The role of NT-proBNP in the management of suspected heart failure
The role of NT-proBNP in the management of suspected heart failure
The role of NT-proBNP in the management of suspected heart failure
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
disease focus<br />
C ardiovascular Disease<br />
As published <strong>in</strong> CLI - September 2006<br />
<strong>The</strong> <strong>role</strong> <strong>of</strong> <strong>NT</strong>-<strong>proBNP</strong> <strong>in</strong> <strong>the</strong> <strong>management</strong><br />
<strong>of</strong> <strong>suspected</strong> <strong>heart</strong> <strong>failure</strong><br />
by Dr P. Hildebrandt<br />
Chronic <strong>heart</strong> <strong>failure</strong> is <strong>of</strong>ten under- or mis-diagnosed due to lack <strong>of</strong> diagnostic resources. Measurement <strong>of</strong> <strong>NT</strong>-<strong>proBNP</strong> level<br />
for screen<strong>in</strong>g patients with symptoms suggestive <strong>of</strong> chronic <strong>heart</strong> <strong>failure</strong> has been shown to have a very high sensitivity and<br />
an acceptable specificity, mak<strong>in</strong>g it ideal for such screen<strong>in</strong>g, as well as allow<strong>in</strong>g a reduction <strong>in</strong> <strong>the</strong> number <strong>of</strong> echocardiographies<br />
carried out. In acute <strong>heart</strong> <strong>failure</strong> patients <strong>NT</strong>-<strong>proBNP</strong> level has proved to be very valuable for cl<strong>in</strong>icians mak<strong>in</strong>g decisions<br />
on appropriate action at <strong>in</strong>itial presentation, dur<strong>in</strong>g treatment and at discharge. In <strong>the</strong> acute sett<strong>in</strong>g additional markers<br />
such as tropon<strong>in</strong> T, CK MB and haemoglob<strong>in</strong> are frequently <strong>in</strong>dicated for evaluat<strong>in</strong>g o<strong>the</strong>r cardiac conditions, e.g. myocardial<br />
<strong>in</strong>farction. <strong>The</strong>se analyses can be carried out ei<strong>the</strong>r on a laboratory platform or us<strong>in</strong>g PoC test<strong>in</strong>g.<br />
One <strong>of</strong> <strong>the</strong> major challenges <strong>in</strong> modern cardiology<br />
is <strong>the</strong> appropriate treatment <strong>of</strong> <strong>heart</strong> <strong>failure</strong><br />
patients. Heart <strong>failure</strong> can occur <strong>in</strong> chronic (CHF)<br />
[1] and acute (AHF) forms [2], <strong>the</strong> latter <strong>in</strong>clud<strong>in</strong>g<br />
patients with de novo <strong>heart</strong> <strong>failure</strong> as well as<br />
patients with an acute exacerbation <strong>of</strong> CHF. Both<br />
<strong>of</strong> <strong>the</strong>se disease expressions present <strong>the</strong> cl<strong>in</strong>ician<br />
with diagnostic and screen<strong>in</strong>g challenges, for<br />
which levels <strong>of</strong> B-type natriuretic peptides have<br />
proved to be valuable.<br />
Chronic <strong>heart</strong> <strong>failure</strong> (CHF) - background<br />
<strong>The</strong> aetiology <strong>of</strong> CHF is most <strong>of</strong>ten ischaemic, but<br />
