Community Health Needs Assessment 2012 - Saint Joseph Hospital
Community Health Needs Assessment 2012 - Saint Joseph Hospital
Community Health Needs Assessment 2012 - Saint Joseph Hospital
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
<strong>Community</strong> <strong>Health</strong> <strong>Needs</strong><br />
<strong>Assessment</strong><br />
FY 2013
<strong>Community</strong> <strong>Health</strong> <strong>Needs</strong> <strong>Assessment</strong> 2013<br />
Contents<br />
Introduction ...........................................................................................................................1<br />
Executive Summary .................................................................................................................... 1<br />
Organization Description ........................................................................................................... 3<br />
How the <strong>Assessment</strong> was Conducted...................................................................................6<br />
<strong>Community</strong> Served by the <strong>Hospital</strong> ....................................................................................7<br />
Identification and Description of Geographical <strong>Community</strong> .................................................. 7<br />
Defined <strong>Community</strong> or Service Area ......................................................................................... 7<br />
<strong>Community</strong> Population and Demographics ............................................................................. 10<br />
Socioeconomic Characteristics of the <strong>Community</strong> ................................................................. 11<br />
Income, Poverty and Unemployment .................................................................................. 11<br />
Uninsured Status ................................................................................................................. 12<br />
Education............................................................................................................................. 12<br />
<strong>Community</strong> <strong>Health</strong> Care Resources ........................................................................................ 14<br />
<strong>Hospital</strong>s .............................................................................................................................. 14<br />
Ambulatory Care Clinics ..................................................................................................... 15<br />
Other Licensed Facilities ..................................................................................................... 15<br />
<strong>Health</strong> Departments ............................................................................................................. 15<br />
<strong>Health</strong> Status of the <strong>Community</strong> .......................................................................................16<br />
Leading Causes of Death .......................................................................................................... 17<br />
Primary <strong>Health</strong> Conditions Responsible for Inpatient <strong>Hospital</strong>ization ............................... 18<br />
<strong>Health</strong> Outcomes and Factors............................................................................................ 19<br />
<strong>Health</strong> Statistics and Rankings ................................................................................................ 19<br />
Primary Data .......................................................................................................................22<br />
<strong>Community</strong> Input-Surveys ....................................................................................................... 22<br />
<strong>Community</strong> Input-Focus Group and Interview Results ........................................................ 27<br />
Key Themes Provided Through Participant Comments ...................................................... 29<br />
<strong>Health</strong> Issues of Uninsured Persons, Low-Income Persons<br />
and Minority Groups .................................................................................................... 29
<strong>Community</strong> <strong>Health</strong> <strong>Needs</strong> <strong>Assessment</strong> 2013<br />
Contents (continued)<br />
Children at Risk................................................................................................................... 31<br />
Key Themes Provided Through Participant Comments ...................................................... 31<br />
Key Themes Provided Through Participant Comments ...................................................... 29<br />
Violence in the <strong>Community</strong> ...................................................................................................... 32<br />
Priority <strong>Community</strong> <strong>Health</strong> <strong>Needs</strong> Identified ..................................................................33<br />
Appendices ..................................................................................................................................... 37<br />
Appendix A: <strong>Saint</strong> <strong>Joseph</strong> Berea CHNA Advisory Committees<br />
Appendix B: CHNA Timeline<br />
Appendix C: <strong>Saint</strong> <strong>Joseph</strong> Berea CHNA Survey Tool<br />
Appendix D: Summary of SJB CHNA Survey, Focus Groups and Interview Results<br />
Appendix E: CHNA <strong>Community</strong> Analysis and Evaluation Meeting<br />
Appendix F: Acknowledgements – May need to put steering committee here<br />
Appendix G: Sources
<strong>Community</strong> <strong>Health</strong> <strong>Needs</strong> <strong>Assessment</strong> 2013<br />
Introduction<br />
During <strong>2012</strong>, a community health needs assessment was conducted by <strong>Saint</strong> <strong>Joseph</strong> Berea to support its<br />
mission to enhance the health of people in the communities it serves, to comply with the Patient Protection<br />
and Affordable Care Act of 2010 and federal tax-exemption requirements, and to identify health needs of<br />
the community to help prioritize the allocation of hospital resources to meet those needs. Based on current<br />
literature and other guidance from the Treasury and IRS, the following steps were completed as part of the<br />
community health needs assessment:<br />
The ―community‖ served by was defined utilizing inpatient and outpatient data on patient origin.<br />
This process is further described in <strong>Community</strong> Served by the <strong>Hospital</strong>.<br />
Population demographics and socioeconomic characteristics of the community were gathered and<br />
reported using various sources (See Appendix G). The health status of the community was then<br />
reviewed. Information on the leading causes of death and morbidity information was analyzed in<br />
conjunction with health outcomes and factors reported for the community by County<strong>Health</strong>rankings.org.<br />
<strong>Health</strong> factors with significant opportunity for improvement were noted.<br />
An inventory of health care facilities and resources was prepared.<br />
Through a collaborative process conducted by <strong>Saint</strong> <strong>Joseph</strong> Berea with the Madison County<br />
<strong>Health</strong> Department, the Kentucky <strong>Hospital</strong> Association and the University of Kentucky, community<br />
input was obtained through a community survey, a series of six focus groups and six key informant<br />
interviews..<br />
Information gathered in the steps above was analyzed and reviewed to identify health issues of uninsured<br />
persons, low-income persons and minority groups and the community as a whole. <strong>Health</strong> needs were prioritized<br />
utilizing a method that weighs: 1) the ability to evaluate outcomes; 2) the size of the problem; 3)<br />
the seriousness of the problem; 4) prevalence of common themes; 5) how closely the need aligns with the<br />
strategies and strengths of the hospital and KentuckyOne <strong>Health</strong>; and 6) an evaluation of existing hospital<br />
programs responding to the identified need. Information gaps were identified during the prioritization<br />
process and reported.<br />
Executive Summary<br />
<strong>Saint</strong> <strong>Joseph</strong> Berea conducted the required <strong>Community</strong> <strong>Health</strong> <strong>Needs</strong> <strong>Assessment</strong> in FY12 –FY13 to further<br />
assist the hospital in understanding the health needs of the community and how it can address those<br />
needs, recognizing that some things are beyond its capacity. The hospital worked in collaboration with the<br />
Madison County <strong>Health</strong> Department, local businesses, community groups, churches, city and county agencies,<br />
local physicians and hospital leadership to fulfill the requirements of the assessment. Primary data<br />
made available through a health needs assessment survey, focus groups and key informant interviews was<br />
collected and compiled giving a perspective on what the community sees as primary health needs and<br />
possible solutions. Secondary data from local, state and federal sources was compiled from information on<br />
disease prevalence, health indicators, health equity and mortality.<br />
Page 1
<strong>Community</strong> <strong>Health</strong> <strong>Needs</strong> <strong>Assessment</strong> 2013<br />
Identified needs were prioritized utilizing a method that weighs: 1) the impact on vulnerable populations;<br />
2) the importance to the community; 3) the size of the problem; 4) the seriousness of the problem; 5) prevalence<br />
of common themes; 6) how closely the need aligns with the strategies and strengths of the hospital<br />
and KentuckyOne <strong>Health</strong>; and 7) an evaluation of existing hospital programs responding to the identified<br />
need. by a community advisory group and given to the hospital steering committee for review. Once the<br />
primary health issues in the community were identified, <strong>Saint</strong> <strong>Joseph</strong> Berea went through the process of<br />
grouping and identifying the health priorities to be addressed.<br />
The top five priorities include:<br />
o Mental health – including, but not limited to alcohol/drug abuse, depression/anxiety, mental/behavioral<br />
health problems, suicide…<br />
o Obesity – specifically, nutrition and physical activity…<br />
o Cardiopulmonary – heart disease/stroke, high blood pressure, pulmonary…<br />
o Senior issues – physical issues connected with aging, Alzheimer’s/dementia, resources…<br />
o Collaboration of care - pulling community resources/groups together to address common health issues<br />
and concerns…<br />
<strong>Saint</strong> <strong>Joseph</strong> Berea is grateful to the community members who collaborated with us in completing this<br />
community health needs assessment. This is an active community that truly wants to better the health of<br />
those who live here.<br />
Page 2
<strong>Community</strong> <strong>Health</strong> <strong>Needs</strong> <strong>Assessment</strong> 2013<br />
Organization Description<br />
<strong>Saint</strong> <strong>Joseph</strong> Berea, formerly Berea <strong>Hospital</strong>, began in 1898, as an eight-bed cottage on the Berea College<br />
campus in Berea, Kentucky. Now a 25-bed facility, <strong>Saint</strong> <strong>Joseph</strong> - Berea provides health care to residents<br />
in Madison, Jackson, Rockcastle and Garrard Counties. Berea is located in Madison County and according<br />
to the <strong>2012</strong> County <strong>Health</strong> Rankings, it is the 20 th healthiest county of Kentucky’s 120 counties. On April<br />
1, 2003, Berea <strong>Hospital</strong> joined Catholic <strong>Health</strong> Initiatives, one of the largest Catholic health care systems<br />
in the U.S. In November of 2005, the hospital consolidated with <strong>Saint</strong> <strong>Joseph</strong> <strong>Health</strong>Care Kentucky (becoming<br />
<strong>Saint</strong> <strong>Joseph</strong> <strong>Health</strong> System in Lexington in 2007), taking a new name – <strong>Saint</strong> <strong>Joseph</strong> Berea. And<br />
in December 2011, <strong>Saint</strong> <strong>Joseph</strong> <strong>Health</strong> System became part of KentuckyOne <strong>Health</strong>, maintaining the<br />
Catholic legacy and original mission of the hospital to bring quality health care to the Appalachian communities<br />
that it serves regardless of their race, creed or ability to pay.<br />
<strong>Saint</strong> <strong>Joseph</strong> Berea is a critical access hospital, which serves over 19,000 families. The hospital is known<br />
for providing excellence of care while utilizing advanced medical technology in a friendly, family-like atmosphere.<br />
Competence, commitment and dedication are the hallmarks of <strong>Saint</strong> <strong>Joseph</strong> Berea, which is licensed<br />
by The Joint Commission on Accreditation of <strong>Health</strong>care Organizations and the Kentucky Cabinet<br />
of <strong>Health</strong> Services. Memberships in the American and<br />
Kentucky <strong>Hospital</strong> Associations are also held. Since joining<br />
the Catholic <strong>Health</strong> Initiatives (CHI) system, <strong>Saint</strong><br />
<strong>Joseph</strong> Berea has adopted CHI’s mission and core values.<br />
With a full complement of inpatient and outpatient services,<br />
<strong>Saint</strong> <strong>Joseph</strong> Berea is committed to providing the<br />
highest quality of care at a reasonable cost in a personal<br />
and compassionate family-oriented environment. Through<br />
provision of a broad range of hospital and community<br />
services <strong>Saint</strong> <strong>Joseph</strong> Berea works with an extensive<br />
medical staff of primary care physicians and specialists to<br />
deliver services and programs that embrace superior value<br />
and integrity.<br />
Services include a fully staffed 24 hour emergency department that treats more than 22,000 patients a year.<br />
The emergency department also trains for disaster preparedness annually with the federal governments<br />
Chemical Stockpile Emergency Preparedness Program (CSEPP) and has a 24/7 Sexual Assault Nurse Examiner<br />
(SANE) program. Services also include acute and intensive care; general surgery; outpatient surgical<br />
services; physical, occupational and speech therapy; diabetes treatment; diagnostic services including<br />
MRI, radiology and nuclear medicine; outpatient laboratory; cardiopulmonary services, and oncology services.<br />
Specialty clinics include services in cardiology, gynecology, neurology, psychology, orthopedics,<br />
oncology, ophthalmology, pulmonary, ENT/Hearing Tests, podiatry and cardiothoracic surgery.<br />
Special departments of the hospital are Berea Family Medicine (a designated rural health care clinic),<br />
Breast Center, Berea Specialty Clinic, Diabetes and Nutrition Center, Cardiovascular Services through the<br />
<strong>Saint</strong> <strong>Joseph</strong> Berea Heart Institute, Senior Renewal Center, Sleep Wellness Center, Surgical Services, Pain<br />
Management Clinic, MedWorks and Wound Care Center.<br />
Page 3
<strong>Community</strong> <strong>Health</strong> <strong>Needs</strong> <strong>Assessment</strong> 2013<br />
<strong>Community</strong> involvement and partnerships are very important to <strong>Saint</strong> <strong>Joseph</strong> Berea. The hospital has a<br />
close relationship with the Madison County <strong>Health</strong> Department, local government, businesses, civic organizations,<br />
educational systems and community agencies. This includes Bowl for Kids’ Sake, Relay for Life,<br />
A Day of Hope, hosting the Berea Farmers’ Market, Spoonbread Festival, blood drives, medical screenings<br />
and health fairs. Lights for Life is a community and employee supported program that provides prescription<br />
