Final Clinical Study Report for CA180003 - Bristol-Myers Squibb
Final Clinical Study Report for CA180003 - Bristol-Myers Squibb
Final Clinical Study Report for CA180003 - Bristol-Myers Squibb
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
Dasatinib<br />
BMS-354825<br />
Name of Sponsor/Company:<br />
<strong>Bristol</strong>-<strong>Myers</strong> <strong>Squibb</strong><br />
Name of Finished Product:<br />
Individual <strong>Study</strong> Table Referring<br />
to the Dossier<br />
<strong>CA180003</strong><br />
<strong>Clinical</strong> <strong>Study</strong> <strong>Report</strong><br />
(For National Authority Use<br />
Only)<br />
Name of Active Ingredient:<br />
SYNOPSIS<br />
<strong>Final</strong> <strong>Clinical</strong> <strong>Study</strong> <strong>Report</strong> <strong>for</strong> <strong>CA180003</strong><br />
TITLE OF STUDY: A Phase I Dose-Escalation <strong>Study</strong> of BMS-354825 in Patients with Refractory Solid<br />
Tumors<br />
INVESTIGATORS/STUDY CENTERS: 2 sites in the United States and 1 site in the European Union<br />
PUBLICATIONS: None<br />
STUDY PERIOD: <strong>Study</strong> Initiation Date: 28-Jun-2004 CLINICAL PHASE: 1<br />
(First Subject First Visit)<br />
<strong>Study</strong> Completion Date: 12-Jul-2007<br />
(Last Subject Last Visit)<br />
OBJECTIVES: The primary objective of this study was to establish the maximum tolerated dose (MTD),<br />
dose limiting toxicity (DLT), and a recommended Phase 2 dose of dasatinib when administered orally on an<br />
(i) every 12 hours <strong>for</strong> 5 consecutive days followed by 2 nontreatment days every week (5D2) schedule and<br />
(ii) on a twice daily continuous dosing (CDD) schedule in subjects with metastatic solid tumors that were<br />
refractory to standard therapies or <strong>for</strong> which no effective standard therapy existed. Secondary objectives<br />
were:<br />
1) To assess the safety and tolerability of dasatinib when administered orally on a (i) 5D2 and (ii) CDD<br />
schedule<br />
2) To characterize the plasma pharmacokinetics (PK) of dasatinib when administered orally on a (i) 5D2<br />
and (ii) CDD schedule<br />
3) To assess the effect of food (high-fat breakfast) on the PK of dose levels 1 and 5 of dasatinib<br />
4) To assess the effect of predose administration of a single dose of famotidine 40 mg on the PK of (i)<br />
dose levels 2 and 6 of dasatinib, and (ii) dose levels 3 and 7 of dasatinib administered 5 minutes after a<br />
high-fat breakfast<br />
5) To assess the effect of predose and postdose administration of aluminum hydroxide/magnesium<br />
hydroxide/simethicone or aluminum hydroxide/magnesium hydroxide on the PK of dose levels 4 and 8<br />
of dasatinib<br />
6) To describe any preliminary evidence of efficacy of dasatinib in the treatment of solid tumors as<br />
defined by the modified World Health Organization (WHO) criteria<br />
7) To per<strong>for</strong>m correlative scientific studies to explore effects of dasatinib on several biomarkers of kinase<br />
activity, signaling, response and/or toxicity (eg, SRC, KIT, FAK, EPH) in peripheral blood cells,<br />
plasma and, whenever possible, in serial tumor biopsy samples from subjects with solid tumors<br />
Approved v1.0 930024906 2.0
Dasatinib<br />
BMS-354825<br />
<strong>CA180003</strong><br />
<strong>Clinical</strong> <strong>Study</strong> <strong>Report</strong><br />
8) To describe any preliminary evidence of modulation by dasatinib of tumor glycolytic pathways using<br />
18F-FDG positron emission tomography (PET)<br />
9) To describe any preliminary effect of dasatinib on platelet function as assessed by bleeding time<br />
measurements and/or platelet aggregometry<br />
10) To analyze mRNA expression in pretreatment blood and archived tumor samples and identify potential<br />
