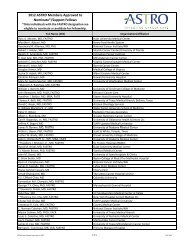
Anal and Rectal Cancers - ASTRO
Anal and Rectal Cancers - ASTRO
Anal and Rectal Cancers - ASTRO
- TAGS
- anal
- rectal
- cancers
- astro
- www.astro.org
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
<strong>Anal</strong> <strong>and</strong> <strong>Rectal</strong> <strong>Cancers</strong>:<br />
Anatomy, Contouring <strong>and</strong><br />
Considerations for IMRT<br />
Planning<br />
Karyn y A. Goodman, , MD<br />
Associate Attending Radiation Oncologist<br />
Memorial Sloan Sloan-Kettering Kettering Cancer Center
� None<br />
Disclosures
Learning Objectives<br />
Objectives<br />
• Describe the challenges <strong>and</strong> outcomes in IMRT for<br />
the lower GI sites (anal <strong>and</strong> rectal cancers)<br />
• Discuss the role of IMRT planning <strong>and</strong> routine imageguidance<br />
g for lower GI cancers<br />
• List the challenges associated with management of<br />
g g<br />
motion <strong>and</strong> deformation in treating lower GI cancers
Outline<br />
• Pelvic Anatomy <strong>and</strong> Nodal Drainage Patterns<br />
• Contouring <strong>and</strong> planning recommendations<br />
for IMRT in the treatment of <strong>Anal</strong> Cancer<br />
• IMRT in <strong>Rectal</strong> Cancer<br />
• IGRT <strong>and</strong> motion issues in the treatment of<br />
pelvic tumors
Anatomy of the Rectum <strong>and</strong> Anus<br />
Mesorectal fat<br />
Peritoneal Reflection<br />
12-15 cm
Anatomy<br />
Mesorectal Fascia Mesorectal Fascia<br />
• T2 axial images<br />
• Mesorectal fascial involvement associated with higher risk of<br />
positive circumferential resection margin
Nodal Drainage Patterns
Nodal Anatomy<br />
Superior Hemorrhoidal Vessels Mesorectal Nodes<br />
Courtesy of Corinne Winston, MD
Nodal Anatomy<br />
External Iliac Nodes Inguinal Nodes Great Saphenous Vein<br />
Internal Iliac Nodes<br />
Courtesy of Corinne Winston, MD
Nodal Anatomy
Nodal Anatomy
Outline<br />
• Pelvic Anatomy <strong>and</strong> Nodal Drainage Patterns<br />
• Contouring <strong>and</strong> planning recommendations<br />
for IMRT in the treatment of <strong>Anal</strong> Cancer<br />
• IMRT in <strong>Rectal</strong> Cancer<br />
• IGRT <strong>and</strong> motion issues in the treatment of<br />
pelvic tumors
644 <strong>Anal</strong><br />
SCC Patients<br />
5-Year Rates<br />
Disease Disease-free free Survival<br />
Local Relapse<br />
Colostomy<br />
Distant Mets.<br />
Overall Survival<br />
RTOG 98 98-11 11<br />
RT + MMC/5-FU<br />
Cis/5-FU<br />
RT + Cis/5-FU<br />
C/F�RT C/F�RT+C/F C/F RT RT+MMC/F MMC/F<br />
(%)<br />
(%)<br />
p<br />
Ajani JA et al., JAMA 2008;299:1941-1921
RTOG 9811<br />
Relapse l bby<br />
TN Category<br />
TN<br />
No. Local Local-Regional Regional Distant Metastasis<br />
C Category t<br />
Pt Pts TF(#) 5yr(%) TF(#) 5yr(%)<br />
T2N0 302 50 19 31 12<br />
T3N0 115 25 22 12 14<br />
T4N0 31 13 50 5 21<br />
T2N1 T2N1-3 95 37 40 22 31<br />
T3N1 T3N1-3 47 27 58 12 32<br />
T4N1 T4N1-3 25 14 64 4 17<br />
Gunderson LL et al., <strong>ASTRO</strong> 2010
• AP/PA – RTOG<br />
