2007 Cancer Annual Report - St.Joseph's Hospital
2007 Cancer Annual Report - St.Joseph's Hospital
2007 Cancer Annual Report - St.Joseph's Hospital
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
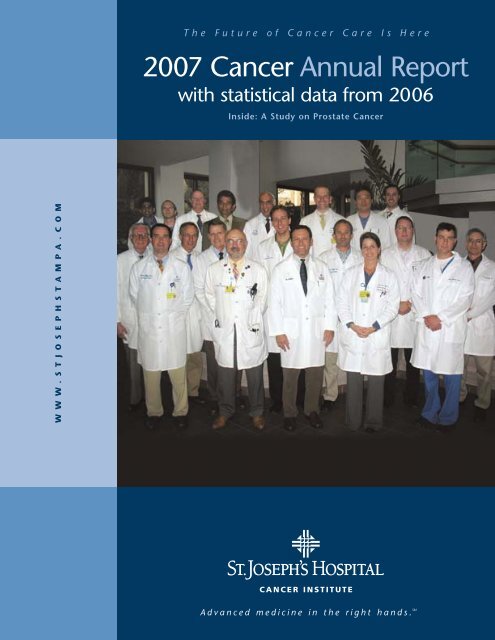
The Future of <strong>Cancer</strong> Care Is<br />
<strong>2007</strong> <strong>Cancer</strong> <strong>Annual</strong> <strong>Report</strong><br />
with statistical data from 2006<br />
Inside: A <strong>St</strong>udy on Prostate <strong>Cancer</strong><br />
Here<br />
W W W . S T J O S E P H S T A M P A . C O M<br />
CANCER INSTITUTE<br />
Advanced medicine in the right hands. SM
<strong>Cancer</strong> Committee<br />
2006-<strong>2007</strong> Members<br />
Anthony Brannan, M.D.<br />
<strong>Cancer</strong> Committee Chairman<br />
ACoS Liaison<br />
General Surgeon<br />
Manjul Derasari, M.D.<br />
Pain Management<br />
Christopher George, M.D.<br />
<strong>Cancer</strong> Conference Coordinator<br />
Medical Oncology<br />
Giselle Ghurani, M.D.<br />
GYN Oncology<br />
Gabriel Gonzales-Portillo, M.D.<br />
Neurosurgery<br />
David Hochberg, M.D.<br />
Urology<br />
Brian Jeffrey, M.D.<br />
Pathology<br />
<strong>St</strong>ephen Kennedy, M.D.<br />
Radiology<br />
Alex Mirakian, M.D.<br />
Radiation Oncology<br />
Joseph Sinkovics, M.D.<br />
Medical Oncology<br />
Cameron Tebbi, M.D.<br />
Pediatric Oncology<br />
Waide Weaver, M.D.<br />
Medical Oncology/Hematology<br />
Cheri Andrews, R.N.<br />
OCN Clinical Inpatient<br />
Holly Anglen<br />
Marketing<br />
Susan Baker, R.N.<br />
Nurse Navigator<br />
Delphine Ballard<br />
Rehabilitation<br />
Christina Bastone<br />
Business Development<br />
Moira Boyd<br />
Social Services<br />
Ronda Buffington, R.N.<br />
OCN <strong>Cancer</strong> Helpline<br />
Brian Cupari<br />
Marketing<br />
George Francis<br />
Chaplain<br />
Merrianne Furlong<br />
Women’s Health<br />
Kimberly Guy, COO<br />
SJWH (ex-officio)<br />
Kristal Hollingsworth<br />
Lymphedema Program<br />
Whitney Lisica<br />
Lymphedema Program<br />
Lorraine Lutton, COO<br />
SJH (ex-officio)<br />
Dawn MacCartney, R.N.<br />
SJCH<br />
Deanna Macon<br />
Medical Records<br />
Jan Marshburn<br />
Moffitt<br />
Jody Meguiar<br />
Medical <strong>St</strong>aff Services<br />
Susan Mills, R.N.<br />
Radiation Therapy<br />
Nancy Nethery<br />
ACS Patient Service Representative<br />
Susan Pearce, R.N.<br />
Quality Outcome<br />
Kim Perez, Pharm D.<br />
CI Pharmacy<br />
Janet Pindral<br />
Breast Center<br />
Martha Priede<br />
Medical <strong>St</strong>aff Services<br />
Mary Pritchard, R.N.<br />
Research/Infusion Center<br />
Julieann Ramsey<br />
CI Administration<br />
Fran Rinchuse, RD<br />
Nutrition<br />
Sharon Shoyer<br />
SJCH Patient Services<br />
Carol Silver<br />
Social Services<br />
John Surprenant<br />
CI Administrative Director<br />
Michele Tison<br />
Lymphedema Program<br />
Laurie Winkles<br />
Marketing<br />
Christina Wirebjer<br />
Lymphedema Program<br />
Victoria Young<br />
CTR <strong>Cancer</strong> Registry
Table of Contents<br />
<strong>Cancer</strong> Committee Chairman’s <strong>Report</strong> ..............................................................................4<br />
What We Know About Prostate <strong>Cancer</strong> ............................................................................5<br />
Prostate <strong>Cancer</strong> at <strong>St</strong>. Joseph’s <strong>Hospital</strong> (PCE <strong>St</strong>udy) ........................................................6<br />
PCE <strong>St</strong>udy Charts and Graphs ..........................................................................................8<br />
<strong>Cancer</strong> Registry Data Summary ......................................................................................10<br />
Primary Site Tabulation for Cases in 2006 ......................................................................11<br />
<strong>Cancer</strong> Registry <strong>Report</strong>....................................................................................................13<br />
<strong>Cancer</strong> Liaison Physician <strong>Report</strong> ....................................................................................13<br />
<strong>Cancer</strong>-Related Programs and Services ............................................................................14<br />
<strong>Cancer</strong> Patient Support Services......................................................................................15<br />
2006-<strong>2007</strong> <strong>Cancer</strong> Program Highlights ..........................................................................16<br />
<strong>Cancer</strong> Research ..............................................................................................................17<br />
<strong>Cancer</strong> Program Leaders..................................................................................................18<br />
Important Phone Numbers..............................................................................................18<br />
Index of Physicians Associated with <strong>Cancer</strong> Program......................................................19<br />
Affiliated with…<br />
H. Lee Moffitt <strong>Cancer</strong> Center & Research Institute<br />
In Partnership with…<br />
American <strong>Cancer</strong> Society – Formal <strong>Hospital</strong> Partnership<br />
Axis Palliative Care, LLC – a subsidiary of LifePath Hospice<br />
Florida Dialogue on <strong>Cancer</strong> – Group working to set cancer priorities in Florida<br />
CureSearch – Unites childhood cancer research organizations to promote research:<br />
Children’s Oncology Group and National Childhood <strong>Cancer</strong> Foundation<br />
Radiation Therapy Oncology Group
<strong>Cancer</strong> Committee<br />
Chairman’s <strong>Report</strong><br />
The <strong>Cancer</strong> Committee of <strong>St</strong>. Joseph’s <strong>Hospital</strong> is pleased to submit our <strong>2007</strong> <strong>Annual</strong> <strong>Report</strong>, which outlines the activities and<br />
accomplishments of our cancer program for the year and provides the statistical information of the cancer patients served at our facility<br />
during 2006.<br />
<strong>St</strong>atistics indicate that clinical outcomes among patients treated at <strong>St</strong>. Joseph’s <strong>Hospital</strong> compare favorably when measured against<br />
benchmark data retrievable from national repositories. This year’s annual report reviews and updates <strong>St</strong>. Joseph’s <strong>Hospital</strong>’s experience<br />
with prostate cancer from 2000 to 2006. <strong>St</strong>. Joseph’s <strong>Hospital</strong> survival rate from prostate cancer is equal to the state and national<br />
survival rates. There has been a steady rise in the use of robotic prostatectomy over the last four years at <strong>St</strong>. Joseph’s <strong>Hospital</strong> reflecting<br />
the increased availability and expertise in the area.<br />
The journey of having a cancer diagnosis and treatment is never a pleasant one. There are physical, psychological and emotional<br />
challenges. We have tried to evaluate and quantify the issue of the patients’ experience at <strong>St</strong>. Joseph’s <strong>Hospital</strong> <strong>Cancer</strong> Institute. Patient<br />
satisfaction surveys for both our inpatient and outpatient cancer care have scored among the highest in the hospital. This is truly a<br />
tribute to the outstanding physicians, nurses and ancillary staff who are dedicated to providing exceptional and compassionate care.<br />
The guiding principles of our cancer program are: the patient comes first, work is a unified effort and excellence is expected in all we<br />
do. Success is a cooperative effort and is dependent upon everyone involved in the care of cancer patients.<br />
This past year has been a very successful year for our <strong>Cancer</strong> Program. Below are just a few highlights of what has been accomplished.<br />
<strong>St</strong>. Joseph’s <strong>Hospital</strong> formally entered into an affiliation relationship with the H. Lee Moffitt <strong>Cancer</strong> Center & Research Institute,<br />
Florida’s only National <strong>Cancer</strong> Institute (NCI) designated center. This relationship allows both <strong>St</strong>. Joseph’s <strong>Hospital</strong> and the Moffitt<br />
<strong>Cancer</strong> Center to do what they do best: <strong>St</strong>. Joseph’s <strong>Hospital</strong> to provide primary care and Moffitt <strong>Cancer</strong> Center to conduct research.<br />
<strong>St</strong>. Joseph’s <strong>Hospital</strong> led the way in the region by formally entering into a partnership with the American <strong>Cancer</strong> Society. Through this<br />
partnership, <strong>St</strong>. Joseph’s <strong>Hospital</strong> has made a commitment to inform cancer patients of the extended resources available through the<br />
American <strong>Cancer</strong> Society, as well as other community resources, and to actively promote cancer screening and education. Of special<br />
note, is the selection of <strong>St</strong>. Joseph’s <strong>Hospital</strong> to be recognized by the American <strong>Cancer</strong> Society for its innovative and expanded Reach to<br />
Recovery Breast Program, and for being chosen by the Florida division of the American <strong>Cancer</strong> Society to be a pilot site for the national<br />
program called Clinician’s Portal. This unique program affords newly diagnosed patients access to timely and customized education,<br />
services and programs.<br />
A dedicated nurse navigator was hired to assist newly diagnosed breast cancer patients at The Breast Center at <strong>St</strong>. Joseph’s Women’s<br />
<strong>Hospital</strong>. Various quality initiatives and studies were undertaken to ensure the highest level of care for our patients. Our outreach and<br />
screening programs provided 54 support group meetings with almost 800 patients in attendance; six community educational seminars<br />
on various topics; two region-wide colorectal cancer awareness screening campaigns along with CVS Pharmacies and WFTS – ABC 28 in<br />
which more than 95,000 free screening kits were distributed. The <strong>Cancer</strong> Institute has held numerous special events including A Special<br />
<strong>Cancer</strong> Survivors Day Celebration, A Woman’s Journey Through <strong>Cancer</strong> art exhibition in conjunction with Lilly Pharmaceutical and an<br />
Oncology Nursing Society nurses review course.<br />
The <strong>Cancer</strong> Program sponsored weekly tumor conferences and held three Grand Rounds presentations on topics important to our<br />
professional staff.<br />
Each year as we reflect on the accomplishments of our cancer professionals, we again want to express appreciation for the enthusiasm<br />
