SYNOPSIS - Clinical Trials - Bristol-Myers Squibb
SYNOPSIS - Clinical Trials - Bristol-Myers Squibb
SYNOPSIS - Clinical Trials - Bristol-Myers Squibb
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
Abatacept<br />
BMS-188667<br />
Name of Sponsor/Company:<br />
<strong>Bristol</strong>-<strong>Myers</strong> <strong>Squibb</strong><br />
Name of Finished Product:<br />
Abatacept (BMS-188667)<br />
Name of Active Ingredient:<br />
Abatacept (BMS-188667)<br />
Individual Study Table Referring<br />
to the Dossier<br />
IM101100<br />
<strong>Clinical</strong> Study Report<br />
(For National Authority Use<br />
Only)<br />
<strong>SYNOPSIS</strong><br />
TITLE OF STUDY: A Phase IIB, Multicenter, Randomized, Double-Blind, Placebo-Controlled Study to<br />
Evaluate the Safety and <strong>Clinical</strong> Efficacy of Two Different Doses of BMS-188667 (Abatacept)<br />
Administered Intravenously to Subjects with Active Rheumatoid Arthritis While Receiving Methotrexate<br />
INVESTIGATORS/STUDY CENTERS AND COUNTRIES: 66 sites worldwide: 32 sites in the<br />
United States; 19 sites in Europe (Belgium, France, Germany, Ireland, Netherlands, and United Kingdom);<br />
7 sites in Canada; 4 sites in Australia; 2 sites in Argentina; and 2 sites in South Africa<br />
PUBLICATIONS:<br />
1. Becker JP, Kremer J, Westhovens R et al. 2002 EULAR Annual Congress of Rheumatology. Abstract<br />
Session 12: Treatment including biologics. [OP7000] A Phase IIB, multi-center, randomized,<br />
double-blind, placebo-controlled study to evaluate the safety and clinical efficacy of two different doses<br />
of CTLA4Ig administered intravenously to subjects with active rheumatoid arthritis.<br />
2. Emery P, Williams GR, Li T et al. 2002 EULAR Annual Congress of Rheumatology. Health services,<br />
economics and outcome research. [SAT0309] Treatment of patients with active rheumatoid arthritis<br />
using methotrexate with CTLA4Ig improves health-related quality of life.<br />
3. Kremer J, Westhovens R et al. A Phase 2B, multi-center, randomized, double-blind, placebo-controlled<br />
study to evaluate the safety and clinical efficacy of two different doses of CTLA4Ig administered<br />
intravenously to subjects with active rheumatoid arthritis while receiving methotrexate. Arthritis and<br />
Rheumatism. September 2002; 46(9, supplement): S203.<br />
4. Williams GR, Li T et al. Impact on health-related quality of life following treatment with CTLA4Ig in<br />
patients with active rheumatoid arthritis using methotrexate. Arthritis and Rheumatism. September<br />
2002; 46(9, supplement): S515.<br />
5. Tugewell P, Emery P, Kremer J, Li T, Williams GR, Ge G, Nuamah I, Bombardier C. 2003 American<br />
College of Rheumatology. Physical function after treatment of CTLA4Ig (BMS-188667), a costimulation<br />
blocker, in patients with active rheumatoid arthritis using methotrexate.<br />
6. Emery P, Russell A, Kremer J, Williams GR, Li T, Nuamah I, Becker JC, Weisman MH. 2003<br />
American College of Rheumatology. Improvement in health-related quality of life with treatment of<br />
CTLA4Ig (BMS-188667), a co-stimulation blocker, over one year in patients with active rheumatoid<br />
arthritis using methotrexate.<br />
7. Kremer KM, Westhovens R et al. Treatment of rheumatoid arthritis by selective inhibition of T-cell<br />
activation with fusion protein CTLA4IG. NEJM 2003; 349 (20): 1907-1915.<br />
2<br />
Approved v1.0 930006747 2.0
Abatacept<br />
BMS-188667<br />
IM101100<br />
<strong>Clinical</strong> Study Report<br />
STUDY PERIOD:<br />
First Subject, First Visit: 11-Dec-2000<br />
Last Subject, Last 6-Month Visit: 11-Dec-2001<br />
Last Subject, Last 12-Month Visit: 13-Jun-2002<br />
CLINICAL PHASE: Phase IIB<br />
OBJECTIVES:<br />
Primary Objective: The primary objective of this study was to compare the clinical efficacy of two<br />
different doses of abatacept (BMS-188667; 10 and 2 mg/kg) combined with methotrexate (MTX) with<br />
MTX plus placebo in subjects with active rheumatoid arthritis (RA) as assessed by ACR 20 at 6 months.<br />
