Pectoralis major flap - Vula - University of Cape Town
Pectoralis major flap - Vula - University of Cape Town
Pectoralis major flap - Vula - University of Cape Town
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
OPEN ACCESS ATLAS OF OTOLARYNGOLOGY, HEAD &<br />
NECK OPERATIVE SURGERY<br />
THE PECTORALIS MAJOR FLAP<br />
The pectoralis <strong>major</strong> <strong>flap</strong> comprises the<br />
pectoralis <strong>major</strong> muscle, with or without<br />
overlying skin, and may include the underlying<br />
ribs. It has an axial blood supply, and<br />
is based superiorly on the pectoral branch<br />
<strong>of</strong> the thoracoacromial artery.<br />
Johan Fagan<br />
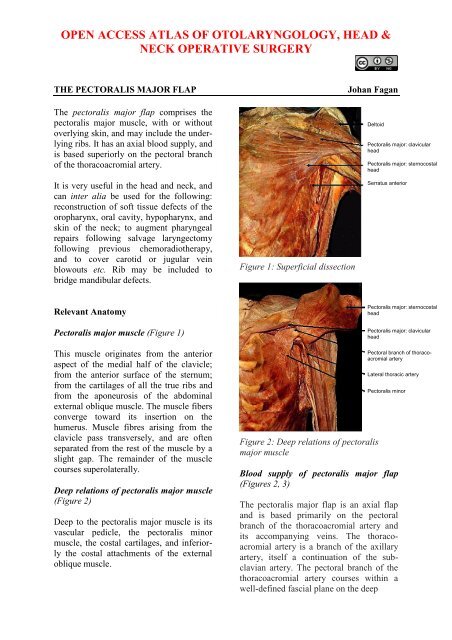
Deltoid<br />
<strong>Pectoralis</strong> <strong>major</strong>: clavicular<br />
head<br />
<strong>Pectoralis</strong> <strong>major</strong>: sternocostal<br />
head<br />
It is very useful in the head and neck, and<br />
can inter alia be used for the following:<br />
reconstruction <strong>of</strong> s<strong>of</strong>t tissue defects <strong>of</strong> the<br />
oropharynx, oral cavity, hypopharynx, and<br />
skin <strong>of</strong> the neck; to augment pharyngeal<br />
repairs following salvage laryngectomy<br />
following previous chemoradiotherapy,<br />
and to cover carotid or jugular vein<br />
blowouts etc. Rib may be included to<br />
bridge mandibular defects.<br />
Figure 1: Superficial dissection<br />
Serratus anterior<br />
Relevant Anatomy<br />
<strong>Pectoralis</strong> <strong>major</strong> muscle (Figure 1)<br />
<strong>Pectoralis</strong> <strong>major</strong>: sternocostal<br />
head<br />
<strong>Pectoralis</strong> <strong>major</strong>: clavicular<br />
head<br />
This muscle originates from the anterior<br />
aspect <strong>of</strong> the medial half <strong>of</strong> the clavicle;<br />
from the anterior surface <strong>of</strong> the sternum;<br />
from the cartilages <strong>of</strong> all the true ribs and<br />
from the aponeurosis <strong>of</strong> the abdominal<br />
external oblique muscle. The muscle fibers<br />
converge toward its insertion on the<br />
humerus. Muscle fibres arising from the<br />
clavicle pass transversely, and are <strong>of</strong>ten<br />
separated from the rest <strong>of</strong> the muscle by a<br />
slight gap. The remainder <strong>of</strong> the muscle<br />
courses superolaterally.<br />
Deep relations <strong>of</strong> pectoralis <strong>major</strong> muscle<br />
(Figure 2)<br />
Deep to the pectoralis <strong>major</strong> muscle is its<br />
vascular pedicle, the pectoralis minor<br />
muscle, the costal cartilages, and inferiorly<br />
the costal attachments <strong>of</strong> the external<br />
oblique muscle.<br />
Figure 2: Deep relations <strong>of</strong> pectoralis<br />
<strong>major</strong> muscle<br />
Blood supply <strong>of</strong> pectoralis <strong>major</strong> <strong>flap</strong><br />
(Figures 2, 3)<br />
Pectoral branch <strong>of</strong> thoracoacromial<br />
artery<br />
Lateral thoracic artery<br />
<strong>Pectoralis</strong> minor<br />
The pectoralis <strong>major</strong> <strong>flap</strong> is an axial <strong>flap</strong><br />
and is based primarily on the pectoral<br />
branch <strong>of</strong> the thoracoacromial artery and<br />
its accompanying veins. The thoracoacromial<br />
artery is a branch <strong>of</strong> the axillary<br />
artery, itself a continuation <strong>of</strong> the subclavian<br />
artery. The pectoral branch <strong>of</strong> the<br />
thoracoacromial artery courses within a<br />
well-defined fascial plane on the deep
Thoracoacromial a<br />
denervated muscle loses bulk with time<br />
which might be advantageous or disadvantageous,<br />
depending on the functional<br />
and cosmetic objectives <strong>of</strong> the <strong>flap</strong>.<br />
Pectoral branch<br />