assistance and other medical supplies if there is a need when they are discharged from the hospital.<br />
Henrietta Childs fund provides assistance for uninsured Berea residents who need to have a small procedure<br />
but do not have the means to pay. Each year the hospital hosts Get <strong>Health</strong>y Berea, an event coordinated<br />
with local schools and businesses to promote health and wellness. Medical staff volunteers for<br />
Surgery on Sunday, a program for patients who do not have insurance or the means to pay for needed surgical<br />
procedures. All medical staff volunteer their time for this program. It is also a clinical site for Eastern<br />
Kentucky University, Somerset, University of Kentucky and Berea College for students who need clinical<br />
hours in a variety of medical professions including Nursing, Emergency Room, <strong>Health</strong> Information, Pharmacy,<br />
Pulmonary, Lab and Radiology.<br />
Another important community relationship is the volunteer services provided at <strong>Saint</strong> <strong>Joseph</strong> Berea. The<br />
volunteers not only run the gift shop, greet visitors, provide information and assist as needed, they support<br />
hospital programs such as providing a gift bag to all oncology patients who come to their first chemotherapy<br />
treatment and providing items for the patient clothing closet. Two large projects they have helped us<br />
with includes paying to seal and re-stripe the front parking lot to promote safety for visitors and purchasing<br />
a Cholestech machine that will enable us to provide more thorough community health screenings.<br />
<strong>Saint</strong> <strong>Joseph</strong> Berea <strong>Hospital</strong> is part of KentuckyOne <strong>Health</strong>, the largest health system in Kentucky with<br />
more than 200 locations including hospitals, outpatient facilities and physician offices, and more than<br />
3,100 licensed beds. An 18-member volunteer board of directors governs KentuckyOne <strong>Health</strong>, its facilities<br />
and operations, including <strong>Saint</strong> <strong>Joseph</strong> Berea <strong>Hospital</strong>, with this mission:<br />
Our Purpose<br />
To bring wellness, healing and hope to all, including the underserved.<br />
Our Future<br />
To transform the health of communities, care delivery and health care professions so that individuals and<br />
families can enjoy the best of health and wellbeing.<br />
Our Values<br />
Reverence: Respecting those we serve and those who serve.<br />
Integrity: Doing the right things in the right way for the right reason.<br />
Compassion: Sharing in others’ joys and sorrows.<br />
Excellence: Living up to the highest standards.<br />
Page 4
<strong>Community</strong> <strong>Health</strong> <strong>Needs</strong> <strong>Assessment</strong> 2013<br />
How the <strong>Assessment</strong> was Conducted<br />
<strong>Saint</strong> <strong>Joseph</strong> Berea collaborated with the Madison County <strong>Health</strong> Department, the Kentucky <strong>Hospital</strong> Association<br />
and local community groups to conduct the <strong>Community</strong> <strong>Health</strong> <strong>Needs</strong> <strong>Assessment</strong> (CHNA). An<br />
advisory committee consisting of representatives from the Madison County <strong>Health</strong> Department, Berea College,<br />
Senior Citizens, HeadStart, Union Church, St. Clare’s Catholic Church, Madison County Schools,<br />
Berea Police Department, White House Clinic and hospital leadership and staff began meeting in January<br />
<strong>2012</strong> to decide how the assessment would be conducted and what it would consist of. See Appendix B for<br />
CHNA Timeline.<br />
Once the primary service area was determined a survey was sent to random households inviting individuals<br />
to complete and return to <strong>Saint</strong> <strong>Joseph</strong> Berea. The survey covered a broad range of topics from access<br />
to health care to perception about the most pressing health care needs and recommendations. The survey<br />
was also available online. It was available in English and Spanish. The survey was conducted from September<br />
1 – November 9, <strong>2012</strong>. There were a total of 949 respondents. No one responded in Spanish. 74%<br />
were from Madison County: 43% of which were from Berea and 29% from Richmond, 8% from Jackson<br />
County, 6% from Rockcastle County and 6% from Garrard County. The majority of the respondents were<br />
female (67%). The most responses were from the 65+ (31%) age group; second, 40-54 (26%); third was<br />
55-64 (25%) and the under 26 groups were 18%. The majority of respondents were Caucasian (96%). Only<br />
3% were African American; 1% was Native American; less than 1% was Hispanic; 1% was of other ethnicities.<br />
The information on race closely corresponds to that of Madison County (2011 MCCHIP). See Appendix<br />
C for Survey Tool.<br />
Six focus groups were conducted with different community groups to seek their input on the health care<br />
needs of the community.<br />
Senior Citizen Advisory Group<br />
Berea Head Start Center with parents and administrator<br />
Shannon Johnson Elementary Teachers<br />
St <strong>Joseph</strong> Berea employees/volunteers<br />
First Responders group with EMS, Fire and Police departments<br />
Farristown Baptist Church event with community members<br />
There was a total of 61 participants plus facilitators. The focus groups were held from October 3 through<br />
November 16.The groups represented a broad spectrum of the community including African American,<br />
business, first responders, religious community, education, lower income, various age groups, caregivers<br />
and those with medical needs.<br />
Six interviews were conducted with physicians, community leaders, business and community members.<br />
We thought this would be a more personal approach. The responses were similar to the focus groups but<br />
with a little more detail. See Appendix D for survey, focus group and interview questions and results.<br />
In addition, secondary data from local, state and federal sources was compiled from demographic and socioeconomic<br />
sources from information on disease prevalence, health indicators, health equity and mortality.<br />
Identified needs were prioritized through that process and presented to hospital administration for<br />
review.<br />
Page 5
<strong>Community</strong> <strong>Health</strong> <strong>Needs</strong> <strong>Assessment</strong> 2013<br />
<strong>Community</strong> Served by the <strong>Hospital</strong><br />
Identification and Description of Geographical <strong>Community</strong><br />
Berea, population 13,561 (2010), is located in Madison County, Kentucky. Berea is only 40 miles south of<br />
Lexington, KY and 15 miles from Richmond, KY. Incorporated in 1890, Berea was named in 1854 by<br />
Rev. John Fee for the town mentioned in Acts 17:10 where the inhabitants ―received the word with all eagerness‖<br />
and at that time opposed slavery (in a slave state); a commitment which has evolved today into<br />
broad support for human equality. The town is known for Berea College, with its commitment to interracial<br />
co-education and service to the Appalachian Region. Berea is the ―Folk Arts and Crafts Capital of<br />
Kentucky- Where Art’s Alive.‖ Berea hosts the headquarters of the Kentucky Guild of Artists and<br />
Craftsmen-50 years old in 2011, the Kentucky Artisan Center, along with a colony of studio artists; its employment<br />
base includes over 3,500 jobs in manufacturing. Berea has a pedestrian-friendly culture supported<br />
by miles of bike trails, sidewalks and regularly held 5K-walks and 10K-runs.<br />
Madison County’s population density is just over 187 people per square mile. A little more than half of the<br />
residents can be found in Richmond (31,364 residents), which is the county seat, and in Berea (13,561)<br />
with approximately 38,000 living in many of Madison County’s unincorporated communities including<br />
Waco, paint Lick, Boonesboro, Bighill, Bybee, Kirksville, Round Hill, Union City and Valley View or in<br />
the more rural farming areas.<br />
Interstate 75 bisects Madison County from North to South, running through Richmond and Berea. Berea is<br />
located 33 miles south of Lexington (second largest city in Kentucky), 114 miles south of Louisville (largest<br />
city in Kentucky), 119 miles south of Cincinnati, Ohio and 134 miles north of Knoxville, Tennessee.<br />
Interstate 75 brings travelers to the community of Berea because of its cultural contributions. The interstate<br />
also brings travelers to <strong>Saint</strong> <strong>Joseph</strong> Berea who fall ill or are in accidents while passing through the area.<br />
(http://bereaky.gov/for-visitors/community-profile)/<br />
Defined <strong>Community</strong> or Service Area<br />
A community is defined as the geographic area from which a significant number of the patients utilizing<br />
hospital services reside. While the community health needs assessment considers other types of health<br />
care providers, hospitals are the single largest provider of acute care services. For this reason, the utilization<br />
of hospital services provides the clearest definition of the community.<br />
<strong>Saint</strong> <strong>Joseph</strong> Berea primary service area was identified based on the patient origin of inpatient discharges<br />
by zip code from July 1, 2011 to June 30, <strong>2012</strong> (See Exhibit 1). <strong>Saint</strong> <strong>Joseph</strong> Berea defines its community<br />
for this community health needs assessment based on where the majority of its inpatients reside. It is<br />
followed by a map showing <strong>Saint</strong> <strong>Joseph</strong> Berea’s geographic location and the footprint of <strong>Saint</strong> <strong>Joseph</strong><br />
Berea primary service area identified in Exhibit 1 which includes Madison, Jackson, Rockcastle and Garrard<br />
Counties. A demographic snapshot for these zip codes is provided in Exhibit 2 and displays the hospital’s<br />
defined primary service area, identifies the zip codes that comprise this community, and illustrates<br />
its geographic relationship to surrounding counties.<br />
When specific information is not available by zip code, this community health needs assessment relies on<br />
county-level data.<br />
Page 6
<strong>Community</strong> <strong>Health</strong> <strong>Needs</strong> <strong>Assessment</strong> 2013<br />
Because over 63 percent of <strong>Saint</strong> <strong>Joseph</strong> Berea’s discharges originate in Madison County, it collaborated<br />
with the Madison County <strong>Health</strong> Department in conducting its community health needs assessment.<br />
Jackson, Rockcastle and Garrard Counties are also served by served by <strong>Saint</strong> <strong>Joseph</strong> Berea but in a much<br />
smaller capacity.<br />
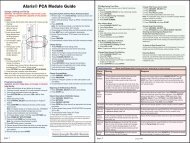
Exhibit 1<br />
<strong>Saint</strong> <strong>Joseph</strong> Berea CHNA <strong>Community</strong><br />
Summary of Inpatient Discharges by Zip Code (Descending Order)<br />
7/1/11 – 6/30/12<br />
Zip Code City County Discharges<br />
% of Total Discharges<br />
40403 Berea Madison 625 51.1%<br />
40447 McKee Jackson 172 14.1%<br />
40456 Mt. Vernon Rockcastle 66 5.4%<br />
40461 Paint Lick Garrard 59 4.8%<br />
40475 Richmond Madison 126 10.3%<br />
40481 Sandgap Jackson 38 3.1%<br />
The <strong>Community</strong> <strong>Needs</strong> Index (CNI) identifies the severity of health disparity for every zip code in the<br />
United States and demonstrates the link between community need, access to care, and preventable hospitalizations.<br />
The CNI uses research, literature and experiential evidence to identify top five prominent barriers<br />
that enables them to quantify health care access in communities across the nation. These barriers include<br />
those related to income, culture/language, education, insurance, and housing. Using this data a score is assigned<br />
to each barrier condition (with 1 representing less community need and 5 representing more community<br />
need). The scores are then aggregated and averaged for a final CNI score (each barrier receives<br />
equal weight in the average). A score of 1.0 indicates a zip code with the lowest socio-economic barriers,<br />
while a score of 5.0 represents a zip code with the most socio-economic barriers.<br />
The CNI for <strong>Saint</strong> <strong>Joseph</strong> Berea’s service area is presented in Exhibit 2 on the following page.<br />
Page 7
<strong>Community</strong> <strong>Health</strong> <strong>Needs</strong> <strong>Assessment</strong> 2013<br />
Exhibit 2<br />
<strong>Saint</strong> <strong>Joseph</strong> Berea CHNA <strong>Community</strong><br />
CNI <strong>Health</strong> Disparities<br />
Source: http://www.dignityhealth.org/Who_We_Are/<strong>Community</strong>_<strong>Health</strong>/212401<br />
Page 8
<strong>Community</strong> <strong>Health</strong> <strong>Needs</strong> <strong>Assessment</strong> 2013<br />
<strong>Community</strong> Population and Demographics<br />
<strong>Saint</strong> <strong>Joseph</strong> Berea’s primary service area is comprised of four counties: Madison, Jackson, Rockcastle and<br />
Garrard, but since approximately 63% of the hospital’s discharges come from Madison County, our focus<br />
for this report will be on Madison County. Exhibit 3 shows demographics and socioeconomic characteristics<br />
of <strong>Saint</strong> <strong>Joseph</strong> Berea’s primary service area for the most recent period available.<br />
Madison County is one of Kentucky’s fastest growing areas. According to the 2010 US Census, the population<br />
of Madison County was 82,916, a 17% increase over its 2000 population count. Berea is the third<br />
fastest growing city in Kentucky at a rate of 34.3%. This has brought additional housing, industries and<br />
businesses, schools, and expanded community resources. Interstate 75, crossing through the county from<br />
north to south (see above map), influenced the growth of the county. Interstate accessibility provided opportunities<br />
both in and out of the county for labor, shopping, and access to additional services not available<br />
locally.<br />
Exhibit 3<br />
<strong>Saint</strong> <strong>Joseph</strong> Berea CHNA <strong>Community</strong><br />
<strong>2012</strong> Demographic Snapshot<br />
DEMOGRAPHIC CHARACTERISTICS<br />
Madison County Kentucky USA<br />
Number % of Total Number % of Total Number % of Total<br />
Total Population 82,916 100% 4,339,367 100% 308,745,538<br />
100%<br />
2010 Population<br />
Total Male Population 40,264 49% 2,134,952 42.9% 151,902,805 49.2%<br />
Total Female Population 42,652 51% 2,204,415 50.8% 156,842,733<br />
50.8%<br />
2000 Population 82,916 100% 4,042,288 100%<br />
Population, %age Change,<br />
2000-2010<br />
17% 7.4%<br />
Percent of Population that<br />
is Older than 64 years<br />
8.8% 13.3% 12.9%<br />
Median Household Income $38,596 $42,248 $52,762<br />
U.S. Census Bureau American Fact Finder<br />
AGE DISTRIBUTION<br />
Madison County Kentucky USA<br />
Age Group Number % of Total Number % of Total Number % of Total<br />
0-4 years 5,069 6.1% 290,407 6.7% 20,201,362 6.5%<br />
5-19 years 17,116 20.6% 850,736 19.7% 63,066,194 20.4%<br />
20-34 years 20,665 24.9% 867,398 20.1% 62,649,947 20.3%<br />
35-44 years 10,751 13.0% 584,865 13.6% 41,070,606 13.3%<br />
45-54 years 10,888 13.1% 636,992 14.8% 45,006,716 14.6%<br />
55-64 years 9,115 11.0% 513,381 11.9% 36,482,729 11.8%<br />
65+ years 9,312 11.2% 570,334 13.2% 40,267,984 13.0%<br />
Total 82,916 99.9% 4,314,113 100% 308,745,538 99.9%<br />
U.S. Census Bureau American Fact Finder<br />
Page 9
<strong>Community</strong> <strong>Health</strong> <strong>Needs</strong> <strong>Assessment</strong> 2013<br />
The 65+ year age group is becoming the fastest growing age group as Baby Boomers age. This brings<br />
with it a whole other set of issues in areas, such as Madison County, where a number of retirees haven<br />
chosen to relocate.<br />
