Laryngocoele, laryngocele - Vula - University of Cape Town
Laryngocoele, laryngocele - Vula - University of Cape Town
Laryngocoele, laryngocele - Vula - University of Cape Town
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
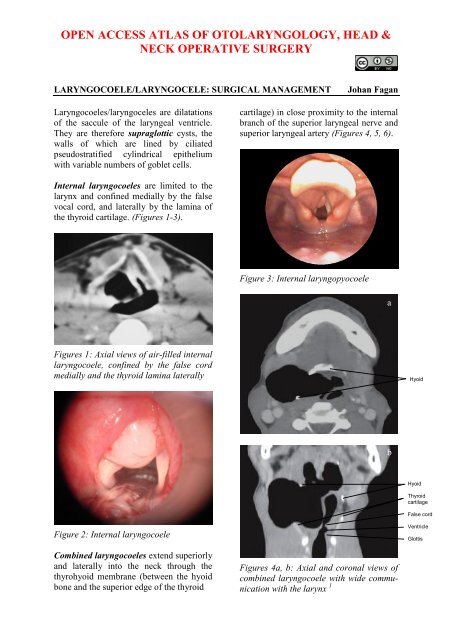
abHyoidExternalsacInternalsacEpiglottisInternaljugularCarotidarteryAlthough not an uncommon incidentalpostmortem finding, laryngocoeles aregenerally asymptomatic. Patients may presentwith voice change or a lateral swellingin the neck overlying the thyrohyoidmembrane which may visibly distendwhen increasing intraluminal pressure e.g.glass blowers and trumpet or reed instrumentplayers (Figures 7a, b).aHyoidExternal sacInternal sacThyroidcartilageFigures 5 a, b: Fluid-filled combinedlaryngocoele<strong>Laryngocoele</strong>s are filled with air whenthey retain a communication with thelaryngeal lumen (Figures 1, 4); when theybecome isolated from the laryngeal lumenthey become fluid-filled (Figures 3, 5) orinfected (laryngopyocoele) (Figure 6).bFigure 7a, b: Visible laryngocoelesFigure 6: Laryngopyocoele causingairway obstructionPatients, especially those with laryngopyocoeles,may present with acute airwayobstruction (Figure 6, 8). Occasionally alaryngocoele may be the presenting symptom<strong>of</strong> laryngeal malignancy obstructingthe saccule.2
The superior laryngeal nerve is at risk <strong>of</strong>injury when resecting a laryngocoele dueto its intimate relationship to the externalcomponent <strong>of</strong> the cyst. It arises from theganglion nodosum <strong>of</strong> the vagus nerve,descends alongside the pharynx, passesbehind the internal carotid artery, and dividesinto external and internal branches.The internal branch crosses the thyrohyoidmembrane and pierces it, accompanied bythe superior laryngeal artery, and providessensory innervation to the larynx (Figure11).The superior laryngeal artery is encounteredduring surgery and can either bepreserved or sacrificed. It is a branch <strong>of</strong> thesuperior thyroid artery (Figure 12).Figure 12: The superior laryngeal arterybranches <strong>of</strong>f the superior thyroid arteryThe muscles encountered during resection<strong>of</strong> the external component <strong>of</strong> a laryngocoeleare illustrated in Figure 13. Thethyrohyoid muscle is draped over the cystand may have to be divided; the omohyoidcan be retracted anteriorly or divided; andthe sternomastoid retracted posteriorly.ImagingSuperior laryngealarteryThe differential diagnosis <strong>of</strong> a combinedlaryngocoele includes a branchial cyst,neck abscess, cold abscess (tuberculosis),Figure 13: The thyrohyoid, omohyoid andsternomastoid muscles surround theexternal component <strong>of</strong> the laryngocoele(thyrohyoid membrane in green)lymphoadenopathy, and a laterally-locatedthyroglossal duct cyst. An internal laryngocoelecan be confused with a carcinomacentered deep in the ventricle which bulgesthe ventricular fold upwards and medially,and other unusual non-ulcerating massessuch as intralaryngeal plasmacytoma, lymphomaand minor salivary gland malignancy.CT scan will however distinguish betweenair- and fluid-filled cysts and solid masses.CT evidence <strong>of</strong> a cyst extending throughthe thyrohyoid membrane is pathognomonic<strong>of</strong> a combined laryngocoele. MRIyields similar information.ManagementThis depends on the significance <strong>of</strong> thesymptoms and signs, and the size andextent <strong>of</strong> the laryngocoele. Laryngoscopyis done to exclude the possibility <strong>of</strong> underlyingmalignancy in the larynx.Needle aspirationAn acutely inflamed combined cyst mayfirst be aspirated percutaneously with aneedle and treated with appropriate anti-4
iotics to avoid doing a suboptimal resectionin a septic field; needle aspiration mayalso be employed as an emergency measureto relieve acute airway obstruction.Internal <strong>Laryngocoele</strong>s (Figures 1-3)Small, asymptomatic laryngocoeles do notrequire surgical intervention. Symptomaticinternal laryngocoeles and saccular cystsare widely dero<strong>of</strong>ed/uncapped or excisedendoscopically, ideally with CO 2 laser.Larger internal laryngocoeles, especially ifrecurrent, can also be excised by anexternal approach (see below).Combined <strong>Laryngocoele</strong>sThe surgery is done under general anaesthesiawith endotracheal intubationtaking care not to rupture the cystPlace a transverse skin incision in askin crease over the thyrohyoid