Chronic Kidney Disease Pathway Document Description Presented ...
Chronic Kidney Disease Pathway Document Description Presented ...
Chronic Kidney Disease Pathway Document Description Presented ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
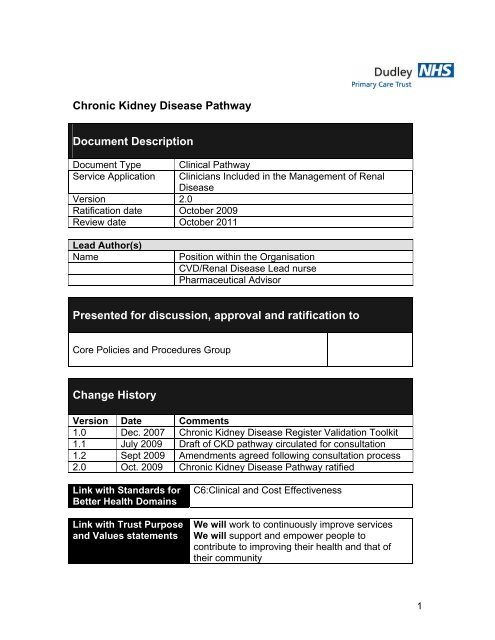
<strong>Chronic</strong> <strong>Kidney</strong> <strong>Disease</strong> <strong>Pathway</strong><br />
<strong>Document</strong> <strong>Description</strong><br />
<strong>Document</strong> Type<br />
Service Application<br />
Version 2.0<br />
Ratification date October 2009<br />
Review date October 2011<br />
Clinical <strong>Pathway</strong><br />
Clinicians Included in the Management of Renal<br />
<strong>Disease</strong><br />
Lead Author(s)<br />
Name<br />
Position within the Organisation<br />
CVD/Renal <strong>Disease</strong> Lead nurse<br />
Pharmaceutical Advisor<br />
<strong>Presented</strong> for discussion, approval and ratification to<br />
Core Policies and Procedures Group<br />
Change History<br />
Version Date Comments<br />
1.0 Dec. 2007 <strong>Chronic</strong> <strong>Kidney</strong> <strong>Disease</strong> Register Validation Toolkit<br />
1.1 July 2009 Draft of CKD pathway circulated for consultation<br />
1.2 Sept 2009 Amendments agreed following consultation process<br />
2.0 Oct. 2009 <strong>Chronic</strong> <strong>Kidney</strong> <strong>Disease</strong> <strong>Pathway</strong> ratified<br />
Link with Standards for<br />
Better Health Domains<br />
Link with Trust Purpose<br />
and Values statements<br />
C6:Clinical and Cost Effectiveness<br />
We will work to continuously improve services<br />
We will support and empower people to<br />
contribute to improving their health and that of<br />
their community<br />
1
Summary Sheet<br />
This pathway is intended to provide information on the management of people<br />
with <strong>Chronic</strong> <strong>Kidney</strong> <strong>Disease</strong> (CKD) to reduce their risks and to identify, prevent<br />
or delay the progression of associated co-morbid vascular and metabolic<br />
conditions. It is also intended to identify people who are deemed to be at high risk<br />
of developing CKD, to promote active screening of these people and to reduce or<br />
eliminate individual risk factors to reduce their overall level of risk.<br />
This policy applies directly to all staff members employed by NHS Dudley and<br />
Dudley Community Services who are involved in the management of people with<br />
CKD and is recommended as good practice guidance for each of the<br />
independent contractor professions. National and local guidance, policies, reports<br />
and/or papers which this particular document should be read in conjunction with:<br />
Local Guidance:<br />
• Best practice Guidelines for Lifestyle Assessment<br />
• Cardiovascular Risk pathway<br />
• Hyperlipidaemia Guidelines<br />
• Dudley Guidelines for the Pharmacological Management of Hypertension<br />
National Guidance: NICE Guidelines for:<br />
• Management of <strong>Chronic</strong> <strong>Kidney</strong> <strong>Disease</strong><br />
• Secondary Prevention of Myocardial Infarction<br />
• Management of Patients with Heart Failure<br />
• Management of Hypertension<br />
• Lipid Modification<br />
• Management of Obesity<br />
National Service Frameworks for:<br />
• Coronary Heart <strong>Disease</strong><br />
• Renal Services Part II<br />
• Diabetes<br />
This document will be subject to formal review in October 2011 led by the<br />
Vascular Programmes Local Implementation Team.<br />
2
<strong>Pathway</strong> for the Identification and Management of<br />
<strong>Chronic</strong> <strong>Kidney</strong><br />
<strong>Disease</strong><br />
In the Primary Care Setting<br />
Implementation date: October 2009<br />
Review date: October 2011<br />
<strong>Pathway</strong> overview<br />
3
This CKD pathway has been produced by the CKD pathway group, a sub-group<br />
of the Dudley Renal LIT. It is intended to be used by practice and community<br />
teams, GPs, practice nurses, HCAs and administrative/I.T staff to:<br />
• Build and validate accurate CKD registers in line with the Quality and<br />
Outcomes Framework of the GMS contract and nationally expected<br />
prevalence rates.<br />
• Promote an awareness of CKD and the need for reduction of risk, early<br />
identification and diagnosis.<br />
• Inform the management of people with CKD in line with best practice as<br />
demonstrated in local and national guidelines<br />
• Support the appropriate referral to acute services and/or promotion of<br />
joint working with acute and community services to provide optimum<br />
outcomes in terms of management and patient choice.<br />
Consultation has included:<br />
• Renal LIT<br />
• Diabetes DIP<br />
• Vascular LIT<br />
• Nephrologists at DGoH<br />
• Diabetologists at DGoH<br />
• Consultant Chemical Pathologist<br />
• Dudley Clinical Commissioning Forum (DCF)<br />
• Dudley Clinical Executive Team<br />
• Community Diabetes Team<br />
• Renal Dieticians<br />
• Dudley <strong>Kidney</strong> Patients’ Association<br />
This pathway may be used wholly electronically by downloading onto the practice<br />
system, or in paper form. Practices may wish to use the pathway in either way, or<br />
may wish to download certain sections only.<br />
For further information on the development of the CKD pathway please contact:<br />
Cardiovascular and Renal <strong>Disease</strong> Lead Nurse Tel. 01384 366880<br />
Falcon House Fax. 01384 366460<br />
The Minories Mob. 07786 338072<br />
Dudley<br />
DY2 8PG Courier 114<br />
4
Contents<br />
Introduction ……………………………………………………………………….7<br />
Renal <strong>Pathway</strong> Overview ……………….……………………………………. ..9<br />
High Risk Groups ……………………………………………………………….10<br />
Read Codes ……………………………………………………………………..12<br />
Identification of CKD in patients not in a High Risk Group …………………14<br />
Acute Renal Failure …………………………………………………………….15<br />
Contact Details ……………………………………………….. ………………. 17<br />
Diagnosis of CKD ……………………………………………………………... 18<br />
CKD Stages ……………………………………………………………………. 19<br />
Prevalence of CKD ……………………………………………………………. 20<br />
Practice Action Plan Template ………………………………………………. .21<br />
Stages 1 and 2 …………………………………………………………………. 30<br />
Patient information ……………………………………………… 30<br />
Cardiovascular risk ……………………………………………… 31<br />
Hypertension …………………………………………………….. 33<br />
Initiating ACE Inhibitor …………………………………………… 36<br />
Salt intake ………………………………………………………… 36<br />
Nephrotoxic drugs ……………………………………………….. 36<br />
Renal Artery Stenosis …………………………………………… 37<br />
Urinalysis …………………………………………………………. 40<br />
Diet ………………………………………………………………... 44<br />
Diabetic Control …………………………………………………. .45<br />
Hepatitis B ……………………………………………………… 48<br />
5
Influenza/Pneumococcal Vaccination ……………………….. 49<br />
Follow-up ……………………………………………………….. 50<br />
Stage 3 …………………………………………………………………………… 51<br />
Anaemia ……………………………………………………….. 51<br />
Stage 4 …………………………………………………………………………… 54<br />
One-Stop Renal Clinic ………………………………………. 54<br />
Bone Metabolism …………………………………………….. 56<br />
Annual Review ……………………………………………….. 57<br />
Stage 5 ………………………………………………………………………….. 59<br />
Referral ……………………………………………………….. 60<br />
Renal Ultrasound ……………………………………………. 61<br />
Abbreviations …………………………………………………………………… 62<br />
Appendix 1:<br />
Calcium and Phosphate Balance pathway …………………………………. 63<br />
6
Introduction<br />
<strong>Chronic</strong> kidney disease (CKD) describes abnormal kidney function and/or<br />
structure. It is common, frequently unrecognised and often exists together with<br />
other conditions (for example, cardiovascular disease and diabetes). When<br />
advanced, it also carries a higher risk of mortality. The risk of developing CKD<br />
increases with increasing age, and some conditions that coexist with CKD<br />
become more severe as kidney dysfunction advances. CKD can progress to<br />
established renal failure in a small but significant percentage of people.<br />
CKD is usually asymptomatic, but it is detectable, and tests for detecting CKD<br />
are both simple and freely available. There is evidence that treatment can<br />
prevent or delay the progression of CKD, reduce or prevent the development of<br />
complications and reduce the risk of cardiovascular disease. However, because<br />
of a lack of specific symptoms, people with CKD are often not diagnosed, or<br />
diagnosed late when CKD is at an advanced stage.<br />
http://www.nice.org.uk/nicemedia/pdf/CG073NICEGuideline.pdf<br />
Normal <strong>Kidney</strong> Ageing<br />
A normal estimated glomerular filtration rate (eGFR) is about 100 ml/min in young<br />
adults. However, this may be somewhat lower, some young adults with normal<br />
kidneys may have an eGFR as low as 75 ml/min. Normal kidney function<br />
deteriorates with age and falls by about 1 ml/min per year. Therefore as people<br />
get older, many healthy people aged 75+ may have an eGFR of < 60 ml/min.<br />
Recent research suggests that 1 in 10 of the population may have chronic kidney<br />
disease (CKD), but it is less common in young adults, being present in 1 in 50<br />
people. In those aged over 75 years, CKD is present in 1 out of 2 people.<br />
However, many elderly people with an eGFR < 60 mls/min may not have<br />
‘diseased’ kidneys, but have normal ageing of their kidneys. Although severe<br />
kidney failure will not occur with normal ageing of the kidneys, there is an<br />
increased chance of high blood pressure and heart disease or stroke.<br />
It is recommended that all patients with CKD stage 1 – 5, including elderly<br />
patients are added to the CKD register for the GMS Contract Quality and<br />
Outcomes Framework and undergo annual screening to monitor the rate of<br />
progression, blood pressure, proteinuria and development of associated<br />
cardiovascular risk factors.<br />
http://www.kidney.org.uk/Medical-Info/ckd-info/index.html<br />
Late referral of patients with CKD requiring renal replacement therapy (RRT) to<br />
specialist renal services is associated with significant cost and poor clinical<br />
outcomes. On average 30% of people with advanced kidney disease are<br />
referred late to nephrology services from both primary and secondary care,<br />
causing increased mortality and morbidity.<br />
http://www.nice.org.uk/nicemedia/pdf/CG073NICEGuideline.pdf<br />
7
The great majority of patients starting RRT have progressed from earlier stages<br />
and most could therefore have been identified, managed and referred more<br />
appropriately at an earlier stage from primary care. Early CKD is common<br />
however and referral of all patients with early CKD would completely overwhelm<br />
existing specialist services. The great majority of patients with early CKD do not<br />
progress to end-stage renal disease (ESRD), but do have a substantially<br />
increased risk of cardiovascular morbidity and mortality. Optimal management of<br />
the risk factors for cardiovascular disease, such as hypertension and proteinuria<br />
will reduce the risk of progression from early CKD to ESRD and can be managed<br />