POPULATION DISTRIBUTION – RACE/ETHNICITY<br />
Madison County Kentucky USA<br />
Number % of Total Number % of Total Number % of Total<br />
White 74,967 90.4% 3,809,537 87.8% 223,553,265 72.4%<br />
African-American 3,565 4.3% 337,520 7.8% 38,929,319 12.6%<br />
Hispanic/Latino 1,813 2.2% 132,836 3.1% 50,477,594 16.3%<br />
American Indian/Alaska Native<br />
225 0.3% 10,120 0.2% 2,932,248 0.9%<br />
Two or More Races 1,447 1.7% 75,208 1.7% 9,009,073 2.9%<br />
Asian 753 0.9% 48,930 1.1% 14,674,252 4.8%<br />
Some Other Race Alone 116 0.1% 55,551 1.3% 19,107,368 6.2%<br />
Native Hawaiian/Pacific Islander<br />
30 0.0% 2,501 0.1% 540,013 0.2%<br />
U.S. Census Bureau American Fact Finder<br />
HOUSEHOLD INCOME DISTRIBUTION<br />
Madison County Kentucky USA<br />
Household Income Number<br />
% of Totatatal<br />
% of To-<br />
% of To-<br />
Number<br />
Number<br />
<strong>Community</strong> <strong>Health</strong> <strong>Needs</strong> <strong>Assessment</strong> 2013<br />
Exhibit 4<br />
<strong>Saint</strong> <strong>Joseph</strong> Berea CHNA <strong>Community</strong><br />
Median Household Income, Poverty and Unemployment Rates of <strong>Community</strong><br />
2007-2011 Data<br />
Garrard<br />
County<br />
Jackson<br />
County<br />
Madison<br />
County<br />
Rockcastle<br />
County<br />
Kentucky<br />
U.S.<br />
Median Household Income $40,137 $21,448 $41,876 $26,967 $42,248 $52,762<br />
Population in Poverty 20.9% 35.6% 20.3% 29.2% 18.1% 14.3%<br />
Unemployment Rate 10.3% 16.2% 7.7% 11.7% 9.5% 8.9%<br />
U.S. Census Bureau & Bureau of Labor Statistics<br />
Median household income below <strong>2012</strong> Federal Poverty Level ($23,050) for a family of two adults and two children.<br />
Uninsured Status<br />
Exhibit 5<br />
<strong>Saint</strong> <strong>Joseph</strong> Berea CHNA <strong>Community</strong><br />
<strong>Health</strong> Insurance coverage Status by Age (Under 65 Years) and Income<br />
(at or Below 400%) of Poverty 2010<br />
All Income Levels<br />
At or Below 400% of FPL<br />
Under 65 Percent Under 65 Percent Under 65 Percent Under 65 Percent<br />
County Uninsured Uninsured Insured Insured Uninsured Uninsured Insured Insured<br />
Garrard 3,118 21.7% 11,231 78.3% 2,849 25.8% 8,185 74.2%<br />
Jackson 2,386 20.6% 9,203 79.4% 2,258 22.5% 7,774 77.5%<br />
Madison 12,898 18.9% 55,248 81.1% 11,755 24.1% 36,946 75.9%<br />
Rockcastle 3,010 21.0% 11,340 79.0% 2,333 23.2% 9,360 76.8%<br />
Kentucky 640,974 17.5% 3,012,207 82.5% 585,339 22.4% 2,032,203 77.6%<br />
Source: US Census Bureau<br />
<strong>Saint</strong> <strong>Joseph</strong> Berea community has more uninsured than both Kentucky and the US benchmark for uninsured.<br />
About one quarter of the community who is below poverty level is uninsured and without a means<br />
to pay for many of their medical expenses.<br />
Education<br />
The educational attainment of community residents may impact the local economy. Higher levels of<br />
education generally lead to higher wages, less unemployment and job stability. These factors may<br />
indirectly influence community health. Exhibit 6 provides a profile of Madison County Schools.<br />
Page 11
<strong>Community</strong> <strong>Health</strong> <strong>Needs</strong> <strong>Assessment</strong> 2013<br />
Exhibit 6<br />
<strong>Saint</strong> <strong>Joseph</strong> Berea CHNA <strong>Community</strong><br />
Madison County Schools<br />
Grade Levels School System Programs<br />
K-12<br />
Madison County School District<br />
Berea Independent School District<br />
(Berea <strong>Community</strong> School)<br />
10 Elementary schools<br />
4 Middle Schools<br />
2 High Schools<br />
1 Semi-Private (Model Lab)<br />
1 Elementary<br />
1 M-iddle School<br />
1 High School<br />
Private Schools Bluegrass Christian K-12<br />
St Mark’s Catholic PK-5<br />
Colleges<br />
/Universities<br />
Berea College<br />
Eastern Kentucky University<br />
National College<br />
Liberal arts college that was established in 1855 and does<br />
not charge tuition. Students participate in a full work study<br />
program. It offers bachelor degree programs. There are<br />
approximately 1550 students from 44 states and 58 foreign<br />
countries. 70% of students come from Appalachia region of<br />
Kentucky.<br />
EKU offers more than 160 degree programs in associate,<br />
bachelors, masters and doctoral levels. The enrollment is<br />
over 16,500 including satellite campuses.<br />
A small Private two-year career college offering associate<br />
degrees and diplomas in health care, business, and other<br />
vocations.<br />
Exhibit 7<br />
<strong>Saint</strong> <strong>Joseph</strong> Berea CHNA <strong>Community</strong><br />
Educational Attainment by County – Ages 25 and Over<br />
2005-2009 Estimate (ACS)<br />
High School<br />
Diploma, GED<br />
or more<br />
Bachelor’s<br />
Degree or<br />
Higher<br />
Kentucky<br />
H.S. College H.S. College<br />
Madison 83.6% 26.4% 80.3% 20% 84.6% 27.5%<br />
Jackson 55% 9.1% 80.3% 20% 84.6% 27.5%<br />
Rockcastle 58.5% 10.1% 80.3% 20% 84.6% 27.5%<br />
Garrard 67.4% 12.1% 80.3% 20% 84.6% 27.5%<br />
Source: UK AG <strong>Community</strong> & Economic Initiative of Kentucky (CEDIK)<br />
Exhibit 7 indicates Madison County residents obtain a bachelor’s degree or higher at rates greater than<br />
state and national averages; in Madison County the rate is 26.4 percent.<br />
USA<br />
Page 12
<strong>Community</strong> <strong>Health</strong> <strong>Needs</strong> <strong>Assessment</strong> 2013<br />
<strong>Community</strong> <strong>Health</strong> Care Resources<br />
The availability of health care resources is critical to the health of a county’s residents and a measure of<br />
the soundness of the area’s health care delivery system. An adequate number of health care facilities and<br />
health care providers is vital to sustain a community’s health status. Fewer health care facilities and health<br />
care providers can impact the timely delivery of services. A limited supply of health resources, especially<br />
providers, results in the limited capacity of the health care delivery system to absorb charity and indigent<br />
care as there are fewer providers upon which to distribute the burden of indigent care. The next section<br />
addresses the availability of health care resources to the residents of <strong>Saint</strong> <strong>Joseph</strong> Berea’s service area.<br />
<strong>Hospital</strong>s<br />
Madison County has one other hospital besides <strong>Saint</strong> <strong>Joseph</strong> Berea. Patty A Clary is located in Richmond,<br />
14 miles north of Berea. A third hospital in the area is Rockcastle Regional, in Rockcastle County. Exhibit<br />
9 provides a listing of hospitals.<br />
Exhibit 8<br />
<strong>Saint</strong> <strong>Joseph</strong> Berea CHNA <strong>Community</strong><br />
Summary of Area <strong>Hospital</strong>s<br />
Facility County Facility Type Total Beds ICU Beds<br />
Baptist <strong>Health</strong> Richmond Madison Acute Care 105 8<br />
<strong>Saint</strong> <strong>Joseph</strong> Berea Madison Critical Access 25 4<br />
Rockcastle Regional Rockcastle Acute Care 26 2<br />
Ambulatory Care Clinics<br />
Exhibit 9 provides a list of ambulatory care center as of FY<strong>2012</strong> most of which are in Fayette County,<br />
adjacent to Madison County. Fayette is also where <strong>Saint</strong> <strong>Joseph</strong> Berea sends patients for care not available<br />
here.<br />
Facility<br />
Exhibit 9<br />
<strong>Saint</strong> <strong>Joseph</strong> Berea CHNA <strong>Community</strong><br />
Summary of Ambulatory Care Clinics<br />
Location<br />
Pinnacle Management LLC dba Richmond Open MRI 103 Alycia Drive Richmond KY 40475<br />
Dermatology Associates of Ky, PSC 250 Fountain Court Lexington KY 40509<br />
Kentucky Imaging Center 3475 Richmond Road, Suite 150 Lexington KY 40509<br />
Kentucky Surgery Center 240 Fountain Court Lexington KY 40509<br />
Lexington Clinic 1221 South Broadway Lexington KY 40504<br />
Lexington Diagnostic Center 1725 Harrodsburg Road Suite 100 Lexington KY 40504<br />
Lexington Surgery Center 1451 Harrodsburg Road, Ste 102 Lexington KY 40544<br />
Physician Services 1721 Nicholasville Rd. Lexington KY 40503<br />
Stone Road Surgery Center 280 Pasadena Dr. Lexington KY 40503<br />
Source: http://chfs.ky.gov/ohp/healthdata<br />
Page 13
<strong>Community</strong> <strong>Health</strong> <strong>Needs</strong> <strong>Assessment</strong> 2013<br />
Other Licensed Facilities<br />
There are licensed services other than hospitals and ambulatory care clinics in Madison County. These include<br />
home health, hospice, adult day care, ambulatory surgery centers, rehabilitation agencies and private<br />
duty nursing providers. A complete inventory may be obtained through the Kentucky Cabinet for <strong>Health</strong><br />
and Family Services at http://chfs.ky.gov/ohp/con/inventory.htm.<br />
Physicians<br />
Exhibit 10<br />
<strong>Saint</strong> <strong>Joseph</strong> Berea CHNA<br />
Physicians<br />
<strong>Health</strong> Care Providers<br />
Available Madison Kentucky Physicians Available Madison Kentucky<br />
All Physicians 108 10,115 Total Physicians 108 10,115<br />
Primary Care Physicians 67 4,241 Total Primary Care 67 4,241<br />
Physician Specialists 41 5,874 Family Practice 27 1,547<br />
Registered Nurses 1,072 47,948 General Practice 3 116<br />
Nurse Practitioners 56 2,797 Internal Medicine 22 1,375<br />
Physician Assistants 15 772<br />
Obstetrics and Gynecology<br />
5 493<br />
Pharmacists 86 4,524 Pediatrics 10 710<br />
Dentists 31 2,461 Other Specialty 41 5,874<br />
<strong>Health</strong> Departments<br />
Madison County <strong>Health</strong> Department is the only health department in Madison County two offices, one in<br />
Richmond and one in Berea. <strong>Saint</strong> <strong>Joseph</strong> Berea has a very good collaborative relationship with them, especially<br />
the office in Berea.<br />
Page 14
<strong>Community</strong> <strong>Health</strong> <strong>Needs</strong> <strong>Assessment</strong> 2013<br />
<strong>Health</strong> Status of the <strong>Community</strong><br />
This section of the assessment reviews the health status of Madison County residents. As in the previous<br />
section, comparisons are provided with the state of Kentucky and the United States. This in-dept assessment<br />
of the mortality and morbidity data, health outcomes, health factors and mental health indicators of<br />
Madison County residents that make up the community will enable <strong>Saint</strong> <strong>Joseph</strong> Berea to identify priority<br />
health issues related to the health status of its residents.<br />
Good health can be defined as a state of physical, mental, and social well-being, rather than the absence of<br />
disease or infirmity. According to <strong>Health</strong>y People 2010, the national health objectives released by the U.S.<br />
Department of <strong>Health</strong> and Human Services, individual health is closely linked to community health.<br />
<strong>Community</strong> health, which includes both the physical and social environment in which individuals live,<br />
work and play, is profoundly affected by the collective behaviors, attitudes and beliefs of everyone who<br />
lives in the community. <strong>Health</strong> people are among a community’s most essential resources.<br />
Numerous factors have a significant impact on an individual’s health status: lifestyle and behavior, human<br />
biology, environmental and socioeconomic conditions, as well as access to adequate and appropriate health<br />
care and medical services. Studies by the American Society of Internal Medicine conclude that up to 70<br />
percent of an individual’s health status is directly attributable to personal lifestyle decisions and attitudes.<br />
People who do not smoke, who drink in moderation (if at all), use automobile seat belts (car seats for infants<br />
and small children)j, maintain a nutritious low-fat, high-fiber diet, reduce excess stress in daily living<br />
and exercise regularly have a significantly greater potential of avoiding debilitating diseases, infirmities<br />
and premature death.<br />
The interrelationship among lifestyle/behavior, personal health attitude and poor health status is gaining<br />
recognition and acceptance by both the general public and health care providers. Some examples of<br />
lifestyle/behavior and related health care problems include the following:<br />
Lifestyle/Behavior<br />
Primary Disease Factor<br />
Smoking Lung cancer Emphysema<br />
Cardiovascular disease<br />
Chronic bronchitis<br />
Alcohol/Drug Abuse Cirrhosis of liver Malnutrition<br />
Motor vehicle crashes<br />
Mental illness<br />
Unintentional injuries<br />
Suicide<br />
Poor Nutrition<br />
Driving at Excessive Speeds<br />
Lack of Exercise<br />
Overstressed<br />
Obesity<br />
Digestive disease<br />
Depression<br />
Trauma<br />
Motor vehicle crashes<br />
Cardiovascular disease<br />
Depression<br />
Mental illness<br />
Alcohol/Drug abuse<br />
Cardiovascular disease<br />
Page 15
<strong>Community</strong> <strong>Health</strong> <strong>Needs</strong> <strong>Assessment</strong> 2013<br />
<strong>Health</strong> problems should be examined in terms of morbidity as well as mortality. Morbidity is defined as<br />
the incidence of illness or injury and mortality is defined as the incidence of death. However, the law does<br />
not require reporting the incidence of a particular disease, except when the public health is potentially<br />
endangered.<br />
Due to limited morbidity data, this health assessment relies heavily on death and death rate statistics for<br />
leading causes in death. Such information provides useful indicators of health status trends and permits an<br />
assessment of the impact of changes in health services on a resident population during an established<br />
period of time. <strong>Community</strong> attention and health care resources may then be directed to those areas of<br />
greatest impact and concern.<br />
Leading Causes of Death<br />
Exhibit 10<br />
<strong>Saint</strong> <strong>Joseph</strong> Berea CHNA<br />
Leading Causes of Death in Madison County,<br />
Kentucky and the US, 2007<br />
Rate per 100,000 Total Population<br />
Leading Causes of death<br />
Madison<br />
Co. Kentucky US<br />
250<br />
200<br />
Cancer 208.7 211.1 178.4<br />
150<br />
Heart Disease 211.8 218.2 190.9<br />
100<br />
Stroke 58.3 47.2 42.2<br />
Chronic Lower Respiratory<br />
Disease 56.8 58.6 40.8<br />
Unintentional Injuries 37.6 51.8 40<br />
50<br />
0<br />
Cancer<br />
Heart<br />
Disease<br />
Stroke<br />
Chronic<br />
Low er<br />
Respiratory<br />
Disease<br />
Unintentional<br />
Injuries<br />
Source: 2011 MCCHIP<br />
Madison Co. Kentucky US<br />
According to the 2011 Kentucky <strong>Health</strong> Facts, the leading causes of cancer in Madison County were lung,<br />
colorectal, breast and prostrate. Madison County ranks higher than the national benchmark for all except<br />
unintentional injuries and lower than Kentucky benchmark for all except deaths due to strokes. Kentucky,<br />
as a whole, ranks higher than the US benchmark in leading causes of death.<br />
Page 16
<strong>Community</strong> <strong>Health</strong> <strong>Needs</strong> <strong>Assessment</strong> 2013<br />
Primary <strong>Health</strong> Conditions Responsible for Inpatient <strong>Hospital</strong>ization<br />
The Top 10 primary health conditions responsible for inpatient hospitalizations in Madison County are listed<br />
below. The top four for Madison County include circulatory, respiratory, labor and delivery and digestive<br />
system. However, <strong>Saint</strong> <strong>Joseph</strong> Berea does not provide services for labor and delivery.<br />
Top 10 Primary <strong>Health</strong> Conditions Responsible for Inpatient<br />
<strong>Hospital</strong>izations (Rate per 100,000),<br />
Madison County, 2011<br />
Mental Diseases/Disorders<br />
Metabolic Diseases/Disorders<br />
Kidney and Urinary Tract<br />
Nervous System<br />
Musculoskeletal Sys & Connective Tissue<br />
Digestive System<br />
Newborns/Neonates<br />
