THE JOURNAL OF TEHRAN UNIVERSITY HEART CENTER
THE JOURNAL OF TEHRAN UNIVERSITY HEART CENTER
THE JOURNAL OF TEHRAN UNIVERSITY HEART CENTER
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
Zohair Yousef Al-halees, MD , FRCSC, FACS<br />
King Faisal Heart Institute, Saudi Arabia<br />
Yadolah Dodge, PhD<br />
University of Neuchâtel, Switzerland<br />
Ali Dodge–Khatami, MD, PhD<br />
University of Hamburg- Eppendorf School of Medicne, Germany<br />
Iradj Gandjbakhch, MD<br />
Hopital Pitie, France<br />
Omer Isik, MD<br />
Yeditepe University, School of Medicine, Turkey<br />
Sami S. Kabbani, MD<br />
Damascus University Cardiovascular Surgical Center, Syria<br />
Kayvan Kamalvand, MD, FRCP, FACC<br />
William Harvey Hospital, United Kingdom<br />
Jean Marco, MD, FESC<br />
Centre Cardio- Thoracique de Monaco, France<br />
Ali Massumi, MD<br />
Texas Heart Institute, U. S. A<br />
Carlos-A. Mestres, MD<br />
University of Barcelona, Spain<br />
Hossien Ahmadi, MD<br />
Tehran University of Medical Sciences<br />
Shahin Akhondzadeh, PhD<br />
Tehran University of Medical Sciences<br />
Mohammad Alidoosti, MD<br />
Tehran University of Medical Sciences<br />
Mohammad Ali Boroumand, MD<br />
Tehran University of Medical Sciences<br />
Gholamreza Davoodi, MD<br />
Tehran University of Medical Sciences<br />
Ahmad Reza Dehpour, PhD<br />
Tehran University of Medical Sciences<br />
Alimohammad Haji Zeinali, MD<br />
Tehran University of Medical Sciences<br />
Abbasali Karimi, MD<br />
Tehran University of Medical Sciences<br />
Ali Kazemi Saeed, MD<br />
Tehran University of Medical Sciences<br />
Seyed Ebrahim Kassaian, MD<br />
Tehran University of Medical Sciences<br />
Davood Kazemi Saleh, MD<br />
Baghiatallah University of Medical Sciences<br />
Majid Maleki, MD<br />
Tehran University of Medical Sciences<br />
Mehrab Marzban, MD<br />
Shahid Beheshti University of Medical Sciences<br />
<strong>THE</strong><br />
<strong>JOURNAL</strong> <strong>OF</strong> <strong>TEHRAN</strong><br />
<strong>UNIVERSITY</strong> <strong>HEART</strong><br />
<strong>CENTER</strong><br />
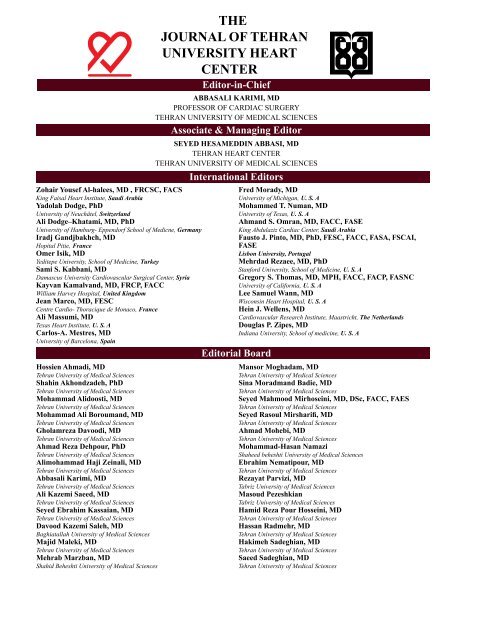
Editor-in-Chief<br />
ABBASALI KARIMI, MD<br />
PR<strong>OF</strong>ESSOR <strong>OF</strong> CARDIAC SURGERY<br />
<strong>TEHRAN</strong> <strong>UNIVERSITY</strong> <strong>OF</strong> MEDICAL SCIENCES<br />
Associate & Managing Editor<br />
SEYED HESAMEDDIN ABBASI, MD<br />
<strong>TEHRAN</strong> <strong>HEART</strong> <strong>CENTER</strong><br />
<strong>TEHRAN</strong> <strong>UNIVERSITY</strong> <strong>OF</strong> MEDICAL SCIENCES<br />
International Editors<br />
Editorial Board<br />
Fred Morady, MD<br />
University of Michigan, U. S. A<br />
Mohammed T. Numan, MD<br />
University of Texas, U. S. A<br />
Ahmand S. Omran, MD, FACC, FASE<br />
King Abdulaziz Cardiac Center, Saudi Arabia<br />
Fausto J. Pinto, MD, PhD, FESC, FACC, FASA, FSCAI,<br />
FASE<br />
Lisbon University, Portugal<br />
Mehrdad Rezaee, MD, PhD<br />
Stanford University, School of Medicine, U. S. A<br />
Gregory S. Thomas, MD, MPH, FACC, FACP, FASNC<br />
University of California, U. S. A<br />
Lee Samuel Wann, MD<br />
Wisconsin Heart Hospital, U. S. A<br />
Hein J. Wellens, MD<br />
Cardiovascular Research Institute, Maastricht, The Netherlands<br />
Douglas P. Zipes, MD<br />
Indiana University, School of medicine, U. S. A<br />
Mansor Moghadam, MD<br />
Tehran University of Medical Sciences<br />
Sina Moradmand Badie, MD<br />
