S3-Guideline “Exocrine Pancreatic Carcinoma” 20071 ... - DGVS
S3-Guideline “Exocrine Pancreatic Carcinoma” 20071 ... - DGVS
S3-Guideline “Exocrine Pancreatic Carcinoma” 20071 ... - DGVS
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
458<br />
Leitlinie<br />
of these results is not known. Therefore, this type of monitoring<br />
should only be done under study conditions [86 – 88, 104].<br />
Chronic pancreatitis<br />
Patients with many years of chronic pancreatitis have an increased<br />
risk of developing pancreatic carcinoma.<br />
Evidence level 2b, strong consensus<br />
Comments<br />
The data on the relative risk are heterogeneous and vary from<br />
2.3 to 18.5. The cumulative incidence is reported to be 1.1% after<br />
5 years, 1.8% after 10 years, and 4% after 20 years [105 – 109].<br />
Type 2 diabetes mellitus<br />
Patients with type 2 diabetes mellitus have an increased risk for<br />
pancreatic carcinoma.<br />
Evidence level 2b, consensus<br />
Comments<br />
About 1% of diabetics age 50 years and younger develop pancreatic<br />
carcinoma in the following 3 years. That is equal to an<br />
about 8-fold higher risk [110]. Further studies show a risk that<br />
is lower [50, 111 – 118]. It must be taken into account that diabetes<br />
can be caused by pancreatic carcinoma [119, 120].<br />
Recommendation on genetic consultation<br />
The genetic consultation of patients with genetic syndromes and<br />
their relatives is performed according to the directives of the German<br />
Medical Association.<br />
Recommendation grade: A, consensus<br />
Topic 2:<br />
Diagnostics<br />
!<br />
Diagnostics in case of newly occurring symptoms<br />
Recommendation<br />
Newly occurring pain in the epigastric region and back should<br />
result in tests for diagnosing pancreatic carcinoma.<br />
Recommendation grade: C, evidence level 3, strong consensus<br />
Comments<br />
In general, newly occurring pain in the epigastric region or<br />
back which could be caused by pancreatitis or pancreatic carcinoma<br />
mandate further diagnostics. No literature is available<br />
that states for which symptoms alone or in combination and<br />
from which age pancreatic carcinoma should be considered.<br />
The diagnostics alone or in combination that are necessary to<br />
exclude pancreatic tumors have also not been reported. Newly<br />
occurring back pain alone which cannot be explained by alterations<br />
of the musculoskeletal system should not result in<br />
testing for pancreatic carcinoma.<br />
l " Table 8 suggests an age and suspicion level adapted procedure<br />
which is based on expert opinion.<br />
Recommendation<br />
A newly occurring or manifest type 2 diabetes mellitus with no further<br />
pancreatic carcinoma symptoms should not lead to pancreatic<br />
carcinoma diagnostic testing.<br />
Recommendation grade: B, evidence level 2b, consensus<br />
Adler G et al. <strong>S3</strong>-<strong>Guideline</strong> <strong>“Exocrine</strong> <strong>Pancreatic</strong>… Z Gastroenterol 2008; 46: 449–482<br />
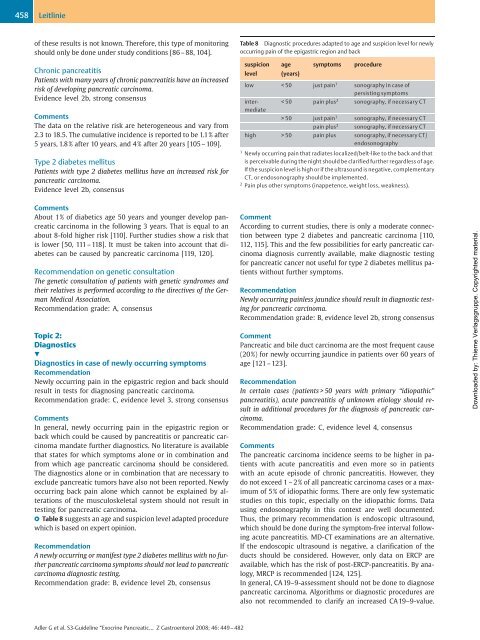
Table 8 Diagnostic procedures adapted to age and suspicion level for newly<br />
occurring pain of the epigastric region and back<br />
suspicion<br />
level<br />
age<br />
(years)<br />
symptoms procedure<br />
low < 50 just pain1 sonography in case of<br />
persisting symptoms<br />
intermediate<br />
50 justpain1 sonography, if necessary CT<br />
pain plus2 sonography, if necessary CT<br />
high > 50 pain plus sonography, if necessary CT/<br />
endosonography<br />
1 Newly occurring pain that radiates localized/belt-like to the back and that<br />
is perceivable during the night should be clarified further regardless of age.<br />
If the suspicion level is high or if the ultrasound is negative, complementary<br />
CT, or endosonography should be implemented.<br />
2 Pain plus other symptoms (inappetence, weight loss, weakness).<br />
Comment<br />
According to current studies, there is only a moderate connection<br />
between type 2 diabetes and pancreatic carcinoma [110,<br />
112, 115]. This and the few possibilities for early pancreatic carcinoma<br />
diagnosis currently available, make diagnostic testing<br />
for pancreatic cancer not useful for type 2 diabetes mellitus patients<br />
without further symptoms.<br />
Recommendation<br />
Newly occurring painless jaundice should result in diagnostic testing<br />
for pancreatic carcinoma.<br />
Recommendation grade: B, evidence level 2b, strong consensus<br />
Comment<br />
<strong>Pancreatic</strong> and bile duct carcinoma are the most frequent cause<br />
(20%) for newly occurring jaundice in patients over 60 years of<br />
age [121 –123].<br />
Recommendation<br />
In certain cases (patients > 50 years with primary “idiopathic”<br />
pancreatitis), acute pancreatitis of unknown etiology should result<br />
in additional procedures for the diagnosis of pancreatic carcinoma.<br />
Recommendation grade: C, evidence level 4, consensus<br />
Comments<br />
The pancreatic carcinoma incidence seems to be higher in patients<br />
with acute pancreatitis and even more so in patients<br />
with an acute episode of chronic pancreatitis. However, they<br />
do not exceed 1 – 2% of all pancreatic carcinoma cases or a maximum<br />
of 5% of idiopathic forms. There are only few systematic<br />
studies on this topic, especially on the idiopathic forms. Data<br />
using endosonography in this context are well documented.<br />
Thus, the primary recommendation is endoscopic ultrasound,<br />
which should be done during the symptom-free interval following<br />
acute pancreatitis. MD-CT examinations are an alternative.<br />
If the endoscopic ultrasound is negative, a clarification of the<br />
ducts should be considered. However, only data on ERCP are<br />
available, which has the risk of post-ERCP-pancreatitis. By analogy,<br />
MRCP is recommended [124, 125].<br />
In general, CA 19–9-assessment should not be done to diagnose<br />
pancreatic carcinoma. Algorithms or diagnostic procedures are<br />
also not recommended to clarify an increased CA 19–9-value.<br />
Downloaded by: Thieme Verlagsgruppe. Copyrighted material.