Utility of History, Physical Examination, Electrocardiogram, and ...
Utility of History, Physical Examination, Electrocardiogram, and ...
Utility of History, Physical Examination, Electrocardiogram, and ...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
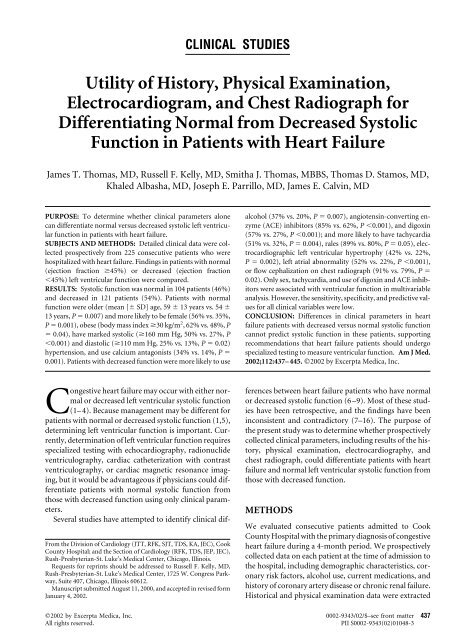
CLINICAL STUDIES<br />
<strong>Utility</strong> <strong>of</strong> <strong>History</strong>, <strong>Physical</strong> <strong>Examination</strong>,<br />
<strong>Electrocardiogram</strong>, <strong>and</strong> Chest Radiograph for<br />
Differentiating Normal from Decreased Systolic<br />
Function in Patients with Heart Failure<br />
James T. Thomas, MD, Russell F. Kelly, MD, Smitha J. Thomas, MBBS, Thomas D. Stamos, MD,<br />
Khaled Albasha, MD, Joseph E. Parrillo, MD, James E. Calvin, MD<br />
PURPOSE: To determine whether clinical parameters alone<br />
can differentiate normal versus decreased systolic left ventricular<br />
function in patients with heart failure.<br />
SUBJECTS AND METHODS: Detailed clinical data were collected<br />
prospectively from 225 consecutive patients who were<br />
hospitalized with heart failure. Findings in patients with normal<br />
(ejection fraction 45%) or decreased (ejection fraction<br />
45%) left ventricular function were compared.<br />
RESULTS: Systolic function was normal in 104 patients (46%)<br />
<strong>and</strong> decreased in 121 patients (54%). Patients with normal<br />
function were older (mean [ SD] age, 59 13 years vs. 54 <br />
13 years, P 0.007) <strong>and</strong> more likely to be female (56% vs. 35%,<br />
P 0.001), obese (body mass index 30 kg/m 2 , 62% vs. 48%, P<br />
0.04), have marked systolic (160 mm Hg, 50% vs. 27%, P<br />
0.001) <strong>and</strong> diastolic (110 mm Hg, 25% vs. 13%, P 0.02)<br />
hypertension, <strong>and</strong> use calcium antagonists (34% vs. 14%, P <br />
0.001). Patients with decreased function were more likely to use<br />
Congestive heart failure may occur with either normal<br />
or decreased left ventricular systolic function<br />
(1– 4). Because management may be different for<br />
patients with normal or decreased systolic function (1,5),<br />
determining left ventricular function is important. Currently,<br />
determination <strong>of</strong> left ventricular function requires<br />
specialized testing with echocardiography, radionuclide<br />
ventriculography, cardiac catheterization with contrast<br />
ventriculography, or cardiac magnetic resonance imaging,<br />
but it would be advantageous if physicians could differentiate<br />
patients with normal systolic function from<br />
those with decreased function using only clinical parameters.<br />
Several studies have attempted to identify clinical dif-<br />
From the Division <strong>of</strong> Cardiology (JTT, RFK, SJT, TDS, KA, JEC), Cook<br />
County Hospital; <strong>and</strong> the Section <strong>of</strong> Cardiology (RFK, TDS, JEP, JEC),<br />
Rush-Presbyterian-St. Luke’s Medical Center, Chicago, Illinois.<br />
Requests for reprints should be addressed to Russell F. Kelly, MD,<br />
Rush-Presbyterian-St. Luke’s Medical Center, 1725 W. Congress Parkway,<br />
Suite 407, Chicago, Illinois 60612.<br />
Manuscript submitted August 11, 2000, <strong>and</strong> accepted in revised form<br />
January 4, 2002.<br />
alcohol (37% vs. 20%, P 0.007), angiotensin-converting enzyme<br />
(ACE) inhibitors (85% vs. 62%, P 0.001), <strong>and</strong> digoxin<br />
(57% vs. 27%, P 0.001); <strong>and</strong> more likely to have tachycardia<br />
(51% vs. 32%, P 0.004), rales (89% vs. 80%, P 0.05), electrocardiographic<br />
left ventricular hypertrophy (42% vs. 22%,<br />
P 0.002), left atrial abnormality (52% vs. 22%, P 0.001),<br />
or flow cephalization on chest radiograph (91% vs. 79%, P <br />
0.02). Only sex, tachycardia, <strong>and</strong> use <strong>of</strong> digoxin <strong>and</strong> ACE inhibitors<br />
were associated with ventricular function in multivariable<br />
analysis. However, the sensitivity, specificity, <strong>and</strong> predictive values<br />
for all clinical variables were low.<br />
CONCLUSION: Differences in clinical parameters in heart<br />
failure patients with decreased versus normal systolic function<br />
cannot predict systolic function in these patients, supporting<br />
recommendations that heart failure patients should undergo<br />
specialized testing to measure ventricular function. Am J Med.<br />
2002;112:437– 445. 2002 by Excerpta Medica, Inc.<br />
ferences between heart failure patients who have normal<br />
or decreased systolic function (6 –9). Most <strong>of</strong> these studies<br />
have been retrospective, <strong>and</strong> the findings have been<br />
inconsistent <strong>and</strong> contradictory (7–16). The purpose <strong>of</strong><br />
the present study was to determine whether prospectively<br />
collected clinical parameters, including results <strong>of</strong> the history,<br />
physical examination, electrocardiography, <strong>and</strong><br />
chest radiograph, could differentiate patients with heart<br />
failure <strong>and</strong> normal left ventricular systolic function from<br />
those with decreased function.<br />
METHODS<br />
We evaluated consecutive patients admitted to Cook<br />
