Streptococcus bovis - Gundersen Lutheran Health System
Streptococcus bovis - Gundersen Lutheran Health System
Streptococcus bovis - Gundersen Lutheran Health System
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
Th e<br />
<strong>Gundersen</strong><br />
Lu T h e r a n<br />
M e d i C A L J o u r n A L<br />
Volume 6, number 1<br />
June 2009<br />
oriGinAL reSeArCh ArtiCLeS<br />
Placebo Effects on Exercise Performance<br />
Outcomes from a Screening Procedure for Oropharyngeal Dysphagia<br />
Following Acute Stroke<br />
CASe reportS<br />
Colonoscopic Diagnosis of Appendicitis in a Patient with Ulcerative<br />
Colitis: A Case Report and Review of the Literature<br />
Intracranial Mycotic Aneurysm Due to <strong>Streptococcus</strong> <strong>bovis</strong><br />
Endocarditis<br />
Giant-Cell Reaction to a Bioabsorbable Implant<br />
Post–Cesarean Delivery Septic Ovarian Vein Thrombosis<br />
hiStory of MediCine<br />
Historical Notes on Amputation and Phantom Limb Pain:<br />
“All Quiet on the Western Front?”<br />
The History of Cardiac Rehabilitation at the University of<br />
Wisconsin–La Crosse
1<br />
3<br />
8<br />
14<br />
18<br />
21<br />
24<br />
26<br />
30<br />
Th e<br />
Gu n d e r s e n<br />
Lu T h e r a n<br />
M e d i C A L J o u r n A L<br />
Contents<br />
Editor’s Message<br />
David E. Hartman, PhD, BC-ANCDS(A)<br />
oriGinAL reSeArCh ArtiCLeS<br />
Placebo Effects on Exercise Performance<br />
Glenn Wright, PhD; John P. Porcari, PhD, RCEP; Carl C. Foster, PhD; Heidi Felker, MS; Ashley Kosholek, MS;<br />
Jennifer Otto, MS; Erik M. Sorenson, MS; Brian E. Udermann, PhD, ATC, FACSM<br />
Outcomes from a Screening Procedure for Oropharyngeal Dysphagia Following Acute Stroke<br />
David E. Hartman, PhD, BC-ANCDS(A); Melissa Hunter; Richard D. Hutter, MD; Claudia Schneller, RN;<br />
Jake Gundrum, MS<br />
CASe reportS<br />
Colonoscopic Diagnosis of Appendicitis in a Patient with Ulcerative Colitis: A Case Report and Review of the<br />
Literature<br />
Alexander D. Wade, MD; Frank J. Aberger, MD<br />
Intracranial Mycotic Aneurysm Due to <strong>Streptococcus</strong> <strong>bovis</strong> Endocarditis<br />
Abhishek Tandon, MD; Steven B. Pearson, MD; Todd J. Kowalski, MD<br />
Giant-Cell Reaction to a Bioabsorbable Implant<br />
Robert E. Ryan, MA, ATC; Troy E. Ward, MA, ATC; Steven R. Murray, DA; Mitchell T. Copeland, DO; Brian E.<br />
Udermann, PhD, ATC, FACSM; Robert W. Pettitt, PhD, ATC<br />
Post–Cesarean Delivery Septic Ovarian Vein Thrombosis<br />
Meghana Raghavendra, MB, BS; William A. Agger, MD<br />
hiStory of MediCine<br />
Historical Notes on Amputation and Phantom Limb Pain: “All Quiet on the Western Front?”<br />
Ines H. Berger, MD, PhD; Douglas R. Bacon, MD, MA<br />
The History of Cardiac Rehabilitation at the University of Wisconsin–La Crosse<br />
Brian E. Udermann, PhD, ATC, FACSM; John P. Porcari, PhD, RCEP; Carl C. Foster, PhD
editor<br />
David E. Hartman, PhD, BC-ANCDS(A)<br />
Department of Neurology<br />
Speech Pathology<br />
MAnAGinG editor<br />
Cathy Mikkelson Fischer, MA<br />
<strong>Gundersen</strong> <strong>Lutheran</strong> Medical Foundation<br />
editoriAL boArd MeMberS<br />
William A. Agger, MD, FACP<br />
Department of Internal Medicine<br />
Section of Infectious Disease<br />
Director of Research<br />
<strong>Gundersen</strong> <strong>Lutheran</strong> Medical Foundation<br />
Robert H. Caplan, MD, FACP, FACE<br />
Department of Internal Medicine<br />
Section of Endocrinology<br />
David H. Chestnut, MD<br />
Department of Anesthesiology<br />
Director of Medical Education<br />
<strong>Gundersen</strong> <strong>Lutheran</strong> Medical Foundation<br />
As sociate Dean for the Western Academic<br />
Campus<br />
University of Wisconsin School of Medicine<br />
and Public <strong>Health</strong><br />
Ronald S. Go, MD<br />
Department of Hematology<br />
Steven B. Pearson, MD, FACP<br />
Department of Internal Medicine<br />
Internal Medicine Residency Program Director<br />
Jeffrey S. Sartin, MD<br />
Department of Internal Medicine<br />
Section of Infectious Disease<br />
Mark L. Saxton, MD, FACS<br />
Department of Surgery<br />
Pediatric Surgery<br />
Brian E. Udermann, PhD, ATC, FACSM<br />
Department of Exercise and Sport Science<br />
University of Wisconsin–La Crosse<br />
Support StAff<br />
Deborah Brostrom<br />
Research Manager<br />
<strong>Gundersen</strong> <strong>Lutheran</strong> Medical Foundation<br />
Pamela Maas<br />
Chief Officer<br />
Business Development & Marketing<br />
Sarah J. Fillbach<br />
Marketing & Communication Specialist<br />
Business Development & Marketing<br />
Barbara K. Beeson<br />
Graphic Designer<br />
Business Development & Marketing<br />
Beth A. Frechette<br />
Marketing & Communication Specialist<br />
Business Development & Marketing<br />
<strong>Gundersen</strong> <strong>Lutheran</strong> Medical Journal publishes material related to the life sciences. We welcome submission of original research, reviews, case reports,<br />
commentaries, and letters. Please consult our “Instructions for Authors,” provided on our Website, for submission and manuscript preparation<br />
guidelines. Direct questions or submit manuscripts for consideration to<br />
<strong>Gundersen</strong> <strong>Lutheran</strong> Medical Journal<br />
<strong>Gundersen</strong> <strong>Lutheran</strong> Medical Foundation<br />
C03-006B<br />
1836 South Avenue<br />
La Crosse, WI 54601<br />
Telephone: (608) 775-6648<br />
Fax: (608) 775-1565<br />
Email: glmjeditor@gundluth.org<br />
Website: http://www.gundluth.org/journal<br />
Ad hoC reVieWerS<br />
<strong>Gundersen</strong> <strong>Lutheran</strong> Medical Journal is a peer-reviewed journal published by <strong>Gundersen</strong> <strong>Lutheran</strong> Medical Foundation,<br />
1836 South Avenue, La Crosse, WI 54601. Copyright 2009 by <strong>Gundersen</strong> <strong>Lutheran</strong> Medical Foundation. All rights reserved.<br />
Joseph B. Binegar, MD<br />
Christopher P. Born, MD<br />
Heather J. Chial, MD<br />
Mark E. Domroese MD, PhD<br />
A. Erik <strong>Gundersen</strong>, MD<br />
Michael J. Henry, MD<br />
Richard D. Hutter, MD<br />
Todd J. Kowalski, MD<br />
John D. Larson, MD<br />
Kenneth W. Merkitch, MD<br />
Jerry J. Miller, MD<br />
Kurt K. Mueller, MD<br />
Edward R. Winga, MD<br />
Individuals may photocopy parts of the Journal for educational purposes. The Journal is archived on the <strong>Gundersen</strong> <strong>Lutheran</strong> Medical Journal Website.<br />
Permission for use of the Journal for other purposes must be obtained in writing from the Editor. <strong>Gundersen</strong> <strong>Lutheran</strong> Medical Journal accepts no<br />
responsibility for statements made by contributors.
editor’S MeSSAGe<br />
Welcome to the Summer issue of the GLMJ ! Thanks to our authors for their<br />
contributions, and to the reviewers for taking time out of their busy schedules to review<br />
and comment on the submissions.<br />
The Journal’s Editorial Board is exploring ways in which it can contribute to <strong>Gundersen</strong><br />
<strong>Lutheran</strong>’s mission: “We distinguish ourselves through excellence in patient care,<br />
education, research, and through improved health in the communities we serve.” In<br />
order to increase awareness of the depth and breadth of our collective scholarly and<br />
research interests, each year we will publish abstracts of professional oral and poster<br />
presentations and of published journal articles. We will note publication of books<br />
and book chapters, as well. The Board is also developing a timeline for implementing<br />
the steps necessary to make successful application to have the Journal indexed in<br />
MEDLINE. Among these steps are expanding distribution of the Journal, increasing<br />
the number and quality of submissions, and recruiting more authors and reviewers from<br />
outside our organization.<br />
In the Original Research section of this issue, Dr Wright and colleagues from the<br />
University of Wisconsin–La Crossse apply the concept of the placebo effect to exercise.<br />
They tested whether groups who believed they were receiving a nutritional ergogenic aid<br />
(in fact, a placebo) experienced improvement in their exercise performance.<br />
My colleagues and I reviewed the efficacy and outcomes for a screening measure for<br />
dysphagia implemented for acute stroke patients for a consecutive 8-year period. Coauthor<br />
Melissa Hunter was my summer fellow in 2007 through the <strong>Gundersen</strong> <strong>Lutheran</strong><br />
Medical Foundation. Her diligent work and assistance saw this project through to<br />
fruition.<br />
This issue’s Case Reports section features several unusual cases. Drs Wade and Aberger<br />
present a case of colonoscopically diagnosed appendicitis in a patient with known<br />
ulcerative colitis, possibly the first such case reported in the literature.<br />
Dr Tandon and colleagues discuss the history and course for a patient with infective<br />
endocarditis who developed neurologic signs and radiographic evidence for multiple<br />
intracranial mycotic aneurysms. Mycotic aneurysms are usually fatal if not diagnosed<br />
and treated in a timely manner.<br />
Mr Ryan and colleagues, representing institutions in Colorado, Minnesota, and<br />
Wisconsin, discuss a case of a giant-cell reaction to a bioabsorbable implant used to<br />
repair a torn supraspinatus muscle in a patient with impingement syndrome.<br />
Drs Raghavendra and Agger offer insights into diagnosis and treatment of postpartum<br />
ovarian vein thrombosis.<br />
Finally, in the History of Medicine section, Drs Berger and Bacon provide an interesting<br />
and detailed history of phantom limb syndrome, while Dr Udermann and colleagues<br />
from the University of Wisconsin–La Crossse provide a comprehensive story of cardiac<br />
rehabilitation in La Crosse since its inception in 1970.<br />
Along with the Editorial Board, I hope that you enjoy this issue of the GLMJ. Your<br />
contributions and suggestions for the Journal are welcomed and encouraged. We<br />
encourage <strong>Gundersen</strong> <strong>Lutheran</strong> staff to document their presentations and publications<br />
1
through our online Scholarly Activity Report as they are completed. We’d hate to miss including<br />
your abstract in our winter issue. Please feel free to contact me or Cathy L. Fischer, Managing<br />
Editor, with your submissions, comments, or concerns.<br />
David E. Hartman, PhD, BC-ANCDS(A)<br />
Editor<br />
<strong>Gundersen</strong> <strong>Lutheran</strong> Medical Journal<br />
2 <strong>Gundersen</strong> <strong>Lutheran</strong> Medical Journal • Volume 6, Number 1, June 2009
Authors:<br />
Glenn Wright, PhD<br />
John P. Porcari, PhD, RCEP<br />
Carl C. Foster, PhD<br />
Heidi Felker, MS<br />
Ashley Kosholek, MS<br />
Jennifer Otto, MS<br />
Erik M. Sorenson, MS<br />
Brian E. Udermann, PhD, ATC,<br />
FACSM<br />
Department of Exercise and<br />
Sport Science<br />
University of Wisconsin–La Crossse<br />
Address for correspondence:<br />
Glenn Wright, PhD<br />
Department of Exercise and<br />
Sport Science<br />
University of Wisconsin–La Crossse<br />
1725 State Street<br />
La Crosse, WI 54601<br />
email: wright.glen@uwlax.edu<br />
Placebo Effects on Exercise Performance<br />
AbStrACt<br />
The concept of controlling for placebo effects during<br />
experimental and clinical intervention studies is well<br />
established. The power of the placebo effect has been recognized<br />
in the literature, with the general expectation that about 33% of<br />
experimental subjects or patients will respond solely on the basis of<br />
the placebo effect. 1 Well-documented effects related to subjective<br />
outcome measures, 2 depression, 3 pain relief, 4 symptom relief, 5,6<br />
blood pressure reduction, 7 and asthma relief 8 have been reported.<br />
Although virtually all exercise intervention studies include control<br />
groups to account for the placebo effect, data documenting the<br />
magnitude of the placebo effect during exercise are limited.<br />
Accordingly, the purpose of this study was to assess the magnitude<br />
of the placebo effect during exercise, with particular reference to<br />
the type of exercise (aerobic vs anaerobic) and exerciser (athletes,<br />
healthy nonathletes, patients).<br />
MethodS<br />
Approach to the Problem<br />
This study was designed to test the hypothesis that there would<br />
be a significant placebo effect during exercise in different types of<br />
exercise and in different types of exercisers. It was conducted in 3<br />
distinct parts. In all parts of the study, subjects provided written<br />
informed consent, and the study protocols had been approved by<br />
the university Institutional Review Board. In all parts of the study,<br />
the subjects had performed a practice trial of the criterion task to<br />
ensure that they were fully task habituated. Placebo and control<br />
studies were performed in random order with ≥ 48 hours without<br />
heavy exercise prior to each trial.<br />
Despite the routine use of placebo control in exercise intervention studies, there is inadequate<br />
information about the magnitude of the placebo effect and how it might respond during<br />
different types of exercise. This study was designed to evaluate the placebo effect in different<br />
populations and in different types of exercise. In a 3-part study the effect of purported<br />
nutritional ergogenic aids was measured in: (A) trained runners in a 5-km time trial, (B) physical<br />
education students during a high-intensity cycle sprint test, and (C) in clinically stable patients<br />
during a 6-minute walk test. In A, performance was improved by 83 seconds (6.5%), with a<br />
larger placebo effect in the slower runners. In B, there was no significant effect on peak or mean<br />
power output, or on the pattern of fatigue. In C, although there was no significant difference<br />
in the distance completed in the 6-minute walk test, there was a significant trend (P = .08) for<br />
patients to walk faster during the first minute of the test. The results suggest that the placebo<br />
effect may be of significant magnitude, particularly during more prolonged tasks, and may<br />
influence both athletes and patients.<br />
9 -14<br />
SubJeCtS<br />
In Part A, healthy, well-trained competitive runners ranging<br />
from university to recreational class (23 men, mean [SD] age 28<br />
[13] years; 9 women, mean [SD] age 30 [13] years) were studied<br />
during 5-km running time trials. In Part B, healthy physical<br />
education students (8 men, mean [SD] age 20 [1] years; 10<br />
women, mean [SD] age 21 [1] years) were studied during highintensity<br />
sprint cycling (Wingate Test). In Part C, patients with<br />
stable cardiovascular disease who were participants for longer than<br />
1 year in a community-based exercise program (6 men, mean [SD]<br />
age 62 [10] years; 4 women, mean [SD] age 64 [8] years) were<br />
studied while performing the 6-minute walk test.<br />
proCedureS<br />
In all 3 parts of the study, subjects were intentionally<br />
misinformed of the purported beneficial effects of the placebo agent<br />
by having them view a video (Part A = super-oxygenated water), by<br />
having them attend a graduate class on ergogenic aids (Part B = fastacting<br />
creatine monohydrate), or by having them read a brochure<br />
purporting to report results of previous studies (Part C = Peligrino<br />
Spa water). In all cases, subjects were given an inactive agent (tap<br />
water) in both the placebo and control conditions. We deliberately<br />
let the subjects know when they were receiving the “active” agent,<br />
so that they would be expecting an ergogenic benefit. Polling of the<br />
subjects indicated that they generally felt that the “active” agent (ie,<br />
placebo) was likely to help their performance.<br />
In Part A, the subjects ran two 5-km time trials (running<br />
without the benefit of other competitors) on an indoor 200-m<br />
track. The warm-up before each run was based on the normal pre-<br />
<strong>Gundersen</strong> <strong>Lutheran</strong> Medical Journal • Volume 6, Number 1, June 2009 3
competition practice of each subject, and was consistent between<br />
trials within each subject. During the trial, the time for each lap<br />
was called to the subject to facilitate pacing, which is a common<br />
practice during competitions. Prior to the warm-up (~30 minutes<br />
prior to the beginning of the time trial) each subject consumed<br />
300 ml of tap water. In the placebo trial, the water was labeled<br />
“super-oxygenated water” in order to create the impression that<br />
subjects were consuming an ergogenic aid. In the control trial,<br />
the water was correctly labeled as “water.” During the time<br />
trials, running time was recorded for each of the 25 laps, and<br />
heart rate was recorded using radio telemetry (Polar Electro OY,<br />
Finland). Within 60 seconds of completing the trial, blood lactate<br />
concentration was measured in capillary blood using an enzyme<br />
electrode system (YSI Sport, Yellow Springs, OH), and the rating<br />
of perceived exertion (RPE) was measured using the Borg category<br />
ratio scale (CR10 Scale). 15<br />
In Part B the subjects performed 2 Wingate anaerobic tests 16<br />
on an electronically braked cycle ergometer (LODE Excalibur,<br />
Netherlands), with the resistance set at 75 g.kg -1 body weight.<br />
These tests were performed at least 3 days apart. The warm-up<br />
was standardized for each subject and consisted of continuous<br />
cycling at 75 watts (W) for 10 minutes. During the last 5 minutes<br />
of the warm-up, the subjects accelerated to maximal power output<br />
for ~5 seconds on 2 occasions in order to ensure that the subject<br />
had a sense of the feeling of the power output required during the<br />
test. Following the warm-up the subjects recovered by pedaling at<br />
25 W for 5 minutes. The protocol of the test was controlled by<br />
software in the cycle, with a 30-second countdown prior to the test<br />
initiation. The subjects began maximal acceleration of the pedals at<br />
-3 seconds, and rapid adjustment of the resistance was performed<br />
by the ergometer software, such that the required resistance was<br />
achieved at the start of the 30-second Wingate test protocol.<br />
Subjects were verbally encouraged to pedal at maximal pedal<br />
revolutions (ie, the highest possible power output) throughout the<br />
test. The ergometer recorded the power output during each second<br />
of the test. In order to create the impression that they were taking<br />
an ergogenic aid, subjects in the placebo group were instructed<br />
to report to the laboratory to mix and consume 300 ml of water<br />
with 5 g of white powder labeled “alpha-hydroxycreatine” (placebo<br />
as maltodextrin) approximately 24 hours prior to the test, while<br />
the control group subjects consumed 300 ml of known water. An<br />
Lap Velocity, m.s -1<br />
5<br />
4.5<br />
4<br />
3.5<br />
C ontrol<br />
Placebo<br />
Lap Velocity<br />
0 1000 2000 3000 4000 5000<br />
Distance, m<br />
additional dose of the placebo or control beverage was consumed<br />
prior to the warm-up of the respective trial approximately<br />
30 minutes prior to the test.<br />
In Part C the subjects performed two 6-minute walk tests in a<br />
36-m hallway. An investigator positioned at the midpoint of the<br />
hall timed the subjects each time they touched the wall or passed<br />
the midpoint of the hallway, allowing velocity to be calculated<br />
over every 18 m. This was later converted to average velocity over<br />
every 30 seconds of the test. Heart rate was determined using radio<br />
telemetry. RPE was measured using the Category Ratio RPE scale.<br />
Prior to performing the test, subjects had walked for 10 minutes<br />
at their normal exercise training pace and had rested for 5 minutes<br />
immediately prior to beginning the test. In order to create the<br />
impression that they were taking an ergogenic aid, subjects in<br />
the placebo group were instructed to consume 300 ml of a liquid<br />
labelled “Pelegrino Spa Water” approximately 30 minutes before<br />
the warm-up, while the control group consumed 300 ml of a<br />
liquid labelled “water.”<br />
StAtiStiCAL AnALySiS<br />
For all parts of the study, outcome measures were analyzed<br />
using repeated measures analysis of variance (ANOVA) for an<br />
intervention by serial measurement design. Post hoc analyses<br />
were performed using the Tukey test when justified by ANOVA.<br />
Statistical significance was accepted when P < .05.<br />
reSuLtS<br />
All tests were completed without complication by all subjects.<br />
Questioning of the subjects indicated that the procedures used to<br />
create the expectation that the intervention beverage would confer<br />
an ergogenic effect were effective.<br />
pArt A<br />
On average, subjects ran the placebo trial significantly faster<br />
(83 seconds faster, 6.5%) than they ran the control trial (mean<br />
[SD] 19:41 [2:32] minutes vs 21:04 [3:34] minutes). Average<br />
running velocity, distributed fairly evenly within the trial, was<br />
0.23 m.s -1 faster during the placebo trial (Figure 1 left). Heart rate<br />
(HR) (mean [SD] 179 [13] beats.min -1 vs 179 [11] beats.min -1 ),<br />
figure 1. (Left) Running velocity per lap during 5-km time trials in the control (solid circles) and placebo (open circles) conditions. (Right)<br />
Comparison of total running time for 5 km during the placebo and control trials. There was a significant overall effect (83 seconds) attributable<br />
to the placebo, but a proportionally larger placebo effect in the slower (> 1200 seconds) runners compared with the faster runners (2:22 ± 1:02<br />
vs 0:28 ± 1:08).<br />
4 <strong>Gundersen</strong> <strong>Lutheran</strong> Medical Journal • Volume 6, Number 1, June 2009<br />
Placebo Time, s<br />
1800<br />
1700<br />
1600<br />
1500<br />
1400<br />
1300<br />
1200<br />
1100<br />
1000<br />
900<br />
Control vs Placebo Time<br />
900 1000 1100 1200 1300 1400 1500 1600 1700 1800<br />
Control Time, s
RPE (0-10 scale) (mean [SD] 7.7 [1.2] vs 7.7 [1.4]), and blood<br />
lactate concentration (mean [SD] 10.2 [3.7] mmol.l -1 vs 9.8 [3.9]<br />
mmol.l -1 ) were not different between placebo and control trials,<br />
respectively. Using a 1.5% difference as a meaningful difference in<br />
performance, 17 75% of the subjects ran faster during the placebo<br />
trial, and 9% ran faster during the control trial. A direct comparison<br />
of performance during placebo and control trials suggested that the<br />
relatively slower subjects (control trial >1200 seconds) had a larger<br />
mean improvement in performance (mean [SD] 2:22 [1:02]) than<br />
the relatively faster subjects (control trial
effect. These data suggest that the placebo effect is more likely to<br />
be present during exercise that may need to be sustained for some<br />
moments and is more likely in individuals least likely to adequately<br />
monitor their physical response to exercise. The magnitude of<br />
effect supports the concept that something in excess of one-third<br />
of individuals will be responsive to the placebo effect. 1<br />
