong>of</strong> the<br />
onset <strong>of</strong> symptoms. The reasons for this time constraint are not known but may be due to the<br />
unique activities that tPA has in the brain beyond its well established role as a fibrinolytic enzyme.<br />
For example, tPA has been shown to play a role in regulating cerebrovascular permeability<br />
after stroke; however, the specific substrate for tPA in brain is not known. The recent discovery<br />
that tPA cleaves latent PDGF-CC lead us to hypothesize that tPA may mediate cerebrovascular<br />
permeability via activation <strong>of</strong> latent PDGF-CC. To test this possibility, active PDGF-CC was<br />
injected directly into the CSF in the absence <strong>of</strong> ischemia <strong>and</strong> the extravasation <strong>of</strong> Evans Blue<br />
dye in the brain was examined. These studies showed a significant increase in Evans Blue<br />
extravasation after active PDGF-CC injection. This effect was similar to that seen with tPA<br />
injection, suggesting that tPA <strong>and</strong> PDGF-CC may be acting on the same pathway. To test this<br />
neutralizing antibodies against PDGF-CC were co-injected with tPA <strong>and</strong> were found to block<br />
the effect <strong>of</strong> tPA. To evaluate whether PDGF-CC plays a role in regulating cerebrovascular<br />
permeability during stroke, the PDGF receptor inhibitor Gleevec was used in a photothrombotic<br />
stroke model. Stroke is induced specifically in the middle cerebral artery by the local activation<br />
<strong>of</strong> intravenous Rose Bengal with a cold laser. Mice treated with Gleevec showed significant<br />
reductions in Evans Blue extravasation at 24-hours <strong>and</strong> stroke volumes at 72-hours, indicating a<br />
strong effect <strong>of</strong> PDGF signaling on cerebrovascular integrity. Taken together, these data suggest<br />
that PDGF-CC is a downstream substrate <strong>of</strong> tPA in the CNS. These studies may provide important<br />
insights into new therapeutic strategies for treating stroke patients.<br />
22 X I t h I n t e r n a t i o n a l W o r k s h o p o n
i011i<br />
<strong>Plasminogen</strong> Activator Inhibitor-1 Gene Regulation:<br />
Cross Talk between Hypoxia <strong>and</strong> Insulin Signalling<br />
Flugel D <strong>and</strong> Kietzmann T*<br />
Faculty <strong>of</strong> Chemistry, Department Biochemistry, University <strong>of</strong> Kaiserslautern, Kaiserslautern, Germany<br />
Presenting author e-mail: tkietzm@gwdg.de<br />
A number <strong>of</strong> pathological conditions like cancer, diabetes or the metabolic syndrome are<br />
associated with enhanced plasminogen activator inhibitor-1 (PAI-1) levels. In addition, these<br />
diseases are <strong>of</strong>ten combined with hypoxia <strong>and</strong> an impaired insulin signalling. Therefore we asked<br />
whether hypoxia <strong>and</strong> insulin can exert direct effects on PAI-1 expression. We found that hypoxia<br />
induced PAI-1 expression via the hypoxia-inducible transcription factor-1 (HIF-1) which binds<br />
to hypoxia responsive elements in the PAI-1 promoter. HIF-1 is a heterodimer from which HIF-<br />
1alpha becomes hydroxylated under normoxia. This enables binding <strong>of</strong> the von Hippel-Lindau<br />
(VHL) protein which targets HIF-1alpha for proteasomal degradation.<br />
Interestingly, HIF-1a can also respond to non-hypoxic stimuli like insulin which acts via<br />
phosphatidylinositol 3-kinase <strong>and</strong> protein kinase B. Although PKB induces HIF-1alpha<br />
stabilization, HIF-1a is not a direct substrate for PKB/Akt. Therefore, we aimed to investigate<br />
whether glycogen synthase kinase-3 (GSK3) may have an impact on the VHL-dependent HIF-<br />
1alpha degradation.<br />
We found that inhibition <strong>of</strong> GSK3 with LiCl <strong>and</strong> insulin as well as depletion with siRNA induced<br />
HIF-1alpha <strong>and</strong> PAI-1 expression whereas overexpression <strong>of</strong> GSK3alpha <strong>and</strong> GSK3beta reduced it.<br />
These effects were mediated posttranslationally via the oxygen-dependent degradation domain <strong>of</strong><br />
HIF-1alpha. Mutation <strong>of</strong> the proline residues critical for the VHL-dependent degradation as well<br />
as usage <strong>of</strong> VHL-deficient cells did not prevent GSK3-mediated ubiquitylation <strong>and</strong> degradation <strong>of</strong><br />
HIF-1alpha. However, inhibition <strong>of</strong> the proteasome by MG132 partially reversed the GSK3 effects<br />
indicating that GSK3 could target HIF-1alpha to the proteasome by phosphorylation. Further,<br />
we identified three putative target sites for GSK3 within HIF-1alpha <strong>and</strong> mutation <strong>of</strong> these sites<br />
increased HIF-1alpha transactivity, protein stability <strong>and</strong> PAI-1 expression.<br />
Thus, the present data show that hypoxia <strong>and</strong> insulin signalling merge at HIF-1alpha which<br />
appears to have a prominent role for the regulation <strong>of</strong> PAI-1 expression.<br />
<strong>Molecular</strong> & <strong>Cellular</strong> <strong>Biology</strong> <strong>of</strong> <strong>Plasminogen</strong> <strong>Activation</strong> 23
i012i<br />
Role <strong>of</strong> Rho GTPases <strong>and</strong> p38 MAP Kinase in the Regulation <strong>of</strong><br />
t-PA <strong>and</strong> PAI-1 Expression in Cultured Human Endothelial Cells<br />
Fish RJ*, Dunoyer-Geindre S, Kruith<strong>of</strong> EKO<br />
Service <strong>of</strong> Angiology <strong>and</strong> Haemostasis, Department <strong>of</strong> Internal Medicine, Geneva University Hospital<br />
<strong>and</strong> Medical School, Geneva, Switzerl<strong>and</strong><br />
Presenting author e-mail: Richard.Fish@medecine.unige.ch<br />
HMG-CoA reductase inhibitors, or statins, are used as cholesterol-lowering drugs for<br />
cardiovascular disease (CVD). Clinical evidence suggests that statins are also beneficial for CVD<br />
patients independently from their effects on cholesterol levels. Statins increase endothelial cell<br />
expression <strong>of</strong> t-PA while lowering levels <strong>of</strong> PAI-1. This could increase the fibrinolytic potential<br />
<strong>of</strong> the endothelium <strong>and</strong> be beneficial in CVD. We investigated the mechanism <strong>of</strong> statin-induced<br />
changes in t-PA <strong>and</strong> PAI-1 expression in HUVEC. t-PA <strong>and</strong> PAI-1 mRNA were measured by<br />
quantitative RT-PCR. A time- <strong>and</strong> dose-dependent increase in t-PA, <strong>and</strong> decrease in PAI-1,<br />
were measured in fluvastatin-treated HUVEC. These changes were reversed by mevalonate<br />
or geranylgeranyl pyrophosphate, <strong>and</strong> mimicked by a geranylgeranyl transferase inhibitor -<br />
demonstrating that the statins effects were mediated by inhibition <strong>of</strong> protein geranylgeranylation.<br />
Rho family GTPases are geranylgeranylated <strong>and</strong> therefore potential targets for the effects <strong>of</strong><br />
fluvastatin. Dominant negative (DN) RhoA, Rac1 <strong>and</strong> Cdc42 were expressed in HUVEC. A<br />
minor increase in t-PA expression was measured in cells expressing DNRhoA, while DNRac1<br />
or DNCdc42 expression each lead to a three-fold increase. PAI-1 expression decreased in cells<br />
expressing DNRhoA or DNRac1, but not in cells expressing DNCdc42. Fluvastatin-induced t-PA<br />
expression is most likely mediated by p38 MAP kinase (p38) because the p38 inhibitor, SB202190,<br />
reversed fluvastatin-induced t-PA expression but not the decrease in PAI-1. Our results show<br />
a role for p38 in statin-induced t-PA, with geranylgeranylated Rho GTPases as potential statin<br />
targets. Endothelial t-PA <strong>and</strong> PAI-1 expression appear to be differentially regulated by Rho<br />
GTPases.<br />
24 X I t h I n t e r n a t i o n a l W o r k s h o p o n
i013i<br />
Urokinase Receptor/Alpha5Beta1 Integrin Interaction <strong>and</strong><br />
Signaling in Cancer Cells<br />
Wei Y*, Tang CH, Kim Y, Robillard L, Kugler MC, Hill M, Brumwell A, Chapman HA<br />
Pulmonary <strong>and</strong> Critical Care Division, Department <strong>of</strong> Medicine, Cardiovascular Research Institute,<br />
University <strong>of</strong> California, San Francisco, California, USA<br />
Presenting author e-mail: ying.wei@ucsf.edu<br />
The urokinase receptor (uPAR) is commonly upregulated in tumor cells <strong>and</strong> thought to promote<br />
cancer invasion <strong>and</strong> metastasis. Our previous studies show that uPAR binds fibronectin (Fn)<br />
receptor a5b1 integrin, the complex shifting the integrin binding site on Fn from the canonical<br />
RGD motif to a nearby Fn heparin binding domain (HepII). We hypothesized that uPAR<br />
interactions with a5b1 modulate Fn signaling <strong>and</strong> promote tumor progression in vivo. To study the<br />
effects <strong>of</strong> uPAR/a5b1 interactions on signaling, endogenous uPAR was stably silenced by RNAi in<br />
malignant tumor cell lines HT1080 <strong>and</strong> H1299 <strong>and</strong> reconstituted with WT uPAR or a uPAR point<br />
mutant (H249A) discovered to be defective in a5b1-binding. Fn attachment initiated src/FAK,<br />
Rac1, <strong>and</strong> ERK activation followed by MMP-9 expression. In both uPAR knockdown <strong>and</strong> H249A<br />
uPAR bearing tumor cells Fn adhesion initiated src/FAK activation but was unable to activate<br />
Rac1 or ERK or induce MMP-9. Thus MMP-9 induction by Fn depends on two signals: one from<br />
a5b1 leading to active src/FAK <strong>and</strong> one from a5b1/uPAR leading to active Rac1. Both are required<br />
from ERK activation <strong>and</strong> MMP-9 induction. In vivo, knockdown <strong>of</strong> uPAR in tumor cells injected<br />
intravenously or into the lung orthotopically resulted in markedly reduced tumor incidence <strong>and</strong><br />
size. UPAR knockdown cells maintained low levels <strong>of</strong> MMP-9 after at least two days in the mouse<br />
lungs. Collectively, these data demonstrate that uPAR/a5b1 complexes are required for MMP-9<br />
induction through an ERK-dependent <strong>and</strong> that this signaling pathway may be relevant to tumor<br />
development in vivo.<br />
<strong>Molecular</strong> & <strong>Cellular</strong> <strong>Biology</strong> <strong>of</strong> <strong>Plasminogen</strong> <strong>Activation</strong> 25
i014i<br />
Activated Human Neutrophils Rapidly Release the Chemotactically<br />
Active D2D3 Form <strong>of</strong> the Urokinase-type <strong>Plasminogen</strong> Activator<br />
Receptor (uPAR/CD87)<br />
Pliyev BK* 1,2 <strong>and</strong> Tkachuk VA 1,2<br />
1Department <strong>of</strong> Biological <strong>and</strong> Medical Chemistry, School <strong>of</strong> Basic Medicine, Moscow State University,<br />
Moscow, Russia;<br />
2<strong>Molecular</strong> Endocrinology Laboratory, Institute <strong>of</strong> Experimental Cardiology, Cardiology Research<br />
Center, Moscow, Russia<br />
Presenting author e-mail: bpliyev@cardio.ru<br />
The urokinase-type plasminogen activator receptor (uPAR/CD87) exists both in cell-bound <strong>and</strong><br />
soluble forms. Soluble uPAR (suPAR) is readily detected in blood <strong>and</strong> is markedly increased<br />
during inflammation <strong>and</strong> cancer. Neutrophils contain extensive intracellular pools <strong>of</strong> uPAR that<br />
are translocated to the plasma membrane upon activation. In the present study, we investigated<br />
the ability <strong>of</strong> human neutrophils to shed uPAR from cell surface following activation <strong>and</strong><br />
addressed the possible involvement <strong>of</strong> the released receptor in inflammatory response. We<br />
first observed that resting neutrophils spontaneously release suPAR. This release was strongly<br />
<strong>and</strong> rapidly (within minutes) enhanced by calcium ionophore ionomycin <strong>and</strong> to a lesser extent<br />
when cells were primed with TNF-alpha or LPS <strong>and</strong> then stimulated with fMLP or IL-8. We<br />
demonstrate that suPAR is produced by resting <strong>and</strong> activated neutrophils predominantly as a<br />
truncated form devoid <strong>of</strong> N-terminal D1 domain (D2D3 form) that lacks GPI anchor. Migration<br />
<strong>of</strong> human embryonic kidney (HEK) 293 cells stably transfected with the human formyl peptide<br />
receptor FPRL1 towards the supernatants harvested from activated neutrophils was significantly<br />
diminished when suPAR was immunodepleted from the supernatants. We conclude that activated<br />
neutrophils release the chemotactically active D2D3 form <strong>of</strong> suPAR that acts as a lig<strong>and</strong> <strong>of</strong><br />
FPRL1. The release <strong>of</strong> suPAR by activated cells was significanty but not completely inhibited by<br />
alpha 1-antichymotrypsin, a specific inhibitor <strong>of</strong> cathepsin G, indicating that cathepsin G acts as<br />
a shedding protease for membrane-bound uPAR. Neutrophils isolated from synovial fluids <strong>of</strong><br />
rheumatoid arthritis patients released significantly (p < 0.01) higher amounts <strong>of</strong> suPAR compared<br />
with cells isolated from pared peripheral blood samples suggesting that the release <strong>of</strong> suPAR by<br />
neutrophils is increased in vivo in the sites <strong>of</strong> acute inflammation. We suggest that production <strong>of</strong><br />
the chemotactically active D2D3 form <strong>of</strong> suPAR by activated human neutrophils in vivo could<br />
contribute to the recruitment <strong>of</strong> monocytes <strong>and</strong> other formyl peptide receptors-expressing cells to<br />
the sites <strong>of</strong> acute inflammation where neutrophils accumulation <strong>and</strong> activation occur.<br />
26 X I t h I n t e r n a t i o n a l W o r k s h o p o n
i015i<br />
PDGF-DD Bioavailability Is Regulated by the uPA/uPAR System:<br />
Implications for Tumor Growth<br />
Ehnman M*, Li H, Fredriksson L, Eriksson U<br />
Ludwig Institute for Cancer Research, Stockholm Branch, Karolinska Institutet, Stockholm, Sweden<br />
Presenting author e-mail: monika.ehnman@licr.ki.se<br />
Members <strong>of</strong> the Platelet-derived growth factor (PDGF) family are involved in many physiological<br />
<strong>and</strong> pathological events such as embryonic development, blood vessel maturation, fibrotic<br />
disease <strong>and</strong> cancer. In contrast to the classical PDGFs, the novel <strong>and</strong> closely related PDGF-CC<br />
<strong>and</strong> PDGF-DD are latent factors that need to be extracellularly processed before they can initiate<br />
PDGF receptor activation. We have previously identified tissue plasminogen activator (tPA) as<br />
an activator <strong>of</strong> PDGF-CC <strong>and</strong> we are now elucidating the biological relevance <strong>of</strong> the urokinase<br />
plasminogen activator (uPA) <strong>and</strong> its receptor for the proteolytic activation <strong>of</strong> PDGF-DD.<br />
Both tPA <strong>and</strong> uPA are plasminogen activators accounting for the generation <strong>of</strong> plasmin in<br />
different tissues, including blood, thereby initializing a proteolytic cascade leading to breakdown<br />
<strong>of</strong> extracellular matrix components, activation <strong>of</strong> other proteases <strong>and</strong> growth factors. The uPA/<br />
uPAR system has been extensively studied during the years <strong>and</strong> the components have been<br />
shown to play a role as prognostic markers in various cancers <strong>and</strong> in the metastatic process.<br />
Here we have elucidated the structural requirements for uPA-mediated activation <strong>of</strong> PDGF-DD.<br />
To further explore if this activation process may play a role in NIH/3T3 cell transformation <strong>and</strong><br />
subsequent tumor growth in nude mice, we generated stable NIH/3T3 cell lines expressing either<br />
activated PDGF-DD or latent PDGF-DD <strong>and</strong> compared their in vitro growth capacity <strong>and</strong> in vivo<br />
tumorigenicity. Our data suggest that regulated PDGF-DD activation is important for NIH/3T3<br />
tumor development in vivo <strong>and</strong> indicate that the uPA/uPAR system may be <strong>of</strong> importance for<br />
localized <strong>and</strong> regulated PDGF-DD activation.<br />
<strong>Molecular</strong> & <strong>Cellular</strong> <strong>Biology</strong> <strong>of</strong> <strong>Plasminogen</strong> <strong>Activation</strong> 27
i016i<br />
TGF-b1-Induced <strong>Plasminogen</strong> Activator Inhibitor-<br />
1 Expression in Vascular Smooth Muscle Cells Requires<br />
Cooperative Rho/ROCK <strong>and</strong> EGFR Signaling<br />
Higgins PJ* <strong>and</strong> Samarakoon R<br />
Center for Cell <strong>Biology</strong> & Cancer Research, Albany Medical College, Albany, New York, USA<br />
Presenting author e-mail: higginp@mail.amc.edu<br />
TGF-b1 <strong>and</strong> its target gene encoding plasminogen activator inhibitor-1 (PAI-1) are major causative<br />
factors in the pathophysiology <strong>of</strong> arteriosclerosis <strong>and</strong> perivascular fibrosis. The definition <strong>of</strong> TGFb1-activated<br />
signaling networks that impact PAI-1 transcription in vascular smooth muscle cells<br />
(VSMC) may identify novel, therapeutically-relevant, opportunities to manage PAI-1-associated<br />
cardiovascular disease. TGF-b1-induced PAI-1 expression in VSMC required cooperative EGFR/<br />
MEK-ERK <strong>and</strong> Rho/ROCK signaling. Transient transfection <strong>of</strong> a dominant negative RhoA (DN-<br />
RhoA) expression construct or pretreatment <strong>of</strong> VSMC with C3 transferase (a Rho inhibitor) <strong>and</strong><br />
Y-27632 (an inhibitor <strong>of</strong> p160ROCK, a downstream effector <strong>of</strong> Rho) dramatically attenuated the<br />
TGF-b1-initiated PAI-1 inductive response. Genetic EGFR1 deficiency or pharmacologic inhibition<br />
<strong>of</strong> EGFR activity (with AG1478) virtually ablated TGF-b1-stimulated ERK1/2 activation as well<br />
as PAI-1 expression but not SMAD2 phosphorylation. Interference with Rho/ROCK signaling,<br />
in contrast, prevented SMAD2 activation <strong>and</strong> nuclear accumulation. Infection <strong>of</strong> VSMC with<br />
an adenovirus encoding a mutant Y845F-EGFR effectively decreased TGF-b1-induced PAI-1<br />
expression implicating the pp60c-src phosphorylation site (Y845) <strong>of</strong> the EGFR in the inductive<br />
response. This is consistent with previous findings that pp60c-src is activated by TGF-b1 in<br />
VSMC <strong>and</strong> that dominant negative pp60c-src (DN-Src) expression vectors significantly block<br />
TGF-b1 induced PAI-1 expression. SMAD2 activation, moreover, is not sufficient to induce PAI-<br />
1 expression by TGF-b1 in the absence <strong>of</strong> EGFR signaling both in VSMC <strong>and</strong> mouse embryonic<br />
fibroblasts. Thus, two distinct but cooperative pathways involving EGFR/MEK-ERK signaling<br />
<strong>and</strong> Rho-dependent SMAD2 activation are required for TGF-b1-induced PAI-1 expression in<br />
VSMC.<br />
28 X I t h I n t e r n a t i o n a l W o r k s h o p o n
i017i<br />
A Novel Neuronal Death Pathway Triggered by<br />
Excess Tissue <strong>Plasminogen</strong> Activator<br />
Li J* 1 , Snyder EY 2 , Sidman RL 1<br />
1Department <strong>of</strong> Neurology, Beth Israel Deaconess Medical Center, Harvard Medical School, Boston,<br />
Massachusetts, USA;<br />
2 Stem Cell <strong>and</strong> Regeneration Program, The Burnham Institute for Medical Research, La Jolla, California,<br />
USA<br />
Presenting author e-mail: jli7@caregroup.harvard.edu<br />
We have explored molecular features <strong>of</strong> the cell death pathway in nervous (nr) mutant mice<br />
that show mitochondrial abnormalities <strong>and</strong> dendritic growth retardation in cerebellar Purkinje<br />
neurons (PNs) in postnatal weeks 2-3, <strong>and</strong> massive PN degeneration <strong>and</strong> motor incoordination<br />
thereafter. We found a mutation-induced dramatic 10-fold excess <strong>of</strong> tissue plasminogen activator<br />
(tPA) in nr cerebellum, affecting two types <strong>of</strong> downstream targets: voltage-dependent anion<br />
channels (VDACs) <strong>and</strong> neurotrophins. VDACs affect synaptic communication <strong>and</strong> apoptotic<br />
cell death, as well as mitochondrial metabolite fluxes. The tPA/plasmin system contains five<br />
‘’kringle’’ binding segments, <strong>of</strong> which kringle 5 can specifically bind brain mitochondrial VDACs<br />
to induce partial closure <strong>of</strong> these channels <strong>and</strong> interfere with mitochondria-related regulation <strong>of</strong><br />
intracellular calcium <strong>and</strong> pH. Neurotrophins participate in regulation <strong>of</strong> neuronal morphogenesis<br />
<strong>and</strong> maintenance. Degradation <strong>of</strong> particular neurotrophins by tPA/plasmin may account for<br />
tPA-mediated decreases in synaptic organization <strong>and</strong> neuronal survival. We have established<br />
that neural stem cells (NSCs) transplanted into neonatal nr cerebellum rescued PNs from cell<br />
death weeks later by restoring molecular homeostasis <strong>of</strong> tPA <strong>and</strong> its downstream targets. Two<br />
weeks after NSC injection, <strong>and</strong> a week before onset <strong>of</strong> PN degeneration, correction <strong>of</strong> tPA was<br />
accompanied by 1) normal amount <strong>and</strong> distribution <strong>of</strong> VDACs <strong>and</strong> normal mitochondrial shape,<br />
<strong>and</strong> 2) neurotrophin normalcy <strong>and</strong> PN dendritic growth. Likewise, NSCs contacting cerebellar<br />
slices in vitro rectified tPA levels <strong>and</strong> rescued host PNs, as did pharmacological decrease <strong>of</strong> tPA to<br />
normal but not subnormal levels. Neurotoxic action <strong>of</strong> tPA is open to further study in this system.<br />
<strong>Molecular</strong> & <strong>Cellular</strong> <strong>Biology</strong> <strong>of</strong> <strong>Plasminogen</strong> <strong>Activation</strong> 29
i018i<br />
The Inhibitor <strong>of</strong> Serine Proteases Protease Nexin-1 <strong>and</strong> its Receptor<br />
LRP Modulate SHH Signalling during Cerebellar Development<br />
Vaillant C 1 , Michos O 2 , Orolicki S 1 , Brellier F 1 , Taieb S 1 , Moreno E 1 , Té H 1 , Zeller R 2 , Monard D* 1<br />
1 Friedrich Miescher Institute for Biomedical Research, Basel, Switzerl<strong>and</strong>;<br />
2 Developmental Genetics, DKBW Center for Biomedicine, University <strong>of</strong> Basel Medical School, Basel,<br />
Switzerl<strong>and</strong><br />
Presenting author e-mail: denis.monard@fmi.ch<br />
Development <strong>of</strong> the postnatal cerebellum relies on tight regulation <strong>of</strong> the cell number by<br />
morphogens that control the balance between cell proliferation, survival <strong>and</strong> differentiation. Here<br />
we analyze the role <strong>of</strong> the serine protease inhibitor Protease Nexin-1 (PN-1) in the proliferation<br />
<strong>and</strong> differentiation <strong>of</strong> Cerebellar Granular Neuron Precursors (CGNPs) via modulation <strong>of</strong> their<br />
main mitogenic factor, Sonic Hedgehog (SHH). Our studies show that PN-1 interacts with the<br />
Low-density lipoprotein receptor-Related Proteins (LRPs) to antagonize SHH-induced CGNP<br />
proliferation <strong>and</strong> inhibits the activity <strong>of</strong> the SHH transcriptional target Gli1. The binding <strong>of</strong><br />
PN-1 to LRPs interferes with SHH-induced Cyclin D1 expression. CGNPs isolated from PN-<br />
1 deficient mice exhibit enhanced basal proliferation rates due to over-activation <strong>of</strong> the SHH<br />
pathway <strong>and</strong> show higher sensitivity to exogenous SHH. In vivo, the PN-1 deficiency alters the<br />
expression <strong>of</strong> SHH target genes. In addition, the onset <strong>of</strong> CGNP differentiation is delayed, which<br />
results in an enlarged outer External Granular Layer. Furthermore, the PN-1 deficiency leads<br />
to an overproduction <strong>of</strong> CGNPs <strong>and</strong> enlargement <strong>of</strong> the Internal Granular Layer in a subset <strong>of</strong><br />
cerebellar lobes during late development <strong>and</strong> adulthood. We propose that PN-1 contributes to<br />
shaping <strong>of</strong> the cerebellum by promoting cell cycle exit.<br />
30 X I t h I n t e r n a t i o n a l W o r k s h o p o n
i019i<br />
Fibrin Deposition Accelerates Neurovascular Damage <strong>and</strong><br />
Neuroinflammation in Mouse Models <strong>of</strong> Alzheimer’s Disease<br />
Paul J* <strong>and</strong> Strickl<strong>and</strong> S<br />
Laboratory <strong>of</strong> Neurobiology <strong>and</strong> Genetics, The Rockefeller University, New York, New York, USA<br />
Presenting author e-mail: jpaul@rockefeller.edu<br />
Cerebrovascular dysfunction contributes to the pathology <strong>and</strong> progression <strong>of</strong> Alzheimer’s disease<br />
(AD) but the mechanisms are not completely understood. Using transgenic mouse models <strong>of</strong><br />
Alzheimer’s disease (TgCRND8 <strong>and</strong> Tg2576), we evaluated blood-brain barrier damage <strong>and</strong><br />
the role <strong>of</strong> fibrin <strong>and</strong> fibrinolysis in the progression <strong>of</strong> b-amyloid pathology. These mouse<br />
models showed age-dependent fibrin deposition coincident with areas <strong>of</strong> blood-brain barrier<br />
permeability as demonstrated by Evans blue extravasation. Three lines <strong>of</strong> evidence suggest that<br />
fibrin contributes to the pathology: 1, AD mice with only one functional plasminogen gene <strong>and</strong><br />
therefore with reduced fibrinolysis have increased neurovascular damage relative to AD mice;<br />
2 Conversely, AD mice with only one functional fibrinogen gene have decreased blood-brain<br />
barrier damage; 3, Treatment <strong>of</strong> AD mice with the plasmin inhibitor tranexamic acid aggravated<br />
pathology, while removal <strong>of</strong> fibrinogen from the circulation <strong>of</strong> AD mice with ancrod treatment<br />
attenuated measures <strong>of</strong> neuroinflammation <strong>and</strong> vascular pathology. These results suggest fibrin<br />
is a mediator <strong>of</strong> inflammation <strong>and</strong> may impede the reparative process for neurovascular damage<br />
in AD. Fibrin <strong>and</strong> the mechanisms involved in its accumulation <strong>and</strong> clearance may present novel<br />
therapeutic targets in slowing the progression <strong>of</strong> Alzheimer’s disease.<br />
<strong>Molecular</strong> & <strong>Cellular</strong> <strong>Biology</strong> <strong>of</strong> <strong>Plasminogen</strong> <strong>Activation</strong> 31
i020i<br />
Anxiety-like Behavior <strong>and</strong> Impaired Fear Extinction in Mice with<br />
Altered Control <strong>of</strong> Extracellular Brain Proteolytic Activity<br />
Meins M*, Herry C, Moreno E, Fischer C, Lüthi A, Monard D<br />
Friedrich Miescher Institute for Biomedical Research, Basel, Switzerl<strong>and</strong><br />
Presenting author e-mail: mmeins@fmi.ch<br />
Regulation <strong>of</strong> serine proteases has been implicated in modulating synaptic plasticity. Protease<br />
nexin-1 (PN-1), an endogenous serine protease inhibitor, is expressed in specific neuronal<br />
subpopulations in the adult central nervous system. The in vivo expression <strong>of</strong> PN-1 is regulated<br />
by neuronal activity. In mice lacking PN-1 (PN-1 –/–), the brain homogenate proteolytic pr<strong>of</strong>ile<br />
is altered <strong>and</strong> NMDA receptor-mediated transmission is reduced. To examine the in vivo<br />
consequences <strong>of</strong> these changes, we compared cognitive <strong>and</strong> emotional responses <strong>of</strong> PN-1 –/– mice<br />
to their wildtype littermates. No memory impairments were detected. In contrast, PN-1 –/– mice<br />
displayed enhanced anxiety-like <strong>and</strong> avoidance behavior. Differences between wildtype <strong>and</strong><br />
PN-1 –/– littermates were also detected in cued fear conditioning. Reduced extinction <strong>of</strong> freezing<br />
behavior was detected in the PN-1 –/– mice. This was reflected at the cellular level by decreased<br />
immunoreactivity <strong>of</strong> c-FOS, an indicator <strong>of</strong> neuronal activity, in the PN-1 –/– basolateral<br />
amygdala. Surprisingly, increased immunoreactivity was detected in the same area in the PN-1<br />
–/– mice which underwent fear conditioning without extinction training. This may suggest that<br />
the increased reaction displayed by PN-1 –/– mice to some stressful situations may be the result<br />
<strong>of</strong> increased neuronal activation <strong>of</strong> the relevant neurons. The increased anxiety-like behavior <strong>and</strong><br />
the reduced fear extinction in the PN-1 –/– mice could be explained by an impaired modulation<br />
<strong>of</strong> NDMA receptor mediated activity in some regions <strong>of</strong> the amygdala. To investigate this<br />
hypothesis, we are analyzing downstream effectors <strong>of</strong> NMDA receptor activation in these areas.<br />
These results not only corroborate findings supporting the importance <strong>of</strong> the control <strong>of</strong> proteolytic<br />
activity in synaptic plasticity but they also suggest the PN-1 –/– mice as an interesting model to<br />
study the brain structures <strong>and</strong> the molecular mechanisms involved in fear extinction.<br />
32 X I t h I n t e r n a t i o n a l W o r k s h o p o n
i021i<br />
Tissue <strong>Plasminogen</strong> Activator Is Co-Packaged <strong>and</strong><br />
Co-Transported to Synaptic Sites with a Key<br />
Neuromodulator Associated with Synaptic Plasticity<br />
Lochner JE* 1 , Spangler E 1 , Schuttner LC 1 , Scalettar BA 2<br />
1 Biochemistry & <strong>Molecular</strong> <strong>Biology</strong>, 2 Physics, Lewis & Clark College, Portl<strong>and</strong>, Oregon, USA<br />
Presenting author e-mail: lochner@lclark.edu<br />
Tissue plasminogen activator (tPA) is highly expressed in the hippocampus <strong>and</strong> is implicated<br />
in modifying synaptic efficacy during learning <strong>and</strong> memory. tPA is postulated to exert its<br />
influence on synaptic plasticity by initiating an extracellular proteolytic cascade that promotes the<br />
conversion <strong>of</strong> precursor brain-derived neurotrophic factor (proBDNF) to mature BDNF (mBDNF)<br />
extracellularly, at synapses. mBDNF is a potent neuromodulator that is known to augment<br />
synapse density <strong>and</strong> elicit long-lasting enhancement <strong>of</strong> synaptic transmission. Motivated by<br />
recent interest in possible interactions between tPA <strong>and</strong> proBDNF, we have developed a system<br />
that facilitates study <strong>of</strong> the packaging, transport, <strong>and</strong> secretion <strong>of</strong> these two neuromodulatory<br />
proteins in cultured hippocampal neurons. We find 89% colocalization <strong>of</strong> tPA <strong>and</strong> proBDNF<br />
chimeras within dense-core granules (DCGs) <strong>of</strong> mature hippocampal neurons, indicating efficient<br />
co-packaging <strong>of</strong> these neuromodulators. Additionally, we find that these two neuromodulators<br />
undergo rapid co-transport (at speeds <strong>of</strong> ~1 µm/s) along neuronal processes, suggesting that tPA<br />
<strong>and</strong> pro-BDNF are co-delivered to synaptic sites in DCGs. Evaluation <strong>of</strong> the colocalization <strong>of</strong> these<br />
two neuromodulators at the organelle level in post-synaptic dendritic spines reveals that tPA<br />
<strong>and</strong> proBDNF chimeras colocalize in individual DCGs in 27% <strong>of</strong> spines, <strong>and</strong> that 80% <strong>of</strong> spines<br />
which contain DCGs contain both chimeras in the same DCG. Our results suggest that efficient<br />
co-packaging <strong>and</strong> co-transport produces a pool <strong>of</strong> DCGs containing both tPA <strong>and</strong> proBDNF at<br />
post-synaptic sites, where these neuromodulators can undergo activity-dependent co-release from<br />
DCGs <strong>and</strong> then interact <strong>and</strong>/or mediate changes that influence learning <strong>and</strong> memory.<br />
<strong>Molecular</strong> & <strong>Cellular</strong> <strong>Biology</strong> <strong>of</strong> <strong>Plasminogen</strong> <strong>Activation</strong> 33
i022i<br />
Tissue <strong>Plasminogen</strong> Activator Modulates <strong>Cellular</strong><br />
<strong>and</strong> Behavioral Response to Cocaine<br />
Maiya R* 1 , Zhou Y 2 , Norris EH 1 , Kreek MJ 2 , Strickl<strong>and</strong> S 1<br />
1 2 Laboratory <strong>of</strong> Neurobiology <strong>and</strong> Genetics, Laboratory <strong>of</strong> the <strong>Biology</strong> <strong>of</strong> Addictive Diseases, The<br />
Rockefeller University, New York, New York, USA<br />
*Presenting author e-mail: rmaiya@mail.rockefeller.edu<br />
Cocaine exposure induces long lasting molecular <strong>and</strong> cellular adaptations in the brain. Tissue<br />
plasminogen activator (tPA), an extracellular protease implicated in regulating neuronal plasticity,<br />
may orchestrate some <strong>of</strong> these cocaine-induced neuro-adaptations. In this study, the effects<br />
<strong>of</strong> acute <strong>and</strong> chronic cocaine administration on tPA activity in the brain were examined. Mice<br />
were injected with cocaine in the acute (3 injections <strong>of</strong> 15 mg/kg) or chronic (3x15mg/kg for 14<br />
days) ‘’binge’’ paradigm. In situ <strong>and</strong> in-gel zymography revealed that in the amygdala <strong>of</strong> WT<br />
animals, acute cocaine exposure increased tPA activity whereas chronic cocaine administration<br />
decreased tPA activity. Acute cocaine also elevated levels <strong>of</strong> plasma corticosterone, corticotropin<br />
releasing factor (CRF), <strong>and</strong> CRF receptor 1 (CRF-R1) mRNAs in the amygdala <strong>of</strong> both WT <strong>and</strong><br />
tPA–/– animals. Phosphorylation <strong>of</strong> extracellular signal regulated kinase 1/2 (ERK1/2), a marker<br />
for post-synaptic plasticity events, was observed in the amygdala <strong>of</strong> WT but not tPA–/– mice<br />
after acute cocaine exposure. In comparison to WT animals, tPA–/– animals showed attenuated<br />
c-fos expression in the amygdala after acute cocaine administration. These results suggest altered<br />
cocaine-induced neuro-adaptation in the amygdala <strong>of</strong> tPA–/– mice. Cocaine-induced anxiety<br />
was also examined in both WT <strong>and</strong> tPA–/– animals using the elevated plus maze. In contrast to<br />
WT animals, tPA–/– animals were resistant to the anxiogenic effects <strong>of</strong> acute cocaine. After acute<br />
cocaine, tPA–/– mice displayed increased total arm entries in comparison to WT mice, suggesting<br />
enhanced cocaine-induced locomotor stimulation. In summary, these results suggest a significant<br />
role for tPA in the modulation <strong>of</strong> cocaine-induced behaviors <strong>and</strong> neuronal plasticity.<br />
34 X I t h I n t e r n a t i o n a l W o r k s h o p o n
i023i<br />
Characterisation <strong>of</strong> the Pathway <strong>of</strong> Polymerisation<br />
<strong>of</strong> Wildtype Neuroserpin <strong>and</strong> the Ser49Pro Mutant<br />
that Underlies the Dementia FENIB<br />
Hägglöf P*, Belorgey D, Karlsson-Li S, Sharp LK, Lomas DA<br />
Department <strong>of</strong> Medicine, University <strong>of</strong> Cambridge, Cambridge Institute for Medical Research,<br />
Cambridge, United Kingdom<br />
Presenting author e-mail: pmh43@cam.ac.uk<br />
Neuroserpin is expressed during the late stage <strong>of</strong> development in neurons <strong>of</strong> the central <strong>and</strong><br />
peripheral nervous system <strong>and</strong> in the adult brain. The target proteinase <strong>of</strong> neuroserpin is tissue<br />
plasminogen activator (tPA) <strong>and</strong> it is likely to be important in the control <strong>of</strong> synaptic plasticity,<br />
in learning, memory <strong>and</strong> can act as a neuroprotectant. It can decrease the toxicity <strong>of</strong> the Ab1-<br />
42 peptide that is central to the pathogenesis <strong>of</strong> Alzheimer’s disease. Point mutations in the<br />
neuroserpin gene underlie the autosomal dominant dementia, familial encephalopathy with<br />
neuroserpin inclusion bodies, (FENIB). This is characterised by the retention <strong>of</strong> ordered polymers<br />
<strong>of</strong> neuroserpin within the endoplasmic reticulum <strong>of</strong> neurons. We have previously shown that<br />
polymers result from the sequential linkage between the reactive centre loop <strong>of</strong> one neuroserpin<br />
molecule <strong>and</strong> b-sheet A <strong>of</strong> another. We show here that the polymerisation <strong>of</strong> both wildtype <strong>and</strong><br />
the Ser49Pro mutant <strong>of</strong> neuroserpin that causes FENIB is dependent <strong>of</strong> pH demonstrating that<br />
the His-338 residue in the shutter region is important for in the opening <strong>of</strong> b-sheet A. Tryptophan,<br />
extrinsic fluorescence <strong>and</strong> fluorphore labelled cysteine mutants suggest that the RCL may be<br />
