Value of the ventilation / perfusion scan in acute pulmonary ...
Value of the ventilation / perfusion scan in acute pulmonary ...
Value of the ventilation / perfusion scan in acute pulmonary ...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
t' ,<br />
~. ..Orig<strong>in</strong>al Contributions (\"f§;) 1fJ- \<br />
JI<br />
,<br />
<strong>Value</strong> <strong>of</strong> <strong>the</strong> Ventilation/Perfusion Scan<br />
<strong>in</strong> Acute Pulmonary Embolism<br />
Results <strong>of</strong> <strong>the</strong> Prospective Investigation <strong>of</strong><br />
Pulmonary Embolism Diagnosis (PIOPED)<br />
The PIOPED Investigators<br />
To determ<strong>in</strong>e <strong>the</strong> sensitivities and specificities <strong>of</strong> <strong>ventilation</strong>/<strong>perfusion</strong> lung nosis (PIOPED) <strong>in</strong>vestigators have as<strong>scan</strong>s<br />
for <strong>acute</strong> <strong>pulmonary</strong> embolism, a random sample <strong>of</strong> 933 <strong>of</strong> 1493 patients sessed <strong>the</strong> diagnostic usefulness <strong>of</strong>V/Q<br />
was studied prospectively. N<strong>in</strong>e hundred thirty-one underwent sc<strong>in</strong>tigraphy and lung <strong>scan</strong>s <strong>in</strong> <strong>acute</strong> <strong>pulmonary</strong> embo-<br />
755 underwent <strong>pulmonary</strong> angiography; 251 (33%) <strong>of</strong> 755 demonstrated pulmo- lism. ~e project protocol and consent<br />
nary embolism. Almost all patients with <strong>pulmonary</strong> embolism had abnormal forms. were approved by th.e .<strong>in</strong>st.itution<strong>scan</strong>s<br />
<strong>of</strong> high, <strong>in</strong>termediat8\ or low probability, but so did most without <strong>pulmonary</strong> al reV1ew b.o~rds.<strong>of</strong> all partlclpatl."g ce~-<br />
embolism (sensitivity, 98%; specificity, 10%). Of 116 patients with high-probabili- te~. (PartlcIFa;l~g c~nt~rs an~ ln~es~lty<br />
<strong>scan</strong>s an~ def<strong>in</strong>itive angiograms, 102 (88%) had <strong>pulmonary</strong> embolism, but ~i~~.)are IS eat e en 0 t e<br />
only a m<strong>in</strong>ority with <strong>pulmonary</strong> embolism had high-probability <strong>scan</strong>s (sensitivity,<br />
41 %; specificity, 97%). Of 322 with <strong>in</strong>termediate-probability <strong>scan</strong>s and def<strong>in</strong>itive METHODS<br />
angiograms, 105 (33%) had <strong>pulmonary</strong> embolism. Follow-up and angiography Patient Enrollment<br />
toge<strong>the</strong>r suggest pulmo~~ry embolism occurred amon.g 12% <strong>of</strong> ~at~ents with From January 1985 through Septemlo~~!-probability<br />
<strong>scan</strong>s. Cl<strong>in</strong>ical assessment comb<strong>in</strong>ed with <strong>the</strong> ventllatlon/perfu- ber 1986 <strong>in</strong> each <strong>of</strong> six cl<strong>in</strong>ical centers,<br />
sion <strong>scan</strong> established <strong>the</strong> diagnosis or exclusion <strong>of</strong> <strong>pulmonary</strong> embolism only for all patients for whom a request for a V/Q<br />
a m<strong>in</strong>ority <strong>of</strong> patients-those with clear and concordant cl<strong>in</strong>ical and <strong>ventilation</strong>! <strong>scan</strong> or a <strong>pulmonary</strong> angiogram was<br />
<strong>perfusion</strong> <strong>scan</strong> f<strong>in</strong>d<strong>in</strong>gs. made were considered for study entry.<br />
(lAMA. 1990;263:2753-2759) The eligible study population consisted<br />
, <strong>of</strong> patients, 18 years or older, <strong>in</strong>patients<br />
PERFUSION lung <strong>scan</strong>s have been re- would be abnormal <strong>in</strong> areas <strong>of</strong> pneumaand<br />
outpatients, <strong>in</strong> whom symptoms<br />
that suggested <strong>pulmonary</strong> embolism<br />
were present with<strong>in</strong> 24 hours <strong>of</strong> study<br />
ported to be sensitive <strong>in</strong> detect<strong>in</strong>g pul- nia or local hypo<strong>ventilation</strong>, but that <strong>in</strong> entry and without contra<strong>in</strong>dications to<br />
monary emboli, but many o<strong>the</strong>r condi- <strong>pulmonary</strong> embolism <strong>ventilation</strong> would angiography such as pregnancy, serum<br />
F edit t I t 2794<br />
or or 8 com men see p.<br />
be normal.z A number <strong>of</strong> <strong>in</strong>vestigator!<br />
have attempted to make <strong>ventilation</strong>/<br />
perfusIon .. (V/Q) <strong>scan</strong>s more useful for<br />
creat<strong>in</strong><strong>in</strong>e level greater than 260<br />
lJ.JnoUL, or hypersensitivity to contrast<br />
matena. I 0nce approac hed<br />
for <strong>the</strong><br />
diagnos<strong>in</strong>g <strong>pulmonary</strong> embolism by study, patients with recurrences were<br />
tions such as pneumonia or local classify<strong>in</strong>g <strong>the</strong>m not just as normal or not approached for recruitment a secbronchospasm<br />
cause <strong>perfusion</strong> defects.' abnormal, but if abnormal, as <strong>in</strong>dicat<strong>in</strong>g ond time.<br />
Ventilation <strong>scan</strong>s were added to <strong>perfusion</strong><br />
<strong>scan</strong>s with <strong>the</strong> idea that <strong>ventilation</strong><br />
high probability, <strong>in</strong>termediate probability<br />
(<strong>in</strong>determ<strong>in</strong>ate), or low probability<br />
I<br />
Recru tment<br />
<strong>of</strong> <strong>pulmonary</strong> embolism.s Under <strong>the</strong> aug;. A total <strong>of</strong> 5587 requests for V/Q <strong>scan</strong>s<br />
Repr<strong>in</strong>t requests to Division <strong>of</strong> Lung Diseases. Na. pices <strong>of</strong> <strong>the</strong> National Heart Lung and<br />
tional Room6A165333WestbardAve.Be<strong>the</strong>Sda.MD20892<br />
Heart. Lung. and BkJOd InstiMe. Westwood Bldg. Blood InstItute, . <strong>the</strong> Prospectlve '.' Inveswere<br />
recorded <strong>in</strong> <strong>the</strong> six PIOPED cl<strong>in</strong>i-<br />
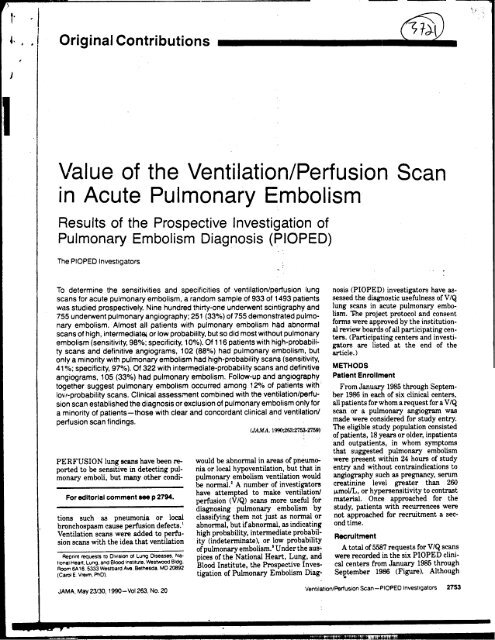
c al centers from January 1985t hrough (Carol E Vrelm. PhD) tigation <strong>of</strong> Pulmonary Embolism Diag- Sel1tember 1986 (Figure). Although<br />
JAMA. May 23/30. 1990-VoI263, No. 20 Ventilation/Perfusion Scan-PIOPED Investigators 2753<br />
,<br />
-
<strong>scan</strong>s were obta<strong>in</strong>ed with 1.5 x 10" Bq <strong>of</strong><br />
, technetium Tc 99m macroaggregated<br />
album<strong>in</strong> that conta<strong>in</strong>ed 100 000 to<br />
Requests for Lung Scans 700 000 particles us<strong>in</strong>g a 20% symmetric<br />
5587 w<strong>in</strong>dow set over <strong>the</strong> 140-keV energy<br />
peak. Particles were <strong>in</strong>jected <strong>in</strong>to an<br />
I I antecubital ve<strong>in</strong> over 5 to 10 respiratory<br />
cycles, with <strong>the</strong> patient sup<strong>in</strong>e or at<br />
Scan Requests Cancelled. most semierect. The <strong>perfusion</strong> images<br />
Scans Requested for Research Purposes. El19lbl~abents consisted <strong>of</strong> anterior, posterior, both<br />
I Diagnoses O<strong>the</strong>r Than Acute 6 posterior oblique, and both anterior<br />
Pulmonary Embolism, oblique views, with 750 000 counts per<br />
Patients In Whom Angiography ..<br />
Contra<strong>in</strong>dicated. and O<strong>the</strong>r Reasons Consent Consent l~age for each. Fo~ <strong>the</strong> lateral vIew<br />
, ( for Ineligibility Accord<strong>in</strong>g to Given Refused W1t~ <strong>the</strong> best perfusIon, 500 000 counts<br />
Study Design 1493 1523 per Image were collected: <strong>the</strong> o<strong>the</strong>r lat-<br />
~ 2571 eral view was obta<strong>in</strong>ed for <strong>the</strong> same<br />
length <strong>of</strong> time. Sc<strong>in</strong>tillation cameras<br />
f Random Sample with a wide field <strong>of</strong> view (38.1 cm <strong>in</strong><br />
; -diameter) were used with parallel-hole,<br />
; I low-energy, all-purpose collimators.<br />
t Not Selected for Selected for Perfus~on <strong>scan</strong>s were sat~sfa~tory or<br />
f Sensitivity and Sensitivity and better In 96% <strong>of</strong> cas.es, <strong>ventilation</strong> <strong>scan</strong>s<br />
! Specificity Analyses SpeCIficity Analyses adequate or better In 95%.<br />
( 560 933<br />
(<br />
I Angiography<br />
i I The femoral-ve<strong>in</strong> Seld<strong>in</strong>ger tech-<br />
I Inlerpretable Scan Scan nique with a multiple side-holed, 6F to<br />
Not Compleled Completed 8F pi<br />
gtai l ca<strong>the</strong>ter was used Small<br />
2 931 ..<br />
I: amounts <strong>of</strong> contrast matenal (5 to 8 mI,.)<br />
'; were <strong>in</strong>jected by hand, to check <strong>the</strong> pa-<br />
I tency <strong>of</strong> <strong>the</strong> <strong>in</strong>ferior vena cava by fluo-<br />
! roscopy. The ca<strong>the</strong>ter was directed <strong>in</strong>to<br />
Angiogram I Angiogram I <strong>the</strong> ma<strong>in</strong> <strong>pulmonary</strong> artery <strong>of</strong> <strong>the</strong> lung<br />
Completed Not Completed with <strong>the</strong> greatest V/Q <strong>scan</strong> abnormali-<br />
755 176 ty. I mtla .. 1 fil mlng .. was In t h e antero-<br />
