Streptococcus bovis - Gundersen Lutheran Health System
Streptococcus bovis - Gundersen Lutheran Health System
Streptococcus bovis - Gundersen Lutheran Health System
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
outCoMeS froM A SCreeninG proCedure for orophArynGeAL dySphAGiA<br />
patients who passed GLADS, these patients’ strokes were likely<br />
ischemic. Like those patients passing GLADS, those who failed<br />
had normal or minimally impaired speech, language, or cognitive<br />
function (78 patients, 45%). For those patients with impairment, a<br />
motor speech disorder was most common (44 patients, 25%), and<br />
a focal language disorder (aphasia) was least common (19 patients,<br />
11%). Thirty-four patients had dementia. We found no significant<br />
association between these deficits and pneumonia (P = .61), nor, as<br />
for those patients passing GLADS, were they good predictors of a<br />
patient’s ability to maintain a safe oral diet after stroke (P = .89).<br />
Median length of stay for patients failing GLADS was 5 days<br />
(range 1-62 days), significantly higher than for those patients who<br />
passed (3 days, P < .0001). Median cost of hospitalization for these<br />
patients was $11,703, which was also significantly higher than<br />
for those who passed (P < .0001). For the 14 patients who failed<br />
GLADS and developed pneumonia during hospitalization, the<br />
median length of stay was 7 days, and the median cost $19,933.<br />
Moreover, if odds ratios are considered, the 175 patients failing<br />
GLADS were 4 times more likely to develop pneumonia during<br />
hospitalization than were the 578 who passed (95% CI, 1.86-<br />
9.04). Table 2 summarizes the findings for the 175 patients failing<br />
GLADS.<br />
diSCuSSion<br />
Results of the current investigation suggest that GLADS is an<br />
effective screening measure for oropharyngeal dysphagia following<br />
acute stroke when administered by carefully trained nurses in<br />
conjunction with an ASCP. Barring unrelated stroke complications,<br />
over 90% of patients passing GLADS were able to maintain a safe<br />
and nutritionally sound oral diet without pneumonia or further<br />
comprehensive evaluation for dysphagia during hospitalization.<br />
They were also less likely than patients who failed GLADS to<br />
develop pneumonia during their hospitalization or after discharge.<br />
We found that neither site of lesion nor communicative or cognitive<br />
deficits was a predictor of who would develop pneumonia. We<br />
also found that prior stroke—even with related comorbidities<br />
including dysphagia or speech or cognitive deficits—was not a<br />
good predictor of a patient’s ability to maintain a safe oral diet<br />
following a new stroke. Not surprisingly, cost of hospitalization<br />
and length of stay were reduced when stroke was not complicated<br />
by pneumonia.<br />
One might argue that the 175 patients who failed GLADS<br />
had more devastating strokes that resulted in a complicated course<br />
with protracted hospitalization, increased expense, and a higher<br />
death rate than those who passed GLADS. Interestingly, however,<br />
with time and dysphagia therapy, almost half of these patients<br />
