Do Not Attempt Resuscitation (DNAR) Policy - Dudley Primary Care ...
Do Not Attempt Resuscitation (DNAR) Policy - Dudley Primary Care ...
Do Not Attempt Resuscitation (DNAR) Policy - Dudley Primary Care ...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
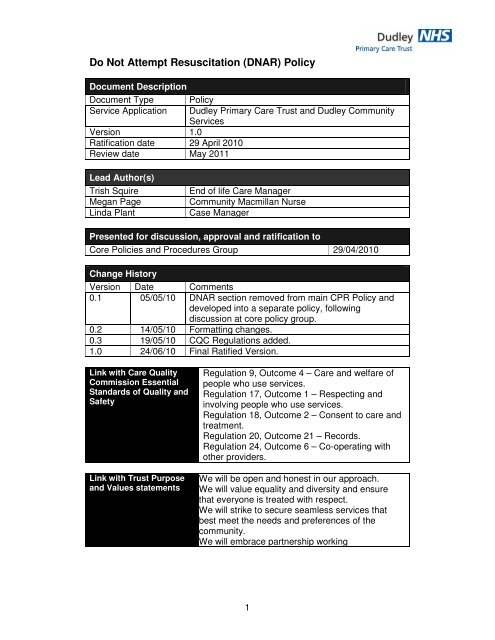
<strong>Do</strong> <strong>Not</strong> <strong>Attempt</strong> <strong>Resuscitation</strong> (<strong>DNAR</strong>) <strong>Policy</strong><br />
<strong>Do</strong>cument Description<br />
<strong>Do</strong>cument Type <strong>Policy</strong><br />
Service Application <strong>Dudley</strong> <strong>Primary</strong> <strong>Care</strong> Trust and <strong>Dudley</strong> Community<br />
Services<br />
Version 1.0<br />
Ratification date 29 April 2010<br />
Review date May 2011<br />
Lead Author(s)<br />
Trish Squire End of life <strong>Care</strong> Manager<br />
Megan Page Community Macmillan Nurse<br />
Linda Plant Case Manager<br />
Presented for discussion, approval and ratification to<br />
Core Policies and Procedures Group 29/04/2010<br />
Change History<br />
Version Date Comments<br />
0.1 05/05/10 <strong>DNAR</strong> section removed from main CPR <strong>Policy</strong> and<br />
developed into a separate policy, following<br />
discussion at core policy group.<br />
0.2 14/05/10 Formatting changes.<br />
0.3 19/05/10 CQC Regulations added.<br />
1.0 24/06/10 Final Ratified Version.<br />
Link with <strong>Care</strong> Quality<br />
Commission Essential<br />
Standards of Quality and<br />
Safety<br />
Link with Trust Purpose<br />
and Values statements<br />
Regulation 9, Outcome 4 – <strong>Care</strong> and welfare of<br />
people who use services.<br />
Regulation 17, Outcome 1 – Respecting and<br />
involving people who use services.<br />
Regulation 18, Outcome 2 – Consent to care and<br />
treatment.<br />
Regulation 20, Outcome 21 – Records.<br />
Regulation 24, Outcome 6 – Co-operating with<br />
other providers.<br />
We will be open and honest in our approach.<br />
We will value equality and diversity and ensure<br />
that everyone is treated with respect.<br />
We will strike to secure seamless services that<br />
best meet the needs and preferences of the<br />
community.<br />
We will embrace partnership working<br />
1
Summary Sheet<br />
Every patient has the right to die in peace and with dignity and there will<br />
inevitably be cases where resuscitation following cardio-respiratory arrest<br />
cannot be justified on medical or quality of life grounds, as being in the<br />
patient's interests.<br />
It may also be against the clearly stated wishes of the patient to prolong what<br />
the patient sees as a poor quality of life by attempting Cardio-Pulmonary<br />
<strong>Resuscitation</strong> (CPR).<br />
Such cases should be clearly identified and all staff involved in the patient’s<br />
care should be made aware of the action to take in the event of cardiorespiratory<br />
arrest.<br />
The aim of this <strong>Policy</strong> is to:-<br />
• Ensure that clinicians understand the key ethical and legal issues that<br />
are used as a framework to inform decisions about CPR and when not<br />
to resuscitate a patient.<br />
• That clinicians clearly document these decisions using the required<br />
paperwork.<br />
• That these decisions are clearly and correctly communicated to all<br />
other providers and outside organisations that may be involved in the<br />
patient’s care.<br />
These guidelines do not address the complex legal, ethical and clinical issues<br />
that surround some cases and in this instance clinicians are advised to seek<br />
further guidance and support from senior management. This policy relates<br />
specifically to <strong>Do</strong> <strong>Not</strong> <strong>Attempt</strong> Cardio-Pulmonary <strong>Resuscitation</strong> and does not<br />
replace the existing <strong>Dudley</strong> CPR <strong>Policy</strong> (2009). Neither does it refer to other<br />
life sustaining treatments.<br />
