synopsis clinical study report - Clinical Trials - Bristol-Myers Squibb
synopsis clinical study report - Clinical Trials - Bristol-Myers Squibb
synopsis clinical study report - Clinical Trials - Bristol-Myers Squibb
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
Taxol®BMS-181339Name of Sponsor/Company:<strong>Bristol</strong>-<strong>Myers</strong> <strong>Squibb</strong>Name of Finished Product:Individual Study Table Referringto the DossierCA139-368<strong>Clinical</strong> Study Report(For National Authority UseOnly)Name of Active Ingredient:SYNOPSISCLINICAL STUDY REPORTTITLE OF STUDY: PHASE II STUDY OF CARBOPLATIN AND WEEKLY PACLITAXEL ASFIRST LINE TREATMENT OF ELDERLY PATIENTS WITH NON-SMALL CELL LUNG CANCERINVESTIGATORS: Prof. JL PUJOL, Hopital Arnaud de Villeneuve, Montpellier, France (coordinator)STUDY CENTERS: Eight <strong>study</strong> centers in FrancePUBLICATIONS:NoneSTUDY PERIOD: Date first subject enrolled: 20/02/2002Date last subject completed: 31/07/2003CLINICAL PHASE: IIOBJECTIVES:Primary objectives:- To evaluate the <strong>clinical</strong> activity of the combination of carboplatin (Paraplatine®) and weekly paclitaxel(Taxol®) given as first line chemotherapy in elderly patients with advanced or metastatic non-smallcell lung cancer (NSCLC) as measured by the tumor response rate.Secondary objectives:- To evaluate safety of the combination of Paraplatine® and weekly Taxol®.- To assess the response duration and time to progression- To evaluate the Quality of Life.METHODOLOGY:This is a Phase II, multi-center, non randomized, open-label <strong>study</strong> designed to evaluate the tumor responserate of the combination of Paraplatine® and weekly Taxol® given to elderly patients with NSCLC. Patientsdid not have received prior chemotherapy for advanced or metastatic NSCLC.2Approved v 1.0930027446
Taxol®BMS-181339CA139-368<strong>Clinical</strong> Study ReportA Simon optimal two-stage design was used to evaluate the objective tumor response rate in patientstreated with Taxol® in combination with Paraplatine®. This design required 19 response evaluable patientsfor the first stage. An interim analysis was performed at the end of the first stage: if there were 3 or fewerresponders, the <strong>study</strong> was to be terminated. Otherwise, an additional 25 response evaluable patients couldbe enrolled. This drug combination was considered of <strong>clinical</strong> interest if, at the end of the second stage,there were at least 11 responders out of the total of 44 response evaluable patients.NUMBER OF PATIENTS:Planned: 44 evaluable patients.Included: 51 patients, 44 evaluable.DIAGNOSIS AND MAIN CRITERIA FOR INCLUSION:Patients with stage IIIB or stage IV histologically or cytologically confirmed NSCLC who did not receiveprior chemotherapy for their advanced or metastatic disease including patients with local or metastaticfailure after surgery and/or radiotherapy. Patients were 70 years old with an ECOG performance status(PS) 2 and a life expectancy of at least 12 weeks. Patients had to have measurable disease. Adequaterecovery from recent surgery and radiation therapy, elapsed of at least one week from the time of a minorsurgery, and at least 3 weeks for major surgery or radiation therapy. Adequate hematologic, hepatic andrenal functions were to be established. Patients had to be accessible for treatment follow-up and had to givewritten informed consent.TEST PRODUCT, DOSE AND MODE OF ADMINISTRATION, BATCH NUMBERS:Taxol® was administered on Day 1, 8 and 15 of a 28-day cycle at a dose of 90 mg/m 2 and Paraplatine®was administered on Day 1 of each 28-day cycle at an AUC of 6 mg/mL.min.DURATION OF TREATMENT:Duration of treatment was based on tumor reassessments done every second cycle. Patients withprogressive disease were taken off <strong>study</strong>. Patients with stable disease (SD) or partial response (PR)received treatment until disease progression or a maximum of 6 cycles. Patients with SD or PR couldreceived additional treatment if it was in their best interest, and agreed to by both the Investigator and theSponsor. Patients who achieved a complete response (CR) received treatment for up to a maximum of4 cycles post CR. Treatment was also discontinued at any time if unacceptable toxicity occurred.REFERENCE THERAPY, DOSE AND MODE OF ADMINISTRATION BATCH NUMBERS:Not applicable.3Approved v 1.0930027446