County Hospital with the primary diagnosis <strong>of</strong> congestive<br />
heart failure during a 4-month period. We prospectively<br />
collected data on each patient at the time <strong>of</strong> admission to<br />
the hospital, including demographic characteristics, coronary<br />
risk factors, alcohol use, current medications, <strong>and</strong><br />
history <strong>of</strong> coronary artery disease or chronic renal failure.<br />
Historical <strong>and</strong> physical examination data were extracted<br />
2002 by Excerpta Medica, Inc. 0002-9343/02/$–see front matter 437<br />
All rights reserved. PII S0002-9343(02)01048-3
from the attending physician’s note (internist or cardiologist)<br />
from hospital day 1 or 2; whether the attending<br />
physicians were aware <strong>of</strong> a patient’s systolic function<br />
when a note was written is unknown. Recorded symptoms<br />
included dyspnea at rest, dyspnea with exertion,<br />
orthopnea, paroxysmal nocturnal dyspnea, angina, <strong>and</strong><br />
nonanginal chest pain. <strong>Physical</strong> examination findings included<br />
height, weight, heart rate, systolic <strong>and</strong> diastolic<br />
blood pressure, jugular venous distention, hepatojugular<br />
reflux, rales, wheezing, S 3 <strong>and</strong> S 4 gallops, <strong>and</strong> pedal<br />
edema. Pulse pressure was calculated as systolic minus<br />
diastolic blood pressure, <strong>and</strong> body mass index was calculated<br />
as weight (in kg) divided by height (in m 2 ). Most<br />
parameters (80%) were recorded in 97% <strong>of</strong> the patients.<br />
We assessed whether patients met the Framingham<br />
criteria for heart failure (17).<br />
Admission electrocardiograms (ECGs) were assessed<br />
by a cardiologist who was unaware <strong>of</strong> other patient data<br />
for rhythm (recorded as sinus, atrial fibrillation, or other),<br />
presence <strong>of</strong> abnormal Q waves, left ventricular hypertrophy<br />
by the Estes criteria (18), <strong>and</strong> left atrial abnormality<br />
(defined as P terminal force in V 1 more negative than<br />
0.04 ms, or a notched P wave 0.12 s) (19). The admission<br />
chest radiograph was evaluated by an attending radiologist<br />
for the presence <strong>of</strong> cardiomegaly, flow cephalization,<br />
pleural effusion, <strong>and</strong> pulmonary edema.<br />
Left ventricular systolic function was determined by<br />
echocardiography. All ECGs were performed at Cook<br />
County Hospital <strong>and</strong> were interpreted by experienced<br />
cardiologists who were unaware <strong>of</strong> the specific clinical<br />
findings in the patients. Normal systolic function was defined<br />
as an ejection fraction 45% (20) as assessed by<br />
visual inspection. Decreased systolic function was defined<br />
as ejection fraction 45%. Patients were excluded if<br />
left ventricular function was not measured, <strong>and</strong> also if<br />
primary valvular disease was present. Patients with mitral<br />
or tricuspid regurgitation judged to be a result <strong>of</strong> heart<br />
failure, rather than the cause <strong>of</strong> the condition, were not<br />
excluded.<br />
Statistical Analysis<br />
Chi-squared tests were used to compare categorical variables,<br />
<strong>and</strong> two-sided t tests were used for continuous variables.<br />
The sensitivity, specificity, <strong>and</strong> positive <strong>and</strong> negative<br />
predictive values for normal systolic function were<br />
calculated for each clinical variable. Multivariate logistic<br />
regression analysis was also performed, including variables<br />
with univariate P values 0.10, to identify independent<br />
predictors <strong>of</strong> decreased systolic function. Receiver<br />
operating characteristic curves were constructed for these<br />
predictors. A sub-analysis was performed in which patients<br />
with markedly depressed systolic function (ejection<br />
fraction 30%) were compared with those who had an<br />
ejection fraction 30%. A P value 0.05 (two sided) was<br />
Clinical Findings in Heart Failure/Thomas et al<br />
438 April 15, 2002 THE AMERICAN JOURNAL OF MEDICINE Volume 112<br />
considered significant. This study was approved by the<br />
Scientific Committee <strong>of</strong> Cook County Hospital.<br />
RESULTS<br />
A total <strong>of</strong> 282 patients were admitted with a primary diagnosis<br />
<strong>of</strong> congestive heart failure. Left ventricular function<br />
was not documented during the index admission in<br />
43 patients (15%), <strong>and</strong> 14 patients (5%) had primary valvular<br />
disease; these patients were excluded. The remaining<br />
225 patients comprised the study sample, <strong>of</strong> whom<br />
121 (54%) had decreased left ventricular systolic function.<br />
Of the 225 patients, 75% (n 169) were black, 10%<br />
(n 22) were white, 11% (n 25) were Hispanic, <strong>and</strong><br />
4% (n 9) were <strong>of</strong> other races. All but 2 <strong>of</strong> these patients<br />
met the Framingham criteria for congestive heart failure<br />
(17).<br />
Patients with normal systolic function were older <strong>and</strong><br />
more likely to be female than were those with decreased<br />