This is a Trust wide policy for the attention of all clinicians and it is<br />
recommended it is read in conjunction with the following local and national<br />
documents:<br />
Decisions relating to cardio-pulmonary resuscitation. The revised joint<br />
statement from the British Medical Association, <strong>Resuscitation</strong> Council (UK)<br />
and the Royal College of Nursing (2007)<br />
<strong>Resuscitation</strong> – <strong>Do</strong> not resuscitate orders position statement. Nursing and<br />
Midwifery Council (2000)<br />
Withholding and withdrawing Life Sustaining Treatment- Guidance for doctors.<br />
Good Medical Practice (2006)<br />
End of Life <strong>Care</strong> Strategy (DH 2008)<br />
End of Life <strong>Care</strong> Pathway (West Midlands Clinical Pathway Group 2008)<br />
<strong>Dudley</strong> PCT Baseline Review of Services for End of Life <strong>Care</strong> (DH Operating<br />
Framework 2007/08)<br />
Advance <strong>Care</strong> Planning: A Guide for Health and Social <strong>Care</strong> Staff (NHS End<br />
2
of Life <strong>Care</strong> Programme 2007)<br />
End of life <strong>Care</strong> Programme (NHS) (2004-2007)<br />
Mental Capacity Act (2005)<br />
<strong>Dudley</strong> PCT Mental Capacity <strong>Policy</strong> (2008)<br />
Preferred Place of <strong>Care</strong> <strong>Do</strong>cument<br />
(www.endoflifecareforadults.nhs.uk/eolc/ppc.)<br />
Liverpool <strong>Care</strong> Pathway (www.mcpcil.org.uk)<br />
Gold Standards Framework (www.goldstandardsframework.nhs.uk)<br />
The <strong>DNAR</strong> <strong>Policy</strong> is subject to formal review after 1 year and every 2 years<br />
thereafter. The review will be undertaken by the End of Life <strong>Care</strong> Manager in<br />
consultation with the Specialist Palliative <strong>Care</strong> and End of Life <strong>Care</strong> Steering<br />
Group. A review of this guidance may occur at any time if it is deemed<br />
necessary by this group.<br />
This <strong>Policy</strong> was developed in consultation with the following:<br />
GP, Medical Director Mary Stevens Hospice<br />
<strong>Resuscitation</strong> Officer, <strong>Dudley</strong> Group of Hospitals<br />
End of Life Clinical Lead,, West Midlands Ambulance Service<br />
GP, PEC Chair<br />
Senior Solicitor, Mills & Reeve<br />
Macmillan Specialist Nurse<br />
District Nurse Out of Hours Manager<br />
Primecare Manager<br />
Associate Director of Governance<br />
3
Contents<br />
Pg No<br />
Introduction 5<br />
Scope 5<br />
Patients who wish to make a <strong>DNAR</strong> decision 5<br />
Guidelines for <strong>DNAR</strong> decisions 6<br />
<strong>Do</strong>cumentation of the decision 6<br />
Patient transfers 7<br />
Review of the <strong>DNAR</strong> decision 8<br />
Communication of the <strong>DNAR</strong> document 8<br />
Clinical and Professional conflict 9<br />
Summary 10<br />
References 10<br />
Appendix 1 DNACPR form 11-14<br />
4
Non-performance of Cardio-Pulmonary <strong>Resuscitation</strong><br />
Introduction<br />
The decision not to provide cardio-pulmonary resuscitation (CPR) to a patient<br />
should be made before the patient goes into cardiac arrest, ensuring the<br />
consideration of all relevant legal principles and be correctly communicated to<br />
all appropriate staff. A decision not to resuscitate can only be made by an<br />
appropriate Consultant/GP or by the patient if they are an adult and with<br />
mental capacity to make that decision. If a patient does not want to be<br />
resuscitated or medical doctor and/or nursing staff feel that resuscitation<br />
would be inappropriate the Consultant/GP responsible for that patient’s<br />
treatment should be informed immediately.<br />
Scope<br />
This policy applies to all clinicians working within <strong>Dudley</strong> community and<br />
primary care services and other organisations who deliver care to patients<br />
registered with a <strong>Dudley</strong> GP such as <strong>Dudley</strong> Group of Hospitals, Medical Out<br />