predictors of response and toxicity to dasatinib<br />
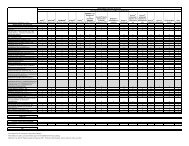
METHODOLOGY: This was an open-label, Phase 1 dose-escalation study. Treatment began at 70 mg<br />
total daily dose (TDD) on the 5D2 regimen and was escalated as shown in the following table. At least<br />
3 subjects were enrolled per cohort and followed <strong>for</strong> 4 weeks on study drug. If a DLT was reported, that<br />
dose cohort was expanded to 6 subjects. Dose escalation continued as long as fewer than one-third of<br />
subjects in a cohort had a DLT in their first 2 weeks of treatment. Once the MTD was reached on the 5D2<br />
schedule, new subjects were enrolled on the CDD schedule beginning at 2 dose levels below the MTD with<br />
the 5D2 schedule. Dose escalation on the CDD schedule continued until an MTD was reached.<br />
Dose Level of Dasatinib<br />
Dose Every 12 hours<br />
(Total Daily Dose)<br />
1 35 mg q 12 hr (70 mg TDD)<br />
2 50 mg q 12 hr (100 mg TDD)<br />
3 70 mg q 12 hr (140 mg TDD)<br />
4 90 mg q 12 hr (180 mg TDD)<br />
5 120 mg q 12 hr (240 mg TDD)<br />
6 160 mg q 12 hr (320 mg TDD)<br />
7 200 mg q 12 hr (400 mg TDD)<br />
8 250 mg q 12 hr (500 mg TDD)<br />
A treatment cycle was defined as 4 weeks (28 days). Dasatinib was administered according to the assigned<br />
concomitant treatments (ie, with food and/or famotidine, or aluminum hydroxide/magnesium hydroxide, as<br />
described in secondary objectives 3 through 5) with the morning dose on Day 1 of Cycle 1. Thereafter,<br />
dasatinib was administered without these treatments.<br />
The plasma PK of dasatinib and BMS-606181 were evaluated <strong>for</strong> all treated subjects after the morning dose<br />
on Day 1. The plasma PK of dasatinib were also to be evaluated after the morning dose once on Days 3 to 5<br />
(fasted), and once on Days 24 to 26 (fasted). However, examination of the data revealed that the majority<br />
of data from subjects on the 5D2 schedule was collected on Day 8, after the 2-day drug holiday. Subjects<br />
were monitored continuously <strong>for</strong> toxicity.<br />
NUMBER OF SUBJECTS (Planned and Analyzed): Subjects were accrued to each dose level in<br />
cohorts of 3 to 6. A total of 85 subjects were enrolled and 67 were treated, 33 on the 5D2 schedule and<br />
34 on the CDD schedule. Data from all treated subjects were included in the analyses of safety and<br />
efficacy, data from those with adequate concentration profiles were included in the PK analyses, and data<br />
from those with a baseline and at least 1 postdose assessment were included in the pharmacodynamic<br />
analyses.<br />
DIAGNOSIS AND MAIN CRITERIA FOR INCLUSION: Subjects were ≥ 18 years of age with an<br />
Eastern Cooperative Oncology Group (ECOG) per<strong>for</strong>mance status score 0 – 1, had histologic or cytologic<br />
diagnosis of a primary solid (ie, nonhematologic) malignancy and evidence (radiographic or tissue<br />
Approved v1.0 930024906 2.0
Dasatinib<br />
BMS-354825<br />
<strong>CA180003</strong><br />
<strong>Clinical</strong> <strong>Study</strong> <strong>Report</strong><br />
confirmation) of metastatic disease which had progressed on or following currently available standard<br />
therapies or <strong>for</strong> which no standard therapy existed.<br />
TEST PRODUCT, DOSE AND MODE OF ADMINISTRATION, DURATION OF TREATMENT,<br />
BATCH NUMBERS: Dasatinib doses of 70 mg to 320 mg TDD were administered orally on the 5D2<br />
schedule and doses of 140 to 240 mg TDD were administered orally on the CDD schedule. Overall, the<br />
median duration of therapy ranged from 0.8 to 4.0 months/subject across dose cohorts and the median<br />
cumulative dose ranged from 1400 to 20,875 mg/subject. Excluding dose interruptions, the net dose<br />