Key Secondary Objectives:<br />
1. ACR 70 assessed at all post-baseline visits.<br />
2. ACR 50 at Day 180 (Month 6) and Day 360 (Month 12).<br />
3. ACR 20, ACR 50, ACR 70, ACR-N at all post-baseline visits and ACR-N AUC.<br />
4. Physical function as assessed by the Modified Health Assessment Questionnaire (mHAQ) and the<br />
physical component summary scale of the Health Outcomes Questionnaire SF-36.<br />
5. SF-36 to assess quality of life.<br />
Tertiary Objective: Radiographic measurements of hands/wrists and feet (Genant modified Sharp score,<br />
joint space narrowing, erosion counts) at 6 months and 1 year.<br />
METHODOLOGY: Randomized, double-blind, placebo-controlled trial with parallel-dosing. The<br />
12-month teatment period was divided into 2 periods Days 1 to 180 and Days 181 to 360. During Days 1 to<br />
180, subjects were maintained on a stable dose of MTX (10-30 mg/wk). During Days 181 to 360,<br />
adjustments in corticosteroids (maximum 10 mg/day) and MTX (maximum 30 mg/wk) were permitted as<br />
was addition of either hydroxychloroquine, sulfasalazine, gold or azathioprine. No other changes in<br />
anti-rheumatic therapy were allowed. After completing the 12-month treatment period, subjects could have<br />
continued in a long-term extension. Results of the long-term extension will be reported separately.<br />
NUMBER OF SUBJECTS: 339 subjects were randomized, 115 to receive abatacept 10 mg/kg plus MTX,<br />
105 to receive abatacept 2 mg/kg plus MTX, and 119 to receive placebo plus MTX.<br />
DIAGNOSIS AND MAIN CRITERIA FOR INCLUSION/EXCLUSION: Adult subjects with active<br />
RA and inadequate response to MTX. Key inclusion/exclusion criteria: 1) Males or females ≥ 18 years of<br />
age; 2) Diagnosis of RA and RA functional classes I, II, or III; 3) Treated with MTX (10-30 mg/wk) for at<br />
least 6 months, at a stable dose for 28 days prior to Day 1; 4) Had the following criteria for disease activity<br />
at entry: ≥ 10 swollen joints (66 joint count), ≥ 12 tender joints (68 joint count), and a CRP level<br />
≥ 1.0 mg/mL.<br />
TEST PRODUCT, DOSE AND MODE OF ADMINISTRATION, BATCH NUMBERS: Abatacept<br />
(10 and 2 mg/kg) administered IV at Weeks 0, 2 and 4 and then once a month. Batch numbers were<br />
C00157, C00196, and C98283.<br />
REFERENCE THERAPY, DOSE AND MODE OF ADMINISTRATION, BATCH NUMBERS:<br />
Placebo administered IV at Weeks 0, 2 and 4 weeks and then once a month. Batch numbers for placebo<br />
were C98247, C00113 and C01236. All subjects received MTX (10-30 mg/wk), orally.<br />
3<br />
Approved v1.0 930006747 2.0
Abatacept<br />
BMS-188667<br />
CRITERIA FOR EVALUATION:<br />
IM101100<br />
<strong>Clinical</strong> Study Report<br />
Efficacy: The primary efficacy endpoint was the proportion of subjects meeting the ACR criteria for<br />
20% improvement (ACR 20) at 6 months (Day 180). Key secondary evaluations included 50%<br />
improvement (ACR 50) and 70% improvement (ACR 70). Other efficacy measurements included<br />
radiographic evaluation of joint damage progression and quality of life (SF-36).<br />
Safety: Adverse events (AEs), vital signs, clinical laboratory tests, including immunoglobulin levels (IgG,<br />
IgA, and IgM), and the presence of antibodies specific for abatacept (immunogenicity) were examined.<br />
Pharmacokinetics: Blood samples for PK analysis were collected prior to dosing from all subjects.<br />
Additional blood samples for a more complete PK profile were collected from subjects participating in a<br />
site-specific PK substudy. PK parameters for abatacept included: maximum observed serum concentration<br />
of (Cmax), time of occurrence of Cmax, area under the concentration time curve between Day 60 and<br />
Day 90 (AUC[TAU]), trough serum concentration (Cmin), total body clearance normalized to body weight<br />
(CLT), volume of distribution at steady-state normalized to body weight (VSS), and serum elimination<br />
half-life (T 1/2 ).<br />
Biomarker and Pharmacodynamics: Biomarker and PD outcome measures included CRP, sIL-2r, RF,<br />