systolic function (Table 1). There were no significant differences<br />
between the groups with respect to coronary risk<br />
factors (including hypertension), history <strong>of</strong> coronary disease,<br />
or history <strong>of</strong> chronic renal failure. A history <strong>of</strong> alcohol<br />
use was significantly more common in patients with<br />
decreased systolic function. More patients with decreased<br />
function were taking angiotensin-converting enzyme<br />
(ACE) inhibitors <strong>and</strong> digoxin (both P 0.001), whereas<br />
use <strong>of</strong> calcium antagonists (P 0.001) <strong>and</strong> beta-blockers<br />
(P 0.08) tended to be higher in patients with normal<br />
function. Symptoms were similar in the patients with<br />
normal or decreased systolic function, except that angina<br />
was more common in patients with decreased systolic<br />
function. Those with normal function tended to have a<br />
higher body mass index (P 0.06), <strong>and</strong> significantly<br />
more patients with normal function had a body mass index<br />
30 kg/m 2 (P 0.04).<br />
Mean heart rate was significantly higher in patients<br />
with decreased systolic function, <strong>and</strong> tachycardia (heart<br />
rate 100 beats per minute) was more common (Table<br />
1). Systolic blood pressure <strong>and</strong> pulse pressure were significantly<br />
higher in those with normal function, who were<br />
also significantly more likely to have a systolic blood pressure<br />
160 mm Hg or a pulse pressure 60 mm Hg. Although<br />
there was no difference in mean diastolic blood<br />
pressure between the groups, patients with normal function<br />
were significantly more likely to have a diastolic pressure<br />
110 mm Hg. There were no significant differences<br />
in the presence <strong>of</strong> jugular venous distention, pedal<br />
edema, or S 4 gallop sounds. An S 3 gallop tended to be<br />
more common in patients with decreased function (P <br />
0.07), whereas rales were significantly more common in<br />
those with normal function (P 0.05).<br />
There were no significant differences in heart rhythm<br />
or the prevalence <strong>of</strong> abnormal Q waves. Left ventricular
Table 1. Characteristics <strong>of</strong> Patients with Normal Left Ventricular Systolic Function (Ejection Fraction 45%) or Decreased Function<br />
(Ejection Fraction 45%)<br />
Characteristic<br />
Normal Systolic Function<br />
(n 104)<br />
Decreased Systolic Function<br />
(n 121) P Value<br />
Age (years) 59 13<br />
Number (%) or Mean SD<br />
54 13 0.007<br />
Age 60 years 54 (53) 47 (40) 0.05<br />
Male sex<br />
Risk factors<br />
46 (44) 79 (65) 0.001<br />
Hypertension 81 (78) 88 (74) 0.49<br />
Diabetes mellitus 42 (40) 40 (34) 0.30<br />
Hyperlipidemia 6 (6) 7 (6) 0.97<br />
Smoking 40 (39) 54 (45) 0.33<br />
Obesity (body mass index 30 kg/m 2 )<br />
Other conditions<br />
60 (62) 51 (48) 0.04<br />
<strong>History</strong> <strong>of</strong> coronary disease 23 (22) 36 (30) 0.17<br />
Chronic renal failure 16 (15) 11 (9) 0.16<br />
Alcohol use<br />
Medications<br />
21 (20) 44 (37) 0.007<br />
ACE inhibitors 64 (62) 100 (85) 0.001<br />
Diuretics 96 (93) 112 (95) 0.59<br />
Beta-blockers 19 (18) 12 (10) 0.08<br />
Digoxin 28 (27) 67 (57) 0.001<br />
Calcium antagonists 34 (34) 17 (14) 0.001<br />
Hydralazine<br />
Symptoms<br />
16 (16) 13 (11) 0.32<br />
Dyspnea at rest 39 (39) 53 (44) 0.44<br />
Dyspnea on exertion 101 (98) 118 (98) 0.88<br />
Orthopnea 89 (86) 101 (86) 0.86<br />
Paroxysmal nocturnal dyspnea 74 (74) 89 (77) 0.57<br />
Angina 4 (4) 13 (11) 0.05<br />
Nonanginal chest pain<br />
<strong>Physical</strong> examination<br />
38 (37) 32 (26) 0.10<br />
Heart rate (beats per minute) 91 21 100 19 0.001<br />
Heart rate 100 beats per minute 32 (32) 61 (51) 0.004<br />
Systolic blood pressure (mm Hg) 161 40 146 31 0.002<br />
Systolic blood pressure 160 mm Hg 52 (50) 32 (27) 0.001<br />
Diastolic blood pressure (mm Hg) 92 26 89 19 0.34<br />
Diastolic blood pressure 110 mm Hg 26 (25) 15 (13) 0.02<br />
Pulse pressure (mm Hg) 69 26 57 23 0.001<br />
Pulse pressure 60 mm Hg 63 (61) 53 (45) 0.01<br />
Jugular venous distention 73 (72) 87 (74) 0.81<br />
Pedal edema 85 (83) 91 (75) 0.18<br />
Rales 83 (80) 108 (89) 0.05<br />
S3 gallop 25 (28) 42 (41) 0.07<br />
S4 gallop<br />
<strong>Electrocardiogram</strong><br />
Rhythm<br />
9 (11) 7 (7) 0.39<br />
Sinus rhythm 78 (79) 102 (86) 0.14<br />
Atrial fibrillation 19 (19) 12 (10) 0.09<br />
Other rhythm 2 (2) 5 (4) 0.85<br />
Abnormal Q waves 18 (18) 25 (21) 0.56<br />
Left ventricular hypertrophy 22 (22) 49 (42) 0.002<br />
Left atrial abnormality<br />
Chest radiograph<br />
19 (22) 58 (52) 0.001<br />
Cardiomegaly 88 (86) 109 (93) 0.09<br />
Cephalization 81 (79) 106 (91) 0.02<br />
Pulmonary edema 14 (14) 17 (15) 0.99<br />
Pleural effusion 27 (26) 22 (19) 0.18<br />
ACE angiotensin-converting enzyme.<br />
Clinical Findings in Heart Failure/Thomas et al<br />
April 15, 2002 THE AMERICAN JOURNAL OF MEDICINE Volume 112 439
Table 2. Sensitivity, Specificity, <strong>and</strong> Positive <strong>and</strong> Negative Predictive Values <strong>of</strong> Clinical Findings for Normal Systolic Function<br />
(Ejection Fraction 45%)<br />
