Global Initiative for Chronic Obstructive Lung Disease - GOLD
Global Initiative for Chronic Obstructive Lung Disease - GOLD
Global Initiative for Chronic Obstructive Lung Disease - GOLD
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
<strong>GOLD</strong>_WR_05 8/18/05 12:56 PM Page 7<br />
surfaces of the lung (alveoli), is a pathological term that<br />
is often (but incorrectly) used clinically and describes<br />
only one of several structural abnormalities present in<br />
patients with COPD. <strong>Chronic</strong> bronchitis, or the presence<br />
of cough and sputum production <strong>for</strong> at least 3 months in<br />
each of two consecutive years, remains a clinically and<br />
epidemiologically useful term. However, it does not<br />
reflect the major impact of airflow limitation on morbidity<br />
and mortality in COPD patients. It is also important to<br />
recognize that cough and sputum production may precede<br />
the development of airflow limitation; conversely, some<br />
patients develop significant airflow limitation without<br />
chronic cough and sputum production.<br />
NATURAL HISTORY<br />
COPD has a variable natural history and not all individuals<br />
follow the same course. However, COPD is generally a<br />
progressive disease, especially if a patient's exposure<br />
to noxious agents continues. If exposure is stopped, the<br />
disease may still progress due to the decline in lung<br />
function that normally occurs with aging. Nevertheless,<br />
stopping exposure to noxious agents, even after<br />
significant airflow limitation is present, can result in<br />
some improvement in function and will certainly slow or<br />
even halt the progression of the disease.<br />
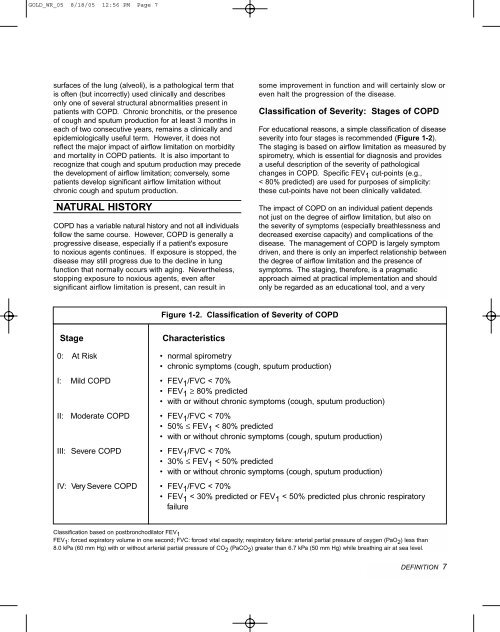
Classification of Severity: Stages of COPD<br />
For educational reasons, a simple classification of disease<br />
severity into four stages is recommended (Figure 1-2).<br />
The staging is based on airflow limitation as measured by<br />
spirometry, which is essential <strong>for</strong> diagnosis and provides<br />
a useful description of the severity of pathological<br />
changes in COPD. Specific FEV 1 cut-points (e.g.,<br />
< 80% predicted) are used <strong>for</strong> purposes of simplicity:<br />
these cut-points have not been clinically validated.<br />
The impact of COPD on an individual patient depends<br />
not just on the degree of airflow limitation, but also on<br />
the severity of symptoms (especially breathlessness and<br />
decreased exercise capacity) and complications of the<br />
disease. The management of COPD is largely symptom<br />
driven, and there is only an imperfect relationship between<br />
the degree of airflow limitation and the presence of<br />
symptoms. The staging, there<strong>for</strong>e, is a pragmatic<br />
approach aimed at practical implementation and should<br />
only be regarded as an educational tool, and a very<br />
Figure 1-2. Classification of Severity of COPD<br />
Stage<br />
Characteristics<br />
0: At Risk • normal spirometry<br />
• chronic symptoms (cough, sputum production)<br />
I: Mild COPD • FEV 1 /FVC < 70%<br />
• FEV 1 ≥ 80% predicted<br />
• with or without chronic symptoms (cough, sputum production)<br />
II: Moderate COPD • FEV 1 /FVC < 70%<br />
• 50% ≤ FEV 1 < 80% predicted<br />
• with or without chronic symptoms (cough, sputum production)<br />
III: Severe COPD • FEV 1 /FVC < 70%<br />
• 30% ≤ FEV 1 < 50% predicted<br />
• with or without chronic symptoms (cough, sputum production)<br />
IV: Very Severe COPD • FEV 1 /FVC < 70%<br />
• FEV 1 < 30% predicted or FEV 1 < 50% predicted plus chronic respiratory<br />
failure<br />
Classification based on postbronchodilator FEV 1<br />
FEV 1 : <strong>for</strong>ced expiratory volume in one second; FVC: <strong>for</strong>ced vital capacity; respiratory failure: arterial partial pressure of oxygen (PaO 2 ) less than<br />
8.0 kPa (60 mm Hg) with or without arterial partial pressure of CO 2 (PaCO 2 ) greater than 6.7 kPa (50 mm Hg) while breathing air at sea level.<br />
DEFINITION 7





![Di Bari [NO].pdf - GOLD](https://img.yumpu.com/21544924/1/190x143/di-bari-nopdf-gold.jpg?quality=85)










