Vol. 2007, No. 15 (08/01/2007) PDF - Administrative Rules - Utah.gov
Vol. 2007, No. 15 (08/01/2007) PDF - Administrative Rules - Utah.gov
Vol. 2007, No. 15 (08/01/2007) PDF - Administrative Rules - Utah.gov
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
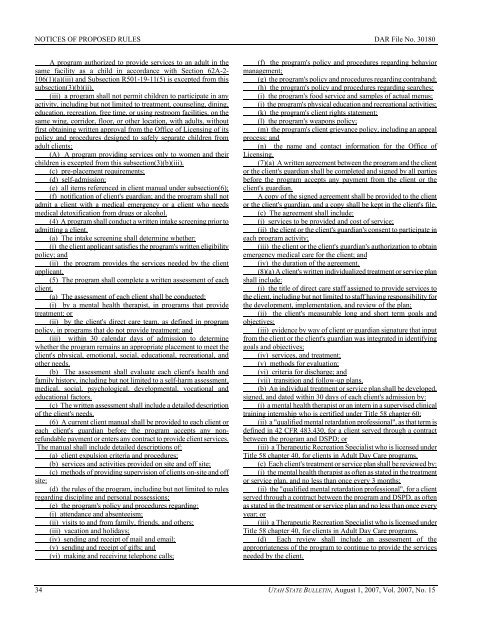
NOTICES OF PROPOSED RULES DAR File <strong>No</strong>. 3<strong>01</strong>80<br />
A program authorized to provide services to an adult in the<br />
same facility as a child in accordance with Section 62A-2-<br />
106(1)(a)(iii) and Subsection R5<strong>01</strong>-19-11(5) is excepted from this<br />
subsection(3)(b)(ii).<br />
(iii) a program shall not permit children to participate in any<br />
activity, including but not limited to treatment, counseling, dining,<br />
education, recreation, free time, or using restroom facilities, on the<br />
same wing, corridor, floor, or other location, with adults, without<br />
first obtaining written approval from the Office of Licensing of its<br />
policy and procedures designed to safely separate children from<br />
adult clients;<br />
(A) A program providing services only to women and their<br />
children is excepted from this subsection(3)(b)(iii).<br />
(c) pre-placement requirements;<br />
(d) self-admission;<br />
(e) all items referenced in client manual under subsection(6);<br />
(f) notification of client's guardian; and the program shall not<br />
admit a client with a medical emergency or a client who needs<br />
medical detoxification from drugs or alcohol.<br />
(4) A program shall conduct a written intake screening prior to<br />
admitting a client.<br />
(a) The intake screening shall determine whether:<br />
(i) the client applicant satisfies the program's written eligibility<br />
policy; and<br />
(ii) the program provides the services needed by the client<br />
applicant.<br />
(5) The program shall complete a written assessment of each<br />
client.<br />
(a) The assessment of each client shall be conducted:<br />
(i) by a mental health therapist, in programs that provide<br />
treatment; or<br />
(ii) by the client's direct care team, as defined in program<br />
policy, in programs that do not provide treatment; and<br />
(iii) within 30 calendar days of admission to determine<br />
whether the program remains an appropriate placement to meet the<br />
client's physical, emotional, social, educational, recreational, and<br />
other needs.<br />
(b) The assessment shall evaluate each client's health and<br />
family history, including but not limited to a self-harm assessment,<br />
medical, social, psychological, developmental, vocational and<br />
educational factors.<br />
(c) The written assessment shall include a detailed description<br />
of the client's needs.<br />
(6) A current client manual shall be provided to each client or<br />
each client's guardian before the program accepts any nonrefundable<br />
payment or enters any contract to provide client services.<br />
The manual shall include detailed descriptions of:<br />
(a) client expulsion criteria and procedures;<br />
(b) services and activities provided on site and off site;<br />
(c) methods of providing supervision of clients on-site and off<br />
site;<br />
(d) the rules of the program, including but not limited to rules<br />
regarding discipline and personal possessions;<br />
(e) the program's policy and procedures regarding:<br />
(i) attendance and absenteeism;<br />
(ii) visits to and from family, friends, and others;<br />
(iii) vacation and holidays;<br />
(iv) sending and receipt of mail and email;<br />
(v) sending and receipt of gifts; and<br />
(vi) making and receiving telephone calls;<br />
(f) the program's policy and procedures regarding behavior<br />
management;<br />
(g) the program's policy and procedures regarding contraband;<br />
(h) the program's policy and procedures regarding searches;<br />
(i) the program's food service and samples of actual menus;<br />
(j) the program's physical education and recreational activities;<br />
(k) the program's client rights statement;<br />
(l) the program's weapons policy;<br />
(m) the program's client grievance policy, including an appeal<br />
process; and<br />
(n) the name and contact information for the Office of<br />
Licensing.<br />
(7)(a) A written agreement between the program and the client<br />
or the client's guardian shall be completed and signed by all parties<br />
before the program accepts any payment from the client or the<br />
client's guardian.<br />
A copy of the signed agreement shall be provided to the client<br />
or the client's guardian, and a copy shall be kept in the client's file.<br />
(c) The agreement shall include:<br />
(i) services to be provided and cost of service;<br />
(ii) the client or the client's guardian's consent to participate in<br />
each program activity;<br />
(iii) the client or the client's guardian's authorization to obtain<br />
emergency medical care for the client; and<br />
(iv) the duration of the agreement.<br />
(8)(a) A client's written individualized treatment or service plan<br />
shall include:<br />
(i) the title of direct care staff assigned to provide services to<br />
the client, including but not limited to staff having responsibility for<br />
the development, implementation, and review of the plan;<br />
(ii) the client's measurable long and short term goals and<br />
objectives;<br />
(iii) evidence by way of client or guardian signature that input<br />
from the client or the client's guardian was integrated in identifying<br />
goals and objectives;<br />
(iv) services, and treatment;<br />
(v) methods for evaluation;<br />
(vi) criteria for discharge; and<br />
(vii) transition and follow-up plans.<br />
(b) An individual treatment or service plan shall be developed,<br />
signed, and dated within 30 days of each client's admission by:<br />
(i) a mental health therapist or an intern in a supervised clinical<br />
training internship who is certified under Title 58 chapter 60;<br />
(ii) a "qualified mental retardation professional", as that term is<br />
defined in 42 CFR 483.430, for a client served through a contract<br />
between the program and DSPD; or<br />
(iii) a Therapeutic Recreation Specialist who is licensed under<br />
Title 58 chapter 40, for clients in Adult Day Care programs.<br />
(c) Each client's treatment or service plan shall be reviewed by:<br />
(i) the mental health therapist as often as stated in the treatment<br />
or service plan, and no less than once every 3 months;<br />
(ii) the "qualified mental retardation professional", for a client<br />
served through a contract between the program and DSPD, as often<br />
as stated in the treatment or service plan and no less than once every<br />
year; or<br />
(iii) a Therapeutic Recreation Specialist who is licensed under<br />
Title 58 chapter 40, for clients in Adult Day Care programs.<br />
(d) Each review shall include an assessment of the<br />
appropriateness of the program to continue to provide the services<br />
needed by the client.<br />
34 UTAH STATE BULLETIN, August 1, <strong>2007</strong>, <strong>Vol</strong>. <strong>2007</strong>, <strong>No</strong>. <strong>15</strong>






![Lynx avoidance [PDF] - Wisconsin Department of Natural Resources](https://img.yumpu.com/41279089/1/159x260/lynx-avoidance-pdf-wisconsin-department-of-natural-resources.jpg?quality=85)