<strong>Pectoralis</strong> <strong>major</strong><br />
<strong>Pectoralis</strong> minor<br />
Figure 3: Blood supply <strong>of</strong> pectoralis <strong>major</strong><br />
<strong>flap</strong><br />
surface <strong>of</strong> the pectoralis <strong>major</strong> muscle<br />
(Figures 2, 9). There is a clear dissection<br />
plane between this fascial layer and the<br />
superficial aspect <strong>of</strong> the pectoralis minor<br />
muscle making it possible to strip the<br />
pectoralis <strong>major</strong> and its blood supply <strong>of</strong>f<br />
the pectoralis minor with blunt finger<br />
dissection. Additional blood supply arises<br />
medially from the internal mammary<br />
artery, and laterally from the long thoracic<br />
artery, branches <strong>of</strong> which are generally<br />
sacrificed during elevation <strong>of</strong> the <strong>flap</strong> to<br />
secure adequate pedicle length. Care has to<br />
be taken should the skin island be located<br />
distally in the region <strong>of</strong> the costal margin<br />
at, or beyond, the lower extent <strong>of</strong> the<br />
pectoralis <strong>major</strong> muscle, as the blood<br />
supply then becomes random as opposed to<br />
axial, making perfusion <strong>of</strong> the <strong>flap</strong> less<br />
reliable.<br />
Flap design<br />
The <strong>flap</strong> may be employed either as a<br />
muscular or musculocutaneous <strong>flap</strong>, with<br />
or without the 4 th or 5 th ribs. The following<br />
discussion will focus on raising a<br />
musculocutaneous island <strong>flap</strong>.<br />
Positioning, prepping and draping<br />
The patient is placed in a supine position<br />
with the chest exposed and prepped up to<br />
the midline, and inferiorly to the costal<br />
margin. The upper arm is abducted slightly<br />
to expose the anterior axillary fold and<br />
lateral chest wall.<br />
Surface markings <strong>of</strong> vascular pedicle<br />
The surface markings <strong>of</strong> the vascular<br />
pedicle are determined by drawing a line<br />
from the shoulder to the xiphisternum and<br />
another line vertically from the midpoint <strong>of</strong><br />
the clavicle to intersect the 1 st line (Figure<br />
4).<br />
Innervation<br />
The pectoralis <strong>major</strong> is innervated by the<br />
lateral pectoral nerve which can be located<br />
just inferior to the clavicle with the<br />
pectoral branch <strong>of</strong> the thoracoacromial<br />
artery. The medial pectoral nerve passes<br />
through the pectoralis minor muscle and<br />
sends 2 to 3 branches to the pectoralis<br />
<strong>major</strong>. All these nerves are normally<br />
divided during elevation <strong>of</strong> the <strong>flap</strong>. The<br />
Figure 4: Surface markings <strong>of</strong> pectoral<br />
branch <strong>of</strong> thoracoacromial artery<br />
2
Skin paddle design<br />
The skin paddle is positioned over the<br />
pectoralis <strong>major</strong> muscle along the course<br />
<strong>of</strong> the pectoral branch <strong>of</strong> the thoracoacromial<br />
artery (Figures 4, 5, 6). In order<br />
to ensure that the pedicle is <strong>of</strong> adequate<br />
length, the distance between the top <strong>of</strong> the<br />
skin paddle and the inferior edge <strong>of</strong> the<br />
clavicle should equal or exceed the<br />
distance between the recipient site for the<br />
<strong>flap</strong> and the inferior edge <strong>of</strong> the clavicle. In<br />
women the paddle may be placed in the<br />
inframammary crease to include skin on<br />
either side <strong>of</strong> the crease, so as to avoid<br />
excessive bulk from breast tissue and for<br />
cosmetic reasons (Figure 5).<br />
surface <strong>of</strong> the pectoralis <strong>major</strong> muscle. As<br />
the vascular pedicle is located deep to the<br />
