PDF version - National Hospice and Palliative Care Organization
PDF version - National Hospice and Palliative Care Organization
PDF version - National Hospice and Palliative Care Organization
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
The Monthly Membership Publication of the <strong>National</strong> <strong>Hospice</strong> <strong>and</strong> <strong>Palliative</strong> <strong>Care</strong> <strong>Organization</strong> June 2013<br />
Inside<br />
Determining Caseloads<br />
Gilchrist <strong>Hospice</strong> <strong>Care</strong>’s clinical director,<br />
Regina Shannon Bodnar, walks us through<br />
her use of the NHPCO Staffing Guidelines to<br />
illustrate how valuable it can be in helping to<br />
determine optimal caseloads. “We’ve been<br />
using the Guidelines since 2011,” she says,<br />
“<strong>and</strong> it has helped me delineate differing<br />
needs by service line <strong>and</strong>, in some cases, also<br />
by team.”<br />
Quality on Display<br />
How have providers prepared their staff<br />
for the quality reporting requirements?<br />
Two of the providers that were recognized<br />
for their work by the NHPCO Quality <strong>and</strong><br />
St<strong>and</strong>ards Committee discuss the steps they<br />
took to prepare for implementation of the<br />
Comfortable Dying Measure.<br />
PT in <strong>Hospice</strong><br />
Karen Mueller of the NCHPP Allied Therapist<br />
Steering Committee speaks to the value of<br />
physical therapy in helping hospice patients<br />
<strong>and</strong> families meet their goals of care. (Be sure<br />
to also see the impressive list of published<br />
research on this topic that she provides on<br />
page 29.)<br />
Short Takes:<br />
• Award Winners Recognized at MLC<br />
• Circle of Life Call for Nominations<br />
A Message From Don<br />
Member News <strong>and</strong> Notes<br />
Compliance Tip<br />
Educational Offerings<br />
Videos Worth Watching<br />
News from NHF<br />
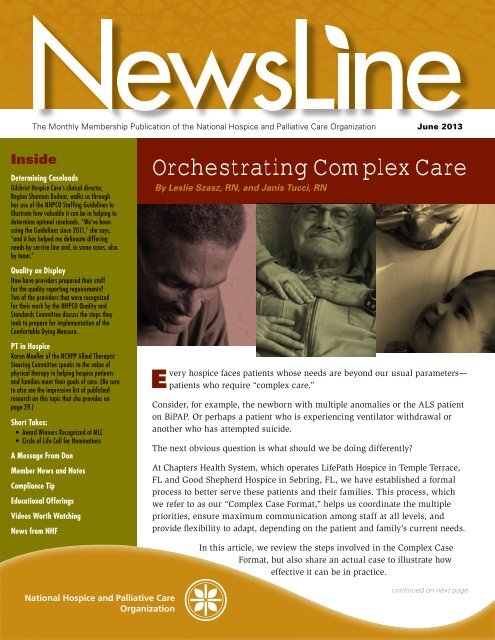
Orchestrating Complex <strong>Care</strong><br />
By Leslie Szasz, RN, <strong>and</strong> Janis Tucci, RN<br />
E<br />
very<br />
hospice faces patients whose needs are beyond our usual parameters—<br />
patients who require “complex care.”<br />
Consider, for example, the newborn with multiple anomalies or the ALS patient<br />
on BiPAP. Or perhaps a patient who is experiencing ventilator withdrawal or<br />
another who has attempted suicide.<br />
The next obvious question is what should we be doing differently?<br />
At Chapters Health System, which operates LifePath <strong>Hospice</strong> in Temple Terrace,<br />
FL <strong>and</strong> Good Shepherd <strong>Hospice</strong> in Sebring, FL, we have established a formal<br />
process to better serve these patients <strong>and</strong> their families. This process, which<br />
we refer to as our “Complex Case Format,” helps us coordinate the multiple<br />
priorities, ensure maximum communication among staff at all levels, <strong>and</strong><br />
provide flexibility to adapt, depending on the patient <strong>and</strong> family’s current needs.<br />
In this article, we review the steps involved in the Complex Case<br />
Format, but also share an actual case to illustrate how<br />
effective it can be in practice.<br />
continued on next page
continued from previous page<br />
The Complex Case<br />
Format<br />
There are four primary steps in<br />
this process:<br />
1. Gather Information<br />
Obtain the past <strong>and</strong> current<br />
medical information about the<br />
patient, but also identify family<br />
dynamics, the decision-makers,<br />
caregivers <strong>and</strong> spokesperson, as<br />
well as what the patient <strong>and</strong> the<br />
family expects <strong>and</strong> wants.<br />
2. Inform All Involved<br />
Advise the patient <strong>and</strong> family<br />
of what to expect from us,<br />
including timeframes <strong>and</strong><br />
specifics such as the name <strong>and</strong><br />
phone number of their hospice<br />
contact person. It’s also equally<br />
important to make sure that<br />
all staff who will be providing<br />
the care have the pertinent<br />
information about the patient<br />
<strong>and</strong> family.<br />
3. Conduct a Complex Case<br />
Conference<br />
Oftentimes conducted as a<br />
conference call, this meeting<br />
should present <strong>and</strong> discuss the<br />
case, <strong>and</strong> ultimately determine<br />
if the hospice should admit or<br />
not admit the patient to service.<br />
Thus, it’s essential that all<br />
necessary parties take part in the<br />
meeting, such as the certifying<br />
physician; MD or ARNP who<br />
will be attending the patient; RN<br />
who has been coordinating the<br />
admission; social worker <strong>and</strong>/or<br />
chaplain; admissions manager;<br />
manager of the receiving team<br />
<strong>and</strong>/or designee; <strong>and</strong> any<br />
specialty staff (e.g., respiratory<br />
or infusion therapist).<br />
4. Debrief<br />
After the high-intensity<br />
portion of the patient’s care is<br />
accomplished, have the same<br />
people who participated in the<br />
conference reconvene to assess<br />
<strong>and</strong> identify what went well <strong>and</strong><br />
what changes might be needed<br />
in future complex cases.<br />
At Chapters, we not only follow<br />
these steps when admitting<br />
a new patient with complex<br />
needs, but also when an existing<br />
patient’s care becomes complex.<br />
By including all of the players in<br />
the discussion—patient, family<br />
<strong>and</strong> staff—everyone underst<strong>and</strong>s<br />
what is expected, each other’s<br />
role <strong>and</strong> function, <strong>and</strong> how the<br />
pieces work together. This level<br />
of coordination helps to reduce<br />
anxiety <strong>and</strong> empowers staff<br />
to make wise decisions. The<br />
process itself can be likened<br />
to that of an orchestra, where<br />
planning <strong>and</strong> communication<br />
ensure a harmonious outcome.<br />
Of course, the dem<strong>and</strong>s <strong>and</strong><br />
available resources for each<br />
hospice may be quite different,<br />
so this format is really only<br />
meant to be a starting point for<br />
your organization, not a “one<br />
size fits all” solution.<br />
continued on page 4<br />
2 NewsLine
Important Points About the<br />
Proposed FY2014 Rule<br />
The Centers for Medicare <strong>and</strong> Medicaid Services released a proposed<br />
rule (posted by CMS on April 29 <strong>and</strong> published in the Federal<br />
Register on May 10) which would update the fiscal year FY2014 hospice<br />
reimbursement rates. But that wasn’t all.<br />
There were a number of other important things addressed that all providers<br />
should be aware of, including: clarification on coding requirements; hospice<br />
quality reporting; an update on hospice payment reform options; a shortstay<br />
add-on payment; rebasing the routine home care rate; a site of service<br />
adjustment for hospice patients in nursing facilities; <strong>and</strong> a cost report<br />
analysis. Given this, please be sure to review the information that our<br />
Regulatory Team makes available. A good place to start is with the NHPCO<br />
Regulatory Alert issued on April 30.<br />
One particular point that concerns me greatly is the claim from CMS that<br />
under the proposed rule hospices would receive “a 1.1 percent market<br />
basket increase” in their reimbursement. As I shared in a message to<br />
members when the proposed rule was posted, the numbers don’t add up.<br />
The impact of sequestration cuts was not calculated in this figure. Under<br />
current law, the CMS proposed payment update would actually mean a<br />
minus 0.9 percent decrease for the nation’s hospice community.<br />
Please be assured that NHPCO, the <strong>Hospice</strong> Action Network <strong>and</strong> our<br />
lobbyists are all working to emphasize the damage that a negative update<br />
would bring to the hospice community. Furthermore, our official letter to<br />
CMS will be submitted by the July deadline for comments.<br />
<strong>Hospice</strong>s are already struggling with an increased regulatory burden,<br />
heightened scrutiny, <strong>and</strong> existing productivity cuts. Given the value<br />
that hospice brings to the federal system <strong>and</strong> the patients <strong>and</strong> families<br />
we serve, we must work collaboratively <strong>and</strong> carry our unified voice to<br />
Capitol Hill.<br />
There is also a part you can play. The <strong>Hospice</strong> Action Network will be<br />
hosting its annual Advocacy Intensive in Washington, DC on July 29 <strong>and</strong><br />
30, 2013. We need to bring as many advocates as possible to the nation’s<br />
capital to carry our voice to members of Congress. And every voice<br />
matters—hospice directors, clinical staff, volunteers, board members <strong>and</strong><br />
supporters! Registration is now open, so please consider joining us.<br />
J. Donald Schumacher, PsyD<br />
President/CEO<br />
NewsLine 3
continued from page 2<br />
How It’s Used at Chapters<br />
At our hospice programs, an RN<br />
begins gathering information<br />
as part of the initial patient<br />
assessment. This includes a<br />
thorough medical-history review<br />
<strong>and</strong> an initial conversation with<br />
the patient <strong>and</strong> family. During<br />
this first meeting, the RN asks<br />
two important questions: What<br />
have the doctors told you about<br />
your situation <strong>and</strong> what do you<br />
want for yourself <strong>and</strong> your loved<br />
one(s)? The RN also explains<br />
what the patient <strong>and</strong> family<br />
should expect from us.<br />
This initial conversation is<br />
tremendously important since<br />
it reveals what the patient <strong>and</strong><br />
family underst<strong>and</strong> about the<br />
patient’s medical condition.<br />
It also helps to identify their<br />
psychosocial, emotional <strong>and</strong><br />
spiritual needs, <strong>and</strong> sheds light<br />
on what the family is prepared<br />
to accept—be that caring for<br />
the patient with the hope of an<br />
improved prognosis or allowing<br />
the patient to experience a<br />
natural death.<br />
If the patient is alert <strong>and</strong><br />
oriented, the conversation is<br />
held with both the patient <strong>and</strong><br />
family. If the patient is comatose,<br />
obtunded, or intermittently<br />
awake, we safeguard <strong>and</strong> respect<br />
the patient’s known desires<br />
through advance directives.<br />
If the patient is only partially<br />
aware, we ask family members<br />
to be present while our staff<br />
talks with the patient <strong>and</strong> strives<br />
for answers to the bottom-line<br />
questions: Do you underst<strong>and</strong><br />
that you are very, very sick? Do<br />
you want to try to get better or<br />
are you ready to let go <strong>and</strong> pass<br />
on? If the patient seems to be<br />
interacting, but does not respond<br />
to a particular question, we then<br />
explain to the family that we<br />
interpret the answer as “I don’t<br />
know.”<br />
When withdrawal of life support<br />
is an issue, we are equally direct<br />
<strong>and</strong> clear in the questions we<br />
pose to the patient: “You know<br />
the tube you have down your<br />
throat? Your family tells me you<br />
want that tube out, is that right?<br />
Do you want that tube removed<br />
even if it means you will die?”<br />
While this questioning may<br />
seem harsh, when voiced with<br />
compassion, it reassures the<br />
patient <strong>and</strong> family that we<br />
are here to honor the patient’s<br />
wishes <strong>and</strong> do what he or she<br />
wants. If the patient is alert <strong>and</strong><br />
aware enough, this questioning<br />
usually elicits a response.<br />
4 NewsLine
Our practice is to follow the<br />
patient’s expressed wishes. If<br />
the patient has been interacting,<br />
but does not answer a particular<br />
question, we interpret this as<br />
“I don’t know,” <strong>and</strong> then stop<br />
the process. If the patient is<br />
unresponsive, we rely on advance<br />
directives. In the absence of<br />
advance directives, we identify<br />
the legal decision-maker<br />
according to our policy.<br />
We conclude the conversation<br />
by explaining what to expect<br />
from us, what might be needed<br />
from them, <strong>and</strong> who will be their<br />
contact persons at our program.<br />
Our admitting nurse then notifies<br />
the receiving team to anticipate<br />
this complex case, <strong>and</strong> arranges<br />
for a social worker <strong>and</strong> chaplain<br />
to meet the patient <strong>and</strong> family to<br />
assess the psycho-social-spiritual<br />
aspects of their lives <strong>and</strong> the<br />
implications for care.<br />
This is the time to clarify who is<br />
considered “family.” Is the patient<br />
legally married to one partner,<br />
but currently living with another<br />
who has assumed that role? Does<br />
the staff at the patient’s long-term<br />
care facility consider themselves<br />
family <strong>and</strong> want to be informed<br />
of the patient’s care at every stage<br />
of decline? If there is complex<br />
care to be rendered, is there<br />
someone who is willing <strong>and</strong> able<br />
to assist in a caregiving capacity?<br />
If so, who will be training them?<br />
What exactly are the orders <strong>and</strong><br />
instructions for that care?<br />
Finally, does your organization’s<br />
policies <strong>and</strong> procedures support<br />
the care that is needed <strong>and</strong><br />
requested? During our review of<br />
the case, a nursing director or<br />
chief clinical officer reviews all<br />
policies that apply to the patient’s<br />
situation. Any questions that<br />
surface from this review must<br />
then be addressed.<br />
In Practice:<br />
The Case of Jimmy<br />
Jimmy was a 32-year-old man<br />
with Down Syndrome, whose<br />
multiple medical conditions had<br />
brought him to a terminal state.<br />
He had been a long-term resident<br />
of a group home that cared for the<br />
developmentally disabled until<br />
his care required admittance to<br />
the area hospital. The group home<br />
<strong>and</strong> hospital were about 150 miles<br />
away from his parents’ home,<br />
which was located in our service<br />
area. Now, given his illness,<br />
his parents wanted to have him<br />
closer to them.<br />
Pages <strong>and</strong> pages of records about<br />
Jimmy arrived at our hospice for<br />
review. The physician <strong>and</strong> staff at<br />
our hospice house reviewed every<br />
page, looking for clues about the<br />
best way to manage his care. We<br />
learned that Jimmy was in fourcontinued<br />
on next page<br />
A nursing director<br />
or chief clinical officer<br />
reviews all policies<br />
that apply to the<br />
patient’s situation.<br />
NewsLine 5
continued from previous page<br />
point restraints at the hospital<br />
where staff described him as<br />
“unmanageable” <strong>and</strong> “physically<br />
aggressive.” The group home<br />
staff, on the other h<strong>and</strong>,<br />
had described him as fairly<br />
independent, <strong>and</strong> needing only<br />
verbal direction <strong>and</strong> guidance.<br />
They also said he only exhibited<br />
aggression when his personal<br />
space was invaded.<br />
Our hospice house manager<br />
contacted Jimmy’s father,<br />
gathered further information<br />
about him, <strong>and</strong> explained what<br />