The results can be understood in terms of the anticipatoryperceived<br />
exertion feedback model, recently proposed by Tucker<br />
and Noakes. 18 According to this model, the pattern of energy<br />
output during a task is defined by a template based on individual<br />
expectations regarding the appropriate effort distribution and<br />
experience with the task. In the presence of a placebo, some<br />
individuals may revise their pre-exercise template and start exercise<br />
at a higher intensity. In most individuals (eg, the patients during<br />
the 6-minute walk test and the more accomplished runners)<br />
feedback from homeostatic disturbances during exercise causes a<br />
reduction of an overly ambitious pace to a more appropriate pace.<br />
This concept is supported by recent work in our laboratory 19 that<br />
has shown that the relative growth of effort sense (ie, RPE) during<br />
exercise is remarkably stable despite differences in task duration<br />
and/or the blinded administration of a hypoxic gas mixture.<br />
Similar findings have been reported in relation to running<br />
distance 20 and during both hypoxia and hyperoxia. 21-23 Morgan 24<br />
has demonstrated that less accomplished competitive runners do<br />
not adequately attend to the growth of fatigue during marathon<br />
running, preferring to dissociate from the sensations of running.<br />
This observation may explain the frequency of “hitting the wall”<br />
in less accomplished runners. It may also explain the persistence of<br />
a higher running pace in the less accomplished runners during the<br />
placebo trial, many of whom may not have raced enough to fully<br />
use their physiological capacity during competitions.<br />
Past experience with the criterion task may also affect the<br />
way energy is expended. Previous work from our laboratory 25 has<br />
demonstrated that performance often changes over the first several<br />
trials of a new task, primarily attributable to the subject being<br />
willing to begin at a faster pace. Given the failure to slow as much<br />
after the first laps of the 5 km (Part A) and the trend toward a faster<br />
start in the 6-minute walk (Part C), it seems reasonable to suggest<br />
that one of the ways in which the placebo works is to encourage a<br />
faster start. Similar results have been demonstrated with the clinical<br />
use of the 6-minute walk test, 26 where patients typically take 2 to 3<br />
trials to achieve a stable performance. It likewise seems reasonable<br />
to suggest that experience with performing a task and the placebo<br />
effect would influence performance in the same way.<br />
The failure to observe a significant placebo effect during the<br />
high-intensity exercise bout can be attributed to both the protocol<br />
employed and the nature of the task. In the Wingate Test it is<br />
ordinary to allow the subject to increase the pedaling rate of the<br />
cycle ergometer prior to loading the flywheel. 16 However, this may<br />
spuriously elevate the measured power output during the first<br />
seconds of the test. Although this pre-load spinning is a normal<br />
way of conducting this test, Havenetidis 27 and Reiser 28 have<br />
discussed the limitations of this approach. Mendez-Villaneuva 29<br />
has demonstrated in a repeated sprint protocol that losses in power<br />
output are attributable to an inherent loss of motor unit recruitment<br />
rather than to reductions of effort. Thus, both the nature of the<br />
experimental approach (peak power) and the way that power is<br />
reduced in sprint exercise (mean power), the Wingate Test would<br />
be somewhat resistant to demonstrating a placebo effect.<br />
In conclusion, the results of this study demonstrate that the<br />
placebo effect is of sufficient magnitude to justify the normal<br />
practice of including control groups for intervention studies<br />
involving exercise capacity as an outcome from exercise training 30<br />
or pharmacologic interventions. 31 Although the specific results<br />
of this study (Part B) did not demonstrate an effect on sprint<br />
performance, the results of the other portions of the study suggest<br />
that the general practice of using a control group is well-justified.<br />
referenCeS<br />
1. Beecher HK. The powerful placebo. J Am Med Assoc. 1955;159(17):1602-1606.<br />
2. Turner JA, Deyo RA, Loeser JD, Von Korff M, Fordyce WE. The importance of<br />
placebo effects in pain treatment and research. JAMA. 1994;271(20):1609-1614.<br />
3. Kirsch IPD, Sapirstein GPD. Listening to Prozac but hearing placebo: a metaanalysis<br />
of antidepressant medication. Prevention & Treatment. 1998;1(2).<br />
4. Benson H, McCallie DP Jr. Angina pectoris and the placebo effect. N Engl J Med.<br />
1979;300(25):1424-1429.<br />
5. Hashish I, Harvey W, Harris M. Anti-inflammatory effects of ultrasound therapy:<br />
evidence for a major placebo effect. Br J Rheumatol. 1986;25(1):77-81.<br />
6. Moseley JB, O’Malley K, Petersen NJ, et al. A controlled trial of arthroscopic<br />
surgery for osteoarthritis of the knee. N Engl J Med. 2002;347(2):81-88.<br />
7. Preston RA, Materson BJ, Reda DJ, Williams DW. Placebo-associated blood<br />
pressure response and adverse effects in the treatment of hypertension: observations<br />
from a Department of Veterans Affairs cooperative study. Arch Intern Med.<br />
2000;160(10):1449-1454.<br />
8. Godfrey S, Silverman M. Demonstration by placebo response in asthma by means<br />
of exercise testing. J Psychosom Res. 1973;17(4):293-297.<br />
9. Ariel G, Saville W. Anabolic steroids: the physiological effects of placebos. Med Sci<br />
Sports Exerc. 1972;4:124-126.<br />
10. Clark VR, Hopkins WG, Hawley JA, Burke LM. Placebo effect of carbohydrate<br />
feedings during a 40-km cycling time trial. Med Sci Sports Exerc. 2000;32(9):1642-<br />
1647.<br />
11. Maganaris CN, Collins DJ, Sharp M. Expectancy effects and strength training:<br />
do steroids make a difference? Sport Psychologist. 2000;14:272-278.<br />
12. Sonetti DA, Wetter TJ, Pegelow DF, Dempsey JA. Effects of respiratory muscle<br />
training versus placebo on endurance exercise performance. Respir Physiol.<br />
2001;127(2-3):185-199.<br />
13. Beedie CJ, Stuart EM, Coleman DA, Foad AJ. Placebo effects of caffeine on<br />
cycling performance. Med Sci Sports Exerc. 2006;38(12):2159-2164.<br />
14. Beedie CJ, Coleman DA, Foad AJ. Positive and negative placebo effects resulting<br />
from the deceptive administration of an ergogenic aid. Int J Sport Nutr Exerc<br />
Metab. 2007;17(3):259-269.<br />
15. Borg G. Borg’s Perceived Exertion and Pain Scales. Champaign, IL: Human<br />
Kinetics; 1998:104.<br />
16. Maud PJ, Berning JM, Foster C, et al. Testing for anaerobic ability. In: Maud PJ,<br />
Foster C, eds. Physiological Assessment of Human Fitness. 2nd ed. Champaign, IL:<br />
Human Kinetics; 2006:77-92.<br />
17. Hopkins WG, Schabort EJ, Hawley JA. Reliability of power in physical<br />
performance tests. Sports Med. 2001;31(3):211-234.<br />
18. Tucker R, Noakes TD. The anticipatory regulation of performance: the<br />
physiological basis for pacing strategies and the development of the perceptionbased<br />
model for exercise and performance [published online ahead of print<br />
February 17, 2009]. Br J Sports Med. doi:10.1136/bjsm.2008.050799.<br />
6 <strong>Gundersen</strong> <strong>Lutheran</strong> Medical Journal • Volume 6, Number 1, June 2009
19. Joseph T, Johnson B, Battista RA, et al. Perception of fatigue during simulated<br />
competition. Med Sci Sports Exerc. 2008;40(2):381-386.<br />
20. Faulkner J, Parfitt G, Eston R. The rating of perceived exertion during competitive<br />
running scales with time. Psychophysiology. 2008;45(6):977-985.<br />
21. Amann M, Eldridge MW, Lovering AT, Stickland MK, Pegelow DF, Dempsey JA.<br />
Arterial oxygenation influences central motor output and exercise performance<br />
via effects on peripheral locomotor muscle fatigue in humans. J Physiol. 2006;575<br />
(Pt 3):937-952.<br />
22. Peltonen JE, Rantamaki J, Niittymaki SP, Sweins K, Viitasalo JT, Rusko HK.<br />
Effects of oxygen fraction in inspired air on rowing performance. Med Sci Sports<br />
Exerc. 1995;27(4):573-579.<br />
23. Tucker R, Kayser B, Rae E, Raunch L, Bosch A, Noakes T. Hyperoxia improves<br />
20 km cycling time trial performance by increasing muscle activation levels while<br />
perceived exertion stays the same. Eur J Appl Physiol. 2007;101(6):771-781.<br />
24. Morgan WP, Pollock ML. Psychologic characterization of the elite distance<br />
runner. Ann N Y Acad Sci. 1977;301:382-403.<br />
25. Foster C, Hendrickson K, Peyer K, et al. Pattern of developing the performance<br />
template [published online ahead of print January 5, 2009]. Br J Sports Med.<br />
doi:10.1136/bjsm.2008.054841.<br />
pLACebo effeCtS on exerCiSe perforMAnCe<br />
26. Guyatt GH, Pugsley SO, Sullivan MJ, et al. Effect of encouragement on walking<br />
test performance. Thorax. 1984;39(11):818-822.<br />
27. Havenetidis K, Cooke CB, Butterly R, King RF. Incorrect calculation of power<br />
outputs masks the ergogenic capacity of creatine supplementation. Appl Physiol<br />
Nutr Metab. 2006;31(5):635-642.<br />
28. Reiser RF 2nd, Broker JP, Peterson ML. Inertial effects on mechanically braked<br />
Wingate power calculations. Med Sci Sports Exerc. 2000;32(9):1660-1664.<br />
29. Mendez-Villanueva A, Hamer P, Bishop D. Fatigue in repeated-sprint exercise is<br />
related to muscle power factors and reduced neuromuscular activity. Eur J Appl<br />
Physiol. 2008;103(4):411-419.<br />
30. Foster C, Pollock ML, Anholm JD, et al. Work capacity and left ventricular<br />
function during rehabilitation after myocardial revascularization surgery.<br />
Circulation. 1984;69(4):748-755.<br />
31. Squires RW, Rod JL, Pollock ML, Foster C. Effects of propranolol on perceived<br />
exertion soon after myocardial revascularization surgery. Med Sci Sports Exerc.<br />
1982;14(4):276-280.<br />
Zebra Family Jeff Hillesland<br />
Trauma & Emergency Center<br />
<strong>Gundersen</strong> <strong>Lutheran</strong> Medical Journal • Volume 6, Number 1, June 2009 7
Authors:<br />
David E. Hartman, PhD,<br />
BC-ANCDS(A)<br />
Speech Pathology, Department of<br />
Neurology<br />
<strong>Gundersen</strong> <strong>Lutheran</strong> <strong>Health</strong> <strong>System</strong><br />
Melissa Hunter<br />
Department of Research<br />
<strong>Gundersen</strong> <strong>Lutheran</strong> Medical<br />
Foundation<br />
Richard D. Hutter, MD<br />
Department of Neurology<br />
<strong>Gundersen</strong> <strong>Lutheran</strong> <strong>Health</strong> <strong>System</strong><br />
Claudia Schneller, RN<br />
Department of Nursing<br />
<strong>Gundersen</strong> <strong>Lutheran</strong> <strong>Health</strong> <strong>System</strong><br />
Jake Gundrum, MS<br />
Department of Research<br />
<strong>Gundersen</strong> <strong>Lutheran</strong> Medical<br />
Foundation<br />
Address for correspondence:<br />
David E. Hartman, PhD,<br />
BC-ANCDS(A)<br />
Mail Stop EB3-005<br />
<strong>Gundersen</strong> <strong>Lutheran</strong> <strong>Health</strong> <strong>System</strong><br />
1900 South Avenue<br />
La Crosse, WI 54601<br />
Telephone: (608) 782-7300<br />
Facsimile: (608) 791-6358<br />
email: dehartma@gundluth.org<br />
Outcomes from a Screening Procedure for<br />
Oropharyngeal Dysphagia Following Acute Stroke<br />
AbStrACt<br />
Stroke is the third leading cause of death and number one<br />
cause of adult disability in the United States, affecting more<br />
than 700 000 Americans each year, including 160 000 deaths from<br />
stroke-related causes. 1 It is estimated that over 3 million Americans<br />
are permanently disabled from stroke. 2 In 1999, stroke cost the<br />
United States approximately 30 billion dollars in healthcare<br />
costs and lost productivity. 1 Given inflation, more sophisticated<br />
technology for evaluation and treatment, and the overall rise in the<br />
cost of healthcare, this figure has steadily increased over the years.<br />
Stroke is the most common etiology for dysphagia, with<br />
30% or more of patients showing signs of aspiration by clinical<br />
examination or videofluorographic study of swallow (VFSS). 3-8 The<br />
likelihood of developing pneumonia is 7 times greater in stroke<br />
patients who aspirate than in those who do not, even though the<br />
typical course for dysphagia after stroke is gradual improvement<br />
over a 6-month period. 3,6,9,10 Untreated or undiagnosed dysphagia<br />
can lead to malnutrition, while pneumonia increases the chance of<br />
mortality 3-fold, particularly in those institutions that do not have<br />
a screening protocol for dysphagia. 11,12<br />
It has been the general consensus that in acute stroke, a<br />
bedside examination, even if supplemented by available dysphagia<br />
Oropharyngeal dysphagia and aspiration pneumonia are common sequelae to stroke. The<br />
purpose of the current investigation was to assess the effectiveness of a screening procedure<br />
for dysphagia and aspiration following acute stroke. Medical records of 753 patients who<br />
were seen through an acute stroke care pathway and screened for dysphagia and aspiration<br />
using the <strong>Gundersen</strong> <strong>Lutheran</strong> Acute Dysphagia Screen (GLADS) between 1998 and 2006<br />
were reviewed. Dysphagia, pneumonia, nutritional outcomes, and neurologic characteristics<br />
of patients who passed GLADS were compared with those of patients who failed. Five hundred<br />
seventy-eight patients passed GLADS. Of these, 524 (91%) remained stable on an oral diet and<br />
free of pneumonia during their hospitalization; 18 (3%) developed pneumonia during the study.<br />
One hundred seventy-five patients failed GLADS and had further evaluation and treatment.<br />
Eighty-two of these patients (47%) remained stable on an oral diet and free of pneumonia<br />
during their hospitalization; 16 (9%) developed pneumonia during the study. Patients who<br />
passed GLADS had significantly lower rates of pneumonia than those who failed. Length of<br />
hospital stay and cost of hospitalization were considerably greater for patients failing GLADS.<br />
Premorbid stroke and dysphagia were not good predictors of a patient’s ability to maintain<br />
a safe oral diet. No significant association was found between site of lesion, communicative<br />
or cognitive deficits, and pneumonia. Communicative or cognitive deficits were not good<br />
predictors of a patient’s ability to maintain a safe oral diet after stroke. GLADS appears to be an<br />
effective screening tool for dysphagia and preventing pneumonia following acute stroke.<br />
screening tools, is inadequate for assessing deglutitory function<br />
and for predicting dysphagia or its ramifications, including<br />
aspiration, pneumonia, or malnutrition. 7,8,13-19 Recently, however,<br />
Trapl and colleagues 20 described a bedside screening protocol used<br />
for 50 acute-stroke patients that, with further investigation, may<br />
allow for institution of a safe oral diet without the need for further<br />
evaluation of swallowing function.<br />
Martino and colleagues 21 and Perry and Love 22 conducted<br />
comprehensive literature reviews that identified several articles that<br />
met strict research criteria for dysphagia screening following acute<br />
stroke. Their combined results indicated a need for both creation<br />
and validation of efficacious screening procedures for dysphagia<br />
after stroke. This issue was also stressed in the 1999 Agency for<br />
<strong>Health</strong> Care Policy and Research report for dysphagia, 23 and by<br />
the Joint Commission, 24 Smith and colleagues, 25 Teramoto and<br />
Fukuchi, 26 Mosheim, 27 and Swigert, 11 particularly as bedside<br />
screening procedures are used to detect aspiration.<br />
In 1997, professional staff at our institution representing<br />
neurology, speech-language pathology, physical medicine and<br />
rehabilitation, internal medicine, neurosurgery, and nursing<br />
developed a comprehensive care pathway—Acute Stroke Care<br />
8 <strong>Gundersen</strong> <strong>Lutheran</strong> Medical Journal • Volume 6, Number 1, June 2009
outCoMeS froM A SCreeninG proCedure for orophArynGeAL dySphAGiA<br />
Pathway (ASCP)—for evaluating and treating acute stroke patients<br />
admitted to our medical center. Various stroke pathways have been<br />
described elsewhere 12,28 and have been found to be efficacious for<br />
caring for acute stroke patients.<br />
In conjunction with the ASCP and based upon previous literature<br />
concerning bedside screening examinations for oropharyngeal<br />
dysphagia, 3,5,13-15,18,19,21,22,28-42 3 of the authors developed a screening<br />
tool, <strong>Gundersen</strong> <strong>Lutheran</strong> Acute Dysphagia Screen (GLADS), for<br />
use by nurses. In brief, GLADS used a checklist that incorporated<br />
several observable risk factors (ie, Critical Criteria) relevant for<br />
both dysphagia and aspiration, and assessment tools for secretions,<br />
swallowing frequency, and water swallows. 26,31,33,40,41 Prior to using<br />
it with stroke patients, a select cadre of 20 registered nurses was<br />
trained by the 3 authors to administer GLADS.<br />
Through the ASCP, medically stable and adequately alert<br />
patients were screened a minimum of 3 times following admission<br />
and up to 48 hours prior to a consultation being generated for more<br />
comprehensive evaluation of swallowing function. Observations<br />
of (1) 1 or more critical criteria, (2) continuous intermittent<br />
coughing on secretions, (3) coughing with water swallow trials, 32,33<br />
or (4) swallowing frequency fewer than 1 per minute or 4 per<br />
5 minutes 40,41 denoted failure on GLADS, prompted a nothing<br />
by mouth order, and generated referral for further evaluation.<br />
If available in liquid form, necessary medications were given<br />
intravenously or intramuscularly.<br />
Results from a pilot study using GLADS for 118 acute<br />
stroke patients showed that none developed either pneumonia<br />
or malnutrition during hospitalization or at 3-month followup<br />
and suggested that trained nurses could effectively implement<br />
a screening procedure for dysphagia following stroke. 43,44 The<br />
purpose of the current retrospective investigation was to (1)<br />
determine the outcomes for pneumonia and nutrition for patients<br />
admitted through the ASCP between 1998 and 2006 and<br />
undergoing GLADS as part of the stroke protocol, (2) determine<br />
the effectiveness of GLADS as a screening procedure for dysphagia<br />
and aspiration, and (3) compare the neurological characteristics of<br />
patients who passed GLADS with those of patients who failed.<br />
MethodS<br />
Approval for retrospective review of patient medical records<br />
was obtained from <strong>Gundersen</strong> <strong>Lutheran</strong> <strong>Health</strong> <strong>System</strong>’s<br />
Research Committee and Institutional Review Board. All<br />
patients admitted through the ASCP between January 1998 and<br />
December 2006 were identified by service code and their medical<br />
records reviewed by the authors. Of these, the records of those<br />
patients who underwent screening using GLADS were reviewed<br />
for outcomes during hospitalization and at 35 days following<br />
discharge from hospital. A determination of pneumonia was made<br />
by reviewing the comments and diagnoses made by the primary<br />
service (typically internal medicine or neurology) or pulmonary<br />
medicine and the findings from chest radiographs. Nutritional<br />
status was determined by reviewing the nutritional assessment<br />
recommendations made by registered dieticians or the metabolic<br />
support team. General statistical associations and proportion<br />
comparisons with categorical variables were assessed with the χ 2<br />
test. The Fisher exact test was used in place of the χ 2 test when at<br />
least 25% of the cells had counts less than 5. Univariate logistical<br />
models were used when predictive ability was tested. The cost and<br />
length-of-stay comparisons between groups were done with the<br />
Wilcoxon rank sum test of equal distributions. Exact confidence<br />
limits were calculated for the reported odds ratio. A P value < .05<br />
was considered significant.<br />
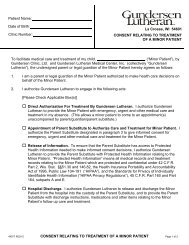
<strong>Gundersen</strong> <strong>Lutheran</strong> Acute Dysphagia Screen<br />
(GLADS)<br />
reSuLtS<br />
Seven hundred fifty-three stroke patients, average age 74 years,<br />
had GLADS administered in conjunction with the ASCP between<br />
January 1998 and December 2006. Five hundred seventy-eight<br />
patients (77%) passed GLADS. Of these, 571 did not undergo<br />
further assessment for dysphagia prior to implementation of an<br />
oral diet; the remaining 7 patients had normal VFSS test results<br />
and were started on an oral diet subsequent to study. However, 4<br />
of these patients had inadequate oral intake and were given enteral<br />
feedings, as well. One hundred seventy-five patients (23%) failed<br />
GLADS and went on for further evaluation (ie,VFSS, fiberoptic<br />
study of swallow, 29,45 or both) and treatment.<br />
Of the patients passing GLADS, 287 were men and 291 were<br />
women. By report, 10 patients had premorbid dysphagia, although<br />
its nature was unclear. Although 1 patient was described as having<br />
aspiration premorbidly, no patients were diagnosed with pneumonia<br />
at the point of admission through the ASCP. Five hundred twentyfour<br />
patients (91%) maintained an oral diet and were free from<br />
pneumonia during their hospitalization and within 35 days of<br />
<strong>Gundersen</strong> <strong>Lutheran</strong> Medical Journal • Volume 6, Number 1, June 2009 9<br />
ID Stamp:<br />
Reason for Admission/Primary Diagnosis:____________________________________________<br />
Date of Admission:_____________ Attending Staff:__________________________________<br />
House Staff:___________________________ RN Completing Index:_____________________<br />
Dates:________________________________________________________________________<br />
Trials<br />
Critical Criteria* Check if Present Check if Present Check if Present<br />
Decreased volitional cough _____ _____ _____<br />
Wet hoarseness _____ _____ _____<br />
Audible oropharyngeal pooling<br />
of secretions _____ _____ _____<br />
Decreased mental status _____ _____ _____<br />
Tracheostomy _____ _____ _____<br />
Tube feedings, NG or gastrostomy _____ _____ _____<br />
Assessment*<br />
Coughs on secretions _____ _____ _____<br />
Coughs on 3-ounce H2O trials _____ _____ _____<br />
Swallowing frequency (4 or < in 5’) _____ _____ _____<br />
This screen should be administered a minimum of three times within 24-48 hours of admission.<br />
If patient demonstrates one or more of the critical criteria, coughs on secretions, has failed H2O<br />
swallowing trials, or swallows four times or less in a five minute time period, then status should<br />
be NPO including medications unless they can only be given orally) until the screen is passed or<br />
formal evaluation of deglutitory function has been completed.