intensity ranged from 54 to 198.5 mg/day/subject. Dasatinib tablets were provided in the 5-mg strength<br />
(batch numbers 5F02041, 3C72889, 4C88975, 4G78659, 5A01426, 5C02739) and in the 50-mg strength<br />
(batch numbers 3C72907, 4A81197, 4C91969, 4G78663, 5A01431, 5C04559).<br />
REFERENCE THERAPY, DOSE AND MODE OF ADMINISTRATION, DURATION OF<br />
TREATMENT, BATCH NUMBERS: There was no reference therapy in this study.<br />
CRITERIA FOR EVALUATION:<br />
Efficacy: Tumor response was assessed after every second cycle (i.e., every 8 weeks), every 12 weeks<br />
after 24 weeks of treatment, and at the end of treatment and classified as complete response, partial<br />
response, stable disease, or progressive disease. Subjects with a complete or partial response were to have<br />
confirmatory tumor measurements within 4 to 6 weeks after response. Safety: Dose limiting toxicity was<br />
defined as any of the following events which were judged to be at least possibly related to dasatinib and<br />
occurred during the first 4 weeks of drug administration:Grade 3 or 4 nausea, vomiting, or diarrhea despite<br />
the use of adequate/ maximal medical intervention and/or prophylaxis<br />
• Any other drug-related Grade 3 or greater nonhematological toxicity except alopecia or fatigue<br />
• Any grade toxicity which in the judgment of the investigator or sponsor required dose reduction or<br />
removal from the study<br />
• Delayed recovery from toxicity related to treatment with dasatinib which delayed scheduled<br />
retreatment <strong>for</strong> > 14 days<br />
• A QTc interval ≥ 500 msec<br />
• Grade 4 neutropenia (ANC < 500 cells/mm 3 )<strong>for</strong> ≥ 5 consecutive days or febrile neutropenia (ie, fever ≥<br />
38.5° C with ANC < 1000/mm 3 )<br />
• Thrombocytopenia ≤ 25,000 cells/mm 3 or bleeding requiring a platelet transfusion<br />
For each schedule, the dose level below the maximum administered dose (MAD) was considered the MTD,<br />
providing DLT was reported in less than one-third of subjects at that dose level. The determination of the<br />
MTD and recommended Phase 2 dose were defined by DLT occurring in the first 4 weeks of treatment.<br />
Additional safety evaluations included monitoring of adverse events (AEs), serious adverse events (SAEs),<br />
electrocardiograms (ECG), vital signs, physical examinations, and clinical laboratory tests. Adverse events<br />
and other symptoms were graded according to the National Cancer Institute Common Terminology Criteria<br />
<strong>for</strong> Adverse Events (NCI-CTCAE) Version 3.0.<br />
Pharmacokinetics: Pharmacokinetic blood samples <strong>for</strong> determination of dasatinib and the metabolite<br />
BMS-606181 concentrations were collected during Cycle 1 following the morning doses on Day 1, once on<br />
nominal Day 8, and once on nominal Days 24 to 26 at the following time points: predose, 30 minutes, and<br />
1, 1.5, 2, 3, 4, 5, 6, 8, and 10 hours post dose. The PK parameters determined <strong>for</strong> dasatinib and BMS-<br />
686181 were: maximum plasma concentration (Cmax), time to Cmax (Tmax), plasma half-life (T-HALF),<br />
apparent oral clearance (CLo), apparent volume of distribution in the terminal phase (Vz/F), and area under<br />
the curve (AUC) from zero extrapolated to infinity [AUC (INF)], within the dosing interval [AUC(TAU)],<br />
and from zero to the last quantifiable sampling time (AUCt). Since samples had been collected after the 2-<br />
day drug holiday, AUC(INF) on Day 8 instead of AUC(TAU) was used <strong>for</strong> the 5D2 schedule while<br />
Approved v1.0 930024906 2.0
Dasatinib<br />
BMS-354825<br />
<strong>CA180003</strong><br />
<strong>Clinical</strong> <strong>Study</strong> <strong>Report</strong><br />
