Gait disorder in older adults: Is it NPH? - ResearchGate
Gait disorder in older adults: Is it NPH? - ResearchGate
Gait disorder in older adults: Is it NPH? - ResearchGate
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
<strong>Ga<strong>it</strong></strong> <strong>disorder</strong> <strong>in</strong> <strong>older</strong> <strong>adults</strong>: <strong>Is</strong> <strong>it</strong> <strong>NPH</strong>?<br />
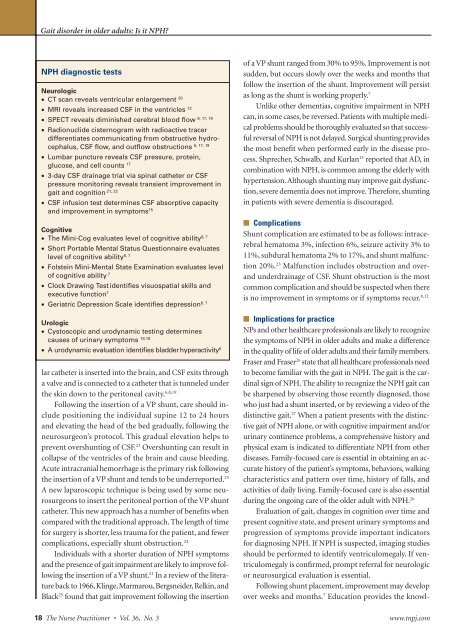
<strong>NPH</strong> diagnostic tests<br />
Neurologic<br />
• CT scan reveals ventricular enlargement 20<br />
• MRI reveals <strong>in</strong>creased CSF <strong>in</strong> the ventricles 12<br />
6, 17, 19<br />
• SPECT reveals dim<strong>in</strong>ished cerebral blood flow<br />
• Radionuclide cisternogram w<strong>it</strong>h radioactive tracer<br />
differentiates communicat<strong>in</strong>g from obstructive hydrocephalus,<br />
CSF flow, and outflow obstructions<br />
6, 17, 19<br />
• Lumbar puncture reveals CSF pressure, prote<strong>in</strong>,<br />
glucose, and cell counts 17<br />
• 3-day CSF dra<strong>in</strong>age trial via sp<strong>in</strong>al catheter or CSF<br />
pressure mon<strong>it</strong>or<strong>in</strong>g reveals transient improvement <strong>in</strong><br />
21, 22<br />
ga<strong>it</strong> and cogn<strong>it</strong>ion<br />
• CSF <strong>in</strong>fusion test determ<strong>in</strong>es CSF absorptive capac<strong>it</strong>y<br />
and improvement <strong>in</strong> symptoms 15<br />
Cogn<strong>it</strong>ive<br />
• The M<strong>in</strong>i-Cog evaluates level of cogn<strong>it</strong>ive abil<strong>it</strong>y 6, 7<br />
• Short Portable Mental Status Questionnaire evaluates<br />
level of cogn<strong>it</strong>ive abil<strong>it</strong>y 6, 7<br />
• Folste<strong>in</strong> M<strong>in</strong>i-Mental State Exam<strong>in</strong>ation evaluates level<br />
of cogn<strong>it</strong>ive abil<strong>it</strong>y 7<br />
• Clock Draw<strong>in</strong>g Test identifies visuospatial skills and<br />
executive function 7<br />
• Geriatric Depression Scale identifies depression 6, 7<br />
Urologic<br />
• Cystoscopic and urodynamic test<strong>in</strong>g determ<strong>in</strong>es<br />
causes of ur<strong>in</strong>ary symptoms 18,19<br />
• A urodynamic evaluation identifies bladder hyperactiv<strong>it</strong>y 8<br />
lar catheter is <strong>in</strong>serted <strong>in</strong>to the bra<strong>in</strong>, and CSF ex<strong>it</strong>s through<br />
a valve and is connected to a catheter that is tunneled under<br />
the sk<strong>in</strong> down to the per<strong>it</strong>oneal cav<strong>it</strong>y. 6,8,19<br />
Follow<strong>in</strong>g the <strong>in</strong>sertion of a VP shunt, care should <strong>in</strong>clude<br />
pos<strong>it</strong>ion<strong>in</strong>g the <strong>in</strong>dividual sup<strong>in</strong>e 12 to 24 hours<br />
and elevat<strong>in</strong>g the head of the bed gradually, follow<strong>in</strong>g the<br />
neurosurgeon’s protocol. This gradual elevation helps to<br />
prevent overshunt<strong>in</strong>g of CSF. 23 Overshunt<strong>in</strong>g can result <strong>in</strong><br />
collapse of the ventricles of the bra<strong>in</strong> and cause bleed<strong>in</strong>g.<br />
Acute <strong>in</strong>tracranial hemorrhage is the primary risk follow<strong>in</strong>g<br />
the <strong>in</strong>sertion of a VP shunt and tends to be underreported. 23<br />
A new laparoscopic technique is be<strong>in</strong>g used by some neurosurgeons<br />
to <strong>in</strong>sert the per<strong>it</strong>oneal portion of the VP shunt<br />
catheter. This new approach has a number of benef<strong>it</strong>s when<br />
compared w<strong>it</strong>h the trad<strong>it</strong>ional approach. The length of time<br />
for surgery is shorter, less trauma for the patient, and fewer<br />
complications, especially shunt obstruction. 24<br />
Individuals w<strong>it</strong>h a shorter duration of <strong>NPH</strong> symptoms<br />
and the presence of ga<strong>it</strong> impairment are likely to improve follow<strong>in</strong>g<br />
the <strong>in</strong>sertion of a VP shunt. 21 In a review of the l<strong>it</strong>erature<br />
back to 1966, Kl<strong>in</strong>ge, Marmarou, Bergsneider, Relk<strong>in</strong>, and<br />
Black 25 found that ga<strong>it</strong> improvement follow<strong>in</strong>g the <strong>in</strong>sertion<br />
of a VP shunt ranged from 30% to 95%. Improvement is not<br />