discharge. Twelve patients (2%) developed pneumonia during<br />
their hospitalization, 6 of whom were diagnosed with aspiration<br />
pneumonia by clinical examination and chest radiograph. Neither<br />
prior stroke nor premorbid dysphagia were good predictors of a<br />
patient’s ability to maintain a safe oral diet (P = .34; P = .26). Six<br />
patients (1%) developed pneumonia after discharge from hospital<br />
and subsequent placement in an extended care facility. Thirty-two<br />
patients (6%) died during the course of the study, 3 of whom had<br />
pneumonia, although it was not determined if pneumonia was the<br />
cause of death. Three patients were lost to followup.<br />
Of the 578 patients who passed GLADS, 222 experienced a<br />
left cerebral hemisphere stroke, 190 had a right hemisphere stroke,<br />
25 had a brainstem stroke, and 21 had bihemispheric cerebral<br />
strokes, based upon clinical examination, radiographic study, or<br />
table 1. Demographic and Clinical Characteristics of 578 Patients<br />
Passing GLADS<br />
Characteristic n (%)<br />
Sex<br />
Men<br />
Women<br />
Prior stroke<br />
Yes<br />
No<br />
Premorbid conditions<br />
Dysphagia<br />
Pneumonia<br />
Aspiration<br />
Nutritional / pneumonia outcomes<br />
Adequate oral diet, no pneumonia<br />
Pneumonia during hospital stay<br />
Aspiration pneumonia<br />
Pneumonia after discharge<br />
Total pneumonias<br />
Supplemental nutrition<br />
Deaths<br />
Deaths with concurrent pneumonia<br />
Lost to follow-up<br />
Stroke location<br />
Left cerebral hemisphere<br />
Right cerebral hemisphere<br />
Brainstem<br />
Bihemispheric<br />
Undetermined<br />
Stroke type<br />
Ischemic<br />
Hemorrhagic<br />
Ischemic / hemorrhagic<br />
Undetermined<br />
Communicative / cognitive deficit<br />
Dysarthria / dyspraxia<br />
Aphasia<br />
Dementia<br />
None<br />
287<br />
291<br />
201<br />
377<br />
10<br />
0<br />
1<br />
524<br />
12<br />
6<br />
6<br />
18<br />
4<br />
32<br />
3<br />
3<br />
222<br />
190<br />
25<br />
21<br />
120<br />
334<br />
12<br />
4<br />
228<br />
124<br />
82<br />
99<br />
273<br />
(50)<br />
(50)<br />
(35)<br />
(65)<br />
(2)<br />
(0)<br />
(0)<br />
(91)<br />
(2)<br />
(50)<br />
(1)<br />
(3)<br />
(1)<br />
(6)<br />
(9)<br />
(1)<br />
(38)<br />
(33)<br />
(4)<br />
(4)<br />
(21)<br />
(58)<br />
(2)<br />
(1)<br />
(39)<br />
(21)<br />
(14)<br />
(17)<br />
(47)<br />
both. Site of lesion could not be determined from neuroimaging<br />
for the remaining 120 patients. We found no significant association<br />
between site of lesion and pneumonia (P = .24).<br />
Three hundred thirty-four patients (58%) experienced an<br />
ischemic stroke with the current admission, 12 hemorrhagic, and<br />
4 with features of both ischemic and hemorrhagic stroke. For<br />
228 (39%) patients, medical records failed to indicate if stroke<br />
was ischemic or hemorrhagic. However, all patients had at least<br />
1 neuroimaging study, so a hemorrhagic lesion, if present, likely<br />
would have been identified. Thus, it could be argued that these<br />
strokes were ischemic. Two hundred seventy-three patients (47%)<br />
had normal or minimally affected speech, language, and/or<br />
cognition. One hundred twenty-four patients had distinct focal<br />
speech deficits, that is, dysarthria or dyspraxia of speech. Eightytwo<br />
patients had aphasia, and 99 patients had findings consistent<br />
with dementia. There was no significant association between these<br />
findings and pneumonia (P = .15). Moreover, having either a<br />
communicative or cognitive deficit was not a good predictor of a<br />
patient’s ability to maintain a safe oral diet after stroke (P = .89).<br />
The median length of stay for patients passing GLADS was 3 days<br />
(range 1-38 days), and the median cost of hospitalization was<br />
$7,967. For the 12 patients who passed GLADS but developed<br />
pneumonia during hospitalization, the median length of stay was<br />
6.5 days, and the median cost was $20,099. Table 1 summarizes<br />
the findings for the 578 patients passing GLADS.<br />
Of the 175 patients failing GLADS, 88 were men and 87<br />
were women. Sixty-nine patients (39%) had a history of prior<br />
stroke. Thirteen patients reportedly had pre-existing dysphagia,<br />
the nature of which was unclear. Neither prior stroke nor preexisting<br />
dysphagia was a good predictor of a patient’s ability to<br />
safely tolerate an oral diet (P = .92, P = .28).<br />
With behavioral therapy for their dysphagia, 84 patients (48%)<br />
maintained an oral diet and 82 remained free from pneumonia<br />
within the study period. Fourteen patients developed pneumonia<br />
during their hospitalization—7 presumably due to aspiration—and<br />
2 developed pneumonia after discharge, for an overall pneumonia<br />
rate of 9%, a rate significantly higher than that of the patients who<br />
passed GLADS, both during hospitalization and after discharge<br />
(P = .0002; P = .0008).<br />
Thirty-two patients (18%) required enteral nutritional<br />
support in conjunction with their dysphagia therapy. Fifty-five<br />
patients (31%) died during the study period, 11 possibly due<br />
to pneumonia. Three patients were placed on comfort care, and<br />
1 patient was lost to follow-up. The death rate was significantly<br />
higher for patients who failed GLADS than for those who passed<br />
(31% vs 5.5%, odds ratio 7.8; range 4.9-12.6; P < .0001). Sixtyfive<br />
patients experienced a left hemispheric and 68 patients a right<br />
hemispheric stroke. Fourteen patients had brainstem and 4 patients<br />
had bihemispheric stroke, while site of lesion was undetermined<br />
from neuroimaging for 24 patients. Like those who passed, patients<br />
who failed GLADS exhibited no significant association between<br />
the site of lesion and pneumonia (P = .75).<br />
Like those patients who passed GLADS, most patients who<br />
failed had experienced an ischemic stroke (106 patients, 61%).<br />
Seven patients had experienced a hemorrhagic stroke, while for 62<br />
patients (35%), medical records failed to indicate if the stroke was<br />
ischemic or hemorrhagic. However, as previously posited for those<br />
10 <strong>Gundersen</strong> <strong>Lutheran</strong> Medical Journal • Volume 6, Number 1, June 2009
outCoMeS froM A SCreeninG proCedure for orophArynGeAL dySphAGiA<br />
patients who passed GLADS, these patients’ strokes were likely<br />
ischemic. Like those patients passing GLADS, those who failed<br />
had normal or minimally impaired speech, language, or cognitive<br />
function (78 patients, 45%). For those patients with impairment, a<br />
motor speech disorder was most common (44 patients, 25%), and<br />
a focal language disorder (aphasia) was least common (19 patients,<br />
11%). Thirty-four patients had dementia. We found no significant<br />
association between these deficits and pneumonia (P = .61), nor, as<br />
for those patients passing GLADS, were they good predictors of a<br />
patient’s ability to maintain a safe oral diet after stroke (P = .89).<br />
Median length of stay for patients failing GLADS was 5 days<br />
(range 1-62 days), significantly higher than for those patients who<br />
passed (3 days, P < .0001). Median cost of hospitalization for these<br />
patients was $11,703, which was also significantly higher than<br />
for those who passed (P < .0001). For the 14 patients who failed<br />
GLADS and developed pneumonia during hospitalization, the<br />
median length of stay was 7 days, and the median cost $19,933.<br />
Moreover, if odds ratios are considered, the 175 patients failing<br />
GLADS were 4 times more likely to develop pneumonia during<br />
hospitalization than were the 578 who passed (95% CI, 1.86-<br />
9.04). Table 2 summarizes the findings for the 175 patients failing<br />
GLADS.<br />
diSCuSSion<br />
Results of the current investigation suggest that GLADS is an<br />
effective screening measure for oropharyngeal dysphagia following<br />
acute stroke when administered by carefully trained nurses in<br />
conjunction with an ASCP. Barring unrelated stroke complications,<br />
over 90% of patients passing GLADS were able to maintain a safe<br />
and nutritionally sound oral diet without pneumonia or further<br />
comprehensive evaluation for dysphagia during hospitalization.<br />
They were also less likely than patients who failed GLADS to<br />
develop pneumonia during their hospitalization or after discharge.<br />
We found that neither site of lesion nor communicative or cognitive<br />
deficits was a predictor of who would develop pneumonia. We<br />
also found that prior stroke—even with related comorbidities<br />
including dysphagia or speech or cognitive deficits—was not a<br />
good predictor of a patient’s ability to maintain a safe oral diet<br />
following a new stroke. Not surprisingly, cost of hospitalization<br />
and length of stay were reduced when stroke was not complicated<br />
by pneumonia.<br />
One might argue that the 175 patients who failed GLADS<br />
had more devastating strokes that resulted in a complicated course<br />
with protracted hospitalization, increased expense, and a higher<br />
death rate than those who passed GLADS. Interestingly, however,<br />
with time and dysphagia therapy, almost half of these patients<br />
went on to become functional and safe oral feeders during their<br />
hospitalization. This finding could also represent the influence of<br />
the comprehensiveness and intensity of the ASCP itself.<br />
The importance of a swallowing screen as a component of an<br />
ASCP has been stressed by others. 42 Using a speech pathologist or<br />
certified nurse to screen for dysphagia, they found that 48 of 124<br />
patients (39%) failed the initial screen and required dietary texture<br />
change, as well as direct dysphagia therapy. Whereas in our study<br />
patients who failed GLADS were referred for further evaluation<br />
prior to initiation of an oral diet, their patients apparently did<br />
not undergo further workup for dysphagia or aspiration prior<br />
table 2. Demographic and Clinical Characteristics of 175 Patients<br />
Failing GLADS<br />
Characteristic n (%)<br />
Sex<br />
Men<br />
Women<br />
Prior stroke<br />
Yes<br />
No<br />
Premorbid conditions<br />
Dysphagia<br />
Pneumonia<br />
Aspiration<br />
Nutritional / pneumonia outcomes<br />
Adequate oral diet, no pneumonia<br />
Pneumonia during hospital stay<br />
Aspiration pneumonia<br />
Pneumonia after discharge<br />
Total pneumonias<br />
Supplemental nutrition<br />
Deaths<br />
Deaths with concurrent pneumonia<br />
Comfort measures<br />
Lost to follow-up<br />
Stroke location<br />
Left cerebral hemisphere<br />
Right cerebral hemisphere<br />
Brainstem<br />
Bihemispheric<br />
Undetermined<br />
Stroke type<br />
Ischemic<br />
Hemorrhagic<br />
Undetermined<br />
Communicative / cognitive deficit<br />
Dysarthria / dyspraxia<br />
Aphasia<br />
Dementia<br />
None<br />
to initiating an oral diet. However, none of their patients were<br />
reported to have developed aspiration pneumonia. Using a water<br />
swallow screening test for 100 consecutive acute stroke patients,<br />
Nilsson et all have reported a pneumonia rate of 14% (2 of 14<br />
dysphagic patients). 46 Apparently neither of the patients who<br />
developed pneumonia received direct swallowing therapy. In our<br />
study, 14 of 175 patients failing GLADS developed pneumonia<br />
during hospitalization, which—if odds ratios are considered—is 4<br />
times the likelihood of the 578 patients who passed.<br />
Aspiration pneumonia following stroke has a reported<br />
incidence rate of 13%. 47 Moreover, the incidence of pneumonia<br />
increases with age, particularly over 65 years. 48 Hinchey et al 12<br />
found from a prospective multicenter study that institutions that<br />
had formal dysphagia screening protocols for acute stroke had<br />
<strong>Gundersen</strong> <strong>Lutheran</strong> Medical Journal • Volume 6, Number 1, June 2009 11<br />
88<br />
87<br />
69<br />
106<br />
13<br />
0<br />
0<br />
82<br />
14<br />
7<br />
2<br />
16<br />
32<br />
55<br />
11<br />
3<br />
1<br />
65<br />
68<br />
14<br />
4<br />
24<br />
106<br />
7<br />
62<br />
44<br />
19<br />
34<br />
78<br />
(50)<br />
(50)<br />
(39)<br />
(61)<br />
(7)<br />
(0)<br />
(0)<br />
(47)<br />
(8)<br />
(50)<br />
(1)<br />
(9)<br />
(18)<br />
(31)<br />
(34)<br />
(2)<br />
(.5)<br />
(37)<br />
(39)<br />
(8)<br />
(2)<br />
(14)<br />
(61)<br />
(4)<br />
(35)<br />
(25)<br />
(11)<br />
(19)<br />
(45)
pneumonia rates of 2.4%, versus 5.4% for those that did not.<br />
Although the specific nature of the protocols was not fully<br />
described, and randomization was an issue, their results led<br />
them to conclude that “A formal dysphagia screen prevented<br />
pneumonia even after adjusting for stroke severity.” 12(p1973)<br />
Outcomes from the current and previous studies<br />
incorporating a screening procedure for dysphagia<br />
in acute stroke in conjunction with an acute care<br />
pathway 12,42 may be a reflection of the propensity of<br />
dysphagia following stroke to improve or resolve within<br />
6 months of onset, 3,9 the nature of acute stroke pathways, which<br />
are inherently designed to provide the most comprehensive<br />
and efficacious treatment for the patient and to prevent<br />
complications from acute stroke, or a combination of these<br />
factors. Other than diet modification and regular observation<br />
by the medical and nursing team for signs of change in status<br />
related to oral feedings, none of the 578 patients who passed<br />
GLADS received formal dysphagia therapy. Thus, it could be<br />
concluded that their dysphagia, if present, was mild and not<br />
disabling.<br />
Median length of hospital stay and cost of hospitalization<br />
were lower for those patients whose stroke was not<br />
complicated by pneumonia. Similar trends have been noted<br />
previously. 12,28,49<br />
Like others, 13 we believe that screening procedures like<br />
GLADS do not delineate the specific nature of dysphagia,<br />
only whether the patient is having or may be at risk for<br />
swallowing difficulties. Nonetheless, based upon the results<br />
of the current investigation as well as the work of others, 42<br />
we conclude that nursing staff can be trained to administer<br />
a screening tool for dysphagia following acute stroke that<br />
will allow implementation of oral feedings with minimal or<br />
no complications, even though the nature of the swallowing<br />
disorder may not have been fully delineated.<br />
We believe GLADS was effective not only because it was<br />
administered by trained nursing staff, but also because of<br />
elements included in the screening tool itself and how they<br />
were used, rather than individual screening measures that<br />
have been used previously for dysphagia, for example, the 3-oz<br />
water swallow test, 32,33 swallowing frequency, or a timed test<br />
of swallowing. 40,41 The importance of co-occuring risk factors<br />
(Critical Criteria) has been stressed by others as well. 5,7,18,34,50<br />
If a screening tool alone, such as GLADS, is effective<br />
for implementing an uncomplicated oral feeding regimen<br />
following acute stroke, what, then, is the role of VFSS and<br />
videoendoscopic swallowing evaluation? We propose, as<br />
implemented at our institution and suggested elsewhere, 23<br />
that these procedures be reserved for patients who fail a<br />
comprehensive screening procedure or who have inconclusive<br />
screening results, who have unstable medical conditions that<br />
can potentially affect deglutitory function and subsequent<br />
respiration, or who require radiographic or photographic<br />
documentation of swallowing function prior to and following<br />
an invasive or surgical procedure.<br />
Finally, we believe that we have taken a step in meeting<br />
1 of the recommendations concerning the need for further<br />
development of efficacious screening procedures and best<br />
practice strategies for dysphagia. 21-23 Although it proved<br />
difficult logistically to incorporate into this retrospective study,<br />
a measure of interrater reliability for nurses administering<br />
GLADS should be included in future prospective investigations.<br />
Given today’s healthcare environment, more research is both<br />
needed and recommended to develop safe, reliable, and costeffective<br />
screening tools for dysphagia following stroke.<br />
ACknoWLedGMentS<br />
The authors thank <strong>Gundersen</strong> <strong>Lutheran</strong> Medical<br />
Foundation for sponsoring Melissa Hunter’s summer research<br />
fellowship. We also wish to thank Cathy Lazarus, PhD,<br />
BRS-S, New York University School of Medicine, for her<br />
insightful and critical comments, and <strong>Gundersen</strong> <strong>Lutheran</strong><br />
<strong>Health</strong> <strong>System</strong> and <strong>Gundersen</strong> <strong>Lutheran</strong> Medical Foundation<br />
for their ongoing support for research.<br />
referenCeS<br />
1. National Stroke Association. National Stroke Association’s Complete Guide<br />
to Stroke. 1999, pp 3. National Stroke Association Web site. http://www.<br />
stroke.org/site/DocServer/NSA_ complete_guide.pdf?docID =341. Accessed<br />
December 10, 2007.<br />
2. American Heart Association. Heart & Stroke Facts: 1996 Statistical<br />
Supplement. New York: American Heart Association; 1996.<br />
3. Barer DH. The natural history and functional consequences of dysphagia<br />
after hemispheric stroke. J Neurol Neurosurg Psychiatry. 1989;52(2):236-<br />
241.<br />
4. Veis SL, Logemann JA. Swallowing disorders in persons with cerebrovascular<br />
accident. Arch Phys Med Rehabil. 1985;66(6):372-375.<br />
5. Horner J, Massey EW, Riski JE, Lathrop DL, Chase KN. Aspiration following<br />
stroke: clinical correlates and outcome. Neurology. 1988;38(9):1359-1362.<br />
6. Groher ME, Bukatman R. The prevalence of swallowing disorders in two<br />
teaching hospitals. Dysphagia. 1986;1(1):3-6.<br />
7. Horner J, Massey EW. Silent aspiration following stroke. Neurology. 1988;38(2):<br />
317-319.<br />
8. Linden P, Siebens AA. Dysphagia: predicting laryngeal penetration. Arch<br />
Phys Med Rehabil. 1983;64(6):281-284.<br />
9. Smithard DG, O’Neill PA, England RE, et al. The natural history of<br />
dysphagia following a stroke. Dysphagia. 1997;12(4):188-193.<br />
10. Schmidt J, Holas M, Halvorson K, Reding M. Videofluoroscopic evidence<br />
of aspiration predicts pneumonia and death but not dehydration following<br />
stroke. Dysphagia. 1994;9(1):7-11.<br />
11. Swigert NB. NPO until dysphagia screen. Presented at: American Heart<br />
Association Telephone Conference; July 4, 2007.<br />
12. Hinchey JA, Shephard T, Furie K, et al. Formal dysphagia screening<br />
protocols prevent pneumonia. Stroke. 2005;36(9):1972-1976.<br />
13. Logemann JA, Veis S, Colangelo L. A screening procedure for oropharyngeal<br />
dysphagia. Dysphagia. 1999;14(1):44-51.<br />
14. Logemann JA. Evaluation and Treatment of Swallowing Disorders. San<br />
Diego, CA: College-Hill Press; 1983:249.<br />
15. Splaingard ML, Hutchins B, Sulton LD, Chaudhuri G. Aspiration in<br />
rehabilitation patients: videofluoroscopy vs bedside clinical assessment.<br />
Arch Phys Med Rehabil. 1988;69(8):637-640.<br />
12 <strong>Gundersen</strong> <strong>Lutheran</strong> Medical Journal • Volume 6, Number 1, June 2009
outCoMeS froM A SCreeninG proCedure for orophArynGeAL dySphAGiA<br />
16. McCullough GH, Wertz RT, Rosenbek JC, Dinneen C. Clinicians’ preferences<br />
and practices in conducting clinical/bedside and videofluoroscopic swallowing<br />
examinations in an adult neurogenic population. American Journal of Speech-<br />
Language Pathology. 1999;8:149-163.<br />
17. Farrell Z, Murphy E. A comment on “the natural history of dysphagia following a<br />
stroke” (Dysphagia 1997;12:188-193). Dysphagia. 1998;13(4):230-231.<br />
18. Garon BR, Engle M, Ormiston C. Reliability of the 3-oz water swallow<br />
test utilizing cough reflex as sole indicator of aspiration. J Neurol Rehabil.<br />
1995;9(3):139-143.<br />
19. Garon BR, Engle M, Ormiston C. Silent aspiration: results of 1,000<br />
videofluoroscopic swallow evaluations. J Neurol Rehabil. 1996;10(2):121-126.<br />
20. Trapl M, Enderle P, Nowotny M, et al. Dysphagia bedside screening for<br />
acute-stroke patients: the Gugging Swallowing Screen. Stroke. 2007;38(11):<br />
2948-2952.<br />
21. Martino R, Pron G, Diamant N. Screening for oropharyngeal dysphagia in<br />
stroke: insufficient evidence for guidelines. Dysphagia. 2000;15(1):19-30.<br />
22. Perry L, Love CP. Screening for dysphagia and aspiration in acute stroke: a<br />
systematic review. Dysphagia. 2001;16(1):7-18.<br />
23. Eisenberg JM, Kamerow DB. Diagnosis and Treatment of Swallowing Disorders<br />
(Dysphagia) in Acute-Care Stroke Patients. Evidence Report/Technology<br />
Assessment Number 8. Rockville, MD: Agency for <strong>Health</strong> Care Policy and<br />