AUC(TAU) was used <strong>for</strong> the CDD schedule <strong>for</strong> statistical analyses of AUC. The PK parameters<br />
determined <strong>for</strong> BMS-606181 were Cmax, AUCt, and Tmax.<br />
Pharmacodynamics: Blood samples were collected <strong>for</strong> phosphorylated SRC and phosphorylated FAK in<br />
peripheral blood mononuclear cells on Day 1, once on Days 3 to 5, and once on Days 24 to 26 of Cycle 1<br />
predose and 4, 8 and 24 hours post dose. Assessment of KIT and stem cell factor was optional and no site<br />
elected to participate. Blood samples <strong>for</strong> potential plasma markers of response or toxicity were collected<br />
pre-dose and within 1 month after clinical determination of either response or progression. Tumor<br />
metabolism was assessed with 18F-FDG PET 1 to 2 times within 21 days prior to dosing on Day 1, and<br />
following dosing during Weeks 1, 4, and 8 of treatment.<br />
Pharmacogenomics: Freshly obtained tumor sample was collected (as feasible) pretreatment or up to<br />
2 times while on-treatment <strong>for</strong> immunohistochemistry (IHC), mRNA expression, and genotyping. Archived<br />
tumor tissue was collected (as feasible) pretreatment and/or on-treatment <strong>for</strong> IHC, mRNA expression and<br />
genotyping.<br />
STATISTICAL CONSIDERATIONS: Descriptive statistics were used to summarize efficacy, safety,<br />
PK, and pharmacodynamic observations. Categorical variables were summarized in frequency tables.<br />
Continuous variables were summarized with mean, median, and minimum and maximum values. For the<br />
PK analyses, geometric means and coefficients of variation were presented <strong>for</strong> Cmax, AUCt, AUC(TAU),<br />
and AUC(INF). Medians, minima, and maxima were reported <strong>for</strong> Tmax. To estimate the effect of food on<br />
the PK of dasatinib, an analysis of variance was per<strong>for</strong>med on log(Cmax) and log(AUC), <strong>for</strong> each dose<br />
separately and across doses. Similar analyses were per<strong>for</strong>med to estimate the effects of famotidine,<br />
famotidine after food, and aluminum hydroxide/magnesium hydroxide on the PK of dasatinib. To assess<br />
dose proportionality, a statistical linear regression analyses of log(AUC) on log(dose), <strong>for</strong> Day 8 and Day<br />
26 was conducted.<br />
SUMMARY OF RESULTS:<br />
Disposition, Demographics, and Other Pertinent Baseline Characteristics: Of the 67 treated subjects,<br />
33 received dasatinib on the 5D2 schedule and 34 on the the CDD schedule. Two subjects, both in the CDD<br />
group, completed treatment. The majority of subjects went off study due to documented disease<br />
progression (34/67, 50.7%), deterioration without documented progression (15/67, 22.4%), or study drug<br />
toxicity (12/67, 17.9%). Two subjects went off study due to death, 1 at subject request, and 1 due to an<br />
adverse event (AE) unrelated to study treatment The median age of all 67 subjects was 56.4 years, 92.5%<br />
were white, and all had a baseline ECOG per<strong>for</strong>mance status score of 0 or 1. Sixty-six subjects (98.5%) had<br />
a target lesion at baseline; a majority had more than 1. The most frequent sites of disease (in ≥10% of<br />
subjects) were visceral (liver and lung), skin/soft tissue, lymph node, other sites, pelvis, and peritoneum.<br />
The median time from cancer diagnosis to study start was 43.1 months. Sixty-six (98.5%) subjects reported<br />
at least 1 medical condition at baseline and 32 (47.8%) reported at least 1 pretreatment clinical complaint or<br />
finding. Prior treatments <strong>for</strong> cancer included chemotherapy (63/67, 94.0%), surgery (67/67, 100%),<br />