Pregnancy, Childbirth, and Puerperium<br />
Respiratory System<br />
Circulatory System<br />
313<br />
357<br />
445<br />
529<br />
690<br />
739<br />
996<br />
1,124<br />
1,124<br />
1,176<br />
Rate per 100,000<br />
Population<br />
Source: Kentucky Inpatient <strong>Hospital</strong>izations Claims Files, Kentucky Department for Public <strong>Health</strong><br />
Page 17
<strong>Community</strong> <strong>Health</strong> <strong>Needs</strong> <strong>Assessment</strong> 2013<br />
<strong>Health</strong> Outcomes and Factors<br />
<strong>Health</strong> Statistics and Rankings<br />
An analysis of various health outcomes and factors for a particular community can, if improved, help make<br />
that community a healthier place to live, learn, work, and play. And a better understanding of the factors<br />
that affect the health of the community will assist with how to improve the community’s habits, culture<br />
and environment. This portion of the community health needs assessment utilizes information from<br />
County <strong>Health</strong> Rankings, a key component of the Mobilizing Action Toward <strong>Community</strong> <strong>Health</strong><br />
(MATCH) project, a collaboration between the Robert Wood Johnson Foundation and the University of<br />
Wisconsin Population <strong>Health</strong> Institute.<br />
The County <strong>Health</strong> Rankings model is grounded in the belief that programs and policies implemented at<br />
the local, state and federal levels have an impact on the variety of factors that, in turn, determine the health<br />
outcomes for communities across the nation. The model ranks all 50 states and the counties within each<br />
state based on two types of health outcomes—how long people live (mortality) and how healthy people<br />
feel (morbidity)—and four health factors. These are defined below:<br />
<strong>Health</strong> Outcomes – rankings are based on an equal weighting of one length of life (mortality)<br />
measure and four quality of life (morbidity) measures.<br />
<strong>Health</strong> Factors – rankings are based on weighted scores of four factors:<br />
o<br />
o<br />
o<br />
o<br />
<strong>Health</strong> behaviors (6 measures)<br />
Clinical care (5 measures)<br />
Social and economic (7 measures)<br />
Physical environment (4 measures)<br />
Those having high ranks, e.g. 1 or 2, are considered to be the ―healthiest.‖ A more detailed discussion<br />
about the ranking system, data sources and measures, data quality and calculating scores and ranks can be<br />
found at the website for County <strong>Health</strong> Rankings (www.countyhealthrankings.org).<br />
As part of this community health needs assessment, the relative health status of Madison County is<br />
compared to the state of Kentucky and a national benchmark. A better understanding of the factors that<br />
affect the health of the community will assist with how to improve the community’s habits, culture and<br />
environment.<br />
Page 18
<strong>Community</strong> <strong>Health</strong> <strong>Needs</strong> <strong>Assessment</strong> 2013<br />
The following table from County <strong>Health</strong> Rankings summarizes the <strong>2012</strong> health outcomes for all counties<br />
that comprise the majority of the community for <strong>Saint</strong> <strong>Joseph</strong> Berea. Each measure is described and<br />
includes a confidence interval or error margin surrounding it–– if a measure is above the state average and<br />
the state average is beyond the error margin for the county, then further investigation is recommended.<br />
<strong>Health</strong> Outcomes—rankings are based on an equal weighting of one length of life (mortality) measure and<br />
four quality of life (morbidity) measures. While most of the counties within <strong>Saint</strong> <strong>Joseph</strong> Berea’s service<br />
area compare favorably to state of Kentucky, each measure was significantly below national benchmarks<br />
with opportunities for improvement.<br />
Exhibit 11<br />
<strong>Saint</strong> <strong>Joseph</strong> Berea CHNA <strong>Community</strong><br />
<strong>Health</strong> Outcomes (<strong>2012</strong>)<br />
Garrard Jackson Madison Rockcastle National<br />
County County County County KY Benchmark<br />
Mortality<br />
Premature death - Years of potential life lost<br />
before age 75 per 100,000 population (ageadjusted)<br />
7,706 12,070 7,285 10,411 8,761 5,466<br />
Morbidity<br />
Poor or fair health - Percent of adults reporting<br />
fair or poor health (age-adjusted) 19% 36% 18% 29% 22% 10%<br />
Poor physical health days - Average number<br />
of physically unhealthy days reported in past<br />
30 days (age-adjusted) 5.5 7.3 4.3 6.6 4.7 2.6<br />
Poor mental health days - Average number<br />
of mentally unhealthy days reported in past<br />
30 days<br />
(age-adjusted)<br />
3.6 7.4 3.6 5.0 4.3 2.3<br />
Low birth weight - Percent of live births<br />
with low birth weight (
<strong>Community</strong> <strong>Health</strong> <strong>Needs</strong> <strong>Assessment</strong> 2013<br />
Exhibit 12<br />
<strong>Saint</strong> <strong>Joseph</strong> Berea CHNA <strong>Community</strong><br />
<strong>Health</strong> Factors (<strong>2012</strong>)<br />
Garrard Jackson Madison Rockcastle National<br />
County County County County KY Benchmark<br />
<strong>Health</strong> Behaviors<br />
Adult smoking - Percent of adults that report<br />
smoking at least 100 cigarettes and that they currently<br />
smoke 0.0% 35.0% 22.0% 32.0% 27.0% 14.0%<br />
Adult obesity - Percent of adults that report a<br />
BMI >= 30 33.0% 33.0% 30.0% 36.0% 33.0% 25.0%<br />
Physical inactivity - Percent of adults aged 20<br />
and over reporting no leisure time physical activity 36.0% 37.0% 30.0% 38.0% 31.0% 21.0%<br />
Excessive drinking - Percent of adults that report<br />
excessive drinking in the past 30 days 10.0% 6.0% 10.0% 10.7% 8.0%<br />
Motor vehicle crash death rate - Motor vehicle<br />
deaths per 100K population 16.0 43.0 16.0 32.0 22 12<br />
Sexually transmitted infections - Chlamydia rate<br />
per 100K population 188.0 147.0 223.0 83.0 311 84<br />
Teen birth rate - Per 1,000 female population,<br />
ages 15-19 48.0 62.0 33.0 62.0 52 22<br />
Clinical Care<br />
Uninsured - Percent of population under age 65<br />
without health insurance 20.0% 21.0% 18.0% 20.0% 17.0% 11.0%<br />
Primary care physicians - Ratio of population to<br />
primary care physicians 2,431:1 13,385:1 1,679:1 1,664:1 1232:1 631:1<br />
Preventable hospital stays - <strong>Hospital</strong>ization rate<br />
for ambulatory-care sensitive conditions per 1,000<br />
Medicare enrollees 88.0 102.0 66.0 186.0 104 49<br />
Diabetic screening - Percent of diabetic Medicare<br />
enrollees that receive HbA1c screening 90.0% 85.0% 88.0% 80.0% 82.0% 89.0%<br />
Mammography screening - Percent of female<br />
Medicare enrollees that receive mammography<br />
screening 61.0% 49.0% 61.0% 56.0% 63.0% 74.0%<br />
Social & Economic Factors<br />
High school graduation - Percent of ninth grade<br />
cohort that graduates in 4 years 73.0% 72.0% 77.0% 83.0% 78.0%<br />
Some college - Percent of adults aged 25-44<br />
years with some post-secondary education 43.0% 35.0% 62.0% 39.0% 55.0% 68.0%<br />
Unemployment - Percent of population age 16+<br />
unemployed but seeking work 11.8% 17.1% 8.8% 11.3% 10.5% 5.4%<br />
Children in poverty - Percent of children under<br />
age 18 in<br />
poverty 26% 40% 25.0% 35.0% 26.0% 13.0%<br />
Inadequate social support - Percent of adults<br />
without social/emotional support 26.0% 17.0% 26.0% 20.0% 14.0%<br />
Children in single-parent households - Percent<br />
of children that live in household headed by single<br />
parent 24.0% 34.0% 33.0% 24.0% 32.0% 20.0%<br />
Violent crime rate - Deaths due to homicide per<br />
100,000 population (age-adjusted) 67.0 35.0 204.0 87.0 288 73<br />
Physical Environment<br />
Air pollution-particulate matter days - Annual<br />
number of unhealthy air quality days due to fine<br />
particulate matter 0 0 0 0 2 -<br />
Air pollution-ozone days - Annual number of<br />
unhealthy air quality days due to ozone 0 0 0 0 2 -<br />
Access to recreational facilities - Rate of recreational<br />
facilities per 100,000 population 0.0% 0 13.0% 0 8 0.0%<br />
Limited access to healthy foods - Percent of<br />
population who are low-income and do not live<br />
close to a grocery store 0% 0% 0% 0% 7.0% 16<br />
Fast food restaurants - Percent of all restaurants<br />
that are fast-food establishments 50 50.0% 59.0% 41.0% 54.0% 25.0%<br />
Page 20
<strong>Community</strong> <strong>Health</strong> <strong>Needs</strong> <strong>Assessment</strong> 2013<br />
Primary Data<br />
As part of the <strong>Community</strong> <strong>Health</strong> <strong>Needs</strong> <strong>Assessment</strong> (CHNA) conducted by <strong>Saint</strong> <strong>Joseph</strong> Berea, feedback<br />
was sought from the general public regarding what they considered the greatest health needs and possible<br />
opportunities in the community. The primary data was collected from September –November <strong>2012</strong>. Methodology<br />
used to collect data included a community wide survey, focus groups and interviews. Please<br />
refer to Section II – ―How the <strong>Assessment</strong> was Conducted‖ for details regarding methodology used.<br />
<strong>Community</strong> Input-Surveys<br />
The survey was mailed to random households in our primary service area. It was available in English and<br />
in Spanish. As previously mentioned, there were 949 respondents. Our primary objective was to have a<br />
better understanding of community perception regarding greatest health problems, personal health issues,<br />
barriers, opportunities and whether people knew about and/or used the services of <strong>Saint</strong> <strong>Joseph</strong> Berea.<br />
The chart reflects all of the responses regarding the most important health problems in the community.<br />
More than three were often selected; this was allowed because we did not have a way to identify top ones.<br />
The top ten identified in the survey were obesity, alcohol/drug abuse, diabetes, cancers, heart disease, aging<br />
problems, high blood pressure, depression/anxiety, Alzheimer’s/dementia and child abuse/neglect. The<br />
comment responses included drug abuse and health insurance/costs. Based on the percentages we carried<br />
this to the top 13 to include respiratory, mental health and dental. This information was weighted with other<br />
data collected to determine our top five health problems. This was explained earlier in the ―How the <strong>Assessment</strong><br />
was Conducted‖ section of the report.<br />
Page 21
<strong>Community</strong> <strong>Health</strong> <strong>Needs</strong> <strong>Assessment</strong> 2013<br />
When asked to rate the respondent’s personal health, 45.7% said they were healthy, 9.1% said they were<br />
very healthy and 35.1% said they were somewhat healthy. This was interesting when asked if they had any<br />
chronic diseases. After evaluation of data, it was presumed that those with the mentioned health issues had<br />
them under control (through medication, diet) or believed themselves healthy despite their health issues.<br />
Page 22
<strong>Community</strong> <strong>Health</strong> <strong>Needs</strong> <strong>Assessment</strong> 2013<br />
Over 23.9% (nearly 1/3) of respondents have had a family member diagnosed with Alzheimer’s or dementia.<br />
The largest group of respondents to our survey was in the 65+ group. Their comments were personal<br />
and supportive of individuals with this disease. Many family members in the <strong>Saint</strong> <strong>Joseph</strong> Berea community<br />
try to care for the elderly and those with dementia at home.<br />
What can <strong>Saint</strong> <strong>Joseph</strong> Berea do to help those with dementia? The majority of comments centered around<br />
these areas:<br />
• Educate employees on how to care for patients with dementia.<br />
• Education and resources and support in an effort to keep them at home.<br />
• Show respect and compassion; help patient and family to maintain dignity.<br />
• Listen to and involve the caregivers.<br />
• Provide quality ER care for elderly and patients with dementia.<br />
When asked if your family had been affected by alcohol abuse, the majority said no (60.3%), but almost<br />
40% said yes (39.7), confirming other data which identified alcohol abuse as a top need.<br />
Page 23
<strong>Community</strong> <strong>Health</strong> <strong>Needs</strong> <strong>Assessment</strong> 2013<br />
How would you address alcohol/drug<br />
abuse?<br />
• Counseling/rehabilitation<br />
• Education<br />
• Jail/stiffer penalties<br />
• Hold doctors responsible<br />
Respondents were asked to identify major barriers in seeking health care. The majority of respondents<br />
have some form of health care coverage whether it is private, Medicare, Medicaid or Military/VA. Still,<br />
almost 60% of the 532 respondents said co-pay, or out-of-pocket expenses prevented them or someone in<br />
their household for seeking health care. Other health barriers included procedures not covered by insurance<br />
and high deductibles. However, 62% saw their family doctor at least twice in the last 12 months.<br />
Respondents skipped the following services due to out-of-pocket costs:<br />
Page 24
<strong>Community</strong> <strong>Health</strong> <strong>Needs</strong> <strong>Assessment</strong> 2013<br />
Information was gathered regarding usage of health care services at <strong>Saint</strong> <strong>Joseph</strong> Berea and other facilities<br />
and counties.<br />
• 52% said they use the services provided at <strong>Saint</strong> <strong>Joseph</strong> Berea.<br />
• When asked how they heard about the hospital, word of mouth (49%) and physicians (32%) were the<br />
main responses. Advertising (25%) and community outreach (10%) were also listed.<br />
• 19% were hospitalized in the last 12 months. Other hospitals used were Baptist <strong>Health</strong> (Patty A. Clay)<br />
21% and Rockcastle Regional (4%). 41% were not hospitalized.<br />
• 82% of respondents said they seek health care in Madison County, 55% seek care in Fayette County<br />
(major hospitals in Central Kentucky), less than 15% sought care in Rockcastle, Jackson or Garrard<br />
Counties.<br />
Page 25
<strong>Community</strong> <strong>Health</strong> <strong>Needs</strong> <strong>Assessment</strong> 2013<br />
<strong>Community</strong> Input-Focus Group and Interview Results<br />
Focus groups and key informant interviews provided opportunities for the community to express strengths,<br />
needs and opportunities. The same general questions were asked the focus group and interview participants.<br />
Each responded based on the background and affiliation of the particular group or individual.<br />
1. What are the health issues that have impacted you or the community?<br />
Obesity<br />
Diabetes<br />
Heart disease<br />
Cancer<br />
Oral health<br />
COPD<br />
Alzheimer’s disease/dementia<br />
Stroke<br />
Drugs/Alcohol<br />
Mental <strong>Health</strong><br />
Kidney Disease<br />
Falls<br />
Arthritis/Joint Pain/Fibromyalgia<br />
Vision<br />
As with the survey results a connection can be made between the different diseases. Obesity is listed as the<br />
number one problem. This one disease alone can be the cause of other diseases listed. According to an article<br />
from the Kentucky Department for Public <strong>Health</strong>, obesity in children has short term and long term<br />
results put them at risk as youth/teens and adults. Diabetes, heart disease, stroke, high cholesterol, high<br />
blood pressure, bone and joint problems (arthritis), sleep apnea, several types of cancer and social/psychological<br />
problems such as poor self-esteem.<br />
http://chfs.ky.gov/NR/rdonlyres/70814C96-7EA2-470F-B5A2-<br />
75A1249A348F/0/101409ObesityChildren.doc<br />
2. What are the resources and barriers?<br />
Resources:<br />
Two colleges: Berea and EKU<br />
Walking/Hiking/Bike trails<br />
<strong>Hospital</strong> location and services<br />
Food Bank/BUURR<br />