Research; 1999. AHCPR Publication No. 99-E024.<br />
24. The Joint Commission. Stroke Performance Measurement Implementation<br />
Guide. The Joint Commission Web site. http://www.jointcommission.org/<br />
CertificationPrograms/PrimaryStrokeCenters/guide_table_contents.htm.<br />
Accessed December 10, 2007.<br />
25. Smith HA, Lee SH, O’Neill PA, Connolly MJ. The combination of bedside<br />
swallowing assessment and oxygen saturation monitoring of swallowing in acute<br />
stroke: a safe and humane screening tool. Age Ageing. 2000;29(6):495-499.<br />
26. Teramoto S, Fukuchi Y. Detection of aspiration and swallowing disorder in older<br />
stroke patients: simple swallowing provocation test versus water swallowing test.<br />
Arch Phys Med Rehabil. 2000;81(11):1517-1519.<br />
27. Mosheim J. Swallow screening: a protocol for the front line of patient care.<br />
Advance for Speech Language Pathologists and Audiologists. 2007;17(5):6-9.<br />
28. Odderson IR, McKenna BS. A model for management of patients with<br />
stroke during the acute phase. outcome and economic implications. Stroke.<br />
1993;24(12):1823-1827.<br />
29. Lim SH, Lieu PK, Phua SY, et al. Accuracy of bedside clinical methods compared<br />
with fiberoptic endoscopic examination of swallowing (FEES) in determining<br />
the risk of aspiration in acute stroke patients. Dysphagia. 2001;16(1):1-6.<br />
30. Selley WG, Flack FC, Ellis RE, Brooks WA. The Exeter Dysphagia Assessment<br />
Technique. Dysphagia. 1990;4(4):227-235.<br />
31. Daniels SK, McAdam CP, Brailey K, Foundas AL. Clinical assessment of<br />
swallowing and prediction of dysphagia severity. Am J Speech Lang Pathol.<br />
1997;6(4):17-24.<br />
32. DePippo KL, Holas MA, Reding MJ. Validation of the 3-oz water swallow test<br />
for aspiration following stroke. Arch Neurol. 1992;49(12):1259-1261.<br />
33. DePippo KL, Holas MA, Reding MJ. The Burke Dysphagia Screening<br />
Test: validation of its use in patients with stroke. Arch Phys Med Rehabil.<br />
1994;75(12):1284-1286.<br />
34. Daniels SK, Brailey K, Priestly DH, Herrington LR, Weisberg LA, Foundas AL.<br />
Aspiration in patients with acute stroke. Arch Phys Med Rehabil. 1998;79(1):14-19.<br />
35. Addington WR, Stephens RE, Gilliland K, Rodriguez M. Assessing the laryngeal<br />
cough reflex and the risk of developing pneumonia after stroke. Arch Phys Med<br />
Rehabil. 1999;80(2):150-154.<br />
36. Addington WR, Stephens RE, Gilliland KA. Assessing the laryngeal cough reflex<br />
and the risk of developing pneumonia after stroke: an interhospital comparison.<br />
Stroke. 1999;30(6):1203-1207.<br />
37. Warms T, Richards J. “Wet voice” as a predictor of penetration and aspiration in<br />
oropharyngeal dysphagia. Dysphagia. 2000;15(2):84-88.<br />
38. Linden P, Kuhlemeier KV, Patterson C. The probability of correctly predicting<br />
subglottic penetration from clinical observations. Dysphagia. 1993;8(3):170-179.<br />
39. Mari F, Matei M, Ceravolo MG, Pisani A, Montesi A, Provinciali L. Predictive<br />
value of clinical indices in detecting aspiration in patients with neurological<br />
disorders. J Neurol Neurosurg Psychiatry. 1997;63(4):456-460.<br />
40. Murray J, Langmore SE, Ginsberg S, Dostie A. The significance of accumulated<br />
oropharyngeal secretions and swallowing frequency in predicting aspiration.<br />
Dysphagia. 1996;11(2):99-103.<br />
41. Nathadwarawala KM, Nicklin J, Wiles CM. A timed test of swallowing capacity<br />
for neurological patients. J Neurol Neurosurg Psychiatry. 1992;55(9):822-825.<br />
42. Odderson IR, Keaton JC, McKenna BS. Swallow management in patients<br />
on an acute stroke pathway: quality is cost effective. Arch Phys Med Rehabil.<br />
1995;76(12):1130-1133.<br />
43. Hartman DE, Havlik P, Hutter RD, Schneller C. Screening for oropharyngeal<br />
dysphagia in acute stroke. Paper presented at: Annual Meeting of the American<br />
Speech-Language-Hearing Association; November 2001; New Orleans, LA.<br />
44. Hartman DE, Hutter RD, Schneller C, Havlik P. A screening procedure for<br />
oropharyngeal dysphagia in an acute stroke care pathway. Paper presented at:<br />
Annual Meeting of the Wisconsin Speech-Language-Hearing Association;<br />
February 2002; Milwaukee, WI.<br />
45. Langmore SE, Schatz K, Olsen N. Fiberoptic endoscopic examination of<br />
swallowing safety: a new procedure. Dysphagia. 1988;2(4):216-219.<br />
46. Nilsson H, Ekberg O, Olsson R, Hindfelt B. Dysphagia in stroke: a prospective<br />
study of quantitative aspects of swallowing in dysphagic patients. Dysphagia.<br />
1998;13(1):32-38.<br />
47. Young EC, Durant-Jones L. Developing a dysphagia program in an acute care<br />
hospital: a needs assessment. Dysphagia. 1990;5(3):159-165.<br />
48. Houston MS, Silverstein MD, Suman VJ. Community-acquired lower<br />
respiratory tract infection in the elderly: a community-based study of incidence<br />
and outcome. J Am Board Fam Pract. 1995;8(5):347-356.<br />
49. Katzan IL, Dawson NV, Thomas CL, Votruba ME, Cebul RD. The cost of<br />
pneumonia after acute stroke. Neurology. 2007;68(22):1938-1943.<br />
50. Langmore SE, Terpenning MS, Schork A, et al. Predictors of aspiration<br />
pneumonia: how important is dysphagia? Dysphagia. 1998;13(2):69-81.<br />
<strong>Gundersen</strong> <strong>Lutheran</strong> Medical Journal • Volume 6, Number 1, June 2009 13
Authors:<br />
Alexander D. Wade, MD<br />
Department of Medical Education<br />
<strong>Gundersen</strong> <strong>Lutheran</strong> Medical<br />
Foundation<br />
Frank J. Aberger, MD<br />
Department of Gastroenterology<br />
<strong>Gundersen</strong> <strong>Lutheran</strong> <strong>Health</strong> <strong>System</strong><br />
Address for correspondence:<br />
Frank J. Aberger, MD<br />
Mail Stop H05-007<br />
<strong>Gundersen</strong> <strong>Lutheran</strong> <strong>Health</strong> <strong>System</strong><br />
1900 South Avenue<br />
La Crosse, WI 54601<br />
Telephone: (608) 775-2702<br />
Facsimile: (608) 775-6395<br />
email: fjaberge@gundluth.org<br />
A<br />
Colonoscopic Diagnosis of Appendicitis in a<br />
Patient with Ulcerative Colitis:<br />
A Case Report and Review of the Literature<br />
AbStrACt<br />
ppendicitis is a common cause of acute abdominal pain.<br />
Over the past 2 decades, a number of cases of appendicitis<br />
due to colonoscopy have been reported, 1-8 as well as cases of<br />
appendicitis diagnosed by colonoscopy, 9-18 often when other<br />
diagnostic modalities have failed to diagnose appendicitis or have<br />
suggested other diagnoses. Unusual presentations of appendicitis,<br />
particularly in patients with abdominal comorbidities, sometimes<br />
lead to colonoscopy, which is almost never used as a first line of<br />
investigation because of the risk of complications such as bleeding or<br />
perforation, and because noninvasive tests such as ultrasonography<br />
and computed tomography (CT) are highly sensitive. 19<br />
CASe report<br />
A 17-year-old boy came to our urgent care clinic with a 2-week<br />
complaint of increasing periumbilical and right lower quadrant<br />
abdominal pain and recent rectal bleeding. He was known to have<br />
ulcerative colitis, diagnosed in 2001 by colonoscopy with biopsies.<br />
He had been hospitalized in 2005 for ulcerative colitis, at which time<br />
CT scan documented a 6- to 7-mm appendix but no inflammation.<br />
He was compliant with his medication (sulfasalazine 1000 mg by<br />
mouth twice a day), and his ulcerative colitis had been quiescent.<br />
His temperature was normal, his white blood cell (WBC) count was<br />
14 000/µL (75.2% neutrophils, 26% of which were bands), and<br />
his erythrocyte sedimentation rate (ESR) (105 mm/h, reference<br />
range = 0-15) and C-reactive protein (CRP) concentration (13.1<br />
mg/L, reference range = 0.08-3.1) were elevated. Results of an<br />
abdominal CT scan were normal (Figure 1).<br />
The patient’s gastroenterologist was notified and scheduled<br />
the patient for flexible sigmoidoscopy the following day, which<br />
documented normal rectal mucosa, decreasing the likelihood<br />
that the patient’s symptoms were attributable to ulcerative colitis.<br />
With his pain, rectal bleeding, and normal flexible sigmoidoscopy<br />
findings, Crohn disease was believed to be a possible diagnosis.<br />
A 17-year-old boy with a known history of ulcerative colitis came to urgent care with a 2-week<br />
history of periumbilical pain and an episode of rectal bleeding. His evaluation included a<br />
computed tomographic (CT) scan, gastroenterology consultation, flexible sigmoidoscopy, CT<br />
enterography, abdominal ultrasonography, double-contrast upper gastrointestinal study,<br />
esophagogastroduodenoscopy, and, ultimately, a complete colonoscopic examination<br />
that revealed pus exuding from the appendiceal orifice. Repeat CT scan, with knowledge<br />
of the colonoscopy results, was interpreted as normal. Laparoscopic appendectomy was<br />
performed and confirmed the diagnosis of suppurative appendicitis. The patient had a benign<br />
postoperative course, and his symptoms have not recurred. We review the English-language<br />
literature regarding colonoscopically diagnosed appendicitis. To our knowledge, this is the first<br />
report in the literature of a case of colonoscopically diagnosed appendicitis in a patient with<br />
ulcerative colitis.<br />
CT enterography demonstrated normal small bowel caliber and<br />
wall thickness.<br />
The patient’s pain persisted. He was scheduled for<br />
ultrasonographic examination of the abdomen, as well as a doublecontrast<br />
upper gastrointestinal (GI) series. The gastroenterologist<br />
suggested a complete colonoscopic examination to look for possible<br />
Crohn disease if these studies failed to diagnose the etiology of<br />
the pain.<br />
Two days later, because of persisting pain, the patient underwent<br />
abdominal ultrasonography. A single loop of slightly thick-walled<br />
small bowel (4.7 mm) was identified as the only abnormality. This<br />
was followed by a double-contrast upper GI series and small bowel<br />
follow-through that revealed a normal esophagus and stomach, and<br />
no evidence of hiatal hernia or gastroesophageal reflux. Transit time<br />
through the small bowel into the colon was approximately 2 hours.<br />
The small bowel loops, including the terminal ileum, appeared<br />
normal. By this time, the patient’s leukocytosis had normalized,<br />
although his ESR (78 mm/hr) and CRP concentration (2.8 mg/L)<br />
remained elevated.<br />
Almost 2 weeks after his initial visit, the patient was again seen<br />
by his gastroenterologist. He remained symptomatic, complaining<br />
of diarrhea and abdominal pain. Laboratory studies revealed a<br />
WBC count within reference range, with neutrophilia (77.9%,<br />
reference range = 34%-67%) and a persistently elevated ESR<br />
(46 mm/hr). Mild anemia was also detected (hemoglobin<br />
concentration 11.9 g/dL). His CRP concentration was within<br />
normal range. Findings from an upper endoscopic examination<br />
were unremarkable.<br />
He underwent a colonoscopy, the results of which proved<br />
negative for colitis. The rectum appeared normal, indicating that<br />
the symptoms were not related to his ulcerative colitis. The cecum<br />
and the distal ileum were examined and appeared normal, thus<br />
reducing the likelihood of Crohn disease as the etiology for the<br />
symptoms. A small amount of mucin or pus was seen to emanate<br />
14 <strong>Gundersen</strong> <strong>Lutheran</strong> Medical Journal • Volume 6, Number 1, June 2009
figure 1. Axial reformatted computed tomographic scan of the<br />
abdomen and pelvis performed on the day of presentation. The<br />
appendix appears normal, and no other pathology is present to<br />
explain the patient’s pain.<br />
from the appendiceal orifice (Figure 2). This was aspirated and sent<br />
to the laboratory, where analysis detected a large number of white<br />
blood cells, gram-negative rods, and gram-positive cocci. Results of<br />
the biopsy of the mucosa at the base of the appendix demonstrated<br />
mild nonspecific chronic and focal acute inflammation.<br />
The general surgeon on call was notified and observed the<br />
appendiceal findings at colonoscopy. The patient’s generally<br />
benign condition and the duration of the symptoms were<br />
taken into consideration, as was the interesting finding of freely<br />
flowing pus from the appendiceal orifice. The surgeon elected to<br />
observe the patient over the weekend and repeat a CT scan if his<br />
symptoms persisted.<br />
The patient remained symptomatic and underwent a repeat CT<br />
scan. The radiologist noted that this scan was similar in appearance<br />
to the patient’s previous studies and that the appendix was fluidfilled,<br />
although the walls were not thickened and there were no<br />
inflammatory changes. The remainder of the abdomen and pelvis<br />
appeared normal.<br />
The following day, the patient underwent laparoscopic<br />
appendectomy. Intraoperative findings included an enlarged,<br />
inflamed appendix and mild mesenteric scarring around the<br />
CoLonoSCopiC diAGnoSiS of AppendiCitiS<br />
terminal ileum. No signs of active Crohn disease or ulcerative colitis<br />
were identified. No signs of a Meckel diverticulum were present.<br />
Routine pathologic evaluation of the appendix later confirmed the<br />
diagnosis of acute suppurative appendicitis with benign lymphoid<br />
hyperplasia. The patient was discharged home after a brief and<br />
benign recovery.<br />
Just over a month later, the patient was seen in the emergency<br />
department for recurrent abdominal pain, which quickly resolved<br />
without intervention. His postoperative course had been benign<br />
until that point, with the exception of a knee joint effusion, possibly<br />
related to trauma from playing basketball. Since that episode 24<br />
months ago, the patient has reported no abdominal pain.<br />
To our knowledge, this is the first report of colonoscopic<br />
diagnosis of appendicitis in a patient with known ulcerative colitis<br />
and possible Crohn disease, which significantly confounded the<br />
evaluation.<br />
diSCuSSion<br />
In 1994, Said et al reported a case of atypical appendicitis that<br />
was diagnosed by colonoscopy. The patient had experienced<br />
abdominal pain and fever for 2 weeks and was hospitalized and<br />
treated nonoperatively. The results of laboratory studies were<br />
consistent with inflammation. Workup included ultrasonography<br />
and upper endoscopy. On the third day after admission,<br />
colonoscopy was performed, pus was aspirated from the<br />
appendiceal orifice, and the patient’s symptoms resolved within<br />
a day. Interval appendectomy was performed 5 months later and<br />
confirmed a previous diagnosis of appendicitis. 14<br />
figure 2. Colonoscopy demonstrates pus from the appendiceal os,<br />
slight inflammation near the base of the appendix.<br />
<strong>Gundersen</strong> <strong>Lutheran</strong> Medical Journal • Volume 6, Number 1, June 2009 15
Since that report, other authors have reported colonoscopic<br />
diagnosis of appendicitis in a patient with symptoms suggestive of<br />
inflammatory bowel disease, 15 a patient with symptoms suggestive<br />
of cecal cancer, 15 a cystic fibrosis patient with chronic abdominal<br />
pain and possible inflammatory bowel disease, 17 and a patient with<br />
intermittent abdominal pain seen for polyp surveillance. 16 A case of<br />
appendiceal intussusception in chronic appendicitis diagnosed by<br />
colonoscopy was noted in a patient with symptoms of 8 months’<br />
duration. 13 An asymptomatic 67-year-old patient undergoing<br />
surveillance colonoscopy had acute appendicitis, and emergency<br />
surgery was performed and confirmed the diagnosis. 12<br />
This case demonstrates a fact well known among experienced<br />
surgeons but often poorly understood by referring caregivers:<br />
Appendicitis is often difficult to diagnose, as alluded to at a<br />
personal injury attorney’s Website:<br />
Appendicitis is one of the most commonly misdiagnosed<br />
conditions because its symptoms can masquerade as many<br />
other types of problems. The most common symptoms of<br />
appendicitis are generalized or acute pain in the abdomen and<br />
nausea, vomiting and fever. When presented with symptoms<br />
of likely appendicitis, the standard of care requires doctors to<br />
operate immediately. If a physician fails to perform a proper<br />
physical examination, including manual manipulation of the<br />
abdomen, or impress upon a patient the importance of coming<br />
in immediately should symptoms continue or worsen, he or<br />
she could be liable for medical malpractice. 20<br />
The experienced medical practitioner knows that a proper<br />
physical examination, along with an adequate history, is only the<br />
beginning of an evaluation for possible appendicitis. Even with<br />
“manual manipulation of the abdomen,” appendicitis can go<br />
unrecognized.<br />
Our patient had undergone extensive evaluation by experienced<br />
physicians who took into account his history of ulcerative colitis<br />
and the chronic, indolent nature of the complaint. Crohn disease<br />
was strongly considered in the differential diagnosis. This case,<br />
however, is unusual in that the patient’s appendix was unruptured<br />
after 2 to 6 weeks of inflammation without antibiotic treatment.<br />
Before CT scan imaging was widely available to evaluate patients<br />
with abdominal pain, the rate of appendectomy performed in<br />
the absence of clear signs and symptoms of appendicitis was much<br />
higher. This higher rate was justified in order to prevent a missed<br />
appendicitis. This, however, carries unacceptably high risks of<br />
morbidity and mortality. The increased use of CT for the evaluation<br />
of abdominal pain, and thus the diagnosis of appendicitis, has<br />
reduced the likelihood of inappropriate appendectomy from 15%<br />
or 20% to closer to 2%. The sensitivity of CT scan for appendicitis<br />
is high— according to 1 study, 94% (95% CI, 92%-97%) in<br />
children and 95% (95% CI, 94%-96%) in adults. 19 Unfortunately,<br />
our patient was among the 5% of patients who have false-negative<br />
CT findings. According to 1 study, 21 the specificity of CT scan<br />
for possible appendicitis is 88.3%, meaning that approximately<br />
8 in 9 patients without appendicitis will have a CT scan negative<br />
for appendicitis.<br />
It is impossible to determine unequivocally the true etiology of<br />
this patient’s early abdominal pain. Interestingly, the appendicitis<br />
occurred coincidentally during the workup for the as-yet-<br />
figure 3. Axial reformatted computed tomographic scan obtained<br />
after the colonoscopically diagnosed appendicitis continues to<br />
demonstrate a paucity of findings indicative of inflammation or<br />
infection of the appendix.<br />
unexplained chronic abdominal pain. Most surgeons would be<br />
reluctant to accept acute appendicitis as the explanation for the<br />
6 weeks of pain, knowing that the natural history of untreated<br />
appendicitis does not commonly involve such a benign course. It<br />
is possible that the diagnosis of acute appendicitis was ultimately<br />
incorrect—that a diagnosis of recurrent or chronic appendicitis<br />
was more accurate. Although this could explain the diagnostic<br />
conundrum, it is not universally accepted that chronic or recurrent<br />
appendicitis even exists. Conversely, since his appendectomy, this<br />
patient has had only 1 episode of abdominal pain, which quickly<br />
resolved, suggesting that the appendix was directly related to the<br />
symptoms.<br />
In summary, the diagnosis of appendicitis is rarely made<br />
by colonoscopy. This is the first case we know of in which a<br />
colonoscopic diagnosis of appendicitis was made in a patient with<br />
ulcerative colitis. We do not, however, suggest that colonoscopy<br />
be used as the tool for diagnosis in patients with suspected<br />
appendicitis. For our patient, who had no clear diagnosis for<br />
abdominal pain and a very low suspicion for appendicitis, the<br />
endoscopic findings are of interest and should be considered by<br />
other clinicians who encounter patients with similar unexplained<br />
abdominal discomfort.<br />
16 <strong>Gundersen</strong> <strong>Lutheran</strong> Medical Journal • Volume 6, Number 1, June 2009
eferenCeS<br />
1. Houghton A, Aston N. Appendicitis complicating colonoscopy. Gastrointest<br />
Endosc. 1988;34:489.<br />
2. Vender R, Larson J, Garcia J, Topazian M, Ephraim P. Appendicitis as a<br />
complication of colonoscopy. Gastrointest Endosc. 1995;41:514-516.<br />
3. Hirata K, Noguchi J, Yoshikawa I, et al. Acute appendicitis immediately after<br />
colonoscopy. Am J Gastroenterol. 1996;91:2239-2240.<br />
4. Lipton S, Estrin J. Postcolonoscopy appendicitis: a case report. J Clin Gastroenterol.<br />
1999;28:255-256.<br />
5. Srivastava V, Pink J, Swarnkar K, Feroz A, Stephenson BM. Colonoscopically<br />