radiotherapy (19/67, 28.4%), hormonal/immuno/biologic therapy (4/67, 6.0%), and other investigational<br />
agents (8/67, 11.9%).<br />
Efficacy Results: No confirmed objective tumor responses were achieved in this study. Eleven (16.4%)<br />
subjects had a best clinical response rating of stable disease while on therapy, including 7/33 (21.2%) of<br />
subjects on the 5D2 schedule and 4/34 (11.8%) of subjects on the CDD schedule. Thirty-one subjects<br />
(46.3%) had progressive disease, including 19/33 (57.6%) treated on the 5D2 schedule and 12/34 (35.3%)<br />
on the CDD schedule. Thirteen (19.4%) subjects had a rating of clinical progression, which was based on<br />
in<strong>for</strong>mation included in the CRF providing evidence that patients had symptoms of progression in the<br />
absence of radiographic evidence. Ten subjects, all of whom were treated on the CDD schedule, were<br />
discontinued due to drug toxicity. Two subjects (one on each schedule) had no data available.<br />
Safety Results: The MTD on the 5D2 schedule was 240 mg TDD, with 1 of 6 evaluable subjects reporting<br />
DLT (Grade 3 tumor lysis syndrome). The 240-mg dose was 1 level below the MAD of 320 mg, at which 3<br />
Approved v1.0 930024906 2.0
Dasatinib<br />
BMS-354825<br />
<strong>CA180003</strong><br />
<strong>Clinical</strong> <strong>Study</strong> <strong>Report</strong><br />
of 4 evaluable subjects had DLT (recurrent Grade 2 rash; Grade 3 lethargy; and 1 subject with Grade 3<br />
prolonged bleeding time and Grade 3 hypocalcemia).<br />
The MTD on the CDD schedule was 140 mg TDD, at which no subjects reported DLT. Treatment on this<br />
schedule was initiated at 140 mg and escalated to the MAD of 240 mg, at which 3 of 4 evaluable subjects<br />
reported DLT (Grade 3 nausea; Grade 3 fatigue; and 1 subject with Grade 2 proteinuria and Grade 3 rash).<br />
The first 4 subjects at an intermediate dose level of 200 mg TDD reported no DLT; however, when this<br />
cohort was expanded with an additional 12 subjects, 6 of the 13 evaluable subjects reported DLT( Grade 3<br />
dyspnea; Grade 3 constipation; Grade 2 proteinuria; Grade 4 fatigue; Grade 3 lethargy; and 1 subject with<br />
Grade 2 myocardial toxicity, Grade 4 elevated cardiac troponin, and Grade 2 ECG T-wave inversion). At<br />
the 180-mg dose, which was 1 level below the MAD, 2 of 7 evaluable subjects reported DLT (Grade 3<br />
proteinuria and Grade 2 rash in 1 subject and Grade 1 cognitive impairment, and Grade 2 somnolence,<br />
altered taste, slurred speech, and unsteady gait in the other subject).<br />
All but 1 of the 67 subjects (98.5%) reported at least 1 AE. Grade 3 to 5 AEs were reported at a similar<br />
incidence among subjects treated on the 5D2 (17/33, 52%) and CDD (20/34, 59%) schedules. A total of<br />
64/67 subjects (95.5%) reported at least 1 drug-related AE; the incidence was 33/33 subjects (100%) on the<br />
5D2 schedule and 31/34 subjects (91.2%) on the CDD schedule. The most frequent AEs (regardless of<br />
relationship) were nausea, anorexia, and fatigue. Nausea and fatigue were reported at a similar incidence on<br />
either schedule; anorexia was reported more frequently among subjects on the CDD schedule (21/34,<br />
61.8%) compared with the 5D2 schedule (13/33, 39.4%). The incidence of AEs and drug-related AEs was<br />
not dose related.<br />
Eighteen subjects died, 10 during the study period or within 30 days of their last dose of dasatinib and 8<br />
more than 30 days after their last dose of dasatinib. All but 1 of these deaths were due to disease<br />
progression; 1 subject died due to gastrointestinal bleeding that the investigator considered most likely due<br />
to disease progression but could not rule out a possible contribution by the study drug. Thirty-four (34/67,<br />
