Jarvie Journal - College of Dental Medicine - Columbia University
Jarvie Journal - College of Dental Medicine - Columbia University
Jarvie Journal - College of Dental Medicine - Columbia University
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
Volume 56, Spring 2013<br />
Evaluation <strong>of</strong> Fracture Resistance <strong>of</strong> Cement-Retained Zirconium and<br />
Lithium Disilicate Implant Abutments.<br />
Fotini N. Chrisopoulos 1 , Techkouhie Hamalian 1 , Thomas Hill 2 ,<br />
Anthony Randi 1<br />
1 Postgraduate Prosthodontics, <strong>College</strong> <strong>of</strong> <strong>Dental</strong> <strong>Medicine</strong>, <strong>Columbia</strong> <strong>University</strong>, N.Y.<br />
2 Manager <strong>of</strong> Scientific Services, Research and Development, Ivoclar Vivadent<br />
Introduction: Various ceramic abutment systems with different implant- abutment connection<br />
designs are available and present different modulus <strong>of</strong> elasticity and fracture resistance. Zirconia<br />
implant abutments exhibit excellent fracture resistance due to transformation toughening.<br />
However, some <strong>of</strong> their limitations are the mechanism <strong>of</strong> crack propagation and the fact that<br />
zirconia is a non- silica based ceramic with controversial cementation protocols. Lithium<br />
disilicate glass ceramic provides the option <strong>of</strong> either conventional cementation or an adhesive<br />
bonding protocol. Therefore, this material has the potential to be used for definitive implant<br />
restoration and can create a strong bond at the abutment- crown interface.<br />
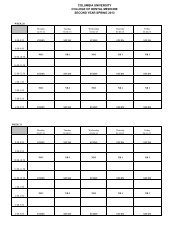
Objective and Methods: The in-vitro single-load study evaluates the fracture resistance <strong>of</strong><br />
zirconia and lithium disilicate implant abutments using titanium metallic inserts. Metallic<br />
inserts were either retained by clamping or cementing into the ceramic abutments according to<br />
the manufacturer’s guidelines.<br />
Discussion: In the literature, use <strong>of</strong> cementable abutments can provide resistance to rotational<br />
forces that may cause screw loosening. Moreover, the luting agent interface between metal<br />
surfaces will allow small discrepancies not acceptable in a screw maintained fixture and may<br />
even act as a shock absorber. From this research was noted that failure <strong>of</strong> all zirconia and<br />
lithium disilicate systems originates with screw bending at approximately 370-400N. The<br />
authors were concerned about the additional mode <strong>of</strong> failure <strong>of</strong> cementable abutments (adhesion<br />
or cohesive) at the zirconia or lithium disilicate- Ti abutment interface. No cement failures were<br />
noted in either group up to 600 N. Preload will be lost from abutment retaining screw prior to<br />
fracture <strong>of</strong> the abutmentcrown complex. Improved failure loads may be possible if screws with<br />
increased bending resistance are used.<br />
Conclusion: The type <strong>of</strong> ceramic abutment material and implant connection influences stability<br />
and fracture resistance <strong>of</strong> ceramic abutments. The failure mode <strong>of</strong> both test and control groups<br />
was similar; bending <strong>of</strong> abutment retaining screw. The cementable zirconia and lithium<br />
disilicate abutments had similar fracture resistance, which was higher than other 2-piece<br />
zirconia and pressed lithium disilicate abutment systems. All test samples demonstrated<br />
adequate strength for use in the anterior region.<br />
47