I posterior projection. Seventy-six per-<br />
I cent iod<strong>in</strong>ated contrast material was<br />
Pulmonary Embolism Pulmonary Embolism Pulmonary ~rnbolism <strong>in</strong>jec~d at a rate <strong>of</strong> 20 to 35 mL/s for a<br />
Present Absent Uncer1a<strong>in</strong> total <strong>of</strong> 40 to 50 mL (2-second <strong>in</strong>jection).<br />
251 480 24 Film ra~s were three per second for 3<br />
seconds, followed by one per second for<br />
4 to 6 seconds. Depend<strong>in</strong>g on <strong>the</strong> size <strong>of</strong><br />
i .<strong>the</strong> lungs, film<strong>in</strong>g was not magnified or<br />
:' Flow char1 illustrat<strong>in</strong>g <strong>the</strong> numbers <strong>of</strong> r1!Quests for lung <strong>scan</strong>s. recruitment <strong>of</strong> patients, completion <strong>of</strong> lung given a low magnification <strong>of</strong> 1.4. A 12:1<br />
<strong>scan</strong>s. and results <strong>of</strong> angiography <strong>in</strong> <strong>the</strong> Prospectiw InvestigatIOn <strong>of</strong> Pulmonary Embolism Diagnosis. grid was used and roentgenographic<br />
factors were <strong>in</strong> <strong>the</strong> range <strong>of</strong> 70 to 80<br />
kilovolts (peak) and 0.025 to 0.040 sec-<br />
". onds at 1000 mA (large focal spot <strong>of</strong> 1.2<br />
...to 1.5 mm <strong>in</strong> diameter). If emboli were<br />
some patients could not be thoroughly Lung Scan :: not identified, <strong>in</strong>jections were repeated<br />
evaluatedpriortocompletion<strong>of</strong><strong>the</strong>V/Q and magnification (1.8 to 2.0 times)<br />
<strong>scan</strong>, cl<strong>in</strong>ical <strong>in</strong>vestigators made every The protocol directed <strong>ventilation</strong> and oblique views were obta<strong>in</strong>ed <strong>of</strong> <strong>the</strong> ar-<br />
effort to record <strong>the</strong>ir <strong>in</strong>dividual cl<strong>in</strong>ical <strong>perfusion</strong> studies with <strong>the</strong> subject <strong>in</strong> <strong>the</strong> eas suspicious for <strong>pulmonary</strong> embolism.<br />
impressions as to <strong>the</strong> likelihood <strong>of</strong> pul- upright position, but o<strong>the</strong>r positions Films were obta<strong>in</strong>ed with an air-gap<br />
monary embolism prior to learn<strong>in</strong>g <strong>the</strong> were acceptable. VentilatiOn studies technique (ie, no grid used). Roent-<br />
i results <strong>of</strong> V/Q <strong>scan</strong>s and angiography. were performed with 5.6 x 10' to genographic factors were <strong>in</strong> <strong>the</strong> range <strong>of</strong><br />
: Impressions were based on an agreed on 11.1 x 10' Bq <strong>of</strong> xenon 133 us<strong>in</strong>g a 20% 78 to 88 kV(p) and 0.040 to 0.080 seconds<br />
~ set <strong>of</strong> <strong>in</strong>formation-history, results <strong>of</strong> symmetric w<strong>in</strong>dow set over <strong>the</strong> 8O-keV at 160 mA (small focal spot <strong>of</strong> 0.3 to 0.6<br />
1 physical exam<strong>in</strong>ation, arterial blood gas energy peak. They started with a mm <strong>in</strong> diameter). If no emboli were<br />
: analyses, chest roentgenograms, and 100 OOO-count, pos~rior-view, first- found <strong>in</strong> <strong>the</strong> first lung, or if bila~ral<br />
electrocardiograms-but without stan- breath image and <strong>the</strong>n pos~rior equi- angiography <strong>in</strong> <strong>the</strong> cl<strong>in</strong>ical cen~r was<br />
dardized diagnostic algorithms. The librium (wash-<strong>in</strong>) images for two con- rout<strong>in</strong>e, identical techniques were used<br />
medical records <strong>of</strong> a random sample <strong>of</strong> secutive 120-second periods. Washout for <strong>the</strong> second lung. Angiography was<br />
patients who refused or were <strong>in</strong>eligible consisted <strong>of</strong> three serial 45-second pos- completed with<strong>in</strong> 24 hours, and usually<br />
for study entry (refuser/<strong>in</strong>eligible pa- terior views, 45-second left and right with<strong>in</strong> 12 hours <strong>of</strong> V/Q <strong>scan</strong>s. Pulmo-<br />
'. -tients) were evaluated retrospectively pos~rior oblique views, and a f<strong>in</strong>al 45- .nary angiograms were adequate or bet-<br />
,.~ for comparison with study patients. second pos~rior view. Then, <strong>perfusion</strong> ~r <strong>in</strong> ~5% <strong>of</strong> cases.<br />
;~<br />
jf 2754 JAMA. May 23/30. 1990-VoI263, No 20 Ventilation/Perfusion Scan-PIOPED Investigators~
.<br />
'Pq <strong>of</strong> Central Scan and Table 1-PIOPED Central Scan Interpretation Categories and Criteria'<br />
'gated<br />
)() ~o<br />
Angiogram Interpretations<br />
Two nuclear medic<strong>in</strong>e readers, not<br />
c,,-~ ---~-~,,~ -<br />
High probability<br />
;,,2 Large (> 750/0 <strong>of</strong> a segment) segmental perf1JSIOn defects WIthout correspond<strong>in</strong>g ~ntilation or roenlgenonetric<br />
from <strong>the</strong> center that performed <strong>the</strong> graphIC abnom1alitles or substantially larger than eI<strong>the</strong>r match<strong>in</strong>g ventIlation or chest roentgenogram<br />
nergy<br />
Ito an ~<br />
-atory<br />
or at<br />
llages<br />
..abnom181ltles<br />
<strong>scan</strong>, mdepe?dently Interpreted <strong>the</strong><br />
lung <strong>scan</strong>s WIth chest roentgenograms<br />
accordl 'ng to preestabl ' h d t d .t<br />
IS e S u y cn e-<br />
ria (Table 1). Angiograms were likewise<br />
d I . d ..Bordertlne<br />
ran om y asslgne. .w pairs <strong>of</strong> angIo-<br />
;,,2 Moderate segmental (;,,25% and ~75% <strong>of</strong> a segment) perf1JsK)n defects without match<strong>in</strong>g ~ntilation or chest<br />
roentgenogram abnOm1alitles and 1 large mIsmatched segmental defect<br />
;,,4 Moderate segmental perf1JsK)n defects without <strong>ventilation</strong> or chest roentgenogram abnom1alities<br />
IntermedIate probabIlity (Indetem1<strong>in</strong>ate)<br />
Not lall<strong>in</strong>g <strong>in</strong>to nom1al. ve~low-. low-, or high-probability categories<br />
high or borderlIne low<br />
DIfficult to categonze as low or high<br />
both<br />
terior<br />
ts<br />
per<br />
VIeW<br />
~ounts<br />
er latsame<br />
graphers from clInical centers o<strong>the</strong>r<br />
than <strong>the</strong> ori .nnat<strong>in</strong> g hos p ital The an-<br />
.e' .'.<br />
gIogram readers Interpreted <strong>the</strong> angIograms<br />
with lung <strong>scan</strong>s as hav<strong>in</strong>g <strong>acute</strong><br />
uI b I ..Large<br />
p m.onary e~ 0 I.sm present-which<br />
required <strong>the</strong> IdentIfication <strong>of</strong> an embo-<br />
I b t t . I th tl ' f<br />
US 0 S ruc mg a vesse or e ou me 0<br />
Low probability<br />
Nonsegmental perf1Jsion defects (~, ~ry small effusion caus<strong>in</strong>g blunt<strong>in</strong>g <strong>of</strong> <strong>the</strong> costophrenic angle. cardiomegaly.<br />
enlarged aorta. hIla. and medIastInum, and elevated dIaphragm)<br />
S<strong>in</strong>gle moderate mIsmatched segmental perfuSK)n defect with nom1al chest roentgenogram<br />
Any perf1JSlon defect with a substantially larger chest roentgenogram abnOm1ality<br />
or moderate segmental perf1JSIOn defects InvolvIng no more than 4 segments <strong>in</strong> 1 lung and no more than<br />
3 segments In 1 lung regIOn with match<strong>in</strong>g ~ntilation defects ei<strong>the</strong>r equal to or larger In size and chest<br />
roentgenogram eI<strong>the</strong>r nom1al or with abnom1alltles substantially smaller than perf1JSIOn defects<br />
>3 Small segmental perf1JsK)n defects «25% <strong>of</strong> a segment) with a nom1al chest roentgen.v.ram<br />
Very low probability .._"<br />
me~<br />
cm m<br />
an embolus (fill<strong>in</strong>g deti ct) with<strong>in</strong> a vesse<br />
I -a b sent, or uncert . m. If two read-<br />
~3 Small segmental perf1Jsion defects with a nom1al chest roentgenogram<br />
Nom1al No perf1Jsion defects present<br />
l<br />
-hole, ers disagreed, <strong>the</strong> <strong>in</strong>terpretations'were Perf1J$ion outl<strong>in</strong>es exactly <strong>the</strong> shape <strong>of</strong> <strong>the</strong> lungs as seen on <strong>the</strong> chest roentgenogram (hilar and aortic impressions<br />
ators. adjudicated by readers who were se- may be si3en. chest roentgenogram and/or <strong>ventilation</strong> study may be abnom1al)<br />
ry or le~t~d randomly fro~ .<strong>the</strong>. rema<strong>in</strong><strong>in</strong>g 'PIOPED <strong>in</strong>dicates Prospectiw Investigation <strong>of</strong> Pulmonary Embolism Dia nosis<br />
<strong>scan</strong>s clInical centers. If adJudIcatIng readers g<br />
did not agree with ei<strong>the</strong>r <strong>of</strong> <strong>the</strong> first two<br />
readers, <strong>scan</strong>s or angiograms went to<br />
panels <strong>of</strong> nuclear medic<strong>in</strong>e or angiogra- Table 2 -Recruitment <strong>of</strong> Patients and Completion <strong>of</strong> Angiography'<br />
phy readers. The f<strong>in</strong>al adjudicated V IQ<br />
tech- <strong>scan</strong> read<strong>in</strong>gs consisted <strong>of</strong> four catego- 0/. <strong>of</strong><br />
