The Principles of the Alexander Discipline - New York University
The Principles of the Alexander Discipline - New York University
The Principles of the Alexander Discipline - New York University
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
<strong>The</strong> <strong>Principles</strong> <strong>of</strong> <strong>the</strong> <strong>Alexander</strong> <strong>Discipline</strong><br />
Richard G. <strong>Alexander</strong><br />
A<br />
<strong>The</strong> <strong>Alexander</strong> <strong>Discipline</strong> is based on <strong>the</strong> premise <strong>of</strong> a number <strong>of</strong> principles.<br />
This article lists and briefly describes <strong>the</strong>se principles and <strong>the</strong> reason each is<br />
considered important in <strong>the</strong> management <strong>of</strong> <strong>the</strong> orthodontic patient in <strong>the</strong><br />
<strong>Alexander</strong> <strong>Discipline</strong>, (Semin Orthod 2001;7:62-66,) Copyright © 2001 by<br />
W.B. Saunders Company<br />
nY enduring principle must be built on a<br />
solid foundation, on certain beliefs that<br />
have been tested and proven by time and experience.<br />
In <strong>the</strong> Mexander <strong>Discipline</strong>, a certain<br />
number <strong>of</strong> principles are followed that give this<br />
technique its uniqueness. <strong>The</strong> first three principles<br />
focus on <strong>the</strong> philosophic nature and <strong>the</strong><br />
attitudinal approach to <strong>the</strong> delivery <strong>of</strong> <strong>the</strong> <strong>Discipline</strong>.<br />
One <strong>of</strong> <strong>the</strong> original goals <strong>of</strong> <strong>the</strong> technique is<br />
to make treatment easy and more comfortable<br />
for <strong>the</strong> patient. For any technique in orthodontics<br />
to be successful, <strong>the</strong> patient must be involved<br />
in <strong>the</strong> procedures. Even though some appliances<br />
are said to be noncompliant, <strong>the</strong> reality is that<br />
no such thing is possible. Each patient must be<br />
willing to keep <strong>the</strong>ir teeth clean, take care <strong>of</strong> <strong>the</strong><br />
appliances, watch what <strong>the</strong>y eat, and be present<br />
for <strong>the</strong>ir appointments. Allowing <strong>the</strong> patient to<br />
become a partner in <strong>the</strong> treatment procedures<br />
not only gives <strong>the</strong>m some ownership in <strong>the</strong> process,<br />
but it ensures that <strong>the</strong> results will reach a<br />
higher level.<br />
Patient compliance is critical to <strong>the</strong> success <strong>of</strong><br />
this technique. Too <strong>of</strong>ten, o<strong>the</strong>r techniques focus<br />
on <strong>the</strong> mechanics <strong>of</strong> treatment. Mechanics<br />
are important, however, mechanics alone will<br />
not produce <strong>the</strong> optimal result without patient<br />
cooperation. In orthodontic education, perhaps<br />
<strong>the</strong> forgotten skill is teaching <strong>the</strong> student motivational<br />
techniques for successful results. 1,2<br />
From Arlington, TX.<br />
Address correspondence to IL G. leVi& <strong>Alexander</strong>, DDS, MSD,<br />
840 West Mitchell, Arlington, TX 76013.<br />
Copyright © 2001 by W.B. Saunders Company<br />
1073-8746/01/0702-0001535.00/0<br />
doi: l O. 1053/sodo. 2001.23536<br />
When <strong>the</strong> need for this skill is understood, <strong>the</strong><br />
clinician will accept <strong>the</strong> responsibility to learn<br />
techniques that will enhance <strong>the</strong>ir ability to mo-<br />
tivate <strong>the</strong>ir patients while producing high-quality<br />
results.<br />
Principle number 1 is taken from Allen's 3<br />
book As a Man Thinketh, "In all human affairs<br />