and generosity they bring to their work. With their leadership and support, we are confident in our ability to fulfill our mission to<br />
provide the best cancer services available in our community.<br />
4<br />
Anthony N. Brannan, M.D.<br />
<strong>Cancer</strong> Committee Chairman<br />
<strong>Cancer</strong> Liaison Physician
What We Know About Prostate <strong>Cancer</strong><br />
Prostate cancer is the most common type of cancer among men and is the<br />
second leading cause of cancer death. It is estimated by the American<br />
<strong>Cancer</strong> Society that in <strong>2007</strong>, there will be 218,890 new cases of prostate<br />
cancer in the United <strong>St</strong>ates and 27,050 men, or one in 34, will die from<br />
this disease. The good news is that death rates for prostate cancers are<br />
decreasing and the disease is being detected earlier.<br />
According to the American <strong>Cancer</strong> Society, the chance of a man having<br />
prostate cancer is one in six. The chance increases as a man gets older;<br />
approximately two of every three prostate cancers are found in men over<br />
the age of 65. <strong>St</strong>udies suggest that men with close family members<br />
(father, brother, son) who have had prostate cancer are more likely to get<br />
it themselves. Their risk becomes greater if their family member<br />
contracted cancer at an early age. For African-American men, prostate<br />
cancer incidence rates are the highest in the world.<br />
Although we know some of the risk factors linked to prostate cancer, we<br />
do not know what causes most cases. <strong>Cancer</strong>s have different risk factors.<br />
Some risk factors, such as smoking, can be controlled. Others, like a<br />
person’s age or family history, cannot be changed. But having a risk factor,<br />
or even several, does not mean that a person will get prostate cancer.<br />
Doctors can often find prostate cancer early by testing the amount of<br />
prostate-specific antigen (PSA) in the patient’s blood. They can also find it<br />
early by performing a digital rectal exam (DRE). The American <strong>Cancer</strong><br />
Society believes that doctors should offer the PSA blood test and a DRE<br />
yearly, beginning at age 50, to men who do not have any major medical<br />
problems. Men at high risk should begin testing at age 45 and include<br />
African-Americans and those with a close relative who had prostate cancer<br />
before age 65.<br />
Patients should discuss options for the best management of their prostate<br />
cancer with their physicians, since more than one treatment option may be<br />
available. The best treatment depends on a number of factors that take into<br />
account the patient’s age, overall health, the stage and grade of cancer, and<br />
the patient’s treatment preferences. Surgery, radiation therapy and hormone<br />
therapy are the most common treatments for prostate cancer.<br />
Chemotherapy may be used in some cases, and for those not on an active<br />
form of treatment, watchful waiting may be an option for some men.<br />
Robotic prostatectomy is the most advanced surgical option for qualifying<br />
prostate cancer patients. The benefits for patients who undergo this<br />
minimally invasive and nerve-sparing surgery include faster recovery times,<br />
less blood loss, less pain and shorter hospital stays.<br />
Men treated for prostate cancer today have a more favorable outlook. In fact,<br />
99 percent of men diagnosed with this disease survive at least five years. In<br />
addition, 90 percent of all prostate cancers are found while they are still<br />
within the prostate or have spread only to nearby areas. The five-year relative<br />
survival rate for these men is nearly 100 percent; clearly revealing the<br />
importance of early detection. Older men who follow a recommended testing<br />
schedule and have regular clinical exams maximize their chances for<br />
detecting and recovering from cancer and other prostate conditions. As with<br />
most types of cancer, the earlier the tumor is discovered, the better the<br />
patient’s chances for survival. Tumors discovered at an early stage often<br />
respond well to treatment. Treatment options vary depending on many<br />
patient factors and should be discussed with a physician.<br />
Prostate Facts at a Glance<br />
• Prostate cancer is the most common type of cancer found in American<br />
men, other than skin cancer.<br />
• Prostate cancer is the second leading cause of cancer death in men.<br />
• The American <strong>Cancer</strong> Society estimates that there will be about 218,890<br />
new cases of prostate cancer in the United <strong>St</strong>ates in <strong>2007</strong>. About 27,050<br />
men will die of this disease.<br />
• While one man in six will get prostate cancer during his lifetime, only<br />
one man in 34 will die of this disease.<br />
• African-American men are more likely to have prostate cancer and have a<br />
higher mortality rate than Caucasian or Asian men. The reasons for this<br />
are still unknown.<br />
• Although men of any age can get prostate cancer, it is found most often<br />
in men over 50.<br />
5
Prostate <strong>Cancer</strong> at <strong>St</strong>. Joseph’s <strong>Hospital</strong><br />
2002-2006 Patient Care <strong>St</strong>udy • PCE <strong>St</strong>udy<br />
6<br />
Dr. George<br />
Dr. Hochberg<br />
Dr. Mastandrea<br />
Dr. Mirakian<br />
The cancer program at <strong>St</strong>. Joseph’s <strong>Hospital</strong> last reviewed<br />
prostate cancer in 1999. This study will review and update<br />
the experience with prostate cancer from 2000-2006.<br />
Prostate cancer is the most common non-skin cancer<br />
diagnosed in males in the United <strong>St</strong>ates. The annual<br />
incidence is estimated to be approximately 218,000 new<br />
cases in the United <strong>St</strong>ates in <strong>2007</strong>. Approximately one<br />
man in six will develop prostate cancer in his lifetime,<br />
making the incidence comparable to the incidence of<br />
breast cancer in women. Roughly 27,000 patients are<br />
expected to die of prostate cancer in the year <strong>2007</strong>. This<br />
number has decreased approximately 2% per year,<br />
1995-2001. This decline in the death rate may be due to<br />
detection of lower risk disease, increased public awareness<br />
and early detection.<br />
Prostate cancer has an incredible heterogeneity of<br />
behavior. Some men will present with low-grade disease<br />
at an elderly age, with little impact on either the length or<br />
quality of life. Younger men with high-grade disease will<br />
likely have a significantly shortened survival rate. Thus,<br />
the identification and aggressive management of high risk<br />
patients becomes of paramount importance. The biologic<br />
heterogeneity of prostate cancer has led to considerable<br />
controversy in the management of diagnosis and<br />
treatment of prostate cancer. The development of prostatespecific<br />
antigen (PSA) in the late 1980s as a screening and<br />
management tool has led to earlier diagnosis of prostate<br />
cancer. As a result, most patients are now diagnosed with<br />
clinically localized disease. The decision process for<br />
treatment will need to include a number of factors<br />
including Gleason score, age, life expectancy, PSA level,<br />
stage, co-morbidities, and finally patient preference.<br />
Robotic Surgery at <strong>St</strong>. Joseph’s <strong>Hospital</strong><br />
An evolutionary step in prostate cancer treatment has<br />
occurred. With the advent of robotic-assisted laparoscopic<br />
prostatectomy, the surgical treatment of prostate cancer<br />
has changed. Robotic surgery offers a lower risk of<br />
bleeding, incontinence, and improved potency post<br />
procedure, as well as a more rapid recovery for the<br />
patient. This has made robotic surgery the modality of<br />
choice for many patients. <strong>St</strong>. Joseph’s <strong>Hospital</strong> has seen<br />
this change occur due to the foresight of this institution in<br />
being one of the first hospitals in Florida to acquire and<br />
use the da Vinci ® Surgical System. Because of this<br />
foresight, more men in our community are choosing<br />
robotic surgery as their treatment of choice for prostate<br />
cancer. <strong>St</strong>. Joseph’s <strong>Hospital</strong> has become a Center of<br />
Excellence for robotic surgery. <strong>St</strong>. Joseph’s <strong>Hospital</strong> was<br />
the first in the state to purchase and use the da Vinci<br />
system. Because of this, we have acted as a training<br />
center for most of the sites in the state.<br />
The da Vinci robotic surgery system was created to take<br />
laparoscopic surgery to the next level. Using laparoscopic<br />
ports, tubes which permit thin instruments to enter the<br />
body, allowing the performance of more complex<br />
surgeries. The standard laparoscopic instruments do not<br />
allow the surgeon to suture and dissect tissue easily. These<br />
instruments are straight and rigid and seem like<br />
chopsticks. The robotic instruments are thin and straight,<br />
but the ends move like the human hand. This turns the<br />
surgeon’s hands into two seven-millimeter instruments.<br />
This, coupled with the binocular vision, which allows for<br />
depth perception and 10 times magnification of the scope,<br />
gives the surgeon the ability to perform an operation<br />
better than by human hand. We can now do complex<br />
procedures in very small spaces in the body and do them<br />
with superior vision.<br />
Because of these improvements, patients who have robotic<br />
radical prostatectomies need blood transfusions less than<br />
one percent of the time. Compared with open surgery,<br />
this is a great improvement. Also, the incontinence rate<br />
with robotic surgery is much less than with open surgery<br />
and can approach as low as one percent.<br />
Most men with prostate cancer are concerned about<br />
potency after treatment. With robotic surgery and the<br />
more precise dissection of the neurovascular bundle (the<br />
nerves that give a man an erection), most men having this<br />
surgery can be potent afterwards. What men appreciate<br />
most after having robotic surgery is the decreased level of<br />
pain and the rapid return to normal activities.<br />
Rather than spending several days in the hospital and<br />
months afterwards recovering as with open surgery patients,<br />
robotic surgery patients can go home the day after their<br />
surgery and be back to normal activities within two weeks.<br />
<strong>St</strong>. Joseph’s <strong>Hospital</strong> is excited to be at the forefront of this<br />
technology, and we are proud to provide this level of care to<br />
our community.