preinserted in b-sheet A <strong>and</strong> then expelled during in an at least two steps in the formation <strong>of</strong><br />
polymers: a fast unimolecular process that is likely to reflect opening <strong>of</strong> b-sheet A followed by<br />
the slower process <strong>of</strong> polymer formation. Taken together these data suggest a two-step kinetic<br />
mechanism for the formation <strong>of</strong> the polymers <strong>of</strong> neuroserpin that underlie the dementia FENIB.<br />
<strong>Molecular</strong> & <strong>Cellular</strong> <strong>Biology</strong> <strong>of</strong> <strong>Plasminogen</strong> <strong>Activation</strong> 35
i024i<br />
Matriptase Is an Essential Inhibitory Target for<br />
Hepatocyte Growth Factor Activator Inhibitor-1 during<br />
both Embryonic Development <strong>and</strong> Postnatal Life<br />
Szabo R*, Molinolo A, List K, Bugge TH<br />
Oral <strong>and</strong> Pharyngeal Cancer Branch, NIDCR, NIH, Bethesda, Maryl<strong>and</strong>, USA<br />
Presenting author e-mail: rszabo@nidcr.nih.gov<br />
Hepatocyte growth factor activator inhibitor-1 (HAI-1) is a Kunitz-type transmembrane serine<br />
protease inhibitor proposed to inhibit the activity <strong>of</strong> several trypsin-like serine proteases,<br />
including hepsin, hepatocyte growth factor activator, prostasin (CAP1/PRSS8), <strong>and</strong> matriptase.<br />
Here we generated HAI-1-deficient mice to determine the biological function <strong>of</strong> HAI-1 <strong>and</strong><br />
identify physiological HAI-1 inhibitory targets during development <strong>and</strong> postnatal life. HAI-<br />
1-deficient mice died at mid-gestation due to placental insufficiency caused by a disruption <strong>of</strong><br />
the epithelial integrity <strong>of</strong> placental chorionic trophoblasts associated with chorionic basement<br />
membrane dissolution, loss <strong>of</strong> E-cadherin, <strong>and</strong> loss <strong>of</strong> membrane-associated b-catenin.<br />
Interestingly, however, matriptase gene ablation in HAI-1-deficient embryos restored the integrity<br />
<strong>of</strong> chorionic trophoblasts <strong>and</strong> enabled both normal placentation <strong>and</strong> development to term. HAI-<br />
1 was recently reported to also be required for mouse postnatal survival beyond two weeks. To<br />
determine the inhibitory targets for HAI-1 during postnatal life, we generated HAI-1 null mice<br />
in a matriptase hypomorphic background, which display 82 - >99 % reduction in matriptase<br />
mRNA levels in epithelial tissues. Low matriptase levels enabled both embryonic development<br />
<strong>and</strong> normal postnatal survival <strong>of</strong> HAI-1-deficient mice when followed for up to six months. Taken<br />
together, this study identifies matriptase as an essential inhibitory target for HAI-1 during both<br />
embryonic development <strong>and</strong> postnatal life.<br />
36 X I t h I n t e r n a t i o n a l W o r k s h o p o n
i025i<br />
Mice with very low Matriptase Are Viable <strong>and</strong> Phenocopy<br />
Human Autosomal Ichthyosis with Hypotrichosis Syndrome<br />
List K* 1 , Currie B 1 , Scharschmidt T 2 , Szabo R 1 , Molinolo A 1 , Shireman J 1 , Segre J 2 , Bugge TH 1<br />
1 Oral <strong>and</strong> Pharyngeal Cancer Branch, NIDCR, NIH, Bethesda, Maryl<strong>and</strong>, USA;<br />
2 National Human Genome Research Institute, NIH, Bethesda, Maryl<strong>and</strong>, USA<br />
Presenting author e-mail: klist@nidcr.nih.gov<br />
Complete deficiency <strong>of</strong> the type II transmembrane serine protease matriptase or its c<strong>and</strong>idate<br />
downstream target, the GPI-anchored serine protease prostasin, causes epidermal barrier<br />
disruption <strong>and</strong> neonatal death <strong>of</strong> mice. Here we report the surprising observation that mice with a<br />
one-hundred-fold reduction in epidermal matriptase mRNA levels, generated by inserting a leaky<br />
splice acceptor site into intron 1 <strong>of</strong> the matriptase gene, are viable <strong>and</strong> fertile. Interestingly, these<br />
matriptase hypomorphic mice display skin <strong>and</strong> hair defects that are identical to those <strong>of</strong> humans<br />
with Autosomal Recessive Ichthyosis with Hypotrichosis (ARIH): an inherited disorder recently<br />
linked to homozygosity for a G827R substitution in the matriptase serine protease domain. Thus,<br />
matriptase hypomorphic mice developed marked hyperkeratosis with impaired desquamation<br />
<strong>and</strong> focal dermal inflammation, as well as hypotrichosis with brittle, thin, uneven, <strong>and</strong> sparse<br />
hair. Proteomic analysis <strong>of</strong> matriptase hypomorphic epidermis revealed markedly reduced<br />
prostasin activation <strong>and</strong> pr<strong>of</strong>ilaggrin proteolytic processing. This work strongly supports reduced<br />
matriptase activity as one etiological origin <strong>of</strong> human ARIH <strong>and</strong> provides a mouse model for the<br />
exploration <strong>of</strong> matriptase in other physiological <strong>and</strong> pathological processes, including epithelial<br />
carcinogenesis.<br />
<strong>Molecular</strong> & <strong>Cellular</strong> <strong>Biology</strong> <strong>of</strong> <strong>Plasminogen</strong> <strong>Activation</strong> 37
i026i<br />
Role <strong>of</strong> Urokinase-Receptor in Hematopoietic Stem Cell Trafficking<br />
Montuori N 1 , Selleri C 2 , Ricci P 2 , Visconte V 1 , Carriero MV 3 , Rotoli B 2 , Rossi G 1 , Ragno P* 4<br />
1 Department <strong>of</strong> <strong>Cellular</strong> <strong>and</strong> <strong>Molecular</strong> <strong>Biology</strong> <strong>and</strong> Pathology, 2 Department <strong>of</strong> Biochemistry <strong>and</strong><br />
Medical Biotechnology, ‘’Federico II’’ University, Naples, Italy;<br />
3 Department <strong>of</strong> Experimental Oncology, National Cancer Institute, Naples, Italy;<br />
4 Department <strong>of</strong> Chemistry, University <strong>of</strong> Salerno, Salerno, Italy<br />
Presenting author e-mail: pragno@unisa.it<br />
Cleaved forms <strong>of</strong> soluble urokinase-receptor (c-suPAR) have been detected in body fluids from<br />
patients affected by various tumors. We reported increased c-suPAR levels in sera <strong>of</strong> healthy<br />
donors during granulocyte colony-stimulating factor (G-CSF)-induced mobilization <strong>of</strong> CD34+<br />
hematopoietic stem cells (HSCs). In vitro, c-suPAR or its derived chemotactic peptide (uPAR84-<br />
95) stimulated migration <strong>of</strong> human CD34+ HSCs <strong>and</strong> inactivated CXCR4, the chemokine receptor<br />
primarily responsible for HSC retention in bone marrow (BM). These results suggested that<br />
c-suPAR could potentially contribute to regulate HSC trafficking from <strong>and</strong> to BM. Therefore, we<br />
investigated uPAR84-95 effects on mobilization <strong>of</strong> mouse CD34+ hematopoietic stem/progenitor<br />
cells (HSCs/HPCs). We first demonstrated that uPAR84-95 stimulated in vitro dose-dependent<br />
migration <strong>of</strong> mouse CD34+ M1 leukemia cells <strong>and</strong> inactivated murine CXCR4. uPAR84-95<br />
capability to induce mouse HSC/HPC release from bone marrow <strong>and</strong> migration into the<br />
circulation was then investigated in vivo. uPAR84-95 intraperitoneal administration induced rapid<br />
leukocytosis, which was associated with an increase in peripheral blood CD34+ HSCs/HPCs. In<br />
vitro colony assays confirmed that uPAR84-95 mobilized hematopoietic progenitors, showing an<br />
increase in circulating colony-forming cells.<br />
We are now studying suPAR <strong>and</strong> c-suPAR effects on HSCs, to investigate their role in HSC<br />
retention in BM, <strong>and</strong>, therefore, their potential contribution also to the homing <strong>and</strong> the<br />
engraftment <strong>of</strong> HSCs to the BM. In vitro effects <strong>of</strong> anti-uPAR antibodies <strong>and</strong> <strong>of</strong> suPAR <strong>and</strong> csuPAR<br />
on adhesion <strong>and</strong> proliferation <strong>of</strong> human G-CSF-mobilized <strong>and</strong> BM HSCs have been<br />
examined in long-term cultures (LTC), which represent the best surrogate in vitro <strong>of</strong> BM<br />
hematopoiesis.<br />
38 X I t h I n t e r n a t i o n a l W o r k s h o p o n
i027i<br />
<strong>Plasminogen</strong> Activator Inhibitor-1, PAI-1, Regulates<br />
the Akt Survival Pathway<br />
Rømer MU, Larsen L, Offenberg H, Brünner N, Lademann U*<br />
Department <strong>of</strong> Veterinary Pathobiology, Faculty <strong>of</strong> Life Science, University <strong>of</strong> Copenhagen, Frederiksberg,<br />
Denmark<br />
Presenting auther e-mail: ul@life.ku.dk<br />
<strong>Plasminogen</strong> Activator Inhibitor-1, PAI-1, inhibits the activation <strong>of</strong> the plasminogen activation<br />
system, which is involved in cancer growth <strong>and</strong> dissemination. Increased tumor tissue levels <strong>of</strong><br />
PAI-1 would therefore be expected to inhibit cancer cell progression. However, PAI-1 is elevated<br />
in many solid tumors <strong>and</strong> this elevation has consistently been shown to be associated with shorter<br />
patient survival. The reason for this has remained unclear.<br />
The phosphatidylinositol-3 kinase (PI3K)/Akt pathway is overactivated in a wide range <strong>of</strong> tumor<br />
types, <strong>and</strong> this triggers a cascade <strong>of</strong> responses, including inhibition <strong>of</strong> apoptosis. PAI-1 has been<br />
reported to modulate the PI3 kinase /Akt pathway, thus it is possible that PAI-1 inhibits apoptosis<br />
<strong>of</strong> tumor cells via activation <strong>of</strong> this pathway.<br />
We have previously shown that PAI-1–/– fibrosarcoma cells are significantly more sensitive than<br />
wild-type fibrosarcoma cells to etoposide-induced apoptosis. To further study the signalling<br />
pathways involved in the anti-apoptotic function <strong>of</strong> PAI-1 we asked the question whether Akt<br />
activation is involved in PAI-1 mediated inhibition <strong>of</strong> apoptosis. We demonstrate that Akt is<br />
hyperfosforylated in wild type fibrosarcoma cells (endogenous PAI-1 expression) compared<br />
with PAI-1–/– fibrosarcoma cells. This hyperphosphorylation is accompanied by increased<br />
phosphorylation <strong>of</strong> downstream targets <strong>of</strong> Akt. When wild type fibrosarcoma cells were treated<br />
with a specific inhibitor against Akt1/2 (Akt inhibitor VIII) <strong>and</strong> PI3K (LY294002) it induced a<br />
sensitizing effect on etoposide induced cell death, further supporting an apoptosis regulating role<br />
<strong>of</strong> the PI3K/Akt survival pathway in our cell model.<br />
Altogether, our data suggests that PAI-1 inhibits etoposide induced cell death via activation <strong>of</strong> the<br />
Akt survival pathway.<br />
<strong>Molecular</strong> & <strong>Cellular</strong> <strong>Biology</strong> <strong>of</strong> <strong>Plasminogen</strong> <strong>Activation</strong> 39
i028i<br />
A Host <strong>Plasminogen</strong> Activator Inhibitor-1 Deficiency Promotes<br />
Proliferation <strong>and</strong> Resistance to Apoptosis by <strong>Activation</strong><br />
<strong>of</strong> the PI3-K/Akt Pathway in Endothelial Cells<br />
Balsara RD* 1,2,3 , Castellino FJ 1,2,3 , Ploplis VA 1,2,3<br />
1 2 3 W. M. Keck Center for Transgene Research, Department <strong>of</strong> Chemistry <strong>and</strong> Biochemistry, Notre Dame<br />
Cancer Institute, University <strong>of</strong> Notre Dame, Indiana, USA<br />
Presenting author e-mail: rbalsara@nd.edu<br />
Angiogenic function <strong>of</strong> plasminogen activator inhibitor-1 (PAI-1) <strong>and</strong> its underlying mechanism<br />
were studied utilizing endothelial cells (EC) isolated from the aortas <strong>of</strong> wild-type (WT) <strong>and</strong> PAI-<br />
1-deficient mice. The enhanced proliferation <strong>of</strong> PAI-1–/– EC was associated with hyperactivation<br />
<strong>of</strong> Akt(P-Ser473) <strong>and</strong> accompanied by resistance to apoptosis. Disruption <strong>of</strong> VEGF/VEGFR-1<br />
interaction attenuated activation <strong>of</strong> Akt(P-Ser473) in PAI-1–/– EC. Involvement <strong>of</strong> the PI3k/Akt<br />
survival axis in both WT <strong>and</strong> PAI-1–/– EC was discerned by treating cells with the<br />
pharmacological inhibitor wortmannin, which also diminished cell proliferation. Furthermore,<br />
the higher levels <strong>of</strong> Akt(P-Ser473) in PAI-1–/– EC were regulated by higher levels <strong>of</strong> inactive<br />
phosphatase PTEN. In PAI-1–/– EC, increased levels <strong>of</strong> Akt(P-Ser473) were associated with higher<br />
levels <strong>of</strong> inactive caspase-9, which is a direct phosphorylation target <strong>of</strong> Akt. Subsequently lower<br />
protein levels <strong>and</strong> activity <strong>of</strong> pro- <strong>and</strong> active-caspase-3 were detected in PAI-1–/– EC. Treatment<br />
<strong>of</strong> PAI-1–/– EC with exogenous r-PAI-1 controlled the increased rate <strong>of</strong> cell proliferation with<br />
concomitant modulation <strong>of</strong> the components <strong>of</strong> the Akt pathway. In the presence <strong>of</strong> r-PAI-1, levels<br />
<strong>of</strong> inactive PTEN(P-Ser380) <strong>and</strong> Akt(P-Ser473) were decreased, <strong>and</strong> the levels <strong>of</strong> pro- <strong>and</strong> activecaspase-3<br />
were increased. A r-PAI-1 mutant that had compromised binding ability to low density<br />
lipoprotein receptor-related protein (LRP) failed to alter cell proliferation <strong>of</strong> PAI-1–/– cells. These<br />
results indicate that PAI-1 mediates its anti-proliferative activity in an LRP-dependent manner.<br />
Additionally, PAI-1 plays a pivotal role in modulating the Akt pathway, which is an important<br />
participant in transducing signaling events during angiogenesis.<br />
40 X I t h I n t e r n a t i o n a l W o r k s h o p o n
i029i<br />
Bomapin Is a Redox-regulated Serpin which Stabilizes Retinoblastoma<br />
Protein during Apoptosis <strong>and</strong> Increases Proliferation <strong>of</strong> Leukemia Cells<br />
Przygodzka P, Olausson B, Tengel T, Larsson G, Wilczynska M*<br />
Department <strong>of</strong> Medical Biochemistry <strong>and</strong> Biophysics, Umeå University, Umeå, Sweden<br />
Presenting author e-mail: Malgorzata.Wilczynska@medchem.umu.se<br />
Bomapin is a hematopoietic- <strong>and</strong> leukemia-specific intracellular serine protease inhibitor.<br />
Its expression is restricted to bone marrow <strong>and</strong> to peripheral blood leukocytes <strong>of</strong> patients<br />
with myeloid leukemias. Consistent with this, bomapin is also constitutively expressed in<br />
promyelocytic <strong>and</strong> monocytic cell lines (HL60, THP1, <strong>and</strong> AML-193). Herein we show that<br />
naturally expressed bomapin is localized in the nucleus, where it is stabilized by a disulfide<br />
bond linking the only two bomapin cysteines. Computer modeling has shown that the cysteines<br />
are distant in the reduced bomapin, but can easily be disulfide-linked without distortion <strong>of</strong><br />
the overall bomapin structure. Stable, ectopic expression <strong>of</strong> wild-type bomapin in K562 cells<br />
increased cell proliferation by about 50%. Importantly, the enhancement <strong>of</strong> cell proliferation was<br />
not observed for a bomapin mutant lacking the disulfide bond. We show also that in proliferating<br />
leukemia cells, bomapin existed in a multi-protein complex including lamin-A/C, retinoblastoma<br />
(Rb) protein, beta-actin, <strong>and</strong> non-muscle myosin IIA. Bomapin expression resulted in stabilization<br />
<strong>of</strong> Rb protein during serum deprivation-induced apoptosis. We propose that bomapin is a<br />
redox-regulated serpin which enhances proliferation potential <strong>of</strong> leukemia cells via assembly<br />
into a multi-protein complex including also the Rb protein, <strong>and</strong> stabilizes Rb protein against<br />
degradation during apoptosis.<br />
<strong>Molecular</strong> & <strong>Cellular</strong> <strong>Biology</strong> <strong>of</strong> <strong>Plasminogen</strong> <strong>Activation</strong> 41
i030i<br />
Hespin as a Cell Survival Factor<br />
Qiu D, Owen K, Edwards DR, Ellis V*<br />
Biomedical Research Centre, School <strong>of</strong> Biological Sciences, University <strong>of</strong> East Anglia, Norwich, United<br />
Kingdom<br />
Presenting author e-mail: v.ellis@uea.ac.uk<br />
Hepsin is a type II transmembrane serine protease upregulated in a variety <strong>of</strong> cancers <strong>and</strong> may<br />
be functionally involved in disease progression. How hepsin might mediate these effects <strong>and</strong><br />
via which substrates is currently unknown. Our qRT-PCR data show that hepsin expression<br />
in prostate cancer tissue is positively correlated with both malignancy (p
i031i<br />
Urokinase (uPA) Protects Endothelial Cell against Apoptosis by<br />
Upregulating the X-linked Inhibitor <strong>of</strong> Apoptosis Protein (XIAP)<br />
Prager GW* 1,2 , Koschelnick Y 1 , Mihaly J 1 , Brunner P 1 , Binder BR 1<br />
1 Department <strong>of</strong> Vascular <strong>Biology</strong> <strong>and</strong> Thrombosis Research, Centre for Bio-<strong>Molecular</strong> Medicine <strong>and</strong><br />
Pharmacology, 2 Clinical Division <strong>of</strong> Oncology, Department <strong>of</strong> Medicine I <strong>and</strong> Cancer Center, Medical<br />
University Vienna, Austria<br />
Presenting author e-mail: gerald.prager@meduniwien.ac.at<br />
uPA has originally been implicated to assist the angiogenic process by it’s proteolytic properties.<br />
It is now becoming increasingly evident that uPA additionally elicits many pro-angiogenic<br />
responses like differentiation, proliferation <strong>and</strong> cell migration in a non-proteolytic fashion via<br />
induction <strong>of</strong> intracellular signal transduction.<br />
We now demonstrate that in endothelial cells uPA protects against apoptosis by transcriptional<br />
upregulation <strong>of</strong> inhibitor <strong>of</strong> apoptosis proteins (IAPs), among them most prominently the Xlinked<br />
inhibitor <strong>of</strong> apoptosis protein (XIAP). In contrast to canonical growth factors, like vascular<br />
endothelial growth factor (VEGF), uPA elicits anti-apoptosis independently <strong>of</strong> the PI3-kinase<br />
pathway. uPA-induced cell survival is dependent on the type <strong>of</strong> extracellular matrix used<br />
indicating the involvement <strong>of</strong> integrin adhesion receptors. Thereby, uPA induces phosphorylation<br />
<strong>of</strong> the CDC42 downstream effector p21-activated kinase 1 (PAK1) <strong>and</strong> phosphorylation <strong>of</strong><br />
IkappaB kinase alpha (IKKa), which itself induces NFkappaB activation. Blocking NFkappaB by<br />
the use <strong>of</strong> the specific NFkappaB inhibitor BAY 11-7082 or by adenoviral-mediated overexpression<br />
<strong>of</strong> its inhibitor IkB, inhibits uPA-induced XIAP expression as well as uPA-induced cell survival.<br />
Furthermore, silencing XIAP expression by siRNA significantly reduces cell survival efficiencies<br />
<strong>of</strong> uPA in endothelial cells.<br />
From these data we conclude that uPA, which is a main player in endothelial cell migration <strong>and</strong><br />
invasion, provides an additional, PI3-kinase independent autocrine or paracrine cell survival<br />
mechanism.<br />
<strong>Molecular</strong> & <strong>Cellular</strong> <strong>Biology</strong> <strong>of</strong> <strong>Plasminogen</strong> <strong>Activation</strong> 43
i032i<br />
Pro-fibrinolytic Effects <strong>of</strong> Metalloproteinases during Skin<br />
Wound Healing in the Absence <strong>of</strong> <strong>Plasminogen</strong><br />
Lund LR* 1 , Green KA 1 , Almholt K 1 , Ploug M 1 , Bugge TH 2 , Rømer J 1<br />
1 Finsen Laboratory, Rigshospitalet, Copenhagen Biocenter, Copenhagen, Denmark;<br />
2Proteases <strong>and</strong> Tissue Remodeling Unit, National Institute <strong>of</strong> Dental <strong>and</strong> Crani<strong>of</strong>acial Research, National<br />
Institutes <strong>of</strong> Health, Bethesda, Maryl<strong>and</strong>, USA<br />
Presenting author e-mail: lund@inet.uni2.dk<br />
Genetic ablation <strong>of</strong> plasminogen as well as pharmacological inhibition <strong>of</strong> metalloproteinase<br />
activity delays skin wound healing in mice, while the combined inhibition <strong>of</strong> these two<br />
enzyme systems completely prevents healing. In the present study the impact <strong>of</strong> plasmin <strong>and</strong><br />
metalloproteinases as pro-fibrinolytic enzymes has been investigated by comparing skin wound<br />
healing in the absence <strong>and</strong> presence <strong>of</strong> fibrin. <strong>Plasminogen</strong>-deficiency impairs skin wound<br />
healing kinetics, but this delay is only partially restored in the absence <strong>of</strong> fibrin. This suggests that<br />
plasmin-mediated fibrinolysis is the primary, but not the exclusive, requirement for healing <strong>of</strong><br />
wounds in these mice. In addition, we observe that lack <strong>of</strong> fibrin reduces plasminogen activation<br />
significantly during wound healing. The pro-fibrinolytic role <strong>of</strong> metalloproteinases is revealed<br />
by the finding that lack <strong>of</strong> fibrin partially restores the otherwise arrested healing <strong>of</strong> plasminogendeficient<br />
wounds after metalloproteinase-inhibition. In conclusion, the residual impairment<br />
<strong>of</strong> skin wound healing in the absence <strong>of</strong> fibrin suggests the existence <strong>of</strong> a fibrin-independent<br />
substrate(s) for plasmin <strong>and</strong> metalloproteinases. Furthermore, these in vivo data reveal that<br />
galardin-sensitive metalloproteinases mediate compensatory fibrinolysis to facilitate wound<br />
healing in the absence <strong>of</strong> plasmin.<br />
44 X I t h I n t e r n a t i o n a l W o r k s h o p o n
i033i<br />
Complementary Roles <strong>of</strong> Intracellular <strong>and</strong> Pericellular Collagen<br />
Degradation Pathways in Mesenchymal Cell Survival <strong>and</strong> Proliferation<br />
Wagenaar-Miller RA 1 , Engelholm LH 2 , Gavard J 1 , Yamada S 3 , Gutkind JS 1 , Behrendt N 2 , Holmbeck K 3 ,<br />
Bugge TH* 1<br />
1 Oral <strong>and</strong> Pharyngeal Cancer Branch, NIDCR, NIH, Bethesda, Maryl<strong>and</strong>, USA;<br />
2 Finsen Laboratory, Copenhagen, Denmark;<br />
3 Skeletal Morphogenesis Branch, NIDCR, NIH, Bethesda, Maryl<strong>and</strong>, USA<br />
Presenting author e-mail: thomas.bugge@nih.gov<br />
Mesenchymal cells must be capable <strong>of</strong> proteolytically remodeling their collagen-rich pericellular<br />
environments to survive, proliferate, <strong>and</strong> properly differentiate. Two key turnover pathways<br />
have been described for collagen: intracellular cathepsin-mediated degradation <strong>and</strong> pericellular<br />
collagenase-mediated degradation. Here we show that intracellular <strong>and</strong> pericellular collagen<br />
turnover pathways have complementary functions in collagen remodeling. Combined, but<br />
not individual, deficits in intracellular collagen degradation (uPARAP/Endo180 ablation) <strong>and</strong><br />
pericellular collagen degradation (MT1-MMP ablation) caused proliferative failure <strong>and</strong> poor<br />
survival <strong>of</strong> osteoblasts <strong>and</strong> chondrocytes within their respective collagen type I- <strong>and</strong> collagen<br />
type II-rich osteogenic <strong>and</strong> chondrogenic niches. This severely impaired overall bone formation,<br />
leading to uniform postnatal death <strong>of</strong> combined uPARAP/Endo180;MT1-MMP-deficient<br />
mice. These findings have important implications for the use <strong>of</strong> pharmacological inhibitors <strong>of</strong><br />
collagenase activity aimed at preventing connective tissue destruction in a variety <strong>of</strong> diseases.<br />
<strong>Molecular</strong> & <strong>Cellular</strong> <strong>Biology</strong> <strong>of</strong> <strong>Plasminogen</strong> <strong>Activation</strong> 45
i034i<br />
Interplay between MMPs <strong>and</strong> the Endocytic Collagen<br />
Receptor, uPARAP/Endo180, in Collagen Degradation<br />
Behrendt N* 1 , Madsen DH 1 , Ingvarsen S 1 , Hillig T 1 , Wagenaar-Miller R 2 , Kjøller L 1 , Gårdsvoll H 1 ,<br />
Høyer-Hansen G 1 , Bugge TH 2 , Engelholm LH 1<br />
1 The Finsen Laboratory, Rigshospitalet, Copenhagen, Denmark;<br />
2Oral & Pharyngeal Cancer Branch, National Institute <strong>of</strong> Dental <strong>and</strong> Crani<strong>of</strong>acial Research, NIH,<br />
Bethesda, Maryl<strong>and</strong>, USA<br />
Presenting author e-mail: niels.behrendt@finsenlab.dk<br />
The uPAR-associated protein (uPARAP/Endo180) is an endocytic cell surface receptor on<br />
mesenchymal cells that is centrally engaged in the turnover <strong>of</strong> collagens <strong>of</strong> several subtypes. It<br />
has recently become clear that uPARAP/Endo180-mediated collagen degradation takes place<br />
both during bone development <strong>and</strong> in the invasive growth <strong>of</strong> malignant tumors. In this work, we<br />
have focused on the interplay between this new mechanism <strong>and</strong> the more extensively studied,<br />
extracellular routes <strong>of</strong> collagenolysis. In collagen internalization assays, collagen that has been<br />
pre-cleaved by a mammalian collagenase is taken up much more efficiently than intact, native<br />
collagen by uPARAP/Endo180 positive cells. This preference is governed by the acquisition <strong>of</strong><br />
a gelatin like structure <strong>of</strong> collagen, occurring upon collagenase mediated cleavage under native<br />
conditions. Furthermore, the growth <strong>of</strong> uPARAP/Endo180 deficient fibroblasts on a native<br />
collagen matrix leads to a dramatic accumulation <strong>of</strong> large collagen fragments in the culture<br />
supernatant. In contrast, wildtype fibroblasts possess the ability to direct a complete collagen<br />
breakdown sequence, including both initial, extracellular cleavage, endocytic (uPARAP/Endo180<br />
mediated) uptake <strong>of</strong> large, defined fragments <strong>and</strong> a final, intracellular degradation step. Thus,<br />
our work shows that extracellular collagenolysis <strong>and</strong> endocytic collagen turnover can occur as<br />
an integrated mechanism in cultured fibroblasts <strong>and</strong> fibroblast-like cells. Most likely, a similar<br />
mechanism is operative in the stromal cell types that are responsible for collagenolysis during<br />
tumor invasion.<br />
46 X I t h I n t e r n a t i o n a l W o r k s h o p o n
i035i<br />
The Urokinase Receptor Ko Mice Have Reduced Keratinocytes<br />
Proliferation <strong>and</strong> Migration during Wound Healing <strong>and</strong><br />
Are Protected in a Skin Carcinogenesis Protocol<br />
D’Alessio S, Mazzieri R, Gerasi L, Blasi F*<br />
H. San Raffaele <strong>and</strong> IFOM (FIRC Institute <strong>of</strong> <strong>Molecular</strong> Oncology), Milan, Italy<br />
Presenting author e-mail: Blasi.Francesco@hsr.it<br />
We have found that the urokinase receptor (uPAR) is implicated in multistage mouse skin<br />
carcinogenesis, since uPAR Ko mice show a reduced susceptibility to tumor formation after a<br />
DMBA-TPA protocol, compared to wt-mice. The uPAR Ko mice have 70% less <strong>and</strong> much smaller<br />
papillomas. However, the rate <strong>of</strong> conversion <strong>of</strong> papillomas to carcinomas, is not different between<br />
wt <strong>and</strong> Ko mice, indicating that the role <strong>of</strong> uPAR is in the first stage <strong>of</strong> tumorigenesis. We also<br />
have noticed that uPAR is also involved in the regulation <strong>of</strong> wound healing, as uPAR Ko mice<br />
display a slight delay in wound closure compared to wt-skin. In order to directly underst<strong>and</strong><br />
the role <strong>of</strong> endogenous uPAR in these two in vivo events, we examined uPAR null-<strong>and</strong> wildtype<br />
keratinocytes behaviour in vitro. Under non–permissive conditions uPAR wt grow faster<br />
than uPAR Ko keratinocytes (<strong>and</strong> differentiate faster). After a strong growth stimulation, such<br />
as addition <strong>of</strong> EGF or serum, the difference becomes even larger as the uPAR Ko keratinocytes<br />
do not respond to EGF. Moreover EGF induces cell growth <strong>and</strong> activates ERK/MAP kinase<br />
in murine keratinocytes only when these cells express uPAR even though the EGF receptor<br />
(EGFR) expression level was not different uPAR Ko <strong>and</strong> wt cells, both in the absence <strong>and</strong> in the<br />
presence <strong>of</strong> EGF. Moreover EGFR tyrosine phosphorylation, which is involved in cell growth, was<br />
specifically decreased in uPAR Ko expressing cells both in the absence <strong>and</strong> in the presence <strong>of</strong> EGF.<br />
In terms <strong>of</strong> cell proliferation, the rescue <strong>of</strong> the uPAR +/+ phenotype was achieved by expressing<br />
murine, but not human, uPAR cDNA, in uPAR Ko cells. This suggests a role for also for uPA in<br />
EGFR activation, possibly through an autocrine signalling, as murine uPA cannot bind the human<br />
uPAR.<br />
Besides a reduced growth rate in vitro, uPAR-deficient keratinocytes are also unable to migrate,<br />
adhere <strong>and</strong> spread on a glass substrate because they fail to produce <strong>and</strong> secrete their own LN-5<br />
substrate, which is an important requirement for reepithelialization <strong>of</strong> cutaneous wounds. In fact,<br />
when we generated full-thickness excision wounds in the skin, immunological analysis <strong>of</strong> frozen<br />
sections 3 days after injury, revealed that LN5 was highly expressed in uPAR wt but was almost<br />
absent in uPAR-deficient mice, meaning that also in vivo LN5 deposition is controlled by the uPAR<br />
genotype. This effect can be observed at both RNA <strong>and</strong> protein level.<br />
In summary, our data provide evidence that uPAR controls cell migration <strong>and</strong> proliferation both<br />
in vivo <strong>and</strong> in vitro under stressed conditions such as tumor growth <strong>and</strong> wound healing.<br />
<strong>Molecular</strong> & <strong>Cellular</strong> <strong>Biology</strong> <strong>of</strong> <strong>Plasminogen</strong> <strong>Activation</strong> 47
i036i<br />
Distinct Roles <strong>of</strong> Plasmin in Staphylococcus aureus-induced<br />
Sepsis <strong>and</strong> Infection Models<br />
Guo Y*, Li J, Hagström E, Ny T<br />
Department <strong>of</strong> Medical Biochemistry <strong>and</strong> Biophysics, Umeå University, Umeå, Sweden<br />
Presenting author e-mail: yong-zhi.guo@medchem.umu.se<br />
Plasmin is an important mediator in inflammatory cell migration <strong>and</strong> activation during host<br />
defense against bacterial infection. However, the exact functional role <strong>of</strong> plasmin/ogen during<br />
infection <strong>and</strong> sepsis is unclear. We have investigated the role <strong>of</strong> plasmin in murine Staphylococcus<br />
aureus-induced sepsis <strong>and</strong> infection models by using wild-type (plg +/+ ) <strong>and</strong> plasminogen-deficient<br />
(plg –/– ) mice. Our results showed that when mice were injected intravenously with 1 × 10 7 CFU <strong>of</strong><br />
S. aureus to induce systemic infection, the plg +/+ control mice had a 21-day survival rate <strong>of</strong> 86.7%.<br />
The 21-day survival rate in the plg –/– group was 50%. However, when 16 times more bacteria were<br />
injected to the mice, the average survival day for the plg –/– mice was 3 days longer than for the<br />
plg +/+ mice. 24 hours after the induction <strong>of</strong> sepsis, serum IL-6 <strong>and</strong> IL-10 levels <strong>and</strong> the bacterial<br />
counts in all detected organs were significantly higher in plg +/+ mice than in plg –/– mice. In plg +/+<br />
mice, blockade <strong>of</strong> IL-6 by intravenous injection <strong>of</strong> anti-IL-6 antibodies significantly prolonged<br />
the onset <strong>of</strong> mortality <strong>and</strong> improved the survival rate during sepsis. During sepsis, both the<br />
phosphorylated <strong>and</strong> total STAT3 protein levels were dramatically lower in the neutrophils <strong>of</strong><br />
plg –/– mice as compared with plg +/+ mice. These data indicate that plasmin plays different roles<br />
during infection <strong>and</strong> sepsis. In the infectious model plasmin has beneficial effects on host antibacterial<br />
immune responses. However, in the septic model, plasmin seems to excessively promote<br />
the production <strong>of</strong> inflammatory cytokines <strong>and</strong> tissue destruction, cripples neutrophil function, as<br />
well as impairs bacterial killing ability in plg +/+ mice.<br />
48 X I t h I n t e r n a t i o n a l W o r k s h o p o n
i037i<br />
Proteolytic <strong>Activation</strong> <strong>of</strong> the Human Urokinase/Plasmin System<br />
by Staphylococcus aureus<br />
Beaufort N* 1 , Wojciechowski P 1,2 , Sommerh<strong>of</strong>f CP 3 , Schmitt M 1 , Potempa J 2 , Magdolen V 1<br />
1 Department <strong>of</strong> Obstetrics <strong>and</strong> Gynecology, Technical University <strong>of</strong> Munich, Munich, Germany;<br />
2Department <strong>of</strong> Microbiology, Faculty <strong>of</strong> Biochemistry, Biophysics <strong>and</strong> Biotechnology, Jagiellonian<br />
University, Krakow, Pol<strong>and</strong>;<br />
3Department <strong>of</strong> Clinical Chemistry <strong>and</strong> Clinical Biochemistry, Ludwig-Maximilians-University,<br />
Munich, Germany<br />
Presenting author e-mail: nbeaufortgbb@yahoo.fr<br />
The major opportunistic human pathogen Staphylococcus aureus is known to interact with <strong>and</strong><br />
engage the human plasminogen activation system through plasmin(ogen) binding <strong>and</strong> nonproteolytic<br />
activation, a capacity which is thought to participate to bacterial spread <strong>and</strong> invasion.<br />
We here report that staphylococcal reference <strong>and</strong> clinical strains efficiently convert the zymogen<br />
pro-urokinase (pro-uPA) into its active counterpart uPA. Using selective protease inhibitors,<br />
purified bacterial proteases, <strong>and</strong>/or protease-deficient bacterial strains, we establish that this<br />
processing involves the secreted thermolysin-like metalloprotease aureolysin, <strong>and</strong> displays a<br />
2.6 x 10-3 M-1 s-1 catalytic efficiency. Additionally, aureolysin not only targets pro-uPA, but also<br />
cleaves <strong>and</strong> disables the serpins plasminogen activator inhibitor-1 <strong>and</strong> a2-antiplasmin, whereas it<br />
converts plasminogen into angiostatin <strong>and</strong> mini-plasminogen.<br />
Altogether, we propose that, in parallel to the staphylokinase-dependent activation <strong>of</strong><br />
plasminogen, aureolysin contributes significantly to the activation <strong>of</strong> the fibrinolytic system by S.<br />
aureus, <strong>and</strong> thus may promote bacterial spread <strong>and</strong> invasion.<br />
<strong>Molecular</strong> & <strong>Cellular</strong> <strong>Biology</strong> <strong>of</strong> <strong>Plasminogen</strong> <strong>Activation</strong> 49
i038i<br />
The Maintenance <strong>of</strong> High Affinity <strong>Plasminogen</strong> Binding by PAM<br />
Variants from Group A Streptococci Is Mediated by Conserved<br />
Arg <strong>and</strong> His Residues in Both the a1 <strong>and</strong> a2 Repeat Domains<br />
Ranson M* 1 , S<strong>and</strong>erson-Smith ML 1 , Walker MJ 1 , Fu Q 2 , Castellino FJ 2 , Prorok M 2<br />
1 School <strong>of</strong> Biological Sciences, University <strong>of</strong> Wollongong, Australia;<br />
2W.M. Keck Center for Transgene Research <strong>and</strong> Department <strong>of</strong> Chemistry <strong>and</strong> Biochemistry, University<br />
<strong>of</strong> Notre Dame, Notre Dame, Indiana, USA<br />
Presenting author e-mail: mranson@uow.edu.au<br />
Subversion <strong>of</strong> the plasminogen activation system is implicated in the virulence <strong>of</strong> Group A<br />
streptococci (GAS). GAS display several receptors for human plasminogen on the cell surface<br />
including the high affinity plasminogen-binding group A streptococcal M protein (PAM),<br />
which mediates an important virulence mechanism for a subset <strong>of</strong> GAS isolates. The major<br />
plasmin(ogen)-binding domain <strong>of</strong> PAM is comprised <strong>of</strong> two characteristic t<strong>and</strong>em repeats<br />
designated a1 <strong>and</strong> a2. We have recently shown that mutation <strong>of</strong> previously identified key<br />
residues Lys98, Arg101, His102 <strong>and</strong> Lys111 within the a1 <strong>and</strong> a2 repeats reduced, but did not<br />
abrogate plasminogen binding by full-length PAM using solid-phase binding assays. Loss <strong>of</strong><br />
plasminogen binding was only observed following simultaneous mutation <strong>of</strong> Arg101, Arg114,<br />