to expect, including planned<br />
timelines. A Complex Case<br />
Conference was then scheduled<br />
by phone for the same day.<br />
Participants on the call included<br />
our chief clinical officer; a<br />
nursing director; the hospice<br />
house physician, manager <strong>and</strong><br />
team leaders; our infusion<br />
manager; <strong>and</strong> the nurse caring<br />
for Jimmy at the hospital.<br />
During the call we learned<br />
more about this young man’s<br />
physical decline <strong>and</strong> his very<br />
supportive family. His hospital<br />
nurse reported that he was<br />
nonverbal, currently had an IV,<br />
had taken nothing by mouth for<br />
three days, had a Foley catheter<br />
in place, <strong>and</strong> was incontinent.<br />
He was unable to maintain his<br />
body temperature <strong>and</strong> required<br />
a warming blanket at all times.<br />
The hospital nurse also said he<br />
could be physically aggressive<br />
with both h<strong>and</strong>s <strong>and</strong> feet <strong>and</strong><br />
that, for everyone’s safety, had<br />
been restrained during the entire<br />
month of his hospitalization.<br />
By the end of the call, we<br />
had decided to admit him the<br />
next day. We established the<br />
preliminary care plan, identified<br />
several tasks, <strong>and</strong> assigned staff<br />
members for follow-up. The<br />
focus of the plan of care included<br />
establishing communication with<br />
the patient; working to eliminate<br />
the restraints; <strong>and</strong> removing the<br />
IV <strong>and</strong> Foley. The preadmission<br />
tasks included communicating<br />
with staff at his group home;<br />
obtaining a warming blanket;<br />
<strong>and</strong> arranging for his parents to<br />
tour the hospice house <strong>and</strong> sign<br />
the hospice consent forms.<br />
Our team leader made contact<br />
with the patient’s group home.<br />
Our DME manager procured<br />
a warming blanket. The<br />
admissions manager made<br />
multiple calls to ensure a smooth<br />
transfer. The staff members who<br />
were assigned other specific<br />
tasks during the call completed<br />
them <strong>and</strong> reported back to the<br />
manager of the hospice house.<br />
Because everyone worked in<br />
concert, there was no need for a<br />
follow-up call.<br />
6 NewsLine
When Jimmy arrived at the<br />
hospice house, he truly was<br />
restrained at both the wrists <strong>and</strong><br />
ankles. The transport crew from<br />
the hospital reported a relatively<br />
quiet time during transit. Jimmy<br />
was awake, alert <strong>and</strong> looking at<br />
everyone who now surrounded<br />
him. He may have been nonverbal,<br />
but he said volumes<br />
with his eyes. He was calm <strong>and</strong><br />
looked at everyone questioningly<br />
as staff gently held the straps to<br />
his restraints while assessing his<br />
response to us <strong>and</strong> his possible<br />
level of aggression.<br />
Based on what we had learned<br />
in our extensive pre-admission<br />
review of his records, we were<br />
determined to create a calm,<br />
respectful environment for him<br />
<strong>and</strong> his parents. We greeted him<br />
by name, told him our names,<br />
<strong>and</strong> told him that we wanted to<br />
make him comfortable.<br />
“Jimmy took my h<strong>and</strong> <strong>and</strong> at<br />
first, was calm, but then, while<br />
maintaining eye contact with me,<br />
began to press his thumbnail into<br />
my h<strong>and</strong>,” said a member of the<br />
hospice team. “I gently pulled<br />
his thumb away <strong>and</strong> explained<br />
that it hurt me when he did that.<br />
I then assured him that I was not<br />
going to hurt him, so he should<br />
not hurt me. As I released his<br />
thumb, he continued to hold my<br />
h<strong>and</strong>, but without any aggression.<br />
This method of responding to him<br />
was repeated by other staff in the<br />
room when he behaved the same<br />
way with them. Each time, he<br />
stopped the behavior <strong>and</strong> finally,<br />
he stopped altogether. He would<br />
simply allow someone to gently<br />
take his h<strong>and</strong>.”<br />
Based on these interactions,<br />
we were ready to remove the<br />
restraints, but started first by<br />
removing the ankle restraints.<br />
With these removed, he was able<br />
to make himself more comfortable<br />
in bed by pulling his legs up<br />
against himself. There were no<br />
attempts to kick at any of us. Next,<br />
we removed his wrist restraints<br />
<strong>and</strong>, again, there were no attempts<br />
to strike out at any of us.<br />
His IV had become dislodged<br />
during transfer, so the tape was<br />
also removed. Our physician<br />
agreed to leave the IV out for now<br />
<strong>and</strong> see if he would resume eating<br />
<strong>and</strong> drinking. He was offered<br />
water which he drank without<br />
difficulty. Shortly after this, we<br />
removed his catheter <strong>and</strong> used an<br />
adult brief instead.<br />
We also replaced the gown he<br />
was wearing with a t-shirt <strong>and</strong><br />
he relaxed even more. Bless the<br />
volunteers <strong>and</strong> community groups<br />
who support what we do at our<br />
hospice house. We gave him one<br />
of the small, silky smooth quilts<br />
continued on next page<br />
Based on what<br />
we learned, staff<br />
was determined to<br />
create a calm <strong>and</strong><br />
respectful<br />
environment<br />
for him…<br />
NewsLine 7
continued from previous page<br />
they provide <strong>and</strong> he loved it,<br />
stroking both sides <strong>and</strong> then<br />
pulling it up to his chin <strong>and</strong><br />
holding it there. We also gave<br />
him a very soft egg-shaped<br />
pillow made at Easter time by<br />
the local women’s club, which he<br />
also liked. We then offered him<br />
one of the dolls that the local<br />
junior women’s club provides<br />
for our more-restless patients,<br />
but that didn’t go over quite as<br />
well. “Nope, he was all boy,”<br />
said a hospice staff member. “He<br />
pitched it to the end of the bed.”<br />
Fortunately, the staff discovered<br />
that he liked watching baseball,<br />
which helped engage him.<br />
Under the watchful, skilled<br />
<strong>and</strong> compassionate care of our<br />
hospice staff, this young man<br />
was kept comfortable. There<br />
was nothing poking, pulling or<br />
irritating him. Everyone spoke<br />
gently <strong>and</strong> kindly to him. While<br />
a volunteer stayed by his bedside<br />
during his stay at the hospice<br />
house, restraints were never used.<br />
For several days, Jimmy was able<br />
to take food <strong>and</strong> drink again.<br />
His stage II sacral decubitus<br />
began to heal. He rested quietly,<br />
<strong>and</strong> over the next 19 days his<br />
parents <strong>and</strong> brother were at his<br />
bedside throughout the day <strong>and</strong><br />
every evening, finally moving<br />
in <strong>and</strong> staying with him during<br />
the final few days of his life. On<br />
one of those days as he <strong>and</strong> his<br />
father hugged, his mother said<br />
tearfully, “We prayed so hard for<br />
him to live when he was born<br />
<strong>and</strong> now we are praying for God<br />
to take him home.”<br />
Jimmy died at 12:25 on a<br />
summer afternoon, with his<br />
family by his side.<br />
In Closing<br />
Because of the Complex Case<br />
process we followed, this young<br />
man’s care was organized before<br />
his arrival <strong>and</strong> throughout his<br />
stay with us, allowing him <strong>and</strong><br />
his family to find peace <strong>and</strong><br />
closure. It’s also a clear reminder<br />
of why we all work in hospice.<br />
Please see the opposite page<br />
for a print-friendly copy of the<br />
Complex Case Format to print<br />
<strong>and</strong>/or share with staff.<br />
Leslie Szasz is a senior nurse<br />
preceptor at Chapters Health<br />
System, with 38 years of<br />
healthcare experience. In her<br />
current role, she provides both<br />
classroom <strong>and</strong> in-home training<br />
for team preceptors <strong>and</strong> staff.<br />
Janis Tucci has worked in the<br />
field of nursing for 45 years. She<br />
joined LifePath <strong>Hospice</strong> in 2008,<br />
<strong>and</strong> has served as the manager of<br />
Melech <strong>Hospice</strong> House since 2009.<br />
8 NewsLine
The Complex Case Format<br />
Courtesy of Chapters Health System, Temple Terrace, FL<br />
Examples of a Complex Case:<br />
Multiple infusions; inotrope<br />
infusions; new tracheostomy;<br />
pediatrics; complex family or<br />
caregiver dynamics; safety issues;<br />
complex nursing care; withdrawal<br />
of life support.<br />
Purpose of the CC Format:<br />
• Honor the patient <strong>and</strong> family’s<br />
wishes<br />
• Bring together many entities<br />
• Facilitate a very emotional<br />
situation<br />
• Coordinate the plan of care<br />
• Identify <strong>and</strong> address any<br />
staff needs<br />
• Prepare for foreseeable<br />
problems<br />
• Empower staff to address<br />
the unforeseen problems<br />
according to policies <strong>and</strong> the<br />
plan of care.<br />
Steps in the CC Format:<br />
1. 1 Gather Information<br />
• What does the patient want?<br />
• What does the family want?<br />
• Medical history—both the<br />
current <strong>and</strong> past<br />
• Identify family dynamics, the<br />
decision-makers, caregivers<br />
<strong>and</strong> spokesperson<br />
• Determine the physical <strong>and</strong><br />
spiritual needs.<br />
2. 2 Inform All Involved<br />
• Inform the patient <strong>and</strong> family<br />
of what to expect, including<br />
timeframes <strong>and</strong> the name<br />
<strong>and</strong> phone number of their<br />
hospice contact person.<br />
• Provide basic information<br />
about the patient to the<br />
hospice staff who will be<br />
caring for him or her, along<br />
with when the complex case<br />
conference will be held.<br />
3. 3 Determine Who Needs to<br />
Attend the Complex Case<br />
Conference<br />
For example, the certifying<br />
physician; MD or ARNP who<br />
will be attending the patient;<br />
RN who has been coordinating<br />
the admission; social worker<br />
<strong>and</strong>/or chaplain; the admissions<br />
manager; manager of the<br />
receiving team <strong>and</strong>/or designee;<br />
<strong>and</strong> any specialty staff, such<br />
as a respiratory or infusion<br />
therapist.<br />
4. 4 Hold the Complex Case<br />
Conference<br />
The conference, which can be<br />
held by phone or as a meeting,<br />
should present <strong>and</strong> discuss the<br />
case, <strong>and</strong> ultimately determine<br />
if the hospice should admit or<br />
not admit the patient to service.<br />
For example, does the hospice’s<br />
policies <strong>and</strong> procedures support<br />
the care this patient <strong>and</strong> family<br />
needs <strong>and</strong> wants? Are there any<br />
issues or questions that must be<br />
answered or tasks completed<br />
before a decision can be<br />
reached?<br />
If a follow-up conference call is<br />
needed before a decision can<br />
be reached, set up the day <strong>and</strong><br />
time of the call before ending<br />
the current call.<br />
Finally, if you decide to admit<br />
the patient, identify what each<br />
of the staff members is to do at<br />
admission or when the patient is<br />
transferred to your hospice.<br />
5. 5 Debrief<br />
After the high-intensity<br />
portion of the patient’s care is<br />
accomplished, reconvene the<br />
same people who participated<br />
in the CCC to assess <strong>and</strong><br />
identify what went well <strong>and</strong><br />
what changes might be needed<br />
in future complex cases.<br />
NewsLine 9
Determining<br />
Caseloads<br />
Gilchrist <strong>Hospice</strong><br />
<strong>Care</strong> on Its Process<br />
By Regina Shannon Bodnar, RN, MS, MSN, CHPCA<br />
Staffing! Having the right people in the correct numbers is an essential foundation of a<br />
quality-driven hospice organization. But a hospice is not a hospice is not a hospice. In<br />
the same way that you individualize patient care, the art of knowing your ideal caseload<br />
numbers—for clinical staff as well as administrative support—must be based on an insightful<br />
underst<strong>and</strong>ing of both your business model <strong>and</strong> your community.<br />
Fortunately, NHPCO’s “Staffing Guidelines for <strong>Hospice</strong> Home <strong>Care</strong> Teams,” which was released in<br />
March of 2011, walks you through an analysis process to help you determine what your caseloads<br />
should be, based on these factors <strong>and</strong> others.<br />
At Gilchrist <strong>Hospice</strong> <strong>Care</strong> (GHC), where I serve as the director of clinical services, utilizing this<br />
analysis process has helped me delineate differing needs by service line <strong>and</strong>, in some cases, also by<br />
team. And in this article, I show you precisely how. But first, some background.<br />
10 NewsLine
Short Takes:<br />
• Results from the Education N eds A se sment<br />
• VA Reaching Out Grant Recipients<br />
• New NHDD Website<br />
• JPSM Ca l for Papers<br />
• New Volunt er Outreach Materials.<br />
News about NHPCO members.<br />
The Analysis Process<br />
The Staffing Guidelines is a wellorganized<br />
36-page document that<br />
utilizes a multi-step systematic<br />
assessment process to estimate<br />
optimal staffing levels for hospice<br />
programs, with the process broken<br />
out into ‘digestible’ sections.<br />
While an introduction with<br />
an overview is included in the<br />
document, let me briefly review<br />
the process for the purpose of this<br />
discussion:<br />
• Section I covers the “prep”<br />
work you should perform first.<br />
This includes:<br />
- A review of pertinent<br />
statistics from NHPCO’s<br />
<strong>National</strong> Summary of<br />
<strong>Hospice</strong> <strong>Care</strong> to give you<br />
an underst<strong>and</strong>ing of what<br />
hospices, nationwide, are<br />
currently doing; <strong>and</strong><br />
- A review of those factors<br />
that will influence<br />
your final caseload<br />
determinations, such as<br />
length of service, staffing<br />
models (e.g., Admissions<br />
Model; Bereavement<br />
Model); <strong>and</strong> organizational<br />
characteristics.<br />
• Section II covers the actual<br />
staffing analysis process,<br />
which calls for the completion<br />
of two one-page worksheets.<br />
This involves assembling your<br />
hospice data; comparing your<br />
current staffing caseloads to<br />
the national caseload statistics<br />
from the <strong>National</strong> Summary;<br />
<strong>and</strong> estimating your own<br />
staffing caseloads accordingly.<br />
• Section III covers the evaluation<br />
process, <strong>and</strong> is followed<br />
by sections which provide<br />
completed worksheets for three<br />
hospice programs to serve<br />
as examples, a convenient<br />
glossary of terms, <strong>and</strong> the<br />
pertinent tables from the<br />
<strong>National</strong> Summary.<br />
As you can see, implementing<br />
the guidelines does require an<br />
investment of time, but based on<br />
my experience, it is time well spent.<br />
GHC’s Analysis by<br />
Service Line<br />
Gilchrist <strong>Hospice</strong> <strong>Care</strong> (GHC),<br />
which serves patients in the<br />
jurisdictions of Central Maryl<strong>and</strong>,<br />
has an average daily census of<br />
