Global Initiative for Chronic Obstructive Lung Disease - GOLD
Global Initiative for Chronic Obstructive Lung Disease - GOLD
Global Initiative for Chronic Obstructive Lung Disease - GOLD
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
<strong>GOLD</strong>_WR_05 8/18/05 12:56 PM Page 9<br />
SCOPE OF THE REPORT<br />
The focus of this Report is primarily on COPD caused by<br />
inhaled particles and gases, the most common of which<br />
worldwide is tobacco smoke. Poorly reversible airflow<br />
limitation associated with bronchiectasis, cystic fibrosis,<br />
tuberculosis, or asthma is not included except insofar as<br />
these conditions overlap with COPD.<br />
Asthma and COPD<br />
COPD can coexist with asthma, the other major chronic<br />
obstructive airway disease characterized by an underlying<br />
airway inflammation. Asthma and COPD have their major<br />
symptoms in common, but these are generally more<br />
variable in asthma than in COPD. The underlying chronic<br />
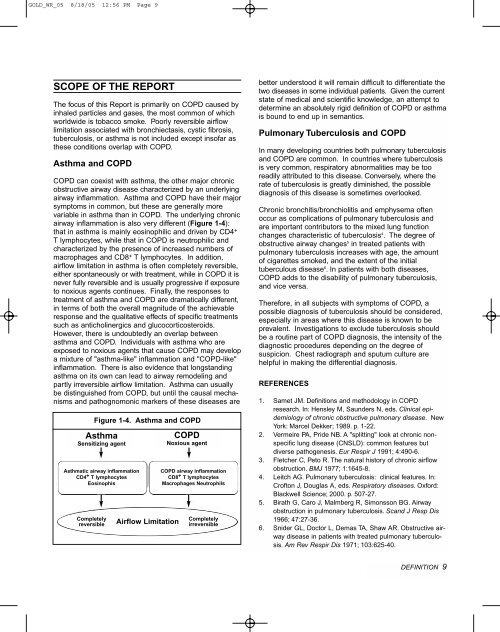
airway inflammation is also very different (Figure 1-4):<br />
that in asthma is mainly eosinophilic and driven by CD4 +<br />
T lymphocytes, while that in COPD is neutrophilic and<br />
characterized by the presence of increased numbers of<br />
macrophages and CD8 + T lymphocytes. In addition,<br />
airflow limitation in asthma is often completely reversible,<br />
either spontaneously or with treatment, while in COPD it is<br />
never fully reversible and is usually progressive if exposure<br />
to noxious agents continues. Finally, the responses to<br />
treatment of asthma and COPD are dramatically different,<br />
in terms of both the overall magnitude of the achievable<br />
response and the qualitative effects of specific treatments<br />
such as anticholinergics and glucocorticosteroids.<br />
However, there is undoubtedly an overlap between<br />
asthma and COPD. Individuals with asthma who are<br />
exposed to noxious agents that cause COPD may develop<br />
a mixture of "asthma-like" inflammation and "COPD-like"<br />
inflammation. There is also evidence that longstanding<br />
asthma on its own can lead to airway remodeling and<br />
partly irreversible airflow limitation. Asthma can usually<br />
be distinguished from COPD, but until the causal mechanisms<br />
and pathognomonic markers of these diseases are<br />
Figure 1-4. Asthma and COPD<br />
Asthma<br />
Sensitizing agent<br />
Asthmatic airway inflammation<br />
CD4 + T lymphocytes<br />
Eosinophis<br />
Completely<br />
reversible<br />
Airflow Limitation<br />
COPD<br />
Noxious agent<br />
COPD airway inflammation<br />
CD8 + T lymphocytes<br />
Macrophages Neutrophils<br />
Completely<br />
irreversible<br />
better understood it will remain difficult to differentiate the<br />
two diseases in some individual patients. Given the current<br />
state of medical and scientific knowledge, an attempt to<br />
determine an absolutely rigid definition of COPD or asthma<br />
is bound to end up in semantics.<br />
Pulmonary Tuberculosis and COPD<br />
In many developing countries both pulmonary tuberculosis<br />
and COPD are common. In countries where tuberculosis<br />
is very common, respiratory abnormalities may be too<br />
readily attributed to this disease. Conversely, where the<br />
rate of tuberculosis is greatly diminished, the possible<br />
diagnosis of this disease is sometimes overlooked.<br />
<strong>Chronic</strong> bronchitis/bronchiolitis and emphysema often<br />
occur as complications of pulmonary tuberculosis and<br />
are important contributors to the mixed lung function<br />
changes characteristic of tuberculosis 4 . The degree of<br />
obstructive airway changes 5 in treated patients with<br />
pulmonary tuberculosis increases with age, the amount<br />
of cigarettes smoked, and the extent of the initial<br />
tuberculous disease 6 . In patients with both diseases,<br />
COPD adds to the disability of pulmonary tuberculosis,<br />
and vice versa.<br />
There<strong>for</strong>e, in all subjects with symptoms of COPD, a<br />
possible diagnosis of tuberculosis should be considered,<br />
especially in areas where this disease is known to be<br />
prevalent. Investigations to exclude tuberculosis should<br />
be a routine part of COPD diagnosis, the intensity of the<br />
diagnostic procedures depending on the degree of<br />
suspicion. Chest radiograph and sputum culture are<br />
helpful in making the differential diagnosis.<br />
REFERENCES<br />
1. Samet JM. Definitions and methodology in COPD<br />
research. In: Hensley M, Saunders N, eds. Clinical epidemiology<br />
of chronic obstructive pulmonary disease. New<br />
York: Marcel Dekker; 1989. p. 1-22.<br />
2. Vermeire PA, Pride NB. A "splitting" look at chronic nonspecific<br />
lung disease (CNSLD): common features but<br />
diverse pathogenesis. Eur Respir J 1991; 4:490-6.<br />
3. Fletcher C, Peto R. The natural history of chronic airflow<br />
obstruction. BMJ 1977; 1:1645-8.<br />
4. Leitch AG. Pulmonary tuberculosis: clinical features. In:<br />
Crofton J, Douglas A, eds. Respiratory diseases. Ox<strong>for</strong>d:<br />
Blackwell Science; 2000. p. 507-27.<br />
5. Birath G, Caro J, Malmberg R, Simonsson BG. Airway<br />
obstruction in pulmonary tuberculosis. Scand J Resp Dis<br />
1966; 47:27-36.<br />
6. Snider GL, Doctor L, Demas TA, Shaw AR. <strong>Obstructive</strong> airway<br />
disease in patients with treated pulmonary tuberculosis.<br />
Am Rev Respir Dis 1971; 103:625-40.<br />
DEFINITION 9





![Di Bari [NO].pdf - GOLD](https://img.yumpu.com/21544924/1/190x143/di-bari-nopdf-gold.jpg?quality=85)