His102 <strong>and</strong> His115 in both the a1 <strong>and</strong> a2 repeats regardless <strong>of</strong> the presence <strong>of</strong> residues Lys98<br />
<strong>and</strong> Lys111. The on- <strong>and</strong> <strong>of</strong>f-rate constants underlying the Kd values obtained from these assays<br />
were further examined using PAM <strong>and</strong> select variants by surface plasmon resonance (SPR). The<br />
relative affinity <strong>of</strong> PAM for streptokinase-resistant murine plasminogen compared to human<br />
plasminogen was also investigated by SPR <strong>and</strong> will be reported. This demonstration <strong>of</strong> a nonlysine-dependent,<br />
high affinity interaction between plasminogen <strong>and</strong> a receptor is unique. We<br />
suggest that the highly conserved Arg <strong>and</strong> His residues from either the a1 or a2 repeats in PAMlike<br />
proteins compensates for variation elsewhere in the binding repeats, or indeed for loss <strong>of</strong> one<br />
<strong>of</strong> the repeats, <strong>and</strong> explains the maintenance <strong>of</strong> high affinity plasminogen binding by naturally<br />
occurring PAM-like variants.<br />
50 X I t h I n t e r n a t i o n a l W o r k s h o p o n
i039i<br />
<strong>Plasminogen</strong> Activator Inhibitor-1 (PAI-1) Is an<br />
Inhibitor <strong>of</strong> Factor VII-Activating Protease in Patients<br />
with Acute Respiratory Distress Syndrome<br />
Wygrecka M* 1 , Morty RE 2 , Markart P 2 , Kanse SM 1 , Andreasen PA 3 , Wind T 3 , Guenther A 2 , Preissner KT 1<br />
1 2 Department <strong>of</strong> Biochemistry, Department <strong>of</strong> Internal Medicine, Faculty <strong>of</strong> Medicine, Justus-Liebig-<br />
University Giessen, Giessen, Germany;<br />
3 Department <strong>of</strong> <strong>Molecular</strong> <strong>and</strong> Structural <strong>Biology</strong>, University <strong>of</strong> Aarhus, Aarhus, Denmark<br />
Presenting author e-mail:malgorzata.wygrecka@innere.med.uni-giessen.de<br />
Factor VII-activating protease (FSAP) is a novel plasma-derived serine protease structurally<br />
homologous to tissue-type (tPA) <strong>and</strong> urokinase-type (uPA) plasminogen activators. We<br />
demonstrate that plasminogen activator inhibitor-1 (PAI-1), the predominant inhibitor <strong>of</strong> tPA <strong>and</strong><br />
uPA in plasma <strong>and</strong> tissues, is an inhibitor <strong>of</strong> FSAP as well. We detected PAI-1-FSAP complexes<br />
in addition to high levels <strong>of</strong> extracellular RNA, an important FSAP c<strong>of</strong>actor, in bronchoalveolar<br />
lavage fluids from patients with acute respiratory distress syndrome (ARDS). Hydrolytic activity<br />
<strong>of</strong> FSAP was inhibited by PAI-1 with a second-order inhibition rate constant (Ka) <strong>of</strong> 3.38 ± 1.12 x<br />
10 5 M-1.s-1. Residue Arg346 was a critical recognition element on PAI-1 for interaction with FSAP.<br />
RNA, but not DNA, fragments (>400 nucleotides in length) dramatically enhanced the reactivity<br />
<strong>of</strong> PAI-1 with FSAP, <strong>and</strong> 4 µg.ml-1 RNA increased the Ka to 1.61 ± 0.94 x 10 6 M-1.s-1. RNA also<br />
stabilized the active conformation <strong>of</strong> PAI-1, increasing the half-life for spontaneous conversion <strong>of</strong><br />
active to latent PAI-1 from 48.4 ± 8 min to 114.6 ± 5 min. In contrast, little effect <strong>of</strong> DNA on PAI-1<br />
stability was apparent. Residues Arg76 <strong>and</strong> Lys80 in PAI-1 were key elements mediating binding<br />
<strong>of</strong> nucleic acids to PAI-1. FSAP-driven inhibition <strong>of</strong> vascular smooth muscle cell proliferation<br />
was antagonized by PAI-1, suggesting functional consequences for the FSAP-PAI-1 interaction.<br />
These data indicate that extracellular RNA <strong>and</strong> PAI-1 can regulate FSAP activity, thereby playing<br />
a potentially important role in hemostasis <strong>and</strong> cell functions under various pathophysiological<br />
conditions such as ARDS.<br />
<strong>Molecular</strong> & <strong>Cellular</strong> <strong>Biology</strong> <strong>of</strong> <strong>Plasminogen</strong> <strong>Activation</strong> 51
i040i<br />
Improved Muscle Regeneration in PAI-1-deficient Mice<br />
Is Associated with an Enhanced Inflammatory Response<br />
<strong>and</strong> Reduced Fibrin Deposition after Injury<br />
Ardite E*, Vidal B, Jardí M, González B, Muñoz-Cánoves P<br />
Center for Genomic Regulation (CRG), Program on Differentiation <strong>and</strong> Cancer, Barcelona, Spain<br />
Presenting author e-mail: esther.ardite@crg.es<br />
We have previously shown that uPA activity is required for muscle regeneration in vivo, since<br />
muscle regeneration was impaired in uPA-deficient mice (uPA–/–) after injury, correlating with<br />
persistent accumulation <strong>of</strong> fibrin. In contrast, mice lacking the uPA inhibitor PAI-1 (PAI-1–/–)<br />
showed an improved <strong>and</strong> accelerated muscle regeneration with respect to wild-type (WT) mice<br />
after injury, which correlated with decreased fibrin deposition in PAI-1–/– muscles. These data<br />
suggest that the regulation <strong>of</strong> fibrinolysis by the uPA/PAI-1 balance is important for efficient<br />
muscle regeneration. Moreover, while the recruitment <strong>of</strong> inflammatory cells to regenerating<br />
muscle was reduced in uPA–/– mice, it was increased in PAI-1–/– mice with respect to WT<br />
mice, suggesting that uPA/PAI-1 activities may play a role in the inflammatory response at the<br />
site <strong>of</strong> injury. To test this hypothesis, we analyzed whether transplantation <strong>of</strong> WT bone marrow<br />
would rescue the defective regeneration <strong>of</strong> uPA–/– mice. Transplantation <strong>of</strong> WT bone marrow<br />
into uPA–/– mice restored the inflammatory cell recruitment to damaged uPA–/– muscle to the<br />
levels normally observed in WT mice; more importantly, this normalized inflammatory response<br />
was accompanied by a rescued muscle regeneration in uPA–/– mice. Additional transplantation<br />
experiments <strong>of</strong> WT bone marrow into PAI-1 –/– mice are ongoing. Altogether, these results<br />
indicate that the uPA/PAI-1 balance may be important for efficient inflammation <strong>and</strong> muscle<br />
regeneration, with important implications for human muscular dystrophies.<br />
52 X I t h I n t e r n a t i o n a l W o r k s h o p o n
i041i<br />
Invasion <strong>and</strong> Metastasis <strong>of</strong> Carcinoma Cells Is Prevented by<br />
Urokinase-Derived Antagonists <strong>of</strong> avb5 Integrin <strong>Activation</strong><br />
Franco P 1 , Vocca I 1 , Alfano D 1 , Votta G 1 , Carriero MV 2 , Estrada Y 4 , Netti PA 3 , Ossowski L 4 ,<br />
Stoppelli MP* 1<br />
1 Institute <strong>of</strong> Genetics <strong>and</strong> Biophysics ‘’Adriano Buzzati-Traverso’’, National Research Council, Naples,<br />
Italy;<br />
2 National Cancer Institute <strong>of</strong> Naples, Via M. Semmola, Naples, Italy;<br />
3 Department <strong>of</strong> Materials <strong>and</strong> Production Engineering, University ‘’Federico II’’, Piazzale Tecchio,<br />
Naples, Italy;<br />
4 Department <strong>of</strong> Medicine, Mount Sinai School <strong>of</strong> Medicine, New York, New York, USA<br />
Presenting author e-mail: stoppell@igb.cnr.it<br />
We have previously shown that phosphorylation <strong>of</strong> urokinase (uPA) as well as substitution <strong>of</strong><br />
the critical serine with glutamic acid residues (His-uPA138E/303E) impairs its motogen ability.<br />
Phospho-mimicking uPA strongly inhibited carcinoma cell invasion, as shown by the reduced<br />
metastatic ability <strong>of</strong> HEp3 cell clones stably expressing His-uPA138E/303E in the chick embryo<br />
chorioallantoic membrane. The relationship between this inhibitory effect <strong>and</strong> urokinase receptor<br />
(uPAR) expression was analyzed by using several uPA variants lacking the uPAR binding<br />
domain (residues 9-45 <strong>of</strong> the human sequence) <strong>and</strong> carrying the relevant Ser to Glu substitutions<br />
(dGFa138E/303E) in HEK-293 cells. A strong inhibitory effect <strong>of</strong> cell migration toward different<br />
matrix chemoattractants resulted, in a growth factor domain- <strong>and</strong> uPAR-independent manner.<br />
The inhibitory uPA reduces the speed <strong>of</strong> cell translocation by 5 fold <strong>and</strong> alters the pattern <strong>of</strong> Factin<br />
formation in HEK-293 cells. His-uPA138E/303E <strong>and</strong> dGFa138E/303E specifically bind to<br />
avb5 integrin, as binding is inhibited by specific anti-integrin antibodies <strong>and</strong> by pre-incubation<br />
<strong>of</strong> lig<strong>and</strong> with purified avb5. Finally, cell exposure to picomolar concentrations <strong>of</strong> His-uPA138E/<br />
303E or dGFa138E/303E decreases the affinity <strong>of</strong> avb5 integrin for 125I-vitronectin <strong>and</strong> impairs<br />
cell chemotactic response to vitronectin. Also, the extent <strong>of</strong> talin associated to h5 is markedly<br />
decreased. Although the uPA-derived antagonists do not bind directly to a5b1, a4b1, a1b1,<br />
they prevent cell response to fibronectin, laminin <strong>and</strong> collagen. Similarly, a general inhibition is<br />
observed in the presence <strong>of</strong> the natural antagonist endostatin, which binds to avb5 <strong>and</strong> in the<br />
presence <strong>of</strong> anti- avb5 blocking antibodies. These data, taken together, show that avb5 can convey<br />
a strong signal inhibiting cell migration <strong>and</strong> suggest that this inhibition extends to other integrins.<br />
<strong>Molecular</strong> & <strong>Cellular</strong> <strong>Biology</strong> <strong>of</strong> <strong>Plasminogen</strong> <strong>Activation</strong> 53
i042i<br />
Urokinase Receptor/Integrin Interactions in Lung Tumor Development<br />
Tang CH, Hill M, Kim Y, Wei Y, Chapman HA*<br />
Pulmonary <strong>and</strong> Critical Care Division, Department <strong>of</strong> Medicine, Cardiovascular Research Institute,<br />
University <strong>of</strong> California, San Francisco, California, USA<br />
Presenting author e-mail: hal.chapman@ucsf.edu<br />
Upregulation <strong>of</strong> urokinase receptors (uPAR) is common during cancer progression <strong>and</strong> thought to<br />
promote invasion <strong>and</strong> metastasis. Urokinase receptors bind urokinase <strong>and</strong> a set <strong>of</strong> beta1 integrins,<br />
but it remains unclear whether or how uPAR/integrin binding contributes to tumor progression.<br />
Using site-directed mutagenesis, single amino acid mutants <strong>of</strong> the urokinase receptor were<br />
identified that fail to associate with either integrins alpha3beta1 (D262A) or alpha5beta1 (H249A).<br />
A recombinant uPAR bearing both D262A <strong>and</strong> H249A mutations (H/D uPAR) was found to be<br />
expressible, to bind urokinase normally, but to no longer co-precipitate with beta1 integrins. To<br />
study the functional effects <strong>of</strong> these mutations, endogenous uPAR was first stably silenced in<br />
H1299 lung cancer cells <strong>and</strong> then wild type or mutant uPARs expressed. Orthotopic implantation<br />
into nude mice <strong>of</strong> H1299 cells with uPAR knockdown resulted in lower incidence <strong>and</strong> markedly<br />
suppressed lung tumor area (8 mm2 vs 1.5 mm2 , n = 14) compared to parent cells at 32 days,<br />
<strong>and</strong> this was reversed by wild type but not H/D uPAR re-constitution. H1299 cells expressing<br />
wt <strong>and</strong> H/D mutant uPAR were compared for matrix-induced ERK activation, MMP expression,<br />
<strong>and</strong> invasion through matrigel-coated transwells in vitro. Compared with wt uPAR reconstituted<br />
H1299 cells, H/D uPAR cells showed virtually no fibronectin or laminin-induced ERK activation,<br />
MMP upregulation, or matrix-dependent migration. Collectively, these data indicate that uPAR/<br />
integrin complexes are required for matrix-dependent induction <strong>of</strong> MMP through an ERKdependent<br />
pathway in H1299 cells <strong>and</strong> that this signaling pathway appears important to lung<br />
tumor development in vivo.<br />
54 X I t h I n t e r n a t i o n a l W o r k s h o p o n
i043i<br />
uPA- <strong>and</strong> uPAR-Expressing Stromal Cells Accompany<br />
the Transition to Invasive Breast Cancer<br />
Nielsen BS* 1 , Rank F 2 , Illemann M 1 , Lund LR 1 , Danø K 1<br />
1 The Finsen Laboratory, Rigshospitalet, Copenhagen, Denmark;<br />
2 Department <strong>of</strong> Pathology, Rigshospitalet, Copenhagen, Denmark<br />
Presenting author e-mail: schnack@finsenlab.dk<br />
The transition from ductal carcinoma in situ (DCIS) <strong>of</strong> the breast to invasive ductal carcinoma is<br />
facilitated by proteolytic degradation <strong>of</strong> the basement membrane. The transition can be identified<br />
as microinvasive foci in a small proportion <strong>of</strong> DCIS lesions. We have previously reported that<br />
MMP-13 is frequently expressed in such foci. To establish if plasmin-directed proteolysis is<br />
likely to be involved in early invasion we have studied the expression <strong>of</strong> urokinase plasminogen<br />
activator (uPA) <strong>and</strong> its receptor (uPAR) in human DCIS lesions with <strong>and</strong> without microinvasion.<br />
uPA mRNA was detected in periductal stromal cells in all <strong>of</strong> 9 DCIS lesions with microinvasion<br />
<strong>and</strong> in 2 <strong>of</strong> 9 DCIS lesions without microinvasion by in situ hybridization. The uPA mRNA<br />
signal was seen in numerous stromal cells in microinvasive areas together with MMP-13 mRNA<br />
expressing cells. Double immun<strong>of</strong>luorescence analyses, using emission fingerprinting, showed<br />
that the uPA expressing stromal cells included both macrophages <strong>and</strong> my<strong>of</strong>ibroblasts. uPAR was<br />
focally upregulated in periductal stromal cells in all <strong>of</strong> the 9 DCIS lesions with microinvasion<br />
<strong>and</strong> in only 2 <strong>of</strong> the 9 DCIS lesions without microinvasion. uPAR was seen in both macrophages<br />
<strong>and</strong> my<strong>of</strong>ibroblasts in microinvasive areas <strong>and</strong> it was evident that uPA <strong>and</strong> uPAR co-localized<br />
in both fibroblast-like cells <strong>and</strong> macrophage-like cells. The early invasive carcinoma cells were<br />
negative for both uPA <strong>and</strong> uPAR. We conclude that periductal macrophages <strong>and</strong> my<strong>of</strong>ibroblasts<br />
are strongly involved in the initial steps <strong>of</strong> breast cancer invasion by focally upregulating the<br />
expression <strong>of</strong> the plasminogen activation system <strong>and</strong> MMP-13.<br />
<strong>Molecular</strong> & <strong>Cellular</strong> <strong>Biology</strong> <strong>of</strong> <strong>Plasminogen</strong> <strong>Activation</strong> 55
i044i<br />
Generation <strong>of</strong> the Malignant Phenotype in HT-1080 Tumor Cells by<br />
PAI-1 Involves Modulation <strong>of</strong> Proteasomal Activity <strong>and</strong> Phosphatases<br />
Mihaly J* 1 , Carroll VA 2 , Breuss JM 1 , Prager GW 1,3 , Binder BR 1<br />
1 Department <strong>of</strong> Vascular <strong>Biology</strong> <strong>and</strong> Thrombosis Research, Medical University Vienna, Austria;<br />
2 Imperial College <strong>of</strong> Medicine, Oxford, United Kingdom;<br />
3 First Clinic for Internal Medicine, Oncology, Medical University Vienna, Austria<br />
Presenting author e-mail: judit.mihaly@meduniwien.ac.at<br />
Elevated levels <strong>of</strong> PAI-1 are <strong>of</strong>ten found in several types <strong>of</strong> cancer <strong>and</strong> increased PAI-1 levels<br />
positively correlate with poor outcome <strong>and</strong> prognosis. We described that prolonged exposure <strong>of</strong><br />
‘’non-malignant’’, low PAI-1 secreting HT-1080 cells to exogenous PAI-1 increased cell adhesion<br />
via redistribution <strong>of</strong> integrins <strong>of</strong> the broad substrate specificity alpha-v heterodimer type to<br />
the cell surface. This PAI-1 induced integrin redistribution was dependent on the presence <strong>of</strong><br />
uPA, uPAR <strong>and</strong> a member <strong>of</strong> the LDLR-family as shown by the use <strong>of</strong> firboblasts derived from<br />
respective gene deficient mice <strong>and</strong> involved sustained activation <strong>of</strong> the ERK/MAPK pathway.<br />
The involvement <strong>of</strong> ERK1 in that process was also demonstrated by overexpression <strong>of</strong> EGFP<br />
tagged ERK1 that mimicked integrin redistribution <strong>and</strong> cell adhesion. Furthermore, exposure<br />
to exogenous PAI-1 also influences proteasomal activity: at early timepoints (2 hours) a PAI-1/<br />
uPA/LDLR dependent increase <strong>of</strong> proteasomal activity was found, whereas after 18 hours the<br />
proteasomal activity in PAI-1 stimulated cells dropped below levels measured in unstimulated<br />
control. The activity <strong>of</strong> ERK1/2 is tightly controlled by dual specificity phosphatases, whereby<br />
one <strong>of</strong> the major players is the MKP1/DUSP1 <strong>and</strong> exposure <strong>of</strong> cells to exogenous PAI-1 also<br />
modulated DUSP-1 on the mRNA <strong>and</strong> protein levels, while DUSP4 remained unaffected. Active<br />
ERK1/2 controls proteasomal degradation <strong>of</strong> its regulator MKP1/DUSP1 by phosphorylation.<br />
From these data we propose a model in which PAI-1 triggered sustained ERK activation is<br />
maintained by a fine tuned regulatory mechanism involving modulation <strong>of</strong> the proteasomal<br />
activity providing the optimal kinase-phosphatase balance required for survival <strong>of</strong> detached/<br />
metastasizing <strong>and</strong> proliferation <strong>of</strong> the lodged cells.<br />
56 X I t h I n t e r n a t i o n a l W o r k s h o p o n
i045i<br />
PEGylated DX-1000: Pharmacokinetics: Anti-Tumor <strong>and</strong><br />
Anti-Metastatic Effects <strong>of</strong> a Specific Plasmin Inhibitor<br />
Devy L* 1 , Rabbani SA 2 , Stochl M 3 , Ruskowski M 4 , Mackie I 5 , Naa L 1 , Toews M 3 , van Gool R 1 , Chen J 3 ,<br />
Ley A 3 , Ladner RC 3 , Dransfield DT 3 , Henderikx P 1<br />
1 Dyax s.a. Building 22, Sart-Tilman, Liege, Belgium;<br />
2 Department <strong>of</strong> Medicine <strong>and</strong> Oncology, McGill University Health Centre, Montreal, QC, Canada;<br />
3 Dyax Corporation, Cambridge, Massachusetts, USA;<br />
4Department <strong>of</strong> Radiology, Division <strong>of</strong> Nuclear Medicine, University <strong>of</strong> Massachusetts Medical School,<br />
Worcester, Massachusetts, USA;<br />
5 Haematology Department, University College London, London, United Kingdom<br />
Presenting author e-mail: ldevy@dyax.com<br />
Using phage display, we identified a TFPI-derived Kunitz domain protein which is a specific high<br />
affinity inhibitor <strong>of</strong> plasmin (Ki=99±15pM) referred to as DX-1000. DX-1000 blocked plasminmediated<br />
proMMP-9 activation, invasiveness (44-66%) <strong>of</strong> uPA-expressing HT-1080 cells <strong>and</strong><br />
tube formation <strong>of</strong> HUVECs (IC 50 =1.4±0.3nM) <strong>and</strong> mouse endothelial cells (IC 50 =16.6± 0.1nM).<br />
DX-1000 did not significantly affect haemostasis <strong>and</strong> coagulation in vitro. However, due to its<br />
low molecular weight (~7 kDa), the protein exhibited a rapid plasma clearance rate in vivo (b<br />
phase half-life=27 minutes in mice <strong>and</strong> 1 hour in rabbits). After site-specific PEGylation, DX-1000<br />
retained its activity <strong>and</strong> exhibited a decreased plasma clearance (b phase half-life=13 hours in<br />
mice <strong>and</strong> 59 hours in rabbits). 4PEG-DX-1000 was effective in vitro, <strong>and</strong> inhibited growth <strong>of</strong> MDA-<br />
MB231 tumor cells in nude mice (45% TGI). 4PEG-DX-1000 treatment caused a marked inhibition<br />
<strong>of</strong> angiogenesis, a significant reduction <strong>of</strong> uPA expression, <strong>and</strong> inhibition <strong>of</strong> tumor proliferation<br />
<strong>and</strong> MAPK phosphorylation. 4PEG-DX-1000 treatment significantly reduced the number <strong>of</strong><br />
metastatic foci in the lung (46%) <strong>and</strong> the liver (57%) <strong>and</strong> decreased the level <strong>of</strong> active FAK in the<br />
primary tumors. Together, the results from these studies provide compelling evidence for the role<br />
<strong>of</strong> plasmin inhibitors as therapeutic agents for blocking breast cancer growth <strong>and</strong> metastasis.<br />
<strong>Molecular</strong> & <strong>Cellular</strong> <strong>Biology</strong> <strong>of</strong> <strong>Plasminogen</strong> <strong>Activation</strong> 57
i046i<br />
Cytotoxic Potential <strong>of</strong> a Novel uPA-activity Dependent<br />
<strong>and</strong> EGF Receptor-targeting Pro-drug<br />
Rønø B* 1, 5 , Bae Kim G 2 , Liu S 3 , Kristjansen PEG 4 , Neville DM 2 , Leppla SH 3 , Bugge TH 5 , Rømer J 1<br />
1 Finsen Laboratory, Rigshospitalet, Copenhagen, Copenhagen, Denmark;<br />
2 National Institutes <strong>of</strong> Mental Health, NIH, Bethesda, Maryl<strong>and</strong>, USA;<br />
3 National Institutes <strong>of</strong> Allergy <strong>and</strong> Infectious Diseases, NIH, Bethesda, Maryl<strong>and</strong>, USA;<br />
4 Institute <strong>of</strong> <strong>Molecular</strong> Pathology, University <strong>of</strong> Copenhagen, Copenhagen, Denmark;<br />
5 National Institutes <strong>of</strong> Dental <strong>and</strong> Crani<strong>of</strong>acial Research, NIH, Bethesda, Maryl<strong>and</strong>, USA<br />
Presenting author e-mail: brono@finsenlab.dk<br />
To exploit this preferential expression <strong>of</strong> uPA <strong>and</strong> uPAR in cancer we have constructed a novel<br />
pro-drug whose activation is dependent on proteolytic processing by uPA. To further improve<br />
the cancer specificity, the pro-drug targets epidermal growth factor receptor (EGFR) expressing<br />
cells solely. The pro-drug, termed DT-U2-TGFa, was generated by replacing the native proteolytic<br />
activation sequence in the diphtheria toxin with an amino acid sequence recognised by uPA <strong>and</strong><br />
in addition by exchanging the diphtheria receptor-binding domain with transforming growth<br />
factor alpha (TGFa).<br />
We have examined the activation, specificity, <strong>and</strong> cytotoxic potential <strong>of</strong> the pro-drug. By<br />
incubating the pro-drug with recombinant uPA DTU2TGFa was cleavaged by uPA in a<br />
time dependent manner. In a cell culture based assay, the uPA/uPAR <strong>and</strong> EGFR expressing<br />
human head <strong>and</strong> neck cancer cell line, HN6, bound, activated, <strong>and</strong> internalised DT-U2-TGFa.<br />
Furthermore, a colorimetric cytotoxicity assay showed that the cells were killed by DT-U2-TGFa<br />
in a dose dependent manner. Incubation with different uPA inhibitors prior to treatment with<br />
DT-U2-TGFa efficiently reduced activation <strong>of</strong> the pro-drug, substantiating the requirement for<br />
active uPA. EGFR transduced murine fibroblasts, NR6W, were sensitive to DT-U2-TGFa, while<br />
the parental EGFR negative NR6 cells were not affected, indicating that the cytotoxicity <strong>of</strong> DTU2-<br />
TGFa is restricted to EGFR expressing cells. In support <strong>of</strong> these data HN6 cells pre-incubated with<br />
TGFa were completely rescued from DT-U2-TGFa induced cell death.<br />
In conclusion, we have constructed, produced, <strong>and</strong> tested a novel pro-drug that targets uPA/<br />
uPAR <strong>and</strong> EGFR expressing cells. Our data provides evidence <strong>of</strong> a highly specific pro-drug with<br />
promising cytotoxic efficacy in cancer cells.<br />
58 X I t h I n t e r n a t i o n a l W o r k s h o p o n
i047i<br />
Inhibition <strong>of</strong> Mouse uPA Activity by Mouse<br />
Monoclonal Antibodies in vitro <strong>and</strong> in vivo<br />
Lund IK*, Jögi A, Behrendt N, Ploug M, Gårdsvoll H, Lund LR, Rømer J, Høyer-Hansen G<br />
Finsenlaboratoriet, Copenhagen BioCenter, Copenhagen, Denmark<br />
Presenting author e-mail: ikl@finsenlab.dk<br />
The potential <strong>of</strong> monoclonal antibodies (mAbs) as anti-cancer therapeutics has lately been<br />
demonstrated for a number <strong>of</strong> antigens. To enable in vivo therapy experiments using mAbs in<br />
murine cancer models, we immunized mice deficient in murine urokinase plasminogen activator<br />
(muPA) with recombinant muPA, thus developing murine mAbs directed against muPA.<br />
We have selected 5 mAbs (mU1-mU5) reacting with muPA in ELISA, Surface Plasmon Resonance<br />
(SPR) analysis, <strong>and</strong> Western blotting. Analysing the epitope location on muPA using the<br />
recombinant amino-terminal fragment <strong>of</strong> muPA (mATF) <strong>and</strong> the B-chain revealed that only<br />
mU1 recognized an epitope exclusively located in the B-chain, encompassing the catalytic site <strong>of</strong><br />
muPA. SPR analyses demonstrated that mU2 was unable to bind receptor (muPAR)-bound muPA<br />
<strong>and</strong> prevented binding <strong>of</strong> muPAR to muPA. In vitro cell binding experiments using 125I-mATF<br />
illustrated an efficient mU2-induced interference <strong>of</strong> muPA-muPAR interaction on the cell surface.<br />
Using an enzyme kinetic assay measuring muPA-dependent plasminogen activation, four mAbs<br />
were found to inhibit muPA catalytically activity to various extend, with mU1 having the most<br />
pronounced effect. Application <strong>of</strong> mU1 or mU2 in an anthrax toxin assay dependent on muPA<br />
activity yielded a very high cell rescue.<br />
Importantly, treatment <strong>of</strong> tissue-type plasminogen (tPA) deficient mice with mU1 resulted in<br />
significantly delayed wound healing mimicking the phenotype observed in uPA;tPA doubledeficient<br />
mice. Moreover, data concerning the in vivo effect <strong>of</strong> mU1 on liver fibrin deposits <strong>of</strong> tPA<br />
deficient mice as compared to uPA;tPA double-deficient mice will be provided.<br />
<strong>Molecular</strong> & <strong>Cellular</strong> <strong>Biology</strong> <strong>of</strong> <strong>Plasminogen</strong> <strong>Activation</strong> 59
i048i<br />
Crystal Structure <strong>of</strong> Human Urokinase Complexed<br />
with a Cyclic Peptidyl Inhibitor, uPAin-1<br />
Zhao G 1 , Yuan C 1 , Bian C 1 , Wind T 2 , Andreasen PA 2 , Huang M* 1<br />
1State Key Laboratory <strong>of</strong> Structural Chemistry, Fujian Institute <strong>of</strong> Research on the Structure <strong>of</strong> Matter,<br />
Chinese Academy <strong>of</strong> Sciences, Fuzhou, Fujian, China;<br />
2 Department <strong>of</strong> <strong>Molecular</strong> <strong>Biology</strong>, University <strong>of</strong> Aarhus, Aarhus, Denmark<br />
Presenting author e-mail: mhuang@fjirsm.ac.cn<br />
Urokinase-type plasminogen activator (uPA) plays a crucial role in the regulation <strong>of</strong> tumor<br />
cell adhesion <strong>and</strong> migration. The inhibition <strong>of</strong> uPA activity is a promising mechanism for anticancer<br />
therapy. A cyclic peptidyl inhibitor, upain-1, CSWRGLENHRMC, was identified recently<br />
as a competitive <strong>and</strong> highly specific uPA inhibitor (Hansen et al. J Biol Chem 280, 38424-37). We<br />
determined the crystal structure <strong>of</strong> uPA in complex with upain-1 at 2.15 Å. The structure reveals<br />
that the cyclic peptide adopts a rigid conformation stabilized by two tight beta turns formed by<br />
Leu6-His9 <strong>and</strong> His9-Cys12 segments, respectively. The Glu7 residue <strong>of</strong> upain-1 forms hydrogen<br />
bonds with the main chain nitrogen atoms <strong>of</strong> residues 4, 5, <strong>and</strong> 6 <strong>of</strong> upain-1, <strong>and</strong> is also critical<br />
for maintaining the active conformation <strong>of</strong> upain-1. The Arg4 <strong>of</strong> upain-1 is inserted into the uPA’s<br />
specific S1 pocket. The Ser2 residue <strong>of</strong> upain-1 locates close to the S1b pocket <strong>of</strong> uPA. The Gly5<br />
<strong>and</strong> Glu7 residues <strong>of</strong> upain-1 occupy the S2 pocket <strong>and</strong> the oxyanion hole <strong>of</strong> uPA, respectively.<br />
Furthermore, the Asn8 residue <strong>of</strong> upain-1 binds to the 37-loop <strong>and</strong> 60-loop <strong>of</strong> uPA <strong>and</strong> renders<br />
the specificity <strong>of</strong> upain-1 for uPA. The steric hindrance <strong>of</strong> the side chain <strong>of</strong> Glu7 <strong>and</strong> the indole<br />
ring <strong>of</strong> Trp3 residue <strong>of</strong> upain-1 prevents the carboxyl group <strong>of</strong> Arg4 residue at the cleavage site to<br />
be accessible by the catalytic Ser195 residue <strong>of</strong> uPA, thus making upain-1 behave as an inhibitor<br />
rather than a substrate. Based on this structure, we propose a new pharmacophore for the design<br />
<strong>of</strong> highly specific uPA inhibitors.<br />
60 X I t h I n t e r n a t i o n a l W o r k s h o p o n
i049i<br />
Discovery <strong>of</strong> a Novel Zymogen Targeting Inhibitor <strong>of</strong><br />
Urokinase-type <strong>Plasminogen</strong> Activator: Evidence for<br />
Structural Flexibility <strong>of</strong> the Protease Domain<br />
Blouse GE 1 , Bøtkjær KA 1 , Deryugina EI 3 , Kjelgaard S 1 , Byszuk O 1 , Mortensen KK 1 , Quigley JP 3 ,<br />
Andreasen PA* 1<br />
1 2 Laboratory <strong>of</strong> <strong>Cellular</strong> Protein Science, BioDesign Laboratory, Department <strong>of</strong> <strong>Molecular</strong> <strong>Biology</strong>,<br />
University <strong>of</strong> Aarhus, Aarhus, Denmark;<br />
3 Department <strong>of</strong> Cell <strong>Biology</strong>, Scripps Research Institute, La Jolla, California, USA<br />
Presenting author e-mail: pa@mb.au.dk<br />
Considerable interest is emerging for pharmacologic interference with proteolytic enzyme targets.<br />
One such validated target is urokinase-type plasminogen activator (uPA), which has received<br />
much attention due to a suspected causal role in the clinical progression <strong>of</strong> cancer <strong>and</strong> other<br />
processes <strong>of</strong> pathological tissue remodeling. Nonetheless, development <strong>of</strong> specific small molecule<br />
inhibitors has proven a daunting task. In nature, a key mechanism <strong>of</strong> protease regulation is the<br />
point <strong>of</strong> zymogen activation. Thus far, controlling protease activity by targeting the zymogen<br />
activation step is an underexploited strategy. We have now designed a specific monoclonal<br />
antibody inhibitor (Mab-112) with sub-nanomolar affinity to pro-uPA. A detailed mechanistic<br />
evaluation with several biophysical methods elucidated a novel multifunctional mechanism<br />
whereby Mab-112 retards the protelytic conversion <strong>of</strong> single-chain pro-uPA into the two-chain<br />
form <strong>and</strong> subsequently averts the conformational transition to a mature protease by sequestering<br />
the two-chain form in a zymogen-like state. Furthermore, Mab-112 is a non-competitive inhibitor<br />
<strong>of</strong> two-chain uPA, stabilising the protease in a non-catalytic conformation. Functional studies<br />
employing high intravasating (HT-hi/diss) <strong>and</strong> low intravasating (HT-lo/diss) variants <strong>of</strong> the<br />
human HT-1080 cell line demonstrate that Mab-112 is an effective inhibitor <strong>of</strong> intravasation in the<br />
chorioallantoic membrane assay. These findings show the utility <strong>of</strong> pharmacological interference<br />
<strong>of</strong> zymogen activation as a plausible <strong>and</strong> robust means to regulate uPA activity <strong>and</strong> the<br />
downstream effects <strong>of</strong> plasminogen activation. Furthermore, a strategy that targets regions related<br />
to pro-enzyme activation likely provide a unique inhibitor-protease interaction surface <strong>and</strong> is thus<br />
expected to enhance the chances <strong>of</strong> engineering high inhibitor specificity.<br />
<strong>Molecular</strong> & <strong>Cellular</strong> <strong>Biology</strong> <strong>of</strong> <strong>Plasminogen</strong> <strong>Activation</strong> 61
i050i<br />
A Novel Type <strong>of</strong> Agent Blocking the Association <strong>of</strong> uPA<br />
to its Receptor uPAR: uPA-binding Aptamers<br />
Dupont DM* 1,2 , Madsen JB 1 , Kjems J 1,2 , Andreasen PA 1,2<br />
1 Department <strong>of</strong> <strong>Molecular</strong> <strong>Biology</strong>, 2 iNANO Centre, University <strong>of</strong> Aarhus, Aarhus, Denmark<br />
Presenting author e-mail: dmd@mb.au.dk<br />
Systematic evolution <strong>of</strong> lig<strong>and</strong>s by exponential enrichment (SELEX) is a relatively new approach<br />
for generating agents <strong>of</strong> potential therapeutic <strong>and</strong> diagnostic interest. The technique combines<br />
the ability <strong>of</strong> RNA or DNA oligonucleotides to fold into a variety <strong>of</strong> three-dimensional structures,<br />
with the possibility <strong>of</strong> selecting, from very large pools <strong>of</strong> r<strong>and</strong>om sequences (~10 15 ), the ones<br />
capable <strong>of</strong> binding to a target <strong>of</strong> interest. We have generated a library <strong>of</strong> serum-stable 2´-fluoropyrimidine<br />
modified RNA oligonucletides <strong>and</strong> used it in a SELEX experiment to select sequences,<br />
or so-called aptamers, binding to human urokinase-type plasminogen activator (uPA). As<br />
analysed by surface plasmon resonance (SPR), the aptamers bind to the amino terminal fragment<br />
<strong>of</strong> human, but not murine, uPA, with K D -values in the low nanomolar range. SPR analyses <strong>and</strong><br />
cell binding assays have shown that the aptamers block the association <strong>of</strong> uPA with its receptor<br />
uPAR. In consistency with their binding area in the amino terminal fragment, they do not inhibit<br />
the uPA proteolytic activity directly, but inhibit uPAR-dependent plasminogen activation on cell<br />
surfaces. By RNA sequence alignments <strong>and</strong> computerised secondary structure predictions, we<br />
were able to identify the uPA binding regions <strong>of</strong> the aptamers <strong>and</strong> delete regions unnecessary<br />
for uPA binding. uPA-binding aptamers represent a promising principle for interfering with the<br />
pathophysiological functions <strong>of</strong> the plasminogen activation system. Targeting the receptor-lig<strong>and</strong><br />
interaction through uPA may be advantageous as compared to uPAR-targeting agents which may<br />
not be antagonists <strong>of</strong> all functions <strong>of</strong> uPAR. Aptamers are also potential tools for analytical <strong>and</strong><br />
imaging purposes.<br />
62 X I t h I n t e r n a t i o n a l W o r k s h o p o n
Abstracts for Poster Presentations<br />
i051i<br />
Identification <strong>and</strong> Analysis <strong>of</strong> the Vn Binding Site in Mouse uPAR<br />
Pirazzoli V* 1 , Andolfo AP 1 , Madsen CD 1 , Sidenius N 1,2<br />
1 IFOM Fondation, FIRC Institute <strong>of</strong> <strong>Molecular</strong> Oncology, Milan, Italy;<br />
2 <strong>Molecular</strong> Genetics Unit, DIBIT, Università Vita-Salute San Raffaele, Milan, Italy<br />
Presenting author e-mail: valentina.pirazzoli@ifom-ieo-campus.it<br />
A complete functional alanine scan <strong>of</strong> human uPAR conducted recently in our laboratory<br />
identified the interaction with Vn as being the only essential direct uPAR-interaction required for<br />
the receptor to induce changes in cell adhesion, morphology, migration <strong>and</strong> signaling. To address<br />
the importance <strong>of</strong> the Vn-interaction in vivo it is our goal to generate a knock-in mouse where the<br />
uPAR gene has been modified to encode a receptor deficient in Vn-binding but otherwise normal<br />
(i.e. with normal uPA-binding). With such a goal in mind, we now report the analysis <strong>of</strong> the<br />
Vn-binding epitope in mouse uPAR. When over-expressed in CHO cells, wild-type mouse uPAR<br />
(muPAR) was found to induce changes in cell morphology <strong>and</strong> colony formation very similar<br />
to that <strong>of</strong> the human receptor. These changes include the formation <strong>of</strong> actin-rich lamellipodia,<br />
loss <strong>of</strong> stress fibers, reduced cell-cell contact as well as a complete failure to form colonies when<br />
seeded a low density. We had previously identified 5 residues in human uPAR which appear to<br />
engage Vn directly <strong>and</strong> which when changed into alanine disrupt the Vn-interaction completely<br />
or partially. To establish if the corresponding, fully conserved, residues in muPAR (W32, R58, I63,<br />
R92 <strong>and</strong> Y93) are also responsible for Vn-binding we mutated these into alanine <strong>and</strong> tested their<br />
ability to induce RGD-independent Vn-adhesion as well as changes in cell morphology. The result<br />
<strong>of</strong> this analysis documented that a substitution <strong>of</strong> any <strong>of</strong> these residues completely impaired<br />