of Hours providers and <strong>Care</strong> Homes.<br />
1. Patients wishing to make an advance decision relating to <strong>Do</strong> <strong>Not</strong><br />
<strong>Attempt</strong> <strong>Resuscitation</strong> (<strong>DNAR</strong>)<br />
1.1 Healthcare professionals have an important role in helping patients<br />
participate in advance care planning and making appropriate plans for<br />
their future care in a sensitive but realistic manner, making it clear<br />
whether or not attempted CPR could be successful.<br />
1.2 A competent patient can make an Advance Decision to Refuse<br />
Treatment (ADRT) including life sustaining treatment such as CPR as<br />
outlined in the Mental Capacity Act (MCA) (2005). These legally binding<br />
decisions have to be made within the legal framework outlined within the<br />
MCA (2005) and recorded in the written format recommended within the<br />
Act. Health Professionals are bound to comply when the refusal<br />
specifically addresses the situation that has arisen. <strong>Resuscitation</strong> should<br />
not be attempted if CPR is contrary to the recorded, sustained wishes of<br />
an adult who was mentally competent and aware of the implications at<br />
the time of making that advance decision.<br />
1.3 In 2007 the British Medical Association, the Royal College of Nursing<br />
and the <strong>Resuscitation</strong> Council (UK) published a joint statement on<br />
decisions relating to CPR which considers these issues in more detail.<br />
Professionals should refer to that statement if they are approached by a<br />
patient to make an ADRT. Further information is also contained in the<br />
Mental Capacity Act in Practice: Guidance for End of Life <strong>Care</strong> (2008)<br />
published by the National Council for Palliative <strong>Care</strong> and the MCA<br />
(2005).<br />
NB Adults who lack capacity<br />
Patients over 16 years of age are presumed to have capacity to make<br />
decisions for themselves unless there is evidence to the contrary. Refer to the<br />
5
British Medical Association, the Royal College of Nursing and the<br />
<strong>Resuscitation</strong> Council (UK) 2007 for further guidance on this complex area<br />
and the MCA (2005) or <strong>Dudley</strong> MCA <strong>Policy</strong> (2008) for assessment of capacity<br />
guidelines and assessment tools.<br />
2. Guidelines for <strong>Do</strong> <strong>Not</strong> <strong>Attempt</strong> <strong>Resuscitation</strong> decisions<br />
2.1 The overall responsibility for a decision that a patient should have a<br />
<strong>DNAR</strong> order rests with the senior member of the Medical Team available<br />
(Consultant or GP) in charge of the patient’s care. This should be made<br />
after appropriate consultation and consideration of all aspects of the<br />
patient’s condition. It is important that Consultants, GP’s or Senior<br />
Nurses, etc. lead and counsel their junior staff during such decisionmaking.<br />
2.2 It is appropriate to consider a <strong>DNAR</strong> decision in the following<br />
circumstances:-<br />
• The likely clinical outcome, including the likelihood of successfully<br />
restarting the patient’s heart and breathing, and the overall benefit<br />
achieved from a successful resuscitation.<br />
• The patient’s known or ascertainable wishes.<br />
• The patient’s human rights, including the right to life and the right to<br />
be free from degrading treatment.<br />
2.3 A <strong>DNAR</strong> order applies solely to the treatment of cardio-pulmonary<br />
resuscitation in a cardiac or respiratory arrest. Other forms of treatment<br />
are not precluded and must not be influenced by a <strong>DNAR</strong> decision.<br />
2.4 Proper understanding of a <strong>DNAR</strong> order is impossible without knowing the<br />
rationale behind it. The reasons for any decision not to resuscitate,<br />
together with the discussion with the patient and/or relatives and/or<br />
friends, must be fully documented in the patient’s medical record and the<br />