effectively in primary care.<br />
CKD Stages According to Established Estimated Glomerular Filtration Rate<br />
(eGFR)<br />
CKD Stage<br />
<strong>Description</strong><br />
1 Normal eGFR > 90 mL/min/1.73m 2<br />
*With other evidence of chronic kidney damage present<br />
2 Mild Impairment - 60-89 mL/min/1.73m 2<br />
*With other evidence of chronic kidney damage present<br />
3 Moderate Impairment - 30-59 mL/min/1.73m 2<br />
3A 45 - 59<br />
3B 44 - 30<br />
4 Severe Impairment – 15-29 mL/min/1.73m 2<br />
5 Established Renal Failure (ERF)<br />
< 15 mL/min/1.73m 2 or on dialysis<br />
*Other Evidence of <strong>Chronic</strong> <strong>Kidney</strong> Damage<br />
• Persistent microalbuninuria, proteinuria or haematuria (after exclusion of<br />
other causes)<br />
• Structural abnormalities seen on X-ray (e.g. polycystic kidney disease)<br />
• Biopsy proven chronic glomerulonephritis<br />
8
CKD <strong>Pathway</strong><br />
D<br />
I<br />
A<br />
G<br />
N<br />
O<br />
S<br />
I<br />
S<br />
Ensure annual assessment<br />
of people in high risk groups<br />
Introduction<br />
1. Confirm diagnosis<br />
2. Identify CKD stage 1 - 5<br />
3. Enter onto practice system with appropriate<br />
read code compatible with GMS contract to form<br />
register.<br />
4. Check register prevalence<br />
5. Consider use of practice action plan template<br />
Suspicion of <strong>Chronic</strong> <strong>Kidney</strong> <strong>Disease</strong><br />
(CKD) following investigation for other<br />
unrelated condition<br />
Is it Acute Renal<br />
Failure<br />
Urgent<br />
Admission<br />
M<br />
A<br />
N<br />
A<br />
G<br />
E<br />
M<br />
E<br />
N<br />
T<br />
CKD stage 1 and 2.<br />
Patient information and<br />
education<br />
Address progressing factors:-<br />
CV risk<br />
Hypertension<br />
lifestyle<br />
Initiation of ACE/ARB<br />
Drugs with high salt content<br />
Nephrotoxic/renally excreted<br />
drugs, inc. OTC medication<br />
Renal Artery Stenosis<br />
Urinalysis<br />
Diet in CKD<br />
Glycaemic control<br />
Flu/pneumo vac<br />
Hepatitis B immunisation<br />
Follow-up<br />
Stage 3 (3A 3B)<br />
As stage 1 and 2<br />
plus:<br />
Management of<br />
anaemia<br />
ESA pathway<br />
CKD stage 4<br />
As I, 2 and 3 plus shared<br />
care plan initiation. Refer to<br />
"One-Stop" Renal clinic<br />
Bone metabolism<br />
<strong>Pathway</strong> for the<br />
Management of Calcium<br />
and Phosphate Balance<br />
CKD stage 5<br />
Urgent referral<br />
if clinically<br />
appropriate<br />
exceptions<br />
Annual<br />
review in<br />
primary<br />
care<br />
R<br />
E<br />
F<br />
E<br />
R<br />
R<br />
A<br />
L<br />
Criteria for referral to<br />
Specialist Nephrology<br />
services<br />
Renal Ultrasound<br />
Information to include<br />
with referral<br />
Palliative care trust protocol<br />
Prescribing /symptom control in advanced<br />
renal disease<br />
Seeking Advice from<br />
Nephrologist / Renal<br />
Dept. DGOH<br />
Contact information<br />
Frequently asked<br />
questions<br />
9
High Risk Groups<br />
Renal function should be measured and recorded annually for all patients who<br />
fall into a high risk group. This is measured by Estimated Glomerular Filtration<br />
Rate (eGFR). Measurement of eGFR is available from the pathology department<br />
at Dudley Group of Hospitals. It accompanies the report following any request for<br />
Urea and Electrolytes (U+E), being calculated from the serum creatinine assay.<br />
Patients in the high risk groups are considered to be at a higher than normal risk<br />
of developing renal impairment due to co-morbities and/or medical history.<br />
Ethnicity also increases risk with black and minority ethnic (BME) groups in the<br />
U.K having up to 4 times greater risk of developing CKD.<br />
http://www.britishrenal.org/conferences/brs2007/posters/CKD%20General-48.doc<br />
The high risk groups fall into 3 main categories, morbidity, drug related and<br />
urinary.<br />
Morbidity:<br />
• Patients with Vascular disease<br />
o Coronary Heart disease<br />
o Stroke<br />
o Peripheral Vascular disease<br />
• Heart Failure<br />
• Hypertension<br />
• Diabetes<br />
• Multi-system diseases which involve the kidney, e.g. systemic lupus<br />
erythematosus, rheumatoid arthritis.<br />
• A first-degree relative with CKD stage 5.<br />
Drug related:<br />
• Patients on ACE inhibitors or angiotensin receptor blockers (ARBs)<br />
• Patients on NSAIDs, including COX II<br />
• Patients on diuretics<br />
• Patients on lithium carbonate<br />
• Mesalazine and other 5-aminosalicylic drugs<br />
• Calcineurin inhibitors (cyclosporin, tacrolimus)<br />
Urinary:<br />
• Recurrent Urinary Tract Infections<br />
• Bladder outflow obstruction<br />
• Recurrent kidney stones (>1/year) or predisposing condition, e.g. primary<br />
hyperoxaluria<br />
• Neurogenic bladder<br />
• Past surgical urinary diversion<br />
• Polycystic kidney disease<br />
• Reflux nephropathy<br />
• Biopsy proven chronic glomerulonephritis<br />
• Persistent proteinuria<br />
• Urologically unexplained persistent haematuria<br />
10
<strong>Kidney</strong> function deteriorates naturally with age. However the conditions above<br />
may cause the kidneys to deteriorate more rapidly. Careful management of<br />
progressing factors (see pathway) could ensure a normal or close to<br />
normal/expected pattern of deterioration.<br />
<strong>Kidney</strong> function by eGFR measurement should be monitored annually in the high<br />
risk groups identified above.<br />
Frequency of monitoring of <strong>Kidney</strong> function in CKD is indicated by the table<br />
below.<br />
Frequency of Monitoring of <strong>Kidney</strong> Function in Established CKD<br />
K/DOQI eGFR<br />
Frequency<br />
Stage mls/min<br />
1 > 90 Annually<br />
2 60 - 89 Annually<br />
3 30 - 59 Annually<br />
(6 monthly if newly diagnosed or progressive**)<br />
4 15 - 29 6 monthly<br />
(3 monthly if newly diagnosed or progressive**)<br />
5 < 15 3 monthly<br />
Stable kidney function is defined as a change of < 2mls/min in 6 months<br />
** Progressive kidney function is defined as a change of > 2mls/min in 6 months<br />
Any patient assessed with a progressive condition should receive assessment of<br />
progressing factors and discussion/referral to nephrology services.<br />
Stage 3 Classification<br />
The UK Consensus Conference on early CKD has recommended that the <strong>Kidney</strong><br />
<strong>Disease</strong> Outcomes Quality Initiative (KDOQI) classification should be modified by<br />
dividing CKD stage 3 into CKD 3A and 3B and that a suffix “p” should be used for<br />
all stages to denote patients with urine protein to creatinine ratio >100mg/mmol,<br />
who are at increased risk for progression and/or the development of<br />
cardiovascular disease e.g. CKD stages 2p, 3Bp.<br />
CKD stage 3 is sub-classified into 2 groups, 3A and 3B.<br />
Stage eGFR Progression to ESRD<br />
3A 45 - 59 Lower risk<br />
3B 44 - 30 Higher risk<br />
11
Using the existing classification at least 4% of the adult population have stage 3<br />
CKD, many of whom are elderly. They are at increased risk of cardiovascular<br />
disease but most will not progress to end stage kidney disease. The priority<br />
should therefore be to identify those at risk of kidney disease progression.<br />
Persistent proteinuria (protein:creatinine ratio (PCR) > 100 mg/mmol) is the<br />
best indicator of risk of progression to ESRD.<br />
In diabetic patients urinary albumin /microalbumin estimations should be used.<br />
It is recommend that all patients with suspected early CKD should have a urine<br />
dipstick for proteinuria and, if positive, quantification of the PCR. This is included<br />
in the Quality and Outcomes Framework. Urine albumin:creatinine ratio (ACR)<br />
should be used in line with national guidelines in people with diabetes.<br />
(Patients undergoing dialysis have the suffix D added to their CKD stage, e.g.<br />
5D. Those who have had a transplant should be classified according to eGFR but<br />
have the suffix T added, e.g. 3T)<br />
Read Codes<br />
1Z15. CKD stage 3A<br />
1Z16. CKD stage 3B<br />
1Z17. CKD stage 1 with proteinuria / 1P<br />
1Z18. CKD stage 1 without proteinuria<br />
1Z19. CKD stage 2 with proteinuria / 2P<br />
1Z1A. CKD stage 2 without proteinuria<br />
1Z1B.<br />
1Z1C.<br />
1Z1D.<br />
1Z1E.<br />
1Z1F.<br />
1Z1G.<br />
1Z1H.<br />
1Z1J.<br />
1Z1K.<br />
1Z1L.<br />
CKD stage 3 with proteinuria / 3P<br />
CKD stage 3 without proteinuria<br />
CKD stage 3A with proteinuria / 3AP<br />
CKD stage 3A without proteinuria<br />
CKD stage 3B with proteinuria / 3BP<br />
CKD stage 3B without proteinuria<br />
CKD stage 4 with proteinuria / 4P<br />
CKD stage 4 without proteinuria<br />
CKD stage 5 with proteinuria / 5P<br />
CKD stage 5 without proteinuria<br />
http://www.renal.org/CKDguide/consensus.html<br />
References<br />
12
Joint Speciality Committee - Royal College of Physicians, The Renal Association<br />
(2006) <strong>Chronic</strong> <strong>Kidney</strong> <strong>Disease</strong> in Adults, UK Guidelines for Identification,<br />
Management and Referral.<br />
http://www.renal.org/CKDguide/full/CKDprintedfullguide.pdf<br />
University Hospital – Leicester (2005) Renal Guidelines Adults with <strong>Chronic</strong><br />
<strong>Kidney</strong> <strong>Disease</strong> http://www.britishrenal.org/Other/RenalGuideline.pdf<br />
Department of Health (2005) The National Service Framework for Renal<br />
Services: Part Two: <strong>Chronic</strong> <strong>Kidney</strong> <strong>Disease</strong>, Acute Renal Failure and End of Life<br />
Care.<br />
http://www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicy<br />
AndGuidance/DH_4101902<br />
Return to overview<br />
13
Identification of CKD in Patients who are not in a High Risk Group<br />
There are few specific signs or symptoms which would alert suspicion to the<br />
possibility of CKD in groups who are not routinely tested due to the presence of<br />
morbidities which would put them at high risk. As a result these patients often<br />
present at a late stage. Another reason for this would be the lack of<br />
understanding of clinical staff on the significance of kidney function testing when<br />
relying only on measurements of serum creatinine concentration. It is therefore<br />
recommended that eGFR be requested as this gives a more accurate picture of<br />
decline in kidney function than rising serum creatinine alone. Currently at Dudley<br />
Group of Hospitals any request for urea and electrolytes (U+E) will automatically<br />
have eGFR calculated and will accompany the results.<br />
Any patient with an eGFR of < 60 mls/min should be investigated following<br />
the renal pathway.<br />
An eGFR of > 60 without other evidence of renal disease should not be<br />
considered significant and these patients should not be subject to further<br />
investigation. However, a diagnosis of Acute Renal Failure should be considered.<br />
In many cases the possibility of renal impairment only comes to light when a<br />
patient receives routine monitoring at a well person clinic, insurance medicals or<br />
during routine investigations for acute illness or any assessment which involves<br />
the monitoring of serum creatinine and/or U+E and/or urinalysis. It is worth<br />
remembering that the majority of these patients will feel well and therefore the<br />
diagnosis of renal impairment will be unexpected, especially if it comes to light as<br />
part of a routine assessment.<br />
Joint Speciality Committee - Royal College of Physicians, The Renal Association<br />
(2006) <strong>Chronic</strong> <strong>Kidney</strong> <strong>Disease</strong> in Adults, UK Guidelines for Identification,<br />
Management and Referral.<br />
http://www.renal.org/CKDguide/full/CKDprintedfullguide.pdf<br />
Return to overview<br />
14
Acute Renal Failure<br />
Acute Renal Failure (ARF) is a medical emergency as deterioration can be rapid<br />
and fatal in many cases. Prognosis for recovery of kidney function is dependent<br />
on the time delay between presentation and diagnosis. It is therefore extremely<br />
important that people with suspected ARF are identified and investigated<br />
promptly to ensure best possible outcomes. These patients should receive<br />
prompt admission to acute nephrology services/emergency department.<br />
ARF is characterised by rapid deterioration in renal function over a period of<br />
hours or days. It should be suspected in the presence of an acute illness with<br />
the following signs/symptoms:<br />
• A 50% rise in serum creatinine concentration<br />
• A 25% fall in eGFR (if baseline unknown, assume 75mls/min)<br />
N.B. eGFR should be interpreted with caution as it should be calculated in<br />
stable creatinine concentrations<br />
• Oliguria (urinary output
Management of a Previously Undiagnosed Patient with eGFR <<br />
60mls/min<br />
Is the YES patient acutely unwell<br />
NO<br />
YES<br />
Manage illness as appropriate.<br />
Repeat eGFR within 1-5 days<br />
(Go to *)<br />
Symptoms of outflow<br />
obstruction**<br />
YES<br />
Palpate for bladder<br />
Urgent renal ultrasound<br />
(Renal ultrasound scan if history<br />
suggestive of urological disease)<br />
NO<br />
* Has a reduced eGFR (< 60mls/min) or<br />
raised creatinine been measured<br />
previously<br />
NO<br />
Repeat eGFR within 5 days<br />
Suspect ARF in the presence of<br />
any of the following:<br />
eGFR < 30 ml/min<br />
eGFR fall of 25%<br />
Creatinine rise of 50%<br />
Blood and Protein in urine<br />
YES<br />
Check previous eGFR results.<br />
Calculate eGFR using the 4-<br />
variable MDRD formula from<br />
previous creatinine results.<br />
Compare results and track rate of<br />
progression chronologically.<br />
Suspect ARF if there is:<br />
• A fall in eGFR of 25%<br />
• A rise in Creatinine of 50%<br />
• eGFR < 30 ml/min<br />
• Blood and Protein in urine<br />
URGENT<br />
ADMISSION<br />
Refer to/<br />
Discuss with<br />
nephrologist.<br />
Contact details<br />
**People with CKD and renal outflow obstruction should normally be referred to urological<br />
services, unless urgent medical intervention is required.<br />
16
Next Steps<br />
Any patient suspected to have ARF should be admitted urgently to nephrology<br />
services/emergency department with as much information as possible, including<br />
all previous results available for:<br />
• Creatinine<br />
• eGFR<br />
• Blood pressure<br />
• Urinalysis<br />
• HbA1C (if diabetic)<br />
To include a list of current medication (including OTC) and any relevant medical<br />
history.<br />
Further information upon which to make a clinical decision should be sought<br />
urgently by contacting the nephrology department.<br />
Contact details:<br />
On call renal consultant:<br />
(Advice/Urgent admission)<br />
01384 244432 (direct line)<br />
(or 01384 456111 to switchboard at<br />
RHH and ask for on-call renal<br />
consultant)<br />
Fax./urgent paper referral 01384 244543<br />
Haemodialysis 01384 244384<br />
(Nursing Station Renal Unit)<br />
CAPD 01384 244388<br />
(Nursing Station Renal Unit)<br />
Return to overview<br />
Diagnosis of CKD<br />
17
The diagnosis of CKD is made by assessment of kidney function using estimated<br />
Glomerular Filtration Rate (eGFR). eGFR is calculated from serum creatinine<br />
levels, but depends on the method of creatinine assay used by each pathology<br />
department. Therefore independent calculations of eGFR from previous<br />
creatinine results will not give reliable results, as a correction factor needs to be<br />
applied for the method used by Dudley group of hospitals pathology dept.<br />
There is no need for 24-hour urine collection to measure creatinine clearance in<br />
primary care.<br />
The method for calculating eGFR is the 4-variable MDRD formula:<br />
eGFR (mL/min/1.73m 2 )= 186 x [Serum Creatinine (umol/L) x 0.0113] -1.154 x<br />
Age(years) -0.203 (x 0.742 if female) and 1.21 if African Caribbean.<br />
An online calculator can be downloaded from:<br />
http://www.renal.org/eGFRcalc/GFR.pl<br />
N.B. The 4-variable MDRD formula:<br />
• Is suitable for adults only (>17 years of age)<br />
• Results are unreliable for eGFR > 60 mL/min/1.73m 2 .<br />
• Results will NOT reflect true GFR if patient is receiving dialysis therapy.<br />
• The formula has not been validated for Asian people.<br />
• Results may deviate from true GFR values with extremes of body<br />
composition, dietary intake or severe liver disease.<br />
• The formula has NOT been validated for drug dosing. Use the Cockcroft<br />
and Gault formula<br />
Diagnosis of CKD should be made during a period of wellness by<br />
measurement of eGFR.<br />
Advise the person not to eat meat for at least 12 hours before the eGFR blood<br />
test.<br />
If the eGFR is < 60 mls/min then the guidance in this pathway should be followed<br />
to exclude acute renal failure.<br />
A diagnosis of renal impairment should not be made on the basis of<br />
one result; at least 2 results should be considered which should be at<br />
least 3 months apart.<br />
If both of the results are< 60 mls/min then the patient should be considered to<br />
have CKD and be added to the practice register. The patient should then be<br />
managed following the guidance in this pathway.<br />
18
Return to overview<br />
CKD Stages<br />
CKD Stage<br />
<strong>Description</strong><br />
1 Normal eGFR > 90 mL/min/1.73m 2<br />
With other evidence of chronic kidney damage<br />
2 Mild Impairment - 60-89 mL/min/1.73m 2<br />
With other evidence of chronic kidney damage<br />
3 Moderate Impairment - 30-59 mL/min/1.73m 2<br />
3A 45 - 59<br />
3B 44 - 30<br />
4 Severe Impairment – 15-29 mL/min/1.73m 2<br />
5 Established Renal Failure (ERF)<br />
< 15 mL/min/1.73m 2 or on dialysis<br />
*Other Evidence of <strong>Chronic</strong> <strong>Kidney</strong> Damage<br />
• Persistent microalbuminuria<br />
• Persistent proteinuria<br />
• Persistent haematuria (after exclusion of other causes)<br />
• Structural abnormalities seen on X-ray (e.g. polycystic kidney disease)<br />
• Biopsy proven chronic glomerulonephritis<br />
Patients found to have an eGFR of 60-89 mls/min without one of the markers<br />
above should not be considered to have CKD as these levels are considered<br />
normal and therefore should not be subject to further investigation unless there<br />
are additional reasons to do so, e.g. belonging to a high risk group.<br />
Prevalence of CKD<br />
The prevalence of CKD in at stage 3-5 in the UK based on neoErica data is<br />
4.9% 1<br />
19
(Where stage 4 = 0.7%, and stage 5 = 0.2%)<br />
Screening of patients with hypertension, diabetes and > 55 would yield approx.<br />
93% of the CKD register, with this approach being the most effective strategy to<br />
detect patients with CKD 2 .<br />
Based on an expected prevalence of 4.9%:<br />
• For a practice population of 2000:<br />
The approx. number of patients with CKD = 94<br />
(4 pts. at stage 4 and 4 pts. at stage 5)<br />
• For a practice population of 5000<br />
The approx. number of patients with CKD = 245<br />
(10 pts. at stage 4 and 10 pts. at stage 5<br />
• For a practice population of 10 000<br />
The approx. number of patients with CKD = 490<br />
(20 pts. at stage 4 and 20 pts. at stage 5)<br />
For guidance on building and validating a practice CKD register see practice<br />
action plan - compiling a chronic kidney disease register.<br />
References<br />
1. de Lusignan S, Chan T, Stevens P, O'Donoghue D, Hague N, Dzregah B,<br />
Van Vlymen J, Walker M and Hilton S. Identifying patients with chronic<br />
kidney disease from general practice computer records. Family Practice<br />
2005; 22: 234–241<br />
http://fampra.oxfordjournals.org/cgi/content/full/22/3/234<br />
2. Hallan S et al. Screening strategies for chronic kidney disease in the<br />
general population: follow-up of cross sectional health survey BMJ<br />
2006;333(7577):1047. http://www.bmj.com/cgi/con<br />
Return to overview<br />
20
Practice Action Plan<br />
Compiling a <strong>Chronic</strong> <strong>Kidney</strong> <strong>Disease</strong> Register<br />
Name of Practice …………………………………………………………………………………………………………………………<br />
Aim: To build a register of patients with <strong>Chronic</strong> <strong>Kidney</strong> <strong>Disease</strong> to meet the requirements of the Quality and<br />
Outcomes Framework of the GMS contract: CKD1<br />
This action plan sets out the method and rationale behind each action in a step wise approach, assigning responsibility to<br />
each part of the task. Practice expected prevalence should be calculated, allowing for assessment of the completeness of<br />
the final register.<br />
Support for completing these actions is available from the Cardiovascular and Renal <strong>Disease</strong> Lead Nurse, (address<br />
below)<br />
Shelagh.cleary@dudley.nhs.uk Tel. 01384 362754<br />
Please sign below and send a copy of this front sheet to:<br />
Cardiovascular and Renal <strong>Disease</strong> Lead Nurse<br />
Service Development Dept. 5 th Floor, Falcon House, The Minories, Dudley. DY2 8PG. Courier no. 114, Fax 01384 366460<br />
Signed ………………………………………………. Position ………………………………………...<br />
Print …………………………………………………. Date ……………………………………………<br />
21
Practice Demographics<br />
Population size ……………………………….<br />
Estimated CKD prevalence at stage 3-5 = 4.9%<br />
Stage 4 = 0.7%, and stage 5 = 0.2%<br />
(Based on UK figures from NeoErica 1 )<br />
Estimated practice prevalence of CKD stage 3-5 = ……………………. patients<br />
(Stage 4 = ………. patients<br />
Stage 5 = ……….. patients)<br />
Number on practice system with read coded CKD diagnosis ……………………………….<br />
(Read codes compatible with QoF)<br />
This information can be found from population manager or clinical audit facility on the practice system. Or a practice query<br />
can be run as outlined on p.4<br />
22
Action Rationale Responsible<br />
Run a search on the practice system to identify<br />
all patients with an eGFR
one
eGFR
3.1.07 eGFR = 35<br />
26.1.07 eGFR = 41<br />
3.3.07 eGFR = 38<br />
4741 30.6.06 eGFR = 50<br />
10.10.06 eGFR = 56<br />
22.5.07 eGFR = 46<br />
Last BP 139/71<br />
On ACE<br />
Achieving all 4 clinical indicators.<br />
Diagnosis confirmed CKD 3. Added to register.<br />
Last BP 144/70<br />
Not on ACE<br />
Achieving CKD 1,2 and 3<br />
26
CKD Stages<br />
CKD Stage <strong>Description</strong> Read Code<br />
1 Normal GFR > 90 mL/min/1.73m 2<br />
*With other evidence of chronic kidney damage<br />
2 Mild Impairment - 60-89 mL/min/1.73m 2<br />
*With other evidence of chronic kidney damage<br />
3 Moderate Impairment - 30-59 mL/min/1.73m 2 1Z12<br />
4 Severe Impairment – 15-29 mL/min/1.73m 2 1Z13<br />
5 Established Renal Failure (ERF)<br />
< 15 mL/min/1.73m 2 or on dialysis<br />
eGFR<br />
(estimated glomerular filtration rate)<br />
1Z14<br />
451E<br />
*Other Evidence of <strong>Chronic</strong> <strong>Kidney</strong> Damage<br />
• Persistent microalbuminuria<br />
• Persistent proteinuria<br />
27
• Persistent haematuria (after exclusion of other causes)<br />
• Structural abnormalities seen on X-ray (e.g. polycystic kidney disease)<br />
• Biopsy proven chronic glomerulonephritis<br />
Patients found to have an eGFR of 60-89 mls/min without one of the markers above should not be considered to have<br />
CKD and should not be subject to further investigation unless there are additional reasons to do so, e.g. belonging to a<br />
high risk group.<br />
References<br />
de Lusignan S, Chan T, Stevens P, O'Donoghue D, Hague N, Dzregah B, Van Vlymen J, Walker M and Hilton S.<br />
Identifying patients with chronic kidney disease from general practice computer records. Family Practice 2005; 22: 234–<br />
241 http://fampra.oxfordjournals.org/cgi/content/full/22/3/234<br />
Return to overview<br />
28
References<br />
Joint Speciality Committee - Royal College of Physicians, The Renal Association<br />
(2006) <strong>Chronic</strong> <strong>Kidney</strong> <strong>Disease</strong> in Adults, UK guidelines for Identification,<br />
Management and Referral.<br />
http://www.renal.org/CKDguide/full/CKDprintedfullguide.pdf<br />
Department of Health (2005) The National Service Framework for Renal<br />
Services: Part Two: <strong>Chronic</strong> <strong>Kidney</strong> <strong>Disease</strong>, Acute Renal Failure and End of Life<br />
Care.<br />
http://www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicy<br />
AndGuidance/DH_4101902<br />
University Hospital Leicester (2005) Renal Guidelines – Adults with <strong>Chronic</strong><br />
<strong>Kidney</strong> <strong>Disease</strong> http://www.britishrenal.org/Other/RenalGuideline.pdf<br />
British Medical Association (2007) <strong>Chronic</strong> <strong>Kidney</strong> <strong>Disease</strong> Frequently Asked<br />
Questions. NHS Employers<br />
http://www.primarycarecontracting.nhs.uk/uploads/QOF/june_07/qof__faq_in_chr<br />
onic_kidney_disease.pdf<br />
Return to overview<br />
29
Stages 1 and 2<br />
Patient Information and Education<br />
The following websites are useful for downloading information and materials for<br />
patients and for use in clinics.<br />
It is worth noting however, that a diagnosis at stage 3/4 CKD may have been<br />
made on blood test results alone. The patient will most likely have not had any<br />
symptoms and therefore will not be expecting the diagnosis.<br />
<strong>Kidney</strong> Patient Guide<br />
Web: www.kidneypatientguide.org.uk<br />
The <strong>Kidney</strong> Patient Guide provides web-based patient information for renal<br />
patients, their families, health professionals and others interested in kidney<br />
disease. The site is described as follows: "It includes information not only on<br />
physical aspects of kidney failure - how the kidneys function, what happens when<br />
they don't, and the treatments available - but also on wider issues such as<br />
emotional, social and financial implications.<br />
The site is designed primarily with a UK focus but will be of value to anyone who<br />
is affected by the condition." Information is included on the following topics.<br />
• What patients say.<br />
• The physical aspects of kidney failure.<br />
• The treatment of kidney failure.<br />
• Emotional effects.<br />
• Diet.<br />
• Financial implications.<br />
• Holidays.<br />
• Carers, partners, family & friends.<br />
• Support groups.<br />
<strong>Kidney</strong> Health Information<br />
http://www.kidneyresearchuk.org/index.phpoption=com_content&task=view&id=<br />
15&Itemid=32<br />
<strong>Kidney</strong> Health Information is a service for kidney patients, their families and<br />
carers, as well as medical professionals and researchers. The service is provided<br />
by <strong>Kidney</strong> Research UK and the information is available to everyone at no<br />
charge. It has a downloadable factfile section.<br />
Return to overview<br />
30
Cardiovascular Risk<br />
All patients with CKD have a greatly increased risk of developing heart disease<br />
and other diseases of blood vessels, including strokes. For many, this is more<br />
important than the danger of progressing to end-stage renal disease due to the<br />
10 fold increase in cardiovascular events and mortality at CKD stage 3.<br />
Furthermore, when events occur, mortality is higher for people with CKD and<br />
they have less favourable outcomes from intervention such as angioplasty. This<br />
increased risk begins at the very earliest stages, for example when there is<br />
microalbuminuria without a reduced eGFR. The prevalence of CKD at stage 3-5<br />
in the population is currently approximately 4.9%. However the prevalence of<br />
CKD at stages 4-5 is approximately 0.9%. The chief reason for the reduction of<br />
the numbers of people going on to stage 4 or 5 is due in the most part to their<br />
cardiovascular mortality at an earlier stage. For this reason reducing<br />
cardiovascular risk is of crucial importance to impact on mortality and as a<br />
progressing factor for further renal deterioration.<br />
For this reason, CVD risk calculators, including JBS2, are not recommended for<br />
use in calculating risk in patients with CKD. CKD at stage 3-5 is in itself a marker<br />
for CVD, therefore no calculation is needed and these patients should be<br />
considered high risk.<br />
Dyslipidaemia<br />
Patients with established macrovascular disease should receive treatment for<br />
hyperlipidaemia according to the current PCT Hyperlipidaemia Guidelines. Treat<br />
with simvastatin 40mg, aim for cholesterol of < 4mmol/l.<br />
Patients with diabetes and CKD but no established macrovascular disease<br />
should be offered lipid-lowering drug treatment according to the current PCT<br />
Hyperlipidaemia Guidelines.<br />
Patients with CKD who do not have diabetes and who do not have established<br />
macrovascular disease should be offered the options of lipid-lowering treatment<br />
according to the current PCT Hyperlipidaemia Guidelines if estimated 10-year<br />
risk of cardiovascular disease is ≥20%.<br />
Health Economy Formulary Drug of Choice - simvastatin 40mg.<br />
For further information see Dudley Guidelines for the Drug Treatment of<br />
Hyperlipidaemia. http://joint.dudley.nhs.uk/cmsextra/documents/cms/222-2008-2-<br />
22-5663216.pdf<br />
It would follow that patients with CKD should receive lipid therapy if they are<br />
considered to be at high risk. However, studies evidencing benefit from the use<br />
31
of statins such as HPS and ASCOT excluded patients with CKD therefore<br />
reliable evidence is not available. The Study of Heart and Renal Protection<br />
(SHARP) with a cohort of over 9000 patients will hopefully provide the evidence<br />
required. Until then, patients with CKD and no cardiovascular disease or diabetes<br />
should be treated with a statin if their 10 year CVD risk is > 20% (Renal<br />
Association). However, tables for calculating risk of CVD are not recommended<br />
for use in patients with CKD, but it would follow that due to their presenting<br />
condition, they would be considered at high risk of cardiovascular disease.<br />
Antiplatelet therapy<br />
Aspirin should be considered for all patients with an estimated 10 year risk of<br />
Cardiovascular (CVD) disease of >20%, so long as blood pressure is 50<br />
o Calculated to have a 10 year CVD risk of > 20%<br />
Health Economy Formulary Drug of Choice - aspirin dispersible 75mg OD<br />
See Aspirin Initiation Protocol<br />
Also see:<br />
Hypertension<br />
Lifestyle<br />
Primary Prevention of Cardiovascular <strong>Disease</strong> Protocol<br />
Return to overview<br />
32
Hypertension<br />
Blood pressure should be measured by a health care professional who has<br />
undergone training, using a machine which is regularly serviced and calibrated.<br />
The patient should be seated comfortably and relaxed with:<br />
• arm supported at chest level<br />
• ensuring correct cuff size is used ie. inner bladder fits 80 – 100% of the<br />
circumference of the upper arm.<br />
On the first visit:<br />
• BP should be measured in both arms and the arm with the higher<br />
reading used. This arm can then be noted and used for each<br />
subsequent visit.<br />
• At least 2 readings should be taken, with an interval of at least a<br />
minute between readings and an average of the readings recorded.<br />
• If the BP is above treatment threshold, (either systolic, diastolic, or<br />
both) check the BP again at the end of the consultation or after a short<br />
interval of 5 – 10 minutes, where patient remains seated comfortably.<br />
Target BP Range in CKD<br />
Aim for: Systolic of
If BP is above threshold, check this reading on 2 more visits 2 – 4 weeks apart or<br />
check home readings.<br />
If the BP trend is found to be above the treatment threshold as stated, a decision<br />
on initiating pharmacological management should be made. Inhibition or<br />
blockade of the renin/angiotensin/aldosterone system with ACE inhibitors or<br />
ARBs has been found to confer renal and cardio protection over and above the<br />
effects of their BP lowering effect. For this reason they are recommended as first<br />
line treatment for people with CKD.<br />
See Initiation of ACE/ARB.<br />
See Renal artery stenosis<br />
For non-pharmacological management discuss lifestyle measures as detailed in<br />
the “Best Practice Guidelines for Lifestyle Assessment” with particular attention<br />
to salt content in the diet and also in prescribed or OTC drugs.<br />
Note that in the checklist below for those with CKD the dietary advice differs from<br />
that which is usually recommended:<br />
• Fruit and vegetables are to be at a maximum of 5 portions a day due to<br />
their potassium content<br />
• Oily fish should be one portion only per week due to high phosphate<br />
levels.<br />
Lifestyle Measures Checklist<br />
• Stop smoking<br />
• Correct dyslipidaemia<br />
• Screen for diabetes<br />
• Maintain normal weight for adults (body mass index 20-25 kg/m2)<br />
• Avoid central obesity
Further information on the pharmacological management of hypertension can be<br />
found in the:<br />
“Dudley Guidelines for the Pharmacological Management of Hypertension”,<br />
http://joint.dudley.nhs.uk/cmsextra/documents/cms/222-2007-12-19-5392411.pdf<br />
For further information on taking blood pressure measurements, guides using<br />
electronic machines and anaeroid and mercury sphygmomanometers may be<br />
downloaded from the british hypertension society www.bhsoc.org<br />
For patients with T2 diabetes, please refer to NICE Guidelines, Inherited<br />
Guideline H “Management of Type 2 Diabetes: Management of Blood Pressure<br />
and Blood Lipids”<br />
http://guidance.nice.org.uk/page.aspxo=38564<br />
Return to overview<br />
35
Initiation of ACE Inhibitor / ARB<br />
ACE inhibitors and ARBs reduce hypertension in renal disease, but also confer<br />
major prognostic benefits over that which can be attributed to the reduction in<br />
blood pressure alone. For this reason they are recommended for use in CKD.<br />
Threshold for initiation – see hypertension<br />
Dual blockade with combinations of ACE and ARB should only be initiated under<br />
specialist supervision.<br />
Serum creatinine and potassium concentration should be checked<br />
• prior to starting ACE and/or ARB<br />
• within two weeks of initiation<br />
• two weeks after any subsequent dose increase<br />
• during severe intercurrent illness, particularly if there is a risk of<br />
hypovolaemia<br />
• annually (or more frequently if indicated, according to kidney function, see<br />
follow-up.)<br />
A rise of serum creatinine concentration of >20% or fall in estimated GFR of<br />
>15% after initiation or dose increase should be followed by a further<br />
measurement within two weeks.<br />
If deterioration in kidney function is confirmed, before the ACE or ARB is<br />
discontinued, a specialist opinion should be sought (not necessarily by<br />
formal referral) on whether the drug treatment should be stopped or the<br />
patient subjected to investigation for renal artery stenosis.<br />
If hyperkalaemia is present (K >6.0 mmol/l)<br />
• Stop relevant drugs, such as NSAIDs, K sparing diuretics.<br />
• Check diet, e.g. “low-salt” salt substitute discontinue use.<br />
If hyperkalaemia persists despite these measures, then advice should be sought<br />
from the nephrology dept on management with the ACE/ARB. Contact details<br />
Health Economy Formulary Drugs of Choice<br />
Lisinopril*<br />
Ramipril capsules<br />
Candesartan (not specific CKD licence)<br />
36
Irbesartan*<br />
Valsartan<br />
Losartan*<br />
*Specifically licensed for patients with type 2 diabetes and<br />
nephropathy/microalbuminuria.<br />
ARBs should be used as a second line treatment, only in patients who do not<br />
tolerate ACE inhibitors (usually due to development of persistent dry cough which<br />
does not disappear within two months of starting the ACE – check no other<br />
caveats).<br />
N.B Heart Failure<br />
The commonest fear for not using an ACE/ARB in patients with Heart Failure<br />
(HF) is the potential for worsening renal function. However, although the<br />
CONSENSUS trial demonstrated a 30% rise in Creatinine; the subsequent<br />
follow-up showed 19% returned to baseline and the ACE was generally well<br />
tolerated.<br />
Drug treatment with an ACE or ARB can contribute to hyperkalaemia, which can<br />
also be exacerbated by treatment with spironolactone (indicated in the treatment<br />
of heart failure).Severe hypovolaemia, may complicate the treatment of heart<br />
failure with high dose diuretics, as it may also cause hyperkalaemia in the<br />
presence of CKD, although in the presence of volume overload, diuretic<br />
treatment may be a logical treatment for hyperkalaemia. For these reasons,<br />
working out the cause and appropriate treatment of hyperkalaemia can be<br />
difficult, and a good reason for referral to / advice from a nephrologist.<br />
NSAIDs are associated with worsened outcomes in Heart Failure because they<br />
oppose the benefits of ACE by inhibiting the production of prostacyclin.<br />
Spironolactone should be avoided in patients with a GFR < 30 but can be used<br />
with caution in patients where eGFR is between 30 – 60 ml/min. It should be<br />
withheld in patients with diarrhoea and vomiting, who have heart failure and<br />
CKD, due to dehydration and hyperkalaemia.<br />
Spironolactone, ACE and ARB should be reduced or stopped if the serum<br />
potassium is greater than 6.0 mmol/l. This includes potassium sparing diuretics.<br />
http://www.renal.org/CKDguide/ckd.html<br />
37
K/DOQI Recommended Monitoring Intervals<br />
Salt Intake<br />
All patients with hypertension should be advised to reduce dietary sodium intake<br />
to
• Diuretics<br />
• Lithium carbonate<br />
• Mesalazine and other 5-aminosalicylic drugs<br />
• Calcineurin inhibitors (cyclosporin, tacrolimus)<br />
For further information see appendix 3 of the BNF.<br />
http://www.bnf.org/bnf/bnf/current/41003.htm<br />
or contact the Dudley Medicines Management team:<br />
CKD clinical services lead clair.huckerby@dudley.nhs.uk<br />
P.A. for the team Tel. 01384 366589<br />
Patients with CKD should be offered a 6 monthly medication review by a Practice<br />
Based Pharmacist if on 4 or more medicines. This could be more or less frequent<br />
depending on the needs of the individual patient.<br />
Return to overview<br />
Renal Artery Stenosis<br />
Suspect Atherosclerotic Renal Artery Stenosis (ARAS) in patients whom:<br />
• There is a rise in serum creatinine of > 20% or a fall in eGFR of > 15%<br />
during the first 2 months after initiation of ACE or after any dose increase.<br />
• A rise in serum creatinine of > 20% or a fall in eGFR of > 15% in a 12<br />
month period where there is evidence or suspicion of widespread<br />
atherosclerosis.<br />
• Refractory hypertension – where BP remains >150/90 despite 3<br />
antihypertensives.<br />
• Recurrent episodes of pulmonary oedema despite normal LV function on<br />
echocardiogram (flash pulmonary oedema)<br />
• Unexplained hypokalaemia with hypertension.<br />
These patients should receive referral to nephrology for further investigation and<br />
specialist management.<br />
Return to overview<br />
39
Urinalysis<br />
Protein<br />
No diabetes<br />
Proteinuria is a significant risk factor for progression in renal disease and for<br />
cardiovascular morbidity and mortality. Unlike haematuria, proteinuria almost<br />
always has a renal origin. Management should include assessment of:<br />
• Albumin/creatinine ratio (ACR) / Protein/creatinine ratio (PCR)<br />
• Haematuria<br />
• Serum creatinine and eGFR<br />
To detect and identify proteinuria, use ACR in preference, as it has greater<br />
sensitivity than PCR for low levels of proteinuria. For quantification and<br />
monitoring of proteinuria, PCR can be used as an alternative. ACR is the<br />
recommended method for people with diabetes.<br />
http://www.nice.org.uk/nicemedia/pdf/CG073QuickRefGuide.pdf<br />
Urine should be tested for protein annually in stage 3, and 6 monthly in stages 4<br />
and 5 if stable. If protein is detected, exclude infection (only if symptoms suggest)<br />
and retest.<br />
Measurements should not be made during acute illness.<br />
Send an early morning urine specimen for microalbumin and ACR level.<br />
Persistent proteinuria is defined as 2 or more positive tests, ACR > 30<br />
spaced by 1-2 weeks.<br />
A positive ACR test (>30) in the presence of hypertension indicates<br />
initiation of an ACE inhibitor<br />
http://www.nice.org.uk/nicemedia/pdf/CG073QuickRefGuide.pdf<br />
However, patients with CKD have an increased risk of CVD mortality.<br />
Consideration should be given to initiating ACE inhibitors in patients with CKD,<br />
positive microalbumin (< 30mg/day) and increased CVD risk, due to their<br />
cardioprotective effect.<br />
http://www.sign.ac.uk/pdf/sign103.pdf<br />
40
Recommendation:<br />
Therefore consider ACE inhibitor therapy regardless of established proteinuria for<br />
patients with CKD and:<br />
• Hypertension<br />
• Heart failure<br />
• Coronary, cerebral or peripheral vascular disease<br />
• Diabetes mellitus<br />
• Multi-system disease including SLE, rheumatoid arthritis, vasculitis<br />
For many in this patient group, the cardiovascular impact of their renal disease is<br />
more significant than the risk of continuing to end stage renal failure.<br />
http://renux.dmed.ed.ac.uk/edren/Unitbits/CKDmanagement.html<br />
see initiation of ACE/ARB<br />
Protein/creatinine ratio PCR<br />
PCR is the best test to confirm clinical proteinuria at higher levels. ACR at higher<br />
levels (> 45) may be inaccurate. If using PCR, then proteinuria is defined as<br />
Positive results: PCR > 50<br />
In 2 separate specimens spaced by 1-2 weeks.<br />
http://www.nice.org.uk/nicemedia/pdf/CG073QuickRefGuide.pdf<br />
ACR >70 (PCR 70 (PCR >100)<br />
• Refer to nephrologist.<br />
41
Diabetes<br />
All people with diabetes should receive annual assessment of microalbumin and<br />
albumin/creatinine ratio.<br />
If raised ACR :<br />
• ACR >2.5mg/mmol (male)<br />
• ACR >3.5mg/mmol (female)<br />
or<br />
• Microalbumin level > 30 mg/day<br />
Repeat test at next two clinic visits over 3–4 months<br />
Microalbuminuria is confirmed if at least one out of two or more results is also<br />
raised. http://www.nice.org.uk/nicemedia/pdf/CG66T2DQRG.pdf<br />
Microalbuminuria with eGFR >60ml/min/1.73m 2 is stage 1 / 2 CKD.<br />
In patients with diabetes (type 1 or type 2), microalbuminuria/proteinuria is an<br />
indication for:<br />
• Treatment with ACE inhibitors (or Angiotensin receptor blockers if those<br />
are not tolerated), with titration up to maximum dose or maximum<br />
tolerated dose irrespective of initial blood pressure<br />
• Control of hypertension to target<br />
• Tight glycaemic control<br />
• Monitoring of ACR, serum creatinine and eGFR.<br />
• Consider referral to / discussion with the diabetic team or joint<br />
diabetic/nephrology clinic for review<br />
• Consider referral to Nephrologist. See referral criteria<br />
Blood<br />
Microscopic haematuria without proteinuria, eGFR >60ml/min<br />
• Age >50, refer to Urology<br />
• Age 50 with negative urological investigations, treat as CKD<br />
stage<br />
Microscopic haematuria with proteinuria eGFR >60ml/min<br />
• Refer nephrology<br />
42
Lower levels of proteinuria should be monitored annually and patients managed<br />
according to CKD stage.<br />
Macroscopic haematuria<br />
(Use reagent strips and not microscopy)<br />
• Fast track Urology referral<br />
• If deteriorating function (eGFR), urgent nephrology referral; urgent<br />
imaging to exclude obstruction<br />
• If GFR
Diet in CKD<br />
Information on nutritional recommendations can be found on EdREN, the<br />
website of the Renal Unit of the Royal Infirmary of Edinburgh.<br />
http://renux.dmed.ed.ac.uk/EdREN/EdRenINFObits/Diet_CRF.html<br />
Summary of Downloads<br />
Keeping salt intake down<br />
Cutting Down Potassium<br />
A short leaflet about Fluid<br />
Controlling phosphate<br />
Increasing your calorie intake<br />
Weight control<br />
Renal Diets for Christmas and other holidays<br />
Return to overview<br />
44
Glycaemic Control<br />
CKD and Diabetes<br />
Diabetes mellitus is the most common cause of chronic kidney disease<br />
worldwide (Burrows-Hudson 2005) (Levy et al 2006) and at least 20-30% of<br />
people with diabetes will have some evidence of the disease (Audit Commission<br />
2002). There is a variation in the incidence of diabetes among racial and ethnic<br />
groups, with people of South Asian, African and African-Caribbean descent<br />
having a higher than average risk of type 2 diabetes (DOH 2001). The risk of<br />
nephropathy is related to the duration of diabetes with microalbuminuria being<br />
the first sign, progressing to albuminuria then nephropathy. The presence of<br />
urine albumin whether microalbuminuria or albuminuria strongly increases the<br />
person’s cardiovascular risk (University Hospital of Leicester 2006). Thereby a<br />
person with diabetes should not be assessed in isolation for kidney disease but<br />
also for lipid lowering, anti-platelet therapy and hypertension in tandem. Optimal<br />
glycaemic control should be the cornerstone of all treatment for diabetes care.<br />
For guidance please see Dudley Diabetes Management Guidelines for Adults<br />
2006.<br />
Persistent hyperglycaemia results in the thickening of the basement membranes<br />
and accumulation of proteins in the glomeruli (Levy et al 2006). Research studies<br />
suggest that intensive glycaemic control can reduce the rate of microalbuminuria,<br />
proteinuria and nephropathy (Gross et al 2005) and improvement in glycaemic<br />
control may reduce the risk of patients with diabetes developing both<br />
macrovascular and microvascular complications (DOH 2001). Studies relating to<br />
hypertension control also suggest similar results in relation to prevention of renal<br />
failure (DOH 2001) recommending the use of ACE inhibitors (Angiotension<br />
Converting Enzyme Inhibitors) or ARBs (Angiotension Receptor Blockers) to<br />
delay the onset of diabetic nephropathy in people with microalbuminuria.<br />
45
Screening and Management for People with Diabetes<br />
Annual urine analysis: Protein or<br />
Albumin Creatinine Ratio + U&Es<br />
and eGFR<br />
Follow<br />
urology/<br />
nephrology<br />
guidelines.<br />
Does patient have<br />
persistent haematuria<br />
YES<br />
NO<br />
Does patient have proteinuria YES Present on repeat<br />
test >2 weeks<br />
later<br />
NO<br />
Does patient have eGFR
References<br />
Audit Commission (2002) Testing Times: A Review of Diabetes Services in<br />
England and Wales.<br />
Burrows-Hudson (2005) <strong>Chronic</strong> <strong>Kidney</strong> <strong>Disease</strong>: an overview. American Journal<br />
of Nursing.<br />
DOH (2001) National Standard Framework for Diabetes: Standards. The<br />
Stationary Office. London<br />
Gross J.L., de Azevedo MJ, Silveiro S.P., Canani L.H., Caramori M.L.,<br />
Zelmanovitz T. (2005) Diabetic Nephropathy: Diagnosis, Prevention, and<br />
Treatment. Diabetes Care. 28, 1l 164-176.<br />
Levy J., Pussey C., Singh A. (2006) Fast Fact: Renal Disorders. Health Press,<br />
Oxford<br />
University Hospitals of Leicester NHS Trust (2006)<br />
Return to overview<br />
47
Immunisation Against Hepatitis B<br />
National Guidelines:<br />
“Immunisation against HBV is recommended for patients on dialysis or in<br />
transplantation programmes. Patients with chronic renal failure should be<br />
immunised as soon as it is anticipated that they may require dialysis or<br />
transplantation. Vaccine and, if appropriate, hepatitis B immunoglobulin should<br />
be given to susceptible patients who have been exposed to HBV.”<br />
Department of Health<br />
Good Practice Guidelines for Renal Dialysis/Transplantation Units 2002<br />
Prevention and Control of Blood-borne Virus Infection<br />
“Patients with CKD in whom dialysis is anticipated, should be screened for<br />
hepatitis B and C as well as HIV infection. Patients who are hepatitis B surface<br />
antigen and hepatitis B surface antibody negative should be immunised and their<br />
antibody levels measured post vaccination.”<br />
UK Renal Association Clinical Practice Guidelines 4th Edition 2007<br />
Clinical Practice Guidelines for the Care of Patients with <strong>Chronic</strong> <strong>Kidney</strong><br />
<strong>Disease</strong><br />
Immunisation Programme<br />
• Use standard course (0, 1, 6 months) and titre level taken 6 weeks after<br />
last dose<br />
• Recommended dose 40mcg<br />
• Intramuscularly in the upper arm<br />
Return to overview<br />
48
Influenza and Pneumococcal Vaccine<br />
All patients with CKD should be advised to have an influenza vaccine by the<br />
practice at the appropriate time each year. Efforts should be made to target the<br />
patients who appear on the CKD register.<br />
Pnuemococcal vaccine should also be offered to patients who remain<br />
unimmunised. This may be given at the same time as the influenza vaccine, but<br />
patients who have not received pneumococcal vaccine may be immunised at any<br />
time during the year.<br />
Contraindications, criteria and schedule for the flu and pneumococcal vaccine<br />
and can be found in product literature and in the British National Formulary<br />
• Influenza - http://www.bnf.org/bnf/bnf/current/6509.htm<br />
• Pneumococcal - http://www.bnf.org/bnf/bnf/current/6490.htm<br />
Guidelines for administration of the flu vaccine can be found in the “green book”,<br />
“Immunisation Against Infectious <strong>Disease</strong>s”.<br />
Return to overview<br />
49
Follow-up<br />
Suggested follow-up plan<br />
Stage <strong>Description</strong> Frequency<br />
3 eGFR 30 – 59 mls/min 6 monthly<br />
(12 monthly if<br />
stable*)<br />
4 eGFR 15 – 29 mls/min 3 monthly<br />
(6 monthly if<br />
stable*)<br />
5 eGFR < 15 mls/min 6 weekly<br />
*Stability = < 5mls/min fall in eGFR over 12 months<br />
Take the following steps to identify progressive CKD:<br />
• Obtain a minimum of three eGFR estimations over a period of not less<br />
than 90 days.<br />
• Define progression as a decline in eGFR of > 5 ml/min/1.73 m 2 within<br />
1 year, or > 10 ml/min/1.73 m 2 within 5 years.<br />
• Focus particularly on those in whom a decline of eGFR continuing at the<br />
observed rate would lead to the need for renal replacement therapy within<br />
their lifetime (eGFR
Stage 3<br />
Management at stage 3 should include all of the interventions as<br />
detailed for stages 1 and 2 plus the following section/s for stage 3.<br />
Management of Anaemia<br />
Lower levels of kidney function have been proven to be associated with lower<br />
haemoglobin levels and a higher prevalence and severity of anaemia.This is<br />
especially true in patients with diabetes and CKD. Anaemia can occur early in<br />
the course of diabetic kidney disease and is associated with inappropriately low<br />
erythropoietin concentrations 1 .<br />
In patients with chronic renal disease, normochromic normocytic anaemia may<br />
develop from decreased renal synthesis of erythropoietin. The anaemia becomes<br />
more severe as the GFR decreases 2 . No reticulocyte response occurs, red blood<br />
cell survival is decreased, and there is an associated increased bleeding<br />
tendency due to uraemia-induced platelet dysfunction.<br />
An eGFR of less than 60 ml/min (stage 3 onwards) should trigger investigation<br />
into whether anaemia is due to CKD. When the eGFR is greater than or equal to<br />
60 ml/min (stage 1 and 2) anaemia is more likely to be related to other causes 3 .<br />
All patients at stage 3 CKD should have an annual measurement of<br />
haemoglobin (Hb)<br />
If the Hb is < 11 g/dl<br />
Not all anaemia in patients with CKD will be ‘renal anaemia’ and causes of<br />
anaemia other than CKD should be actively excluded before a diagnosis of<br />
anaemia associated with CKD can be made 3 .<br />
Other causes:<br />
• <strong>Chronic</strong> blood loss<br />
• Iron deficiency<br />
• Vitamin B 12 or folate deficiency<br />
• Hypothyroidism<br />
• <strong>Chronic</strong> infection or inflammation<br />
• Hyperparathyroidism (consider referral for assessment)<br />
• Aluminum toxicity<br />
51
• Malignancy<br />
• Haemolysis<br />
• Bone marrow infiltration<br />
• Pure red cell aplasia<br />
(Iron deficiency anaemia is the most common cause of anaemia either due to<br />
negative iron balance through blood loss (most commonly gastrointestinal or<br />
menstrual), inadequate nutritional intake, or related to poor gastrointestinal<br />
absorption).<br />
Check:<br />
• full blood count (if not already done)<br />
• serum ferritin<br />
• total iron binding capacity<br />
• B 12 and folate<br />
• Other investigations will be determined by the likely alternative diagnoses<br />
and cardiovascular effects of anaemia, e.g. thyroid function test,<br />
echocardiography, cause of GI bleeding<br />
Serum ferritin<br />
Serum ferritin levels may be used to assess iron deficiency in people with CKD.<br />
Because serum ferritin is an acute-phase reactant and frequently raised in CKD,<br />
the diagnostic cut-off value should be interpreted differently to non-CKD<br />
patients 4 .<br />
Iron-deficiency anaemia should be:<br />
• diagnosed in people with stage 5 CKD with a ferritin level of less<br />
than 100 micrograms/l<br />
• considered in people with stage 3 and 4 CKD if the ferritin level is<br />
less than 100 micrograms/l.<br />
In people with CKD who have serum ferritin levels greater than100 micrograms/l,<br />
functional iron deficiency, (and therefore those patients who are most likely to<br />
benefit from intravenous iron therapy) should be defined by:<br />
• percentage of hypochromic red cells greater than 6%, where the<br />
test is available, or<br />
• transferrin saturation less than 20%, when the measurement of the<br />
percentage of hypochromic red cells is unavailable.<br />
Supplements of vitamin C, folic acid or carnitine should not be prescribed<br />
specifically for the treatment of anaemia of CKD.<br />
52
If all other causes for the anaemia have been excluded, (or where diagnosis<br />
is unclear) then referral may be indicated for assessment and possible<br />
initiation of Erythropoietin Stimulating Agent (ESA).<br />
References<br />
1. El Achkar et al. Higher prevalence of anemia with diabetes mellitus in<br />
moderate kidney insufficiency: The <strong>Kidney</strong> Early Evaluation Program<br />
(KEEP). <strong>Kidney</strong> International 2005; 67: 1483-8.<br />
2. National Health and Nutritional Examination Survey III (NHANES III) data<br />
cited in Royal College of Physicians. Anaemia Management in CKD:<br />
National Clinical Guideline for Management in Adults and Children.<br />
http://www.nice.org.uk/nicemedia/pdf/Anaemia_Management_full_guideline.pdf<br />
3. NICE clinical guideline 39: Anaemia Management in People with CKD<br />
http://www.nice.org.uk/nicemedia/pdf/AMCKD_NICE_guideline_v8.1.pdf<br />
4. Royal College of Physicians. Anaemia Management in CKD: National<br />
Clinical Guideline for Management in Adults and Children.<br />