induced appendicitis. Colorectal Dis. 2004;6:124-125.<br />
6. Izzedine H, Thauvin H, Maisel A, Bourry E, Deschamps A. Post-colonoscopy<br />
appendicitis: case report and review of the literature. Am J Gastroenterol.<br />
2005;100:2815-2817.<br />
7. Rosen MJ, Sands BE. Acute appendicitis following colonoscopy. J Clin<br />
Gastroenterol. 2005;39:78.<br />
8. Volchok J, Cohn M. Rare complications following colonoscopy: case reports of<br />
splenic rupture and appendicitis. JSLS. 2006;10:114-116.<br />
9. Petro M, Minocha A. Asymptomatic early acute appendicitis initiated and<br />
diagnosed during colonoscopy: a case report. World J Gastroenterol. 2005;11:<br />
5398-5400.<br />
10. Chang HS, Yang SK, Myung SJ, et al. The role of colonoscopy in the diagnosis<br />
of appendicitis in patients with atypical presentations. Gastrointest Endosc.<br />
2002;56:343-348.<br />
11. Johnson TR, DeCosse JJ. Colonoscopic diagnosis of grumbling appendicitis.<br />
Lancet. 1998;351:495.<br />
CoLonoSCopiC diAGnoSiS of AppendiCitiS<br />
12. Uehara A, Ohta H, Nagamine M, Kawashima T, Kuribayashi H, KohgoY.<br />
Colonoscopic diagnosis of asymptomatic acute appendicitis. Am J Gastroenterol.<br />
2000;95:3010-3011.<br />
13. Nyam DC, Davendran K, Seow-Choen F. An endoscopic diagnosis of appendicular<br />
intussusception in chronic appendicitis. Singapore Med J. 1997;38:131.<br />
14. Said M, Ledochowski M, Dietze O, Simader H. Colonoscopic diagnosis and<br />
treatment of acute appendicitis. Eur J Gastroenterol Hepatol. 1995;7:569-571.<br />
15. Chen YY, Soon MS, Yen HH. Images of interest. Gastrointestinal: colonoscopic<br />
features of acute appendicitis. J Gastroenterol Hepatol. 2005;20:1940.<br />
16. Courtney ED, Melville D, Leicester RJ. Chronic appendicitis diagnosed<br />
incidentally by colonoscopy. Hosp Med. 2003;64:434-435.<br />
17. Theilmann L, Bachmann K, Kuhl PG. An unusual presentation of chronic<br />
appendicitis. Endoscopy. 2003;35:377.<br />
18. Johnson EA, Spier BJ, Mozena MG, Pfau PR. Colonoscopic clues cinch the<br />
diagnosis. Am J Med. 2007;120:942-944.<br />
19. Doria AS, Moineddin R, Kellenberger CJ, et al. US or CT for diagnosis of<br />
appendicitis in children and adults? A meta-analysis. Radiology. 2006;241:<br />
83-94.<br />
20. Digestive Disorders & Injuries. Illinois Personal Injury Legal Resource Web site.<br />
//www.il-injury.com/html/digestive-disorders-injuries.html. Accessed March 24,<br />
2008.<br />
21. Flum DR, McClure TD, Morris A, Koepsell T. Misdiagnosis of appendicitis and<br />
the use of diagnostic imaging. J Am Coll Surg. 2005;201:933-939.<br />
River Fog at Dawn Daniel Schraith<br />
Pathology<br />
<strong>Gundersen</strong> <strong>Lutheran</strong> Medical Journal • Volume 6, Number 1, June 2009 17
Authors:<br />
Abhishek Tandon, MD<br />
Department of Medical Education<br />
<strong>Gundersen</strong> <strong>Lutheran</strong> Medical<br />
Foundation<br />
Steven B. Pearson, MD<br />
Department of Internal Medicine<br />
<strong>Gundersen</strong> <strong>Lutheran</strong> <strong>Health</strong> <strong>System</strong><br />
Todd J. Kowalski, MD<br />
Section of Infectious Disease<br />
<strong>Gundersen</strong> <strong>Lutheran</strong> <strong>Health</strong> <strong>System</strong><br />
Address for correspondence:<br />
Todd J. Kowalski, MD<br />
Mail Stop C02-007<br />
<strong>Gundersen</strong> <strong>Lutheran</strong> <strong>Health</strong> <strong>System</strong><br />
1900 South Avenue<br />
La Crosse, WI 54601<br />
Telephone: (608) 775-6882<br />
Facsimile: (608) 775-5542<br />
email: tjkowals@gundluth.org<br />
W<br />
Intracranial Mycotic Aneurysm Due to<br />
<strong>Streptococcus</strong> <strong>bovis</strong> Endocarditis<br />
AbStrACt<br />
illiam Osler first used the term mycotic aneurysm in his<br />
1885 Gulstonian Lecture series1 to refer to an aneurysm<br />
resulting from an infectious process of the arterial wall, although<br />
a more accurate term might have been endovascular infection or<br />
infective vasculitis, because mycotic aneurysms are not due to<br />
a fungal organism. Intracranial mycotic aneurysms (ICMAs)<br />
complicate about 2% to 3% of infective endocarditis (IE) cases,<br />
although as many as 15% to 29% of patients with IE have<br />
neurologic symptoms. 2-4 Of all intracerebral aneurysms, only 2%<br />
to 6% have an infectious etiology. Signs and symptoms of mycotic<br />
aneurysms may be misleading during the early stages, resulting in<br />
misdiagnosis and delays in treatment. 5 Early diagnosis of ICMA is<br />
the cornerstone of effective treatment.<br />
CASe report<br />
A 63-year-old man had a 2-month history of headaches,<br />
malaise, decreased appetite, night sweats, low-grade intermittent<br />
fevers, and unintentional 10-pound weight loss. His headaches<br />
were spasmodic and intense, and would partially remit with<br />
acetaminophen. He reported no history of trauma, new neurological<br />
deficits, visual changes, sensory or visual aura, radiation to the<br />
neck, or positional variation. He denied use of tobacco, alcohol,<br />
and illicit drugs.<br />
The patient had an extensive medical history, including<br />
a remote history of hemorrhagic stroke, subacute bacterial<br />
endocarditis, sigmoid colon cancer with successful resection, and<br />
ischemic stroke. Post-stroke deficits included moderate weakness<br />
in his left arm and left leg, and moderate vocal cord impairment.<br />
Family history was significant for stomach cancer.<br />
The patient was in no acute distress. His vital signs were:<br />
temperature, 36.6°C; blood pressure, 140/100 mm Hg; respiratory<br />
Mycotic aneurysm usually appears as a painful, pulsatile, and often enlarging mass in a patient<br />
with associated systemic features of infection. This condition is usually fatal without treatment.<br />
We report the case of a patient with infective endocarditis who exhibited neurological signs<br />
and symptoms and was subsequently found to have multiple intracranial mycotic aneurysms.<br />
We also review the recent literature on the diagnosis and treatment of intracranial mycotic<br />
aneurysms.<br />
rate, 18 breaths/min; heart rate, 76 beats/min; and oxygen<br />
saturation, 100% on room air. He had a 2/6 systolic ejection<br />
murmur over the mitral area on cardiac examination. Pulses were<br />
equal bilaterally, and no pedal edema was noted. He had residual<br />
left-sided weakness and decreased sensation in his left arm and<br />
left leg. No meningeal or cerebellar signs were noted, and findings<br />
from examination of the cranial nerve were normal.<br />
Laboratory studies revealed hematuria, an elevated erythrocyte<br />
sedimentation rate (49 mm/hr), and an elevated white blood cell<br />
count (15 400/µL). Computed tomographic (CT) scan of the head<br />
revealed an acute right hemispheric hemorrhagic stroke with right<br />
basil ganglion hemorrhage. Computed tomographic angiography<br />
(CTA) was recommended by neurosurgery to evaluate for vasculitis<br />
or arteriovenous malformation, and revealed multiple cerebral<br />
aneurysms. When compared with old imaging studies, CTA<br />
showed a new, large aneurysm that, based upon its appearance, was<br />
believed to be mycotic. A new, lobulated, irregular aneurysm of the<br />
distal right internal carotid artery, a left internal maxillary artery<br />
aneurysm, and a left external carotid pseudoaneurysm—versus<br />
mycotic aneurysm—were noted. Blood cultures subsequently grew<br />
<strong>Streptococcus</strong> <strong>bovis</strong> in all bottles. Echocardiogram demonstrated<br />
bileaflet mitral valve prolapse with posterior leaflet rupture and<br />
vegetations on the mitral valve consistent with endocarditis.<br />
Neurosurgical consultation was obtained, and nonoperative<br />
management of the aneurysms was recommended due to their<br />
location and number. Thus, with this recommendation and<br />
the infectious nature of the disease, ceftriaxone was initiated.<br />
Unfortunately, the patient developed worsening hemodynamic<br />
parameters, specifically hypotension, and was transferred to the<br />
intensive care unit. Despite vigorous medical management, over the<br />
next several days he experienced 2 grand mal seizures and became<br />
unresponsive. A repeat CT scan of the head demonstrated extensive,<br />
18 <strong>Gundersen</strong> <strong>Lutheran</strong> Medical Journal • Volume 6, Number 1, June 2009
intrACrAniAL MyCotiC AneurySM due to StreptococcuS boviS endoCArditiS<br />
Large lobulated mycotic aneurysm arising from the internal carotid<br />
artery is indicated by the white arrow.<br />
new, right basal ganglia and right frontal lobe intraparenchymal<br />
hemorrhages consistent with rupture of the mycotic aneurysm.<br />
The patient’s family opted for comfort care measures, and the<br />
patient died shortly thereafter. An autopsy was not performed.<br />
diSCuSSion<br />
Mycotic aneurysms can be divided into 4 types: (1) embolic,<br />
secondary to bacterial endocarditis (embolomycotic aneurysms);<br />
(2) extravascular, secondary to extension of contiguous infection<br />
from a septic focus neighboring an artery; (3) cryptogenic or primary<br />
bacteremic; and (4) direct contamination following arterial wall<br />
trauma, which may be postprocedural. 6 Aneurysms can occur in<br />
the cerebral circulation, usually at points of vessel bifurcation, or<br />
in the systemic circulation. 7 In IE-associated mycotic aneurysms,<br />
septic emboli are released from infected cardiac vegetations. These<br />
tiny septic emboli occlude the vasa vasorum or entire arterial lumen,<br />
which leads to damage to the muscular layer of the vessel. ICMA<br />
tend to occur in the more distal portions of the middle cerebral<br />
artery, near the surface of the brain, involving the secondary and<br />
tertiary branches. In contrast, berry aneurysms occur at proximal<br />
branch points in or near the circle of Willis. 4 The outcome depends<br />
upon the anatomical location of the embolus, the causative<br />
bacteria and associated virulence of the organism, underlying host<br />
defenses, and appropriate antibiotic therapy. Mycotic aneurysms<br />
can decrease, increase, remain the same in size, or even disappear<br />
during treatment for endocarditis. 8<br />
Patients with bacterial intracranial aneurysms have<br />
variable neurological symptoms, and early symptoms of<br />
infection may be subtle. In ICMA, patients may have<br />
symptoms ranging from nonspecific, general complaints,<br />
including fever or headache, to neurological deficits or<br />
catastrophic intracranial hemorrhage. Laboratory results are<br />
typically suggestive of an underlying inflammatory process and<br />
may include leukocytosis, elevated erythrocyte sedimentation<br />
rate and/or C-reactive protein concentration, and anemia. Blood<br />
cultures are almost universally positive for microbial growth.<br />
Computed tomographic angiography, magnetic resonance<br />
angiography (MRA), and catheter angiography are used to study<br />
the size, location, and morphology of intracranial aneurysms.<br />
Aneurysms 5 mm in diameter or larger can be detected by CTA and<br />
MRA. Smaller aneurysms are detected less reliably or detected in<br />
retrospect after comparison with cerebral angiography. 9-11 Cerebral<br />
angiography is the gold standard and is often used in preoperative<br />
assessment and in determining prognosis 12 ; however, it is not<br />
routinely recommended due to risk of complications associated<br />
with it. The size of the aneurysm during therapy can be safely and<br />
accurately monitored using CTA and MRA. In our patient, CTA<br />
was selected as the diagnostic tool.<br />
Treatment of ICMA is controversial, in that the appropriate<br />
patients for surgical intervention, need for follow-up imaging,<br />
and most efficacious treatment are not well delineated in the<br />
medical literature. The appropriate treatment always involves<br />
medical and sometimes surgical therapies. 13 Moreover, there is no<br />
single uniformly accepted approach to the treatment of ICMA<br />
in IE. The aim of therapy is to cure the underlying infection<br />
and avoid complications from the aneurysm. Some lesions will<br />
resolve with antibiotic therapy alone. The decision to pursue<br />
surgical management is complex and involves a number of factors,<br />
including the number, site, and anatomy of the aneurysm(s) and<br />
the comorbidities of the patient. Treatment options for unruptured<br />
aneurysms include observation or surgical approaches, such as<br />
craniotomy and clipping or endovascular coiling. 14,15 The surgical<br />
choice of treatment for ICMA is controversial, patient-specific, and<br />
is generally beyond the scope of this article. Four- to 6-week courses<br />
of pathogen-specific intravenous antibiotic are recommended.<br />
In addition, medical therapy should include control of<br />
hypertension and seizures. Therapy should be monitored with<br />
serial CTA or MRA, and surgical intervention is generally<br />
recommended for enlarging aneurysms in accessible locations.<br />
Ruptured aneurysms are treated emergently with surgery to<br />
prevent rebleeding if possible.<br />
Staphylococcus aureus (~30%), Salmonella species (~15%),<br />
and less commonly viridans group streptococci are some of<br />
the causitive organisms of mycotic aneurysms in the<br />
postantibiotic era. 16 Recent reports suggest <strong>Streptococcus</strong><br />
pneumoniae, including penicillin-resistant strains, are re-emerging<br />
as a cause of mycotic aneurysms. 17 Our patient was infected<br />
with <strong>Streptococcus</strong> <strong>bovis</strong>, a gram-positive cocci classified as group<br />
D streptococci. Endocarditis is the most significant clinical<br />
infection associated with S <strong>bovis</strong>, but bacteremia from enteric<br />
origins also occurs. S <strong>bovis</strong> accounts for 2% to 6% of streptococcal<br />
bloodstream isolates from hospitalized patients and for 2.4% to<br />
25% of organisms associated with IE. 18-22 S <strong>bovis</strong> is a rare cause of<br />
ICMA, however. Interestingly, S <strong>bovis</strong> endocarditis or bacteremia<br />
is associated with concomitant undiagnosed gastrointestinal (GI)<br />
tumors in up to 56 % of patients. 23 GI diseases associated with S<br />
<strong>bovis</strong> endocarditis include colonic cancers, gastric ulcers, gastric<br />
<strong>Gundersen</strong> <strong>Lutheran</strong> Medical Journal • Volume 6, Number 1, June 2009 19
cancer, duodenal ulcers, inflammatory bowel disease, colonic<br />
diverticula, angiodysplasia, and liver cirrhosis. 18,24-26 Thus, any<br />
patient with S <strong>bovis</strong> bacteremia should undergo screening for occult<br />
GI malignancy. Although our patient died before such screening<br />
could be completed, he did have a family history of gastric cancer<br />
and a personal history of colon cancer.<br />
ConCLuSion<br />
S <strong>bovis</strong> bacteremia should prompt consideration of IE and<br />
occult GI malignancy. Our patient had multiple ICMAs secondary<br />
to S <strong>bovis</strong>, which ultimately led to his death. This case illustrates<br />
3 key take-home points for clinicians: (1) Subacute bacterial<br />
endocarditis often has vague, nonspecific symptoms that do<br />
not overtly suggest infection, but blood cultures are almost<br />
always diagnostic; (2) If a patient with IE has neurological<br />
complications or symptoms, ICMA should be considered;<br />
and (3) Patients with S <strong>bovis</strong> bacteremia should be screened for<br />
GI malignancy.<br />
referenCeS<br />
1. Osler W. Malignant endocarditis (Gulstonian Lecture I). Lancet. 1885;1:415-418.<br />
2. Chan FY, Crawford ES, Coselli JS, Safi HJ, Williams TW Jr. In situ prosthetic<br />
graft replacement for mycotic aneurysm of the aorta. Ann Thorac Surg. 1989;47(2):<br />
193-203.<br />
3. Bohmfalk GL, Story JL, Wissinger JP, Brown WE Jr. Bacterial intracranial<br />
aneurysm. J Neurosurg. 1978;48(3):369-382.<br />
4. Jones HR Jr, Siekert RG. Neurological manifestations of infective endocarditis.<br />
Review of clinical and therapeutic challenges. Brain. 1989;112(Pt 5):1295-1213.<br />
5. Leo PJ, Pearl J, Tsang W. Mycotic aneurysm: a diagnostic challenge. Am J Emerg<br />
Med. 1996;14(1):70-73.<br />
6. Cloft HJ, Kallmes DF, Jensen ME, Lanzino G, Dion JE. Endovascular treatment<br />
of ruptured, peripheral cerebral aneurysms: parent artery occlusion with short<br />
guglielmi detachable coils. AJNR Am J Neuroradiol. 1999;20(2):308-310.<br />
7. Shaikholeslami R, Tomlinson CW, Teoh KH, Molot MJ, Duke RJ.<br />
Mycotic aneurysm complicating staphylococcal endocarditis. Can J Cardiol.<br />
1999;15(2):217-222.<br />
8. Ziment I. Nervous system complications in bacterial endocarditis. Am J Med.<br />
1969;47(4):593-607.<br />
9. Walsh DW, Ho VB, Haggerty MF. Mycotic aneurysm of the aorta: MRI and MRA<br />
features. J Magn Reson Imaging. 1997;7(2):312-315.<br />
10. Huston J 3rd, Nichols DA, Luetmer PH, et al. Blinded prospective evaluation of<br />
sensitivity of MR angiography to known intracranial aneurysms: importance of<br />
aneurysm size. AJNR Am J Neuroradiol. 1994;15(9):1607-1614.<br />
11. Schwartz RB, Tice HM, Hooten SM, Hsu L, Stieg PE. Evaluation of cerebral<br />
aneurysms with helical CT: correlation with conventional angiography and MR<br />
angiography. Radiology. 1994;192(3):717-722.<br />
12. Benjamin ME, Cohn EJ Jr, Purtill WA, Hanna DJ, Lilly MP, Flinn WR. Arterial<br />
reconstruction with deep leg veins for the treatment of mycotic aneurysms. J Vasc<br />
Surg. 1999;30(6):1004-1015.<br />
13. Johnston SC, Wilson CB, Halbach VV, et al. Endovascular and surgical<br />
treatment of unruptured cerebral aneurysms: comparison of risks. Ann Neurol.<br />
2000;48(1):11-19.<br />
14. Bederson JB, Awad IA, Wiebers DO, et al. Recommendations for the management<br />
of patients with unruptured intracranial aneurysms: a statement for healthcare<br />
professionals from the Stroke Council of the American Heart Association. Stroke.<br />
2000;31(11):2742-2750.<br />
15. Johnston SC, Zhao S, Dudley RA, Berman MF, Gress DR. Treatment of<br />
unruptured cerebral aneurysms in California. Stroke. 2001;32(3):597-605.<br />
16. Brown SL, Busuttil RW, Baker JD, Machleder HI, Moore WS, Barker WF.<br />
Bacteriologic and surgical determinants of survival in patients with mycotic<br />
aneurysms. J Vasc Surg. 1984;1(4):541-547.<br />
17. Brouwer RE, van Bockel JH, van Dissel JT. <strong>Streptococcus</strong> pneumoniae, an emerging<br />
pathogen in mycotic aneurysms? Neth J Med. 1998;52(1):16-21.<br />
18. Ballet M, Gevigney G, Gare JP, Delahaye F, Etienne J, Delahaye JP. Infective<br />
endocarditis due to <strong>Streptococcus</strong> <strong>bovis</strong>. A report of 53 cases. Eur Heart J.<br />
1995;16(12):1975-1980.<br />
19. Murray HW, Roberts RB. <strong>Streptococcus</strong> <strong>bovis</strong> bacteremia and underlying<br />
gastrointestinal disease. Arch Intern Med. 1978;138(7):1097-1099.<br />
20. Selton-Suty C, Hoen B, Delahaye F, et al. Comparison of infective endocarditis<br />
in patients with and without previously recognized heart disease. Am J Cardiol.<br />
1996;77(12):1134-1137.<br />
21. Cabell CH, Jollis JG, Peterson GE, et al. Changing patient characteristics and the<br />
effect on mortality in endocarditis. Arch Intern Med. 2002;162(1):90-94.<br />
22. Roberts RB. Streptococcal endocarditis: the viridans and beta hemolytic<br />
streptococci. In: Kaye D, ed. Infective Endocarditis. 2nd ed. New York: Raven<br />
Press; 1992:191.<br />
23. Hoen B, Briancon S, Delahaye F, et al. Tumors of the colon increase the risk of<br />
developing <strong>Streptococcus</strong> <strong>bovis</strong> endocarditis: case-control study. Clin Infect Dis.<br />
1994;19(2):361-362.<br />
24. Zarkin BA, Lillemoe KD, Cameron JL, Effron PN, Magnuson TH, Pitt HA. The<br />
triad of <strong>Streptococcus</strong> <strong>bovis</strong> bacteremia, colonic pathology, and liver disease. Ann<br />
Surg. 1990;211(6):786-791.<br />
25. Kupferwasser I, Darius H, Muller AM, et al. Clinical and morphological<br />
characteristics in <strong>Streptococcus</strong> <strong>bovis</strong> endocarditis: a comparison with other<br />
causative microorganisms in 177 cases. Heart. 1998;80(3):276-280.<br />
26. Friedrich IA, Wormser GP, Gottfried EB. The association of remote <strong>Streptococcus</strong><br />
<strong>bovis</strong> bacteremia with colonic neoplasia. Am J Gastroenterol. 1982;77(2):82-84.<br />
20 <strong>Gundersen</strong> <strong>Lutheran</strong> Medical Journal • Volume 6, Number 1, June 2009
Authors:<br />
Robert E. Ryan, MA, ATC<br />
Troy E. Ward, MA, ATC<br />
Steven R. Murray, DA<br />
Mesa State College<br />
Grand Junction, Colorado<br />
Mitchell T. Copeland, DO<br />
Western Orthopedics and<br />
Sports Medicine<br />
Grand Junction, Colorado<br />
Brian E. Udermann, PhD, ATC,<br />
FACSM<br />
University of Wisconsin–La Crossse<br />
La Crosse, Wisconsin<br />
Robert W. Pettitt, PhD, ATC<br />