Taxol®BMS-181339CRITERIA FOR EVALUATION:CA139-368<strong>Clinical</strong> Study ReportEfficacy:Efficacy analysis was performed on the ITT population for all parameters and on evaluable populations forthe objective response rate assessed by the investigator and reviewed by an expert panel using RECISTcriteria.The primary efficacy outcome was the response rate calculated on response evaluable patients according tothe experts and the investigator. Responses included CR and PR.The secondary efficacy outcomes were:Time to response, time to progression, duration of response and overall survival.Quality of life evaluated over time measured by the Lung Cancer Symptoms Scale (LCSS).Safety:Analysis of safety was performed on all patients who received at least one dose of <strong>study</strong> medications(Taxol®, Paraplatine® or both). Analysis of safety included the incidence of biological and <strong>clinical</strong> adverseevents (AEs) and serious adverse events (SAEs) using CTC grade scales.STATISTICAL METHODS:- A Simon optimal two-stage design was used to test whether the objective response rate was of <strong>clinical</strong>interest. A response rate in excess of 15% was considered of <strong>clinical</strong> interest. The Simon design tested thenull hypothesis that the true response rate was less or equal to 15% versus the alternative hypothesis thatit exceeds 15%. The type I error rate was 5% and the design had 90% power to reject the null hypothesiswhen the true response rate was 35%.- Descriptive statistics were used to analyze the efficacy and safety endpoints.- Ninety-five percent confidence intervals for objective response rate were computed and adjusted for thetwo-stage design.- Estimation of time to response, time to progression, duration of response and survival were plotted usingKaplan-Meier curves.4Approved v 1.0930027446
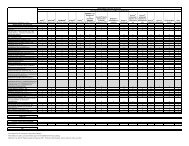
Taxol®BMS-181339CA139-368<strong>Clinical</strong> Study ReportEFFICACY RESULTS:- In the evaluable population (N=44), according to the investigator’s assessment there were 1 CR and 20PR leading to an objective tumor response rate of 48% [33 – 62]. According to the expert panelassessment, there were 1 CR and 21 PR i.e. a <strong>clinical</strong> objective rate of 50% [30 – 57].- Time to response, time to progression, duration of response and overall survival according to theinvestigators assessment are presented in the table below. Similar results were found with the expert panelassessment.Secondary efficacy outcome – Investigator’s assessment (median time with [95% CI])ITT population(N = 51 )Time to response (months) 1.84 [1.81 – 2.00]Time to progression (months) 7.49 [6.21 -9.43]Duration of response (months) 7.98 [6.60 – 9.43]Overall survival (months) 13.63 [7.49 – 17.05]Relative survival (months) 18.11 -- Quality of Life: no change over time in the total score of the LCSS was evidenced in this <strong>study</strong>.SAFETY RESULTS:- 761 AEs were <strong>report</strong>ed during the <strong>study</strong>. Overall, 61% of these AEs were considered by the investigatoras related to the <strong>study</strong> treatment. Most AEs were gastrointestinal disorders, mainly nausea experienced in41% of patients, constipation (31%), vomiting (27%), and diarrhea (22%). Paresthesia/peripheral sensoryneuropathy was experienced by 35% of patients. Other very frequently <strong>report</strong>ed AEs were fatigue (65%of patients) and alopecia (57%). The most frequent Grade 3-4 toxicities are presented in the Table below:Grade 3-4 adverse events and hematotoxicity of grade 3 and grade 4<strong>report</strong>ed in at least 2 patientsSafety Set (N = 51)Grade 3 Grade 4Adverse eventsFatigue 7 (14%) 1 (2%)Dyspnea 6 (12%) 1 (2%)Anorexia 2 (4%) 1 (2%)Neuropathy* 2 (2%) 1 (2%)Constipation 2 (4%) -HematotoxicityHemoglobin 9 (18%) -White blood cells 14 (27%) 1 (2%)Neutrophils 12 (24%) 8 (16%)Platelets 3 (6%) 1 (2%)* neuropathy Nos, peripheral neuropathy Nos,peripheral sensory neuropathy or paresthesia,5Approved v 1.0930027446
Taxol®BMS-181339CA139-368<strong>Clinical</strong> Study Report- 9 patients (27%) terminated the <strong>study</strong> prematurely because of progressive disease, 11 patients (33%) werewithdrawn from the trial for toxicity (including 3 patients for hematological toxicity and 4 patients forneuropathy).- 30 deaths were recorded during the <strong>study</strong>. Among them, 4 patients died for an other reason than diseaseprogression: 2 cases of cerebral stroke, 1 pulmonary embolism, and 1 bronchial infection withoutneutropenia). None of these events were considered by the investigator as related to the <strong>study</strong> drugs.- 50 SAEs were experienced by 23 (45%) patients. Seven patients (13.7%) experienced a serious adverseevent considered as treatment-related by the investigator.- Hematological toxicity was frequent: 20 patients experienced neutropenia of grade 3 (12 patients) andgrade 4 (8 patients). Thrombocytopenia of grade 3 and grade 4 was experienced in 3 (6%) and 1 (2%)patients, respectively. Nine patients (18%) also <strong>report</strong>ed severe anemia of grade 3.CONCLUSIONS:In conclusion, with 22 objective responses according to the expert’s assessment, the objective of the <strong>study</strong>was achieved which allowed to conclude to the strong <strong>clinical</strong> interest of the combination of Taxol® (90mg/m 2 on day 1, 8 and 15 of 28-day cycle) and Paraplatine® (AUC of 6 on day 1 of 28-day cycle) in firstline therapy of advanced or metastatic NSCLC in the elderly. The good Safety profile strengthened the<strong>clinical</strong> interest of the Taxol/Paraplatin combination.DATE OF REPORT: 21 November 20056Approved v 1.0930027446