Libraries<br />
Adult Day Care<br />
Family centers at schools<br />
SJB Patient and Family Fund<br />
Affordable Care Act<br />
Hopes Wings for battered/abused women<br />
Liberty Place for Women with alcohol/drug<br />
problems<br />
Barriers:<br />
Lack of pediatricians<br />
Urgent care not adequate<br />
Misunderstanding of behavioral/mental<br />
issues<br />
Medicaid coverage issues<br />
Cost of healthy or organic foods<br />
Lack of preventative care for the poor<br />
without Berea <strong>Health</strong> Ministries<br />
Lack of sidewalks<br />
Money for programs<br />
Page 26
<strong>Community</strong> <strong>Health</strong> <strong>Needs</strong> <strong>Assessment</strong> 2013<br />
3. What is your vision for a healthy community?<br />
Outpatient services for mental/behavioral health issues<br />
Better access to health care for preventative care: free/low cost health assessments, blood pressure,<br />
diabetes, etc.<br />
Increase hiking, recreational and walking trails, exercise programs, playgrounds, weight management<br />
programs to address obesity<br />
Incentives for providers to come/stay in Berea<br />
Ability for seniors to stay at home<br />
<strong>Health</strong> meals at food banks, fast foods, meal services in schools<br />
Support programs for elderly, families, alcohol/drug, etc.<br />
Smoking bans<br />
Environmental concerns with fumes from factories<br />
“A health community has residents who have access to preventative care, with places to exercise and<br />
where they can buy healthy food.”<br />
“Sustainability and environmental concerns are considered as extremely important and necessary<br />
components of all projects and policies.”<br />
4. What are some solutions to improving the health of the community? What can the community<br />
do?<br />
In addition to what is listed in the vision of a health community, participants suggested:<br />
Address and follow up care for drug/alcohol issues<br />
Obesity clinic and nutrition education for children and adults<br />
Expand bike and walking trails<br />
Address mental health issues in a positive way<br />
Domestic violence awareness and programs<br />
Diabetes support and education<br />
Senior services that provide at home care and long term care support<br />
<strong>Community</strong> wide smoking cessation program<br />
Additional surgeon at the hospital and a pediatrician<br />
Expanded transportation in the community<br />
Inpatient mental health beds<br />
Improve public awareness<br />
5. What is great about our community?<br />
Libraries<br />
Small town; feel safe<br />
Necessary services available<br />
<strong>Community</strong> members work together to achieve a common goal<br />
Affordable housing<br />
Access to employment<br />
<strong>Saint</strong> <strong>Joseph</strong> Berea: Love the community art in the hospital and it is a caring and compassionate<br />
hospital<br />
Page 27
<strong>Community</strong> <strong>Health</strong> <strong>Needs</strong> <strong>Assessment</strong> 2013<br />
Participants in the survey, focus groups and interviews were also asked to give their perception of<br />
<strong>Saint</strong> <strong>Joseph</strong> Berea.<br />
Strong focus on its mission – Services provided for all not matter their ability to pay.<br />
Personal experience and that of family members has been very good<br />
The cardiovascular center is a good addition.<br />
The emergency room meets a community need<br />
o Most respondents mentioned positive experiences, but a few were not so good because of<br />
the wait primarily<br />
Would like to see more diabetes education<br />
Appreciate the services that are provided: heart institute, outpatient dietician, wound care center,<br />
specialists, chemotherapy, pain clinic, Senior Renewal<br />
Involvement in and support of the community and schools<br />
Registration for lab, X-rays, etc. sometimes takes too long<br />
Unclear of all the services provided; suggest promoting more through different community resources<br />
Concern about the speed bumps that have been added and impact on patients in ambulances<br />
Key Themes Provided Through Participant Comments<br />
“We may have many resources for the elderly to utilize, but there needs to be a connector, someone/group<br />
that can pull all of the resources together to provide care the elderly need.”<br />
“Madison County needs affordable drug abuse treatment. Jail isn’t the answer, treatment is.”<br />
“Make sure your cafeteria and vending machines offer healthy food options. Promote healthy food and set<br />
an example for other work places in the community.”<br />
“We like having services close to home without traveling to Lexington all of the time.”<br />
“The obesity rate is appalling…I worry about the long term affects it will have on the community.”<br />
“My husband and I are raising our three grandchildren. He has Medicare, but I don’t have insurance due<br />
to cost. Neither of us has dental care…Working people who don’t qualify for assistance are left to suffer.”<br />
―I definitely feel more should be done for depression and mental problems. These diseases are so misunderstood.”<br />
<strong>Health</strong> Issues of Uninsured Persons, Low-Income Persons and Minority Groups<br />
To assess health issues impacting those in the community who are low-income and uninsured, <strong>Saint</strong> <strong>Joseph</strong><br />
Berea referred to the Madison County <strong>Health</strong> Department’s <strong>Community</strong> <strong>Health</strong> <strong>Needs</strong> <strong>Assessment</strong><br />
for 2011 (MCCHIP). Their analysis reported that Madison County residents faired better than the state as<br />
a whole. (See Appendix for website to view full report).<br />
Page 28
<strong>Community</strong> <strong>Health</strong> <strong>Needs</strong> <strong>Assessment</strong> 2013<br />
However, the Madison County <strong>Health</strong> Rankings <strong>2012</strong> report noted that the county showed improvement<br />
overall except in Clinic Care and Social and Economic Factors which went from being 5 th highest county<br />
in Kentucky in 2010 to 19 th in <strong>2012</strong>. Changes were attributed to reduced high school graduation, increased<br />
unemployment, children in poverty, inadequate social support and single-parent households (Madison<br />
County, KY - County <strong>Health</strong> Rankings 2010-<strong>2012</strong> Report)<br />
Comments received from the CHNA survey and focus groups sighted lack of preventative care for those<br />
who are poor and do not have insurance. Some have been refused treatment because they did not have the<br />
ability to pay. Lack of dental care and inability to pay for treatment came up as a major health concern.<br />
Berea <strong>Health</strong> Ministries provided service until it closed its doors in August, <strong>2012</strong>. Richmond has <strong>Health</strong><br />
Now! for those with no insurance and limited to no ability to pay. <strong>Saint</strong> <strong>Joseph</strong> Berea Family Medicine has<br />
been designated a rural health clinic. Neither the clinic nor the hospital refuse treatment for anyone who is<br />
in need. Financial counselors work with patients to make sure they have medical treatment that is needed.<br />
Per Capita Income & Poverty Level, 2011<br />
30.0%<br />
27.4%<br />
25.0%<br />
20.0%<br />
20.3%<br />
20.6%<br />
18.1%<br />
Per Capita Income<br />
15.0%<br />
10.0%<br />
Persons below poverty<br />
level<br />
5.0%<br />
0.0%<br />
Madison Co.<br />
Kentucky<br />
Percent Without <strong>Health</strong> Insurance, 25-65 y.o.<br />
18.8%<br />
18.6%<br />
18.4%<br />
18.2%<br />
18.0%<br />
17.8%<br />
17.6%<br />
18.6%<br />
Madison Co.<br />
18.0%<br />
Kentucky<br />
Page 29
<strong>Community</strong> <strong>Health</strong> <strong>Needs</strong> <strong>Assessment</strong> 2013<br />
Children at Risk:<br />
Madison Co.<br />
2006<br />
Madison Co.<br />
2010<br />
Kentucky<br />
2010<br />
U.S.<br />
2010<br />
Children living in Poverty 19.8% 25% 26% 13%<br />
Children in single-parent households 33% 32% 20%<br />
Free and reduced rate lunches 47% 50%<br />
Source: Madison County <strong>Community</strong> <strong>Health</strong> Improvement Plan 2009<br />
The concern stems from a study in the 2011 Kids Count Data Book that shows the amount of children living<br />
in poverty in Madison County from 19.8% in 2006 to over 25% in 2010. To go along with this the<br />
number of free lunches and reduced meals for children has increased from 47% in 2006 to 50% in 2011.<br />
Diseases associated with children living in poverty include untreated dental problems, causing them to lose<br />
teeth too early; poor nutrition leading to health problems and obesity in some; and living in unsafe housing<br />
conditions can worsen asthma or chronic bronchitis.<br />
Children living in single-parent households are measured because children in these households are statistically<br />
―at risk for adverse health outcomes such as mental health problems (including substance abuse, depression,<br />
and suicide) and unhealthy behaviors such as smoking and excessive alcohol use.‖ In addition,<br />
self-reported health and mortality among lone parents tended to be worse than parents living as couples<br />
(Excerpted from an article in the Richmond Register on April 12, <strong>2012</strong>, ―18 Percent in County without<br />
<strong>Health</strong> Insurance).<br />
The Madison County <strong>Health</strong> Department has made an effort to increase enrollment of the number of youth<br />
under the age of 19 enrolled in Kentucky Child <strong>Health</strong> Insurance Program (KCHIP). Their goal was to increase<br />
it from 9% in 2000 to 15% by 2014 (from 1262 youths to 1451).<br />
Aging Population<br />
According to the Department of Aging<br />
for Kentucky, the over 60 population<br />
is the fastest growing population<br />
and estimated to increase 91%<br />
from the year 2000 to the year 2030.<br />
In Disabilities (including Alzheimer’s/Dementia)<br />
and poverty levels<br />
are unique needs that will impact<br />
this group and put an extra burden<br />
on families who take the role as caregivers.<br />
Another factor in looking<br />
at the aging demographic is that over<br />
half of the grandparents in Kentucky<br />
care for their grandchildren. Additionally,<br />
23% of aging make up total mental health population in Kentucky. Services for the aging population<br />
are limited, and the ones available are not always known by the elderly or their caregivers. Information<br />
is based on the Kentucky State Plan on Aging, 2009-<strong>2012</strong> report.<br />
Page 30
<strong>Community</strong> <strong>Health</strong> <strong>Needs</strong> <strong>Assessment</strong> 2013<br />
Violence in the <strong>Community</strong><br />
Crime (excluding violent crime) has increased in Madison County up from 5,115 arrests in 2005 to 7,048<br />
arrests in 2010. Violent crimes include homicide, forcible rape, robbery and aggravated assault.<br />
Violent Crime Rate<br />
per 100,000 population<br />
350<br />
300<br />
288<br />
250<br />
200<br />
204<br />
150<br />
100<br />
73<br />
50<br />
0<br />
Madison Co. Kentucky U.S.<br />
Page 31
<strong>Community</strong> <strong>Health</strong> <strong>Needs</strong> <strong>Assessment</strong> 2013<br />
Priority <strong>Community</strong> <strong>Health</strong> <strong>Needs</strong> Identified<br />
Using findings obtained through the community survey and collection of primary and secondary data,<br />
<strong>Saint</strong> <strong>Joseph</strong> Berea completed an analysis of these inputs (see Appendix D and E) to identify community<br />
health needs. The following data was analyzed to identify health needs for the community:<br />
Using all of the data we had received we came up with our Top Five Priorities.<br />
<strong>Saint</strong> <strong>Joseph</strong> Berea CHNA <strong>Community</strong><br />
Top Five Priority <strong>Health</strong> Issues<br />
Rank Primary Need Groupings<br />
1 Mental <strong>Health</strong> Alcohol & drug abuse<br />
Depression/anxiety<br />
Mental/behavioral health problems<br />
Suicide<br />
2 Obesity Nutrition<br />
Physical Inactivity<br />
3 Cardiopulmonary Heart disease/stroke<br />
High blood pressure<br />
Pulmonary<br />
4 Senior issues Physical issues connected with aging<br />
Alzheimer’s/Dementia<br />
Lack of Resources<br />
5 Collaboration of Care Resource guide for community<br />
Screenings<br />
Education<br />
Prevention<br />
<strong>Community</strong> wellness council<br />
Process<br />
Several steps were taken to determine the top priorities.<br />
First, we took the results of our primary data from the survey, focus groups and interviews initially. We<br />
brought together our CHNA advisory group, SJB steering committee and other members of the community<br />
to discuss the findings and come up with what they considered top priorities. The participants were divided<br />
into two groups. Each group went through a series of questions to determine needs and how to address<br />
them. (See Appendix E for list of participants and methodology).<br />
Page 32
<strong>Community</strong> <strong>Health</strong> <strong>Needs</strong> <strong>Assessment</strong> 2013<br />
Activity 1:<br />
Given the mission, vision and values of SJB and the <strong>Community</strong> <strong>Assessment</strong> data, identify the most important<br />
health issues or problems for St. <strong>Joseph</strong> Berea <strong>Hospital</strong> to address in the next 3-5 years.<br />
Group #1<br />
1. Mental health services/Drug addiction<br />
2. Collaboration of care/services<br />
3. Chronic disease prevention<br />
4. Lack of insurance<br />
Group #2<br />
1. <strong>Health</strong>y Family<br />
2. Dental Care<br />
3. Alcohol/Drug Abuse<br />
4. Exercise Programs<br />
5. Address Connection Between Issues/ <strong>Health</strong>y<br />
Education In All Ages<br />
(Their complete analysis of top needs can be found in Appendix E).<br />
The following process was used in weighting the primary and secondary data described above. Once this<br />
was finished the <strong>Saint</strong> <strong>Joseph</strong> Berea steering committee reviewed the findings and data that had been<br />
weighted (See Exhibit 13), grouped needs and identified the top five health priority issues.<br />
Leading Causes of Death: Leading causes of death for the community were reviewed and the death rates<br />
for the leading causes of death for each county within the <strong>Saint</strong> <strong>Joseph</strong> Berea CHNA community were<br />
compared to U.S. adjusted death rates. Causes of death in which the county rate compared unfavorably to<br />
the U.S. Adjusted death rate resulted in a health need for the CHNA <strong>Community</strong>.<br />
Primary Causes for Inpatient <strong>Hospital</strong>ization: The primary causes for inpatient hospitalization resulted in<br />
an identified health need for the community.<br />
<strong>Health</strong> Outcomes and Factors: An analysis of the County <strong>Health</strong> Rankings health outcomes and factors<br />
data was prepared for each county within the <strong>Saint</strong> <strong>Joseph</strong> Berea CHNA <strong>Community</strong>. County rates and<br />
measurements for health behaviors, clinical care, social and economic factors and the physical<br />
environment were compared to national benchmarks. County rankings in which the county rate compared<br />
unfavorably (by greater than 30 percent of the national benchmark) resulted in an identified health need.<br />
Primary Data: <strong>Health</strong> needs identified through community surveys, focus groups and key informant<br />
interviews (if applicable) were included as health needs. <strong>Needs</strong> for vulnerable populations were separately<br />
reported on the analysis in order to facilitate the prioritization process.<br />
To facilitate prioritization of identified health needs, a ranking and prioritization process was used. <strong>Health</strong><br />
needs were ranked based on the following seven factors. Each factor received a score between 0<br />
and 4.<br />