muscle, this may be quickly and safely<br />
performed using the bovie / monopolar<br />
diathermy. Care has to be exercised not to<br />
undercut the skin paddle, but rather to<br />
bevel the dissection radially so as to<br />
include as many myocutaneous perforators<br />
as possible that supply the skin paddle<br />
(Figure 6). The skin paddle is tacked to the<br />
underlying pectoralis <strong>major</strong> muscle with a<br />
few sutures so as to minimise the risk <strong>of</strong><br />
shearing injury to the myocutaneous perforators<br />
(Figure 7).<br />
Figure 5: Inframammary skin paddle<br />
Should additional pedicle length be<br />
required, the <strong>flap</strong> may be extended up to<br />
2.5cms beyond the pectoralis <strong>major</strong> muscle<br />
inferiorly at the costal margin, with the<br />
knowledge that the <strong>flap</strong> then becomes a<br />
random pattern <strong>flap</strong> and the blood supply<br />
more tenuous.<br />
Elevation <strong>of</strong> skin paddle<br />
The skin is incised around the skin paddle,<br />
and the dissection is extended onto the<br />
Figure 6: Dissection <strong>of</strong> skin paddle onto<br />
pectoralis <strong>major</strong> muscle, and incision<br />
along anterior axillary fold<br />
Exposure <strong>of</strong> pectoralis <strong>major</strong> muscle<br />
An incision is extended laterally from the<br />
peripheral margin <strong>of</strong> the skin paddle along<br />
the anterior axillary fold, which corresponds<br />
with the lateral margin <strong>of</strong> the pectoralis<br />
<strong>major</strong> muscle (Figure 6). The skin<br />
and breast tissue above the skin paddle is<br />
then widely elevated from the pectoralis<br />
<strong>major</strong> muscle with diathermy up to the<br />
clavicle (Figure 7).<br />
3
surface <strong>of</strong> the pectoralis <strong>major</strong> muscle<br />
(Figure 9).<br />
Figure 7: Exposure <strong>of</strong> pectoralis <strong>major</strong><br />
muscle pedicle<br />
Elevation <strong>of</strong> pedicle<br />
The pectoralis <strong>major</strong> muscle is incised with<br />
cautery medially and inferiorly to the skin<br />
paddle, and is dissected from the ribs and<br />
intercostal muscles. The muscle is not<br />
divided superior to the skin paddle, as this<br />
might divide the vascular pedicle.<br />
Figure 8: Elevating pectoralis <strong>major</strong> from<br />
pectoralis minor along lateral margin <strong>of</strong><br />
muscle<br />
The pectoralis <strong>major</strong> muscle is then freed<br />
alongside the sternum with cautery. During<br />
this dissection perforators from the internal<br />
mammary artery are transected and<br />
cauterized.<br />
The dissection plane between the pectoralis<br />
minor and <strong>major</strong> muscles and the<br />
vascular pedicle is found by dissecting<br />
along the lateral border <strong>of</strong> the pectoralis<br />
<strong>major</strong> muscle with electrocautery (Figure<br />
8). Once this intermuscular plane has been<br />
identified, one can readily free the pectoralis<br />
<strong>major</strong> and its vascular pedicle from the<br />
pectoralis minor by stripping with a finger<br />
towards the clavicle (Figure 8). This<br />
brings the vascular pedicle (pectoral<br />
branch <strong>of</strong> thoracoacromial artery) clearly<br />
into view within the fascia on the deep<br />
Figure 9: Vascular pedicle visible on deep<br />
aspect <strong>of</strong> pectoralis <strong>major</strong> muscle<br />
The pedicle is kept in view and protected<br />
from injury while the branches from the<br />
lateral thoracic artery, and the branches <strong>of</strong><br />
4
the medial pectoral nerve that traverse the<br />
pectoralis minor and enter the deep surface<br />
<strong>of</strong> the <strong>flap</strong>, are divided. The pectoralis<br />
<strong>major</strong> muscle is divided lateral to the<br />