Tehran University of Medical Sciences<br />
Seyed Mahmood Mirhoseini, MD, DSc, FACC, FAES<br />
Tehran University of Medical Sciences<br />
Seyed Rasoul Mirsharifi, MD<br />
Tehran University of Medical Sciences<br />
Ahmad Mohebi, MD<br />
Tehran University of Medical Sciences<br />
Mohammad-Hasan Namazi<br />
Shaheed beheshti University of Medical Sciences<br />
Ebrahim Nematipour, MD<br />
Tehran University of Medical Sciences<br />
Rezayat Parvizi, MD<br />
Tabriz University of Medical Sciences<br />
Masoud Pezeshkian<br />
Tabriz University of Medical Sciences<br />
Hamid Reza Pour Hosseini, MD<br />
Tehran University of Medical Sciences<br />
Hassan Radmehr, MD<br />
Tehran University of Medical Sciences<br />
Hakimeh Sadeghian, MD<br />
Tehran University of Medical Sciences<br />
Saeed Sadeghian, MD<br />
Tehran University of Medical Sciences
Mojtaba Salarifar, MD<br />
Tehran University of Medical Sciences<br />
Nizal Sarraf –Zadegan, MD<br />
Isfahan University of Medical Sciences<br />
Ahmad Yaminisharif, MD<br />
Tehran University of Medical Sciences<br />
Kiyomars Abbasi, MD<br />
Tehran University of Medical Sciences<br />
Seifollah Abdi, MD<br />
Tehran University of Medical Sciences<br />
Hassan Aghajani, MD<br />
Tehran University of Medical Sciences<br />
Alireza Amirzadegan, MD<br />
Tehran University of Medical Sciences<br />
Naser Aslanabadi, MD<br />
Tabriz University of Medical Sciences<br />
Carlo Briguori, MD<br />
Clinica Mediterranea Hospital, Naples, Italy<br />
Alaide Chieffo, MD<br />
San Raffaele Scientific Institute, Milano, Italy<br />
Sirous Darabian, MD<br />
St. John Cardiovascular Reserach Center, USA<br />
Saeed Davoodi, MD<br />
Tehran University of Medical Sciences<br />
Iraj Firoozi, MD<br />
Tehran University of Medical Sciences<br />
Seyed Khalil Foroozannia, MD<br />
Shaheed Sadoghi University of Medical Sciences<br />
Alfredo R. Galassi MD, FACC, FESC, FSCAI<br />
Cannizzaro Hospital, Catania, Italy<br />
Armen Gasparyan MD, PhD<br />
Armenia<br />
Ali Ghaemian, MD<br />
Mazandaran University of Medical Sciences<br />
Namvar Ghasemi Movahedi, MD<br />
Tehran University of Medical Sciences<br />
Abbas Ghiasi, MD<br />
Tehran University of Medical Sciences<br />
Mahmood Sheikh Fathollahi, PhD<br />
Arash Jalali, PhD<br />
Farshad Amouzadeh<br />
Fatemeh Esmaeili Darabi<br />
Advisory Board<br />
Statistical Consultant<br />
Technical Editors<br />
Graphic Design & Office<br />
Mohammad Reza Zafarghandi, MD<br />
Tehran University of Medical Sciences<br />
Aliakbar Zeinaloo, MD<br />
Tehran University of Medical Sciences<br />
Mohammad Jafar Hashemi, MD<br />
Tehran University of Medical Sciences<br />
Seyed Kianoosh Hoseini<br />
Tehran University of Medical Sciences<br />
Elise Langdon- Neuner<br />
European Medical Writers Association, Austria<br />
Jalil Majd Ardekani, MD<br />
Tehran University of Medical Sciences<br />
Fardin Mirbolook, MD<br />
Gilan University of Medical Sciences<br />
Mehdi Najafi, MD<br />
Tehran University of Medical Sciences<br />
Younes Nozari, MD<br />
Tehran University of Medical Sciences<br />
Mohammad Saheb Jam, MD & PT<br />
Tehran University of Medical Sciences<br />
Abbas Salehi Omran, MD<br />
Tehran University of Medical Sciences<br />
Mahmood Shabestari, MD<br />
Mashhad University of Medical Sciences<br />
Shapour Shirani, MD<br />
Tehran University of Medical Sciences<br />
Abbas Soleimani, MD<br />
Tehran University of Medical Sciences<br />
Seyed Abdolhosein Tabatabaei, MD<br />