http://www.nice.org.uk/nicemedia/pdf/Anaemia_Management_full_guideline.pdf<br />
Return to overview<br />
53
Stage 4<br />
Management at stage 4 should include all of the interventions as<br />
detailed for stages 1, 2 and 3 plus the following section/s for stage 4.<br />
Patients at CKD stage 4 should be referred for specialist nephrology opinion. For<br />
most patients management at this stage can be achieved by a shared care<br />
programme between the nephrology dept. and primary care, with the provision of<br />
a detailed shared care management plan from the nephrology team.<br />
Referral for patients at this stage with no other referral indication should be to the<br />
"One-Stop" renal clinic.<br />
“One-Stop” Renal Clinic<br />
Introduction:<br />
The “one-stop” renal clinic is an innovative and modern concept delivering health<br />
services designed around patients' needs and lifestyles. The clinics are an<br />
integral part of the drive towards building a patient-centred NHS, providing care,<br />
which minimises waits and delays, and removes unnecessary hospital visits.<br />
The service is committed to raising individual and community health status and<br />
awareness through high quality, evidence based screening, advisory, therapeutic<br />
and support services.<br />
A patient referred to a “one-stop” clinic will typically receive a specialist<br />
consultation, undergo diagnostic testing e.g. renal ultrasound, doppler,<br />
blood tests, basic echocardiography etc., receive their results in the clinic<br />
and have treatment initiated where appropriate.<br />
Clinic aims:<br />
• To provide seamless care and patient flows from primary to secondary care<br />
and vice versa.<br />
• Quicker, more convenient and timely diagnosis and investigation. Faster and<br />
better care, same day diagnostic tests etc.<br />
• Reduction in the number of hospital visits.<br />
• Reduction in patient anxiety levels associated with disease.<br />
• Smoother and quicker access to other specialties and health care<br />
professionals (eg. renal specialist dietician) if required.<br />
54
Clinic inclusion criteria:<br />
Patients can be referred directly by the GPs (Choose and book or paper<br />
referrals). Patients waiting for conventional appointment may be transferred to<br />
the “one-stop” clinic by the GP or Consultant if appropriate.<br />
The clinic is suitable for:<br />
• Elderly patients<br />
• Those with borderline eGFR where diagnosis may be unclear<br />
• Patients with borderline referral criteria<br />
• A specialist second opinion requested by the GP<br />
• A specific question requested rather than a formal referral<br />
Exclusion criteria<br />
The clinic is not suitable for established and/or advanced renal disease,<br />
which requires many diagnostic tests and long-term follow up.<br />
All patients who attend the “one-stop” clinic are sent a leaflet with their<br />
appointment letter explaining the range of tests they may have, how long the<br />
tests will take and when they can expect results. They are informed that they are<br />
very welcome to bring someone with them. The leaflet also contains contact<br />
numbers for the clinic coordinator should patients wish to access any further<br />
information or alter their appointment time.<br />
Patients benefit by completing their outpatient appointment with a timely and<br />
clear understanding of their diagnosis and management plan rather than<br />
experiencing weeks of uncertainty and apprehension whilst waiting for individual<br />
tests and results. Where immediate treatment is not feasible, the patient will be<br />
given a date for a further appointment before they leave and the referring primary<br />
care clinician informed.<br />
The clinic is currently held at Russells Hall hospital twice monthly with future<br />
plans for further expansion.<br />
For housebound patients this service can be requested as a domiciliary visit from<br />
the Community CKD Team, as an outreach service from Dudley Group of<br />
Hospitals. Portable scanning equipment is available for use by the team. It is<br />
recommended that patients are supported by a member of the primary care<br />
team, usually district nursing services, who meet the CKD team in the patient’s<br />
home. An individual shared care management plan is developed by the CKD<br />
team for use by primary care. Referral is by referral letter to Nephrology Services<br />
at Dudley Group of Hospitals.<br />
55
Contact details:<br />
Clinic co-ordinator<br />
Lead Clinician<br />
Renal Administrative Secretary<br />
Tel. 01384 244432, Fax. 01384 244543<br />
Claire.miles@dgoh.nhs<br />
Senior Consultant Renal Physician<br />
Tel. 01384 244432, Fax. 01384 244543<br />
Claire.miles@dgoh.nhs<br />
Consultants Tel. 01384 244432, Fax. 01384 244543<br />
Claire.miles@dgoh.nhs<br />
Renal Dieticians Tel. 01384 244017, Fax. 01384 244017<br />
Christine.morgan@dgoh.nhs<br />
Radiology Support Tel. 01384 456111 ext. 2541<br />
Peter.oliver@dgoh.nhs<br />
Out-Patient Manager Tel. 01384 456111 ext. 2406<br />
Rose.tonty@dgoh.nhs<br />
Return to overview<br />
Bone Metabolism<br />
Patients at stage 4 and 5 should have regular calcium, phosphate and<br />
parathyroid hormone (PTH) concentrations measured. Specimens need to be in<br />
path lab within 1 hour. Therefore it would be recommended that the specimens<br />
are taken at the phlebotomy clinic at Russells Hall Hospital. Blood requests<br />
should include:<br />
• Calcium phosphate<br />
• PTH<br />
• Bicarbonate (in selected patients)<br />
• Serum calcium and phosphate plus alkaline phosphatase (in selected<br />
patients)<br />
• 1,25 dihydroxycholecalciferol (in selected patients)<br />
It is recommended that the management of bone metabolism is carried out by<br />
specialist nephrologist, unless practices are confident to do so under advice from<br />
the nephrology dept. Investigations into bone metabolism are included in the<br />
one-stop clinic assessment and in the shared management plan with primary<br />
care.<br />
56
Where vitamin D supplementation is indicated:<br />
Stage 1 – 3A<br />
Initiate alfacalcidol 0.25mcg alternate days and titrate according to PTH and<br />
serum calcium and phosphate. Consider adcal / calcichew D3 1 twice daily in<br />
patients at risk of osteoporosis.<br />
Stage 3B - 5<br />
Initiate alfacalcidol, dose titrated according to PTH, serum calcium and<br />
phosphate and continue to monitor calcium and phosphate levels<br />
See Appendix 1 - <strong>Pathway</strong> for the Management of Calcium and Phosphate<br />
Balance in <strong>Chronic</strong> <strong>Kidney</strong> <strong>Disease</strong><br />
Osteoporosis – initiate biphosphonates in stages 1 – 3B<br />
Dudley PCT formulary drug of choice - Alendronate 70mg weekly<br />
N.B. Avoid if eGFR
At CKD stage 4 and 5:<br />
• Measurement of serum calcium, phosphate and PTH levels<br />
Return to overview<br />
58
Stage 5<br />
Patients identified at CKD stage 5 should be referred urgently for<br />
specialist management unless they are already known to the nephrology<br />
dept. Shared management plans should be agreed between primary and<br />
secondary care, especially for patients who chose to be treated<br />
conservatively and for those who are being worked up for renal<br />
replacement therapy.<br />
Exceptions to Referral<br />
• Patients with deteriorating kidney function as a consequence of another<br />
terminal illness<br />
• Patients for whom further investigation and management is clearly<br />
inappropriate<br />
• Patients with stable function with all appropriate investigations and<br />
interventions completed who have agreed and understood their individual<br />
care pathway.<br />
Shared care management should include:<br />
• 3 monthly follow-up where serum creatinine, eGFR, Hb, calcium, phosphate,<br />
PTH are monitored and acted upon including correction of acidosis.<br />
• Dietary assessment and advice/referral<br />
• Hepatitis B immunisation<br />
• Information and support for patient and family in treatment options<br />
• Timely provision of renal replacement therapy depending on patient choice<br />
Return to overview<br />
59
Referral<br />
Criteria for Referral to Specialist Nephrology Services According to eGFR<br />
eGFR mls.min<br />
Indication<br />
< 15<br />
Stage 5<br />
15 – 29<br />
Stage 4<br />
Urgent referral (exceptions)<br />
Referral to “one stop” clinic for assessment, investigations and<br />
shared management plan<br />
30 – 59<br />
Stage 3<br />
Routine referral/advice indications:<br />
• Where condition is not shown to be stable ie. progressive<br />
deterioration in kidney function<br />
• Microscopic haematuria<br />
• PCR >45 mg/mmol (ACR > 70mg/mmol)<br />
• Unexplained anaemia (Hb < 11)<br />
• Continuing abnormal potassium, calcium or phosphate levels<br />
despite advice in this pathway<br />
• Suspected systemic illness, e.g. SLE<br />
• Uncontrolled hypertension (>150/90 on 3 agents)<br />
> 60<br />
Stage 1 and 2<br />
Indications<br />
irrespective of<br />
eGFR<br />
Referral not required unless other problems present (see below)<br />
Immediate referral:<br />
• Accelerated hypertension<br />
• Hyperkalaemia (K > 7.0 mmol/l)<br />
Urgent referral<br />
• Nephrotic syndrome (proteinuria, oedema and low serum<br />
albumin)<br />
Routine referral<br />
• Dipstick proteinuria present and PCR >100 mg/mmol<br />
• Dipstick proteinuria and microscopic haematuria present<br />
• Macroscopic haematuria with negative urological testing<br />
• People with, or suspected of having, rare or genetic causes<br />
of CKD<br />
• Suspected renal artery stenosis.<br />
60
Information to include with referral<br />
• General medical history and details of co-morbidities<br />
• Urinary symptoms<br />
• Medication<br />
• Current blood pressure reading and all blood pressure readings over the<br />
last 2-3 years or back to normal levels, in date order, in graph form if<br />
available. If incomplete, send as much information as available<br />
• Current eGFR and serum creatinine levels and all levels over the last 2-3<br />
years or back to normal levels, in date order, or graph if available. If<br />
incomplete, send as much information as available.<br />
• Examination findings, e.g. oedema, palpable bladder<br />
• Urine dipstick results for blood and protein<br />
• PCR if proteinuria present. If no proteinuria present, microalbumin for all<br />
patients, plus ACR for diabetic patients.<br />
• U and E, FBC, albumin, calcium, phosphate, cholesterol. HbA1c if<br />
diabetic.<br />
• Results of any renal ultrasound scan if available.<br />
Once a referral has been made and a plan jointly agreed, consider routine<br />
follow-up in primary care rather than in the specialist clinic.<br />
Specify criteria for future referral / re-referral and when to seek advice.<br />
Renal Ultrasound<br />
Renal ultrasound is indicated in:<br />
• progressive CKD<br />
• visible or persistent invisible haematuria<br />
• symptoms of urinary tract obstruction<br />