<strong>the</strong>re are efforts and <strong>the</strong>re are results, and <strong>the</strong><br />
strength <strong>of</strong> <strong>the</strong> effort is <strong>the</strong> measure <strong>of</strong> <strong>the</strong> re-<br />
suit." From this sentence comes <strong>the</strong> formula,<br />
Effort = Results.<br />
Principle number 2 is based on ano<strong>the</strong>r<br />
quote, "Sometimes when I consider what tre-<br />
mendous consequences come from little things,<br />
I am tempted to think, <strong>the</strong>re are no little<br />
things. ''4<br />
Principle number 3 comes from World War II<br />
and is used in many variations today, "keep it<br />
simple stupid. ''3 Of course, <strong>the</strong> acronym is KISS.<br />
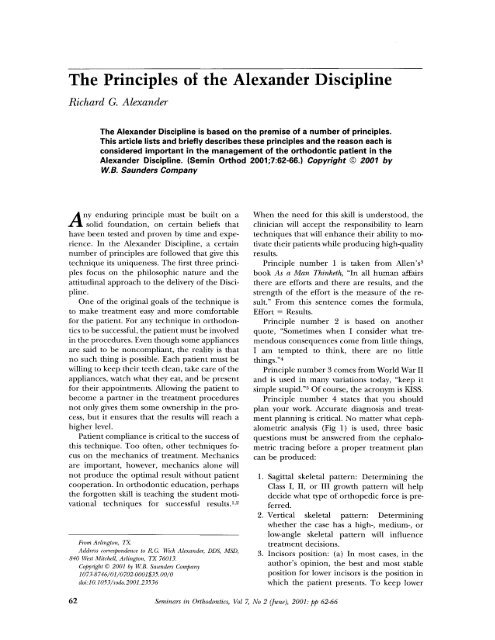
Principle number 4 states that you should<br />
plan your work. Accurate diagnosis and treat-<br />
ment planning is critical. No matter what ceph-<br />
alometric analysis (Fig 1) is used, three basic<br />
questions must be answered from <strong>the</strong> cephalo-<br />
metric tracing before a proper treatment plan<br />
can be produced:<br />
62 Seminars in Orthodontics, Vol 7, No 2 (June), 2001: pp 62-66<br />
1. Sagittal skeletal pattern: Determining <strong>the</strong><br />
Class I, II, or III growth pattern will help<br />
decide what type <strong>of</strong> orthopedic force is pre-<br />
ferred.<br />
2. Vertical skeletal pattern: Determining<br />
whe<strong>the</strong>r <strong>the</strong> case has a high-, medium-, or<br />
low-angle skeletal pattern will influence<br />
treatment decisions.<br />
3. Incisors position: (a) In most cases, in <strong>the</strong><br />
author's opinion, <strong>the</strong> best and most stable<br />
position for lower incisors is <strong>the</strong> position in<br />
which <strong>the</strong> patient presents. To keep lower
<strong>Alexander</strong> <strong>Discipline</strong> 63<br />
POINTS OF MEASUREMENT<br />
Figure 1. Cephalometric measurements used to determine sagital and vertical skeletal patterns and incisor<br />
positions.<br />
incisors in <strong>the</strong>ir original positions is <strong>of</strong>ten<br />
our goal. (b) In extraction cases, lower inci-<br />
sors are almost always uprighted. (c) Our<br />
studies 5-7 have shown that lower incisors can<br />
be advanced up to 3 ° and remain stable.<br />
Beyond that degree, instability is more<br />
likely. <strong>The</strong> only time <strong>the</strong> lower incisors are<br />
advanced beyond this degree is when <strong>the</strong>y<br />
are abnormally retroclined. <strong>The</strong> latter situa-<br />
tion is commonly seen in Class II, Division 2,<br />
and Class II, Division 1 deep-bite cases.<br />
By maintaining good torque control <strong>of</strong> <strong>the</strong><br />
upper incisors, along with <strong>the</strong> lower incisors, a<br />
balanced interincisal angle is created. This is<br />
critical for long-term stability, s<br />
Principle number 5 describes our goals for<br />
stability. Objectives include mandibular incisors<br />
that are balanced on basal bone with a good<br />
interincisal angle, cuspids not expanded, proper<br />
root artistic positioning, upright mandibular<br />
molars, normal overbite and overjet, and a func-<br />
tional occlusion in centric relation. <strong>The</strong>se goals,<br />
when achieved, have been found to create<br />
healthy, aes<strong>the</strong>tically pleasing, and stable re-<br />
sults.5.6.s-10<br />
Principle number 6 describes specific brack-<br />
ets designed for increased interbracket space;<br />
wings for rotation and correction, <strong>the</strong>n control;<br />
precision pretorqued slots; and precision base<br />
variation. Details <strong>of</strong> <strong>the</strong> bracket system are dis-<br />
cussed by Bagden on page 74 in this issue <strong>of</strong><br />
Seminars in Orthodontics.<br />
Principle number 7 recommends "building<br />