1) How many people are affected by the issue or size of the issue? For this factor ratings were<br />
based on the percentage of the community who are impacted by the identified need. The<br />
following scale was utilized. >20% of the community=4; >10% and 5% and
<strong>Community</strong> <strong>Health</strong> <strong>Needs</strong> <strong>Assessment</strong> 2013<br />
2) What are the consequences of not addressing this problem? Identified health needs which<br />
have a high death rate or have a high impact on chronic diseases received a higher rating for this<br />
factor.<br />
3) The impact of the problem on vulnerable populations. <strong>Needs</strong> which pertain particularly to<br />
vulnerable populations were received a rating of 4 for this factor.<br />
4) How important the problem is to the community. <strong>Needs</strong> identified through community<br />
surveys and/or focus groups.<br />
5) Prevalence of common themes. Determined by how many sources of data (Leading Causes of<br />
Death, Primary Causes for Inpatient <strong>Hospital</strong>ization, <strong>Health</strong> Outcomes and Factors and Primary<br />
Data) identified the need.<br />
6) How closely does the need align with KentuckyOne <strong>Health</strong> strategies?<br />
7) Does the hospital have existing programs which respond to the identified need?<br />
Page 34
<strong>Community</strong> <strong>Health</strong> <strong>Needs</strong> <strong>Assessment</strong> 2013<br />
Exhibit 13<br />
<strong>Saint</strong> <strong>Joseph</strong> Berea<br />
Prioritization of <strong>Health</strong> <strong>Needs</strong><br />
Each need was ranked based on these seven prioritization metrics. These were the top priority issues that emerged:<br />
How many<br />
people are<br />
affected by the<br />
issue?<br />
What are the<br />
consequences<br />
of not addressing<br />
this<br />
problem?<br />
What is the<br />
impact on<br />
vulnerable<br />
populations?<br />
How Important<br />
is it to the<br />
community?<br />
How many<br />
sources<br />
identified<br />
the need?<br />
How closely<br />
does the<br />
need align<br />
with Kentucky-One<br />
<strong>Health</strong><br />
strategies?<br />
Does the<br />
hospital<br />
have existing<br />
programs<br />
which respond<br />
to<br />
the identified<br />
need?<br />
Total<br />
Cancer 1 4 0 4 2 4 2 17<br />
Heart Disease 1 4 4 4 1 4 3 21<br />
Chronic Lower<br />
Respiratory Disease<br />
1 4 4 3 1 4 2 19<br />
Stroke Cerebrovascular<br />
Disease 1 4 0 3 1 4 1 14<br />
Adult Smoking 4 3 0 1 1 1 1 11<br />
Adult Obesity 4 3 4 4 2 2 1 20<br />
Physical Inactivity 4 3 4 4 1 1 1 18<br />
Motor Vehicle<br />
Crash Rate 1 1 0 1 1 1 1 6<br />
Sexually Transmitted<br />
Infections 2 2 0 2 1 1 1 9<br />
Teen Birth Rate 2 2 0 1 1 1 1 8<br />
Uninsured 3 2 4 2 1 2 4 18<br />
Lack of Primary<br />
Care Physicians 4 3 2 2 1 4 3 19<br />
Children in Poverty<br />
4 4 4 2 1 3 2 20<br />
Page 1
<strong>Community</strong> <strong>Health</strong> <strong>Needs</strong> <strong>Assessment</strong> 2013<br />
Children in Single<br />
Parent Households<br />
4 4 2 3 1 1 2 17<br />
Violent Crime<br />
Rate 4 1 0 4 1 1 1 12<br />
Limited Access to<br />
<strong>Health</strong>y Foods 3 3 3 3 1 2 1 16<br />
Substance Abuse 4 2 0 4 1 4 1 16<br />
Diabetes 3 3 0 4 1 4 3 18<br />
Aging Problems 3 2 4 4 1 3 3 20<br />
High Blood Pressure<br />
3 3 0 4 1 3 3 17<br />
Mental <strong>Health</strong> 4 3 3 4 1 4 2 21<br />
Child<br />
Abuse/neglect 3 4 0 4 1 1 13 14<br />
Dental 3 4 3 2 1 1 1 15<br />
<strong>Health</strong> Care Costs 0 4 3 3 1 3 3 17<br />
Lack of Transportation<br />
2 2 1 1 1 1 8<br />
Finally, the <strong>Saint</strong> <strong>Joseph</strong> Berea steering committee came together to evaluate all of the findings. We prioritized based on CHNA data, analysis/evaluation<br />
meeting, secondary data and hospital data/needs. The top five priorities were selected and five sub-committees were formed to deal with each one.<br />
Page 2
<strong>Saint</strong> <strong>Joseph</strong> Berea <strong>Community</strong> <strong>Health</strong> <strong>Needs</strong> <strong>Assessment</strong><br />
APPENDICES<br />
Appendix
Appendix A: <strong>Saint</strong> <strong>Joseph</strong> Berea CHNA Advisory Committee<br />
There were two groups that oversaw the work of completing the <strong>Saint</strong> <strong>Joseph</strong> Berea CHNA:<br />
<strong>Saint</strong> <strong>Joseph</strong> Berea CHNA Project Steering Committee<br />
Greg Gerard, President<br />
<strong>Saint</strong> <strong>Joseph</strong> Berea<br />
Chris Schill, Director<br />
<strong>Saint</strong> <strong>Joseph</strong> Berea Foundation<br />
Kate Heckman, Public Relations<br />
<strong>Saint</strong> <strong>Joseph</strong> Berea<br />
Chris Schweighardt, CNO/COO<br />
<strong>Saint</strong> <strong>Joseph</strong> Berea<br />
Elena Baker, Employee <strong>Health</strong>/Education<br />
<strong>Saint</strong> <strong>Joseph</strong> Berea<br />
Ruth Hawkins, Director<br />
Madison County <strong>Health</strong> Dept<br />
Flora Washburn, Mgr, Mission Services<br />
<strong>Saint</strong> <strong>Joseph</strong> Berea<br />
<strong>Saint</strong> <strong>Joseph</strong> Berea CHNA <strong>Community</strong> Advisory Committee<br />
Carla Gilbert, Retired Pastor<br />
Union Church<br />
Chris Schweighardt, CNO/COO<br />
<strong>Saint</strong> <strong>Joseph</strong> Berea<br />
Cora Fletcher, Director<br />
Berea <strong>Health</strong> Ministries<br />
Elena Baker, RN<br />
<strong>Saint</strong> <strong>Joseph</strong> Berea Education<br />
Flora Washburn, Mgr, Mission Services<br />
<strong>Saint</strong> <strong>Joseph</strong> Berea Mission<br />
Fr Michael Flanagan, Priest<br />
<strong>Saint</strong> Clare's Catholic Church<br />
Greg Gerard, President<br />
<strong>Saint</strong> <strong>Joseph</strong> Berea<br />
Jake Reed, Lieutenant<br />
Berea Police Dept<br />
Jim Rousey, Consultant<br />
Consultant, Kentucky Department for Public<br />
<strong>Health</strong><br />
Kathy Todd, P.E. Teacher<br />
Madison County Schools<br />
Luke Finster, Director<br />
Berea Headstart<br />
Nancy Mowbray, RN<br />
<strong>Saint</strong> <strong>Joseph</strong> Berea RN<br />
Paula Woodman, Director<br />
Berea Senior Citizens<br />
Ruth Hawkins, Director<br />
Madison County <strong>Health</strong> Dept<br />
Sarah Mashburn, OT<br />
<strong>Saint</strong> <strong>Joseph</strong> Berea Rehab<br />
Stephanie Moore, Executive Director<br />
White House Clinic<br />
David Gregory, Chief<br />
Berea Police Dept<br />
Tamara Sandberg, Executive Director<br />
Kentucky Association of Food Banks<br />
<strong>Saint</strong> <strong>Joseph</strong> Berea <strong>Community</strong> <strong>Health</strong> <strong>Needs</strong> <strong>Assessment</strong><br />
2<br />
Appendix 2/19/2013
Appendix B: <strong>Saint</strong> <strong>Joseph</strong> Berea CHNA Timeline<br />
(Updated: October 20, <strong>2012</strong>)<br />
Task 1 Task 2 Task 3<br />
January <strong>2012</strong> Establish <strong>Assessment</strong><br />
Infrastructure<br />
o Facilitator: Flora Washburn<br />
o Steering Committee: SJB<br />
o Data Gatherer: EKU and<br />
Berea College Interns<br />
KyOne Timeline Established<br />
o Jan-June <strong>2012</strong>: start process<br />
o July <strong>2012</strong>: Begin assessment<br />
forums, surveys, etc<br />
o Sept-Oct <strong>2012</strong>: Surveys/forums<br />
completed by end of month<br />
o December 2013 Review data<br />
o January 2013 Draft finalized<br />
o April 2013 Present to Board<br />
o May 2013 Revise and finalize<br />
o June 2013 Publish CHNA<br />
Identify <strong>Community</strong><br />
Representatives<br />
o Key community<br />
representatives<br />
o Identify interest<br />
groups for input<br />
February <strong>2012</strong><br />
Feb 2 – First CHNA community<br />
meeting<br />
Establish meeting schedule<br />
March <strong>2012</strong><br />
No Meeting<br />
April <strong>2012</strong><br />
May <strong>2012</strong><br />
CHNA Committee<br />
o Requirements<br />
o Process<br />
o Timeline<br />
o Resources needed<br />
o Roles<br />
Establish questions for SJB<br />
CHNA survey.<br />
o Answers will help us to know<br />
how to address health issues.<br />
Establish <strong>Assessment</strong> Timeline<br />
o Review requirements<br />
o Review steps<br />
Review meeting schedule after<br />
discussion of timeline<br />
Establish <strong>Community</strong><br />
Definition<br />
o Discuss<br />
appropriate<br />
definition of<br />
geographical area<br />
for “community”<br />
to be completed by<br />
June meeting<br />
No meeting. Correspondence<br />
through email.<br />
June <strong>2012</strong><br />
Plan focus groups; delivery of<br />
survey, process for July<br />
July <strong>2012</strong><br />
Beginning of KyOne FY2013<br />
o Now able to begin surveys<br />
o Now able to have focus group<br />
meetings<br />
o May begin process for<br />
identifying needs<br />
CHNA to be started and completed<br />
within this fiscal year: Begin surveys,<br />
reporting, etc after July, <strong>2012</strong>; report<br />
must be complete and published by<br />
June 30, 2013<br />
August <strong>2012</strong><br />
Focus groups<br />
Interviews<br />
Surveys<br />
Delayed until September due to<br />
production of survey<br />
September <strong>2012</strong><br />
Focus groups<br />
Interviews<br />
Surveys<br />
On target<br />
<strong>Saint</strong> <strong>Joseph</strong> Berea <strong>Community</strong> <strong>Health</strong> <strong>Needs</strong> <strong>Assessment</strong><br />
3<br />
Appendix 2/19/2013
October <strong>2012</strong><br />
November <strong>2012</strong><br />
November <strong>2012</strong><br />
Dec 4, <strong>2012</strong><br />
December <strong>2012</strong><br />
All data to be collected by<br />
October 31.<br />
Focus groups and interviews<br />
extended to November 9.<br />
Organize data and information<br />
that has been collected.<br />
Convene <strong>Community</strong> Committee<br />
o Review survey information<br />
o Identify significant needs<br />
Steering Committee Finalizes<br />
<strong>Needs</strong> List<br />
o Review data and input from<br />
community and community<br />
committee<br />
o Identify Top 5 needs<br />
Surveys completed by Oct 31.<br />
Focus groups and interviews<br />
extended.<br />
Develop Draft Report of data<br />
collected and analyzed to present at<br />
Implementation meeting.<br />
Identify <strong>Needs</strong> & implementation<br />
o Committee makes<br />
recommendation on significant<br />
needs<br />
o Identify needs that should not be<br />
addressed and why<br />
Use all data collected to make this<br />
decision.<br />
January 15, 2013 CHNA Draft Report due KentuckyOne <strong>Health</strong> system <strong>Health</strong>y<br />
<strong>Community</strong> committee will review<br />
and prepare board report.<br />
January 24, 2013 SJB Implementation Meeting o Top 5 identified needs<br />
o Identify which needs are<br />
appropriate and financially<br />
feasible for the hospital to meet<br />
o Identify which needs cannot be<br />
met and why<br />
Create an<br />
implementation plan<br />
based on SJB/KYOne<br />
<strong>Health</strong> strategic plan.<br />
February 12, 2013<br />
February-March,<br />
2013<br />
CHNA Written Report and<br />
Implementation plans due<br />
KentuckyOne <strong>Health</strong> system<br />
strategy team reviewing for<br />
implementation plan for system<br />
and strategic plan<br />
Completed report with<br />
implementation strategy to KYOne<br />
Will return to hospitals for questions,<br />
concerns, strategies.<br />
March 2013 Develop System-level plan KentuckyOne <strong>Health</strong> Communities:<br />
Montgomery/Bridges/Francis<br />
April 3, 2013<br />
Present CHNA Reports to the<br />
KyOne Board<br />
o Ask for approval<br />
o Bring back recommendations<br />
May 2013<br />
Convene <strong>Community</strong> Committee<br />
for Final time<br />
o Provide report from KyOne<br />
<strong>Saint</strong> <strong>Joseph</strong> Berea <strong>Community</strong> <strong>Health</strong> <strong>Needs</strong> <strong>Assessment</strong><br />
4<br />
Appendix 2/19/2013
June 2013<br />
board<br />
o Seek final recommendations<br />
Finalize Report for Publication<br />
and Reporting in Schedule H,<br />
Form 990<br />
Make available on hospital website<br />
<strong>Saint</strong> <strong>Joseph</strong> Berea <strong>Community</strong> <strong>Health</strong> <strong>Needs</strong> <strong>Assessment</strong><br />
5<br />
Appendix 2/19/2013
Appendix C: <strong>Saint</strong> <strong>Joseph</strong> Berea Survey Tool<br />
<strong>Saint</strong> <strong>Joseph</strong> Berea <strong>Community</strong> <strong>Health</strong> <strong>Needs</strong> <strong>Assessment</strong><br />
6<br />
Appendix 2/19/2013
Appendix D: Summary of Survey, Focus Groups & Interviews<br />
<strong>Saint</strong> <strong>Joseph</strong> Berea <strong>Community</strong><br />
<strong>Health</strong> <strong>Needs</strong> <strong>Assessment</strong><br />
Results of Survey, Focus Groups & Interviews<br />
Mission of <strong>Saint</strong> <strong>Joseph</strong> Berea<br />
The mission of Catholic <strong>Health</strong> Initiatives is<br />
to nurture the healing ministry of the Church<br />
by bringing it new life, energy and viability in<br />
the 21st century. Fidelity to the Gospel<br />
urges us to emphasize human dignity and<br />
social justice as we move toward the<br />
creation of healthier communities.<br />
<strong>Saint</strong> <strong>Joseph</strong> Berea <strong>Community</strong> <strong>Health</strong> <strong>Needs</strong> <strong>Assessment</strong><br />
7<br />
Appendix 2/19/2013
Vision<br />
Our Vision is to live up to our name as<br />
One CHI<br />
Catholic: Living our Mission and Core Values.<br />
<strong>Health</strong>: Improving the health of the people and<br />
communities we serve.<br />
Initiatives: Pioneering models and systems of care to<br />
enhance care delivery.<br />
Core Values<br />
Reverence<br />
Profound respect and awe for all of creation, the foundation that shapes<br />
spirituality, our relationships with others and our journey to God.<br />
Integrity<br />
Moral wholeness, soundness, fidelity, trust, truthfulness in all we do.<br />
Compassion<br />
Solidarity with one another, capacity to enter into another’s joy and sorrow.<br />
Excellence<br />
Preeminent performance, becoming the benchmark, putting forth our<br />
personal and professional best.<br />
Reviewing the Data<br />
• Purpose: Gather information from our primary<br />
service area regarding health needs and<br />
opportunities<br />
• Data collection:<br />
– Survey: sent to primary service area<br />
– Focus Groups: community groups<br />
– Interviews: community members<br />
<strong>Saint</strong> <strong>Joseph</strong> Berea <strong>Community</strong> <strong>Health</strong> <strong>Needs</strong> <strong>Assessment</strong><br />
8<br />
Appendix 2/19/2013
Survey<br />
• Dates: September – November 9, <strong>2012</strong><br />
• Distribution:<br />
– Random mailing<br />
– Farmers market, health fairs, etc.<br />
– and on-line link<br />
• Number of Questions: 28 questions<br />
– Opportunities for comments: 5<br />
• Respondents: 949<br />
1.<br />
1.<br />
2.<br />
<strong>Saint</strong> <strong>Joseph</strong> Berea <strong>Community</strong> <strong>Health</strong> <strong>Needs</strong> <strong>Assessment</strong><br />
9<br />
Appendix 2/19/2013
3.<br />
4.<br />
Comment: If you have a family member with<br />
Alzheimer's or dementia, what can we do to help them<br />
in our hospital?<br />
• Train employees on how to care for patients with dementia.<br />
• Transportation<br />
• Family resources and support; ways to keep them at home.<br />
• Show them respect and help patient and family maintain dignity.<br />
• Better care and attention for those with dementia when in the hospital.<br />
• Do not let age or dementia be a factor in quality of care when in the ER.<br />
• Medications.<br />
• Compassion, love and care.<br />
• Keep doing what you are doing.<br />
• Listen to the POA/Caregivers! Don't speak to us as if patient is not there!<br />