hypertrophy <strong>and</strong> left atrial abnormality were significantly<br />
more common in those with decreased systolic function.<br />
Radiographic cardiomegaly <strong>and</strong> flow cephalization were<br />
significantly more common in patients with decreased<br />
function, whereas rates <strong>of</strong> pleural effusion <strong>and</strong> pulmonary<br />
edema were similar.<br />
Some clinical parameters had a high sensitivity or a<br />
high specificity for normal systolic function, but none<br />
had both a high sensitivity <strong>and</strong> a high specificity (Table 2).<br />
No clinical parameters had a high positive or negative<br />
Clinical Findings in Heart Failure/Thomas et al<br />
Sensitivity Specificity<br />
Positive<br />
Predictive Value<br />
Negative<br />
Predictive Value<br />
Percentage<br />
Historical factors<br />
Age 60 years 52 61 53 60<br />
Female sex 56 65 58 63<br />
Hypertension 78 26 48 57<br />
Diabetes mellitus 40 66 51 56<br />
Hyperlipidemia 6 94 46 53<br />
Smoking 39 55 43 51<br />
<strong>History</strong> <strong>of</strong> coronary disease 22 70 39 51<br />
Chronic renal failure 15 91 59 55<br />
Alcohol use<br />
Symptoms<br />
20 63 32 48<br />
Dyspnea at rest 39 56 42 52<br />
Dyspnea on exertion 98 2 46 50<br />
Orthopnea 86 14 47 55<br />
Paroxysmal nocturnal dyspnea 74 23 45 50<br />
Angina 4 89 24 52<br />
Nonanginal chest pain<br />
<strong>Physical</strong> examination<br />
37 74 54 57<br />
Body mass index 30 kg/m 2<br />
62 52 54 60<br />
Heart rate 100 beats per minute 31 50 34 45<br />
Systolic blood pressure 160 mm Hg 50 73 62 63<br />
Diastolic blood pressure 110 mm Hg 25 87 63 57<br />
Pulse pressure 60 mm Hg 61 55 54 62<br />
Jugular venous distention 72 26 46 53<br />
Pedal edema 83 25 48 63<br />
Rales 80 11 43 38<br />
S3 gallop 28 59 37 49<br />
S4 gallop<br />
<strong>Electrocardiogram</strong><br />
11 93 56 55<br />
Atrial fibrillation 19 90 61 57<br />
Abnormal Q waves 18 79 42 53<br />
Left ventricular hypertrophy 22 58 31 47<br />
Left atrial abnormality<br />
Chest radiograph<br />
22 48 25 45<br />
Cardiomegaly 86 7 45 36<br />
Cephalization 79 9 43 34<br />
Pleural effusion 26 81 55 56<br />
Pulmonary edema 14 85 45 53<br />
440 April 15, 2002 THE AMERICAN JOURNAL OF MEDICINE Volume 112<br />
predictive value for differentiating normal from decreased<br />
systolic function.<br />
In a multivariate analysis, several clinical findings were<br />
independent predictors <strong>of</strong> normal systolic function, including<br />
female sex (odds ratio [OR] 2.3; 95% confidence<br />
interval [CI]: 1.3 to 4.2; P 0.03), heart rate 100<br />
beats per minute (OR 1.9; 95% CI: 1.1 to 3.9; P <br />
0.005), use <strong>of</strong> ACE inhibitors (OR 0.34; 95% CI: 0.17 to<br />
0.67; P 0.001), <strong>and</strong> use <strong>of</strong> digoxin (OR 0.35; 95% CI:<br />
0.20 to 0.66; P 0.03). The area under the receiver oper-
ating characteristic curves for the clinical features were<br />
0.62 for sex <strong>and</strong> 0.63 for heart rate. Of the patients with<br />
decreased systolic function, 44 (36%) were male <strong>and</strong> had<br />
tachycardia, compared with 11 (11%) <strong>of</strong> those with normal<br />
function, yielding a sensitivity <strong>of</strong> 36%, specificity <strong>of</strong><br />
89%, positive predictive value <strong>of</strong> 80%, <strong>and</strong> negative predictive<br />
value <strong>of</strong> 55% for the combination <strong>of</strong> these two<br />
clinical predictors.<br />
When medications were excluded from the multivariate<br />
analysis, variables that were significantly more common<br />
in patients with normal systolic function included<br />
female sex (OR 2.4; 95% CI: 1.2 to 4.6; P 0.002),<br />
heart rate 100 beats per minute (OR 3.5; 95% CI:<br />
1.7 to 7.1; P 0.001), <strong>and</strong> systolic blood pressure<br />
160 mm Hg (OR 3.7; 95% CI: 1.8 to 7.4; P 0.03),<br />
while left atrial abnormality on ECG was significantly less<br />
common in these patients (OR 0.24; 95% CI: 0.12 to<br />
0.50; P 0.04).<br />
There were greater differences between the 89 patients<br />
with markedly decreased systolic function (ejection fraction<br />
30%) <strong>and</strong> the 136 patients with ejection fractions<br />
30% (Table 3). However, the sensitivity, specificity, <strong>and</strong><br />
positive <strong>and</strong> negative predictive values for these clinical<br />
features were again low (Table 4).<br />
DISCUSSION<br />
This prospective study <strong>of</strong> patients hospitalized with heart<br />
failure observed that some clinical findings were more<br />
common in patients with systolic or diastolic heart failure.<br />
However, none <strong>of</strong> these findings could differentiate<br />
reliably between patients with normal <strong>and</strong> decreased systolic<br />
function.<br />
Several previous studies have compared clinical findings<br />
in patients with systolic or diastolic heart failure,<br />
with inconsistent results. Some investigators have found<br />
that no clinical variables correlated with left ventricular<br />
systolic function (10,13,14,16,17), while others found—<br />
as we did—that older age (8,11,12), hypertension<br />
(7,9,15), female sex (8,9), absence <strong>of</strong> an S 3 gallop (11,12),<br />
