Global Initiative for Chronic Obstructive Lung Disease - GOLD
Global Initiative for Chronic Obstructive Lung Disease - GOLD
Global Initiative for Chronic Obstructive Lung Disease - GOLD
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
<strong>GOLD</strong>_WR_05 8/18/05 12:56 PM Page 29<br />
time, inflammation damages the lungs and leads to the<br />
pathologic changes characteristic of COPD.<br />
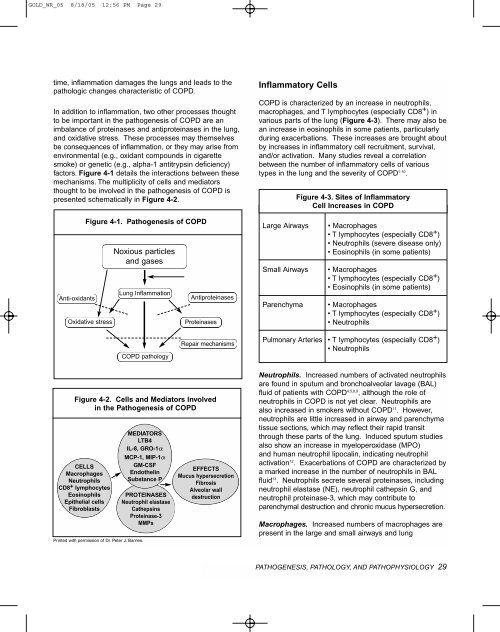
In addition to inflammation, two other processes thought<br />
to be important in the pathogenesis of COPD are an<br />
imbalance of proteinases and antiproteinases in the lung,<br />
and oxidative stress. These processes may themselves<br />
be consequences of inflammation, or they may arise from<br />
environmental (e.g., oxidant compounds in cigarette<br />
smoke) or genetic (e.g., alpha-1 antitrypsin deficiency)<br />
factors. Figure 4-1 details the interactions between these<br />
mechanisms. The multiplicity of cells and mediators<br />
thought to be involved in the pathogenesis of COPD is<br />
presented schematically in Figure 4-2.<br />
Inflammatory Cells<br />
COPD is characterized by an increase in neutrophils,<br />
macrophages, and T lymphocytes (especially CD8 + ) in<br />
various parts of the lung (Figure 4-3). There may also be<br />
an increase in eosinophils in some patients, particularly<br />
during exacerbations. These increases are brought about<br />
by increases in inflammatory cell recruitment, survival,<br />
and/or activation. Many studies reveal a correlation<br />
between the number of inflammatory cells of various<br />
types in the lung and the severity of COPD 1-10 .<br />
Figure 4-3. Sites of Inflammatory<br />
Cell Increases in COPD<br />
Anti-oxidants<br />
Figure 4-1. Pathogenesis of COPD<br />
Oxidative stress<br />
Noxious particles<br />
and gases<br />
<strong>Lung</strong> Inflammation<br />
Antiproteinases<br />
Proteinases<br />
Large Airways<br />
Small Airways<br />
Parenchyma<br />
• Macrophages<br />
• T lymphocytes (especially CD8 + )<br />
• Neutrophils (severe disease only)<br />
• Eosinophils (in some patients)<br />
• Macrophages<br />
• T lymphocytes (especially CD8 + )<br />
• Eosinophils (in some patients)<br />
• Macrophages<br />
• T lymphocytes (especially CD8 + )<br />
• Neutrophils<br />
COPD pathology<br />
Repair mechanisms<br />
Pulmonary Arteries • T lymphocytes (especially CD8 + )<br />
• Neutrophils<br />
Figure 4-2. Cells and Mediators Involved<br />
in the Pathogenesis of COPD<br />
CELLS<br />
Macrophages<br />
Neutrophils<br />
CD8 + lymphocytes<br />
Eosinophils<br />
Epithelial cells<br />
Fibroblasts<br />
Printed with permission of Dr. Peter J. Barnes.<br />
MEDIATORS<br />
LTB4<br />
IL-8, GRO-1<br />
MCP-1, MIP-1<br />
GM-CSF<br />
4<br />
Endothelin<br />
Substance P<br />
-1<br />
PROTEINASES<br />
Neutrophil elastase<br />
Cathepsins<br />
Proteinase-3<br />
MMPs<br />
EFFECTS<br />
Mucus hypersecretion<br />
Fibrosis<br />
Alveolar wall<br />
destruction<br />
Neutrophils. Increased numbers of activated neutrophils<br />
are found in sputum and bronchoalveolar lavage (BAL)<br />
fluid of patients with COPD 4,5,8,9 , although the role of<br />
neutrophils in COPD is not yet clear. Neutrophils are<br />
also increased in smokers without COPD 11 . However,<br />
neutrophils are little increased in airway and parenchyma<br />
tissue sections, which may reflect their rapid transit<br />
through these parts of the lung. Induced sputum studies<br />
also show an increase in myeloperoxidase (MPO)<br />
and human neutrophil lipocalin, indicating neutrophil<br />
activation 12 . Exacerbations of COPD are characterized by<br />
a marked increase in the number of neutrophils in BAL<br />
fluid 13 . Neutrophils secrete several proteinases, including<br />
neutrophil elastase (NE), neutrophil cathepsin G, and<br />
neutrophil proteinase-3, which may contribute to<br />
parenchymal destruction and chronic mucus hypersecretion.<br />
Macrophages. Increased numbers of macrophages are<br />
present in the large and small airways and lung<br />
PATHOGENESIS, PATHOLOGY, AND PATHOPHYSIOLOGY 29





![Di Bari [NO].pdf - GOLD](https://img.yumpu.com/21544924/1/190x143/di-bari-nopdf-gold.jpg?quality=85)