RT Technique<br />
– 30 30.6 6 to t pelvis l i<br />
– 45 Gy to true pelvis (drop superior<br />
border to SI joints)<br />
– 54 - 59 59.4 4 Gy to GTV + 22-3 3cm cm<br />
margin for T3+ disease
<strong>Anal</strong> Cancer:<br />
NCCN GGuidelines id li VVersion i 22.2012 2012<br />
RT Guidelines:<br />
45 Gy for T1/T2, T1/T2<br />
9-14 Gy boost for T3/T4<br />
Field reduction after<br />
30.6 Gy (bottom of sacroiliacal<br />
joints)<br />
36 Gy y( (N0-inguinal g nodes) )<br />
IMRT may be used in the treatment<br />
IMRT may be used in the treatment<br />
of patients with anal cancer
180 patients<br />
45 locoregional persistence or failure<br />
28 local-only 7 local <strong>and</strong> regional 10 regional only
Local Recurrences in Relation to<br />
Conventional Pelvic Fields<br />
n=2<br />
n=25 n=25<br />
Posterior Posterior-anterior anterior field Lateral field<br />
n=2
RTOG 0529: Dose Painted IMRT in<br />
<strong>Anal</strong> Cancer (Kachnic et al )<br />
<strong>Anal</strong> Cancer (Kachnic, et al.)<br />
Mitomycin-C 10 mg/m² IV bolus on<br />
days 1 & 29 IMRT<br />
5-FU 1000 mg/m²/day by CI on<br />
days y 1-4 & 29-32 IMRT<br />
T2 <strong>and</strong> above<br />
*HIV pts eligible DP-IMRT<br />
T2N0: 50.4 Gyy tumor; ; 42 Gyy elective<br />
nodes in 28 fxs over 5.5 weeks<br />
T3N0 or T4N0: 54 Gy tumor; 45 Gy<br />
elective e ect e nodes odes in 30 fxss over o e 6<br />
weeks<br />
N+: 50.4 Gy < 3 cm or 54 Gy > 3 cm<br />
<strong>ASTRO</strong> 2009, 2009 2010<br />
in 30 fxs over 6 weeks
Study Endpoints<br />
� Primary: Reduce combined grade 2+ GI/GU toxicities by<br />
15%, as compared to 98-11 5FU/MMC arm (n=59 pts)<br />
� Secondary: all AEs vs. 98-11<br />
� Secondary: feasibility (< 5 cases with major deviations)<br />
� Secondary: two year outcomes
CTV A includes:<br />
• MMesorectallnodes d<br />
– Perirectal<br />
– “Presacral”<br />
• Internal iliac nodes<br />
CTV B includes:<br />
• External iliac nodes<br />
CTV C includes:<br />
• Inguinal nodes<br />
RTOG guidelines guidelines<br />
Myerson RJ RJ, Kachnic LA LA, IJROBP IJROBP, 2009 2009.
RTOG 0529: IMRT vs. RTOG 9811<br />
0529<br />
(n=52)<br />
9811-MMC-arm<br />
(n=324)<br />
Acute Morbidity # y<br />
% %<br />
≥ Grade 3 GI/GU AE 22* 36*<br />
≥ Grade 3 skin AE 20* 47*<br />
Endpoint& 2y-% 2y-%<br />
Local-Regional Failure 20 23<br />
Colostomy Failure 8 10<br />
Overall Survival 88 91<br />
Disease-Free Survival 77 71<br />
Colostomy-Free Survival 86 84<br />
Distant Failure 15 10<br />
# Kachnic Kachnic L et al al., <strong>ASTRO</strong> 2009; & Kachnic L et al al., <strong>ASTRO</strong> 2010
Ng M, Int J Radiat Oncol Biol Phys, 2012
Ng M, Int J Radiat Oncol Biol Phys, 2012
Ng M, Int J Radiat Oncol Biol Phys, 2012
Contouring Guidelines<br />
Ng M, M Int J Radiat Oncol Biol Phys Phys, 2012
IMRT plan for <strong>Anal</strong> Cancer
Comparison of APPA v. IMRT Fields<br />
AP/PA (left) <strong>and</strong> IMRT (right). Inguinal nodes highlighted in pink, PTV in red. Isodose lines: 5400 cGy blue, 5250 cGy yellow,<br />
5000 cGy cyan, 4725 cGy green, 4500 cGy magenta, 4275 cGy orange, 2500 cGy pink.
