Medicines Management Policy - Dudley Primary Care Trust
Medicines Management Policy - Dudley Primary Care Trust
Medicines Management Policy - Dudley Primary Care Trust
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
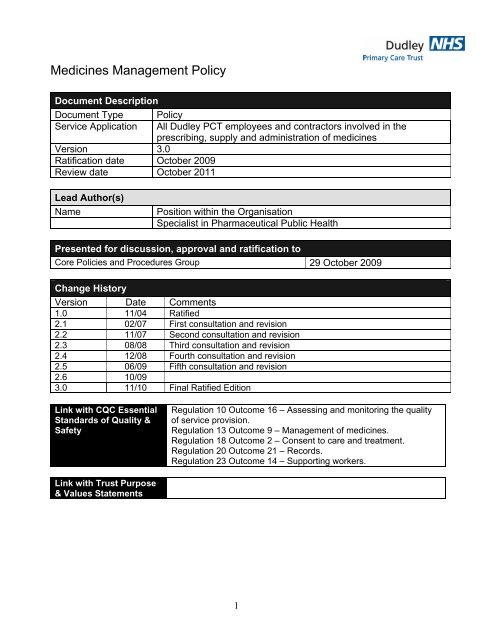
<strong>Medicines</strong> <strong>Management</strong> <strong>Policy</strong><br />
Document Description<br />
Document Type <strong>Policy</strong><br />
Service Application<br />
Version 3.0<br />
Ratification date October 2009<br />
Review date October 2011<br />
All <strong>Dudley</strong> PCT employees and contractors involved in the<br />
prescribing, supply and administration of medicines<br />
Lead Author(s)<br />
Name<br />
Position within the Organisation<br />
Specialist in Pharmaceutical Public Health<br />
Presented for discussion, approval and ratification to<br />
Core Policies and Procedures Group 29 October 2009<br />
Change History<br />
Version Date Comments<br />
1.0 11/04 Ratified<br />
2.1 02/07 First consultation and revision<br />
2.2 11/07 Second consultation and revision<br />
2.3 08/08 Third consultation and revision<br />
2.4 12/08 Fourth consultation and revision<br />
2.5 06/09 Fifth consultation and revision<br />
2.6 10/09<br />
3.0 11/10 Final Ratified Edition<br />
Link with CQC Essential<br />
Standards of Quality &<br />
Safety<br />
Regulation 10 Outcome 16 – Assessing and monitoring the quality<br />
of service provision.<br />
Regulation 13 Outcome 9 – <strong>Management</strong> of medicines.<br />
Regulation 18 Outcome 2 – Consent to care and treatment.<br />
Regulation 20 Outcome 21 – Records.<br />
Regulation 23 Outcome 14 – Supporting workers.<br />
Link with <strong>Trust</strong> Purpose<br />
& Values Statements<br />
1
Summary<br />
Medication is widely used in the health service to improve health, however there is a<br />
significant amount of legislation concerning its use while professional bodies have also<br />
issued good practice guidance on systems and processes. This policy describes the<br />
procedures and good practice that should be used when providing medication to a<br />
patient whether by prescribing, supplying or administering a product. It covers the<br />
legal and professional standards that are expected of different staff groups and the<br />
personal responsibility involved. It covers all aspects of the process from accurate<br />
prescription writing to safe administration of products. It been developed with the<br />
assistance of other partners including <strong>Dudley</strong> Metropolitan Borough Council and<br />
<strong>Dudley</strong> Group of Hospitals Foundation <strong>Trust</strong> to ensure that it is consistent with local<br />
arrangements where possible.<br />
This <strong>Policy</strong> should be read in conjunction with:<br />
1. The sections on 'Guidance on Prescribing' and 'Prescription writing' in the BNF<br />
(most recent edition)<br />
2. The Nursing and Midwifery Council Guidance for the administration of<br />
medicines (February 2008).<br />
3. The Nursing and Midwifery Council Code of professional conduct (April 2008)<br />
4. The Nursing and Midwifery Council Standards of proficiency for nurse and<br />
midwife prescribers (April 2006)<br />
5. <strong>Medicines</strong>, Ethics and Practice: a guide for pharmacists (most recent edition)<br />
6. Local policies and formularies as detailed in the document (These can be found<br />
in the Policies and Procedures section of the intranet)<br />
NB: This is a general policy covering any member of staff in PCT dealing with<br />
medicines. Individuals have a level of personal responsibility to read and<br />
understand this policy. Non-compliance with this policy may lead to<br />
performance management and disciplinary consequences. In very serious<br />
matters professional, civil and criminal legal consequences may occur also.<br />
Some areas are covered by more detailed local policies. It is the responsibility<br />
of managers and staff to ensure they follow the more detailed policies where<br />
they are applicable.<br />
2
CONTENTS<br />
Section<br />
Page<br />
1. Introduction 5<br />
2. Prescribing of medicines 7<br />
3. Supply of prescription Pads 15<br />
4. Security and Safe Handling of Prescriptions 17<br />
5. Obtaining medicines 18<br />
6. Transport of <strong>Medicines</strong> 19<br />
7. Storage and Security of <strong>Medicines</strong> 20<br />
8. Responsibilities of the Person administering<br />
the Medication 23<br />
9. Administration 24<br />
10. Controlled drugs 28<br />
11. <strong>Management</strong> of errors or incidents associated<br />
with medicines 35<br />
12. Verbal orders for the Administration of Medication 37<br />
13. Disposal of <strong>Medicines</strong> when off site 38<br />
14. Alcohol 39<br />
15. Illegal substances 40<br />
16. Theft 42<br />
17. General notes for the handling of medicines 43<br />
18. Patients at risk from Self-Poisoning 44<br />
19. Compliance aids 45<br />
20. Vaccines 46<br />
3
21. Syringe drivers 47<br />
22. Cytotoxic medicines 48<br />
23. Prescribing of oxygen 49<br />
24. Monitoring the <strong>Policy</strong> 50<br />
Supporting Documents 52<br />
Glossary 52<br />
Useful telephone numbers 52<br />
4
1. Introduction<br />
This policy deals with all aspects of the management and administration of<br />
medicines for patients/clients cared for by the <strong>Primary</strong> <strong>Care</strong> <strong>Trust</strong>. All <strong>Trust</strong> staff<br />
working within these areas are required to adhere to the procedures described<br />
within it. The policy has been compiled by a multi-disciplinary team and is<br />
intended to be used by all individuals, employed or contracted by the <strong>Trust</strong>, who<br />
deal with medicines within the <strong>Trust</strong> (including all locum and agency staff). It<br />
replaces all previous <strong>Medicines</strong> <strong>Management</strong> Policies.<br />
1.1 Overall Responsibility<br />
The following individuals are responsible for guidelines or training and<br />
information on all aspects of the safe and secure handling of medicines within<br />
the whole organisation and report directly to the Chief Executive for this<br />
purpose.<br />
<strong>Dudley</strong> <strong>Primary</strong> <strong>Care</strong> <strong>Trust</strong><br />
<strong>Dudley</strong> Provider Services<br />
All controlled drug issues<br />
Medical Director<br />
Managing Director of <strong>Dudley</strong> Community<br />
Services<br />
Accountable Officer<br />
1.2 Application and personal responsibility.<br />
This <strong>Policy</strong>, which contains the standards and procedures associated with the<br />
prescribing, administration, requisitioning and storage of medicinal products, is<br />
mandatory for all staff employed by and/or working within <strong>Dudley</strong> <strong>Primary</strong> <strong>Care</strong><br />
<strong>Trust</strong>, including those working on a sessional basis. Staff seconded to other<br />
organisations must abide by the standards of that organisation.<br />
It is the professional responsibility of each member of staff to update himself or<br />
herself on this <strong>Policy</strong> on at least an annual basis.<br />
Managers are responsible for ensuring that copies of this <strong>Policy</strong> are available to<br />
all their clinical staff and to ensure that they are fully aware of their<br />
responsibilities, competencies and procedures. It is good practice to include an<br />
update as part of each individual annual healthcare-staff appraisal. The <strong>Policy</strong><br />
is part of new healthcare staff induction and staff will have to sign that they<br />
have read and understood the policy. A recognition that staff have updated their<br />
knowledge of the policy will be included as part of annual appraisals.<br />
Consultants and clinical leads are responsible for ensuring that all medical<br />
officers in their team are fully aware of the key points in the <strong>Policy</strong> and are<br />
trained to be competent in all aspects of prescribing of medicines, as specified<br />
in the <strong>Policy</strong>.<br />
5
General Practitioners are responsible for ensuring that their practice operates a<br />
clear medicines management policy that covers all aspects of the use of<br />
medicines within their practice.<br />
6
2. Prescribing of medicines<br />
2.1 Introduction<br />
There are increasing numbers of types of prescribers and methods by which<br />
medicines can be authorised for administration to a patient/client. <strong>Medicines</strong>,<br />
which have not been authorised by a registered prescriber, must not be<br />
administered to patients/clients. This authorisation must be in writing, in the<br />
form of a prescription or Patient Group Direction (PGD), in advance of the<br />
administration of the medicine.<br />
2.2 Independent Prescribing<br />
All prescribers are expected to adhere to the <strong>Dudley</strong> Joint Formulary, wound<br />
care formulary and local prescribing guidelines.<br />
Definition of Independent Prescribing<br />
The Department of Health’s working definition of independent prescribing is<br />
prescribing by a practitioner (e.g. doctor, dentist, nurse, and pharmacist)<br />
responsible and accountable for the assessment of patients with undiagnosed<br />
or diagnosed conditions and for decisions about the clinical management<br />
required, including prescribing<br />
2.3 Non <strong>Dudley</strong> employed clinicians prescribing for inpatients on PCT sites.<br />
Where medical staff from <strong>Dudley</strong> Group of Hospitals, have been asked to<br />
assess a patient and wish to make a recommendation concerning medication,<br />
they should not write on the prescription sheet. Recommendations should be<br />
written in the patient records for addition to the prescription sheet by the<br />
patient’s own clinical team.<br />
2.4 Non-Medical Prescribers<br />
The introduction of prescribing by healthcare professionals other than doctors<br />
and dentists involves them working outside traditional boundaries. This policy<br />
aims to set out the administrative and procedural steps required by each<br />
healthcare profession now eligible to prescribe. It contains advice on good<br />
practice to ensure non-medical prescribers are practicing legally and safely<br />
within a supportive environment.<br />
It is necessary to develop non-medical prescribing guidelines within a Clinical<br />
Governance Framework to encompass quality, education and training, records,<br />
7
and clinical audit, in order to minimize risk and ensure that patients/clients<br />
receive the best quality care.<br />
All NMP must be approved and deemed competent by <strong>Dudley</strong> PCT before<br />
prescribing for a patient as part of their PCT employment.<br />
Registered prescribers now include:<br />
• Nurses who have undertaken the supplementary and/or the independent<br />
prescribers course and are registered as such with the Nursing and<br />
Midwifery Council.<br />
• All Registered Pharmacists who have undertaken the independent<br />
prescribers course and are registered as such with the Royal<br />