Minnesota State University –Mankato<br />
Mankato, Minnesota<br />
Address for correspondence:<br />
Brian E. Udermann, PhD, ATC,<br />
FACSM<br />
149 Mitchell Hall<br />
1725 State Street<br />
University of Wisconsin–La Crossse<br />
La Crosse, WI 54601<br />
Telephone: (608) 785-8181<br />
email: udermann.bria@uwlax.edu<br />
I<br />
n a d 175, the ancient Greek physician Galen used a<br />
resorbable gut suture—the first recorded use of a<br />
bioabsorbable implant. 1 In the mid 1960s, bioabsorbable<br />
technology was introduced for clinical applications, since which<br />
time its use has increased dramatically. 2 Today some 40 different<br />
bioabsorbable polymers are being used for surgical procedures. 1,3<br />
Advantages have been noted for the use of bioabsorbable<br />
implants in orthopedics. First, they are readily absorbed by the<br />
body, thus reducing the need for surgical revisions and the overall<br />
cost of treatment. 4 Second, they prevent radiographic obscurities<br />
typically found with metallic implants. 4 Third, in that they soften<br />
over time, bioabsorbable implants provide an incremental transfer<br />
of stress to the affected bone, thus providing a load-sharing effect<br />
that enhances healing. 1<br />
While they have notable advantages, bioabsorbable implants<br />
have drawbacks, as well. Compared with their metallic counterparts,<br />
bioabsorbable implants are weaker and less stiff, have limited shelflife,<br />
and are initially more costly. 1 They also can cause exaggerated<br />
inflammatory reactions, such as synovitis, osteolysis, and, more<br />
rarely, giant-cell reactions. 5,6<br />
We report a case of a foreign-body giant-cell reaction to<br />
a bioabsorbable implant. This case exemplifies an iatrogenic<br />
etiology that should be considered when treating patients who are<br />
unresponsive to rehabilitative exercise for surgical repair.<br />
Giant-Cell Reaction to a Bioabsorbable Implant<br />
AbStrACt<br />
A 51-year-old woman had shoulder pain and dysfunction 14 months following the surgical<br />
repair of her supraspinatus muscle via a bioabsorbable implant. Diagnostic testing revealed<br />
a giant-cell reaction at the location of the implant. The patient underwent a second surgery<br />
to burr, irrigate, and fill the lytic lesion that resulted from the giant-cell reaction, and the<br />
supraspinatus muscle was sutured to the greater tuberosity of the humerus. The patient<br />
completed a standard rehabilitation protocol for 8 weeks, and at 6 months she had no further<br />
complications with normal daily activities.<br />
CASe report<br />
A 51-year-old woman had pain in her right shoulder.<br />
Examination of the shoulder revealed an impingement syndrome,<br />
acromioclavicular arthrosis, and a tear in the supraspinatus<br />
muscle. Initial conservative treatment with range-of-motion and<br />
strengthening exercises and subacromial injections of steroids<br />
(ie, 3 mg of betamethasone and 6 mg of 0.25% bupivicaine) was<br />
ineffective. The patient was counseled and scheduled for surgery.<br />
Surgery included a 2-step acromioplasty and an 8-mm resection<br />
of the distal clavicle. The supraspinatus muscle was repaired using<br />
a bioabsorbable implant (Arthrex Bio-Corkscrew), with 4 sutures<br />
placed in a figure-of-8 fashion through the greater tuberosity of<br />
the of the humerus. The patient progressed without complications<br />
for 12 weeks until marked pain returned to the shoulder area.<br />
Conservative treatment, including modest range-of-motion and<br />
strengthening exercises, ensued resulting in a return to normal<br />
daily activities, Fourteen months after surgery, a palpable lesion<br />
deficit was found in the area of the of the implant. Radiographs<br />
revealed a 4- to 6-mm circular lytic lesion consistent with the<br />
site of placement of the bioabsorbable implant in the greater<br />
tuberosity (Figure 1). Given the findings and the patient’s course<br />
postoperatively, she was scheduled for shoulder arthroscopy with<br />
possible supraspinatus muscle repair and placement of a bone graft<br />
in the area of erosion.<br />
<strong>Gundersen</strong> <strong>Lutheran</strong> Medical Journal • Volume 6, Number 1, June 2009 21
figure 1. Radiograph depicting a 4- to 6-mm lytic lesion consistent<br />
with the placement of the bioabsorbable implant.<br />
During the second surgery, no sign of a re-tear of the<br />
supraspinatus muscle was present. Pathological findings suggested<br />
that the lytic lesion was caused by a giant-cell reaction to the<br />
bioabsorbable implant used in the first repair of the supraspinatus<br />
muscle (Figure 2). The lesion was burred, irrigated, and filled<br />
with 0.75 cc of Allomatrix. To avoid any further reaction, the<br />
supraspinatus muscle was sutured using #2 FiberWire through<br />
holes in the greater tuberosity.<br />
Two weeks after surgery the patient had less pain and was<br />
improving with passive range-of-motion exercises. Four weeks<br />
after surgery she was instructed to begin active-assisted exercise.<br />
Eight weeks after surgery, the patient was neurovascularly stable,<br />
had improved range of motion, and had no signs of impingement.<br />
The patient was instructed to continue range-of-motion exercises<br />
for another 4 weeks and at 3 months to begin strengthening<br />
exercises. At 6 months the patient had no further complaints<br />
regarding shoulder discomfort on the right side and returned to<br />
normal daily activities.<br />
diSCuSSion<br />
Our case is an example of an exaggerated inflammatory<br />
reaction to a bioabsorbable implant, stressing the need for both<br />
awareness and precaution when using implants for pain. Our<br />
patient developed a giant-cell reaction to a bioabsorbable screw<br />
that was used as an anchor for the sutures in a supraspinatus<br />
muscle repair. A giant-cell reaction is manifested by individual<br />
macrophages adhering to form a large, multinucleated cell that<br />
engulfs the foreign body. The presence of giant cells interferes<br />
with healing at the surgical site of the implant and can lead to a<br />
breakdown of healthy tissue in the surrounding area. 7 As in our<br />
case, this often necessitates a second surgery to correct the defect.<br />
The initial phase of implant degradation is hydrolysis. As the<br />
implant absorbs water, it begins to degrade. The more porous<br />
the implant, the more quickly it absorbs water. 8 Any remaining<br />
fragments are removed by normal phagocytic response; however,<br />
the rapid degradation of these implants, 4 coupled with excessive<br />
stress being placed on the implant, 9 has been postulated to be the<br />
cause of marked foreign-body reaction, as occurred in our patient.<br />
Various factors, including the metabolic activity of the living cells,<br />
figure 2. Multinucleated giant-cell reaction (hematoxalin and eosin<br />
stain under 25X magnification with partial polarized light showing<br />
biorefringent particulate material).<br />
22 <strong>Gundersen</strong> <strong>Lutheran</strong> Medical Journal • Volume 6, Number 1, June 2009
type of implant, method of sterilization, site of implementation,<br />
and the stress placed on the implant, 1,10 affect the degradation of<br />
biodegradeable implants, often making it difficult to pinpoint<br />
the cause of the an exaggerated inflammatory response. Risk<br />
factors purported to be responsible for adverse tissue responses<br />
are “the presence of quinine dye, an implant with a large surface<br />
area such as a screw, and implant sites with low vascularity.” 11<br />
Our patient had 2 of the aforementioned risk factors: a screw<br />
was employed during the surgery, and repeated physical stress<br />
placed on the anchor-bone interface through the superspinatus<br />
tendon, affirming that these risk factors are potentially valid.<br />
Although bioabsorbable implants are absorbed readily by the<br />
body, thus eliminating the need for a follow-up surgery. They<br />
prevent radiographic obscurities, and they provide incremental<br />
stress transfer as they degrade, which promotes healing. However,<br />
clinicians need to be aware of the drawbacks of bioabsorbable<br />
implants. Compared with metallic implants, they are less strong<br />
and less stiff, have a limited shelf-life, cost more initially, and<br />
have a tendency for an exaggerated inflammatory reaction. The<br />
advantages do, however, appear to outweigh the disadvantages. 10<br />
As shown in the case reported here, the risk of an exaggerated<br />
inflammatory response to bioabsorbable implants increases when<br />
the implant has a large surface area, such as a screw, and when it is<br />
subjected to repeated stress. These risk factors should be considered<br />
in the development of treatment options.<br />
GiAnt CeLL reACtion to A bioAbSorbAbLe iMpLAnt<br />
referenCeS<br />
1. Bollom T, Meister K. Surgical principles: biodegradable materials in sports<br />
medicine. In: DeLee JC, Drez DJ, Miller MD, eds. DeLee & Drez’s Orthopaedic<br />
Sports Medicine: Principles and Practice. 2nd ed. Philadelphia, PA: Saunders;<br />
2003.<br />
2. Kulkarni RK, Pani KC, Neuman C, Leonard F. Polylactic acid for surgical implants.<br />
Arch Surg. 1966;93(5):839-843.<br />
3. Claes LE. Mechanical characterization of biodegradable implants. Clin Mater.<br />
1992;10(1-2):41-46.<br />
4. Ciccone WJ,2nd, Motz C, Bentley C, Tasto JP. Bioabsorbable implants in<br />
orthopaedics: new developments and clinical applications. J Am Acad Orthop Surg.<br />
2001;9(5):280-288.<br />
5. Simon JA, Di Cesare PE, Koval KJ. Bioresorbable materials in orthopaedics. Bull<br />
Hosp Jt Dis. 2000;59(4):232-240.<br />
6. Weiler A, Hoffmann RF, Stahelin AC, Helling HJ, Sudkamp NP. Biodegradable<br />
implants in sports medicine: the biological base. Arthroscopy. 2000;16(3):<br />
305-321.<br />
7. Anderson JM, Rodriguez A, Chang DT. Foreign body reaction to biomaterials.<br />
Semin Immunol. 2008;20(2):86-100.<br />
8. Athanasiou KA, Schmitz JP, Agrawal CM. The effects of porosity on in vitro<br />
degradation of polylactic acid-polyglycolic acid implants used in repair of articular<br />
cartilage. Tissue Eng. 1998;4(1):53-63.<br />
9. Glueck D, Wilson TC, Johnson DL. Extensive osteolysis after rotator cuff repair<br />
with a bioabsorbable suture anchor: a case report. Am J Sports Med. 2005;33(5):<br />
742-744.<br />
10. Ambrose CG, Clanton TO. Bioabsorbable implants: review of clinical experience<br />
in orthopedic surgery. Ann Biomed Eng. 2004;32(1):171-177.<br />
11. Bostman OM, Pihlajamaki HK. Adverse tissue reactions to bioabsorbable fixation<br />
devices. Clin Orthop Relat Res. 2000;(371)(371):216-227.<br />
Graceful John Larson<br />
Optometry<br />
<strong>Gundersen</strong> <strong>Lutheran</strong> Medical Journal • Volume 6, Number 1, June 2009 23
Authors:<br />
Meghana Raghavendra, MB, BS<br />
Department of Medical Education<br />
<strong>Gundersen</strong> <strong>Lutheran</strong> Medical<br />
Foundation<br />
Dr. Raghevendra now practices with<br />
IU Medical Group, Indianapolis,<br />
Indiana<br />
William A. Agger, MD<br />
Section of Infectious Disease<br />
Department of Internal Medicine<br />
<strong>Gundersen</strong> <strong>Lutheran</strong> <strong>Health</strong> <strong>System</strong><br />
Address for correspondence:<br />
William A. Agger, MD<br />
Mail Stop C04-007<br />
<strong>Gundersen</strong> <strong>Lutheran</strong> <strong>Health</strong> <strong>System</strong><br />
1900 South Avenue<br />
La Crosse, WI 54601<br />
Telephone: (608) 775-2140<br />
Facsimile: (608) 775-5542<br />
email: waagger@gundluth.org<br />
Post–Cesarean Delivery Septic Ovarian Vein<br />
Thrombosis<br />
AbStrACt<br />
CASe<br />
A 32-year-old pregnant woman at 40 weeks gestation<br />
underwent a cesarean delivery due to failure to advance after<br />
prolonged rupture of membranes followed by chorioamnionitis.<br />
She was discharged 3 days after delivery but required readmission<br />
8 days later for fever, left lower abdominal pain, and fullness in her<br />
left lower abdomen. Her white blood cell count was 22.9 x 10 9 /L<br />
with 24% bands, and her erythrocyte sedimentation rate was<br />
96 mm/h. Urinalysis results were within normal limits. Cultures of<br />
blood drawn on admission remained negative for growth.<br />
Transvaginal ultrasonography revealed a mixed echogenic<br />
mass in the left adnexal area measuring 5.0 x 7.0 x 5.0 cm that<br />
appeared to be a mixture of small abscesses and phlegmon. Despite<br />
48 hours of intravenous treatment with a broad-spectrum antibiotic<br />
(ertapenam), she continued to have fevers as high as 39°C.<br />
A computed tomographic (CT) scan of abdomen and pelvis with<br />
contrast was obtained and revealed left ovarian vein thrombosis<br />
and a complex tubo-ovarian abscess (Figures 1 and 2). Enoxaparin<br />
was begun, and fever resolution occurred within 24 hours. The<br />
patient was discharged home on oral amoxicillin/clavulanate and<br />
warfarin. Her oral anticoagulation was stopped at 5 days due to<br />
uterine bleeding, and she has remained well for the last 6 months.<br />
diSCuSSion<br />
Postpartum ovarian vein thrombosis (OVT) occurs after<br />
0.003% to 0.18% of deliveries, 1,2 after 0.005% of febrile abortions, 3<br />
and occasionally after other inflammatory pelvic pathologies.<br />
Many consider OVT to be an extension of a more controversial<br />
diagnosis, pelvic thrombophlebitis. 2,4,5 OVT should be considered<br />
in women who have lower abdominal pain, lower quadrant mass,<br />
fever, and/or neutrophilia after childbirth or after pelvic surgery. 1,6<br />
Postpartum women with OVT usually develop fever within 48 to<br />
Eleven days after cesarean delivery, a 32-year-old woman was readmitted to hospital<br />
with fever and pain in her lower left abdomen. Her white blood cell count and<br />
erythrocyte sedimentation rate were elevated. Transvaginal ultrasonography revealed<br />
a mixed echogenic mass in the left adnexal area that appeared to be a mixture of<br />
small abscesses and phlegmon. She was started on an intravenous broad-spectrum<br />
antibiotic, but 48 hours later, her fever persisted. A computed tomographic scan<br />
of abdomen and pelvis with contrast was obtained and revealed left ovarian vein<br />
thrombosis and a complex tubo-ovarian abscess. Enoxaparin was begun, and the<br />
patient’s fever resolved within 24 hours. Postpartum pelvic infection with ovarian<br />
thrombosis and its therapy are reviewed.<br />
96 hours after delivery. 1,6 Lower abdominal pain and/or a cord-like,<br />
tender, lower abdominal fullness may be found in 50% to 67%<br />
of patients. 1,6 Nausea, ileus, and other gastrointestinal complaints<br />
may also occur. The differential diagnosis includes appendicitis,<br />
pyelonephritis, tubo-ovarian abscess, and endometritis with or<br />
without retained products of conception.<br />
figure 1. Computed tomographic scan with contrast illustrating left<br />
ovarian vein thrombus (white arrow).<br />
24 <strong>Gundersen</strong> <strong>Lutheran</strong> Medical Journal • Volume 6, Number 1, June 2009
figure 2. Computed tomographic scan with contrast illustrating<br />
complex tubo-ovarian abscess (white arrow).<br />
While our patient had left-sided OVT, a right-sided<br />
predominance has been reported, probably attributable to the<br />
immediate postpartum retrograde flow of venous blood down<br />
the left ovarian vein, through the pelvis, and up the right ovarian<br />
vein. 6,7 With thrombosis, the clotted vein can be imaged along the<br />
psoas muscle to the vena cava on the right or left renal vein, as in<br />
our case. The clot may extend into the vena cava, and pulmonary<br />
embolus may ensue. Imaging studies reveal sensitivities of 100%,<br />
92%, and 50% for CT scans, magnetic resonance imaging scans,<br />
and ultrasonograms, respectively. 8<br />
Blood cultures usually remain negative for pathogens, with<br />
positive cultures seen in only about 3% of patients.1 The bacteria<br />
most commonly associated with OVT reflect the vaginal origin of<br />
these infections: enteric gram-negative rods, including Escherichia<br />
coli, Enterobacter and Klebsiella species, along with microaerophilic<br />
streptococci, and anaerobic bacteria such as Peptostreptococcus,<br />
Bacteroides, and Prevotella species. 1,3 Antimicrobial treatment of<br />
OVT should be directed against these gastrointestinal/genitourinary<br />
facultative and anaerobic flora.<br />
A genetic hypercoaguable state in has been found in 50%<br />
of women with OVT. 9 Our patient had no family history of<br />
thromboembolic disease, thus genetic causes for a hypercoagulable<br />
state were not evaluated. Literature approximately 40 years ago<br />
indicated that anticoagulation had replaced the surgical ligation of<br />
the vena cava or ovarian veins to prevent pulmonary emboli. 3<br />
More recent literature has shown that resolution of fever and<br />
length of hospitalization were not significantly different in women<br />
treated with antibiotics alone versus those treated with antibiotics<br />
and anticoagulation, probably due to a spectrum bias of earlier<br />
detection and, therefore, milder cases. 10<br />
poSt–CeSAreAn deLiVery SeptiC oVAriAn Vein throMboSiS<br />
Despite these recent reports, a short course of anticoagulation<br />
is often given due to concerns of vena cava thrombosis or<br />
pulmonary emboli seen in approximately 13% of OVT, 6 although<br />
the type and duration of anticoagulation for OVT remains<br />
controversial. 7,11,12 Until better evidence is available, the authors<br />
believe anticoagulation should be considered until the patient is<br />
ambulating and asymptomatic, and for 3 to 6 months in cases<br />
complicated by pulmonary emboli. If warfarin is given to a woman<br />
who breast feeds, Vitamin K supplement and coagulation testing<br />
of her infant is considered prudent.<br />
referenCeS<br />
1. Brown TK, Munsick RA. Puerperal ovarian vein thrombophlebitis: a syndrome.<br />
Am J Obstet Gynecol. 1971;109(2):263-273.<br />
2. Dunnihoo DR, Gallaspy JW, Wise RB, Otterson WN. Postpartum ovarian vein<br />
thrombophlebitis: a review. Obstet Gynecol Surv. 1991;46(7):415-427.<br />
3. Josey WE, Staggers SR,Jr. Heparin therapy in septic pelvic thrombophlebitis: a<br />
study of 46 cases. Am J Obstet Gynecol. 1974;120(2):228-233.<br />
4. Garcia J, Aboujaoude R, Apuzzio J, Alvarez JR. Septic pelvic thrombophlebitis:<br />
diagnosis and management. Infect Dis Obstet Gynecol. doi:10.1155/<br />
IDOG/2006/15614.<br />
5. Witlin AG, Mercer BM, Sibai BM. Septic pelvic thrombophlebitis or refractory<br />
postpartum fever of undetermined etiology. J Matern Fetal Med. 1996;5(6):<br />
355-358.<br />
6. Munsick RA, Gillanders LA. A review of the syndrome of puerperal ovarian vein<br />
thrombophlebitis. Obstet Gynecol Surv. 1981;36(2):57-66.<br />
7. Kominiarek MA, Hibbard JU. Postpartum ovarian vein thrombosis: an update.<br />
Obstet Gynecol Surv. 2006;61(5):337-342.<br />
8. Twickler DM, Setiawan AT, Evans RS, et al. Imaging of puerperal septic<br />
thrombophlebitis: prospective comparison of MR imaging, CT, and sonography.<br />
AJR Am J Roentgenol. 1997;169(4):1039-1043.<br />
9. Salomon O, Apter S, Shaham D, et al. Risk factors associated with postpartum<br />
ovarian vein thrombosis. Thromb Haemost. 1999;82(3):1015-1019.<br />
10. Brown CE, Stettler RW, Twickler D, Cunningham FG. Puerperal septic pelvic<br />
thrombophlebitis: incidence and response to heparin therapy. Am J Obstet<br />
Gynecol. 1999;181(1):143-148.<br />
11. Beigi RH, Wiensenfeld HC. Enoxaparin for postpartum ovarian vein thrombosis.<br />
A case report. J Reprod Med. 2004;49(1):55-57.<br />
12. Ortin X, Ugarriza A, Espax RM, et al. Postpartum ovarian vein thrombosis.<br />
Thromb Haemost. 2005;93(5):1004-1005.<br />
<strong>Gundersen</strong> <strong>Lutheran</strong> Medical Journal • Volume 6, Number 1, June 2009 25
Authors:<br />
Ines H. Berger, MD, PhD<br />
Department of Pain Medicine<br />
<strong>Gundersen</strong> <strong>Lutheran</strong> <strong>Health</strong> <strong>System</strong><br />
Douglas R. Bacon, MD, MA<br />
Department of Anesthesiology<br />
Mayo Clinic Foundation<br />
Rochester, Minnesota<br />
Address for correspondence:<br />
Ines H. Berger, MD, PhD<br />
Mail Stop EB3-001<br />
<strong>Gundersen</strong> <strong>Lutheran</strong> <strong>Health</strong> <strong>System</strong><br />
1900 South Avenue<br />
La Crosse, WI 54601<br />
Telephone: (608) 775-9000<br />
Facsimile: (608) 775-1018<br />
email: ihberger@gundluth.org<br />
A<br />
Historical Notes on Amputation and Phantom<br />
Limb Pain: “All Quiet on the Western Front?”<br />
AbStrACt<br />
mputations have been performed since antiquity for<br />
punitive, therapeutic, and ritualistic purposes. 1 Hippocrates<br />
practiced amputation of gangrenous limbs, preferring transection<br />
through the gangrenous portion because it was less painful. Celsus,<br />