approximately 600 patients. Our<br />
organization is arranged around<br />
three clinical service lines:<br />
1. Inpatient <strong>Care</strong> (44 beds across<br />
two facilities)<br />
2. Facility Based <strong>Care</strong> (three<br />
home hospice teams caring<br />
for patients in skilled nursing<br />
facilities <strong>and</strong> assisted living<br />
communities)<br />
continued on next page<br />
Want More<br />
Background<br />
About the<br />
Guidelines’<br />
Development?<br />
See the introductory<br />
article in the March<br />
2011 issue of<br />
NewsLine, which<br />
includes details<br />
about the rationale<br />
for establishing<br />
the analysis process.<br />
The Monthly Membership Publication of the <strong>National</strong> <strong>Hospice</strong> <strong>and</strong> Pa liative <strong>Care</strong> <strong>Organization</strong> March 2011<br />
Later this month, NHPCO wi l be releasing<br />
the eagerly awaited update to its staffing<br />
ratio recommendations—but it is<br />
far more than just an ‘update.’<br />
The new document, “Staffing<br />
Guidelines for <strong>Hospice</strong> Home<br />
<strong>Care</strong> Teams,” will help each<br />
hospice determine its unique<br />
staffing requirements, based<br />
on its model of delivery,<br />
patient characteristics <strong>and</strong><br />
environmental considerations.<br />
In this article, Tara Brodbeck,<br />
the president/CEO of <strong>Hospice</strong> of<br />
the Miami Va ley <strong>and</strong> the co-chair of<br />
the Task Force charged with developing<br />
the new Guidelines, talks about the tool,<br />
including why a new approach was taken,<br />
the member feedback from field testing,<br />
<strong>and</strong> suggestions on using it.<br />
NHPCO’s New Staffing Guidelines:<br />
No Longer a One-Size-Fits-All Approach<br />
Inside<br />
A Message From Don<br />
NHPCO president/CEO, Don Schumacher, talks abou the new series,<br />
“NHPCO Executive Conversations” <strong>and</strong> why it’ so important now.<br />
Capitol Hi l Day 2011<br />
The Voice of NCHPP<br />
A preview of the April 5-6 agenda <strong>and</strong> why a l member should a tend.<br />
In this monthly feature, we shine the light on the work of NCH P <strong>and</strong><br />
each of its 15 professional sections. This month the QAPI Section is<br />
spotlighted, with an article by E len Martin.<br />
By Tara Brodbeck, MS, RN, CHPN<br />
n 2008, as the NHPCO<br />
Quality <strong>and</strong> St<strong>and</strong>ards<br />
Committee began revising<br />
the St<strong>and</strong>ards of Practice for<br />
<strong>Hospice</strong> <strong>Care</strong> to incorporate<br />
the new <strong>Hospice</strong> CoPs, we<br />
knew it was also time to<br />
take on the cha lenging<br />
task of revising the staffing<br />
ratio recommendations in<br />
NHPCO’s “<strong>Hospice</strong> Services<br />
Guidelines <strong>and</strong> Definitions”<br />
(which had been produced back<br />
in 1994!).<br />
A soon as the project was added to<br />
our committee agenda, questions <strong>and</strong><br />
comments began pouring in from members<br />
across the country. It seemed that many had strong ideas abou the topic<br />
<strong>and</strong> wha the revision should address. Here’s a sampling of the initial<br />
feedback we received:<br />
• Resources for Your Social Work Sta f<br />
• CE/CME Training through NHPCO Webinars<br />
New—<strong>Hospice</strong> in the Continuum:<br />
This month’s feature spotlights PACE at Midl<strong>and</strong> <strong>Care</strong><br />
in Topeka, KS.<br />
Plus:<br />
I<br />
People <strong>and</strong> Places<br />
Educational O ferings<br />
continued on next page<br />
NHPCO conferences, Webinars, webcasts <strong>and</strong> E-OL courses.<br />
NewsLine 11
continued from previous page<br />
3. Home <strong>Hospice</strong> <strong>Care</strong> (six<br />
home hospice teams caring<br />
for patients in private<br />
residences, with one<br />
designated exclusively for<br />
pediatric patients).<br />
Since it was first released,<br />
we have used the guidelines<br />
to analyze our needs <strong>and</strong><br />
appropriately budget resource<br />
dollars for each of these three<br />
service lines.(Gilchrist Kids is<br />
excluded from this discussion<br />
since it is staffed differently,<br />
based on the experience of<br />
pediatric-care colleagues around<br />
the country.)<br />
Some Influencing Factors<br />
As part of the “prep” work that<br />
should precede the analysis, we<br />
considered factors unique to our<br />
organization that will impact<br />
staff caseloads. For example,<br />
across our organization, there<br />
are four particular features of our<br />
programmatic design that heavily<br />
impact staffing:<br />
• We have a NEWS Crew that<br />
covers nights, evenings <strong>and</strong><br />
weekends, <strong>and</strong> is staffed with<br />
RNs, LPNs <strong>and</strong>, to a lesser<br />
degree, supportive services.<br />
This Crew is responsible<br />
for responding to the prescheduled<br />
<strong>and</strong> on-call needs<br />
of our patients <strong>and</strong> families<br />
after business hours <strong>and</strong> on<br />
weekends.<br />
• We also employ a designated<br />
admissions team <strong>and</strong><br />
Hospital Liaison Crew seven<br />
days per week to conduct<br />
introductory visits <strong>and</strong> enroll<br />
eligible patients on service.<br />
• Our bereavement services<br />
are provided by a designated<br />
team of professionals separate<br />
from the interdisciplinary<br />
care team.<br />
• And in late 2011, we<br />
established a daytime triage<br />
team to h<strong>and</strong>le clinical calls<br />
during business hours to<br />
help reduce the number of<br />
interruptions on field staff.<br />
Given this programmatic design,<br />
our primary care teams do not<br />
provide bereavement services,<br />
our clinical teams do not h<strong>and</strong>le<br />
admissions or provide 24/7<br />
coverage (except on six holidays<br />
per year), <strong>and</strong> our supportive<br />
services staff has infrequent<br />
after-hours responsibilities. That<br />
said, additional discernment<br />
by each of our service lines is<br />
required—which I review next.<br />
12 NewsLine
The Guidelines in Practice<br />
Staffing for Facility Based <strong>Care</strong><br />
Our Facility Based <strong>Care</strong> (FBC) is composed of three teams: FBC-East,<br />
FBC-Central <strong>and</strong> FBC-West.<br />
We have long accepted that the care provided by these teams requires<br />
enhanced communication skills (since staff is working with family,<br />
facility staff <strong>and</strong> physicians); flexibility in work hours to ensure aroundthe-clock<br />
attention; <strong>and</strong> a true commitment to building <strong>and</strong> maintaining<br />
a respectful partnership in the care of the patients.<br />
Shown below is the completed copy of Worksheet 1 for this particular<br />
service line (this Worksheet appears on page 17 of the guidelines).<br />
As you see, we entered our data on Length of Service <strong>and</strong> Routine Level<br />
of <strong>Care</strong>, <strong>and</strong> then assigned a directional indicator (+/-/=) to represent<br />
higher, lower or equal caseloads for the categories under the Staffing <strong>and</strong><br />
<strong>Organization</strong>al Models.<br />
Factors Associated With <strong>Care</strong> Model FBC East FBC Central FBC West<br />
Length of Service 101 108 121<br />
Staffing Model<br />
Admission Model +/- + +<br />
On Call Model + + +<br />
RN/LPN Model + = -<br />
Shared Team Model = = =<br />
Bereavement Model + + +<br />
Staff Turnover Rate + + +<br />
<strong>Organization</strong>al Model<br />
Percent of Routine Level of <strong>Care</strong> 99 99 99<br />
Access = = =<br />
Aide/Homemaker Delivery Model + + +<br />
Use of Ancillary Therapy<br />
(e.g. PT/OT; art, music)<br />
+ + +<br />
We discovered<br />
that much was the<br />
same across<br />
our three teams<br />
On completion of the Worksheet, we discovered that much was the same<br />
across our three teams.<br />
We also found that the average Length of Service (LOS) for patients<br />
served by these teams (i.e., 101; 108 <strong>and</strong> 121) was significantly higher<br />
than the national average of 69.1 days as reported in the FY2011 <strong>National</strong><br />
Summary (Table 7), as was the Median LOS of 19.1 days.<br />
continued on next page<br />
NewsLine 13
continued from previous page<br />
In addition, our staff turnover rate of 10.3 percent (<strong>and</strong> 12.3 percent<br />
for nursing) was significantly below the national agency mean of 23.6<br />
percent, as reported in the FY2011 <strong>National</strong> Summary (Table 11).<br />
But a bit of variation bubbled up as well. An LPN floater has been<br />
successfully integrated into the FBC-East team, <strong>and</strong> covers cases when<br />
an RN team member is off. This averts the need for the other RN case<br />
managers to assume coverage responsibilities when a nursing colleague<br />
is using benefit time. Theoretically, the RNs on this team should be able<br />
to carry a slightly larger caseload of patients because they no longer<br />
have coverage responsibilities (or the fluctuation in the patient care<br />
responsibilities that coverage brings with it).<br />
These FBC teams have also expressed an interest in conducting a pilot<br />
to admit their own patients <strong>and</strong> not use the services of the admissions<br />
department. They are hopeful that this will increase the likelihood of<br />
team members connecting earlier with family members, which is a<br />
frequent challenge for patients residing in facilities. Because of greater<br />
flexibility in scheduling, they also hope it will decrease the time<br />
between referral <strong>and</strong> admission. This pilot, which is clearly poised for<br />
success, would dictate the need for smaller RN caseloads.<br />
It is also worth noting that the FBC-Central team has a wellestablished<br />
RN/LPN partnership that provides care across settings<br />
for residents of a large continuing care retirement community. Their<br />
caseload is nearly double that of an RN working independently <strong>and</strong> the<br />
arrangement has resulted in many positives, such as continuity of care,<br />
increased responsiveness to emergent needs, <strong>and</strong> a collegial camaraderie<br />
envied by many. It does not, however, impact the caseload size of other<br />
team members.<br />
14 NewsLine
Let’s now turn to the portion of Worksheet 1 concerning the <strong>Organization</strong>al<br />
Model shown on page 13, but also below.<br />
<strong>Organization</strong>al Model FBC East FBC Central FBC West<br />
Percent of Routine Level of <strong>Care</strong> 99 99 99<br />
Access = = =<br />
Aide/Homemaker Delivery Model + + +<br />
Use of Ancillary Therapy<br />
(e.g. PT/OT; art, music)<br />
+ + +<br />
The percentage of routine patients served by our FBC staff is nearly 2<br />
percentage points higher than the national average as reported in the<br />
FY2011 <strong>National</strong> Summary (99 percent versus 97.1 percent).<br />
We also fully utilize hospice aides, routinely use physical therapy to<br />
promote patient safety, <strong>and</strong> have thriving volunteer <strong>and</strong> music therapy<br />
programs (which are reflected by the directional indicators (+/=) we<br />
assigned to these categories).<br />
Also, the GHC Exp<strong>and</strong>ed <strong>Care</strong> Program of concurrent care is well<br />
established, but not frequently tapped by FBC patients because of their<br />
diagnostic mix <strong>and</strong> other factors. Thus, together, these findings suggest<br />
that GHC disciplines assigned to facility based care teams could carry<br />
caseloads that are larger than those reported in the FY2011 <strong>National</strong><br />
Summary.<br />
continued on next page<br />
Together, these<br />
findings suggested<br />
that GHC disciplines…<br />
could carry larger<br />
caseloads…<br />
NewsLine 15
continued from previous page<br />
Other Factors Impacting Caseloads<br />
Worksheet 2 of the Staffing Guidelines (page 19 of the document) lists<br />
13 other factors to consider when determining staffing caseloads. Our<br />
completed worksheet for the FBC service line is shown below.<br />
Other Factors to Consider<br />
for Staffing Caseloads<br />
FBC<br />
East<br />
FBC<br />
Central<br />
FBC<br />
West<br />
GIP <strong>and</strong> Continuous <strong>Care</strong> Variables = = =<br />
Multiple Non-core Roles for IDT - - -<br />
Facility-based Variables<br />
(routine home care)<br />
Primary <strong>Care</strong> Team Models + + +<br />
Provision of Community Services + + +<br />
Psychosocial Issues:<br />
High Social Complexity<br />
= = =<br />
Rate of Growth = = =<br />
Specialty Programs + + +<br />
Spiritual <strong>Care</strong> Support Model +/- +/- +/-<br />
Staff Safety: Require Multiple Staff<br />
or Escorts/Visits<br />
+ + +<br />
Travel Time: Increased = = -<br />
Volunteer Utilization + + +<br />
Other<br />
We found that, even though we have two stellar inpatient facilities, the<br />
use of our inpatient settings for FBC patients is infrequent. Continuous<br />
care is available <strong>and</strong> is often the first choice for symptomatic patients,<br />
based on the belief that moving an FBC patient from a familiar setting<br />
(<strong>and</strong> the faces they recognize) is frequently not the right thing to do. We<br />
also appreciate that our FBC team members are moving in the direction<br />
of embracing their responsibility as the end-of-life care experts for the<br />
facilities in which they work. This will bring enhanced responsibilities<br />
for FBC team members to conduct resident, family <strong>and</strong> professional<br />
education programs that are presently performed by other employees of<br />
the organization.<br />
One true outlier in our analysis of “Other Factors to Consider” was<br />
travel time for the FBC-West team. This team has a significant cluster of<br />
patients who are located more than 30 miles from the team office. It was<br />
determined that this finding should not affect the caseloads of all team<br />
members, but could most easily be addressed by introducing an RN/<br />
16 NewsLine
LPN partnership to this portion of the service area. Like all partnerships,<br />
the relationship is key to a successful RN/LPN pairing. We are presently<br />
in search of an LPN to complement the talents of the RN in this area.<br />
Until a partnership is launched, however, navigating the geography to<br />
best meet patient needs will be accomplished through well-considered<br />
scheduling <strong>and</strong> continued judicious use of per diem staff.<br />
Another point to note is in regard to our spiritual care support. In<br />
addition to their work with patients <strong>and</strong> families, our chaplains offer<br />
support to facility residents <strong>and</strong> staff members. In conjunction with<br />
our bereavement department, the chaplains conduct memorial services<br />
in many facilities on a quarterly basis. This is balanced by GHC’s<br />
commitment to honor patient <strong>and</strong> family relationships established with<br />
community clergy.<br />
Putting It All Together<br />
When considering all the factors collectively, it was determined that our<br />
RNs could <strong>and</strong> should carry caseloads in slight excess of the national<br />
average of 11 patients, as reported in the FY2011 <strong>National</strong> Summary.<br />
This decision is driven mostly by GHC’s organizational commitment<br />
to our NEWS Crew, admissions team, <strong>and</strong> bereavement department, as<br />
well as our vigorous volunteer program <strong>and</strong> the acknowledgment that<br />
travel for most team members is reduced in time <strong>and</strong> distance due to the<br />
clustering of patients in partner facilities. I do anticipate a modification<br />
to staffing numbers for our FBC-East team once it is positioned to assume<br />
responsibility for conducting its own admissions.<br />
One true<br />
outlier in our<br />
analysis was<br />
travel time….<br />
Staffing for Home <strong>Hospice</strong> <strong>Care</strong><br />
Shown at the top of the next page is Worksheet 1 for our Home <strong>Hospice</strong><br />
<strong>Care</strong> (HHC) service line.<br />
There are five teams in this service line that care for patients <strong>and</strong> their<br />
families in private residences. However, they also receive support from<br />
a NEWS Crew, admissions team, hospital liaisons, triage team, <strong>and</strong><br />
bereavement department. These teams are just beginning to migrate<br />
toward an RN/LPN model of care, with some adapting earlier than others.<br />
These teams are also moving towards a modified Shared Team Model that<br />
translates into all members of the team assuming broader responsibilities.<br />
continued on next page<br />
NewsLine 17
continued from previous page<br />
Factors Associated With <strong>Care</strong> Model Central East West Howard Harvard<br />
Length of Service 68 99 59 97 84<br />
Staffing Model<br />
Admission Model + + + + +<br />
On Call Model + + + + +<br />
RN/LPN Model = = = + +<br />
Shared Team Model = = = = =<br />
Bereavement Model + + + + +<br />
Staff Turnover Rate + + + + +<br />
<strong>Organization</strong>al Model<br />
Percent of Routine Level of <strong>Care</strong><br />
Access - - - - -<br />
Aide/Homemaker Delivery Model + + + + +<br />
Use of Ancillary Therapy<br />
(e.g. PT/OT; art, music)<br />
= = = = =<br />
In looking at the Routine Level of <strong>Care</strong> for these home hospice teams,<br />
note that we have deliberately left that row blank. This is due to an<br />
earlier organizational decision to change team assignments for a patient<br />
when the patient transfers from a home care team to an inpatient<br />
hospice setting. This results in no home hospice team having a patient<br />
at the general inpatient level of care.<br />
Like our FBC teams, our HHC teams recognize the important role<br />
that hospice aides play as care providers <strong>and</strong> team members. We staff<br />
these positions assertively, recognizing that if our aides are to truly<br />
meet the basic needs of patients <strong>and</strong> families, they need to visit them<br />
more frequently than any other member of the team. We are also<br />
assertive in incorporating physical therapists (PT) into all plans of<br />
care, acknowledging that those patients who are ambulatory <strong>and</strong> using<br />
assistive devices potentially benefit most from the skilled assessment<br />
<strong>and</strong> coaching that PT brings to the plan of care. Each of these findings<br />
suggests that the care teams could carry larger caseloads than those<br />
reported in the <strong>National</strong> Summary.<br />
As I noted earlier, GHC also has two stellar inpatient facilities. These<br />
facilities are frequently used by our HHC teams for patients who require<br />
complex symptom management. To facilitate seamless transitions in<br />
care, a bed is reserved at all times for use by home hospice patients. In<br />
18 NewsLine
cases of an anticipated weather emergency, the number of beds allocated<br />
for use by home hospice patients is increased. Given this practice, the<br />
coordination <strong>and</strong> h<strong>and</strong>off of patients is predictably less complex. So, even<br />
though transfers into the inpatient setting happen with regularity, this<br />
design supports the home hospice RN case manager in carrying a larger<br />
caseload.<br />
Other Factors Impacting Caseloads<br />
When assessing other factors that may impact staffing caseloads for<br />
the HHC teams, one team, in particular, st<strong>and</strong>s out as different from<br />
the others. The Central team cares for patients in Baltimore City <strong>and</strong><br />
the edges of the surrounding counties <strong>and</strong>, as shown in Worksheet 2<br />
below, the complexity of psychosocial issues encountered by this team<br />
(as reflected by the directional indicator) suggests that social workers<br />
should carry smaller caseloads. The issue of staff safety is also more<br />
commonplace for this team (also reflected by the directional indicator).<br />
Given that more time is required for the coordination of joint visits <strong>and</strong>/<br />
or the utilization of escort services, it was determined that all clinical<br />
disciplines on the Baltimore Central team should carry slightly smaller<br />
case loads.<br />
Other Factors to Consider<br />
for Staffing Caseloads<br />
Central East West Howard Harvard<br />
GIP <strong>and</strong> Continuous <strong>Care</strong> Variables + + + + +<br />
Multiple Non-core Roles for IDT + + + + +<br />
Facility-based Variables<br />
(routine home care)<br />
n/a n/a n/a n/a n/a<br />
Primary <strong>Care</strong> Team Models + + + + +<br />
Provision of Community Services + + + + +<br />
Psychosocial Issues:<br />
High Social Complexity<br />
- + + + +<br />
Rate of Growth = = = = =<br />
Specialty Programs + + + + +<br />
Spiritual <strong>Care</strong> Support Model +/- +/- +/- +/- +/-<br />
Staff Safety: Require Multiple Staff<br />
or Escorts/Visits<br />
- = = = =<br />
Travel Time: Increased = = = - -<br />
Volunteer Utilization + + + + +<br />
Other<br />
The complexity of<br />
psychosocial issues…<br />
suggested the social<br />
workers should<br />
carry smaller<br />
caseloads.<br />
continued on next page<br />
NewsLine 19
continued from previous page<br />
Putting It All Together<br />
In addition to the factors<br />
already noted, our triage<br />
department manages the<br />
majority of weekday calls<br />
from patients cared for<br />
by our HHC teams. This<br />
supported our determination<br />
that these teams could carry<br />
larger caseloads than the<br />
agency means by discipline,<br />
as reported in the FY2011<br />
<strong>National</strong> Summary (Table<br />
14). And this is by design.<br />
Our goal is to limit “the<br />
asks for work” outside of<br />
direct patient care, so these<br />
teams can focus almost<br />
exclusively on providing<br />
interdisciplinary care that is<br />
true to the core principles of<br />
hospice.<br />
The one exception is our<br />
Central team. The multitude<br />
of complex psychosocial<br />
issues <strong>and</strong> very real safety<br />
concerns associated with the<br />
patients they serve suggests<br />
smaller caseloads are<br />
necessary in order to deliver<br />
quality care <strong>and</strong> a positive<br />
patient <strong>and</strong> family experience.<br />
Travel time for both our<br />
Harford <strong>and</strong> Howard County<br />
teams is also acknowledged<br />
as a potential issue since each<br />
covers a broad geography.<br />
The distribution of patients<br />
is occasionally problematic<br />
<strong>and</strong> must be conscientiously<br />
assessed.<br />
In Closing<br />
The key to staffing success<br />
is the commitment to<br />
thoroughly underst<strong>and</strong>ing all<br />
of the factors which impact<br />
the day-to-day operations<br />
of the clinical program <strong>and</strong><br />
a commitment to re-assess<br />
those factors regularly. As I<br />
hope this article illustrates,<br />
NHPCO’s Staffing Guidelines<br />
can help you get there.<br />
Regina Shannon Bodnar is<br />
a registered nurse with more<br />
than 35 years of clinical <strong>and</strong><br />
leadership experience. She<br />
currently serves as the director<br />
of clinical services for Gilchrist<br />
<strong>Hospice</strong> <strong>Care</strong> in Hunt Valley,<br />
MD, a position she has held<br />
since 1993. She is also an<br />
active member of NHPCO,<br />
including service as both a<br />
member of the Quality <strong>and</strong><br />
St<strong>and</strong>ards Committee <strong>and</strong><br />
the Task Force charged with<br />
development of the NHPCO<br />
Staffing Guidelines.<br />
Staffing Guidelines: Available in <strong>PDF</strong> <strong>and</strong> Print<br />
NHPCO’s Staffing Guidelines for <strong>Hospice</strong> Home <strong>Care</strong> Teams can be<br />
downloaded by members, free of charge, from the NHPCO website.<br />
Printed copies ($14.99 for members) are also available for purchase from the<br />
NHPCO Marketplace—<strong>and</strong> can be ordered online or by calling the NHPCO<br />
Solutions Center at 800-646-6460 (M-F, 8:30 a.m. to 5:30 p.m., ET/EDT)<br />
20 NewsLine
NHPCO would like to thank all the conference attendees, the 2013 MLC Planning Committee <strong>and</strong> our<br />
business partners for making the 2013 MLC a success. On behalf of all who participated in the<br />
conference, we offer our deepest gratitude to the following organizations for their generous<br />
educational grants in support of the 28th Management <strong>and</strong> Leadership Conference.<br />
Thank You.<br />
Platinum Conference Supporter:<br />
Gold Conference Supporters:<br />
Silver Conference Supporters:<br />
Bronze Conference Supporters:<br />
NewsLine 21
quality on DISPlay:<br />
Two Honorees Share Their Work<br />
The NHPCO Quality <strong>and</strong> St<strong>and</strong>ards Committee held its second annual “Quality on Display”<br />
event at the November 2012 Clinical Team Conference.<br />
In light of the hospice quality reporting requirements (<strong>and</strong> the October 1, 2012 deadline to begin<br />
data collection), the Committee asked providers to share—on 4-by-8-foot visual displays—how<br />
they were preparing their organizations <strong>and</strong> staff.<br />
NewsLine is proud to share the work of BAYADA <strong>Hospice</strong> in Moorestown, NJ, <strong>and</strong> <strong>Hospice</strong> of<br />
the Bluegrass in Lexington, KY.<br />
Both organizations chose to showcase their strategies for implementation of the NHPCO<br />
Comfortable Dying Measure (NQF 0209), one of the two measures currently required for quality<br />
reporting to CMS. While their visual displays cannot be duplicated here, each organization has<br />
graciously created a <strong>PDF</strong> presentation that outlines its strategy <strong>and</strong> implementation process.<br />
22 NewsLine
BAYADA <strong>Hospice</strong> • Moorestown, NJ<br />
There were three primary components in our strategy:<br />
• Education: This included<br />
providing staff with an<br />
overview of the NHPCO<br />
Comfortable Dying Measure<br />
<strong>and</strong> a six-page FAQ document,<br />
where detailed answers to the<br />
measure were provided.<br />
• Technology Design: This<br />
included the revamping of<br />
assessments to determine<br />
eligibility for participation<br />
in the measure, as well as<br />
collaboration with our EMR<br />
vendor, Homecare Homebase.<br />
• Process Design: It was also<br />
critical to have a process<br />
in place to identify who in<br />
the organization will be<br />
responsible for the daily<br />
logistics of ensuring that every<br />
patient requiring follow-up<br />
receives it in a timely manner.<br />
While we were strategically<br />
positioned to gather <strong>and</strong> report<br />
on this measure through our<br />
partnership with Homecare<br />
Homebase, it did take several<br />
months to prepare our practice for<br />
this change.<br />
The <strong>Hospice</strong> Services (HOS) office<br />
developed education for our staff<br />
about this new measure, including<br />
a m<strong>and</strong>atory assessment through<br />
the Learning Management System<br />
(LMS). This was accomplished<br />
with much assistance from our<br />
Visit Virtual Office senior associate,<br />
Margaret Donohue, <strong>and</strong> our<br />
Learning Curriculum <strong>and</strong> Design<br />
training manager, Victoria McDevitt.<br />
Changes to the Homecare<br />
Homebase assessments also went<br />
into effect, so that our admissions<br />
nurses could easily identify a<br />
patient who requires follow-up <strong>and</strong><br />
should be reported in this measure.<br />
Additionally, HOS worked with<br />
input from four other hospice<br />
directors—Kristin Barnum, Linda<br />
Trout, Phyllis Tarbell, <strong>and</strong> Angela<br />
Snyder—to determine how to<br />
adapt daily operations to ensure<br />
that BAYADA staff was educated<br />
about this requirement <strong>and</strong><br />
available for the required 48-to-72<br />
hour follow-up, even on weekends<br />
<strong>and</strong> holidays.<br />
Sharon Vogel<br />
Director of <strong>Hospice</strong> Services<br />
While we were<br />
strategically positioned…<br />
to gather <strong>and</strong> report on<br />
this measure… it still<br />
took several months<br />
to prepare….<br />
VIEW THE PRESENTATION<br />
continued on next page<br />
NewsLine 23
continued from previous page<br />
<strong>Hospice</strong> of the Bluegrass • Lexington, KY<br />
<strong>Hospice</strong> of the Bluegrass made<br />
an early commitment to hospice<br />
quality reporting. As part of<br />
our strategic goals for 2012, we<br />
provided updates to the board of<br />
directors as well as our executive<br />
management team. With the tone<br />
at the top set, our next challenge<br />
was to educate clinicians on<br />
the NHPCO Comfortable Dying<br />
Measure (NQF 0209) <strong>and</strong> what<br />
it means to their practice <strong>and</strong><br />
workflow.<br />
The quality team (Compliance<br />
Analyst Tim Shockley; Patient<br />
Safety <strong>and</strong> Infection Control<br />
Nurse Kim Whisman; <strong>and</strong><br />
Compliance Coordinator Gale<br />
Hankins) <strong>and</strong> I were charged<br />
with project implementation, but<br />
success couldn’t be accomplished<br />
without help from the clinical<br />
team, led by Chief Clinical<br />
Officer Deede Byrne. But really,<br />
there isn’t a clinical director,<br />
supervisor, team leader, or<br />
clinician that wasn’t part of the<br />
team. As the saying goes, it takes<br />
a village.<br />
We discussed the measure<br />
regularly at quality meetings,<br />
but also at our clinical director<br />
meetings, team leader meetings<br />
<strong>and</strong> staff meetings. It was also<br />
part of the annual quality<br />
presentation that was conducted<br />
at each office. That was round<br />
one. Round two was a “train the<br />
trainer” PowerPoint that was<br />
used in each office leading up to<br />
the October 1 deadline.<br />
Additionally, we supplied staff<br />
with cheat sheets, flowcharts,<br />
decision trees, electronic<br />
medical record screenshots <strong>and</strong><br />
internally-developed FAQs.<br />
Since communication about<br />
patient needs is h<strong>and</strong>led<br />
differently in our rural offices<br />
which have fewer staff,<br />
leadership chose not to be<br />
prescriptive about each office’s<br />
“h<strong>and</strong>-off communications”<br />
process. Instead, we encouraged<br />
each office to use its established<br />
communications system—why<br />
change it if it already works?<br />
In the month prior to the<br />
October 1 deadline, we tested<br />
our electronic forms, reports <strong>and</strong><br />
clinical processes. A centralized<br />
tracking tool was maintained<br />
in the quality department.<br />
Reminder e-mails <strong>and</strong> voice<br />
mails were spearheaded by our<br />
compliance analyst. Through<br />
these communications, it<br />
became evident that each<br />
office was using some sort<br />
of tracking system to keep<br />
up with admissions <strong>and</strong> the<br />
measure’s questions, so the<br />
quality department created an<br />
individualized tracking tool for<br />
each office’s use.<br />
Eugenia Smither,<br />
RN, BS, CHC, CHE, CHP<br />
Corporate Compliance Officer<br />
Vice President of Compliance<br />
<strong>and</strong> Quality Improvement<br />
VIEW THE PRESENTATION<br />
24 NewsLine
What you don’t know<br />
can hurt you<br />
Federal <strong>and</strong> State Exclusions<br />
Database Searches are<br />
REQUIRED by HHS!<br />
igilance service will<br />
perform the m<strong>and</strong>atory<br />
searching of ALL<br />
databases<br />
Just pennies per name<br />
Compliance<br />
Requires<br />
Vigilance<br />
Seeking Board Eligible/Certified <strong>Hospice</strong><br />
<strong>Palliative</strong> Physician - Bethlehem, PA<br />
St. Luke’s University Health Network based in Bethlehem, PA is<br />
seeking a full-time, board certified or board eligible hospice palliative<br />
care physician. You’ll join a group of 2 physicians <strong>and</strong> provide<br />
inpatient consultative services in 3 hospitals; see outpatient palliative<br />
care patients; <strong>and</strong> have the opportunity to teach in our hospice/<br />
palliative care fellowship program along with medical students<br />
from the Temple/St. Luke’s School of Medicine. St. Luke’s currently<br />
has more than 150 physicians enrolled in internship, residency <strong>and</strong><br />
fellowship programs.<br />
The successful c<strong>and</strong>idate will have strong clinical <strong>and</strong> communication<br />
skills, a commitment to excellence <strong>and</strong> compassion in patient<br />
care that is team oriented. Call is 1:3. Previous <strong>Palliative</strong> <strong>Care</strong> experience<br />
is preferred. In addition, we offer:<br />
• Competitive salary<br />
• Attractive compensation/benefit package<br />
• Relocation assistance<br />
• Malpractice coverage<br />
• CME allowance<br />
Bethlehem, PA is only an hour from Philadelphia <strong>and</strong> 80 miles from<br />
New York City. The area provides numerous cultural, recreational,<br />
shopping <strong>and</strong> educational amenities without the high taxes <strong>and</strong><br />
cost of living of New York <strong>and</strong> New Jersey.<br />
Don’t leave your agency at risk<br />
CliCk Here for more information<br />
Advertisement<br />
information@rocsinc.com<br />
(919) 405-2162<br />
“Thank you so much! This is a huge relief.” <strong>Hospice</strong> Compliance Officer<br />
For more information, contact:<br />
Cindy Stokes<br />
800-678-7858 x64517 | cstokes@cejkasearch.com<br />
ID#149895H66<br />
cejkasearch.com<br />
Advertisement<br />
NewsLine<br />
June 2013<br />
1/4 page<br />
When life gets serious<br />
DTD 149895 IM<br />
you’ll want our serious experience on your side.<br />
It can easily happen.<br />
Your employees <strong>and</strong> volunteers have more on their minds than their driving. It may be<br />
a patient in distress, a grieving family or just the nagging pressure of falling behind a<br />
busy schedule. Auto accidents are a major cause of lawsuits against hospices <strong>and</strong> home<br />
health care agencies as well as a cause of serious injuries <strong>and</strong> lost time.<br />
Lawsuits are expensive to defend, <strong>and</strong> some result in very high-dollar losses. That’s why<br />
liability insurance coverage is so important. Glatfelter Healthcare Practice is administered<br />
by Glatfelter Insurance Group, a national agency. We work closely with your insurance<br />
agent to provide competitive proposals <strong>and</strong> friendly service for special businesses like yours.<br />
Remember, before you can take care of others,<br />
you have to take care of yourself.<br />
Advertisement<br />
Insurance for <strong>Hospice</strong>s <strong>and</strong><br />
Home Health <strong>Care</strong> Agencies<br />
■ Professional Liability<br />
■ General Liability<br />
■ Directors & Officers Liability<br />
■ Property Insurance<br />
■ Non-owned Auto Liability<br />
800-233-1957 www.GlatfelterHealthcarePractice.com<br />
Administered by Glatfelter Underwriting Services, Inc.a/k/a Glatfelter Insurance Services in CA, MN, NV, TX, <strong>and</strong> UT <strong>and</strong> Glatfelter Brokerage Services in NY<br />
NewsLine 25
From the NCHPP Allied Therapist Section*<br />
PT in<br />
<strong>Hospice</strong>:<br />
A Shared<br />
Partnership<br />
for Quality<br />
of Life<br />
By Karen Mueller,<br />
PT, DPT, PhD<br />
While most people<br />
do not view<br />
“physical therapy”<br />
<strong>and</strong> “hospice” as an obvious<br />
partnership, emerging evidence<br />
<strong>and</strong> recent healthcare policy<br />
change suggests that the time<br />
has come to reconsider this<br />
viewpoint.<br />
The Medicare <strong>Hospice</strong> Conditions<br />
of Participation (CoPs), for<br />
example, specifically requires<br />
that “physical therapy services<br />
be made available to patients<br />
<strong>and</strong> provided by licensed<br />
professionals.”<br />
When this rule was included in<br />
the 2008 revision of the <strong>Hospice</strong><br />
CoPs, it was no doubt a source<br />
of confusion among many health<br />
care providers, begging the<br />
question, why would any patient<br />
in hospice need the services of a<br />
physical therapist?<br />
The answer is simple, <strong>and</strong><br />
underscores the shared mission<br />
of NHPCO <strong>and</strong> the American<br />
Physical Therapy Association<br />
(APTA): To improve the quality<br />
of life of those we serve.<br />
Some Compelling Evidence<br />
Although physical therapy services<br />
are generally associated with<br />
the improvement of function<br />
through rehabilitation <strong>and</strong> other<br />
interventions, hospice patients also<br />
seek the best possible quality of<br />
life, which for most, involves the<br />
optimization of remaining function<br />
in light of their hospice diagnosis.<br />
Interventions related to the<br />
enhancement of comfort, function,<br />
energy conservation <strong>and</strong> nonpharmacological<br />
approaches to<br />
pain management are all within<br />
the physical therapy profession’s<br />
scope of practice, <strong>and</strong> these<br />
interventions can be highly<br />
effective for patients in hospice.<br />
By way of example, four powerful<br />
testimonies come to mind:<br />
• A two-year-old boy with a<br />
medulloblastoma underwent<br />
surgical resection <strong>and</strong> placement<br />
of a ventriculo-peritoneal<br />
shunt. <strong>Hospice</strong> physical therapy<br />
enabled his parents to address<br />
developmental sequence<br />
activities, positioning, <strong>and</strong><br />
equipment issues to promote<br />
mobility <strong>and</strong> quality of life<br />
during his months at homes<br />
at home.<br />
*The <strong>National</strong> Council of <strong>Hospice</strong> <strong>and</strong> <strong>Palliative</strong> Professionals (NCHPP) is comprised of 15 discipline-specific<br />
Sections that represents the staff <strong>and</strong> volunteers who work for NHPCO provider-members. To learn more<br />
about this NCHPP Section, visit the NHPCO website.<br />
26 NewsLine
• A 60-year-old female with<br />
metastatic cervical cancer<br />
<strong>and</strong> severe bilateral lower<br />
extremity lymphedema was<br />
able to ambulate with a walker<br />
in her home following manual<br />
lymphatic drainage <strong>and</strong> the<br />
application of compression<br />
b<strong>and</strong>aging.<br />
• A 12-year-old girl with<br />
Charcot-Marie-Tooth disease<br />
developed a glioblastoma<br />
<strong>and</strong> used a wheelchair<br />
following surgical resection,<br />
radiation, <strong>and</strong> experimental<br />
chemotherapy. Six-plus months<br />
of palliative home health<br />
physical therapy enabled her<br />
to gain sufficient strength <strong>and</strong><br />
function to return to school<br />
for her sixth-grade graduation,<br />
ambulating with bilateral<br />
AFOs <strong>and</strong> Lofstr<strong>and</strong> crutches.<br />
With her family, she enjoyed<br />
a Make a Wish trip to the<br />
Philippines. After subsequent<br />
tumor recurrence, she received<br />
hospice physical therapy<br />
services for family training in<br />
dependent transfers <strong>and</strong> bed<br />
care.<br />
• A 60-year-old male with<br />
metastatic brain cancer<br />
receiving home health<br />
hospice services requested<br />
physical therapy intervention<br />
for gait training so that he<br />
could walk to the dining<br />
room table for Thanksgiving<br />
dinner with his family. After<br />
three sessions of physical<br />
therapy intervention—which<br />
included strengthening,<br />
training for st<strong>and</strong>ing balance,<br />
<strong>and</strong> instruction in safe use<br />
of a walker— the patient<br />
accomplished his goal.<br />
Spreading the Word:<br />
HPC Special Interest<br />
Group<br />
Given the constraints of<br />
reimbursement <strong>and</strong> forthcoming<br />
changes to Medicare in light of the<br />
Affordable <strong>Care</strong> Act, members of<br />
the physical therapy profession are<br />
well aware of the need to educate<br />
healthcare professionals on the<br />
value of our services in all areas<br />
of practice, including hospice.<br />
To facilitate this education, former<br />
NHPCO Allied Therapist Section<br />
leader, Richard Briggs, MA, PT,<br />
approached the APTA about<br />
forming a <strong>Hospice</strong> <strong>and</strong> <strong>Palliative</strong><br />
<strong>Care</strong> Special Interest Group (HPC-<br />
SIG), which the APTA approved<br />
<strong>and</strong> officially launched in 2008. I<br />
had the honor of serving as vicechair<br />
of the HPC-SIG for the first<br />
three years, <strong>and</strong> became its chair<br />
in January of 2012.<br />
continued on next page<br />
A Few Facts<br />
Worth Noting<br />
• As of 2012, 224 of<br />
the nation’s 226 PT<br />
educational programs<br />
are at the doctoral level.<br />
• The physical therapist’s<br />
primary role is to<br />
enhance the patient’s<br />
subjective well-being<br />
<strong>and</strong> quality of life<br />
through the assessment,<br />
management <strong>and</strong><br />
prevention of health<br />
related conditions<br />
affecting movement,<br />
motor control <strong>and</strong><br />
function.<br />
• Physical therapists<br />
serve persons of<br />
all ages, from the<br />
youngest newborns to<br />
those at the end of life<br />
(many of whom desire<br />
a level of mobility<br />
in order to meet<br />
important life goals).<br />
• Physical therapists<br />
work with patients in a<br />
variety of care settings,<br />
including the home,<br />
hospital, rehab facility,<br />
<strong>and</strong> assisted living or<br />
long-term care setting.<br />
• According to the<br />
U.S. Bureau of Labor<br />
Statistics, there is an<br />
estimated 198,000<br />
physical therapists<br />
in the U.S. (<strong>and</strong> our<br />
aging population is<br />
expected to create a<br />
high dem<strong>and</strong> for their<br />
services).<br />
NewsLine 27
continued from previous page<br />
In the past five years, members of<br />
the HPC-SIG have made inroads<br />
in three key ways:<br />
• Inter-professional Education:<br />
We have been selected to<br />
present several educational<br />
sessions related to clinical<br />
specialties within our<br />
profession at the annual<br />
APTA Combined Section<br />
Meeting (typically held each<br />
February).<br />
• Outcomes Research: We<br />
have also published research<br />
to identify the impact of our<br />
interventions in a hospice<br />
population (see the bibliography<br />
at the end of this article).<br />
• Clinical Practice: We have<br />
also begun the development<br />
of an outcomes measure<br />
toolbox for the assessment of<br />
patients in hospice.<br />
Our efforts have also involved<br />
similar initiatives at the<br />
international level, with recent<br />
presentations at the World Congress<br />
of Physical Therapy (WCPT) in<br />
Amsterdam in 2011. More recently,<br />
Chris Wilson, the vice chair of<br />
our HPC-SIG, has worked with the<br />
WCPT to establish an international<br />
<strong>Hospice</strong> <strong>and</strong> <strong>Palliative</strong> <strong>Care</strong> Special<br />
Interest Group for the world<br />
community of physical therapists.<br />
Opportunities for a<br />
Future Alliance<br />
As we all know, great minds<br />
think alike <strong>and</strong>, thus, a<br />
prominent initiative of the APTA<br />
HPC-SIG is the establishment<br />
of formal liaisons with other<br />
leading organizations related to<br />
hospice <strong>and</strong> palliative care.<br />
Not surprisingly, NHPCO was<br />
the foremost of such professional<br />
groups, <strong>and</strong> in the past few<br />
months, members of the HPC-SIG<br />
have enjoyed several productive<br />
discussions with NCHPP Allied<br />
Therapist Section leader, Valerie<br />
Hartman, RN, CHPN, CTRN,<br />
which have underscored our<br />
shared values <strong>and</strong> mission.<br />
In the course of our discussions,<br />
we have identified several ways<br />
in which our organizations can<br />
align in the service of optimizing<br />
end-of-life care for all members<br />
of society. The first is the sharing<br />
of resources, particularly those<br />
related to clinical assessment<br />
measures. Both of our<br />
organizations also have helpful<br />
websites, educational conferences,<br />
<strong>and</strong> most importantly, a cadre<br />
of passionate professionals with<br />
a vision for delivering the best<br />
possible services to our patients.<br />
Other countless opportunities<br />
also exist, such as reciprocal<br />
28 NewsLine
attendance at APTA <strong>and</strong> NHPCO<br />
conferences, <strong>and</strong> the sharing of<br />
research, educational materials<br />
<strong>and</strong> clinical guidelines. As other<br />
key agencies, such as the Institute<br />
of Medicine (IOM), address the<br />
future of end-of-life care, each<br />
organization has the potential<br />
to shape future policy. For<br />
example, a member of the APTA<br />
provided public testimony from<br />
the HPC-SIG at the February, 2013<br />
inaugural meeting of the IOM<br />
Committee to transform end-of-life<br />
care. As a result of that meeting,<br />
it is hoped that our members will<br />
have the opportunity to provide<br />
comments <strong>and</strong> suggestions to<br />
future committee proceedings.<br />
Looking Ahead<br />
The anticipated changes in<br />
societal demographics (i.e. the<br />
aging of the 80 million-strong<br />
baby boomers), coupled with<br />
the ongoing restructuring of<br />
our nation’s healthcare delivery<br />
system, create unprecedented<br />
opportunities to enhance costeffective<br />
<strong>and</strong> compassionate<br />
end-of-life care in all realms<br />
of influence. Inter-professional<br />
initiatives will likely become<br />
increasingly prominent as the<br />
preferred means to this end.<br />
Thus, organizations with a<br />
shared mission, such as APTA<br />
<strong>and</strong> NHPCO, may best enhance<br />
their mutual efforts through a<br />
recognized alliance. As a member<br />
of both APTA <strong>and</strong> NHPCO, I<br />
am proud of the work of both<br />
organizations, <strong>and</strong> look forward<br />
to the continued exploration of<br />
effective innovative approaches to<br />
end-of-life care.<br />
Karen Mueller is a professor in<br />