muPAR binding to Vn. Additional experiments using recombinant soluble muPAR confirmed the<br />
impaired Vn-binding <strong>and</strong> a normal uPA-binding.<br />
<strong>Molecular</strong> & <strong>Cellular</strong> <strong>Biology</strong> <strong>of</strong> <strong>Plasminogen</strong> <strong>Activation</strong> 63
i052i<br />
Novel uPAR Binding Site in Vitronectin<br />
Andolfo A* 1 <strong>and</strong> Sidenius N 1,2<br />
1 FIRC Institute <strong>of</strong> <strong>Molecular</strong> Oncology Foundation, Milan, Italy;<br />
2 Dibit, Fondazione Vita-salute San Raffaele, Milan, Italy<br />
Presenting author e-mail: annapaola.<strong>and</strong>olfo@ifom-ieo-campus.it<br />
The ability <strong>of</strong> the serum protein vitronectin (Vn) to modulate cell adhesion requires the<br />
aminoterminal somatomedin B (SMB) domain (amino acids 1-44) which binds both plasminogen<br />
activator inhibitor-1 (PAI-1) <strong>and</strong> urokinase-type plasminogen activator receptor (uPAR) as well<br />
as the flanking ArgGlyAsp sequence (RGD, amino acids 45-47) responsible for the interaction<br />
with Vn-receptors <strong>of</strong> the integrin family. Here we report our data on uPAR-Vn interaction site<br />
mapping by a complete alanine scan <strong>of</strong> the SMB domain. We expressed <strong>and</strong> purified the mutants<br />
from mammalian cell cultures <strong>and</strong> assayed their biochemical <strong>and</strong> biological activity. In contrast<br />
to previously published data using SMB domains expressed in E. coli, we find that single alanine<br />
substitution only has marginal effects on PAI-1 binding (< 2-fold reduction in affinity) <strong>and</strong> no<br />
detectable effects on integrin mediated RGD-dependent cell adhesion. We confirm the previously<br />
published data on uPAR binding site in Vn, that is overlapping to the known PAI-1 binding site<br />
(F13, D22, L24, Y27, Y28). Most importantly, we find additional residues in the SMB domain that<br />
are exclusively required for uPAR binding (S4, G7, R8), thus defining a composite site with two<br />
distinct epitopes located on opposite sides <strong>of</strong> the SMB-structure.<br />
In conclusion, the presence <strong>of</strong> two separate uPAR binding sites in the SMB, which are both critical<br />
for binding, raises important questions towards how <strong>and</strong> if a single molecule <strong>of</strong> uPAR can engage<br />
these two sites contemporarily.<br />
64 X I t h I n t e r n a t i o n a l W o r k s h o p o n
i053i<br />
Dissecting Serpin-protease Reaction Pathways<br />
by the Use <strong>of</strong> Monoclonal Antibodies<br />
Bødker JS*, Blouse GE, Dupont DM, Andreasen PA<br />
Department <strong>of</strong> <strong>Molecular</strong> <strong>Biology</strong>, University <strong>of</strong> Aarhus, Aarhus, Denmark<br />
Presenting author e-mail: jsb@mb.au.dk<br />
The formation <strong>of</strong> a stable PAI-1-protease complex is believed to progress through several<br />
separate steps. The steps include exosite interactions between the protease 37-loop <strong>and</strong> the serpin<br />
reactive centre loop (RCL); formation <strong>of</strong> a reversible Michaelis complex; formation <strong>of</strong> a stable<br />
acyl-enzyme intermediate; release <strong>of</strong> exosite interactions; insertion <strong>of</strong> the N-terminal side <strong>of</strong> the<br />
RCL as b-str<strong>and</strong> 4A which translocates the protease to the opposite pole <strong>of</strong> the serpin. We have<br />
now obtained further information about the PAI-1-protease mechanism by several approaches<br />
including the use <strong>of</strong> monoclonal anti-PAI-1 antibodies having epitopes near the path believed<br />
to be followed by the protease during translocation, stopped-flow analyses with fluorescently<br />
labeled PAI-1, BIACORE, <strong>and</strong> site-directed mutagenesis. Mab-5, which has an epitope near the<br />
region where the RCL first inserts into b-sheet A, caused a slight reduction in the rate <strong>of</strong> Michaelis<br />
complex formation, but promoted an 100-fold reduction in the rate <strong>of</strong> RCL insertion, an effect<br />
reduced by mutations known to affect the release from the protease-serpin exosite interactions.<br />
Another antibody, Mab-2, with an epitope in a-helix F, caused a 5–10-fold reduction in the rate <strong>of</strong><br />
loop insertion, induction <strong>of</strong> PAI-1 substrate behaviour, <strong>and</strong> accumulation <strong>of</strong> a rapidly dissociating<br />
complex on BIACORE, presumably an acyl-enzyme complex with partial loop insertion <strong>and</strong><br />
lacking exosite interactions. These results lend further support to the existence <strong>of</strong> two forms for<br />
acyl-enzyme intermediates in the serpin-protease reaction mechanism, one with intact exosite<br />
interactions <strong>and</strong> one in which release <strong>of</strong> exosite interactions is coupled to the initial phase <strong>of</strong> RCL<br />
insertion.<br />
<strong>Molecular</strong> & <strong>Cellular</strong> <strong>Biology</strong> <strong>of</strong> <strong>Plasminogen</strong> <strong>Activation</strong> 65
i054i<br />
PAI-1-vitronectin Interactions Involve an Extended Binding<br />
Surface <strong>and</strong> Mutual Conformational Rearrangements<br />
Blouse GE 1 , Peterson CB 2 , Dupont DM 1 , Ploug M 3 , Gårdsvoll H 3 , Schar CR 2 , Perron MJ 4 , Minor KH 2 ,<br />
Shore JD 4 , Andreasen PA* 1<br />
1 Department <strong>of</strong> <strong>Molecular</strong> <strong>Biology</strong>, University <strong>of</strong> Aarhus, Aarhus, Denmark;<br />
2Department <strong>of</strong> Biochemistry, <strong>Cellular</strong> <strong>and</strong> <strong>Molecular</strong> <strong>Biology</strong>, University <strong>of</strong> Tennessee, Knoxville,<br />
Tennessee, USA;<br />
3 Finsen Laboratory, Rigshospitalet, Copenhagen, Denmark;<br />
4 Department <strong>of</strong> Pathology, Henry Ford Health System, Detroit, Michigan, USA<br />
Presenting author e-mail: pa@mb.au.dk<br />
It has been proposed that binding <strong>of</strong> PAI-1 to native vitronectin induces a reorganisation <strong>of</strong><br />
vitronectin from a closed to an open conformation allowing assembly <strong>of</strong> vitronectin oligomers<br />
with changed cell <strong>and</strong> matrix binding functions. In order to elucidate early molecular events<br />
during interactions between PAI-1 <strong>and</strong> vitronectin, we have applied a robust strategy that<br />
combines protein engineering, fluorescence spectroscopy <strong>and</strong> rapid reaction kinetics. Fluorescence<br />
stopped-flow experiments indicated a fast, concentration dependent, biphasic binding <strong>of</strong> PAI-<br />
1 to native monomeric vitronectin, but a monophasic association with vitronectins N-terminal<br />
somatomedin B domain (SMB), suggesting that multiple phases <strong>of</strong> the binding interaction<br />
occur only when full-length vitronectin is present. Nonetheless, in all cases, the initial fast<br />
interaction was followed by slower fluorescence changes, which we, by the use <strong>of</strong> an engineered,<br />
fluorescently silent PAI-1 with non-natural amino acids, demonstrated to be caused by reciprocal<br />
structural changes within the PAI-1 structure as well as in native vitronectin. Furthermore,<br />
measuring the effect <strong>of</strong> vitronectin on the rate <strong>of</strong> insertion <strong>of</strong> the reactive centre loop into b-sheet A<br />
<strong>of</strong> PAI-1 during reaction with target proteases by the use <strong>of</strong> fluorescently labelled PAI-1 variants,<br />
we observed that both full-length vitronectin <strong>and</strong> SMB had protease-specific effects on the rate<br />
<strong>of</strong> loop insertion, but that the two had clearly different effects. We interpret these results as<br />
support for a model <strong>of</strong> PAI-1-vitronectin binding in which there is an extended interaction surface<br />
implicating parts <strong>of</strong> vitronectin other than the somatomedin B domain.<br />
66 X I t h I n t e r n a t i o n a l W o r k s h o p o n
i055i<br />
Intact (non-cleavable) Cell-surface u-PAR Accelerates<br />
Clearance <strong>of</strong> tcu-PA:PAI-1:u-PAR Complexes <strong>and</strong> Subsequent<br />
Re-surfacing <strong>of</strong> Intact <strong>and</strong> Functional u-PAR<br />
Nieves-Li EC* <strong>and</strong> Manch<strong>and</strong>a N<br />
Department <strong>of</strong> Biochemistry <strong>and</strong> Internal Medicine, University <strong>of</strong> Illinois at Urbana-Champaign,<br />
Urbana, Illinois, USA<br />
Presenting author e-mail: enieves@uiuc.edu<br />
Urokinase plasminogen activator receptor (u-PAR) has been well-defined as a promoter <strong>of</strong><br />
plasminogen activation <strong>and</strong> modulates several cellular processes such as adhesion, proliferation,<br />
<strong>and</strong> migration. U-PAR has been shown to be susceptible to proteolytic cleavage by several<br />
proteases, one <strong>of</strong> them being its lig<strong>and</strong> two-chain u-PA (tcu-PA). This dissociates D1 from<br />
the rest <strong>of</strong> the anchored receptor <strong>and</strong> leads to loss <strong>of</strong> lig<strong>and</strong> binding. However, exposure <strong>of</strong><br />
the chemotactic epitope after D1 removal gives u-PAR a new role in signaling <strong>and</strong> migration.<br />
We found that cell-surface plasminogen activation is impaired upon D1 removal. We have<br />
investigated the role <strong>of</strong> receptor cleavage in the regulation <strong>of</strong> cell-surface plaminogen activation.<br />
We engineered <strong>and</strong> expressed wt u-PAR as well as tcu-PA cleavage resistant u-PAR (tcr-uPAR)<br />
in HEK293 cells. Using three different approaches to follow u-PAR internalization <strong>and</strong> recycling,<br />
i.e. biotin labeled receptor, biotin-labeled tcu-PA-PAI-1 complexes, <strong>and</strong> assays for plasminogen<br />
activation, we found that intact receptor better promotes the internalization <strong>of</strong> cell-surface u-<br />
PAR:u-PA-PAI-1 complexes <strong>and</strong> promotes subsequent re-surfacing <strong>of</strong> unoccupied <strong>and</strong> functional<br />
receptor. We hypothesize that intact cell-surface u-PAR may accelerate removal <strong>of</strong> inhibited<br />
tcu-PA from the cell-surface environment <strong>and</strong> that its re-expression may promote cell-surface<br />
plasminogen activation.<br />
<strong>Molecular</strong> & <strong>Cellular</strong> <strong>Biology</strong> <strong>of</strong> <strong>Plasminogen</strong> <strong>Activation</strong> 67
i056i<br />
The Central b-sheet <strong>of</strong> PAI-1 Demonstrates<br />
Two Dynamically Distinct Regions<br />
Li S* 1 , Lawrence DA 2 , Schwartz BS 1,3<br />
1 Department <strong>of</strong> Biochemistry, University <strong>of</strong> Illinois at Urbana-Chanpaign, Urbana, Illinois, USA;<br />
2 Department <strong>of</strong> Internal Medicine, University <strong>of</strong> Michigan Medical School, Ann Arbor, Michigan, USA;<br />
3 Department <strong>of</strong> Medicine, University <strong>of</strong> Illinois at Urbana-Champaign, Urbana, Illinois, USA<br />
Presenting author e-mail: SLI3@uiuc.edu<br />
PAI-1 is an inhibitory serpin that can spontaneously transit with a half-life <strong>of</strong> 1-2 hours at 37°C<br />
to a latent form whereby the RCL is intact but fully inserted into b-sheet A. The labile nature <strong>of</strong><br />
native PAI-1 is thought to be due to the ability <strong>of</strong> its central sheet to exist in equilibrium between<br />
open <strong>and</strong> closed conformations. The stable variant, 14-1B, contains 4 amino acid substitutions that<br />
convey a 70-fold enhancement in the inhibitory half-life compared to wild-type PAI-1 (wtPAI-<br />
1). X-ray crystal structures <strong>of</strong> latent PAI-1 <strong>and</strong> active 14-1B suggest that some <strong>of</strong> the mutations<br />
in the stable variant keep b-sheet A closed, preventing incorporation <strong>of</strong> the RCL. We tested this<br />
hypothesis using RCL-mimicking peptides, which have been shown to insert into b-sheet A<br />
as s4A. We found that 14-1B is less susceptible than wtPAI-1 to inactivation by such peptides.<br />
The PAI-1 c<strong>of</strong>actor, vitronectin (Vn), did not affect the binding <strong>of</strong> a pentamer, Ac-TVASS, to<br />
14-1B, yet enhanced the binding <strong>of</strong> an octamer, Ac-TVASSSTA. The binding <strong>of</strong> Vn to wtPAI-1<br />
modestly delays the transition to latency. Yet we found that that Vn did not protect wtPAI-1<br />
from inactivation by the peptides, rather slightly enhancing such inactivation. These results are<br />
inconsistent with the currently held model on how active PAI-1 is stabilized by its physiologic<br />
c<strong>of</strong>actor. We propose that sheet A breathes in a pigeon-toed fashion in which the region<br />
underneath a-helix F remains closed <strong>and</strong> the region near the RCL is dynamic.<br />
68 X I t h I n t e r n a t i o n a l W o r k s h o p o n
i057i<br />
Regulation <strong>of</strong> Cancer-Cell Plasmin Generation by<br />
Annexin A2-S100A10 Heterotetramer (AIIt)<br />
Waisman DM*<br />
Department <strong>of</strong> Biochemistry <strong>and</strong> <strong>Molecular</strong> <strong>Biology</strong>, Dalhousie University, Halifax, Nova Scotia,<br />
Canada<br />
Presenting author e-mail: david.waisman@dal.ca<br />
Many findings over several decades strongly suggest an important role for the plasminogen<br />
activation system in cancer cell invasion <strong>and</strong> metastasis. We have investigated the role <strong>of</strong> the<br />
S100A10, annexin A2 <strong>and</strong> the heterotetrameric complex formed by these subunits (AIIt) in<br />
plasminogen regulation. Surface plasmon resonance studies established that S100A10 bound<br />
directly to tPA, plasminogen <strong>and</strong> plasmin whereas the annexin A2 bound only plasmin. AIIt <strong>and</strong><br />
S100A10, but not annexin A2, dramatically stimulated the plasminogen activator-dependent<br />
conversion <strong>of</strong> plasminogen to plasmin in vitro. Immun<strong>of</strong>luorescence microscopy demonstrated<br />
the colocalization <strong>of</strong> S100A10 with the uPA/uPAR complex. We have also utilized both antisense<br />
<strong>and</strong> siRNA methodologies to knockdown S100A10. Loss <strong>of</strong> extracellular S100A10 resulted in a<br />
70-90% loss in cellular plasmin generation. Under these conditions the levels <strong>of</strong> annexin A2 were<br />
unchanged. The S100A10 knockdown cells were also less invasive <strong>and</strong> showed a dramatic loss in<br />
tumor formation <strong>and</strong> metastatic potential. We also observed that the addition <strong>of</strong> plasminogen to<br />
cancer cells resulted in the oxidation <strong>of</strong> annexin A2 <strong>and</strong> S100A10. AIIt stimulated autoproteolysis<br />
<strong>of</strong> the plasmin Lys468-Gly469 bond <strong>and</strong> also catalyzed the reduction <strong>of</strong> the plasmin<br />
Cys462Cys541disulfide. These two reactions resulted in the release <strong>of</strong> angiostatin (Lys78-Lys468)<br />
from plasmin. However, oxidation <strong>of</strong> annexin A2 was not observed after knockdown <strong>of</strong> S100A10.<br />
Thus, AIIt acts as a plasmin reductase, catalyzing the release <strong>of</strong> angiostatin from plasmin. Results<br />
form these studies have established that S100A10 is a key regulatory protein <strong>of</strong> cell surface<br />
plasmin <strong>and</strong> angiostatin generation. Funded by the CIHR <strong>and</strong> NCIC.<br />
<strong>Molecular</strong> & <strong>Cellular</strong> <strong>Biology</strong> <strong>of</strong> <strong>Plasminogen</strong> <strong>Activation</strong> 69
i058i<br />
<strong>Plasminogen</strong> Activator Inhibitor Type 2 Binds to S100A10 in<br />
Annexin 2 Heterotetramer <strong>and</strong> Prevents Annexin 2-dependent<br />
Plasmin In-site Formation by Inhibiting tPA<br />
Lobov S*, Croucher D, Ranson M<br />
School <strong>of</strong> Biological Sciences, University <strong>of</strong> Wollongong, NSW, Australia<br />
Presenting author e-mail: sergei@uow.edu.au<br />
<strong>Plasminogen</strong> Activator Inhibitor type 2 is a well known member <strong>of</strong> the serpin superfamily.<br />
Extracellular PAI-2 efficiently inhibits uPA <strong>and</strong> tPA in solution but there seem to be no<br />
physiological role for PAI-2 as tPA inhibitor. Interestingly however, PAI-2 as well as tPA <strong>and</strong><br />
plasminogen are capable <strong>of</strong> binding to annexin 2 heterotetramer (AIIt). AIIt acts as a receptor<br />
for tPA <strong>and</strong> plasminogen on the cell surface thereby promoting tPA-dependent plasmin in-site<br />
formation. The fact that PAI-2 is capable <strong>of</strong> binding to AIIt is known for more then a decade.<br />
However, neither the mechanism nor the physiological outcomes <strong>of</strong> the binding are known.<br />
Here we show that PAI-2 binds to AIIt via the S100A10 subunit <strong>and</strong> that the CD-loop <strong>of</strong> PAI-2<br />
plays a minor role in the binding. Furthermore, the interaction <strong>of</strong> PAI-2 with AIIt, unlike tPA <strong>and</strong><br />
plasminogen, is AIIt C-terminal lysine independent, which might involve novel binding sites in<br />
S100A10 <strong>and</strong> AIIt. In spite <strong>of</strong> seemingly different sites <strong>of</strong> binding to AIIt, PAI-2 <strong>and</strong> plasminogen<br />
could not simultaneously bind to AIIt. Furthermore, simultaneous binding <strong>of</strong> PAI-2 <strong>and</strong> tPA<br />
seemed to be able to exist only for the PAI-2/tPA complex. Enzyme kinetic analyses confirmed<br />
that PAI-2 inhibits AIIt-bound tPA in vitro <strong>and</strong> thus prevents plasmin in-site formation. We<br />
conclude that there is a complex relationship between PAI-2/plasminogen/tPA when AIIt is<br />
present. We propose that extracellular PAI-2 may have an important physiological role as a tPA<br />
inhibitor on the cell surface.<br />
70 X I t h I n t e r n a t i o n a l W o r k s h o p o n
i059i<br />
Underst<strong>and</strong>ing the Structural Basis <strong>of</strong> the Differential-Receptor-<br />
Mediated Endocytosis Mechanisms <strong>of</strong> PAI-1 <strong>and</strong> PAI-2 in Cancer<br />
Cochran BJ* 1 , Lobov S 1 , Croucher D 2 , Ranson M 1<br />
1 Cancer Research Laboratory, School <strong>of</strong> Biological Sciences, University <strong>of</strong> Wollongong, Australia;<br />
2 Cancer Research Program, Garvan Institute <strong>of</strong> Medical Research, Australia<br />
Presenting author e-mail: blake@uow.edu.au<br />
The urokinase-type plasminogen activator (uPA) <strong>and</strong> its inhibitors, plasminogen activator<br />
inhibitor type-1 (PAI-1) <strong>and</strong> type-2 (PAI-2) play an important role in the progression <strong>of</strong> a number<br />
<strong>of</strong> forms <strong>of</strong> cancer. Whilst both PAI-1 <strong>and</strong> PAI-2 clear uPA activity from the cell surface through<br />
irreversible complex formation, uPA:PAI-1 initiates cell signalling events most likely associated<br />
with poor cancer prognosis. This activation is dependent on interactions between PAI-1 <strong>and</strong><br />
the very low density lipoprotein receptor (VLDLr). Upon internalisation, uPA:PAI-2 does not<br />
activate these cell signalling pathways, possibly accounting for the association between PAI-2<br />
expression <strong>and</strong> good prognosis in some cancer types. The mechanisms underlying this differential<br />
functionality are poorly understood <strong>and</strong> is believed to be due to the absence <strong>of</strong> LDLR binding<br />
sites in the PAI-2 moiety <strong>of</strong> the uPA:PAI-2 complex.<br />
This study aims to reconstitute the LDLR binding ability <strong>of</strong> PAI-1 in PAI-2 via the replacement<br />
<strong>of</strong> structural elements <strong>and</strong> residues <strong>of</strong> PAI-2 with those corresponding to PAI-1. To date, we<br />
have constructed an ahelix D domain swap which retained uPA inhibitory activity. We intend<br />
to compare the LDLR binding characteristics <strong>of</strong> this protein chimera to PAI-1. The findings <strong>of</strong><br />
this research may help explain the underlying reasons for the distinct biological roles <strong>of</strong> PAI-1<br />
<strong>and</strong> PAI-2 in cancer. A more complete underst<strong>and</strong>ing <strong>of</strong> the biological roles <strong>of</strong> PAI-2 will provide<br />
important information relating to the function <strong>of</strong> the plasminogen activation system in cancer <strong>and</strong><br />
may aid in the continuing development <strong>of</strong> highly specific <strong>and</strong> effective anti-uPA treatments.<br />
<strong>Molecular</strong> & <strong>Cellular</strong> <strong>Biology</strong> <strong>of</strong> <strong>Plasminogen</strong> <strong>Activation</strong> 71
i060i<br />
A Low-glycemic-index Diet Reduces Plasma PAI-1 Activity<br />
in Overweight Women<br />
Jensen L* 1 , Krog-Mikkelsen I 2 , Sloth B 2 , Flint A 2 , Astrup A 2 , Raben A 2 , Tholstrup T 2 , Brünner N 1<br />
1 Department <strong>of</strong> Veterinary Pathobiology, 2 Department <strong>of</strong> Human Nutrition, Centre for Advanced Food<br />
Studies, Faculty <strong>of</strong> Life Sciences, University <strong>of</strong> Copenhagen, Frederiksberg, Denmark<br />
Presenting author e-mail: lje@life.ku.dk<br />
An elevated level <strong>of</strong> plasminogen activator inhibitor-1 (PAI-1) in plasma is a core feature <strong>of</strong> the<br />
metabolic syndrome. PAI-1 has been shown to decrease during weight loss. However, effects <strong>of</strong><br />
healthy diets on PAI-1 levels may not solely depend on weight loss. The relevance <strong>of</strong> glycemic<br />
index in preventing the metabolic syndrome is controversial.<br />
The purpose <strong>of</strong> the present study was to investigate the effect <strong>of</strong> 10 weeks intake <strong>of</strong> a low<br />
glycemic index (LGI) vs. a high glycemic index (HGI) high-carbohydrate, low fat ad libitum diet<br />
on plasma PAI-1 activity <strong>and</strong> antigen levels in overweight women.<br />
44 healthy overweight women (BMI 27.5 ± 0.2 kg/m2) were r<strong>and</strong>omly assigned to a parallel 10<br />
week intervention with a LGI (n=22) or HGI (n=22) diet. To study the postpr<strong>and</strong>ial effect <strong>of</strong> LGI<br />
vs. HGI diets a subgroup <strong>of</strong> 29 subjects (LGI, n=14; HGI n=15) were assigned to participate in an<br />
additional 4-h meal test on the last day <strong>of</strong> the intervention. Fasting blood samples were obtained<br />
before <strong>and</strong> after the 10 weeks, <strong>and</strong> postpr<strong>and</strong>ially at 10 weeks.<br />
PAI-1 activity in plasma decreased (P = 0.02) after the LGI diet, a decrease that was significantly<br />
different (P < 0.01) from the change after a HGI diet. Changes in PAI-1 antigen levels were<br />
not significantly different between any groups. Postpr<strong>and</strong>ial PAI-1 concentrations showed no<br />
significant differences between groups.<br />
A LGI diet reduces plasma PAI-1 activity, suggesting that a beneficial role <strong>of</strong> a LGI diet in<br />
overweight adults could be related to PAI-1.<br />
72 X I t h I n t e r n a t i o n a l W o r k s h o p o n
i061i<br />
Urokinase Receptor-independent Signalling <strong>of</strong> the Urokinase-type<br />
<strong>Plasminogen</strong> Activator via Phosporylation <strong>of</strong> STAT1<br />
Ehart M* <strong>and</strong> Binder BR<br />
Department <strong>of</strong> Vascular <strong>Biology</strong> <strong>and</strong> Thrombosis Research, Medical University <strong>of</strong> Vienna, Austria<br />
Presenting author e-mail: monika.ehart@meduniwien.ac.at<br />
Phosphorylation <strong>of</strong> STAT-proteins is one possible way <strong>of</strong> signalling induced by the urokinase-<br />
type plasminogen activator (uPA). We analyzed the dependency <strong>of</strong> STAT1 phosphorylation on the<br />
presence <strong>of</strong> the urokinase receptor in mouse skin fibroblasts. We found that human uPA, which<br />
is assumed not to bind to the mouse urokinase receptor, induces STAT1 phosphorylation. Much<br />
to our surprise this phosphorylation was induced only in cells derived from urokinase receptor<br />
knock out mice, but not in cells derived from wild type mice. Since we <strong>and</strong> others have shown<br />
that gp130 is involved in uPA induced STAT signalling, we analyzed association <strong>of</strong> uPA with<br />
gp130. We could precipitate gp130 together with uPA from cells derived from urokinase receptor<br />
knock out mice but not from cells derived from wild type mice. We further analyzed urokinase<br />
receptor independent uPA signalling in the human kidney epithelial cell line HEK-293 <strong>and</strong> the<br />
human adenocarcinoma cell line MCF-7 <strong>and</strong> obtained data supporting the notion that gp130<br />
transuces uPA signals only in the absence <strong>of</strong> urokinase receptor.<br />
<strong>Molecular</strong> & <strong>Cellular</strong> <strong>Biology</strong> <strong>of</strong> <strong>Plasminogen</strong> <strong>Activation</strong> 73
i062i<br />
Urokinase Receptor Promotes Neo-Angiogenesis through<br />
its Ser88-Arg-Ser-Arg-Tyr92 Chemotactic Sequence<br />
Longanesi-Cattani I* 1 , Bifulco K 1 , Cantelmo AR 1 , Di Carluccio G 1 , Spina R 1 , Liguori E 1 , Stoppelli MP 2 ,<br />
Carriero MV 1<br />
1 Department <strong>of</strong> Experimental Oncology, National Cancer Institute <strong>of</strong> Naples, Italy;<br />
2 Institute <strong>of</strong> Genetics <strong>and</strong> Biophysics ‘’Adriano Buzzati-Traverso,’ Naples, Italy<br />
*Presenting author e-mail: immalonganesi@libero.it<br />
Angiogenesis is a highly coordinated process required for normal development, in response<br />
to injury <strong>and</strong> for tumor growth. This process is sustained by a tightly regulated motility <strong>of</strong><br />
endothelial cells. Angiogenesis is regulated by chemotactic stimuli <strong>and</strong> requires the activation <strong>of</strong><br />
several signalling pathways that converge on cytoskeletal remodelling. The Ser88-Arg-Ser-Arg-<br />
Tyr92 chemotactic sequence <strong>of</strong> the urokinase receptor binds to formyl peptide receptor-like-1<br />
(FPRL-1), a G protein-coupled cell receptor (Resnati et al. 2002). Furthermore, we have found<br />
that the Ser-Arg-Ser-Arg-Tyr (SRSRY) peptide binds to the high affinity formyl peptide receptor<br />
(FPR), <strong>and</strong> specifically promotes cytoskeletal rearrangements <strong>and</strong> directional cell migration in<br />
a vitronectin receptor-dependent manner (Gargiulo et al. 2005). Since Human Umbelical Vein<br />
Endothelial Cells (HUVEC) express FPRL-1 as well as avb3 vitronectin receptors, we investigated<br />
on the possibility that SRSRY may triggers neo-angiogenesis. By conventional Boyden chamber<br />
assays, we found that SRSRY promotes directional cell migration <strong>of</strong> HUVEC in a dose-dependent<br />
manner, with an extent similar to VEGF. Maximal chemotactic effect is reached at 10 nM<br />
SRSRY concentration. In a tube-formation assay, SRSRY shows a remarkable ability to promote<br />
angiogenesis <strong>of</strong> endothelial cells. According to cell migration data, pro-angiogenic effect is dosedependent<br />
<strong>and</strong> peaks at 10 nM SRSRY. Both endothelial cell migration <strong>and</strong> in vitro angiogenesis<br />
promoted by SRSRY are inhibited by cell pre-incubation with blocking anti-avb3 monoclonal<br />
antibodies, indicating that SRSRY exhibits an avb3-dependent pro-angiogenetic effect. Although<br />
preliminary, these data suggest the development <strong>of</strong> SRSRY-derived pharmacological compounds<br />
to be employed in tissue repairing <strong>and</strong> cardiovascular diseases.<br />
74 X I t h I n t e r n a t i o n a l W o r k s h o p o n
i063i<br />
The Density Enhanced Phosphatase 1 (DEP-1) Down-Modulates<br />
Urokinase Receptor (uPAR) Surface Expression in Confluent<br />
Endothelial Cells<br />
Brunner PM* 1 , Heier PC 1 , Prager GW 1,2 , Mihaly J 1 , Priglinger U 3 , Binder BR 1<br />
1Department <strong>of</strong> Vascular <strong>Biology</strong> <strong>and</strong> Thrombosis Research, Center for Biomolecular Medicine <strong>and</strong><br />
Pharmacology, Medical University Vienna, Austria;<br />
2 Clinical Division <strong>of</strong> Oncology, Department <strong>of</strong> Medicine I, Medical University Vienna, Austria;<br />
3 Department <strong>of</strong> Emergency Medicine, Medical University Vienna, Austria<br />
Presenting author e-mail: patricia.heier@univie.ac.at<br />
It is known that a proteolytic machinery is indispensable for ordered endothelial cell migration<br />
<strong>and</strong> tissue invasion. Such machinery is largely provided by the prourokinase-urokinase-plasmin<br />
system. Endothelial cells (ECs) in vessels are forming a confluent layer that can be mimicked<br />
by confluent ECs in cell culture. Compared to sparse cultures we could show that the surface<br />
expression <strong>of</strong> uPAR is decreased by 40%. To examine the cause <strong>of</strong> this decrease we investigated<br />
the MAP-Kinase-pathway being the major regulatory system for uPAR-expression.<br />
We found that between sparse (50,000 cells/cm2), subconfluent (100,000 cells/cm2) <strong>and</strong> confluent<br />
cells (150,000 cells/cm2) there was no change in ERK1/2 expression or its phosphorylation.<br />
Therefore we analyzed phosphatases as possible c<strong>and</strong>idates for density dependent uPARexpression.<br />
While Dual-Specificity Phosphatase 1 (DUSP1) was not <strong>and</strong> DUSP4 was only<br />
borderline upregulated with density, Density Enhanced Phosphatase 1 (DEP-1) significantly<br />
increased with cell density. Transfection <strong>of</strong> ECs with expression plasmids for wild-type<br />
<strong>and</strong> mutated forms <strong>of</strong> DEP-1 revealed that wild-type DEP-1 but not forms mutated in the<br />
phosphatase-domain decreased uPAR-mRNA <strong>and</strong> cell surface expression. To analyse in detail<br />
how DEP-1 interferes with uPAR-expression we applied reporter assays using plasmids encoding<br />
ERK1 <strong>and</strong> different DEP-1 forms. We found that DEP-1 influenced the MAP-Kinase pathway<br />
downstream <strong>of</strong> ERK1/2 in addition to its tyrosine kinase dephosphorylating activity. From this<br />
data we conclude that the quiescent state <strong>of</strong> contact inhibited ECs is at least partially mediated by<br />
DEP-1 (<strong>and</strong> possibly also by DUSP4) that inhibits the MAP-Kinase pathway also downstream <strong>of</strong><br />
ERK1/2.<br />
<strong>Molecular</strong> & <strong>Cellular</strong> <strong>Biology</strong> <strong>of</strong> <strong>Plasminogen</strong> <strong>Activation</strong> 75
i064i<br />
Detection <strong>and</strong> Prevention <strong>of</strong> Hepatic Fibrosis Targeting<br />
Proteolytic TGF-b <strong>Activation</strong> Reaction<br />
Kojima S*<br />
<strong>Molecular</strong> <strong>Cellular</strong> Pathology Research Unit, RIKEN, Japan<br />
Presenting author e-mail: skojima@postman.riken.go.jp<br />
Transforming growth factor (TGF)-b, the most fibrogenic cytokine participating in the<br />
pathogenesis <strong>of</strong> liver diseases, is produced as a high molecular weight latent form, <strong>and</strong> thus must<br />
be activated before exerting its biological activities. TGF-b activation is the reaction, by which 25<br />
kD active TGF-b molecule is released from the latent complex. We showed that TGF-b is activated<br />
by plasmin (PLN) <strong>and</strong> plasma kallikrein (PLK) during pathogenesis <strong>of</strong> liver fibrosis <strong>and</strong> impaired<br />
liver regeneration, respectively, <strong>and</strong> that blockage <strong>of</strong> these activation reactions with low molecular<br />
weight protease inhibitors prevented the development <strong>of</strong> the diseases in animal models.<br />
PLN <strong>and</strong> PLK cleaved between K56-L57 <strong>and</strong> R58-L59 in LAP portion <strong>of</strong> human latent TGF-b1,<br />
respectively. We produced antibodies that specifically recognize the neo-epitopes formed by<br />
protease degradation, namely the cut ends <strong>of</strong> each cleavage site. The anti-R58 antibodies strongly<br />
stained liver sections from patients with fulminant hepatitis compared to normal liver sections<br />
from patients that died from pulmonary embolism. On the other h<strong>and</strong>, the anti-L59 antibodies<br />
were successively used to establish ELISA to detect LAP degradation fragments in mouse serum.<br />
These results suggest a key role for PLN/PLK in the generation <strong>of</strong> active TGF-b, namely that a<br />
PLN/PLK-dependent activation reaction occurs around hepatic stellate cells to produce active<br />
TGF-b, which may induce fibrosis <strong>and</strong> inhibit the proliferation <strong>of</strong> hepatocytes, thereby addressing<br />
a potential use for PLN/PLK inhibitors in hepatitis therapy. These results also suggest a potential<br />
usage <strong>of</strong> a LAP degradate as a biomarker for liver fibrosis.<br />
76 X I t h I n t e r n a t i o n a l W o r k s h o p o n
i065i<br />
Domain 1 <strong>of</strong> uPAR Is Required for its Morphological<br />
<strong>and</strong> Functional b2 Integrin-mediated Connection with<br />
Actin Cytoskeleton in Human Endothelial Cells<br />
Del Rosso M* 1 , Fibbi G 1 , Margheri F 1 , Serratì S 1 , Pucci M 1 , Manetti M 2 , Ibba-Manneschi L 2<br />
1 Department <strong>of</strong> Experimental Pathology <strong>and</strong> Oncology, University <strong>of</strong> Florence, Italy;<br />
2 Department <strong>of</strong> Anatomy, Histology <strong>and</strong> Forensic Medicine, University <strong>of</strong> Florence, Italy<br />
Presenting author e-mail: delrosso@unifi.it<br />
We have previously shown that MMP12-dependent cleavage <strong>of</strong> uPAR domain 1 blocks<br />
angiogenesis in Systemic Sclerosis (SSc) endothelial cell. Since integrin association accounts<br />
for uPAR invasion required in angiogenesis, this study was undertaken to show whether fullsize<br />
<strong>and</strong> truncated uPAR differentially associated to integrins <strong>and</strong> with motor components<br />
<strong>of</strong> the cytoskeleton. Truncated <strong>and</strong> full-size uPAR <strong>and</strong> its association with integrins <strong>and</strong> actin<br />
cytoskeleton in SSc <strong>and</strong> normal (N) microvascular endothelial cells (MVEC), isolated from skin<br />
biopsies, were studied by Confocal Laser Scanning Microscopy <strong>and</strong> immuno-precipitation.<br />
Integrin composition <strong>of</strong> endothelial cells was studied by RT-PCR. Cell migration <strong>and</strong> capillary<br />
morphogenesis were studied on fibrin(ogen) substrates. Involvement <strong>of</strong> Rac <strong>and</strong> Cdc42 was<br />
showed by Western blot.<br />
Only full-size uPAR is connected with actin cytoskeleton in endothelial cells. Such connection<br />
is mediated by uPAR-associated alphaM-beta2 <strong>and</strong> alphaX-beta2 integrins <strong>and</strong> is absent in<br />
endothelial cells <strong>of</strong> SSc patients. The cleaved receptor does not associate with beta2 integrins<br />
<strong>and</strong> with actin. Beta3 integrins associated with both full-size <strong>and</strong> cleaved uPAR at focal contacts.<br />
uPAR-beta2 integrins uncoupling in N-MVEC impaired activation <strong>of</strong> Rac <strong>and</strong> Cdc42, which<br />
mediate uPAR-dependent cytoskeletal rearrangements <strong>and</strong> cell motility, as well as integrin<br />
engagement-delivered signals to actin cytoskeleton. Invasion <strong>and</strong> capillary morphogenesis on<br />
fibrin(ogen)-coated substrates indicated that uPAR ligation by uPA empowers beta2 <strong>and</strong> beta3<br />
integrin-dependent fibrin(ogen) invasion <strong>and</strong> that such system is impaired in SSc endothelial cell.<br />
Conclusions. uPAR truncation <strong>and</strong> the following loss <strong>of</strong> beta2 integrin-mediated uPAR connection<br />
with actin cytoskeleton account for reduced angiogenic properties <strong>of</strong> SSc endothelial cells.<br />
<strong>Molecular</strong> & <strong>Cellular</strong> <strong>Biology</strong> <strong>of</strong> <strong>Plasminogen</strong> <strong>Activation</strong> 77
i066i<br />
The uPA/uPAR/Vn Pathway <strong>of</strong> Signaling to MAPK-activation<br />
Sarra Ferraris GM* 1 , Madsen C 1 , Sidenius N 1,2<br />
1 IFOM Foundation, FIRC Institute <strong>of</strong> <strong>Molecular</strong> Oncology, Milan Italy;<br />
2 <strong>Molecular</strong> Genetics Unit, DIBIT, Università Vita-Salute San Raffaele, Milan Italy<br />
Presenting author e-mail: gianmaria.sarraferraris@ifom-ieo-campus.it<br />
The urokinase-type plasminogen activator receptor (uPA(R)), despite the lack <strong>of</strong> a transmembrane<br />
domain, behaves as a signaling molecule resulting in increased ERK1/2-activation when<br />
overexpressed or upon uPA-binding. In accordance, we find that CHO <strong>and</strong> 293 cells overexpressing<br />
uPAR display increased basal ERK1/2-activation.<br />