Tehran University of Medical Sciences<br />
Murat Ugurlucan, MD<br />
Duzce Ataturk State Hospital, Turkey<br />
Arezou Zoroufian, MD<br />
Tehran University of Medical Sciences<br />
The Journal of Tehran University Heart Center is indexed in PubMed, PubMed Central, Scopus, EMBASE,<br />
CAB Abstracts, Global Health, Chemical Abstract Service, Cinahl, ProQuest, Google Scholar, DOAJ, EBSCO,<br />
Geneva Foundation for Medical Education and Research, Index Copernicus, Index Medicus for the WHO Eastern<br />
Mediterranean Region (IMEMR), ISC, SID, Iranmedex and Magiran<br />
Address<br />
North Kargar Street, Tehran Heart Center, Tehran, Iran. 1411713138. Tel: +98-21-88029720. Fax: +98-21-88029702.<br />
Web Site: http://jthc.tums.ac.ir. E-mail: jthc@tums.ac.ir.
<strong>TEHRAN</strong> <strong>HEART</strong> <strong>CENTER</strong><br />
Content<br />
Volume: 7 Number: 4 Autumn 2012<br />
The Journal of Tehran University Heart Center<br />
Review Article<br />
Prosthetic Tricuspid Valve Thrombosis: Three Case Reports and Literature Review<br />
Ahmad Yaminisharif, Mohammad Javad Alemzadeh-Ansari, Seyed Hossein Ahmadi ……………..…........................................................................... 147<br />
Original Articles<br />
Increased Carotid Artery Intima-Media Thickness in Pregnant Women with Gestational Diabetes Mellitus<br />
Gholamreza Yousefzadeh, Hashem Hojat, Ahmad Enhesari, Mostafa Shokoohi, Nahid Eftekhari, Mehrdad Sheikhvatan …………….....………………. 156<br />
Right Ventricular Myocardial Tissue Velocities, Myocardial Performance Index, and Tricuspid Annular Plane<br />
Systolic Excursion in Totally Corrected Tetralogy of Fallot Patients<br />
Asadolah Tanasan, Keyhan Sayadpour Zanjani, Armen Kocharian, Abdolrazagh Kiani, Mohammad Ali Navabi ……………...……............................ 160<br />
Anatomy of Atrioventricular Node Artery and Pattern of Dominancy in Normal Coronary Subjects: A<br />
Comparison Between Individuals With and Without Isolated Right Bundle Branch Block<br />
Ali Kazemisaeid, Marziyeh Pakbaz, Ahmad Yaminisharif, Gholamreza Davoodi, Masoumeh Lotfi Tokaldany, Elham Hakki Kazazi ……..................... 164<br />
Determinants of Length of Stay in Surgical Ward after Coronary Bypass Surgery: Glycosylated Hemoglobin as<br />
a Predictor in All Patients, Diabetic or Non-Diabetic<br />
Mahdi Najafi, Hamidreza Goodarzynejad …………….......………..........................….................................................................................................... 170<br />
Obvious or Subclinical Right Ventricular Dysfunction in Diabetes Mellitus (Type II): An Echocardiographic<br />
Tissue Deformation Study<br />
Mozhgan Parsaee, Parvaneh Bahmanziari, Maryam Ardeshiri, Maryam Esmaeilzadeh ……...........….....................................................................…… 177<br />
Case Reports<br />
Surgical Treatment of Amplatzer Embolus in a Secundum Atrial Septal Defect Patient<br />
Ahmet Baris Durukan, Hasan Alper Gurbuz, Murat Tavlasoglu, Nevriye Salman, Halil Ibrahim Ucar, Cem Yorgancioglu ………….……….............. 182<br />
Post-Traumatic Chordae Rupture of Tricuspid Valve<br />
Kyomars Abbasi, Hossein Ahmadi, Arezoo Zoroufian, Mohammad Sahebjam, Naghmeh Moshtaghi, Seyed Hessamedin Abbasi ................................ 185<br />
Late Diagnosis of Large Left Ventricular Pseudoaneurysm after Mitral Valve Replacement and Coronary Artery<br />
Bypass Surgery by Real-Time Three-Dimensional Echocardiography<br />