sICAM-1, E-selectin, sIL-6, and TNFα.<br />
STATISTICAL METHODS: All statistical tests were carried out using a 5% level (two-tailed) of<br />
significance. If comparison of the ACR 20 response between the 10 mg/kg and placebo groups was<br />
significant, the comparison between the 2 mg/kg and placebo groups was to be carried out. This sequential<br />
procedure using the Chi-square test was also used to test for differences in ACR 50 and ACR 70 responses.<br />
All efficacy analyses used the intent-to-treat population (all subjects who received at least one dose of<br />
study medication). For the ACR analyses, subjects who discontinued the study due to lack of efficacy were<br />
considered ACR non-responders at all subsequent time points. Subjects who discontinued for other reasons,<br />
their last ACR response was carried forward. For analyses of the individual components of the<br />
ACR criteria, the last observation was carried forward (LOCF) for any subjects who discontinued from the<br />
study.<br />
SUBJECT POPULATION RESULTS: A greater proportion of subjects in the abatacept groups<br />
completed 360 days of treatment compared with the placebo group: 78% of those randomized to the<br />
10 mg/kg group, 71% randomized to the 2 mg/kg group and 60% randomized to the placebo group. Lack<br />
of efficacy and AEs were the most common reasons for discontinuation.<br />
Most subjects were white females, with a mean age of 55 years and a mean duration of RA of<br />
approximately 9 to 10 years.<br />
4<br />
Approved v1.0 930006747 2.0
Abatacept<br />
BMS-188667<br />
IM101100<br />
<strong>Clinical</strong> Study Report<br />
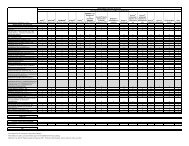
Baseline Characteristics<br />
Abatacept<br />
10 mg/kg<br />
+ MTX<br />
(n=115)<br />
Abatacept<br />
2 mg/kg<br />
+ MTX<br />
(n=105)<br />
Placebo<br />
+ MTX<br />
(n=119)<br />
Age (yrs), Mean (Range) 55.8 (17-83) 54.4 (23-80) 54.7 (23-80)<br />
Gender (% females) 75 63 66<br />
Race (% white) 87 87 87<br />
Duration of RA (yrs), Mean ± SD 9.7 ± 9.8 9.7 ± 8.1 8.9 ± 8.3<br />
Tender Joints (Mean ± SD) 30.8 ± 12.2 28.2 ± 12.0 29.2 ± 13.0<br />
Swollen Joints (Mean ± SD) 21.3 ± 8.4 20.2 ± 8.9 21.8 ± 8.8<br />
Physical Function (mHAQ 0-3), Mean ± SD 1.0 ± 0.5 1.0 ± 0.5 1.0 ± 0.6<br />
CRP (mg/dL), Mean ± SD 2.9 ± 2.8 3.2 ± 2.5 3.2 ± 3.2<br />
EFFICACY RESULTS:<br />
Signs and Symptoms<br />
• Primary efficacy variable: There was a statistically significant (p < 0.001) difference in ACR 20<br />
response at Day 180 for abatacept 10 mg/kg (plus MTX) compared to placebo (MTX alone). There<br />
was no statistically significant difference in ACR 20 responses at Day 180 between the 2 mg/kg group<br />
and the placebo group.<br />
• For abatacept 10 mg/kg, statistically significant differences from the placebo group were seen for ACR<br />
20, 50 and 70 at both Day 180 and Day 360. For 2 mg/kg, statistically significant differences from<br />
MTX alone were observed at Day 180 for ACR 50 and 70, but not at Day 360.<br />
ACR Response Rates: Percentage of Subjects Meeting Criteria<br />
Abatacept<br />
10 mg/kg<br />
+ MTX<br />
(N=115)<br />
Abatacept<br />
2 mg/kg<br />
+ MTX<br />
(N=105)<br />
Placebo<br />
+ MTX<br />
(N=119)<br />
Day 180<br />
ACR 20 60.9 a 41.9 35.3<br />
ACR 50 36.5 a 22.9 a 11.8<br />
ACR 70 16.5 a 10.5 a 1.7<br />
Day 360<br />
ACR 20 62.6 a 41.9 36.1<br />
ACR 50 41.7 a 22.9 20.2<br />
ACR 70 20.9 a 12.4 7.6<br />
ITT Population<br />
a Statistically significant difference for the comparison of abatacept vs. placebo (p < 0.05).<br />
5<br />
Approved v1.0 930006747 2.0
Abatacept<br />
BMS-188667<br />
IM101100<br />
<strong>Clinical</strong> Study Report<br />
• Significantly more subjects in the 10 mg/kg group compared with the placebo group achieved a Major<br />
<strong>Clinical</strong> Response (maintenance of an ACR 70 response over a continuous 6-month period) by<br />
Day 360 (7.8% vs 0.8%, p = 0.008).<br />
• There was rapid onset of action for subjects who received 10 mg/kg, that was demonstrable by<br />