<strong>St</strong>atus of Radiation Therapy at <strong>St</strong>. Joseph’s <strong>Hospital</strong><br />
During the study period 2000-2006, treatment options for prostate cancer<br />
with radiation therapy have undergone numerous developments providing a<br />
drive for change. While radiation therapy has advanced on the technological<br />
front, there has also been the introduction of other competing modalities for<br />
local treatment in the same time period. These include cryosurgical ablation,<br />
laparoscopic prostatectomy and robotic laparoscopic prostatectomy. Data has<br />
also emerged regarding systemic management for intermediate to high risk<br />
patient groups with hormonal therapy and more recently, different<br />
chemotherapeutic combinations.<br />
Previous treatment modalities such as external beam radiotherapy and seed<br />
implantation (a form of low dose rate brachytherapy) have continued as<br />
the main forms of radiation treatment over the past 15 years at <strong>St</strong>. Joseph’s<br />
<strong>Hospital</strong>. Newer techniques including the evolution of image guided<br />
radiation therapy (IGRT) have been developed to provide target<br />
identification, enhance treatment delivery and monitor accuracy. All of<br />
these contribute to improvement of the therapeutic rations, allowing gains<br />
in outcome while continuing to minimize toxicity.<br />
Intensity modulated radiation therapy (IMRT), an advanced form of<br />
external beam radiation therapy that has been in use over the study<br />
period at <strong>St</strong>. Joseph’s <strong>Hospital</strong>, has facilitated more conformal targeting<br />
and allowed dose escalation to the prostate and surrounding tissues while<br />
minimizing excessive dose to surrounding critical structures such as the<br />
rectum and bladder. This has been of particular importance as studies<br />
have shown that delivering a higher dose to the prostate equates to better<br />
long term control of the cancer as measured by blood levels of prostatespecific<br />
antigen (PSA).<br />
Over the past two to three years, the development and implementation of<br />
IGRT as the latest technological advance has allowed more confidence in<br />
knowing that the delivered dose is actually hitting the target. With this<br />
technology, the position of the prostate is evaluated on a daily basis using<br />
pretreatment implanted marker seeds. Small adjustments are made prior to<br />
each treatment to ensure precise targeting of the gland. <strong>St</strong>. Joseph’s <strong>Hospital</strong><br />
will soon be evaluating this as the next step forward in the technology race.<br />
Low dose rate brachytherapy or prostate seed implantation has continued<br />
as an alternative form of local treatment at <strong>St</strong>. Joseph’s <strong>Hospital</strong>, either<br />
alone as monotherapy or in combination with a shorter course of external<br />
beam radiotherapy, usually as IMRT treatment in recent years with<br />
excellent results. Updated data has recently been published on the Seattle<br />
experience, which is the longest worldwide, indicating that after 15 years’<br />
follow-up, their patients are still showing excellent control rates for low<br />
and intermediate risk groups who have previously had this treatment. High<br />
dose rate brachytherapy (HDR), whereby a single radiation seed is used to<br />
deliver the radiation directly into the prostate through hollow catheters<br />
placed within the gland, is also becoming popularized especially due to a<br />
lower rate of side effects.<br />
Overall, <strong>St</strong>. Joseph’s <strong>Hospital</strong> is proud to be able to offer the latest in<br />
technology in combination with excellent care and compassion to its<br />
cancer patients. It is clearly the community leader in all aspects of prostate<br />
cancer treatment that it provides evidenced by this latest report of<br />
treatment results over the past five years. <strong>St</strong>. Joseph’s <strong>Hospital</strong> will continue<br />
to make available to the community the latest in evolving treatments to<br />
ensure the best possible care of its present and future patients.<br />
The predominant management options for initial therapy of early stage disease<br />
include expectant management, radical prostatectomy and radiotherapy.<br />
Recent studies have verified the importance of using age, life expectancy,<br />
Gleason score and stage in predicting the risk of biochemical failure after local<br />
therapy. Using life table analysis, as well as risk nomograms, one can estimate<br />
the risk of post treatment failure. <strong>Cancer</strong>s can then be categorized as low,<br />
intermediate and high risk cancers. Appropriate treatment selection will<br />
include not only the chance for cure, but also an assessment of co-morbid<br />
illness, side effects of treatment and finally, patient preference.<br />
<strong>St</strong>. Joseph’s <strong>Hospital</strong> Prostate <strong>St</strong>udy: 2000-2006<br />
During the period of the study, 1,373 patients were seen and treated at<br />
<strong>St</strong>. Joseph’s <strong>Hospital</strong>, with an average of 200 patients per year. This<br />
represents a slight increase over the previous study period (approximately<br />
160/year), but has been fairly stable over the last seven years (Table 1).<br />
Table 1:<br />
<strong>St</strong>age of Prostate <strong>Cancer</strong> – SJH<br />
YEAR STAGE STAGE STAGE STAGE UNK ALL TOTAL<br />
I II III IV OTHERS<br />
Number Number Number Number Number Number Number<br />
2000 1 189 9 7 2 0 208<br />
2001 2 176 4 7 2 1 192<br />
2002 2 175 12 7 1 3 200<br />
2003 1 151 12 7 0 14 185<br />
2004 0 146 19 9 7 1 182<br />
2005 0 169 17 11 0 4 201<br />
2006 0 176 14 7 3 5 205<br />
OTHERS 0 0 0 0 0 0 0<br />
TOTAL 6 1,182 87 55 15 28 1,373<br />
Source: SJH <strong>Cancer</strong> Registry Database • Retrieved on July 21, <strong>2007</strong><br />
Table 2:<br />
Race of Prostate <strong>Cancer</strong> Patients – SJH<br />
SJH NON- SPANISH, S. OR CENT. UNK TOTAL<br />
RACE SPANISH HISPANIC AMERICAN<br />
OR LATINO (w/o Brazil)<br />
Number Number Number Number Number<br />
WHITE 952 186 10 3 1,151<br />
BLACK 205 2 2 0 209<br />
FILIPINO 2 0 0 0 2<br />
ASIAN, INDIAN,<br />
PAKISTANI 3 0 0 0 3<br />
VIETNAMESE 1 0 0 0 1<br />
OTHER 0 1 0 1 2<br />
UNKNOWN 4 1 0 0 5<br />
ANY OTHERS 0 0 0 0 0<br />
TOTAL 1,167 190 12 4 1,373<br />
Source: SJH <strong>Cancer</strong> Registry Database • Retrieved on July 21, <strong>2007</strong><br />
7
Figure 1: <strong>St</strong>age of Prostate <strong>Cancer</strong> Diagnosed in 2004<br />
Florida vs. National<br />
5%<br />
6%<br />
8%<br />
1%<br />
10%<br />
5%<br />
8%<br />
1%<br />
<strong>St</strong>age I<br />
<strong>St</strong>age II<br />
<strong>St</strong>age III<br />
<strong>St</strong>age IV<br />
Unknown<br />
Figure 4b:<br />
Surgery – Florida vs. National<br />
None<br />
Local tumor destruction, NOS<br />
Local tumor excision, NOS<br />
Subtotal, segmental, or simple prostatectomy<br />
Radical prostatectomy, NOS; total prostatectomy, NOS<br />
.7%<br />
.8%<br />
.3%<br />
Prostatectomy WITH resection<br />
Prostatectomy, NOS<br />
Surgery, NOS<br />
Unknown if surgery performed<br />
.7% .4%<br />
.5% .4%<br />
81%<br />
76%<br />
34%<br />
55%<br />
37%<br />
53%<br />
Figure 2: Race of Prostate <strong>Cancer</strong> Patient Diagnosed in 2004<br />
Florida vs. National<br />
13%<br />
Florida<br />
Data from 7,627 patients<br />
.1%<br />
12%<br />
1%<br />
2%<br />
73%<br />
Florida<br />
Data from 7,627 patients<br />
National<br />
Data from 117,366 patients<br />
Source: NCDB, CoC, ACoS • Benchmark <strong>Report</strong>s, v8.0 - July 22, <strong>2007</strong><br />
.2%<br />
4%<br />
14%<br />
2%<br />
77%<br />
3%<br />
National<br />
Data from 117,366 patients<br />
Source: NCDB, CoC, ACoS • Benchmark <strong>Report</strong>s, v8.0 - July 22, <strong>2007</strong><br />
White<br />
Black<br />
Hispanic<br />
Native American<br />
Asian<br />
Other/Unknown<br />
11%<br />
.1%<br />
.1%<br />
5%<br />
4%<br />
Florida<br />
Data from 67 hospitals<br />
51%<br />
.3%<br />
5%<br />
Surgery only<br />
Radiation only<br />
Radiation & hormone therapy<br />
Surgery & hormone therapy<br />
2%<br />
National<br />
Data from 1,317 hospitals<br />
Source: NCDB, CoC, ACoS • Benchmark <strong>Report</strong>s, v8.0 - July 22, <strong>2007</strong><br />
Figure 5:<br />
Hormone therapy only<br />
Other specified therapy<br />
No first course Rx<br />
3% 3% 4%<br />
3%<br />
8% 4% 9%<br />
6%<br />
3% 4%<br />
3%<br />
5%<br />
21%<br />
Treatment Comparison<br />
17%<br />
SJH Florida National<br />
Data from 1,373 patients Data from 7,627 patients Data from 117,366 patients<br />
39%<br />
17%<br />
26% 23%<br />
Source: SJH <strong>Cancer</strong> Registry Database • Retrieved on July 21, <strong>2007</strong><br />
41%<br />
Figure 3: Age of Prostate <strong>Cancer</strong> Patient Diagnosed in 2004<br />
Florida vs. National<br />
2,448<br />
37<br />
4 207<br />
604<br />
1,416<br />
2911<br />
Florida<br />
Data from 7,627 patients<br />
34,577<br />
575<br />
7<br />
9,297<br />
3,218<br />
53<br />
25,133<br />
44,506<br />
National<br />
Data from 117,366 patients<br />
Source: NCDB, CoC, ACoS • Benchmark <strong>Report</strong>s, v8.0 - July 22, <strong>2007</strong><br />
16-29<br />
30-39<br />
40-49<br />
50-59<br />
60-69<br />
70-79<br />
80-89<br />
90 and older<br />
Table 3: Patient’s Age at Diagnosis – SJH<br />