50.7%) subjects reported SAEs, 13 (19.4%) of whom reported SAEs that were considered drug-related.<br />
Drug-related SAEs were more frequent among subjects treated on the 5D2 schedule (9/33, 27.3%)<br />
compared with subjects treated on the CDD schedule (4/34, 11.8%). Twenty-four (24/67, 35.8%) subjects<br />
discontinued study treatment due to AEs. Discontinuation due to AEs was more frequent among subjects<br />
on the CDD schedule (15/34, 44.1%) compared with subjects on the 5D2 schedule (9/33, 27.3%).<br />
Grade 3 to 4 abnormalities in selected clinical laboratory values <strong>for</strong> hematologic parameters and<br />
electrolytes were infrequent and were not related to the treatment schedule. No clinically meaningful<br />
changes in vital signs measurements or physical examination findings were noted; ECG results will be<br />
reported separately.<br />
Pharmacokinetic Results: Dasatinib was detectable in plasma 30 minutes after oral administration and<br />
reached Cmax at median Tmax values of 0.5 to 3.1 h in absence of any treatment effects (Days 8 and 26).<br />
The AUC increased approximately proportionally to dose; the slope (90% CI) was 1.08 (0.63, 1.54) on Day<br />
8 and 1.07 (0.63, 1.51) on Day 26. The Cmax and AUC values of Day 8 and 26 appeared to be similar,<br />
indicating no clinically relevant accumulation on repeated dosing. Across the range of 70 to 320 mg, the<br />
mean T-HALF of dasatinib was consistent on Days 8 and 26. Although consistent across the dose groups,<br />
the variability <strong>for</strong> both CLo and Vz/F was large.<br />
At the MTD of 140 mg TDD on the CDD schedule, median (min, max) dasatinib Tmax was similar across<br />
days. The Tmax and T-HALF values of dasatinib on Days 8 and 26 were similar to Day 1, indicating no<br />
change in absorption or elimination in the presence of food or famotidine, or after multiple dosing. The<br />
geometric mean (CV%) Cmax and AUC(TAU) values suggested minimal accumulation.<br />
Food decreased dasatinib Cmax by 20% and increased AUC by 1% at 70-mg TDD, and decreased Cmax by<br />
34% and AUC by 9% at 240 mg. Overall, food decreased Cmax by 29% and AUC by 5%; the ratio of<br />
geometric means (90% CI) was 0.71 (0.47, 1.09) <strong>for</strong> Cmax and 0.95 (0.73, 1.22) <strong>for</strong> AUC. Famotidine<br />
decreased dasatinib Cmax by 87% and AUC by 82% at 100 mg, and by 82% and 74%, respectively at<br />
320 mg. Overall, famotidine decreased Cmax by 85% and AUC by 79%; the ratio of geomtric means (90%<br />
Approved v1.0 930024906 2.0
Dasatinib<br />
BMS-354825<br />
<strong>CA180003</strong><br />
<strong>Clinical</strong> <strong>Study</strong> <strong>Report</strong><br />
CI) was 0.15 (0.05, 0.50) <strong>for</strong> Cmax and 0.21 (0.10, 0.45) <strong>for</strong> AUC. Administration of famotidine with a<br />
high-fat breakfast decreased dasatinib Cmax by 73% and AUC by 25%; the ratio of geometric means was<br />
0.27 (0.08, 0.95) <strong>for</strong> Cmax and 0.75 (0.38, 1.50) <strong>for</strong> AUC. Administration of aluminum<br />
hydroxide/magnesium hydroxide resulted in 36% and 24% decrease in dasatinib Cmax and no apparent<br />
decrease in dasatinib AUC; the ratio of geometric means was 0.64 (0.46, 0.89) <strong>for</strong> Cmax and 0.76 (0.54,<br />
1.06) <strong>for</strong> AUC.<br />
Dose<br />
(mg TDD)<br />
/Schedule<br />
Cmax<br />
(ng/mL)<br />
Geom.<br />
Mean<br />
(CV%)<br />
AUC<br />
(ng•h/mL)<br />
Geom.<br />
Mean<br />
(CV%)<br />
Tmax<br />
(h)<br />
Median<br />
(Min,<br />
Max)<br />
Dose<br />
Day Condition N<br />
70/5D2 1 Food 7 16.82 (141) 85.89 (58) a 3.0<br />
8 Fasted 6 24.85 (99) 84.81 (73)<br />
26 Fasted 4 18.56 (84) 84.15 (30)<br />
100/5D2 1 Fam 3 5.0 (20) 24.99 (44)<br />
8 Fasted 3 38.37 (45) 140.31 (22)<br />