the Physical Therapy Program at<br />
Northern Arizona University in<br />
Flagstaff, AZ. She also serves as<br />
a member of the NCHPP Allied<br />
Therapist Steering Committee <strong>and</strong><br />
chair of the <strong>Hospice</strong> <strong>and</strong> <strong>Palliative</strong><br />
<strong>Care</strong> Special Interest Group of<br />
the American Physical Therapy<br />
Association.<br />
Research Supporting the Role<br />
of PT in <strong>Hospice</strong>:<br />
• Toot J. Physical therapy <strong>and</strong> hospice:<br />
concept <strong>and</strong> practice. Physical Therapy.<br />
1984;62(5):665-671.<br />
• Ebel S. The role of the physical therapist in<br />
hospice care. American Journal of <strong>Hospice</strong><br />
<strong>and</strong> <strong>Palliative</strong> <strong>Care</strong>. 1993;10(5):32-35<br />
• Marcant D, Rapin CH. Role of physiotherapist<br />
in palliative care. Journal of Pain <strong>and</strong><br />
Symptom Management. 1993;8(2):68-71.<br />
• Marciniak CM, Sliwa JA, Spill G,<br />
Heinemann AW, Semik PE: Functional<br />
outcome following rehabilitation of cancer<br />
patient. Archives of Physical Medicine <strong>and</strong><br />
Rehabilitation. 1996;77:54-57.<br />
• Briggs R. Physical therapy in hospice care.<br />
Rehabilitation Oncology. 1997;15(3):16-17.<br />
• Sabers SR, Kokal JE, Girardi JC, Philpott<br />
CL, Basford JR, Therneau TM, Schmidt KD,<br />
Gamble GL.: Evaluation of consultationbased<br />
rehabilitation for hospitalized cancer<br />
patients with functional impairment. Mayo<br />
Clinical Proceedings. 1999;74:855–861<br />
• Mackey KM & Sparling JW. Experiences of<br />
older women with cancer receiving hospice<br />
care: significance for physical therapy.<br />
Physical Therapy. 2000;80:459-468.<br />
continued on next page<br />
We have published<br />
research to identify<br />
the impact of our<br />
interventions on<br />
hospice populations…<br />
NewsLine 29
continued from previous page<br />
• Briggs R. Models for physical therapy<br />
practice in palliative medicine.<br />
Rehabilitation Oncology. 2000;18(2):18-19.<br />
• Frost M. The role of physical,<br />
occupational, <strong>and</strong> speech therapy in<br />
hospice: patient empowerment. American<br />
Journal of <strong>Hospice</strong> <strong>and</strong> <strong>Palliative</strong> <strong>Care</strong>.<br />
2001;18(6):397-402.<br />
• Dal Bello-Haas V. A framework for<br />
rehabilitation of neurodegenerative<br />
diseases: planning care <strong>and</strong> maximizing<br />
quality of life. Neurology Report.<br />
2002;26(3):115-129.<br />
• Nieuwboer A, DeWeerdt W, Dom R,<br />
Bogaerts K. Prediction of outcome of<br />
physical therapy in advanced Parkinson’s<br />
disease. Clinical Rehabilitation.<br />
2002;16(8):886-893.<br />
• Montagini M, Lodhi M, Born W. The<br />
utilization of physical therapy in a<br />
palliative care unit. Journal of <strong>Palliative</strong><br />
Medicine. 2003(6)1:1-17<br />
• Pizzi MA, Briggs R. Occupational <strong>and</strong><br />
physical therapy in hospice: the facilitation<br />
of meaning, quality of life, <strong>and</strong> wellbeing.<br />
Topics in Geriatric Rehabilitation.<br />
2004;20(2):120-130.<br />
• Gudas SA. Terminal Illness, in Psychology<br />
in the Physical <strong>and</strong> Manual Therapies. New<br />
York, NY: Churchill Livingstone; 2004;333-<br />
350.<br />
• Galantino ML, Schimd P, Botis S, Dagan C,<br />
Leonard SM, Milos A. Exploring wellness<br />
coaching <strong>and</strong> traditional group support<br />
for breast cancer survivors: A pilot study.<br />
Rehabilitation Oncology. 2010;28(1):20-24.<br />
• Kumar SP, Jim A. Physical Therapy in<br />
<strong>Palliative</strong> <strong>Care</strong>: From Symptom Control to<br />
Quality of Life: A Critical Review. Indian<br />
Journal <strong>Palliative</strong> <strong>Care</strong>. 2010;16(3):138-146.<br />
• Briggs R, Mueller K. <strong>Hospice</strong> <strong>and</strong> end of<br />
life. In: Guccione AA, Wong RA, Avers D.<br />
(eds.) Geriatric Physical Therapy. 3rd ed. St<br />
Louis: Elsevier;2011.<br />
• Downing GM, Lynd PJ, Gallaher R, Hoens<br />
A. Challenges in underst<strong>and</strong>ing functional<br />
decline, prognosis <strong>and</strong> transitions in<br />
advanced illness. Topics in Geriatric<br />
Rehabilitation. 2011;27(1):18-28.<br />
• Javier NSC, Montagini ML. Rehabilitation<br />
of the hospice <strong>and</strong> palliative care<br />
patient. Journal of <strong>Palliative</strong> Medicine.<br />
2011;14(5):638-648.<br />
• Briggs R. Clinical decision making for<br />
physical therapists in patient-centered<br />
end-of-life care. Topics in Geriatric<br />
Rehabilitation. 2011;27(1):10-17.<br />
• Mueller K, Decker I. Impact of physical<br />
therapy intervention on functional<br />
outcomes <strong>and</strong> quality of life in a<br />
community hospice. Topics in Geriatric<br />
Rehabilitation. 2011:27(1):2-9<br />
• Cobb S, Kennedy N. Physical function<br />
in hospice patients <strong>and</strong> physiotherapy<br />
Interventions: A profile of hospice<br />
physiotherapy. Journal of <strong>Palliative</strong><br />
Medicine. 15(7):760-767.<br />
30 NewsLine
Advertisement<br />
HEALTHCARE CONSULTANTS<br />
NHPCO’S<br />
AFFINITY PROGRAM<br />
NHPCO’s Affinity Program is an exclusive NHPCO<br />
member benefit designed to:<br />
• Enhance your NHPCO membership investment<br />
• Offer unique benefits on price, products, <strong>and</strong> services<br />
• Increase value in your organization<br />
The following selected Affinity Program Partner programs <strong>and</strong> services are available<br />
to NHPCO members, their employees <strong>and</strong> volunteers:<br />
Visit www.nhpco.org/affinity to more info. For membership information,<br />
contact NHPCO Solutions Center at 800/646-6460 <strong>and</strong> ask for the Membership Department.<br />
NewsLine 31
Short Takes<br />
Award Winners<br />
Recognized at MLC<br />
Congressman Earl Blumenauer, a longtime hospice<br />
champion, welcomed more than 2,000 members <strong>and</strong><br />
industry experts to NHPCO’s 28th Management <strong>and</strong><br />
Leadership Conference held on April 25–27.<br />
As part of the conference <strong>and</strong> related events, six<br />
awards were presented to leaders involved in the field.<br />
Inaugural Quality Leadership Award:<br />
Joan Teno, MD, MS<br />
This new award<br />
was established<br />
to recognize<br />
demonstrated<br />
leadership,<br />
commitment, <strong>and</strong><br />
innovation that<br />
have significantly<br />
contributed to<br />
hospice organization excellence <strong>and</strong> improved care<br />
delivery <strong>and</strong> outcomes.<br />
Dr. Teno was recognized as the first recipient of this<br />
award for her work as a researcher <strong>and</strong> a clinician<br />
dedicated to underst<strong>and</strong>ing how to measure <strong>and</strong><br />
improve the quality of care for people at the end of life.<br />
Dr. Teno is a professor of Community Health <strong>and</strong><br />
Medicine <strong>and</strong> associate director of the Center<br />
for Gerontology <strong>and</strong> Health <strong>Care</strong> Research at the<br />
Brown Medical School as well as a health services<br />
researcher <strong>and</strong> hospice medical director. She is<br />
board certified in internal medicine, with added<br />
qualifications in Geriatrics <strong>and</strong> <strong>Palliative</strong> Medicine.<br />
Among her many accomplishments was her work as<br />
the lead investigator in a research effort to create a<br />
Toolkit of Instruments to Measure <strong>Care</strong> at the End of<br />
Life. As part of this grant effort, she also created the<br />
Family Evaluation of <strong>Hospice</strong> <strong>Care</strong>, a longst<strong>and</strong>ing<br />
NHPCO performance measure that is used by<br />
hospices nationwide.<br />
COS, FHSSA <strong>and</strong> NHF Also Present Awards<br />
COS Trailblazer Award<br />
The Council of States awarded Hawaii’s state hospice<br />
<strong>and</strong> palliative care organization, Kokua Mau, the<br />
2012 Trailblazer Award for its development of an<br />
innovative method to improve access to palliative<br />
care <strong>and</strong> increase quality of care among Hawaii’s<br />
providers. Its work, which included exp<strong>and</strong>ing<br />
educational opportunities for private healthcare<br />
plans, can serve as a model for other states.<br />
FHSSA Global Partnership Award<br />
The third annual FHSSA Global Partnership Award<br />
was presented to the Center for <strong>Hospice</strong> <strong>Care</strong> <strong>and</strong><br />
the <strong>Hospice</strong> Foundation of South Bend, Indiana, <strong>and</strong><br />
its partner, the <strong>Palliative</strong> <strong>Care</strong> Association of Ug<strong>and</strong>a<br />
in Kampala, Ug<strong>and</strong>a. To learn more, see the release<br />
on the FHSSA website.<br />
Three NHF Awards<br />
At the <strong>National</strong> <strong>Hospice</strong> Foundation Gala, held on<br />
April 25 in conjunction with the conference, three<br />
awards were presented: the Morfogen Art of Caring<br />
Award to Pulitzer-prize winning journalist, Ellen<br />
Goodman; the Philanthropic Inspiration Award to<br />
Run to Remember founder, Stuart Lazarus; <strong>and</strong><br />
the Buchwald Spirit Award for Public Awareness to<br />
actress <strong>and</strong> hospice volunteer, Torrey DeVitto. To<br />
learn more, see Giving Matters.<br />
32 NewsLine
2014 Circle of Life Award:<br />
Call for Nominations Ends August 5<br />
Sponsored annually, the prestigious Circle of Life Award celebrates<br />
innovation in palliative <strong>and</strong> end-of-life care. In 2014, up to three<br />
organizations will win the award while others may be recognized with<br />
citations of honor.<br />
All organizations or groups in the U.S. that provide palliative or endof-life<br />
care are eligible for the award. As a proud sponsor, NHPCO<br />
encourages all members to participate in the nomination process.<br />
Visit the<br />
Website of<br />
the American<br />
Hospital<br />
The Circle of Life Award: Celebrating Innovation in <strong>Palliative</strong> <strong>and</strong> End-of-Life <strong>Care</strong> is<br />
presented annually to honor organizations striving to improve the care provided to<br />
To nominate<br />
patients<br />
an<br />
with<br />
organization<br />
life-threatening conditions<br />
(either<br />
or near<br />
your<br />
the end<br />
own<br />
of life. In<br />
or<br />
2012,<br />
another),<br />
up to three<br />
visit the<br />
organizations will win Circle of Life Awards; additional organizations may receive<br />
website of the Citations American of Honor. Awards Hospital <strong>and</strong> citations Association will be presented the to American request Hospital an application.<br />
Association Health Forum Summit, July 19-21, 2012, in San Francisco.<br />
But please act soon—applications must be submitted by August 5, 2013.<br />
To nominate an organization or program (either your own or another), please go to<br />
http://www.aha.org/aha/news-center/awards/circle-of-life/circleoflife-nominations.html or<br />
e-mail circleoflife@aha.org. The application is available at<br />
http://www.aha.org/aha/news-center/awards/circle-of-life/application.html. All<br />
organizations or groups in the United States that provide palliative or end-of-life care are<br />
eligible for the award.<br />
Association<br />
to Learn More<br />
Applications are due August 8, 2011.<br />
More information on the award <strong>and</strong> previous recipients is available at<br />
http://www.aha.org/circleoflife. Please call the American Hospital Association Office of<br />
the Secretary at 312/422-2704 or e-mail circleoflife@aha.org with questions about the<br />
award process or application.<br />
Major sponsors for the Circle of Life Award are the American Hospital Association, the<br />
Catholic Health Association, <strong>National</strong> Consensus Project for Quality <strong>Palliative</strong> <strong>Care</strong>, <strong>and</strong><br />
the <strong>National</strong> <strong>Hospice</strong> <strong>and</strong> <strong>Palliative</strong> <strong>Care</strong> <strong>Organization</strong> & <strong>National</strong> <strong>Hospice</strong> Foundation;<br />
the American Academy of <strong>Hospice</strong> <strong>and</strong> <strong>Palliative</strong> Medicine <strong>and</strong> the <strong>National</strong> Association<br />
of Social Workers are Circle of Life cosponsors.<br />
The awards are supported, in part, by grants from the Archstone Foundation <strong>and</strong> the<br />
California Health<strong>Care</strong> Foundation, based in Oakl<strong>and</strong>, California.<br />
NewsLine 33
Member News <strong>and</strong> Notes<br />
$10,000 LIVESTRONG Grant to Benefit<br />
HCC’s <strong>Palliative</strong> <strong>Care</strong> Services<br />
In partnership with <strong>Hospice</strong> & Community <strong>Care</strong><br />
(HCC) based in Lancaster, PA, Lancaster General<br />
Hospital has received a $10,000 grant from the<br />
LIVESTRONG Foundation to advance palliative care<br />
<strong>and</strong> pursue certification.<br />
HCC utilized social<br />
media to spread the<br />
word about the grant<br />
competition <strong>and</strong> to request online votes to support<br />
the palliative program within the community.<br />
While 72 organizations throughout the country<br />
received LIVESTRONG grants, Lancaster General<br />
Health was the only Pennsylvania health system to<br />
win funding for its <strong>Palliative</strong> <strong>Care</strong> program.<br />
HOM Recognized for Mobile App to<br />
Improve Communication with Families<br />
<strong>Hospice</strong> of Michigan (based in Gr<strong>and</strong> Rapids) is<br />
being presented with a Spirit of Innovation Award<br />
at the June Home <strong>Care</strong> & <strong>Hospice</strong> LINK Conference<br />
in Chicago.<br />
Its mobile app, HOM<br />
<strong>Care</strong>s, notifies family<br />
members <strong>and</strong> friends<br />
when a care provider<br />
visits a loved one.<br />
Those who have the<br />
app can see a picture<br />
of the caregiver, the<br />
date <strong>and</strong> duration of the visit, <strong>and</strong> information about<br />
the caregiver’s background <strong>and</strong> type of support<br />
provided— such as medical, spiritual or social work.<br />
The app was developed with a $24,500 gift from<br />
Verizon <strong>and</strong> an in-kind donation from Compuware.<br />
<strong>Hospice</strong> by the Sea Wins the <strong>Hospice</strong><br />
Regattas <strong>National</strong> Championship<br />
The sailors who won the 23 regional hospice<br />
regattas held during 2012 gathered on Florida’s<br />
Tampa Bay during the weekend of April 12 to<br />
compete for the national championship.<br />
<strong>Hospice</strong> by the Sea as it takes the lead in the national<br />
championship. (Photo courtesy of St. Petersburg Yacht Club.)<br />
After three days of intense sailing, the four-man<br />
crew representing <strong>Hospice</strong> by the Sea (Boca Raton,<br />
FL) took first place—led by Captain Bret Moss,<br />
whose gr<strong>and</strong>father had taught him to sail more<br />
than 40 years ago <strong>and</strong> had also been served by<br />
hospice. Special kudus also go to the organization’s<br />
senior director of business development, George<br />
Tokesky, who stepped up at the last minute when<br />
one of the regular crew members had to withdraw<br />
from the race.<br />
Avow Wins 34th Annual Telly Award<br />
Avow (based in Naples, FL) took the Bronze at<br />
the 34th Annual Telly Awards which attracted<br />
more than 11,000 entries from 50 states as well as<br />
numerous countries.<br />
The program was recognized for three of its<br />
current broadcast advertisements which feature<br />
a family testimonial <strong>and</strong> two reenactments.<br />
The campaign was produced by members of the<br />
34 NewsLine
Avow advancement team,<br />
with creative services<br />
assistance from a local<br />
marketing firm. The<br />
commercials can be<br />
viewed at avowcares.<br />
org/video-gallery.<br />
Members of the Avow<br />
advancement team<br />
(l to r): Deborah Jonsson,<br />
Kit Chamberlain, Karen<br />
Stevenson <strong>and</strong> Kylee A. Pitts.<br />
Joint Effort Leads to Second Introductory Class on<br />
<strong>Hospice</strong> <strong>Care</strong> at Prestigious Notre Dame<br />
For the second year in a row, the Center for<br />
<strong>Hospice</strong> <strong>Care</strong> (South Bend, IN) <strong>and</strong> the University<br />
of Notre Dame teamed up to offer students a oneday<br />
introduction to hospice <strong>and</strong> palliative care.<br />
This year’s class, which attracted an impressive<br />
95 students (15 more than last year), featured<br />
12 different presentations that focused on how<br />
hospice <strong>and</strong> palliative care is given in the current<br />
Mark Murray<br />
healthcare system. The presentations were taught<br />
by various members of the interdisciplinary team—including Center for<br />
<strong>Hospice</strong> <strong>Care</strong> CEO, Mark Murray.<br />
Have News to Share?<br />
Add Us to Your Media<br />
Distribution List:<br />
newsline@nhpco.org<br />
NHPCO Staff Lend a H<strong>and</strong> as<br />
Spring for Alex<strong>and</strong>ria Volunteers<br />
More than 400 volunteers spent most<br />
of Friday, May 3, at 50 sites around<br />
Alex<strong>and</strong>ria, VA, as part of “Spring for<br />
Alex<strong>and</strong>ria”—an annual effort to make the<br />
city a cleaner, more beautiful place to live<br />
<strong>and</strong> work.<br />
Joining in were 10 staff from NHPCO,<br />
who painted 10 rooms at a local shelter—<br />
then went the extra mile by doing all the<br />
clean-up!<br />
NewsLine 35
Tip of the Month<br />
Compliance With the<br />
New HIPAA Omnibus Rule<br />
On January 17, 2013, an Omnibus<br />
Final Rule was released by the<br />
U.S. Department of Health <strong>and</strong><br />
Human Services’ Office for Civil Rights.<br />
This Final Rule implements modifications to<br />
HIPAA (the Health Information Technology<br />
for Economic <strong>and</strong> Clinical Health Act 1 )—<br />
<strong>and</strong> marks the most significant re-write of<br />
the HIPAA rules since the law was enacted.<br />
Compliance with most of the new<br />
requirements introduced in this rule<br />
is required by September 23, 2013. An<br />
extended compliance period is provided for<br />
the modification of certain existing business<br />
associate agreements, as described in the rule.<br />
So What Do Providers Need to Do?<br />
Be sure to complete the following updates<br />
by the September 23, 2013 deadline:<br />
• Update your patient privacy notices<br />
• Update your policy on reviewing<br />
<strong>and</strong> reporting a breach of protected<br />
health information (PHI) or electronic<br />
protected health information (ePHI)<br />
• Update your business associate<br />
agreements (unless they qualify for an<br />
extended transition period)<br />
• Update your fundraising communication<br />
to include an “opt-out” option for patients.<br />
Learn More:<br />
NHPCO has developed a helpful information<br />
sheet that gives hospice providers more<br />
details about the final rule. To access the<br />
<strong>PDF</strong>, visit www.nhpco.org/hipaa.<br />
The final rule can also be accessed online<br />
for reference: Omnibus Final Rule.<br />
1<br />
The Federal Register <strong>version</strong> of the Final Rule was<br />
published on January 25, 2013. 78 Fed. Reg. 5566<br />
(Jan. 25, 2013).<br />
Make Sure You See Every<br />
Regulatory Alert <strong>and</strong> Round-Up!<br />
Be sure to bookmark the Regulatory<br />
Alerts <strong>and</strong> Publications webpage<br />
of the NHPCO website for<br />
ongoing reference.<br />
It lists all Alerts <strong>and</strong> Round-Ups issued<br />
in chronological order, so it’s a good<br />
way to make sure you’re up to date<br />
on important news <strong>and</strong> changes<br />
affecting hospice providers.<br />
(These notifications are emailed to<br />
members who opt-in for Regulatory<br />
Communications but, oftentimes,<br />
SPAM filters impede delivery.)<br />
36 NewsLine
New Online Courses<br />
from NHPCO’s E-OL<br />
NHPCO’s End-of-Life Online (E-OL) offers online courses<br />
that are convenient, efficient learning modules for<br />
staff <strong>and</strong> volunteers at all levels of your organization.<br />
Here are a few of the recent additions:<br />
• <strong>Hospice</strong> <strong>and</strong> <strong>Palliative</strong> <strong>Care</strong>, Simply the Best with Ira Byock<br />
• Identifying <strong>and</strong> Addressing Traumatic Stress at the End-Of-Life<br />
with Therese R<strong>and</strong>o<br />
• Shed for Success: How to Stay Alive <strong>and</strong> Thrive in the Midst of<br />
Turbulent Healthcare Change with Kathy Dempsey<br />
• Pediatric <strong>Palliative</strong> <strong>Care</strong> Training Series - Module 7:<br />
Pediatric <strong>Palliative</strong> <strong>Care</strong> Symptom Management<br />
Plus, Several on Volunteer Management <strong>and</strong> Leadership:<br />
• Regulatory Matters for Volunteer Leaders with Judy Lund Person<br />
• Do it Well, Make it Fun, the Key to Success in Volunteer<br />
Management with Ron Culberson<br />
• Ignite your Leadership Potential with Claire Tehan<br />
• The New Breed of Volunteer with Thomas McKee<br />
• Volunteers: Exceptionalism in <strong>Care</strong> <strong>and</strong> Practice with<br />
Gary Gardia <strong>and</strong> Danae Delman<br />
Check Out the New ‘A-Z’ Course List Too:<br />
To easily peruse the range of courses available, visit the<br />
E-OL “A to Z Course List” on the NHPCO website <strong>and</strong><br />
simply scroll <strong>and</strong> click on the offerings of interest.<br />
The webpage about each offering shows the cost of<br />
the course, details about what it covers, <strong>and</strong> whether<br />
it qualifies for CE/CME.
Videos Worth Watching<br />
This year’s <strong>National</strong> <strong>Hospice</strong> Foundation<br />
Gala, held on April 25 in conjunction with<br />
MLC, paid tribute to the youngest <strong>and</strong><br />
bravest we care for in hospice—our pediatric<br />
patients. As part of the event’s program,<br />
NHF aired this moving video <strong>and</strong> raised<br />
$28,000 in just 10 minutes. The money will<br />
go toward development of educational resources to raise awareness among<br />
consumers <strong>and</strong> support the work of providers. Watch the video now−<strong>and</strong><br />
feel free to share it with your colleagues <strong>and</strong> supporters.<br />
(The new edition of NHPCO’s ChiPPS Pediatric <strong>Palliative</strong> <strong>Care</strong> E-newsletter<br />
is now out, with articles about supporting fathers <strong>and</strong> the other male<br />
members of the child’s family. Be sure to take a look.)<br />
Links to Some<br />
Resources on the<br />
NHPCO Website<br />
Quality <strong>and</strong> Regulatory<br />
Quality Reporting Requirements<br />
QAPI Resources<br />
Regulatory Center Home Page<br />
Fraud <strong>and</strong> Abuse<br />
Past Regulatory Alerts <strong>and</strong><br />
Roundups<br />
Staffing Guidelines<br />
St<strong>and</strong>ards of Practice<br />
1731 King Street, Suite 100<br />
Alex<strong>and</strong>ria, VA 22314<br />
703/837-1500<br />
www.nhpco.org • www.caringinfo.org<br />
NewsLine is a publication of the <strong>National</strong> <strong>Hospice</strong> <strong>and</strong> <strong>Palliative</strong> <strong>Care</strong> <strong>Organization</strong><br />
Vice President, Communications . . . . . . . . . . . . . . . . . . . . .Jon Radulovic<br />
Editor . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . Sue Canuteson<br />
Advertising Inquiries . . . . . . . . . . . . . . . . . . Grace Zupancic, 703/837-3134<br />
Membership Inquiries . . . . . . . . . . . . . . . . . . . . . . . . . . . 800/646-6460<br />
Copyright © 2012, NHPCO <strong>and</strong> its licensors. All rights reserved. NHPCO does not<br />
endorse the products <strong>and</strong> services advertised in this publication.<br />
All past issues of NewsLine are posted online: www.nhpco.org/newsline.<br />
State-specific Resources<br />
Quality Partners<br />
Self-Assessment System<br />
Outreach<br />
2013 Volunteer Ads<br />
2012-13 Outreach Materials<br />
Resources to Reach<br />
the Underserved<br />
Professional Education<br />
Education Home Page<br />
2013 Monthly Webinars<br />
End-of-Life Online<br />
NCHPP Home Page<br />
Publications<br />
Past issues of weekly NewsBriefs<br />
Affiliates:<br />
Past issues of monthly NewsLine<br />
Past issues of ChiPPS Newsletter
SPRING 2013<br />
<strong>Hospice</strong> Patient <strong>and</strong> Veteran Visits World<br />
War II Memorial<br />
Honoring Service is an Important Part of One Man’s<br />
End-of-Life Experience<br />
On a brisk Monday morning in April, 92-year-old Veteran Kenneth Baeth<br />
absorbed the sight of the World War II Memorial on the <strong>National</strong> Mall in<br />
Washington, DC for the first time. From the viewpoint of his wheelchair,<br />
Baeth participated in a ceremony honoring his service along with that of<br />
dozens of fellow Veterans from his home state of Montana. Each of the<br />
Veterans was flown to Washington under “Big Sky Honor Flight” a Montana<br />
program that is a member of the Honor Flight Network, a non-profit<br />
organization created to honor America’s WWII Veterans for all their sacrifices.<br />
Kenneth Baeth <strong>and</strong> son, Roger, visit the World War II<br />
Memorial in Washington, DC<br />
• CONTENTS<br />
<strong>Hospice</strong> Patient <strong>and</strong> Veteran Visits World<br />
War II Memorial; page 1<br />
<strong>National</strong> <strong>Hospice</strong> Foundation 9th Annual<br />
Gala; page 2<br />
Lighthouse of Hope Fund Provides<br />
Meaningful <strong>and</strong> Memorable Experiencesfor<br />
Adult <strong>Hospice</strong> Patients; page 3<br />
Foundation Board Chair, Samira Beckwith<br />
Elected Vice-Chair of <strong>National</strong> Coalition of<br />
Cancer Survivorship; page 3<br />
Honor. Remember. Invest.; page 4<br />
NHPCO Begins Collaborative Efforts with<br />
the Funeral Industry; page 4<br />
Run to Remember: A Look at Two Special<br />
Kentucky Bourbon Chase Runners; page 5<br />
The program, with 121 hubs in 41 states, brings World War II Veterans to<br />
Washington, DC so that they may see the memorial erected in their honor.<br />
Baeth is facing the end of life with the help of his children <strong>and</strong> Rocky<br />
Mountain <strong>Hospice</strong>. He traveled to Washington with his oldest son, Roger<br />
<strong>and</strong> several volunteers from Rocky Mountain <strong>Hospice</strong>.<br />
“It takes a lot of courage to get old,” said Roger. His father was nervous about traveling<br />
because of his health, Roger said, but he was loving every minute of the experience. Baeth<br />
contracted mesothelioma as a result of asbestos exposure while working in a mine as a<br />
young man; he is now dying of heart disease. Making the trip required extra physical<br />
therapy to increase his stamina <strong>and</strong> mobility.<br />
At the age of 20, Kenneth Baeth’s dream of flying became a reality when he enlisted in the<br />
U.S. Army Air Corps. It was 1942, in the midst of World War II. St<strong>and</strong>ing at 5’2” tall,<br />
Kenneth Baeth looked like a perfect c<strong>and</strong>idate to be a nose gunner, a man who crawled<br />
inside the nose of a fighter plane to operate a machine gun turret.<br />
“I didn’t dream it would be so big,” Baeth remarked about the memorial. “The U.S. can<br />
pull itself together to do anything,” he said. During the ceremony, Baeth met another nose<br />
gunner who fought in the Pacific during the war. The two exchanged phone numbers <strong>and</strong><br />
planned to talk <strong>and</strong> exchange stories upon returning to Montana.<br />
The <strong>National</strong> <strong>Hospice</strong> <strong>and</strong> <strong>Palliative</strong> <strong>Care</strong> <strong>Organization</strong> works with the U.S. Department of<br />
Veterans Affairs (VA) to meet the unique needs of Veterans like Baeth with terminal illness.<br />
The We Honor Veterans program, developed in collaboration with the VA, provides local<br />
hospices with resources to broaden education <strong>and</strong> underst<strong>and</strong>ing of how best to honor<br />
our Veterans <strong>and</strong> respect their wishes <strong>and</strong> concerns at the end of life. Funds raised by the<br />
<strong>National</strong> <strong>Hospice</strong> Foundation support the We Honor Veterans program.<br />
To learn more about We Honor Veterans, visit: www.wehonorveterans.org.<br />
To learn more about the Honor Flight Network, visit: www.honorflight.org.<br />
To make a donation, visit www.nationalhospicefoundation.org/veterans<br />
A newsletter of the <strong>National</strong> <strong>Hospice</strong> Foundation | Spring 2013 1
Employees of The Elizabeth <strong>Hospice</strong> join in on the NHF Gala Celebration<br />
<strong>National</strong> <strong>Hospice</strong> Foundation 9th Annual Gala<br />
Honored Pediatric <strong>Palliative</strong> <strong>Care</strong> <strong>and</strong> <strong>Hospice</strong><br />
Patients <strong>and</strong> <strong>Care</strong>givers<br />
“Our<br />
celebration<br />
was held in<br />
tribute to<br />
the youngest<br />
<strong>and</strong> bravest<br />
of those we<br />
care for in<br />
hospice”<br />
Outst<strong>and</strong>ing Efforts in Supporting<br />
<strong>Hospice</strong> Recognized During<br />
Celebration<br />
On Friday, April 26th, NHF held its 9th<br />
Annual Gala as part of the NHPCO’s 28th<br />
Management <strong>and</strong> Leadership Conference at<br />
the Gaylord <strong>National</strong> Resort <strong>and</strong> Convention<br />
Center at <strong>National</strong> Harbor, MD.<br />
“Our celebration was held in tribute to the<br />
youngest <strong>and</strong> bravest of those we care for in<br />
hospice: our pediatric patients. <strong>Hospice</strong><br />
professionals recognize that caring for<br />
pediatric patients <strong>and</strong> their family members<br />
requires a unique approach <strong>and</strong> set of skills.<br />
NHPCO works to raise awareness <strong>and</strong><br />
provide educational resources to those<br />
providing that care. We’re thankful to those<br />
who joined in our celebration in support of<br />
that work,” said J. Donald Schumacher,<br />
president <strong>and</strong> CEO of NHPCO.<br />
Local ABC News Anchor, Greta Kreuz served<br />
as Mistress of Ceremonies for the event<br />
attended by over 500 guests. Three awards<br />
were presented to individuals who have<br />
contributed to hospice in significant <strong>and</strong><br />
unique ways.<br />
Stuart Lazarus received the Philanthropic<br />
Inspiration Award for his commitment to<br />
raising funds for hospice. In 2002, Lazarus<br />
combined his love of running with his<br />
passion for hospice to create a successful<br />
fundraising program, Run to Remember<br />
(www.runtoremember.org). This program<br />
gives runners <strong>and</strong> walkers an opportunity to<br />
celebrate <strong>and</strong> honor the memory of their<br />
loved ones <strong>and</strong> raises funds for hospice on a<br />
local, national, <strong>and</strong> international level.<br />
Ellen Goodman was granted the<br />
Morfogen Art of Caring Award. The<br />
Pulitzer Prize- winning journalist received<br />
the award for The Conversation Project<br />
(theconversationproject.org), an effort to<br />
engage the public in conversations about<br />
the end of life by sharing stories about<br />
“good deaths” <strong>and</strong> “bad deaths” <strong>and</strong> offering<br />
tools to make these conversations easier.<br />
Torrey DeVitto, an actress <strong>and</strong> active<br />
hospice volunteer, was given the Buchwald<br />
Spirit Award for Public Awareness. As<br />
NHPCO’s very first <strong>Hospice</strong> Ambassador,<br />
DeVitto frequently finds opportunities<br />
through interviews, social media, <strong>and</strong><br />
appearances to bring more attention to<br />
hospice care <strong>and</strong> bring awareness to a<br />
2<br />
A newsletter of the <strong>National</strong> <strong>Hospice</strong> Foundation | Spring 2013
Lighthouse of Hope Fund Provides Meaningful <strong>and</strong><br />
Memorable Experiences for Adult <strong>Hospice</strong> Patients<br />
NHF has launched the Lighthouse of<br />
Hope Fund, a new program that will help<br />
local hospice programs create<br />
meaningful <strong>and</strong> memorable experiences<br />
at the end of life for adult patients <strong>and</strong><br />
their family members.<br />
Kelli Singleton, Tracey Truscott, Cindy Scott, Jennifer<br />
Hudes, Laura Avanesyan <strong>and</strong> Monica Lewis McCommas<br />
of Silverado <strong>Hospice</strong>.<br />
younger age group. She created the theme<br />
for the 2012 <strong>National</strong> <strong>Hospice</strong> <strong>and</strong> <strong>Palliative</strong><br />
<strong>Care</strong> Month, “Comfort. Love. Respect.”<br />
Nearly $100,000 was raised during the event,<br />
including over $29,000 from a live auction.<br />
These funds will be used to support all of<br />
NHPCO’s work in pediatric hospice care.<br />
NHF would like to thank its Gala Sponsors:<br />
Ruby Sponsors:<br />
• Suncoast Solutions<br />
• Suncoast <strong>Hospice</strong><br />
Tanzanite Sponsors:<br />
• Gentiva <strong>Hospice</strong><br />
Amethyst Sponsors:<br />
• Samira K. Beckwith <strong>and</strong> Hope<br />
Health<strong>Care</strong> Services<br />
• Center for <strong>Hospice</strong> <strong>Care</strong><br />
• Chapters Health System<br />
• Community Health Accreditation Program<br />
• The Elizabeth <strong>Hospice</strong><br />
• Gilchrist <strong>Hospice</strong> <strong>Care</strong><br />
• Glatfelter Healthcare Practice<br />
• VITAS Innovative <strong>Hospice</strong> <strong>Care</strong><br />
Next year’s gala will be held on Friday,<br />
March 28, 2014 also at the Gaylord<br />
<strong>National</strong> Resort <strong>and</strong> Convention Center<br />
in conjunction with NHPCO’s 29th<br />
Management <strong>and</strong> Leadership Conference.<br />
By choosing to participate in the Fund,<br />
which includes an annual $500<br />
registration fee, hospice programs will be<br />
able to request up to $1,500 in total on<br />
behalf of their patients by the end of the<br />
year. These funds might be used toward<br />
any number of life experiences for their patients such as flying loved ones in to visit,<br />
special events such as trips or celebrations, or any opportunity to spend quality time<br />
with family <strong>and</strong> friends.<br />
“We know many of the ways hospice improves quality of life for patients <strong>and</strong> family<br />
caregivers through skilled interdisciplinary care. Our new Lighthouse of Hope<br />
program will allow hospices to add another dimension to the services they provide<br />
to those under their care,” said John Mastrojohn, NHF executive director.<br />
Seed funding for the Fund came from the assets of the Lighthouse Foundation,<br />
which were generously designated to NHF in mid-2012 when the parent hospice of<br />
the Lighthouse Foundation was purchased. The Fund will be sustained through<br />
annual fees of participating hospices, generous contributions of individuals,<br />
corporations, <strong>and</strong> foundations.<br />
To learn more about the Lighthouse of Hope Fund, or to make a donation, visit:<br />
www.nationalhospicefoundation/lighthouseofhopefund.<br />
Foundation Board Chair, Samira Beckwith<br />
Elected Vice-Chair of <strong>National</strong> Coalition of<br />
Cancer Survivorship<br />
Samira Beckwith,<br />
Foundation Board Chair<br />
Samira Beckwith, Foundation Board Chair <strong>and</strong> president <strong>and</strong><br />
CEO of Hope Health<strong>Care</strong> Services, has been elected vice chair<br />
of the board of directors for the <strong>National</strong> Coalition of Cancer<br />
Survivorship, which advocates for quality cancer care for all<br />
people touched by cancer <strong>and</strong> provides tools that empower<br />
people to advocate for themselves.<br />
Beckwith has twice survived cancer; she was diagnosed with<br />
Hodgkin’s lymphoma at age 24 <strong>and</strong> later, breast cancer. Her<br />
experiences helped shaped Beckwith’s career mission to ensure access to quality,<br />
compassionate health care services for all.<br />
NHF congratulations Samira on her new role, <strong>and</strong> is grateful for her continued<br />
dedication <strong>and</strong> service to hospice.<br />
A newsletter of the <strong>National</strong> <strong>Hospice</strong> Foundation | Spring 2013<br />
3
NHPCO Begins Collaborative Efforts<br />
with the Funeral Industry<br />
Work Begins with a Joint Effort with<br />
<strong>National</strong> Funeral Directors Association<br />
The end of life is a difficult time for the family members <strong>and</strong> loved<br />
ones helping the patient through the last phase of life. In the<br />
midst of their grief, arrangements must be made to honor the<br />
person who has died, including funeral details. Because of the<br />
shared experience in working with families through this process,<br />
NHPCO has begun efforts to bring hospice professionals <strong>and</strong> the<br />
funeral service industry together to work <strong>and</strong> learn from one<br />
another. The first such collaboration is with the <strong>National</strong> Funeral<br />
Directors Association (NFDA).<br />
<strong>Hospice</strong> professionals are skilled in providing pain management<br />
<strong>and</strong> addressing the psychological, social <strong>and</strong> spiritual needs of<br />
not only the patient, but their loved ones as well. That care<br />
continues into the bereavement process. Memorial services <strong>and</strong><br />
funerals are often an important part of that process, <strong>and</strong> funeral<br />
directors play a critical role in ensuring that those services reflect<br />
the life that is being honored <strong>and</strong> are meaningful to family<br />
members <strong>and</strong> loved ones.<br />
Often, hospice workers develop close bonds with the families they<br />
care for <strong>and</strong> are relied upon for guidance <strong>and</strong> advice following the<br />
death of their loved one. Funeral directors are trained <strong>and</strong><br />
experienced in the many options available to families <strong>and</strong> are<br />
there to work with families to help them commemorate the life of<br />
their loved one in a meaningful way. By working together, hospices<br />
<strong>and</strong> funeral homes can share their expertise <strong>and</strong> assist families<br />
through this emotional process.<br />
“There are many examples of hospices working closely with funeral homes in their area to ease the difficulty of planning for the<br />
emotional time that follows the death of a loved one. By collaborating on an association level, such as with NFDA, we can help to<br />
spread those relationships,” said J. Donald Schumacher, president <strong>and</strong> CEO of NHPCO.<br />
“Each of our professions brings a unique perspective to serving the dying, those who have died, <strong>and</strong> the bereaved. We look<br />
forward to developing materials <strong>and</strong> tools with NHPCO to share our experiences <strong>and</strong> expertise. The families we care for will<br />
benefit by two organizations focused on end-of- life care working h<strong>and</strong>-in-h<strong>and</strong> to ease the transition,” said Robert “Bob” T.<br />
Rosson, CFSP, CPC, NFDA president.<br />
NFDA is the world’s leading <strong>and</strong> largest funeral service association, serving 18,500 individual members who represent nearly<br />
10,000 funeral homes in the United States <strong>and</strong> 43 countries around the world. NFDA offers funeral professionals comprehensive<br />
educational resources, tools to manage successful businesses, guidance to become pillars in their communities <strong>and</strong> the expertise<br />
to foster future generations of funeral professionals. NFDA is headquartered in Brookfield, Wis., <strong>and</strong> has an office in Washington,<br />
D.C. For more information, visit www.nfda.org.<br />
By sharing educational materials <strong>and</strong> resources, hospice <strong>and</strong> funeral service professionals will learn more about the areas of<br />
expertise each bring to the table. Future plans for collaboration include presenting educational tools at the professional<br />
conferences of each organization, <strong>and</strong> eventually developing information directed toward consumers.<br />
4 A newsletter of the <strong>National</strong> <strong>Hospice</strong> Foundation | Spring 2013
Run to Remember: A Look at Two Special Kentucky<br />
Bourbon Chase Runners<br />
Arjit <strong>and</strong> Sourav Guha<br />
One Man Runs in Honor of His Brother Who<br />
Sought to Turn Personal Adversity into<br />
Positive Change for Others<br />
Sourav Guha will join the Run to Remember family this<br />
fall as he <strong>and</strong> 11 of his friends take on the Bourbon<br />
Chase. The race is a 200-mile overnight relay along the<br />
Kentucky Bourbon Trail. The group will be running in<br />
honor of Guha’s brother, Arijit, who died of metastatic<br />
colon cancer earlier this year: www.active.com/donate/<br />
runtoremember2013/souravguha.<br />
Arijit was diagnosed with Stage IV cancer in 2011, shortly after his 30th birthday, while a<br />
graduate student at Arizona State University. After less than a year of treatment, he reached<br />
the lifetime coverage cap on his student health policy. Always a resourceful activist <strong>and</strong><br />
relentless advocate on behalf of himself <strong>and</strong> others, Arijit created a website (poopstrong.org)<br />
to raise awareness of his situation <strong>and</strong> funds for his treatment.<br />
Facing medical bankruptcy, but keenly aware that his situation was not dissimilar from that of<br />
many others, Arijit also took to social networks to dem<strong>and</strong> better coverage <strong>and</strong> received<br />
international press coverage of his successful campaign. As a result, the insurance company<br />
agreed to extend their coverage of his medical bills.<br />
Arjit <strong>and</strong> his wife, Heather, were able to donate the more than $130,000 they had raised to a<br />
variety of cancer-related charities assisting those in financial need. Grateful for opportunity to<br />
help others, Arijit always emphasized that his personal victory should only be considered the<br />
beginning of a much broader movement. He was proud that the attention he received as an<br />
individual was part of a much larger national conversation about inequities in healthcare<br />
access in American society.<br />
Toward the end of 2012, with his tumors having further metastasized, Arijit made the difficult<br />
decision to end treatment. At the beginning of this year, he began receiving palliative home<br />
care from <strong>Hospice</strong> of the Valley in Phoenix. He passed away peacefully, with his wife <strong>and</strong> his<br />
hospice nurse by his side, in March. Arijit faced life <strong>and</strong> death with passion <strong>and</strong> a sense of<br />
humor <strong>and</strong> perspective.<br />
“Wherever he went,” says Sourav, “fun <strong>and</strong> friends were sure to surround him, so the<br />
Bourbon Chase seems a fitting way to remember <strong>and</strong> honor Arijit. He encountered every<br />
situation in life with positivity <strong>and</strong> gratitude, <strong>and</strong> I would like for all of us who loved <strong>and</strong><br />
admired him to try to do the same. We are so grateful for the care <strong>and</strong> respect that he <strong>and</strong><br />
we received from <strong>Hospice</strong> of the Valley, <strong>and</strong> in particular from his nurse, Cheryl Amburgey,<br />
<strong>and</strong> social worker, Ray Unks.”<br />
The 12-person team has come up with an<br />
impressive array of creative fund-raising ideas.<br />
Breeding <strong>and</strong> her colleagues will be<br />
participating in a weekend festival held by<br />
one of their physical therapy clinics. They<br />
plan to raise funds at the festival through a<br />
silent auction, offering pay-per-minute<br />
massages <strong>and</strong> selling tickets to employees<br />
for a chance to throw a pie in the face of their<br />
managers. Additional fund-raising efforts<br />
of the team include:<br />
• Selling chocolates for a local chocolate<br />
factory in Lexington, KY<br />
• Working at a portable st<strong>and</strong> at local<br />
minor league baseball games<br />
• Hosting bake sales<br />
• Holding a charity Hip Hop Hustle<br />
aerobics class<br />
• Organizing a Cornhole Tournament<br />
With all of these creative efforts, there is<br />
no doubt team “Don’t Pull a Hammy” will<br />
reach their goal of raising $6,000 for NHF<br />
<strong>and</strong> <strong>Hospice</strong> of the Bluegrass. Their<br />
donation page is www.active.com/donate/<br />
runtoremember2013/teamdrayer.<br />
NHF wishes Sourav, Christina, their teams <strong>and</strong><br />
all Run to Remember participants the best of<br />
luck in their race <strong>and</strong> fundraising goals! You<br />
too can run any race at any pace to raise funds<br />
for hospice. Visit www.nationalhospice<br />
foundation/runtoremember.org to learn more<br />
about NHF’s signature fundraising <strong>and</strong> race<br />
training program.<br />
Christina Breeding with Lexington Legends mascot<br />
Team “Don’t Pull a Hammy” Pulls Out All the Stops for Creative Fundraising<br />
Christina Breeding will also be participating in the Bourbon Chase in October as team<br />
captain for Drayer Physical Therapy Institute. Team “Don’t Pull a Hammy” will be raising<br />
funds for NHF <strong>and</strong> <strong>Hospice</strong> of the Bluegrass, which cared for both of Christina’s gr<strong>and</strong>fathers<br />
at the end of their lives.<br />
“I want others to experience the same comforting care <strong>and</strong> have the opportunity to be at<br />
home with the people they love the most in those final moments. Running this race in<br />
memory [of my gr<strong>and</strong>parents] is one way I can do that,” said Christina.<br />
A newsletter of the <strong>National</strong> <strong>Hospice</strong> Foundation | Spring 2013<br />
5
1731 King Street, Alex<strong>and</strong>ria, Virginia 22314<br />
Ph: 703-516-4928 or 877-470-6472<br />
Fax: 703-837-1233<br />
info@nationalhospicefoundation.org<br />
Social Networking with NHF<br />
Join the conversation on Facebook!<br />
www.facebook.com/NatHospFdn<br />
Follow our tweets at Nhf_news<br />
Learn more about NHF at<br />
www.nationalhospicefoundation.org