AGE 2000 2001 2002 2003 2004 2005 2006 TOTAL<br />
Number Number Number Number Number Number Number Number<br />
30-39 0 0 0 0 0 0 0 0<br />
40-49 2 4 4 10 3 10 10 43<br />
50-59 33 50 41 39 58 55 46 322<br />
60-69 86 61 83 68 57 75 97 527<br />
70-79 68 55 59 53 51 45 38 369<br />
80-89 16 21 13 15 11 15 14 105<br />
90-99 3 1 0 0 2 1 0 7<br />
TOTAL 208 192 200 185 182 201 205 1,373<br />
Source: SJH <strong>Cancer</strong> Registry Database • Retrieved on July 21, <strong>2007</strong><br />
Figure 4a:<br />
150<br />
120<br />
90<br />
60<br />
30<br />
0<br />
Surgery – SJH<br />
None<br />
Cryosurgery<br />
143<br />
Prostatectomy<br />
Robotic Prostatectomy<br />
116<br />
All Others<br />
121<br />
97<br />
81<br />
67<br />
58<br />
50<br />
51<br />
55<br />
47 43<br />
39<br />
38 36 36<br />
38<br />
26<br />
31<br />
26<br />
30 23<br />
19<br />
13<br />
13<br />
16 19 18<br />
6<br />
9<br />
0 0 0 0<br />
4<br />
2000 2001 2002 2003 2004 2005 2006<br />
Source: SJH <strong>Cancer</strong> Registry Database<br />
Retrieved on July 21, <strong>2007</strong><br />
8
Figure 6a:<br />
100<br />
80<br />
60<br />
40<br />
20<br />
Figure 6c:<br />
100<br />
100<br />
Figure 6b:<br />
80<br />
60<br />
40<br />
20<br />
0<br />
80<br />
60<br />
40<br />
20<br />
0<br />
0<br />
100 95 91 87 85 80<br />
<strong>St</strong>age I <strong>St</strong>age II <strong>St</strong>age III <strong>St</strong>age IV Overall<br />
364 cases 14,224 cases 1,429 cases 854 cases 16,871 cases<br />
100 95 91 86 81 76<br />
Five-year Observed Survival by <strong>St</strong>age – SJH<br />
(Diagnosed 1995-2001)<br />
Five-year Observed Survival by <strong>St</strong>age – Florida<br />
(Diagnosed 1998-1999)<br />
At diagnosis<br />
1 year<br />
2 years<br />
3 years<br />
75-84<br />
Five-year Observed Survival by <strong>St</strong>age – National<br />
(Diagnosed 1998-1999)<br />
At diagnosis<br />
1 year<br />
2 years<br />
3 years<br />
75-77<br />
100 100 9896 99 97 100 100<br />
92<br />
97 94<br />
89<br />
93<br />
85<br />
90<br />
86<br />
90 87<br />
80<br />
83<br />
65<br />
57<br />
49 45<br />
84-86<br />
10098 100 100 100 95 98 92 96 97 89 93 93 85<br />
90 87<br />
89 86<br />
78<br />
82<br />
62<br />
51 43 38<br />
85-85.5<br />
<strong>St</strong>age I <strong>St</strong>age II <strong>St</strong>age III <strong>St</strong>age IV Overall<br />
9,748 cases 175,604 cases 23,430 cases 13,918 cases 222,700 cases<br />
87-87.5<br />
37-39<br />
4 years<br />
5 years<br />
95% Confidence<br />
Interval<br />
Source: NCDB, Commission on <strong>Cancer</strong>, ACoS/ACS • Survival <strong>Report</strong>s, v3.0 – July 22, <strong>2007</strong><br />
84-89<br />
At diagnosis<br />
1 year<br />
2 years<br />
3 years<br />
4 years<br />
5 years<br />
100 100<br />
95<br />
100 99 100 100<br />
92<br />
97 94 9796 9692 8981 91 87 91 89 81<br />
83<br />
84 81 82<br />
84 80<br />
59<br />
48<br />
42<br />
<strong>St</strong>age I <strong>St</strong>age II <strong>St</strong>age III <strong>St</strong>age IV Overall<br />
Source: NCDB, Commission on <strong>Cancer</strong>, ACoS/ACS • Survival <strong>Report</strong>s, v3.0 – July 22, <strong>2007</strong><br />
41-49<br />
4 years<br />
5 years<br />
95% Confidence<br />
Interval<br />
Source: NCDB, Commission on <strong>Cancer</strong>, ACoS/ACS • Survival <strong>Report</strong>s, v3.0 – July 22, <strong>2007</strong><br />
82-84<br />
82<br />
Hormone Therapy<br />
Androgen Deprivation Therapy (ADT) is the mainstay of therapy for<br />
advanced prostate cancer. ADT can be accomplished either medically or<br />
surgically (orchiectomy) and the response and outcome are equivalent.<br />
Medical castration is typically accomplished with a luteinizing hormonereleasing<br />
hormone (LHRH) agonist. The target for ADT is a serum<br />
testosterone level of
<strong>Cancer</strong> Registry Data Summary<br />
2006 <strong>St</strong>atistics<br />
In Florida, an estimated 98,960 cases were expected to be diagnosed in<br />
2006, while 1,399,790 new cases were estimated nationally. According to<br />
the 2006 <strong>Cancer</strong> Facts & Figures, cancer is the second most common cause<br />
of death in the United <strong>St</strong>ates, which accounts for one of every four deaths.<br />
During 2006, the <strong>Cancer</strong> Registry accessioned 2,045 new cases, 77% of<br />
which were analytic cases that were diagnosed and/or treated at <strong>St</strong>. Joseph’s<br />
<strong>Hospital</strong>, <strong>St</strong>. Joseph’s Women <strong>Hospital</strong>, Same Day Surgery, Radiation<br />
Therapy Center, Outpatient Infusion Center and <strong>St</strong>. Joseph’s Children’s<br />
<strong>Hospital</strong> of Tampa. The non-analytic cases account for 23% of patients that<br />
were diagnosed and/or treated elsewhere (Table 6).<br />
The gender distribution of <strong>St</strong>. Joseph’s <strong>Hospital</strong> analytic case population is<br />
43% for males and 57% for females. American <strong>Cancer</strong> Society Facts &<br />
Figures – 2006 estimated 51% male and 49% females diagnosed nationally<br />
(Figure 9).<br />
Race distribution continues to show similarities to previous years at 86%<br />
white, 12% black and 2% other race (Figure 11). The two largest age<br />
populations are 60-69 (25%) and 50-59 (21%), accounting for 46% of<br />
the 2006 patient population. The third largest age group is 70- 79;<br />
females accounts for 11% and males 10% (Figure 10).<br />
<strong>St</strong>aging is essential in determining the choice of therapy and in assessing<br />
prognosis. <strong>St</strong>. Joseph’s <strong>Hospital</strong> analytic cases by AJCC TNM staging<br />
systems assess tumors in three ways: extent of the primary tumor (T),<br />
absence or presence of regional lymph node involvement (N), and absence<br />
or presence of distant metastases (M). These components determine a stage<br />
of I, II, III, or IV; stage I being early stage and IV being advanced. Figure<br />
12 shows slight similarities from 2006: <strong>St</strong>age 0, (8%); <strong>St</strong>age I, (21%); <strong>St</strong>age<br />
II, (24%); <strong>St</strong>age III (13%); <strong>St</strong>age IV, (14%); Unknown, (9%) and <strong>St</strong>age Not<br />
Applicable (N/A) (10%). This demonstrates that 54% of our patient<br />
population was diagnosed with early stage disease (<strong>St</strong>age II or less).<br />
The top ten primary cancer sites (Figure 8) prevalence at <strong>St</strong>. Joseph’s<br />
<strong>Hospital</strong> shows similarities to state and national comparison. Breast cancer<br />
diagnoses at <strong>St</strong>. Joseph’s <strong>Hospital</strong> continue to remain in the forefront. This<br />
is due to the comprehensive Breast Center at <strong>St</strong>. Joseph’s Women’s <strong>Hospital</strong><br />
and diagnosing more breast cases in Hillsborough County.<br />
<strong>St</strong>. Joseph’s <strong>Hospital</strong> treatment modality (Figure 14) shows 38% of<br />
patients had surgery alone, 6% received radiation therapy alone, 6%<br />
received chemotherapy alone, while 34% had combined modality<br />
treatment and 16% elected no treatment.<br />
Figure 7 iIllustrating the five-year relative survival rates by SEER stage<br />
comparison, shows favorable outcomes for <strong>St</strong>. Joseph’s <strong>Hospital</strong> top five<br />
cancer sites.<br />
Figure 7: Five-Year Relative Survival–SJH & U.S.; 1996-2002<br />
100%<br />
90<br />
80<br />
70<br />
60<br />
50<br />
40<br />
30<br />
20<br />
10<br />
0<br />
91 89<br />
100 100<br />
65 65<br />
SJH<br />
U.S.<br />
19 16<br />
61 63<br />
Breast Prostate Colorectal Lung Non-Hodgkin’s<br />
Lymphoma<br />
Obtained from American <strong>Cancer</strong> Society <strong>2007</strong> <strong>Cancer</strong> Facts and Figures<br />
Figure 8:<br />
Top Ten Sites vs. <strong>St</strong>ate and U.S.<br />
30%<br />
25<br />
26<br />
SJH (Total–1,569)<br />
FL (Total–98,960)<br />
U.S. (Total–1,399,790)<br />
26<br />
25<br />
24<br />
20<br />
18<br />
17<br />
15<br />
10<br />
14 15 13 13 13<br />
13<br />
11<br />
10<br />
8<br />
5<br />
0<br />
444<br />
5 4<br />
3<br />
3 3 3 3 3 3<br />
5<br />
4<br />
1 1 1 1<br />
Breast Lung Prostate Colorectal Non-Hodgkin’s Bladder Leukemia Corpus Uteri Melanoma Cervix All Others<br />
Lymphoma<br />
10
Table 6: Primary Site Tabulation for Cases in 2006<br />
A total of 2,045 cases were diagnosed and/or treated at <strong>St</strong>. Joseph’s <strong>Hospital</strong>. The analytic cases of 1,569 accounted for 77% of the total population and the non-analytic cases of<br />
476 accounted for 23%. American <strong>Cancer</strong> Fact & Figures–2006 estimated a total of 1,399,790 new cases were estimated for 2006 nationally, with 98,960 projected for Florida.<br />
Primary Site Total Class Sex<br />
A N/A M F<br />
All Sites 2,045 1,569 476 930 1,115<br />
Oral Cavity 37 26 11 26 11<br />
Lip 0 0 0 0 0<br />
Tongue 16 9 7 10 6<br />
Oropharynx 2 1 1 2 0<br />
Hypopharynx 0 0 0 0 0<br />
Other 19 16 3 14 5<br />
Digestive System 287 220 67 142 145<br />
Esophagus 12 7 5 5 7<br />
<strong>St</strong>omach 20 17 3 11 9<br />
Colon 122 85 37 50 72<br />
Rectum 42 36 6 26 16<br />
Anus/anal canal 11 9 2 5 6<br />
Liver 22 18 4 18 4<br />
Pancreas 40 32 8 20 20<br />
Other 18 16 2 7 11<br />
Respiratory System 287 225 62 172 115<br />
Nasal/sinus 2 1 1 1 1<br />
Larynx 23 12 11 20 3<br />
Lung/bronchus 260 210 50 150 110<br />
Other 2 2 0 1 1<br />
Blood & Bone Marrow 111 76 35 55 56<br />
Leukemia 72 52 20 35 37<br />
Multiple Myeloma 26 21 5 14 12<br />
Other 13 3 10 6 7<br />
Bone 6 3 3 4 2<br />
Connect/Soft Tissue 9 7 2 5 4<br />
Skin 31 10 21 20 11<br />
Melanoma 29 10 19 18 11<br />
Other 2 0 2 2 0<br />
Breast 478 405 73 7 471<br />
Female Genital 148 114 34 0 148<br />
Cervix Uteri 29 22 7 0 29<br />
Corpus Uteri 61 48 13 0 61<br />
Ovary 37 24 13 0 37<br />
Vulva 15 14 1 0 15<br />
Other 6 6 0 0 6<br />
Male Genital 311 218 93 311 0<br />
Prostate 297 205 92 297 0<br />
Testis 14 13 1 14 0<br />
Other 0 0 0 0 0<br />
Urinary System 132 99 33 85 47<br />
Bladder 75 54 21 57 18<br />
Kidney/renal 51 41 10 24 27<br />
Other 6 4 2 4 2<br />
Brain & CNS 41 35 6 19 22<br />
Brain (benign) 4 3 1 1 3<br />
Brain (malignant) 25 21 4 12 13<br />
Other 12 11 1 6 6<br />
Endocrine 38 31 7 16 22<br />
Thyroid 32 28 4 12 20<br />
Other 6 3 3 4 2<br />
Lymphatic System 106 82 24 54 52<br />
Hodgkin’s Disease 19 14 5 8 11<br />
Non-Hodgkin’s 87 68 19 46 41<br />
Unknown Primary 15 13 2 10 5<br />
Other/ill-defined 8 5 3 4 4<br />
13 11
Figure 9:<br />
2006 Gender Distribution<br />
Compared to U.S.<br />
Male<br />
Female<br />
Figure 11:<br />
Race Distribution<br />
2%<br />
White<br />
Black<br />
Other<br />
12%<br />
51% 43%<br />
49% 57%<br />
86%<br />
U.S.<br />
SJH<br />
Male cancer cases comprised 43% (679) of the total analytic cases and females comprised 57% (890).<br />
The American <strong>Cancer</strong> Society Facts & Figures - 2005 estimates there will be 51% male and 49% females<br />
diagnosed with cancer nationally.<br />
Figure 10: Age by Gender Distribution Figure 12: AJCC <strong>St</strong>aging Distribution–1,569 total<br />
(All Sites–Analytic Only)<br />
220<br />
200<br />
180<br />
160<br />
140<br />
120<br />
100<br />
80<br />
60<br />
40<br />
20<br />
0<br />
12 16<br />
10 10<br />
6 8<br />
17<br />
46<br />
51<br />
147<br />
0-9 10-19 20-29 30-39 40-49 50-59 60-69 70-79 80-89 90-99<br />
132<br />
200<br />
220<br />
171<br />
177<br />
160<br />
Male (679 Total)<br />
Female (890 Total)<br />
63<br />
97<br />
8<br />
7<br />
9%<br />
(136)<br />
13%<br />
(200)<br />
10%<br />
(160)<br />
14%<br />
(224)<br />
24%<br />
(383)<br />
8.4%<br />
(131)<br />
21.4%<br />
(335)<br />
<strong>St</strong>age 0<br />
<strong>St</strong>age I<br />
<strong>St</strong>age II<br />
<strong>St</strong>age III<br />
<strong>St</strong>age IV<br />
Unknown<br />
N/A<br />
Figure 13:<br />
50%<br />
40<br />
Top Five Sites vs. <strong>St</strong>ate and U.S.<br />
SJH<br />
FL<br />
U.S.<br />
30<br />
26<br />
20<br />
10<br />
14 15<br />
13 13 13<br />
18 17<br />
13<br />
10 11<br />
7<br />
4<br />
4 4<br />
0<br />
Breast Lung Prostate Colorectal Non-Hodgkin’s<br />
Lymphoma<br />
Figure 14:<br />
Treatment Modality<br />
Surgery<br />
Surgery/Radiation Therapy<br />
Chemotherapy<br />
None<br />
Surgery/Chemotherapy<br />
Other Combined Therapy<br />
22%<br />
38%<br />
9%<br />
16%<br />
9%<br />
6%<br />
12
<strong>Cancer</strong> Registry <strong>Report</strong><br />
The <strong>Cancer</strong> Registry is an integral part of <strong>St</strong>. Joseph’s <strong>Hospital</strong> <strong>Cancer</strong><br />
Institute. The primary function is to provide continuum data<br />
management services under the leadership and support of the <strong>Cancer</strong><br />
Committee. <strong>Cancer</strong> data collection is available to the medical staff for<br />
special studies, audits and research.<br />
<strong>St</strong>. Joseph’s <strong>Hospital</strong> <strong>Cancer</strong> Registry initiated data collection in 1976<br />
with over 40,000 accumulative cases. The registry reference year was<br />
changed to 1990 for better control of maintaining current follow-up and<br />
treatment on over 22,000 patients. Lifetime follow-up for former patients<br />
is a vital component of our cancer program. <strong>Annual</strong> follow-up<br />
encourages patients to continue their yearly medical supervision. The<br />
goal is to maintain current follow-up on all patients in the Electronic<br />
Registry System cancer database.<br />
The registry utilizes the Electronic Registry System (ERS), which better<br />
serves in data collection, analysis and quality improvement to meet the<br />
Florida <strong>Cancer</strong> Data System (FCDS) and the National <strong>Cancer</strong> Database<br />
call for data. The registry software has undergone extensive upgrades to<br />
maximize the elements in providing quality data. The registry data is<br />
used for a variety of screening, early detection and prevention programs.<br />
The medical community can identify higher cancer incidents to increase<br />
public awareness in both preventable and treatable diseases.<br />
2006-<strong>2007</strong> <strong>Cancer</strong> Registry Accomplishments<br />
• Completed 2,045 abstracts for accession year 2006 by maintaining<br />
over 90 percent abstract timeliness requirement<br />
• Submitted 2006 data to National <strong>Cancer</strong> Database call for data to meet<br />
Commission on <strong>Cancer</strong> <strong>St</strong>andards of both quality and timeliness<br />
• Achieved an overall data accuracy of 95 percent per physician audit of<br />
10 percent of analytic cases<br />
• Maintained patient follow-up on over 10,000 eligible patients since<br />
reference year 1990 with a success rate of over 90 percent<br />
• Participated in state and nationwide cancer registry educational<br />
activities annually<br />
• Participated in National <strong>Cancer</strong> Database <strong>St</strong>udy <strong>Cancer</strong> Program<br />
Practice Profile <strong>Report</strong>s (CP3r) for colon and breast cancers<br />
The <strong>Cancer</strong> Registry staff coordinates <strong>Cancer</strong> Conferences for case<br />
presentations. Conferences are held weekly on Fridays (7:30-8:30am) in<br />
the <strong>St</strong>. Joseph’s <strong>Hospital</strong> Medical Arts Building. Breast conferences are<br />
held every other Tuesday (noon) at <strong>St</strong>. Joseph’s Women’s <strong>Hospital</strong><br />
Pavilion 4th floor classrooms. These forums are used to provide<br />
treatment options and improvements in patient care throughout the<br />
Tampa Bay area. Please contact the <strong>Cancer</strong> Registry at (813) 870-4987 to<br />
schedule case presentations.<br />
<strong>St</strong>. Joseph’s <strong>Hospital</strong> <strong>Cancer</strong> Committee encourages the use of Registry<br />
data. The <strong>Cancer</strong> Registry receives numerous requests for statistical<br />
reports. Data is utilized for the following: study analysis, annual statistics,<br />
reports to the <strong>St</strong>ate <strong>Cancer</strong> Registry and the National <strong>Cancer</strong> Data Base,<br />
research activities, survival analysis, quality management studies,<br />
community education, health care planning/delivery and outcome<br />
evaluation/improvement.<br />
The <strong>Cancer</strong> Registry would like to thank our volunteers, physicians and<br />
staff for the collaborative efforts in providing the most current follow-up<br />
and treatment information, to assure the most achievable outcomes of<br />
accurate data in the registry.<br />
Victoria Young, MBA, CTR<br />
<strong>Cancer</strong> Registry Coordinator<br />
<strong>Cancer</strong> Liaison Physician <strong>Report</strong><br />
<strong>St</strong>. Joseph’s <strong>Hospital</strong><br />
The community cancer program at <strong>St</strong>. Joseph’s <strong>Hospital</strong> is approved by<br />
the American College of Surgeons Commission on <strong>Cancer</strong>. As the <strong>Cancer</strong><br />
Liaison Physician at <strong>St</strong>. Joseph’s <strong>Hospital</strong>, I am committed to our cancer<br />
program, supporting compliance and maintenance of Commission on<br />
<strong>Cancer</strong> standards, facilitating a working relationship with the American<br />
<strong>Cancer</strong> Society and working closely with our cancer committee to<br />
improve the quality of our cancer care.<br />
This past year, we worked more closely with the American <strong>Cancer</strong><br />
Society having John Surprenant, Director of the <strong>Cancer</strong> Institute, serving<br />
on their <strong>Cancer</strong> Control Committee and an American <strong>Cancer</strong> Society<br />
representative serving on our <strong>Cancer</strong> Committee. <strong>St</strong>. Joseph’s <strong>Hospital</strong> was<br />
recently recognized by the American <strong>Cancer</strong> Society for our newly organized<br />
and expanded Reach to Recovery Program.<br />
We are currently participating in a Commission on <strong>Cancer</strong> study on the<br />
“Impact of Neoadjuvant Therapy on <strong>St</strong>aging for Rectal and Breast <strong>Cancer</strong><br />
Cases.” The results of this study will be used to identify ways to improve<br />
our treatment of these cancers.<br />
Dr. James Christensen, Dr. Chris George and I preside at our weekly<br />
multidisciplinary cancer conferences. They are well attended and many<br />
prospective cases are presented, which positively impact the treatment<br />
of our patients.<br />
I serve as an active member and chairman of our <strong>Cancer</strong> Committee,<br />
working closely with John Surprenant, Director of the <strong>Cancer</strong> Institute,<br />
and Victoria Young, <strong>Cancer</strong> Registrar, to promote our <strong>Cancer</strong> Institute and<br />
physicians, to improve cancer care, to publish the annual report and to<br />
participate in the periodic American College of Surgeons Commission on<br />