26 Fasted 3 43.35 (100) 157.96 (4)<br />
(0.5, 6.0)<br />
1.5<br />
(0.5, 4.0)<br />
1.4<br />
(0.5, 1.6)<br />
3.0<br />
(3.0, 5.0)<br />
1.0<br />
(0.5, 3.0)<br />
0.5<br />
(0.5, 2.0)<br />
140/5D2 1 Fam+Food 4 18.05 (65) 183.61 (8) b 6.5<br />
(4.0, 10.0)<br />
8 Fasted 3 46.29 (91) 165.08 (78)<br />
0.5<br />
(0.5, 2.0)<br />
26 Fasted 4 25.02 (80) 160.65 (8)<br />
2.0<br />
(1.0, 6.0)<br />
140/CDD 1 Fam+Food 5 14.78 (35) 141.29 (78)<br />
4.0<br />
(2.0, 5.0)<br />
8 Fasted 3 78.41 (90) 245.31 (57)<br />
1.0<br />
(0.5, 6.0)<br />
26 Fasted 3 50.19 (86)<br />
325.34 3.1<br />
(19) b (1.1, 6.1)<br />
180/5D2 1 Maalox 6 63.65 (54) 248.91 (67)<br />
2.3<br />
(1.0, 4.0)<br />
8 Fasted 5 88.94 (44) 251.02 (37)<br />
1.0<br />
(0.5, 4.0)<br />
26 Fasted 5 83.43 (58)<br />
492.07 3.0<br />
(33) c (1.0, 8.0)<br />
180/CDD 1 Maalox 6 41.30 (93) 170.13 (72)<br />
2.2<br />
(0.6, 5.0)<br />
8 Fasted 6 51.80 (84) 204.08 (68)<br />
1.6<br />
(0.0, 3.1)<br />
26 Fasted 5 71.69 (59) 273.54 (45)<br />
1.5<br />
(0.5, 5.0)<br />
200/CDD 1 Fasted<br />
1<br />
227.57 2.0<br />
44.01 (97)<br />
7<br />
(83) d (0.5, 9.8)<br />
8 Fasted<br />
1<br />
218.14 1.5<br />
55.96 (118)<br />
2<br />
(102) (0.5, 3.6)<br />
T-HALF<br />
(h)<br />
Mean<br />
(SD)<br />
3.60<br />
Clo<br />
(L/h)<br />
Mean<br />
(SD)<br />
Vz/F<br />
(L)<br />
Mean<br />
(SD)<br />
(1.63) a -- --<br />
2.97 641.6 3083<br />
(1.13) (650.6) (3866)<br />
3.04 433.0 1842<br />
(0.93) (146.2) (602)<br />
2.84<br />
(1.88)<br />
-- --<br />
3.76 402.4 2144<br />
(0.58) (74.1) (205)<br />
4.43 316.7 2034<br />
(2.19) (12.6) (1052)<br />
2.36 --<br />
(0.43) b --<br />
4.92 1187.7 9464<br />
(1.45) (1715.9 (1417<br />
) 5)<br />
4.32 487.7 3649<br />
(1.58) (37.1) (94)<br />
7.13 --<br />
(3.26)<br />
--<br />
4.00 326.9 2039<br />
(0.82) (209.5) (1715)<br />
2.46 217.2 739<br />
(0.99) b (42.0) b (162) b<br />
3.45 --<br />
(0.92)<br />
--<br />
3.15 437.8 1922<br />
(0.67) (310.5) (1204)<br />
2.34 190.8 600<br />
(0.74) c (64.2) c (82) c<br />
3.32 --<br />
(1.37)<br />
--<br />
4.07 544.9 3516<br />
(1.25) (364.1) (2894)<br />
3.08 409.2 2176<br />
(1.15) (359.7) (2727)<br />
3.65<br />
(1.30) d -- --<br />
4.34 666.9 4224<br />
(1.72) (537.9) (3549)<br />
Approved v1.0 930024906 2.0
Dasatinib<br />
BMS-354825<br />
<strong>CA180003</strong><br />
<strong>Clinical</strong> <strong>Study</strong> <strong>Report</strong><br />
Dose<br />
(mg TDD)<br />
/Schedule<br />
Day<br />
Dose<br />
Condition<br />
N<br />
Cmax<br />
(ng/mL)<br />
Geom.<br />
Mean<br />
(CV%)<br />
AUC<br />
(ng•h/mL)<br />
Geom.<br />
Mean<br />
(CV%)<br />
26 Fasted 7 51.63 (96) 207.01 (79)<br />
240/5D2 1 Food 9 76.92 (64) 352.18 (41)<br />
8 Fasted 5 76.66 (73) 298.27 (66)<br />
26 Fasted 7 98.17 (82)<br />
395.76<br />
(74)<br />
240/CDD 1 Food 5 80.47 (70) 423.42 (64)<br />
8 Fasted 5 130.80 (48) 526.14 (49)<br />
26 Fasted 1 59.94 (.) 207.26 (.)<br />
320/5D2 1 Fam 4 21.09 (164) 102.78 (83)<br />
8 Fasted 2 203.39 (53) 436.39 (56)<br />
26 Fasted 1 177.58 (.) 501.91 (.)<br />
Tmax<br />
(h)<br />
Median<br />
(Min,<br />
Max)<br />
2.0<br />
(0.5, 5.0)<br />
2.0<br />
(0.5, 4.0)<br />
1.0<br />
(0.5, 2.0)<br />
1.0<br />
(0.5, 2.0)<br />
2.0<br />
(1.0, 6.5)<br />
0.5<br />
(0.0, 2.0)<br />
1.5<br />
(1.5, 1.5)<br />
2.0<br />
(0.5, 5.0)<br />
0.8<br />
(0.5, 1.0)<br />
1.5<br />
(1.5, 1.5)<br />
T-HALF<br />
(h)<br />
Mean<br />
(SD)<br />
3.20<br />
(1.71)<br />
3.14<br />
(1.10)<br />
3.24<br />
(0.75)<br />
3.32<br />
(1.53)<br />
4.00<br />
(1.91)<br />
3.35<br />
(0.73)<br />
2.2 (.)<br />
3.57<br />
(1.23)<br />
2.72<br />
(0.56)<br />
2.6 (.)<br />
Clo<br />
(L/h)<br />
Mean<br />
(SD)<br />
696.5<br />
(793.0)<br />
Vz/F<br />
(L)<br />
Mean<br />
(SD)<br />
2740<br />
(2541)<br />
-- --<br />
511.3<br />
(325.6)<br />