<strong>Saint</strong> <strong>Joseph</strong> Berea <strong>Community</strong> <strong>Health</strong> <strong>Needs</strong> <strong>Assessment</strong><br />
10<br />
Appendix 2/19/2013
5. If you are a woman over 50,<br />
have you had a mammogram?<br />
84% (404) Yes 16% (77) No<br />
6. If not, what are barriers?<br />
7.<br />
8. Have you or your family been affected by<br />
alcohol abuse?<br />
60.3% No<br />
39.7% Yes<br />
Comments: How do you think alcohol/drug<br />
issues should be addressed?<br />
<strong>Saint</strong> <strong>Joseph</strong> Berea <strong>Community</strong> <strong>Health</strong> <strong>Needs</strong> <strong>Assessment</strong><br />
11<br />
Appendix 2/19/2013
9. What additional health services are needed<br />
locally to better address the health problems<br />
of Berea and the surrounding area?<br />
(15.2%)<br />
(14.8%)<br />
(13.1%)<br />
(8.2%)<br />
(8.2%)<br />
(7.8%)<br />
(32.7%)<br />
10. If the health care services you need were here,<br />
would you utilize them or still go elsewhere?<br />
11. What kind of health care coverage do you have<br />
for anyone in your family 18 years and older?<br />
<strong>Saint</strong> <strong>Joseph</strong> Berea <strong>Community</strong> <strong>Health</strong> <strong>Needs</strong> <strong>Assessment</strong><br />
12<br />
Appendix 2/19/2013
12. In the past 12 months, have you decided to NOT<br />
use any of the following services because of out of<br />
pocket (personal) cost? (Check all that apply.)<br />
13. Do any of the following prevent you or any member<br />
of your household from seeking health care?<br />
(Check all that apply.)<br />
14. How many times a year do you use the<br />
following services?<br />
<strong>Saint</strong> <strong>Joseph</strong> Berea <strong>Community</strong> <strong>Health</strong> <strong>Needs</strong> <strong>Assessment</strong><br />
13<br />
Appendix 2/19/2013
15. Do you use the services of St. <strong>Joseph</strong><br />
Berea?<br />
16. How do you learn about health care services at<br />
<strong>Saint</strong> <strong>Joseph</strong> Berea? (Check all that apply.)<br />
17. In the past 12 months, have you or a family member<br />
been hospitalized at <strong>Saint</strong> <strong>Joseph</strong> Berea for any of<br />
the following? (Check all that apply.)<br />
<strong>Saint</strong> <strong>Joseph</strong> Berea <strong>Community</strong> <strong>Health</strong> <strong>Needs</strong> <strong>Assessment</strong><br />
14<br />
Appendix 2/19/2013
18. How satisfied were you or someone in your<br />
household with the services you received at <strong>Saint</strong><br />
<strong>Joseph</strong> Berea?<br />
34% (25)<br />
43.0% (320)<br />
53.6% (399)<br />
19. Please check all hospitals where you were<br />
hospitalized overnight or sought care in the past 12<br />
months.<br />
20. What is your zip code?<br />
Berea: Madison Co.<br />
Richmond: Madison Co.<br />
Jackson Co.<br />
Rockastle Co.<br />
Garrard Co.<br />
60<br />
59<br />
72<br />
278<br />
404<br />
Overall Madison Co. = 700 Responses<br />
1.) Berea (40403, 40404, 40405) = 404<br />
2.) Richmond (40475, 40476) = 278<br />
3.) Waco (40385) = 18<br />
Overall Jackson Co. = 72 Responses<br />
1.) Mckee (40447) = 45<br />
2.) Annville (40402) = 15<br />
Waco: Madison Co.<br />
Estill Co.<br />
Lincoln Co.<br />
Other<br />
Fayette Co.<br />
Jessamine Co.<br />
18<br />
13<br />
9<br />
9<br />
3<br />
2<br />
3.) Tyner (40486) = 10<br />
4.) Sand Gap (40481) = 1<br />
5.) Gray Hawk (40434 = 1<br />
Overall Rockcastle Co. = 60 Responses<br />
1.) Mt. Vernon (40456) = 42<br />
2.) Brodhead (40409) = 14<br />
3.) Livingston (40445) = 3<br />
4.) Orlando (40460) = 1<br />
Powell Co.<br />
Laurel Co.<br />
1<br />
1<br />
Overall Garrard Co. = 59<br />
1.) Lancaster (40444) = 30<br />
2.) Paint Lick (40461) = 29<br />
0 50 100 150 200 250 300 350 400 450<br />
<strong>Saint</strong> <strong>Joseph</strong> Berea <strong>Community</strong> <strong>Health</strong> <strong>Needs</strong> <strong>Assessment</strong><br />
15<br />
Appendix 2/19/2013
Demographics<br />
• 21. What is Your Gender?<br />
– Male 33.4% (305)<br />
– Female 66.6% (608)<br />
• 22. What is Your Age?<br />
– 0-18 1.2% (11)<br />
– 19-25 2.0% (18)<br />
– 26-39 15.4% (141)<br />
– 40-54 26.1% (239)<br />
– 55-64 24.9% (228)<br />
– 65+ 30.5% (280)<br />
23. What is Your Marital Status?<br />
24. What is the highest level of education<br />
have you completed?<br />
<strong>Saint</strong> <strong>Joseph</strong> Berea <strong>Community</strong> <strong>Health</strong> <strong>Needs</strong> <strong>Assessment</strong><br />
16<br />
Appendix 2/19/2013
Demographics<br />
• What is Your Race?<br />
– White 95.7% (881)<br />
– Black/African American 2.5% (23)<br />
– Hispanic/Latino 0.8% (7)<br />
– Native American 1.1% (10)<br />
– Other 1.0% (9)<br />
• What is Your Employment Status?<br />
– Full Time 44% (404)<br />
– Retired 38.6% (354)<br />
– Unemployed 7.1% (65)<br />
– Part Time 6.4% (59)<br />
– Student 3.2% 29)<br />
27. What is Your Household Income?<br />
28. What counties do you go to for health<br />
services (doctor, hospital, dentist, etc.)?<br />
<strong>Saint</strong> <strong>Joseph</strong> Berea <strong>Community</strong> <strong>Health</strong> <strong>Needs</strong> <strong>Assessment</strong><br />
17<br />
Appendix 2/19/2013
Focus Groups<br />
• Purpose: Meet with community groups to determine<br />
community health needs<br />
• Held in different locations to ensure diverse representation<br />
• There were six focus groups:<br />
– Senior Citizen Advisory Group<br />
– Berea Head Start Center<br />
– Shannon Johnson Elementary<br />
– St. <strong>Joseph</strong> Berea employees/volunteers<br />
– First Responders<br />
– Farristown Baptist Church Event<br />
• Total of 61 participants plus facilitators<br />
Focus Groups – <strong>Health</strong> Issues That Have<br />
Impacted You or the <strong>Community</strong><br />
• Obesity<br />
• Diabetes<br />
• Heart disease<br />
• Cancer<br />
• Oral health<br />
• COPD 2<br />
• Alzheimer’s disease/dementia<br />
• Stroke<br />
• Drugs/alcohol<br />
• Mental health<br />
• Kidney disease<br />
• Shortage of providers in the area<br />
• Limited healthcare services in Berea<br />
overall<br />
• Wait times to see providers<br />
• Medicaid MCO’s not accepted<br />
• Kentucky Spirit ending contract<br />
• Medicaid recipients treated differently<br />
at providers’ offices<br />
• Falls<br />
• Arthritis<br />
• Joint pain<br />
• Vision<br />
• Fibromyalgia<br />
Focus Groups: What is Your Vision of a<br />
<strong>Health</strong> <strong>Community</strong>?<br />
• Outpatient services for mental health issues<br />
• Better access to health care for all:<br />
– access to free/low cost health assessments: blood pressure, diabetes, etc.<br />
(Preventative care)<br />
• Hiking, recreational trails, walking paths, exercise programs, playgrounds,<br />
weight management programs to address obesity<br />
• Incentives for providers to come to Berea (not travel to Lexington)<br />
• Stay at home services for seniors<br />
• <strong>Health</strong>y meals: food banks, fast foods, meal services, education<br />
• Support programs<br />
• Smoking bans<br />
• Environmental concerns: control fumes from factories<br />
<strong>Saint</strong> <strong>Joseph</strong> Berea <strong>Community</strong> <strong>Health</strong> <strong>Needs</strong> <strong>Assessment</strong><br />
18<br />
Appendix 2/19/2013
Focus Groups: What are Resources &<br />
Barriers?<br />
• Two colleges: Berea and EKU<br />
• Addition of Walking/hiking/bike<br />
trails<br />
• Location of the hospital<br />
• Food bank<br />
• Libraries<br />
• Adult day care<br />
• Family centers at schools<br />
• Lack of pediatricians<br />
• Urgent Care not adequate<br />
• Misunderstanding of behavioral<br />
health issues<br />
• Medicaid coverage<br />
• Cost of organic/healthy foods<br />
• Poverty/unemployment<br />
• Lack of preventative services for<br />
low income (Berea <strong>Health</strong><br />
Ministries)<br />
• Lack of sidewalks<br />
What is your perception of <strong>Saint</strong> <strong>Joseph</strong><br />
Berea?<br />
• Very good experience personally and of family members; staff<br />
helpful; friendly caring staff<br />
• Good services for small community<br />
• Atmosphere: spiritual, artwork<br />
• Involvement in and support of the community and schools<br />
• ER experience: good by most, not so good by others:<br />
appreciate the nurses<br />
• Registration for lab, X-rays, etc takes too long<br />
• Unclear as to all services provided (several comments on<br />
need for diabetes education and support; surprised to hear<br />
SJB offered these services)<br />
What is your perception of <strong>Saint</strong> <strong>Joseph</strong><br />
Berea? List of services mentioned.<br />
• Heart Institute<br />
• Outpatient Dietician<br />
• Wound Care Center<br />
• Specialists<br />
• Chemotherapy<br />
• Pain Clinic<br />
• Senior Renewal<br />
• Access to care for those who do not have insurance/financial<br />
resources<br />
<strong>Saint</strong> <strong>Joseph</strong> Berea <strong>Community</strong> <strong>Health</strong> <strong>Needs</strong> <strong>Assessment</strong><br />
19<br />
Appendix 2/19/2013
What’s great about our community?<br />
• Small, beautiful community that is safe for families<br />
• Welcoming, open to diverse groups<br />
• Having a local college and good libraries<br />
• It is a welcoming community with a fascinating<br />
cultural history and positive collaboration between<br />
resources and local agencies! It has a social<br />
conscience and is cognizant of its role as<br />
environmental steward.<br />
Interviews<br />
• Six interviews from community leaders and citizens<br />
• Purpose: input from those directly involved with the<br />
community and services<br />
• Same questions: Responses to questions similar to<br />
focus groups but with more detail<br />
What is your vision for a healthy<br />
community? (In addition to focus groups)<br />
• Strong faith-based community that supports<br />
spiritually, as well as, local community outreach<br />
• Easy access to Lexington for additional services and<br />
specialized treatments<br />
<strong>Saint</strong> <strong>Joseph</strong> Berea <strong>Community</strong> <strong>Health</strong> <strong>Needs</strong> <strong>Assessment</strong><br />
20<br />
Appendix 2/19/2013
What is your perception of <strong>Saint</strong> <strong>Joseph</strong> Berea<br />
overall and of specific programs and services?<br />
• Strong focus on its mission; good services for all no<br />
matter ability to pay<br />
• Concern about government cuts<br />
• Cardiovascular center a good addition<br />
• Need more diabetes education<br />
• Better art in registration (to fit healing environment)<br />
What Resources are Availability? (In addition<br />
to focus groups)<br />
• SJB Patient and Family Fund<br />
• Affordable Care Act<br />
• Food Bank/BUURR<br />
• Urgent Care and ER<br />
• Church offers screenings and ultrasounds annually<br />
through Life Screening<br />
• Wide variety of health practices available<br />
• <strong>Hospital</strong> is nearby<br />
What are the Barriers? (In addition to focus<br />
groups)<br />
• Funding for projects<br />
• Preconception that smaller hospitals not as good as<br />
larger<br />
• Motivation of individuals to change<br />
• A gatekeeper to determine if someone should go to<br />
ER or stay home<br />
• Poverty: people choose between food or health<br />
<strong>Saint</strong> <strong>Joseph</strong> Berea <strong>Community</strong> <strong>Health</strong> <strong>Needs</strong> <strong>Assessment</strong><br />
21<br />
Appendix 2/19/2013
What can our community do to improve the<br />
health and quality of life in the community?<br />
• Expand bike & walking trails<br />
• Offer nutrition programs where people live so they<br />
don’t have to worry about transportation.<br />
• Organize and promote available resources for elderly<br />
• Improve & address mental health issues in a positive<br />
way<br />
• Promote services that are available<br />
What is Great About Our <strong>Community</strong>?<br />
• Libraries, city efforts in wellness<br />
• Art in hospital<br />
• Caring/compassionate hospital<br />
• Small town; safe overall<br />
• Have most of the services that are needed<br />
• People in the community are willing to work together<br />
to achieve a common goal<br />
• Affordable house; close to larger communities<br />
• Jobs<br />
<strong>Saint</strong> <strong>Joseph</strong> Berea <strong>Community</strong> <strong>Health</strong> <strong>Needs</strong> <strong>Assessment</strong><br />
22<br />
Appendix 2/19/2013
Appendix E: CHNA <strong>Community</strong> Meeting December 4, <strong>2012</strong><br />
Analysis and Evaluation of Priority <strong>Needs</strong> Identified<br />
Attendees:<br />
AGENDA:<br />
Name<br />
Albright, Shelia<br />
Balinger, Dale<br />
Finster, Luke<br />
Gerard, Greg<br />
Hill, Darnell<br />
Hawkins, Ruth<br />
Heckman, Kate<br />
Jones, Jenny<br />
Jordison, Lloyd<br />
Lainhart, Jennifer<br />
Moore, Stephanie<br />
Mowbray, Nancy<br />
schill, Chris<br />
Schweighardt, Chris<br />
Shackelford, Lorah<br />
Washburn, Flora<br />
Woodman, Paula<br />
Affiliation<br />
Comprehensive Care<br />
D & B Electric<br />
Head Start<br />
SJB President<br />
Upward Bound Ministries<br />
Madison County <strong>Health</strong> Dept<br />
SJB Public Relations<br />
Berea Parks & Recreation<br />
Madison County <strong>Health</strong> Dept<br />
Hope's Wings<br />
White House Clinics<br />
SJB Emergency room RN<br />
SJB Foundation<br />
SJB CNO/COO<br />
SJB Rehab+B3<br />
SJB Mission Services<br />
Berea Senior Citizens<br />
St. <strong>Joseph</strong> Berea Survey Data Results Presentation – Flora Washburn<br />
Group Processing – Ruth Hawkins, Facilitators<br />
Activity 1: 9:50 – 10:05 Given the mission, vision and values of SJB and the <strong>Community</strong><br />
<strong>Assessment</strong> data, identify the most important health issues or problems for St. <strong>Joseph</strong><br />
Berea <strong>Hospital</strong> to address in the next 3-5 years.<br />
Process:<br />
Utilize a “round robin” format in each group to list issues or problems (10 minutes)<br />
From the list of issues, each group member then selects the most important 5 issues to<br />
be addressed (5 minutes)<br />
(This will be done by each participant being give 5 sticky dots to cast votes. Participants<br />
may place all 5 votes on 1 issue or they may be spread across multiple issues.)<br />
NOTE: While there may be 1 or more health issues or problems to which you are personally<br />
committed, keep in mind that your focus is related to the needs of the community.<br />
Activity 2: 10:05 – 10:30 Related to each of the TOP 5 health issues or problems, in<br />
order of priority, identify KNOWN services currently offered by St. <strong>Joseph</strong> Berea <strong>Hospital</strong>, medical<br />
& community partners that address each of the TOP 5 health issues or problems identified. (Use<br />
“round robin” technique) (25 minutes)<br />
<strong>Saint</strong> <strong>Joseph</strong> Berea <strong>Community</strong> <strong>Health</strong> <strong>Needs</strong> <strong>Assessment</strong><br />
23<br />
Appendix 2/19/2013
Activity 3: 10:30 – 11:00 Related to each of the TOP 5 health issues or problems,<br />
identify service gaps or needed services to address each issue. (Use “round robin” technique.)<br />
(30 minutes)<br />
Activity 4: 11:00 – 11:20 What actions should St. <strong>Joseph</strong> Berea <strong>Hospital</strong> take in meeting<br />
these health issues or problems? (Use “round robin” technique.) (15 minutes)<br />
From the list of actions, each group member then selects the most important 5 actions to be<br />
taken by the hospital over the next 3-5 years. (5 minutes)<br />
(This will be done by each participant being give 5 sticky dots to cast votes. Participants may<br />
place all 5 votes on 1 issue or they may be spread across multiple issues.)<br />
11:20 – 11:45 Small Group Reporting<br />
11:45 – 12:00 Next Step, Q & A<br />
SMALL GROUP GROUND RULES<br />
Silence all cell phone. Please leave the room if you must respond to a call.<br />
Respond briefly to the group activity, thus allowing each participant an opportunity to<br />
take his/her turn.<br />
Maintain respect of views or opinions that might differ from yours.<br />
<strong>Saint</strong> <strong>Joseph</strong> Berea <strong>Community</strong> <strong>Health</strong> <strong>Needs</strong> <strong>Assessment</strong><br />
24<br />
Appendix 2/19/2013
Summary of Priority <strong>Needs</strong> Identified From Meeting<br />
Purpose of Meeting:<br />
The purpose was to analyze/evaluate and prioritize community health needs in order to give the<br />
hospital a base by which to determine which community health needs it can address and which<br />
ones it can’t.<br />
Format:<br />
Meeting included community leaders and hospital leaders with intention of reviewing the data<br />
that was gathered from CHNA hospital survey, focus groups and interviews. Flora Washburn,<br />
SJB Mission Services, and Ruth Hawkins, Madison County <strong>Health</strong> Department, facilitated the<br />
meeting.<br />
Process:<br />
We reviewed the data as a group. Next step was to form into two smaller groups. Group<br />
members worked through 5 (timed) activities to: 1) identify the top 5 needs based on what they<br />
had heard earlier; 2) identify known services; 3) identify service gaps or services needed to<br />
address the needs; 4) recommend what actions <strong>Saint</strong> <strong>Joseph</strong> Berea should take to address the<br />
needs; and then 5) select the most important 5 actions to be taken by the hospital over the next 3-<br />
5 years.<br />
Outcomes:<br />
Activity 1:<br />
Given the mission, vision and values of SJB and the <strong>Community</strong> <strong>Assessment</strong> data, identify the<br />
most important health issues or problems for St. <strong>Joseph</strong> Berea <strong>Hospital</strong> to address in the next 3-5<br />
years.<br />
Group #1<br />
1. Mental health services/Drug addiction<br />
2. Collaboration of care/services<br />
3. Chronic disease prevention<br />
4. Lack of insurance<br />
Group #2<br />
1. <strong>Health</strong>y Family<br />
2. Dental Care<br />
3. Alcohol/Drug Abuse<br />
4. Exercise Programs<br />
5. Address Connection Between Issues/ <strong>Health</strong>y<br />
Education In All Ages<br />
Activity 2:<br />
Related to each of the TOP 5 health issues or problems, in order of priority, identify KNOWN<br />
services currently offered by St. <strong>Joseph</strong> Berea <strong>Hospital</strong>, medical & community partners that address<br />
each of the TOP 5 health issues or problems identified.<br />
Group #1 Group #2<br />
1/2. MENTAL HEALTH/ DRUG ADDICTION<br />
1. HEALTH FAMILY<br />
• Senior Renewal<br />
• WIC<br />
• Contract with The Ridge<br />
• Park/Rec<br />
• Informal relationship with Comp Care • <strong>Health</strong> Dept.<br />
<strong>Saint</strong> <strong>Joseph</strong> Berea <strong>Community</strong> <strong>Health</strong> <strong>Needs</strong> <strong>Assessment</strong><br />
25<br />
Appendix 2/19/2013
• Local chapter of NAMI<br />
3. COLLABORATION OF CARE/ TRANSITION OF CARE<br />
• Case managers help with transition<br />
• Contract with The Ridge<br />
• Referrals to Comp Care, MCHD<br />
• Meetings with nursing homes<br />
• Informal conversation between partners<br />
• EMR interfacing<br />
• Liberty House<br />
4. CHRONIC DISEASE PREVENTION<br />
• Patient education<br />
• Diabetes educator<br />
• Referrals to MCHD Diabetes center<br />
• <strong>Health</strong> promotion marketing<br />
• Screenings at community events<br />
• (blood pressure, glucose, BMI, body<br />
mechanics)<br />
• Schools/Family Resource Center<br />
• Faith Based<br />
• Berea College<br />
• Comp. Care<br />
• Social Services<br />
• KY River Foothill<br />
• Nami<br />
• <strong>Community</strong> Activities<br />
2. DENTAL CARE<br />
• White house clinic<br />
• <strong>Hospital</strong> fund SJB<br />
• Dr. Jones Pediatric Dentist<br />
• Private Dentist<br />
• Ahec (education)<br />
• Private dental insurance/plans<br />
3. ALCOHOL/DRUG ABUSE<br />
• Comp Care<br />
• AA<br />
• Celebrate Recovery<br />
• Allnon<br />
• Tentative Output Program<br />
• Liberty place<br />
• Subxene clinic<br />
• Upward bound<br />
• <strong>Health</strong> Dept.<br />
• Police Dept. (pill drop, educate parents)<br />
• Colleges<br />
• Public School<br />
• Drug court<br />
• Faith house<br />
<strong>Saint</strong> <strong>Joseph</strong> Berea <strong>Community</strong> <strong>Health</strong> <strong>Needs</strong> <strong>Assessment</strong><br />
26<br />
Appendix 2/19/2013
5. LACK OF INSURANCE<br />
• Charity care<br />
• Financial counselor<br />
• <strong>Community</strong> philanthropy<br />
• Auxiliary medication program<br />
4. EXERCISE PROGRAMS<br />
• Body recall<br />
• Parks/ Rec<br />
• YMCA<br />
• Fitness friend/family<br />
• Jazzercise<br />
• Total fitness<br />
• C Berry Center<br />
• Upward bound<br />
• Youth seg.<br />
• Schools<br />
• Senior Center<br />
• Get healthy Berea<br />
5. CONNECTION BETWEEN ISSUES/ HEALTH<br />
EDUCATION IN ALL AGES<br />
• <strong>Health</strong> Dept.<br />
• SJB (health events, lunch & learn)<br />
• Women & <strong>Health</strong><br />
• Parks/Rec<br />
• Schools<br />
• Fitness Centers<br />
• Physicians<br />
• NAMI<br />
• Hopes Wings<br />
• Comp. Care<br />
• Wic<br />
• Head Start / Pre K<br />
Activity 3:<br />
Related to each of the TOP 5 health issues or problems, identify service gaps or needed<br />
services to address each issue.<br />
Group #1 Group #2<br />
1/2. MENTAL HEALTH/ DRUG ADDICTION<br />
• Inconsistent protocol with referrals<br />
from ER<br />
• Lack of local treatment resources<br />
outside hospital<br />
• Lack of providers within hospital<br />
• Lack of training for providers within<br />
Emergency Dept<br />
• Providers dismiss issue as “untreatable”<br />
• Employee assistance program, Lack of<br />
utilization<br />
1. HEALTHY FAMILY<br />
• Communication (between agency)<br />
• Collaboration<br />
• Pro <strong>Health</strong> Counsel (community)<br />
• Increase community resources<br />
• Promote <strong>Health</strong> Education<br />
• Resource Guide<br />
• Berea Educational Website<br />
• Increase dental care for uninsured.<br />
<strong>Saint</strong> <strong>Joseph</strong> Berea <strong>Community</strong> <strong>Health</strong> <strong>Needs</strong> <strong>Assessment</strong><br />
27<br />
Appendix 2/19/2013
3. COLLABORATION OF CARE/ TRANSITION OF<br />
CARE<br />
• Competition for market share hinders<br />
collaboration<br />
• Lack of concentration of services<br />
• Lack of local services<br />
• Lack of awareness of local services<br />
• Lack of collaboration with home<br />
healthy services.<br />
4. CHRONIC DISEASE PREVENTION<br />
• Collaboration of care – Lack of<br />
• Overcoming barriers for specific<br />
populations<br />
• Lack of community<br />
education/community awareness about<br />
services<br />
• Lack of focus on children/collaboration<br />
with schools<br />
• Comprehensive education<br />
5. LACK OF INSURANCE<br />
• Charity care doesn’t meet all needs<br />
• Providers don’t take into account<br />
patient’s financial needs<br />
• Providers not aware of services hospital<br />
has<br />
• Complicated enrollment<br />
• Medicaid limitations<br />
2. DENTAL CARE<br />
• Co Pay Rates<br />
• Affordable dental care<br />
• No orthodontic/ Oral surgeons in Berea<br />
• Need additional dentist<br />
• Dentist not taking Medicaid<br />
• Dental education<br />
3. ALCOHOL/DRUG ABUSE<br />
• Lack mental health issues<br />
• Faith based<br />
• Kids better counseling<br />
• No treatment centers for men<br />
• Family member support groups<br />
• More centers for withdraw patients<br />
4. EXERCISE PROGRAMS<br />
• Lack on education (mental health)<br />
• Fund programs (scholarships for<br />
memberships)-kids activity<br />
• Increase trails (run, bike)<br />
• Increase pedestrian friendly (sidewalks)<br />
• Gyms<br />
• Rec. centers<br />
• Advertisement<br />
5. CONNECTION BETWEEN ISSUES/ HEALTH<br />
EDUCATION IN ALL AGES<br />
• <strong>Community</strong><br />
• Cross education (facility)<br />
• Preventive health<br />
• Collaboration<br />
Activity 4:<br />
What actions should St. <strong>Joseph</strong> Berea <strong>Hospital</strong> take in meeting these health issues or<br />
problems?<br />
Group #1 Group #2<br />
<strong>Saint</strong> <strong>Joseph</strong> Berea <strong>Community</strong> <strong>Health</strong> <strong>Needs</strong> <strong>Assessment</strong><br />
28<br />
Appendix 2/19/2013
1/2. MENTAL HEALTH/ DRUG ADDICTION<br />
• Continue developing outpatient mental<br />
services 5<br />
• Provide training for providers 1<br />
3. COLLABORATION OF CARE/ TRANSITION OF<br />
CARE<br />
• Continued engagement after discharge 4<br />
votes<br />
• Ask-a- nurse 3 votes<br />
• Outpatient inpatient relationshipformalize<br />
the program 2 votes<br />
• Interfacing EMR in region<br />
• Compile list of local services 1 vote<br />
4. CHRONIC DISEASE PREVENTION<br />
• <strong>Health</strong> dept. resource information in<br />
Emergency Dept<br />
• Collaboration with Ky. River<br />
foothills/LKLP for transportations –<br />
raise awareness 2 votes<br />
• Share marketing tools<br />
• Develop community wide health<br />
education calendar 3 votes<br />
• Develop punch card of preventive SVCS<br />
+ info on where you can get them. 4<br />
votes<br />
• Reach out to schools-focus on BCS 3<br />
votes<br />
5. LACK OF INSURANCE<br />
• Have informational sheets available 24/7<br />
(patients/providers) 3 votes<br />
• Connect hospital resources (PFAF) to<br />
patient needs 3 votes<br />
• <strong>Community</strong> Resource Guide – 11 votes<br />
• Wellness Counsel / Pro <strong>Health</strong> Counsel - 8<br />
• Faith based Communication (TV, Radio,<br />
Media)-4<br />
• Connections (partnering together) -4<br />
• <strong>Community</strong> Outreach -3<br />
• Mobile Clinics -3<br />
• Training Staff – 1 vote<br />
Activity 5:<br />
Identify the 5 most important actions to be taken by the hospital over the next 3-5 years.<br />
Group #1 Group #2<br />
<strong>Saint</strong> <strong>Joseph</strong> Berea <strong>Community</strong> <strong>Health</strong> <strong>Needs</strong> <strong>Assessment</strong><br />
29<br />
Appendix 2/19/2013
1. Continue developing outpatient mental services<br />
-5<br />
2. Continued engagement after discharge -4<br />
3. Develop punch card of preventive SVCS +<br />
info on where you can get them -4<br />
4. Ask a Nurse -3<br />
5. Have informational sheets available 24/7<br />
(patients/providers) -3<br />
6. Connect hospital resources (PFAF) to<br />
patient needs -3<br />
7. Develop community wide health education<br />
calendar 3<br />
8. Reach out to schools-focus on BCS -3<br />
1. Develop a community resource guide.<br />
2. Create a wellness council for the<br />
county/community that could work<br />
together.<br />
3. Agencies coming together for direction,<br />
community resources, and partnering<br />
together; better connections<br />
4. Greater awareness of services through faith<br />
based communication (TV, Radio) and<br />
through the media<br />
5. Provide more community outreach; ie:<br />
mobile clinics<br />
<strong>Saint</strong> <strong>Joseph</strong> Berea <strong>Community</strong> <strong>Health</strong> <strong>Needs</strong> <strong>Assessment</strong><br />
30<br />
Appendix 2/19/2013
Appendix F: Acknowledgements<br />
Acknowledgements<br />
The <strong>Saint</strong> <strong>Joseph</strong> Berea Steering Committee was the convening body for this project. Many other<br />
individuals including community residents, key informants, and community-based organizations<br />
contributed to this community health needs assessment.<br />
Project Steering Committee and CHNA Advisory Committee<br />
Special thanks to all the community members, and hospital employees who committed time and<br />
information in order to complete this CHNA project.<br />
Eastern Kentucky University (EKU) and Berea College Professors and Interns<br />
<strong>Saint</strong> <strong>Joseph</strong> Berea was fortunate to have student interns with the cooperation of their professors assist in<br />
completing survey results, interviews and focus groups. They collected data, assisted with focus groups,<br />
worked on special projects and generally agreed to do all that was asked of them. Their assistance in<br />
pulling the pieces together was extremely helpful.<br />
Key Informants<br />
Thank you to the business persons, physicians, city officials, and individuals who participated in our key<br />
informant interview process, offering their perspective on community health needs.<br />
Focus Group Participants<br />
People from different walks of life participated in the Focus Group for <strong>Saint</strong> <strong>Joseph</strong> Berea <strong>Hospital</strong>’s<br />
CHNA. Focus group participants included members of the hospital’s patient advisory council, current and<br />
former patients, patient caregivers, first responders, parents, teachers and county agencies. In order to<br />
protect the privacy of the participants, individual names have not been listed.<br />
<strong>Saint</strong> <strong>Joseph</strong> Berea <strong>Community</strong> <strong>Health</strong> <strong>Needs</strong> <strong>Assessment</strong><br />
31<br />
Appendix 2/19/2013
Appendix G: Resources<br />
Annie E Casey Foundation: <strong>2012</strong> Kids Count Data Book<br />
http://datacenter.kidscount.org/DataBook/<strong>2012</strong>/OnlineBooks/KIDSCOUNT<strong>2012</strong>DataBookFullReport.pdf<br />
Berea, Kentucky City Government website<br />
http://bereaky.gov/for-visitors/community-profile/<br />
County <strong>Health</strong> Rankings<br />
http://www.countyhealthrankings.org/rankings/ranking-methods/download-rankings-data/KY<br />
Dignity <strong>Health</strong> <strong>Community</strong> <strong>Health</strong> <strong>Needs</strong> Index<br />
www.dignityhealth.org/cni<br />
Kentucky <strong>Health</strong> Facts<br />
www.kentuckyhealthfacts.org<br />
Kentucky State Plan on Aging, 2009-<strong>2012</strong><br />
e83a39f95aa5/0/kentuckystateplanonaging2009<strong>2012</strong>finalproofed91009.pdf<br />
Madison County <strong>Health</strong> Department:<br />
MAPP CHNA Update 2011<br />
http://www.madisoncountyhealthdept.org/Documents/<strong>Community</strong>/MAPP2011.pdf<br />
Madison County Comprehensive <strong>Community</strong> <strong>Health</strong> Improvement Plan (MCCHIP) CHIP)<br />
2009-2014 with 2011 Review and Addendum<br />
http://www.madisoncountyhealthdept.org/Documents/<strong>Community</strong>/CHIP%20rv%2011%20<strong>2012</strong>.pdf<br />
Madison County Quick Facts - Berea<br />
http://www.thinkkentucky.com/EDIS/cmnty<br />
Madison County, KY - County <strong>Health</strong> Rankings 2010-<strong>2012</strong> Report<br />
U.S. Census Bureau<br />
http://factfinder2.census.gov<br />
http://chfs.ky.gov/nr/rdonlyres/3045c0d1-a6c0-498a-9347-<br />
Richmond Register newspaper: Nearly One in Four Madison County Children Live in Poverty<br />
http://richmondregister.com/localnews/x175566435/Nearly-1-in-4-Madison-County-children-live-inpoverty<br />
Richmond Register newspaper: 18 Percent in County without <strong>Health</strong> Insurance<br />
<strong>Saint</strong> <strong>Joseph</strong> Berea <strong>Community</strong> <strong>Health</strong> <strong>Needs</strong> <strong>Assessment</strong><br />
32<br />
Appendix 2/19/2013
http://richmondregister.com/localnews/x101449028/18-percent-in-county-without-health-insurance/print<br />
2011 Kentucky <strong>Health</strong> Issues Poll (KHIP)<br />
http://cincinnati.com/blogs/economics/<strong>2012</strong>/03/14/kentuckians-with-higher-incomes-report-better-healthhowever-more-people-living-in-poverty/<br />
<strong>Saint</strong> <strong>Joseph</strong> Berea <strong>Community</strong> <strong>Health</strong> <strong>Needs</strong> <strong>Assessment</strong><br />
33<br />
Appendix 2/19/2013