<strong>Cancer</strong> survey for re-accreditation.<br />
Thank you for the honor and privilege of serving as <strong>St</strong>. Joseph’s <strong>Hospital</strong><br />
<strong>Cancer</strong> Liaison Physician.<br />
Anthony N. Brannan, M.D.<br />
<strong>Cancer</strong> Liaison Physician<br />
13
<strong>Cancer</strong>-Related Programs and Services<br />
14<br />
da Vinci ® Surgical System<br />
The da Vinci Surgical System is highly sophisticated, minimally invasive<br />
technology that translates each motion of a surgeon’s hands into precise<br />
movements of the micro-instruments for a more accurate surgical<br />
procedure. The size, precision and flexibility of instruments make the<br />
surgical system ideal for prostatectomy where the cancer tissue is tightly<br />
confined and closely surrounded by nerves. It is available at <strong>St</strong>. Joseph’s<br />
<strong>Hospital</strong> and is operated by our experienced team of physicians.<br />
Diagnostic and Interventional Radiology Services<br />
<strong>St</strong>. Joseph’s <strong>Hospital</strong> provides a full array of advanced diagnostic and<br />
interventional imaging services and procedures. In recent years, diagnostic<br />
radiology has made giant strides in the development of minimally invasive<br />
devices and techniques that can better detect cancer.<br />
<strong>St</strong>. Joseph’s <strong>Hospital</strong> radiology physicians and staff are leaders in their fields<br />
and have access to the most advanced technology available today. The<br />
program is ACR accredited. The department is staffed by board-certified and<br />
fellowship-trained radiologists in areas of neurointerventional, interventional,<br />
pediatric, nuclear medicine, MRI, musculoskelatal and breast imaging<br />
specialties. The radiology team is supported by ARRT-certified technologists in<br />
all specialty modalities.<br />
Services provided by the department include breast MRI, breast ultrasound,<br />
full-field digital mammography, PET/CT, stereotactic core needle breast biopsy,<br />
CT, ultrasound and MRI-guided biopsy services, nuclear medicine services<br />
including sentinel lymph node mapping/lymphoscintigraphy, as well as<br />
routine fluoroscopy, MRI, CT and ultrasound.<br />
Interventional imaging includes minimally invasive procedures including<br />
chemo-embolization for treating liver and bone metastatic disease, RF and<br />
cryoablation procedures, aneurysm coilings, stenting and central-line<br />
placements. All modalities are supported by a state-of-the-art 3D post<br />
processing service that provides surgical mapping, stroke analysis and<br />
planning for patient treatments. The radiology department utilizes all digital<br />
imaging equipment and includes 64- and 128-slice CT scanners capable of<br />
cardiac imaging, DR radiology rooms and a comprehensive digital PACS<br />
system for image analysis.<br />
Fred J. Woods Radiation Therapy Center<br />
The Fred J. Woods Radiation Therapy Center is a state-of-the-art facility,<br />
which has been part of <strong>St</strong>. Joseph’s <strong>Hospital</strong> since 1969. It is staffed with<br />
board-certified radiation oncologists, physicists and dosimitrists. The<br />
Center has ten certified radiation technologists, as well as two oncology<br />
trained nurses to provide skilled, compassionate care to the cancer patient.<br />
Existing technology includes: two Varian Clinac 23 EX linear accelerators<br />
with Intensity Modulated Radiation Therapy (IMRT) capabilities; a<br />
dedicated advanced light speed GE CT scanner; <strong>St</strong>ereotactic Radiosurgery<br />
(SRS); Nucletron High Dose Rate Brachytherapy (HDR); Superficial; and<br />
the Phillips Pinnacle Treatment Planning System with fusion capabilities<br />
to receive diagnostic MRI, PET and CT scan.<br />
The Center provides a full-range of treatment options, including<br />
mammosite, prostate seed implants and use of sir spheres for colon and<br />
liver metastasis in addition to traditional external beam therapy. The<br />
Center is approved to participate in Radiation Therapy Oncology Group<br />
clinical trials through the American College of Radiology.<br />
Outpatient Infusion Center<br />
The Outpatient Infusion Center offers convenience for patients who require<br />
infusion of medications, including those with central lines. The staff works<br />
primarily with cancer patients undergoing chemotherapy and those with<br />
blood disorders.<br />
Services and treatments provided include infusion of chemotherapy<br />
agents, biological response modifiers, central line catheter care,<br />
hydration, immunomodulators, IV anti-emetics therapy, IV immune<br />
globulin, monoclonal antibodies, subcutaneous injections, therapeutic<br />
phlebotomy and transfusion of blood products.<br />
Pathology Services<br />
The Pathology Department at <strong>St</strong>. Joseph <strong>Hospital</strong> offers state-of-the-art<br />
diagnostic services in cytology, anatomical, clinical and surgical pathology<br />
and is supported by a variety of specialty laboratories including: histology,<br />
immuno histochemistry, electron microscopy, flow cytometry and molecular<br />
diagnostics. The department is staffed by 11 board-certified pathologists<br />
who are experts in their subspecialty areas.<br />
<strong>St</strong>. Joseph’s Children’s <strong>Hospital</strong> Hematology/Oncology Center<br />
<strong>St</strong>. Joseph’s Children’s <strong>Hospital</strong> Hematology/Oncology Center is a<br />
comprehensive program that incorporates the latest inpatient and outpatient<br />
treatments for all forms of childhood cancers. We are a member of the<br />
Children’s Oncology Group (COG), an international research cooperative that<br />
designs and reviews the most advanced treatments for childhood cancer. We<br />
are also a member of the Florida Association of Pediatric Tumor Programs.<br />
Our participation in COG provides for affiliation in CureSearch, which<br />
unites the world’s largest cancer research organizations (COG and National<br />
Childhood <strong>Cancer</strong> Foundation) in a shared mission to cure childhood<br />
cancer through research. Dr. Cameron Tebbi, a nationally known expert in<br />
pediatric oncology, leads a team of board-certified pediatric oncologists,<br />
practitioners and research nurses as part of our center. There are currently<br />
78 COG studies open to enrollment with 30 active patients. Additionally,<br />
there are two pharmaceutical studies available to qualified participants.<br />
<strong>St</strong>. Joseph’s Children’s <strong>Hospital</strong> Hematology/Oncology Center provides a<br />
seven-bed state-of-the-art infusion center, as well as dedicated 15-bed<br />
inpatient unit in the <strong>Cancer</strong> Institute. Greater than 60 percent of our<br />
nursing staff has attained CPN or CPON certification. The remainder of<br />
the team is comprised of certified child life specialists, pediatric social<br />
workers, chaplains, audiologists, occupational, physical and speech<br />
therapists, pediatric radiation oncologists and a clinical psychologist.<br />
The Breast Center at <strong>St</strong>. Joseph’s Women’s <strong>Hospital</strong><br />
The Breast Center at <strong>St</strong>. Joseph’s Woman’s <strong>Hospital</strong> provides care,<br />
guidance, information, screening, diagnosis and treatment for breast<br />
cancer patients. The Center offers the highest level of expertise,<br />
compassion and respect in a convenient and comfortable setting.<br />
The Breast Center has dedicated board-certified physicians who are<br />
specialists in their respective fields, and is further enhanced with a dedicated<br />
nurse navigator. The nurse navigator is an experienced specialist who<br />
coordinates the details of patient care, provides personalized information<br />
and support, assists with appointments and scheduling, and is the patients’<br />
link to physicians, resources and therapies.<br />
The Breast Center’s state-of-the-art diagnostic imaging technology includes:<br />
• Digital mammography (breast x-ray)<br />
• <strong>St</strong>ereotactic biopsy – minimally invasive, state-of-the-art technology<br />
that causes less stress and pain to the patient<br />
• Needle localization and biopsy – a specialized mammography<br />
technique that pinpoints the location of the breast lesion<br />
• Breast ultrasound – the use of sound waves to differentiate solid tumors from cysts<br />
• Breast MRI
<strong>Cancer</strong> Patient Support Services<br />
<strong>Cancer</strong> HelpLine/<strong>Cancer</strong> Outreach<br />
<strong>St</strong>. Joseph’s <strong>Hospital</strong> <strong>Cancer</strong> Institute has a no-cost, confidential information<br />
line staffed by a nationally certified oncology nurse. Callers receive cancer<br />
information and referrals to physicians and community services such as free<br />
and low-cost cancer screenings. Call (813) 870-4123.<br />
Enterostomal Therapy Clinic<br />
<strong>St</strong>. Joseph’s <strong>Hospital</strong> offers an Outpatient Enterostomal Therapy (ET)<br />
Clinic for new ostomy patients and any patient who experiences problems<br />
related to their ostomy. Patients must call their primary physician to<br />
request a referral. Call (813) 870-4418 to schedule an appointment.<br />
Hispanic Breast <strong>Cancer</strong> Support Group<br />
This free monthly group is designed for Spanish-speaking women with<br />