6F to . h. h b b ' l ' . d .Eligible No. <strong>of</strong> PfOPEO P.tlent. With<br />
nes- Ig pro a Ilty, mterme late Patient. Lung Scan. Who Were Seiec1ed for Angiogram.<br />
Small probability (<strong>in</strong>determ<strong>in</strong>ate), low proba- Cl<strong>in</strong>ical Center Recruited Anglographlc Pu..ult Obta<strong>in</strong>ed. No. ("!o}<br />
8mL) bility, and low/very low probability ~ukeU~n~~ity 46 --137 1,15-'84)'-'<br />
le pa- through normal (near normal/normal). Henry ~ord Hos~it81 62 228 177 (78)<br />
.~uo- The near-normal/normal category <strong>in</strong>- ~assachus~~ ~eneral Hospjtal 33 140 120 (86)<br />
d Into cludes read<strong>in</strong>gs <strong>of</strong> very low probability University <strong>of</strong> Michigan 52 102 65 (64)<br />
~ lun~ by one reader and low probability by <strong>the</strong> University 01 Pennsylvania 70 168 134 (80)<br />
~all- o<strong>the</strong>r, very low probability by both, ~aleuniversity 43 156 144 (92)<br />
1tero- very low probability by one and normal Total 50 931 755 (81)<br />
per- by <strong>the</strong> o<strong>the</strong>r, and normal by both. Re- ,<br />
1 was fu I. I.. bl t ' ts' PIOPED Indicates Prospective Investigation <strong>of</strong> Pulmonary Embolism Diagnosis<br />
ser me IgI e pa Ien <strong>scan</strong>s were .<br />
~or a read <strong>in</strong> each cl<strong>in</strong>ical center by <strong>the</strong> cl<strong>in</strong>i-<br />
'tlon). cal center's PIOPED nuclear medic<strong>in</strong>e<br />
for 3 reader(s) and not reread.<br />
1d for F II d lants and <strong>in</strong> whom no outcome event 900 to 1000 patients <strong>in</strong> <strong>the</strong> random sam-<br />
:ze <strong>of</strong> 0 ow-up an ..suggested <strong>pulmonary</strong> embolism. Pul- pie for PIOPED angiography was<br />
d or Outcome ClassIfication monary embolism status could be deter- planned to obta<strong>in</strong> estimates <strong>of</strong> sensitiv-<br />
12:1 Patients were contacted by telephone m<strong>in</strong>ed as positive or negative for 902 ityand specificity with 95% CIs no wid-<br />
1hic at I, 3, 6, and 12 months after study patients. A cl<strong>in</strong>ical assessment <strong>of</strong> <strong>the</strong> er than == 8%. To determ<strong>in</strong>e <strong>the</strong> sensi-<br />
; 80 entry. Deaths, new studies for pulmo- likelihood <strong>of</strong> <strong>pulmonary</strong> embolism was tivity and specificity <strong>of</strong> V IQ lung <strong>scan</strong>s<br />
,ec- nary embolism, and major bleed<strong>in</strong>g available for 887 (98%) <strong>of</strong> <strong>the</strong>se patients. without <strong>the</strong> biases associated with hap-<br />
1.2 complications were reviewed by an out- hazard patierlt selection (ie, conveere<br />
come classification committee us<strong>in</strong>g all Statistical Methods nience sampl<strong>in</strong>g).8.t a 933-patient sam-<br />
lted available <strong>in</strong>formation. Only 23 (2.5%) <strong>of</strong> Probability values for <strong>the</strong> comparison pie <strong>of</strong> <strong>the</strong> 1493 patients who consented<br />
mes) <strong>the</strong> 931 patients had <strong>in</strong>complete (16) or <strong>of</strong> percentages and proportions and 95% to PIOPED participation was selected<br />
\e ar- no (7) follow-up. Angiograms, follow-up confidence <strong>in</strong>tervals (CIs) were calcu- accord<strong>in</strong>g to random sampl<strong>in</strong>g sched-<br />
\lism, data, and outcome classifications were lated us<strong>in</strong>g standard: tests.' A ~ test ules created separately by <strong>the</strong> data and<br />
r-gap used to determ<strong>in</strong>e <strong>pulmonary</strong> embolism for homogeneity <strong>of</strong> proportions was coord<strong>in</strong>at<strong>in</strong>g center for each cl<strong>in</strong>ical cenoent-<br />
status as positive for patients with an- used to compare distributions.' Sensi- ter, The PIOPED protocol required<br />
1ge <strong>of</strong> giograms that showed <strong>pulmonary</strong> em- tivity is def<strong>in</strong>ed as <strong>the</strong> proportion <strong>of</strong> <strong>the</strong>se 933 patients to undergo angiogra-<br />
:onds boli and for patients for whom outcome cases <strong>of</strong> <strong>pulmonary</strong> embolism correctly phy if <strong>the</strong>ir <strong>scan</strong>s were abnormal, Of <strong>the</strong><br />
:00.6 review established <strong>the</strong> presence <strong>of</strong> pul- diagnosed and specificity as <strong>the</strong> pro- 933 patients selected for angiography, 1<br />
were monary emboli at <strong>the</strong> time <strong>of</strong> PIOPED portion <strong>of</strong> diagnoses that <strong>pulmonary</strong> patient died before <strong>the</strong> V/Q <strong>scan</strong> could<br />
lteral recruitment. Pulmonary embolism sta- embolism is absent for patients without be completed and 1 o<strong>the</strong>r patient's V/Q<br />
.was tus was determ<strong>in</strong>ed as negative for pa- <strong>pulmonary</strong> embolism. Sensitivity, spe- <strong>scan</strong> was determ<strong>in</strong>ed to be un<strong>in</strong>terpreused<br />
tients with angiograms that did not cificity, and percent agreement have table. These 2 patients are not fur<strong>the</strong>r<br />
.was show <strong>pulmonary</strong> emboli and no contrary been calculated accord<strong>in</strong>g to standard reported here<strong>in</strong>.<br />
ually outcome review and for patients who methods for proportion8,' Analyses<br />
.lImo- lacked a def<strong>in</strong>itive angiogram read<strong>in</strong>g were performed with <strong>the</strong> Statistical RESULTS<br />
.bet- who were discharged from <strong>the</strong> hospital Package for <strong>the</strong> Social Sciences statisti- Of <strong>the</strong> 3016 patients eligible for<br />
without a prescription for anticoagu- cal s<strong>of</strong>tware package.' Recruitment <strong>of</strong> PIOPED, 1493 (50%) gave consent to<br />
gators JAMA. May 23/30. 1990-VoI263, No 20 Ventilation/Perfusion Scan-PIOPED Investigators 2755<br />
~~- "';::: -I<br />
.
., Table 3-Patienl Characteristics' Table 4-Comparison <strong>of</strong> Scan Category With Angiogram F<strong>in</strong>d<strong>in</strong>gs<br />
Refuser! Pulmonary Pulmonary Pulmonary<br />
Ta<br />
-<br />
PtOPEO<br />
IN = 931l<br />
<strong>in</strong>eligible<br />
IN = 326) Scan Category<br />
Embolism<br />
Present<br />
Embolism<br />
Ab8ent<br />
Embolism<br />
Uncerta<strong>in</strong><br />
No<br />
Angiogram<br />
Tota'<br />
No,<br />
Age (mean), y 56.1 564 High probability 102 14 1 7 124<br />
Male. %<br />
Service. %<br />
45 44<br />
Intermediate probability 105 217 9 33 364<br />
Medical/CCU 40<br />
Surgical 18<br />
Emergency depanmenVcllnoc 30<br />
36<br />
21<br />
32<br />
low probability<br />
Near normai/normai<br />
~<br />
39<br />
5<br />
199<br />
50<br />
12<br />
2<br />
62<br />
74<br />
312<br />
131 H;<br />
-<br />
ICU 10 10 Total 251 480 24 178 931 ~<br />
O<strong>the</strong>r<br />
Hospital monaiity. %<br />
1<br />
9<br />
1<br />
10<br />
La<br />
N;<br />
-<br />
'PIOPED Indicates Prospective Investigation at Pul- To<br />
and<br />
monary<br />
ICU,<br />
Embolism<br />
<strong>in</strong>tensive<br />
DiagnosIs'<br />
care unit."<br />
CCU coronary care unit.<br />
,<br />
"<br />
,able 5.-Companson <strong>of</strong> Scan Category With Angiogram F<strong>in</strong>d<strong>in</strong>gs. Sensitivity and SpecifICity<br />
-<br />
Scan Category<br />
High probability<br />
Sen81tlvtty, %<br />
41<br />
Specificit y % .'<br />
97<br />
cli<br />
High or <strong>in</strong>termediate probability 82 52<br />
participate <strong>in</strong> PIOPED (Figure). The High. <strong>in</strong>lermediate. or low probability 98 10<br />
cl<strong>in</strong>ical centers varied <strong>in</strong> <strong>the</strong> percentage er<br />
<strong>of</strong> eligible patients for whom consent<br />
could be obta<strong>in</strong>ed, from 33% to 70%, and<br />
p,<br />
a<br />
<strong>in</strong> <strong>the</strong> percentage <strong>of</strong> patients for whom <strong>of</strong> angiograms, respectively. In only 13 sitivity for thromboemboli on angiogra- U<br />
angiograms were obta<strong>in</strong>ed among those<br />
selected to determ<strong>in</strong>e <strong>the</strong> sen~tivity<br />
(1.7%) <strong>of</strong> i55 angiograms was panel adjudication<br />
necessary.<br />
phy <strong>in</strong>creased to 207 (82%) <strong>of</strong> 251 (95%<br />
CI, 78% to 87%). If <strong>the</strong> patient had ei-<br />
~<br />
It<br />
and specificity <strong>of</strong> V /Q lung <strong>scan</strong>s.<br />
(PIOPED angiographic pursuit). from Scan F<strong>in</strong>d<strong>in</strong>gs<br />
<strong>the</strong>r a high-, <strong>in</strong>termediate-, or lowprobability<br />
V/Q <strong>scan</strong>, <strong>the</strong>n 246 <strong>of</strong> 251<br />
a;<br />
P<br />
64% to 92% (Table 2). The PIOPED pa- Most (676) <strong>of</strong> <strong>the</strong> 931 patients had had thromboemboli on angiography, a \\<br />
tients resembled refuser/<strong>in</strong>eligible pa- <strong>in</strong>termediate- or low-probability V/Q sensitivity <strong>of</strong> 98% (95% CI, 96% to (~<br />