senior member of the Medical Team or GP must ensure that the decision<br />
is effectively communicated to other members of staff. The decision not<br />
to resuscitate must then be clearly noted in the nursing care plan/ Single<br />
Assessment Process (SAP). A reasonable explanation as to why the<br />
decision has been made must be stated. It is not acceptable simply to<br />
record ‘<strong>Not</strong> For <strong>Resuscitation</strong>’.<br />
3. <strong>Do</strong>cumentation of the Decision<br />
3.1 Whilst national guidance suggests that a GP, Consultant OR Senior<br />
nurse may sign the <strong>DNAR</strong> form, <strong>Dudley</strong>’s <strong>Policy</strong> doesn’t support this. If<br />
the patient’s GP or Consultant is the first person signing then a second<br />
signature is not required. However if a senior nurse is the first signatory<br />
then the patient’s GP or Consultant must countersign the form as the<br />
second person signing.<br />
6
3.2 If there is disagreement between professionals or the patient or family<br />
members regarding the <strong>DNAR</strong> decision it would be best practice to have<br />
the document countersigned by another senior clinician who knows the<br />
patient.<br />
3.3 It is important that once the <strong>DNAR</strong> decision has been made that a<br />
recognised document is used. It is quite acceptable to use the National<br />
<strong>Resuscitation</strong> Council’s document, <strong>Dudley</strong> PCT’s own <strong>DNAR</strong> document<br />
or the new combined West Midlands Ambulance Service (WMAS) and<br />
<strong>Dudley</strong> <strong>DNAR</strong> form (see appendix 1).<br />
3.4 It is also important that once the <strong>DNAR</strong> decision has been made, that it<br />
is recorded in both the medical case notes and the nursing care plan. It<br />
is the responsibility of the nurse in attendance to transcribe the decision<br />
into the nursing notes.<br />
The only acceptable entry in the medical and nursing case notes will be: -<br />
‘<strong>Not</strong> For Cardio-Pulmonary <strong>Resuscitation</strong>’<br />
Or<br />
‘<strong>Do</strong> <strong>Not</strong> <strong>Attempt</strong> Cardio-Pulmonary <strong>Resuscitation</strong>’<br />
3.5 It is unacceptable practice to use abbreviations, codes or symbols to<br />
denote the patient’s resuscitation status. Such practice could lead to<br />
confusion or misunderstanding.<br />
3.6 The date of the decision must be recorded along with the next scheduled<br />
review date (if appropriate, see point 5.2).<br />
3.7 The patient’s known wishes must always be communicated when<br />
referred or discharged to another service.<br />
3.8 Health <strong>Care</strong> Teams will ensure that patients are treated with respect and<br />
dignity, and that every effort is made to avoid a “conspiracy” of silence,<br />
from the patient’s perspective, about his/her resuscitation status.<br />
NB If the new WMAS form is used then please follow the guidance notes for<br />
completion.<br />
4. Patient Transfers<br />
<strong>Do</strong>cumentation required when a patient who is designated <strong>Not</strong> for Cardio-<br />
Pulmonary <strong>Resuscitation</strong> and is being transferred across different care<br />
settings or a different provider. There are two sets of occasions when<br />
patients are being transferred and these will need to be dealt with differently.<br />
4.1 When the patient remains under the care of the Consultant / GP making<br />
the decision (transfer across sites).<br />
7
In this case the Consultant / GP must appropriately communicate to the<br />
staff concerned that the patient is not for resuscitation using the form in<br />
appendix 1.<br />
4.2. The patient has been discharged to the care of another Consultant or<br />
his/her GP.<br />
In this case it is necessary for the Consultant or GP to communicate all<br />
relevant clinical information, including that relating to non-resuscitation,<br />
