Molekulare Physiologie und Pathobiochemie ausgewählter Magen ...
Molekulare Physiologie und Pathobiochemie ausgewählter Magen ...
Molekulare Physiologie und Pathobiochemie ausgewählter Magen ...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
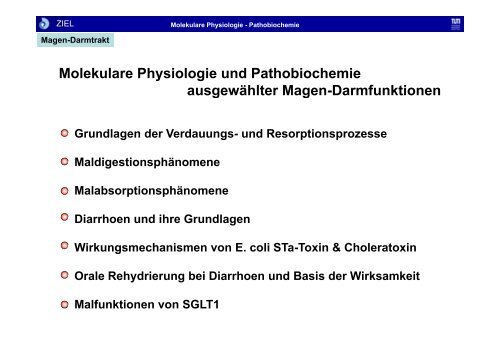
ZIEL<br />
<strong>Magen</strong>-Darmtrakt<br />
<strong>Molekulare</strong> <strong>Physiologie</strong> - <strong>Pathobiochemie</strong><br />
<strong>Molekulare</strong> <strong>Physiologie</strong> <strong>und</strong> <strong>Pathobiochemie</strong><br />
<strong>ausgewählter</strong> g <strong>Magen</strong>-Darmfunktionen<br />
g<br />
Gr<strong>und</strong>lagen der Verdauungs Verdauungs- <strong>und</strong> Resorptionsprozesse<br />
Maldigestionsphänomene<br />
Malabsorptionsphänomene<br />
Di Diarrhoen h <strong>und</strong> d ihre ih Gr<strong>und</strong>lagen<br />
G dl<br />
Wirkungsmechanismen von E. coli STa-Toxin & Choleratoxin<br />
Orale Rehydrierung bei Diarrhoen <strong>und</strong> Basis der Wirksamkeit<br />
Malfunktionen von SGLT1
ZIEL<br />
<strong>Molekulare</strong> <strong>Physiologie</strong> - <strong>Pathobiochemie</strong><br />
Gastrointestinaltrakt: Anatomie <strong>und</strong> Passagezeiten
ZIEL<br />
<strong>Molekulare</strong> <strong>Physiologie</strong> - <strong>Pathobiochemie</strong><br />
Intestinaltrakt: Morphologie <strong>und</strong> Ultrastruktur
ZIEL<br />
<strong>Molekulare</strong> <strong>Physiologie</strong> - <strong>Pathobiochemie</strong><br />
Intestinaltrakt: Morphologie <strong>und</strong> Ultrastruktur
ZIEL<br />
<strong>Molekulare</strong> <strong>Physiologie</strong> - <strong>Pathobiochemie</strong><br />
White-light endoscopy, in vivo imaging and histology of normal villi architecture of the terminal ileum<br />
Kiesslich R et al (2007) Technology Insight: confocal laser endoscopy for in vivo diagnosis of colorectal cancer<br />
Kiesslich R et al. (2007) Technology Insight: confocal laser endoscopy for in vivo diagnosis of colorectal cancer<br />
Nat Clin Pract Oncol 4: 480–490 doi:10.1038/ncponc0881
ZIEL<br />
<strong>Molekulare</strong> <strong>Physiologie</strong> - <strong>Pathobiochemie</strong><br />
Übersicht zur Verdauung <strong>und</strong> Resorption von Nährstoffen
ZIEL<br />
Gallenblase<br />
Pankreas<br />
<strong>Magen</strong><br />
Duodenum<br />
ca. 30 cm<br />
<strong>Molekulare</strong> <strong>Physiologie</strong> - <strong>Pathobiochemie</strong><br />
Jejunum<br />
ca. 120 cm<br />
α<br />
α<br />
Ileum<br />
ca. 180 cm<br />
Dickdarm<br />
Rektum<br />
membrangeb<strong>und</strong>ene<br />
Phase
ZIEL<br />
-AMYLASE<br />
<strong>Molekulare</strong> <strong>Physiologie</strong> - <strong>Pathobiochemie</strong><br />
Mechanismen der Resorption der Monosaccharide<br />
Amylose<br />
Amylopectin<br />
Gl Glycogen<br />
MMembrangeb<strong>und</strong>ene b b d Di-<strong>und</strong> Di d Oligosaccharid-Hydrolasen<br />
Oli h id H d l<br />
-Dextrine<br />
Malto-oligosaccharide<br />
Maltose<br />
Glucose<br />
Saccharose<br />
Lactose<br />
Glucose<br />
Galactose<br />
Fructose<br />
Glucose<br />
Galactose<br />
Fructose<br />
SGLT1<br />
Glut5<br />
Energiemetabolismus<br />
Na +<br />
Glucose<br />
Glut2<br />
Fructose<br />
Glut2<br />