tients <strong>in</strong> a variety <strong>of</strong> cl<strong>in</strong>ical characteris- <strong>scan</strong> read<strong>in</strong>gs (39% and 34%, respec- 100%).<br />
tics (Table 3). The PIOPED patients tively) (Table 4). Only 131 (14%) had Only 14 (3%) <strong>of</strong> 480 patients who did: g<br />
and refuser/<strong>in</strong>eligible patients were different,<br />
however, <strong>in</strong> <strong>the</strong>ir lung <strong>scan</strong> abnormalities<br />
(P
~ Table 6 -Pulmonary Embolism (PE) Status'<br />
ul<br />
o.<br />
-~ Cl<strong>in</strong>ical Science Prob8bllity, %<br />
.-<br />
24<br />
-"<br />
54<br />
12 Scan Ca1egory<br />
80.100<br />
~ +/No.<br />
<strong>of</strong> Patient. %<br />
20-79<br />
PE + /No.<br />
<strong>of</strong> Patient. %<br />
0019<br />
-.<br />
PE + /No<br />
<strong>of</strong> Patient. Of.<br />
All PTObabllltte.<br />
PE + /No<br />
<strong>of</strong> Patient. °/.<br />
.11 High probability 28/29 96 70/80 88 -5~ ~ -'1~~;;~'~'. ~~<br />
.11 Intem1ediateprobability 27/41 66 66/236 2~ 1~~ ~~ ;~~ ~<br />
-Low ., probability ,, , 6/15 ~- 40 30/191 ~~ ~ .~ ';~ ~,-~V ~ ,~<br />
Near normal/normal<br />
~<br />
0/5 0 4/62<br />
~-~~-<br />
6 1/61 2<br />
-~"~V<br />
5/128 4<br />
~<br />
Total 61~ 66 170/569 30 21/228 9 252/887 28<br />
-emboll~m status IS based on anglogr~m Interpretation tor 713 patients, on angiogram <strong>in</strong>terpretation and outcome classification commit1ee reassignment tor 4 patients, and on<br />
~ CllnlCallntormation alone (wi1hout def<strong>in</strong>itIVe angIography) tor 170 patients.<br />
-embolism was only 74% (14/19), com- before <strong>the</strong> <strong>scan</strong> was performed ("prior COMMENT<br />
pared with 91% (88/97) for those without probability") was compared with pula<br />
history <strong>of</strong> <strong>pulmonary</strong> embolism monary embolism status as determ<strong>in</strong>ed The PIOPED study was conducted as<br />
~- (~% ~Ict:ve valu,es reflects ,a,loss I)f specifi~- tion (T~~le 6) for 887 patients with pri.or mate <strong>the</strong> sensitivity and specificity <strong>of</strong><br />
ei- Ity m <strong>the</strong> hIgh-probabIlity V/Q <strong>scan</strong> dI- probabIlIty assessments and defimte <strong>the</strong> V/Q lung <strong>scan</strong> for <strong>the</strong> diagnosis <strong>of</strong><br />
,w- agnosis for patie~ts with histories <strong>of</strong> <strong>pulmonary</strong> embolism status. A cl<strong>in</strong>ical <strong>pulmonary</strong> embolism. O<strong>the</strong>r retrospec-<br />
:51 <strong>pulmonary</strong> embolIsm (88%) vs those assessment <strong>of</strong> 80% to 100% likelihood <strong>of</strong> tive and prospective studies have fo-<br />
.a with no prior <strong>pulmonary</strong> embolism <strong>pulmonary</strong> embolism was made <strong>in</strong> 00 cused on positive predictive values.<br />
to (98%) (P
,} successfully recruited for PIOPED. If ment with <strong>the</strong> <strong>in</strong>terpretation <strong>of</strong> <strong>the</strong> <strong>scan</strong> grams. N<strong>in</strong>ety-five patients (31%) had CI<br />
anyth<strong>in</strong>g, this selection bias would sug- is supported by <strong>the</strong> PIOPED study. The <strong>pulmonary</strong> emboli demonstrated on an- Du<br />
gest that PIOPED tends to overesti- predictive value <strong>of</strong> <strong>the</strong> high- and low- giography. The predictive values from I<br />
mate V /Q <strong>scan</strong>s' sensitivities and:under- probability lung <strong>scan</strong>s improved when <strong>the</strong>ir study are similar to PIOPED re- ~<br />
estimate specificities. supported by similar cl<strong>in</strong>ical assess- suits <strong>in</strong> <strong>the</strong> high-probability and <strong>in</strong>ter- .<br />
Cl<strong>in</strong>ical decisions are <strong>of</strong>ten made on ments. For 90 patients, <strong>the</strong> negative mediate-probability (<strong>in</strong>deterrn<strong>in</strong>ate) ~<br />
<strong>the</strong> basis <strong>of</strong> <strong>the</strong> predictive values, which predictive value <strong>of</strong> <strong>the</strong> low-probability <strong>scan</strong> categories. The PIOPED study, He!<br />
depend not only on <strong>the</strong> test's sensitivity <strong>scan</strong> rose to 96% when accompanied by a likewise, found <strong>pulmonary</strong> emboli F<br />
and specificity, but also on <strong>the</strong> preva- cl<strong>in</strong>ical assessment <strong>of</strong> low likelihood. In among patients with <strong>scan</strong>s <strong>in</strong> <strong>the</strong> low- ~<br />
lence <strong>of</strong> disease <strong>in</strong> <strong>the</strong> population stud- 29 patients, <strong>the</strong> positive predictive val- probability category, but fewer than ,4<br />
ied. Based on angiogram resul~~, <strong>the</strong> ue <strong>of</strong> a high-probability <strong>scan</strong> <strong>in</strong>creased <strong>the</strong> 25% for subsegrnental matched le- M~<br />
prevalence <strong>of</strong> <strong>pulmonary</strong> embolIsm <strong>in</strong> to 96% if supported by a high-likelihood sions and 40% for subsegrnental mis- ~<br />
PIOPED was 33% (251/755) (Table 4); cl<strong>in</strong>ical assessment. In <strong>the</strong> PIOPED ex- matched lesions found by Hull et al. Pa- (<br />
based on <strong>pulmonary</strong> embolism status- perience, comb<strong>in</strong><strong>in</strong>g a lung <strong>scan</strong> <strong>in</strong>ter- tient referral patterns or lung <strong>scan</strong> J.<br />
derived from angiogram evaluation and! pretation with a strong cl<strong>in</strong>ical suspi- <strong>in</strong>terpretation criteria may account for ~<br />
or cl<strong>in</strong>ical evaluation-<strong>the</strong> prevalence cion as to whe<strong>the</strong>r <strong>acute</strong> <strong>pulmonary</strong> <strong>the</strong> differences between PIOPED re- u~<br />
was 28% (Table 6), similar to <strong>the</strong> preva- embolism is present is a sound diagnoslences<br />
described <strong>in</strong> previous reports. '3-21 tic strategy, as previously suggested by<br />
suIts and <strong>the</strong> Hamilton study results.<br />
S<strong>in</strong>ce angiographic studies are not<br />
J<br />
E<br />
In PIOPED, <strong>the</strong> posi~i.ve predictive val- M~Neil and collea~es, ~,21 but is. suf- available ~nd cl<strong>in</strong>ical fol~ow-up has not ~<br />
ue <strong>of</strong> <strong>the</strong> high-probabIlIty <strong>scan</strong> was .8$_%, ficient for only a mmonty <strong>of</strong> patIents been applIed to determ<strong>in</strong>e <strong>pulmonary</strong> v<br />
whereas <strong>the</strong> negative predictive v"a1\i'e (Table 6). For a substantial number <strong>of</strong> embolism status for <strong>the</strong> 110 patients<br />
<strong>of</strong> a low-probability <strong>scan</strong> was 84%. The<br />
negative predictive value <strong>of</strong> <strong>the</strong> nearpatients<br />
<strong>in</strong> <strong>the</strong> PIOPED study, angiography<br />
was required for a def<strong>in</strong>itive diagwithout<br />
adequate angiography, for <strong>the</strong><br />
22 patients without adequate ventila-<br />
.<br />
Re<br />
norrnaVnorrnal <strong>scan</strong> category was bet- nosis <strong>of</strong> <strong>pulmonary</strong> embolism, tion <strong>scan</strong>s, and for <strong>the</strong> patients with 1.<br />
ter at 91 %. Estimates <strong>of</strong> negative pre- The PIOPED study employed pulmo- norrnal <strong>scan</strong>s <strong>in</strong> <strong>the</strong> Hamilton District Me<br />
dictive values <strong>in</strong>creased when analyses nary angiography, which proved to be a Thromboembolism Programme, com- ~~<br />
took <strong>in</strong>to account patients who did "nOt safe and accurate method <strong>of</strong> diagnos<strong>in</strong>g parisons <strong>of</strong> estimates <strong>of</strong> sensitivity and 2.<br />
undergo angiography, did not receive <strong>pulmonary</strong> embolism, although it is <strong>in</strong>- specificity between <strong>the</strong> two studies are Jos<br />
anticoagulants, and had no evidence <strong>of</strong> vasive, The four patients (0.5%) for not possible. agr<br />
<strong>pulmonary</strong> embolism occurr<strong>in</strong>g dur<strong>in</strong>g 1 whom <strong>the</strong> outcome classification com- The PIOPED results lead to a num- : i~<br />
year <strong>of</strong> follow-up. Includ<strong>in</strong>g <strong>the</strong>se pa- mittee disagreed with bl<strong>in</strong>ded angio- ber <strong>of</strong> conclusions that settle controver- BA<br />
tients among those not hav<strong>in</strong>g pulmo- gram <strong>in</strong>terpretations that showed <strong>acute</strong> sies about <strong>the</strong> diagnostic value <strong>of</strong> <strong>the</strong> mo<br />
nary embolism <strong>in</strong> <strong>the</strong> analysis improved <strong>pulmonary</strong> embolism to be absent must lung <strong>scan</strong> <strong>in</strong> <strong>pulmonary</strong> embolism.~'" A 100<br />
<strong>the</strong> negative predictive value <strong>of</strong> <strong>the</strong> low- be considered carefully <strong>in</strong> light <strong>of</strong> <strong>the</strong> high-probability <strong>scan</strong> usually <strong>in</strong>dicates ~<br />