went on to become functional and safe oral feeders during their<br />
hospitalization. This finding could also represent the influence of<br />
the comprehensiveness and intensity of the ASCP itself.<br />
The importance of a swallowing screen as a component of an<br />
ASCP has been stressed by others. 42 Using a speech pathologist or<br />
certified nurse to screen for dysphagia, they found that 48 of 124<br />
patients (39%) failed the initial screen and required dietary texture<br />
change, as well as direct dysphagia therapy. Whereas in our study<br />
patients who failed GLADS were referred for further evaluation<br />
prior to initiation of an oral diet, their patients apparently did<br />
not undergo further workup for dysphagia or aspiration prior<br />
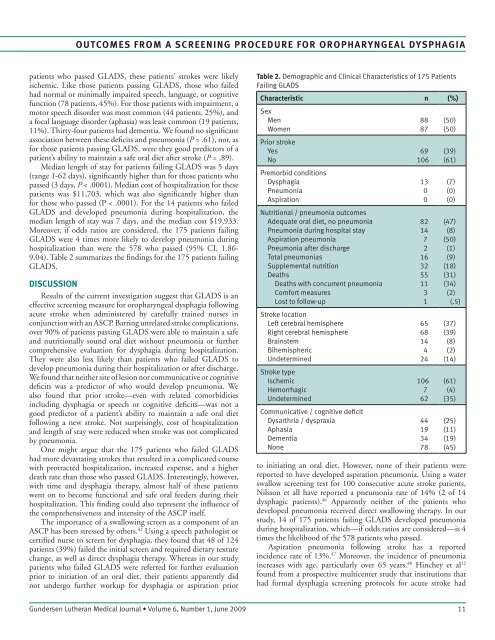
table 2. Demographic and Clinical Characteristics of 175 Patients<br />
Failing GLADS<br />
Characteristic n (%)<br />
Sex<br />
Men<br />
Women<br />
Prior stroke<br />
Yes<br />
No<br />
Premorbid conditions<br />
Dysphagia<br />
Pneumonia<br />
Aspiration<br />
Nutritional / pneumonia outcomes<br />
Adequate oral diet, no pneumonia<br />
Pneumonia during hospital stay<br />
Aspiration pneumonia<br />
Pneumonia after discharge<br />
Total pneumonias<br />
Supplemental nutrition<br />
Deaths<br />
Deaths with concurrent pneumonia<br />
Comfort measures<br />
Lost to follow-up<br />
Stroke location<br />
Left cerebral hemisphere<br />
Right cerebral hemisphere<br />
Brainstem<br />
Bihemispheric<br />
Undetermined<br />
Stroke type<br />
Ischemic<br />
Hemorrhagic<br />
Undetermined<br />
Communicative / cognitive deficit<br />
Dysarthria / dyspraxia<br />
Aphasia<br />
Dementia<br />
None<br />
to initiating an oral diet. However, none of their patients were<br />
reported to have developed aspiration pneumonia. Using a water<br />
swallow screening test for 100 consecutive acute stroke patients,<br />
Nilsson et all have reported a pneumonia rate of 14% (2 of 14<br />
dysphagic patients). 46 Apparently neither of the patients who<br />
developed pneumonia received direct swallowing therapy. In our<br />
study, 14 of 175 patients failing GLADS developed pneumonia<br />
during hospitalization, which—if odds ratios are considered—is 4<br />
times the likelihood of the 578 patients who passed.<br />
Aspiration pneumonia following stroke has a reported<br />
incidence rate of 13%. 47 Moreover, the incidence of pneumonia<br />
increases with age, particularly over 65 years. 48 Hinchey et al 12<br />
found from a prospective multicenter study that institutions that<br />
had formal dysphagia screening protocols for acute stroke had<br />
<strong>Gundersen</strong> <strong>Lutheran</strong> Medical Journal • Volume 6, Number 1, June 2009 11<br />
88<br />
87<br />
69<br />
106<br />
13<br />
0<br />
0<br />
82<br />
14<br />
7<br />
2<br />
16<br />
32<br />
55<br />
11<br />
3<br />
1<br />
65<br />
68<br />
14<br />
4<br />
24<br />
106<br />
7<br />
62<br />
44<br />
19<br />
34<br />
78<br />
(50)<br />
(50)<br />
(39)<br />
(61)<br />
(7)<br />
(0)<br />
(0)<br />
(47)<br />
(8)<br />
(50)<br />
(1)<br />
(9)<br />
(18)<br />
(31)<br />
(34)<br />
(2)<br />
(.5)<br />
(37)<br />
(39)<br />
(8)<br />
(2)<br />
(14)<br />
(61)<br />
(4)<br />
(35)<br />
(25)<br />
(11)<br />
(19)<br />
(45)