<strong>the</strong> condition can also be <strong>the</strong> result <strong>of</strong> hypertension<br />
or valve diseases. CHF is a common disease<br />
with a prevalence <strong>of</strong> approximately 1% <strong>of</strong> <strong>the</strong><br />
population, a prevalence which is <strong>in</strong>creas<strong>in</strong>g, presumably<br />
due to better treatment <strong>of</strong> patients with<br />
acute <strong>heart</strong> <strong>failure</strong> as well as ischaemic <strong>heart</strong> disease,<br />
lead<strong>in</strong>g to an <strong>in</strong>creased survival <strong>of</strong> patients<br />
with chronic <strong>heart</strong> disease. CHF is a serious disease<br />
with a very high risk <strong>of</strong> mortality, equivalent<br />
to many cancers, and is fur<strong>the</strong>rmore an expensive<br />
disease for society because <strong>of</strong> <strong>the</strong> many hospital<br />
readmissions. On <strong>the</strong> positive side, <strong>the</strong> emergence<br />
<strong>of</strong> modern pharmacological and mechanical treatment<br />
options has reduced morbidity and mortality.Unfortunately,<br />
a major problem <strong>in</strong> <strong>the</strong> <strong>management</strong><br />
<strong>of</strong> <strong>heart</strong> <strong>failure</strong> is <strong>the</strong> large <strong>in</strong>cidence <strong>of</strong><br />
under- and mis-diagnoses.<br />
Chronic <strong>heart</strong> <strong>failure</strong> - def<strong>in</strong>ition and diagnosis<br />
<strong>The</strong> most commonly used def<strong>in</strong>ition <strong>of</strong> <strong>heart</strong> <strong>failure</strong><br />
is <strong>the</strong> presence <strong>of</strong> symptoms suggestive <strong>of</strong><br />
<strong>heart</strong> <strong>failure</strong> (most <strong>of</strong>ten dyspnoea, peripheral<br />
oedema or fatigue) as well as objective evidence <strong>of</strong><br />
impaired cardiac function. <strong>The</strong> most commonly<br />
used method for evaluation <strong>of</strong> cardiac function is<br />
echocardiography, an <strong>in</strong>vestigation which requires<br />
expensive equipment and tra<strong>in</strong>ed sonographers.<br />
Because <strong>the</strong> symptoms <strong>of</strong> <strong>heart</strong> <strong>failure</strong> are ra<strong>the</strong>r<br />
nonspecific, and also occur <strong>in</strong> o<strong>the</strong>r illnesses and<br />
<strong>in</strong> decondition<strong>in</strong>g, <strong>the</strong>re is a risk that patients will<br />
not be appropriately <strong>in</strong>vestigated. <strong>The</strong> diagnosis<br />
<strong>of</strong> <strong>heart</strong> <strong>failure</strong> may be missed, or patients diagnosed<br />
with <strong>heart</strong> <strong>failure</strong> without proper evaluation<br />
may be treated for <strong>the</strong> condition when <strong>the</strong>y<br />
are not suffer<strong>in</strong>g from it.<br />
In order to identify patients with <strong>heart</strong> <strong>failure</strong><br />
some algorithms have been used but without great<br />