IMRT for <strong>Anal</strong> Cancer<br />
• 17 patients treated with definitive CMT<br />
• 9 field IMRT plans<br />
• Compared to AP/PA plans in 7 patients<br />
• IMRT reduced mean <strong>and</strong> threshold doses to<br />
small bowel bowel, bladder, bladder genitalia<br />
• 3/17 patients failed � APR<br />
• MMedian di f/ f/u 20 20.3 3 months th<br />
• 2 yr OS, DFS, CFS: 91%, 65%, 82%<br />
Milano, IJROBP, 2005
Milano, IJROBP, 2005
Multicenter Experience<br />
• 53 patients <strong>Anal</strong> SCC SCC, 3 academic centers<br />
• Definitive chemoradiation (5-FU-based<br />
chemo)<br />
• Median f/u = 14.5 mos<br />
• 18 month OS, CFS, freedom from LF: 93%,<br />
84%, 84%<br />
Salama, J Clin Oncol, 2007
Multicenter Experience<br />
• 42% had a treatment break<br />
– median of 4 days<br />
• 15% had acute grade 3 GI toxicity<br />
– 34% Grade 3-4 toxicity on RTOG 98-11<br />
Salama, J Clin Oncol, 2007
Potential Limitations of IMRT<br />
• Highly conformal fields with steep dose fall off<br />
may underdose nodal regions at risk<br />
• Potential for higher regional failure rates<br />
• Cautionary report from McGill<br />
– 66 pts treated for anal SCC (40-3DCRT, 26 IMRT)<br />
– Increased Grade 3+ BM toxicity in IMRT grp (42% v<br />
17.5%)<br />
– 1 yr LR rate: 28.6% (IMRT) v. 15.2% (3DCRT)<br />
VVuong, PProc ASCO, ASCO 2008
Propensity Score <strong>Anal</strong>ysis<br />
• 223 <strong>Anal</strong> SCC patients treated from 1991-2010<br />
• 45 – IMRT, 178 – conventional RT<br />
• Median follow-up: 5 yrs (6.1 yrs - CRT, 2.3 yrs - IMRT)<br />
• Patients treated with IMRT had significantly higher N<br />
stage <strong>and</strong> were less likely to receive induction chemo<br />
3-year<br />
Outcomes<br />
IMRT<br />
(%)<br />
Conventional RT<br />
(%)<br />
P value<br />
LRFS 87 79 .20 20<br />
DMFS 86 88 .62<br />
CFS 96 89 .10 10<br />
OS 89 86 .91<br />
DasGupta, Submitted, 2012
Simulation Set-up Set up<br />
CT Simulation<br />
– Prone (or supine)<br />
– Aquaplast / Vac-loc Bag (or equivalent)<br />
– Full Bladder<br />
– IV Contrast + SB contrast<br />
– <strong>Anal</strong> Marker Marker; Wire around aro nd Distal Extent E tent of Disease; Disease<br />
Vaginal Marker<br />
– PET-CT simulation if available or fuse diagnostic g<br />
PET
Outline<br />
• Pelvic Anatomy <strong>and</strong> Nodal Drainage Patterns<br />
• Contouring <strong>and</strong> planning recommendations<br />
for IMRT in the treatment of <strong>Anal</strong> Cancer<br />
• IMRT in <strong>Rectal</strong> Cancer<br />
• IGRT <strong>and</strong> motion issues in the treatment of<br />
pelvic tumors
Preoperative 5FU<br />
+5040cGy pelvic RT<br />
German <strong>Rectal</strong> Cancer Study<br />
Locally Advanced<br />
<strong>Rectal</strong> Cancer<br />
Surgery<br />
Surgery Postoperative 5FU<br />
+5580 cGy pelvic RT<br />
Sauer Sauer, NEJM 2004
St<strong>and</strong>ard Pelvic Fields for <strong>Rectal</strong> Cancer
Dosimetric Benefit of IMRT for <strong>Rectal</strong><br />
Cancer<br />
• MMultiple lti l ddosimetric i t i studies t di hhave compared d<br />
conventional fields (bony anatomy), 3DCRT,<br />
33-field fi ld sIMRT, IMRT multi-field lti fi ld IMRT planning l i<br />
• Target coverage <strong>and</strong> bowel volume<br />
irradiated better for all plans compared to<br />
conventional Urbano M, IJROBP, 2006<br />
Callister M, Proc <strong>ASTRO</strong>, 2006<br />
Guerrero Urbano MT, IJROBP 2006<br />
Arbea L, Radiat Oncol, 2010<br />
Tho LM LM, IJROBP. IJROBP 2006
RTOG 0822 Phase II <strong>Rectal</strong> IMRT Trial<br />
cT3-4NxM0 or cTxN1-2M0<br />
Preop for planned<br />
resection<br />
Radiation<br />
capecitabine<br />
it bi<br />
+ oxaliplatin<br />
Pelvic IMRT: 45 Gy in 25 fx<br />
3D-CRT boost: 5.4 Gy in 3 fx to total dose of<br />
50.4 Gy in 28 fx<br />
+<br />
Adjuvant<br />
Chemo<br />
FOLFOX<br />
Surgery<br />
LAR or or APR<br />
APR
<strong>Rectal</strong> Cancer – Target Definition<br />
• GTV: Primary y tumor + involved nodes<br />
– As defined on physical exam, ERUS, MRI, CT, <strong>and</strong>/or<br />
PET<br />
– Include tumor +entire rectal circumference at that<br />
level<br />
• CTV: Elective nodal regions<br />
– St<strong>and</strong>ard: Peri-rectal, internal iliac, <strong>and</strong> superior<br />
hemorrhoidal (CTVA)<br />
– For T4 tumors extending anteriorly: include external<br />
iliac (CTVA + B)<br />
– For tumors invading anal canal: include inguinal <strong>and</strong><br />
external iliac (CTVA+B+C)<br />
Myerson RJ, Kachnic LA, IJROBP, 2009.
