Streptococcus bovis - Gundersen Lutheran Health System
Streptococcus bovis - Gundersen Lutheran Health System
Streptococcus bovis - Gundersen Lutheran Health System
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
outCoMeS froM A SCreeninG proCedure for orophArynGeAL dySphAGiA<br />
Pathway (ASCP)—for evaluating and treating acute stroke patients<br />
admitted to our medical center. Various stroke pathways have been<br />
described elsewhere 12,28 and have been found to be efficacious for<br />
caring for acute stroke patients.<br />
In conjunction with the ASCP and based upon previous literature<br />
concerning bedside screening examinations for oropharyngeal<br />
dysphagia, 3,5,13-15,18,19,21,22,28-42 3 of the authors developed a screening<br />
tool, <strong>Gundersen</strong> <strong>Lutheran</strong> Acute Dysphagia Screen (GLADS), for<br />
use by nurses. In brief, GLADS used a checklist that incorporated<br />
several observable risk factors (ie, Critical Criteria) relevant for<br />
both dysphagia and aspiration, and assessment tools for secretions,<br />
swallowing frequency, and water swallows. 26,31,33,40,41 Prior to using<br />
it with stroke patients, a select cadre of 20 registered nurses was<br />
trained by the 3 authors to administer GLADS.<br />
Through the ASCP, medically stable and adequately alert<br />
patients were screened a minimum of 3 times following admission<br />
and up to 48 hours prior to a consultation being generated for more<br />
comprehensive evaluation of swallowing function. Observations<br />
of (1) 1 or more critical criteria, (2) continuous intermittent<br />
coughing on secretions, (3) coughing with water swallow trials, 32,33<br />
or (4) swallowing frequency fewer than 1 per minute or 4 per<br />
5 minutes 40,41 denoted failure on GLADS, prompted a nothing<br />
by mouth order, and generated referral for further evaluation.<br />
If available in liquid form, necessary medications were given<br />
intravenously or intramuscularly.<br />
Results from a pilot study using GLADS for 118 acute<br />
stroke patients showed that none developed either pneumonia<br />
or malnutrition during hospitalization or at 3-month followup<br />
and suggested that trained nurses could effectively implement<br />
a screening procedure for dysphagia following stroke. 43,44 The<br />
purpose of the current retrospective investigation was to (1)<br />
determine the outcomes for pneumonia and nutrition for patients<br />
admitted through the ASCP between 1998 and 2006 and<br />
undergoing GLADS as part of the stroke protocol, (2) determine<br />
the effectiveness of GLADS as a screening procedure for dysphagia<br />
and aspiration, and (3) compare the neurological characteristics of<br />
patients who passed GLADS with those of patients who failed.<br />
MethodS<br />
Approval for retrospective review of patient medical records<br />
was obtained from <strong>Gundersen</strong> <strong>Lutheran</strong> <strong>Health</strong> <strong>System</strong>’s<br />
Research Committee and Institutional Review Board. All<br />
patients admitted through the ASCP between January 1998 and<br />
December 2006 were identified by service code and their medical<br />
records reviewed by the authors. Of these, the records of those<br />
patients who underwent screening using GLADS were reviewed<br />
for outcomes during hospitalization and at 35 days following<br />
discharge from hospital. A determination of pneumonia was made<br />
by reviewing the comments and diagnoses made by the primary<br />
service (typically internal medicine or neurology) or pulmonary<br />
medicine and the findings from chest radiographs. Nutritional<br />
status was determined by reviewing the nutritional assessment<br />
recommendations made by registered dieticians or the metabolic<br />
support team. General statistical associations and proportion<br />
comparisons with categorical variables were assessed with the χ 2<br />
test. The Fisher exact test was used in place of the χ 2 test when at<br />
least 25% of the cells had counts less than 5. Univariate logistical<br />
models were used when predictive ability was tested. The cost and<br />
length-of-stay comparisons between groups were done with the<br />
Wilcoxon rank sum test of equal distributions. Exact confidence<br />
limits were calculated for the reported odds ratio. A P value < .05<br />
was considered significant.<br />
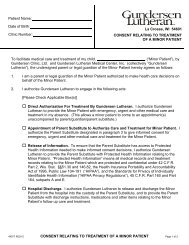
<strong>Gundersen</strong> <strong>Lutheran</strong> Acute Dysphagia Screen<br />
(GLADS)<br />
reSuLtS<br />
Seven hundred fifty-three stroke patients, average age 74 years,<br />
had GLADS administered in conjunction with the ASCP between<br />
January 1998 and December 2006. Five hundred seventy-eight<br />
patients (77%) passed GLADS. Of these, 571 did not undergo<br />
further assessment for dysphagia prior to implementation of an<br />
oral diet; the remaining 7 patients had normal VFSS test results<br />
and were started on an oral diet subsequent to study. However, 4<br />
of these patients had inadequate oral intake and were given enteral<br />
feedings, as well. One hundred seventy-five patients (23%) failed<br />
GLADS and went on for further evaluation (ie,VFSS, fiberoptic<br />
study of swallow, 29,45 or both) and treatment.<br />
Of the patients passing GLADS, 287 were men and 291 were<br />
women. By report, 10 patients had premorbid dysphagia, although<br />
its nature was unclear. Although 1 patient was described as having<br />
aspiration premorbidly, no patients were diagnosed with pneumonia<br />
at the point of admission through the ASCP. Five hundred twentyfour<br />
patients (91%) maintained an oral diet and were free from<br />
pneumonia during their hospitalization and within 35 days of<br />
<strong>Gundersen</strong> <strong>Lutheran</strong> Medical Journal • Volume 6, Number 1, June 2009 9<br />
ID Stamp:<br />
Reason for Admission/Primary Diagnosis:____________________________________________<br />
Date of Admission:_____________ Attending Staff:__________________________________<br />
House Staff:___________________________ RN Completing Index:_____________________<br />
Dates:________________________________________________________________________<br />
Trials<br />
Critical Criteria* Check if Present Check if Present Check if Present<br />
Decreased volitional cough _____ _____ _____<br />
Wet hoarseness _____ _____ _____<br />
Audible oropharyngeal pooling<br />
of secretions _____ _____ _____<br />
Decreased mental status _____ _____ _____<br />
Tracheostomy _____ _____ _____<br />
Tube feedings, NG or gastrostomy _____ _____ _____<br />
Assessment*<br />
Coughs on secretions _____ _____ _____<br />
Coughs on 3-ounce H2O trials _____ _____ _____<br />
Swallowing frequency (4 or < in 5’) _____ _____ _____<br />
This screen should be administered a minimum of three times within 24-48 hours of admission.<br />
If patient demonstrates one or more of the critical criteria, coughs on secretions, has failed H2O<br />
swallowing trials, or swallows four times or less in a five minute time period, then status should<br />
be NPO including medications unless they can only be given orally) until the screen is passed or<br />
formal evaluation of deglutitory function has been completed.