to the doctor assuming the care of the patient. However, the Consultant<br />
or GP cannot issue a directive concerning the management of a patient<br />
who is no longer under his/her care. Only the responsible doctor can<br />
take this decision. The ambulance staff should receive guidance from<br />
the appropriate doctor when transporting a patient who is not to be<br />
resuscitated. Any communication with ambulance staff should be either<br />
written in patients single assessment process (SAP) folders or via<br />
ambulance control if alert is flagged on the patients address. This will<br />
ensure there is a permanent record of the instruction as all telephone<br />
conversations with ambulance control are recorded.<br />
5. Review of the Decision regarding Patient’s <strong>Resuscitation</strong> Status<br />
5.1 The Law does not prescribe the frequency with which reviews must be<br />
undertaken. Any order not to resuscitate however, should be reviewed<br />
regularly since the frequency or otherwise of the review will be produced<br />
in evidence in the course of litigation arising from this type of case.<br />
Therefore a review should be undertaken at least six monthly by the<br />
multi-disciplinary team, as the patient resuscitation status may change as<br />
a result of either a change in health or a change in legal status of the<br />
patient. Such changes must be recorded and communicated to all<br />
members of the health care team<br />
5.2 There will be situations where the decision will stand indefinitely and<br />
review may be unnecessary, i.e. terminal care for malignancy etc.<br />
<strong>Do</strong>cumentation in the notes for such scenarios must be clear,<br />
unambiguous and also documented in all patient notes.<br />
5.3 The clinician-in-charge has a duty to keep the medical staff informed of<br />
any changes in the patient’s condition and must do so particularly if<br />
he/she considers it likely that the patient’s resuscitation status could be<br />
affected.<br />
6. Communicating <strong>Do</strong> <strong>Not</strong> <strong>Attempt</strong> <strong>Resuscitation</strong> Decisions Made<br />
6.1 Assuming that the decision has been made following the above<br />
guidelines and documented accordingly, it is the senior medical or<br />
nursing professional’s responsibility to ensure that it is readily accessible<br />
to all health professionals who may need to know it, including hospital<br />
staff, GPs, deputising services, Out of Hours services and ambulance<br />
staff.<br />
8
Please note that there are now two new forms (appendix 1) to document<br />
and transfer the information across to Out Of Hours providers and West<br />
Midlands Ambulance Service (WMAS).<br />
6.2 Part one of the form is the <strong>DNAR</strong> document and may replace the<br />
organisations existing form. However if a <strong>DNAR</strong> form has already been<br />
made and is valid then there is no need to replace it. This form must<br />
stay with the patient held notes in the patient’s own home and must not<br />
on any account be photocopied.<br />
6.3 Part two of the form is the document required to transfer the information<br />
to WMAS. This information may be the <strong>DNAR</strong> status of the patient but<br />
may also be other information regarding end of life care, management<br />
and or patient preferences regarding place of care. This part of the form<br />
is to be faxed to WMAS (using the safe-haven fax number on the form).<br />
6.4 By following the guidelines on the form the patient’s <strong>DNAR</strong> status, and or<br />
other end of life care preferences or management, will be registered with<br />
WMAS. In the event of an emergency call to the ambulance service the<br />
crew will then be aware that there is a <strong>DNAR</strong> document in the house and<br />
will also have additional information if the special patient notes have<br />
been completed as well.<br />
6.5 WMAS will confirm receipt of the fax within 30 minutes of receiving it and<br />