approximately 15 days from the start of study medication (significant differences compared to the<br />
placebo group in subject reported measures of pain and disease activity). In the 10 mg/kg group<br />
compared with the placebo group, statistically significant improvements in ACR 50 and ACR 70<br />
responses were observed as early as Day 30 and for ACR 20 as early as Day 60.<br />
• Mean percentage improvements in each individual ACR component (tender and swollen joint counts,<br />
pain, subject global assessment, physician global assessment, CRP) at both Day 180 and Day 360 were<br />
significantly higher for the 10 mg/kg group relative to improvements for the placebo group.<br />
Physical Function:<br />
• Subjects treated with 10 mg/kg had improvements in physical function (mHAQ) at both Day 180 and<br />
Day 360 that were significantly (p < 0.05) higher relative to improvements for the placebo group.<br />
Health Outcomes:<br />
• <strong>Clinical</strong>ly and statistically significant (p < 0.05) improvement in all mental health and physical health<br />
domains of the SF-36 were observed in the 10 mg/kg group compared with the placebo group at<br />
Day 180 and Day 360.<br />
Structural Damage:<br />
• There was a trend for subjects treated with abatacept to demonstrate less progression of structural<br />
damage than subjects treated with placebo, as measured by the percent of subjects with evidence of<br />
radiographic progression.<br />
Biomarkers:<br />
• There was a dose related trend in the reduction of levels for most of the pro-inflammatory biomarkers<br />
(sIL-2r, sIL-6, RF, sICAM-1, TNF-α and E-selectin) on both Days 180 and 360.<br />
PHARMACOKINETIC RESULTS: The multiple-dose, steady-state, PK data indicate that both Cmax<br />
and AUC(TAU) values increased proportionally to the dose increment. T 1/2 , CLT, and VSS values appeared<br />
to be comparable and dose-independent. T 1/2 was approximately 13 days for both the 10 mg/kg and<br />
2 mg/kg groups. The small VSS value (0.07 L/kg for both dose level) suggests that abatacept is confined<br />
primarily to the vascular system and does not significantly distribute into extra-vascular spaces.<br />
Comparison of mean Cmin values at Days 60, 90, and 180 indicated that abatacept did not appear to<br />
accumulate following monthly dosing. The pharmacokinetic results for abatacept support once-a-month<br />
dosing.<br />
SAFETY RESULTS: The AE profile was generally similar among the 3 treatment groups.<br />
6<br />
Approved v1.0 930006747 2.0
Abatacept<br />
BMS-188667<br />
IM101100<br />
<strong>Clinical</strong> Study Report<br />
Overview of Adverse Events<br />
Abatacept<br />
10 mg/kg<br />
+ MTX<br />
(N=115)<br />
Number (%) of Subjects<br />
Abatacept<br />
2 mg/kg<br />
+ MTX<br />
(N=105)<br />
Placebo<br />
+ MTX<br />
(N=119)<br />
Deaths 0 1 (1.0) 0<br />
Serious Adverse Events 14 (12.2) 19 (18.1) 19 (16.0)<br />
Discontinuations due to Adverse Events 6 (5.2) 10 (9.5) 11 (9.2)<br />
Adverse Events 104 (90.4) 104 (99.0) 112 (94.1)<br />
Most Frequently (≥ 10% of Subjects in Any Group) Reported Adverse Events<br />
Rheumatoid Arthritis a 28 (24.3) 41 (39.0) 50 (42.0)<br />
Nasopharyngitis 17 (14.8) 19 (18.1) 11 (9.2)<br />
Headache 17 (14.8) 17 (16.2) 18 (15.1)<br />
Nausea 16 (13.9) 12 (11.4) 17 (14.3)<br />
Cough 15 (13.0) 10 (9.5) 15 (12.6)<br />
Diarrhea 13 (11.3) 10 (9.5) 9 (7.6)<br />
Upper Respiratory Tract Infection 13 (11.3) 10 (9.5) 9 (7.6)<br />
Dyspepsia 10 (8.7) 12 (11.4) 7 (5.9)<br />
Hypertension 8 (7.0) 12 (11.4) 8 (6.7)<br />
Fatigue 7 (6.1) 9 (8.6) 15 (12.6)<br />
Arthralgia 7 (6.1) 17 (16.2) 13 (10.9)<br />
All treated subjects<br />
MedDRA Version 6.1<br />
a The primary AE term “rheumatoid arthritis” included “worsening arthritis” and did not include other<br />
non-rheumatoid arthritis AEs.<br />
Additional safety results include:<br />
• The majority of AEs reported with abatacept and placebo were mild to moderate in intensity.<br />
• One subject (2 mg/kg) died due to complications following coronary artery bypass graft surgery<br />
