OPENING SESSION - ismrm
OPENING SESSION - ismrm
OPENING SESSION - ismrm
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
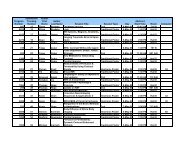
Monday AM<br />
14:24 91. Apparent Diffusion Coefficient Predicts Biochemical Response in Neuroendocrine<br />
Liver Metastases Treated Using Targeted Radiolabelled Therapy<br />
Dow-Mu Koh 1 , Keiko Miyazaki 2 , Matthew Orton 2 , Toni Wallace 1 , David J. Collins 2 ,<br />
Martin O. Leach 2 , Val Lewington 3<br />
1 Department of Radiology, Royal Marsden NHS Foundation Trust, Sutton, Surrey, United Kingdom; 2 CRUK-<br />
EPSRC Cancer Imaging Centre, Institute of Cancer Research, Sutton, Surrey, United Kingdom; 3 Department of<br />
Nuclear Medicine, Royal Marsden NHS Foundation Trust, Sutton, Surrey, United Kingdom<br />
We investigated diffusion-weighted MR imaging (DW-MRI) for assessing treatment response of liver metastases of neuroendocrine<br />
origin to targeted radiolabelled therapy 90Y-DOTATOC. The quantitative apparent diffusion coefficient (ADC) appears to be a<br />
promising response and prognostic biomarker. Responders were found to have a lower pre-treatment value compared with nonresponders;<br />
and also demonstrated a significant increase in ADC at 2 months after the first cycle of treatment. Response defined by<br />
ADC changes also showed good agreement with biochemical response.<br />
14:36 92. Diffusion-Weighted MR Imaging of Pulmonary Lesions: Effectiveness of Apparent<br />
Diffusion Coefficient Quantification and Lesion-To-Spinal Cord Signal Intensity Ratio in the<br />
Lesion Characterization<br />
Nevzat Karabulut 1 , Vefa Çakmak 1<br />
1 Radiology, Pamukkale University, School of Medicine, Denizli, Turkey<br />
Diffusion-weighted imaging (DWI) of lung is a useful adjunct to conventional chest MR imaging sequences improving lesion<br />
characterization. Differentiation of malignant tumors from benign lesions can be achieved using apparent diffusion coefficient (ADC)<br />
quantification and lesion-to-spinal cord signal intensity ratio (LSR). Due to increased cellularity and less extracellular space impeding<br />
the water diffusion, malignant tumors tend to have reduced ADC and increased LSR. Our results show that ADC quantification is<br />
more accurate than LSR for the differentiation of lung lesions. Because DWI is a non-invasive technique improving lesion<br />
characterization, it should be incorporated into routine chest MR imaging protocols.<br />
14:48 93. Improving IVIM Derived F-Maps of Pancreatic Tumors with Automatic Duct and<br />
Vessel Segmentation<br />
Thomas Joseph Re 1,2 , Mirium Klauss 3 , Andreas Lemke 4 , Frederik B. Laun 2 , Dirk Simon 5 ,<br />
Riccardo Manfredi 1 , Roberto Pozzi Mucelli 1 , Stefan Delorme 2 , Bram Stieltjes 2<br />
1 Radiology, University of Verona, Verona, Italy; 2 Radiology, DKFZ, Heidelberg, BW, Germany; 3 Radiology,<br />
University of Heidelberg, Heidelberg, BW, Germany; 4 MS Computer Assisted Clinical Medicine, University of<br />
Heidelberg; 5 Software Development for Integrated Diagnostics and Therapy, DKFZ, Heidelberg, BW, Germany<br />
Maps of IVIM model derived perfusion fraction f (f-maps) of the pancreas show potential for the identification of pancreatic<br />
adenocarcinoma lesions which appear hypointense in these images. Unfortunately, since bile and pancreatic ducts also appear as<br />
hypointense in f-maps, their presence adjacent to tumors can lead to tumor delineation errors. A novel approach which automatically<br />
segmented vessels and ducts in the f-maps based on integrated diffusion coefficient D data was tested in 43 patients and proved to be<br />
superior to both the ADC or f-map for tumor delineation.<br />
15:00 94. Higher Pre-Treatment Apparent Diffusion Coefficient Predicts Poorer Disease<br />
Survival in Patients with Colorectal Hepatic Metastasis<br />
Henry Ho Ching Tam 1 , David J. Collins 2 , Gina Brown 1 , Ian Chau 3 , David Cunningham 3 ,<br />
Martin O. Leach 2 ,<br />
Dow-Mu Koh 1<br />
1 Department of Radiology, Royal Marsden NHS Foundation Trust, Sutton, Surrey, United Kingdom; 2 CRUK-<br />
EPSRC Cancer Imaging Centre, Institute of Cancer Research, Sutton, Surrey, United Kingdom; 3 Department of<br />
Medical Oncology (Gastrointestinal), Royal Marsden NHS Foundation Trust, Sutton, Surrey, United Kingdom<br />
We report the use of DW-MRI for assessing response to chemotherapy and long-term outcome in patients with colorectal hepatic<br />
metastasis. Non-responders were found to have a higher pre-treatment apparent diffusion coefficient (ADC). High pre-treatment ADC<br />
was also associated with a shorter progression free survival time, independent of response to chemotherapy and other prognostic<br />
factors. This study demonstrates the potential of DW-MRI as a biologically relevant response and prognostic biomarker.<br />
15:12 95. Value of Diffusion Weighted Imaging (DWI) as an Early Imaging Biomarker for<br />
Prediction of Therapy Effect in Patients with Colorectal Metastases Following Selective<br />
Internal Radiotherapy (SIRT)<br />
Martin Zeile 1 , Christian Wybranski 1 , David Loewenthal 1 , Maciej Pech 1 , Frank<br />
Fischbach 1 , Ricarda Ruehl 1 , Holger Amthauer 1 , Jens Ricke 1 , Oliver Dudeck 1<br />
1 Clinic for Radiology and Nuclear Medicine, University Clinic Magdeburg, Magdeburg, 39120, Germany<br />
Clinical studies revealed the potential of diffusion weighted imaging (DWI) as a biomarker for predicting tumor response. 41<br />
colorectal liver metastases in 18 patients who underwent SIRT were examined before, 1 to 3 days after and 6 weeks following<br />
radioembolization by MRI including DWI. Lesions were categorized in responding (RL) and non-responding (NRL) according to<br />
change in tumor volume after 6 weeks. On early MRI, NRL showed no change in apparent diffusion coefficient (ADC), while a