<strong>and</strong> obesity (9) were associated with normal systolic function.<br />
Other studies have reported that normal systolic<br />
function was associated with atrial fibrillation (8), absence<br />
<strong>of</strong> jugular venous distention (9), peripheral edema<br />
(15), or the presence (15) or absence (12) <strong>of</strong> paroxysmal<br />
nocturnal dyspnea.<br />
One reason for the inconsistency between studies may<br />
be differences in study design. Most studies have been<br />
retrospective, <strong>and</strong> some were reviews <strong>of</strong> patients who underwent<br />
echocardiography or other tests to evaluate left<br />
ventricular function. In contrast, we performed prospective<br />
measurements in consecutive patients who had presented<br />
with heart failure. In addition, different definitions<br />
<strong>of</strong> “normal” systolic function have been used. We<br />
Clinical Findings in Heart Failure/Thomas et al<br />
defined normal function as an ejection fraction 45%, as<br />
suggested by the European Study Group on Diastolic<br />
Heart Failure (20). Other studies have also used this definition<br />
(3,6,7,14,21,22), whereas some have used an ejection<br />
fraction 50% (2,4,8,11,13,23–27), 55% (12,28),<br />
or other values (9,10,29). When an ejection fraction cut<strong>of</strong>f<br />
value <strong>of</strong> 30% was used, significant differences in clinical<br />
features were more evident in our study, but the sensitivity,<br />
specificity, <strong>and</strong> predictive values <strong>of</strong> these clinical<br />
findings for identifying patients with severe left ventricular<br />
systolic dysfunction remained poor.<br />
Given the inconsistent <strong>and</strong> even contradictory findings<br />
<strong>of</strong> previous studies, it is not surprising that we did not<br />
find any clinical parameters that could distinguish patients<br />
who had normal function from those with decreased<br />
systolic function. Increased filling pressures are<br />
characteristic <strong>of</strong> both diastolic <strong>and</strong> systolic heart failure;<br />
all patients in our study were hospitalized, perhaps explaining<br />
why the clinical findings <strong>of</strong> congestion were similar<br />
in the two groups. Other studies have compared<br />
physical findings <strong>and</strong> invasive hemodynamic measurements<br />
in patients with chronic heart failure, <strong>and</strong> have<br />
shown that the physical examination is a relatively insensitive<br />
technique for identifying elevated filling pressures<br />
(30).<br />
There were several differences in medication use between<br />
the patients with normal <strong>and</strong> decreased systolic<br />
function. It is possible that medications may have affected<br />
the clinical findings; for example, the higher prevalence <strong>of</strong><br />
ACE inhibitor use may have reduced the blood pressure<br />
<strong>and</strong> the frequency <strong>of</strong> an S 3 gallop in patients with decreased<br />
systolic function. Similarly, lower heart rates in<br />
the patients with normal function may have been due in<br />
part to use <strong>of</strong> beta-blockers or rate-lowering calcium antagonists.<br />
One puzzling issue is why the prevalence <strong>of</strong> an S 3 gallop<br />
did not differ significantly between the groups; the borderline<br />
P values (univariate P 0.07, multivariate P <br />
0.09) suggest that this may have been due to an insufficient<br />
sample size. However, an S 3 gallop was present in<br />
41% <strong>of</strong> patients with decreased systolic function <strong>and</strong> in<br />
28% <strong>of</strong> those with normal function, suggesting that it<br />
would not be a clinically useful discriminator even if the<br />
difference was statistically significant. The mechanism <strong>of</strong><br />
an S 3 gallop in patients with normal function, <strong>and</strong> the<br />
reason for the relatively low prevalence <strong>of</strong> an S 3 gallop in<br />
those with decreased function, are not clear. Prior studies<br />
have also noted that an S 3 gallop is common in patients<br />
with diastolic heart failure (7,11,24).<br />
We found an independent association between left<br />
atrial abnormality on ECG <strong>and</strong> systolic dysfunction. Left<br />
atrial abnormality correlates more with left atrial volume<br />
than with left atrial pressure (19), <strong>and</strong> heart failure patients<br />
with low ejection fractions commonly have an enlarged<br />
left atrium. Left ventricular hypertrophy on ECG<br />
April 15, 2002 THE AMERICAN JOURNAL OF MEDICINE Volume 112 441
Table 3. Characteristics <strong>of</strong> Patients with a Left Ventricular Ejection Fraction 30% Compared with 30%<br />
Characteristic<br />
Ejection Fraction<br />
30%<br />
(n 136)<br />
Ejection Fraction<br />
30%<br />
(n 89) P Value<br />
Number (%) or Mean SD<br />
Age (years) 58 14 53 13 0.008<br />
Age 60 years 67 (50) 34 (39) 0.10<br />
Male sex<br />
Risk factors<br />
65 (49) 60 (67) 0.004<br />
Hypertension 108 (81) 61 (69) 0.04<br />
Diabetes mellitus 55 (41) 27 (30) 0.10<br />
Hyperlipidemia 8 (6) 5 (6) 0.91<br />
Smoking 54 (41) 40 (45) 0.52<br />
Obesity (body mass index 30 kg/m 2 )<br />