367.5<br />
(234.4)<br />
2223<br />
(1079)<br />
1679<br />
(1145)<br />
-- --<br />
269.8<br />
(195.0)<br />
590.4<br />
(.)<br />
1401<br />
(1336)<br />
1877<br />
(.)<br />
-- --<br />
411.0<br />
(223.8)<br />
318.8<br />
(.)<br />
1523<br />
(549)<br />
1195<br />
(.)<br />
Cmax = maximum plasma concentration; AUC = area under the plasma concentration-time curve, AUC(INF) <strong>for</strong> Day 1 and Day 8 <strong>for</strong><br />
5D2 schedule and AUC(TAU) <strong>for</strong> Day 8 <strong>for</strong> CDD schedule and Day 26 <strong>for</strong> both schedules ;Tmax = time to reach Cmax; T-HALF =<br />
terminal elimination half-life; Geom. = geometric; -- = missing or not calculated; Fam = famotidine<br />
a: N=6; b: N=2; c: N=4; d: N=14<br />
BMS-606181 was rapidly <strong>for</strong>med after oral administration of dasatinib with Cmax reached at 1.0 to 10.0 h.<br />
The summary statistics on Day 8 suggest that AUCt and Cmax increased in a dose-related manner.<br />
Variability in Cmax and AUCt <strong>for</strong> BMS-606181 was greater than the parent drug. The ratio of the<br />
geometric mean of the AUC of BMS-606181 over that of dasatinib on Days 8 and 26, unadjusted <strong>for</strong> the<br />
molecular weight difference (which was less than 10%), ranged from less than 1% to 13%, except <strong>for</strong> the<br />
140 mg/5D2 schedule where the metabolite ratio was 25%. At the proposed MTD dose of 140 mg TDD<br />
with the CDD schedule, the ratios of geometric mean of the AUC of BMS-606181 over that of dasatinib<br />
were 2.7%, 12.6% and 5.8% on Days 1, 8 and 26, respectively.<br />
Pharmacodynamic Results: Results of other pharmacodynamic parameters will be reported separately.<br />
Pharmacogenomic Results: The results of IHC, mRNA expression, and genotyping will be reported<br />
separately.<br />
CONCLUSIONS: These results indicate that:<br />
• The MTD of dasatinib is 240 mg TDD on the 5D2 schedule and 140 mg TDD on the CDD schedule;<br />
these are the recommended Phase 2 doses<br />
• The DLTs among subjects treated on the 5D2 schedule are dehydration, anorexia, hyponatremia, tumor<br />
lysis syndrome, rash, lethargy, increased bleeding time and hypocalcemia<br />
• The DLTs among subjects treated on the the CDD schedule are cognitive impairment, somnolence,<br />
altered taste, slurred speech, and unsteady gait, proteinuria, rash, dyspnea, constipation, fatigue,<br />
lethargy, myocardial toxicity, troponin elevation, ECG alterations, and nausea<br />
• Overall, dasatinib demonstrated an acceptable safety profile when given orally on a BID regimen in<br />
subjects with advanced malignancies<br />
Approved v1.0 930024906 2.0
Dasatinib<br />
BMS-354825<br />
<strong>CA180003</strong><br />
<strong>Clinical</strong> <strong>Study</strong> <strong>Report</strong><br />
• No objective tumor responses were reported; long-lasting stabilization of disease was noted in some<br />
subjects<br />
• Pharmacokinetic parameters of dasatinib administered on the 5D2 and CDD schedules were reasonably<br />
comparable. The PK parameters of dasatinib in solid tumor subjects were similar to PK parameters<br />
obtained in CML subjects<br />
• Administration of dasatinib with a high-fat breakfast had no clinically significant effect on the<br />
exposure (AUC) of dasatinib<br />
• Administration of dasatinib with famotidine under fasted condition markedly decreased the exposure<br />
of dasatinib<br />
• Administration of dasatinib with famotidine and a high-fat breakfast resulted in a larger decrease in<br />
Cmax than in AUC; administration of dasatinib with famotidine and aluminum hydroxide/magnesium<br />
hydroxide also resulted in a larger decrease in Cmax than in AUC<br />
DATE OF REPORT: 19-Dec-2007<br />
Approved v1.0 930024906 2.0