probability <strong>scan</strong> from 84% to 88% and <strong>of</strong> angiographic criteria's design for <strong>acute</strong> <strong>pulmonary</strong> embolism, but only a m<strong>in</strong>or- 100<br />
<strong>the</strong> near-norrnaVnorrnal <strong>scan</strong> from 91% <strong>pulmonary</strong> embolism, <strong>the</strong> variable time ity <strong>of</strong> patients with <strong>pulmonary</strong> embo- 5. , i<br />
to 96%. Because some <strong>in</strong>stances <strong>of</strong> <strong>acute</strong> between angiographic evaluation and lism have a high-probability <strong>scan</strong>. A his- <strong>the</strong> I<br />
<strong>pulmonary</strong> embolism may not have been <strong>the</strong> patients' deaths, and <strong>the</strong> variability tory <strong>of</strong> <strong>pulmonary</strong> embolism decre~es ~<br />
detected among <strong>the</strong>se patients, <strong>the</strong> true <strong>in</strong> pathophysiology and pathological <strong>in</strong>- <strong>the</strong> accuracy <strong>of</strong> diagnoses based on hlgh- Sor,<br />
negative predictive values may be less terpretation <strong>of</strong>thromboemboli <strong>in</strong> evolu- probab~lity <strong>scan</strong>s. A. .low-probabil.ity 7. :<br />
than 88% for low-probability <strong>scan</strong>s and tion. In <strong>the</strong> PIOPED study, a norrnal <strong>scan</strong> WIth a strong clInical ImpreSSIon NY<br />
96% for near-norrnaVnorrnal <strong>scan</strong>s, but angiogram almost excluded <strong>the</strong> possibil- that <strong>pulmonary</strong> embolism is not likely ~:<br />
still ought to be closer to <strong>the</strong>se latter<br />
values than to <strong>the</strong> 84% and 91% which<br />
ity <strong>of</strong> <strong>pulmonary</strong> embolism, confirm<strong>in</strong>g<br />
<strong>the</strong> results <strong>of</strong> two previous studies. '4,'0<br />
makes <strong>the</strong> possibility <strong>of</strong> lJulmonary embolism<br />
remote. Near-norrnal/norrnal<br />
197<br />
9.<br />
did not account for patients without an- The PIOPED f<strong>in</strong>d<strong>in</strong>gs extend ob- lung <strong>scan</strong>s make <strong>the</strong> diagnosis <strong>of</strong> <strong>acute</strong> mo;<br />
giography results. servations made by o<strong>the</strong>r <strong>in</strong>vesti~- <strong>pulmonary</strong> embolis~ :"ery u~likely. A~ ~::<br />
Although <strong>pulmonary</strong> emboli did occur tors,l-3,I2-8! from whom <strong>the</strong> PIOPED m- IntermedIate-probabIlIty (mdeternll-<br />
<strong>in</strong> patients with <strong>scan</strong>s classified <strong>in</strong> <strong>the</strong> vestigators derived stu?y criteria, for n.ate) sc.an is not <strong>of</strong> help <strong>in</strong> establish<strong>in</strong>g a<br />
categories between low probability and angiogramand.V/.Q <strong>scan</strong> mterpreta.tIon. d~agnosl~. In. ~IOPED, <strong>the</strong> <strong>scan</strong> c°':l1norrnal,<br />
<strong>pulmonary</strong> embolism was docu- Although predIctIve values for patIents bmed WI~h clI~lcal.asses~ment pe~Itmented<br />
<strong>in</strong> only 5 (4%) <strong>of</strong> 131 <strong>of</strong> such with high-probability <strong>scan</strong>s and pa- ted a nOn<strong>in</strong>vasIve dlagnosI~ or excluslo~<br />
patients. The true proportion <strong>of</strong> pa- tients with low-probability <strong>scan</strong>s i~ pre- <strong>of</strong> a.cute pul':l1°nary embolism for a mItients<br />
with <strong>pulmonary</strong> embolism must vious series are generally consIstent nonty<strong>of</strong>patlents.<br />
be <strong>in</strong>ferred with caution, because large with <strong>the</strong> PIOPED f<strong>in</strong>d<strong>in</strong>gs, <strong>the</strong> underb<br />
f ' . h V t t. f t. t '<br />
norrnal <strong>scan</strong>s were not successfully re- probability <strong>scan</strong>s m preVIous studIes 34010, NO1-HR-34011, NO1-HR-34012. and NO1cruited<br />
for <strong>the</strong> study. Only 42% <strong>of</strong> <strong>the</strong> has <strong>in</strong> <strong>the</strong> past led to an exaggerated HR-34013 from <strong>the</strong> National Heart. Lung. and<br />
131 PIOPED patients <strong>in</strong> this category<br />
comp Ie ted ang1ograp .h y. 0 n 1 yo. 3 f<strong>the</strong> 21<br />
impression <strong>of</strong> <strong>the</strong> sensitivity <strong>of</strong> <strong>the</strong> high-<br />
Probabilit y lung <strong>scan</strong>. -111'<br />
Blood Institute: Be<strong>the</strong>sda, Md.<br />
been The greatly secretarial appreCIated. asSIStance <strong>of</strong> JoAnne Decker has<br />
patients with lung <strong>scan</strong>s read as norrnal The f<strong>in</strong>d<strong>in</strong>gs <strong>of</strong> Hull and colleagues'<br />
by both readers on <strong>the</strong> f<strong>in</strong>al read<strong>in</strong>g<br />
completed anmography' e" all 3 had normal<br />
<strong>pulmonary</strong> angiograms. None <strong>of</strong> <strong>the</strong><br />
rema<strong>in</strong><strong>in</strong>g 18 had cl<strong>in</strong>ically evident pul-<br />
.. m()nary embolI on follow-up. This f<strong>in</strong>di!1<br />
<strong>the</strong> Hamilton District ~romboe;mbolIsm<br />
". Programme are partIcularly . mterestmg<br />
m companson W1 th <strong>the</strong> PIOPED<br />
results. Of <strong>the</strong> 305 patients with susd<br />
1 b 1. d b<br />
pecte pu ':I1°nary em 0 I~m an, a nor-<br />
Steer<strong>in</strong>g Committee<br />
. II<br />
ThePIOP~LJlnvestlgatorsareaslo<br />
-,<br />
ows:<br />
H~rbert A. s~ MD, chairman; Abass<br />
AlaV1, MD, Rlch~reenspan, MD, Charles A.<br />
Hales, MD, Paul 0, ~ MD, Michael Terr<strong>in</strong>.<br />
<strong>in</strong>g is consistent with <strong>the</strong> f<strong>in</strong>d<strong>in</strong>gs <strong>of</strong> mal perfusIon lung <strong>scan</strong>s m <strong>the</strong>Ir ~tU?y, MD. MPH, Carol Vreim. PhD, John G. Weg, MD;<br />
Kipper et al.~ 173 (57%) had adequate ventllatl~n alternates: ChristOB Athanasoulis, MD, Alexander<br />
The value <strong>of</strong> comb<strong>in</strong><strong>in</strong>g cl<strong>in</strong>ical judg- <strong>scan</strong>s and adequate <strong>pulmonary</strong> anglo- Gottschalk,.\iD.<br />
num<br />
e<br />
r<br />
g<br />
0<br />
p<br />
a<br />
t<br />
I<br />
e<br />
n<br />
t<br />
s<br />
W<br />
I<br />
t<br />
n<br />
e<br />
a<br />
r<br />
-<br />
n<br />
o<br />
r<br />
r<br />
n<br />
a<br />
r<br />
e<br />
p<br />
r<br />
e<br />
s<br />
~<br />
~<br />
a<br />
I<br />
o<br />
n<br />
0<br />
.<br />
p<br />
a<br />
l<br />
e<br />
n<br />
4'::' 2758 JAMA, May 23/30, 1990-VoI263, No 20 VentilationlPerfusionScan-PIOPED Investigators JAM<br />
~~,.j;<br />
'\;'I<br />
~, I<br />
.<br />
i<br />
~<br />
W<br />
I<br />
t<br />
h I<br />
~<br />
w<br />
-<br />
3<br />
4<br />
0<br />
0<br />
7<br />
,<br />
T<br />
h<br />
i<br />
s<br />
s<br />
t<br />
u<br />
d<br />
y<br />
w<br />
a<br />
s<br />
s<br />
u<br />
p<br />
p<br />
o<br />
r<br />
t<br />
e<br />
d<br />
b<br />
v<br />
c<br />
o<br />
n<br />
t<br />
r<br />
a<br />
c<br />
t<br />
s<br />
N<br />
O<br />
1<br />
-<br />
H<br />
R<br />
-<br />
N<br />
O<br />
1<br />
-<br />
H<br />
R<br />
-<br />
3<br />
4<br />
0<br />
0<br />
8<br />
.<br />
N<br />
O<br />
I<br />
-<br />
H<br />
R<br />
-<br />
3<br />
4<br />
0<br />
0<br />
9<br />
.<br />
N<br />
O<br />
1<br />
-<br />
H<br />
R<br />
-
~ j Cl<strong>in</strong>ical Centers University <strong>of</strong> Pennsylvania " LaFrance. MD, GerardJ. Prnd'homme. MA. Sharn-<br />
Duke University Abass AlaVI. MD. pnnClpallnvestlgator; Marga- on Prnitt. Paul<strong>in</strong>e Raiz. Broce Thompeon. PhD.<br />
Herbert ~tzman. MD. pr<strong>in</strong>cipal <strong>in</strong>vestiga- ret Ahearn-Spera. RNC. MSN. Dana R. Burke. Heidi Weissman. MD.<br />
m tJ;r;RU8sell Bl<strong>in</strong>aen1D. R. Edward Coleman. MD. Jeffrey Carson. MD. Mark A. Kelley. MD. .<br />
e- MD, N. Reed Dunnick, MD; William J. Fulker- Gordon K. McLean, MD. Steven G. Meranze. Project Office<br />
r- J MD L Mall tratt RN Carl E R MD. Harold I. Palevsky, MD. Sanford Schwartz.<br />
:ri r. ,ee a " .aVln. MD. Nati?nal Heart. Lung, and Blood TnBtitute: Carol<br />
e) H . F rd H "tal Yale University E. Vrelm. PhD, Margaret Wu. PhD.<br />
V enry 0 OSpl R" hard H G MD al " .<br />
..PaulO Ste<strong>in</strong> MD pr<strong>in</strong>cipal <strong>in</strong>vestigator' Debo- IC .reenspan. .pnnclp mvestlga-<br />
)li raiiAriimi:RN .'<strong>of</strong> tth B k MD J' W tor; Donald F. Denny. Jr. MD. Alexander Gott. Policy and Data Safety<br />
N- Froelic~MD, Ke:net::WV. ~ee~r. MD~r;am: .chalk. MD, Lee H. Greenwood, MD. Jacob S. o. Monitor<strong>in</strong>g Board<br />
Le MD J h Po h J .Loke, MD. RIchard A. Matthay. MD. Steven S.<br />
m A. seer, .0 n poVlC. r. MD. P. C. Morse, MD, H. Dirk Sostman. MD, Felicia Myron Stem. MD, chairman: Daniel M. Biello.<br />
e- Shetty, MD. James Thrall, MD. Tencza, MPH. MD (deceased). Sarah Greene Burger. MPH. Robs-<br />
Massachusetts General HospItal" .ert Henk<strong>in</strong>, MD, Thomas Hyers. MD, Paul S.<br />
Charles A. Hales. MD. pnnClpal mvestlgator; Data and Coord<strong>in</strong>at<strong>in</strong>g Center Levy. ScD. Frankl<strong>in</strong> Miller. Jr. MD, Robert E.<br />