RTOG 0822<br />
• Primary endpoint: Comparison of Grade 2+ GI<br />
toxicity i i to RTOG 0247 ( (non-IMRT) IMRT)<br />
• 68 analyzable patients<br />
• 90% T3, 55% N+<br />
• 51% Grade 2+ GI toxicity compared to 58% on<br />
RTOG 0247 (NS)<br />
• Only 5 (7%) had unacceptable CTV<br />
Garafalo MM, <strong>ASTRO</strong> 2011
IMRT v. CRT<br />
• 92 rectal cancer pts<br />
treated from 2004-2009<br />
• 61 – CRT CRT, 31 – IMRT<br />
• 45/50.4 Gy for CRT<br />
• 45/50 Gy for IMRT using<br />
an integrated boost<br />
Samuelian JM JM, IJROBP IJROBP, 2012
Grade 2+<br />
GI toxicity t i it<br />
Grade 2+<br />
Diarrhea<br />
Grade 2+<br />
enteritis<br />
IMRT CRT P<br />
(%) (%) value<br />
48 62 .006<br />
23 30 .62<br />
10 38 .10<br />
pCR 19 28 NS<br />
IMRT v. CRT<br />
Samuelian JM, IJROBP, 2012
Indications for IMRT for <strong>Rectal</strong> Cancer<br />
• Low <strong>Rectal</strong> Tumors or T4 tumors<br />
– Invading anal sphincter, cover inguinal nodes<br />
– AAnterior t i T4 extension, t i cover external t l ili iliac nodes d<br />
• Post-operative chemoradiation<br />
– Minimize bowel dose since bowel falls into<br />
pelvis<br />
• Recurrent colon cancer in the pelvis
Indications for IMRT for <strong>Rectal</strong> Cancer
<strong>Rectal</strong> Cancer - Radiation Techniques<br />
CT Simulation<br />
– Supine (thin) or Prone<br />
– Belly Board / Bowel Compression if Prone<br />
– AAquaplast l t/ / VVac-loc l B Bag ( (or equivalent) i l t)<br />
– Full Bladder<br />
– Oral (SB Follow Through) +/- IV Contrast<br />
– <strong>Anal</strong> marker; consider vaginal marker<br />
– ≤ 3mm Slice Thickness<br />
– Use Multiple Fields<br />
– Consider IMRT for Select Cases (nodal burden, small bowel<br />
issues)
Outline<br />
• Pelvic Anatomy <strong>and</strong> Nodal Drainage Patterns<br />
• Contouring <strong>and</strong> planning recommendations<br />
for IMRT in the treatment of <strong>Anal</strong> Cancer<br />
• IMRT in <strong>Rectal</strong> Cancer<br />
• IGRT <strong>and</strong> motion issues in the treatment of<br />
pelvic tumors
IGRT <strong>and</strong> Motion Issues<br />
• Improvements in pelvic imaging<br />
– EUS, CT, MRI, PET<br />
• <strong>Rectal</strong> Motion<br />
– Day-to-day variation in rectal filling
<strong>Rectal</strong> Protocol CT
<strong>Rectal</strong> MRI<br />
Mercury Study group, British Medical Journal, 2006
<strong>Rectal</strong> MRI<br />
• Studies have validated use of MRI to:<br />
– measure depth of extramural spread accurately<br />
– Predict circumferential resection margin (CRM)<br />
positivity iti it when h ttumor iis ≤ 1 mm from f mesorectal t l<br />
fascia on MRI<br />
– Assess tumor <strong>and</strong> nodal response to pre- pre<br />
operative chemoradiation<br />
• Good correlation with pathology p gy<br />
measurements in resection specimens<br />
Brown G, Radiology, 1999; Beets-Tan R; Lancet, 2001; Mercury Study group, Radiology, 2007;<br />
Mercury Study group, British Medical Journal, 2006.