Pharmaceutical Society of Great Britain (RPSGB) and approved by the<br />
PCT.<br />
• Supplementary prescribers are health professionals who have undertaken a<br />
further qualification and are registered as such with their professional body.<br />
These prescribers can prescribe within a clinical management plan for<br />
individual patients, in conjunction with an independent prescriber (currently<br />
only applies to medical practitioner/dentist) and the patient. These<br />
professionals can be 1 st level nurses, pharmacist, chiropodists/podiatrists,<br />
physiotherapists and radiographers (Allied Health Professionals - AHP). All<br />
prescribers must comply with current legislation for prescribing and be<br />
accountable for that practice.<br />
Exceptions to this are as follows:<br />
• In areas where there are no resident prescribers and in cases of<br />
exceptional clinical urgency a verbal instruction is acceptable. (See section<br />
12)<br />
• Certain medicines may be administered following Patient Group Directions<br />
approved by the PCT Prescribing Sub Committees. Criteria for supply and<br />
administration under a PGD will be defined within the respective PGD.<br />
• State registered chiropodists may supply or administer medicines specified<br />
in the <strong>Medicines</strong> Act 1968, and in orders made under the Act, providing they<br />
also hold a certificate of competence in the use of the medicines, issued by<br />
or with the approval of the Chiropodist Board. The supply or administration<br />
shall be only in the course of their professional practice.<br />
Medical Students or Clinical Attachments are not permitted to<br />
prescribe medicines.<br />
2.4.1 What a Nurse or Pharmacist independent prescriber can prescribe<br />
8
Nurse and Pharmacist Independent Prescriber may prescribe any licensed<br />
medicine for any medical condition that the nurse or pharmacist is competent to<br />
treat. This allows access to virtually the whole of the British National Formulary<br />
with the exception of Controlled Drugs and unlicensed medicines.<br />
Current legislation allows nurses to prescribe some controlled drugs (see<br />
section 10) but at present this does not apply to pharmacists.<br />
2.4.2 What a Community Practitioner Prescriber can prescribe<br />
The items that may be prescribed are listed in the British National Formulary<br />
(BNF) or Drug Tariff.<br />
2.4.3 Supplementary Prescribing by Nurses, Pharmacists,<br />
Chiropodists/Podiatrists, Physiotherapists and Radiographers.<br />
Definition of Supplementary Prescribing<br />
Supplementary prescribing is a voluntary prescribing partnership between the<br />
independent prescriber (doctor or dentist) and supplementary prescriber to<br />
implement an agreed patient-specific clinical management plan (CMP), with the<br />
patient’s agreement.<br />
2.4.4 What a Supplementary Prescriber can prescribe<br />
Following agreement of the CMP, the supplementary prescriber may prescribe<br />
any medicine for the patient that is referred to in the plan, until the next review<br />
by the independent prescriber. There is no formulary for supplementary<br />
prescribing, and no restrictions on the medical conditions that can be managed<br />
under these arrangements.<br />
This mechanism of prescribing will be helpful for nurse and pharmacist<br />
prescribers when they are newly qualified. It will also be appropriate in specific<br />
situations, for instance<br />
- When working within a team where a doctor is accessible<br />
- For specific long-term conditions<br />
- For situations involving Controlled Drugs.<br />
Supplementary Prescribers can prescribe Controlled Drugs and unlicensed<br />
medicines in partnership with a doctor, where the doctor agrees within a<br />
patient’s CMP. From July 2006 chiropodists/podiatrists physiotherapists and<br />
radiographers are also able to prescribe Controlled Drugs as supplementary<br />
9
prescribers, but only where there is a patient need and the doctor has agreed in<br />
a patient’s CMP.<br />
More detailed information on supplementary prescribing can be found on the<br />
Department’s web site: www.dh.gov.uk/supplementaryprescribing.<br />
2.5 Patient Group Directions<br />
A Patient Group Direction (PGD) is defined as a written instruction for the<br />
supply or administration of medicines to a group of patients who may not be<br />
individually identified before presentation for treatment. It is not a form of<br />
prescribing.<br />
Further guidance on the use of PGDs can be found in the <strong>Trust</strong> <strong>Policy</strong><br />
document ‘Patient Group Directions General <strong>Policy</strong> for the Supply and<br />
Administration of Medicinal Products by Approved Practitioners (Non- Medical)’.<br />
2.6 Clinical Awareness and Competence of person writing prescription<br />
2.6.1 The healthcare professional must be aware of, and able to demonstrate<br />
knowledge of, the action of the prescribed item, the usual dosage, the common<br />
side effects, interactions, local prescribing guidelines, current evidence and how<br />
these relate to the treatment of the individual patient/client overall. They should<br />
be familiar with sources of information about medication such as the BNF.<br />
Whenever possible, prescribers should have access to the patient’s current<br />
medical record.<br />
2.6.2 As part of their continuing professional development standard as laid down by<br />
their professional body. The healthcare professional must make every<br />
reasonable effort to maintain and develop knowledge of the common<br />
medications used in his/her area of practice. This knowledge should include<br />
awareness of;<br />
a) The signs of adverse drug reactions (ADR) to medication and the actions<br />
to be taken should this occur.<br />
b) Reactions that may occur when different medicines are combined.<br />
c) Contra-indications<br />
2.7 Writing Prescriptions<br />
Prescriptions written by doctors or other authorised prescribers employed by<br />
<strong>Dudley</strong> <strong>Primary</strong> <strong>Care</strong> <strong>Trust</strong> must conform to the following guidelines.<br />
10
2.7.1 Clarity<br />
The prescription form or medication record card must clearly state the required<br />
patient/client’s details i.e.<br />
Name<br />
Age & Date of birth (N.B. legal requirement for Prescription Only<br />
Medicine (POM) if under 12)<br />
Address<br />
NHS number<br />
Each item must be clearly written in blue or black indelible ink, preferably using<br />
block capitals. Prescriptions must be computer generated where possible.<br />
2.7.2 Generic Prescribing<br />
<strong>Medicines</strong> should be prescribed using approved (generic) name where<br />
possible. Where bioavailability is important the patient/client should continue to<br />
receive the same brand: in such cases, the manufacturer’s brand name should<br />
be stated. Examples are listed in the BNF e.g. anticonvulsants, lithium,<br />
theophyllines.<br />
2.7.3 Requirements for Prescription Pricing Division (PPD) prescriptions e.g.<br />
FP10<br />
Each item must include the following;<br />
• name of drug (approved name)<br />
• metric dosage<br />
• frequency<br />
• form and strength<br />
• route to be used<br />
• clear directions as to any site of application of treatment must be present.<br />
• be signed and dated by the prescriber – NB name of prescriber should be<br />
printed beside signature.<br />
• PCT and practice code<br />
• PCT practice address<br />
• contact telephone number<br />
• prescriber code for non-medical prescriber<br />
11
2.7.4 Requirements for in-patient treatment cards<br />
• name of drug (approved name)<br />
• metric dosage<br />
• frequency<br />
• form and strength<br />
• route to be used<br />
• clear directions as to any site of application of treatment must be present.<br />
• be signed and dated by the prescriber<br />
• time of administration (in 24 hour clock)<br />
• PCT Unit (e.g. ward, house etc)<br />
• unit number<br />
• consultant<br />
• drug sensitivities (including writing ‘none’ if none known)<br />
2.7.5 Documentation of Allergies/Hypersensitivities<br />
All treatment cards must specify whether or not the patient has any drug<br />
allergies/hypersensitivities. It is the responsibility of the admitting medical/dental<br />
officer to record these on the prescription sheet as well as in the medical notes.<br />
Medical officers, pharmacists and nurses may also document any that become<br />
apparent during the in-patient stay.<br />
2.7.6 Errors<br />
When an error is made in writing a prescription, the incorrect information must<br />
be struck out with a single line, signed by the prescriber and the correct<br />
information written in a new section.<br />
2.7.7 The following points should be noted when prescribing strengths and<br />
quantities<br />
i) unnecessary use of decimal points should be avoided, e.g. 3mg, not 3.0mg<br />
ii) quantities less than 1 gram should be written in milligrams, e.g.500mg, not<br />
0.5g<br />
iii) quantities less than 1mg should be written in micrograms,<br />
e.g.100micrograms, not 0.1mg.<br />
iv) a zero should be written in front of a decimal point where there is no other<br />
figure, e.g. 0.5ml, not .5ml<br />
v) 'micrograms', 'nanograms' and 'units' should not be abbreviated<br />
12
2.7.8 Recognised abbreviations<br />
Only the following abbreviations are recognised within the health economy. All<br />
other regimens must be written out in full or followed according to an agreed<br />
protocol.<br />
Dose<br />
OD Once daily<br />
OM Each morning<br />
ON Each night<br />
BD Twice daily<br />
TDS Three times daily<br />
QDS Four times daily<br />
Mane Morning<br />
Nocte At night<br />
For patient records<br />
Route<br />
Ext<br />
IM<br />
Inh<br />
IV<br />
O<br />
PO<br />
NG<br />
Neb<br />
PR<br />
PV<br />
SC<br />
S/L<br />
Top<br />
PEG<br />
External use<br />
Intramuscular<br />
Inhalation<br />
Intravenous<br />
By mouth<br />
By mouth<br />
Nasogastric tube<br />
Nebulisation<br />
Per rectum<br />
Per vagina<br />
Subcutaneous<br />
Sublingual<br />
Topical<br />
PEG feed<br />
Depot injections should be prescribed with the interval expressed using the<br />
term “every” (e.g. ‘every 3 weeks’ rather than ‘3 weekly’, which can be<br />
misinterpreted. This can be abbreviated as every 3/52)<br />
In the case of “when required medicines” the prescription should state the<br />
circumstances when it is to be used/taken, the maximum number of doses to be<br />
given and specify a time interval e.g. 4 hourly and where appropriate the<br />
maximum dose in 24 hours. The criteria where a doctor must be contacted<br />
should also be noted if appropriate.<br />
Errors have occurred in both the dispensing and administration of<br />
unclear prescriptions and for that reason the use of abbreviations such as<br />
mdu and prn must not be used and clear directions written as above.<br />
13
2.8 Prescribing Controlled Drugs- see section 10.<br />
2.9 How to report a suspected ADR i.e. use of the yellow card system.<br />