treatment" into <strong>the</strong> bracket placement. In plac-<br />
ing brackets, three dimensions are considered:<br />
bracket height, bracket angulation, and mesio-<br />
distal bracket position. This is also described<br />
later.<br />
Principle number 8 is to obtain predictable<br />
orthopedic correction by using a face bow, face<br />
mask, rapid palatal expansion, lip bumper, or<br />
o<strong>the</strong>r auxiliary appliances such as <strong>the</strong> transpala-<br />
tal arch, <strong>the</strong> Nance, lingual arch, magnets, and<br />
distalizing mechanics.<br />
Face bow treatment is discussed in ano<strong>the</strong>r<br />
article in this issue. In <strong>the</strong> Mexander <strong>Discipline</strong>,<br />
a face bow and face mask are used primarily for<br />
orthopedic forces. This means that <strong>the</strong>se forces<br />
are placed on consolidated, tied-back arch wires<br />
in growing patients. If arch wires are not tied
64 Richard G. <strong>Alexander</strong><br />
back, <strong>the</strong> facebow forces are changed to orth-<br />
odontic forces, resulting in tooth movement.<br />
Principle number 9 discusses <strong>the</strong> use <strong>of</strong> a<br />
proven arch form design 12 (Fig 2) and a contem-<br />
porary arch wire force system. 13 Most patients<br />
are treated by using continuous arch wires be-<br />
ginning with <strong>the</strong> maxillary arch. <strong>The</strong> initial arch<br />
wire is round and flexible (.016 NiTi). <strong>The</strong> tran-<br />
sitional arch wire has intermediate stiffness (.016<br />
stainless steel or 17 × 25 titanium alloy). <strong>The</strong><br />
final wire is stiff, 17 × 25 stainless steel. <strong>The</strong> only<br />
difference in <strong>the</strong> mandibular sequence is that<br />
<strong>the</strong> initial arch wire is a flexible rectangular wire,<br />
for initial torque control. <strong>The</strong> functions <strong>of</strong> <strong>the</strong><br />
arch wires include: elimination <strong>of</strong> rotations, de-<br />
velopment <strong>of</strong> arch form, leveling <strong>the</strong> arches,<br />
control <strong>of</strong> torque, and final arch form.<br />
Principle number 10 is to consolidate<br />
arches early in treatment. <strong>The</strong> purpose <strong>of</strong> clos-<br />
ing spaces is to change 10 to 12 independent<br />
force units (<strong>the</strong> teeth) into 1 unit. When this<br />
has been accomplished, orthopedic forces,<br />
such as a face bow or a face mask, can create<br />
skeletal changes ra<strong>the</strong>r than dental changes.<br />
Also, iutraoral elastics, when attached to <strong>the</strong><br />
ball hooks on <strong>the</strong> brackets, will not move in-<br />
dividual teeth or cause spaces to open between<br />
<strong>the</strong> teeth. Consolidated arches are a goal <strong>of</strong><br />
this treatment.<br />
Principle number 11 is to obtain complete<br />
bracket engagement when placing arch wires,<br />
ligating with steel ligatures, and maintaining<br />
consolidation with omega loops "tied back."<br />
One <strong>of</strong> <strong>the</strong> most important concepts <strong>of</strong> <strong>the</strong> dis-<br />
cipline is using tied-back arch wires.<br />
Principle number 12 is to level arches and<br />
open <strong>the</strong> bite with accentuated and reverse<br />
curves <strong>of</strong> Spee. Clinical experience and re-<br />
search 1:~,14 have substantiated that leveling <strong>the</strong><br />
arches and opening <strong>the</strong> bite with <strong>the</strong> Mexander<br />
<strong>Discipline</strong> is not only successful, but also stable<br />
(Fig 3).<br />
Principle number 13 advocates progressing<br />
into finishing arch wires rapidly and allowing<br />
sufficient time for <strong>the</strong> arch wire to move <strong>the</strong><br />
teeth to <strong>the</strong>ir desired position. By following<br />