Other conditions<br />
75 (61) 36 (44) 0.01<br />
<strong>History</strong> <strong>of</strong> coronary disease 32 (24) 27 (30) 0.29<br />
Chronic renal failure 20 (15) 7 (8) 0.11<br />
Alcohol use<br />
Medications<br />
29 (22) 36 (40) 0.003<br />
ACE inhibitors 88 (67) 76 (85) 0.002<br />
Diuretics 124 (94) 84 (94) 0.89<br />
Beta-blockers 25 (19) 6 (7) 0.01<br />
Digoxin 39 (30) 56 (63) 0.001<br />
Calcium antagonists 41 (32) 10 (11) 0.001<br />
Hydralazine<br />
Symptoms<br />
21 (16) 8 (9) 0.14<br />
Dyspnea at rest 52 (39) 40 (45) 0.39<br />
Dyspnea on exertion 132 (98) 87 (99) 0.55<br />
Orthopnea 114 (85) 76 (87) 0.64<br />
Paroxysmal nocturnal dyspnea 98 (75) 65 (76) 0.86<br />
Angina 11 (8) 6 (7) 0.71<br />
Nonanginal chest pain<br />
<strong>Physical</strong> examination<br />
49 (36) 21 (24) 0.05<br />
Heart rate (beats per minute) 92 20 102 20 0.001<br />
Heart rate 100 beats per minute 46 (35) 47 (53) 0.005<br />
Systolic blood pressure (mm Hg) 162 39 139 27 0.001<br />
Systolic blood pressure 160 mm Hg 67 (50) 17 (19) 0.001<br />
Diastolic blood pressure (mm Hg) 92 26 88 16 0.15<br />
Diastolic blood pressure 110 mm Hg 32 (24) 9 (10) 0.01<br />
Pulse pressure (mm Hg) 70 26 51 19 0.001<br />
Pulse pressure 60 mm Hg 89 (66) 27 (31) 0.001<br />
Jugular venous distention 91 (69) 69 (79) 0.09<br />
Pedal edema 113 (84) 63 (71) 0.02<br />
Rales 111 (82) 80 (90) 0.09<br />
S3 gallop 33 (29) 34 (45) 0.02<br />
S4 gallop<br />
<strong>Electrocardiogram</strong><br />
Rhythm<br />
14 (12) 2 (3) 0.02<br />
Sinus rhythm 108 (82) 72 (83) 0.91<br />
Atrial fibrillation 21 (16) 10 (11) 0.46<br />
Other rhythm 2 (2) 5 (6) 0.18<br />
Abnormal Q waves 26 (20) 17 (20) 0.98<br />
Left ventricular hypertrophy 36 (27) 35 (41) 0.04<br />
Left atrial abnormality<br />
Chest radiograph<br />
34 (30) 43 (52) 0.001<br />
Cardiomegaly 114 (86) 83 (97) 0.01<br />
Cephalization 107 (80) 80 (93) 0.01<br />
Pulmonary edema 17 (13) 14 (16) 0.47<br />
Pleural effusion 34 (26) 15 (17) 0.16<br />
ACE angiotensin-converting enzyme.<br />
Clinical Findings in Heart Failure/Thomas et al<br />
442 April 15, 2002 THE AMERICAN JOURNAL OF MEDICINE Volume 112
Table 4. Sensitivity, Specificity, <strong>and</strong> Positive <strong>and</strong> Negative Predictive Values <strong>of</strong> Clinical Findings for Markedly Decreased Systolic<br />
Function (Ejection Fraction 30%)<br />
Sensitivity Specificity<br />
was more common in patients with decreased systolic<br />
function, even though it is commonly considered to be a<br />
characteristic <strong>of</strong> diastolic heart failure. This result is a<br />
reminder that concentric or eccentric hypertrophy is<br />
common in heart failure regardless <strong>of</strong> the etiology.<br />
A limitation <strong>of</strong> this study is that some <strong>of</strong> the history <strong>and</strong><br />
physical examinations were performed by an internist<br />
rather than by a cardiologist, <strong>and</strong> the clinical skills <strong>of</strong> the<br />
examining physicians were not assessed. Our results<br />
might have been different if all patients had been interviewed<br />
<strong>and</strong> examined by a cardiologist. However, this<br />
study does represent the real-world situation, in which<br />
Clinical Findings in Heart Failure/Thomas et al<br />
Positive Predictive<br />
Value<br />
Negative Predictive<br />
Value<br />
Percentage<br />
Historical factors<br />
Age 60 years 39 50 34 55<br />
Male sex 67 52 48 71<br />
Hypertension 69 19 36 48<br />
Diabetes mellitus 30 59 33 56<br />
Hyperlipidemia 6 94 38 60<br />
Smoking 45 59 43 62<br />
<strong>History</strong> <strong>of</strong> coronary disease 30 76 46 62<br />
Chronic renal failure 8 85 26 58<br />
Alcohol use<br />
Symptoms<br />
40 78 55 66<br />
Dyspnea at rest 45 61 43 62<br />
Dyspnea on exertion 99 2 40 75<br />
Orthopnea 87 15 40 65<br />
Paroxysmal nocturnal dyspnea 76 25 40 62<br />
Angina 7 92 35 60<br />
Nonanginal chest pain<br />
<strong>Physical</strong> examination<br />
24 64 30 56<br />
Body mass index 30 kg/m 2<br />
44 39 32 51<br />
Heart rate 100 beats per minute 53 65 51 68<br />
Systolic blood pressure 160 mm Hg 19 50 20 49<br />
Diastolic blood pressure 110 mm Hg 10 76 22 56<br />
Pulse pressure 60 mm Hg 31 34 23 42<br />
Jugular venous distention 79 31 43 69<br />
Pedal edema 71 16 36 46<br />
Rales 90 18 42 74<br />
S3 gallop 45 71 51 66<br />
S4 gallop<br />
<strong>Electrocardiogram</strong><br />
3 88 12 58<br />
Atrial fibrillation 11 84 32 59<br />
Abnormal Q waves 20 80 40 61<br />
Left ventricular hypertrophy 41 73 49 65<br />
Left atrial abnormality<br />
Chest radiograph<br />
52 70 56 67<br />
Cardiomegaly 97 14 42 86<br />
Cephalization 93 20 43 81<br />
Pleural effusion 17 74 31 58<br />
Pulmonary edema 16 87 45 62<br />
many patients with heart failure are managed by primary<br />
care physicians. A related limitation is that the study included<br />
all patients with an admitting diagnosis <strong>of</strong> heart<br />
failure; no other definition <strong>of</strong> heart failure was applied.<br />
However, all but 2 <strong>of</strong> the 225 patients met the Framingham<br />
criteria for congestive heart failure (17).<br />
Another limitation is that we included only patients<br />