Mohammad Sahebjam, Abbas Salehiomran, Neda Ghaffari-Marandi, Azam Safir …………….....………..…............................................................... 188<br />
Letter to the Editor<br />
A Memorandum of "World Heart Day 2012": Myocardial Infarction Mortality in Women in Birjand, 2008-2009<br />
Toba Kazemi, Gholam Reza Sharifzadeh …………........................................................................................................................................................... 191<br />
Photo Clinic<br />
Ball in Chest<br />
Mohammad Bagher Rahim, Mohammad Hossein Mandegar, Farideh Roshanali …………............................................................................................. 192<br />
The Journal of Tehran University Heart Center
<strong>TEHRAN</strong> <strong>HEART</strong> <strong>CENTER</strong>
<strong>TEHRAN</strong> <strong>HEART</strong> <strong>CENTER</strong><br />
Volume: 7 Number: 4<br />
Summary of Contents<br />
What you will find<br />
in this Issue<br />
Autumn 2012<br />
REVIEW ARTICLE<br />
147 Prosthetic Tricuspid Valve Thrombosis:<br />
Three Case Reports and Literature Review<br />
Ahmad Yaminisharif, MD, Mohammad Javad Alemzadeh-<br />
Ansari, MD * , Seyed Hossein Ahmadi, MD<br />
Tehran Heart Center, Tehran University of Medical Sciences,<br />
Tehran, Iran.<br />
*<br />
Mohammad Javad Alemzadeh-Ansari, Department of<br />
Cardiology, Tehran University of Medical Sciences, Tehran<br />
Heart Center, Karegar Street, Tehran, Iran. 1411713138.<br />
Tel: +98 21 88029600. Fax: +98 21 88029731. E-mail:<br />
aansari@razi.tums.ac.ir.<br />
common complication of prosthetic heart<br />
A valves is thrombosis. Although the incidence<br />
of prosthetic valve thrombosis (PVT) in the tricuspid<br />
position is high, there are not enough data on the<br />
management of it, in contrast to left-sided PVT.<br />
Here, we describe three cases of tricuspid PVT with<br />
three different management approaches: thrombolytic<br />
therapy; close observation with oral anticoagulants;<br />
and surgery. The first case was a woman who suffered<br />
from recurrent PVT, for which we successfully used<br />
Tenecteplase for second and third episodes. We<br />
employed Tenecteplase in this case for the first time in<br />
the therapy of tricuspid PVT. The second case had fixed<br />
leaflets in open position while being symptomless. At<br />
six months' follow-up, with the patient having taken<br />
oral anticoagulants, the motion of the leaflets was<br />
restricted and she was symptom-free. The last case<br />
was a woman who had a large thrombus in the right<br />
atrium immediately after mitral and tricuspid valvular<br />
replacement. The patient underwent re-replacement<br />
surgery and a new biological valve was implanted in<br />
the tricuspid position. Also, we review the literature<br />
on the pathology, signs and symptoms, diagnosis, and<br />
management of tricuspid PVT.<br />
ORIGINAL ARTICLES<br />
156 Increased Carotid Artery Intima-Media<br />
Thickness in Pregnant Women with<br />
Gestational Diabetes Mellitus<br />
GholamrezaYousefzadeh, MD 1 , Hashem Hojat, MD 1 , Ahmad<br />
Enhesari, MD 1 , Mostafa Shokoohi, MSc 2* , Nahid Eftekhari,<br />
MD 1 , Mehrdad Sheikhvatan, MD 3<br />
1<br />
Physiology Research Center, Kerman University of Medical<br />
Sciences, Kerman, Iran.<br />
2<br />
Research Center for Modeling in Health, Kerman University<br />
of Medical Sciences, Kerman, Iran.<br />
3<br />
