Drug Disposition Overview - Pharmacology and at UCSD
Drug Disposition Overview - Pharmacology and at UCSD
Drug Disposition Overview - Pharmacology and at UCSD
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
BIOM/PHAR 255 Winter 2013 Halpert - Jan. 17, 2013<br />
<strong>Drug</strong> Metabolism <strong>and</strong> <strong>Disposition</strong><br />
BIOM/PHAR 255<br />
James R. Halpert, Ph.D.<br />
Tuesday, January 17, 2013<br />
10:00 -12:00<br />
• Absorption<br />
– Transporters<br />
• Distribution<br />
– Transporters<br />
• Metabolism<br />
– Enzymes<br />
• Excretion<br />
– Transporters<br />
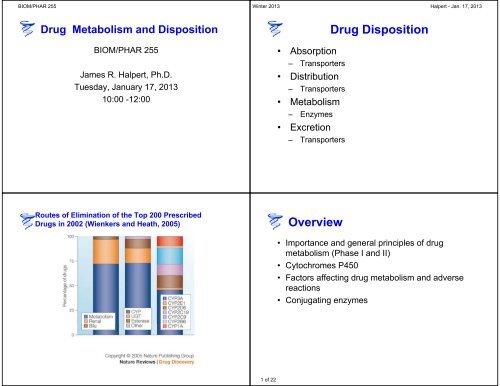
Routes of Elimin<strong>at</strong>ion of the Top 200 Prescribed<br />
<strong>Drug</strong>s in 2002 (Wienkers <strong>and</strong> He<strong>at</strong>h, 2005) <strong>Overview</strong><br />
1 of 22<br />
<strong>Drug</strong> <strong>Disposition</strong><br />
• Importance <strong>and</strong> general principles of drug<br />
metabolism (Phase I <strong>and</strong> II)<br />
• Cytochromes P450<br />
• Factors affecting drug metabolism <strong>and</strong> adverse<br />
reactions<br />
• Conjug<strong>at</strong>ing enzymes
BIOM/PHAR 255 Winter 2013 Halpert - Jan. 17, 2013<br />
Importance <strong>and</strong> General Principles<br />
of <strong>Drug</strong> Metabolism<br />
<strong>Drug</strong> Therapy: The challenges<br />
1. Non-responders<br />
Only 30-60 % of p<strong>at</strong>ients respond to the<br />
common drugs.<br />
2. Serious adverse drug reactions (ADRs):<br />
5-7 % of all hospital admissions<br />
2 days prolonged hospital visit<br />
$2,500 per p<strong>at</strong>ient, $100 billion in USA per year<br />
100,000 de<strong>at</strong>hs annually in US<br />
2 of 22<br />
<strong>Drug</strong> Metabolism in Clinical<br />
Practice<br />
• Goals<br />
– Underst<strong>and</strong> factors th<strong>at</strong><br />
affect metabolism of a<br />
drug<br />
– Predict metabolism of<br />
the drug in an individual<br />
– Design r<strong>at</strong>ional therapy<br />
regimen th<strong>at</strong> is safe <strong>and</strong><br />
effective.<br />
• Need to know<br />
– Which enzymes<br />
(isoforms) metabolize<br />
the drug<br />
– How each enzyme is<br />
affected by genetic<br />
<strong>and</strong> environmental<br />
factors (including other<br />
drugs)<br />
– The rel<strong>at</strong>ive<br />
therapeutic efficacies<br />
<strong>and</strong> toxicities of drug<br />
<strong>and</strong> metabolites<br />
Reasons for termin<strong>at</strong>ion of drug c<strong>and</strong>id<strong>at</strong>es in<br />
development in 2000<br />
Attrition due to PK/bioavailability decreased from 40% to 8% between 1991 <strong>and</strong><br />
2000 in large measure due to incorpor<strong>at</strong>ion of these concepts in early drug<br />
discovery. Guengerich, F.P. (2007). Chem Res.<br />
Toxicol. 20:344-369.
BIOM/PHAR 255 Winter 2013 Halpert - Jan. 17, 2013<br />
Metabolism → Termin<strong>at</strong>ion of drug action<br />
Bioinactiv<strong>at</strong>ion<br />
Detoxific<strong>at</strong>ion<br />
Elimin<strong>at</strong>ion<br />
Metabolism → Bioactiv<strong>at</strong>ion<br />
Active Metabolites<br />
Prodrugs<br />
Toxific<strong>at</strong>ion<br />
Role of the liver in drug<br />
metabolism<br />
• The liver is the most important organ in the<br />
biotransform<strong>at</strong>ion of most xenobiotics (foreign<br />
compounds).<br />
– All compounds absorbed from the g.i. tract reach<br />
the liver via the portal vein before they reach<br />
other organs.<br />
– The liver is the largest organ in the body <strong>and</strong><br />
contains the highest content of xenobioticmetabolizing<br />
enzymes.<br />
3 of 22<br />
Sites of drug<br />
biotransform<strong>at</strong>ion<br />
• Liver<br />
• Gastrointestinal tract<br />
• Kidney<br />
• Respir<strong>at</strong>ory tissues<br />
– lung<br />
– nose<br />
• Brain, skin, heart<br />
<strong>Drug</strong> metabolism <strong>and</strong> elimin<strong>at</strong>ion<br />
From Weinshilboum, R.(2003) NEJM 348 (6): 529-537
BIOM/PHAR 255 Winter 2013 Halpert - Jan. 17, 2013<br />
Conversion of a Hydrophobic <strong>Drug</strong> to a<br />
W<strong>at</strong>er-Soluble Metabolite<br />
Phenytoin<br />
O<br />
H<br />
N<br />
NH<br />
O<br />
CYP<br />
HO<br />
4-Hydroxy<br />
phenytoin<br />
O<br />
W<strong>at</strong>er solubility<br />
H<br />
N<br />
NH<br />
O<br />
UGT<br />
COOH<br />
O<br />
O<br />
HO OH<br />
General P<strong>at</strong>hways of <strong>Drug</strong> Metabolism<br />
REACTION ENZYME<br />
Hydrolysis<br />
Reduction<br />
Oxid<strong>at</strong>ion<br />
Esterase, peptidase, epoxide hydrolase<br />
Azo <strong>and</strong> nitro reduction<br />
Carbonyl, disulfide, sulfoxide, quinone<br />
Alchohol <strong>and</strong> aldehyde dehydrogenase<br />
Xanthine <strong>and</strong> diamine oxidase<br />
Monomine oxidase<br />
Prostagl<strong>and</strong>in H synthase<br />
Flavin-monooxygenases<br />
Cytochrome P450s<br />
Conjug<strong>at</strong>ion Glucuronide, sulf<strong>at</strong>e, glut<strong>at</strong>hione, acyl<strong>at</strong>ion,<br />
methyl<strong>at</strong>ion<br />
4-Hydroxy-phenytoin<br />
Β-D-glucuronide<br />
OH<br />
O<br />
H<br />
N<br />
Expose or<br />
Introduce.<br />
-OH<br />
-NH 2<br />
-SH<br />
-COOH<br />
NH<br />
Synthetic<br />
O<br />
4 of 22<br />
Phase I:<br />
Purpose of phase I <strong>and</strong> phase II<br />
metabolism<br />
Detoxify<br />
Enhance excretion<br />
RH --> ROH (more w<strong>at</strong>er<br />
soluble <strong>and</strong> prepares for<br />
phase II)<br />
Phase II = Conjug<strong>at</strong>ion:<br />
Enhance excretion<br />
Detoxify (e.g. GSH)<br />
Acts on parent drug<br />
Acts on phase I<br />
metabolite<br />
Cytochrome<br />
P450<br />
Cytochromes P450<br />
Excretion<br />
Xenobiotic<br />
Phase I<br />
Metabolism<br />
Excretion<br />
Phase II<br />
Metabolism<br />
Glucuronides<br />
Sulf<strong>at</strong>es<br />
GSH-conjug<strong>at</strong>es<br />
Other conjug<strong>at</strong>es<br />
Excretion
BIOM/PHAR 255 Winter 2013 Halpert - Jan. 17, 2013<br />
General Fe<strong>at</strong>ures of Cytochromes P450<br />
• Heme protein<br />
• Loc<strong>at</strong>ed in the smooth endoplasmic reticulum (<strong>and</strong><br />
sometimes mitochondria) of all major organs <strong>and</strong><br />
tissues<br />
• Require NADPH cytochrome P450 reductase to<br />
deliver electrons<br />
• Many are inducible<br />
Class II (Mammalian) Xenobiotic Metabolism System<br />
more polar<br />
metabolite<br />
H 2O<br />
Cytochrome<br />
P450<br />
heme<br />
lipophilic substr<strong>at</strong>e<br />
O 2<br />
Cytochrome<br />
P450 Reductase<br />
FMN<br />
FAD<br />
2 NADPH<br />
2 e -<br />
2 NADP +<br />
5 of 22<br />
Cytochromes P450 (CYP)<br />
Show peak <strong>at</strong> 450 nm in the<br />
P450 red-CO form<br />
Biochemical reaction:<br />
RH + O 2 + NADPH + H + ROH + H 2O + NADP +<br />
Heme pocket of cytochromes P450<br />
H H<br />
O<br />
Fe 3+<br />
S<br />
The heme group in P450 is invariant. It is the size <strong>and</strong> shape of the<br />
binding pocket th<strong>at</strong> distinguishes different P450 enzymes.
BIOM/PHAR 255 Winter 2013 Halpert - Jan. 17, 2013<br />
Types of P450 Reactions<br />
1. Hydroxyl<strong>at</strong>ion of aliph<strong>at</strong>ic or arom<strong>at</strong>ic carbons<br />
2. Epoxid<strong>at</strong>ion of a double bond<br />
3. Hetero<strong>at</strong>om (S-, N-) oxygen<strong>at</strong>ion <strong>and</strong> N-hydroxyl<br />
4. Hetero<strong>at</strong>om (O-, S-, N-) dealkyl<strong>at</strong>ion<br />
5. Oxid<strong>at</strong>ive group transfer<br />
6. Cleavage of esters<br />
7. Dehydrogen<strong>at</strong>ion<br />
P450 oxid<strong>at</strong>ion reactions<br />
Epoxid<strong>at</strong>ion (arene oxide form<strong>at</strong>ion)<br />
benzo[a]pyrene<br />
N-, O- <strong>and</strong> S-dealkyl<strong>at</strong>ion<br />
O<br />
H3 C CH3 N<br />
CH3CH2 C C CH2CH CH3 methadone<br />
O<br />
benzo[a]pyrene-7,8-epoxide<br />
H3C H<br />
O N<br />
CH3 CH2 C C CH2CH CH3 +<br />
H C<br />
H<br />
O<br />
6 of 22<br />
P450 reactions: oxid<strong>at</strong>ion <strong>at</strong><br />
C<br />
aliph<strong>at</strong>ic hydroxyl<strong>at</strong>ion<br />
H 3 C<br />
CH 3CH 2<br />
O<br />
CH2 CH2 CH2 CH3 pentobarbital<br />
arom<strong>at</strong>ic hydroxyl<strong>at</strong>ion<br />
CH 3CH 2<br />
O<br />
phenobarbital<br />
N<br />
NH ONa<br />
O<br />
NH ONa<br />
O<br />
N<br />
HO<br />
H 3C<br />
CH 3 CH 2<br />
P450 nomencl<strong>at</strong>ure<br />
Based on sequence identity:<br />
O<br />
CH<br />
OH<br />
CH 3 CH 2<br />
CH 2<br />
N<br />
O<br />
CH2 CH3 NH ONa<br />
O<br />
NH ONa<br />
MELSVLLLLALLTGLLLLMARGHPKAYGHLPPGPRP…<br />
MEFSLLLLLAFLAGLLLLLFRGHPKAHGRLPPGPSP…<br />
Family: ≥ 40% sequence identity.<br />
for example: CYP1, CYP2<br />
Subfamily: 40% - 55% sequence identity.<br />
for example: CYP2A, CYP2B<br />
Within subfamily: ≥ 55% sequence identity.<br />
for example: CYP2B1, CYP2B4<br />
O<br />
N
BIOM/PHAR 255 Winter 2013 Halpert - Jan. 17, 2013<br />
Major Human Liver <strong>Drug</strong><br />
Metabolizing Cytochromes P450<br />
P450 Substr<strong>at</strong>e Inducer Inhibitor<br />
1A2 Caffeine PAH Furafylline<br />
2A6 Coumarin Phenytoin Tranylcypromine<br />
2B6 Bupropion Phenobarbital Ticlopidine<br />
2C8 Taxol Rifampicin Trimethoprim<br />
2C9 Tolbutamide Secobarbital Sulfaphenazole<br />
2C19 S-Mephenytoin Rifampicin Benzylnirvanol<br />
2D6 Debrisoquine Quinidine<br />
2E1 Chlorzoxazone Ethanol Diethyldithiocarbam<strong>at</strong>e<br />
3A4 Midazolam Rifampicin Trole<strong>and</strong>omycin<br />
3A5 Midazolam Glucocorticoids Ketoconazole<br />
Cytochrome P450 1A2<br />
Planar arom<strong>at</strong>ic/heterocyclic amines <strong>and</strong> amides<br />
Substr<strong>at</strong>es Inhibitor<br />
Caffeine<br />
Phenacetin<br />
Furafylline (MBI)<br />
MBI = mechanismbased<br />
inactiv<strong>at</strong>or<br />
7 of 22<br />
Characteristics of Human P450 Substr<strong>at</strong>es<br />
•1A2: Planar arom<strong>at</strong>ic/heterocyclic amines <strong>and</strong> amides<br />
• 2A6: Small polar compounds with a ketone or nitroso group<br />
•2B6: Non-planar (often V-shaped), lipophilic molecules<br />
•2C8: Large organic anions<br />
•2C9: Weakly acidic compounds<br />
•2C19:Neutral or basic compounds<br />
•2D6: Nitrogenous bases with site of metabolism 4-7 Å<br />
from basic nitrogen<br />
•2E1 Generally neutral compounds of low molecular weight<br />
•3A4 Structurally diverse compounds of rel<strong>at</strong>ively high<br />
molecular weight<br />
Cytochrome P450 2A6<br />
Small polar compounds with a ketone or nitroso group<br />
Substr<strong>at</strong>es Inhibitors<br />
Coumarin<br />
(R)-(+)Menthofuran (MBI)<br />
Tranylcypromine
BIOM/PHAR 255 Winter 2013 Halpert - Jan. 17, 2013<br />
Cytochrome P450 2B6<br />
Substr<strong>at</strong>es Inhibitor<br />
(S)-Mephenytoin<br />
Buproprion<br />
Non-planar (often V-shaped), lipophilic molecules<br />
Cytochrome P450 2C9<br />
Ticlopidine (MBI)<br />
Substr<strong>at</strong>es Inhibitors<br />
Tolbutamide<br />
Diclofenac<br />
Weakly acidic compounds<br />
Tienilic acid (MBI)<br />
Sulfaphenazole<br />
8 of 22<br />
Cytochrome P450 2C8<br />
Large organic anions<br />
Substr<strong>at</strong>e Inhibitor<br />
Taxol (paclitaxel) Trimethoprim<br />
Cytochrome P450 2C19<br />
Neutral or basic compounds<br />
Substr<strong>at</strong>e Inhibitor<br />
(S)-Mephenytoin<br />
(+)-N-3-Benzyl-nirvanol
BIOM/PHAR 255 Winter 2013 Halpert - Jan. 17, 2013<br />
Cytochrome P450 2D6<br />
Nitrogenous bases with site of metabolism 4-<br />
7 Å from basic nitrogen<br />
Substr<strong>at</strong>es Inhibitors<br />
Debrisoquine<br />
Dextromorphan Hydrobromide<br />
Testosterone<br />
Cytochrome P450 3A4<br />
Quinidine<br />
Paroxetine (QI)<br />
QI = quasi-irreversible<br />
Structurally diverse compounds of rel<strong>at</strong>ively high molecular weight<br />
Substr<strong>at</strong>es Inhibitors<br />
Midazolam<br />
Ketoconazole<br />
9 of 22<br />
Cytochrome P450 2E1<br />
Generally neutral compounds of low molecular weight<br />
Substr<strong>at</strong>es Inhibitors<br />
Chlorzoxazone<br />
N-Nitrosodimethylamine<br />
Cytochrome P450 3A4<br />
4-Methylpyrazole<br />
Diethyldithiocarbam<strong>at</strong>e<br />
Substr<strong>at</strong>es Inhibitors<br />
Erythromycin Trole<strong>and</strong>omycin (QI)
BIOM/PHAR 255 Winter 2013 Halpert - Jan. 17, 2013<br />
Cytochromes P450 (Enzyme<br />
Structures)<br />
Six Protein Regions th<strong>at</strong> Contribute to<br />
Substr<strong>at</strong>e Selectivity: SRS<br />
Substr<strong>at</strong>e Recognition Sites<br />
(SRS)<br />
Gotoh (1992) J. Biol. Chem. 267,<br />
83-90.<br />
SRS1<br />
SRS2<br />
SRS3<br />
SRS4<br />
SRS5<br />
SRS6<br />
heme<br />
2B4<br />
PDB 1SUO<br />
10 of 22<br />
General Structure of Mammalian<br />
Cytochromes P450<br />
Structural<br />
components<br />
alpha helix<br />
beta sheet<br />
heme<br />
protoporphyrin<br />
IX prosthetic<br />
group<br />
2B4<br />
PDB: 1PO5<br />
Major structural fe<strong>at</strong>ures th<strong>at</strong><br />
determine specificity of P450 enzymes<br />
• Length <strong>and</strong> positioning of α−helices <strong>and</strong> βsheets<br />
determines size <strong>and</strong> shape of binding<br />
pocket<br />
• Identity of active site residues determines<br />
binding orient<strong>at</strong>ion of substr<strong>at</strong>es
BIOM/PHAR 255 Winter 2013 Halpert - Jan. 17, 2013<br />
Comparison between the active site cavity volumes for human P450 1A2 (A) (PDB: 2HI4),<br />
P450 2A6 (B) (PDB: 1Z10 (6)), <strong>and</strong> P450 3A4 (C) (PDB: 1TQN (14)).<br />
Sansen S et al. J. Biol. Chem. 2007;282:14348-14355<br />
©2007 by American Society for Biochemistry <strong>and</strong> Molecular Biology<br />
Comparison of P450 Inhibition <strong>and</strong> Induction<br />
Inhibition Induction<br />
Mechanism Direct effect on Synthesis of new<br />
existing enzyme protein<br />
Onset Rapid Slow<br />
Prior exposure Not needed Needed<br />
11 of 22<br />
Factors Affecting <strong>Drug</strong> Metabolism <strong>and</strong><br />
Adverse <strong>Drug</strong> Reactions<br />
Age<br />
Diet<br />
Disease<br />
<strong>Drug</strong> Dose<br />
Enzyme Induction<br />
Enzyme Inhibition<br />
Gender<br />
Genetics<br />
Pregnancy<br />
Metabolic Basis of <strong>Drug</strong> Interactions<br />
Perpetr<strong>at</strong>or Victim Consequence<br />
P450 Inhibitor <strong>Drug</strong> Increased effect/ADR<br />
P450 Inhibitor Pro-<strong>Drug</strong> Decreased effect<br />
P450 Inducer <strong>Drug</strong> Decreased effect<br />
P450 Inducer Pro-<strong>Drug</strong> Increased effect/ADR
BIOM/PHAR 255 Winter 2013 Halpert - Jan. 17, 2013<br />
Mechanisms of P450 Inhibition<br />
•Altern<strong>at</strong>e substr<strong>at</strong>e inhibition<br />
•Binding of nitrogen heterocycles to heme<br />
iron (ketoconazole, itraconazole)<br />
•Binding of a metabolite to the reduced<br />
heme iron (trole<strong>and</strong>omycin, paroxetine)<br />
•Irreversible modific<strong>at</strong>ion of the protein or<br />
heme moiety by a reactive metabolite<br />
(tienilic acid, ticlopidine, chloramphenicol)<br />
Factors affecting drug metabolism<br />
Enzyme induction: examples<br />
12 of 22<br />
Effect of fluovoxamine on caffeine<br />
pharmacokinetics (>10-fold increase in<br />
t 1/2 <strong>and</strong> AUC)<br />
Nuclear Receptors Th<strong>at</strong> Induce <strong>Drug</strong> Metabolism<br />
RECEPTOR LIGANDS<br />
• Aryl hydrocarbon receptor (AhR)<br />
• Constitutive <strong>and</strong>rostane receptor<br />
(CAR)<br />
• Pregnane X receptor (PXR)<br />
• Farnesoid X receptor (FXR)<br />
• Vitamin D receptor<br />
• Peroxisome prolifer<strong>at</strong>or activ<strong>at</strong>ed<br />
receptor (PPAR)<br />
• Retinoic acid receptor (RAR)<br />
• Retinoid X receptor (RXR)<br />
• Omeprazole, Flavonoids<br />
• Phenobarbital<br />
• Rifampin<br />
• Bile Acids<br />
• Vitamin D<br />
• Fibr<strong>at</strong>es<br />
• all-trans-Retinoic acid<br />
• 9-cis-Retinoic acid
BIOM/PHAR 255 Winter 2013 Halpert - Jan. 17, 2013<br />
Model for PXR in Xenobiotic Regul<strong>at</strong>ion<br />
Xenobiotic Pregnane X<br />
PXR RXR<br />
CYP3A gene<br />
“Other drug metabolism genes”<br />
Xenobiotic<br />
CYP3A<br />
Common Perpetr<strong>at</strong>or <strong>Drug</strong>s<br />
HO-Xenobiotic<br />
Steroid<br />
HO-Steroid<br />
•Strong inducers of CYP3A4 (rifampicin, dexamethasone,<br />
phenobarbital, carbamazepine)<br />
•Strong inhibitors of CYP3A4 (ritonavir, ketoconazole)<br />
•Strong inhibitors of CYP2D6 (quinidine, fluoxetine,<br />
paroxetine)<br />
•Inhibitors of multiple P450 enzymes (fluvoxamine)<br />
Common Victim <strong>Drug</strong>s<br />
•<strong>Drug</strong>s with a narrow therapeutic index (warfarin,<br />
phenytoin, digoxin)<br />
•Substr<strong>at</strong>es of CYP3A with low oral bioavailability<br />
(triazolam)<br />
13 of 22<br />
Why are clinically significant drug<br />
interactions rel<strong>at</strong>ively uncommon?<br />
•The interaction, while st<strong>at</strong>istically significant, is<br />
too small to produce a clinically important<br />
change in the dynamics of the drug.<br />
•The therapeutic index of the victim drug is<br />
large enough th<strong>at</strong> even a substantial change in<br />
plasma levels does not alter therapeutics or<br />
toxicity.<br />
•Kinetics <strong>and</strong> response to the victim drug are so<br />
variable th<strong>at</strong> they overshadow changes in<br />
plasma levels due to the interaction.<br />
CYP dependent metabolism of drugs (80 % of<br />
all phase I metabolism of drugs)<br />
Beta blockers<br />
Antidepressants<br />
Antipsychotics<br />
Dextromethorphan<br />
Codeine<br />
Debrisoquine<br />
CYP2D6* CYP2C19*<br />
CYP2E1<br />
CYP1A2<br />
CYP2B6*<br />
CYP3A4/5/7<br />
Cyclosporin<br />
Taxol<br />
Tamoxifen<br />
Tacrolimus<br />
Amprenavir<br />
Amiodarone<br />
Cerivast<strong>at</strong>in<br />
Erythromycin<br />
Methadone<br />
Quinine<br />
CYP2C9*<br />
Tolbutamide<br />
Warfarin<br />
Phenytoin<br />
NSAID<br />
Diazepam<br />
Citalopram<br />
Anti ulcer drugs<br />
Clozapine<br />
Ropivacaine<br />
Efavirenz<br />
Cyclophosphamide<br />
40 % of the phase I<br />
metabolism is carried out<br />
by polymorphic P450s<br />
(enzymes in Italics)
BIOM/PHAR 255 Winter 2013 Halpert - Jan. 17, 2013<br />
Consequences of genetically impaired<br />
metabolism (similar to chemical inhibition)<br />
•When drug is inactiv<strong>at</strong>ed by<br />
metabolism: Higher blood levels<br />
= increased therapeutic effect<br />
<strong>and</strong> risk for side effects.<br />
•When drug is activ<strong>at</strong>ed by<br />
metabolism: Higher blood levels<br />
of unchanged prodrug <strong>and</strong> lower<br />
levels of active metabolite =<br />
decreased therapeutic effect.<br />
Single dose<br />
Poor metabolizer<br />
(PM)<br />
Time<br />
Mult iple dosage<br />
PM, t 1 / 2 = 2 4 h<br />
Cm ean = 2 8 m / L<br />
EM, t1/ 2 = 6 h<br />
C mean = 7 .5<br />
mg/ L<br />
Time<br />
Extensive<br />
m e t aboliz e r<br />
(EM)<br />
Molecular Mechanisms th<strong>at</strong> Alter CYP Function<br />
Log (plasma conc.)<br />
TiPS, 20: 342, 1999<br />
14 of 22<br />
Gene Dosage Effect (similar to induction)<br />
Nortriptyline<br />
antidepressant<br />
CYP2D6 genes<br />
Major P450 Alleles<br />
10-hydroxynortriptyline<br />
TiPS, 20: 342, 1999<br />
TiPS, 20: 342, 1999
BIOM/PHAR 255 Winter 2013 Halpert - Jan. 17, 2013<br />
Most Clinically Relevant CYP<br />
Polymorphisms (2C9, 2C19. 2D6)<br />
Ingelman-Sundberg, M. (2004) TIPS 25: 193-200<br />
Metabolic Activ<strong>at</strong>ion of Ticlopidine<br />
<strong>and</strong> Clopidogrel<br />
Metabolic activ<strong>at</strong>ion of ticlopidine, 1a, <strong>and</strong> clopidogrel, 1b, into their pharmacologically active thiol<br />
deriv<strong>at</strong>ives 3a (5) <strong>and</strong> 3b (6). Metabolite 3b was identified after trapping with acrylonitrile leading to<br />
3′b (6).<br />
Published in: P<strong>at</strong>rick M. Dansette; Julie Libraire; Gildas Bertho; Daniel Mansuy; Chem. Res. Toxicol. 2009, 22, 369-373.<br />
DOI: 10.1021/tx8004828<br />
Copyright © 2009 American Chemical Society<br />
15 of 22<br />
S-mephenytoin<br />
hexobarbital<br />
R-mephobarbital<br />
phenytoin<br />
diazepam<br />
citalopram<br />
omeprazole<br />
lansoprazole<br />
pantoprazole<br />
CYP2C19 Substr<strong>at</strong>es<br />
R-warfarin (8-OH)<br />
propranolol (in part)<br />
imipramine<br />
clomipramine<br />
amitryptylline<br />
proguanil<br />
teniposide<br />
nilutamide<br />
indomethacin<br />
moclobemide<br />
Human Cytochromes P450 Involved in the Oxid<strong>at</strong>ion<br />
of Clopidogrel<br />
CYP2C19 contributes substantially to both oxid<strong>at</strong>ion steps required to<br />
form the active metabolite of clopidogrel. Kazui, M. et al., <strong>Drug</strong> Metab<br />
Dispos. 38:92-9. 2010.
BIOM/PHAR 255 Winter 2013 Halpert - Jan. 17, 2013<br />
Rel<strong>at</strong>ionship between CYP2C19 Genetic Classific<strong>at</strong>ion <strong>and</strong><br />
Pharmacokinetic <strong>and</strong> Pharmacodynamic Responses after the<br />
Rel<strong>at</strong>ionship between CYP2C19 Genetic Classific<strong>at</strong>ion <strong>and</strong> Pharmacokinetic <strong>and</strong><br />
Pharmacodynamic Responses after the Administr<strong>at</strong>ion of Loading <strong>and</strong> Maintenance Doses of<br />
Administr<strong>at</strong>ion of Loading <strong>and</strong> Maintenance Doses of<br />
Clopidogrel in Healthy Subjects<br />
Clopidogrel in Healthy Subjects<br />
Mega JL et al. N Engl J Med 2009;360:354-362<br />
Carriers of a reduced-function CYP2C19 allele had lower levels of active metabolite form<strong>at</strong>ion,<br />
diminished pl<strong>at</strong>elet inhibition, <strong>and</strong> higher risk of major adverse cardiovascular effects.<br />
Role of Genetics in Codeine Metabolism<br />
1. Codeine to norcodeine <strong>and</strong><br />
codeine 6G accounts for 80%<br />
of the metabolism<br />
2. Conversion of codeine to<br />
morphine by CYP2D6 accounts<br />
for 10% of the metabolism<br />
3. Fast CYP2D6 metabolizers will<br />
accumul<strong>at</strong>e excess morphine<br />
4. Morphine <strong>and</strong> morphine 6G<br />
have opioid activity<br />
Gashe Y. et al. N. Engl. J. Med 2005<br />
16 of 22<br />
Conversion of an active drug to an<br />
active metabolite<br />
CYP2D6<br />
Codeine<br />
CYP3A4<br />
<strong>Drug</strong> metabolizing systems<br />
Evans, W.E. (1999). Science 286:487-491.
BIOM/PHAR 255 Winter 2013 Halpert - Jan. 17, 2013<br />
Conjug<strong>at</strong>ing Enzymes<br />
A comparison of the major conjug<strong>at</strong>ion<br />
p<strong>at</strong>hways<br />
Reaction Cosubstr<strong>at</strong>e Functional Groups Capacity<br />
Glucuronid<strong>at</strong>ion UDP-glucuronic acid -OH, -COOH, -NH 2,<br />
-SH, -NR 2, -R 3C-H<br />
Sulf<strong>at</strong>ion 3´-phosphoadeno sine-5´phosphosulf<strong>at</strong>e<br />
(PAPS)<br />
-OH, -NH 2<br />
High<br />
Acetyl<strong>at</strong>ion Acetyl-CoA -OH, -NH 2 Variable<br />
Glut<strong>at</strong>hione<br />
conjug<strong>at</strong>ion<br />
Amino acid<br />
conjug<strong>at</strong>ion<br />
Low<br />
Glut<strong>at</strong>hione Electrophiles Low<br />
Amino acids -COOH Medium<br />
Methyl<strong>at</strong>ion S-adenosylmethionine -OH, -NH 2<br />
17 of 22<br />
Properties of Phase II Enzymes<br />
• C<strong>at</strong>alyze biosynthetic reactions<br />
• Utilize a high-energy co-factor<br />
• Generally react with nucleophilic groups (OH<br />
<strong>and</strong> NH2 most common)<br />
• Generally lead to increase in w<strong>at</strong>er solubility<br />
Notable exceptions:<br />
• Glut<strong>at</strong>hione reacts with electrophiles<br />
• Acetyl<strong>at</strong>ion leads to decreased w<strong>at</strong>er solubility<br />
Cofactors Utilized in Phase 2 Reactions<br />
UDP-glucuronic acid<br />
Glut<strong>at</strong>hione<br />
N<br />
H<br />
COOH<br />
H<br />
OH<br />
O<br />
H<br />
H<br />
OH<br />
O UDP<br />
H OH<br />
Phosphoadenosine-<br />
Phosphosulf<strong>at</strong>e (PAPS)<br />
N<br />
H 2<br />
N<br />
N<br />
N<br />
O-<br />
CH2O P<br />
OH<br />
O<br />
P<br />
O<br />
O SO 3 -<br />
C<br />
H 3<br />
N<br />
H 2<br />
N<br />
N<br />
C<br />
N<br />
H 2<br />
CH 2 CH 2 CO NH CH<br />
H 2 C<br />
SH<br />
Acetyl-CoA<br />
CH 2 NH CH 2 COOH<br />
N<br />
OH OH<br />
N<br />
CH2O P O P O<br />
O<br />
O O<br />
CH3 OH<br />
CH2 CH<br />
H3C CO NH CH2 CH2 S<br />
O<br />
C<br />
OH O PO3H2 S-adenosyl-methionine<br />
N<br />
NH 2<br />
N<br />
N<br />
N<br />
CH2 OH HO<br />
O<br />
S +<br />
CH 3<br />
CH 2 CH 2 CH 2 COOH<br />
CH 3
BIOM/PHAR 255 Winter 2013 Halpert - Jan. 17, 2013<br />
Properties of UGTs<br />
• Normally detoxifying, but can be involved in bioactiv<strong>at</strong>ion<br />
• Glucuronides excreted in bile or urine<br />
– Smaller glucuronides excreted in urine<br />
– Larger glucuronides excreted in bile (undergo enterohep<strong>at</strong>ic<br />
circul<strong>at</strong>ion)<br />
• Genetic defect in UGT1A1 leads to hyperbilirubinemia<br />
diseases<br />
• Glucuronid<strong>at</strong>ion can be impaired when cofactor is<br />
depleted (e.g fasting)<br />
18 of 22<br />
OH<br />
OCH 2 CHCH 2 NHCH(CH 3 ) 2<br />
Propanolol<br />
(Alkylhydroxy-glucuronide)<br />
N<br />
CH 2 CH 2 CH 2 N<br />
Imipramine<br />
(Qu<strong>at</strong>ernary-glucuronide)<br />
Examples: UGT Substr<strong>at</strong>es<br />
(CH 3 ) 2<br />
HO<br />
O<br />
Morphine<br />
OH<br />
H 2 N<br />
N<br />
N<br />
CH3 N-Hydroxy-PhIP<br />
(N-glucuronide)<br />
N<br />
Benzidine<br />
(Arylamine-glucuronide)<br />
A single gene encodes multiple UGTs with differing<br />
substr<strong>at</strong>e preferences<br />
(Ritter et al, 1992)<br />
Each isoform of UGT1 results from differential splicing of<br />
exon1s (N-terminal 287 AA) to common exons 2-5 (245 AA).<br />
1A12<br />
1A10 1A8 1A6 1A4 1A2 2 3 4 5<br />
1A11 1A9 1A7 1A5 1A3 1A1<br />
pseudogene<br />
H<br />
OH<br />
NH 2<br />
UGT1A
BIOM/PHAR 255 Winter 2013 Halpert - Jan. 17, 2013<br />
Sulfotransferases<br />
(sulf<strong>at</strong>e ester form<strong>at</strong>ion)<br />
The reaction<br />
PAPS + R-OH<br />
sulfotransferases<br />
-----------------> R-OSO -<br />
3 + ADP<br />
UGT1A1<br />
ONLY<br />
Synthesis of PAPS<br />
SO 2-<br />
4 + ATP<br />
ATP sulfurylase<br />
-----------------> Adenosine 5'-phosphosulf<strong>at</strong>e (APS) + PPi<br />
APS kinase<br />
APS + ATP -----------------> 3'-phosophoadenosine- 5'-phosphosulf<strong>at</strong>e<br />
(PAPS) + ATP<br />
NHCOCH 3<br />
NHCOCH 3<br />
+ 3'-phosphoadenosine-<br />
5'-phosphosulf<strong>at</strong>e<br />
(PAPS)<br />
sulfotransferase<br />
+ PAP<br />
OH<br />
-<br />
OSO 3<br />
acetaminophen acetaminophen sulf<strong>at</strong>e<br />
19 of 22<br />
Reduced levels of conjug<strong>at</strong>ed bilirubin<br />
Sulfotransferases <strong>and</strong> sulfon<strong>at</strong>ion<br />
reactions<br />
• PAPS concentr<strong>at</strong>ions in cells are rel<strong>at</strong>ively low: highaffinity,<br />
low-capacity system<br />
– e.g. acetaminophen is mainly sulf<strong>at</strong>ed <strong>at</strong> low<br />
concentr<strong>at</strong>ions, mainly glucuronid<strong>at</strong>ed <strong>at</strong> high<br />
concentr<strong>at</strong>ions<br />
• Nucleophilic <strong>at</strong>tack of substr<strong>at</strong>e on electrophilic sulfur of<br />
PAPS<br />
• Substr<strong>at</strong>es include<br />
– -OH groups: alcohols, phenols, c<strong>at</strong>echols<br />
–NH 2 groups <strong>and</strong> N-oxides
BIOM/PHAR 255 Winter 2013 Halpert - Jan. 17, 2013<br />
Human cytosolic sulfotransferases<br />
SULT Substr<strong>at</strong>es Remarks<br />
1A1<br />
1A2<br />
simple phenols, Minoxidil,<br />
acetaminophen, N-OHPhIP<br />
N-OH-AAF, simple phenols<br />
Most abundant 1A form in liver<br />
Only found in humans. Protein may not be<br />
expressed.<br />
1A3 Dopamine, other c<strong>at</strong>echolamines Low in liver, high in intestine, placenta<br />
1A4<br />
1B1<br />
C<strong>at</strong>echolamines<br />
Thyroid hormones Liver, intestine, leukocytes<br />
1C2 N-OH-AAF, simple phenols<br />
1C4 N-OH-AAF, simple phenols Highest in fetal liver, kidney<br />
Highest in fetal liver, kidney<br />
1E1 estrogens Liver, intestine, secretory endometrium<br />
Inhibited by PCB metabolites<br />
2A1 Steroids, DHEA, hydroxymethyl<br />
PAHs<br />
Liver, intestine, steroidogenic organs<br />
2B1 Steroids, cholesterol<br />
2 variants with altern<strong>at</strong>ive exons 1<br />
4A1 ?<br />
2 variants. High in brain<br />
N-Acetyl Transferase<br />
• Significant route of biotransform<strong>at</strong>ion<br />
• Two enzymes in humans<br />
NAT1-most tissues, abundant in bladder<br />
NAT2-primarily in liver<br />
Arom<strong>at</strong>ic - R-NH 2<br />
Hydrazines R-NH-NH 2<br />
CoA-S-COCH 3<br />
Arom<strong>at</strong>ic - R-NH-COCH 3<br />
Hydrazines R-NH-NH 2-COCH 3<br />
NAT2 – approxim<strong>at</strong>ely 50% slow acetyl<strong>at</strong>ors in US<br />
Leads to increased side effects of isoniazid,<br />
sulfonamides, procainamide, <strong>and</strong> hydralazine.<br />
20 of 22<br />
N-acetyltransferases<br />
CH 3<br />
N<br />
COO -<br />
CO NH NH 2<br />
H 2N S NH 2<br />
sulfanilamide<br />
O<br />
CoA-S-acetyltransferase<br />
+ CoASH CH3 C<br />
O<br />
O<br />
N-acetyltransferase<br />
H 3 C<br />
O<br />
C<br />
CO NH NH C<br />
N<br />
O<br />
O<br />
S CoA<br />
CH 3<br />
N S NH 2<br />
H<br />
Less w<strong>at</strong>er soluble<br />
Glut<strong>at</strong>hione conjug<strong>at</strong>ion<br />
• Enzym<strong>at</strong>ic <strong>and</strong> nonenzym<strong>at</strong>ic reactions<br />
• Crucial role in cellular protection from electrophilic, oxidizing xenobiotics<br />
<strong>and</strong> their metabolites<br />
e.g. epoxides<br />
• Glut<strong>at</strong>hione S-transferases c<strong>at</strong>alyze both substitution <strong>and</strong> addition reactions<br />
on electrophilic substr<strong>at</strong>es<br />
• [GSH] is usually very high in cells-10 mM range<br />
Substitution<br />
Addition<br />
Cl<br />
NO 2<br />
+<br />
γ-Glu-Cys-Gly<br />
glut<strong>at</strong>hione (GSH)<br />
NO2 2,4-dinitro-1-chlorobenzene<br />
O<br />
CH2 CH2 +<br />
γ-Glu-Cys-Gly<br />
glut<strong>at</strong>hione (GSH)<br />
Glut<strong>at</strong>hione<br />
S-transferase<br />
Glut<strong>at</strong>hione<br />
S-transferase<br />
NO 2<br />
O<br />
S glut<strong>at</strong>hione<br />
NO2 OH<br />
CH CH2 SG
BIOM/PHAR 255 Winter 2013 Halpert - Jan. 17, 2013<br />
Properties of Glut<strong>at</strong>hione S-Transferases<br />
• Cytosolic GSTs: Homo- <strong>and</strong> heterodimers of <strong>at</strong> least 15 subunits<br />
– Alpha family: hGSTA1-5 (main forms in liver <strong>and</strong> kidney)<br />
– Pi family: hGSTP1a,1b (allelic variants: lung, gut, tumors)<br />
– Mu family: hGSTM1-5 (muscle, brain)<br />
– Theta family: hGSTT1-2<br />
– Single members of sigma <strong>and</strong> zeta families in humans<br />
• Microsomal GST - membrane associ<strong>at</strong>ed proteins in eicosanoid <strong>and</strong><br />
glut<strong>at</strong>hione metabolism (MAPEG) -<br />
• Mitochondrial GST - hGSTK1 (soluble)<br />
• Widespread tissue distribution<br />
• Some GSTs have nonc<strong>at</strong>alytic binding sites for hydrophobic lig<strong>and</strong>s:<br />
involved in intracellular transport<br />
• Differential regul<strong>at</strong>ion of GSTs<br />
– Chemicals<br />
– Sex differences, development<br />
– Increased expression in tumors - drug resistance<br />
Routes of Elimin<strong>at</strong>ion of the Top 200 Prescribed<br />
<strong>Drug</strong>s in 2002 (Wienkers <strong>and</strong> He<strong>at</strong>h, 2005)<br />
Other Conjug<strong>at</strong>ion P<strong>at</strong>hways<br />
Amino acid conjug<strong>at</strong>ion<br />
COOH<br />
+ ATP<br />
CoASH<br />
CO S CoA<br />
N-acetyltransferase<br />
+ NH 2 -CH 2 -COOH<br />
benzoic acid benzoyl-CoA glycine hippuric acid<br />
Methyl<strong>at</strong>ion<br />
+ S-adenosylmethionine<br />
methyltransferase<br />
N H<br />
(CH2 ) 2 N<br />
CH3 desmethylimipramine<br />
N CH3 (CH2 ) 2 N<br />
CH3 imipramine<br />
Ingelman-Sundberg, M., J Int Med 250: 186-200, 2001,<br />
21 of 22<br />
Interindividual differences in drug action<br />
CO NHCH 2 COOH<br />
+<br />
+ CoASH<br />
S-adenosylhomocysteine
BIOM/PHAR 255 Winter 2013 Halpert - Jan. 17, 2013<br />
Clinically significant drug interactions due to<br />
inhibition of Phase II enzymes are rel<strong>at</strong>ively rare<br />
because:<br />
• N-acetyl<strong>at</strong>ion <strong>and</strong> sulf<strong>at</strong>ion represent the primary<br />
clearance mechanism for few drugs.<br />
• UGTs are the primary clearance mechanism for<br />