Jarvie Journal - College of Dental Medicine - Columbia University
Jarvie Journal - College of Dental Medicine - Columbia University
Jarvie Journal - College of Dental Medicine - Columbia University
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
Volume 56, Spring 2013<br />
Circulating Endothelial Progenitor Cells in Periodontitis<br />
T. Spinell, D. Jönsson, A. Vrettos, R.T. Demmer, R. Celenti, S. Chen, M. Kebschull, P.N. Papapanou<br />
Division <strong>of</strong> Periodontics, Section <strong>of</strong> Oral and Diagnostic Sciences,<br />
<strong>Columbia</strong> <strong>University</strong> <strong>College</strong> <strong>of</strong> <strong>Dental</strong> <strong>Medicine</strong>, NY, NY<br />
Introduction: Circulating Endothelial Progenitor Cells (cEPCs) are bone marrow-derived stem cells that are<br />
recruited into the blood stream and can home to sites <strong>of</strong> endothelial injury where they can develop into functional<br />
endothelial cells. cEPCs have attracted attention as markers for endothelial function and due to their potential use<br />
in therapeutic angiogenesis, but also because <strong>of</strong> their association with a number <strong>of</strong> pathologic conditions,<br />
including sepsis, atherosclerosis, rheumatoid arthritis and inflammatory bowel disease. From a biological<br />
plausibility point <strong>of</strong> view, there are two distinct alternatives through which periodontal infections may be related<br />
to cEPC levels: The transient bacteremias and the state <strong>of</strong> systemic inflammation and endothelial damage that are<br />
associated with periodontitis may induce enhanced EPC recruitment from the bone marrow, resulting in an<br />
increase in the levels <strong>of</strong> cEPCs in the bloodstream. On the other hand, vascular endothelial damage may result in<br />
cEPC homing to sites <strong>of</strong> endothelial injury, and systemic inflammation may impair cEPC proliferation and<br />
increase cEPC apoptosis resulting in an exhaustion <strong>of</strong> the cEPC pool and lower cEPC levels.<br />
Objective: The aim <strong>of</strong> this cross-sectional study was to compare the levels <strong>of</strong> endothelial progenitor cells in the<br />
peripheral blood <strong>of</strong> patients with moderate to severe periodontitis to that <strong>of</strong> age-, gender- and menstruation cyclematched<br />
periodontally healthy controls.<br />
Materials and Methods: A total <strong>of</strong> 110 participants, men and women between 25-65 years <strong>of</strong> age with >20 teeth<br />
present, have been enrolled to date. These included periodontitis patients (> 2 teeth per quadrant with a probing<br />
depth <strong>of</strong> ≥ 5 mm and clinical attachment loss <strong>of</strong> ≥3 mm as well as bleeding on probing at ≥30% <strong>of</strong> their sites) and<br />
periodontally healthy controls (no teeth with probing depth <strong>of</strong> >5 mm or interproximal attachment loss > 2mm).<br />
Individuals using antibiotics within 3 months <strong>of</strong> recruitment, those diagnosed with systemic conditions known to<br />
affect periodontitis or EPC levels (i.e., hypertension, hypercholesterolemia, rheumatoid arthritis), pregnant<br />
women and current smokers were excluded.<br />
All participants underwent a comprehensive evaluation <strong>of</strong> their periodontal status including assessments <strong>of</strong><br />
plaque, bleeding on probing, probing depth (PD) and clinical attachment loss (CAL). Body mass index (BMI) and<br />
systolic blood pressure (SBP) were recorded, and a 60 ml blood sample was obtained. Hemangioblastic cEPC<br />
levels were assessed as a percentage <strong>of</strong> viable peripheral blood mononuclear cells using flow cytometry, based on<br />
the expression <strong>of</strong> progenitor cell markers CD34 and CD133 and <strong>of</strong> endothelial cell marker KDR (kinase insert<br />
domain receptor). Monocytic cEPC levels were assessed after culture <strong>of</strong> peripheral blood mononuclear cells and<br />
subsequent characterization using fluorescent microscopy on the basis <strong>of</strong> LDL uptake and lectin staining.<br />
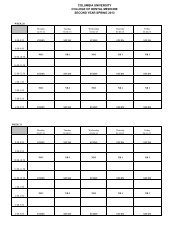
Results and Conclusions: Thus far, hemangioblastic cEPC levels have been assessed in 88 subjects (46<br />
periodontitis patients and 42 periodontally healthy controls) and monocytic cEPC levels in 45 subjects (22<br />
periodontitis patients and 23 controls). Analyses based on 42 matched pairs showed higher hemangioblastic cEPC<br />
levels in periodontitis patients than controls (p=0.057) but comparable monocytic cEPC levels (p=0.443).<br />
Regression analyses adjusting for age, gender, BMI and SBP showed that the % <strong>of</strong> pockets with probing depth ≥ 4<br />
mm (p=0.046) or ≥ 6 mm (p=0.008) and the % <strong>of</strong> sites with attachment loss ≥ 6 mm (p=0.019) were associated<br />
with hemangioblastic cEPC levels. Levels <strong>of</strong> hemangioblastic and monocytic cEPCs were positively correlated<br />
(r=0.392, p=0.008).<br />
Discussion: Poor periodontal status appears to be positively associated with cEPC levels, indicating an increased<br />
mobilization <strong>of</strong> EPCs from the bone marrow in response to endothelial injury in periodontitis. The kinetics <strong>of</strong> this<br />
mobilization and its association with vascular repair and function need to be elucidated further.<br />
55