membrane,from the anterior border <strong>of</strong> thesternocleidomastoid to the midline <strong>of</strong>the neck (Figure 14)Figure 15: Expose cyst and define thesurrounding structuresUsing careful sharp and blunt dissecttion,find the dissection plane on thethin cyst wall and identify the superiorthyroid (STA) and superior laryngealarteries (SLA) behind the cyst (Figure16)SubmandibularglandCystOmohyoidSuperiorthyroid artery(STA)Superiorlaryngealartery (SLA)Superiorthyroid artery(STA)Figure 14: Skin incision over the cystbetween hyoid bone and thyroid cartilageElevate subplatysmal flaps to exposesubmandibular salivary gland superiorly,omohyoid muscle anteriorly andsternocleidomastoid muscle posteriorlyFigure 16: Expose superior thyroidand superior laryngeal arteriesIdentify the superior laryngeal nerve(SLN); it emerges deep to the superiorthyroid artery (Figure 17)Reflect the cyst upwards, and retractthe omohyoid and thinly stretchedthyrohyoid muscles anteriorly to exposethyroid lamina. If necessary, transectthe thyrohyoid muscle that overliesthe cyst for additional exposure(Figure 18)5
SLNSLASTAAdminister 24hrs’ perioperative antibioticsshould mucosa be breachedInsert a suction/pencil/corrugated drainand close the woundBecause mucosal defects would besupraglottic, postoperative surgical emphysemaand airway obstruction areunusualInternal cystNeckFigure 17: Identify the superior laryngealnerve (SLN) where it emergesdeep to the superior thyroid arteryExternal cystSLASLNSTAThyroidFigure 19: Free cyst from the superiorlaryngeal artery (SLA), superior laryngealnerve (SLN) and deliver it fromparaglottic spaceThyrohyoidOmohyoidFigure 18: Retract omohyoid andthyrohyoid muscles to expose top edge<strong>of</strong> thyroid cartilageSLNSLASTAFree the cyst from the perichondriumon the medial aspect <strong>of</strong> the thyroidlamina, and deliver it from the paraglotticspace. Carefully peel the cyst<strong>of</strong>f the internal branch <strong>of</strong> the superiorlaryngeal nerve and from the mucosaoverlying the medial aspect <strong>of</strong> the aryepiglotticfold, and deliver the cyst(Figures 19, 20)Inspect the wound for tears or breachesin the mucosa which, if present, arerepaired with absorbable suturesFigure 20: Final view <strong>of</strong> key structuresTo gain additional exposure to the internalcomponent <strong>of</strong> the cyst in the paraglotticspaceIncise the thyroid perichondrium alongthe superior and posterior margins <strong>of</strong>the thyroid lamina (Figure 21)6
Reflect the perichondrium from thelateral aspect <strong>of</strong> the thyroid laminawith a Freer dissectorRemember that the vocal cord issituated midway between the thyroidnotch and the lower edge to the thyroidcartilage; therefore make the horizontalcartilage cut above this pointCut through the cartilage with aknife/oscillating saw, taking care not toenter the larynx (Figure 21)Remove and discard the posterosuperiorquadrant <strong>of</strong> the thyroid lamina togain access to the internal component<strong>of</strong> the laryngocoele (Figure 22)Following removal <strong>of</strong> the cyst, suturethe perichondrial flap back to itsoriginal positionFigure 21: Cuts (yellow line) in thyroidcartilage to remove posterosuperior quadrant<strong>of</strong> thyroid cartilage (green)References1. Pinho M da C, et al. External <strong>laryngocele</strong>:sonographic appearance - a casereport. Radiol Bras. 2007 Aug[cited 2013 Mar 09]; 40(4):279-82http://dx.doi.org/10.1590/S0100-398420070004000152. de Paula Felix JA, Felix F, de MelloLFP. Laryngocele: a cause <strong>of</strong> upperairway obstruction. Rev. Bras. Otorrinolaringol.2008 Feb [cited 2013Mar 09]; 74(1): 143-6.http://dx.doi.org/10.1590/S0034-72992008000100023Author & EditorJohan Fagan MBChB, FCORL, MMedPr<strong>of</strong>essor and ChairmanDivision <strong>of</strong> Otolaryngology, <strong>University</strong> <strong>of</strong><strong>Cape</strong> <strong>Town</strong><strong>Cape</strong> <strong>Town</strong>South Africajohannes.fagan@uct.ac.zaFigure 22: Note how removal <strong>of</strong> thyroidlamina improves access to internal component<strong>of</strong> laryngocoeleTHE OPEN ACCESS ATLAS OFOTOLARYNGOLOGY, HEAD & NECKOPERATIVE SURGERYwww.entdev.uct.ac.zaThe Open Access Atlas <strong>of</strong> Otolaryngology, Head & NeckOperative Surgery by Johan Fagan (Editor)johannes.fagan@uct.ac.za is licensed under a CreativeCommons Attribution - Non-Commercial 3.0 Unported License7