If a patient suffers a suspected adverse reaction to a prescribed, over-thecounter<br />
(General Sales List) or herbal medicine, the adverse reaction should be<br />
reported via the Yellow Card Scheme.<br />
The Yellow Card Scheme is a voluntary scheme through which healthcare<br />
professionals notify the <strong>Medicines</strong> Control Agency (MCA)/Committee on the<br />
Safety of <strong>Medicines</strong> (CSM) of suspected adverse drug reactions (ADR’s). The<br />
MCA/CSM encourage the reporting of ADR’s to newly licensed medicines that<br />
are under intensive monitoring (identified by a ▼ symbol both on the product<br />
information for the drug and in the BNF and MIMS) and all serious or<br />
unexpected suspected ADRs to all other established drugs.<br />
Serious reactions include those that are fatal, life-threatening, disabling,<br />
incapacitating or which result in prolonged hospitalisation and/or are medically<br />
significant e.g. teratogenicity. The new electronic Yellow Card provides a simple<br />
and fast way to report suspected ADRs. The electronic Yellow Card, together<br />
with instructions on how to use it, is available on the MCA website<br />
(www.mca.gov.uk).<br />
Health professionals are encouraged to report all suspected ADRs using this<br />
method, although hard copy Yellow Cards are also acceptable (and can be<br />
found bound to the back of the BNF and Drug Tariff. All ADRs must be<br />
recorded in the patients Medical Records. The supplementary prescriber should<br />
also inform the independent prescriber of any reported ADRs.<br />
14
3. Supply of prescription Pads<br />
N.B. The prescription pad and forms are the property of the <strong>Primary</strong> <strong>Care</strong> <strong>Trust</strong>.<br />
Prescriptions must only be issued to patients for whom <strong>Dudley</strong> PCT holds<br />
responsibility. It is the responsibility of the prescriber to ensure the security of<br />
the pad/form at all times. (For further information see section 4)<br />
Please also refer to section 7 and appendix 5 in the Facilities <strong>Management</strong><br />
Centre (FMC) Procurement and Facilities Department, “Controlled Stationery<br />
Procedures Manual.”<br />
3.1 For Non Medical Prescribers employed by <strong>Dudley</strong> PCT<br />
3.1.1 The NMP is responsible for supplying details of registration status to their line<br />
manager.<br />
3.1.2 Prior to commencing prescribing, the line manager or designated member of<br />
staff will ensure that the member of staff has access to NMP resource pack<br />
http://joint.dudley.nhs.uk/cmsextra/Pharmacy-Prescribing-<br />
<strong>Medicines</strong>/index.aspid=7286 and the NMP lead has been informed so as to<br />
update the NMP prescribing database.<br />
3.1.3 The line manager is responsible for ensuring the PPD is notified by completing<br />
an Annex Form 1 (version 3) for the notification of newly qualified Non medical<br />
Prescribers/Change in circumstances. This can be done by the FMC. For NMPs<br />
employed within General Practice, this will be done through the GP system via<br />
the Warehouse Manager at the FMC, Pensnett Trading Estate by completing<br />
Annex Form 2 (version 3). For details on nurse prescribing forms please see<br />
www.ppa.org.uk/ppa/Pct/nurses/pctNurse.htm<br />
3.1.4 Once the NMP is registered with the PPD the line manager will order<br />
prescription pads, firstly via telephone to the supplier and confirming this on the<br />
proforma for ordering FP10 secure prescription pads. See Appendix 1 to<br />
<strong>Medicines</strong> <strong>Management</strong> <strong>Policy</strong> 2.4 dec 08 doc.xls<br />
3.1.5 When the prescription pads arrive the line manager will give out a maximum of<br />
2 pads to each NMP (for nurses employed by General Practitioners, pads will<br />
be forwarded to the appropriate surgery via the GP courier system). The line<br />
manager will record the first and last serial number of each pad and also the<br />
signature of the person issuing and receiving the pad. The Practice Manager<br />
will record appropriate details on attached paperwork that should be returned<br />
within 72hrs of receipt. A copy must be maintained by the Warehouse Manager<br />
15
& Practice Manager on a file. Note: For security reasons pads can only be<br />
collected in person by the NMP.<br />
3.1.6 Any un-issued prescription pads must be kept in a locked cupboard and treated<br />
as controlled stationery.<br />
.<br />
3.1.7 Prescription forms will be supplied in pads of 50 forms from an approved<br />
supplier. The pads will be ready personalised, with the nurse prescribers<br />
details.<br />
3.1.8 Any NMP who is employed by more than one PCT or GP Practice must have<br />
separate prescription pads for each organisation. It is the prescriber’s<br />
responsibility to ensure that all prescriptions are endorsed with the correct<br />
practice code.<br />
3.1.9 All NMPs will be reviewed regularly using the NMP prescribing competency<br />
framework to ensure competency.<br />
3.2 Medical Prescribers employed by <strong>Dudley</strong> PCT<br />
Medical prescribers must order prescription pads for the service they are<br />
prescribing for via the line manager in charge of the service. The line manager<br />
will record the first and last serial number of each pad and also the signature of<br />
the person issuing and receiving the pad. The line manager will record<br />
appropriate details on attached paperwork that should be returned within 72hrs<br />
of receipt. A copy must be maintained by the Warehouse Manager & line<br />
manager on a file. Note: For security reasons pads can only be collected in<br />
person by the prescriber.<br />
16
4.0 Security and Safe Handling of Prescriptions<br />
Thefts and losses over recent years of prescription forms in general have<br />
dramatically increased and the security of prescription forms are the<br />
responsibility of the prescriber. Stock levels of the forms held should be kept to a<br />
minimum.<br />
4.1 General security<br />
The prescription form must only be produced when needed and never left<br />
unattended. When not in use they must be placed in a locked drawer/secure<br />
stationery cupboard. When on patient visits the prescriber must keep the<br />
prescription pad on their person. Prescription forms should never be left in a car.<br />
If prescription pads are taken off PCT premises, they must be kept safe and<br />
secure from other family members and visitors. Under no circumstances<br />
should blank prescription forms be pre-signed before use.<br />
4.2 In the event of loss or suspected theft.<br />
All prescribers should follow the procedures below:<br />
• The prescriber should immediately contact their line manager. For community<br />
nurses this will be their line manager and for practice nurses, their practice<br />
manager.<br />
• The manager will then inform the Personal Assistant to Specialists in<br />
Pharmaceutical Public Health, (SiPPH) <strong>Dudley</strong> <strong>Primary</strong> <strong>Care</strong> <strong>Trust</strong><br />
Direct Line: 01384 366589, Fax: 01384 241115<br />
• The Personal Assistant will then inform the Head of Security, the Counter Fraud<br />
Specialist and activate the cascade system by notifying the local community<br />
pharmacists through the “Early Warning System”.<br />
• A Senior Pharmacist will review the circumstances and decide upon any<br />
necessary additional action.<br />
• Prescribers will be asked to temporarily write/sign prescriptions in red or green<br />
coloured ink.<br />
• The incident must be logged on Sentinel.<br />
• The police should also be informed by the manager as soon as possible after<br />
the loss/theft is confirmed, giving details of the approximate number of<br />
prescriptions stolen, their identification numbers, and where and when they<br />
were stolen.<br />
• A crime reference or loss reference number should be recorded against each<br />
incident.<br />
4.3 Recording of prescription numbers<br />
It is good practice at regular intervals to note the prescription number issued to<br />
a patient in the patient’s notes so that should prescription pad or individual<br />
prescription be stolen the prescriber is able to indicate how many forms have<br />
been taken.<br />
17
5. Obtaining <strong>Medicines</strong><br />
<strong>Medicines</strong> may be obtained from the Hospital Pharmacy Service or a<br />
Community Pharmacy depending on the system in place for each Community<br />
Service.<br />
5.1 Obtaining medicines via the Hospital Pharmacy Service.<br />
<strong>Medicines</strong> may be obtained from the Hospital Pharmacy via Pharmacy top-up<br />
system or presentation of a signed written order. A signed written order may<br />
either be a prescription signed by a doctor or other authorised prescriber, or a<br />
stock requisition signed by the nurse in charge. Any signature must have the<br />
name of person printed beside it. Staff collecting medicines must present ID<br />
badges.<br />
5.1.1 All order books and blank order forms must be stored in a secure place to<br />
prevent unauthorised access. Only one stock and one Controlled Drug book<br />
may be in use and held by each clinical area at any one time.<br />
5.1.2 All drug requisitions must travel to and from the pharmacy department in sealed<br />
tamper evident containers or by a person authorised by the registered nurse in<br />
charge.<br />
5.1.3 When requisitioning an order all remaining blank lines must be cancelled out<br />
before signature. Completed requisition forms and requisition books must be<br />
retained in the requesting department for two years from the date of order or<br />
date of last entry.<br />
5.2 Obtaining <strong>Medicines</strong> from a Community Pharmacy<br />
Some services have Service Level Agreements for the supply of medicines<br />
from other suppliers. All ordering must be done as specified under the SLA with<br />
authorised signatures and a robust monitoring arrangement.<br />
18
6. Transport of <strong>Medicines</strong><br />
6.1 All medicines will be transported in such a manner as to prevent loss or improper<br />
use.<br />
6.2 If a messenger service (e.g. porter, driver) is used the medicines will be<br />
contained in a sealed tamper evident satchel or other sealed container and kept<br />
in charge of the messenger until handed to the individual in charge.<br />
6.3 When items requiring refrigeration are transported, care must be taken to<br />
maintain the cold chain.<br />
6.4 If medicines are being transported by non-clinical members of PCT staff or Social<br />
Services staff they must have received training in the safe transport of medicines<br />
and follow the guidance in section 7.6 below.<br />
6.5 Community Nurses may act as the patient/client’s representative in collecting<br />
prescription medicines from a Pharmacy. This should only be done in<br />
circumstances where it is essential for the patient/client’s immediate treatment.<br />
A Community Pharmacy delivery service must be used, where available, when<br />
the patient/client has difficulty collecting their medication or returning items no<br />
longer required.<br />
6.6 Members of staff transporting medicines, including dressings, should:<br />
i) Carry the absolute minimum stock required.<br />
ii) Carry the medicines in such a manner as not to be obvious.<br />
iii) Whenever possible, travel direct to the place where the medicines are to<br />
be administered but in any case within that span of duty N.B. CDs<br />
(controlled drugs) must be delivered immediately once collected.<br />
Avoid leaving medicines unattended in a vehicle unless in very<br />
exceptional circumstances. Where it is necessary to leave medicines in<br />
a vehicle they must always be stored out of sight and the vehicle locked.<br />
iv) Return directly back to the site of storage with any unused medicines.<br />
<strong>Medicines</strong> or products prescribed for an individual patient on a PPD<br />
(Prescription Pricing Authority e.g. FP(10)) prescription form must be left<br />
with the patient since it is their property.<br />
v) Record when and where medicines have been transported.<br />
6.7 Used syringes, needles and any part used injections must be discarded into a<br />
suitable sharps container prior to transporting back to base. Please refer to<br />
PCT Sharps <strong>Policy</strong>.<br />
19
7. Storage and Security of <strong>Medicines</strong><br />
(See also PCT security policy)<br />
http://joint.dudley.nhs.uk/cmsextra/documents/cms/489-2008-8-5-3796510.pdf)<br />
7.1 For each area of PCT managed service, the manager responsible for the<br />
service is responsible for the safe storage, custody and administration of all<br />
medicines used within her/his area, in accordance with this policy.<br />
7.2 All medication on <strong>Trust</strong> property must be stored in a locked cupboard, drug<br />
trolley or refrigerator designated for the sole purpose of storing medication. In<br />
exceptional circumstances and where there are no other facilities, small<br />
quantities of a patient’s own medication may be stored in a locked drawer as a<br />
temporary measure. These storage facilities must be kept locked at all times.<br />
7.3 There should be a single key for each lockable storage facility with a duplicate<br />
key stored in a designated safe area or with a senior manager. Loss of keys<br />
must be reported to the line manager on duty who will arrange an investigation<br />
and change of locks or authorise temporary use of a second set of keys. When<br />
drug cupboards and/or their locks are replaced or new keys cut for drug<br />
cupboards this must be done only following verbal authorisation from the senior<br />
manager responsible for the service and the incident must be logged on<br />
Sentinel. The senior manager must inform the Pharmaceutical Advisor and<br />
<strong>Trust</strong> Security Officer at the earliest opportunity. Any new key must be<br />
managed as in 7.3.<br />
7.4 The safe keeping and whereabouts of the drug cupboard keys is the<br />
responsibility of the most senior person on duty. Wherever possible the drug<br />
cupboard keys should be held personally by the senior officer in charge. If this<br />
is impractical the drug cupboard keys must be stored in a designated place of<br />
safekeeping and be managed in such a way (i.e. record signatures as key is<br />
issued and returned) to prevent unauthorised access. Duplicate keys must be<br />
stored in a similar manner, preferably in a different designated place of<br />
safekeeping.<br />
7.5 Preventing unauthorised access to keys is of paramount importance and the<br />
location of key storage (including the duplicate key) should be approved and<br />
documented by the manager responsible for the service.<br />
7.6 When a unit where medicines are stored is temporarily not involved in the<br />
active treatment of patients/clients or closed e.g. overnight or weekend, the<br />
drug cupboard keys must be returned to their designated place of safe keeping<br />
and secured in such a manner to prevent unauthorised access. Where the<br />
duration of closure is longer than overnight or a weekend the advice of the<br />
manager responsible must be sought.<br />
20
7.7 All medicines shall be returned to lockable medicine cupboards when not in use<br />
except for emergency drug kits e.g. Cardiac Arrest Boxes, which shall be stored<br />
in a manner not obvious to the general public.<br />
7.8 Stocks must be checked on a monthly basis for out of date items. Except for<br />
controlled drugs, all out of date medicines generated by healthcare<br />
professionals, must be disposed of in the waste container and transported back<br />
to the base/clinic for collection via the waste collection service for surgeries and<br />
clinics.<br />
For disposal of Controlled drugs see section 10 and Disposal of a<br />
patient/client’s own medication see section 13<br />
7.8 Where an area is covered by the Service Level Agreement with <strong>Dudley</strong> Group<br />
of Hospitals (DGoH) Pharmacy department, the PCT staff and the Hospital<br />
Pharmacy staff are responsible for ensuring that the stock is appropriate to the<br />
field of practice and that the stock remains in date. The healthcare professional<br />
is responsible for ensuring that systems are followed the stock is kept tidy and<br />
clean and is stored in a way that facilitates ease of use. Where an area is not<br />
covered by the SLA, then the Head of <strong>Medicines</strong> management and healthcare<br />
professional staff are responsible<br />
7.9 It is the healthcare professional’s responsibility to ensure that any medications<br />
administered by them appear to be of suitable quality for use and have been<br />
stored according to manufacturer’s guidance. If a defect is suspected the<br />
guidance in section 5.4 must be followed.<br />
7.10 If items are required to be refrigerated then a lockable medicines fridge must be<br />
used for drug storage only. The temperature should be recorded regularly (daily<br />
or each time the area is used if less frequently than daily) with a<br />
maximum/minimum thermometer on an audit sheet.<br />
7.11 Storage in a drug trolley<br />
Drug trolleys must be secured to the wall when not in use. When unlocked they<br />
must be supervised by a member of staff at all times (preferably two, in case<br />
one gets called away). The members of staff are responsible for ensuring that<br />
the trolley is always supervised and must lock the trolley if the contents are not<br />
under direct observation. When a drug round is in progress the drug trolley lid<br />
must be closed if the contents are not in direct sight i.e. turning away to give an<br />
item to a patient. In an emergency the trolley may be left locked but not secured<br />
to a wall, however reasonable steps should be taken to prevent this happening.<br />
21
7.12 Storage in the patient/client’s home.<br />
Healthcare professionals are responsible for advising patients/clients and/or<br />
their relatives or carers on security and safe storage of medicines to be<br />
administered at home. Where possible patients/clients and carers should be<br />
encouraged to store medicines in a locked cupboard, out of reach of children.<br />
<strong>Medicines</strong> should not be stored in a kitchen or bathroom area.<br />
For syringe driver boxes kept at patient/clients home please refer to the<br />
<strong>Dudley</strong> PCT <strong>Policy</strong> for the Use of Syringe Drivers in the Community (Palliative<br />
<strong>Care</strong>). Syringe driver policy<br />
7.13 Storage in the GP surgery<br />
<strong>Medicines</strong> for use in the GP surgery should be stored in a locked cupboard or<br />
locked medicine refrigerator kept solely for this purpose. General Practitioners<br />
are personally responsible for ensuring the safe keeping of all medicines within<br />
the surgery.<br />
22
8. Responsibilities of the person administering the medication<br />
8.1 The healthcare professional must be aware of the action of the prescribed item,<br />
the usual dosage, the common side effects, interactions and how these relate<br />
to the treatment of the individual patient/client overall. They should be familiar<br />
with sources of information about medication such as the BNF.<br />
8.2 The healthcare professional must make every reasonable effort to maintain and<br />
develop knowledge of the common medications used in his/her area of practice.<br />
This knowledge should include awareness of:<br />
i. The signs of adverse reactions (ADR) to medication and the actions to<br />
be taken should this occur.<br />
ii Reactions that may occur when different medicines are combined.<br />
iii Contra indications<br />
iv How to report a suspected ADR i.e. use of the yellow card system.<br />
8.3 Where a healthcare professional has concerns about the clarity of the<br />
prescriber’s instruction or the appropriateness of a drug treatment then it should<br />
be raised with the prescriber or a pharmacist.<br />
8.4 Concerns about defective products should be raised with the supplying<br />
pharmacy as soon as possible. The pharmacy should advise on the action<br />
required concerning the medicine, and the necessity of obtaining an alternative<br />
supply. The product must be quarantined immediately. The incident must be<br />
logged on Sentinel which will be passed to the prescribing team. The person<br />
discovering the defect must inform the prescriber if the patient has received the<br />
product.<br />
8.5 The healthcare professional is responsible for teaching<br />
• The patient/client about medication in a manner commensurate with the<br />
individual’s ability to comprehend. This teaching should include the names<br />
and purpose of the medication, the dose and timing and the common<br />
potential side effects.<br />
• Student nurses about issues related to the prescribing and administration of<br />
medicines as outlined above.<br />
8.6 Where supervising a student health professional, the qualified professional<br />
must clearly countersign the signature of the student.<br />
23
9. Administration<br />
Registered healthcare professionals will normally undertake the administration<br />
of medicines. Exceptions are Community Health <strong>Care</strong> Staff and Social<br />
Services staff that have been trained in, and assessed as competent in, the<br />
administration of medication (with the exception of CDs which are not to be<br />
personally administered by these staff). Documentation of training should be<br />
maintained by the Team Leader/Coordinator who has responsibility for ensuring<br />
such training is completed. A record of this training should be held in the staff<br />
member’s personnel file.<br />
Only medicines that have been authorised by a medical or dental practitioner,<br />
or other authorised prescriber or a healthcare professional authorised via a<br />
Patient Group Direction must be administered to patients/clients. This<br />
authorisation must be in writing, in the form of a prescription, in advance of the<br />
administration of the medicine, (see section 2, Prescribing of medicines).<br />
In areas where there are no resident prescribers and in cases of clinical<br />
urgency a verbal instruction is acceptable (see section 12), except for schedule<br />
2 and 3 controlled drugs, other than Phenobarbital for epilepsy.<br />
See section 10 for further guidance on the administration of controlled drugs<br />
.<br />
9.1 Administration must be carried out in accordance with the patient/client’s<br />
prescription. This can be ascertained by having present at the time of<br />
administration one of the following:<br />
a) A clear written direction from an independent prescriber or a PGD.<br />
b) A duplicate copy of the discharge medication.<br />
c) Verbal prescription in extreme circumstances only. (Section 12)<br />
If there is any uncertainty regarding the prescriber’s intention this must be<br />
clarified prior to administration, e.g. clarification of abbreviations not included in<br />
2.7.6<br />
9.2 The healthcare professional responsible for the drug administration must<br />
ensure the following elements of the procedure are achieved: -<br />
i) The patient/client is correctly identified and informed consent gained<br />
before taking their medication or there is authorisation of administration.<br />
ii) The patient/client is assessed to ensure they are able to receive the<br />
medication and that it is safe to administer it.<br />
iii) The correct drug and formulation is selected.<br />
iv) The correct dose (i.e. strength or quantity) is selected.<br />
v) The correct route is used to administer the drug.<br />
24
vi)<br />
vii)<br />
viii)<br />
ix)<br />
The drug is being given at the correct time and on the correct date.<br />
The drug has been prescribed by an authorised prescriber or is<br />
administered in accordance with an approved PGD.<br />
The drug has not passed its expiry date.<br />
Administration is completed to the correct patient/client*<br />
*Generally, completion means that the patient/client has swallowed the<br />
medication or received an injection or suppository. There are a<br />
few exceptions, e.g. sub-lingual tablets, syringe drivers.<br />
9.3 Orally administered medicines must be offered to the patient/client<br />
accompanied by a drink (excluding sub-lingual administration), if<br />
appropriate.<br />
9.4 <strong>Medicines</strong> must not be crushed, broken or mixed with food or liquid unless<br />
specified by the prescriber, as per manufacturers’ instructions or in consultation<br />
with a pharmacist or speech and language therapist. This changes the<br />
pharmaceutical qualities of the medication and may be construed as covert<br />
administration. This includes administering medicines via PEG feeds.<br />
As a general principle, by disguising medication in food or drink, the client or<br />
patient is being led to believe that they are not receiving medication, when in<br />
fact they are. The health professional will need to be sure that what they are<br />
doing is in the client’s best interests and be accountable for that decision. .See<br />
NMC documents on covert administration:-<br />
http://www.nmc-uk.org/aDisplayDocument.aspxDocumentID=3602 and<br />
http://www.nmc-uk.org/aDisplayDocument.aspxdocumentID=3954<br />
9.5 <strong>Medicines</strong> should not be administered to or taken by any member of staff<br />
unless purchased for personal use, prescribed by occupational health or<br />
prescribed by a practitioner with whom that person is registered.<br />
9.6 Only those medicines supplied by a pharmacy or assessed as suitable by<br />
pharmacy shall be administered to patients/clients. All samples/clinical trial<br />
medicines must be supplied only via a pharmacy.<br />
9.7 Once a drug has been given the person administering the drug must make a<br />
record. This record should be made at the time of administration and be in the<br />
patient/client’s records or on an appropriate Medication Record Card which<br />
must be filed in the patient/client’s records once complete. Home <strong>Care</strong> Staff<br />
must sign a Medication Administration Record (MAR) sheet to confirm<br />
administration. The record must include:<br />
25
i) Drug administered<br />
ii) Dose<br />
iii) Route<br />
iv) Site, if appropriate e.g. depot injections<br />
v) Date of administration, and time if appropriate<br />
vi) Signature and designation of the person administering the drug.<br />
vii) Batch number and expiry date of injection (if applicable)<br />
viii) Patient consent according to PCT consent policy (if applicable)<br />
9.9 Non-administration of a drug may be due to patient/client nonattendance/refusal,<br />
adverse drug reaction or non-availability of a drug. In all<br />
instances of non-administration of a drug all relevant details must be recorded<br />
in the patient/client’s records and the patient/client’s doctor or consultant<br />
contacted for advice.<br />
Some clinical areas use a reference code to be entered on the treatment sheet<br />
explaining non-administration. Staff must be made aware if such reference<br />
codes are used. Codes must be clear and will be consistent across the PCT<br />
and hospital.<br />
9.10 In cases of non-attendance active effort must be made to trace the patient/client<br />
and administer the drug within a reasonable length of time. When the drug can<br />
be administered with a delay that does not pose a problem clinical judgement<br />
can be used with regards as to whether the patient/client’s doctor should be<br />
contacted.<br />
9.11 In cases of non-availability of a drug every effort must be made to obtain the<br />
drug within a reasonable period of time. The reason for non-availability must be<br />
recorded in the patient/client’s records and the doctor or consultant contacted<br />
regarding alternative treatment or the possibility of delaying administration until<br />
the drug is available.<br />
9.12 In cases of adverse drug reaction or patient/client refusal the patient/client’s<br />
doctor or consultant must be contacted immediately and advice sought. For a<br />
suspected ADR, a ‘yellow card’ should be completed according to the<br />
guidelines from the Committee on Safety of <strong>Medicines</strong> (see section 2.9)<br />
9.13 Community Nurses may only apply non-medicated inert dressings until<br />
prescribed treatment is available.<br />
9.14 <strong>Medicines</strong> must not be prepared in advance of administration except for<br />
• Those done by pharmacy staff<br />
• Antibiotic syrups<br />
• The filling of concordance aids<br />
26
• Insulin injections by District Nurses for patients for self administration at<br />
home<br />
9.15 Protocols for specialist procedures such as non-clinical staff giving insulin or<br />
social services staff undertaking administration of medicines are being<br />
developed and will be circulated as appendices when approved. It is the<br />
responsibility of the member of staff to check if there is a relevant protocol.<br />
9.16 If it is suspected that the patient/client, their carer or representative are giving<br />
higher doses than prescribed then the RMO/GP must be informed to discuss<br />
review of medication with the patient/client their carer or representative.<br />
27
10. Controlled Drugs (CDs)<br />
NB<br />
Accountability for the use of controlled drugs rests with the Accountable<br />
Officer for the PCT (currently the Specialist in Pharmaceutical Public<br />
Health)<br />
10.1 Who can prescribe controlled drugs<br />
All medical prescribers can prescribe schedule 2, 3, 4 and 5 CDs.<br />
Following agreement by the Home Office’s Advisory Council on the Misuse of<br />
Drugs (ACMD), changes to regulations on 1 May 2006 enable nurse<br />
independent prescribing of some CDs. Nurse Independent Prescribers can<br />
prescribe some CDs independently, but only for specific conditions. These<br />
include diamorphine and morphine for palliative care and post-operative pain<br />
relief. A list of these CDs and medical conditions is contained in the Drug Tariff<br />
(see part XVIIbii) and also in the BNF. For further information visit www.ppa.org<br />
and www.bnf.org.uk .<br />
Nurse Independent Prescribers are also able to prescribe lower strength<br />
Pharmacy (P) and General Sales List (GSL) medicines containing codeine<br />
phosphate and dihydrocodeine tartrate.<br />
Community Practitioners and Pharmacist Independent Prescribers cannot at<br />
present prescribe CDs independently.<br />
All supplementary prescribers are able to prescribe any CD provided it is listed<br />
in the clinical management plan.<br />
Controlled drug schedules are as follows:<br />
Schedule 1 (CD licence)<br />
• Have no recognised medicinal use and include hallucinogenic drugs.<br />
• Examples include coca leaf, LSD and mescaline.<br />
• Production, possession and supply of these drugs are limited to research or<br />
other special purposes.<br />
• Practitioners and pharmacists may not lawfully possess Schedule 1 drugs<br />
except under licence.<br />
Schedule 2 (CD)<br />
• Includes the opiates, secobarbital, amphetamine and cocaine.<br />
28
• Are subject to safe custody requirements and so must be stored in a locked<br />
receptacle, usually in an appropriate CD cabinet or approved safe, which can<br />
only be opened by the person in lawful possession of the CD or a person<br />
authorised by that person.<br />
• A licence is required to import or export drugs in Schedule 2.<br />
• The drug may be administered to a patient by a doctor or dentist, or by any<br />
person acting in accordance with the directions of a doctor or dentist.<br />
• A register must be kept for Schedule 2 CDs and this register must comply with<br />
the relevant regulations.<br />
• The destruction of CDs in Schedule 2 must be appropriately authorised and the<br />
person witnessing the destruction must be authorised to do so.<br />
• Are subject to handwriting requirements as in 10.3.1<br />
Schedule 3 (CD No Register)<br />
• Includes a small number of minor stimulant drugs and other drugs which are<br />
less likely to be misused than the drugs in Schedule 2.<br />
• Are exempt from safe custody requirements and can be stored on the open<br />
dispensary shelf except for temazepam, buprenorphine and diethylpropion,<br />
which must be stored in a locked CD receptacle.<br />
• Are subject to the same special handwriting requirements as Schedule 2 CDs,<br />
except for temazepam and phenobarbital. Phenobarbital and temazepam can<br />
be dispensed in response to a computer-generated prescription but the<br />
prescriber's signature must be added by hand.<br />
• There is no legal requirement to record transactions in a CD register.<br />
• The requirements relating to destruction do not apply unless the CDs are<br />
manufactured by the individual.<br />
• Invoices must be retained for a minimum of two years.<br />
Schedule 4 (CD Benzodiazepines and CD Anabolic steroids)<br />
• Are exempt from safe custody requirements, with destruction requirements only<br />
applying to importers, exporters and manufacturers.<br />
• Specific CD prescription-writing requirements do not apply.<br />
• CD registers do not need to be kept, although records should be kept if such<br />
CDs are produced, or if a licensed person imports or exports such drugs.<br />
o<br />
Part 1 (CD Benzodiazepines):<br />
29
• Includes most of the benzodiazepines, plus eight other<br />
substances including fencamfamin and mesocarb.<br />
• Possession of is an offence without an appropriate prescription.<br />
Possession by practitioners and pharmacists acting in their<br />
professional capacities is authorised.<br />
• Are subject to full import and export control.<br />
o<br />
Part 2 (CD Anabolic steroids):<br />
• Includes most of the anabolic and androgenic steroids such as<br />
testosterone, together with clenbuterol (adrenoreceptor stimulant)<br />
and growth hormones.<br />
• There is no restriction on the possession when it is part of a<br />
medicinal product.<br />
• A Home Office licence is required for the importation and<br />
exportation of substances unless the substance is in the form of a<br />
medicinal product and is for self-administration by a person.<br />
Schedule 5 (CD Invoice)<br />
• Includes preparations of certain CDs (e.g. codeine, pholcodine, morphine)<br />
which are exempt from full control when present in medicinal products of low<br />
strengths as their risk of misuse is reduced.<br />
• No restriction on the import, export, possession, administration or destruction of<br />
these preparations and safe custody regulations do not apply.<br />
• A practitioner, pharmacist or a person holding an appropriate licence may<br />
manufacture or compound any CD in Schedule 5.<br />
• Invoices must be kept for a minimum of two years.<br />
10.2 Situation for supply and administration<br />
Nurses can supply and administer some CDs under the terms of a Patient<br />
Group Direction (PGD). PGDs can be used for the supply and administration of<br />
Schedule 4 and 5 controlled drugs-with the exception of anabolic steroids.<br />
Paramedics, chiropodists/podiatrists, orthoptists, physiotherapists and<br />
radiographers can supply and administer schedule 4 and 5 CDs under the terms<br />
of a PGD, with the exception of anabolic steroids. Occupational therapists and<br />
prosthetists and orthotists were added to the list of those who can supply and<br />
administer schedule 4 and 5 CDs under a PGD from July 2006.<br />
30
10.3 Prescribing Controlled Drugs<br />
10.3.1 Legal Prescription requirements<br />
Prescriptions written for Schedule 2 and 3 controlled drugs and marked as CD<br />
in the BNF, with the exception of temazepam and Phenobarbital are subject to<br />
the following strict legal requirements (see relevant BNF section):<br />
a) Be printed or written in ink, or other indelible substance<br />
b) Specify the dose, dosage form (e.g. tablets) and where appropriate the<br />
strength of the preparation.<br />
c) State in words and figures the total quantity of the drug or total<br />
number of dose units that are to be supplied or given.<br />
d) Bear the patient/client's name, address and registration number.<br />
e) Be dated<br />
f) Be signed (not just initialled) by the prescriber.<br />
g) Supply should be no more than 30 days supply (except in exceptional<br />
clinical circumstances). N.B. On FP10MDA forms only 14 days supply<br />
is permitted.<br />
N.B.<br />
* All CD prescriptions are valid for 28 days from date on prescription for<br />
S2, 3 and 4 CDs (does not apply to S5).<br />
* Dental prescriptions must have written the words “for dental<br />
treatment only”.<br />
10.3.2 Safety issues<br />
(see NPSA alert 2008/RRR05 Reducing Dosing Errors with Opioid <strong>Medicines</strong><br />
http://www.npsa.nhs.uk/nrls/alerts-and-directives/rapidrr/reducing-dosingerrors-with-opioid-medicines/<br />
)<br />
When opioid medicines are prescribed, dispensed or administered, in anything<br />
other than acute emergencies, the healthcare practitioner concerned, or their<br />
clinical supervisor, should:<br />
• Confirm any recent opioid dose, formulation, frequency of administration and<br />
any other analgesic medicines prescribed for the patient. This may be done for<br />
example through discussion with the patient or their representative (although<br />
not in the case of treatment for addiction), the prescriber or through medication<br />
records.<br />
• Ensure where a dose increase is intended, that the calculated dose is safe for<br />
the patient (e.g. for oral morphine or oxycodone in adult patients, not normally<br />
more than 50% higher than the previous dose).<br />
31
• Ensure they are familiar with the following characteristics of that medicine and<br />
formulation: usual starting dose, frequency of administration, standard dosing<br />
increments, symptoms of overdose, common side effects.<br />
10.4 Transport<br />
PCT staff should not carry controlled drugs unless in exceptional<br />
circumstances or to deliver services to patients such as:<br />
• Terminal patients receiving drugs via syringe drivers.<br />
• Patients undergoing detoxification regimens<br />
• If a nurse is asked by a GP or the GP out-of-hours (OOH) deputising<br />
service, when on the premises, to take out a controlled drug from the<br />
surgery and administer to a patient. It is also the nurse’s responsibility to<br />
ensure this is recorded in the surgery controlled drugs register.<br />
Community Pharmacy delivery services should be used wherever possible<br />
when the patient/client has difficulty collecting their medication.<br />
On occasion it may be necessary for a nurse to collect an urgent prescription<br />
from the pharmacy. The medication must have been prescribed for a specific<br />
patient and the member of staff is collecting them under the direction of the<br />
patient for administration immediately. The nurse should go straight to the<br />
patient’s home and must not leave the prescription in the vehicle unattended at<br />
any point.<br />
When medicines are supplied out of hours, the OOH procedure should be<br />
followed. See - http://joint.dudley.nhs.uk/cmsextra/documents/cms/222-2008-4-<br />
29-4062085.pdf<br />
10.5 Records<br />
Controlled drugs should be documented as follows.<br />
10.5.1 Patient/Client held stock<br />
A running balance should be kept in the patient/client’s records to account for<br />
this stock. If a discrepancy arises then efforts should be made to account for<br />
this. If no reason can be found then the incident should be reported to the team<br />
co-ordinator who is responsible for deciding on what further action should be<br />
taken. The incident reporting procedure must be followed.<br />
32
10.5.2 Stock held at PCT premises or other healthcare settings.<br />
Records must be kept for schedule 2 controlled drugs by all persons authorised<br />
to possess them.<br />
The following particulars are to be recorded for CDs received:<br />
a) Date on which received;<br />
b) Name and address of person or firm from who received;<br />
c) Amount received;<br />
d) form in which received.<br />
For CDs supplied/administered the following must be recorded:<br />
a) Date on which the supply/administration was undertaken;<br />
b) Name and address of person to who supplied/administered;<br />
c) Particulars as to the licence or authority of the person<br />
Supplied/administered to be in possession of CDs;<br />
d) Amount supplied;<br />
e) Form in which supplied.<br />
The above particulars are the minimum fields of information that must be<br />
recorded in the CD register<br />
A running balance should be kept in an official controlled drug register with<br />
entries of both obtained and supplied controlled drugs. (Further detailed<br />
information is available in the <strong>Medicines</strong> Ethics and Practice booklet (RPSGB)<br />
or visit www.rpsgb.org)<br />
10.6 Destruction<br />
10.6.1 Controlled Drugs no longer required by the patient/client.<br />
Schedule 2 injectable CDs should be destroyed by the healthcare professional<br />
at the patient/client’s home, and witnessed by the patient/client, their carer or<br />
representative or another member of staff. A CD destruction/denaturing kit<br />
must be used for all liquid schedule 2 CDs. Once denatured, drugs may be<br />
disposed of in clinical waste containers. A note should be made in the<br />
patient/client’s records that must be signed by both parties. For all other CDs<br />
the patient/client, their carer or representative should be advised to return it to<br />
their community pharmacy.<br />
33
10.6.2 In the event of a patient dying at home<br />
In the event of a patient dying the above would also apply, as under the Misuse<br />
of Drugs Act possession of CDs cannot pass to another person therefore all<br />
must be destroyed. The nurse present should record all CD drugs not used<br />
(recording form, strength and quantity) sign and date the record and, if possible,<br />
ask a witness to sign that the record is true. A copy of the record should be<br />
kept with the drugs for transfer to the community pharmacy for destruction and<br />
a copy kept with the patient’s notes. If there is no carer/relative to return drugs<br />
to a community pharmacy, all drugs should be destroyed as soon as possible.<br />
10.7 Breakages and Damages<br />
If any healthcare professional finds or accidentally causes a supply to be<br />
damaged or broken (e.g. ampoules/bottle) this incident shall be reported<br />
promptly to the nurse manager. An entry on such incidents will need to be<br />
made directly in the patient records detailing the date, time, quantity of stock<br />
damaged or broken, the signature of the member of staff who found this and<br />
the signature of the member of staff or other person present who witnessed the<br />
incident. The staff involved may wish to add additional information if thought<br />
necessary. If damaged or broken supply is discovered by a patient or carer then<br />
the same procedure should be followed noting who made the discovery.<br />
10.8 Storage<br />
All controlled drugs should be stored in a locked cupboard specifically for that<br />
purpose, separate to other drugs. CD cupboards must have a daily stock check.<br />
Please refer to the <strong>Medicines</strong> Ethics and Practice booklet (RPSGB) or visit<br />
www.rpsgb.org for details.<br />
For checking CD stocks held on PCT premises serviced by the Pharmacy<br />
Department, <strong>Dudley</strong> Group of Hospitals please refer to DGoH <strong>Medicines</strong><br />
<strong>Management</strong> <strong>Policy</strong>. It is an audit requirement that there is a pharmacy check<br />
once every six months.<br />
For further information on CDs legislation and best practice please contact the<br />
<strong>Medicines</strong> <strong>Management</strong> Team at the PCT or see the controlled drug section on<br />
the PCT website.<br />
34
11. <strong>Management</strong> of errors or incidents associated with medicines.<br />
It is recognised that despite careful checking mistakes do happen. Errors in<br />
administration can include for example selecting the wrong medication,<br />
administering an incorrect dose, using the wrong route, giving the medication to<br />
the wrong patient/client, failing to ensure that the patient/client has received it or<br />
may involve a dispensing error from the pharmacy.<br />
Any error/incident must be reported via the PCT Sentinel reporting<br />
systems.<br />
Errors or incidents concerning the administration of medicines require<br />
investigation under the Serious Untoward Incident Investigation <strong>Policy</strong>. This<br />
does NOT mean that disciplinary action will automatically follow. Each incident<br />
will be considered in its particular context.<br />
11.1 Clinical Errors by Staff involving <strong>Medicines</strong><br />
<strong>Dudley</strong> PCT operates a ‘fair blame’ policy which to encourage all errors to be<br />
reported and investigated as to the cause. Local training course are available in<br />
investigation of incidents.<br />
Whenever errors in the administration of medicines are found then the<br />
healthcare professional administering will:-<br />
i) Contact the appropriate prescriber for the patient/client so that if<br />
necessary remedial action can be taken to ensure the safety of the<br />
patient/client. If the prescriber is not the patient’s GP then they must be<br />
informed as to the nature of the error and the steps taken.<br />
ii)<br />
iii)<br />
Report the incident to the senior manager in charge who has the<br />
responsibility of investigating the incident.<br />
The healthcare professional must also ensure<br />
a) The patient/client’s blood pressure and pulse is taken and recorded, if<br />
possible, and observe for any signs of shock.<br />
b) Follow the incident reporting procedure and inform Clinical<br />
Governance. Clinical Governance will inform the <strong>Medicines</strong><br />
<strong>Management</strong> Team.<br />
c) Enter details of the event in the patient/client’s records including<br />
details of any remedial action taken and the individuals informed.<br />
It is the responsibility of the nurse in charge to ensure that the patient (and/or<br />
relatives, dependent on circumstances) is advised at an early stage. How this<br />
35
occurs, and by whom, will need to take account of the nature of the error and<br />
any adverse consequences suffered by the patient. Any discussions should be<br />
documented in the patient's case notes.<br />
11.2 Consequences of an error<br />
Actions following an error may range from a review of processes, assessment<br />
of individual accountability and training needs to a report to the National Patient<br />
Safety Agency on the circumstances. Professionals may be referred to their<br />
professional body. Repeated errors may lead to performance management<br />
processes being activated.<br />
11.3 Errors by Medical staff<br />
The Medical Director will have responsibility for investigating the incident and<br />
reporting the incident following the Incident Procedure.<br />
11.4 Dispensing errors<br />
In the case of a suspected dispensing error the medicines must be quarantined<br />
immediately. The Pharmacist in Charge of either the hospital or community<br />
pharmacy, from where the drug was dispensed, must be contacted for advice<br />
on the action required concerning the drug and obtaining a replacement. If the<br />
drug has been administered then the action laid out in 11.1 must be followed.<br />
If the drug has not been administered the <strong>Medicines</strong> <strong>Management</strong> Team must<br />
be contacted for advice, as above. The incident should be reported via sentinel<br />
and documented in the patient/client’s records. The Clinical Governance Team<br />
will advise on any risk management issues arising from an incident.<br />
If the dispensing pharmacy is closed then the error must be reported the next<br />
working day.<br />
36
12. Verbal orders for the Administration of Medication<br />
It is recognised that in extreme circumstances it may be necessary to accept<br />
verbal instructions about medication.<br />
12.1 Verbal Prescriptions via Telephone<br />
12.1.1 Verbal instructions from a doctor to adjust the dose of a medicine may be<br />
accepted by a Registered Nurse in exceptional circumstances. In very rare<br />
circumstances a verbal instruction may be accepted to initiate a medicine. If<br />
possible a fax or email should be used to confirm the prescription.<br />
A verbal message cannot be accepted to initiate a Controlled Drug; however a<br />
request to increase the dose may be acceptable in exceptional circumstances.<br />
For increasing the dose of a syringe driver see section 21.<br />
12.1.2 The nurse must record on the patient/client’s records<br />
i) the name of the prescriber<br />
ii) the details of the instruction<br />
iii) the date and time of the order<br />
iv) an indication that it is a verbal instruction<br />
This record must be annotated "TELEPHONE ORDER" and signed by the<br />
nurse. It is good practice for a second member of staff to listen to the doctor<br />
repeating the instructions.<br />
12.1.3 The instructions should be read back to the Doctor, in the presence of a second<br />
registered nurse or other healthcare professional if possible, confirming the<br />
patient/client's name and registration number and the name and dosage of the<br />
medicine.<br />
The details of the verbal order must be entered in the patient/client’s records<br />
and signed by the nurse receiving the verbal order and the second nurse if one<br />
is involved.<br />
12.1.4 The nurse receiving the verbal order must administer the medicine in<br />
accordance with the procedures for drug administration.<br />
12.1.5 It is the prescriber’s responsibility to provide written confirmation of the verbal<br />
request as soon as practicable but within 24 hours in all circumstances.<br />
12.1.6 Only one dose of any drug can be given - subsequent doses should not be<br />
given without a written prescription from a doctor.<br />
37
13. Disposal of <strong>Medicines</strong> when off site.<br />
Please refer to PCT Waste <strong>Policy</strong> for extra information. waste policy<br />
13.1 <strong>Medicines</strong> once dispensed to a patient/client are their property. They should<br />
not be removed for disposal without the patient/client’s consent. If any<br />
medication is not current therapy the patient/client or their<br />
relative/representative/carer should be encouraged to give their consent to the<br />
disposal of such medication by a pharmacy. Patients/clients, their relatives,<br />
representatives or carers should be advised to take the medication to a<br />
community pharmacy. If a patient is utilising a community pharmacy delivery<br />
service then unused medication may be returned to the driver when they next<br />
make a delivery.<br />
13.2 If it is felt unsafe to leave non-required medication in the possession of a<br />
patient/client, but the patient/client is unwilling to give consent for disposal, the<br />
registered nurse should contact the doctor in charge or patient/client’s doctor to<br />
advise them of concerns. This action must be fully documented in the<br />
patient/client’s record along with the name of the doctor contacted.<br />
13.3 When Controlled Drugs are no longer required they must be destroyed as<br />
specified in section 10.6<br />
38
14 Alcohol<br />
14.1 Patient/client under the influence of alcohol.<br />
In the circumstance where the patient/client is thought to be under the influence<br />
of alcohol or illicit drugs the community nurse should not administer the<br />
prescribed treatment (unless it is life saving) but make alternative arrangements<br />
to administer required doses at a later time. The patient/client’s Registered<br />
Medical Officer (RMO) or GP should be informed immediately and the guidance<br />
on non-administration of a drug (section 9.9) must be followed.<br />
14.2 Possession of alcohol on trust premises<br />
All patients should be informed of the general policy of no alcohol on <strong>Trust</strong><br />
premises. If a patient is found in possession of alcohol, it must be stored in an<br />
appropriate place until the patient is to be discharged or removed from the ward<br />
by a family member with the patient’s permission. If the patient has been<br />
informed about <strong>Trust</strong> policy, staff can remove the alcohol from the patient on<br />
best interests ground.<br />
Some clients in long-term care may be allowed small amounts of alcohol, which<br />
are purchased by PCT staff and consumed under supervision. NB: the effect of<br />
alcohol on any medication must be checked with a pharmacist.<br />
39
15. Illegal Substances<br />
.<br />
15.1 Patient/clients found in possession of illegal controlled drugs.<br />
Each professional worker must be aware of the procedures appertaining to<br />
safety, risk assessment and risk management and adhere to these procedures<br />
at all times.<br />
15.1.1 On <strong>Trust</strong> premises.<br />
If a patient/client is found in possession of illegal drugs or a substance thought<br />
to be illegal, then he or she should be advised that the possession of the item is<br />
unlawful. The <strong>Trust</strong> Head of Security should be contacted for advice on further<br />
action. The medical staff and police must be informed and the incident logged<br />
on Sentinel.<br />
If a member of staff suspects a visitor to be dealing in drugs they must inform<br />
the <strong>Trust</strong> Head of Security immediately.<br />
If a suspicious substance is discovered, not in the possession of an individual,<br />
the police must be informed. The supervisor or second member of staff must be<br />
notified and the incident logged on sentinel. The substance must be locked<br />
away and the senior manager in charge holds the key until the police arrive.<br />
15.1.2 On Social Services Premises<br />
The community nurse must inform the manager of the establishment who will<br />
follow their own policy and procedures in dealing with the situation.<br />
15.1.3 In the patient/client’s home<br />
PCT staff must use their professional judgement in dealing with each situation.<br />
Where concern exists that the patient/client is using or is in possession of illicit<br />
substances the situation must be discussed with the patient/client’s RMO and<br />
documented in the patient/client’s record.<br />
PCT staff must not receive illegal substances but encourage the client to<br />
dispose of them. Staff should be aware of personal safety issues at all time.<br />
http://joint.dudley.nhs.uk/cmsextra/documents/cms/489-2008-8-14-3025847.pdf<br />
15.2 Suspicion of dealing<br />
In general the patient/client’s right to confidentiality must be preserved and a<br />
member of staff must not divulge the identity of the patient/client to the police.<br />
However this would not be the case when the quantity of substance involved<br />
40
may imply dealing, as breach of confidentiality would be justified because of the<br />
wider public implications. In such an event the PCT staff must seek guidance<br />
from the <strong>Trust</strong> Head of Security.<br />
41
16. Theft<br />
16.1 If medicines under the care of a member of staff are lost or stolen then the<br />
member of staff must take action immediately to inform their line manager, the<br />