Tehran Heart Center, Tehran University of Medical Sciences,<br />
Tehran, Iran.<br />
*<br />
Mostafa Shokoohi, Research Center for Modeling in Health,<br />
Kerman University of Medical Sciences, Jihad Blvd, Shariati Street,<br />
Azadi Square, Kerman, Iran. 7619813159. Tel: +98 341 2263983.<br />
Fax: +98 341 2264079. E-mail: shokouhi.mostafa@gmail.com.<br />
Background: Pregnant women with previous<br />
gestational diabetes mellitus are at increased<br />
risk of progressive carotid artery disorders. The current<br />
study evaluated carotid intima-media thickness (IMT)<br />
in pregnant women with gestational diabetes at two<br />
time points of mid-term and full-term pregnancy to<br />
determine whether gestational diabetes mellitus causes<br />
increased IMT.<br />
Conclusion: In conclusion, an impaired OGCT<br />
test is proven to be an independent risk factor for<br />
increased carotid IMT and subsequent coronary artery<br />
disease. Even with this small study, we were able to<br />
find an increased IMT after diabetes appearance, which<br />
might be used as an indicator of a potential increased<br />
vascular risk. Furthermore, IMT measurements in<br />
diabetic pregnant women could offer an opportunity<br />
to identify a high-risk group of women who might
<strong>TEHRAN</strong> <strong>HEART</strong> <strong>CENTER</strong><br />
benefit from early screening and preventive measures.<br />
These measures could include lifestyle interventions<br />
such as improving diet and physical activity as well as<br />
increased surveillance of blood pressure, serum lipids,<br />
and particularly blood glucose.<br />
160 Right Ventricular Myocardial Tissue<br />
Velocities, Myocardial Performance<br />
Index, and Tricuspid Annular Plane<br />
Systolic Excursion in Totally Corrected<br />
Tetralogy of Fallot Patients<br />
Asadolah Tanasan, MD 1 , Keyhan Sayadpour Zanjani,<br />
MD 2* , Armen Kocharian, MD 2 , Abdolrazagh Kiani, MD 2 ,<br />
Mohammad Ali Navabi, MD 2<br />
1<br />
Besat Hospital, Hamadan University of Medical Sciences,<br />
Hamadan, Iran.<br />
2<br />
Children’s Medical Center, Tehran University of Medical<br />
Sciences, Tehran, Iran.<br />
*<br />
Keyhan Sayadpour Zanjani, Assistant Professor of Pediatric<br />
Cardiology, Tehran University of Medical Sciences, Children’s<br />
Medical Center, No.62, Dr Gharib Street, Tehran, Iran. 1419733151.<br />
Tel: +98 21 66911029. Fax: +98 21 66930024. E-mail: sayadpour@<br />
tums.ac.ir.<br />
Background: Longer survival after the total<br />
repair of the Tetralogy of Fallot increases<br />
the importance of late complications such as right<br />
ventricular dysfunction. This is a prospective study<br />
of the right ventricular function in totally corrected<br />
Tetralogy of Fallot patients versus healthy children.<br />
Conclusion: RVMPI was significantly correlated<br />
with PR severity without the presence of a significant<br />
correlation between RVMPI (obtained by pulsed wave<br />
Doppler) and the RV function indices obtained by tissue<br />
Doppler imaging (EA, Aa, Ea/Aa, and Sa). We suggest<br />
that these indices, RVMPI by tissue Doppler and PRi,<br />
be measured basically at postoperative and follow-up<br />
evaluations. In addition, as TAPSE was significantly<br />
decreased in the totally corrected T<strong>OF</strong> patients and<br />
there was a significant correlation between TAPSE and<br />
Sa, we suggest that TAPSE be also measured as the<br />