Glut2<br />
Glut2<br />
Glucose<br />
K +<br />
Na +<br />
Glucose<br />
Galactose<br />
FFructose t<br />
Portalvenen-Blut
ZIEL<br />
Pankreasproteasen<br />
<strong>Molekulare</strong> <strong>Physiologie</strong> - <strong>Pathobiochemie</strong><br />
Mechanismen der Resorption der Aminosäuren<br />
Proteine<br />
Oligopeptide<br />
Di-/Tripeptide<br />
freie Aminosäuren<br />
Di-/Tripeptide<br />
H +<br />
PEPT-1 PEPT 1<br />
Imino<br />
Membran-geb<strong>und</strong>ene Peptidhydrolasen<br />
Aminosäuren<br />
ß<br />
B<br />
Aminosäuren-Pool<br />
X- X AG<br />
b 0,+<br />
cytosolische<br />
Hydrolasen ? Di-/Tripeptide<br />
Aminosäuren Aminosäuren<br />
B<br />
ASC<br />
L<br />
y +<br />
Aminosäuren<br />
Portalvene
ZIEL<br />
α<br />
β<br />
γ<br />
FS<br />
FS<br />
FS<br />
Triglyzeride mit<br />
llangkettigen k tti FS<br />
Lipase<br />
Lipase<br />
Lipase p<br />
<strong>Molekulare</strong> <strong>Physiologie</strong> - <strong>Pathobiochemie</strong><br />
Mechanismen der Resorption der Lipide<br />
FS<br />
α<br />
β<br />
γ<br />
α<br />
β<br />
γ<br />
FS<br />
FS<br />
FS<br />
OH<br />
OH<br />
FS<br />
OH<br />
ca. ca 10% 0%<br />
ca. 70%<br />
BP<br />
FS-BP<br />
ATP CoA-SH<br />
Thiokinase<br />
AMP + PP i<br />
FS-CoA<br />
OH<br />
FS<br />
OH<br />
Acyltransferasen<br />
CoA-SH<br />
FS FS, FFettsäure; ä BP BP, Bi Bindungsprotein<br />
d i<br />
FS Blutgefäße<br />
FS<br />
FS<br />
α OH<br />
FS<br />
FS<br />
β OH ca. 20% Lymphgefäße<br />
γ OH Apolipoproteine<br />
α FS<br />
β FS<br />
γ FS<br />
Triglyzeride mit kurz<strong>und</strong><br />
mittelkettigen FS<br />
Lipase<br />
Glyzerin<br />
FS<br />
Lymphgefäße<br />
y p g<br />
Blutgefäße
ZIEL<br />
<strong>Molekulare</strong> <strong>Physiologie</strong> - <strong>Pathobiochemie</strong><br />
Maldigestion (Ursachen von Verdauungsstörungen)<br />
Reduzierung oder Ausfall der Verdauungsfunktion des <strong>Magen</strong>s:<br />
Ursachen: Resektion, chronische atrophische Gastritis<br />
Folgen: Pepsin ↓: leicht durch Pankreasenzyme kompensierbar;<br />
Achlorhydrie: Bildung schwer lösl. Eisenkomplexe im neutralen Milieu = Eisenmangel<br />
Reduzierung oder Ausfall der exokrinen Pankreasfunktion:<br />
Ursachen: chronische Pankreatitis Pankreatitis, Karzinom Karzinom, Resektion Resektion, Fehlen von CCK <strong>und</strong> Sekretin<br />
nach <strong>Magen</strong>resektion.<br />
Folgen: Lipase (am störanfälligsten) ↓ mit Steatorrhoe, deren Ausmaß eine Klassifizierung<br />
der Pankreasinsuffizienz ermöglicht: leicht – nur nach Erhöhung des Fettanteils in<br />
der Nahrung; mäßig – bei Normalkost; schwer – bei fettreduzierter Kost.<br />
Gewichtsreduktion, Mangel an fettlöslichen Vitaminen, Durchfallneigung.<br />
Reduzierung oder Ausfall der Gallensäurenwirkung:<br />
Ursachen: Cholestase, Gallensäuren-Verlustsyndrom durch Ileumentzündung,<br />
stark beschleunigte Passage, Bestrahlungsschäden, bakterielle Fehlbesiedelung.<br />
FFolgen: l Fettverdauung F tt d <strong>und</strong> d –resorption ti ↓ (GS (GS-Verlust V l t mit it <strong>und</strong> d ohne h KKompensation), ti )<br />
chologene Diarrhoe durch sek. GS im Kolon, Gallensteinbildung, enterale Hyperoxalurie<br />
mit Nierensteinbildung durch Detergenzwirkung der GS im Kolon.