Two different alanine substitution in uPAR (W32A <strong>and</strong> T54A), which impair Vn-binding, both<br />
failed to cause increased basal ERK1/2-activation. The addition <strong>of</strong> uPA to cells expressing the<br />
T54A receptor induced rapid binding to vitronectin <strong>and</strong> ERK1/2 activation, while uPA binding<br />
to cells expressing the W32A mutant failed to induce both vitronectin binding <strong>and</strong> ERK1/2<br />
activation. Both mutants bind uPA equally well <strong>and</strong> these data thus allow us to conclude<br />
that uPA-induced ERK1/2 activation is mediated by the induction <strong>of</strong> the uPAR/vitronectininteraction.<br />
Using cells expressing theT54A receptor we compared the kinetics <strong>of</strong> uPAR/Vn-induced ERK1/2<br />
activation with the ones triggered by other signalling receptors.<br />
uPA <strong>and</strong> LPA treatments caused a sustained ERK1/2 activation while EGF an Mn2+ displayed a<br />
peek at 5 minutes followed by a rapid decrease <strong>of</strong> phosphorylated ERK1/2 levels.<br />
Moreover EGF receptor inhibitors, LPA1 receptor inhibitor <strong>and</strong> Pertussis Toxin did not affect uPAuPAR<br />
signalling pathway while PI3 kinase inhibitors decreased partially but significantly ERK1/2<br />
activation in response to uPA <strong>and</strong> LPA.<br />
These data underline the importance <strong>of</strong> Vn binding in the uPA-uPAR signalling, suggesting a new<br />
way, which is independent <strong>of</strong> the EGFR <strong>and</strong> pertussis toxin sensitive GPCR’s, by which uPAR<br />
may signal to ERK1/2.<br />
78 X I t h I n t e r n a t i o n a l W o r k s h o p o n
i067i<br />
Regulation <strong>of</strong> tPA <strong>and</strong> PAI-1 Gene Expression in Astrocytes<br />
Hultman K* 1 , Tjärnlund-Wolf A 1 , Blomstr<strong>and</strong> F 1 , Nilsson M 1 , Medcalf R 2 , Jern C 1<br />
1 Institute <strong>of</strong> Neuroscience <strong>and</strong> Physiology, the Sahlgrenska Academy at Göteborg University, Sweden;<br />
2 Australian Centre for Blood Diseases, Monash University, Alfred Medical Research <strong>and</strong> Education<br />
Precinct (AMREP), Australia<br />
Presenting author e-mail: karin.hultman@neuro.gu.se<br />
We have shown that PKC activation acts in synergy with retinoic acid (RA) to induce tissue-type<br />
plasminogen activator (tPA) gene expression in human endothelial cells. The aim <strong>of</strong> the present<br />
study was to investigate whether tPA is regulated in a similar manner in astrocytes, as well as to<br />
characterize plasminogen activator inhibitor type 1 (PAI-1) gene expression in these cells.<br />
Native human astrocytes were treated with RA, PKC activator (PMA), PKA activator (forskolin),<br />
cytokines or growth factors for 3, 6, 14 <strong>and</strong> 20 hours. RA or PMA alone induced a 3-fold upregulation<br />
<strong>of</strong> tPA at 20 hours. Combined treatment resulted in a 9-fold induction <strong>and</strong> increased<br />
intracellular storage pools <strong>of</strong> tPA as visualized by immunocytochemistry. Pretreatment with<br />
actinomycin D or cycloheximide completely blocked both RA <strong>and</strong> PMA mediated tPA mRNA<br />
increase. Cytokines <strong>and</strong> growth factors caused a general weak up-regulation <strong>of</strong> tPA <strong>and</strong> PAI-1 at<br />
3 <strong>and</strong> 6 hours followed by a slight down-regulation at 20 hours. Forskolin induced a strong timedependent<br />
down-regulation <strong>of</strong> both proteins. For all treatments, similar inductions were observed<br />
at the mRNA (RT-PCR) <strong>and</strong> protein level (ELISA).<br />
We show for the first time that in astrocytes, RA <strong>and</strong> PKC activation induce a strong up-regulation<br />
<strong>of</strong> tPA gene expression <strong>and</strong> that this response is dependent on both gene transcription <strong>and</strong> de<br />
novo protein synthesis. As we <strong>and</strong> others have identified functional variants in the tPA <strong>and</strong> PAI-1<br />
promoters, we will now proceed by investigating whether there is an allele-specific regulation in<br />
human astrocytes.<br />
<strong>Molecular</strong> & <strong>Cellular</strong> <strong>Biology</strong> <strong>of</strong> <strong>Plasminogen</strong> <strong>Activation</strong> 79
i068i<br />
Identification <strong>of</strong> a Mitotic Epitope in the Domain 2 <strong>of</strong> the<br />
Urokinase Receptor (uPAR)<br />
Degryse B* 1 , Eden G 2 , Arnaudova R 1 , Furlan F 1 , Blasi F 1,2<br />
1Department <strong>of</strong> <strong>Molecular</strong> <strong>Biology</strong> <strong>and</strong> Functional Genomics, DIBIT, University Vita Salute San<br />
Raffaele, Milan, Italy;<br />
2 IFOM, FIRC Institute <strong>of</strong> <strong>Molecular</strong> Oncology, Milan, Italy<br />
Presenting author e-mail: degryse.bernard@hsr.it<br />
The first characterized chemotactic sequence <strong>of</strong> uPAR (SRSRY) is located in the linker region<br />
between domain 1 <strong>and</strong> 2. SRSRY peptide promotes cell migration through binding to receptors<br />
such as FPRL1. Recently, we identified in the domain 2 another chemotactic epitope that we<br />
named D2A, 130IQEGEEGRPKDDR142 (Degryse et al., 2005, J. Biol. Chem. 280, 24792-24803). D2A<br />
synthetic peptide dose-dependently stimulates cell migration with a maximum at 1 pM. We have<br />
also shown that D2A promotes cell migration through binding to avb3 <strong>and</strong> a5b1 integrins <strong>and</strong><br />
activation <strong>of</strong> integrin-dependent signaling.<br />
Since uPAR can regulate cell proliferation, we have started investigating the effects <strong>of</strong> D2A on<br />
cell growth. D2A stimulates cell growth in a dose-dependent manner in various cell types <strong>and</strong><br />
species, whereas a scrambled version <strong>of</strong> D2A has no effect. In rat smooth muscle cells, the optimal<br />
dose is 1-10 pM while in human HT29 <strong>and</strong> HT1080 cells it is 100 pM. These results demonstrate<br />
that D2A is a mitogen at doses that are slightly higher compared to the optimal dose required for<br />
chemotaxis.<br />
We have identified a mitotic/chemotactic epitope in the domain 2 <strong>of</strong> uPAR showing that this<br />
region is particularly important for uPAR-induced signaling. These data suggest that uPAR is a<br />
membrane-bound mitogen acting through binding to other membrane receptor(s).<br />
80 X I t h I n t e r n a t i o n a l W o r k s h o p o n
i069i<br />
Vitronectin Inhibits <strong>Plasminogen</strong> Activator Inhibitor-1<br />
(PAI-1)-Induced Chemotaxis by Blocking PAI-1<br />
Binding to the LDL Receptor-Related Protein<br />
Neels JG 1,2 , Kamikubo Y 1,3 , Degryse B* 1,4<br />
1Division <strong>of</strong> Vascular <strong>Biology</strong>, Department <strong>of</strong> Cell <strong>Biology</strong>, The Scripps Research Institute, La Jolla,<br />
California, USA;<br />
Present addresses:<br />
2 Department <strong>of</strong> Medicine, University <strong>of</strong> California San Diego, La Jolla, California, USA;<br />
3Department <strong>of</strong> <strong>Molecular</strong> <strong>and</strong> Experimental Medicine, The Scripps Research Institute, La Jolla,<br />
California, USA;<br />
4Department <strong>of</strong> <strong>Molecular</strong> <strong>Biology</strong> <strong>and</strong> Functional Genomics, DIBIT, University Vita-Salute San<br />
Raffaele, Milan, Italy<br />
Presenting author e-mail: degryse.bernard@hsr.it<br />
We have previously shown (Degryse et al., 2004, J. Biol. Chem. 279, 22595-22604) that PAI-1<br />
activates the Jak/Stat signaling pathway <strong>and</strong> stimulates cell migration by binding to the LDL<br />
receptor-related protein (LRP), a large endocytic receptor. Since vitronectin (VN) influences most<br />
<strong>of</strong> the biological functions <strong>of</strong> PAI-1, we explored the effects <strong>of</strong> VN on PAI-1-induced signaling <strong>and</strong><br />
cell migration. In fact, VN inhibits PAI-1-promoted signaling <strong>and</strong> chemotaxis. VN acts by binding<br />
to PAI-1 inhibiting the activation <strong>of</strong> the Jak/Stat pathway <strong>and</strong> cell migration. VN exerts these<br />
inhibitory effects by blocking PAI-1 binding to LRP, its motogenic receptor.<br />
We have unveiled a new inhibitory role <strong>of</strong> VN which has all the hallmarks <strong>of</strong> a molecule that can<br />
regulate every steps <strong>of</strong> the cell migration cycle by providing ‘’Stop’’ (under the form <strong>of</strong> VN/PAI-<br />
1 complex) <strong>and</strong> ‘’Go’’ signals to the cell. VN shares striking similarities with urokinase, which is<br />
the other main lig<strong>and</strong> <strong>of</strong> uPAR <strong>and</strong> can also generate ‘’Stop’’ <strong>and</strong> ‘’Go’’ signals. Furthermore, it is<br />
intriguing that urokinase <strong>and</strong> VN induce ‘’Stop’’ signals by creating uPA/PAI-1 <strong>and</strong> VN/PAI-1<br />
complexes that block uPAR-, integrin- <strong>and</strong> LRP-dependent cell migration.<br />
<strong>Molecular</strong> & <strong>Cellular</strong> <strong>Biology</strong> <strong>of</strong> <strong>Plasminogen</strong> <strong>Activation</strong> 81
i070i<br />
Estradiol Inhibits EGF-induced Cell Migration <strong>and</strong> uPAR Expression in<br />
Estrogen Receptor-a Negative, GPR30 Positive Ovarian Cancer Cells<br />
Henic E* 1 , Noskova V 1 , Høyer-Hansen G 2 , Hansson S 1 , Casslén B 1<br />
1 Department <strong>of</strong> Gynecology & Obstetrics, University Hospital, Lund, Sweden;<br />
2 Finsen Laboratory, Rigshospitalet, Copenhagen, Denmark<br />
Presenting author e-mail: emir.henic@med.lu.se<br />
EGF is a stimulator <strong>of</strong> proliferation as well as migration in ovarian cancer cells. In contrast, the<br />
effects <strong>of</strong> estrogen are incompletely explored <strong>and</strong> some results are contradictory. In addition to<br />
genomic effects via classical nuclear estrogen receptors (ER), accumulating evidence suggest that<br />
estrogens initiate rapid non-genomic signaling through cell membrane receptors. GPR30 is a<br />
newly identified receptor with all characteristics <strong>of</strong> a membrane ER.<br />
In this study we show that estradiol attenuates the stimulatory effect <strong>of</strong> EGF on both cell<br />
migration <strong>and</strong> uPAR expression in ovarian cancer cell lines. We have previously shown that EGF<br />
up-regulates uPAR expression via three distinct mechanisms. Studying each <strong>of</strong> these mechanisms<br />
in the presence <strong>of</strong> estradiol, we found no inhibition <strong>of</strong> neither the production <strong>of</strong> uPAR, i.e.<br />
the level <strong>of</strong> uPAR mRNA, nor the elimination <strong>of</strong> cell surface uPAR, i.e. by internalization for<br />
lysosomal degradation or by shedding to the medium. Instead estradiol inhibited the very rapid<br />
increase <strong>of</strong> detergent extractable uPAR, which occurs within minutes <strong>of</strong> EGF stimulation, <strong>and</strong> is<br />
likely to represent mobilization <strong>of</strong> uPAR from detergent resistant domains, like lipid rafts. ICI<br />
182,780, which is a nuclear ER antagonist, has agonistic properties with GPR30. This compound,<br />
like estradiol, inhibited the immediate effect <strong>of</strong> EGF on uPAR expression, <strong>and</strong> also did not inhibit<br />
that effect <strong>of</strong> estradiol. OVCAR-3 cells are ERa negative, but express mRNA for GPR30.<br />
Thus, our observations suggest that modulation <strong>of</strong> the EGF response by estradiol is mediated by<br />
GPR30.<br />
82 X I t h I n t e r n a t i o n a l W o r k s h o p o n
i071i<br />
Methylation <strong>of</strong> the PAI-1 Gene in Oral Squamous<br />
Cell Carcinomas <strong>and</strong> Normal Oral Mucosa<br />
Gao S 1 , Krogdahl A 2 , Sørensen JA 3 , Dabelsteen E 4 , Andreasen PA* 1<br />
1 Department <strong>of</strong> <strong>Molecular</strong> <strong>Biology</strong>, University <strong>of</strong> Aarhus, Aarhus, Denmark;<br />
2 Department <strong>of</strong> Pathology, Odense University Hospital, Odense, Denmark;<br />
3 Department <strong>of</strong> Plastic Surgery, Odense University Hospital, Odense, Denmark;<br />
4 School <strong>of</strong> Dentistry, University <strong>of</strong> Copenhagen, Copenhagen, Denmark<br />
Presenting author e-mail: pa@mb.au.dk<br />
It has become clear that CpG methylation plays an important role in development <strong>and</strong><br />
progression <strong>of</strong> cancer <strong>and</strong> the associated changes in gene expression. We have become interested<br />
in the possibility that decreased CpG methylation <strong>of</strong> specific genes may lead to over-expression<br />
in tumours <strong>and</strong> have studied the plasminogen activator inhibitor-1 (PAI-1) gene in this respect.<br />
The PAI-1 gene has 25 CpG sites within 960 bp around the transcription initiation site. We studied<br />
CpG methylation <strong>of</strong> the PAI-1 gene by bisulfite sequencing <strong>and</strong> PAI-1 mRNA levels by real-time<br />
RT-PCR. In a series <strong>of</strong> 20 cases <strong>of</strong> oral carcinomas <strong>and</strong> matched samples <strong>of</strong> adjacent histologically<br />
normal tissue from the same patients, we observed that the methylation frequency in tumours<br />
was lower than in the adjacent non-tumour tissue. By real time RT-PCR analysis, 17 <strong>of</strong> 20 patients<br />
with oral carcinoma were found to have between 2.5 <strong>and</strong> 50 fold increased PAI-1 mRNA levels,<br />
as compared with the adjacent non-tumour tissue. The mRNA level in the tumours was inversely<br />
correlated with decreased methylation frequency in the tumours. We conclude that demethylation<br />
<strong>of</strong> the PAI-1 gene promoter region may contribute to the higher expression <strong>of</strong> PAI-1 in the tumour<br />
than in surrounding histologically normal tissue in some oral carcinoma patients. The methylation<br />
at some specific CpG sites may play an important role in the regulation <strong>of</strong> PAI-1 gene expression.<br />
<strong>Molecular</strong> & <strong>Cellular</strong> <strong>Biology</strong> <strong>of</strong> <strong>Plasminogen</strong> <strong>Activation</strong> 83
i072i<br />
Urokinase Signaling through Its Receptor Promotes<br />
Invasiveness <strong>and</strong> Metastasis <strong>of</strong> Pancreatic Cancer Cells<br />
Xue A*, Xue M, Jackson C, Song E, Allen BJ, Smith RC<br />
The University <strong>of</strong> Sydney, Department <strong>of</strong> Surgery, Royal North Shore Hospital, NSW, Australia<br />
Presenting author e-mail: aiqunn@med.usyd.edu.au<br />
Urokinase-type plasminogen activator (uPA) system plays an important role in tumour<br />
pathogenesis. However, non-specific inhibition <strong>of</strong> all uPA system members causes side-effects,<br />
so it is necessary to clarify the specific function <strong>of</strong> uPA system members to provide the basis for<br />
selective blockade <strong>and</strong> reduction <strong>of</strong> therapeutic side-effects. In this study, we explored the role <strong>of</strong><br />
uPA, uPA receptor (uPAR) <strong>and</strong> PA inhibitor (PAI) in pancreatic ductal adenocarcinoma (PDAC)<br />
pathogenesis in vitro. Cox regression analysis showed that uPAR was independently associated<br />
with shorter overall patient survival, whereas increased levels <strong>of</strong> tumour-associated PAI-2 is a<br />
potential indicator <strong>of</strong> good outcome for patients. Receiver-operating characteristic area under the<br />
curve (ROC AUC) further confirmed that uPAR mRNA levels, as a signer factor, had achieved<br />
the highest AUC (AUC=0.84, p < 0.0001 ) in PDAC. When analysis <strong>of</strong> uPAR was combined with<br />
uPA, AUC was significantly increased up to 0.93, with sensitivity <strong>of</strong> 88.2% <strong>and</strong> specificity <strong>of</strong> 87.5%<br />
(p < 0.000). We also found that silencing uPAR by the specific small interfering RNA (siRNA)<br />
significantly inhibits cell proliferation, induces G0-G1 arrest <strong>and</strong> cell apoptosis, <strong>and</strong> suppresses<br />
cell migration in pancreatic cancer cells. Moreover, suppression <strong>of</strong> uPAR or uPA expression<br />
differentially regulates the activation <strong>of</strong> MAP kinases. However, specific blocking PAI-2 has not<br />
been observed significant impact on pancreatic cancer cell proliferation <strong>and</strong> migration. Taken<br />
together, our data indicate that uPAR may be important biomarker for human pancreatic cancer<br />
progression <strong>and</strong> prognosis as well as potentially selective therapeutic target.<br />
84 X I t h I n t e r n a t i o n a l W o r k s h o p o n
i073i<br />
Tissue <strong>Plasminogen</strong> Activator Induces Cell Proliferation in Pancreatic<br />
Cancer by a Non-catalytic Mechanism that Requires ERK1/2 <strong>Activation</strong><br />
through Epidermal Growth Factor Receptor <strong>and</strong> Annexin A2<br />
Ortiz-Zapater E 1,2 , Peiró S 1,2 , Roda O 1,2 , Corominas JM 3 , Aguilar S 1 , Ampurdanés C 1 , Real FX 1,2 ,<br />
Navarro P* 1<br />
1 Unitat de Biologia Cel-lular i <strong>Molecular</strong>, IMIM-prbb, Barcelona, Spain;<br />
2 Departament de Ciències Experimentals i de la Salut, Facultat de Ciències de la Salut i de la Vida,<br />
Universitat Pompeu Fabra, Barcelona, Spain;<br />
3 Departament de Patologia, Hospital del Mar, UAB, Barcelona, Spain<br />
Presenting author e-mail: pnavarro@imim.es<br />
Pancreatic cancer is one <strong>of</strong> the most aggressive human tumors, being the fifth-leading cause <strong>of</strong><br />
cancer death in the developed countries. Our previous data have shown that tissue plasminogen<br />
activator (tPA) is overexpressed in pancreatic ductal adenocarcinomas, playing a critical role<br />
in several events associated to tumor progression such as cell proliferation, invasion <strong>and</strong><br />
angiogenesis. Prior work supports the notion that the effects <strong>of</strong> tPA on cell invasion require its<br />
proteolytic activity. Here, we identify the molecular mechanism responsible for the proliferative<br />
effects <strong>of</strong> tPA on pancreatic tumor cells. tPA activates the ERK1/2 signalling pathway in a<br />
manner that is independent <strong>of</strong> its catalytic activity. We also show that at least two membrane<br />
receptors, EGFR <strong>and</strong> AnxA2, which are overexpressed in pancreatic cancer, are involved in<br />
the transduction <strong>of</strong> tPA signalling in pancreatic tumors, suggesting the establishment <strong>of</strong> an<br />
amplification loop involved in tumor cell proliferation. These results add novel insights into the<br />
non-catalytic functions <strong>of</strong> tPA in cancer <strong>and</strong> the molecular mechanisms involved in its effects on<br />
cell proliferation.<br />
<strong>Molecular</strong> & <strong>Cellular</strong> <strong>Biology</strong> <strong>of</strong> <strong>Plasminogen</strong> <strong>Activation</strong> 85
i074i<br />
Modulation <strong>of</strong> Lung Carcinoma Cell Lines <strong>and</strong> Primary<br />
Cultures Migration by uPA-Derived <strong>and</strong> EGFR Inhibitors<br />
Franco P* 1 , Mancini A 2 , Votta G 1 , Caputi M 2 , Stoppelli MP 1<br />
1 Institute <strong>of</strong> Genetics <strong>and</strong> Biophysics ‘’Adriano Buzzati-Traverso’’, National Research Council, Naples,<br />
Italy;<br />
2 Department <strong>of</strong> Cardiothoracic <strong>and</strong> Respiratory Sciences, Second University <strong>of</strong> Naples, Naples,Italy<br />
Presenting author e-mail: franco@igb.cnr.it<br />
The detachment <strong>of</strong> malignant cells from primary tumors <strong>and</strong> their subsequent migration to<br />
distant sites, including intravasation <strong>and</strong> extravasation, leads to tumor dissemination. The<br />
uPA/uPAR system plays a crucial role in tumor progression <strong>and</strong> invasion. Over-expression <strong>of</strong><br />
uPAR correlates with a poor prognosis in many neoplastic conditions, including lung tumors,<br />
suggesting that the specific inhibition <strong>of</strong> the uPA/uPAR system or/<strong>and</strong> the relative interactors<br />
may be a useful strategy to prevent metastasis. Among the functional partners <strong>of</strong> uPAR is the<br />
EGFR, which is over-expressed in NSCL (non-small-cell-lung) cancers <strong>and</strong> correlates with an high<br />
metastatic ability <strong>of</strong> the tumor. In particular, the EGFR is a widely recognised molecular target for<br />
anti-neoplastic therapies.<br />
In this study, we investigated the functional cross-talk between the two systems <strong>and</strong> the<br />
possibility to simultaneously inhibit both receptors by the aid <strong>of</strong> uPAR or EGFR inhibitors.<br />
In particular, we demostrated that both epidermoid carcinoma Calu-1 <strong>and</strong> squamous<br />
mucoepidermoid NCI-H-292 cell lines pre-treated with anti-EGFR antibodies, fail to migrate not<br />
only toward EGF but also toward uPA. Similarly, pre-treatment <strong>of</strong> the same cells with anti-uPAR<br />
antibodies, induce a strong inhibition <strong>of</strong> both uPA- <strong>and</strong> EGF-dependent migration.<br />
We also tested whether the anti-proliferative pharmacological inhibitors <strong>of</strong> EGFR kinase, namely<br />
IRESSA or gefitinib (ZD1839) <strong>and</strong> tyrphostin (AG-1478) may interfere with the Calu-1 <strong>and</strong> the<br />
NCI-H-292 cell migration. These inhibitors prevent not only EGF-dependent but also uPAdependent<br />
migration, suggesting that EGFR tyrosine kinase activity is required for uPA-induced<br />
directional migration.<br />
To further investigate the relationship between the two systems, we employed non-transformed<br />
human retinal pigment epithelial (RPE) <strong>and</strong> breast carcinoma MCF-7 cell lines in which uPAR<br />
expression level is stably reduced by the RNA-interference technology. In these clones, EGFR<br />
levels are not modified. However, in RPE <strong>and</strong> MCF-7 clones EGF-dependent migration is strongly<br />
impaired, confirming that the uPAR is required to the EGF/EGFR-dependent migration.<br />
These results show that the EGF/EGFR <strong>and</strong> uPA/uPAR systems are functionally interdependent<br />
in lung carcinoma cell migration <strong>and</strong> suggest that targeting either one may affect both systems.<br />
86 X I t h I n t e r n a t i o n a l W o r k s h o p o n
i075i<br />
A Novel Role <strong>of</strong> Ku80 in Regulation <strong>of</strong> PAI-1 Gene Expression<br />
in Migrating Endothelial Cells Induced by Thymosin b4<br />
Bednarek R* 1 , Boncela J 1 , Smolarczyk K 1 , Cierniewski CS 1,2<br />
1 Center <strong>of</strong> Medical <strong>Biology</strong>, Polish Academy <strong>of</strong> Science, Lodz, Pol<strong>and</strong>;<br />
2 Department <strong>of</strong> Medical <strong>and</strong> <strong>Molecular</strong> Biophysics, Medical University, Lodz, Pol<strong>and</strong><br />
Presenting author e-mail: rbednarek@cbm.pan.pl<br />
Our data demonstrate that increased intracellular expression <strong>of</strong> thymosin b4 (Tb4) is<br />
necessary <strong>and</strong> sufficient to induce PAI-1 gene expression in endothelial cells. To describe the<br />
mechanism <strong>of</strong> this effect, we produced Tb4 mutants with impaired functional motifs <strong>and</strong> tested<br />
their intracellular location <strong>and</strong> activity. Cytoplasmic distributions <strong>of</strong> Tb4(AcSDKPT/4A),<br />
Tb4(KLKKTET/7A), <strong>and</strong> Tb4(K16A) mutants fused with GFP did not differ significantly<br />
from those <strong>of</strong> wild Tb4. Overexpression <strong>of</strong> Tb4, Tb4(AcSDKPT/4A) <strong>and</strong> Tb4(K16A) affected<br />
intracellular formation <strong>of</strong> actin filaments. As expected, Tb4(K16A) uptake by nuclei was impaired.<br />
On the other h<strong>and</strong>, overexpression <strong>of</strong> Tb4(KLKKTET/7A) resulted in developing the actin<br />
filament network typical <strong>of</strong> adhering cells, indicating that the mutant lacked the actin binding<br />
site. The mechanism by which intracellular Tb4 induced the PAI-1 gene did not depend upon<br />
the N-terminal tetrapeptide AcSDKP, <strong>and</strong> depended only partially on its ability to bind G actin<br />
or enter the nucleus. Both Tb4 <strong>and</strong> Tb4(AcSDKPT/4A) induced the PAI-1 gene to the same<br />
extent, while mutants Tb4(KLKKTET/7A) <strong>and</strong> Tb4(K16A) retained about 60% <strong>of</strong> the original<br />
activity. By proteomic analysis, the Ku80 subunit <strong>of</strong> ATP-dependent DNA helicase II was found<br />
to be associated with Tb4. Ku80 <strong>and</strong> Tb4 consistently co-immunoprecipitated in a complex from<br />
endothelial cells. Furthermore, downregulation <strong>of</strong> Ku80 by specific siRNA resulted in dramatic<br />
reduction in PAI-1 expression, both at the level <strong>of</strong> mRNA <strong>and</strong> protein synthesis. These data<br />
suggest that Ku80 functions as a novel receptor for Tb4, initiates signaling leading to activation <strong>of</strong><br />
PAI-1 expression by an as yet unknown mechanism, <strong>and</strong> mediates the intracellular activity <strong>of</strong> Tb4.<br />
<strong>Molecular</strong> & <strong>Cellular</strong> <strong>Biology</strong> <strong>of</strong> <strong>Plasminogen</strong> <strong>Activation</strong> 87
i076i<br />
Signaling Pathway Involved in Inhibition <strong>of</strong><br />
PAI-1 Expression by CNP in Endothelial Cells<br />
Jerczynska H*, Cierniewski CS, Pawlowska Z<br />
Department <strong>of</strong> <strong>Molecular</strong> <strong>and</strong> Medical Biophysics, Medical University in Lodz, Lodz, Pol<strong>and</strong><br />
Presenting author e-mail: hanuka@zdn.am.lodz.pl<br />
We have reported previously that C-type natriuretic peptide (CNP) was an effective inhibitor <strong>of</strong><br />
PAI-1 synthesis <strong>and</strong> release from human endothelial cells. This inhibitory effect was stronger in<br />
Tumor Necrosis Factor alpha TNFa - stimulated cells.<br />
The signaling pathways required for this effect have not been elucidated. In the current study we<br />
investigated the signal transduction pathway involved in the inhibitory CNP action in human<br />
endothelial cells. We examined if CNP can modulate the known signaling pathways involved<br />
in the regulation <strong>of</strong> PAI-1 expression as well as a potential cGMP role. To characterize the signal<br />
transduction pathway, we used selective inhibitors <strong>of</strong> MAP kinase, PI3K/Akt, <strong>and</strong> 8-bromocGMP,<br />
a soluble analog <strong>of</strong> cGMP. The activation level <strong>of</strong> ERK1/2, JNK <strong>and</strong> NFaB was determined<br />
by ELISA with the use <strong>of</strong> specific antibodies. Our results imply that CNP inhibition <strong>of</strong> TNFaactivated<br />
PAI-1 gene expression takes place via regulation <strong>of</strong> signal transduction pathways<br />
involving directly PI3K/Akt <strong>and</strong> cGMP-dependent protein kinase, possibly by inhibiting NFkBdependent<br />
pathways. Thus, our results explain at least in part the mechanism involved in PAI-1<br />
expression inhibition by CNP in TNF-stimulated endothelial cells.<br />
88 X I t h I n t e r n a t i o n a l W o r k s h o p o n
i077i<br />
Interaction <strong>of</strong> Alzheimer’s Amyloid b-peptide (Ab) 1-40 with PAI-2<br />
Pabba M* 1 , Przygodzki T 1 , Malisauskas M 1 , Ol<strong>of</strong>sson A 2 , Morozova-Roche L 1 , Wilczynska M 1 , Ny T 1<br />
1 Department <strong>of</strong> Medical Biochemistry <strong>and</strong> Biophysics, 2 Umeå Center for <strong>Molecular</strong> Pathogenesis, Umeå<br />
University, Umeå, Sweden<br />
Presenting author e-mail: pabba.mohan@medchem.umu.se<br />
Alzheimer’s disease (AD) is one <strong>of</strong> the most known dementia in elderly. The disease is<br />
characterized by the presence <strong>of</strong> senile plaques that are almost entirely composed <strong>of</strong> an amyloid<br />
b-peptide. Amyloid b-peptide which is a proteolytic fragment produced from amyloid precursor<br />
protein, is also found in intracellular compartments, <strong>and</strong> recently several physiological roles <strong>of</strong> the<br />
peptide have been proposed. Acceleration as well as inhibition <strong>of</strong> Ab-peptide protein aggregation<br />
during Alzheimer’s disease is accomplished by various factors, including serpins. Serpins are<br />
the largest <strong>and</strong> broadly distributed superfamily <strong>of</strong> protease inhibitors. <strong>Plasminogen</strong> activator<br />
inhibitor type 2 (PAI-2) belongs to ovalbumin sub-clade <strong>of</strong> the serpin superfamily. Although it<br />
has been extensively studied, its biological functions remain unknown. It has been shown that<br />
expression <strong>of</strong> PAI-2 is high in microglia cells surrounding senile plaques in the brain <strong>of</strong> patients<br />
with Alzheimer’s disease, suggesting that PAI-2 might have a role in disease. Our western<br />
blot <strong>and</strong> sucrose cushion sedimentation experiments show that Ab-peptide interacted <strong>and</strong> coaggregate<br />
with PAI-2. In addition, atomic force microscopy <strong>and</strong> thi<strong>of</strong>lavin-T analyses reveal that<br />
PAI-2 inhibit prot<strong>of</strong>ibril formation by the Ab-peptide. Taken together these data suggest that<br />
Ab-peptide 1-40 interacts with PAI-2 in vitro. Studies on interaction <strong>of</strong> Ab-peptide with PAI-2 in<br />
neuronal cells are in progress.<br />
<strong>Molecular</strong> & <strong>Cellular</strong> <strong>Biology</strong> <strong>of</strong> <strong>Plasminogen</strong> <strong>Activation</strong> 89
i078i<br />
The Subcellular Itinerary <strong>of</strong> Hepatocyte Growth<br />
Factor Activator Inhibitor-1 in MDCK Cells<br />
Godiksen S 1 , Selzer-Plon J 1 , Pedersen EDK 1 , Borger Rasmussen H 1 , Bugge TH 2 , Vogel LK* 1<br />
1 Department <strong>of</strong> <strong>Cellular</strong> <strong>and</strong> <strong>Molecular</strong> Medicine, University <strong>of</strong> Copenhagen, Denmark;<br />
2 Oral <strong>and</strong> Pharyngeal Cancer Branch, NIDCR, NIH, Bethesda, Maryl<strong>and</strong>, USA<br />
Presenting author e-mail: vogel@imbg.ku.dk<br />
Hepatocyte growth factor activator inhibitor-1 (HAI-1) is a Kunitz-type transmembrane serine<br />
protease inhibitor that forms inhibitor complexes with several trypsin-like serine proteases that<br />
is required for mouse placental development <strong>and</strong> embryo survival <strong>and</strong> is a key regulator <strong>of</strong><br />
carcinogenesis. HAI-1 is expressed in polarized epithelial cells, where the plasma membrane<br />
is divided by tight juntions into an apical <strong>and</strong> a basolateral domain. Here we show that HAI-<br />
1 at steady state is mainly located on the basolateral membrane in both MDCK cells <strong>and</strong><br />
mammary gl<strong>and</strong> epithelial cells. After biosynthesis HAI-1 is exocytosed to the basolateral plasma<br />
membrane from where 20% <strong>of</strong> the HAI-1 molecules are proteolytically cleaved <strong>and</strong> released<br />
into the basolateral media. The remaining membrane associated HAI-1 is endocytosed <strong>and</strong><br />
recycles between the basolateral plama membrane <strong>and</strong> endosomes. However, a minor fraction<br />
<strong>of</strong> basolaterally located HAI-1 is trancytosed to the apical plasma membrane, from where it<br />
is probably cleaved <strong>and</strong> released into the media. HAI-1 is raft associated during most <strong>of</strong> its<br />
intracellular transport in a methyl-b-cyclodextrin dependent manner.<br />
90 X I t h I n t e r n a t i o n a l W o r k s h o p o n
i079i<br />
Evidence for a Matriptase-Prostasin (CAP1/PRSS8) Serine Protease<br />
Zymogen-Cascade-Regulating Epithelial Differentiation<br />
List K* 1 , Netzel-Arnett S 2 , Currie B 1 , Szabo R 1 , Molinolo A 1 , Antalis TM 2 , Bugge TH 1<br />
1 Oral <strong>and</strong> Pharyngeal Cancer Branch, NIDCR, NIH, Bethesda, Maryl<strong>and</strong>, USA;<br />
2 Center for Vascular <strong>and</strong> Inflammatory Disease, University <strong>of</strong> Maryl<strong>and</strong>, Baltimore, Maryl<strong>and</strong>, USA<br />
Presenting author e-mail: klist@nidcr.nih.gov<br />
Epidermal ablation <strong>of</strong> matriptase <strong>and</strong> prostasin has identical deleterious effects on terminal<br />
differentiation, suggesting a functional interrelationship between the two membrane serine<br />
proteases. Here we present histological, biochemical, <strong>and</strong> genetic evidence for a matriptaseprostasin<br />
zymogen cascade regulating epithelial differentiation. Enzymatic gene trapping <strong>of</strong><br />
matriptase combined with prostasin immunohistochemistry revealed that matriptase was colocalized<br />
with prostasin in transitional layer cells <strong>of</strong> the epidermis, <strong>and</strong> that the developmental<br />
onset <strong>of</strong> expression <strong>of</strong> the two membrane proteases correlated with acquisition <strong>of</strong> epidermal<br />
barrier function. Purified soluble matriptase efficiently converted soluble prostasin zymogen to<br />
an active two-chain form that formed SDS-stable complexes with the serpin protease nexin-1.<br />
Whereas two forms <strong>of</strong> prostasin with molecular weights corresponding to the prostasin zymogen<br />
<strong>and</strong> active prostasin were present in wildtype epidermis, prostasin was exclusively found in<br />
the zymogen form in matriptase-deficient epidermis. Moreover, we found that matriptase <strong>and</strong><br />
prostasin displayed a near-ubiquitous co-localization in simple, stratified, <strong>and</strong> pseudo-stratified<br />
epithelia <strong>of</strong> the integumentary system, digestive tract, respiratory tract, <strong>and</strong> urogenital tract,<br />
suggesting that the proposed matriptase-prostasin zymogen cascade may have additional roles in<br />
epithelial biology besides regulating terminal epidermal differentiation. Because matriptase is an<br />
auto-activating protease, it may serve as the initiator <strong>of</strong> zymogen cascades, similar to the closely<br />
related protease, enteropeptidase.<br />
<strong>Molecular</strong> & <strong>Cellular</strong> <strong>Biology</strong> <strong>of</strong> <strong>Plasminogen</strong> <strong>Activation</strong> 91
i080i<br />
The <strong>Plasminogen</strong> <strong>Activation</strong> System in Monocytic Cell<br />
Differentiation <strong>and</strong> Proliferation: Potential Target for<br />
<strong>Plasminogen</strong> <strong>Activation</strong> Inhibitor Type-2-Based Therapeutics<br />
Lee JA* 1 , Croucher DR 2 , Ranson M 1<br />
1 School <strong>of</strong> Biological Sciences, University <strong>of</strong> Wollongong, NSW Australia;<br />
2 Cancer Research Program, Garvan Institute <strong>of</strong> Medical Research, Sydney, Australia<br />
Presenting author e-mail: jal31@uow.edu.au<br />
The progression <strong>of</strong> tumours to malignancy is aided by the surrounding stroma <strong>and</strong> infiltrating<br />
leukocytes, <strong>of</strong> which tumour associated macrophages (TAMs) contribute up to 70% <strong>of</strong> the tumour<br />
mass in some cancers. TAMs potentiate malignancy by contributing to the production <strong>of</strong> the<br />
extracellular protease, plasmin. Originating from peripheral blood monocytes, TAMs have been<br />
found to over express components <strong>of</strong> the u-PA system <strong>and</strong> this behaviour identifies them as<br />
potential targets in the development <strong>of</strong> anti-u-PA targeted cancer therapies. One such potential<br />
therapy utilises the accelerated internalisation mechanisms <strong>of</strong> cell surface u-PA upon inhibition<br />
by its specific inhibitor, plasminogen activation inhibitor (PAI) type-2. This research shows for<br />
the first time that the internalisation <strong>of</strong> PAI-2 by differentiated U-937 <strong>and</strong> THP-1 monocytic cell<br />
lines is mediated in part by the low density lipoprotein receptor (LDLr) family <strong>of</strong> endocytosis<br />
receptors, in a u-PA dependent manner. Importantly, this shows that TAMs expressing high levels<br />
<strong>of</strong> u-PA may be targeted using PAI-2 therapeutics. Assessment <strong>of</strong> physiological consequences<br />
associated with exogenous PAI interactions at the cell surface revealed a reduction in proliferation<br />
for both cell lines when cultured in the presence <strong>of</strong> PAI-2 <strong>and</strong> PAI type-1, suggesting that u-PA:<br />
PAI complex formation at the cell surface disrupts mitogenic signalling cascades mediated via<br />
receptor bound u-PA. Based on these findings current research is being directed at the role <strong>of</strong><br />
exogenous PAI-2 in proliferation <strong>and</strong> differentiation <strong>of</strong> monocytes.<br />
92 X I t h I n t e r n a t i o n a l W o r k s h o p o n
i081i<br />
Identification <strong>and</strong> Localization <strong>of</strong> Novel Serine<br />
Proteases in the Mouse Ovary<br />
Wahlberg P*, Nyl<strong>and</strong>er Å, Kui L, Ny T<br />