MRI to Risk Stratify <strong>Rectal</strong> Cancer
Impact on Management<br />
Tumor abuts mesorectal fascia T4 Bladder invasion
MRI as a Biomarker<br />
• Regression of tumor microvasculature is an<br />
early surrogate marker for treatment response<br />
• New MRI techniques can assess these changes<br />
non-invasively<br />
– DDynamic i CContrast-Enhanced t t E h d IImaging i (DCE)<br />
– Diffusion-Weighted Imaging (DWI)
Functional MR Imaging for <strong>Rectal</strong><br />
Cancer<br />
Axial T2 anatomic image DCE-MRI Ktrans Map<br />
DWI-MRI ADC Map<br />
Dzik-Jurasz ASK, Br J Radiol, 2005
PET for Treatment Planning
Impact of PET on RT Planning<br />
• Evaluate interobserver variability in<br />
contouring rectal cancer cases<br />
• <strong>Rectal</strong> cancer volumes contoured by 4<br />
radiation oncologists at Stanford<br />
– CT alone l<br />
– CT + PET
Impact of PET on RT Planning<br />
Patel, TCRT, 2007
Impact of PET on RT Planning<br />
• 20 rectal cancer, cancer 3 anal cancer patients<br />
• PET altered treatment volume in 17%<br />
• PET altered l d overall ll treatment plan l iin 2 25% %<br />
– Detection of distant metastases in rectal cancer<br />
patients<br />
Anderson, IJROBP, 2007
<strong>Rectal</strong> Tumor Motion<br />
• IMRT for rectal cancer limited by uncertainty in<br />
targeting i rectal ltumors<br />
• Consequence of rectal motion due to filling <strong>and</strong><br />
ddeformation f ti<br />
• Data from studies of prostate gl<strong>and</strong> motion using<br />
cine cine-MRI MRI demonstrate<br />
– <strong>Rectal</strong> motion <strong>and</strong> filling was a main determinant of<br />
prostate p intra-fraction motion<br />
• Inter-fraction motion for rectal tumors may be<br />
even greater Ghilezan M, IJROBP, 2005
<strong>Rectal</strong> CBCT Study<br />
• On-board CBCT can be used to quantify<br />
degree of rectal motion <strong>and</strong> volume change<br />
during RT<br />
• CBCT to measure accuracy <strong>and</strong> d precision of f a<br />
simulated IMRT treatment delivery model<br />
• 9 patients (8 rectal, 1 anal cancer) underwent<br />
> 1 CBCT during a course of RT<br />
• Co-registered to respective simulation CT<br />
scan by y matching g bony y anatomyy
Serial CT Scans<br />
Max RL Mean RL Max AP Mean AP<br />
Centroid<br />
motion (cm) 2.6 0.71 3.77 0.97
Degree of <strong>Rectal</strong> Deformation<br />
• IMRT plans generated for 8 rectal cases <strong>and</strong><br />
forward calculations were applied to the<br />
subsequent CBCT scans<br />
• 7 of 8 patients had adequate rectal coverage<br />
with ith IMRT plan l using i 15 mm margin i ddespite it<br />
rectal motion <strong>and</strong> deformation
Recommendations for IGRT for Pelvic<br />
Radiotherapy d h<br />
• Immobilization is essential essential, even with 3DCRT<br />
due to sacral rotation<br />
– Aquaplast mold mold, vacbag<br />
• Daily image guidance is necessary for highly<br />
conformal pelvic fields due to rectal motion<br />
– Daily KV<br />
– Daily l CBCT?<br />
– Fiducials
Conclusions<br />
• IMRT reduces toxicity associated with pelvic<br />
radiotherapy di th ffor anal l cancer <strong>and</strong> d with ith<br />
appropriate contouring, results in excellent<br />
local control<br />
• IMRT for rectal cancer has not been shown to<br />
reduce toxicity but may be beneficial in select<br />
cases<br />
• Incorporating better imaging into planning<br />
pelvic radiotherapy may allow for more<br />
targeted treatments
Thank you