ZIEL<br />
<strong>Molekulare</strong> <strong>Physiologie</strong> - <strong>Pathobiochemie</strong><br />
MMalabsorption l b ti (Ursachen (U h von Dünndarmepithelstörungen)<br />
Dü d ith l tö )<br />
Erkrankungen g des Dünndarms mit den Leitsymptomen y Diarrhoe <strong>und</strong> Gewichtsverlust<br />
primär: Mucosa morphologisch unverändert;<br />
sek<strong>und</strong>är: Schädigung (Atrophie) der Mucosa oder Behinderung des Abtransportes<br />
resorbierter Stoffe durch Blut oder Lymphe.<br />
Beispiel: Zöliakie<br />
Hematoxylin-eosin stained cross-sections of intestinal villi: normal epithelium<br />
(left) and celiac epithelium (right), characterized by infiltration of intraepithelial lymphocytes and flattened villi.
ZIEL<br />
<strong>Molekulare</strong> <strong>Physiologie</strong> - <strong>Pathobiochemie</strong><br />
Celiac Disease (Zöliakie=glutensensitive Enteropathie<br />
Prävalenz auf 1:500 in Deutschland <strong>und</strong> Dänemark <strong>und</strong> etwa 1:110 in den USA <strong>und</strong> Großbritannien,<br />
im weltweiten Durchschnitt ungefähr 1:270<br />
Symptoms of celiac disease are caused by a glutamine and proline rich peptides fo<strong>und</strong> in gluten that<br />
initiates the inflammatory response when bo<strong>und</strong> to these HLA haplotypes (Shan, (Shan Lu et al, al 2002). 2002) The<br />
primary HLA association in most patients with celiac disease is with DQ2 (DQA*05/DQB1*02) and in a<br />
minority of patients with DQ8 (DQA1*03/DQB1*0302). Approximately 97% of individuals with celiac disease<br />
have the HLA-D2Q or HLA-DQ8, compared to 40% of the general population (NIH, 2006). The x-ray crystal<br />
structure of the soluble domain of HLA HLA-DQ2 DQ2 was observed bo<strong>und</strong> to the deaminated gluten epitope alpha- alpha<br />
I-gliadin. The HLA association in celiac disease can be explained by a superior ability of DQ2 to bind the<br />
repertoire of proline-rich gluten pepties that have survived gastrointestinal digestion and that have been<br />
deaminated by tissue transglutaminase (Kim et al., 2004).<br />
Celiac disease is diagnosed in about 10% of first degree relatives of an individual with celiac disease<br />
(Logan, 1992). Although hereditary factors play a significant role, genetic factors alone do not explain the<br />
development of the disease because the disease is concordant in only 60% to 70% of identical twins. All<br />
people with HLA DQ2 and DQ8 do not develop into disease, and others without those alleles can develop<br />
celiac disease, so more genes may be involved. Additional factors such as hormones and infectious<br />
agents may also be involved in linking the ingestion of gluten with a chronic inflammatory reaction in the<br />
intestine in genetically predisposed individuals (Fasano,1996).