Department <strong>of</strong> Medical Biochemistry <strong>and</strong> Biophysics, Umeå University, Umeå, Sweden<br />
Presenting author e-mail: patrik.wahlberg@medchem.umu.se<br />
Proteolytic degradation <strong>of</strong> extracellular matrix components is believed to play an essential role<br />
for ovulation to occur. Recent studies in our laboratory have suggested that the plasminogen (PA)<br />
<strong>and</strong> matrix metalloproteinase (MMP) systems are not required in this process. In this study, we<br />
have used a microarray approach to identify new proteases that are involved in ovulation. We<br />
discovered three new serine proteases that were relatively highly expressed during ovulation:<br />
HtrA1, which was not regulated during ovulation; PRSS23, which was downregulated by<br />
gonadotropins; <strong>and</strong> PRSS35, which was upregulated by gonadotropins. We have investigated<br />
the expression patterns <strong>of</strong> these proteases during gonadotropin-induced ovulation in immature<br />
mice <strong>and</strong> in the corpus luteum (CL) <strong>of</strong> pseudopregnant mice. We found that HtrA1 was highly<br />
expressed in granulosa cells throughout follicular development <strong>and</strong> ovulation. It was also highly<br />
expressed in the forming <strong>and</strong> regressing CL. PRSS23 was highly expressed in atretic follicles <strong>and</strong><br />
it was expressed in the ovarian stroma <strong>and</strong> theca tissues after ovulation was induced. PRSS35 was<br />
expressed in the theca layers <strong>of</strong> developing follicles. It was also highly induced in granulosa cells<br />
<strong>of</strong> preovulatory follicles. PRSS35 was also expressed in the forming <strong>and</strong> regressing CL. These data<br />
suggest that HtrA1 <strong>and</strong> PRSS35 are involved in ovulation <strong>and</strong> CL formation <strong>and</strong> regression <strong>and</strong><br />
that PRSS23 may play a role in follicular atre.<br />
<strong>Molecular</strong> & <strong>Cellular</strong> <strong>Biology</strong> <strong>of</strong> <strong>Plasminogen</strong> <strong>Activation</strong> 93
i082i<br />
Alpha-enolase/<strong>Plasminogen</strong> Binding Is Required<br />
during Myogenesis in vitro <strong>and</strong> in vivo<br />
Diaz-Ramos A*, Llorens A, Luque T, López-Alemany R<br />
Institute <strong>of</strong> Biomedical Investigation <strong>of</strong> Bellvitge (IDIBELL), <strong>Molecular</strong> Oncology Center (COM),<br />
L’Hospitalet de Llobregat, Barcelona, Spain<br />
Presenting author e-mail: madiaz@idibell.org<br />
During myogenesis, an important proteolyitc activity <strong>and</strong> extensive extracellular matrix (ECM)<br />
remodelation takes place. Plasmin, generated by activation <strong>of</strong> plasminogen, is an extracellular<br />
protease specialized in the degradation <strong>of</strong> the ECM components. Alpha-enolase constitutes a<br />
receptor for plasminogen in several cell lines, serving to focalize proteolytic activity on the cell<br />
surface.<br />
Previous studies show a role for components <strong>of</strong> the plasminogen activation system during<br />
myogenesis in vitro <strong>and</strong> in vivo. Preliminary results <strong>of</strong> our laboratory have shown that alphaenolase<br />
expression was up-regulated in a myogenic cell line upon differentiation, but the role <strong>of</strong><br />
alpha-enolase as a plasminogen receptor in myogenesis deserves further analysis.<br />
In the presence <strong>of</strong> inhibitors <strong>of</strong> plasminogen/alpha-enolase binding, myogenic differentiation,<br />
fusion <strong>and</strong> migration were abrograted, using primary cultures <strong>of</strong> myogenic cells or Muscle<br />
Precursor Cells (MPCs).<br />
The effect <strong>of</strong> inhibitors <strong>of</strong> plasminogen/alpha-enolase binding were evaluated in a regeneration<br />
model in mice after a muscle. Regeneration parameters were blocked by inhibitors <strong>of</strong><br />
plasminogen/alpha-enolase. The mdx mice (the animal model for Duchenne Muscular Dystrophy,<br />
DMD) presented a more severe dystrophinopathy with the same treatment. Inflammatory cells<br />
infiltration <strong>and</strong> fibrin deposition in injured tissues are currently being evaluated.<br />
Since inhibitors <strong>of</strong> plasminogen/alpha-enolase binding have an inhibitory effect on MPCs<br />
differentiation <strong>and</strong> muscle regeneration in vivo, our results demonstrate that plasmin activity<br />
is necessary for myogenesis to take place correctly, in an alpha-enolase dependent way.<br />
<strong>Plasminogen</strong>/alpha-enolase binding therefore could be an important target in the development <strong>of</strong><br />
treatments for DMD.<br />
94 X I t h I n t e r n a t i o n a l W o r k s h o p o n
i083i<br />
The Serpinb8 Is Alternatively Spliced to the Known<br />
Long Form <strong>and</strong> a Novel Short Form<br />
Olausson B* 1 , Przygodzka P 1 , Dahl L 2 , Carlsson L 2 , Wilczynska M 1<br />
1 2 Department <strong>of</strong> Medical Biochemistry <strong>and</strong> Biophysics, Umeå Center for <strong>Molecular</strong> Medicine, Umeå<br />
University, Umeå, Sweden<br />
Presenting author e-mail: bjorn.olausson@medchem.umu.se<br />
Serpinb8 belongs to the ovoalbumin-serpin subfamily, <strong>and</strong> is known as an intracellular protease<br />
inhibitor with a unique distribution pattern in human tissues. Here we show that serpinb8 can<br />
be alternatively spliced to the already known long form <strong>and</strong> to a novel short form. Compared to<br />
the long form, the short form <strong>of</strong> serpinb8 is missing exon 7, <strong>and</strong> instead it has a short nucleotide<br />
extension. Exon 7 in the long serpinb8 encodes part <strong>of</strong> beta-sheet A <strong>and</strong> the reactive center loop.<br />
Therefore, the short form <strong>of</strong> serpinb8 can be predicted not to function as protease inhibitor. By<br />
using real-time PCR, we found that in myelomonocytic leukemia cell lines, as well as in mouse<br />
hematopoietic stem cells, the long form <strong>of</strong> serpinb8 is expressed at very low levels, but the<br />
expression increases during monocytic, granulocytic, <strong>and</strong> megakaryocytic differentiations to<br />
reach maximum in finally differentiated blood cells. In contrast, the short form <strong>of</strong> serpinb8 is<br />
temporarily expressed during monocytic differentiation <strong>of</strong> HL-60 cells <strong>and</strong> is not detectable in the<br />
differentiated monocytes. Our preliminary real-time PCR data on the RNA from 18 human tissues<br />
suggest that the short form <strong>of</strong> serpinb8 is expressed only in few tissues as pancreas, oesophagus,<br />
<strong>and</strong> kidney. Studies on the cellular localization <strong>of</strong> the spliced forms <strong>of</strong> serpinb8 are in progress.<br />
<strong>Molecular</strong> & <strong>Cellular</strong> <strong>Biology</strong> <strong>of</strong> <strong>Plasminogen</strong> <strong>Activation</strong> 95
i084i<br />
Characterization <strong>of</strong> a Combined PAI-1 <strong>and</strong> TIMP-1<br />
Gene-deficient Mouse Model<br />
Harslund J* 1 , Nielsen OL 2 , Brünner N 1 , Offenberg H 1<br />
1 2 Section <strong>of</strong> Biomedicine, Section <strong>of</strong> Pathology, Department <strong>of</strong> Veterinary Pathobiology, Faculty <strong>of</strong> Life<br />
Sciences, University <strong>of</strong> Copenhagen, Frederiksberg, Denmark<br />
Presenting author e-mail: jhar@life.ku.dk<br />
The endogenous proteinase inhibitors PAI-1 <strong>and</strong> TIMP-1 are two distinct proteins with separate<br />
molecular pathways. However, a much closer relationship between PAI-1 <strong>and</strong> TIMP-1 has been<br />
proposed indicating some degree <strong>of</strong> functional overlap due to their involvement in ECM turnover,<br />
tissue remodelling <strong>and</strong> cellular migration <strong>and</strong> signalling. To study the physiological implications<br />
<strong>of</strong> PAI-1 <strong>and</strong> TIMP-1 we have generated a combined PAI-1 <strong>and</strong> TIMP-1 gene deficient mouse<br />
model. We present the results on generating this specific mouse model with particular emphasis<br />
on phenotypical characteristics, haematological parameters, a histological evaluation <strong>and</strong> gene<br />
expression studies <strong>of</strong> PAI-1 <strong>and</strong> TIMP-1 in various organs. We observed a significant deviation in<br />
segregation <strong>of</strong> <strong>of</strong>fspring only in male mice (p
i085i<br />
Dual Role <strong>of</strong> the uPA/uPAR System in Apoptosis <strong>of</strong><br />
Mesangial Cells <strong>and</strong> Diabetic Nephropathy<br />
Tkachuk N, Tkachuk S*, Kiyan J, Shushakova N, Haller H, Dumler I<br />
Nephrology Department, Hannover Medical School, Hannover, Germany<br />
Presenting author e-mail: Tkatchouk.Sergei@mh-hannover.de<br />
In diabetic nephropathy apoptosis has been considered as a major mechanism for regulation<br />
<strong>of</strong> cell amount in the places <strong>of</strong> mesangial hypercellularity. Given these functions for apoptosis<br />
together with the observation that uPAR <strong>and</strong> uPA may be upregulated during renal injury, the<br />
present study was designed to investigate the role <strong>of</strong> the uPA/uPAR system in apoptosis <strong>of</strong><br />
mesangial cells (MC) under high glucose <strong>and</strong> growth factors withdrawal conditions. Our data<br />
show that uPA can elicit both pro-apoptotic <strong>and</strong> anti-apoptotic effects in human MC depending<br />
on the apoptosis-inducing stimulus. Thus, uPA abrogated MC apoptosis induced by growth<br />
factors withdrawal conditions, whereas apoptosis initiated in MC by high glucose was enhanced<br />
in presence <strong>of</strong> uPA. Amino-terminal fragment (ATF) <strong>of</strong> uPA completely retained effects <strong>of</strong> uPA.<br />
uPAR was shown to be involved in both pro-apoptotic <strong>and</strong> anti-apoptotic effects <strong>of</strong> uPA. <strong>Cellular</strong><br />
redistribution <strong>of</strong> uPAR in response to high glucose was observed. Members <strong>of</strong> MAPK <strong>and</strong> PI3kinase<br />
pathways <strong>and</strong> Bad protein were found to be downstream molecules mediating the effects<br />
<strong>of</strong> uPA. The opposite effects <strong>of</strong> uPA on MC apoptosis are directed via different uPAR-interacting<br />
transmembrane partners. Thus, whereas the anti-apoptotic effect <strong>of</strong> uPA was mediated by<br />
integrins, its pro-apoptotic effect required uPAR interaction with cation-independent mannose-<br />
6-phosphate receptor (M6PR). In vivo, uPAR <strong>and</strong> M6PR were upregulated in the kidney <strong>of</strong> mice<br />
in streptozotocin (STZ)-induced diabetes that confirmed an important role for these receptors in<br />
mediating functional response <strong>of</strong> mesangial cells to high glucose.<br />
<strong>Molecular</strong> & <strong>Cellular</strong> <strong>Biology</strong> <strong>of</strong> <strong>Plasminogen</strong> <strong>Activation</strong> 97
i086i<br />
Phenotypic Consequences <strong>of</strong> <strong>Plasminogen</strong> Activator<br />
Inhibitor-1 Gene Ablation on STAT1 <strong>Activation</strong> <strong>and</strong> Cell<br />
Cycle Progression in Proliferating Endothelial Cells<br />
Balsara RD* 1,2,3 , Morin SJ 1 , Meyer CA 1 , Castellino FJ 1,2,3 , Ploplis VA 1,2,3<br />
1 2 3 W. M. Keck Center for Transgene Research, Department <strong>of</strong> Chemistry <strong>and</strong> Biochemistry, Notre Dame<br />
Cancer Institute, University <strong>of</strong> Notre Dame, Indiana, USA<br />
Presenting author e-mail: rbalsara@nd.edu<br />
The enhanced proliferation observed in PAI-1-deficient endothelial cells (EC) is associated with<br />
Akt hyperactivation resulting in loss <strong>of</strong> growth control <strong>and</strong> resistance to apoptosis. Additionally,<br />
involvement <strong>of</strong> other signaling pathways that regulate cell proliferation was investigated.<br />
Evaluation <strong>of</strong> the STAT protein pr<strong>of</strong>ile revealed that PAI-1–/– EC exhibited lower levels <strong>of</strong><br />
STAT1, which is a negative regulator <strong>of</strong> cellular proliferation. The pro-proliferative STAT3 <strong>and</strong><br />
STAT5 protein levels were similar in WT <strong>and</strong> PAI-1–/– cells. Furthermore, the activation status <strong>of</strong><br />
STAT1 between WT <strong>and</strong> PAI-1–/– EC differs. The extent <strong>of</strong> phosphorylation <strong>of</strong> Ser727 within the<br />
STAT1 transcriptional activation domain is lower in PAI-1–/– EC. Immun<strong>of</strong>luorescent analyses<br />
<strong>of</strong> proliferating WT <strong>and</strong> PAI-1–/– EC demonstrate that the cellular distribution <strong>of</strong> STAT1(P-<br />
Tyr701), which is crucial for STAT1 dimerization <strong>and</strong> nuclear translocation, is different between<br />
the two cell types. In WT cells, STAT1(P-Tyr701) appears to be diffuse throughout the whole<br />
cell, including the nucleus. In contrast, in PAI-1–/– cells, STAT1(P-Tyr701) seems to be localized<br />
in the cytoplasm <strong>and</strong> plasma membrane. Additionally, it was observed that in WT cells STAT1<br />
preferentially binds to Jak1, whereas in the PAI-1–/– EC, STAT1 is preferentially bound to Jak2.<br />
This differential binding may be responsible for the different activation states <strong>of</strong> STAT1. Cell cycle<br />
progression analysis demonstrated that a higher percentage <strong>of</strong> PAI-1–/– EC are in the S-phase<br />
compared to WT cells, which is likely a consequence <strong>of</strong> diminished STAT1 levels observed in the<br />
PAI-1-deficient cells.<br />
98 X I t h I n t e r n a t i o n a l W o r k s h o p o n
i087i<br />
Urokinase <strong>and</strong> its Receptor as Novel C-Myc Target<br />
Genes Affecting Cell Migration <strong>and</strong> Apoptosis<br />
Alfano D*, Iaccarino I, Stoppelli MP<br />
Institute <strong>of</strong> Genetics <strong>and</strong> Biophysics ‘’Adriano Buzzati-Traverso’’, National Research Council, Naples,<br />
Italy<br />
Presenting author e-mail: alfano@igb.cnr.it<br />
The binding <strong>of</strong> the serine protease urokinase (uPA) to its receptor (uPAR) plays a central role<br />
in cell adhesion, migration <strong>and</strong> invasion. According to our recently published data, uPAR<br />
overexpression <strong>and</strong> signalling prevents DNA damage-induced apoptosis as well as anoikis <strong>of</strong><br />
retinal pigment epithelial cells (RPE). Among the genes regulating cell proliferation <strong>and</strong> survival<br />
is the oncogene c-Myc. In an attempt to characterise the effect <strong>of</strong> c-Myc activation on uPA <strong>and</strong><br />
uPAR expression as well as on the cell survival/apoptosis balance, we employed an RPE cell line<br />
carrying an inducible c-MycER. As previously reported in other cell systems, induction <strong>of</strong> c-Myc<br />
in RPE cells leads to an increased cell sensitivity to different pro-apototic stimuli, like uv-light<br />
<strong>and</strong> serum starvation. To investigate the genes regulated in these conditions, the gene expression<br />
pr<strong>of</strong>ile following c-Myc activation for 4-16 hrs was determined. Surprisingly, a marked downregulation<br />
<strong>of</strong> the mRNAs coding for uPA <strong>and</strong> uPAR was observed. Furthermore, addition <strong>of</strong><br />
recombinant uPA to the culture medium improuves cell survival, suggesting that<br />
c-Myc-induced apoptosis is, at least in part, due to uPA down-regulation. As expected, following<br />
c-Myc activation, we observed a remarkable decrease in cell migration ability. In conclusion, the<br />
uPA/uPAR system is subjected to a c-Myc-dependent downregulation under conditions in which<br />
a concomitant increase in the sensitivity to apoptosis <strong>and</strong> a decrease in cell motility is observed.<br />
We propose that during oncogenic transformation the uPA/uPAR system might restrain c-Myc<br />
proliferative <strong>and</strong> invasive potential.<br />
<strong>Molecular</strong> & <strong>Cellular</strong> <strong>Biology</strong> <strong>of</strong> <strong>Plasminogen</strong> <strong>Activation</strong> 99
i088i<br />
Effect <strong>of</strong> <strong>Plasminogen</strong> on Cell Migration Using an in vitro Wound Model<br />
Sulniute R*, Li J, Ny T<br />
Department <strong>of</strong> Medical Biochemistry <strong>and</strong> Biophysics, Umeå University, Umeå, Sweden<br />
Presenting author e-mail: rima.sulniute@medchem.umu.se<br />
In vivo studies on incisional wounds have shown that plasminogen (plg) plays an important role<br />
in wound healing. However, due to the complexity <strong>of</strong> the in vivo system, the exact functional roles<br />
that plg plays in wound healing at the molecular level remain obscure.<br />
We therefore established a simplified in vitro model in order to directly investigate the molecular<br />
mechanism by which plg affects keratinocyte migration in wound healing. In this model, a<br />
scratch wound is made on a monolayer <strong>of</strong> adherent DOK (early neoplastic/dysplastic human oral<br />
keratinocytes) cell line <strong>and</strong> the wound closure process is monitored thereafter. Our data reveal<br />
that at 24 hours after scratch wounding, DOK cells had migrated about 65% <strong>of</strong> the original wound<br />
area in the presence <strong>of</strong> 2 µM plg (mimicking the plasma level <strong>of</strong> plg), whereas these cells only<br />
migrated about 45% when incubated in the plg-depleted medium. Furthermore, wound closure<br />
was accelerated up to 80% <strong>of</strong> the original wound when the level <strong>of</strong> plg was doubled<br />
(4 µM). Interestingly, when PMSF, a serine protease inhibitor, was added in the presence <strong>of</strong> plg,<br />
the cells had the same migration rate as those in the plg-depleted medium. Altogether, our data<br />
suggest that plg, probably through its proteolytic activity, is essential in keratinocyte migration in<br />
an in vitro wound healing model. These findings are in consistence with our in vivo studies in plg<br />
deficient mice.<br />
100 X I t h I n t e r n a t i o n a l W o r k s h o p o n
i089i<br />
uPA, but not its Receptor uPAR, Is Necessary for Experimentallyinduced<br />
<strong>and</strong> Pathological Muscle Regeneration<br />
Vidal B*, Serrano AL, Jardí M, Suelves M, Muñoz-Cánoves P<br />
Center for Genomic Regulation (CRG), Differentiation <strong>and</strong> Cancer Program, Barcelona, Spain<br />
Presenting author e-mail: berta.vidal@crg.es<br />
Extracellular proteolysis takes place during skeletal muscle regeneration. We have previously<br />
shown that uPA is required for muscle regeneration in vivo, since regeneration was impaired<br />
in uPA–/– mice after muscle injury. Moreover, the double mutant uPA–/–mdx mice showed<br />
exacerbated dystrophinopathy compared to uPA+/+mdx mice, the animal model for Duchenne<br />
muscular dystrophy. uPA was critical for a correct inflammatory response, as demonstrated by<br />
the reduced number <strong>of</strong> infiltrated macrophages <strong>and</strong> T-cells in uPA–/–mdx mice, as compared<br />
to uPA+/+mdx mice. Consistent herewith, loss <strong>of</strong> uPA also reduced the number <strong>of</strong> infiltrated<br />
inflammatory cells in experimentally-injured muscle. In contrast, the muscular compartment<br />
did not seem to be affected by loss <strong>of</strong> uPA, since isolated uPA–/– satellite cells showed normal<br />
myogenesis in vitro. Since several cellular functions <strong>of</strong> uPA do not require its proteolytical activity,<br />
but rather its ability to bind uPAR, <strong>and</strong> because uPAR expression was induced in regenerating<br />
muscle <strong>of</strong> WT <strong>and</strong> mdx mice, we hypothesized that the role <strong>of</strong> uPA in muscle regeneration might<br />
be dependent, at least in part, on its binding to uPAR. Thus, we analyzed the consequences <strong>of</strong><br />
uPAR deficiency (uPAR–/– mice) in experimentally-induced muscle regeneration <strong>and</strong> mdx<br />
dystrophinopathy (uPAR–/–mdx mice). Experimentally-induced muscle regeneration was<br />
indistinguishable between WT <strong>and</strong> uPAR–/– mice after histological analyses at 2, 10 <strong>and</strong> 25<br />
days post-injury. Muscular dystrophy was also similar in uPAR+/+mdx <strong>and</strong> uPAR–/–mdx<br />
mice, indicating that uPAR is dispensable for muscle tissue remodeling during regeneration.<br />
These results suggest that uPA regulates key processes during muscle regeneration in a uPARindependent<br />
manner.<br />
<strong>Molecular</strong> & <strong>Cellular</strong> <strong>Biology</strong> <strong>of</strong> <strong>Plasminogen</strong> <strong>Activation</strong> 101
i090i<br />
Urokinase-type <strong>Plasminogen</strong> Activator Deficiency Strongly Attenuates<br />
Ischemia Reperfusion Injury <strong>and</strong> Acute Kidney Allograft Rejection<br />
Gueler F 1 , Rong S 1 , Mengel M 2 , Park J-K 1 , Kirsch T 1 , Haller H 1 , Dumler I 1 , Shushakova N* 1<br />
1 Department <strong>of</strong> Nephrology, 2 Department <strong>of</strong> Pathology, Medical School Hanover, Hanover, Germany<br />
Presenting author e-mail: nshushakova@phenos.com<br />
Central mechanisms leading to ischemia induced allograft rejection are apoptosis <strong>and</strong><br />
inflammation, processes highly regulated by the urokinase-type plasminogen activator (uPA)<br />
<strong>and</strong> its specific receptor (uPAR). Recently, up-regulation <strong>of</strong> uPA <strong>and</strong> uPAR has been shown to<br />
correlate with allograft rejection in human biopsies. However, the causal connection <strong>of</strong> uPA/<br />
uPAR in mediating <strong>of</strong> transplant rejection <strong>and</strong> underlying molecular mechanisms remain poorly<br />
understood. In this study, we evaluated the role <strong>of</strong> uPA/uPAR in a mice model for IR injury<br />
<strong>and</strong> for acute kidney allograft rejection. uPAR but not uPA deficiency strongly protected kidney<br />
from IR injury. For the transplant model, allografts from H2b uPA–/–, uPAR–/– <strong>and</strong> wildtype<br />
(WT) mice were transplanted into MHC-incompatible H2d WT recipients. Again uPAR but not<br />
uPA deficiency <strong>of</strong> the allograft caused superior recipient survival <strong>and</strong> strongly attenuated loss <strong>of</strong><br />
renal function. We could demonstrate that uPAR-deficient allografts showed reduced generation<br />
<strong>of</strong> reactive oxygen species (ROS) <strong>and</strong> apoptosis. Moreover, transplant-induced up-regulation<br />
<strong>of</strong> adhesion molecule ICAM-1 was completely abrogated in uPAR-deficient allografts due to<br />
inadequate C5a <strong>and</strong> TNFa signalling, leading to reduced leukocyte infiltration. Our results<br />
demonstrate that the local renal uPAR plays an important role in the apoptotic <strong>and</strong> inflammatory<br />
responses mediating IR-injury <strong>and</strong> transplant rejection.<br />
102 X I t h I n t e r n a t i o n a l W o r k s h o p o n
i091i<br />
a1-antitrypsin Polymerization Studies using Gas-phase<br />
Electrophoretic Mobility <strong>Molecular</strong> Analysis (GEMMA)<br />
Przygodzki T* 1 , Mallya M 2 , Phillips RL 2 , Belorgey D 2 , Hägglöf P 2 , Lomas DA 2 , Ny T 1<br />
1 Department <strong>of</strong> Medical Biochemistry <strong>and</strong> Biophysics, Umeå University, Umeå, Sweden;<br />
2 Department <strong>of</strong> Medicine, University <strong>of</strong> Cambridge, Cambridge Institute for Medical Research,<br />
Cambridge, United Kingdom<br />
Presenting author e-mail: tomasz.przygodzki@medchem.umu.se<br />
Several proteins from the serpin superfamily are known to have capability <strong>of</strong> forming polymers.<br />
One <strong>of</strong> them is the elastase inhibitor-a1-antitrypsin (AT). Beside wild type AT which does not<br />
polymerize in physiological conditions, a highly polymerizing, natural mutant, Z AT, has been<br />
described.<br />
The kinetics <strong>of</strong> serpin polymerization is still a matter <strong>of</strong> debate. We followed this process by a<br />
novel approach: gas-phase electrophoretic mobility molecular analysis (GEMMA). This technique<br />
allows the analysis <strong>of</strong> the distribution <strong>of</strong> macromolecules in solution with respect to their size. A<br />
relatively short time required for sample analyses, a broad range <strong>of</strong> macromolecule size that can<br />
be separated as well as the fact that non-covalent complexes remain intact upon measurement<br />
make this technique very useful for the study <strong>of</strong> protein assembly.<br />
We followed the polymerization process <strong>of</strong> both wild type <strong>and</strong> Z AT over time at three<br />
temperatures. We observed no oligomers formation <strong>of</strong> wild type AT at temperatures <strong>of</strong> 36°C <strong>and</strong><br />
45°C whereas Z AT was polymerizing in all conditions. Velocity <strong>of</strong> wt AT oligomers formation<br />
at 55°C was approximately 10 times lower than that for the Z mutant. We have observed<br />
dimeric, trimeric, tetrameric <strong>and</strong> pentameric species in the case <strong>of</strong> both proteins indicating that<br />
polymerization proceeds, by sequential addition <strong>of</strong> monomers, however the fast formation <strong>of</strong><br />
dimers suggests that the dimer can also be a building block in formation <strong>of</strong> the polymers.<br />
<strong>Molecular</strong> & <strong>Cellular</strong> <strong>Biology</strong> <strong>of</strong> <strong>Plasminogen</strong> <strong>Activation</strong> 103
i092i<br />
The <strong>Plasminogen</strong> Interaction <strong>of</strong> Antigen 85B Protein<br />
from Mycobacterium Tuberculosis: Role <strong>of</strong> Lys89<br />
Xolalpa W* 1 , Vallecillo AJ 1 , Rosales L 2 , Ruiz BH 2 , Espitia C 1<br />
1 Departamento de Inmunología y, 2 Departamento de Biología <strong>Molecular</strong>, Instituto de Investigaciones<br />
Biomédicas, Universidad Nacional Autónoma de México, México, México<br />
Presenting author e-mail: wendyxv@hotmail.com<br />
Interactions <strong>of</strong> microorganims with the <strong>Plasminogen</strong> (Plg) system molecules have been<br />
recognized in numerous bacteria species. Our group has recently identified several Plg binding<br />
proteins in Mycobacterium tuberculosis extracts combining 2D-PAGE <strong>and</strong> Lig<strong>and</strong> Blotting tools.<br />
Interestingly, proteins belonging to the antigen 85 (Ag85) complex, which have a role on cell wall<br />
synthesis <strong>and</strong> bind the extracellular matrix protein fibronectin, were identified as Plg binding<br />
proteins. This binding was inhibited by the lysine analogue e-aminocaproic acid, involving<br />
the participation <strong>of</strong> lysine binding sites (LBSs) <strong>of</strong> Plg kringles. In order to characterize the Plg-<br />
Ag85 interaction, we took advantage <strong>of</strong> molecular modeling tools. Using the theoretical model<br />
<strong>of</strong> the lysine-LBS interaction <strong>of</strong> the homodimeric complex <strong>of</strong> kringle 2 from tPA as reference <strong>of</strong><br />
interactions between a kringle domain <strong>and</strong> a non C-terminal lysine, the Lys89 from Ag85A <strong>and</strong><br />
Ag85B was recognized as a better c<strong>and</strong>idate to mediate Plg interaction. To assess the role <strong>of</strong> this<br />
aa, site-specific mutation was introduced in the M. tuberculosis Ag85B recombinant protein<br />
replacing the lysine by arginine. Recombinant Ag85B <strong>and</strong> Ag85BArg89 proteins were evaluated<br />
in their capability to bind to Plg by a solid-phase binding assay on ELISA plates. The results<br />
demonstrate that Plg binding on Ag85BArg89 protein is reduced until 90 percent in comparison<br />
with the wild type Ag85B protein. Binding to fibronectin was also evaluated in both proteins but<br />
no significant difference was found. These results confirm the specific role <strong>of</strong> Lys89 on Ag85B-Plg<br />
interaction giving to Ag85B a new role as putative Plg receptor.<br />
104 X I t h I n t e r n a t i o n a l W o r k s h o p o n
i093i<br />
<strong>Plasminogen</strong> as a Factor in Innate Immunity<br />
Ahlskog N*, Guo Y, Ny T<br />
Department <strong>of</strong> Medical Chemistry <strong>and</strong> Biophysics, Umeå University, Umeå, Sweden<br />
Presenting author e-mail: nina.ahlskog@medchem.umu.se<br />
Recent results in our group strongly indicate a link between plasmin/plasminogen <strong>and</strong> the innate<br />
immune system, the body’s initial response to infection. <strong>Plasminogen</strong>-deficient mice were shown<br />
to have a higher mortality during S. aureus-induced infection (i. v. injection <strong>of</strong> low dose viable<br />
bacteria), but had a better survival rate during the initial stages <strong>of</strong> sepsis (high dose bacteria) as<br />
compared to their wild-type littermates. This phenotypic switch was shown to be specific to the<br />
active plasmin, as well as dependent on plasmin levels.<br />
Using a human mast cell line (HMC-1.2) <strong>and</strong> a mouse intra-peritoneal macrophage cell line (J774),<br />
we have found that the phenotypic switch seen in vivo, is not due to the phagocytizing capability<br />
<strong>of</strong> the macrophages or the anti-microbial activity <strong>of</strong> the mast cells in response to infection <strong>and</strong><br />
sepsis. The cells were exposed to viable bacteria in doses mimicking infection <strong>and</strong> sepsis for 20<br />
hours, after which the bacterial number, as well as the cell number, was ascertained. The antimicrobial<br />
response <strong>of</strong> both the cell types was comparable, regardless <strong>of</strong> the presence or absence<br />
<strong>of</strong> plasminogen in the medium. The migrating capability <strong>of</strong> the cells was tested using Boyden<br />
Micro Chemotaxis Chamber, where the percentage <strong>of</strong> cells migrating through the membrane <strong>of</strong><br />
the chamber was found to be comparable for both cell types, with or without plasminogen in the<br />
medium. The cellular response, e.g. release <strong>of</strong> cytokines <strong>and</strong> proteases, <strong>of</strong> the cells upon exposure<br />
to bacteria will be studied further as well as other leukocytic cell types.<br />
<strong>Molecular</strong> & <strong>Cellular</strong> <strong>Biology</strong> <strong>of</strong> <strong>Plasminogen</strong> <strong>Activation</strong> 105
i094i<br />
The Inflammatory Cytokine Oncostatin M Induces <strong>Plasminogen</strong><br />
Activator Inhibitor-1 in Human Vascular Smooth Muscle Cells in<br />
vitro via PI3 kinase <strong>and</strong> MAP-kinase Dependent Pathways<br />
Demyanets S 1 , Kaun C 1 , Rychli K 1 , Rega G 1 , Pfaffenberger S 1 , Maurer G 1 , Huber K 2 , Wojta J* 1<br />
1Department <strong>of</strong> Internal Medicine II, Medical University <strong>of</strong> Vienna, Ludwig Boltzmann Foundation for<br />
Cardiovascular Research, Vienna, Austria;<br />
2 3rd Medical Department for Cardiology <strong>and</strong> Emergency Medicine, Wilhelminenspital, Vienna, Austria<br />
Presenting author e-mail: johann.wojta@meduniwien.ac.at<br />
<strong>Plasminogen</strong> activator inhibitor-1 (PAI-1) plays a pivotal role in the regulation <strong>of</strong> the fibrinolytic<br />
system <strong>and</strong> in the modulation <strong>of</strong> extracellular proteolysis. Increased expression <strong>of</strong> PAI-1 was<br />
found in atherosclerotic lesions <strong>and</strong> high PAI-1 plasma levels were shown to be associated<br />
with coronary heart disease. Smooth muscle cells seem to be a major source <strong>of</strong> PAI-1 within<br />
the vascular wall <strong>and</strong> PAI-1 was implicated in smooth muscle cell migration, proliferation <strong>and</strong><br />
apoptosis. We treated human coronary artery smooth muscle cells (HCASMC) <strong>and</strong> human aortic<br />
SMC (HASMC) with the glycoprotein 130 (gp130) lig<strong>and</strong>s cardiotrophin-1 (CT-1), interleukin-<br />
6 (IL-6), leukemia inhibitory factor (LIF) or oncostatin M (OSM). OSM, but not CT-1, IL-6 or<br />
LIF increased PAI-1 production significantly in both HCASMC <strong>and</strong> HASMC up to 20-fold as<br />
determined by a specific ELISA. OSM upregulated also mRNA specific for PAI-1 up to 4.5-fold<br />
after 24 hours in these cells <strong>and</strong> HCASMC <strong>and</strong> HASMC were shown to express gp130, OSM<br />
receptor, IL-6 receptor <strong>and</strong> LIF receptor using RealTime-polymerase chain reaction (RealTime-<br />
PCR). PD98059, a MEK inhibitor <strong>and</strong> LY294002, a PI3K inhibitor, but not AG-490, a JAK/STAT<br />
inhibitor, abolished the OSM-dependent PAI-1 induction almost completely. We hypothesize that<br />
if the effect <strong>of</strong> OSM on PAI-1 expression in smooth muscle cells is operative in vivo it could—via<br />
modulation <strong>of</strong> fibrinolysis <strong>and</strong> extracellular proteolysis—be involved in the development <strong>of</strong><br />
vascular pathologies such as plaque progression, destabilization <strong>and</strong> subsequent thrombus<br />
formation, <strong>and</strong> restenosis <strong>and</strong> neointima formation.<br />
106 X I t h I n t e r n a t i o n a l W o r k s h o p o n
i095i<br />
Crohn’s Disease but not Chronic Ulcerative Colitis<br />
Induces the Expression <strong>of</strong> PAI-1 in Enteric Neurons<br />
Laerum OD* 1,2 , Illemann M 1 , Skarstein A 3 , Helgel<strong>and</strong> L 2 , Øvrebø K 3 , Danø K 1 , Nielsen BS 1<br />
1 The Finsen Laboratory, Rigshospitalet, Copenhagen, Denmark;<br />
2The Gade Institute, Section <strong>of</strong> Pathology, University <strong>of</strong> Bergen <strong>and</strong> Department <strong>of</strong> Pathology, Haukel<strong>and</strong><br />
University Hospital, Bergen, Norway;<br />
3Department <strong>of</strong> Surgical Sciences, University <strong>of</strong> Bergen, <strong>and</strong> Department <strong>of</strong> Surgery, Haukel<strong>and</strong><br />
University Hospital, Bergen, Norway<br />
Presenting author e-mail: ole.laerum@gades.uib.no<br />
Chronic inflammation <strong>of</strong> the intestinal wall is the common characteristic <strong>of</strong> Crohn’s disease<br />
<strong>and</strong> ulcerative colitis; disorders, which in some cases can be difficult to distinguish. The<br />
inflammation also affects the local neuronal plexuses <strong>of</strong> the enteric nervous system. It is known<br />
that plasminogen activator inhibitor-1 (PAI-1) <strong>and</strong> urokinase receptor (uPAR) are upregulated in<br />
neurons after experimental peripheral nerve injury <strong>and</strong> have been linked to nerve regeneration.<br />
The expression <strong>of</strong> PAI-1 <strong>and</strong> uPAR in neuronal cells in lesions <strong>of</strong> the gastrointestinal tract was<br />
analyzed by immunohistochemical techniques. PAI-1 was found in a subset <strong>of</strong> neurons primarily<br />
located in the submucosal plexus <strong>of</strong> the small <strong>and</strong> large intestine in 24 <strong>of</strong> 28 cases (86%) with<br />
Crohn’s disease, but in none <strong>of</strong> 17 cases with chronic ulcerative colitis <strong>and</strong> not in normal colon<br />
(n=5), acute appendicitis (n=9) or colon adenocarcinomas (n=17). The PAI-1 was seen in the<br />
perikarya <strong>of</strong> the neurons <strong>and</strong> a few proximal axons, whereas nerves were negative. uPAR was<br />
seen in nerves in all types <strong>of</strong> lesion varying from 21-88% <strong>of</strong> the cases, most frequent in colon<br />
adenocarcinomas. No uPAR-positive nerves were detected in normal colon. PAI-1-positive<br />
neurons in inflammatory bowel disease are linked to chronic inflammation in Crohn’s disease,<br />
implying PAI-1 as a potential parameter for the differential diagnosis between Crohn’s disease<br />
<strong>and</strong> ulcerative colitis. The findings also suggest that PAI-1 in neurons is related to pain <strong>and</strong> that<br />
both PAI-1 <strong>and</strong> uPAR are involved in neuronal repair in the inflamed tissue.<br />
<strong>Molecular</strong> & <strong>Cellular</strong> <strong>Biology</strong> <strong>of</strong> <strong>Plasminogen</strong> <strong>Activation</strong> 107
i096i<br />
The Effect <strong>of</strong> Matrix Metalloprotease 3 Deficiency<br />
in Spontaneous Metastasis<br />
Juncker-Jensen A*, Rømer J, Almholt K<br />
Finsenlaboratoriet, Rigshospitalet, København, Denmark<br />
Presenting author e-mail: ajjensen@finsenlab.dk<br />
Cancer metastasis is dependent on proteolytic degradation <strong>of</strong> extracellular matrix barriers,<br />
making extracellular proteolysis an attractive target for anti-cancer therapy. The matrix<br />
metalloprotease (MMP) family consists <strong>of</strong> 23 (human) MMPs that are involved in physiological<br />
<strong>and</strong> pathological degradation <strong>of</strong> extracellular matrix. Several MMPs are expressed in human<br />
breast cancer, <strong>and</strong> we have demonstrated that a number <strong>of</strong> MMPs are expressed in tumors in<br />