a- Christos Athanasoulis. MD. Stuart Geller. MD, O'Mara. MD, Morris Simon. MD. Gerard Tur<strong>in</strong>o.<br />
<strong>in</strong> Kenneth McKusick. MD. Deborah Qu<strong>in</strong>n. RN, Maryland Medical Research Institute: Michael MD. George W. Williams. PhD.<br />
Jr MS. B. Taylor Thompson. MD. Arthur C. Walt- L. Terr<strong>in</strong>. MD, MPH. pr<strong>in</strong>cipal <strong>in</strong>vestigator; Wile-<br />
man. MD. ." mot Ball. MD, Mary Burke. Martha Canner. MS, Outcome Classification Committee<br />
UnIversIty <strong>of</strong> MIchIgan Paul Canner. PhD. Margie Carroll. Mart<strong>in</strong> Gold- "<br />
8. John G. Weg, MD, pr<strong>in</strong>cipal <strong>in</strong>vestigator; Grace man. MD. Carol Handy, Elizabeth He<strong>in</strong>z. Thomas Mark.~. Kelley. MD. chatnnan; Jeffrey Carson.<br />
ot Ball, RN, KyungJ. Cho. MD. ctlarles A. Easton, E. Hobb<strong>in</strong>s. MD, Frank Hooper. ScD, Steven ~D, Wllltam.J. FUlkerson. MD, Thomas E. Hobot<br />
MD, Andrew Fl<strong>in</strong>t. MD. Thomas A. Griggs. MD. Kaufman. MD, Christian R. Klimt. MD. DrPH blnB. MD. RIchard A. M~tthay, MD, Harold Pa-<br />
Jack E. Juni, MD, Jerold Wallis, MD, David (pr<strong>in</strong>cipal <strong>in</strong>vestigator. September 1983 through levsky, MD, John PopoVIch. Jr. MD. B. Taylor<br />
7 Williams. MD. September 1984), William F. Krol. PhD, Norman Thompson, MD. John G. Weg. MD.<br />
ts<br />
le Ref8rence8<br />
a-<br />
~h 1. Wagner HN. Sabiston DC. Tio M. McAfee JG. noetic test <strong>in</strong> unselected populations. N E1I91 I ,'tied. 1983;98:891-899.<br />
ct MeyerJK, Langan JK. Regional <strong>pulmonary</strong> blood ,'tied. 1006;274:1171-1175. 18. Hull RD, Hirsh J. Carter CJ, et aI. Diagnostic<br />
n- flow <strong>in</strong> man by radioisotope <strong>scan</strong>n<strong>in</strong>g. lAMA. 11. Li OK. Seltzer SG. McNeil BJ. V/Q mis- value <strong>of</strong> <strong>ventilation</strong>-<strong>perfusion</strong> lung <strong>scan</strong>n<strong>in</strong>g <strong>in</strong> pad<br />
1004;187:601-603. matches unassociated with <strong>pulmonary</strong> embolism: tients with suspected <strong>pulmonary</strong> embolism. Chest.<br />
1 2. Wagner HN Jr. Lopez-Majano V, Langan JK, case report and review <strong>of</strong> <strong>the</strong> literature. I Nucl 1985;88:819-828.<br />
re Joshi RC. Radioactive xenon <strong>in</strong> <strong>the</strong> differential di- .'tIed. 1978;19:1331-1333. 19. Poulose KP. Reba RC, Gilday DL. Deland FH.<br />
agnosia <strong>of</strong> <strong>pulmonary</strong> embolism. Radiology. 12. Biello DR. Kumar B. Symmetrical <strong>perfusion</strong> Wagner HN. Diagnosis <strong>of</strong> <strong>pulmonary</strong> embolism: a<br />
1968;91:1168-1184. defects without <strong>pulmonary</strong> embolism. EUl" I Nucl correlative study <strong>of</strong> <strong>the</strong> cl<strong>in</strong>ical. <strong>scan</strong>, ano angi()n-<br />
3. Biello DR. Mattar AG. McKnight RC. Siegel .'tIed.1982;7:197-199; graphic f<strong>in</strong>d<strong>in</strong>gs. B.'tII. 1970;3:67-71.<br />
r- BA. Ventilation <strong>perfusion</strong> studies <strong>in</strong> suspected pul- 13. Alderson PO. Mart<strong>in</strong> EC. Pulmonary embo- 20. McNeil BJ. Ventilation-<strong>perfusion</strong> studies and<br />
Ie monary embolism. Am I Radiol. 1979;133:1033- lism: diagnosis with multiple Imag<strong>in</strong>g modalities. <strong>the</strong> diagnoses <strong>of</strong> <strong>pulmonary</strong> embolism: concise com-<br />
A 1037. Radiology. 1987;164:297-312. munication. I Nucl ,'tied. 1980;21:319-323.<br />
, ~. Snedecor JW, Cochran WG. StatiStical Meth- 1~. Cheely R, McCartney WH, Perry JR. et aI. 21. McNeil BJ. Hessel SJ, Branch WT. Bjork L.<br />
-8 odA. 6th ed. Ames: Iowa State University Press; The role <strong>of</strong> non<strong>in</strong>vasive tests versus <strong>pulmonary</strong> Adelste<strong>in</strong> SJ' Measures <strong>of</strong> cl<strong>in</strong>ical efficacy, III: <strong>the</strong><br />
r- 1967. angiography <strong>in</strong> <strong>the</strong> diagnosis <strong>of</strong> <strong>pulmonary</strong> embo- value <strong>of</strong> <strong>the</strong> lung <strong>scan</strong> <strong>in</strong> <strong>the</strong> evaluation <strong>of</strong> young<br />
()- 5. Cochran WG. Some methods <strong>of</strong> streng<strong>the</strong>n<strong>in</strong>g li.m. Ami Med. 1981;70:17-22. patients with pleuritic chest pa<strong>in</strong>. I Nucl ,'tied.<br />
s- <strong>the</strong> common X2te8ts. Biometrics. 1954;10:417-451. 15. Novell<strong>in</strong>e RA, Baitarowich OH. Athanasoulis 1976;17:163-169.<br />
,<br />
_8<br />
6. Fleiss JL. Statistical ,'tIethAJda fOl" Rates and<br />
PropoI"tion.!. 2nd ed. New York, NY: John Wiley &<br />
CA. Waltman AC. Greenfield AJ. Mckusick KA.<br />
The cl<strong>in</strong>ical course <strong>of</strong> patients with suspected pul-<br />
22. Kipper MS. Moser KM. Kortman KE, Ashburn<br />
WL. Long-term follow-up <strong>of</strong> patients with sus-<br />
1- Sons Inc; 1981. monary embolism and a negative <strong>pulmonary</strong> arte- pected <strong>pulmonary</strong> embolism and a normal lung<br />
:y 7. Nie NH, ed. SPSs" USel"~ Gltide. New York. riogram. Radiology. 1978;126:561-567. <strong>scan</strong>. Chest. 1982:82:411-415.<br />
In NY: McGraw-HilI International Book Co; 1983. 16. Sasahara AA. Ste<strong>in</strong> M, Simon M, Littmann D. 23. Rob<strong>in</strong> ED. Over diagnosis and over treatment<br />
l<br />
y<br />
8. Hill AB. Pr<strong>in</strong>ciples <strong>of</strong> ,o,{edical Statistics. 9th<br />
ed. New York, NY: Oxford University Press Inc;<br />
Pulmonary angiography <strong>in</strong> <strong>the</strong> diagnosis <strong>of</strong> thromboembolic<br />
disease. N E1I91 J Med. 1004;270:1075<strong>of</strong><br />
<strong>pulmonary</strong> embolism: <strong>the</strong> emperor may have no<br />
clo<strong>the</strong>s. Ann lntel"n Med. 1977;87:775-781.<br />
1- 1971. 1081. 24. Biello DR. Radiological (sc<strong>in</strong>tigraphic) evalua-<br />
Ii 9. Murphy EA. Probability <strong>in</strong> Medic<strong>in</strong>e. Balti- 17. Hull RD, Hirsh J. Carter CJ, et aI. Pulmonary tion <strong>of</strong> patients with suspected <strong>pulmonary</strong> throme<br />
more, Md: The JohnB Hopk<strong>in</strong>8 University Press; angiography, <strong>ventilation</strong> lung <strong>scan</strong>n<strong>in</strong>g and venog- boembolism. lAMA. 1987;257:3257-3259.<br />
n<br />
1979.<br />
10. Vecchio JJ. Predictive value <strong>of</strong> a s<strong>in</strong>gle diagraphy<br />
for cl<strong>in</strong>ically suspected <strong>pulmonary</strong> emboli8m<br />
with abnormal <strong>perfusion</strong> lung <strong>scan</strong>. Ann lntel"n<br />
a .<br />
11<br />
i- '<br />
t.<br />
t- -<br />
l-<br />
Id ~.<br />
18 .<br />
S<br />
'. I;<br />
,r .<br />
s JAMA. May 23/30, 1990-VoI263. No. 20 Ventilation/Perfuslon Scan-PIOPED Investigators 2759<br />
,<br />
..' '- I<br />
.'.:. -j
I<br />
}"<br />
~.. Editorials di<br />
tc<br />
Ie<br />
Ventilation/Perfusion Scan <strong>in</strong> Pulmonary Embolism : T:<br />
I 'The Emperor Is Incompletely Attired' :<br />
One <strong>of</strong> <strong>the</strong> most difficult diagnoses to make <strong>in</strong> medic<strong>in</strong>e today tive diagnosis <strong>of</strong> <strong>pulmonary</strong> embolic disease_2.4 The relatively c~<br />
is that <strong>of</strong> <strong>pulmonary</strong> embolic disease, In a study done <strong>in</strong> <strong>the</strong> low sensitivity <strong>of</strong> high-probability <strong>scan</strong>s (41%) means that tl<br />
i I early 1970s, , evidence <strong>of</strong> <strong>pulmonary</strong> embolism at autopsy <strong>scan</strong>s, alone, are <strong>in</strong>adequate to ascerta<strong>in</strong> <strong>the</strong> presence <strong>of</strong><br />
'i correlated poorly to antemortem diagnosis <strong>of</strong> <strong>pulmonary</strong> em- <strong>pulmonary</strong> embolism- On <strong>the</strong> o<strong>the</strong>r hand, only 3% <strong>of</strong> patients<br />
bolic disease; <strong>in</strong> only one third <strong>of</strong> cases were emboli correctly <strong>in</strong> <strong>the</strong> Prospective Investigation <strong>of</strong> Pulmonary Embolism<br />
identified. A batt<strong>in</strong>g average
'. t.<br />
'- . ,<br />
I .diagnos<strong>in</strong>g <strong>pulmonary</strong> embolic disease today, <strong>the</strong> cl<strong>in</strong>ical his- lism, <strong>the</strong> emperor has a "well-clo<strong>the</strong>d" appearance. When -\<br />
tory, used i~ c~njunction.with evaluation <strong>of</strong>.arte~al blood gas <strong>the</strong>re is significant doubt, a <strong>pulmonary</strong> angiogram should be '<br />
levels, ventIlation/<strong>perfusion</strong> <strong>scan</strong>s, and nOnInvaSive studies <strong>of</strong> done. . I<br />
<strong>the</strong> ~e.ep, ve<strong>in</strong>s. <strong>of</strong> <strong>the</strong> legs, should markedly improve <strong>the</strong> Roger C. Bone, MD<br />
physIcian s battIng average. If <strong>the</strong> postmortem studies <strong>of</strong> <strong>the</strong>, I<br />
1970 d d . h ., .1. ModanB.SharonE.JelmN.Factorscontribut<strong>in</strong>gto<strong>the</strong><strong>in</strong>con'eCtdiagnosis i<br />