<strong>Magen</strong>-Darmtrakt<br />
<strong>Molekulare</strong> <strong>Physiologie</strong> - <strong>Pathobiochemie</strong><br />
Gliadins are compact and in the globular shape and the glutenins are linear and have<br />
relatively higher molecular weight 50,000-millions compare with the molecular weight of gliadins 20,000-50,000.
ZIEL<br />
<strong>Molekulare</strong> <strong>Physiologie</strong> - <strong>Pathobiochemie</strong><br />
Digestion breaks down gluten (A) into peptides (B) that are absorbed by the small intestine.<br />
There, the enzyme tissue transglutaminase (C) modifies certain peptides, which are picked up<br />
by dendritic cells and, in people with celiac disease, stimulate immune cells (D) to attack the intestine.<br />
Nearly all people with the disease have one of two immune-molecule types: About 90 percent<br />
ea y a peop e t t e d sease a e o e o t o u e o ecu e types bout 90 pe ce t<br />
carry so-called DQ2 molecules, and most of the rest carry DQ8 molecules.<br />
Genetics determines whether a person has either or both of these disease-associated molecules
ZIEL<br />
<strong>Molekulare</strong> <strong>Physiologie</strong> - <strong>Pathobiochemie</strong><br />
Depiction of the intestinal mucosa with emphasis on the factors that take part in the development and control of coeliac disease. a | The parts of gluten that are<br />
resistant to processing p gby y luminal and brush-border enzymes y will survive digestion, g , and can be transported p across the mucosal epithelium p as polypeptides.<br />
p yp p<br />
Gluten peptides are deamidated by tissue transglutaminase (TG2), which, in the intestinal mucosa, is located mainly extracellularly in the subepithelial region,<br />
but is also fo<strong>und</strong> in the brush border. CD4+ T cells in the lamina propria recognize deamidated gluten peptides predominantly, presented by HLA-DQ2 or -DQ8<br />
molecules on the cell surface of antigen-presenting cells (APCs). b | Immunofluorescence staining of TG2 (pink), HLA-DQ (green) and T cells (CD3; purple) in<br />
the small-intestine mucosa of an untreated coeliac-disease patient. Note that there is a close spatial relationship between TG2, APCs that express HLA-DQ and<br />
T cells just beneath the epithelium.
ZIEL<br />
<strong>Molekulare</strong> <strong>Physiologie</strong> - <strong>Pathobiochemie</strong><br />
Factors that might contribute to this clustering are indicated. | Proline protects peptides from proteolytic degradation during digestion. | Proline has a<br />
dominant role in the specificity of tissue transglutaminase (TG2) and guides which glutamine residues can be deamidated. c | Oligomerized epitopes<br />
can be particularly efficient as T-cell antigens and TG2 substrates. A 33-mer fragment of α-gliadin, which results from physiological processing, is<br />
shown. This fragment contains three unique T-cell epitopes, which are present three, two and one times, respectively. d | Proline can facilitate binding<br />
to HLA-DQ2 by acting as an anchor residue or by inducing a type-II polyproline helical conformation.
ZIEL<br />
<strong>Molekulare</strong> <strong>Physiologie</strong> - <strong>Pathobiochemie</strong><br />
Gliadin peptide fragment derived from gluten protein is presented by antigen-presenting<br />
cells with specific class II HLA-DQ alleles.<br />
Model of the gliadin peptide.<br />
Surface of HLA-DQ with bo<strong>und</strong> gliadin peptide to red region.<br />
Hydrogen-bonding network in the HLA-DQ-gliadin complex
ZIEL<br />
<strong>Molekulare</strong> <strong>Physiologie</strong> - <strong>Pathobiochemie</strong><br />
Gliadin is absorbed into the lamina propia and presented in conjunction with HLA-DQ2 or DQ8 cell-surface antigens by antigen-presenting cells,<br />
probably dendritic cells, to sensitized T cells expressing the α/β TT-cell cell receptor. Tissue transglutaminase deaminates gliadin peptides, generating<br />
acidic, negatively charged residues of glutamic acid from neutral glutamines (inset). Since negatively charged residues are preferred in positions 4,6,<br />
and 7 of the antigen-binding groove of HLA-DQ2, deaminated gliadin elicits a stronger T-cell response. These lymphocytes then activate other<br />
lymphocytes to generate cytokines, such as interferon-γ, interleukin-4, and tumor necrosis factor α (TNF- α), which damage the villi, resulting in<br />
enteritis. Induction of aberrant HLA class II cell-surface antigens on the enterocytes may permit these cells to present additional antigens to the<br />
sensitized lymphocytes (Westerberg et al.,2006).