police and the <strong>Trust</strong> Head of Security. The Serious Untoward Incident<br />
Investigation <strong>Policy</strong> must be followed.<br />
16.2 If theft of medicines by a member of staff is suspected the matter should be<br />
reported to the line manager and <strong>Trust</strong> Head of Security. The <strong>Trust</strong> Head of<br />
Security is responsible for deciding on what further action should be taken.<br />
http://joint.dudley.nhs.uk/cmsextra/documents/cms/489-2008-8-5-3796510.pdf<br />
42
17. General Notes on the Handling of <strong>Medicines</strong><br />
17.1 The contents of one container must never be transferred to another container<br />
without pharmaceutical advice as the stability and product liability of the product<br />
may be affected. Part empty containers must either be disposed of or the drug<br />
should continue to be used until the container is empty.<br />
No drug should be removed from its container/packaging except for immediate<br />
administration or for counting purposes, when only one container may be<br />
removed at a time.<br />
17.2 With the exception of pharmacists, under no circumstances may members of<br />
staff alter labels. Clarification of the prescriber’s intentions is permissible<br />
providing this does not obscure or change the original instructions.<br />
17.3 Due attention should be paid to additional information e.g. hazard-warning<br />
labels on drug containers.<br />
17.4 If drug labels are unclear or dirty, the container must be returned to the<br />
supplying Pharmacy.<br />
17.5 Under no circumstances should samples of medicines, dressings, topical<br />
products, nutritional products or medical devices be accepted from members of<br />
the Pharmaceutical Industry for use on patients/clients.<br />
17.6 Under no circumstances should medication returned from patients’ own homes<br />
be used on another patient, it must be disposed of as waste.<br />
43
18. Patients at Risk from Self-Poisoning<br />
If a Healthcare Professional on a Community visit considers that a patient<br />
is at risk and capable of planned or accidental self-poisoning with their<br />
prescribed medication they should:-<br />
• Remove the medicines from the home with the patient’s or relative’s<br />
permission, and store in a locked cupboard at team base. The medicines<br />
removed must be recorded in the patient’s records.<br />
• Document reasons for decision and notify Psychiatrist and/or GP.<br />
• Enter details of visit, reason for removal, medicine, strength and quantity in<br />
the patient’s nursing record.<br />
• If there are mental health capacity issues then the prescriber must be<br />
contacted for further discussion<br />
If the situation does not warrant immediate removal but the healthcare<br />
professional has a concern these must be documented and shared with the rest<br />
of the team and prescriber.<br />
If a patient being discharged or given leave from hospital is similarly at risk,<br />
they should only be provided with a small amount of medicine, exact quantities<br />
can be discussed with the prescriber.<br />
44
19. Compliance aids<br />
All compliance aids should be filled by <strong>Dudley</strong> Group of Hospitals Pharmacy<br />
Department or by a community pharmacist after prior agreement with the<br />
supplier. <strong>Medicines</strong> quality and effectiveness can be affected by decanting into<br />
these aids and pharmaceutical advice is essential before one can be supplied.<br />
45
20. Vaccines<br />
Vaccines are usually fridge items and handling of the products must be<br />
undertaken in line with the PCT cold chain guidelines. See:-<br />
http://pctnet.dudley.nhs.uk/cmsintra/Immunisation/index.aspid=566&doc=show<br />
Please refer to the <strong>Dudley</strong> PCT Immunisation Website for details on individual<br />
vaccines and immunisation schedules.<br />
http://www.dudley.nhs.uk/sites/immunisations/index.aspid=3195<br />
46
21. Syringe Drivers<br />
Please refer to the current ‘<strong>Policy</strong> for the use of Graseby MS26 Syringe Drivers<br />
in Palliative <strong>Care</strong>’ compiled by <strong>Dudley</strong> Macmillan Community Palliative <strong>Care</strong><br />
Team. (http://joint.dudley.nhs.uk/cmsextra/documents/cms/191-2008-1-21-<br />
5949772.pdf)<br />
Patients/clients may receive subcutaneous infusions of medicines such as<br />
morphine, diamorphine, heparin and insulin via an electronically powered<br />
syringe driver. Macmillan Nurses and District Nurses may operate syringe<br />
drivers provided that they have received training and are competent as laid<br />
down in the current syringe driver policy.<br />
21.1 Administration must be carried out in accordance with guidance in section 9 of<br />
the MMP.<br />
21.2 When a dose increase is required outside of the patient/client’s drug<br />
regimen/ceiling dose, the doctor/competent independent prescriber is expected<br />
to attend and re-assess the patient/client and give written instructions on dose<br />
adjustments. In exceptional circumstances a verbal instruction to adjust a dose<br />
can be accepted and the procedure in section 12 followed.<br />
In very exceptional circumstances it is permissible for a verbal instruction to be<br />
taken to increase the dose of a syringe driver containing a controlled drug<br />
providing that it is at the direction of the patient/client’s doctor/competent<br />
independent prescriber and it is in the patient/client’s best interest to do so. A<br />
community nurse acting on such a verbal instruction should be aware of<br />
possible consequences resulting from such action and the importance of fully<br />
documenting the incident as described in section 10. The doctor/competent<br />
independent prescriber must provide written confirmation of the dosage<br />
alteration as soon as practicable but within 24 hours in all circumstances.<br />
An additive label must be completed and attached to the syringe ensuring that<br />
graduation markings are obscured, in order to ensure that the dose is<br />
measured in mm not ml as per ‘West Midlands Palliative <strong>Care</strong> Guidelines.’<br />
47
22. Cytotoxic <strong>Medicines</strong><br />
22.1 Intravenous administration<br />
Patients requiring cytotoxic medicines to be administered by the intravenous<br />
route should be referred to the Georgina Unit, Russells Hall Hospital.<br />
22.2 Subcutaneous administration of cytotoxic drugs<br />
This must only be undertaken after specific training.<br />
22.3 Oral administration of cytotoxic drugs<br />
A minimal touch technique should be used and hands washed immediately<br />
before and after administration. Tablets must NOT be crushed. In cases of<br />
swallowing difficulty a suspension may be available from the supplying<br />
pharmacy.<br />
22.4 Disposal of cytotoxic waste<br />
The nurse administering the treatment must ensure that appropriate waste<br />
receptacles and collection arrangements are followed as laid down in the Joint<br />
<strong>Trust</strong> Waste <strong>Management</strong> <strong>Policy</strong>.<br />
http://pctnet.dudley.nhs.uk/documents/cms/149-2007-1-9-5025008.pdf<br />
48
23. Prescribing of Oxygen<br />
Please refer to the Home Oxygen section of the <strong>Dudley</strong> PCT website for details<br />
on home ordering of oxygen on the ‘Home Oxygen Service’ page. See:-<br />
http://pctnet.dudley.nhs.uk/cmsintra/general-Practice/index.aspid=4840<br />
For further assistance please contact the <strong>Dudley</strong> Respiratory Support Service<br />
at <strong>Dudley</strong> Group of Hospitals on 01384 244383<br />
49
24. Monitoring the policy<br />
If you have any questions regarding this policy or about medicines please<br />
contact <strong>Medicines</strong> <strong>Management</strong> Team at the PCT.<br />
A Pharmacist shall inspect all areas where medicines are stored at regular<br />
intervals. A report of each unit will be made in writing to the unit manager<br />
responsible for drug storage, which will be copied to the Pharmaceutical<br />
Advisor and General Manager, should there be any indication that the<br />
procedure detailed above is not being followed.<br />
Knowledge and implementation of the <strong>Policy</strong> will be discussed and documented<br />
as part of annual Personal Development Plans<br />
50
This policy was produced by Specialist in Pharmaceutical Public Health and<br />
Pharmacist, <strong>Dudley</strong> PCT.<br />
The policy was circulated amongst managers and local clinical networks for comment<br />
at various stages of development. Other areas such as chiropody, dentistry,<br />
Community nursing teams, local authority staff, general practice, clinical governance<br />
and training and development were consulted.<br />
51
Supporting Documents:<br />
Duthie Report "Department of Health Guidelines for the Safe and Secure<br />
Handling of <strong>Medicines</strong>" 1988<br />
Controls Assurance Standards <strong>Medicines</strong> <strong>Management</strong>.<br />
<strong>Dudley</strong> PCT Waste <strong>Management</strong> <strong>Policy</strong> and Procedures (2009)<br />
<strong>Dudley</strong> PCT <strong>Policy</strong> for the use of Graseby MS26 Syringe Drivers in the<br />
community in palliative care (2007)<br />
<strong>Dudley</strong> PCT Non Medical Prescribing <strong>Policy</strong> (2004)<br />
<strong>Dudley</strong> PCT Patient Group Direction Information Pack (2007)<br />
<strong>Dudley</strong> PCT Serious Untoward Incident Investigation <strong>Policy</strong> (2008)<br />
<strong>Dudley</strong> Group of Hospitals <strong>Medicines</strong> <strong>Management</strong> <strong>Policy</strong> (2009)<br />
<strong>Dudley</strong> PCT Security <strong>Policy</strong> (2008)<br />
<strong>Dudley</strong> PCT Protocol for supply of Palliative <strong>Care</strong> <strong>Medicines</strong> Out of Hours<br />
(2007)<br />
<strong>Dudley</strong> PCT Sharps <strong>Policy</strong> (2009)<br />
Abbreviations<br />
ADR<br />
AHP<br />
BNF<br />
CD<br />
CMP<br />
DGoH<br />
FMC<br />
NMC<br />
NMP<br />
PCT<br />
PGD<br />
POM<br />
PPD<br />
RPSGB<br />
SiPPH<br />
SLA<br />
Adverse Drug Reaction<br />
Allied Health Professional<br />
British National Formulary<br />
Controlled drug<br />
Clinical <strong>Management</strong> Plan<br />
<strong>Dudley</strong> Group of Hospitals<br />
Facilities <strong>Management</strong> Centre<br />
Nursing and midwifery Council<br />
Non Medical Prescriber<br />
<strong>Primary</strong> <strong>Care</strong> <strong>Trust</strong><br />
Patient Group Direction<br />
Prescription Only <strong>Medicines</strong><br />
Prescription Pricing Division<br />
Royal Pharmaceutical Society of Great Britain<br />
Specialist in Pharmaceutical Public Health<br />
Service Level Agreement<br />
Contact telephone numbers:<br />
<strong>Medicines</strong> <strong>Management</strong> Team/NMP lead: 01384 366589<br />
Nurse Prescribing Lead:<br />
<strong>Dudley</strong> Group of Hospitals <strong>Medicines</strong> Information Department: 01384 244088<br />
PCT Head of Security: 01384 366470; mobile 07825681857<br />
Police: 0845 113500<br />
52