in contrast, stressed the necessity to sever between the healthy and<br />
the diseased body part. Since the 16th century, especially in France<br />
and in Germany, barber surgeons have attempted to perfect the<br />
techniques of amputation. Until the advent of adequate general<br />
and regional anesthesia techniques, an amputation was probably<br />
the most challenging operation a surgeon could perform. Although<br />
opium had been known for a long time, it did not find its use<br />
in amputations. With the lack of perioperative analgesia, the<br />
operation had to be short. It took an experienced barber surgeon<br />
3 to 4 minutes to amputate a leg and was performed as a circular<br />
cut—a single cut for skin, muscles, bone and tendon (Figure 1). A<br />
limb amputation was associated with an extremely high morbidity<br />
and mortality (50%-80%) prior to the introduction of antisepsis<br />
in the late 19th century.<br />
The invention of cannon balls and gunpowder worsened<br />
the injuries sustained in battle. Many famous surgeons, such<br />
as Ambroise Paré (Figure 2) and Baron Larrey, who reportedly<br />
amputated 200 limbs in a day, 2 have been associated with battle<br />
surgery. Important progress was made with the introduction of<br />
vessel ligature. Previously, hemostasis had to be achieved by<br />
immersing the stump in substances such as hot oil or vitriol, or<br />
cauterizing with a hot iron. Ambroise Paré described an arterial<br />
forceps for the use of vessel ligation in 1590, thereby significantly<br />
reducing blood loss. 3<br />
Amputations in the 16th and 17th centuries were primarily<br />
accomplished in a single cut through the soft tissue, thereby<br />
necessitating an assistant holding the limb. This was consequently<br />
modified into 2- and 3-stage circular cuts to reduce the tension<br />
on sutures. Lowdham (1679), Verduyn (1696), and Langenbeck<br />
(1810) changed the operative technique with the creation of a<br />
soft tissue flap to cover the stump without tension. Despite these<br />
advances, mortality was high and amputation remained the best<br />
option possible. William Keen, an American Civil War surgeon,<br />
The first detailed description of phantom limb pain is credited to the French barber surgeon<br />
Ambroise Paré (ad 1552) in his tract on “harquebusses and other guns.” He differentiated<br />
phantom limb pain from stump pain and phantom sensations. Paré speculated on peripheral<br />
and central nervous system involvement, as well as psychological factors in the algogenesis of<br />
this pain. Although classically described as occurring after limb amputation, the sensation can<br />
occur after a spinal cord injury, nerve avulsion, mastectomy, or removal or deafferentation of<br />
many other organs or body parts. Almost 450 years later, the incidence of phantom limb pain<br />
has remained high (up to 80% in some studies). Paré’s observation and theories are still the<br />
basis of our current treatment strategies, including aggressive postoperative analgesia, nerve<br />
blocks, centrally acting medications, physiotherapy and behavioral/psychological interventions.<br />
figure 1. Plate illustrating amputation at the thigh. Courtesy of the<br />
National Library of Medicine.<br />
wrote: “The popular opinion that the surgeons did a large amount<br />
of unnecessary amputating may have been justified in a few cases,<br />
but, taking the army as a whole, I have no hesitation in saying<br />
that far more lives were lost from refusal to amputate than by<br />
26 <strong>Gundersen</strong> <strong>Lutheran</strong> Medical Journal • Volume 6, Number 1, June 2009
amputation.” 4 Given that a lot of these procedures were performed<br />
in fields or stables, it comes as no surprise to find gangrene, sepsis,<br />
hemorrhage, and tetanus as constantly dreaded complications<br />
associated with these operations. 4,5<br />
Postamputation pain<br />
Along with the lack of pain control during the amputation,<br />
the phenomenon of postamputation pain has been recognized<br />
for many centuries. Admiral Lord Nelson lost his right arm at an<br />
attack on Santa Cruz de Tenerife. 6 Not only was the amputation<br />
in itself quite challenging, but imagine the difficulty of performing<br />
this under a most compromised situation, namely, on a moving<br />
battleship, with little space, in the semi-darkness of the ship’s<br />
interior. Admiral Nelson, who barely survived hypothermia and<br />
considerable blood loss, found himself in tremendous pain after he<br />
survived the amputation of his arm—in the amputated arm! He<br />
found the emergence of painful phantom sensations to be proof of<br />
the existence of the soul, given that an extremity that was no longer<br />
there could hurt so much. Fortunately, a second operation, which<br />
likely relieved an inadvertently placed suture on the median nerve,<br />
relieved most of his pain and restored him to function. However,<br />
through the ages, a significant percentage of amputees could not<br />
be delivered from their torturous pain. 7,8<br />
S. Weir Mitchell, who is considered the Father of American<br />
Neurology, wrote a short story, “The Case of George Dedlow,”<br />
in 1886. 9 The central character, George Dedlow, progressively<br />
loses all 4 extremities and is befallen by phantom limb pain: “I<br />
was suddenly aware of a sharp cramp in my leg. I tried to get at it<br />
to rub it with my single arm, but finding myself too weak, hailed<br />
an attendant: ‘Just rub my left calf,’ said I, ‘if you please.’ ‘Calf?’<br />
said he. ‘You ain’t none, pardner. It’s took off.’ ‘I know better,’ said<br />
I. ‘I have pain in both legs.’ ‘Wall, I never!’ said he. ‘You ain’t got<br />
nary leg.’” In this story, George Dedlow becomes the symbol for<br />
the cost of the Civil War, which left 500 000 soldiers disfigured,<br />
disabled, and in chronic pain. 10<br />
Erich Maria Remarque described in his classic novel All Quiet on<br />
the Western Front the sufferings endured by the generation involved<br />
in the atrocities of trench warfare in World War I. 11 Standing at<br />
the bedside of his severely injured friend, Franz Kemmerich,<br />
Albert Kropp asks, “How goes it Franz?” “Not so bad…but I have<br />
such a damned pain in my foot.” The leg has been amputated.<br />
With more than one meaning, Kropp commends, “Now you will<br />
soon be going home.” During the next visit, Franz is dying from<br />
complications of the amputation. He gives his “good army boots”<br />
to his friend Müller, also giving hope to go on fighting not only a<br />
war, but also the adversities in life.<br />
Ambroise Paré (1510-1590) described phantom pain in<br />
a surprisingly comprehensive fashion. 12 He differentiated<br />
preamputation pain from postamputation symptoms, and stump<br />
pain from phantom sensations and phantom limb pain. Paré<br />
recognized a psychological component in pain perception, as well<br />
as pain-alleviating and pain-modulating modalities.<br />
Paré’s tract was geared toward his surgical colleagues who were<br />
familiar with the challenges of treating postamputation pain.<br />
Paré rejected the use of multiple limb-shortening procedures for<br />
persistent pain and advocated for early amputation of necrotic<br />
limbs and nonsurgical treatment of phantom pain as a combination<br />
hiStoriCAL noteS on AMputAtion And phAntoM LiMb pAin<br />
figure 2. Ambroise Paré (1510-1590), French barber surgeon<br />
credited with the first detailed description of phantom limb pain.<br />
Courtesy of the National Library of Medicine.<br />
of massage therapy for the stump and neck and the use of an<br />
antispasmodic ointment. Paré used 2 neurological models to<br />
explain phantom sensation/pain: (1) A peripheral model focused<br />
on contractures of muscles, nerves, and tendons; contractures<br />
postinjury were commonplace in his era and, therefore, widely<br />
recognized; and (2) A central nervous system model that identified<br />
“pain memory” as the cause of pain without contractures.<br />
Silas Weir Mitchell, a 19th-century neurologist, is credited<br />
with coining the term phantom limb and the first concise description<br />
of the phantom pain phenomena, 13-15 though Charles Bell, a<br />
British physician, had also described phantom limb sensations in<br />
1830 in his monograph The Nervous <strong>System</strong> of the Human Body. 16,17<br />
Guéniot 18 described in an 1861 tract About Hallucination of<br />
Feeling in Certain Amputees, the phenomenon of regressive<br />
deformation, also known as telescoping. Telescoping refers to<br />
the process of shrinking of the phantom sensation as the digits<br />
become approximated to the stump, a phenomenon that seems<br />
more likely to occur in the arm than in the leg. It is a gradual<br />
process that occurs in 25% to 75% of amputees and is usually<br />
complete after the first year. Pain, recurrent trauma, and other<br />
similar events can reverse this process.<br />
Since these original descriptions, phantom limb phenomena<br />
have also been described with multiple other organ extirpations,<br />
such as the tongue, penis, testicle, breast, bladder, gallbladder, and<br />
teeth, as well as with spinal cord and nerve avulsion injuries. Bors<br />
described in 1951 phantom pain associated with spinal cord injury<br />
<strong>Gundersen</strong> <strong>Lutheran</strong> Medical Journal • Volume 6, Number 1, June 2009 27
and nerve root avulsion. Simmel, in 1956, described phantom<br />
phenomena associated with thalamic lesions. Despite the<br />
many discoveries and blessings of modern-day medicine, the<br />
incidence of phantom limb pain has remained high, with<br />
estimates varying widely up to 79%. 19 Wartan describes an<br />
incidence of 55% in British war veterans after 50 years. 8 The<br />
pain from preamputation to postamputation state remains<br />
strikingly similar in quality and location, 19 and preamputation<br />
and acute pain are the best predictors of persistent chronic<br />
pain after the amputation. 20<br />
Although phantom limb pain has been recognized for<br />
several centuries, some people do not accept the phenomenon<br />
and believe the pain is imagined. Those who experience<br />
phantom pain and/or sensations make the point that their<br />
experience is real and that the missing or deafferented body<br />
part is the phantom. “Even 50 years after loosing my leg in<br />
World War II, the burning still comes. I don’t talk about it<br />
much: the doctor told me that it was all in my head. I just…<br />
try to get through the pain.” 7<br />
How do we understand and treat phantom limb<br />
pain today?<br />
Saints Cosmas and Damian, the twin physicians, are<br />
credited with the first attempt to cure phantom limb pain by<br />
transplantation of a new limb. This heroic attempt failed even<br />
in these “holy hands” and probably contributed to the fact<br />
that the physicians were also known as the “silver-less ones.”<br />
However, the fact that even saint physicians could not heal<br />
this deafferentation pain state illustrates the challenge that we<br />
encounter to this day: phantom limb pain continues to be<br />
exceedingly difficult to treat.<br />
The assumption of a psychogenic origin of this type of<br />
pain has not been supported in the recent literature. 21<br />
The aggravating effects of stress, anxiety, exhaustion, and<br />
depression on chronic pain, however, are well accepted. 22<br />
Peripheral mechanisms have been implicated in modulating<br />
phantom sensations via alterations in blood flow and stump<br />
manipulations. Spinal mechanisms are recognized<br />
in disinhibition of the dorsal horn neurons, thereby<br />
facilitating transmission of phantom pain. 23 Melzack<br />
proposed a central origin of phantom pain with the<br />
concept of a neuromatrix, with a somatosensory memory<br />
of the pain experienced. 24 The topographic representation<br />
of the body in the thalamus and cerebral cortex can be<br />
significantly altered by amputation. Thalamic mapping has<br />
supported the hypothesis that the thalamic representation<br />
of the limb or organ remains functional or even increases<br />
after amputation. Thalamic microstimulation of this area<br />
has been shown to reproduce phantom pain. 25 Somatotopic<br />
mapping using magnetoencephalography has revealed<br />
significant reorganization in cortical topography following<br />
deafferentation. 26 Recently, linking of cortical topography<br />
with perceptual experiences has also received tremendous<br />
impetus. 27 Harris recently hypothesized that disorganized or<br />
inappropriate cortical representation of proprioception may<br />
falsely signal incongruence between motor intention and<br />
movement, which results in pathological pain. 28<br />
Meticulous care of the amputation stump and wellfitted<br />
prosthesis are the prerequisites to stump and pain<br />
management. 22 In addition to traditional opioids and<br />
nonsteroidal antiinflammatories, antidepressants, and<br />
anticonvulsants, highly invasive techniques, such as deep brain<br />
stimulation and primary motor cortex stimulation, have added<br />
to the arsenal of possible treatment options. 29-31 Preemptive<br />
analgesia methods aim to minimize or prevent central<br />
neuroplastic changes from occurring in response to tissue<br />
injury and pain. Effective multimodal perioperative analgesia<br />
techniques, including regional anesthesia, nonsteroidal antiinflammatory<br />
drugs, local anesthetics, α 2 agonists, ketamine,<br />
α 2 δ ligands, and opioids have been successfully implemented<br />
to improve pain control in phantom pain. 32-35<br />
The functional relationship between cortical and<br />
subcortical reorganization and phantom limb pain suggests<br />
that neuromodulatory treatments aimed at modifying<br />
cortical reorganization and restoring the integrity of cortical<br />
information processing offer intriguing possibilities in treating<br />
the devastating symptoms of chronic pain after suffering the<br />
loss of bodily integrity. Ironically, after countless suggestions<br />
that amputees’ phantom limb pain is “all in their head,” it<br />
might truly be—albeit not in the original sense of the phrase.<br />
We need to shift our conceptualization of chronic pain away<br />
from Descartes’ notion of pain pathways that can be severed<br />
to treat pain 36 toward that of a complex neuromodulatory<br />
process that integrates physiological as well as psychological<br />
components. Doing so will affect not only our approach to<br />
the patient suffering from phantom pain, but also open a<br />
new dimension to our understanding and treatment of other<br />
neuropathic and centralized pain states.<br />
Paré’s observations led him to propose peripheral, spinal,<br />
and central mechanisms as causes for phantom limb pain.<br />
Today we are using the same peripheral, spinal, and central<br />
targets for our treatment strategies.<br />
After almost 450 years, there is new hope for relief from<br />
a syndrome that Paré described so well, even with the limited<br />
methodology of his time. We shall take the “good boots” of<br />
comrade Kemperich to accelerate our knowledge and give<br />
hope to those who suffer from unrelenting pain, knowing that<br />
Saints Cosmas and Damian, the patron saints of healers, are<br />
still a step ahead of us.<br />
referenCeS<br />
1. Magee R. Amputation through the ages: the oldest major surgical operation.<br />
Aust N Z J Surg. 1998;68(9):675-678.<br />
2. Larrey DJ. Mémoires De Chirurgie Militaire Et Campagnes. Paris: J Smith;<br />
1812:Vol IV, 57.<br />
3. Paré A. Les Oeuvres d’Ambroise Paré, Conseiller Et Premier Chirurgien Du<br />
Roy. Divisées En Vingt-Huit Livres, Avec Les Figures Et Portraits, Tant De<br />
l’Anatomie, Que Des Instruments De Chirurgie, & De Plusieurs Montres.<br />
Revues & Augmentées Par l’Auteur. Quatrième ed. FR; Paris: G. Buon;<br />
1585:387-388.<br />
4. Keen WW. Surgical reminiscences of the Civil War. Transactions and Studies<br />
of the College of Physicians of Philadelphia, Third Series. 1905;27:95-114.<br />
28 <strong>Gundersen</strong> <strong>Lutheran</strong> Medical Journal • Volume 6, Number 1, June 2009
5. Sachs M, Bojunga J, Encke A. Historical evolution of limb amputation. World J<br />
Surg. 1999;23(10):1088-1093.<br />
6. Rüttimann B. Nelsons Oberarm-Amputation. Z Orthop Ihre Grenzgeb.<br />
1982;120(1):86-88.<br />
7. Machin P, de C Williams AC. Stiff upper lip: coping strategies of World War II<br />
veterans with phantom limb pain. Clin J Pain. 1998;14(4):290-294.<br />
8. Wartan SW, Hamann W, Wedley JR, McColl I. Phantom pain and sensation<br />
among British veteran amputees. Br J Anaesth. 1997;78(6):652-659.<br />
9. Mitchell SW. The Autobiography of a Quack: And, the Case of George Dedlow. New<br />
York: The Century Co.; 1900:115-149.<br />
10. Figg L, Farrell-Beck J. Amputation in the Civil War: physical and social<br />
dimensions. J Hist Med Allied Sci. 1993;48(4):454-475.<br />
11. Remarque EM. All Quiet on the Western Front. Boston: Little, Brown, and<br />
Company; 1983.<br />
12. Keil G. Sogenannte Erstbeschreibung des Phantomschmerzes von Ambroise<br />
Paré. Fortschr Med. 1990;108(4):62-66.<br />
13. Nathanson M. Phantom limbs as reported by S. Weir Mitchell. Neurology.<br />
1988;38(3):504-505.<br />
14. Mitchell SW. Phantom limbs. Lippincott’s Magazine of Popular Literature &<br />
Science. 1871;8:563-569.<br />
15. Mitchell SW. Neural maladies of stumps. In: Mitchell SW, ed. Injuries<br />
of Nerves and Their Consequences. Philadelphia: J.B. Lippincott; 1872:<br />
342-368.<br />
16. Furukawa T. Charles Bell’s description of the phantom phenomenon in 1830.<br />
Neurology. 1990;40(12):1830.<br />
17. Bell C. The Nervous <strong>System</strong> of the Human Body: Embracing the Papers Delivered<br />
to the Royal Society on the Subject of the Nerves. London: Longman, Rees, Orme,<br />
Brown, and Green; 1830:238, clxxvi.<br />
18. Guéniot M. D’une hallucination du toucher (ou hétéroptopie subjective des<br />
extrémités) particulière à certains amputés. Journal de la Physiologie de l’Homme<br />
et des Animaux. 1861;4:416-430.<br />
19. Katz J, Melzack R. Pain ‘memories’ in phantom limbs: review and clinical<br />
observations. Pain. 1990;43(3):319-336.<br />
20. Hanley MA, Jensen MP, Smith DG, Ehde DM, Edwards WT, Robinson LR.<br />
Preamputation pain and acute pain predict chronic pain after lower extremity<br />
amputation. J Pain. 2007;8(2):102-109.<br />
21. Sherman RA, Sherman CJ, Bruno GM. Psychological factors influencing<br />
chronic phantom limb pain: an analysis of the literature. Pain. 1987;28<br />
(3):285-295.<br />
hiStoriCAL noteS on AMputAtion And phAntoM LiMb pAin<br />
22. Sherman RA, Sherman CJ, Gall NG. A survey of current phantom limb pain<br />
treatment in the United States. Pain. 1980;8(1):85-99.<br />
23. Mackenzie N. Phantom limb pain during spinal anaesthesia. Recurrence in<br />
amputees. Anaesthesia. 1983;38(9):886-887.<br />
24. Melzack R. Phantom limbs and the concept of a neuromatrix. Trends Neurosci.<br />
1990;13(3):88-92.<br />
25. Davis KD, Kiss ZH, Luo L, Tasker RR, Lozano AM, Dostrovsky JO. Phantom<br />
sensations generated by thalamic microstimulation. Nature. 1998;391(6665):385-<br />
387.<br />
26. Birbaumer N, Lutzenberger W, Montoya P, et al. Effects of regional anesthesia on<br />
phantom limb pain are mirrored in changes in cortical reorganization. J Neurosci.<br />
1997;17(14):5503-5508.<br />
27. Ramachandran VS, Rogers-Ramachandran D. Phantom limbs and neural<br />
plasticity. Arch Neurol. 2000;57(3):317-320.<br />
28. Harris AJ. Cortical origin of pathological pain. Lancet. 1999;354(9188):<br />
1464-1466.<br />
29. Owen SL, Green AL, Nandi DD, Bittar RG, Wang S, Aziz TZ. Deep<br />
brain stimulation for neuropathic pain. Acta Neurochir Suppl. 2007;97<br />
(Pt 2):111-116.<br />
30. Saitoh Y, Yoshimine T. Stimulation of primary motor cortex for intractable<br />
deafferentation pain. Acta Neurochir Suppl. 2007;97(Pt 2):51-56.<br />
31. Wesolowski JA, Lema MJ. Phantom limb pain. Reg Anesth. 1993;18<br />
(2):121-127.<br />
32. Pinzur MS, Garla PG, Pluth T, Vrbos L. Continuous postoperative infusion of<br />
a regional anesthetic after an amputation of the lower extremity. A randomized<br />
clinical trial. J Bone Joint Surg Am. 1996;78(10):1501-1505.<br />
33. Madabhushi L, Reuben SS, Steinberg RB, Adesioye J. The efficacy of<br />
postoperative perineural infusion of bupivacaine and clonidine after lower<br />
extremity amputation in preventing phantom limb and stump pain. J Clin<br />
Anesth. 2007;19(3):226-229.<br />
34. Bach S, Noreng MF, Tjellden NU. Phantom limb pain in amputees during the<br />
first 12 months following limb amputation, after preoperative lumbar epidural<br />
blockade. Pain. 1988;33(3):297-301.<br />
35. Reuben SS, Buvanendran A. Preventing the development of chronic pain after<br />
orthopaedic surgery with preventive multimodal analgesic techniques. J Bone<br />
Joint Surg Am. 2007;89(6):1343-1358.<br />