the MMTV-PyMT transgenic breast cancer model in mice. MMP-3 (stromelysin 1) is expressed<br />
in many parts <strong>of</strong> the stroma <strong>of</strong> the tumors, resembling the expression <strong>of</strong> MMP-3 in fibroblasts <strong>of</strong><br />
human breast cancers.<br />
We have now studied the effect <strong>of</strong> MMP-3 deficiency in MMTV-PyMT mice, in a cohort <strong>of</strong> 63<br />
mice consisting <strong>of</strong> 32 MMTV-PyMT,MMP3 wild-type mice <strong>and</strong> 31 MMTV-PyMT,MMP3 knockout<br />
mice. Primary tumor growth was monitored by weekly measurements <strong>of</strong> the tumor volume<br />
<strong>and</strong> lung metastasis was quantitated using unbiased, stereological methods. All mice were<br />
sacrificed at age 87 +/– 3 days. There was no difference in tumor onset or final tumor burden<br />
when comparing wild-type <strong>and</strong> MMP-3 deficient mice. The median lung metastasis volume was<br />
increased from 0,04 mm3 in wild-type mice to 0,13 mm3 in MMP-3 deficient mice. Due to large<br />
variations in the lung metastasis volumes, this increase is not significant (Mann-Whitney U test,<br />
p=0,40).<br />
We are currently analyzing lymph node metastasis in the same mice, <strong>and</strong> we are analyzing the<br />
tumor activity <strong>of</strong> potential MMP-3 targets including the metastasis-associated MMP-2 <strong>and</strong> -9.<br />
108 X I t h I n t e r n a t i o n a l W o r k s h o p o n
i097i<br />
Tumor-Cell Expression <strong>of</strong> C4.4A, a Structural Homologue<br />
<strong>of</strong> the Urokinase Receptor, Correlates with Poor<br />
Prognosis in Non-Small Cell Lung Cancer<br />
Skov BG 1 , Hansen LV 2 , Ploug M 2 , Pappot H* 2<br />
1 2 KAS Herlev, Department <strong>of</strong> Pathology, div. Gent<strong>of</strong>te, The Finsen Laboratory, Copenhagen University<br />
Hospital, Copenhagen, Denmark<br />
Presenting author e-mail: pappot@rh.regionh.dk<br />
C4.4A is a metastasis associated protein. This glycolipid-anchored protein is a structural<br />
homologue <strong>of</strong> the urokinase receptor, uPAR, which is a well-established prognostic marker in<br />
various human cancers. Although, several pilot studies demonstrate C4.4A expression in various<br />
human tumors, little is known about its prognostic significance. We therefore aim to explore<br />
the possible association between C4.4A expression <strong>and</strong> clinicopathological features <strong>and</strong> disease<br />
prognosis in patients with non-small cell lung cancer (NSCLC).<br />
Tissue sections from 109 NSCLC patients were subjected to immunohistochemical staining using<br />
a polyclonal antibody that specifically recognizes human C4.4A. Staining frequency <strong>and</strong> intensity<br />
was scored semiquantitatively <strong>and</strong> grouped into cancers with high <strong>and</strong> low expression <strong>of</strong> C4.4A.<br />
Kaplan-Meier survival curves were generated to evaluate the significance <strong>of</strong> C4.4A expression in<br />
prognosis <strong>of</strong> NSCLC patients.<br />
High C4.4A expression was observed in 44% <strong>of</strong> the specimens analyzed, <strong>and</strong> it correlates with<br />
overall survival (P=0.012). Intriguingly, a very strong correlation was noted between high<br />
expression <strong>of</strong> C4.4A in pulmonary adenocarcinoma <strong>and</strong> survival (P
i098i<br />
Urokinase Receptor Splice Variant uPAR-del4/5 <strong>and</strong><br />
rab31 mRNA Expression in Breast Cancer<br />
Magdolen V* 1 , Kotzsch M 2 , Sieuwerts A 3 , Grosser M 2 , Meye A 4 , Smid M 3 , Schmitt M 1 , Luther T 4 ,<br />
Foekens JA 3<br />
1 Institute <strong>of</strong> Pathology, Technical University Dresden, Germany;<br />
2 Clinical Research Unit, Department Obstetrics <strong>and</strong> Gynecology, Technical University München,<br />
Germany;<br />
3 Department <strong>of</strong> Medical Oncology, Erasmus Medical Center Rotterdam, Netherl<strong>and</strong>s;<br />
4 Medizinisches Labor Ostsachsen, Bautzen, Germany<br />
Presenting author e-mail: viktor.magdolen@lrz.tum.de<br />
In the present study, we evaluated the impact <strong>of</strong> mRNA expression <strong>of</strong> the uPAR splice variant<br />
uPAR-del4/5 (lacking exons 4 <strong>and</strong> 5) on metastasis-free survival (MFS) in 280 node-negative<br />
breast cancer patients. Furthermore, microarray techniques were applied to identify differentially<br />
expressed genes associated with high uPAR-del4/5 mRNA levels in tumor tissue <strong>and</strong> tumor cell<br />
lines.<br />
High uPAR-del4/5 mRNA values were strongly associated with shorter MFS <strong>of</strong> breast cancer<br />
patients (P=0.001). In multivariate analysis, uPAR-del4/5 significantly contributed to the base<br />
model <strong>of</strong> traditional prognostic factors for MFS (HR=3.29). By microarray analyses, the gene<br />
encoding rab31, a member <strong>of</strong> the Ras oncogene superfamily, was identified as one <strong>of</strong> seven<br />
genes to be more than 2-fold upregulated in tumor samples <strong>and</strong> cell lines with high uPARdel4/5<br />
mRNA expression. rab31 was selected for analysis <strong>of</strong> mRNA expression in the same set<br />
<strong>of</strong> 280 patients. High rab31 mRNA values were significantly associated with shorter DMFS in<br />
multivariate analysis (HR=2.27, P
i099i<br />
PN-1, a Serine Protease Inhibitor, Increases MMP-9 Activity<br />
in Breast Cancer Cell Line<br />
Fayard B* <strong>and</strong> Monard D<br />
Friedrich Miesher Institute, Basel, Switzerl<strong>and</strong><br />
Presenting author e-mail: berengere.fayard@fmi.ch<br />
Protease Nexin-1 (PN-1) belongs to the serpin family (serine protease inhibitor), acting on a<br />
broad range <strong>of</strong> protease including tPA, uPA, FactorXIa <strong>and</strong> thrombin. PN-1 is overexpressed in<br />
many malignant tumors, its role in cancer remains however unknown. To study its involvement<br />
in tumor cells <strong>and</strong> particularly in invasion, we used four cell lines isolated from the same mouse<br />
mammary tumor named as 67NR, 168FARN, 4T07 <strong>and</strong> 4T1 but displaying different metastatic<br />
properties once reinjected in the mouse mammary fat pad. Here we show that, in these cell lines,<br />
the level <strong>of</strong> Matrix Metalloproteinase-9 (MMP-9) activity, known to be one <strong>of</strong> the key molecules in<br />
invasion, correlates with PN-1 expression. Indeed, the less invasive cell line, 168FARN, presents<br />
the lowest MMP-9 activity but also does not express PN-1. In contrast, the three other cell lines<br />
showing high levels <strong>of</strong> MMP-9 activity express PN-1.<br />
In 168FARN, addition <strong>of</strong> PN-1 leads to an increase <strong>of</strong> secreted MMP-9. This effect is mediated<br />
through its binding to LRP (lipoprotein receptor-related protein) as indicated by the inhibitory<br />
effect <strong>of</strong> a peptide known to antagonize binding <strong>of</strong> PN-1 to LRP <strong>and</strong> by assays performed in LRP–<br />
/– MEF cells. PN-1 does not lead to an increase in MMP-9 mRNA but an increased intracellular<br />
level <strong>of</strong> the metalloprotease is detected when secretion is blocked by Brefeldin.<br />
Unexpectedly, PN-1 showed ability to increase MMP-9 activity in cancer cell lines by a mechanism<br />
dependent <strong>of</strong> its binding to LRP receptor. These results provide evidence for a new function for<br />
PN-1, which as protease inhibitor, regulates the levels <strong>of</strong> secreted MMP-9 proteinas a mean to<br />
affect the cellular invasive behavior <strong>of</strong> tumor cells.<br />
<strong>Molecular</strong> & <strong>Cellular</strong> <strong>Biology</strong> <strong>of</strong> <strong>Plasminogen</strong> <strong>Activation</strong> 111
i100i<br />
Cleavage <strong>of</strong> uPAR: Mechanism <strong>and</strong> Prognostic Significance<br />
Høyer-Hansen G*, Almasi CE, Pappot H<br />
Finsen Laboratory, Copenhagen Biocenter, Copenhagen Denmark<br />
Presenting author e-mail: gunilla@finsenlab.dk<br />
On the cell surface uPA cleaves uPAR(I-III) in the linker region between domains I <strong>and</strong> II <strong>of</strong> uPAR.<br />
Physiological concentrations <strong>of</strong> uPA cleave glycolipid-anchored uPAR but not soluble uPAR<br />
(suPAR). This is due to a difference in the conformation <strong>of</strong> the linker region between domains I<br />
<strong>and</strong> II. In media from PMA-stimulated U937 cells intact suPAR, but not cleaved, suPAR(II-III), is<br />
present even though on the cell surface both uPAR(I-III) <strong>and</strong> uPAR(II-III) are present in similar<br />
amounts. Treatment <strong>of</strong> the cells with Pi-PLC releases both uPAR forms from the cell surface.<br />
Biotinylation <strong>of</strong> cell surface proteins verified the localization <strong>of</strong> both uPAR forms, whereas nonbiotinylated<br />
uPAR(I-III) <strong>and</strong> uPAR(II-III) were found in the water-phase indicating intracellular<br />
location. When uPA mediated uPAR cleavage was inhibited by incubation with a neutralizing<br />
anti-uPA antibody, uPAR(II-III) was not found on the cell surface. The intracellular pattern <strong>of</strong><br />
uPAR(I-III) <strong>and</strong> uPAR(II-III) was not affected by inhibiting the cell surface cleavage. However, in<br />
the media from cells grown in the presence <strong>of</strong> the neutralizing anti-uPA antibody, both suPAR(I-<br />
III) <strong>and</strong> suPAR(II-III) were present. This indicates that uPAR(II-III) is shed from the cell surface<br />
when uPA-mediated cleavage <strong>of</strong> uPAR is blocked.<br />
The total amount <strong>of</strong> all uPAR forms in tumor lysates or blood correlates with prognosis in several<br />
forms <strong>of</strong> cancer. However, the amounts <strong>of</strong> the cleaved forms may be directly related to the uPA<br />
activity <strong>and</strong> in lung cancer uPAR(I) is an even stronger prognostic marker than the total amount<br />
<strong>of</strong> all uPAR forms.<br />
112 X I t h I n t e r n a t i o n a l W o r k s h o p o n
i101i<br />
Expression <strong>of</strong> Urokinase Receptor (uPAR) <strong>and</strong><br />
<strong>Plasminogen</strong> Activator Inhibitor-1 (PAI-1) in Human<br />
Colon Cancer <strong>and</strong> their Matched Liver Metastases<br />
Illemann M* 1 , Bird N 2 , Majeed A 2 , Laerum OD 1,3 , Lund LR 1 , Danø K 1 , Nielsen BS 1<br />
1 The Finsen Laboratory, Rigshospitalet, Copenhagen, Denmark;<br />
2 Academic Surgical Unit, University <strong>of</strong> Sheffield, Sheffield, Engl<strong>and</strong>;<br />
3 The Gade Institute, Haukel<strong>and</strong> University Hospital, Bergen, Norway<br />
Presenting author e-mail: millemann@finsenlab.dk<br />
In primary colon adenocarcinomas, expression <strong>of</strong> uPAR <strong>and</strong> PAI-1 is focally upregulated in<br />
the invasive front, primarily in recruited <strong>and</strong> activated inflammatory cells <strong>and</strong> my<strong>of</strong>ibroblasts.<br />
To compare the expression <strong>of</strong> uPAR <strong>and</strong> PAI-1 in primary colon adenocarcinomas with that<br />
in colon cancer liver metastases, we have analyzed matched samples from 14 patients. In the<br />
primary tumors, we found uPAR-immunoreactivity primarily in macrophages <strong>and</strong> PAI-1immunoreactivity<br />
primarily in my<strong>of</strong>ibroblasts located in the invasive front in agreement with<br />
previous findings. The growth pattern <strong>of</strong> colon cancer liver metastases can be divided into<br />
two major groups, those with desmoplastic encapsulation (desmoplastic growth pattern) <strong>and</strong><br />
those without (solid growth pattern). In the current material we had 8 <strong>and</strong> 6 cases, respectively.<br />
In all liver metastases with desmoplastic <strong>and</strong> one with solid growth pattern we found uPARimmunoreactivity<br />
primarily in macrophages <strong>and</strong> neutrophils located in the tumor edge,<br />
whereas the remaining 5 cases showing solid growth had uPAR-immunoreactivity almost only<br />
in neutrophils. PAI-1 was in cases with desmoplastic growth seen in my<strong>of</strong>ibroblasts within<br />
the desmoplastic capsule, while metastases with solid growth had only a few PAI-1 positive<br />
my<strong>of</strong>ibroblasts. Our findings suggest that metastasis-induced desmoplasia with recruitment <strong>of</strong><br />
macrophages upregulate the expression <strong>of</strong> uPAR <strong>and</strong> PAI-1 in a pattern similar to that in the<br />
primary tumors. The metastases with solid growth, in contrast, do not induce uPAR expression in<br />
the recruited macrophages <strong>and</strong> PAI-1 is limited to the sporadically appearing my<strong>of</strong>ibroblasts.<br />
<strong>Molecular</strong> & <strong>Cellular</strong> <strong>Biology</strong> <strong>of</strong> <strong>Plasminogen</strong> <strong>Activation</strong> 113
i102i<br />
A Structural Basis for Differential Cell Signaling Initiated by<br />
PAI-1 <strong>and</strong> PAI-2: Implications for Metastatic Potential<br />
Croucher D* 1 , Saunders D 1 , Ranson M 2<br />
1 Cancer Research Program, Garvan Institute <strong>of</strong> Medical Research, Sydney, Australia;<br />
2 School <strong>of</strong> Biological Sciences, University <strong>of</strong> Wollongong, Wollongong, Australia<br />
Presenting author e-mail: d.croucher@garvan.org.au<br />
Tumour expression <strong>of</strong> the uPA inhibitor PAI-1 strongly correlates with poor patient prognosis.<br />
However, tumour expression <strong>of</strong> the related uPA inhibitor PAI-2 generally correlates with good<br />
patient prognosis. Currently, there are no adequate biochemical/functional data to explain this<br />
discrepancy.<br />
One theory for the tumour-promoting effects <strong>of</strong> PAI-1 is based on the signaling events initiated<br />
upon PAI-1 inhibition <strong>of</strong> cell surface uPA. On MCF-7 cells, uPA binding to uPAR induces a<br />
transient pulse <strong>of</strong> ERK activation. Inhibition by PAI-1 unveils a cryptic high affinity site within the<br />
PAI-1 moiety that binds to members <strong>of</strong> the LDLR endocytosis receptor family. Binding <strong>of</strong> this high<br />
affinity site in PAI-1 to VLDLr sustains ERK phosphorylation <strong>and</strong> initiates cell proliferation via an<br />
as yet unknown mechanism.<br />
Through biochemical analysis we have shown that unlike PAI-1, the PAI-2 moiety <strong>of</strong> uPA:PAI-2<br />
does not contain a high affinity site for LDLR members, although the uPA:PAI-2 complex is still<br />
efficiently endocytosed by these receptors. Therefore, upon inhibition <strong>of</strong> uPA, PAI-2 does not<br />
induce the sustained ERK phosphorylation <strong>and</strong> proliferation associated with PAI-1 inhibition.<br />
This differential binding <strong>and</strong> subsequent signal propagation is possibly due to an incomplete<br />
LDLR binding motif within the helix-D <strong>of</strong> PAI-2, which is complete in the helix-D PAI-1.<br />
These data present a possible mechanism by which PAI-2 is able to clear cell surface uPA, <strong>and</strong><br />
hence proteolytic activity, via VLDLr without initiating the cell signaling events <strong>and</strong> increased<br />
metastatic potential associated with high PAI-1. This may partially explain why high tumour<br />
levels <strong>of</strong> PAI-1 correlate with poor prognosis, whereas high tumour levels <strong>of</strong> PAI-2 correlate with<br />
good prognosis.<br />
114 X I t h I n t e r n a t i o n a l W o r k s h o p o n
i103i<br />
Thrombin Induces Tumor Invasion through the Induction<br />
<strong>and</strong> Association <strong>of</strong> Matrix Metalloproteinase-9 <strong>and</strong> b-1 Integrin<br />
on the Cell Surface<br />
Bruno K* 1 , Radjabi R 2 , Sawada K 2 , Montag A 3,4 , Kossiak<strong>of</strong>f A 1 , Lengyel E 2<br />
1 Biochemistry <strong>and</strong> <strong>Molecular</strong> <strong>Biology</strong>, 2 Departments <strong>of</strong> Obstetrics <strong>and</strong> Gynecology/Section <strong>of</strong><br />
Gynecologic Oncology, 3 Pathology, 4 Committee on Cancer <strong>Biology</strong>, University <strong>of</strong> Chicago, Chicago,<br />
Illinois, USA<br />
Presenting author e-mail: kbruno@uchicago.edu<br />
The procoagulatory serine protease thrombin is known to induce invasion <strong>and</strong> metastasis in<br />
various cancers. However, the mechanisms by which it promotes tumorigenesis are poorly<br />
understood. Since the 92 kDa gelatinase (MMP-9) is a known mediator <strong>of</strong> tumor cell invasion,<br />
we sought to determine if <strong>and</strong> how thrombin regulates MMP-9. The thrombin receptor,PAR-1, is<br />
expressed in osteosarcomas, as determined by immunohistochemistry <strong>and</strong> RT-PCR. Stimulation<br />
<strong>of</strong> U2-OS osteosarcoma cells with thrombin <strong>and</strong> a thrombin receptor activating peptide (TRAP)<br />
induced pro-MMP-9 secretion as well as cell surface associated pro-MMP-9 expression <strong>and</strong><br />
proteolytic activity. This was paralleled by an increase in MMP-9 mRNA <strong>and</strong> MMP-9 promoter<br />
activity. Thrombin induced invasion <strong>of</strong> U2-OS cells through matrigel could be inhibited with<br />
a MMP-9 antibody <strong>and</strong> was mediated by the PI3-kinase signaling pathway. The stimulation<br />
<strong>of</strong> MMP-9 by thrombin was paralleled by an increase in b1-integrin mRNA <strong>and</strong> b1-integrin<br />
expression on the cell surface, which was also mediated by PI3-kinase <strong>and</strong> was also required for<br />
invasion. Thrombin activation induced <strong>and</strong> co-localized both b1-integrin <strong>and</strong> pro-MMP-9 on the<br />
cell membrane, as evidenced by coprecipitation <strong>and</strong> confocal microscopy. The thrombin mediated<br />
association <strong>of</strong> these two proteins, as well as thrombin mediated invasion <strong>of</strong> U2-OS cells could be<br />
blocked with a cyclic peptide <strong>and</strong> with an antibody preventing binding <strong>of</strong> the MMP-9 hemopexin<br />
domain to the b1-integrin I-like domain. These results suggest that thrombin induces expression<br />
<strong>and</strong> association <strong>of</strong> b1-integrin with MMP-9 <strong>and</strong> that the cell surface localization <strong>of</strong> the protease by<br />
the integrin promotes tumor cell invasion.<br />
<strong>Molecular</strong> & <strong>Cellular</strong> <strong>Biology</strong> <strong>of</strong> <strong>Plasminogen</strong> <strong>Activation</strong> 115
i104i<br />
Overexpression <strong>of</strong> Protease Nexin-1 mRNA in<br />
Oral Squamous Cell Carcinomas<br />
Gao S 1 , Krogdahl A 2 , Sørensen JA 3 , Dabelsteen E 4 , Andreasen PA* 1<br />
1 Department <strong>of</strong> <strong>Molecular</strong> <strong>Biology</strong>, University <strong>of</strong> Aarhus, Aarhus, Denmark;<br />
2 Department <strong>of</strong> Pathology, Odense University Hospital, Odense, Denmark;<br />
3 Department <strong>of</strong> Plastic Surgery, Odense University Hospital, Odense, Denmark;<br />
4 School <strong>of</strong> Dentistry, University <strong>of</strong> Copenhagen, Copenhagen, Denmark<br />
Presenting author e-mail: pa@mb.au.dk<br />
Protease nexin-1 (PN-1) belongs to the serpin family <strong>of</strong> serine protease inhibitors. It is the<br />
phylogenetically closest relative <strong>of</strong> plasminogen activator inhibitor-1 (PAI-1). PN-1 is less specific<br />
than PAI-1, inhibiting, besides uPA, also plasmin <strong>and</strong> thrombin at physiologically relevant rates.<br />
While there are numerous studies <strong>of</strong> the occurrence <strong>and</strong> functions <strong>of</strong> PAI-1 in cancer, a possible<br />
tumour biological role <strong>of</strong> PN-1 has been almost totally neglected. We have now initiated studies<br />
<strong>of</strong> the occurrence <strong>of</strong> PN-1 in tumours, also with the presumption that investigations <strong>of</strong> the tumour<br />
biological functions <strong>of</strong> PN-1 may provide clues to the uncertainty about the molecular <strong>and</strong><br />
cellular mechanisms underlying the correlation between a high PAI-1 level in tumours <strong>and</strong> a poor<br />
prognosis for the patient. We compared the level <strong>of</strong> PN-1 mRNA in 20 cases <strong>of</strong> oral squamous cell<br />
carcinomas <strong>and</strong> in matched samples <strong>of</strong> the corresponding normal oral tissues. We found that the<br />
average PN-1 levels in tumours <strong>and</strong> normal tissues were significantly different, being increased<br />
up to 13 fold in tumour samples compared with the average level in normal tissues. The PN-1<br />
mRNA level was significantly higher in tumours from patients with lymph node metastasis than<br />
in tumours from patients without. We could conclude that PN-1 is frequently overexpressed in<br />
oral squamous cell carcinoma <strong>and</strong> may correlate with lymph node metastasis. Development <strong>of</strong> an<br />
anti-PN-1 antibody suitable for immunohistochemical identification <strong>of</strong> PN-1 expressing cell types<br />
in different carcinoma types may help us to underst<strong>and</strong> its tumour biological functions.<br />
116 X I t h I n t e r n a t i o n a l W o r k s h o p o n
i105i<br />
The Matrix Metalloprotease (MMP) Inhibitor Galardin Increases<br />
Collagen Deposition <strong>and</strong> Reduces Spontaneous Metastasis<br />
in the MMTV-PymT Transgenic Breast Cancer Model<br />
Almholt K* 1 , Lærum OD 2 , Lund LR 1 , Danø K 1 , Johnsen M 3 , Rømer J 1<br />
1 Finsen Laboratory, Rigshospitalet, Copenhagen, Denmark;<br />
2 The Gade Institute, Section <strong>of</strong> Pathology, Haukel<strong>and</strong> University Hospital, Bergen, Norway;<br />
3 Department <strong>of</strong> <strong>Molecular</strong> <strong>Biology</strong>, University <strong>of</strong> Copenhagen, Copenhagen, Denmark<br />
Presenting author e-mail: kasper@finsenlab.dk<br />
Matrix metalloproteases (MMPs) <strong>and</strong> other extracellular proteases are recognized as critical<br />
factors in cancer progression. MMP inhibitors (MMPIs) have proven effective primarily by<br />
reducing growth <strong>of</strong> xenograft tumors in mice. However, small molecule MMPIs have not been<br />
tested in any transgenic/spontaneous tumor model. We chose the MMTV-PymT transgenic breast<br />
cancer model to analyze the effect <strong>of</strong> galardin/GM6001, a potent MMPI that reacts with most<br />
MMPs. Prior to the experiment on cancer-bearing mice we determined a treatment regimen based<br />
on the ability to inhibit skin wound healing in mice. We then followed a cohort <strong>of</strong> 54 MMTV-<br />
PymT-transgenic mice that received either galardin or placebo. Treatment was started at age 6<br />
weeks with galardin at 100 mg/kg/day in the form <strong>of</strong> s.c. implanted slow-release tablets. The<br />
growth <strong>of</strong> the primary tumors was reduced but not severely retarded by galardin treatment. All<br />
mice were killed at age 13½ weeks, at which time the average primary tumor burden was reduced<br />
to 1.69 cm3 in galardin-treated mice compared to 3.29 cm3 in control mice (t-test, p=0.0014). It is<br />
likely that some MMPs promote while others inhibit tumor growth, <strong>and</strong> the net effect <strong>of</strong> inhibiting<br />
a whole range <strong>of</strong> MMPs was not sufficient to prevent tumor growth. However, the tumors<br />
from galardin-treated mice <strong>of</strong>ten had a lower tumor grade as determined by histopathological<br />
evaluation. The tumors from galardin-treated mice also showed a much higher degree <strong>of</strong> collagen<br />
deposition compared to tumors from placebo-treated mice. We then quantified the total lung<br />
metastases volume in the same mice. The median metastasis volume was reduced to 0.003 mm3 in<br />
galardin-treated mice compared to 0.56 mm3 in control mice (t-test, p
i106i<br />
Proteomics <strong>of</strong> uPAR Protein: Protein Interactions in Cancer Metastasis<br />
Saldanha R, Molloy M, Xu N, Baker MS*<br />
Australian Proteome Analysis Facility Ltd <strong>and</strong> CORE in Biomolecular Frontiers, Macquarie University,<br />
Sydney, Australia<br />
Presenting author e-mail: mbaker@proteome.org.au<br />
uPAR is a key player in cancer metastasis. Our past studies show that when metastatic HCT116<br />
cells express a 5’ uPAR antisense cDNA fragment this results in (i) reduced uPAR cell surface<br />
expression; (ii) reduced cell-surface uPA binding, (iii) reduced adhesion <strong>and</strong> plasminogendependant<br />
matrix degradation, (iv) reduced Erk MAP kinase activity, Src kinase activity <strong>and</strong><br />
MMP-9 secretion; (v)reduced metastasis in Nu/Nu mice <strong>and</strong> (vi) new data that shows statistically<br />
significant expression/phosphorylation changes in only a small percentage (~4%) <strong>of</strong> the ~850<br />
proteins reproducibly detected by 2DE (e.g., stathmin, C-Myc binding protein, translation<br />
initiation factor 3, tropomyosin 3, histone H2B type 12, pr<strong>of</strong>ilin-2, importin, HSP90 to name but<br />
a few). To further characterize how uPAR operates we have now identified (<strong>and</strong> are quantifying<br />
using IP-iTRAQ) uPAR protein binding complexes from malignant OVCA 429 cells. Proteins<br />
that specifically co-purified with anti-uPAR mAbs were validated using orthogonal approaches<br />
(e.g., cross-over IP Westerns). Of particular interest were a range <strong>of</strong> signal transduction proteins,<br />
proteins previously associated with plasminogen activation (phospholipase C, LRP, <strong>and</strong> annexin<br />
A2, enolase, thrombospondin) <strong>and</strong> some novel proteins (TGF-bR2 <strong>and</strong> only the integrin, av-b6<br />
(although these cells express other integrins). Physical sites <strong>of</strong> interaction between uPAR <strong>and</strong> avb6<br />
were definitively identified by peptide mapping strategies as was direct interaction <strong>of</strong> TGF-bR2<br />
with uPAR. Functional consequences <strong>of</strong> uPAR interactions are being studied <strong>and</strong> preliminary data<br />
show that uPAR mediates many biological effects through protein:protein interactions.<br />
118 X I t h I n t e r n a t i o n a l W o r k s h o p o n
i107i<br />
A New Tagging System for Production <strong>of</strong> Recombinant Proteins in<br />
Drosophila S2 Cells Using the Third Domain <strong>of</strong> the Urokinase Receptor<br />
Gårdsvoll H* 1 , Hansen LV 1 , Jørgensen TJD 2 , Ploug M 1<br />
1 Finsen Laboratory, Rigshospitalet, Copenhagen, Denmark;<br />
2 Department <strong>of</strong> Biochemistry <strong>and</strong> <strong>Molecular</strong> <strong>Biology</strong>, University <strong>of</strong> Southern Denmark, Odense,<br />
Denmark<br />
Presenting author e-mail: gvoll@finsenlab.dk<br />
The use <strong>of</strong> protein fusion tag technology greatly facilitates detection, expression <strong>and</strong> purification<br />
<strong>of</strong> recombinant proteins, <strong>and</strong> the dem<strong>and</strong>s for new <strong>and</strong> more effective systems are therefore<br />
exp<strong>and</strong>ing. We have used a soluble truncated form <strong>of</strong> the third domain <strong>of</strong> the urokinase<br />
receptor as a convenient C-terminal fusion partner for various recombinant extracellular human<br />
proteins used in basic cancer research. The stability <strong>of</strong> this cystein-rich domain, which structure<br />
adopts a three-finger fold, provides an important asset for its applicability as a fusion tag for<br />
expression <strong>of</strong> recombinant proteins. Up to 20 mg <strong>of</strong> intact fusion protein were expressed by<br />
stably transfected Drosophila S2 cells per liter <strong>of</strong> culture using this strategy. Purification <strong>of</strong> these<br />
secreted fusion proteins from the conditioned serum free medium <strong>of</strong> S2 cells was accompanied<br />
by an efficient one-step immunoaffinity chromatography procedure using the immobilized<br />
anti-uPAR monoclonal antibody R2. An optional enterokinase cleavage site is included between<br />
the various recombinant proteins <strong>and</strong> the linker region <strong>of</strong> the tag, which enables generation <strong>of</strong><br />
highly pure preparations <strong>of</strong> tag-free recombinant proteins. Using this system we successfully<br />
produced soluble <strong>and</strong> intact recombinant forms <strong>of</strong> extracellular proteins such as CD59, C4.4A <strong>and</strong><br />
vitronectin, as well as a number <strong>of</strong> truncated domain constructs <strong>of</strong> these proteins. In conclusion,<br />
the present tagging system <strong>of</strong>fers a convenient general method for the robust expression <strong>and</strong><br />
efficient purification <strong>of</strong> a variety <strong>of</strong> recombinant proteins.<br />
<strong>Molecular</strong> & <strong>Cellular</strong> <strong>Biology</strong> <strong>of</strong> <strong>Plasminogen</strong> <strong>Activation</strong> 119
i108i<br />
Photoaffinity Labeling <strong>of</strong> uPAR with Cyclic Peptides<br />
Jacobsen B* 1 , Gårdsvoll H 1 , Barkholt V 2 , Østergaard S 3 , Ploug M 1<br />
1 Finsen Laboratory, Rigshospitalet, Copenhagen Biocenter, Denmark;<br />
2 Enzyme <strong>and</strong> Protein Chemistry, BioCentrum-DTU, The Technical University <strong>of</strong> Denmark, Denmark;<br />
3 Novo Nordisk A/S, Novo Research Park, Denmark<br />
Presenting author e-mail: bjacobsen@finsenlab.dk<br />
In view <strong>of</strong> its involvement in cancer invasion <strong>and</strong> metastasis, the high-affinity uPA-uPAR<br />
interaction represents an attractive target for rational drug design, thus requiring detailed<br />
knowledge <strong>of</strong> the receptor-lig<strong>and</strong> interface. In this study, we use photoaffinity labeling as a tool<br />
for delineation <strong>of</strong> structural aspects <strong>of</strong> this interaction. The technique enables the covalent crosslinking<br />
<strong>of</strong> two molecules by excitation <strong>of</strong> a photoactivatable probe, which thereby can abstract a<br />
hydrogen atom from a C-H-bond in its vicinity. This has been used successfully to identify the<br />
uPAR-binding sites <strong>of</strong> linear phage-display peptides. We have now synthesized a range <strong>of</strong> cyclic<br />
peptides mimicking the long b-hairpin <strong>of</strong> the growth factor-like domain <strong>of</strong> uPA, which includes<br />
residues essential for its binding to uPAR (Tyr24, Phe25, Ile28 <strong>and</strong> Trp30). In the peptides AE03<br />
<strong>and</strong> AE04, the photoprobe p-benzoyl-L-phenylalanine has been inserted at positions equivalent to<br />
Trp30 <strong>and</strong> Tyr24 in uPA, respectively, <strong>and</strong> biotin has been included as a detection <strong>and</strong> purification<br />
tag. Photolysis <strong>of</strong> uPAR-peptide complexes causes a covalent incorporation <strong>of</strong> the cyclic peptides<br />
into uPAR. The specificity <strong>of</strong> this insertion reaction was certified by the inhibition obtained when<br />
preincubating with receptor-binding derivatives <strong>of</strong> uPA. By cleavage with chymotrypsin <strong>and</strong><br />
western blotting with streptavidin, AE03 is shown to incorporate into uPAR domain I, while AE04<br />
is domains II + III-specific. These results are supported by the recently solved crystal structure<br />
<strong>of</strong> uPAR in complex with the amino-terminal fragment <strong>of</strong> uPA, revealing a hydrophobic lig<strong>and</strong>binding<br />
cavity formed by the assembly <strong>of</strong> all three domains <strong>of</strong> uPAR.<br />
120 X I t h I n t e r n a t i o n a l W o r k s h o p o n
i109i<br />
In Vivo Inhibition <strong>of</strong> the Murine uPA-uPAR Interaction using<br />
Monoclonal Antibodies Raised in uPAR Deficient Mice<br />
Rasch MG*, Pass J, Jögi A, Rønø B, Gårdsvoll H, Lund LR, Høyer-Hansen G, Lund IK<br />
Finsen Laboratory, Copenhagen Biocenter, Copenhagen, Denmark<br />
Presenting author e-mail: mrasch@finsenlab.dk<br />
The interaction between uPA <strong>and</strong> uPAR is a potential target for anti-invasive cancer therapy.<br />
Cancer invasion <strong>and</strong> metastasis is dependent on the interaction between cancer <strong>and</strong> stromal cells,<br />
which can be studied in genetically induced murine cancer models. To enable in vivo studies <strong>of</strong><br />
the effect on inhibition <strong>of</strong> uPA-uPAR binding in genetically induced murine cancer models, we<br />
have generated murine mAbs against murine uPAR (muPAR) by immunizing uPAR–/– mice with<br />
recombinant muPAR.<br />
We have selected five mAbs (mR1-mR5) <strong>of</strong> which mR1, mR3, <strong>and</strong> mR5 recognize epitopes in<br />
domain I <strong>of</strong> muPAR, while mR2 <strong>and</strong> mR4 recognize epitopes in domain II-III <strong>of</strong> muPAR. In cell<br />
binding experiments mR1 <strong>and</strong> mR4 antagonized the binding <strong>of</strong> 125I-mATF with IC50 values <strong>of</strong><br />
0.67 nM for mR1 <strong>and</strong> 0.40 nM for mR4 compared to 0.14 nM for unlabeled mATF. Additionally,<br />
mR1 could rescue 50% P388D.1 cells in an anthrax-toxin based assay, which requires cell-bound<br />
uPA to kill the cells. In contrast to all previously generated uPAR specific mAbs, mR3 binds<br />
domain I without interfering with uPA binding.<br />
In vivo efficacy <strong>of</strong> mR1 was demonstrated by the ability <strong>of</strong> mR1 to rescue mice treated with a lethal<br />
dose <strong>of</strong> uPA-activatable anthrax toxins. Another in vivo approach showed that mR1 treated<br />
tPA–/– mice mimicked the hepatic fibrin deposits <strong>of</strong> uPAR–/–/tPA–/– mice. Thus, mR1 is<br />
an efficient in vivo antagonist <strong>of</strong> the uPA-uPAR interaction <strong>and</strong> well suited for therapeutic<br />
intervention.<br />
<strong>Molecular</strong> & <strong>Cellular</strong> <strong>Biology</strong> <strong>of</strong> <strong>Plasminogen</strong> <strong>Activation</strong> 121
i110i<br />
RNA Interference for Urokinase-Targeting Limits Growth<br />
<strong>of</strong> Hepatocellular Carcinoma Xenografts in Nude Mice<br />
Salvi A*, Arici B, Barlati S, De Petro G<br />
Division <strong>of</strong> <strong>Biology</strong> <strong>and</strong> Genetics, Department <strong>of</strong> Biomedical Sciences <strong>and</strong> Biotechnology, IDET Centre<br />
<strong>of</strong> Excellence, University <strong>of</strong> Brescia, Brescia, Italy<br />
Presenting author e-mail: asalvi@med.unibs.it<br />
Gene expression <strong>of</strong> urokinase-type plasminogen activator (u-PA) is up-regulated in human<br />
hepatocellular carcinoma (HCC) <strong>and</strong> the levels <strong>of</strong> u-PA mRNA are inversely related to HCC<br />
patients’ survival. The purpose <strong>of</strong> this study was to examine the effects <strong>of</strong> vector-based RNA<br />
interference (RNAi) <strong>of</strong> u-PA on the growth <strong>of</strong> human HCC xenografts in nude mice in order to<br />
investigate the u-PA role in human HCC.<br />
Our results showed that the s.c. injection <strong>of</strong> siRNA u-PA SKHep1C3 stable transfected cells<br />
(pSsiRNAu-PA) led to a growth delay in xenograft development. The molecular characterization<br />
<strong>of</strong> nodules (carried out by PCR, RT-PCR/Agilent technology <strong>and</strong> immunoistochemical analysis)<br />
revealed the presence <strong>of</strong> plasmid DNA, the u-PA gene expression knock-down, at both mRNA<br />
<strong>and</strong> protein levels, giving evidences <strong>of</strong> a long-term <strong>and</strong> target-specific inhibition by vectorbased<br />
RNAi 11 weeks after cell inoculation. Furthermore the immunohistochemical <strong>and</strong><br />
immun<strong>of</strong>luorescence evaluation <strong>of</strong> fibronectin (FN) expression <strong>and</strong> organization revealed FN<br />
fibrils in pSsiRNAu-PA xenografts <strong>and</strong> in pSsiRNA u-PA-cells. These results represent the first<br />
experimental approach to inhibit u-PA in HCC xenografts using an ablative strategy, supporting<br />
the notion that u-PA is involved in HCC development, with a major role for u-PA in the initial<br />
phases <strong>of</strong> HCC growth; providing evidence that u-PA siRNA construct can be maintained in each<br />
xenograft for up to 11 weeks <strong>of</strong> tumour development; also identifying the ability to organize FN<br />
fibrils by SKHep1C3 cells as a downstream effect <strong>of</strong> u-PA knock-down. These data could open<br />
the possibility for experimental HCC gene therapy by vector-based RNAi against u-PA in animal<br />
models.<br />
122 X I t h I n t e r n a t i o n a l W o r k s h o p o n
i111i<br />
Potent <strong>and</strong> Broad Anti-tumor Activity <strong>of</strong> an Engineered<br />
Matrix Metalloproteinase-activated Anthrax Lethal<br />
Toxin that Targets Tumor Vasculature<br />
Liu S 1 , Wang H 1 , Currie BM 2 , Molinolo A 2 , Leung HJ 1 , Moayeri M 1 , Alfano RW 3 , Frankel AE 3 ,<br />