<strong>the</strong> previous principles and sequencing <strong>the</strong><br />
treatment plan, <strong>the</strong> finishing arch wire is usu-<br />
ally placed in 6 to 9 months in nonextraction<br />
patients. In extraction treatment procedures,<br />
progressing into finishing arch wires may take<br />
9 to 12 months All <strong>of</strong> <strong>the</strong> final finishing re-<br />
ORMCO ®<br />
Part No 20%0060<br />
Figure 2. Most maxillary arch forms will fall<br />
within 1 SD <strong>of</strong> this template. Two mandibular arch<br />
forms are needed to accomplish this. (Courtesy <strong>of</strong><br />
Ormco Corp, Gleudora, CA.)<br />
quirements are placed into <strong>the</strong> stainless steel<br />
finishing arch wire: arch form, torque, curve,<br />
and omega loops. After this wire has been<br />
properly tied in (full-bracket engagement and<br />
tied back with steel ligature wires), time is<br />
needed for <strong>the</strong> generated forces to have <strong>the</strong>ir<br />
effects and to move <strong>the</strong> teeth into <strong>the</strong>ir final<br />
positions. Often this wire will remain in place<br />
until fixed appliances are removed.<br />
Principle number 14 focuses on creating sym-<br />
metry. Coordination <strong>of</strong> <strong>the</strong> arches is essential to<br />
establish occlusal symmetry. <strong>The</strong> maxillary and<br />
mandibular arch forms have now been individ-<br />
ually finalized and <strong>the</strong> goal <strong>the</strong>n is to get <strong>the</strong><br />
maxillary and mandibular arches coordinated.<br />
Coordination is accomplished by using pre-<br />
formed arch wires in both arches as well as sym-<br />
metrically adjusting <strong>the</strong> inner bow <strong>of</strong> <strong>the</strong> face<br />
bow and <strong>the</strong> lip bumper. Final symmetry is es-
<strong>Alexander</strong> <strong>Discipline</strong> 65<br />
Figure 3. Mandibular heat-treated 17 x 25 ss arch wire with reverse curve <strong>of</strong> Spee tied in and tied back (A).<br />
Six months later with both arches level (B).<br />
tablished by specific elastics in finishing arch<br />
wires.<br />
Principle number 15 recommends that finish-<br />
ing arch wires be in place before initiating elastic<br />
wear. By establishing arch form and proper<br />
torque controls before using intraoral elastics,<br />
<strong>the</strong> elastic forces act more orthopedically, mov-<br />
ing <strong>the</strong> entire arches without adversely affecting<br />
<strong>the</strong> teeth. <strong>The</strong> exceptions to this rule include:<br />
<strong>the</strong> use <strong>of</strong> cross-bite elastics when necessary;<br />
Class III elastics may be used when <strong>the</strong> lower<br />
arch is initially bonded to prevent flaring <strong>of</strong> <strong>the</strong><br />
lower incisors, and/or while closing lower ex-<br />
traction spaces with a closing loop arch wire in<br />
maximum anchorage situations; and Class I1<br />
elastics may be used when closing lower extrac-<br />
tion spaces with a closing-loop arch wire to move<br />
lower molars forward in minimum anchorage<br />
situations.<br />
Principle number 16, in nonextraction cases, u~<br />
recommends initiating treatment in <strong>the</strong> upper<br />
arch and progressing into finishing arch wires as<br />
soon as possible. Because <strong>the</strong> major goal in non-<br />
extraction treatment is to control <strong>the</strong> position <strong>of</strong><br />
<strong>the</strong> lower anterior teeth, total focus can <strong>the</strong>n be<br />
placed on <strong>the</strong>se teeth when <strong>the</strong> lower arch is<br />
banded/bonded. <strong>The</strong> lower anterior teeth are<br />
controlled by -5 ° torque in lower incisor brack-<br />
ets, -6 ° tip on lower first molars, <strong>the</strong> use <strong>of</strong><br />
initial flexible rectangular arch wire, slenderiz-<br />
ing teeth if necessary, and Class II1 elastics if<br />
necessary.<br />
Principle number 17 recommends that, in<br />
extraction cases, treatment be initiated in <strong>the</strong><br />
upper arch. <strong>The</strong> objective is to remove potential<br />
bracket interferences by improving <strong>the</strong> overbite<br />
with an accentuated cmwe <strong>of</strong> Spee and retract-<br />
ing <strong>the</strong> cuspids before bonding/banding <strong>the</strong><br />
lower arch.<br />
Upper cuspid teeth are retracted with power<br />
chains on .016 stainless steel arch wire. This<br />
procedure usually takes 6 to 8 months.<br />
Principle number 18 recommends that, in<br />
extraction cases, 17 treatment is delayed in <strong>the</strong><br />
mandibular arch to allow time for driftodontics<br />
(Fig 4). This is <strong>the</strong> term <strong>the</strong> author coined to<br />
describe <strong>the</strong> spontaneous unraveling <strong>of</strong> <strong>the</strong><br />
lower anterior teeth, making it much easier<br />
to place brackets after 4 to 6 months. When<br />
<strong>the</strong> upper cuspids have been retracted to a<br />
Class I relationship, <strong>the</strong> lower arch should be<br />
bonded/banded.<br />
Principle number 19 advises <strong>the</strong> use <strong>of</strong> a spe-<br />
cific retention plan ls,-~ incorporating retainer<br />
design, time sequence, and resolution <strong>of</strong> third<br />
molar teeth in an effort to ensure long-term<br />
stability. <strong>The</strong> upper "wrap-around" retainer wire<br />
is fabricated to a specific design and has proven<br />
to be extremely effective according to <strong>the</strong> au-<br />
thor. Also recommended is <strong>the</strong> fixed lower cus-<br />
pid-to-cuspid retainer design using an .0215 Tri-<br />
ple-Flex wire (Ormco, Glendora, CA) bonded to<br />
each tooth. After bracket removal, <strong>the</strong> upper<br />
retainer is worn only 8 to 10 hours per 24-hour<br />
period, being placed after dinner and removed<br />
<strong>the</strong> next morning. <strong>The</strong> patient is instructed not<br />
to wear it out <strong>of</strong> <strong>the</strong>ir home. <strong>The</strong> resulting re-<br />
duction <strong>of</strong> lost and broken retainers has been<br />
remarkable.<br />
Principle number 20 is "to work your plan."<br />
Although every case is unique in some ways,<br />
in many ways every case is also <strong>the</strong> same. <strong>The</strong><br />
general treatment plan in most cases as out-<br />
lined in <strong>the</strong>se principles is to treat <strong>the</strong> upper
66 Richard G. <strong>Alexander</strong><br />
Figure 4. Pretreatment mandibular occlusal view (A). Four months later, showing driftodontics (B).<br />
arch first by using a specific series <strong>of</strong> arch<br />
wires. If <strong>the</strong> case requires orthopedic correc-<br />
tion, it is initiated on <strong>the</strong> maxillary arch with<br />
an rapid palatal expander (RPE) and/or face<br />
bow or facemask. Approximately 6 months af-<br />
ter commencing maxillary arch treatment,<br />
treatment is initiated in <strong>the</strong> lower arch. A<br />
specific series <strong>of</strong> arch wires are used to posi-<br />
tion <strong>the</strong> mandibular teeth. After <strong>the</strong> finishing<br />
arch wires are in place, appropriate elastics are<br />
used to coordinate <strong>the</strong> arches and finalize <strong>the</strong><br />
occlusion. Retainers are <strong>the</strong>n placed.<br />
Following <strong>the</strong>se basic step-by-step procedures<br />
allows <strong>the</strong> clinician to control treatment<br />
progress. By being able to anticipate treatment<br />
objectives <strong>of</strong> <strong>the</strong> next appointment, future<br />