S were repeate to ay, usIng t IS recent InformatIon, <strong>the</strong> nf<strong>pulmonary</strong> embolic disease. Che.t. 1972:62:388-393. I<br />
results should be much better. My suggestions for diagnostic 2. The PIOPED l,nvestigators. <strong>Value</strong> <strong>of</strong> <strong>the</strong> <strong>ventilation</strong>/<strong>perfusion</strong> <strong>scan</strong> <strong>in</strong> <strong>acute</strong><br />
~ evaluation are <strong>in</strong>cluded <strong>in</strong> an algorithm that uses some <strong>of</strong> <strong>the</strong> pulmo~ary e.mbollsm: results <strong>of</strong> <strong>the</strong> Prospective Inve.tigation <strong>of</strong> Pulmonary<br />
most recent<br />
.'<br />
InformatIon from <strong>the</strong><br />
..,<br />
article m todays<br />
.Emboll.m<br />
Issue <strong>of</strong><br />
Diagno"," (PIOPEDJ.<br />
:I. Rob<strong>in</strong> ED. Overdiagnosis<br />
JA,\f A. 1900:263:2753-2759.<br />
and overtreatment <strong>of</strong> <strong>pulmonary</strong> emboli.m: <strong>the</strong> "<br />
THE JOURNAL, as well as <strong>in</strong>formation published on <strong>the</strong> diag- emperor may h,ave no clo<strong>the</strong>s. Ann Intm! ,\fed. 1977:87:775-781. I<br />
nos tic accuracy <strong>of</strong> non<strong>in</strong>vasive studies for dee p venous throm- 4. Hull RD~ HI~hJ. C~rterCJ.etal. Diagnootic VaJueOf<strong>ventilation</strong>.perfu"ion<br />
bosls<br />
..lung<br />
(Flgure)..,..T 1985;88:819-828.<br />
<strong>scan</strong>n<strong>in</strong>g In patients WIth suspected <strong>pulmonary</strong> embolism. Che../.<br />
'<br />
\<br />
The <strong>ventilation</strong>/<strong>perfusion</strong> lung <strong>scan</strong>, taken <strong>in</strong> isolation, rep- 5. Hull RD. Hirs.h!. Carter CJ. et al. Diagn~stic efficacy <strong>of</strong> impedance plethys-<br />
th "th h I th " "th mography for cl<strong>in</strong>Ically suspected deep-ve<strong>in</strong> thrombosIs. Ann In/","" ,~fed.<br />
resen t s nel . er e emperor as no c 0 es nor e emper- 1985:102:21.28.<br />
or I th is fully clo<strong>the</strong>d." b t .. Indeed, <strong>the</strong> emperor may have some 6. Polak JF. Culler SS. O'Leary DH. Deep ve<strong>in</strong>s <strong>of</strong> <strong>the</strong> calf: assessment ,,;th \<br />
{ CO es on, u untO rt una tel Y h e . IS, as ye t , . mcomp I e t e I y at- 7Doppler Whl ' te<br />
flow<br />
RH<br />
imag<strong>in</strong>g. McGah a. Radiology. nJP D asc hb<br />
1989:1iI:481-485. ac, h MM .ar H I mg ' RP .lagnoSI" D ' 0 fd eep-<br />
t tired. In <strong>the</strong> maJonty <strong>of</strong> cases <strong>of</strong> suspected <strong>pulmonary</strong>embo- ve<strong>in</strong> thrombosis us<strong>in</strong>g duplex ultrasound. Ann In/ern ,\fed. 1989:111:29;.304.<br />
r i ,<br />
Methods <strong>of</strong> Smok<strong>in</strong>g Cessation.-F<strong>in</strong>ally,<br />
Some Answers<br />
Forty million liv<strong>in</strong>g Americans have quit smok<strong>in</strong>g.' While not are much more likely to participate <strong>in</strong> an organized cessation<br />
as catchy, perhaps, as "Fifty million Frenchmen can't be program than persons who smoke less. '<br />
"'TOn~' o~ "~illions have rea? t.he book,.now see <strong>the</strong> movie," These data, and <strong>the</strong> conclusions derived from <strong>the</strong>m, are a .I<br />
<strong>the</strong> pnnclple IS <strong>the</strong> same-this IS a massive number <strong>of</strong> people movable feast-<strong>the</strong>y provide a wide variety <strong>of</strong> health pr<strong>of</strong>es- ,<br />
focused on one activity. sionals, and smokers <strong>the</strong>mselves, with specific actions each II<br />
can take to help reduce smok<strong>in</strong>g prevalence. Among <strong>the</strong><br />
See also p 2760. groups <strong>in</strong>g: who can benefit from <strong>the</strong> <strong>in</strong>formation are <strong>the</strong> follow- \<br />
Unfortunately, until now we have known very little, or Physicians. The primary message for physicians is that<br />
have had to surmise, how so many smokers have achieved <strong>the</strong>ir advice is a key element <strong>in</strong> motivat<strong>in</strong>g smokers to make<br />
<strong>the</strong>ir goal <strong>of</strong> quitt<strong>in</strong>g. The article by Fiore et al' <strong>in</strong> this issue <strong>of</strong> quit attempts. Even if smokers do not quit <strong>the</strong> first or second<br />
THE JOURNAL, however, f<strong>in</strong>ally provides some answers and, time <strong>the</strong>y receive <strong>the</strong>ir physician's advice to do so-and most<br />
even more important, guidance on this issue. data suggest this is <strong>the</strong> case-<strong>the</strong> advice <strong>of</strong> <strong>the</strong> physician can<br />
Among <strong>the</strong> important f<strong>in</strong>d<strong>in</strong>gs presented by Fiore et al are help move smokers from one stage to ano<strong>the</strong>r <strong>in</strong> <strong>the</strong> quitt<strong>in</strong>g<br />
<strong>the</strong> follow<strong>in</strong>g: process,3' eventually lead<strong>in</strong>g to successful abst<strong>in</strong>ence from<br />
.More than 90% <strong>of</strong> successful quitters do so on <strong>the</strong>ir own, smok<strong>in</strong>g.<br />
without participation <strong>in</strong> an organized cessation program. In keep<strong>in</strong>g with <strong>the</strong>se data, <strong>the</strong> National Cancer Institute<br />
.Quit rates (def<strong>in</strong>ed as §mok<strong>in</strong>g abst<strong>in</strong>ence for ~1 year) recently developed a simple protocol to help physicians pro-<br />
are twice as high for those who quit on <strong>the</strong>ir own compared vide advice about smok<strong>in</strong>g cessation.' The National Cancer<br />
with those who participate <strong>in</strong> a cessation program. However, Institute suggests that <strong>the</strong> physician's <strong>of</strong>fice or cl<strong>in</strong>ic be<br />
this f<strong>in</strong>d<strong>in</strong>g is not based on randomly allocat<strong>in</strong>g smokers to smoke free, that all smokers <strong>in</strong> <strong>the</strong> practice be identified, and<br />
one method or <strong>the</strong> o<strong>the</strong>r. Ra<strong>the</strong>r, smokers who enter cessa- that <strong>the</strong> physician (and o<strong>the</strong>r <strong>of</strong>fice support staff> ask about<br />
tion programs may be those who were unable to quit on <strong>the</strong>ir smok<strong>in</strong>g at each patient visit; advise smokers to stop at every<br />
own. opportunity; assist smokers <strong>in</strong> stopp<strong>in</strong>g by help<strong>in</strong>g <strong>the</strong>m set a ;<br />
.Smokers who quit "cold turkey" are more likely to re- quit- date, provid<strong>in</strong>g self-help material, and prescrib<strong>in</strong>g phar-<br />
ma<strong>in</strong> abst<strong>in</strong>ent than those who gradually decrease <strong>the</strong>ir daily maci>logical adjuncts as appropriate; and arrange follow-up<br />
consumption <strong>of</strong> cigarettes, switch to cigarettes with lower tar contact with <strong>the</strong> patient to prevent relapse.<br />
or nicot<strong>in</strong>e, or use special filters or holders. PtLblic Health Planners/Practitioners. Among <strong>the</strong> mes-<br />
.Quit attempte are nearly twice as likely to occur among sages for those <strong>in</strong>volved <strong>in</strong> public health plann<strong>in</strong>g or practice<br />
smokers who receive nonsmok<strong>in</strong>g advice from <strong>the</strong>ir physi- are <strong>the</strong> follow<strong>in</strong>g: (1) Efforts should be directed at motivat<strong>in</strong>g<br />
cians compared with those who are not advised to quit. more smokers to make serious quit attempts, ra<strong>the</strong>r than<br />
.Heavy (~25 cigarettes a day), more addicted smokers develop<strong>in</strong>g new progrartts; (2) exist<strong>in</strong>g self-help cessation<br />
materials should be made more widely available; <strong>in</strong>creased<br />
~Iynn IS <strong>the</strong> Program Director for Smok<strong>in</strong>g Research at <strong>the</strong> National~ availability will be more successful than develop<strong>in</strong>g new ma-<br />
Inst,tu1e. Be<strong>the</strong>sda, Md terials or "f<strong>in</strong>e tun<strong>in</strong>g" exist<strong>in</strong>g materials; and (3) consider-<br />
9(XX) Repnnt Rockvllle reQuests Pike to Be<strong>the</strong>sda. National MD Cancer 20892-4200 Institute (Dr ExecutIVe Glynn) ~laza North. Room 320.. atIon should.be gIven to ~usmg ' on t h e h eaVler, . more severe-<br />
JAMA. May 23/30. 1990-VoI263, No 20 Editorials 2795<br />
I<br />
\<br />
\
ly addicted smoker <strong>in</strong> organized cessation programs. Similar (4) advis<strong>in</strong>g patients to seek <strong>the</strong> support, even if quitt<strong>in</strong>g "on<br />
" ,. recommendations were made recently by a National Cancer <strong>the</strong>ir own," <strong>of</strong>aspouse, friend, or someone else <strong>in</strong> a position to<br />
Institute expert advisory panel, which also encouraged pro- help re<strong>in</strong>force <strong>the</strong>ir decision to quit. F<strong>in</strong>ally, recent research<br />