pedicle while keeping the pedicle in view,<br />
thereby freeing it from the humerus.<br />
Skin tunnel over clavicle<br />
The <strong>flap</strong> is generally passed into the neck<br />
superficial to the clavicle through a wide<br />
subcutaneous tunnel (Figure 10). The<br />
tunnel should be large enough to permit<br />
easy delivery <strong>of</strong> the <strong>flap</strong> into the neck<br />
without shearing the musculocutaneous<br />
perforators supplying the skin paddle, and<br />
to avoid strangulating the vascular pedicle.<br />
Dividing the subdermal connective tissue<br />
fibers <strong>of</strong> the skin above the skin tunnel<br />
with an upturned scalpel is a helpful<br />
adjunct to gain additional space.<br />
Figure 11: Check that pedicle is not twisted<br />
<strong>major</strong> muscle just below the clavicle,<br />
taking great care to preserve the vascular<br />
pedicle (Figure 12). An infraclavicular<br />
segment <strong>of</strong> muscle may also be excised.<br />
This has the benefit that the pedicle is<br />
directly applied to the clavicle, without<br />
intervening muscle. It has the added bonus<br />
<strong>of</strong> avoiding an unsightly, bulky pedicle<br />
over the clavicle. The 2 nd maneuver to gain<br />
additional length is to pass the <strong>flap</strong> behind<br />
the clavicle.<br />
Figure 10: Flap is passed over the clavicle<br />
though a wide skin tunnel<br />
After passing the <strong>flap</strong> into the neck, check<br />
that the pedicle is not twisted (Figure 11).<br />
Gaining additional length<br />
In the event that the pedicle is too short,<br />
two manoeuvres may add additional<br />
length. The 1 st is to transect the pectoralis<br />
Figure 12: Vascular pedicle visible<br />
following division <strong>of</strong> muscular pedicle.<br />
Closure <strong>of</strong> donor site defect<br />
The donor site is either closed primarily<br />
with a closed suction drain, or a split skin<br />
5
graft is applied. Primary closure may be<br />
facilitated by undermining the surrounding<br />
skin.<br />
pectoralis <strong>major</strong> <strong>flap</strong> interposed between<br />
oropharynx and gastric pull-up that was<br />
too short to reach oropharynx<br />
Some Clinical examples<br />
Figure 13: Reconstruction following total<br />
glossectomy<br />
Figure 16: Reconstruction <strong>of</strong> (a) pharyngocutaneous<br />
fistula with (b) pectoralis<br />
<strong>major</strong> muscle <strong>flap</strong> and (c) split skin graft<br />
and (d) final result<br />
Figure 14: Augmentation <strong>of</strong> pharynx with<br />
pectoralis <strong>major</strong> myocutaneous <strong>flap</strong> following<br />
total laryngectomy with partial<br />
pharyngectomy<br />
Figure 17: Reconstruction following segmental<br />
mandibulectomy and resection <strong>of</strong><br />
tonsil, s<strong>of</strong>t palate, and base <strong>of</strong> tongue<br />
Video <strong>of</strong> pectoralis <strong>major</strong> <strong>flap</strong> (<strong>University</strong> <strong>of</strong><br />
Iowa, USA)<br />
Author & Editor<br />
Figure 15: Laryngopharyngoesophagectomy<br />
defect reconstructed with tubed<br />
Johan Fagan MBChB, FCORL, MMed<br />
Pr<strong>of</strong>essor and Chairman<br />
Division <strong>of</strong> Otolaryngology<br />
<strong>University</strong> <strong>of</strong> <strong>Cape</strong> <strong>Town</strong><br />
<strong>Cape</strong> <strong>Town</strong>, South Africa<br />
johannes.fagan@uct.ac.za<br />
6
THE OPEN ACCESS ATLAS OF<br />
OTOLARYNGOLOGY, HEAD &<br />
NECK OPERATIVE SURGERY<br />
www.entdev.uct.ac.za<br />
The Open Access Atlas <strong>of</strong> Otolaryngology, Head & Neck<br />
Operative Surgery by Johan Fagan (Editor)<br />
johannes.fagan@uct.ac.za is licensed under a Creative<br />
Commons Attribution - Non-Commercial 3.0 Unported License<br />
7