sudden, but occurs slowly over the weeks and months that<br />
follow the <strong>in</strong>sertion of the shunt. Improvement will persist<br />
as long as the shunt is work<strong>in</strong>g properly. 7<br />
Unlike other dementias, cogn<strong>it</strong>ive impairment <strong>in</strong> <strong>NPH</strong><br />
can, <strong>in</strong> some cases, be reversed. Patients w<strong>it</strong>h multiple medical<br />
problems should be thoroughly evaluated so that successful<br />
reversal of <strong>NPH</strong> is not delayed. Surgical shunt<strong>in</strong>g provides<br />
the most benef<strong>it</strong> when performed early <strong>in</strong> the disease process.<br />
Shprecher, Schwalb, and Kurlan 15 reported that AD, <strong>in</strong><br />
comb<strong>in</strong>ation w<strong>it</strong>h <strong>NPH</strong>, is common among the elderly w<strong>it</strong>h<br />
hypertension. Although shunt<strong>in</strong>g may improve ga<strong>it</strong> dysfunction,<br />
severe dementia does not improve. Therefore, shunt<strong>in</strong>g<br />
<strong>in</strong> patients w<strong>it</strong>h severe dementia is discouraged.<br />
■ Complications<br />
Shunt complication are estimated to be as follows: <strong>in</strong>tracerebral<br />
hematoma 3%, <strong>in</strong>fection 6%, seizure activ<strong>it</strong>y 3% to<br />
11%, subdural hematoma 2% to 17%, and shunt malfunction<br />
20%. 23 Malfunction <strong>in</strong>cludes obstruction and overand<br />
underdra<strong>in</strong>age of CSF. Shunt obstruction is the most<br />
common complication and should be suspected when there<br />
is no improvement <strong>in</strong> symptoms or if symptoms recur. 8,12<br />
■ Implications for practice<br />
NPs and other healthcare professionals are likely to recognize<br />
the symptoms of <strong>NPH</strong> <strong>in</strong> <strong>older</strong> <strong>adults</strong> and make a difference<br />
<strong>in</strong> the qual<strong>it</strong>y of life of <strong>older</strong> <strong>adults</strong> and their family members.<br />
Fraser and Fraser 26 state that all healthcare professionals need<br />
to become familiar w<strong>it</strong>h the ga<strong>it</strong> <strong>in</strong> <strong>NPH</strong>. The ga<strong>it</strong> is the card<strong>in</strong>al<br />
sign of <strong>NPH</strong>. The abil<strong>it</strong>y to recognize the <strong>NPH</strong> ga<strong>it</strong> can<br />
be sharpened by observ<strong>in</strong>g those recently diagnosed, those<br />
who just had a shunt <strong>in</strong>serted, or by review<strong>in</strong>g a video of the<br />
dist<strong>in</strong>ctive ga<strong>it</strong>. 27 When a patient presents w<strong>it</strong>h the dist<strong>in</strong>ctive<br />
ga<strong>it</strong> of <strong>NPH</strong> alone, or w<strong>it</strong>h cogn<strong>it</strong>ive impairment and/or<br />
ur<strong>in</strong>ary cont<strong>in</strong>ence problems, a comprehensive history and<br />
physical exam is <strong>in</strong>dicated to differentiate <strong>NPH</strong> from other<br />
diseases. Family-focused care is essential <strong>in</strong> obta<strong>in</strong><strong>in</strong>g an accurate<br />
history of the patient’s symptoms, behaviors, walk<strong>in</strong>g<br />
characteristics and pattern over time, history of falls, and<br />
activ<strong>it</strong>ies of daily liv<strong>in</strong>g. Family-focused care is also essential<br />
dur<strong>in</strong>g the ongo<strong>in</strong>g care of the <strong>older</strong> adult w<strong>it</strong>h <strong>NPH</strong>. 26<br />
Evaluation of ga<strong>it</strong>, changes <strong>in</strong> cogn<strong>it</strong>ion over time and<br />
present cogn<strong>it</strong>ive state, and present ur<strong>in</strong>ary symptoms and<br />
progression of symptoms provide important <strong>in</strong>dicators<br />
for diagnos<strong>in</strong>g <strong>NPH</strong>. If <strong>NPH</strong> is suspected, imag<strong>in</strong>g studies<br />
should be performed to identify ventriculomegaly. If ventriculomegaly<br />
is confirmed, prompt referral for neurologic<br />
or neurosurgical evaluation is essential.<br />
Follow<strong>in</strong>g shunt placement, improvement may develop<br />
over weeks and months. 7 Education provides the knowl-<br />
18 The Nurse Pract<strong>it</strong>ioner • Vol. 36, No. 3 www.tnpj.com<br />
Copyright © 2011 Lipp<strong>in</strong>cott Williams & Wilk<strong>in</strong>s. Unauthorized reproduction of this article is prohib<strong>it</strong>ed.