global RV systolic function index.<br />
164 Anatomy of Atrioventricular Node Artery<br />
and Pattern of Dominancy in Normal<br />
Coronary Subjects: A Comparison between<br />
Individuals with and without Isolated<br />
Right Bundle Branch Block<br />
Ali Kazemisaeid, MD, Marziyeh Pakbaz, MD * , Ahmad<br />
Yaminisharif, MD, Gholamreza Davoodi, MD, Masoumeh<br />
Lotfi Tokaldany, MD, Elham Hakki Kazazi, MD<br />
Tehran Heart Center, Tehran University of Medical Sciences,<br />
Tehran, Iran.<br />
*<br />
Marziyeh Pakbaz, Department of Cardiology, Tehran University<br />
of Medical Sciences, Tehran Heart Center, North Kargar Street,<br />
Tehran, Iran.1411713138. Tel: +98 21 88029256. Fax: +98 21<br />
88029256. E-Mail: marzi.pakbaz@gmail.com.<br />
Background: Isolated right bundle branch block<br />
(RBBB) is a common finding in the general<br />
population. The atrioventricular node (AVN) artery<br />
contributes to the blood supply of the right bundle<br />
branch. Our hypothesis was that the anatomy of<br />
the AVN artery and the pattern of dominancy differ<br />
between subjects with and without RBBB.<br />
Conclusion: According to our observations, there<br />
was no relationship between the dominancy of the<br />
epicardial arteries and the presence of RBBB in<br />
subjects with normal coronary arteries. There was<br />
a great variation of the AVN artery origin. Non-crux<br />
origination of the AVN artery was more common than<br />
the crux origination in both groups, and the prevalence<br />
of non-crux origination of the AVN artery was<br />
significantly higher in the cases than in the controls.<br />
Origination of the AVN artery from the right circulatory<br />
system was more common in both groups and the<br />
prevalence of the right origin of the AVN artery was<br />
significantly higher in the cases than in the controls.<br />
The AVN artery most commonly originated from the<br />
dominant artery but not necessarily from the crux.<br />
170 Determinants of Length of Stay in Surgical<br />
Ward after Coronary Bypass Surgery:<br />
Glycosylated Hemoglobin as a Predictor in<br />
All Patients, Diabetic or Non-Diabetic<br />
Mahdi Najafi, MD * , Hamidreza Goodarzynejad, MD
1<br />
Tehran Heart Center, Tehran University of Medical Sciences,<br />
Tehran, Iran.<br />
*<br />
Mahdi Najafi, Assistant Professor of Anesthesiology, Tehran<br />
Heart Center, Tehran University of Medical Sciences, Tehran Heart<br />
Center, North Karegar Street, Tehran, Iran. 1411713138. Tel: +98 21<br />
88029600. Fax: +98 21 88029731. E-mail: najafik@sina.tums.ac.ir.<br />
Background: Reports on the determinants of<br />
morbidity in coronary artery bypass graft surgery<br />
(CABG) have focused on outcome measures such as<br />
length of postoperative stay in the Intensive Care Unit<br />
(ICU). We proposed that major comorbidities in the<br />
ICU hampered the prognostic effect of other weaker<br />
but important preventable risk factors with effect on<br />
patients’ length of hospitalization. So we aimed at<br />
evaluating postoperative length of stay in the ICU and<br />
surgical ward separately.<br />
Conclusion: Among the five predictors of the LOS<br />
in the surgical ward, three were the indices of glycemic<br />
control. HbA1c is the most reliable marker of outcome<br />
because its level is not influenced by perioperative<br />
events. Taking these findings into consideration,<br />
the prognostic role of HbA1c for the LOS following<br />