success. Symptoms and electrocardiography<br />
(ECG) have been used most frequently for screen<strong>in</strong>g.<br />
Dur<strong>in</strong>g recent years biochemical markers<br />
have been evaluated for screen<strong>in</strong>g purposes, especially<br />
neurohormonal markers, as <strong>in</strong> <strong>heart</strong> <strong>failure</strong><br />
<strong>the</strong> neurohormonal system <strong>in</strong> general is activated.<br />
<strong>The</strong> ideal marker should be effective for screen<strong>in</strong>g,<br />
have a high sensitivity, have prognostic impact, be<br />
stable and simple to use and<br />
not be too expensive. More<br />
recently some very useful<br />
markers have emerged,<br />
namely <strong>the</strong> natriuretic peptides.<br />
<strong>The</strong> natriuretic peptides<br />
<strong>The</strong> natriuretic peptides<br />
have been known for<br />
decades, especially atrial<br />
natriuretic peptide (ANP)<br />
and bra<strong>in</strong> or B-type natriuretic<br />
peptide (BNP). After<br />
commercial analysis became<br />
available, <strong>in</strong>formation on <strong>the</strong><br />
use <strong>of</strong> <strong>the</strong>se markers <strong>in</strong> cl<strong>in</strong>ical<br />
practice <strong>in</strong>creased substantially.<br />
From a cl<strong>in</strong>ical<br />
po<strong>in</strong>t <strong>of</strong> view <strong>the</strong> <strong>in</strong>terest is ma<strong>in</strong>ly concentrated<br />
on BNP and its <strong>in</strong>active stable split product N-term<strong>in</strong>al<br />
pro-BNP (<strong>NT</strong>-<strong>proBNP</strong>). BNP is secreted<br />
from <strong>the</strong> left ventricular myocardium and to a<br />
lesser degree from <strong>the</strong> atria and <strong>the</strong> right ventricle,<br />
<strong>the</strong> stimulus for secretion be<strong>in</strong>g wall stress.<br />
Studies have shown that BNP and <strong>NT</strong>-<strong>proBNP</strong> are<br />
very effective prognostic markers <strong>of</strong> cardiovascular<br />
morbidity and mortality for many cardiovascular<br />
diseases <strong>in</strong> several populations [3], but currently<br />
<strong>the</strong>ir <strong>role</strong> as risk markers has not yet been<br />
established <strong>in</strong> <strong>the</strong> cl<strong>in</strong>ic. <strong>The</strong> current use <strong>of</strong> BNP<br />
and <strong>NT</strong>-<strong>proBNP</strong> is primarily concentrated on<br />
screen<strong>in</strong>g for acute and chronic <strong>heart</strong> <strong>failure</strong>.<br />
Natriuretic peptides and CHF<br />
As mentioned previously one <strong>of</strong> <strong>the</strong> ma<strong>in</strong> problems<br />
<strong>in</strong> CHF patient <strong>management</strong> is <strong>the</strong> effective screen<strong>in</strong>g<br />
<strong>of</strong> symptomatic patients prior to carry<strong>in</strong>g out fur<strong>the</strong>r<br />
diagnostic procedures. Measurement <strong>of</strong> BNP and<br />
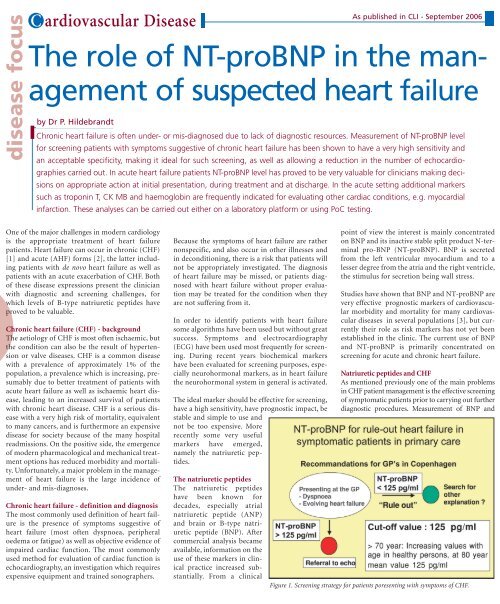
Figure 1. Screen<strong>in</strong>g strategy for patients poresent<strong>in</strong>g with symptoms <strong>of</strong> CHF.
Figure 2. Proposed use <strong>of</strong> <strong>NT</strong>-<strong>proBNP</strong> <strong>in</strong> AHF patients.<br />
<strong>NT</strong>-<strong>proBNP</strong> levels have been shown to be highly suitable<br />
for this purpose.<br />
Generally speak<strong>in</strong>g <strong>heart</strong> <strong>failure</strong> is caused by systolic<br />
<strong>failure</strong>, diastolic <strong>failure</strong>, <strong>heart</strong> valve disease and<br />
arrhythmias. <strong>The</strong> most frequent, and best evaluated<br />
cause <strong>of</strong> <strong>the</strong> condition <strong>in</strong> terms <strong>of</strong> diagnosis and<br />
treatment, is systolic <strong>failure</strong>.<br />
Several <strong>in</strong>vestigations demonstrate that systolic <strong>heart</strong><br />
<strong>failure</strong> with normal BNP / <strong>NT</strong>-<strong>proBNP</strong> level is very<br />
unusual, although it is observed <strong>in</strong> rare cases <strong>of</strong><br />
patients with CHF and reduced systolic LV function,<br />
who are asymptomatic or only slightly symptomatic<br />
when given optimal <strong>heart</strong> <strong>failure</strong> treatment.<br />
In patients with symptoms suggestive <strong>of</strong> <strong>heart</strong> <strong>failure</strong>,<br />
who are referred for echocardiography by general<br />
practitioners, an elevated BNP / <strong>NT</strong>-<strong>proBNP</strong> level<br />
below <strong>the</strong> cut-<strong>of</strong>f value <strong>of</strong> 125 pg/mL has been generally<br />
validated for rul<strong>in</strong>g-out CHF, with a sensitivity for substantial<br />
cardiac dysfunction and systolic dysfunction <strong>of</strong><br />
97 - 100% and a specificity <strong>of</strong> approximately 50% [4, 5].<br />
This very high sensitivity results <strong>in</strong> a very low risk <strong>of</strong><br />
overlook<strong>in</strong>g patients with <strong>heart</strong> <strong>failure</strong>, which is<br />
required for a good screen<strong>in</strong>g method. One essential<br />
reason for this screen<strong>in</strong>g value is <strong>the</strong> fact that BNP / <strong>NT</strong><strong>proBNP</strong><br />
levels are normal even <strong>in</strong> patients with severe<br />
pulmonary disease. It is only necessary to carry out<br />
echocardiography <strong>in</strong> patients with values above <strong>the</strong><br />
aforementioned cut-<strong>of</strong>f levels, which would be cost<br />
effective as it could result <strong>in</strong> approximately 40% less<br />
echocardiographies be<strong>in</strong>g carried out.<br />
As mentioned previously, several <strong>in</strong>vestigations have<br />
demonstrated <strong>the</strong> very high prognostic<br />
value <strong>of</strong> measur<strong>in</strong>g BNP /<br />
<strong>NT</strong>-<strong>proBNP</strong> levels <strong>in</strong> mild as well<br />
as severe <strong>heart</strong> <strong>failure</strong>. In most <strong>of</strong><br />
<strong>the</strong>se studies <strong>the</strong> prognostic value<br />
is considerably greater than with<br />
traditional risk markers for this<br />
disease, which <strong>in</strong>clude New York<br />
Heart Association Class and LV<br />
ejection fraction. <strong>The</strong> very high<br />
prognostic value <strong>of</strong> measur<strong>in</strong>g<br />
BNP / <strong>NT</strong>-<strong>proBNP</strong> levels supports<br />
<strong>the</strong> use <strong>of</strong> such screen<strong>in</strong>g, as<br />
an <strong>in</strong>creased level is highly <strong>in</strong>dicative<br />
that fur<strong>the</strong>r <strong>in</strong>vestigation is<br />
warranted, <strong>in</strong> order to f<strong>in</strong>d a<br />
potentially reversible cardiac aetiology<br />
or to <strong>in</strong>tensify <strong>the</strong> treatment<br />
be<strong>in</strong>g given. Screen<strong>in</strong>g<br />
accord<strong>in</strong>g to <strong>the</strong> scheme shown<br />
<strong>in</strong> Figure 1 is relevant for patients present<strong>in</strong>g to <strong>the</strong> GP<br />
with symptoms <strong>of</strong> CHF. Tests can be carried out <strong>in</strong><br />
ei<strong>the</strong>r <strong>the</strong> central laboratory, or at <strong>the</strong> po<strong>in</strong>t <strong>of</strong> care.<br />
Alleged errors<br />
It is important to stress that BNP / <strong>NT</strong>-<strong>proBNP</strong> levels<br />
<strong>in</strong>crease with age even <strong>in</strong> subjects without cardiac disease<br />
[6]. <strong>The</strong> reasons for this could be <strong>the</strong> age-related<br />
changes which occur <strong>in</strong> <strong>the</strong> metabolism <strong>of</strong> natriuretic<br />
peptides, age-dependent changes <strong>in</strong> <strong>the</strong> <strong>heart</strong>, or <strong>the</strong><br />
decrease <strong>in</strong> renal function which occurs with age. It is a<br />
subject <strong>of</strong> discussion whe<strong>the</strong>r <strong>the</strong> cut-<strong>of</strong>f values for<br />
screen<strong>in</strong>g symptomatic patients should be age-dependent,<br />
but until now no consensus concern<strong>in</strong>g this has<br />
been reached. BNP / <strong>NT</strong>-<strong>proBNP</strong> levels <strong>in</strong>creases with<br />
decreas<strong>in</strong>g renal function, primarily <strong>in</strong> patients with<br />
serum creat<strong>in</strong><strong>in</strong> levels above 200 mol/L. In general values<br />
are higher <strong>in</strong> females than males and lower <strong>in</strong> obese<br />
subjects, though <strong>the</strong> magnitudes <strong>of</strong> <strong>the</strong>se differences are<br />
fairly small and are <strong>of</strong> m<strong>in</strong>imal importance <strong>in</strong> cl<strong>in</strong>ical<br />
screen<strong>in</strong>g. Values are <strong>in</strong>creased <strong>in</strong> patients with left<br />
ventricular hypertrophy, atrial fibrillation, severe aortic<br />
stenosis and presumably also with milder form <strong>of</strong> aortic<br />
stenosis, as well as <strong>in</strong> patients with o<strong>the</strong>r valve diseases.<br />
BNP / <strong>NT</strong>-<strong>proBNP</strong> levels are <strong>in</strong>fluenced by medical<br />
treatment, thus ACE <strong>in</strong>hibitors, angiotens<strong>in</strong> II antagonists,<br />
spironolactone and diuretics reduce <strong>the</strong> level, while<br />
betablockers <strong>in</strong>duce a very small <strong>in</strong>crease or decrease.<br />
Natriuretic peptides <strong>in</strong> monitor<strong>in</strong>g <strong>the</strong>rapy<br />
A promis<strong>in</strong>g new application for <strong>NT</strong>-<strong>proBNP</strong> measurement<br />
<strong>in</strong> CHF could be its use <strong>in</strong> guid<strong>in</strong>g and<br />
monitor<strong>in</strong>g treatment. Several studies on this topic<br />
are ongo<strong>in</strong>g, utilis<strong>in</strong>g laboratory platforms as well as<br />
po<strong>in</strong>t <strong>of</strong> care test<strong>in</strong>g. In an ongo<strong>in</strong>g study <strong>in</strong> <strong>the</strong><br />
Danish Network <strong>of</strong> Heart Failure Cl<strong>in</strong>ics stable CHF<br />
patients are randomised for follow up by GPs, follow<br />
up by Heart Failure Cl<strong>in</strong>ics with standard care or follow<br />
up <strong>in</strong> Heart Failure Cl<strong>in</strong>ics utilis<strong>in</strong>g <strong>NT</strong>-<strong>proBNP</strong><br />
level, measured ei<strong>the</strong>r by <strong>the</strong> Elecsys platform or<br />
us<strong>in</strong>g <strong>the</strong> Roche Cardiac <strong>proBNP</strong> test.<br />
Acute <strong>heart</strong> <strong>failure</strong> (AHF)<br />
Admissions for AHF are frequent and expensive. In<br />
Denmark <strong>the</strong> annual admission rate is approximately<br />
2 per 1000 <strong>in</strong>habitants, mak<strong>in</strong>g AHF <strong>the</strong> fourth<br />
most costly disease for hospitals. A rapid and effective<br />
diagnosis, prompt and effective treatment and a<br />
reduced hospital stay are important for both improv<strong>in</strong>g<br />
<strong>the</strong> prognosis and reduc<strong>in</strong>g costs. In order to do<br />
this it is important that dyspnoea due to AHF and<br />
dyspnoea result<strong>in</strong>g from ano<strong>the</strong>r disease (usually a pulmonary<br />
disease) can be differentiated <strong>in</strong> <strong>the</strong> emergency<br />
room. This differentiation has generally been made<br />
based on cl<strong>in</strong>ical judgement, but recently measurement<br />
<strong>of</strong> <strong>NT</strong>-<strong>proBNP</strong> levels has been shown to very helpful<br />
ei<strong>the</strong>r alone or comb<strong>in</strong>ed with cl<strong>in</strong>ical judgement [7].<br />
This has been demonstrated <strong>in</strong> academic sett<strong>in</strong>gs, but<br />
its value would presumably be even greater <strong>in</strong> more<br />
rural areas, where <strong>the</strong>re are fewer tra<strong>in</strong>ed doctors <strong>in</strong><br />
emergency rooms.<br />
It has been proposed that by utilis<strong>in</strong>g <strong>NT</strong>-<strong>proBNP</strong><br />
level, patients can be divided <strong>in</strong>to three groups: one<br />
group with a high level <strong>of</strong> <strong>NT</strong>-<strong>proBNP</strong> (>450 - 1800<br />
pg/mL, dependent on age) and a very high risk for<br />
AHF, one group with a low <strong>NT</strong>-<strong>proBNP</strong> (< 300 pg/mL,<br />
age-<strong>in</strong>dependent) and very low risk for AHF, and a relatively<br />
small <strong>in</strong>termediate grey zone group. Us<strong>in</strong>g <strong>the</strong>se<br />
values results <strong>in</strong> a high sensitivity <strong>of</strong> 90 - 95% while still<br />
reta<strong>in</strong><strong>in</strong>g a good specificity <strong>of</strong> 60% [7], <strong>the</strong> sensitivity<br />
be<strong>in</strong>g highest <strong>in</strong> younger subjects.<br />
<strong>The</strong> Basel study [8] demonstrated that BNP guided<br />
<strong>management</strong> <strong>of</strong> AHF resulted <strong>in</strong> significantly shorter<br />
<strong>in</strong>-patient hospital stays, and lower costs <strong>of</strong> approximately<br />
80% <strong>of</strong> usual patient <strong>management</strong> costs.<br />
A proposal for <strong>the</strong> use <strong>of</strong> <strong>NT</strong>-<strong>proBNP</strong> level <strong>in</strong> AHF<br />
patient <strong>management</strong> [based on 7] is shown <strong>in</strong> Figure 2.<br />
It is <strong>of</strong> importance that <strong>the</strong> cut-<strong>of</strong>f values for <strong>NT</strong><strong>proBNP</strong><br />
level are <strong>in</strong> general three times higher than <strong>the</strong><br />
cut-<strong>of</strong>f values for patients with chronic <strong>heart</strong> <strong>failure</strong>. If<br />
<strong>NT</strong>-<strong>proBNP</strong> level is used for this purpose, tested ei<strong>the</strong>r<br />
<strong>in</strong> <strong>the</strong> central lab or <strong>in</strong> a PoC sett<strong>in</strong>g, results should be<br />
rapidly available to allow a quick decision on <strong>the</strong> need<br />
for admission and treatment, and to optimise patient<br />
<strong>management</strong> for maximum benefit.