• family history of polycystic kidney disease and are aged over 20<br />
• stage 4 or 5 CKD<br />
• nephrologist recommendation for renal biopsy.<br />
Advise people with a family history of inherited kidney disease about the<br />
implications of an abnormal result before arranging the scan.<br />
Return to overview<br />
61
Abbreviations<br />
ACE<br />
ARB<br />
ARF<br />
BP<br />
CAPD<br />
CKD<br />
DGoH<br />
DIP<br />
eGFR<br />
ERF<br />
ESA<br />
FBC<br />
GI<br />
GMS<br />
Hb<br />
KDOQI<br />
LIT<br />
MDRD<br />
NSAID<br />
OTC<br />
QMAS<br />
QOF<br />
RHH<br />
U+E<br />
UTI<br />
Angiotensin Converting Enzyme<br />
Angiotensin Receptor Blocker<br />
Acute Renal Failure<br />
Blood Pressure<br />
Continuous Ambulatory Peritoneal Dialysis<br />
<strong>Chronic</strong> <strong>Kidney</strong> <strong>Disease</strong><br />
Dudley Group of Hospitals<br />
Diabetes Improvement Partnership<br />
estimated Glomerular Filtration Rate<br />
Established Renal Failure<br />
Erythropoietin Stimulating Agent<br />
Full Blood Count<br />
Gastrointestinal<br />
General Medical Services<br />
Haemoglobin<br />
<strong>Kidney</strong> <strong>Disease</strong> Outcomes Quality Initiative<br />
Local Implementation Team<br />
Modified Diet in Renal <strong>Disease</strong><br />
Non- Steroidal Anti-Inflammatory Drug<br />
Over The Counter<br />
Quality Management and Analysis System<br />
Quality and Outcomes Framework<br />
Russell’s Hall Hospital<br />
Urea and Electrolytes<br />
Urinary Tract Infection<br />
Return to overview<br />
62
Appendix 1<br />
The Dudley Group of Hospitals<br />
NHS Trust<br />
<strong>Pathway</strong> for the Management of Calcium and Phosphate balance in<br />
<strong>Chronic</strong> <strong>Kidney</strong> <strong>Disease</strong> within Dudley Health Economy<br />
Rationale: Hyperphosphataemia (elevated serum phosphate) is recognised as an important risk factor for many adverse outcomes in dialysis<br />
patients, including vascular calcification, calciphylaxis, secondary hyperparathyroidism and mortality. Retention of phosphate occurs much earlier in<br />
the course of CKD. Serum phosphate concentration increases when eGFR falls below 30 mls/minute (CKD 4).<br />
Aim: To maintain phosphate levels between 0.9-1.5 mmol/L (1) and between 1.1 and 1.8 mmol/L in dialysis patients.<br />
Dietary Modification: Patients with CKD may need to follow a reduced phosphate diet. Phosphate rich foods include chocolate, nuts, dairy, eggs,<br />
meat and fish. This needs to be balanced carefully and so referral to a specialist dietitian is essential.<br />
If phosphate or intact PTH levels cannot be controlled within target range despite dietary phosphate restriction then prescribe a phosphate binder.<br />
Calcium containing phosphate binders<br />
1 st Line Choice:<br />
Calcium Carbonate (Calcichew®) 1.25g<br />
(Contains 500mg elemental calcium per tablet)<br />
Dose: To be titrated starting at 1 bd up to 2 tds<br />
with meals<br />
S/E: diarrhoea, hypercalcaemia<br />
Alternatives: Adcal ® 1.5g<br />
(Contains 600mg elemental calcium per tablet)<br />
or add D3 in those at risk of Osteoporosis with<br />
CKD stages 1-3<br />
2 nd Line Choice:<br />
Calcium Acetate (Phosex®) 1000mg<br />
Indication – hyperphosphataemia and<br />
intolerance to calcium carbonate or contraindicated.<br />
NB - contains less elemental calcium<br />
compared to calcium carbonate for the same<br />
phosphate binding capacity; this is also<br />
affected less by gastric pH.<br />
Dose: 1g tds with meals titrated according to<br />
serum phosphate levels, max 12 daily.<br />
S/E: nausea and vomiting, constipation.<br />
NB - Prescribing should be in line with an<br />
effective shared care agreement (ESCA)<br />
Calcium Acetate.doc<br />
* MONITORING<br />
Parameter<br />
Serum<br />
Phosphorous<br />
concentration<br />
Serum<br />
calcium<br />
concentration<br />
Frequency<br />
of<br />
Monitoring<br />
Every 2-4<br />
weeks until<br />
stable levels<br />
are reached<br />
and then 1-3<br />
months as<br />
directed by<br />
the clinician<br />
Target (KDOQI,<br />
Renal Association,<br />
recommendations<br />
for stages of CKD)<br />
CKD Stage 3/4 0.9 –<br />
1.5 mmol/l<br />
Dialysis 1.1 – 1.8<br />
mmol/l<br />
1-2 monthly CKD Stage 3/4 2.1 -<br />
2.6 mmol/l<br />
Dialysis 2.2 – 2.5<br />
mmol/l<br />
Ca x P CKD Stage 3/4 2.6 mmols/l<br />
SEVELAMER (RENAGEL®) 800mg<br />
Indication: hyperphosphataemia as monotherapy<br />
or in combination with calcium containing<br />
phosphate binder. May also decrease total and<br />
LDL cholesterol.<br />
Dose: 1 tds with meals, titrate dose according to<br />
calcium and phosphate balance, max 5 per<br />
meal.<br />
SE’s/CI: CI in hypersensitivity,<br />
hypophosphataemia, bowel obstruction, young<br />
children, gastroparesis, swallowing disorders.<br />
NB – Prescribing should be in line with an ESCA<br />
Sevelamer.doc<br />
OR<br />
LANTHANUM (FOSRENOL®)<br />
Indication: hyperphosphataemia<br />
NB – May be beneficial in those who are<br />
intolerant to sevelamer or where it is desirable to<br />
reduce the pill burden.<br />
Dose: 500mg, 750mg or 1000mg with meals<br />
titrated to 1500mg or 3000mg daily.<br />
S/E’s: Abdominal pain, constipation, diarrhoea,<br />
nausea and vomiting.<br />
NB – Prescribing should be in line with an ESCA<br />
Lanthanum.doc<br />
PRESCRIBING COSTS:- / DRUG<br />
INFORMATION<br />
Phosphate binders<br />
Calcichew 2tds £15.67<br />
Phosex 2tds £18.47<br />
Sevelamer 3tds £171.86<br />
Lanthanum 1tds 750mg £142.03<br />
Cost of 28 days<br />
treatment (BNF 56)<br />
63
SUPPORTING INFORMATION:<br />
Introduction:<br />
Phosphate retention occurs in chronic kidney disease due to the reduction in the glomerular filtration rate. Hyperphosphataemia leads to a series of changes<br />
resulting in secondary hyperparathyroidism. This is a major concern because the high parathyroid hormone (PTH) levels play an important role in the<br />
development of renal osteodystrophy and considered as a “uraemic toxin” as well.<br />
From the viewpoint of calcium and phosphate balance, initially the hypersecretion of PTH may be appropriate. This would increase the calcium and phosphate<br />
release from bone and enhances urinary phosphate excretion as well. It can thus correct the hypocalcaemia and to some extent hyperphosphataemia. However,<br />
when the glomerular filtration rate (GFR) falls below 30 mls/min, this physiological change is no more maintained. At this stage, dietary phosphate restriction<br />
may still reduce the plasma phosphate and PTH levels to an extent but may not normalise the values. As a result, oral phosphate binders are more often<br />
required. This problem gets worse once the renal failure is advanced, especially in dialysis patients. In end stage renal disease (CHD 5), there is essentially no<br />
phosphate excretion by the kidneys and oral phosphate binders are a must to limit the dietary phosphate absorption.<br />
The combination of hyperphosphataemia and calcium product (determined by multiplying plasma, calcium and phosphate in mmol/L) when in excess of 4.4,<br />
there is a tendency for calcium to precipitate in soft tissues such as arteries, joints and viscera. This phenomena can lead to various vascular complications<br />
including coronary artery disease and peripheral vascular disease. Thus both morbidity and mortality rate increases with these advanced complications.<br />
Phosphate restriction: Restricting phosphate intake can be attempted with about 800 to 1000mgs per day (1)which some patients find acceptable. However,<br />
care must be exercised as limiting phosphate intake significantly can reduce protein intake resulting in malnutrition which can also increase the morbidity and<br />
mortality. A Specialist Renal Dietitian’s advice will be very useful in balancing such a diet. Most often in dialysis patients, we encourage them to avoid<br />
unnecessary dietary phosphate products such as colas, certain vegetables and excessive dairy products. At the same time, high biological value protein<br />
sources must also be increased to avoid malnutrition. Lengthening the dialysis or using larger and high efficiency dialysers may influence very marginally the<br />
phosphate removal. Many patients with chronic <strong>Kidney</strong> disease and all dialysis patients require the administration of oral phosphate binders to limit the<br />
absorption of dietary phosphate. Agents used to regulate phosphate balance include calcium salts and more recently Sevelamer and Lanthanum carbonate.<br />
Magnesium and Aluminium containing binders are now avoided because of safety concerns.<br />
Phosphate binders – bind phosphate in the gut and prevent its absorption. They must be taken with phosphate containing foods to be effective, they should<br />
not be taken at the same time as iron preparations and some antibiotics because together they form insoluble compounds in the gut – which reduces the<br />
efficacy of both drugs.<br />
There is some evidence that calcium containing phosphate binders are related to arterial/vascular calcification when compared to non-calcium containing<br />
binders. Hypocalcaemia can also cause soft tissue calcification.<br />
Produced by:<br />
Jane Elvidge, Senior Renal Pharmacist, RHH<br />
Clair Huckerby, Pharmaceutical Adviser, Dudley PCT<br />
Dr K A Shiva Kumar, Consultant Renal Physician, RHH<br />
Christine Morgan, Senior Specialist Renal Dietitian, RHH<br />
Alison Whitlock, Clinical Pharmacist<br />
Lucy White, Administration, Public Health Dept. Dudley PCT<br />
In consultation with:<br />
AMMC<br />
Renal LIT<br />
References:<br />
1. Renal Association Guidelines for the treatment of adult patients with renal failure; 4th Edition.<br />
2. National <strong>Kidney</strong> Foundation. K/DOQI clinical practice guidelines for bone metabolism and disease in chronic kidney disease. AM J <strong>Kidney</strong> Dis 2003;<br />
42(Suppl 3): S1-S202.<br />
3. Summary of product characteristics for Sevelamer (Renagel).<br />
4. Block GA, Hulbert-Shearon TE, Levin NW, Port FK. Association of serum phosphorus and calcium x phosphate product with mortality risk in chronic<br />
haemodialysis patients: a national study. AM J <strong>Kidney</strong> Dis 1998; 31: 607-617.<br />
5. Goodman WG, Goldin J, Kuizon BD et al. Coronary-artery calcification in young adults with end stage renal disease who are undergoing dialysis. N<br />
Engl J Med 2000; 342: 1478-1483.<br />
6. Guerin AP, London GM, Marchais SJ, Metivier F. Arterial stiffening and vascular calcifications in end stage renal disease. Nephrol Dial Transplant<br />
2000; 15: 1014-1021.<br />
7. Hutchison A, Webster I. Lanthanum carbonate, a novel, non-aluminium, non-calcium phosphate binder, is effective and well tolerated in<br />
hyperphosphataemia. Poster presented at the 9 th Asian Pacific Congress of Nephrology, 16-20 February 2003, Pattaya, Thailand.<br />
8. Wilson J. ARIF request on the risk of cardiovascular problems in patients using calcium versus metal- free (non- calcium) phosphate binders to treat<br />
hyperphosphataemia. ARIF. University of Birmingham.<br />
64