will inform the named clinician on the form if they are called to the<br />
patient.<br />
6.6 The clinician completing the form is responsible for informing WMAS of<br />
any changes to the patient clinical status, including <strong>DNAR</strong> status, if the<br />
patient dies or if the patient has changed address.<br />
6.7 If WMAS are called out to the patient they will inform the lead clinician of<br />
the outcome on the next working day.<br />
6.8 The form can also be faxed to Medical and District Nursing OOH using<br />
the existing arrangements for special patient notes for palliative and end<br />
of life care patients.<br />
7. Clinical and Professional Conflict Resolution<br />
7.1 Where there is clinical and professional conflict over the decision taken<br />
about the patient’s resuscitation status, urgent decisions must take place<br />
between the Senior Medical Practitioner and the local manager. If the<br />
matter cannot be resolved at local level, then the Medical Director and<br />
senior management lead must be involved as a matter of urgency. As<br />
this is a complex area of law the Consultant or GP may also wish to seek<br />
specific legal advice via the Chief Executive’s Office.<br />
9
8. Summary<br />
• There are no rules about who should or should not be resuscitated. The<br />
Healthcare team must consider every case individually in collaboration<br />
with the patient and their carer(s).<br />
• The use of a ‘blanket policy’ for who should or should not be resuscitated<br />
is illegal and is contrary to the professional duty of the Trust’s staff, who<br />
are expected to act in the best interests of the individual patient at all<br />
times.<br />
• Healthcare professionals need to be aware of the law in relation to<br />
decision making for different groups including adults with mental capacity<br />
to make decisions about their treatment.<br />
• It is important to note that an adult’s relatives/carers have no legal right to<br />
give or withhold consent for resuscitation, unless they have been given<br />
Lasting Power of Attorney for Health Decisions by the patient/client.<br />
However, their views must be sought whenever possible and taken into<br />
account before a decision is made.<br />
• Where there is concern or confusion about resuscitation, the offer of a<br />
second opinion by an appropriate specialist should be made available to<br />
the patient or relatives/carers. Until such a decision has been reached the<br />
situation should be treated as that of an “emergency situation”.<br />
References<br />
British Medical Association, <strong>Resuscitation</strong> Council (UK) and the Royal College<br />
of Nursing (2007) Decisions relating to cardio-pulmonary resuscitation. (The<br />
revised joint statement)<br />
Mental Capacity Act (2005) The Lasting Powers of Attorney, Enduring Powers<br />
of Attorney and Public Guardian Regulations.<br />
Nursing and Midwifery Council (2000) <strong>Resuscitation</strong> – <strong>Do</strong> not resuscitate<br />
orders position statement NMC.<br />
<strong>Resuscitation</strong> Guidelines (2005) <strong>Resuscitation</strong> Council (UK) London.<br />
Withholding and withdrawing Life Sustaining Treatment- Guidance for doctors.<br />
(2006) Good Medical Practice.<br />
10
Appendix 1<br />
Can be used in all care settings<br />
<strong>Do</strong> <strong>Not</strong> <strong>Attempt</strong> Cardio Pulmonary <strong>Resuscitation</strong><br />
Patient Details<br />
Patient Name NHS No.<br />
Date of Birth GP<br />
Address Practice<br />
Postcode Tel No.<br />
Tel No. Fax No.<br />
Next of Kin Support Provider ( note 1 overleaf)<br />
Name Name<br />
Relationship Role<br />
Tel No. Tel No.<br />
Mobile Mobile<br />
Action to be undertaken in the event of Cardiac Arrest<br />
Cardio Pulmonary <strong>Resuscitation</strong> (CPR) is not to be undertaken on this patient because:<br />
(Please tick all relevant boxes)<br />
