PDF version - National Hospice and Palliative Care Organization
PDF version - National Hospice and Palliative Care Organization
PDF version - National Hospice and Palliative Care Organization
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
The Monthly Membership Publication of the <strong>National</strong> <strong>Hospice</strong> <strong>and</strong> <strong>Palliative</strong> <strong>Care</strong> <strong>Organization</strong> June 2013<br />
Inside<br />
Determining Caseloads<br />
Gilchrist <strong>Hospice</strong> <strong>Care</strong>’s clinical director,<br />
Regina Shannon Bodnar, walks us through<br />
her use of the NHPCO Staffing Guidelines to<br />
illustrate how valuable it can be in helping to<br />
determine optimal caseloads. “We’ve been<br />
using the Guidelines since 2011,” she says,<br />
“<strong>and</strong> it has helped me delineate differing<br />
needs by service line <strong>and</strong>, in some cases, also<br />
by team.”<br />
Quality on Display<br />
How have providers prepared their staff<br />
for the quality reporting requirements?<br />
Two of the providers that were recognized<br />
for their work by the NHPCO Quality <strong>and</strong><br />
St<strong>and</strong>ards Committee discuss the steps they<br />
took to prepare for implementation of the<br />
Comfortable Dying Measure.<br />
PT in <strong>Hospice</strong><br />
Karen Mueller of the NCHPP Allied Therapist<br />
Steering Committee speaks to the value of<br />
physical therapy in helping hospice patients<br />
<strong>and</strong> families meet their goals of care. (Be sure<br />
to also see the impressive list of published<br />
research on this topic that she provides on<br />
page 29.)<br />
Short Takes:<br />
• Award Winners Recognized at MLC<br />
• Circle of Life Call for Nominations<br />
A Message From Don<br />
Member News <strong>and</strong> Notes<br />
Compliance Tip<br />
Educational Offerings<br />
Videos Worth Watching<br />
News from NHF<br />
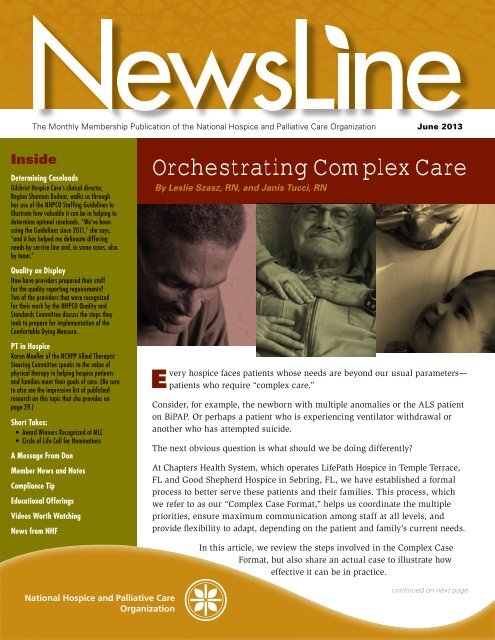
Orchestrating Complex <strong>Care</strong><br />
By Leslie Szasz, RN, <strong>and</strong> Janis Tucci, RN<br />
E<br />
very<br />
hospice faces patients whose needs are beyond our usual parameters—<br />
patients who require “complex care.”<br />
Consider, for example, the newborn with multiple anomalies or the ALS patient<br />
on BiPAP. Or perhaps a patient who is experiencing ventilator withdrawal or<br />
another who has attempted suicide.<br />
The next obvious question is what should we be doing differently?<br />
At Chapters Health System, which operates LifePath <strong>Hospice</strong> in Temple Terrace,<br />
FL <strong>and</strong> Good Shepherd <strong>Hospice</strong> in Sebring, FL, we have established a formal<br />
process to better serve these patients <strong>and</strong> their families. This process, which<br />
we refer to as our “Complex Case Format,” helps us coordinate the multiple<br />
priorities, ensure maximum communication among staff at all levels, <strong>and</strong><br />
provide flexibility to adapt, depending on the patient <strong>and</strong> family’s current needs.<br />
In this article, we review the steps involved in the Complex Case<br />
Format, but also share an actual case to illustrate how<br />
effective it can be in practice.<br />
continued on next page
continued from previous page<br />
The Complex Case<br />
Format<br />
There are four primary steps in<br />
this process:<br />
1. Gather Information<br />
Obtain the past <strong>and</strong> current<br />
medical information about the<br />
patient, but also identify family<br />
dynamics, the decision-makers,<br />
caregivers <strong>and</strong> spokesperson, as<br />
well as what the patient <strong>and</strong> the<br />
family expects <strong>and</strong> wants.<br />
2. Inform All Involved<br />
Advise the patient <strong>and</strong> family<br />
of what to expect from us,<br />
including timeframes <strong>and</strong><br />
specifics such as the name <strong>and</strong><br />
phone number of their hospice<br />
contact person. It’s also equally<br />
important to make sure that<br />
all staff who will be providing<br />
the care have the pertinent<br />
information about the patient<br />
<strong>and</strong> family.<br />
3. Conduct a Complex Case<br />
Conference<br />
Oftentimes conducted as a<br />
conference call, this meeting<br />
should present <strong>and</strong> discuss the<br />
case, <strong>and</strong> ultimately determine<br />
if the hospice should admit or<br />
not admit the patient to service.<br />
Thus, it’s essential that all<br />
necessary parties take part in the<br />
meeting, such as the certifying<br />
physician; MD or ARNP who<br />
will be attending the patient; RN<br />
who has been coordinating the<br />
admission; social worker <strong>and</strong>/or<br />
chaplain; admissions manager;<br />
manager of the receiving team<br />
<strong>and</strong>/or designee; <strong>and</strong> any<br />
specialty staff (e.g., respiratory<br />
or infusion therapist).<br />
4. Debrief<br />
After the high-intensity<br />
portion of the patient’s care is<br />
accomplished, have the same<br />
people who participated in the<br />
conference reconvene to assess<br />
<strong>and</strong> identify what went well <strong>and</strong><br />
what changes might be needed<br />
in future complex cases.<br />
At Chapters, we not only follow<br />
these steps when admitting<br />
a new patient with complex<br />
needs, but also when an existing<br />
patient’s care becomes complex.<br />
By including all of the players in<br />
the discussion—patient, family<br />
<strong>and</strong> staff—everyone underst<strong>and</strong>s<br />
what is expected, each other’s<br />
role <strong>and</strong> function, <strong>and</strong> how the<br />
pieces work together. This level<br />
of coordination helps to reduce<br />
anxiety <strong>and</strong> empowers staff<br />
to make wise decisions. The<br />
process itself can be likened<br />
to that of an orchestra, where<br />
planning <strong>and</strong> communication<br />
ensure a harmonious outcome.<br />
Of course, the dem<strong>and</strong>s <strong>and</strong><br />
available resources for each<br />
hospice may be quite different,<br />
so this format is really only<br />
meant to be a starting point for<br />
your organization, not a “one<br />
size fits all” solution.<br />
continued on page 4<br />
2 NewsLine
Important Points About the<br />
Proposed FY2014 Rule<br />
The Centers for Medicare <strong>and</strong> Medicaid Services released a proposed<br />
rule (posted by CMS on April 29 <strong>and</strong> published in the Federal<br />
Register on May 10) which would update the fiscal year FY2014 hospice<br />
reimbursement rates. But that wasn’t all.<br />
There were a number of other important things addressed that all providers<br />
should be aware of, including: clarification on coding requirements; hospice<br />
quality reporting; an update on hospice payment reform options; a shortstay<br />
add-on payment; rebasing the routine home care rate; a site of service<br />
adjustment for hospice patients in nursing facilities; <strong>and</strong> a cost report<br />
analysis. Given this, please be sure to review the information that our<br />
Regulatory Team makes available. A good place to start is with the NHPCO<br />
Regulatory Alert issued on April 30.<br />
One particular point that concerns me greatly is the claim from CMS that<br />
under the proposed rule hospices would receive “a 1.1 percent market<br />
basket increase” in their reimbursement. As I shared in a message to<br />
members when the proposed rule was posted, the numbers don’t add up.<br />
The impact of sequestration cuts was not calculated in this figure. Under<br />
current law, the CMS proposed payment update would actually mean a<br />
minus 0.9 percent decrease for the nation’s hospice community.<br />
Please be assured that NHPCO, the <strong>Hospice</strong> Action Network <strong>and</strong> our<br />
lobbyists are all working to emphasize the damage that a negative update<br />
would bring to the hospice community. Furthermore, our official letter to<br />
CMS will be submitted by the July deadline for comments.<br />
<strong>Hospice</strong>s are already struggling with an increased regulatory burden,<br />
heightened scrutiny, <strong>and</strong> existing productivity cuts. Given the value<br />
that hospice brings to the federal system <strong>and</strong> the patients <strong>and</strong> families<br />
we serve, we must work collaboratively <strong>and</strong> carry our unified voice to<br />
Capitol Hill.<br />
There is also a part you can play. The <strong>Hospice</strong> Action Network will be<br />
hosting its annual Advocacy Intensive in Washington, DC on July 29 <strong>and</strong><br />
30, 2013. We need to bring as many advocates as possible to the nation’s<br />
capital to carry our voice to members of Congress. And every voice<br />
matters—hospice directors, clinical staff, volunteers, board members <strong>and</strong><br />
supporters! Registration is now open, so please consider joining us.<br />
J. Donald Schumacher, PsyD<br />
President/CEO<br />
NewsLine 3
continued from page 2<br />
How It’s Used at Chapters<br />
At our hospice programs, an RN<br />
begins gathering information<br />
as part of the initial patient<br />
assessment. This includes a<br />
thorough medical-history review<br />
<strong>and</strong> an initial conversation with<br />
the patient <strong>and</strong> family. During<br />
this first meeting, the RN asks<br />
two important questions: What<br />
have the doctors told you about<br />
your situation <strong>and</strong> what do you<br />
want for yourself <strong>and</strong> your loved<br />
one(s)? The RN also explains<br />
what the patient <strong>and</strong> family<br />
should expect from us.<br />
This initial conversation is<br />
tremendously important since<br />
it reveals what the patient <strong>and</strong><br />
family underst<strong>and</strong> about the<br />
patient’s medical condition.<br />
It also helps to identify their<br />
psychosocial, emotional <strong>and</strong><br />
spiritual needs, <strong>and</strong> sheds light<br />
on what the family is prepared<br />
to accept—be that caring for<br />
the patient with the hope of an<br />
improved prognosis or allowing<br />
the patient to experience a<br />
natural death.<br />
If the patient is alert <strong>and</strong><br />
oriented, the conversation is<br />
held with both the patient <strong>and</strong><br />
family. If the patient is comatose,<br />
obtunded, or intermittently<br />
awake, we safeguard <strong>and</strong> respect<br />
the patient’s known desires<br />
through advance directives.<br />
If the patient is only partially<br />
aware, we ask family members<br />
to be present while our staff<br />
talks with the patient <strong>and</strong> strives<br />
for answers to the bottom-line<br />
questions: Do you underst<strong>and</strong><br />
that you are very, very sick? Do<br />
you want to try to get better or<br />
are you ready to let go <strong>and</strong> pass<br />
on? If the patient seems to be<br />
interacting, but does not respond<br />
to a particular question, we then<br />
explain to the family that we<br />
interpret the answer as “I don’t<br />
know.”<br />
When withdrawal of life support<br />
is an issue, we are equally direct<br />
<strong>and</strong> clear in the questions we<br />
pose to the patient: “You know<br />
the tube you have down your<br />
throat? Your family tells me you<br />
want that tube out, is that right?<br />
Do you want that tube removed<br />
even if it means you will die?”<br />
While this questioning may<br />
seem harsh, when voiced with<br />
compassion, it reassures the<br />
patient <strong>and</strong> family that we<br />
are here to honor the patient’s<br />
wishes <strong>and</strong> do what he or she<br />
wants. If the patient is alert <strong>and</strong><br />
aware enough, this questioning<br />
usually elicits a response.<br />
4 NewsLine
Our practice is to follow the<br />
patient’s expressed wishes. If<br />
the patient has been interacting,<br />
but does not answer a particular<br />
question, we interpret this as<br />
“I don’t know,” <strong>and</strong> then stop<br />
the process. If the patient is<br />
unresponsive, we rely on advance<br />
directives. In the absence of<br />
advance directives, we identify<br />
the legal decision-maker<br />
according to our policy.<br />
We conclude the conversation<br />
by explaining what to expect<br />
from us, what might be needed<br />
from them, <strong>and</strong> who will be their<br />
contact persons at our program.<br />
Our admitting nurse then notifies<br />
the receiving team to anticipate<br />
this complex case, <strong>and</strong> arranges<br />
for a social worker <strong>and</strong> chaplain<br />
to meet the patient <strong>and</strong> family to<br />
assess the psycho-social-spiritual<br />
aspects of their lives <strong>and</strong> the<br />
implications for care.<br />
This is the time to clarify who is<br />
considered “family.” Is the patient<br />
legally married to one partner,<br />
but currently living with another<br />
who has assumed that role? Does<br />
the staff at the patient’s long-term<br />
care facility consider themselves<br />
family <strong>and</strong> want to be informed<br />
of the patient’s care at every stage<br />
of decline? If there is complex<br />
care to be rendered, is there<br />
someone who is willing <strong>and</strong> able<br />
to assist in a caregiving capacity?<br />
If so, who will be training them?<br />
What exactly are the orders <strong>and</strong><br />
instructions for that care?<br />
Finally, does your organization’s<br />
policies <strong>and</strong> procedures support<br />
the care that is needed <strong>and</strong><br />
requested? During our review of<br />
the case, a nursing director or<br />
chief clinical officer reviews all<br />
policies that apply to the patient’s<br />
situation. Any questions that<br />
surface from this review must<br />
then be addressed.<br />
In Practice:<br />
The Case of Jimmy<br />
Jimmy was a 32-year-old man<br />
with Down Syndrome, whose<br />
multiple medical conditions had<br />
brought him to a terminal state.<br />
He had been a long-term resident<br />
of a group home that cared for the<br />
developmentally disabled until<br />
his care required admittance to<br />
the area hospital. The group home<br />
<strong>and</strong> hospital were about 150 miles<br />
away from his parents’ home,<br />
which was located in our service<br />
area. Now, given his illness,<br />
his parents wanted to have him<br />
closer to them.<br />
Pages <strong>and</strong> pages of records about<br />
Jimmy arrived at our hospice for<br />
review. The physician <strong>and</strong> staff at<br />
our hospice house reviewed every<br />
page, looking for clues about the<br />
best way to manage his care. We<br />
learned that Jimmy was in fourcontinued<br />
on next page<br />
A nursing director<br />
or chief clinical officer<br />
reviews all policies<br />
that apply to the<br />
patient’s situation.<br />
NewsLine 5
continued from previous page<br />
point restraints at the hospital<br />
where staff described him as<br />
“unmanageable” <strong>and</strong> “physically<br />
aggressive.” The group home<br />
staff, on the other h<strong>and</strong>,<br />
had described him as fairly<br />
independent, <strong>and</strong> needing only<br />
verbal direction <strong>and</strong> guidance.<br />
They also said he only exhibited<br />
aggression when his personal<br />
space was invaded.<br />
Our hospice house manager<br />
contacted Jimmy’s father,<br />
gathered further information<br />
about him, <strong>and</strong> explained what<br />
to expect, including planned<br />
timelines. A Complex Case<br />
Conference was then scheduled<br />
by phone for the same day.<br />
Participants on the call included<br />
our chief clinical officer; a<br />
nursing director; the hospice<br />
house physician, manager <strong>and</strong><br />
team leaders; our infusion<br />
manager; <strong>and</strong> the nurse caring<br />
for Jimmy at the hospital.<br />
During the call we learned<br />
more about this young man’s<br />
physical decline <strong>and</strong> his very<br />
supportive family. His hospital<br />
nurse reported that he was<br />
nonverbal, currently had an IV,<br />
had taken nothing by mouth for<br />
three days, had a Foley catheter<br />
in place, <strong>and</strong> was incontinent.<br />
He was unable to maintain his<br />
body temperature <strong>and</strong> required<br />
a warming blanket at all times.<br />
The hospital nurse also said he<br />
could be physically aggressive<br />
with both h<strong>and</strong>s <strong>and</strong> feet <strong>and</strong><br />
that, for everyone’s safety, had<br />
been restrained during the entire<br />
month of his hospitalization.<br />
By the end of the call, we<br />
had decided to admit him the<br />
next day. We established the<br />
preliminary care plan, identified<br />
several tasks, <strong>and</strong> assigned staff<br />
members for follow-up. The<br />
focus of the plan of care included<br />
establishing communication with<br />
the patient; working to eliminate<br />
the restraints; <strong>and</strong> removing the<br />
IV <strong>and</strong> Foley. The preadmission<br />
tasks included communicating<br />
with staff at his group home;<br />
obtaining a warming blanket;<br />
<strong>and</strong> arranging for his parents to<br />
tour the hospice house <strong>and</strong> sign<br />
the hospice consent forms.<br />
Our team leader made contact<br />
with the patient’s group home.<br />
Our DME manager procured<br />
a warming blanket. The<br />
admissions manager made<br />
multiple calls to ensure a smooth<br />
transfer. The staff members who<br />
were assigned other specific<br />
tasks during the call completed<br />
them <strong>and</strong> reported back to the<br />
manager of the hospice house.<br />
Because everyone worked in<br />
concert, there was no need for a<br />
follow-up call.<br />
6 NewsLine
When Jimmy arrived at the<br />
hospice house, he truly was<br />
restrained at both the wrists <strong>and</strong><br />
ankles. The transport crew from<br />
the hospital reported a relatively<br />
quiet time during transit. Jimmy<br />
was awake, alert <strong>and</strong> looking at<br />
everyone who now surrounded<br />
him. He may have been nonverbal,<br />
but he said volumes<br />
with his eyes. He was calm <strong>and</strong><br />
looked at everyone questioningly<br />
as staff gently held the straps to<br />
his restraints while assessing his<br />
response to us <strong>and</strong> his possible<br />
level of aggression.<br />
Based on what we had learned<br />
in our extensive pre-admission<br />
review of his records, we were<br />
determined to create a calm,<br />
respectful environment for him<br />
<strong>and</strong> his parents. We greeted him<br />
by name, told him our names,<br />
<strong>and</strong> told him that we wanted to<br />
make him comfortable.<br />
“Jimmy took my h<strong>and</strong> <strong>and</strong> at<br />
first, was calm, but then, while<br />
maintaining eye contact with me,<br />
began to press his thumbnail into<br />
my h<strong>and</strong>,” said a member of the<br />
hospice team. “I gently pulled<br />
his thumb away <strong>and</strong> explained<br />
that it hurt me when he did that.<br />
I then assured him that I was not<br />
going to hurt him, so he should<br />
not hurt me. As I released his<br />
thumb, he continued to hold my<br />
h<strong>and</strong>, but without any aggression.<br />
This method of responding to him<br />
was repeated by other staff in the<br />
room when he behaved the same<br />
way with them. Each time, he<br />
stopped the behavior <strong>and</strong> finally,<br />
he stopped altogether. He would<br />
simply allow someone to gently<br />
take his h<strong>and</strong>.”<br />
Based on these interactions,<br />
we were ready to remove the<br />
restraints, but started first by<br />
removing the ankle restraints.<br />
With these removed, he was able<br />
to make himself more comfortable<br />
in bed by pulling his legs up<br />
against himself. There were no<br />
attempts to kick at any of us. Next,<br />
we removed his wrist restraints<br />
<strong>and</strong>, again, there were no attempts<br />
to strike out at any of us.<br />
His IV had become dislodged<br />
during transfer, so the tape was<br />
also removed. Our physician<br />
agreed to leave the IV out for now<br />
<strong>and</strong> see if he would resume eating<br />
<strong>and</strong> drinking. He was offered<br />
water which he drank without<br />
difficulty. Shortly after this, we<br />
removed his catheter <strong>and</strong> used an<br />
adult brief instead.<br />
We also replaced the gown he<br />
was wearing with a t-shirt <strong>and</strong><br />
he relaxed even more. Bless the<br />
volunteers <strong>and</strong> community groups<br />
who support what we do at our<br />
hospice house. We gave him one<br />
of the small, silky smooth quilts<br />
continued on next page<br />
Based on what<br />
we learned, staff<br />
was determined to<br />
create a calm <strong>and</strong><br />
respectful<br />
environment<br />
for him…<br />
NewsLine 7
continued from previous page<br />
they provide <strong>and</strong> he loved it,<br />
stroking both sides <strong>and</strong> then<br />
pulling it up to his chin <strong>and</strong><br />
holding it there. We also gave<br />
him a very soft egg-shaped<br />
pillow made at Easter time by<br />
the local women’s club, which he<br />
also liked. We then offered him<br />
one of the dolls that the local<br />
junior women’s club provides<br />
for our more-restless patients,<br />
but that didn’t go over quite as<br />
well. “Nope, he was all boy,”<br />
said a hospice staff member. “He<br />
pitched it to the end of the bed.”<br />
Fortunately, the staff discovered<br />
that he liked watching baseball,<br />
which helped engage him.<br />
Under the watchful, skilled<br />
<strong>and</strong> compassionate care of our<br />
hospice staff, this young man<br />
was kept comfortable. There<br />
was nothing poking, pulling or<br />
irritating him. Everyone spoke<br />
gently <strong>and</strong> kindly to him. While<br />
a volunteer stayed by his bedside<br />
during his stay at the hospice<br />
house, restraints were never used.<br />
For several days, Jimmy was able<br />
to take food <strong>and</strong> drink again.<br />
His stage II sacral decubitus<br />
began to heal. He rested quietly,<br />
<strong>and</strong> over the next 19 days his<br />
parents <strong>and</strong> brother were at his<br />
bedside throughout the day <strong>and</strong><br />
every evening, finally moving<br />
in <strong>and</strong> staying with him during<br />
the final few days of his life. On<br />
one of those days as he <strong>and</strong> his<br />
father hugged, his mother said<br />
tearfully, “We prayed so hard for<br />
him to live when he was born<br />
<strong>and</strong> now we are praying for God<br />
to take him home.”<br />
Jimmy died at 12:25 on a<br />
summer afternoon, with his<br />
family by his side.<br />
In Closing<br />
Because of the Complex Case<br />
process we followed, this young<br />
man’s care was organized before<br />
his arrival <strong>and</strong> throughout his<br />
stay with us, allowing him <strong>and</strong><br />
his family to find peace <strong>and</strong><br />
closure. It’s also a clear reminder<br />
of why we all work in hospice.<br />
Please see the opposite page<br />
for a print-friendly copy of the<br />
Complex Case Format to print<br />
<strong>and</strong>/or share with staff.<br />
Leslie Szasz is a senior nurse<br />
preceptor at Chapters Health<br />
System, with 38 years of<br />
healthcare experience. In her<br />
current role, she provides both<br />
classroom <strong>and</strong> in-home training<br />
for team preceptors <strong>and</strong> staff.<br />
Janis Tucci has worked in the<br />
field of nursing for 45 years. She<br />
joined LifePath <strong>Hospice</strong> in 2008,<br />
<strong>and</strong> has served as the manager of<br />
Melech <strong>Hospice</strong> House since 2009.<br />
8 NewsLine
The Complex Case Format<br />
Courtesy of Chapters Health System, Temple Terrace, FL<br />
Examples of a Complex Case:<br />
Multiple infusions; inotrope<br />
infusions; new tracheostomy;<br />
pediatrics; complex family or<br />
caregiver dynamics; safety issues;<br />
complex nursing care; withdrawal<br />
of life support.<br />
Purpose of the CC Format:<br />
• Honor the patient <strong>and</strong> family’s<br />
wishes<br />
• Bring together many entities<br />
• Facilitate a very emotional<br />
situation<br />
• Coordinate the plan of care<br />
• Identify <strong>and</strong> address any<br />
staff needs<br />
• Prepare for foreseeable<br />
problems<br />
• Empower staff to address<br />
the unforeseen problems<br />
according to policies <strong>and</strong> the<br />
plan of care.<br />
Steps in the CC Format:<br />
1. 1 Gather Information<br />
• What does the patient want?<br />
• What does the family want?<br />
• Medical history—both the<br />
current <strong>and</strong> past<br />
• Identify family dynamics, the<br />
decision-makers, caregivers<br />
<strong>and</strong> spokesperson<br />
• Determine the physical <strong>and</strong><br />
spiritual needs.<br />
2. 2 Inform All Involved<br />
• Inform the patient <strong>and</strong> family<br />
of what to expect, including<br />
timeframes <strong>and</strong> the name<br />
<strong>and</strong> phone number of their<br />
hospice contact person.<br />
• Provide basic information<br />
about the patient to the<br />
hospice staff who will be<br />
caring for him or her, along<br />
with when the complex case<br />
conference will be held.<br />
3. 3 Determine Who Needs to<br />
Attend the Complex Case<br />
Conference<br />
For example, the certifying<br />
physician; MD or ARNP who<br />
will be attending the patient;<br />
RN who has been coordinating<br />
the admission; social worker<br />
<strong>and</strong>/or chaplain; the admissions<br />
manager; manager of the<br />
receiving team <strong>and</strong>/or designee;<br />
<strong>and</strong> any specialty staff, such<br />
as a respiratory or infusion<br />
therapist.<br />
4. 4 Hold the Complex Case<br />
Conference<br />
The conference, which can be<br />
held by phone or as a meeting,<br />
should present <strong>and</strong> discuss the<br />
case, <strong>and</strong> ultimately determine<br />
if the hospice should admit or<br />
not admit the patient to service.<br />
For example, does the hospice’s<br />
policies <strong>and</strong> procedures support<br />
the care this patient <strong>and</strong> family<br />
needs <strong>and</strong> wants? Are there any<br />
issues or questions that must be<br />
answered or tasks completed<br />
before a decision can be<br />
reached?<br />
If a follow-up conference call is<br />
needed before a decision can<br />
be reached, set up the day <strong>and</strong><br />
time of the call before ending<br />
the current call.<br />
Finally, if you decide to admit<br />
the patient, identify what each<br />
of the staff members is to do at<br />
admission or when the patient is<br />
transferred to your hospice.<br />
5. 5 Debrief<br />
After the high-intensity<br />
portion of the patient’s care is<br />
accomplished, reconvene the<br />
same people who participated<br />
in the CCC to assess <strong>and</strong><br />
identify what went well <strong>and</strong><br />
what changes might be needed<br />
in future complex cases.<br />
NewsLine 9
Determining<br />
Caseloads<br />
Gilchrist <strong>Hospice</strong><br />
<strong>Care</strong> on Its Process<br />
By Regina Shannon Bodnar, RN, MS, MSN, CHPCA<br />
Staffing! Having the right people in the correct numbers is an essential foundation of a<br />
quality-driven hospice organization. But a hospice is not a hospice is not a hospice. In<br />
the same way that you individualize patient care, the art of knowing your ideal caseload<br />
numbers—for clinical staff as well as administrative support—must be based on an insightful<br />
underst<strong>and</strong>ing of both your business model <strong>and</strong> your community.<br />
Fortunately, NHPCO’s “Staffing Guidelines for <strong>Hospice</strong> Home <strong>Care</strong> Teams,” which was released in<br />
March of 2011, walks you through an analysis process to help you determine what your caseloads<br />
should be, based on these factors <strong>and</strong> others.<br />
At Gilchrist <strong>Hospice</strong> <strong>Care</strong> (GHC), where I serve as the director of clinical services, utilizing this<br />
analysis process has helped me delineate differing needs by service line <strong>and</strong>, in some cases, also by<br />
team. And in this article, I show you precisely how. But first, some background.<br />
10 NewsLine
Short Takes:<br />
• Results from the Education N eds A se sment<br />
• VA Reaching Out Grant Recipients<br />
• New NHDD Website<br />
• JPSM Ca l for Papers<br />
• New Volunt er Outreach Materials.<br />
News about NHPCO members.<br />
The Analysis Process<br />
The Staffing Guidelines is a wellorganized<br />
36-page document that<br />
utilizes a multi-step systematic<br />
assessment process to estimate<br />
optimal staffing levels for hospice<br />
programs, with the process broken<br />
out into ‘digestible’ sections.<br />
While an introduction with<br />
an overview is included in the<br />
document, let me briefly review<br />
the process for the purpose of this<br />
discussion:<br />
• Section I covers the “prep”<br />
work you should perform first.<br />
This includes:<br />
- A review of pertinent<br />
statistics from NHPCO’s<br />
<strong>National</strong> Summary of<br />
<strong>Hospice</strong> <strong>Care</strong> to give you<br />
an underst<strong>and</strong>ing of what<br />
hospices, nationwide, are<br />
currently doing; <strong>and</strong><br />
- A review of those factors<br />
that will influence<br />
your final caseload<br />
determinations, such as<br />
length of service, staffing<br />
models (e.g., Admissions<br />
Model; Bereavement<br />
Model); <strong>and</strong> organizational<br />
characteristics.<br />
• Section II covers the actual<br />
staffing analysis process,<br />
which calls for the completion<br />
of two one-page worksheets.<br />
This involves assembling your<br />
hospice data; comparing your<br />
current staffing caseloads to<br />
the national caseload statistics<br />
from the <strong>National</strong> Summary;<br />
<strong>and</strong> estimating your own<br />
staffing caseloads accordingly.<br />
• Section III covers the evaluation<br />
process, <strong>and</strong> is followed<br />
by sections which provide<br />
completed worksheets for three<br />
hospice programs to serve<br />
as examples, a convenient<br />
glossary of terms, <strong>and</strong> the<br />
pertinent tables from the<br />
<strong>National</strong> Summary.<br />
As you can see, implementing<br />
the guidelines does require an<br />
investment of time, but based on<br />
my experience, it is time well spent.<br />
GHC’s Analysis by<br />
Service Line<br />
Gilchrist <strong>Hospice</strong> <strong>Care</strong> (GHC),<br />
which serves patients in the<br />
jurisdictions of Central Maryl<strong>and</strong>,<br />
has an average daily census of<br />
approximately 600 patients. Our<br />
organization is arranged around<br />
three clinical service lines:<br />
1. Inpatient <strong>Care</strong> (44 beds across<br />
two facilities)<br />
2. Facility Based <strong>Care</strong> (three<br />
home hospice teams caring<br />
for patients in skilled nursing<br />
facilities <strong>and</strong> assisted living<br />
communities)<br />
continued on next page<br />
Want More<br />
Background<br />
About the<br />
Guidelines’<br />
Development?<br />
See the introductory<br />
article in the March<br />
2011 issue of<br />
NewsLine, which<br />
includes details<br />
about the rationale<br />
for establishing<br />
the analysis process.<br />
The Monthly Membership Publication of the <strong>National</strong> <strong>Hospice</strong> <strong>and</strong> Pa liative <strong>Care</strong> <strong>Organization</strong> March 2011<br />
Later this month, NHPCO wi l be releasing<br />
the eagerly awaited update to its staffing<br />
ratio recommendations—but it is<br />
far more than just an ‘update.’<br />
The new document, “Staffing<br />
Guidelines for <strong>Hospice</strong> Home<br />
<strong>Care</strong> Teams,” will help each<br />
hospice determine its unique<br />
staffing requirements, based<br />
on its model of delivery,<br />
patient characteristics <strong>and</strong><br />
environmental considerations.<br />
In this article, Tara Brodbeck,<br />
the president/CEO of <strong>Hospice</strong> of<br />
the Miami Va ley <strong>and</strong> the co-chair of<br />
the Task Force charged with developing<br />
the new Guidelines, talks about the tool,<br />
including why a new approach was taken,<br />
the member feedback from field testing,<br />
<strong>and</strong> suggestions on using it.<br />
NHPCO’s New Staffing Guidelines:<br />
No Longer a One-Size-Fits-All Approach<br />
Inside<br />
A Message From Don<br />
NHPCO president/CEO, Don Schumacher, talks abou the new series,<br />
“NHPCO Executive Conversations” <strong>and</strong> why it’ so important now.<br />
Capitol Hi l Day 2011<br />
The Voice of NCHPP<br />
A preview of the April 5-6 agenda <strong>and</strong> why a l member should a tend.<br />
In this monthly feature, we shine the light on the work of NCH P <strong>and</strong><br />
each of its 15 professional sections. This month the QAPI Section is<br />
spotlighted, with an article by E len Martin.<br />
By Tara Brodbeck, MS, RN, CHPN<br />
n 2008, as the NHPCO<br />
Quality <strong>and</strong> St<strong>and</strong>ards<br />
Committee began revising<br />
the St<strong>and</strong>ards of Practice for<br />
<strong>Hospice</strong> <strong>Care</strong> to incorporate<br />
the new <strong>Hospice</strong> CoPs, we<br />
knew it was also time to<br />
take on the cha lenging<br />
task of revising the staffing<br />
ratio recommendations in<br />
NHPCO’s “<strong>Hospice</strong> Services<br />
Guidelines <strong>and</strong> Definitions”<br />
(which had been produced back<br />
in 1994!).<br />
A soon as the project was added to<br />
our committee agenda, questions <strong>and</strong><br />
comments began pouring in from members<br />
across the country. It seemed that many had strong ideas abou the topic<br />
<strong>and</strong> wha the revision should address. Here’s a sampling of the initial<br />
feedback we received:<br />
• Resources for Your Social Work Sta f<br />
• CE/CME Training through NHPCO Webinars<br />
New—<strong>Hospice</strong> in the Continuum:<br />
This month’s feature spotlights PACE at Midl<strong>and</strong> <strong>Care</strong><br />
in Topeka, KS.<br />
Plus:<br />
I<br />
People <strong>and</strong> Places<br />
Educational O ferings<br />
continued on next page<br />
NHPCO conferences, Webinars, webcasts <strong>and</strong> E-OL courses.<br />
NewsLine 11
continued from previous page<br />
3. Home <strong>Hospice</strong> <strong>Care</strong> (six<br />
home hospice teams caring<br />
for patients in private<br />
residences, with one<br />
designated exclusively for<br />
pediatric patients).<br />
Since it was first released,<br />
we have used the guidelines<br />
to analyze our needs <strong>and</strong><br />
appropriately budget resource<br />
dollars for each of these three<br />
service lines.(Gilchrist Kids is<br />
excluded from this discussion<br />
since it is staffed differently,<br />
based on the experience of<br />
pediatric-care colleagues around<br />
the country.)<br />
Some Influencing Factors<br />
As part of the “prep” work that<br />
should precede the analysis, we<br />
considered factors unique to our<br />
organization that will impact<br />
staff caseloads. For example,<br />
across our organization, there<br />
are four particular features of our<br />
programmatic design that heavily<br />
impact staffing:<br />
• We have a NEWS Crew that<br />
covers nights, evenings <strong>and</strong><br />
weekends, <strong>and</strong> is staffed with<br />
RNs, LPNs <strong>and</strong>, to a lesser<br />
degree, supportive services.<br />
This Crew is responsible<br />
for responding to the prescheduled<br />
<strong>and</strong> on-call needs<br />
of our patients <strong>and</strong> families<br />
after business hours <strong>and</strong> on<br />
weekends.<br />
• We also employ a designated<br />
admissions team <strong>and</strong><br />
Hospital Liaison Crew seven<br />
days per week to conduct<br />
introductory visits <strong>and</strong> enroll<br />
eligible patients on service.<br />
• Our bereavement services<br />
are provided by a designated<br />
team of professionals separate<br />
from the interdisciplinary<br />
care team.<br />
• And in late 2011, we<br />
established a daytime triage<br />
team to h<strong>and</strong>le clinical calls<br />
during business hours to<br />
help reduce the number of<br />
interruptions on field staff.<br />
Given this programmatic design,<br />
our primary care teams do not<br />
provide bereavement services,<br />
our clinical teams do not h<strong>and</strong>le<br />
admissions or provide 24/7<br />
coverage (except on six holidays<br />
per year), <strong>and</strong> our supportive<br />
services staff has infrequent<br />
after-hours responsibilities. That<br />
said, additional discernment<br />
by each of our service lines is<br />
required—which I review next.<br />
12 NewsLine
The Guidelines in Practice<br />
Staffing for Facility Based <strong>Care</strong><br />
Our Facility Based <strong>Care</strong> (FBC) is composed of three teams: FBC-East,<br />
FBC-Central <strong>and</strong> FBC-West.<br />
We have long accepted that the care provided by these teams requires<br />
enhanced communication skills (since staff is working with family,<br />
facility staff <strong>and</strong> physicians); flexibility in work hours to ensure aroundthe-clock<br />
attention; <strong>and</strong> a true commitment to building <strong>and</strong> maintaining<br />
a respectful partnership in the care of the patients.<br />
Shown below is the completed copy of Worksheet 1 for this particular<br />
service line (this Worksheet appears on page 17 of the guidelines).<br />
As you see, we entered our data on Length of Service <strong>and</strong> Routine Level<br />
of <strong>Care</strong>, <strong>and</strong> then assigned a directional indicator (+/-/=) to represent<br />
higher, lower or equal caseloads for the categories under the Staffing <strong>and</strong><br />
<strong>Organization</strong>al Models.<br />
Factors Associated With <strong>Care</strong> Model FBC East FBC Central FBC West<br />
Length of Service 101 108 121<br />
Staffing Model<br />
Admission Model +/- + +<br />
On Call Model + + +<br />
RN/LPN Model + = -<br />
Shared Team Model = = =<br />
Bereavement Model + + +<br />
Staff Turnover Rate + + +<br />
<strong>Organization</strong>al Model<br />
Percent of Routine Level of <strong>Care</strong> 99 99 99<br />
Access = = =<br />
Aide/Homemaker Delivery Model + + +<br />
Use of Ancillary Therapy<br />
(e.g. PT/OT; art, music)<br />
+ + +<br />
We discovered<br />
that much was the<br />
same across<br />
our three teams<br />
On completion of the Worksheet, we discovered that much was the same<br />
across our three teams.<br />
We also found that the average Length of Service (LOS) for patients<br />
served by these teams (i.e., 101; 108 <strong>and</strong> 121) was significantly higher<br />
than the national average of 69.1 days as reported in the FY2011 <strong>National</strong><br />
Summary (Table 7), as was the Median LOS of 19.1 days.<br />
continued on next page<br />
NewsLine 13
continued from previous page<br />
In addition, our staff turnover rate of 10.3 percent (<strong>and</strong> 12.3 percent<br />
for nursing) was significantly below the national agency mean of 23.6<br />
percent, as reported in the FY2011 <strong>National</strong> Summary (Table 11).<br />
But a bit of variation bubbled up as well. An LPN floater has been<br />
successfully integrated into the FBC-East team, <strong>and</strong> covers cases when<br />
an RN team member is off. This averts the need for the other RN case<br />
managers to assume coverage responsibilities when a nursing colleague<br />
is using benefit time. Theoretically, the RNs on this team should be able<br />
to carry a slightly larger caseload of patients because they no longer<br />
have coverage responsibilities (or the fluctuation in the patient care<br />
responsibilities that coverage brings with it).<br />
These FBC teams have also expressed an interest in conducting a pilot<br />
to admit their own patients <strong>and</strong> not use the services of the admissions<br />
department. They are hopeful that this will increase the likelihood of<br />
team members connecting earlier with family members, which is a<br />
frequent challenge for patients residing in facilities. Because of greater<br />
flexibility in scheduling, they also hope it will decrease the time<br />
between referral <strong>and</strong> admission. This pilot, which is clearly poised for<br />
success, would dictate the need for smaller RN caseloads.<br />
It is also worth noting that the FBC-Central team has a wellestablished<br />
RN/LPN partnership that provides care across settings<br />
for residents of a large continuing care retirement community. Their<br />
caseload is nearly double that of an RN working independently <strong>and</strong> the<br />
arrangement has resulted in many positives, such as continuity of care,<br />
increased responsiveness to emergent needs, <strong>and</strong> a collegial camaraderie<br />
envied by many. It does not, however, impact the caseload size of other<br />
team members.<br />
14 NewsLine
Let’s now turn to the portion of Worksheet 1 concerning the <strong>Organization</strong>al<br />
Model shown on page 13, but also below.<br />
<strong>Organization</strong>al Model FBC East FBC Central FBC West<br />
Percent of Routine Level of <strong>Care</strong> 99 99 99<br />
Access = = =<br />
Aide/Homemaker Delivery Model + + +<br />
Use of Ancillary Therapy<br />
(e.g. PT/OT; art, music)<br />
+ + +<br />
The percentage of routine patients served by our FBC staff is nearly 2<br />
percentage points higher than the national average as reported in the<br />
FY2011 <strong>National</strong> Summary (99 percent versus 97.1 percent).<br />
We also fully utilize hospice aides, routinely use physical therapy to<br />
promote patient safety, <strong>and</strong> have thriving volunteer <strong>and</strong> music therapy<br />
programs (which are reflected by the directional indicators (+/=) we<br />
assigned to these categories).<br />
Also, the GHC Exp<strong>and</strong>ed <strong>Care</strong> Program of concurrent care is well<br />
established, but not frequently tapped by FBC patients because of their<br />
diagnostic mix <strong>and</strong> other factors. Thus, together, these findings suggest<br />
that GHC disciplines assigned to facility based care teams could carry<br />
caseloads that are larger than those reported in the FY2011 <strong>National</strong><br />
Summary.<br />
continued on next page<br />
Together, these<br />
findings suggested<br />
that GHC disciplines…<br />
could carry larger<br />
caseloads…<br />
NewsLine 15
continued from previous page<br />
Other Factors Impacting Caseloads<br />
Worksheet 2 of the Staffing Guidelines (page 19 of the document) lists<br />
13 other factors to consider when determining staffing caseloads. Our<br />
completed worksheet for the FBC service line is shown below.<br />
Other Factors to Consider<br />
for Staffing Caseloads<br />
FBC<br />
East<br />
FBC<br />
Central<br />
FBC<br />
West<br />
GIP <strong>and</strong> Continuous <strong>Care</strong> Variables = = =<br />
Multiple Non-core Roles for IDT - - -<br />
Facility-based Variables<br />
(routine home care)<br />
Primary <strong>Care</strong> Team Models + + +<br />
Provision of Community Services + + +<br />
Psychosocial Issues:<br />
High Social Complexity<br />
= = =<br />
Rate of Growth = = =<br />
Specialty Programs + + +<br />
Spiritual <strong>Care</strong> Support Model +/- +/- +/-<br />
Staff Safety: Require Multiple Staff<br />
or Escorts/Visits<br />
+ + +<br />
Travel Time: Increased = = -<br />
Volunteer Utilization + + +<br />
Other<br />
We found that, even though we have two stellar inpatient facilities, the<br />
use of our inpatient settings for FBC patients is infrequent. Continuous<br />
care is available <strong>and</strong> is often the first choice for symptomatic patients,<br />
based on the belief that moving an FBC patient from a familiar setting<br />
(<strong>and</strong> the faces they recognize) is frequently not the right thing to do. We<br />
also appreciate that our FBC team members are moving in the direction<br />
of embracing their responsibility as the end-of-life care experts for the<br />
facilities in which they work. This will bring enhanced responsibilities<br />
for FBC team members to conduct resident, family <strong>and</strong> professional<br />
education programs that are presently performed by other employees of<br />
the organization.<br />
One true outlier in our analysis of “Other Factors to Consider” was<br />
travel time for the FBC-West team. This team has a significant cluster of<br />
patients who are located more than 30 miles from the team office. It was<br />
determined that this finding should not affect the caseloads of all team<br />
members, but could most easily be addressed by introducing an RN/<br />
16 NewsLine
LPN partnership to this portion of the service area. Like all partnerships,<br />
the relationship is key to a successful RN/LPN pairing. We are presently<br />
in search of an LPN to complement the talents of the RN in this area.<br />
Until a partnership is launched, however, navigating the geography to<br />
best meet patient needs will be accomplished through well-considered<br />
scheduling <strong>and</strong> continued judicious use of per diem staff.<br />
Another point to note is in regard to our spiritual care support. In<br />
addition to their work with patients <strong>and</strong> families, our chaplains offer<br />
support to facility residents <strong>and</strong> staff members. In conjunction with<br />
our bereavement department, the chaplains conduct memorial services<br />
in many facilities on a quarterly basis. This is balanced by GHC’s<br />
commitment to honor patient <strong>and</strong> family relationships established with<br />
community clergy.<br />
Putting It All Together<br />
When considering all the factors collectively, it was determined that our<br />
RNs could <strong>and</strong> should carry caseloads in slight excess of the national<br />
average of 11 patients, as reported in the FY2011 <strong>National</strong> Summary.<br />
This decision is driven mostly by GHC’s organizational commitment<br />
to our NEWS Crew, admissions team, <strong>and</strong> bereavement department, as<br />
well as our vigorous volunteer program <strong>and</strong> the acknowledgment that<br />
travel for most team members is reduced in time <strong>and</strong> distance due to the<br />
clustering of patients in partner facilities. I do anticipate a modification<br />
to staffing numbers for our FBC-East team once it is positioned to assume<br />
responsibility for conducting its own admissions.<br />
One true<br />
outlier in our<br />
analysis was<br />
travel time….<br />
Staffing for Home <strong>Hospice</strong> <strong>Care</strong><br />
Shown at the top of the next page is Worksheet 1 for our Home <strong>Hospice</strong><br />
<strong>Care</strong> (HHC) service line.<br />
There are five teams in this service line that care for patients <strong>and</strong> their<br />
families in private residences. However, they also receive support from<br />
a NEWS Crew, admissions team, hospital liaisons, triage team, <strong>and</strong><br />
bereavement department. These teams are just beginning to migrate<br />
toward an RN/LPN model of care, with some adapting earlier than others.<br />
These teams are also moving towards a modified Shared Team Model that<br />
translates into all members of the team assuming broader responsibilities.<br />
continued on next page<br />
NewsLine 17
continued from previous page<br />
Factors Associated With <strong>Care</strong> Model Central East West Howard Harvard<br />
Length of Service 68 99 59 97 84<br />
Staffing Model<br />
Admission Model + + + + +<br />
On Call Model + + + + +<br />
RN/LPN Model = = = + +<br />
Shared Team Model = = = = =<br />
Bereavement Model + + + + +<br />
Staff Turnover Rate + + + + +<br />
<strong>Organization</strong>al Model<br />
Percent of Routine Level of <strong>Care</strong><br />
Access - - - - -<br />
Aide/Homemaker Delivery Model + + + + +<br />
Use of Ancillary Therapy<br />
(e.g. PT/OT; art, music)<br />
= = = = =<br />
In looking at the Routine Level of <strong>Care</strong> for these home hospice teams,<br />
note that we have deliberately left that row blank. This is due to an<br />
earlier organizational decision to change team assignments for a patient<br />
when the patient transfers from a home care team to an inpatient<br />
hospice setting. This results in no home hospice team having a patient<br />
at the general inpatient level of care.<br />
Like our FBC teams, our HHC teams recognize the important role<br />
that hospice aides play as care providers <strong>and</strong> team members. We staff<br />
these positions assertively, recognizing that if our aides are to truly<br />
meet the basic needs of patients <strong>and</strong> families, they need to visit them<br />
more frequently than any other member of the team. We are also<br />
assertive in incorporating physical therapists (PT) into all plans of<br />
care, acknowledging that those patients who are ambulatory <strong>and</strong> using<br />
assistive devices potentially benefit most from the skilled assessment<br />
<strong>and</strong> coaching that PT brings to the plan of care. Each of these findings<br />
suggests that the care teams could carry larger caseloads than those<br />
reported in the <strong>National</strong> Summary.<br />
As I noted earlier, GHC also has two stellar inpatient facilities. These<br />
facilities are frequently used by our HHC teams for patients who require<br />
complex symptom management. To facilitate seamless transitions in<br />
care, a bed is reserved at all times for use by home hospice patients. In<br />
18 NewsLine
cases of an anticipated weather emergency, the number of beds allocated<br />
for use by home hospice patients is increased. Given this practice, the<br />
coordination <strong>and</strong> h<strong>and</strong>off of patients is predictably less complex. So, even<br />
though transfers into the inpatient setting happen with regularity, this<br />
design supports the home hospice RN case manager in carrying a larger<br />
caseload.<br />
Other Factors Impacting Caseloads<br />
When assessing other factors that may impact staffing caseloads for<br />
the HHC teams, one team, in particular, st<strong>and</strong>s out as different from<br />
the others. The Central team cares for patients in Baltimore City <strong>and</strong><br />
the edges of the surrounding counties <strong>and</strong>, as shown in Worksheet 2<br />
below, the complexity of psychosocial issues encountered by this team<br />
(as reflected by the directional indicator) suggests that social workers<br />
should carry smaller caseloads. The issue of staff safety is also more<br />
commonplace for this team (also reflected by the directional indicator).<br />
Given that more time is required for the coordination of joint visits <strong>and</strong>/<br />
or the utilization of escort services, it was determined that all clinical<br />
disciplines on the Baltimore Central team should carry slightly smaller<br />
case loads.<br />
Other Factors to Consider<br />
for Staffing Caseloads<br />
Central East West Howard Harvard<br />
GIP <strong>and</strong> Continuous <strong>Care</strong> Variables + + + + +<br />
Multiple Non-core Roles for IDT + + + + +<br />
Facility-based Variables<br />
(routine home care)<br />
n/a n/a n/a n/a n/a<br />
Primary <strong>Care</strong> Team Models + + + + +<br />
Provision of Community Services + + + + +<br />
Psychosocial Issues:<br />
High Social Complexity<br />
- + + + +<br />
Rate of Growth = = = = =<br />
Specialty Programs + + + + +<br />
Spiritual <strong>Care</strong> Support Model +/- +/- +/- +/- +/-<br />
Staff Safety: Require Multiple Staff<br />
or Escorts/Visits<br />
- = = = =<br />
Travel Time: Increased = = = - -<br />
Volunteer Utilization + + + + +<br />
Other<br />
The complexity of<br />
psychosocial issues…<br />
suggested the social<br />
workers should<br />
carry smaller<br />
caseloads.<br />
continued on next page<br />
NewsLine 19
continued from previous page<br />
Putting It All Together<br />
In addition to the factors<br />
already noted, our triage<br />
department manages the<br />
majority of weekday calls<br />
from patients cared for<br />
by our HHC teams. This<br />
supported our determination<br />
that these teams could carry<br />
larger caseloads than the<br />
agency means by discipline,<br />
as reported in the FY2011<br />
<strong>National</strong> Summary (Table<br />
14). And this is by design.<br />
Our goal is to limit “the<br />
asks for work” outside of<br />
direct patient care, so these<br />
teams can focus almost<br />
exclusively on providing<br />
interdisciplinary care that is<br />
true to the core principles of<br />
hospice.<br />
The one exception is our<br />
Central team. The multitude<br />
of complex psychosocial<br />
issues <strong>and</strong> very real safety<br />
concerns associated with the<br />
patients they serve suggests<br />
smaller caseloads are<br />
necessary in order to deliver<br />
quality care <strong>and</strong> a positive<br />
patient <strong>and</strong> family experience.<br />
Travel time for both our<br />
Harford <strong>and</strong> Howard County<br />
teams is also acknowledged<br />
as a potential issue since each<br />
covers a broad geography.<br />
The distribution of patients<br />
is occasionally problematic<br />
<strong>and</strong> must be conscientiously<br />
assessed.<br />
In Closing<br />
The key to staffing success<br />
is the commitment to<br />
thoroughly underst<strong>and</strong>ing all<br />
of the factors which impact<br />
the day-to-day operations<br />
of the clinical program <strong>and</strong><br />
a commitment to re-assess<br />
those factors regularly. As I<br />
hope this article illustrates,<br />
NHPCO’s Staffing Guidelines<br />
can help you get there.<br />
Regina Shannon Bodnar is<br />
a registered nurse with more<br />
than 35 years of clinical <strong>and</strong><br />
leadership experience. She<br />
currently serves as the director<br />
of clinical services for Gilchrist<br />
<strong>Hospice</strong> <strong>Care</strong> in Hunt Valley,<br />
MD, a position she has held<br />
since 1993. She is also an<br />
active member of NHPCO,<br />
including service as both a<br />
member of the Quality <strong>and</strong><br />
St<strong>and</strong>ards Committee <strong>and</strong><br />
the Task Force charged with<br />
development of the NHPCO<br />
Staffing Guidelines.<br />
Staffing Guidelines: Available in <strong>PDF</strong> <strong>and</strong> Print<br />
NHPCO’s Staffing Guidelines for <strong>Hospice</strong> Home <strong>Care</strong> Teams can be<br />
downloaded by members, free of charge, from the NHPCO website.<br />
Printed copies ($14.99 for members) are also available for purchase from the<br />
NHPCO Marketplace—<strong>and</strong> can be ordered online or by calling the NHPCO<br />
Solutions Center at 800-646-6460 (M-F, 8:30 a.m. to 5:30 p.m., ET/EDT)<br />
20 NewsLine
NHPCO would like to thank all the conference attendees, the 2013 MLC Planning Committee <strong>and</strong> our<br />
business partners for making the 2013 MLC a success. On behalf of all who participated in the<br />
conference, we offer our deepest gratitude to the following organizations for their generous<br />
educational grants in support of the 28th Management <strong>and</strong> Leadership Conference.<br />
Thank You.<br />
Platinum Conference Supporter:<br />
Gold Conference Supporters:<br />
Silver Conference Supporters:<br />
Bronze Conference Supporters:<br />
NewsLine 21
quality on DISPlay:<br />
Two Honorees Share Their Work<br />
The NHPCO Quality <strong>and</strong> St<strong>and</strong>ards Committee held its second annual “Quality on Display”<br />
event at the November 2012 Clinical Team Conference.<br />
In light of the hospice quality reporting requirements (<strong>and</strong> the October 1, 2012 deadline to begin<br />
data collection), the Committee asked providers to share—on 4-by-8-foot visual displays—how<br />
they were preparing their organizations <strong>and</strong> staff.<br />
NewsLine is proud to share the work of BAYADA <strong>Hospice</strong> in Moorestown, NJ, <strong>and</strong> <strong>Hospice</strong> of<br />
the Bluegrass in Lexington, KY.<br />
Both organizations chose to showcase their strategies for implementation of the NHPCO<br />
Comfortable Dying Measure (NQF 0209), one of the two measures currently required for quality<br />
reporting to CMS. While their visual displays cannot be duplicated here, each organization has<br />
graciously created a <strong>PDF</strong> presentation that outlines its strategy <strong>and</strong> implementation process.<br />
22 NewsLine
BAYADA <strong>Hospice</strong> • Moorestown, NJ<br />
There were three primary components in our strategy:<br />
• Education: This included<br />
providing staff with an<br />
overview of the NHPCO<br />
Comfortable Dying Measure<br />
<strong>and</strong> a six-page FAQ document,<br />
where detailed answers to the<br />
measure were provided.<br />
• Technology Design: This<br />
included the revamping of<br />
assessments to determine<br />
eligibility for participation<br />
in the measure, as well as<br />
collaboration with our EMR<br />
vendor, Homecare Homebase.<br />
• Process Design: It was also<br />
critical to have a process<br />
in place to identify who in<br />
the organization will be<br />
responsible for the daily<br />
logistics of ensuring that every<br />
patient requiring follow-up<br />
receives it in a timely manner.<br />
While we were strategically<br />
positioned to gather <strong>and</strong> report<br />
on this measure through our<br />
partnership with Homecare<br />
Homebase, it did take several<br />
months to prepare our practice for<br />
this change.<br />
The <strong>Hospice</strong> Services (HOS) office<br />
developed education for our staff<br />
about this new measure, including<br />
a m<strong>and</strong>atory assessment through<br />
the Learning Management System<br />
(LMS). This was accomplished<br />
with much assistance from our<br />
Visit Virtual Office senior associate,<br />
Margaret Donohue, <strong>and</strong> our<br />
Learning Curriculum <strong>and</strong> Design<br />
training manager, Victoria McDevitt.<br />
Changes to the Homecare<br />
Homebase assessments also went<br />
into effect, so that our admissions<br />
nurses could easily identify a<br />
patient who requires follow-up <strong>and</strong><br />
should be reported in this measure.<br />
Additionally, HOS worked with<br />
input from four other hospice<br />
directors—Kristin Barnum, Linda<br />
Trout, Phyllis Tarbell, <strong>and</strong> Angela<br />
Snyder—to determine how to<br />
adapt daily operations to ensure<br />
that BAYADA staff was educated<br />
about this requirement <strong>and</strong><br />
available for the required 48-to-72<br />
hour follow-up, even on weekends<br />
<strong>and</strong> holidays.<br />
Sharon Vogel<br />
Director of <strong>Hospice</strong> Services<br />
While we were<br />
strategically positioned…<br />
to gather <strong>and</strong> report on<br />
this measure… it still<br />
took several months<br />
to prepare….<br />
VIEW THE PRESENTATION<br />
continued on next page<br />
NewsLine 23
continued from previous page<br />
<strong>Hospice</strong> of the Bluegrass • Lexington, KY<br />
<strong>Hospice</strong> of the Bluegrass made<br />
an early commitment to hospice<br />
quality reporting. As part of<br />
our strategic goals for 2012, we<br />
provided updates to the board of<br />
directors as well as our executive<br />
management team. With the tone<br />
at the top set, our next challenge<br />
was to educate clinicians on<br />
the NHPCO Comfortable Dying<br />
Measure (NQF 0209) <strong>and</strong> what<br />
it means to their practice <strong>and</strong><br />
workflow.<br />
The quality team (Compliance<br />
Analyst Tim Shockley; Patient<br />
Safety <strong>and</strong> Infection Control<br />
Nurse Kim Whisman; <strong>and</strong><br />
Compliance Coordinator Gale<br />
Hankins) <strong>and</strong> I were charged<br />
with project implementation, but<br />
success couldn’t be accomplished<br />
without help from the clinical<br />
team, led by Chief Clinical<br />
Officer Deede Byrne. But really,<br />
there isn’t a clinical director,<br />
supervisor, team leader, or<br />
clinician that wasn’t part of the<br />
team. As the saying goes, it takes<br />
a village.<br />
We discussed the measure<br />
regularly at quality meetings,<br />
but also at our clinical director<br />
meetings, team leader meetings<br />
<strong>and</strong> staff meetings. It was also<br />
part of the annual quality<br />
presentation that was conducted<br />
at each office. That was round<br />
one. Round two was a “train the<br />
trainer” PowerPoint that was<br />
used in each office leading up to<br />
the October 1 deadline.<br />
Additionally, we supplied staff<br />
with cheat sheets, flowcharts,<br />
decision trees, electronic<br />
medical record screenshots <strong>and</strong><br />
internally-developed FAQs.<br />
Since communication about<br />
patient needs is h<strong>and</strong>led<br />
differently in our rural offices<br />
which have fewer staff,<br />
leadership chose not to be<br />
prescriptive about each office’s<br />
“h<strong>and</strong>-off communications”<br />
process. Instead, we encouraged<br />
each office to use its established<br />
communications system—why<br />
change it if it already works?<br />
In the month prior to the<br />
October 1 deadline, we tested<br />
our electronic forms, reports <strong>and</strong><br />
clinical processes. A centralized<br />
tracking tool was maintained<br />
in the quality department.<br />
Reminder e-mails <strong>and</strong> voice<br />
mails were spearheaded by our<br />
compliance analyst. Through<br />
these communications, it<br />
became evident that each<br />
office was using some sort<br />
of tracking system to keep<br />
up with admissions <strong>and</strong> the<br />
measure’s questions, so the<br />
quality department created an<br />
individualized tracking tool for<br />
each office’s use.<br />
Eugenia Smither,<br />
RN, BS, CHC, CHE, CHP<br />
Corporate Compliance Officer<br />
Vice President of Compliance<br />
<strong>and</strong> Quality Improvement<br />
VIEW THE PRESENTATION<br />
24 NewsLine
What you don’t know<br />
can hurt you<br />
Federal <strong>and</strong> State Exclusions<br />
Database Searches are<br />
REQUIRED by HHS!<br />
igilance service will<br />
perform the m<strong>and</strong>atory<br />
searching of ALL<br />
databases<br />
Just pennies per name<br />
Compliance<br />
Requires<br />
Vigilance<br />
Seeking Board Eligible/Certified <strong>Hospice</strong><br />
<strong>Palliative</strong> Physician - Bethlehem, PA<br />
St. Luke’s University Health Network based in Bethlehem, PA is<br />
seeking a full-time, board certified or board eligible hospice palliative<br />
care physician. You’ll join a group of 2 physicians <strong>and</strong> provide<br />
inpatient consultative services in 3 hospitals; see outpatient palliative<br />
care patients; <strong>and</strong> have the opportunity to teach in our hospice/<br />
palliative care fellowship program along with medical students<br />
from the Temple/St. Luke’s School of Medicine. St. Luke’s currently<br />
has more than 150 physicians enrolled in internship, residency <strong>and</strong><br />
fellowship programs.<br />
The successful c<strong>and</strong>idate will have strong clinical <strong>and</strong> communication<br />
skills, a commitment to excellence <strong>and</strong> compassion in patient<br />
care that is team oriented. Call is 1:3. Previous <strong>Palliative</strong> <strong>Care</strong> experience<br />
is preferred. In addition, we offer:<br />
• Competitive salary<br />
• Attractive compensation/benefit package<br />
• Relocation assistance<br />
• Malpractice coverage<br />
• CME allowance<br />
Bethlehem, PA is only an hour from Philadelphia <strong>and</strong> 80 miles from<br />
New York City. The area provides numerous cultural, recreational,<br />
shopping <strong>and</strong> educational amenities without the high taxes <strong>and</strong><br />
cost of living of New York <strong>and</strong> New Jersey.<br />
Don’t leave your agency at risk<br />
CliCk Here for more information<br />
Advertisement<br />
information@rocsinc.com<br />
(919) 405-2162<br />
“Thank you so much! This is a huge relief.” <strong>Hospice</strong> Compliance Officer<br />
For more information, contact:<br />
Cindy Stokes<br />
800-678-7858 x64517 | cstokes@cejkasearch.com<br />
ID#149895H66<br />
cejkasearch.com<br />
Advertisement<br />
NewsLine<br />
June 2013<br />
1/4 page<br />
When life gets serious<br />
DTD 149895 IM<br />
you’ll want our serious experience on your side.<br />
It can easily happen.<br />
Your employees <strong>and</strong> volunteers have more on their minds than their driving. It may be<br />
a patient in distress, a grieving family or just the nagging pressure of falling behind a<br />
busy schedule. Auto accidents are a major cause of lawsuits against hospices <strong>and</strong> home<br />
health care agencies as well as a cause of serious injuries <strong>and</strong> lost time.<br />
Lawsuits are expensive to defend, <strong>and</strong> some result in very high-dollar losses. That’s why<br />
liability insurance coverage is so important. Glatfelter Healthcare Practice is administered<br />
by Glatfelter Insurance Group, a national agency. We work closely with your insurance<br />
agent to provide competitive proposals <strong>and</strong> friendly service for special businesses like yours.<br />
Remember, before you can take care of others,<br />
you have to take care of yourself.<br />
Advertisement<br />
Insurance for <strong>Hospice</strong>s <strong>and</strong><br />
Home Health <strong>Care</strong> Agencies<br />
■ Professional Liability<br />
■ General Liability<br />
■ Directors & Officers Liability<br />
■ Property Insurance<br />
■ Non-owned Auto Liability<br />
800-233-1957 www.GlatfelterHealthcarePractice.com<br />
Administered by Glatfelter Underwriting Services, Inc.a/k/a Glatfelter Insurance Services in CA, MN, NV, TX, <strong>and</strong> UT <strong>and</strong> Glatfelter Brokerage Services in NY<br />
NewsLine 25
From the NCHPP Allied Therapist Section*<br />
PT in<br />
<strong>Hospice</strong>:<br />
A Shared<br />
Partnership<br />
for Quality<br />
of Life<br />
By Karen Mueller,<br />
PT, DPT, PhD<br />
While most people<br />
do not view<br />
“physical therapy”<br />
<strong>and</strong> “hospice” as an obvious<br />
partnership, emerging evidence<br />
<strong>and</strong> recent healthcare policy<br />
change suggests that the time<br />
has come to reconsider this<br />
viewpoint.<br />
The Medicare <strong>Hospice</strong> Conditions<br />
of Participation (CoPs), for<br />
example, specifically requires<br />
that “physical therapy services<br />
be made available to patients<br />
<strong>and</strong> provided by licensed<br />
professionals.”<br />
When this rule was included in<br />
the 2008 revision of the <strong>Hospice</strong><br />
CoPs, it was no doubt a source<br />
of confusion among many health<br />
care providers, begging the<br />
question, why would any patient<br />
in hospice need the services of a<br />
physical therapist?<br />
The answer is simple, <strong>and</strong><br />
underscores the shared mission<br />
of NHPCO <strong>and</strong> the American<br />
Physical Therapy Association<br />
(APTA): To improve the quality<br />
of life of those we serve.<br />
Some Compelling Evidence<br />
Although physical therapy services<br />
are generally associated with<br />
the improvement of function<br />
through rehabilitation <strong>and</strong> other<br />
interventions, hospice patients also<br />
seek the best possible quality of<br />
life, which for most, involves the<br />
optimization of remaining function<br />
in light of their hospice diagnosis.<br />
Interventions related to the<br />
enhancement of comfort, function,<br />
energy conservation <strong>and</strong> nonpharmacological<br />
approaches to<br />
pain management are all within<br />
the physical therapy profession’s<br />
scope of practice, <strong>and</strong> these<br />
interventions can be highly<br />
effective for patients in hospice.<br />
By way of example, four powerful<br />
testimonies come to mind:<br />
• A two-year-old boy with a<br />
medulloblastoma underwent<br />
surgical resection <strong>and</strong> placement<br />
of a ventriculo-peritoneal<br />
shunt. <strong>Hospice</strong> physical therapy<br />
enabled his parents to address<br />
developmental sequence<br />
activities, positioning, <strong>and</strong><br />
equipment issues to promote<br />
mobility <strong>and</strong> quality of life<br />
during his months at homes<br />
at home.<br />
*The <strong>National</strong> Council of <strong>Hospice</strong> <strong>and</strong> <strong>Palliative</strong> Professionals (NCHPP) is comprised of 15 discipline-specific<br />
Sections that represents the staff <strong>and</strong> volunteers who work for NHPCO provider-members. To learn more<br />
about this NCHPP Section, visit the NHPCO website.<br />
26 NewsLine
• A 60-year-old female with<br />
metastatic cervical cancer<br />
<strong>and</strong> severe bilateral lower<br />
extremity lymphedema was<br />
able to ambulate with a walker<br />
in her home following manual<br />
lymphatic drainage <strong>and</strong> the<br />
application of compression<br />
b<strong>and</strong>aging.<br />
• A 12-year-old girl with<br />
Charcot-Marie-Tooth disease<br />
developed a glioblastoma<br />
<strong>and</strong> used a wheelchair<br />
following surgical resection,<br />
radiation, <strong>and</strong> experimental<br />
chemotherapy. Six-plus months<br />
of palliative home health<br />
physical therapy enabled her<br />
to gain sufficient strength <strong>and</strong><br />
function to return to school<br />
for her sixth-grade graduation,<br />
ambulating with bilateral<br />
AFOs <strong>and</strong> Lofstr<strong>and</strong> crutches.<br />
With her family, she enjoyed<br />
a Make a Wish trip to the<br />
Philippines. After subsequent<br />
tumor recurrence, she received<br />
hospice physical therapy<br />
services for family training in<br />
dependent transfers <strong>and</strong> bed<br />
care.<br />
• A 60-year-old male with<br />
metastatic brain cancer<br />
receiving home health<br />
hospice services requested<br />
physical therapy intervention<br />
for gait training so that he<br />
could walk to the dining<br />
room table for Thanksgiving<br />
dinner with his family. After<br />
three sessions of physical<br />
therapy intervention—which<br />
included strengthening,<br />
training for st<strong>and</strong>ing balance,<br />
<strong>and</strong> instruction in safe use<br />
of a walker— the patient<br />
accomplished his goal.<br />
Spreading the Word:<br />
HPC Special Interest<br />
Group<br />
Given the constraints of<br />
reimbursement <strong>and</strong> forthcoming<br />
changes to Medicare in light of the<br />
Affordable <strong>Care</strong> Act, members of<br />
the physical therapy profession are<br />
well aware of the need to educate<br />
healthcare professionals on the<br />
value of our services in all areas<br />
of practice, including hospice.<br />
To facilitate this education, former<br />
NHPCO Allied Therapist Section<br />
leader, Richard Briggs, MA, PT,<br />
approached the APTA about<br />
forming a <strong>Hospice</strong> <strong>and</strong> <strong>Palliative</strong><br />
<strong>Care</strong> Special Interest Group (HPC-<br />
SIG), which the APTA approved<br />
<strong>and</strong> officially launched in 2008. I<br />
had the honor of serving as vicechair<br />
of the HPC-SIG for the first<br />
three years, <strong>and</strong> became its chair<br />
in January of 2012.<br />
continued on next page<br />
A Few Facts<br />
Worth Noting<br />
• As of 2012, 224 of<br />
the nation’s 226 PT<br />
educational programs<br />
are at the doctoral level.<br />
• The physical therapist’s<br />
primary role is to<br />
enhance the patient’s<br />
subjective well-being<br />
<strong>and</strong> quality of life<br />
through the assessment,<br />
management <strong>and</strong><br />
prevention of health<br />
related conditions<br />
affecting movement,<br />
motor control <strong>and</strong><br />
function.<br />
• Physical therapists<br />
serve persons of<br />
all ages, from the<br />
youngest newborns to<br />
those at the end of life<br />
(many of whom desire<br />
a level of mobility<br />
in order to meet<br />
important life goals).<br />
• Physical therapists<br />
work with patients in a<br />
variety of care settings,<br />
including the home,<br />
hospital, rehab facility,<br />
<strong>and</strong> assisted living or<br />
long-term care setting.<br />
• According to the<br />
U.S. Bureau of Labor<br />
Statistics, there is an<br />
estimated 198,000<br />
physical therapists<br />
in the U.S. (<strong>and</strong> our<br />
aging population is<br />
expected to create a<br />
high dem<strong>and</strong> for their<br />
services).<br />
NewsLine 27
continued from previous page<br />
In the past five years, members of<br />
the HPC-SIG have made inroads<br />
in three key ways:<br />
• Inter-professional Education:<br />
We have been selected to<br />
present several educational<br />
sessions related to clinical<br />
specialties within our<br />
profession at the annual<br />
APTA Combined Section<br />
Meeting (typically held each<br />
February).<br />
• Outcomes Research: We<br />
have also published research<br />
to identify the impact of our<br />
interventions in a hospice<br />
population (see the bibliography<br />
at the end of this article).<br />
• Clinical Practice: We have<br />
also begun the development<br />
of an outcomes measure<br />
toolbox for the assessment of<br />
patients in hospice.<br />
Our efforts have also involved<br />
similar initiatives at the<br />
international level, with recent<br />
presentations at the World Congress<br />
of Physical Therapy (WCPT) in<br />
Amsterdam in 2011. More recently,<br />
Chris Wilson, the vice chair of<br />
our HPC-SIG, has worked with the<br />
WCPT to establish an international<br />
<strong>Hospice</strong> <strong>and</strong> <strong>Palliative</strong> <strong>Care</strong> Special<br />
Interest Group for the world<br />
community of physical therapists.<br />
Opportunities for a<br />
Future Alliance<br />
As we all know, great minds<br />
think alike <strong>and</strong>, thus, a<br />
prominent initiative of the APTA<br />
HPC-SIG is the establishment<br />
of formal liaisons with other<br />
leading organizations related to<br />
hospice <strong>and</strong> palliative care.<br />
Not surprisingly, NHPCO was<br />
the foremost of such professional<br />
groups, <strong>and</strong> in the past few<br />
months, members of the HPC-SIG<br />
have enjoyed several productive<br />
discussions with NCHPP Allied<br />
Therapist Section leader, Valerie<br />
Hartman, RN, CHPN, CTRN,<br />
which have underscored our<br />
shared values <strong>and</strong> mission.<br />
In the course of our discussions,<br />
we have identified several ways<br />
in which our organizations can<br />
align in the service of optimizing<br />
end-of-life care for all members<br />
of society. The first is the sharing<br />
of resources, particularly those<br />
related to clinical assessment<br />
measures. Both of our<br />
organizations also have helpful<br />
websites, educational conferences,<br />
<strong>and</strong> most importantly, a cadre<br />
of passionate professionals with<br />
a vision for delivering the best<br />
possible services to our patients.<br />
Other countless opportunities<br />
also exist, such as reciprocal<br />
28 NewsLine
attendance at APTA <strong>and</strong> NHPCO<br />
conferences, <strong>and</strong> the sharing of<br />
research, educational materials<br />
<strong>and</strong> clinical guidelines. As other<br />
key agencies, such as the Institute<br />
of Medicine (IOM), address the<br />
future of end-of-life care, each<br />
organization has the potential<br />
to shape future policy. For<br />
example, a member of the APTA<br />
provided public testimony from<br />
the HPC-SIG at the February, 2013<br />
inaugural meeting of the IOM<br />
Committee to transform end-of-life<br />
care. As a result of that meeting,<br />
it is hoped that our members will<br />
have the opportunity to provide<br />
comments <strong>and</strong> suggestions to<br />
future committee proceedings.<br />
Looking Ahead<br />
The anticipated changes in<br />
societal demographics (i.e. the<br />
aging of the 80 million-strong<br />
baby boomers), coupled with<br />
the ongoing restructuring of<br />
our nation’s healthcare delivery<br />
system, create unprecedented<br />
opportunities to enhance costeffective<br />
<strong>and</strong> compassionate<br />
end-of-life care in all realms<br />
of influence. Inter-professional<br />
initiatives will likely become<br />
increasingly prominent as the<br />
preferred means to this end.<br />
Thus, organizations with a<br />
shared mission, such as APTA<br />
<strong>and</strong> NHPCO, may best enhance<br />
their mutual efforts through a<br />
recognized alliance. As a member<br />
of both APTA <strong>and</strong> NHPCO, I<br />
am proud of the work of both<br />
organizations, <strong>and</strong> look forward<br />
to the continued exploration of<br />
effective innovative approaches to<br />
end-of-life care.<br />
Karen Mueller is a professor in<br />
the Physical Therapy Program at<br />
Northern Arizona University in<br />
Flagstaff, AZ. She also serves as<br />
a member of the NCHPP Allied<br />
Therapist Steering Committee <strong>and</strong><br />
chair of the <strong>Hospice</strong> <strong>and</strong> <strong>Palliative</strong><br />
<strong>Care</strong> Special Interest Group of<br />
the American Physical Therapy<br />
Association.<br />
Research Supporting the Role<br />
of PT in <strong>Hospice</strong>:<br />
• Toot J. Physical therapy <strong>and</strong> hospice:<br />
concept <strong>and</strong> practice. Physical Therapy.<br />
1984;62(5):665-671.<br />
• Ebel S. The role of the physical therapist in<br />
hospice care. American Journal of <strong>Hospice</strong><br />
<strong>and</strong> <strong>Palliative</strong> <strong>Care</strong>. 1993;10(5):32-35<br />
• Marcant D, Rapin CH. Role of physiotherapist<br />
in palliative care. Journal of Pain <strong>and</strong><br />
Symptom Management. 1993;8(2):68-71.<br />
• Marciniak CM, Sliwa JA, Spill G,<br />
Heinemann AW, Semik PE: Functional<br />
outcome following rehabilitation of cancer<br />
patient. Archives of Physical Medicine <strong>and</strong><br />
Rehabilitation. 1996;77:54-57.<br />
• Briggs R. Physical therapy in hospice care.<br />
Rehabilitation Oncology. 1997;15(3):16-17.<br />
• Sabers SR, Kokal JE, Girardi JC, Philpott<br />
CL, Basford JR, Therneau TM, Schmidt KD,<br />
Gamble GL.: Evaluation of consultationbased<br />
rehabilitation for hospitalized cancer<br />
patients with functional impairment. Mayo<br />
Clinical Proceedings. 1999;74:855–861<br />
• Mackey KM & Sparling JW. Experiences of<br />
older women with cancer receiving hospice<br />
care: significance for physical therapy.<br />
Physical Therapy. 2000;80:459-468.<br />
continued on next page<br />
We have published<br />
research to identify<br />
the impact of our<br />
interventions on<br />
hospice populations…<br />
NewsLine 29
continued from previous page<br />
• Briggs R. Models for physical therapy<br />
practice in palliative medicine.<br />
Rehabilitation Oncology. 2000;18(2):18-19.<br />
• Frost M. The role of physical,<br />
occupational, <strong>and</strong> speech therapy in<br />
hospice: patient empowerment. American<br />
Journal of <strong>Hospice</strong> <strong>and</strong> <strong>Palliative</strong> <strong>Care</strong>.<br />
2001;18(6):397-402.<br />
• Dal Bello-Haas V. A framework for<br />
rehabilitation of neurodegenerative<br />
diseases: planning care <strong>and</strong> maximizing<br />
quality of life. Neurology Report.<br />
2002;26(3):115-129.<br />
• Nieuwboer A, DeWeerdt W, Dom R,<br />
Bogaerts K. Prediction of outcome of<br />
physical therapy in advanced Parkinson’s<br />
disease. Clinical Rehabilitation.<br />
2002;16(8):886-893.<br />
• Montagini M, Lodhi M, Born W. The<br />
utilization of physical therapy in a<br />
palliative care unit. Journal of <strong>Palliative</strong><br />
Medicine. 2003(6)1:1-17<br />
• Pizzi MA, Briggs R. Occupational <strong>and</strong><br />
physical therapy in hospice: the facilitation<br />
of meaning, quality of life, <strong>and</strong> wellbeing.<br />
Topics in Geriatric Rehabilitation.<br />
2004;20(2):120-130.<br />
• Gudas SA. Terminal Illness, in Psychology<br />
in the Physical <strong>and</strong> Manual Therapies. New<br />
York, NY: Churchill Livingstone; 2004;333-<br />
350.<br />
• Galantino ML, Schimd P, Botis S, Dagan C,<br />
Leonard SM, Milos A. Exploring wellness<br />
coaching <strong>and</strong> traditional group support<br />
for breast cancer survivors: A pilot study.<br />
Rehabilitation Oncology. 2010;28(1):20-24.<br />
• Kumar SP, Jim A. Physical Therapy in<br />
<strong>Palliative</strong> <strong>Care</strong>: From Symptom Control to<br />
Quality of Life: A Critical Review. Indian<br />
Journal <strong>Palliative</strong> <strong>Care</strong>. 2010;16(3):138-146.<br />
• Briggs R, Mueller K. <strong>Hospice</strong> <strong>and</strong> end of<br />
life. In: Guccione AA, Wong RA, Avers D.<br />
(eds.) Geriatric Physical Therapy. 3rd ed. St<br />
Louis: Elsevier;2011.<br />
• Downing GM, Lynd PJ, Gallaher R, Hoens<br />
A. Challenges in underst<strong>and</strong>ing functional<br />
decline, prognosis <strong>and</strong> transitions in<br />
advanced illness. Topics in Geriatric<br />
Rehabilitation. 2011;27(1):18-28.<br />
• Javier NSC, Montagini ML. Rehabilitation<br />
of the hospice <strong>and</strong> palliative care<br />
patient. Journal of <strong>Palliative</strong> Medicine.<br />
2011;14(5):638-648.<br />
• Briggs R. Clinical decision making for<br />
physical therapists in patient-centered<br />
end-of-life care. Topics in Geriatric<br />
Rehabilitation. 2011;27(1):10-17.<br />
• Mueller K, Decker I. Impact of physical<br />
therapy intervention on functional<br />
outcomes <strong>and</strong> quality of life in a<br />
community hospice. Topics in Geriatric<br />
Rehabilitation. 2011:27(1):2-9<br />
• Cobb S, Kennedy N. Physical function<br />
in hospice patients <strong>and</strong> physiotherapy<br />
Interventions: A profile of hospice<br />
physiotherapy. Journal of <strong>Palliative</strong><br />
Medicine. 15(7):760-767.<br />
30 NewsLine
Advertisement<br />
HEALTHCARE CONSULTANTS<br />
NHPCO’S<br />
AFFINITY PROGRAM<br />
NHPCO’s Affinity Program is an exclusive NHPCO<br />
member benefit designed to:<br />
• Enhance your NHPCO membership investment<br />
• Offer unique benefits on price, products, <strong>and</strong> services<br />
• Increase value in your organization<br />
The following selected Affinity Program Partner programs <strong>and</strong> services are available<br />
to NHPCO members, their employees <strong>and</strong> volunteers:<br />
Visit www.nhpco.org/affinity to more info. For membership information,<br />
contact NHPCO Solutions Center at 800/646-6460 <strong>and</strong> ask for the Membership Department.<br />
NewsLine 31
Short Takes<br />
Award Winners<br />
Recognized at MLC<br />
Congressman Earl Blumenauer, a longtime hospice<br />
champion, welcomed more than 2,000 members <strong>and</strong><br />
industry experts to NHPCO’s 28th Management <strong>and</strong><br />
Leadership Conference held on April 25–27.<br />
As part of the conference <strong>and</strong> related events, six<br />
awards were presented to leaders involved in the field.<br />
Inaugural Quality Leadership Award:<br />
Joan Teno, MD, MS<br />
This new award<br />
was established<br />
to recognize<br />
demonstrated<br />
leadership,<br />
commitment, <strong>and</strong><br />
innovation that<br />
have significantly<br />
contributed to<br />
hospice organization excellence <strong>and</strong> improved care<br />
delivery <strong>and</strong> outcomes.<br />
Dr. Teno was recognized as the first recipient of this<br />
award for her work as a researcher <strong>and</strong> a clinician<br />
dedicated to underst<strong>and</strong>ing how to measure <strong>and</strong><br />
improve the quality of care for people at the end of life.<br />
Dr. Teno is a professor of Community Health <strong>and</strong><br />
Medicine <strong>and</strong> associate director of the Center<br />
for Gerontology <strong>and</strong> Health <strong>Care</strong> Research at the<br />
Brown Medical School as well as a health services<br />
researcher <strong>and</strong> hospice medical director. She is<br />
board certified in internal medicine, with added<br />
qualifications in Geriatrics <strong>and</strong> <strong>Palliative</strong> Medicine.<br />
Among her many accomplishments was her work as<br />
the lead investigator in a research effort to create a<br />
Toolkit of Instruments to Measure <strong>Care</strong> at the End of<br />
Life. As part of this grant effort, she also created the<br />
Family Evaluation of <strong>Hospice</strong> <strong>Care</strong>, a longst<strong>and</strong>ing<br />
NHPCO performance measure that is used by<br />
hospices nationwide.<br />
COS, FHSSA <strong>and</strong> NHF Also Present Awards<br />
COS Trailblazer Award<br />
The Council of States awarded Hawaii’s state hospice<br />
<strong>and</strong> palliative care organization, Kokua Mau, the<br />
2012 Trailblazer Award for its development of an<br />
innovative method to improve access to palliative<br />
care <strong>and</strong> increase quality of care among Hawaii’s<br />
providers. Its work, which included exp<strong>and</strong>ing<br />
educational opportunities for private healthcare<br />
plans, can serve as a model for other states.<br />
FHSSA Global Partnership Award<br />
The third annual FHSSA Global Partnership Award<br />
was presented to the Center for <strong>Hospice</strong> <strong>Care</strong> <strong>and</strong><br />
the <strong>Hospice</strong> Foundation of South Bend, Indiana, <strong>and</strong><br />
its partner, the <strong>Palliative</strong> <strong>Care</strong> Association of Ug<strong>and</strong>a<br />
in Kampala, Ug<strong>and</strong>a. To learn more, see the release<br />
on the FHSSA website.<br />
Three NHF Awards<br />
At the <strong>National</strong> <strong>Hospice</strong> Foundation Gala, held on<br />
April 25 in conjunction with the conference, three<br />
awards were presented: the Morfogen Art of Caring<br />
Award to Pulitzer-prize winning journalist, Ellen<br />
Goodman; the Philanthropic Inspiration Award to<br />
Run to Remember founder, Stuart Lazarus; <strong>and</strong><br />
the Buchwald Spirit Award for Public Awareness to<br />
actress <strong>and</strong> hospice volunteer, Torrey DeVitto. To<br />
learn more, see Giving Matters.<br />
32 NewsLine
2014 Circle of Life Award:<br />
Call for Nominations Ends August 5<br />
Sponsored annually, the prestigious Circle of Life Award celebrates<br />
innovation in palliative <strong>and</strong> end-of-life care. In 2014, up to three<br />
organizations will win the award while others may be recognized with<br />
citations of honor.<br />
All organizations or groups in the U.S. that provide palliative or endof-life<br />
care are eligible for the award. As a proud sponsor, NHPCO<br />
encourages all members to participate in the nomination process.<br />
Visit the<br />
Website of<br />
the American<br />
Hospital<br />
The Circle of Life Award: Celebrating Innovation in <strong>Palliative</strong> <strong>and</strong> End-of-Life <strong>Care</strong> is<br />
presented annually to honor organizations striving to improve the care provided to<br />
To nominate<br />
patients<br />
an<br />
with<br />
organization<br />
life-threatening conditions<br />
(either<br />
or near<br />
your<br />
the end<br />
own<br />
of life. In<br />
or<br />
2012,<br />
another),<br />
up to three<br />
visit the<br />
organizations will win Circle of Life Awards; additional organizations may receive<br />
website of the Citations American of Honor. Awards Hospital <strong>and</strong> citations Association will be presented the to American request Hospital an application.<br />
Association Health Forum Summit, July 19-21, 2012, in San Francisco.<br />
But please act soon—applications must be submitted by August 5, 2013.<br />
To nominate an organization or program (either your own or another), please go to<br />
http://www.aha.org/aha/news-center/awards/circle-of-life/circleoflife-nominations.html or<br />
e-mail circleoflife@aha.org. The application is available at<br />
http://www.aha.org/aha/news-center/awards/circle-of-life/application.html. All<br />
organizations or groups in the United States that provide palliative or end-of-life care are<br />
eligible for the award.<br />
Association<br />
to Learn More<br />
Applications are due August 8, 2011.<br />
More information on the award <strong>and</strong> previous recipients is available at<br />
http://www.aha.org/circleoflife. Please call the American Hospital Association Office of<br />
the Secretary at 312/422-2704 or e-mail circleoflife@aha.org with questions about the<br />
award process or application.<br />
Major sponsors for the Circle of Life Award are the American Hospital Association, the<br />
Catholic Health Association, <strong>National</strong> Consensus Project for Quality <strong>Palliative</strong> <strong>Care</strong>, <strong>and</strong><br />
the <strong>National</strong> <strong>Hospice</strong> <strong>and</strong> <strong>Palliative</strong> <strong>Care</strong> <strong>Organization</strong> & <strong>National</strong> <strong>Hospice</strong> Foundation;<br />
the American Academy of <strong>Hospice</strong> <strong>and</strong> <strong>Palliative</strong> Medicine <strong>and</strong> the <strong>National</strong> Association<br />
of Social Workers are Circle of Life cosponsors.<br />
The awards are supported, in part, by grants from the Archstone Foundation <strong>and</strong> the<br />
California Health<strong>Care</strong> Foundation, based in Oakl<strong>and</strong>, California.<br />
NewsLine 33
Member News <strong>and</strong> Notes<br />
$10,000 LIVESTRONG Grant to Benefit<br />
HCC’s <strong>Palliative</strong> <strong>Care</strong> Services<br />
In partnership with <strong>Hospice</strong> & Community <strong>Care</strong><br />
(HCC) based in Lancaster, PA, Lancaster General<br />
Hospital has received a $10,000 grant from the<br />
LIVESTRONG Foundation to advance palliative care<br />
<strong>and</strong> pursue certification.<br />
HCC utilized social<br />
media to spread the<br />
word about the grant<br />
competition <strong>and</strong> to request online votes to support<br />
the palliative program within the community.<br />
While 72 organizations throughout the country<br />
received LIVESTRONG grants, Lancaster General<br />
Health was the only Pennsylvania health system to<br />
win funding for its <strong>Palliative</strong> <strong>Care</strong> program.<br />
HOM Recognized for Mobile App to<br />
Improve Communication with Families<br />
<strong>Hospice</strong> of Michigan (based in Gr<strong>and</strong> Rapids) is<br />
being presented with a Spirit of Innovation Award<br />
at the June Home <strong>Care</strong> & <strong>Hospice</strong> LINK Conference<br />
in Chicago.<br />
Its mobile app, HOM<br />
<strong>Care</strong>s, notifies family<br />
members <strong>and</strong> friends<br />
when a care provider<br />
visits a loved one.<br />
Those who have the<br />
app can see a picture<br />
of the caregiver, the<br />
date <strong>and</strong> duration of the visit, <strong>and</strong> information about<br />
the caregiver’s background <strong>and</strong> type of support<br />
provided— such as medical, spiritual or social work.<br />
The app was developed with a $24,500 gift from<br />
Verizon <strong>and</strong> an in-kind donation from Compuware.<br />
<strong>Hospice</strong> by the Sea Wins the <strong>Hospice</strong><br />
Regattas <strong>National</strong> Championship<br />
The sailors who won the 23 regional hospice<br />
regattas held during 2012 gathered on Florida’s<br />
Tampa Bay during the weekend of April 12 to<br />
compete for the national championship.<br />
<strong>Hospice</strong> by the Sea as it takes the lead in the national<br />
championship. (Photo courtesy of St. Petersburg Yacht Club.)<br />
After three days of intense sailing, the four-man<br />
crew representing <strong>Hospice</strong> by the Sea (Boca Raton,<br />
FL) took first place—led by Captain Bret Moss,<br />
whose gr<strong>and</strong>father had taught him to sail more<br />
than 40 years ago <strong>and</strong> had also been served by<br />
hospice. Special kudus also go to the organization’s<br />
senior director of business development, George<br />
Tokesky, who stepped up at the last minute when<br />
one of the regular crew members had to withdraw<br />
from the race.<br />
Avow Wins 34th Annual Telly Award<br />
Avow (based in Naples, FL) took the Bronze at<br />
the 34th Annual Telly Awards which attracted<br />
more than 11,000 entries from 50 states as well as<br />
numerous countries.<br />
The program was recognized for three of its<br />
current broadcast advertisements which feature<br />
a family testimonial <strong>and</strong> two reenactments.<br />
The campaign was produced by members of the<br />
34 NewsLine
Avow advancement team,<br />
with creative services<br />
assistance from a local<br />
marketing firm. The<br />
commercials can be<br />
viewed at avowcares.<br />
org/video-gallery.<br />
Members of the Avow<br />
advancement team<br />
(l to r): Deborah Jonsson,<br />
Kit Chamberlain, Karen<br />
Stevenson <strong>and</strong> Kylee A. Pitts.<br />
Joint Effort Leads to Second Introductory Class on<br />
<strong>Hospice</strong> <strong>Care</strong> at Prestigious Notre Dame<br />
For the second year in a row, the Center for<br />
<strong>Hospice</strong> <strong>Care</strong> (South Bend, IN) <strong>and</strong> the University<br />
of Notre Dame teamed up to offer students a oneday<br />
introduction to hospice <strong>and</strong> palliative care.<br />
This year’s class, which attracted an impressive<br />
95 students (15 more than last year), featured<br />
12 different presentations that focused on how<br />
hospice <strong>and</strong> palliative care is given in the current<br />
Mark Murray<br />
healthcare system. The presentations were taught<br />
by various members of the interdisciplinary team—including Center for<br />
<strong>Hospice</strong> <strong>Care</strong> CEO, Mark Murray.<br />
Have News to Share?<br />
Add Us to Your Media<br />
Distribution List:<br />
newsline@nhpco.org<br />
NHPCO Staff Lend a H<strong>and</strong> as<br />
Spring for Alex<strong>and</strong>ria Volunteers<br />
More than 400 volunteers spent most<br />
of Friday, May 3, at 50 sites around<br />
Alex<strong>and</strong>ria, VA, as part of “Spring for<br />
Alex<strong>and</strong>ria”—an annual effort to make the<br />
city a cleaner, more beautiful place to live<br />
<strong>and</strong> work.<br />
Joining in were 10 staff from NHPCO,<br />
who painted 10 rooms at a local shelter—<br />
then went the extra mile by doing all the<br />
clean-up!<br />
NewsLine 35
Tip of the Month<br />
Compliance With the<br />
New HIPAA Omnibus Rule<br />
On January 17, 2013, an Omnibus<br />
Final Rule was released by the<br />
U.S. Department of Health <strong>and</strong><br />
Human Services’ Office for Civil Rights.<br />
This Final Rule implements modifications to<br />
HIPAA (the Health Information Technology<br />
for Economic <strong>and</strong> Clinical Health Act 1 )—<br />
<strong>and</strong> marks the most significant re-write of<br />
the HIPAA rules since the law was enacted.<br />
Compliance with most of the new<br />
requirements introduced in this rule<br />
is required by September 23, 2013. An<br />
extended compliance period is provided for<br />
the modification of certain existing business<br />
associate agreements, as described in the rule.<br />
So What Do Providers Need to Do?<br />
Be sure to complete the following updates<br />
by the September 23, 2013 deadline:<br />
• Update your patient privacy notices<br />
• Update your policy on reviewing<br />
<strong>and</strong> reporting a breach of protected<br />
health information (PHI) or electronic<br />
protected health information (ePHI)<br />
• Update your business associate<br />
agreements (unless they qualify for an<br />
extended transition period)<br />
• Update your fundraising communication<br />
to include an “opt-out” option for patients.<br />
Learn More:<br />
NHPCO has developed a helpful information<br />
sheet that gives hospice providers more<br />
details about the final rule. To access the<br />
<strong>PDF</strong>, visit www.nhpco.org/hipaa.<br />
The final rule can also be accessed online<br />
for reference: Omnibus Final Rule.<br />
1<br />
The Federal Register <strong>version</strong> of the Final Rule was<br />
published on January 25, 2013. 78 Fed. Reg. 5566<br />
(Jan. 25, 2013).<br />
Make Sure You See Every<br />
Regulatory Alert <strong>and</strong> Round-Up!<br />
Be sure to bookmark the Regulatory<br />
Alerts <strong>and</strong> Publications webpage<br />
of the NHPCO website for<br />
ongoing reference.<br />
It lists all Alerts <strong>and</strong> Round-Ups issued<br />
in chronological order, so it’s a good<br />
way to make sure you’re up to date<br />
on important news <strong>and</strong> changes<br />
affecting hospice providers.<br />
(These notifications are emailed to<br />
members who opt-in for Regulatory<br />
Communications but, oftentimes,<br />
SPAM filters impede delivery.)<br />
36 NewsLine
New Online Courses<br />
from NHPCO’s E-OL<br />
NHPCO’s End-of-Life Online (E-OL) offers online courses<br />
that are convenient, efficient learning modules for<br />
staff <strong>and</strong> volunteers at all levels of your organization.<br />
Here are a few of the recent additions:<br />
• <strong>Hospice</strong> <strong>and</strong> <strong>Palliative</strong> <strong>Care</strong>, Simply the Best with Ira Byock<br />
• Identifying <strong>and</strong> Addressing Traumatic Stress at the End-Of-Life<br />
with Therese R<strong>and</strong>o<br />
• Shed for Success: How to Stay Alive <strong>and</strong> Thrive in the Midst of<br />
Turbulent Healthcare Change with Kathy Dempsey<br />
• Pediatric <strong>Palliative</strong> <strong>Care</strong> Training Series - Module 7:<br />
Pediatric <strong>Palliative</strong> <strong>Care</strong> Symptom Management<br />
Plus, Several on Volunteer Management <strong>and</strong> Leadership:<br />
• Regulatory Matters for Volunteer Leaders with Judy Lund Person<br />
• Do it Well, Make it Fun, the Key to Success in Volunteer<br />
Management with Ron Culberson<br />
• Ignite your Leadership Potential with Claire Tehan<br />
• The New Breed of Volunteer with Thomas McKee<br />
• Volunteers: Exceptionalism in <strong>Care</strong> <strong>and</strong> Practice with<br />
Gary Gardia <strong>and</strong> Danae Delman<br />
Check Out the New ‘A-Z’ Course List Too:<br />
To easily peruse the range of courses available, visit the<br />
E-OL “A to Z Course List” on the NHPCO website <strong>and</strong><br />
simply scroll <strong>and</strong> click on the offerings of interest.<br />
The webpage about each offering shows the cost of<br />
the course, details about what it covers, <strong>and</strong> whether<br />
it qualifies for CE/CME.
Videos Worth Watching<br />
This year’s <strong>National</strong> <strong>Hospice</strong> Foundation<br />
Gala, held on April 25 in conjunction with<br />
MLC, paid tribute to the youngest <strong>and</strong><br />
bravest we care for in hospice—our pediatric<br />
patients. As part of the event’s program,<br />
NHF aired this moving video <strong>and</strong> raised<br />
$28,000 in just 10 minutes. The money will<br />
go toward development of educational resources to raise awareness among<br />
consumers <strong>and</strong> support the work of providers. Watch the video now−<strong>and</strong><br />
feel free to share it with your colleagues <strong>and</strong> supporters.<br />
(The new edition of NHPCO’s ChiPPS Pediatric <strong>Palliative</strong> <strong>Care</strong> E-newsletter<br />
is now out, with articles about supporting fathers <strong>and</strong> the other male<br />
members of the child’s family. Be sure to take a look.)<br />
Links to Some<br />
Resources on the<br />
NHPCO Website<br />
Quality <strong>and</strong> Regulatory<br />
Quality Reporting Requirements<br />
QAPI Resources<br />
Regulatory Center Home Page<br />
Fraud <strong>and</strong> Abuse<br />
Past Regulatory Alerts <strong>and</strong><br />
Roundups<br />
Staffing Guidelines<br />
St<strong>and</strong>ards of Practice<br />
1731 King Street, Suite 100<br />
Alex<strong>and</strong>ria, VA 22314<br />
703/837-1500<br />
www.nhpco.org • www.caringinfo.org<br />
NewsLine is a publication of the <strong>National</strong> <strong>Hospice</strong> <strong>and</strong> <strong>Palliative</strong> <strong>Care</strong> <strong>Organization</strong><br />
Vice President, Communications . . . . . . . . . . . . . . . . . . . . .Jon Radulovic<br />
Editor . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . Sue Canuteson<br />
Advertising Inquiries . . . . . . . . . . . . . . . . . . Grace Zupancic, 703/837-3134<br />
Membership Inquiries . . . . . . . . . . . . . . . . . . . . . . . . . . . 800/646-6460<br />
Copyright © 2012, NHPCO <strong>and</strong> its licensors. All rights reserved. NHPCO does not<br />
endorse the products <strong>and</strong> services advertised in this publication.<br />
All past issues of NewsLine are posted online: www.nhpco.org/newsline.<br />
State-specific Resources<br />
Quality Partners<br />
Self-Assessment System<br />
Outreach<br />
2013 Volunteer Ads<br />
2012-13 Outreach Materials<br />
Resources to Reach<br />
the Underserved<br />
Professional Education<br />
Education Home Page<br />
2013 Monthly Webinars<br />
End-of-Life Online<br />
NCHPP Home Page<br />
Publications<br />
Past issues of weekly NewsBriefs<br />
Affiliates:<br />
Past issues of monthly NewsLine<br />
Past issues of ChiPPS Newsletter
SPRING 2013<br />
<strong>Hospice</strong> Patient <strong>and</strong> Veteran Visits World<br />
War II Memorial<br />
Honoring Service is an Important Part of One Man’s<br />
End-of-Life Experience<br />
On a brisk Monday morning in April, 92-year-old Veteran Kenneth Baeth<br />
absorbed the sight of the World War II Memorial on the <strong>National</strong> Mall in<br />
Washington, DC for the first time. From the viewpoint of his wheelchair,<br />
Baeth participated in a ceremony honoring his service along with that of<br />
dozens of fellow Veterans from his home state of Montana. Each of the<br />
Veterans was flown to Washington under “Big Sky Honor Flight” a Montana<br />
program that is a member of the Honor Flight Network, a non-profit<br />
organization created to honor America’s WWII Veterans for all their sacrifices.<br />
Kenneth Baeth <strong>and</strong> son, Roger, visit the World War II<br />
Memorial in Washington, DC<br />
• CONTENTS<br />
<strong>Hospice</strong> Patient <strong>and</strong> Veteran Visits World<br />
War II Memorial; page 1<br />
<strong>National</strong> <strong>Hospice</strong> Foundation 9th Annual<br />
Gala; page 2<br />
Lighthouse of Hope Fund Provides<br />
Meaningful <strong>and</strong> Memorable Experiencesfor<br />
Adult <strong>Hospice</strong> Patients; page 3<br />
Foundation Board Chair, Samira Beckwith<br />
Elected Vice-Chair of <strong>National</strong> Coalition of<br />
Cancer Survivorship; page 3<br />
Honor. Remember. Invest.; page 4<br />
NHPCO Begins Collaborative Efforts with<br />
the Funeral Industry; page 4<br />
Run to Remember: A Look at Two Special<br />
Kentucky Bourbon Chase Runners; page 5<br />
The program, with 121 hubs in 41 states, brings World War II Veterans to<br />
Washington, DC so that they may see the memorial erected in their honor.<br />
Baeth is facing the end of life with the help of his children <strong>and</strong> Rocky<br />
Mountain <strong>Hospice</strong>. He traveled to Washington with his oldest son, Roger<br />
<strong>and</strong> several volunteers from Rocky Mountain <strong>Hospice</strong>.<br />
“It takes a lot of courage to get old,” said Roger. His father was nervous about traveling<br />
because of his health, Roger said, but he was loving every minute of the experience. Baeth<br />
contracted mesothelioma as a result of asbestos exposure while working in a mine as a<br />
young man; he is now dying of heart disease. Making the trip required extra physical<br />
therapy to increase his stamina <strong>and</strong> mobility.<br />
At the age of 20, Kenneth Baeth’s dream of flying became a reality when he enlisted in the<br />
U.S. Army Air Corps. It was 1942, in the midst of World War II. St<strong>and</strong>ing at 5’2” tall,<br />
Kenneth Baeth looked like a perfect c<strong>and</strong>idate to be a nose gunner, a man who crawled<br />
inside the nose of a fighter plane to operate a machine gun turret.<br />
“I didn’t dream it would be so big,” Baeth remarked about the memorial. “The U.S. can<br />
pull itself together to do anything,” he said. During the ceremony, Baeth met another nose<br />
gunner who fought in the Pacific during the war. The two exchanged phone numbers <strong>and</strong><br />
planned to talk <strong>and</strong> exchange stories upon returning to Montana.<br />
The <strong>National</strong> <strong>Hospice</strong> <strong>and</strong> <strong>Palliative</strong> <strong>Care</strong> <strong>Organization</strong> works with the U.S. Department of<br />
Veterans Affairs (VA) to meet the unique needs of Veterans like Baeth with terminal illness.<br />
The We Honor Veterans program, developed in collaboration with the VA, provides local<br />
hospices with resources to broaden education <strong>and</strong> underst<strong>and</strong>ing of how best to honor<br />
our Veterans <strong>and</strong> respect their wishes <strong>and</strong> concerns at the end of life. Funds raised by the<br />
<strong>National</strong> <strong>Hospice</strong> Foundation support the We Honor Veterans program.<br />
To learn more about We Honor Veterans, visit: www.wehonorveterans.org.<br />
To learn more about the Honor Flight Network, visit: www.honorflight.org.<br />
To make a donation, visit www.nationalhospicefoundation.org/veterans<br />
A newsletter of the <strong>National</strong> <strong>Hospice</strong> Foundation | Spring 2013 1
Employees of The Elizabeth <strong>Hospice</strong> join in on the NHF Gala Celebration<br />
<strong>National</strong> <strong>Hospice</strong> Foundation 9th Annual Gala<br />
Honored Pediatric <strong>Palliative</strong> <strong>Care</strong> <strong>and</strong> <strong>Hospice</strong><br />
Patients <strong>and</strong> <strong>Care</strong>givers<br />
“Our<br />
celebration<br />
was held in<br />
tribute to<br />
the youngest<br />
<strong>and</strong> bravest<br />
of those we<br />
care for in<br />
hospice”<br />
Outst<strong>and</strong>ing Efforts in Supporting<br />
<strong>Hospice</strong> Recognized During<br />
Celebration<br />
On Friday, April 26th, NHF held its 9th<br />
Annual Gala as part of the NHPCO’s 28th<br />
Management <strong>and</strong> Leadership Conference at<br />
the Gaylord <strong>National</strong> Resort <strong>and</strong> Convention<br />
Center at <strong>National</strong> Harbor, MD.<br />
“Our celebration was held in tribute to the<br />
youngest <strong>and</strong> bravest of those we care for in<br />
hospice: our pediatric patients. <strong>Hospice</strong><br />
professionals recognize that caring for<br />
pediatric patients <strong>and</strong> their family members<br />
requires a unique approach <strong>and</strong> set of skills.<br />
NHPCO works to raise awareness <strong>and</strong><br />
provide educational resources to those<br />
providing that care. We’re thankful to those<br />
who joined in our celebration in support of<br />
that work,” said J. Donald Schumacher,<br />
president <strong>and</strong> CEO of NHPCO.<br />
Local ABC News Anchor, Greta Kreuz served<br />
as Mistress of Ceremonies for the event<br />
attended by over 500 guests. Three awards<br />
were presented to individuals who have<br />
contributed to hospice in significant <strong>and</strong><br />
unique ways.<br />
Stuart Lazarus received the Philanthropic<br />
Inspiration Award for his commitment to<br />
raising funds for hospice. In 2002, Lazarus<br />
combined his love of running with his<br />
passion for hospice to create a successful<br />
fundraising program, Run to Remember<br />
(www.runtoremember.org). This program<br />
gives runners <strong>and</strong> walkers an opportunity to<br />
celebrate <strong>and</strong> honor the memory of their<br />
loved ones <strong>and</strong> raises funds for hospice on a<br />
local, national, <strong>and</strong> international level.<br />
Ellen Goodman was granted the<br />
Morfogen Art of Caring Award. The<br />
Pulitzer Prize- winning journalist received<br />
the award for The Conversation Project<br />
(theconversationproject.org), an effort to<br />
engage the public in conversations about<br />
the end of life by sharing stories about<br />
“good deaths” <strong>and</strong> “bad deaths” <strong>and</strong> offering<br />
tools to make these conversations easier.<br />
Torrey DeVitto, an actress <strong>and</strong> active<br />
hospice volunteer, was given the Buchwald<br />
Spirit Award for Public Awareness. As<br />
NHPCO’s very first <strong>Hospice</strong> Ambassador,<br />
DeVitto frequently finds opportunities<br />
through interviews, social media, <strong>and</strong><br />
appearances to bring more attention to<br />
hospice care <strong>and</strong> bring awareness to a<br />
2<br />
A newsletter of the <strong>National</strong> <strong>Hospice</strong> Foundation | Spring 2013
Lighthouse of Hope Fund Provides Meaningful <strong>and</strong><br />
Memorable Experiences for Adult <strong>Hospice</strong> Patients<br />
NHF has launched the Lighthouse of<br />
Hope Fund, a new program that will help<br />
local hospice programs create<br />
meaningful <strong>and</strong> memorable experiences<br />
at the end of life for adult patients <strong>and</strong><br />
their family members.<br />
Kelli Singleton, Tracey Truscott, Cindy Scott, Jennifer<br />
Hudes, Laura Avanesyan <strong>and</strong> Monica Lewis McCommas<br />
of Silverado <strong>Hospice</strong>.<br />
younger age group. She created the theme<br />
for the 2012 <strong>National</strong> <strong>Hospice</strong> <strong>and</strong> <strong>Palliative</strong><br />
<strong>Care</strong> Month, “Comfort. Love. Respect.”<br />
Nearly $100,000 was raised during the event,<br />
including over $29,000 from a live auction.<br />
These funds will be used to support all of<br />
NHPCO’s work in pediatric hospice care.<br />
NHF would like to thank its Gala Sponsors:<br />
Ruby Sponsors:<br />
• Suncoast Solutions<br />
• Suncoast <strong>Hospice</strong><br />
Tanzanite Sponsors:<br />
• Gentiva <strong>Hospice</strong><br />
Amethyst Sponsors:<br />
• Samira K. Beckwith <strong>and</strong> Hope<br />
Health<strong>Care</strong> Services<br />
• Center for <strong>Hospice</strong> <strong>Care</strong><br />
• Chapters Health System<br />
• Community Health Accreditation Program<br />
• The Elizabeth <strong>Hospice</strong><br />
• Gilchrist <strong>Hospice</strong> <strong>Care</strong><br />
• Glatfelter Healthcare Practice<br />
• VITAS Innovative <strong>Hospice</strong> <strong>Care</strong><br />
Next year’s gala will be held on Friday,<br />
March 28, 2014 also at the Gaylord<br />
<strong>National</strong> Resort <strong>and</strong> Convention Center<br />
in conjunction with NHPCO’s 29th<br />
Management <strong>and</strong> Leadership Conference.<br />
By choosing to participate in the Fund,<br />
which includes an annual $500<br />
registration fee, hospice programs will be<br />
able to request up to $1,500 in total on<br />
behalf of their patients by the end of the<br />
year. These funds might be used toward<br />
any number of life experiences for their patients such as flying loved ones in to visit,<br />
special events such as trips or celebrations, or any opportunity to spend quality time<br />
with family <strong>and</strong> friends.<br />
“We know many of the ways hospice improves quality of life for patients <strong>and</strong> family<br />
caregivers through skilled interdisciplinary care. Our new Lighthouse of Hope<br />
program will allow hospices to add another dimension to the services they provide<br />
to those under their care,” said John Mastrojohn, NHF executive director.<br />
Seed funding for the Fund came from the assets of the Lighthouse Foundation,<br />
which were generously designated to NHF in mid-2012 when the parent hospice of<br />
the Lighthouse Foundation was purchased. The Fund will be sustained through<br />
annual fees of participating hospices, generous contributions of individuals,<br />
corporations, <strong>and</strong> foundations.<br />
To learn more about the Lighthouse of Hope Fund, or to make a donation, visit:<br />
www.nationalhospicefoundation/lighthouseofhopefund.<br />
Foundation Board Chair, Samira Beckwith<br />
Elected Vice-Chair of <strong>National</strong> Coalition of<br />
Cancer Survivorship<br />
Samira Beckwith,<br />
Foundation Board Chair<br />
Samira Beckwith, Foundation Board Chair <strong>and</strong> president <strong>and</strong><br />
CEO of Hope Health<strong>Care</strong> Services, has been elected vice chair<br />
of the board of directors for the <strong>National</strong> Coalition of Cancer<br />
Survivorship, which advocates for quality cancer care for all<br />
people touched by cancer <strong>and</strong> provides tools that empower<br />
people to advocate for themselves.<br />
Beckwith has twice survived cancer; she was diagnosed with<br />
Hodgkin’s lymphoma at age 24 <strong>and</strong> later, breast cancer. Her<br />
experiences helped shaped Beckwith’s career mission to ensure access to quality,<br />
compassionate health care services for all.<br />
NHF congratulations Samira on her new role, <strong>and</strong> is grateful for her continued<br />
dedication <strong>and</strong> service to hospice.<br />
A newsletter of the <strong>National</strong> <strong>Hospice</strong> Foundation | Spring 2013<br />
3
NHPCO Begins Collaborative Efforts<br />
with the Funeral Industry<br />
Work Begins with a Joint Effort with<br />
<strong>National</strong> Funeral Directors Association<br />
The end of life is a difficult time for the family members <strong>and</strong> loved<br />
ones helping the patient through the last phase of life. In the<br />
midst of their grief, arrangements must be made to honor the<br />
person who has died, including funeral details. Because of the<br />
shared experience in working with families through this process,<br />
NHPCO has begun efforts to bring hospice professionals <strong>and</strong> the<br />
funeral service industry together to work <strong>and</strong> learn from one<br />
another. The first such collaboration is with the <strong>National</strong> Funeral<br />
Directors Association (NFDA).<br />
<strong>Hospice</strong> professionals are skilled in providing pain management<br />
<strong>and</strong> addressing the psychological, social <strong>and</strong> spiritual needs of<br />
not only the patient, but their loved ones as well. That care<br />
continues into the bereavement process. Memorial services <strong>and</strong><br />
funerals are often an important part of that process, <strong>and</strong> funeral<br />
directors play a critical role in ensuring that those services reflect<br />
the life that is being honored <strong>and</strong> are meaningful to family<br />
members <strong>and</strong> loved ones.<br />
Often, hospice workers develop close bonds with the families they<br />
care for <strong>and</strong> are relied upon for guidance <strong>and</strong> advice following the<br />
death of their loved one. Funeral directors are trained <strong>and</strong><br />
experienced in the many options available to families <strong>and</strong> are<br />
there to work with families to help them commemorate the life of<br />
their loved one in a meaningful way. By working together, hospices<br />
<strong>and</strong> funeral homes can share their expertise <strong>and</strong> assist families<br />
through this emotional process.<br />
“There are many examples of hospices working closely with funeral homes in their area to ease the difficulty of planning for the<br />
emotional time that follows the death of a loved one. By collaborating on an association level, such as with NFDA, we can help to<br />
spread those relationships,” said J. Donald Schumacher, president <strong>and</strong> CEO of NHPCO.<br />
“Each of our professions brings a unique perspective to serving the dying, those who have died, <strong>and</strong> the bereaved. We look<br />
forward to developing materials <strong>and</strong> tools with NHPCO to share our experiences <strong>and</strong> expertise. The families we care for will<br />
benefit by two organizations focused on end-of- life care working h<strong>and</strong>-in-h<strong>and</strong> to ease the transition,” said Robert “Bob” T.<br />
Rosson, CFSP, CPC, NFDA president.<br />
NFDA is the world’s leading <strong>and</strong> largest funeral service association, serving 18,500 individual members who represent nearly<br />
10,000 funeral homes in the United States <strong>and</strong> 43 countries around the world. NFDA offers funeral professionals comprehensive<br />
educational resources, tools to manage successful businesses, guidance to become pillars in their communities <strong>and</strong> the expertise<br />
to foster future generations of funeral professionals. NFDA is headquartered in Brookfield, Wis., <strong>and</strong> has an office in Washington,<br />
D.C. For more information, visit www.nfda.org.<br />
By sharing educational materials <strong>and</strong> resources, hospice <strong>and</strong> funeral service professionals will learn more about the areas of<br />
expertise each bring to the table. Future plans for collaboration include presenting educational tools at the professional<br />
conferences of each organization, <strong>and</strong> eventually developing information directed toward consumers.<br />
4 A newsletter of the <strong>National</strong> <strong>Hospice</strong> Foundation | Spring 2013
Run to Remember: A Look at Two Special Kentucky<br />
Bourbon Chase Runners<br />
Arjit <strong>and</strong> Sourav Guha<br />
One Man Runs in Honor of His Brother Who<br />
Sought to Turn Personal Adversity into<br />
Positive Change for Others<br />
Sourav Guha will join the Run to Remember family this<br />
fall as he <strong>and</strong> 11 of his friends take on the Bourbon<br />
Chase. The race is a 200-mile overnight relay along the<br />
Kentucky Bourbon Trail. The group will be running in<br />
honor of Guha’s brother, Arijit, who died of metastatic<br />
colon cancer earlier this year: www.active.com/donate/<br />
runtoremember2013/souravguha.<br />
Arijit was diagnosed with Stage IV cancer in 2011, shortly after his 30th birthday, while a<br />
graduate student at Arizona State University. After less than a year of treatment, he reached<br />
the lifetime coverage cap on his student health policy. Always a resourceful activist <strong>and</strong><br />
relentless advocate on behalf of himself <strong>and</strong> others, Arijit created a website (poopstrong.org)<br />
to raise awareness of his situation <strong>and</strong> funds for his treatment.<br />
Facing medical bankruptcy, but keenly aware that his situation was not dissimilar from that of<br />
many others, Arijit also took to social networks to dem<strong>and</strong> better coverage <strong>and</strong> received<br />
international press coverage of his successful campaign. As a result, the insurance company<br />
agreed to extend their coverage of his medical bills.<br />
Arjit <strong>and</strong> his wife, Heather, were able to donate the more than $130,000 they had raised to a<br />
variety of cancer-related charities assisting those in financial need. Grateful for opportunity to<br />
help others, Arijit always emphasized that his personal victory should only be considered the<br />
beginning of a much broader movement. He was proud that the attention he received as an<br />
individual was part of a much larger national conversation about inequities in healthcare<br />
access in American society.<br />
Toward the end of 2012, with his tumors having further metastasized, Arijit made the difficult<br />
decision to end treatment. At the beginning of this year, he began receiving palliative home<br />
care from <strong>Hospice</strong> of the Valley in Phoenix. He passed away peacefully, with his wife <strong>and</strong> his<br />
hospice nurse by his side, in March. Arijit faced life <strong>and</strong> death with passion <strong>and</strong> a sense of<br />
humor <strong>and</strong> perspective.<br />
“Wherever he went,” says Sourav, “fun <strong>and</strong> friends were sure to surround him, so the<br />
Bourbon Chase seems a fitting way to remember <strong>and</strong> honor Arijit. He encountered every<br />
situation in life with positivity <strong>and</strong> gratitude, <strong>and</strong> I would like for all of us who loved <strong>and</strong><br />
admired him to try to do the same. We are so grateful for the care <strong>and</strong> respect that he <strong>and</strong><br />
we received from <strong>Hospice</strong> of the Valley, <strong>and</strong> in particular from his nurse, Cheryl Amburgey,<br />
<strong>and</strong> social worker, Ray Unks.”<br />
The 12-person team has come up with an<br />
impressive array of creative fund-raising ideas.<br />
Breeding <strong>and</strong> her colleagues will be<br />
participating in a weekend festival held by<br />
one of their physical therapy clinics. They<br />
plan to raise funds at the festival through a<br />
silent auction, offering pay-per-minute<br />
massages <strong>and</strong> selling tickets to employees<br />
for a chance to throw a pie in the face of their<br />
managers. Additional fund-raising efforts<br />
of the team include:<br />
• Selling chocolates for a local chocolate<br />
factory in Lexington, KY<br />
• Working at a portable st<strong>and</strong> at local<br />
minor league baseball games<br />
• Hosting bake sales<br />
• Holding a charity Hip Hop Hustle<br />
aerobics class<br />
• Organizing a Cornhole Tournament<br />
With all of these creative efforts, there is<br />
no doubt team “Don’t Pull a Hammy” will<br />
reach their goal of raising $6,000 for NHF<br />
<strong>and</strong> <strong>Hospice</strong> of the Bluegrass. Their<br />
donation page is www.active.com/donate/<br />
runtoremember2013/teamdrayer.<br />
NHF wishes Sourav, Christina, their teams <strong>and</strong><br />
all Run to Remember participants the best of<br />
luck in their race <strong>and</strong> fundraising goals! You<br />
too can run any race at any pace to raise funds<br />
for hospice. Visit www.nationalhospice<br />
foundation/runtoremember.org to learn more<br />
about NHF’s signature fundraising <strong>and</strong> race<br />
training program.<br />
Christina Breeding with Lexington Legends mascot<br />
Team “Don’t Pull a Hammy” Pulls Out All the Stops for Creative Fundraising<br />
Christina Breeding will also be participating in the Bourbon Chase in October as team<br />
captain for Drayer Physical Therapy Institute. Team “Don’t Pull a Hammy” will be raising<br />
funds for NHF <strong>and</strong> <strong>Hospice</strong> of the Bluegrass, which cared for both of Christina’s gr<strong>and</strong>fathers<br />
at the end of their lives.<br />
“I want others to experience the same comforting care <strong>and</strong> have the opportunity to be at<br />
home with the people they love the most in those final moments. Running this race in<br />
memory [of my gr<strong>and</strong>parents] is one way I can do that,” said Christina.<br />
A newsletter of the <strong>National</strong> <strong>Hospice</strong> Foundation | Spring 2013<br />
5
1731 King Street, Alex<strong>and</strong>ria, Virginia 22314<br />
Ph: 703-516-4928 or 877-470-6472<br />
Fax: 703-837-1233<br />
info@nationalhospicefoundation.org<br />
Social Networking with NHF<br />
Join the conversation on Facebook!<br />
www.facebook.com/NatHospFdn<br />
Follow our tweets at Nhf_news<br />
Learn more about NHF at<br />
www.nationalhospicefoundation.org