Urology & Kidney Disease News Fall 2009 - Cleveland Clinic
Urology & Kidney Disease News Fall 2009 - Cleveland Clinic
Urology & Kidney Disease News Fall 2009 - Cleveland Clinic
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
24 <strong>Urology</strong> & <strong>Kidney</strong> <strong>Disease</strong> <strong>News</strong><br />
Prostate Cancer<br />
Brachytherapy and External Beam<br />
Radiotherapy for Prostate Cancer: A Comparison<br />
Jay P. Ciezki, MD<br />
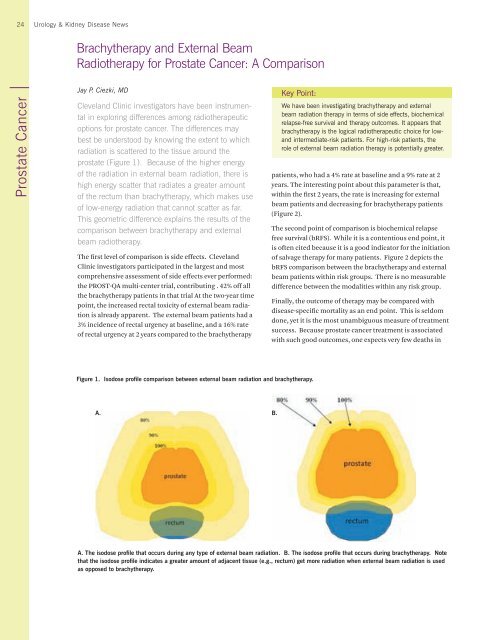
<strong>Cleveland</strong> <strong>Clinic</strong> investigators have been instrumental<br />
in exploring differences among radiotherapeutic<br />
options for prostate cancer. The differences may<br />
best be understood by knowing the extent to which<br />
radiation is scattered to the tissue around the<br />
prostate (Figure 1). Because of the higher energy<br />
of the radiation in external beam radiation, there is<br />
high energy scatter that radiates a greater amount<br />
of the rectum than brachytherapy, which makes use<br />
of low-energy radiation that cannot scatter as far.<br />
This geometric difference explains the results of the<br />
comparison between brachytherapy and external<br />
beam radiotherapy.<br />
The first level of comparison is side effects. <strong>Cleveland</strong><br />
<strong>Clinic</strong> investigators participated in the largest and most<br />
comprehensive assessment of side effects ever performed:<br />
the PROST-QA multi-center trial, contributing . 42% off all<br />
the brachytherapy patients in that trial At the two-year time<br />
point, the increased rectal toxicity of external beam radiation<br />
is already apparent. The external beam patients had a<br />
3% incidence of rectal urgency at baseline, and a 16% rate<br />
of rectal urgency at 2 years compared to the brachytherapy<br />
Key Point:<br />
<br />
A. B.<br />
We have been investigating brachytherapy and external<br />
beam radiation therapy in terms of side effects, biochemical<br />
relapse-free survival and therapy outcomes. It appears that<br />
brachytherapy is the logical radiotherapeutic choice for low-<br />
<br />
role of external beam radiation therapy is potentially greater.<br />
patients, who had a 4% rate at baseline and a 9% rate at 2<br />
years. The interesting point about this parameter is that,<br />
within the first 2 years, the rate is increasing for external<br />
beam patients and decreasing for brachytherapy patients<br />
(Figure 2).<br />
The second point of comparison is biochemical relapse<br />
free survival (bRFS). While it is a contentious end point, it<br />
is often cited because it is a good indicator for the initiation<br />
of salvage therapy for many patients. Figure 2 depicts the<br />
bRFS comparison between the brachytherapy and external<br />
beam patients within risk groups. There is no measurable<br />
difference between the modalities within any risk group.<br />
Finally, the outcome of therapy may be compared with<br />
disease-specific mortality as an end point. This is seldom<br />
done, yet it is the most unambiguous measure of treatment<br />
success. Because prostate cancer treatment is associated<br />
with such good outcomes, one expects very few deaths in