breast cancer, survivors and their family members. Call (813) 870-4747.<br />
Look Good...Feel Better<br />
This program is available for women before, during and after treatment.<br />
Receive a consultation at no charge with a beauty specialist who provides<br />
cosmetic advice, hair/wig styling tips and free makeup kits. Call the<br />
American <strong>Cancer</strong> Society at (800) 227-9954.<br />
Lymphedema Program<br />
Housed at <strong>St</strong>. Joseph’s <strong>Hospital</strong>, this program combines manual lymph<br />
drainage with compressive bandaging, personalized exercise programs<br />
and skin care to help patients manage symptoms and reduce swelling<br />
and pain. Call (813) 870-4877, ext. 1, for more information.<br />
Nutrition<br />
Nutritional counselors are available to assist patients with specific<br />
dietary needs. Call (813) 870-4420.<br />
Outpatient Counseling Services:<br />
BayCare Life Management<br />
Outpatient counseling is a voluntary treatment choice for those needing<br />
short- or long-term behavioral health care. Counseling is done in one of<br />
BayCare Life Management’s convenient locations throughout the Tampa<br />
Bay area. Treatment is accomplished in individual, family and smallgroup<br />
formats. For further information, call (813) 936-0474, ext. 3.<br />
OVACOME<br />
Ovarian and gynecological cancer support group meets on the third<br />
Tuesday of every month from 6-8pm in the Medical Arts Building<br />
Auditorium. Free support group for patients and significant others. Call<br />
the Contact Center at (813) 870-4747 or Ovacome at (813) 223-9108<br />
for more information, or visit www.ovacome.us.<br />
Pain Management Specialist<br />
<strong>St</strong>. Joseph’s <strong>Hospital</strong> Pain Management Specialists are available for all<br />
patients. Physician referral is required.<br />
Palliative Care<br />
<strong>St</strong>. Joseph’s <strong>Hospital</strong> offers a very specialized team that works with your<br />
attending physician to assist in relieving physical pain and suffering,<br />
while also providing emotional and family counseling. Our goal is to<br />
help you and your family make the most of life. Call (813) 870-4114.<br />
Pastoral Care<br />
Our Pastoral Care Department provides supportive spiritual care to<br />
cancer patients and their families, including psycho-spiritual counseling,<br />
prayer, religious services, meditation and referrals. Call (813) 870-4258<br />
or (813) 872-3950.<br />
Prostate <strong>Cancer</strong> Support Group: Man-to-Man<br />
A free American <strong>Cancer</strong> Society support program for prostate cancer<br />
survivors and their significant others. Meets monthly. Guest speakers<br />
and topics vary each month. Contact the American <strong>Cancer</strong> Society at<br />
1 (800) 227-9954 or our <strong>Cancer</strong> HelpLine at (813) 870-4123 for more<br />
information.<br />
Pulmonary Rehabilitation<br />
Provides information and support for those with respiratory illness and<br />
breathing difficulties. Call (813) 870-4844, ext. 4.<br />
Social Services<br />
Social workers are available to help plan for hospital discharge,<br />
including referrals to home health, skilled nursing or rehabilitation<br />
services. Call (813) 870-4974 or (813) 872-3915.<br />
Tampa Area Ostomy Support Group<br />
The Tampa Area Ostomy Support Group is sponsored by <strong>St</strong>. Joseph’s<br />
<strong>Hospital</strong> and is supported by four local WOCN nurses. All ostomates<br />
and their support persons are invited to attend. Meetings are held every<br />
other month on the third Saturday except when otherwise notified.<br />
There is no fee or registration required. Contact one of the following<br />
nurses for more information: Pam Brown, (813) 870-4785;<br />
Beverly Higbea, (813) 870-4418; Barbara Bagby, (813) 558-4900, or<br />
Nancy Scott, (813) 972-8438.<br />
15
2006-<strong>2007</strong> <strong>Cancer</strong> Program Highlights<br />
<strong>Cancer</strong> Committee Goals<br />
• Increase patient and family satisfaction with the palliative care program.<br />
Achieved.<br />
• Increase physician, nursing and ancillary staff cultural awareness and<br />
sensitivity in our diverse patient populations. Achieved.<br />
• Develop in conjunction with Greater Tampa Unit of the American <strong>Cancer</strong><br />
Society a Patient Resource Center. In process—on target.<br />
• Enhance resources on hospital cancer Web site. Achieved.<br />
• Assure that <strong>St</strong>age I-III breast cancer patients receiving highly emetogenic<br />
chemotherapy receive potent antiemetic therapy (5 HT Blockage). Achieved.<br />
• Assure that colorectal cancer patients with <strong>St</strong>age II-III disease receiving<br />
chemotherapy have recorded the body surface area and planned dose<br />
documented in the medical record. Achieved.<br />
• Develop process to evaluate appropriate drug use for new drugs which<br />
are not yet funded by Medicare. Achieved.<br />
• Develop tool for medical oncologists to order outpatient therapies in a<br />
consistent manner. Achieved.<br />
• Develop and maintain “wish list” of opportunities for potential donors for<br />
<strong>St</strong>. Joseph’s <strong>Hospital</strong>s Foundation. Achieved.<br />
• Enhance drug replacement program for safety net cancer patients in the<br />
Outpatient Infusion Center. Achieved.<br />
Screenings<br />
1,224 participants/66 abnormals identified<br />
• African-American Men’s Health Forum<br />
• Colorectal Awareness and Screening Campaign<br />
• <strong>St</strong>. Joseph’s <strong>Hospital</strong> Prostate Screening (2)<br />
Support Groups<br />
54 support groups were held with 799 people in attendance.<br />
• Hispanic Breast <strong>Cancer</strong><br />
• Man-to-Man<br />
• Ostomy Support<br />
Community Educational Seminars<br />
• Look Good...Feel Better<br />
• Mindfulness Meditation<br />
• Ovacome<br />
• Colon <strong>Cancer</strong>s, Hemorrhoids and Fissures – Dr. Lori Slezak<br />
• Continuing Education Conferences for Medical <strong>St</strong>aff<br />
• Genetic Screening in <strong>Cancer</strong> – Rebecca <strong>St</strong>uphen, M.D.<br />
• Gynecological <strong>Cancer</strong>s – Dr. Giselle Ghurani<br />
• Healing Touch Training Seminar<br />
• Molecular Diagnostics – Genotypes Predicts Risk of Toxicity to<br />
Irinotecan – Maura Pieritti, Ph.D.<br />
• Prostate <strong>Cancer</strong> and Robotics Conference – Dr. Frank Mastandrea<br />
• Targeted Therapies for <strong>Cancer</strong> – Dr. Alex Mirakian, Dr. Alison Calkins<br />
and Dr. Gabriel Gonzales-Portillo<br />
Sponsorships<br />
• African-American Men’s Health Forum<br />
• American <strong>Cancer</strong> Society’s Cattlebaron’s Ball<br />
• American <strong>Cancer</strong> Society’s Reach to Recovery Luncheon and Fashion Show<br />
• Ovacome Celebrate Hope<br />
• <strong>St</strong>. Joseph’s <strong>Hospital</strong> Golf Classic<br />
• Susan G. Komen Race for the Cure<br />
• Tancredi Colon <strong>Cancer</strong> Prevention Awareness Run<br />
Special Events<br />
• <strong>Cancer</strong> Survivors’ Day Celebration – June 5<br />
• Lilly Art Exhibit: A Woman’s Journey through <strong>Cancer</strong> – month of October<br />
• Oncology Nurses’ Week<br />
• National Registrar’s Week<br />
• American <strong>Cancer</strong> Society’s Daffodil Days<br />
• Hired Nurse Navigator for The Breast Center – Susan Baker, R.N., Ph.D.<br />
candidate<br />
• Purchased High Dose Rate Brachytherapy Technology and began use –<br />
May 8<br />
• Jointly sponsored Oncology Nursing Society review course with<br />
Morton Plant Mease<br />
• Chris Hubbard, American <strong>Cancer</strong> Society Patient Services<br />
Representative, gave presentation at Tumor Conference on range of<br />
services available through the American <strong>Cancer</strong> Society<br />
• Initiated Safety Net Drug Replacement Program in Outpatient Infusion Center<br />
• Dr. Anthony Brannan and John Surprenant were guest speakers at the<br />
Florida Council of Aging Conference on August 16. Spoke on<br />
Colorectal <strong>Cancer</strong> Awareness and Screening.<br />
• Donated 26 wigs to patients<br />
• Reach to Recovery Program<br />
• Innovative program using hospital breast cancer survivors to visit new<br />
breast cancer patients was started on April 14, 2006. Trained 19<br />
volunteers and saw 97 patients in 2006.<br />
• Purchased new technology to support <strong>Cancer</strong> Conferences at <strong>St</strong>. Joseph’s<br />
Women’s <strong>Hospital</strong><br />
• Florida Dialogue on <strong>Cancer</strong><br />
• Participation in Quality Improvement projects through Six Sigma<br />
– CI-3 patient satisfaction with pain management<br />
– Sitter usage<br />
– Fall prevention<br />
– Increasing effective communication at time of handoff to radiology<br />
– Outpatient Infusion – Maximizing chemotherapy drug reimbursement<br />
– New Drug Decision Matrix Process workout<br />
16
Philanthropy (Fund-Raising Events)<br />
• Carrabba’s Children’s Golf Classic<br />
• Hope on Wheels – Krewe event to support cancer research<br />
• Order of the Eastern <strong>St</strong>ar – To support cancer research<br />
• Bras for a Cause – In support of activities at The Breast Center<br />
Grants<br />
• Joy McGann Community Enrichment Foundation – (Service) To support<br />
bilingual breast cancer patients with access to mammograms and biopsies<br />
• Amgen – (Educational) To support Oncology Nursing Society Review Course<br />
• Komen – The Breast Center and <strong>Cancer</strong> Outreach Nurse<br />