Central analysis or Po<strong>in</strong>t-<strong>of</strong>-Care (PoC) test<strong>in</strong>g<br />
<strong>NT</strong>-<strong>proBNP</strong> measurement can be carried out ei<strong>the</strong>r on<br />
laboratory platform or us<strong>in</strong>g PoC test<strong>in</strong>g, accord<strong>in</strong>g to<br />
<strong>the</strong> local logistics. <strong>The</strong> recently developed Roche<br />
Cardiac <strong>proBNP</strong> shows excellent correlation with <strong>the</strong><br />
laboratory method.<br />
One potential draw-back for PoC test<strong>in</strong>g could be <strong>the</strong><br />
measur<strong>in</strong>g range <strong>of</strong> up to 3000 pg/mL only. However<br />
when used as a screen<strong>in</strong>g test for CHF this is <strong>of</strong> no<br />
importance, as patients with values above 125 pg/mL<br />
(or perhaps somewhat higher <strong>in</strong> older patients) should<br />
undergo additional cardiac evaluation. <strong>The</strong> use <strong>of</strong><br />
ei<strong>the</strong>r a laboratory platform or PoC test<strong>in</strong>g should primarily<br />
depend on local tradition and logistics, e.g. it<br />
could be time-sav<strong>in</strong>g for <strong>the</strong> patient to have <strong>the</strong> PoC<br />
test <strong>in</strong> <strong>the</strong> GP’s or <strong>the</strong> specialist’s facility.<br />
Us<strong>in</strong>g a laboratory platform or PoC test<strong>in</strong>g <strong>in</strong> <strong>the</strong> acute<br />
sett<strong>in</strong>g has advantages and disadvantages, <strong>the</strong> primary<br />
advantage <strong>of</strong> PoC test<strong>in</strong>g be<strong>in</strong>g <strong>the</strong> speed <strong>of</strong> analysis,<br />
allow<strong>in</strong>g <strong>the</strong> result to be available rapidly enough for<br />
acute decisions to be made. If <strong>the</strong> result from <strong>the</strong> central<br />
laboratory is quickly available this is equally satisfactory.<br />
<strong>The</strong> measurement upper limit <strong>of</strong> only 3000 pg/mL is not<br />
a problem <strong>in</strong> acute evaluation <strong>of</strong> <strong>the</strong> patient. In fur<strong>the</strong>r<br />
patient work-up, especially if <strong>NT</strong>-<strong>proBNP</strong> guided follow<br />
up is warranted, <strong>the</strong> upper cut-<strong>of</strong>f limit could be a problem<br />
and <strong>the</strong> use <strong>of</strong> a laboratory platform could be<br />
necessary.<br />
Conclusions<br />
Sufficient evidence exists from measurement <strong>of</strong><br />
<strong>NT</strong>-<strong>proBNP</strong> level <strong>in</strong> patients with <strong>suspected</strong> <strong>heart</strong><br />
<strong>failure</strong> to support <strong>the</strong> implementation <strong>of</strong> this<br />
screen<strong>in</strong>g test <strong>in</strong> patients with symptoms suggestive<br />
<strong>of</strong> chronic <strong>heart</strong> <strong>failure</strong>. Fur<strong>the</strong>r diagnostic tests<br />
such as echocardiography only need to be performed<br />
<strong>in</strong> patients with elevated levels <strong>of</strong> <strong>NT</strong><strong>proBNP</strong>.<br />
In patients with acute dyspnoea, <strong>the</strong>re is<br />
substantial evidence support<strong>in</strong>g <strong>the</strong> use <strong>of</strong> <strong>NT</strong><strong>proBNP</strong><br />
level to aid <strong>in</strong> decisions on treatment, hospitalisation<br />
and discharge. <strong>NT</strong>-<strong>proBNP</strong> level can be<br />
measured ei<strong>the</strong>r <strong>in</strong> a centralised lab or po<strong>in</strong>t <strong>of</strong> care<br />