<strong>Attempt</strong>ing CPR is unlikely to restart the patient’s heart and breathing.<br />
The expected benefit of the treatment is outweighed by the burdens.<br />
<strong>Attempt</strong>ing resuscitation is against the competent patients expressed wishes.<br />
Discussion has taken place with: The patient<br />
The patients relative/significant other<br />
(Name _________________________________ )<br />
This DNACPR is only to be adopted in the case of cardiac/respiratory arrest. All other<br />
appropriate medical support should still be provided<br />
Clinicians’ Details<br />
First Person Signing Second Person Signing (note 2 overleaf)<br />
Designation: Designation:<br />
GMC/NMC Pin: GMC/NMC Pin:<br />
Address Address<br />
Tel Number: Tel Number:<br />
Review Date<br />
(state continuous if not for review):<br />
Signature: Date Signature: Date<br />
Once the DNACPR is completed the WMAS Single Point of Access should be<br />
informed of the details (see note 3 overleaf)<br />
11
Review<br />
Review 1 Review 2<br />
Clinician Name: Clinician Name:<br />
Designation: Designation:<br />
Date reviewed: Date reviewed:<br />
Date for Review: Date for Review:<br />
Signature: Signature:<br />
This space can be used for any general statement of wishes including<br />
preferred place of care. If a formal Advance Decision Refusing<br />
Treatment is required the Patient is advised to use a separate document.<br />
<strong>Not</strong>es on completion of the form:<br />
1. Giving this information enables WMAS to call this relative, friend or professional for<br />
support after they have left the patient’s address.<br />
2. The patients GP, Consultant or senior nurse can sign as first signatory. However the GP<br />
or Consultant MUST sign as the second signatory (as soon as possible) if the senior<br />
nurse is the first signatory. In complex situations or when there is disagreement about a<br />
<strong>DNAR</strong> decision it is recommended as best practice to have 2 signatories from clinicians<br />
who know the patient.<br />
3. <strong>Not</strong>ifying WMAS of the existence of this form will allow Emergency Clinicians the<br />
knowledge of this DNACPR – Please fax details (see enclosed form) to the SPA Hub<br />
4. <strong>Not</strong>ifying WMAS will facilitate the uploading of details onto the WMAS computer (CAD)<br />
system. Although the form is still valid without this communication, this is important<br />
information for WMAS. Make sure the form itself stays with the patient<br />
5. The clinician completing the DNACPR should ensure that all relevant fields are completed<br />
on page one.<br />
6. If the DNACPR is withdrawn the Single Point of Contact SPA HUB should be informed<br />
immediately so that the DNACPR can be removed from the patients address on the CAD<br />
system.<br />
WMAS - October 2009<br />
12
Fax No. 01926832898 ( 24 hours)<br />
Tel No. 01926885082 (24 hours)<br />
Date: __________________<br />
I wish to inform you that a DNACPR/Patient <strong>Not</strong>es (delete as appropriate) has been made<br />
for:<br />
Patient Details NOK Details (as appropriate)<br />
Patient Name Name<br />
Date of Birth<br />
Address Address<br />
Postcode Postcode<br />
Tel No. Tel No.<br />
NHS No.<br />
PT Diagnosis<br />
Authorised Practitioner Details<br />
Name<br />
Job Title<br />
Contact No.<br />
Patient GP<br />
Practice<br />
Address<br />
Postcode<br />
Tel No.<br />
Special <strong>Not</strong>es - Please details any special patient notes in this section – i.e. telephone numbers, referral<br />
routes, out of hour’s information, clinical advice ….<br />
13
Special <strong>Not</strong>es<br />
Please details any special<br />
patient notes in this section<br />
– i.e. telephone numbers,<br />
referral routes, out of<br />
hour’s information, clinical<br />
advice ….<br />
If you require any further information please do not hesitate to contact WMAS.<br />
Upon receipt of this form a WMAS representative will contact you to validate this<br />
request within 30 minutes (24 hours a day)<br />
14