2006-<strong>2007</strong> Seminars<br />
2006<br />
• African-American Men’s Health Forum Event<br />
• African-American Men’s Prostate Screening<br />
• Cervical <strong>Cancer</strong> and Human Papillomavirus<br />
• Ladies Night Out – Breast <strong>Cancer</strong>: Are You At Risk<br />
• Ladies Night Out – Mid-Life Woman: Colon <strong>Cancer</strong>, Hemorrhoids<br />
and Fissures<br />
• Ladies Night Out – Ovarian <strong>Cancer</strong> and Other Gynecological <strong>Cancer</strong>s<br />
• Prostate <strong>Cancer</strong> Screening<br />
<strong>2007</strong><br />
• Advanced Prostate Surgery Using Robotic Technology<br />
• Ladies Health Fair – Screening Mammogram<br />
• Ladies Night Out – Breast <strong>Cancer</strong>: Are You At Risk<br />
• Ladies Night Out – Breast Health<br />
• Ladies Night Out – Ovarian <strong>Cancer</strong> and Other Gynecological <strong>Cancer</strong>s<br />
• Lymphedema Educational Conference<br />
• Men’s Night Out<br />
• Palliative Care: LIVING with Advanced Illness<br />
• Prostate <strong>Cancer</strong> Screening<br />
• Radical Robotic Prostatectomy<br />
• Together Facing Lung <strong>Cancer</strong><br />
• Urological Issues<br />
Marketing and Public Relations<br />
• 2006 and <strong>2007</strong> Colorectal <strong>Cancer</strong> Awareness Campaign – collaborative<br />
partnership with CVS Pharmacies and WFTS - ABC 28<br />
– More than 95,000 test kits given out<br />
– Created hotline for questions staffed by registered nurse<br />
– Live call-in shows with physicians, nurses and pharmacists available<br />
to answer consumer’s questions<br />
– Media stories about the importance of colorectal cancer screening,<br />
guidelines for screening and patient stories<br />
<strong>St</strong>rategic Planning<br />
American <strong>Cancer</strong> Society Partnership<br />
• John Surprenant on Unit Board<br />
• John Surprenant to chair <strong>Cancer</strong> Control<br />
• Formal Partnership Agreement signed<br />
• Advocacy efforts supported<br />
• Participated in research awards dinner<br />
• Participated in Florida Division – Volunteers launch event<br />
• Participated in African-American Women’s <strong>Cancer</strong> Summit in Orlando<br />
• Participated in launch of LifeLine Program for area<br />
• Participate in educational session on Hope Lodge<br />
Moffitt Affiliation<br />
Our affiliation with the H. Lee Moffitt <strong>Cancer</strong> Center & Research<br />
Institute further expands our services so that patients are receiving the<br />
most up-to-date, advanced cancer care available as well as access to<br />
nationally recognized clinical trials. The affiliation reinforces the concept<br />
of delivering primary cancer care in our highly regarded hospital while<br />
tapping the expertise and resources of academic researchers to assist in<br />
the treatment of rare and complicated cancers.<br />
New Medical <strong>St</strong>aff Oriented<br />
• 24 new physicians on staff and one ARNP<br />
<strong>Cancer</strong> Research<br />
<strong>St</strong>. Joseph’s <strong>Hospital</strong> <strong>Cancer</strong> Institute is an affiliate member of the NCI-designated H. Lee Moffitt <strong>Cancer</strong> Center & Research Institute. Through this<br />
affiliation, <strong>St</strong>. Joseph’s <strong>Hospital</strong> physicians can take part in device trials, phase II & III Cooperative Group trials such as the Radiation Therapy Oncology<br />
Group, as well as selected phase II Moffitt Institutional trials. The <strong>Cancer</strong> Institute at <strong>St</strong>. Joseph’s <strong>Hospital</strong> also develops and initiates clinical trials.<br />
Recently, the <strong>Cancer</strong> Institute Department of Radiation Therapy received FDA approval as the only site in the nation to study brachytherapy to the liver<br />
in patients with metastatic breast cancer. In addition, the pediatric cancer program at <strong>St</strong>. Joseph’s Children’s <strong>Hospital</strong> of Tampa takes part in NCI national<br />
clinical trials, as will as pediatric laboratory research.<br />
17
<strong>Cancer</strong> Program Leaders<br />
Anthony N. Brannan, M.D.<br />
<strong>Cancer</strong> Committee Chair<br />
ACoS Physician Liaison<br />
James Christensen, M.D.<br />
Breast <strong>Cancer</strong> Conference Coordinator<br />
Christopher George, M.D.<br />
Medical Director<br />
Chief of Oncology<br />
<strong>Cancer</strong> Conference Coordinator<br />
John L. Surprenant, MA, MDIV, MPH<br />
Administrative Director<br />
Important Phone Numbers<br />
Breast Center: (813) 872-2973<br />
<strong>Cancer</strong> Helpline/Outreach: (813) 870-4123<br />
<strong>Cancer</strong> Institute–Administration: (813) 870-4991<br />
<strong>Cancer</strong> Institute–Inpatient Unit (CI-3): (813) 870-4588<br />
<strong>Cancer</strong> Registry: (813) 870-4987 (phone)<br />
(813) 870-4209 (fax)<br />
<strong>Cancer</strong> Research/Clinical Trials: (813) 870-4257<br />
Diagnostic Center Scheduling: (813) 870-4826<br />
Pediatric Hematology/Oncology: (813) 870-4824<br />
Outpatient Chemotherapy/Infusion: (813) 870-4246<br />
Palliative Care Services: (813) 870-4114<br />
Radiation Therapy: (813) 870-4160<br />
Radiology Scheduling: (813) 870-4601<br />
Surgery Scheduling: (813) 870-4441<br />
18
Index of Physicians Associated<br />
with <strong>Cancer</strong> Program<br />
by last name and specialty<br />
Definition of Terms<br />
American College of Surgeons<br />
Commission on <strong>Cancer</strong> (ACoS CoC)<br />
The organization that surveys<br />
and approves cancer programs.<br />
Analytic (A)<br />
Pertains to those cases initially<br />
diagnosed and/or receiving<br />
their first course of treatment<br />
at <strong>St</strong>. Joseph’s Children’s <strong>Hospital</strong><br />
of Tampa, <strong>St</strong>. Joseph’s <strong>Hospital</strong>,<br />
and <strong>St</strong>. Joseph’s Women’s <strong>Hospital</strong>.<br />
Non-analytic (NA)<br />
A case diagnosed and treated<br />
elsewhere prior to being seen at<br />
<strong>St</strong>. Joseph’s Children’s <strong>Hospital</strong> of<br />
Tampa, <strong>St</strong>. Joseph’s <strong>Hospital</strong>, and<br />
<strong>St</strong>. Joseph’s Women’s <strong>Hospital</strong>.<br />
Cases that were treated more than<br />
four months after initial diagnosis.<br />
Cases that were initially diagnosed<br />
at autopsy are considered nonanalytic<br />
as well.<br />
Florida <strong>Cancer</strong> Data System<br />
The FCDS is an incidence registry<br />
for the <strong>St</strong>ate of Florida. FCDS is a<br />
cancer registry administered by the<br />
Florida Department of Health and<br />
is operated and maintained by the<br />
Sylvester Comprehensive <strong>Cancer</strong><br />
Center at the University<br />
of Miami School of Medicine.<br />
AJCC <strong>St</strong>age System<br />
The registry records stage using the<br />
AJCC (American Joint Committee<br />
on <strong>Cancer</strong>) Manual for staging<br />
guide. <strong>St</strong>age 0, I, II, III, IV<br />
or Unknown.<br />
SEER<br />
National <strong>Cancer</strong> Institute<br />
Surveillance, Epidemiology,<br />
and End Results<br />
NCDB<br />
National <strong>Cancer</strong> Data Base<br />
Relative Survival<br />
The ratio of observed survival<br />
rate to the expected rate for a group<br />
of people in the general population<br />
similar to the patient group with<br />
respect to race, sex and age.<br />
If any physician has been omitted, please contact Julieann Ramsey at (813) 870-4991.<br />
To be revised May 2008.<br />
Observed Survival Rate<br />
Rates computed by the actuarial<br />
method, compounding survival in<br />
one-month intervals from the date<br />
of diagnosis, with death from<br />
any cause as the endpoint.<br />
Accuracy of the Registry data<br />
contained in the 2006 <strong>Annual</strong><br />
<strong>Report</strong> depends upon complete<br />
documentation in the medical<br />
record. If the treatment plan<br />
is not known upon discharge of<br />
the patient, the <strong>Cancer</strong> Registry<br />
contacts the appropriate physician’s<br />
office to ascertain if the first course<br />
of treatment was given at another<br />
institution. In some cases, patients<br />
initially refuse treatment or<br />
subsequently receive treatment<br />
after the first four months.<br />
<strong>Cancer</strong> Registry <strong>St</strong>aff<br />
Victoria Young, MBA, CTR<br />
<strong>Cancer</strong> Registry Coordinator<br />
Laquita Malone<br />
<strong>Cancer</strong> Data Technician<br />
Vacant<br />
<strong>Cancer</strong> Registrar<br />
19
Advanced medicine in the right hands. SM<br />
3001 W. Dr. Martin Luther King Jr. Blvd.<br />
Tampa, FL 33607<br />
www.stjosephstampa.com<br />
(813) 870-4991<br />
<strong>St</strong>. Joseph’s <strong>Hospital</strong>s Foundation relies on the generous support of our community to continually improve patient care at <strong>St</strong>. Joseph’s<br />
<strong>Hospital</strong>, <strong>St</strong>. Joseph’s Women’s <strong>Hospital</strong> and <strong>St</strong>. Joseph’s Children’s <strong>Hospital</strong> of Tampa. Funds contributed make possible new facilities<br />
and equipment, community education and outreach, and special programs to sustain excellence. Individuals, businesses and<br />
foundations provide funding through an array of programs, campaigns and events. For more information on how you can help, call<br />
(813) 872-0979 or visit www.stjosephshospital-foundation.org.<br />
sjb080418-0708