scheduling is simplified and treatment progress<br />
can be easily monitored so that <strong>the</strong> treatment<br />
can be completed on schedule.<br />
<strong>The</strong> ultimate objective is a well-treated pa-<br />
tient, completed in a timely fashion, with a sat-<br />
isfied patient, parents, and doctor.<br />
References<br />
1. <strong>Alexander</strong> RG, <strong>Alexander</strong> CM, <strong>Alexander</strong> C, et al. Cre-<br />
ating <strong>the</strong> compliant patient. J Clin Orthod 1996;30:493-<br />
497.<br />
2. Stroud J. <strong>The</strong> psychosocial effect <strong>of</strong> orthodontic treat-<br />
ment [master's <strong>the</strong>sis]. Dallas, TX: Baylor College <strong>of</strong><br />
Dentistry, 1996.<br />
3. AllenJ. As a man thinketh. Classics <strong>of</strong> inspiration. Kansas<br />
City, MO, Halhnark Cards, Inc, 1971, 57.<br />
4. Covey S. First things first. <strong>New</strong> <strong>York</strong>, Simon and Schus-<br />
ter, 1994, 287.<br />
5. Glenn G, Sinclair PM, <strong>Alexander</strong> RG. Non-extraction<br />
orthodontic <strong>the</strong>rapy: Post-treatment dental and skeletal<br />
stability. AmJ Orthod 1987;92:321-328.<br />
6. Ehns T. <strong>The</strong> long-term stability <strong>of</strong> class II, division 1,<br />
nonextraction cervical face-bow <strong>the</strong>rapy: Part 1, model<br />
analysis. AmJ Clin Orthod 1996;109:271-276.<br />
7. Elms T. <strong>The</strong> long-term stability <strong>of</strong> class II, division 1,<br />
nonextraction cervical face-bow <strong>the</strong>rapy: Part 2, cepha-<br />
lometric analysis. Am J Clin Orthod 1996;109:386-392.<br />
8. Nevant CT, Bnschang PH, <strong>Alexander</strong> RG, et al. Lip<br />
bumper <strong>the</strong>rapy for gaining arch length. Am J Orthod<br />
1991;100:330-336.<br />
9. <strong>Alexander</strong> JM. A comparative study <strong>of</strong> orthodontic sta-<br />
bility in class I extraction cases [master's <strong>the</strong>sis]. Dallas,<br />
TX: Baylor College <strong>of</strong> Dentistry, 1995.<br />
10. <strong>Alexander</strong> RG. Treatment and retention for long-term<br />
stability. In: Retention and stability in orthodontics. Phil-<br />
adelphia, W.B. Saunders, 1993.<br />
11. <strong>Alexander</strong> RG. <strong>The</strong> quest for long-term stability. In:<br />
Sachdeva R (ed). Orthodontics for <strong>the</strong> next millennium.<br />
Glendora, CA: Ormco, 1997.<br />
12. <strong>Alexander</strong> RG. A practical approach to arch form. Clin-<br />
ical Impressions 1992;1:3-5.<br />
13. <strong>Alexander</strong> RG. <strong>The</strong> <strong>Alexander</strong> <strong>Discipline</strong>. In: Engel GA<br />
(ed). Glendora, CA: Ormco, 1986.<br />
14. Bernstein R. Leveling <strong>the</strong> curve <strong>of</strong> Spee with a continu-<br />
ous archwire technique-a long-term cephalometric anal-<br />
ysis. Master's <strong>The</strong>sis, State <strong>University</strong> <strong>of</strong> <strong>New</strong> <strong>York</strong> at<br />
Buffalo, Buffalo, NY, January, 1999.<br />
15. <strong>Alexander</strong> RG. <strong>The</strong> <strong>Alexander</strong> <strong>Discipline</strong>. In: Engel GA<br />
(ed). Glendora, CA: Ormco, 1986, chap 7.<br />
16. <strong>Alexander</strong> RG. <strong>The</strong> <strong>Alexander</strong> <strong>Discipline</strong>. In: Engel GA<br />
(ed). Glendora, CA: Ormco, 1986, chap 9.<br />
17. <strong>Alexander</strong> RG. <strong>The</strong> <strong>Alexander</strong> <strong>Discipline</strong>. In: Engel GA<br />
(ed). Glendora, CA: Ormco, 1986, chap 10.<br />
18. <strong>Alexander</strong> RG. <strong>The</strong> <strong>Alexander</strong> <strong>Discipline</strong>. In: Engel GA<br />
(ed). Glendora, CA: Ormco, 1986, chap 14.<br />
19. <strong>Alexander</strong> RG. <strong>The</strong> vari-simplex discipline-part 4 count-<br />
down to retention. J Clin Orthod 1983;18:214-218.