Prostate Cancer – Staging/restaging case study - Cardinal Health
Prostate Cancer – Staging/restaging case study - Cardinal Health
Prostate Cancer – Staging/restaging case study - Cardinal Health
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
<strong>Prostate</strong> <strong>Cancer</strong> <strong>–</strong> <strong>Staging</strong>/<strong>restaging</strong><br />
<strong>case</strong> <strong>study</strong><br />
Positron Emission Tomography (PET)<br />
50-year-old male with history of <strong>Prostate</strong> <strong>Cancer</strong><br />
Patient history<br />
••This patient was diagnosed two years ago with<br />
prostate cancer, Gleason 9, <strong>Prostate</strong>-Specific<br />
Antigen (PSA) 7.4. He received radiation therapy,<br />
Zometa and Zoladex.<br />
••PSA fell to < 0.1. In the last seven months his<br />
PSA climbed to 1.1 and he was referred to stage<br />
presumed recurrence. MRI was negative.<br />
Clinical question<br />
Can PET/CT be helpful in identifying metastatic<br />
disease in this patient?<br />
The patient’s physician and the patient considered<br />
options; including, ultrasound, CT, Prostascint,<br />
superparamagnetic nanoparticle investigative<br />
imaging, C-11 acetate, F-18 fluorocholine, and<br />
F-18 FDG PET/CT. The decision was made to<br />
begin with FDG-PET.<br />
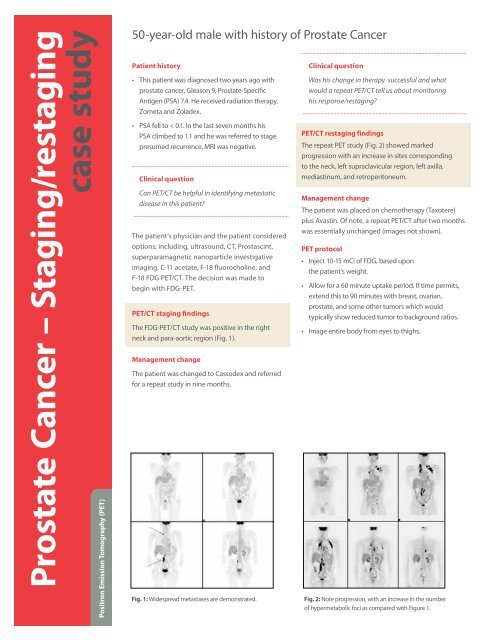
PET/CT staging findings<br />
The FDG-PET/CT <strong>study</strong> was positive in the right<br />
neck and para-aortic region (Fig. 1).<br />
Management change<br />
The patient was changed to Cassodex and referred<br />
for a repeat <strong>study</strong> in nine months.<br />
Fig. 1: Widespread metastases are demonstrated.<br />
Clinical question<br />
Was his change in therapy successful and what<br />
would a repeat PET/CT tell us about monitoring<br />
his response/<strong>restaging</strong>?<br />
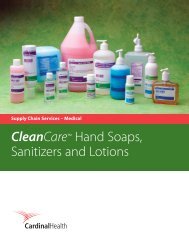
PET/CT <strong>restaging</strong> findings<br />
The repeat PET <strong>study</strong> (Fig. 2) showed marked<br />
progression with an increase in sites corresponding<br />
to the neck, left supraclavicular region, left axilla,<br />
mediastinum, and retroperitoneum.<br />
Management change<br />
The patient was placed on chemotherapy (Taxotere)<br />
plus Avastin. Of note, a repeat PET/CT after two months<br />
was essentially unchanged (images not shown).<br />
PET protocol<br />
••Inject 10-15 mCi of FDG, based upon<br />
the patient’s weight.<br />
••Allow for a 60 minute uptake period. If time permits,<br />
extend this to 90 minutes with breast, ovarian,<br />
prostate, and some other tumors which would<br />
typically show reduced tumor to background ratios.<br />
••Image entire body from eyes to thighs.<br />
Fig. 2: Note progression, with an increase in the number<br />
of hypermetabolic foci as compared with Figure 1.
<strong>Prostate</strong> <strong>Cancer</strong> <strong>–</strong> <strong>Staging</strong>/<strong>restaging</strong><br />
Positron Emission Tomography (PET) is a non-invasive diagnostic imaging procedure<br />
that can provide unique information for accurate TNM staging. Many cancers exhibit<br />
increased glucose metabolic rates which can be identified with PET via the radiopharmaceutical<br />
18F-FDG. Since changes in glucose metabolism often occur before<br />
changes in anatomy (e.g. tumor growth), PET can often identify the presence of disease<br />
earlier than other anatomic imaging techniques. Early disease identification is particularly<br />
critical during the assessment of nodal involvement or the determination of the presence<br />
of metabolic disease.<br />
Prior studies and experience have convinced us that PET has a limited role in the<br />
evaluation of men with prostate cancer. However, most physicians involved with<br />
PET can point to selected <strong>case</strong>s of positive (and valuable) studies.<br />
The National Oncologic PET Registry (NOPR) was created to evaluate the efficacy<br />
and potential applicability of PET in tumors not previously covered by CMS. It began<br />
registering patients on May 8, 2006. Through February 1, 2007, of the top 10 NOPR <strong>Cancer</strong><br />
Sites, prostate was number one. Of the top 10 NOPR <strong>Cancer</strong> Site and Indications, prostate<br />
initial staging, prostate <strong>restaging</strong>, and prostate recurrence were ranked numbers two,<br />
three and four, respectively. This widespread interest in PET and prostate cancer is at least<br />
in part due to the high incidence of this disease (from birth to death, one in six men will<br />
develop prostate cancer), and the suboptimal performance of other imaging modalities.<br />
Anecdotal experience suggests that PET is most helpful in men with high Gleason scores<br />
and/or rapid PSA doubling times.<br />
<strong>Prostate</strong> <strong>Cancer</strong> <strong>–</strong> <strong>Staging</strong><br />
Sensitivity 57%<br />
Specificity Close to 100%<br />
References:<br />
Gambhir SS, Czernin J, Schwimmer J, et al: A tabulated summary of the FDG PET literature.<br />
J Nucl Med 2001, 42;: 53s-55s.<br />
Case <strong>study</strong> courtesy of Dr. Michael Kipper — Pacific Imaging and Treatment Center,<br />
San Diego, California<br />
© 2010 <strong>Cardinal</strong> <strong>Health</strong>. All rights reserved. CARDINAL HEALTH, the <strong>Cardinal</strong> <strong>Health</strong> LOGO<br />
and Essential to care are trademarks or registered trademarks of <strong>Cardinal</strong> <strong>Health</strong>.<br />
All other marks are the property of their respective owners. Lit. No. 7PET5802 (11/2010)<br />
“In selected <strong>case</strong>s I have found<br />
FDG-PET to be of great value in<br />
identifying metastatic prostate<br />
cancer and allowing me to<br />
follow my patient with imaging<br />
as well as <strong>Prostate</strong>-Specific<br />
Antigen (PSA) measurement”.<br />
— Dr. David Bodkin,<br />
Oncologist, San Diego, California<br />
cardinalhealth.com/nps