sett<strong>in</strong>g, accord<strong>in</strong>g to local practice and convenience.<br />
References<br />
1. <strong>The</strong> Task Force on Chronic Heart Failure <strong>of</strong> <strong>the</strong><br />
European Society <strong>of</strong> Cardiology. Executive summary <strong>of</strong><br />
<strong>the</strong> Guidel<strong>in</strong>es on <strong>the</strong> diagnosis and treatment <strong>of</strong> Chronic<br />
Heart Failure. Eur Heart J 2005; 26: 1115-40.<br />
2. <strong>The</strong> Task Force on Acute Heart Failure <strong>of</strong> <strong>the</strong> European<br />
Society <strong>of</strong> Cardiology. Executive summary <strong>of</strong> <strong>the</strong><br />
Guidel<strong>in</strong>es on <strong>the</strong> diagnosis and treatment <strong>of</strong> Acute Heart<br />
Failure. Eur Heart J 2005; 26: 384-416.<br />
3. Kistorp C, Raymond I, Pedersen F et al. N-term<strong>in</strong>al probra<strong>in</strong><br />
natriuretic peptide, C-reactive prote<strong>in</strong> an ur<strong>in</strong>ary<br />
album<strong>in</strong> levels as predictor <strong>of</strong> mortality and cardiovascular<br />
events <strong>in</strong> older adults. JAMA 2005; 293: 1609-16.<br />
4. Gustafsson F, Steensgaard-Hansen F, Badskjaer J,<br />
Poulsen AH, Corell P, Hildebrandt P. Diagnostic and prognostic<br />
performance <strong>of</strong> N-term<strong>in</strong>al <strong>proBNP</strong> <strong>in</strong> primary<br />
care patients with <strong>suspected</strong> <strong>heart</strong> <strong>failure</strong>. J Card Fail 2005;<br />
11(5 suppl): S15-20.<br />
5. Zaphiriou A, Robb S, Murray-Thomas T, Mendez G,<br />
Fox, McDonagh T, Hardman SM, Dargie HJ, Cowie MR.<br />
<strong>The</strong> diagnostic accuracy <strong>of</strong> plasma BNP and <strong>NT</strong>-<strong>proBNP</strong><br />
<strong>in</strong> patients reffered from primary care with <strong>suspected</strong><br />
<strong>heart</strong> <strong>failure</strong>: results <strong>of</strong> <strong>the</strong> UK natriuretic peptide study.<br />
Eur J Heart Fail 2005; 7: 537-41.<br />
6. Raymond I, Groenn<strong>in</strong>g BA, Hildebrandt P, Nilsson JC,<br />
Bauman M, Traw<strong>in</strong>ski J, Pedersen F. <strong>The</strong> <strong>in</strong>fluence <strong>of</strong> age,<br />
sex and o<strong>the</strong>r variables on <strong>the</strong> plasma level <strong>of</strong> N-term<strong>in</strong>al<br />
pro bra<strong>in</strong> natriuretic peptide <strong>in</strong> a large sample <strong>of</strong> <strong>the</strong> general<br />
population. Heart 2003; 89: 745-51.<br />
7. Januzzi JL, Jr, Camargo CA, Anwarudd<strong>in</strong> S, Baggish AL,<br />
Chen AA, Krauser DG, Tung R, Cameron R, Nagurney JT,<br />
Chae CU, Lloyd-Jones DM, Brown DF, Foran-Melanson S,<br />
Sluss PM, Lee-Lewandrowski E, Lewandrowski KB. <strong>The</strong> N-<br />
term<strong>in</strong>al pro-BNP <strong>in</strong>vestigation <strong>of</strong> dyspnea <strong>in</strong> <strong>the</strong> emergency<br />
department (PRIDE) study. Am J Cardiol 2005; 95:<br />
948-54.<br />
8. Mueller C, Scholer A, Laule-ilian K, Mart<strong>in</strong>a B,<br />
Sch<strong>in</strong>dler C, Buser P, Pfisterer M, Perruchoud A. Use <strong>of</strong> B-<br />
type natriuretic peptide <strong>in</strong> <strong>the</strong> evaluation and <strong>management</strong><br />
<strong>of</strong> acute dyspnea. NEJM 2004; 350: 647-54.<br />
<strong>The</strong> author<br />
Per Hildebrandt, DMSci,<br />
Assistant pr<strong>of</strong>essor,<br />
Director <strong>of</strong> <strong>in</strong>ternal medic<strong>in</strong>e and cardiology services,<br />
Roskilde University hospital,<br />
Kogevej 7 - 13,<br />
DK-4000 Roskilde,<br />
Denmark.<br />
e-mail: rspehi@ra.dk