ZIEL<br />
Diät bei Zöliakie<br />
<strong>Molekulare</strong> <strong>Physiologie</strong> - <strong>Pathobiochemie</strong><br />
Momentan ist die einzige gesicherte Möglichkeit Möglichkeit, die Krankheit zu behandeln, behandeln eine lebenslange glutenfreie Diät Diät, wodurch der Darm wieder heilt <strong>und</strong><br />
auch die Risiken der Langzeitfolgen sinken. Strikt zu vermeiden sind alle Getreidesorten mit hohem Glutengehalt (Weizen, Gerste, Roggen, wie auch<br />
deren botanisch verwandten Ursorten Dinkel, Grünkern, Einkorn, Emmer sowie die Roggen-Weizen-Kreuzung Triticale).<br />
Ausdrücklich erlaubt sind Hirse, Mais, Reis, Amarant, Buchweizen, Quinoa, Sojabohnen, Teff, Kastanie, Kochbanane.<br />
Ein Teil dieser Sorten wird beispielsweise auch zur Herstellung von glutenfreiem Bier verwendet verwendet. Ohnehin erlaubt sind Gemüse einschließlich<br />
Kartoffeln, Salate, Früchte, Fleisch <strong>und</strong> Fisch, Eier, Milch <strong>und</strong> Milchprodukte.<br />
Subtotal villous atrophy<br />
Same patient after 4 weeks<br />
on gluten free diet
ZIEL<br />
<strong>Molekulare</strong> <strong>Physiologie</strong> - <strong>Pathobiochemie</strong><br />
Störungen der Elektrolyt- Elektrolyt <strong>und</strong> Wasserresorption
ZIEL<br />
<strong>Magen</strong><br />
ca. 1000 ml<br />
Getränke/Nahrung<br />
ca. 1500 ml<br />
ca. 2000 ml<br />
Pankreas <strong>und</strong> Galle<br />
<strong>Molekulare</strong> <strong>Physiologie</strong> - <strong>Pathobiochemie</strong><br />
Intestinale Flüssigkeitsbilanz beim Ges<strong>und</strong>en<br />
Dünndarm<br />
ca. 2000 ml<br />
Dünndarm Dickdarm Rektum ca. 100 ml im Stuhl<br />
ca. 4500 ml ca. 2000 ml<br />
Resorbiert: ca. 6500 ml
ZIEL<br />
Ileocaecaler<br />
Fluss<br />
Stuhlwasser<br />
<strong>Molekulare</strong> <strong>Physiologie</strong> - <strong>Pathobiochemie</strong><br />
Wasserbewegungen im Darm <strong>und</strong> ihre Störungen<br />
Ges<strong>und</strong> Dünndarmerkrankung Dickdarmerkrankung<br />
2000 ml 4500 ml 5900 ml 2500 ml 2500 ml<br />
100 ml<br />
1900 ml 4400 ml 4400 ml 1000 ml<br />
100 ml<br />
1500 ml<br />
1500 ml 3000 ml<br />
Diarrhoe nein nein ja ja ja<br />
500 ml
ZIEL<br />
<strong>Molekulare</strong> <strong>Physiologie</strong> - <strong>Pathobiochemie</strong><br />
Funktionelle Gr<strong>und</strong>lagen der Elektrolytresorption im Darm (Colon)<br />
Na<br />
K<br />
Cl -<br />
Na<br />
NHE-3<br />
H<br />
K<br />
Na<br />
K K<br />
NaCl NaCl<br />
HCO -<br />
HCO 3<br />
Cl -<br />
CA<br />
HCO -<br />
3<br />
H2O+ CO2 Cl -<br />
Na<br />
0 mV V -40 40 mV V<br />
-20 20 mV V<br />
osmotischer Wasser-Gradient<br />
Cl -
ZIEL<br />
<strong>Molekulare</strong> <strong>Physiologie</strong> - <strong>Pathobiochemie</strong><br />
Von der <strong>Physiologie</strong> y g zur Pathophysiologie p y g <strong>und</strong> ihrer molekularen Gr<strong>und</strong>lagen g
ZIEL<br />
<strong>Molekulare</strong> <strong>Physiologie</strong> - <strong>Pathobiochemie</strong><br />
Diarrhoen als weltweites Ges<strong>und</strong>heitsproblem<br />
In 2002, 142,311 cases of cholera including 4564 deaths<br />
were officially reported to the World Health Organization,<br />
although this is almost certainly an <strong>und</strong>erestimate
ZIEL<br />
<strong>Molekulare</strong> <strong>Physiologie</strong> - <strong>Pathobiochemie</strong><br />
Diarrhoen als weltweites Ges<strong>und</strong>heitsproblem
ZIEL<br />
<strong>Molekulare</strong> <strong>Physiologie</strong> - <strong>Pathobiochemie</strong><br />
Wirkungen von Cholera-Toxin auf die Sekretionsprozesse
ZIEL<br />
<strong>Molekulare</strong> <strong>Physiologie</strong> - <strong>Pathobiochemie</strong><br />
Invasionsweg des Choleratoxins
ZIEL<br />
<strong>Molekulare</strong> <strong>Physiologie</strong> - <strong>Pathobiochemie</strong><br />
Choleratoxin führt zur ADP-Ribosylierung des G-α-Protein der Adenylatcyclase<br />
constitutiv erhöhte<br />
c-AMP-Spiegel
ZIEL<br />
<strong>Molekulare</strong> <strong>Physiologie</strong> - <strong>Pathobiochemie</strong><br />
Vom Cholera-Toxin zu E. coli STa-Toxin (Reisediarrhoe)<br />
( )
ZIEL<br />
<strong>Molekulare</strong> <strong>Physiologie</strong> - <strong>Pathobiochemie</strong><br />
Struktur des Guanylacyclase C-Gens <strong>und</strong> seiner funktionellen Dömänen<br />
Sequenzhomologien/ Sequenzhomologien/-identitäten identitäten in Guanylin <strong>und</strong> EE. coli STa-Toxin<br />
STa Toxin
ZIEL<br />
<strong>Molekulare</strong> <strong>Physiologie</strong> - <strong>Pathobiochemie</strong><br />
Mechanismus der Aktivierung der Guanylatcyclase C<br />
durch Guanylin/E Guanylin/E. coli STa-Toxin
ZIEL<br />
<strong>Molekulare</strong> <strong>Physiologie</strong> - <strong>Pathobiochemie</strong><br />
Signalkette von Guanylin/E. coli STa-Toxin bei der Initiation<br />
der intestinalen Elektrolytsekretion
ZIEL<br />
<strong>Molekulare</strong> <strong>Physiologie</strong> - <strong>Pathobiochemie</strong><br />
Behandlung intestinaler Sekretionsstörungen (Diarrhoen)<br />
Orale Rehydrierungslösung (WHO)
ZIEL<br />
<strong>Molekulare</strong> <strong>Physiologie</strong> - <strong>Pathobiochemie</strong><br />
Die zentrale Rolle von SGLT1 in der oralen Rehydrierung<br />
Immunhistochemischer Nachweis<br />
von SGLT1 im Dünndarmepithel
ZIEL<br />
<strong>Molekulare</strong> <strong>Physiologie</strong> - <strong>Pathobiochemie</strong><br />
Die Membrantopologie von SGLT1<br />
Die SGLT-Proteinfamilie in Prokaryoten <strong>und</strong> Eukaryoten
ZIEL<br />
<strong>Molekulare</strong> <strong>Physiologie</strong> - <strong>Pathobiochemie</strong><br />
HHereditäre ditä Gl Glucose/Galactose /G l t Malabsorption<br />
M l b ti<br />
durch Mutationen (autosomal recessiv) im SGLT1-Gen