36. Benini A, DeLeo JA. Rene Descartes’ physiology of pain. Spine. 1999;24(20):<br />
2115-2119.<br />
<strong>Gundersen</strong> <strong>Lutheran</strong> Medical Journal • Volume 6, Number 1, June 2009 29
Authors:<br />
Brian E. Udermann, PhD, ATC,<br />
FACSM<br />
John P. Porcari, PhD, RCEP<br />
Carl C. Foster, PhD<br />
Department of Exercise and<br />
Sport Science<br />
University of Wisconsin–La Crossse<br />
Address for correspondence:<br />
Brian E. Udermann, PhD, ATC,<br />
FACSM<br />
149 Mitchell Hall<br />
1725 State Street<br />
University of Wisconsin–La Crossse<br />
La Crosse, WI 54601<br />
Telephone: (608) 785-8181<br />
Facsimilie: (608) 785-8172<br />
email: udermann.bria@ulax.edu<br />
The La Crosse Exercise and <strong>Health</strong> Program (LEHP) has<br />
been serving the Seven Rivers Region since 1971. Since<br />
its inception, the program has gone through a number of name<br />
changes. In 1971 the program was known as the La Crosse Cardiac<br />
Rehabilitation Program. In 1976 the name was changed to the<br />
La Crosse Exercise Program, and in 1985 the current program<br />
name (LEHP) was adopted. To avoid confusion, LEHP will<br />
be used throughout this article. Also, in 1971 the Wisconsin<br />
State University of La Crosse underwent a name change to the<br />
University of Wisconsin–La Crossse (UW–L); we will use UW–L<br />
when referring to the university.<br />
The idea of using physical activity to help prevent and treat<br />
illness and disease dates back to nearly 500 b c. 1 Isolated reports<br />
document that some physicians were recommending physical<br />
activity for individuals with heart ailments in the 16th and 17th<br />
centuries, 2,3 but it wasn’t until the 1940s and 1950s that physicians<br />
and researchers started critically analyzing the standard treatment<br />
of coronary patients (eg, bed rest) and began investigating the role<br />
that prescribed physical activity could play in the rehabilitative<br />
process. 4,5 The amount of research and scientific inquiry on<br />
the topic continued to expand through the 1960s, resulting in<br />
unprecedented growth in the area of cardiac rehabilitation. 6-11<br />
In 1970, due in part to a greater acceptance of using exercise<br />
to help treat cardiac patients, a task force was formed in La Crosse<br />
to investigate the feasibility of creating an exercise program for<br />
cardiac patients. Two additional factors precipitated the creation<br />
of this task force. First, UW–L faculty wanted to focus more on<br />
laboratory-based exercise physiology (see Figure 1 for an early<br />
photograph taken in the Human Performance Laboratory at<br />
UW–L). Second, physicians in the Department of Cardiology at<br />
<strong>Lutheran</strong> Hospital were interested in offering expanded services.<br />
The task force consisted of Dr Allen Brailey (cardiologist<br />
and president of the La Crosse County Medical Society),<br />
Mr Jack Forbes (field representative, Wisconsin Heart Association),<br />
Dr Robert Green (cardiologist and consulting physician, La Crosse<br />
County Heart Unit), Dr Robert McMahon (internist and former<br />
director of health services at UW–L), and Dr Philip Wilson<br />
The History of Cardiac Rehabilitation at the<br />
University of Wisconsin–La Crossse<br />
figure 1. Exercise test in the UW–L Human Performance Laboratory.<br />
(associate professor in the College of <strong>Health</strong>, Physical Education,<br />
and Recreation at UW–L). 12 As the task force began the work<br />
of investigating the feasibility of creating a cardiac rehabilitation<br />
program at UW–L, it soon became apparent that the political<br />
climate within the medical community in the area would present a<br />
significant challenge to the idea. La Crosse was home to 2 competing<br />
hospitals: <strong>Lutheran</strong> Hospital, supported by <strong>Gundersen</strong> Clinic; and<br />
St. Francis Hospital, supported by Skemp Grandview Clinic and<br />
La Crosse Clinics. 12 The rivalry between these 2 healthcare facilities<br />
threatened to jeopardize the creation of a collaborative cardiac<br />
rehabilitation program. Dr Robert McMahon, who at different<br />
points in his career was employed by <strong>Gundersen</strong> Clinic, Skemp<br />
Clinic, and UW–L, was instrumental in facilitating discussion and<br />
developing rapport among representatives from the 3 institutions.<br />
As the task force was nearing the completion of its work, it<br />
was decided that 2 representatives (Drs McMahon and Wilson)<br />
30 <strong>Gundersen</strong> <strong>Lutheran</strong> Medical Journal • Volume 6, Number 1, June 2009
the hiStory of CArdiAC rehAbiLitAtion At the uniVerSity of WiSConSin–LA CroSSSe<br />
would visit a number of existing cardiac rehabilitation programs<br />
around the country. The pair traveled to and observed programs<br />
at San Diego State College, the University of San Francisco, the<br />
University of Wisconsin–Madison, and the Cleveland Jewish<br />
Community Center. Shortly after the visits, the task force<br />
drafted a policies and procedures document for the LEHP. In the<br />
spring of 1971, an LEHP executive board was created and held<br />
its first meeting. The board consisted of Drs Robert Batchelder,<br />
Donovan Riley, and Philip Wilson (UW–L); Drs Allen Brailey,<br />
Robert Green, Robert McMahon, and Edward Winga (<strong>Gundersen</strong><br />
Clinic); Dr Charles Link (Skemp Clinic); and Cal Jahn (consumer<br />
representative). The executive board was responsible for developing<br />
and monitoring the policies and procedures of the LEHP.<br />
Even though the LEHP was incorporated as an operational body<br />
of UW–L, the creation of the program truly was a collaborative<br />
effort between the University, the Wisconsin Heart Association,<br />
the La Crosse County Medical Society, and La Crosse <strong>Lutheran</strong><br />
and St. Francis hospitals. The initial cost of LEHP was shared<br />
across institutions, and it was agreed that the program would be<br />
offered for a 1-year pilot period and then evaluated for possible<br />
continuance.<br />
On June 6, 1971, the first exercise session of the newly created<br />
LEHP was offered. Six cardiac rehabilitation patients completed<br />
an exercise class under the supervision of exercise physiologists and<br />
physicians. Program personnel made a strong effort to promote<br />
and market the LEHP, and after the first year the enrollment had<br />
grown from 6 to 31 participants. Area physicians appeared to be<br />
supportive of the program as well, with 14 physicians volunteering<br />
to help supervise LEHP activities.<br />
Over the next few years the program continued to grow in<br />
enrollment, and new policies and procedures were developed.<br />
Program personnel sought grants from the Grandview Foundation,<br />
the National Institutes of <strong>Health</strong>, the Wisconsin Heart Association,<br />
and the United Fund to help offset program costs, and a new cardiac<br />
rehabilitation internship program was created. It was decided<br />
that all cardiac rehabilitation participants would receive a graded<br />
exercise stress test prior to admittance into the program, and again<br />
after 3 and 6 months of participation. It was also decided that<br />
LEHP participants would be divided into cardiac-prone (1 or more<br />
cardiovascular risk factors) and advanced cardiac (known disease)<br />
groups and would exercise on different days of the week.<br />
In 1974, the American College of Cardiology selected UW-L<br />
(with support from <strong>Gundersen</strong> Clinic) as a training center for<br />
physicians interested in cardiac rehabilitation and exercise testing.<br />
It was also about this time that the LEHP sponsored a cardiac<br />
exercise technician workshop. Since the early 1970s, the LEHP has<br />
sponsored and conducted hundreds of educational programs on<br />
topics including cardiac rehabilitation, electrocardiogram (ECG)<br />
interpretation, weight management, industrial fitness, pulmonary<br />
rehabilitation, and exercise testing. One of the more successful<br />
workshops, a sports sciences symposium, was offered in 1984 and<br />
brought more than 600 medical personnel from the United States<br />
and around the world to La Crosse. It is estimated that over the<br />
past 35 years, over 10 000 participants, from all 50 states and 43<br />
countries, have attended LEHP workshops and symposia.<br />
In the fall of 1975 the LEHP began publishing Cardio-Gram,<br />
a bi-monthly newspaper that contained articles of interest to both<br />
LEHP participants and medical personnel working in the field of<br />
cardiac rehabilitation. Over the next few years the paper became<br />
more popular and grew to a circulation of over 3500 subscribers.<br />
In the early 1980s, LEHP staff secured a sponsorship for Cardio-<br />
Gram through Pfizer Laboratories (New York), which resulted in the<br />
paper being circulated to roughly 25 000 healthcare professionals.<br />
The paper was eventually replaced by a program newsletter. The<br />
Sun Rise Express, The Beat Goes On, and The Pacesetter are all titles<br />
the newsletter has had over the past 25 years. The program still<br />
publishes a popular monthly newsletter, The La Crosse Exercise and<br />
<strong>Health</strong> Program Newsletter.<br />
The mid 1970s was also a time when LEHP staff began<br />
offering educational programming to participants. Topics<br />
included nutrition, benefits of exercise, behavior modification,<br />
and risk factors for cardiovascular disease. Offering educational<br />
opportunities to both participants and community members<br />
has been a hallmark of the program for the past 30 years. Some<br />
current examples include 10-minute tidbits—short educational<br />
programs presented to participants every 2 weeks—and the LEHP<br />
<strong>Health</strong> Lecture Series, a new series of talks that will be offered<br />
every February to help recognize the American Heart Association’s<br />
Heart <strong>Health</strong> Month.<br />
Throughout the early and mid 1970s, the LEHP offered exercise<br />
programming for individuals in need of cardiac rehabilitation.<br />
However, in January of 1977, the program expanded services to<br />
nonclinical populations and created an adult fitness unit. The<br />
adult fitness unit was to serve apparently healthy individuals with<br />
the goal of helping participants prevent disease and maintain or<br />
increase fitness levels. Also in 1977, the Board of Regents of the<br />
University of Wisconsin <strong>System</strong> approved a master’s degree in<br />
Adult Fitness and Cardiac Rehabilitation at UW–L. This was an<br />
exciting time for the university because this was the first program<br />
of its kind in the country, and because until this program was<br />
approved, the only UW system school that offered medically<br />
related degree programs was UW–Madison. A number of other<br />
colleges and universities adopted the university-based cardiac<br />
rehabilitation model created at UW–L. In 2004, the Adult Fitness<br />
and Cardiac Rehabilitation Program was renamed and is now<br />
the Clinical Exercise Physiology program. In the past 30 years,<br />
roughly 500 students have graduated from this program and are<br />
employed in cardiac and pulmonary rehabilitation programs in<br />
nearly every state in the country, as well as a number of countries<br />
around the world.<br />
Over the years, LEHP staff has employed a variety of incentivebased<br />
initiatives to help motivate participants. One of the first,<br />
implemented in 1977, was a program in which participants who<br />
attended 3 exercise sessions a week for 6 months were rewarded<br />
with a t-shirt. The LEHP still uses a variety of incentive programs<br />
to help motivate participants to achieve their health- and fitnessrelated<br />
goals. Longtime LEHP member Don Kirby recently posed<br />
for a photograph wearing a 1000 Mile Club shirt he received in the<br />
late 1970s (Figure 2).<br />
In the early to mid 1980s, the LEHP continued to expand the<br />
services offered to the community. A collaborative diabetic services<br />
program was created and implemented with cooperation from<br />
the <strong>Gundersen</strong> and Skemp-Grandview clinics. The program also<br />
began offering services related to pulmonary rehabilitation and<br />
<strong>Gundersen</strong> <strong>Lutheran</strong> Medical Journal • Volume 6, Number 1, June 2009 31
figure 2. Longtime LEHP member Don Kirby wearing an incentive<br />
t-shirt he received in the late 1970s.<br />
continued to expand its health promotion (eg, stress management,<br />
weight management, nutritional counceling, tobacco cessation)<br />
and exercise (eg, low-impact aerobics) programming. In addition,<br />
a program called Nutri Exercise was developed by Jean Storlie,<br />
MS, RD, and offered to area residents.<br />
Phil Wilson, the first executive director of the LEHP retired<br />
in July of 1987. Drs Patricia Hutchenson and Sandra Price each<br />
served as interim executive directors of the LEHP until 1989,<br />
when Dr John Porcari was appointed to the position.<br />
The leadership and staff of the LEHP have been influential in<br />
advancing the disciplines of cardiac and pulmonary rehabilitation.<br />
The American Association of Cardiovascular and Pulmonary<br />
Rehabilitation was formed in 1985, and since that time, 7 of<br />
the individuals who have served as president of that organization<br />
have worked with the LEHP: Philip Wilson, Linda Hall, Martha<br />
Livingston, Mark Williams, Jeanne Ruff, John Porcari, and Karen<br />
Lui, and 3 of these have received its Award of Excellence: Wilson,<br />
Hall, and Williams.<br />
Changes in the last decade have focused mainly on<br />
programmatic offerings. Research documenting the benefits of<br />
resistance training has resulted in approximately 75% of program<br />
participants participating in some sort of strength training, either in<br />
the weight room or in chair weight classes. A very popular offering<br />
is the nightly Rockin’ Rehab low-impact aerobic dance class.<br />
These classes were originally part of student Elaine Gotro’s 1998<br />
master’s project, and they continue to thrive. In fact, they became<br />
so popular that an instructional video tape and DVD have been<br />
produced and are available for participants to purchase. A fairly<br />
recent addition to the program has been stability ball and balance<br />
classes. As individuals get older and recognize the importance of<br />
strength, balance, and flexibility to maintain their independence,<br />
these classes are also increasing in popularity. Enrollment in the<br />
program has been stable over the past 5 to 10 years and is currently<br />
at 262 members—188 adult fitness members and 74 cardiac<br />
rehabilitation members.<br />
Another change to the program is that physicians no longer<br />
supervise the afternoon exercise sessions. The availability of an<br />
automated external defibrillator (AED) and the fact that all staff<br />
are certified in Advanced Cardiac Life Support (ACLS) has resulted<br />
in a change in philosophy regarding program supervision.<br />
Despite the fact that physicians no longer directly supervise<br />
the afternoon exercise sessions, the LEHP continues to work very<br />
closely with both area medical facilities. Students in the Clinical<br />
Exercise Physiology graduate program complete an equal number<br />
of rotations through the Phase I and II cardiac rehabilitation<br />
programs at each facility and rotate through the graded exercise<br />
testing laboratories at each hospital clinic. Physicians routinely<br />
give lectures to students on various topics related to cardiology<br />
and cardiac rehabilitation. The LEHP has a contract with each<br />
facility to provide a half-time exercise physiologist to work in their<br />
exercise physiology departments and to serve as a link between<br />
the University and their respective programs. The University and<br />
the hospitals jointly sponsor the previously mentioned continuing<br />
education workshops in cardiac and pulmonary rehabilitation that<br />
are attended by people from all over the world.<br />
referenCeS<br />
1. Balke B. Historical viewpoints: exercise and health. J Cardiopulm Rehabil.<br />
1990;10:447-454.<br />
2. Heberden W. Some account of a disorder of the breast. Medical Transactions.<br />
1772;2:59-67.<br />
3. Stokes W. The Diseases of the Heart and the Aorta. Dublin: Hodges & Smith; 1854.<br />
4. Harrison TR. Abuse of rest as a therapeutic measure for patients with cardiovascular<br />
disease. JAMA. 1944;125:1075-1077.<br />
5. Levine SA, Lown B. “Armchair” treatment of acute coronary thrombosis. JAMA.<br />
1952;148(16):1365-1369.<br />
6. Cain HD, Frasher WG, Jr., Stivelman R. Graded activity program for safe return<br />
to self-care after myocardial infarction. JAMA. 1961;177:111-115.<br />
7. Naughton J, Balke B, Nagle F. Refinements in method of evaluation and physical<br />
conditioning before and after myocardial infarction. Am J Cardiol. 1964;14:<br />
837-843.<br />
8. Torkelson LO. Rehabilitation of the patient with acute myocardial infarction.<br />
J Chronic Dis. 1964;17(8):685-704.<br />
9. Gottheiner V. Long-range strenuous sports training for cardiac reconditioning and<br />
rehabilitation. Am J Cardiol. 1968;22(3):426-435.<br />
10. Hellerstein HK. Techniques of exercise prescription and evaluation. J S C Med<br />
Assoc. 1969;65(12):46-56.<br />
11. Wenger NK, Gilbert CA, Siegel W. Symposium: The use of physical activity<br />
in the rehabilitation of patients after myocardial infarction. South Med J.<br />
1970;63(8):891-897.<br />
12. Vik CE. Twenty-year History of the La Crosse Exercise and <strong>Health</strong> Program,<br />
1971-1991. [MS]. University of Wisconsin–La Crossse; 1993.<br />
32 <strong>Gundersen</strong> <strong>Lutheran</strong> Medical Journal • Volume 6, Number 1, June 2009
CALL FOR PAPERS<br />
M E D I C A L J O U R N A L<br />
<strong>Gundersen</strong> <strong>Lutheran</strong> Medical Journal (GLMJ) is an interdisciplinary archival journal. To this end, manuscripts<br />
considered for publication are sought from any medical or surgical specialty or subspecialty, or any healthrelated<br />
field. Manuscripts may be based upon, but are not limited to, (1) original, data-driven, high quality,<br />
randomized or nonrandomized, controlled trials; (2) systematic reviews or meta-analyses; (3) clinical<br />
outcome studies; (4) tutorials; (5) case reports; (6) historical reports; and (7) letters to the editor. The Journal<br />
will also consider “vignette” or “how I do it” papers, pieces designed to provide the readership with “pearls,”<br />
rationale, and/or techniques for a given procedure or examination. They may be based upon research, upon<br />
clinical experience, or both. Interesting imaging studies accompanied by a brief descriptive or explanatory<br />
text would be appropriate, as well.<br />
The submission deadline for the next issue is September 15, 2009.<br />
Please prepare manuscripts in accordance with the most recent version of “Uniform Requirements for<br />
Manuscripts Submitted to Biomedical Journals” (www.icmje.org). Assistance in preparing your manuscript is<br />
available through the Journal office (see below).<br />
Submit an electronic version as an attachment via email to glmjeditor@gundluth.org or on 3.5” floppy or<br />
CD, along with any nondigital original figures to:<br />
Cathy Mikkelson Fischer, MA, Managing Editor<br />
<strong>Gundersen</strong> <strong>Lutheran</strong> Medical Journal<br />
<strong>Gundersen</strong> <strong>Lutheran</strong> Medical Foundation<br />
C03-006B<br />
1836 South Avenue<br />
La Crosse, Wisconsin 54601<br />
QUESTIONS?<br />
Please contact:<br />
David E. Hartman, PhD, BC-ANCDS(A), Editor<br />
Cathy Mikkelson Fischer, MA, Managing Editor<br />
<strong>Gundersen</strong> <strong>Lutheran</strong> Medical Journal<br />
<strong>Gundersen</strong> <strong>Lutheran</strong> Medical Foundation<br />
C03-006B<br />
1836 South Avenue<br />
La Crosse, Wisconsin 54601<br />
(608) 775-6648<br />
(800) 362-9567, ext. 56648<br />
Call for papers?<br />
<strong>Gundersen</strong> <strong>Lutheran</strong> Medical Journal is a peer-reviewed<br />
journal published by <strong>Gundersen</strong> <strong>Lutheran</strong> Medical<br />
Foundation. The Journal is available online at<br />
www.gundluth.org/journal.
Summer Splendor Kelly Hodgson Kline<br />
Pediatrics<br />
34 <strong>Gundersen</strong> <strong>Lutheran</strong> Medical Journal • Volume 6, Number 1, June 2009
<strong>Gundersen</strong> <strong>Lutheran</strong> Medical Journal<br />
1836 South Avenue • La Crosse, Wisconsin<br />
(608) 775-6648 or (800) 362-9567, ext. 56648 • www.gundluth.org/journal<br />
Nonprofit<br />
Organization<br />
U.S. Postage<br />
PAID<br />
La Crosse, WI<br />
Permit No. 119<br />
3 <strong>Gundersen</strong> <strong>Lutheran</strong> Medical Journal • Volume 6, Number 1, June 2009