DERGİSİ TIPDERGİSİ - DNT ORTADOĞU YAYINCILIK :: Anasayfa
DERGİSİ TIPDERGİSİ - DNT ORTADOĞU YAYINCILIK :: Anasayfa
DERGİSİ TIPDERGİSİ - DNT ORTADOĞU YAYINCILIK :: Anasayfa
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
Is Percentage Of Cancer Positive Cores In Prostate Biopsy Useful For Predicting The<br />
Changes In Gleason Scores After Radical Prostatectomy?<br />
Introduction<br />
Radical prostatectomy (RP), remains to be the treatment<br />
of choice for the patients with clinically localized prostate<br />
cancer and a life-expectancy of at least 10 years, due to<br />
its continously refined surgical outcomes and decreasing<br />
morbidity and mortality rates. Local recurrence-free survival<br />
rates of 83% and 75% were reported after RP for<br />
10 and 15 years, respectively (1). Prognostic factors after<br />
RP include baseline PSA level, clinical stage, biopsy<br />
Gleason score, postoperative Gleason score and pathological<br />
stage (2-4). It has been demonstrated in various studies<br />
that prostatectomy Gleason score is the most important<br />
prognostic factor for biochemical recurrence after RP<br />
(5, 6). Higher prostatectomy gleason score is associated<br />
with higher postoperative biochemical recurrence and low<br />
cancer-specific survival rates(7). On the other hand, it was<br />
reported that although the biopsy Gleason score remained<br />
unchanged after RP in 31-63% of the patients, it increased<br />
in 35 to 44% of them (8-10). These findings suggest that<br />
a pre-operative low-risk patient for biochemical failure<br />
and cancer-specific survival according to biopsy Gleason<br />
score may be in fact, a high-risk patient with respect to<br />
the RP gleason score. Considering the points mentioned<br />
above, preoperative prediction of the patients who are at<br />
the risk of Gleason score increase after RP may contribute<br />
the overall outcome of the definitive therapy.<br />
The association between the Gleason score increase after<br />
RP and percentage of positive biopsy cores was evaluated<br />
in this study.<br />
Material and Methods<br />
One hundred and ninety-five patients who underwent RP<br />
for clinically localized prostate cancer between January<br />
1997 and may 2008 were included in the study. Clinical<br />
and pathological records of the patients were evaluated retrospectively.<br />
Patients with a history of previous radiation<br />
or hormonal therapy (n=7), with 4ng/ml . PPC was obtained by dividing<br />
the number of cancer positive cores to the total number of<br />
biopsy cores. The total and free PSA levels were measured<br />
with monoclonal tandem assays using various kits in time.<br />
Histological grading of biopsy and RP specimens were<br />
made according to the Gleason grading system (11).<br />
50 ORTADOGU MEDICAL JOURNAL 4 (2): 49- 52 2012<br />
Gleason score increase and decrease were defined as<br />
“higher” and “lower than biopsy” RP scores, respectively.<br />
Clinical and pathological staging were performed according<br />
to the 2002 TNM classification.<br />
Patients were followed every 3 months first year, every 6<br />
months for the next 5 years and annually afterwards, with<br />
DRE, PSA and/or bone scan. Two consecutive PSA levels<br />
≥0.2ng/ml were defined as biochemical failure.<br />
Data were analyzed using SPSS software v11.5. Cathegorical<br />
data were presented as the number and percentage of<br />
the patients whereas continous variables were expressed as<br />
mean±standard deviation. The differences between independent<br />
groups regarding continous variables were evaluated<br />
by Kruskal-Wallis test. For categorical comparisons<br />
Chi-square test was used. P values lower than 0.05 were<br />
considered as statistically significant.<br />
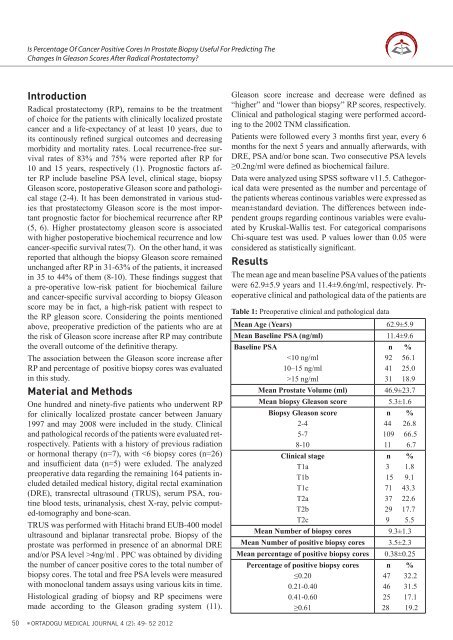
Results<br />
The mean age and mean baseline PSA values of the patients<br />
were 62.9±5.9 years and 11.4±9.6ng/ml, respectively. Preoperative<br />
clinical and pathological data of the patients are<br />
Table 1: Preoperative clinical and pathological data<br />
Mean Age (Years) 62.9±5.9<br />
Mean Baseline PSA (ng/ml) 11.4±9.6<br />
Baseline PSA<br />
n %<br />
15 ng/ml<br />
31 18.9<br />
Mean Prostate Volume (ml) 46.9±23.7<br />
Mean biopsy Gleason score 5.3±1.6<br />
Biopsy Gleason score<br />
n %<br />
2-4<br />
44 26.8<br />
5-7<br />
109 66.5<br />
8-10<br />
11 6.7<br />
Clinical stage<br />
n %<br />
T1a<br />
3 1.8<br />
T1b<br />
15 9.1<br />
T1c<br />
71 43.3<br />
T2a<br />
37 22.6<br />
T2b<br />
29 17.7<br />
T2c<br />
9 5.5<br />
Mean Number of biopsy cores 9.3±1.3<br />
Mean Number of positive biopsy cores 3.5±2.3<br />
Mean percentage of positive biopsy cores 0.38±0.25<br />
Percentage of positive biopsy cores n %<br />
≤0.20<br />
47 32.2<br />
0.21-0.40<br />
46 31.5<br />
0.41-0.60<br />
25 17.1<br />
≥0.61<br />
28 19.2