(considered by the investigator to be unrelated to study drug). One additional death was reported prior<br />
to randomization.<br />
• There was no increase in the frequency of malignancy with abatacept compared with placebo (4 events<br />
in the 10 mg/kg group, 3 events in the placebo group).<br />
• Infections were generally mild, treatable when serious and few subjects discontinued due to an<br />
infection (1 subject in the 2 mg/kg group and 3 subjects in the placebo group).<br />
• Infections (mainly respiratory infections) were seen in a higher proportion of subjects in the abatacept<br />
groups (52-54%) than in the placebo group (44%). Serious infections were reported by 1% of subjects<br />
in the 10 mg/kg group and 3% of subjects each in the 2 mg/kg and placebo groups. No opportunistic<br />
infections were reported in the abatacept groups.<br />
7<br />
Approved v1.0 930006747 2.0
Abatacept<br />
BMS-188667<br />
IM101100<br />
<strong>Clinical</strong> Study Report<br />
• The overall frequencies of peri-infusional AEs (within 24 hours following dosing) were similar among<br />
the abatacept groups and the placebo group.<br />
• No safety issues emerged from the evaluation of laboratory data.<br />
• Abatacept was generally non-immunogenic. Two subjects (1%, one each from the 10 mg/kg and<br />
2 mg/kg groups) seroconverted for antibodies to CTLA.<br />
• No clinically significant decreases (below the normal range) in mean immunoglobulin levels were<br />
observed at Day 180 and Day 360 compared with baseline levels for both doses of abatacept.<br />
CONCLUSIONS: The following are the conclusions from the study:<br />
• The 10 mg/kg dose of abatacept was significantly more effective than placebo (on a background of<br />
MTX) in reducing signs and symptoms associated with RA, but the 2 mg/kg dose of abatacept was not.<br />
• The ACR 20 response rate at Day 180 (the primary efficacy variable) was significantly<br />
higher for the 10 mg/kg group compared with the placebo group (61% vs 35%, p < 0.001).<br />
• The ACR 20 response rate at Day 180 was higher for the 2 mg/kg group compared with the<br />
placebo group, however the difference was not statistically significant (42% vs 35%,<br />
p = 0.31).<br />
• When compared with the placebo group, the 10 mg/kg group had significant (p < 0.05) improvements<br />
in all measurements of physical function and quality of life.<br />
• Though not statistically significant, there was a trend for subjects treated with abatacept 10 mg/kg to<br />
demonstrate less progression of structural damage (using the pre-specified analysis) than the placebo<br />
group.<br />
• There was a dose related reduction in most of the pro-inflammatory biomarker levels (sIL-2r, RF,<br />
sICAM-1, E-selectin, IL-6).<br />
• The overall rates of AEs, SAEs and discontinuations due to AEs with abatacept were comparable with<br />
those for the placebo group.<br />
• No increase in the frequency of malignancies was reported with abatacept compared with<br />
placebo.<br />
• There was an increase in the rate of non-serious infections, mainly upper respiratory<br />
infections, in the abatacept groups compared with the placebo group (all infections: 52-54%<br />
vs 44%), but few were serious (1% in the 10 mg/kg group, 3% in the 2 mg/kg and placebo<br />
groups) or required discontinuation (0% in the 10 mg/kg group, 1% in the 2 mg/kg group,<br />
3% in the placebo group) with similar frequencies among the treatment groups. No<br />
opportunistic infections were reported in the abatacept groups.<br />
• Frequencies of peri-infusional AEs were similar among the abatacept groups and the placebo<br />
group.<br />
• Abatacept was generally non-immunogenic. Two subjects (1%) treated with abatacept seroconverted<br />
for antibodies to CTLA.<br />
• Both doses of abatacept (10 and 2 mg/kg) given for 1 year were well tolerated and had a safety profile<br />
similar to that of placebo.<br />
DATE OF REPORT: 15-Jun-2004<br />
8<br />
Approved v1.0 930006747 2.0