! jects that will provide self-help materials to high-risk popula- suggests that, while tra<strong>in</strong><strong>in</strong>g physicians to give advice about<br />
..tions, especially blacks, Hispanics, and pregnant women, smok<strong>in</strong>g cessation can <strong>in</strong>crease patient quit attempts, it will<br />
whose particular needs have <strong>of</strong>ten been neglected <strong>in</strong> our take greater effort-perhaps several follow-up visits or consmok<strong>in</strong>g-cessation<br />
efforts." tacts-to reduce <strong>the</strong> high relapse rates experienced.,..e..l.<br />
Smok<strong>in</strong>g-Cessation Researchers. In addition to f<strong>in</strong>ally pro- 8 1b provide those <strong>in</strong>volved <strong>in</strong> reduc<strong>in</strong>g smok<strong>in</strong>g pre'llavid<strong>in</strong>g<br />
evidence for <strong>the</strong> widespread belief that <strong>the</strong> majority <strong>of</strong> leme with <strong>the</strong> most expedient means <strong>of</strong> do<strong>in</strong>g so. Too <strong>of</strong>ten,<br />
smokers who quit do so on <strong>the</strong>ir own, <strong>the</strong> f<strong>in</strong>d<strong>in</strong>gs <strong>of</strong> Fiore et al those charged with reduc<strong>in</strong>g smok<strong>in</strong>g prevalence, such as<br />
call our attention to several potential research questions. physicians, nurses, dentists, public health <strong>of</strong>ficers, and smok-<br />
What detenn<strong>in</strong>es relapse, and how can it be prevented? How <strong>in</strong>g-cessation program coord<strong>in</strong>ators, are not provided with or<br />
can we motivate more smokers to make Seri01tS quit at- aware <strong>of</strong> <strong>the</strong> most appropriate <strong>in</strong>formation available to help<br />
tempts? What are <strong>the</strong> most effective means <strong>of</strong> dissem<strong>in</strong>ation smokers stop, especially on <strong>the</strong>ir own. II For physicians, this<br />
and adoption <strong>of</strong> successful cessation methods? may mean not be<strong>in</strong>g aware <strong>of</strong> effective cessation strategies' or<br />
Smokers. Important messages for smokers <strong>in</strong> this article <strong>the</strong> proper use <strong>of</strong> nicot<strong>in</strong>e gum (or <strong>the</strong> transcutaneous nicot<strong>in</strong>e<br />
are (1) <strong>the</strong>y can quit; (2) <strong>the</strong>y can successfully stop smok<strong>in</strong>g if patch that may soon be available). It could also mean be<strong>in</strong>g<br />
<strong>the</strong>y do so on <strong>the</strong>ir own (especially by sett<strong>in</strong>g a specific quit unaware <strong>of</strong> <strong>the</strong> special help for heavy smokers that organized<br />
date and stopp<strong>in</strong>g cold turkey on that date); (3) smok<strong>in</strong>g- cessation programs can provide. For public health <strong>of</strong>ficers<br />
cessation programs are helpful for some, especially heavier, and smok<strong>in</strong>g-cessation program directors, it could be not<br />
more addicted smokers: and (4) permanent quitt<strong>in</strong>g from a realiz<strong>in</strong>g <strong>the</strong> importance <strong>of</strong> provid<strong>in</strong>g simple self-help materifirst<br />
or second attempt is unusual; <strong>the</strong> smoker may suffer an al to as many smokers as possible and not limit<strong>in</strong>g <strong>the</strong>ir efforts<br />
<strong>in</strong>itial relapse and need to learn from that experience <strong>in</strong> order to those who have already expressed an <strong>in</strong>terest <strong>in</strong> giv<strong>in</strong>g up<br />
to make ano<strong>the</strong>r, successful, quit attempt. tobacco. The importance <strong>of</strong> a variety <strong>of</strong> providers and a menu<br />
A major conclusion that may be drawn from <strong>the</strong>se data, <strong>of</strong> methods becomes more important as more smokers are<br />
<strong>the</strong>n, is that we do not need to expand our efforts to <strong>in</strong>volve motivated to make serious quit attempts.<br />
more smokers <strong>in</strong> formal cessation programs. Never<strong>the</strong>less, With <strong>the</strong> knowledge that <strong>the</strong>re will be more than 2 million.<br />
I. \ve should not abandon <strong>the</strong>se programs. 7 as some, such as <strong>the</strong> tobacco-related deaths worldwide from tobacco this year, it is ..<br />
American Lung Association's "Freedom From Smok<strong>in</strong>g" cl<strong>in</strong>- obviously necessary to expand our efforts to reduce smok<strong>in</strong>g<br />
ic program, are successful, and we need to ma<strong>in</strong>ta<strong>in</strong> a variety prevalence not only <strong>in</strong> <strong>the</strong> United States and o<strong>the</strong>r <strong>in</strong>dustrial<strong>of</strong><br />
approaches to cessation. This is especially true for heavier ized countries but, especially, <strong>in</strong> <strong>the</strong> develop<strong>in</strong>g world, where<br />
smokers who wish to try to quit \\;th <strong>the</strong> more formal meth- <strong>the</strong> tobacco <strong>in</strong>dustry is <strong>in</strong>creas<strong>in</strong>g its markets and <strong>the</strong> rates <strong>of</strong><br />
od!l. We do need to focus on <strong>the</strong> broad pllblic health implica- tobacco-related death are ris<strong>in</strong>g. Next week's World Notions<br />
<strong>of</strong> our !lmok<strong>in</strong>g-cessation efforts, and our agenda should Tobacco Day (May 31), sponsored by <strong>the</strong> World Health Orga<strong>in</strong>clude<br />
<strong>the</strong> follow<strong>in</strong>g goals: nization, provides an excellent opportunity to embark on a<br />
8 1b motivate more smokers to make serious quit at. renewed effort to help those who want to quit smok<strong>in</strong>g to do<br />
tempts. While physicians are <strong>in</strong> a unique position to motivate so, and to help those who do not now smoke, especially <strong>in</strong><br />
smokers, it is equally important to motivate <strong>the</strong> smoker on a develop<strong>in</strong>g countries, to rema<strong>in</strong> nonsmokers.<br />
society-wide basis, so that nonsmok<strong>in</strong>g<br />
... ki<br />
cues, such as <strong>in</strong>-<br />
1 d Thomas. J Glynn, PhD<br />
creased tobacco taxes, restnctlve smo ng po ICles, an coun-<br />
teradvertis<strong>in</strong>g campaigns, become "persistent and <strong>in</strong>escap- 1: Pierce JP. Fiore MC, Novotny TE. Hatziandreu EJ, Davis RM. Trends <strong>in</strong><br />
bl "<br />
a e.<br />
Th<br />
e<br />
N t . 1 C<br />
a lona ancer<br />
I t ' t t and<br />
ns I u e<br />
<strong>the</strong> Amen 'can CIgarette smok<strong>in</strong>g In <strong>the</strong> Umted States: projectIons<br />
1989;261:61-65.<br />
to <strong>the</strong> year 2000. JAMA.<br />
Cancer Society, through <strong>the</strong>ir upcom<strong>in</strong>g American Stop 2. Fiore MC, Novotny TE. Pierce JP, et aI. Methods used to quit smok<strong>in</strong>g <strong>in</strong> <strong>the</strong><br />
Smok<strong>in</strong>g Intervention Study for Cancer Prevention, will pro- United States; do ce!!:88tion programs help? JA,\1 A. 19!MJ;263:2760-2765.<br />
., .." 3. Prochaska JO, DiClemente CC. Stages and processes <strong>of</strong> self-change <strong>of</strong><br />
VIde a major demonstration <strong>of</strong> this strategy. smok<strong>in</strong>g: towani an <strong>in</strong>tegrative model <strong>of</strong> change. J COn81tlt Cl<strong>in</strong> Psychol.<br />
8 1b <strong>in</strong>crease s1tCCeSS rates amacco and Health In pre..sso<br />
1<br />
(1) motivat<strong>in</strong>g smok<strong>in</strong>g patients to make senous, SltStalned<br />
quit attempts; (2) help<strong>in</strong>g patients learn, prior to <strong>the</strong> quit<br />
. d . f t. 1 0th<br />
attempt, about <strong>the</strong> seventy and uratlon 0 poten la WI -10.<br />
9. Cohen SJ, Stookey GK. Katz BP. Droo..k CA. Smit..h OM. Encourag1ng<br />
primary ~ physici&ft8 t~ help smokers quIt: a randomized, controlled tnal.<br />
Ann Int~ Med. 1989:110..648-652. '<br />
Cumm<strong>in</strong>gs SR. Coates TJ, Richard RJ. et aI. Tra<strong>in</strong><strong>in</strong>g physicians <strong>in</strong> counsel-<br />
I i drawal symptoms; (3) prescrib<strong>in</strong>g, for heavily addicted smok- <strong>in</strong>g about smok<strong>in</strong>g cessation: a randomized trial <strong>of</strong> <strong>the</strong> 'Quit Cor Life' programo<br />
firs .o th ' 30 ° t f k<strong>in</strong> g or a Ann Int~ Mad. 1989:110:640-647.<br />
ers (eg, t CIgarette WI m mmu es ~ ~ 11. Glynn TJ, Boyd GM. Gruman JC. Self-Gllided Stmtegies for Smok<strong>in</strong>g<br />
cigarette habit <strong>of</strong> more than a pack a day), a mcotme replace- Ce3sation: A Program Plan1!$TJ GltiU.. Be<strong>the</strong>sd..a. ~d: National Cancer Instlment<br />
product, after careful explanation <strong>of</strong> its proper use; and tute. In preMo National Institutes <strong>of</strong> Health publicatIon 90-3104.<br />
2796 JAMA. May 23/30. 1990- Vol 263. No 20 Editorials<br />
~III-.<br />
-,