admitted to the hospital. Outpatients have fewer symptoms<br />
<strong>and</strong> physical findings <strong>of</strong> heart failure, <strong>and</strong> it is possible<br />
that differences between patients with normal <strong>and</strong><br />
decreased systolic function might be more apparent. Furthermore,<br />
only the findings at the time <strong>of</strong> admission were<br />
April 15, 2002 THE AMERICAN JOURNAL OF MEDICINE Volume 112 443
ecorded, <strong>and</strong> it is possible that the temporal evolution <strong>of</strong><br />
symptoms may differ in the two groups <strong>of</strong> patients. We<br />
also excluded patients in whom left ventricular function<br />
was not measured, which may have introduced bias.<br />
However, only 15% <strong>of</strong> admitted patients were excluded<br />
for this reason. In addition, ejection fraction was determined<br />
by visual estimation <strong>of</strong> ECGs. Interobserver <strong>and</strong><br />
intraobserver variability <strong>of</strong> estimates <strong>of</strong> ejection fractions<br />
were not calculated, but this method correlates well with<br />
radionuclide angiography (r 0.88), with low interobserver<br />
variability (r 0.88) in patients with adequate images<br />
(31). Although the data were collected prospectively,<br />
some physicians may have known the ejection fractions<br />
<strong>of</strong> their patients when they recorded their admission<br />
notes. In addition, this study was performed in an innercity<br />
hospital that had patients with a high prevalence <strong>of</strong><br />
hypertension, <strong>and</strong> these results may not apply to other<br />
groups <strong>of</strong> patients. Nevertheless, the prevalence <strong>of</strong> diastolic<br />
dysfunction was similar to that reported in other<br />
studies (11,32).<br />
The etiology <strong>and</strong> prognosis <strong>of</strong> heart failure may be different<br />
in patients with normal or decreased systolic function<br />
(1,5). The treatment <strong>of</strong> diastolic dysfunction is not<br />
well defined; if future trials find that st<strong>and</strong>ard therapies<br />
for systolic dysfunction are equally effective in patients<br />
with diastolic dysfunction, recommendations to determine<br />
left ventricular function in patients with heart failure<br />
may need to be reassessed. However, our results indicate<br />
that differences in clinical parameters are not <strong>of</strong> sufficient<br />
magnitude to allow systolic function to be<br />
predicted reliably in a patient with heart failure, <strong>and</strong> support<br />
the recommendations <strong>of</strong> the American College <strong>of</strong><br />
Cardiology/American Heart Association (5) <strong>and</strong> the<br />
Agency for Health Care Policy <strong>and</strong> Research (33) that all<br />
patients with heart failure should undergo echocardiography<br />
or radionuclide ventriculography to measure left<br />
ventricular function.<br />
REFERENCES<br />
1. Packer M, Cohn JN, on behalf <strong>of</strong> the Steering Committee <strong>and</strong><br />
Membership <strong>of</strong> the Advisory Council to Improve Outcomes Nationwide<br />
in Heart Failure. Consensus recommendations for the<br />
management <strong>of</strong> chronic heart failure. Am J Cardiol. 1999;83:1A–<br />
38A.<br />
2. Senni M, Tribouilloy CM, Rodeheffer RJ, et al. Congestive heart<br />
failure in the community. A study <strong>of</strong> all incident cases in Olmstead<br />
County, Minnesota, in 1991. Circulation. 1998;98:2282–2289.<br />
3. Soufer R, Wohlgelernter D, Vita NA, et al. Intact systolic left ventricular<br />
function in clinical congestive heart failure. Am J Cardiol.<br />
1985;55:1032–1036.<br />
4. McDermott MM, Feinglass J, Lee PI, et al. Systolic function, readmission<br />
rates, <strong>and</strong> survival among consecutively hospitalized patients<br />
with congestive heart failure. Am Heart J. 1997;134:728 –736.<br />
5. Report <strong>of</strong> the American College <strong>of</strong> Cardiology/American Heart Association<br />
Task Force on Practice Guidelines (Committee on Eval-<br />
Clinical Findings in Heart Failure/Thomas et al<br />
444 April 15, 2002 THE AMERICAN JOURNAL OF MEDICINE Volume 112<br />
uation <strong>and</strong> Management <strong>of</strong> Heart Failure). Guidelines for evaluation<br />
<strong>and</strong> management <strong>of</strong> heart failure. Circulation. 1995;92:2764 –<br />
2784.<br />
6. Cohn JN, Johnson G, <strong>and</strong> the VA Cooperative Study Group. Heart<br />
failure with normal ejection fraction: the V-HeFT study. Circulation.<br />
1990;81(Suppl 2):III-48 –III-53.<br />
7. Dougherty AH, Naccarelli GV, Gray EL, et al. Congestive heart<br />
failure with normal systolic function. Am J Cardiol. 1984;54:778 –<br />
782.<br />
8. Wong WF, Gold S, Fukuyama O, Blanchette PL. Diastolic dysfunction<br />
in elderly patients with congestive heart failure. Am J Cardiol.<br />
1989;63:1526 –1528.<br />
9. Ghali JK, Kadadia S, Cooper RS, Liao Y. Bedside diagnosis <strong>of</strong> preserved<br />
versus impaired left ventricular systolic function in heart<br />
failure. Am J Cardiol. 1991;67:1002–1006.<br />
10. Stone GW, Griffin B, Shah PK, et al. Prevalence <strong>of</strong> unsuspected<br />