CABG is promising. We would, therefore, recommend<br />
its use as a simple predictor of outcome after cardiac<br />
surgery in daily practice.<br />
<strong>TEHRAN</strong> <strong>HEART</strong> <strong>CENTER</strong><br />
Background: Diabetes mellitus is capable of<br />
impairing the myocardial function. Several<br />
studies have documented the influential impact of<br />
diabetes mellitus on the left ventricular function. The<br />
right ventricular function plays a significant role in the<br />
overall myocardial contractility; hence, this study was<br />
undertaken to evaluate the effect of diabetes mellitus<br />
type II on the right ventricular function.<br />
Conclusion: Whether the RV diastolic abnormalities<br />
have prognostic implications in the clinical course of<br />
patients with DM type II remains to be investigated. We<br />
believe that serial echocardiography measurements are<br />
warranted in this diabetic population if the progression<br />
from subclinical RV involvement to symptomatic RV<br />
dysfunction is to be followed. In addition, subclinical<br />
RV systolic and diastolic abnormalities should be<br />
considered when planning pharmacotherapy to prevent<br />
the development of symptomatic RV dysfunction.<br />
CASE REPORTS<br />
182 Surgical Treatment of Amplatzer Embolus<br />
in a Secundum Atrial Septal Defect Patient<br />
Ahmet Baris Durukan, MD 1* , Hasan Alper Gurbuz, MD 1 ,<br />
Murat Tavlasoglu, MD 2 , Nevriye Salman, MD 1 , Halil Ibrahim<br />
Ucar, MD 1 , Cem Yorgancioglu, MD 1<br />
1<br />
Medicana International Ankara Hospital, Ankara, Turkey.<br />
2<br />
Diyarbakir Military Hospital, Diyarbakir, Turkey.<br />
177 Obvious or Subclinical Right Ventricular<br />
Dysfunction in Diabetes Mellitus (Type II):<br />
An Echocardiographic Tissue Deformation<br />
Study<br />
Mozhgan Parsaee, MD * , Parvaneh Bahmanziari, MD,<br />
Maryam Ardeshiri, MD, Maryam Esmaeilzadeh, MD<br />
Rajaei Cardiovascular, Medical and Research Center, Tehran<br />
University of Medical Sciences, Tehran, Iran.<br />
*<br />
Mozhgan Parsaee, Assistant Professor of Cardiology,<br />
Department of Echocardiography, Rajaei Cardiovascular, Medical<br />
and Research Center, Vali-Asr Ave. Adjacent to Mellat Park, Tehran,<br />
Iran. 1996911151. Tel: +98 21 23922930. Fax: +98 21 2055594.<br />
E-mail: parsaeemozhgan@yahoo.com.<br />
*<br />
Ahmet Baris Durukan, Medicana International Ankara<br />
Hospital, Umit Mahallesi 2463.sokak 4/18, 06810, Yenimahalle,<br />
Ankara, Turkey. Tel: +90 532 2273814. Fax: +90 312 2203170.<br />
E-mail: barisdurukan@yahoo.com.<br />
Transcatheter device closure of the ASD can lead<br />
to serious complications despite its advantages<br />
over surgical closure. But it should be kept in mind<br />
that even if most cases are successful, not only early,<br />
but also late complications may occur regardless<br />
of the size or type of the current devices. Surgical<br />
treatment of the complications may be mandatory<br />
and should be performed immediately, especially<br />
in cases of embolization. Surgery is quite effective<br />
in treatment, but it is a fact that operative mortality<br />
rises when surgery is performed for the treatment of<br />
complications. Operative mortality is much lower for<br />
primary surgical repair.
<strong>TEHRAN</strong> <strong>HEART</strong> <strong>CENTER</strong><br />
185 Post-Traumatic Chordae Rupture of<br />
Tricuspid Valve<br />
Kyomars Abbasi, MD, