From Invisible to Visible - Positive Deviance Initiative
From Invisible to Visible - Positive Deviance Initiative
From Invisible to Visible - Positive Deviance Initiative
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
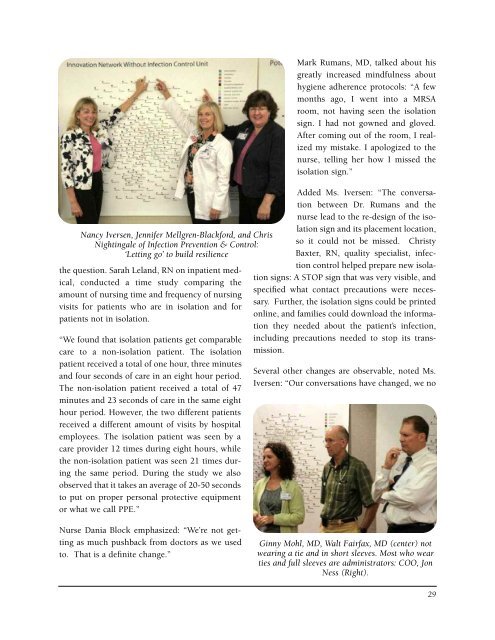
Nancy Iversen, Jennifer Mellgren-Blackford, and Chris<br />
Nightingale of Infection Prevention & Control:<br />
‘Letting go’ <strong>to</strong> build resilience<br />
the question. Sarah Leland, RN on inpatient medical,<br />
conducted a time study comparing the<br />
amount of nursing time and frequency of nursing<br />
visits for patients who are in isolation and for<br />
patients not in isolation.<br />
“We found that isolation patients get comparable<br />
care <strong>to</strong> a non-isolation patient. The isolation<br />
patient received a <strong>to</strong>tal of one hour, three minutes<br />
and four seconds of care in an eight hour period.<br />
The non-isolation patient received a <strong>to</strong>tal of 47<br />
minutes and 23 seconds of care in the same eight<br />
hour period. However, the two different patients<br />
received a different amount of visits by hospital<br />
employees. The isolation patient was seen by a<br />
care provider 12 times during eight hours, while<br />
the non-isolation patient was seen 21 times during<br />
the same period. During the study we also<br />
observed that it takes an average of 20-50 seconds<br />
<strong>to</strong> put on proper personal protective equipment<br />
or what we call PPE.”<br />
Mark Rumans, MD, talked about his<br />
greatly increased mindfulness about<br />
hygiene adherence pro<strong>to</strong>cols: “A few<br />
months ago, I went in<strong>to</strong> a MRSA<br />
room, not having seen the isolation<br />
sign. I had not gowned and gloved.<br />
After coming out of the room, I realized<br />
my mistake. I apologized <strong>to</strong> the<br />
nurse, telling her how I missed the<br />
isolation sign.”<br />
Added Ms. Iversen: “The conversation<br />
between Dr. Rumans and the<br />
nurse lead <strong>to</strong> the re-design of the isolation<br />
sign and its placement location,<br />
so it could not be missed. Christy<br />
Baxter, RN, quality specialist, infection<br />
control helped prepare new isolation<br />
signs: A STOP sign that was very visible, and<br />
specified what contact precautions were necessary.<br />
Further, the isolation signs could be printed<br />
online, and families could download the information<br />
they needed about the patient’s infection,<br />
including precautions needed <strong>to</strong> s<strong>to</strong>p its transmission.<br />
Several other changes are observable, noted Ms.<br />
Iversen: “Our conversations have changed, we no<br />
Nurse Dania Block emphasized: “We’re not getting<br />
as much pushback from doc<strong>to</strong>rs as we used<br />
<strong>to</strong>. That is a definite change.”<br />
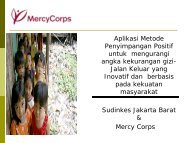
Ginny Mohl, MD, Walt Fairfax, MD (center) not<br />
wearing a tie and in short sleeves. Most who wear<br />
ties and full sleeves are administra<strong>to</strong>rs: COO, Jon<br />
Ness (Right).<br />
29