mitral regurgitation <strong>and</strong> left ventricular diastolic dysfunction in<br />
patients with coronary artery disease <strong>and</strong> acute pulmonary edema<br />
associated with normal or depressed left ventricular systolic function.<br />
Am J Cardiol. 1991;67:37–41.<br />
11. Aronow WS, Ahn C, Kronzon I. Prognosis <strong>of</strong> congestive heart failure<br />
in elderly patients with normal versus abnormal left ventricular<br />
systolic function associated with coronary artery disease. Am J Cardiol.<br />
1990;66:1257–1259.<br />
12. Aguirre FV, Pearson AC, Lewen MK, et al. Usefulness <strong>of</strong> Doppler<br />
echocardiography in the diagnosis <strong>of</strong> congestive heart failure. Am J<br />
Cardiol. 1989;63:1098 –1102.<br />
13. Cocchi A, Zuccala G, Del Sindaco D, et al. Cross-sectional<br />
echocardiography: a window on congestive heart failure in the elderly.<br />
Aging (Milano). 1991;3:257–262.<br />
14. Warnowicz MA, Parker H, Cheitlin MD. Prognosis <strong>of</strong> patients with<br />
acute pulmonary edema <strong>and</strong> normal ejection fraction after acute<br />
myocardial infarction. Circulation. 1983;67:330 –334.<br />
15. Bier AJ, Eichacker PQ, Sinoway LI, et al. Acute pulmonary edema:<br />
clinical <strong>and</strong> noninvasive evaluation. Angiology. 1988;39:211–218.<br />
16. Kinney EL, Wright RJ. Survival in patients with heart failure <strong>and</strong><br />
normal basal systolic wall motion. Angiology. 1989;40:1025–1029.<br />
17. Ho KKL, Anderson KM, Kannel WB, et al. Survival after the onset<br />
<strong>of</strong> congestive heart failure in Framingham Heart Study subjects.<br />
Circulation. 1993;88:107–115.<br />
18. Sgarbossa EB, Wagner GS. Electrocardiography. In: Topol EJ, ed.<br />
Textbook <strong>of</strong> Cardiovascular Medicine. Philadelphia: Lippincott-<br />
Raven; 1998:1545–1589.<br />
19. Chou T-C. Atrial abnormalities. Electrocardiography in Clinical<br />
Practice. 3rd ed. Philadelphia: W. B. Saunders; 1991:23–35.<br />
20. European Study Group on Diastolic Heart Failure. How to diagnose<br />
diastolic heart failure. Eur Heart J. 1998;19:990 –1003.<br />
21. Judge KW, Pawitan Y, Caldwell J, et al. Congestive heart failure<br />
symptoms in patients with preserved left ventricular systolic<br />
function: analysis <strong>of</strong> the CASS registry. J Am Coll Cardiol. 1991;18:<br />
377–382.<br />
22. Cregler LL, Georgiou D, Sosa I. Left ventricular diastolic dysfunction<br />
in patients with congestive heart failure. J Nat Med Assoc. 1991;<br />
83:49 –52.<br />
23. Marantz PR, Tobin JN, Wassertheil-Smoller S, et al. The relationship<br />
between left ventricular systolic function <strong>and</strong> congestive heart<br />
failure diagnosed by clinical criteria. Circulation. 1988;77:607–612.<br />
24. Echeverria HH, Bilsker MS, Myerburg RJ, Kessler KM. Congestive<br />
heart failure: echocardiographic insights. Am J Med. 1983;75:750 –<br />
755.<br />
25. Iriarte M, Murga N, Sagastagoitia D, et al. Congestive heart failure<br />
from left ventricular dysfunction in systemic hypertension. Am J<br />
Cardiol. 1993;71:308 –312.
26. Kitzman DW, Higginbotham MB, Cobb FR, et al. Exercise intolerance<br />
in patients with heart failure <strong>and</strong> preserved left ventricular<br />
systolic function: failure <strong>of</strong> the Frank-Starling mechanism. JAm<br />
Coll Cardiol. 1991;17:1065–1072.<br />
27. Brogan WC, Hillis LD, Flores ED, Lange RA. The natural history <strong>of</strong><br />
isolated left ventricular diastolic dysfunction. Am J Med. 1992;92:<br />
627–630.<br />
28. Given BD, Lee TH, Stone PH, Dzau VJ. Nifedipine in severely hypertensive<br />
patients with congestive heart failure <strong>and</strong> preserved ventricular<br />
systolic function. Arch Intern Med. 1985;145:281–285.<br />
29. Madsen BK, Hansen JF, Stokholm KH, et al. Chronic congestive<br />
heart failure: descriptions <strong>and</strong> survival <strong>of</strong> 190 consecutive patients<br />
with a diagnosis <strong>of</strong> chronic congestive heart failure based on clinical<br />
signs <strong>and</strong> symptoms. Eur Heart J. 1994;15:303–310.<br />
Clinical Findings in Heart Failure/Thomas et al<br />
30. Stevenson LW, Perl<strong>of</strong>f JK. The limited reliability <strong>of</strong> physical signs<br />
for estimating hemodynamics in chronic heart failure. JAMA. 1989;<br />
261:884 –888.<br />
31. Amico AF, Lichtenberg GS, Reisner SA, et al. Superiority <strong>of</strong> visual<br />
versus computerized echocardiographic estimation <strong>of</strong> radionuclide<br />
left ventricular ejection fraction. Am Heart J. 1989;118:<br />
1259 –1265.<br />
32. Grossman W. Diastolic dysfunction in congestive heart failure.<br />
N Engl J Med. 1991;325:1557–1564.<br />
33. Konstam MA, Dracup K, Bottorff MB, et al. Heart Failure: Evaluation<br />
<strong>and</strong> Care <strong>of</strong> Patients with Left Ventricular Systolic Dysfunction.<br />
Rockville, MD: U.S. Dept <strong>of</strong> Health <strong>and</strong> Human Services, Agency<br />
for Health Care Policy <strong>and</strong> Research; 1994 Clinical Practice Guideline<br />
No. 11.<br />
April 15, 2002 THE AMERICAN JOURNAL OF MEDICINE Volume 112 445