Leppla SH 1 , Bugge TH* 2<br />
1 Laboratory <strong>of</strong> Bacterial Diseases, NIAID, NIH, Bethesda, Maryl<strong>and</strong>, USA;<br />
2 Oral <strong>and</strong> Pharyngeal Cancer Branch, NIDCR, NIH, Bethesda, Maryl<strong>and</strong>, USA;<br />
3 Cancer Research Institute <strong>of</strong> Scott <strong>and</strong> White Memorial Hospital, Temple, Texas, USA<br />
Presenting author e-mail: thomas.bugge@nih.gov<br />
Anthrax lethal toxin (LT), which specifically inactivates MEKs, can treat human melanomas with<br />
BRAF V600E mutations, because <strong>of</strong> their addiction to the MEK-ERK pathway. To more selectively<br />
target tumors, we have developed a matrix-metalloproteinase (MMP)-activated anthrax LT, which<br />
specifically targets tumors overexpressing MMPs. Surprisingly, the MMP-activated LT has potent<br />
anti-tumor activity against a wide range <strong>of</strong> other tumor types, regardless <strong>of</strong> their BRAF mutation<br />
status. Moreover, the engineered toxin could be curative to established malignant solid tumors<br />
when used systemically, despite having very low tissue toxicity. This is largely due to the indirect<br />
targeting <strong>of</strong> tumor angiogenesis. Moreover, the engineered toxin not only exhibits much lower<br />
toxicity than wild-type LT to mice, but also shows higher toxicity to tumors because <strong>of</strong> its greater<br />
bioavailability. Thus, in theory, all tumor types are expected to respond to the MMP-activated LT<br />
therapy, <strong>and</strong> patients with tumors containing the BRAF mutation may derive additional benefits<br />
due to the direct toxicity <strong>of</strong> the toxin to the cancer cells. We are currently preparing a clinical trial<br />
to test the MMP-activated LT in cancer patients.<br />
<strong>Molecular</strong> & <strong>Cellular</strong> <strong>Biology</strong> <strong>of</strong> <strong>Plasminogen</strong> <strong>Activation</strong> 123
i112i<br />
Elucidation <strong>of</strong> the Epitope <strong>of</strong> MA-31C9, a Non-inhibitory<br />
Anti-human PAI-1 Antibody<br />
Meissenheimer LM*, Dewilde M, Compernolle G, Declerck PJ, Gils A<br />
Laboratory for Pharmaceutical <strong>Biology</strong>, Katholieke Universiteit Leuven, Leuven, Belgium<br />
Presenting author e-mail: lester.meissenheimer@pharm.kuleuven.be<br />
<strong>Plasminogen</strong> Activator Inhibitor 1 (PAI-1) is the most important physiological inhibitor <strong>of</strong><br />
plasminogen activators in vivo. MA-31C9 is a non-inhibitory monoclonal antibody raised towards<br />
human PAI-1, which is <strong>of</strong>ten used as a control antibody in studies on the evaluation <strong>of</strong> PAI-1<br />
inhibitory antibodies. The goal <strong>of</strong> this study was to elucidate the epitope <strong>of</strong> MA-31C9.<br />
Wild-type human PAI-1 has a high affinity for MA-31C9 (i.e. KA=6.8±1.9x109M-1 using surface<br />
plasmon resonance (SPR)) whereas rat PAI-1 does not bind to MA-31C9 (KA
i113i<br />
Residues outside the Epitope Determine the Function <strong>of</strong><br />
MA-159M12, an Inhibitory Anti-rat PAI-1 Antibody<br />
Meissenheimer LM*, Compernolle G, Declerck PJ, Gils A<br />
Laboratory for Pharmaceutical <strong>Biology</strong>, Katholieke Universiteit Leuven, Leuven, Belgium<br />
Presenting author e-mail: lester.meissenheimer@pharm.kuleuven.be<br />
Rat models have been shown to be suitable for in vivo investigations on thrombolysis <strong>and</strong><br />
fibrinolysis. MA-159M12 is a monoclonal antibody raised towards rat PAI-1 that exerts an<br />
inhibitory effect by accelerating the active to latent conversion. The goal <strong>of</strong> this study was to study<br />
the mechanism <strong>of</strong> action <strong>of</strong> MA-159M12.<br />
MA-159M12 has a high affinity for rat PAI-1 (KA=3.4±1.1x109M-1) but does not bind to human<br />
PAI-1 (KA
i114i<br />
Conformational Probes <strong>and</strong> Activity Regulators <strong>of</strong> <strong>Plasminogen</strong><br />
Activator Inhibitor-1, Isolated from Phage-displayed<br />
Disulphide Bridge-constrained Peptide Libraries<br />
Dupont DM, Jensen JK, Mathiasen L, Blouse GE, Wind T, Andreasen PA*<br />
Department <strong>of</strong> <strong>Molecular</strong> <strong>Biology</strong>, University <strong>of</strong> Aarhus, Aarhus, Denmark<br />
Presenting author e-mail: pa@mb.au.dk<br />
To find new probes <strong>and</strong> inhibitors <strong>of</strong> PAI-1s molecular interactions <strong>and</strong> conformational<br />
changes, we screened a phage-displayed peptide library containing 109 different sequences<br />
with the formats X7, CX7C, CX10C, <strong>and</strong> CX3CX3CX3C with human PAI-1 as bait. We isolated<br />
phages harbouring three families <strong>of</strong> peptides. One family <strong>of</strong> peptides had a consensus core<br />
motif <strong>of</strong> CFGaC, referred to a paionin-1, in which a is an aromatic residue. As determined by<br />
site-directed mutagenesis, paionin-1 bound to in a hydrophobic pocket under a-helix D <strong>and</strong><br />
inhibited the binding <strong>of</strong> uPA-PAI-1 complex to the endocytosis receptors LRP <strong>and</strong> VLDLR. A<br />
second family <strong>of</strong> peptide sequences with the formats CX7C <strong>and</strong> CX10C <strong>and</strong> the common core<br />
sequence WPRY bound to the area <strong>of</strong> PAI-1 becoming exposed upon detachment <strong>of</strong> b-str<strong>and</strong> 1C<br />
during latency transition. The access <strong>of</strong> paionin-3 to its binding site was blocked by the glycans<br />
attached to Asn267 in PAI-1 expressed in mammalian cells. A third peptide was <strong>of</strong> the format<br />
CX3CX3CX3CX5CX3CX3CX3C, will be referred to as paionin-4, <strong>and</strong> probably resulted from<br />
an unplanned cloning artefact in the library. Paionin-4 accelerated the rate <strong>of</strong> conversion <strong>of</strong><br />
PAI-1 to the latent state <strong>and</strong> had a binding area on PAI-1 overlapping with that <strong>of</strong> the latencyinducing<br />
monoclonal antibody MA33B8. Binding analyses showed that paionin-4 has a stronger<br />
affinity to conformational forms <strong>of</strong> PAI-1 with an inserted RCL than to active PAI-1. Thus, some<br />
<strong>of</strong> the isolated peptides are conformational probes, while others represent novel approaches to<br />
pharmacological interference with pathophysiological functions <strong>of</strong> PAI-1.<br />
126 X I t h I n t e r n a t i o n a l W o r k s h o p o n
i115i<br />
Urokinase-type <strong>Plasminogen</strong> Activator-inhibiting Cyclic Peptides<br />
Demonstrate New Modalities for Inhibition <strong>of</strong> Serine Proteases<br />
Andersen LM* 1 , Wind T 1 , Hansen HD 1 , Blouse GE 1 , Christensen A 1 , Jensen JK 1 , Malmendal A 2 ,<br />
Nielsen NC 2 , Andreasen PA 1<br />
1 Department <strong>of</strong> <strong>Molecular</strong> <strong>Biology</strong>, 2 Department <strong>of</strong> Chemistry, University <strong>of</strong> Aarhus, Aarhus, Denmark<br />
Presenting author e-mail: lma@mb.au.dk<br />
In order to find new principles for inhibition <strong>of</strong> the enzymatic activity <strong>of</strong> urokinase-type<br />
plasminogen activator (uPA), we screened phage-displayed r<strong>and</strong>om, disulphide bridgeconstrained<br />
peptide repertoires with human <strong>and</strong> murine uPA as baits. With human uPA, the most<br />
frequently isolated sequence was CSWRGLENHRMC, referred to as upain-1. With murine uPA,<br />
the most frequent isolated sequence was CPAYSRYLDC, referred to as mupain-1. The selected<br />
peptide sequences inhibited human or murine uPA competitively, with Ki values around 500 nM.<br />
The Ki values were in excellent agreement with the KD values determined by BIACORE analysis.<br />
By an inhibitory screen against other murine <strong>and</strong> human serine proteases, including trypsin, both<br />
upain-1 <strong>and</strong> mupain-1 were found to be highly selective for human <strong>and</strong> murine uPA, respectively.<br />
However, upain-1 did not measurably inhibit murine uPA <strong>and</strong> mupain-1 did not measurably<br />
inhibit human uPA. Site-directed mutagenesis <strong>of</strong> the peptides as well as <strong>of</strong> the enzymes identified<br />
Arg4 <strong>of</strong> upain-1 <strong>and</strong> Arg6 <strong>of</strong> mupain-1 as the P1 residues <strong>and</strong> indicated that binding specificity<br />
depends on extended binding interactions involving specific surface loops <strong>of</strong> the enzymes <strong>and</strong><br />
several residues <strong>of</strong> the peptides. Comparison <strong>of</strong> the solution structure <strong>of</strong> upain-1, as determined<br />
by NMR, <strong>and</strong> the results <strong>of</strong> the site-directed mutagenesis indicated that conformational changes <strong>of</strong><br />
the peptide are a prerequisite for upain-1-uPA binding. Peptide-derived inhibitors such as upain-<br />
1 <strong>and</strong> mupain-1 provide novel mechanistic information about enzyme-inhibitor <strong>and</strong> enzymesubstrate<br />
interactions, important tools for dissecting structural determinants <strong>of</strong> substrate <strong>and</strong><br />
inhibitor recognition, <strong>and</strong> alternative methodologies for designing effective protease inhibitors.<br />
<strong>Molecular</strong> & <strong>Cellular</strong> <strong>Biology</strong> <strong>of</strong> <strong>Plasminogen</strong> <strong>Activation</strong> 127
i116i<br />
In vivo Treatment with Monoclonal Antibodies against Mouse<br />
Urokinase-type <strong>Plasminogen</strong> Activator in Cancer Models<br />
Jögi A*, Lund IK, Høyer-Hansen G, Lund LR, Danø K, Rømer J<br />
Finsen Laboratory, Rigshospitalet, Copenhagen Biocenter, København, Denmark<br />
Presenting author e-mail: ajogi@finsenlab.dk<br />
Degradation <strong>of</strong> extra cellular matrix is pivotal to tumor metastasis <strong>and</strong> invasive growth <strong>and</strong><br />
plasmin has a well-documented role in both processes. In a transgenic breast cancer model uPAdeficiency<br />
was shown to confer reduced frequency <strong>of</strong> metastasis (Almholt et al (2005) Int J Cancer).<br />
Inhibition <strong>of</strong> the activity <strong>of</strong> uPA is hence a potential approach to anti-invasive cancer therapy. In<br />
order to evaluate this strategy preclinically in mice, reagents are needed that inhibit the activity <strong>of</strong><br />
murine uPA. This protein <strong>and</strong> its associated factors is highly species specific <strong>and</strong> although several<br />
strong inhibitors <strong>of</strong> human uPA activity are known, none <strong>of</strong> these are efficient inhibitors in the<br />
mouse. In order to develop such inhibitors, we have recently, by immunization <strong>of</strong> uPA-deficient<br />
mice with mouse uPA, generated anti-catalytic monoclonal antibodies (mAbs) against murine<br />
uPA. Here we report the first biological effects from systemic administration <strong>of</strong> such an inhibitory<br />
anti-mouse uPA mAb. In a wound healing model, where migrating leading edge keratinocytes<br />
model the invasive tumor cells, i.p. injections <strong>of</strong> anti-uPA mAb in tPA-deficient mice shifted the<br />
healing time toward that seen in tPA;uPA double-deficient mice. Increasing dose <strong>of</strong> the mAb led<br />
to increasingly delayed healing time in a dose dependent manner, approaching that <strong>of</strong> the genedeficient<br />
mice. Immunoblotting <strong>of</strong> protein extracts from the wounds reveal that less plasmin is<br />
generated in wounds <strong>of</strong> anti-uPA treated mice, compared to none-treated or mock treated mice.<br />
We are currently testing this mAb in a transgenic breast cancer model.<br />
128 X I t h I n t e r n a t i o n a l W o r k s h o p o n
Author Index<br />
(The authors present at the meeting are indicated in bold characters.)<br />
Aguilar, S, 073<br />
Ahlskog, N, 093<br />
Alfano, D, 041, 087, 111<br />
Alfano, RW, 111<br />
Allen, BJ, 072<br />
Almasi, CE, 100<br />
Almholt, K, 032, 096, 105<br />
Ampurdanés, C, 073<br />
Andersen, LM, 115<br />
Andolfo, A, 003, 051, 052<br />
Andreasen, PA, 004, 039, 048, 049,<br />
050, 053, 054, 071, 104, 114, 115<br />
Andreé, J, 010<br />
Antalis, TM, 079<br />
Ardite, E, 040<br />
Arici, B, 110<br />
Arnaudova, R, 068<br />
Astrup, A, 060<br />
Bae Kim, G, 046<br />
Baker, MS, 105<br />
Balsara, RD, 028, 086<br />
Barkholt, V, 108<br />
Barlati, S, 110<br />
Battey, F, 008<br />
Beaufort, N, 037<br />
Bednarek, R, 075<br />
Behrendt, N, 033, 034, 047<br />
Belorgey, D, 023, 091<br />
Betsholtz, C, 010<br />
Bian, C, 048<br />
Bifulco, K, 062<br />
Binder, BR, 031, 044, 061, 063<br />
Bird, N, 101<br />
Blasi, F, 035, 068<br />
Blomstr<strong>and</strong>, F, 067<br />
Blouse, GE, 004, 049, 053, 054, 114,<br />
115<br />
Bødker, JS, 053<br />
Boncela, J, 075<br />
Borger Rasmussen, H, 078<br />
Bøtkjær, KA, 049<br />
Brellier, F, 018<br />
Breuss, JM, 044<br />
Brotzge, XH, 006<br />
Brumwell, A, 013<br />
Brunner, PM, 031, 063<br />
Brünner, N, 027, 060, 084<br />
Bruno, K, 103<br />
Bugge, TH, 024, 025, 032, 033, 034,<br />
046, 078, 079, 111<br />
Byszuk, O, 049<br />
Cale, J, 010<br />
Cantelmo, AR, 062<br />
Caputi, M, 074<br />
Carlsson, L, 083<br />
Carriero, MV, 026, 041, 062<br />
Carroll, VA, 044<br />
Casslén, B, 070<br />
Castellino, FJ, 028, 038, 086<br />
Chapman, HA, 013, 042<br />
Chen, J, 045<br />
Christensen, A, 115<br />
Church, S, 009<br />
Cierniewski, CS, 075, 076<br />
Cochran, BJ, 059<br />
Cohen-Gould, L, 009<br />
Compernolle, G, 112, 113<br />
Corominas, JM, 073<br />
Croucher, D, 058, 059, 080, 102<br />
Cunningham, O, 003<br />
Currie, B, 025, 079, 111<br />
Dabelsteen, E, 071, 104<br />
Dahl, L, 083<br />
D’Alessio, S, 035<br />
Danø, K, 043, 095, 101, 105, 116<br />
De Petro, G, 110<br />
Declerck, PJ, 112, 113<br />
Degryse, B, 068, 069<br />
Del Rosso, M, 065<br />
Demyanets, S, 094<br />
Deora, AB, 009<br />
Deryugina, EI, 049<br />
Devy, L, 045<br />
Dewilde, M, 112<br />
Di Carluccio, G, 062<br />
Diaz-Ramos, A, 082<br />
Dransfield, DT, 045<br />
Dumler, I, 085, 090<br />
Dunoyer-Geindre, S, 012<br />
Dupont, DM, 050, 053, 054, 114<br />
Eden, G, 068<br />
Edwards, DR, 030<br />
Ehart, M, 061<br />
Ehnman, M, 015<br />
Ellis, V, 030<br />
Engelholm, LH, 033, 034<br />
Eriksson, U, 010, 015<br />
Espitia, C, 092<br />
Estrada, Y, 041<br />
Fayard, B, 099<br />
Fibbi, G, 065<br />
Fischer, C, 020<br />
Fish, RJ, 012<br />
Flint, A, 060<br />
Flugel, D, 011<br />
Foekens, JA, 098<br />
Folestad, E, 010<br />
Franco, P, 041, 074<br />
Frankel, AE, 111<br />
Fredriksson, L, 010, 015<br />
Fu, Q, 038<br />
Furlan, F, 068<br />
Gao, S, 071, 104<br />
Gao, Y, 010<br />
Gårdsvoll, H, 002, 034, 047, 054,<br />
107, 108, 109<br />
Gavard, J, 033<br />
Gerasi, L, 035<br />
Geyer, M, 010<br />
Gils, A, 112, 113<br />
Godiksen, S, 078<br />
González, B, 040<br />
Green, KA, 032<br />
Grosser, M, 098<br />
Gueler, F, 090<br />
Guenther, A, 039<br />
Guo, Y, 036, 093<br />
Gutkind, JS, 033<br />
Hägglöf, P, 023, 091<br />
Hagström, E, 036<br />
Hajjar, KA, 009<br />
Haller, H, 085, 090<br />
Hansen, HD, 115<br />
Hansen, LV, 097, 107<br />
Hansson, G, 070<br />
Harslund, J, 084<br />
Heier, PC, 063<br />
Helgel<strong>and</strong>, L, 095<br />
Henderikx, P, 045<br />
Henic, E, 070<br />
Herry, C, 020<br />
Higgins, PJ, 016<br />
Hill, M, 013, 042<br />
Hillig, T, 034<br />
Holmbeck, K, 033<br />
Høyer-Hansen, G, 034, 047, 070,<br />
100, 109, 116<br />
<strong>Molecular</strong> & <strong>Cellular</strong> <strong>Biology</strong> <strong>of</strong> <strong>Plasminogen</strong> <strong>Activation</strong> 129
Huang, M, 048<br />
Huber, K, 094<br />
Hultman, K, 067<br />
Iaccarino, I, 087<br />
Ibba-Manneschi, L, 065<br />
Ihara, H, 007<br />
Illemann, M, 043, 095, 101<br />
Ingvarsen, S, 034<br />
Jackson, C, 072<br />
Jacobsen, B, 108<br />
Jardí, M, 040, 089<br />
Jensen, JK, 004, 114, 115<br />
Jensen, L, 060<br />
Jerczynska, H, 076<br />
Jern, C, 067<br />
Jögi, A, 047, 109, 116<br />
Johnsen, M, 105<br />
Jørgensen, TJD, 107<br />
Juncker-Jensen, A, 096<br />
Kamikubo, Y, 069<br />
Kanse, SM, 039<br />
Karlsson-Li, S, 023<br />
Kaun, C, 094<br />
Kietzmann, T, 011<br />
Kim, Y, 013, 042<br />
Kirsch, T, 090<br />
Kiyan, J, 085<br />
Kjelgaard, S, 049<br />
Kjems, J, 050<br />
Kjøller, L, 034<br />
Kojima, S, 064<br />
Koschelnick, Y, 031<br />
Kossiak<strong>of</strong>f, A, 103<br />
Kotzsch, M, 098<br />
Kreek, MJ, 022<br />
Kristjansen, PEG, 046<br />
Krogdahl, A, 071, 104<br />
Krog-Mikkelsen, I, 060<br />
Kruith<strong>of</strong>, EKO, 012<br />
Kugler, MC, 013<br />
Kui, L, 081<br />
Lademann, U, 027<br />
Ladner, RC, 045<br />
Laerum, OD, 095, 101, 105<br />
Larsen, L, 027<br />
Larsson, G, 029<br />
Lawrence, DA, 010, 056<br />
Lee, JA, 080<br />
Lengyel, E, 103<br />
Leppla, SH, 046, 111<br />
Leung, HJ, 111<br />
Ley, A, 045<br />
Li, H, 015<br />
Li, J, 036, 088<br />
Li, J, 017<br />
Li, S, 056<br />
Li, X, 001<br />
Liguori, E, 062<br />
Lillis, AP, 008<br />
Ling, Q, 009<br />
List, K, 024, 025, 079<br />
Liu, S, 046, 111<br />
Llorens, A, 082<br />
Lobov, S, 058, 059<br />
Lochner, JE, 021<br />
Lomas, DA, 023, 091<br />
Longanesi-Cattani, I, 062<br />
López-Alemany, R, 082<br />
Lu, W, 001<br />
Lund, IK, 047, 109, 116<br />
Lund, LR, 032, 043, 047,<br />
101,105,109,116<br />
Luque, T, 082<br />
Luther, T, 098<br />
Lüthi, A, 020<br />
Lyden, D, 009<br />
Mackie, I, 045<br />
Madsen, CD, 003, 051, 066<br />
Madsen, JB, 050<br />
Madsen, DH, 034<br />
Magdolen, V, 037, 098<br />
Maiya, R, 022<br />
Majeed, A, 101<br />
Malisauskas, M, 077<br />
Mallya, M, 091<br />
Malmendal, A, 115<br />
Manch<strong>and</strong>a, N, 055<br />
Mancini, A, 074<br />
Manetti, M, 065<br />
Mann, K, 010<br />
Margheri, F, 065<br />
Markart, P, 039<br />
Mathiasen, L, 114<br />
Maurer, G, 094<br />
Mazzieri, R, 035<br />
Medcalf, R, 067<br />
Meins, M, 020<br />
Meissenheimer, LM, 112, 113<br />
Mengel, M, 090<br />
Meye, A, 098<br />
Meyer, CA, 086<br />
Michos, O, 018<br />
Migliorini, M, 008<br />
Mihaly, J, 031, 044, 063<br />
Mikhailenko, I, 008<br />
Minor, KH, 004, 054<br />
Moayeri, M, 111<br />
Mogami, H, 007<br />
Molinolo, A, 024, 025, 079, 111<br />
Molloy, M, 105<br />
Monard, D, 018, 020, 099<br />
Montag, A, 103<br />
Montuori, N, 026<br />
Moreno, E, 018, 020<br />
Morin, SJ, 086<br />
Morozova-Roche, L, 077<br />
Mortensen, KK, 049<br />
Morty, RE, 039<br />
Muñoz-Cánoves, P, 040, 089<br />
Naa, L, 045<br />
Navarro, P, 073<br />
Neels, JG, 069<br />
Netti, PA, 041<br />
Netzel-Arnett, S, 079<br />
Neville, DM, 046<br />
Nielsen, BS, 043, 095, 101<br />
Nielsen, NC, 115<br />
Nielsen, OL, 084<br />
Nieves-Li, EC, 055<br />
Nilsson, M, 067<br />
Norris, EH, 022<br />
Noskova, V, 070<br />
Ny, T, 036, 077, 081, 088, 091, 093<br />
Nyl<strong>and</strong>er, A, 081<br />
Offenberg, H, 020, 084<br />
Olausson, B, 029, 083<br />
Ol<strong>of</strong>sson, A, 077<br />
Orolicki, S, 018<br />
Ortiz-Zapater, E, 073<br />
Ossowski, L, 041<br />
Østergaard, S, 108<br />
Øvrebø, K, 095<br />
Owen, K, 030<br />
Pabba, M, 077<br />
Pappot, H, 097, 100<br />
Park, J-K, 090<br />
Pass, J, 109<br />
Paul, J, 019<br />
Pawlowska, Z, 076<br />
Pedersen, EDK, 078<br />
Peiró, S, 073<br />
Perron, MJ, 054<br />
Peterson, CB, 004, 054<br />
Pfaffenberger, S, 094<br />
Phillips, RL, 091<br />
Pietras, K, 010<br />
Pirazzoli, V, 051<br />
Pizzo, SV, 008<br />
Pliyev, BK, 014<br />
Ploplis, VA, 028,086<br />
Ploug, M, 002, 032, 047, 054, 097,<br />
107, 108<br />
Polavarapu, R, 006<br />
Potempa, J, 037<br />
Prager, GW, 031, 044, 063<br />
130 X I t h I n t e r n a t i o n a l W o r k s h o p o n
Preissner, KT, 039<br />
Priglinger, U, 063<br />
Prorok, M, 038<br />
Przygodzka, P, 029, 083<br />
Przygodzki, T, 077, 091<br />
Pucci, M, 065<br />
Qiu, D, 030<br />
Quigley, JP, 049<br />
Rabbani, SA, 045<br />
Raben, A, 060<br />
Radjabi, R, 103<br />
Rafii, S, 009<br />
Ragno, P, 026<br />
Rank, F, 043<br />
Ranson, M, 038, 058, 059, 080, 102<br />
Rasch, MG, 109<br />
Real, FX, 073<br />
Rega, G, 094<br />
Ricci, P, 026<br />
Robillard, L, 013<br />
Robinson, S, 008<br />
Roda, O, 073<br />
Rømer, J, 032, 046, 047, 096, 105, 116<br />
Rømer, MU, 027<br />
Rong, S, 090<br />
Rønø, B, 046, 109<br />
Rosales, L, 092<br />
Rossi, G, 026<br />
Rotoli, B, 026<br />
Ruan, J, 009<br />
Ruiz, BH, 092<br />
Ruskowski, M, 045<br />
Rychli, K, 094<br />
Saldanha, R, 105<br />
Salvi, A, 110<br />
Samarakoon, R, 016<br />
S<strong>and</strong>erson-Smith, ML, 038<br />
Sarra Ferraris, GM, 003, 066<br />
Saunders, D, 102<br />
Sawada, K, 103<br />
Scalettar, BA, 021<br />
Schar, CR, 004, 054<br />
Scharschmidt, T, 025<br />
Schmitt, M, 037, 098<br />
Schuttner, LC, 021<br />
Schwartz, BS, 056<br />
Segre, J, 025<br />
Selleri, C, 026<br />
Selzer-Plon, J, 078<br />
Serrano, AL, 089<br />
Serrati, S, 065<br />
Sharp, LK, 023<br />
Shireman, J, 025<br />
Shore, JD, 054<br />
Shushakova, N, 085, 090<br />
Sidenius, N, 003, 051, 052, 066<br />
Sidman, RL, 017<br />
Sieuwerts, A, 098<br />
Skarstein, A, 095<br />
Skov, BG, 097<br />
Sloth, B, 060<br />
Smid, M, 098<br />
Smith, RC, 072<br />
Smolarczyk, K, 075<br />
Snyder, EY, 017<br />
Sommerh<strong>of</strong>f, CP, 037<br />
Song, E, 072<br />
Sørensen, JA, 071, 104<br />
Spangler, E, 021<br />
Spina, R, 062<br />
Stochl, M, 045<br />
Stoppelli, MP, 041, 062, 074, 087<br />
Strickl<strong>and</strong>, DK, 008, 010<br />
Strickl<strong>and</strong>, S, 019, 022<br />
Su, EJ, 010<br />
Suelves, M, 089<br />
Sui, G-Z, 009<br />
Sulniute, R, 088<br />
Suzuki, Y, 007<br />
Szabo, R, 024, 025, 079<br />
Taieb, S, 018<br />
Tang, CH, 013, 042<br />
Té, H, 018<br />
Tengel, T, 029<br />
Tholstrup, T, 060<br />
Tjärnlund-Wolf, A, 067<br />
Tkachuk, N, 085<br />
Tkachuk, S, 085<br />
Tkachuk, VA, 014<br />
Toews, M, 045<br />
Urano, T, 007<br />
Vaillant, C, 018<br />
Vallecillo, AJ, 092<br />
van Gool, R, 045<br />
Vidal, B, 040, 089<br />
Visconte, V, 026<br />
Vocca, I, 041<br />
Vogel, LK, 078<br />
Votta, G, 041, 074<br />
Wagenaar-Miller, RA, 033, 034<br />
Wahlberg, P, 081<br />
Waisman, DM, 057<br />
Walker, MJ, 038<br />
Wang, H, 111<br />
Wei, Y, 013, 042<br />
Wei, Z, 005<br />
Wilczynska, M, 029, 077, 083<br />
Wind, T, 039, 048, 114, 115<br />
Wojciechowski, P, 037<br />
Wojta, J, 094<br />
Wygrecka, M, 039<br />
Xolalpa, W, 092<br />
Xu, N, 105<br />
Xue, A, 072<br />
Xue, M, 072<br />
Yamada, S, 033<br />
Yan, L, 009<br />
Yepes, M, 006, 010<br />
Yuan, C, 048<br />
Yuan, W, 001<br />
Zeller, R, 018<br />
Zhao, G, 048<br />
Zhou, A, 005<br />
Zhou, Y, 022<br />
Zou, G, 001<br />
<strong>Molecular</strong> & <strong>Cellular</strong> <strong>Biology</strong> <strong>of</strong> <strong>Plasminogen</strong> <strong>Activation</strong> 131
Attendees<br />
Ahlskog, Nina<br />
Umeå University<br />
nina.ahlskog@medchem.umu.se<br />
Alfano, Daniela<br />
Institute <strong>of</strong> Genetics & Biophysics<br />
alfano@igb.cnr.it<br />
Almholt, Kasper<br />
Finsen Laboratory<br />
kasper@finsenlab.dk<br />
Alpízar Alpízar, Warner<br />
The Gades Institute - Haukel<strong>and</strong> University<br />
Hospital<br />
awarnercr@yahoo.com<br />
Andersen, Lisbeth Moreau<br />
University <strong>of</strong> Aarhus<br />
lma@mb.au.dk<br />
Andolfo, Annapaola<br />
Fondazione Ifom<br />
annapaola.<strong>and</strong>olfo@ifom-ieo-campus.it<br />
Andreasen, Peter A.<br />
University <strong>of</strong> Aarhus<br />
pa@mb.au.dk<br />
Antalis, Toni<br />
University <strong>of</strong> Maryl<strong>and</strong> School <strong>of</strong> Medicine<br />
tantalis@som.umaryl<strong>and</strong>.edu<br />
Ardite, Esther<br />
Center for Genomic Regulation (CRG)<br />
esther.ardite@crg.es<br />
Baker, Mark<br />
Australian Proteome Analysis Facility<br />
mbaker@proteome.org.au<br />
Balsara, Rashna<br />
University <strong>of</strong> Notre Dame<br />
rbalsara@nd.edu<br />
Beaufort, Nathalie<br />
KliFo der Frauenklinik, TU München<br />
nbeaufortgbb@yahoo.fr<br />
Bednarek, Radoslaw<br />
Polish Academy <strong>of</strong> Science - Lodz<br />
rbednarek@cbm.pan.pl<br />
Behrendt, Niels<br />
Finsen Laboratory, Rigshospitalet<br />
niels.behrendt@finsenlab.dk<br />
Binder, Bernd R.<br />
Medical University <strong>of</strong> Vienna<br />
bernd.binder@univie.ac.at<br />
Blasi, Francesco<br />
Fondazione Ifom<br />
francesco.blasi@ifom-ieo-campus.it<br />
Bødker, Julie Støve<br />
University <strong>of</strong> Aarhus<br />
jsb@mb.au.dk<br />
Brunner, Patrick<br />
Medical University <strong>of</strong> Vienna<br />
patrick.brunner@meduniwien.ac.at<br />
Bruno, Katharina<br />
University <strong>of</strong> Chicago<br />
kbruno@uchicago.edu<br />
Bugge, Thomas<br />
National Institutes <strong>of</strong> Health<br />
tbugge@mail.nih.gov<br />
Chapman, Hal<br />
University <strong>of</strong> California San Francisco<br />
hal.chapman@ucsf.edu<br />
Cierniewski, Czeslaw<br />
Polish Academy <strong>of</strong> Sciences<br />
cciern@zdn.am.lodz.pl<br />
Cochran, Blake<br />
University <strong>of</strong> Wollongong<br />
blake@uow.edu.au<br />
Croucher, David<br />
University <strong>of</strong> Wollongong<br />
d.croucher@garvan.org.au<br />
Dano, Keld<br />
Finsen Laboratory<br />
kelddano@dadlnet.dk<br />
Degryse, Bernard<br />
Fondazione Ifom<br />
degryse.bernard@hsr.it<br />
Del Rosso, Mario<br />
University <strong>of</strong> Florence<br />
delrosso@unifi.it<br />
Devy, Laetitia<br />
DYAX SA<br />
ldevy@dyax.com<br />
Diaz Ramos, Mª Angeles<br />
Institut Investigacio BiomedicaBellvitge<br />
madiaz@idibell.org<br />
Dumler, Inna<br />
Hannover Medical School<br />
dumler.inna@mh-hannover.de<br />
Dupont, Daniel<br />
University <strong>of</strong> Aarhus<br />
dmd@mb.au.dk<br />
Eden, Gabriele<br />
Fondazione Ifom<br />
gabriele.eden@ifom-ieo-campus.it<br />
132 X I t h I n t e r n a t i o n a l W o r k s h o p o n
Ehart, Monika<br />
Medical University <strong>of</strong> Vienna<br />
monika.ehart@meduniwien.ac.at<br />
Ehnman, Monika<br />
Ludwig Institute for Cancer Research<br />
monika.ehnman@licr.ki.se<br />
Ellis, Vincent<br />
University <strong>of</strong> East Anglia<br />
v.ellis@uea.ac.uk<br />
Fayard, Berengere<br />
Friedrich Miescher Institute for Biomedical<br />
Research<br />
berengere.fayard@fmi.ch<br />
Fibbi, Gabriella<br />
University <strong>of</strong> Florence<br />
fibbi@unifi.it<br />
Fish, Richard<br />
Geneva University Medical Faculty <strong>and</strong> University<br />
Hospital<br />
Richard.Fish@medecine.unige.ch<br />
Franco, Paola<br />
Institute <strong>of</strong> Genetics & Biophysics<br />
franco@igb.cnr.it<br />
Friberger, Petfer<br />
DiA-Service/American Diagnostica<br />
petter.friberger@dia-service.se<br />
Gårdsvoll, Henrik<br />
Finsen Laboratory, Rigshospitalet<br />
gvoll@finsenlab.dk<br />
Gils, Ann<br />
Laboratory for Pharmaceutical <strong>Biology</strong>, KULeuven<br />
ann.gils@pharm.kuleuven.be<br />
Godiksen, Sine<br />
University <strong>of</strong> Copenhagen<br />
sinego@imbg.ku.dk<br />
Guo, YongZhi<br />
Umeå University<br />
Yong-zhi.guo@medchem.umu.se<br />
Hägglöf, Peter<br />
University <strong>of</strong> Cambridge<br />
pmh43@cam.ac.uk<br />
Hajjar, Katherine<br />
Weill Cornell Medical College<br />
khajjar@med.cornell.edu<br />
Harslund, Jakob<br />
University <strong>of</strong> Copenhagen<br />
jhar@life.ku.dk<br />
Henic, Emir<br />
University Hospital Lund<br />
emir.henic@med.lu.se<br />
Høyer-Hansen, Gunilla<br />
Finsen Laboratory<br />
gunilla@finsenlab.dk<br />
Huang, Mingdong<br />
Chinese Academy <strong>of</strong> Sciences<br />
mhuang@fjirsm.ac.cn<br />
Hultman, Karin<br />
Institution <strong>of</strong> Neurosciences <strong>and</strong> Physiology<br />
karin.hultman@neuro.gu.se<br />
Illemann, Martin<br />
Finsen Laboratory<br />
millemann@finsenlab.dk<br />
Jacobsen, Benedikte<br />
Finsen Laboratory, Rigshospitalet<br />
bjacobsen@finsenlab.dk<br />
Jensen, Lotte<br />
University <strong>of</strong> Copenhagen<br />
lje@life.ku.dk<br />
Jerczynska, Hanna<br />
Medical University <strong>of</strong> Lodz - Pol<strong>and</strong><br />
hanuka@zdn.am.lodz.pl<br />
Jerke, Uwe<br />
Franz-Volhard-Klink, Charite-Buch Berlin<br />
uwe.jerke@charite.de<br />
Jern, Christina<br />
Institution <strong>of</strong> Neurosciences <strong>and</strong> Physiology<br />
christina.jern@neuro.gu.se<br />
Juncker-Jensen, Anna<br />
Finsen Laboratory<br />
ajjensen@finsenlab.dk<br />
Kietzmann, Thomas<br />
University <strong>of</strong> Kaiserslautern<br />
tkietzm@gwdg.de<br />
Kinnby, Bertil<br />
Malmö University College<br />
Bertil.Kinnby@od.mah.se<br />
Kojima, Soichi<br />
<strong>Molecular</strong> <strong>Cellular</strong> Pathology Research Unit,<br />
RIKEN<br />
skojima@postman.riken.go.jp<br />
Kruith<strong>of</strong>, Egbert<br />
University Hospital <strong>of</strong> Geneva<br />
egbert.kruith<strong>of</strong>@hcuge.ch<br />
Kusch, Angelika<br />
Charite-Campus Buch, Dept <strong>of</strong> <strong>Molecular</strong> <strong>and</strong><br />
Clinical Cardiology<br />
angelika.kusch@charite.de<br />
Lademann, Ulrik<br />
University <strong>of</strong> Copenhagen<br />
ul@life.ku.dk<br />
Laerum, Ole Didrik<br />
The Gade Institute, University <strong>of</strong> Bergen<br />
ole.laerum@gades.uib.no<br />
Lawrence, Daniel<br />
University <strong>of</strong> Michigan Medical School<br />
dlawrenc@med.umich.edu<br />
Lee, Jodi<br />
University <strong>of</strong> Wollongong<br />
jal31@uow.edu.au<br />
Li, Jianxue<br />
BIDMC, Harvard Medical School<br />
jli7@caregroup.harvard.edu<br />
<strong>Molecular</strong> & <strong>Cellular</strong> <strong>Biology</strong> <strong>of</strong> <strong>Plasminogen</strong> <strong>Activation</strong> 133
Li, Jinan<br />
Umeå University<br />
jinan.li@medchem.umu.se<br />
Li, Shih-Hon<br />
University <strong>of</strong> Illinois at Urbana-Champaign<br />
sli3@uiuc.edu<br />
Lillis, Anna<br />
University <strong>of</strong> Maryl<strong>and</strong> School <strong>of</strong> Medicine<br />
alillis@som.umaryl<strong>and</strong>.edu<br />
Liu, Kui<br />
Umeå University<br />
kui.liu@medchem.umu.se<br />
Lobov, Sergei<br />
University <strong>of</strong> Wollongong<br />
sergei@uow.edu.au<br />
Lochner, Janis<br />
Lewis & Clark College<br />
lochner@lclark.edu<br />
Longanesi Cattani, Immacolata<br />
National Cancer Institute <strong>of</strong> Naples - Italy<br />
immalonganesi@libero.it<br />
Lu, Wuyuan<br />
University <strong>of</strong> Maryl<strong>and</strong><br />
luw@umbi.umd.edu<br />
Lund, Ida K.<br />
Finsen Laboratory<br />
ikl@finsenlab.dk<br />
Lund, Leif R.<br />
Finsen Laboratory<br />
lund@inet.uni2.dk<br />
Madsen, Chris<br />
Fondazione Ifom<br />
chris.madsen@ifom-ieo-campus.it<br />
Magdolen, Viktor<br />
Clinical Research Unit, TU München<br />
viktor-magdolen@lrz.tum.de<br />
Maiya, Rajani<br />
The Rockefeller University<br />
rmaiya@mail.rockefeller.edu<br />
Manch<strong>and</strong>a, Naveen<br />
University <strong>of</strong> Illinois at Urbana-Champaign<br />
manch<strong>and</strong>@uiuc.edu<br />
Markart, Philipp<br />
University <strong>of</strong> Giessen Lung Center<br />
philipp.markart@innere.med.uni-giessen.de<br />
Meins, Marita<br />
Friedrich Miescher Institute for Biomedical<br />
Research<br />
mmeins@fmi.ch<br />
Meissenheimer, Lester<br />
KULeuven: Lab Pharmaceutical <strong>Biology</strong><br />
lester.meissenheimer@pharm.kuleuven.be<br />
Mihaly, Judit<br />
Medical University <strong>of</strong> Vienna<br />
judit.mihaly@meduniwien.ac.at<br />
Monard, Denis<br />
Friedrich Miescher Institute for Biomedical<br />
Research<br />
monard@fmi.ch<br />
Navarro, Pilar<br />
Institut Municipal dInvestigació Mèdica<br />
pnavarro@imim.es<br />
Nielsen, Boye Schnack<br />
Finsen Laboratory, Rigshospitalet<br />
schnack@finsenlab.dk<br />
Nieves-Li, Evelyn<br />
University <strong>of</strong> Illinois at Urbana-Champaign<br />
enieves@uiuc.edu<br />
Nuttall, Robert<br />
Dalhousie University<br />
r.nuttall@dal.ca<br />
Ny, Tor<br />
Umeå University<br />
tor.ny@medchem.umu.se<br />
Olausson, Björn<br />
Umeå University<br />
bjorn.olausson@medchem.umu.se<br />
Pabba, Mohan<br />
Umeå University<br />
pabba.mohan@medchem.umu.se<br />
Pappot, Helle<br />
Rigshospitalet 5073<br />
pappot@rh.regionh.dk<br />
Paul, Justin<br />
The Rockefeller University<br />
jpaul@rockefeller.edu<br />
Peterson, Cynthia<br />
University <strong>of</strong> Tennessee<br />
cbpeters@utk.edu<br />
Pirazzoli, Valentina<br />
Fondazione Ifom<br />
valentina.pirazzoli@ifom-ieo-campus.it<br />
Pliyev, Boris<br />
Moscow State University<br />
bpliyev@cardio.ru<br />
Ploug, Michael<br />
Finsen Laboratory<br />
m-ploug@finsenlab.dk<br />
Prager, Gerald<br />
Medical University <strong>of</strong> Vienna<br />
gerald.prager@meduniwien.ac.at<br />
Przygodzka, Patrycja<br />
Umeå University<br />
patrycja.przygodzka@medchem.umu.se<br />
Przygodzki, Tomasz<br />
Umeå University<br />
tomasz.przygodzki@medchem.umu.se<br />
Ragno, Pia<br />
University <strong>of</strong> Salerno<br />
pragno@unisa.it<br />
134 X I t h I n t e r n a t i o n a l W o r k s h o p o n
Ranson, Marie<br />
University <strong>of</strong> Wollongong<br />
mranson@uow.edu.au<br />
Rasch, Morten<br />
Finsen Laboratory<br />
mrasch@finsenlab.dk<br />
Resnati, Massimo<br />
S.Raffaele Hospital- DIBIT<br />
resnati.massimo@hsr.it<br />
Rønø, Birgitte<br />
Finsen Laboratory<br />
brono@finsenlab.dk<br />
Salvi, Aless<strong>and</strong>ro<br />
University <strong>of</strong> Brescia<br />
asalvi@med.unibs.it<br />
Sarra Ferraris, Gian Maria<br />
Fondazione Ifom<br />
gianmaria.sarraferraris@ifom-ieo-campus.it<br />
Schmitt, Manfred<br />
Clinical Research Unit, Dept. Obstetrics <strong>and</strong><br />
Gynecology<br />
manfred.schmitt@LRZ.tum.de<br />
Schwartz, Brad<br />
University <strong>of</strong> Illinois at Urbana-Champaign<br />
comuc@med.uiuc.edu<br />
Sidenius, Nicolai<br />
Fondazione Ifom<br />
nicolai.sidenius@ifom-ieo-campus.it<br />
Stoppelli, Maria Patrizia<br />
Institute <strong>of</strong> Genetics & Biophysics<br />
stoppell@igb.cnr.it<br />
Strickl<strong>and</strong>, Dudley<br />
University <strong>of</strong> Maryl<strong>and</strong> School <strong>of</strong> Medicine<br />
dstrickl<strong>and</strong>@som.umaryl<strong>and</strong>.edu<br />
Sulniute, Rima<br />
Umeå University<br />
rima.sulniute@medchem.umu.se<br />
Suzuki, Yuko<br />
Hamamatsu University School <strong>of</strong> Medicine<br />
seigan@hama-med.ac.jp<br />
Szabo, Roman<br />
National Institutes <strong>of</strong> Health<br />
rszabo@nidcr.nih.gov<br />
Tkachuk, Sergey<br />
Hannover Medical School<br />
Tkatchouk.Sergei@mh-hannover.de<br />
Urano, Tetsumei<br />
Hamamatsu University School <strong>of</strong> Medicine<br />
uranot@hama-med.ac.jp<br />
Vidal, Berta<br />
Center for Genomic Regulation (CRG)<br />
berta.vidal@crg.es<br />
Vogel, Lotte Katrine<br />
University <strong>of</strong> Copenhagen<br />
vogel@imbg.ku.dk<br />
Wahlberg, Patrik<br />
Umeå University<br />
patrik.wahlberg@medchem.umu.se<br />
Wei, Ying<br />
University <strong>of</strong> California San Francisco<br />
ying.wei@ucsf.edu<br />
Wikström, Clas<br />
Umeå University<br />
clas.wikstrom@medchem.umu.se<br />
Wilczynska, Malgorzata<br />
Umeå University<br />
Malgorzata.Wilczynska@medchem.umu.se<br />
Wojta, Johann<br />
Medical University <strong>of</strong> Vienna<br />
johann.wojta@meduniwien.ac.at<br />
Wygrecka, Malgorzata<br />
University <strong>of</strong> Giessen Lung Center<br />
malgorzata.wygrecka@innere.med.uni-giessen.de<br />
Xolalpa, Wendy<br />
Instituto de Investigaciones Biomedicas UNAM<br />
wendyxolalpa@yahoo.com.mx<br />
Xue, Aiqun<br />
University <strong>of</strong> Sydney Royal North Shore Hospital<br />
aiqunn@med.usyd.edu.au<br />
Yepes, Manuel<br />
Emory University<br />
myepes@emory.edu<br />
Zhou, Aiwu<br />
University <strong>of</strong> Cambridge<br />
awz20@cam.ac.uk<br />
<strong>Molecular</strong> & <strong>Cellular</strong> <strong>Biology</strong> <strong>of</strong> <strong>Plasminogen</strong> <strong>Activation</strong> 135
Notes<br />
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .<br />
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .<br />
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .<br />
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .<br />
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .<br />
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .<br />
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .<br />
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .<br />
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .<br />
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .<br />
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .<br />
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .<br />
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .<br />
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .<br />
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .<br />
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .<br />
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .<br />
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .<br />
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .<br />
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .<br />
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .<br />
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .<br />
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .<br />
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .<br />
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .<br />
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .<br />
136 X I t h I n t e r n a t i o n a l W o r k s h o p o n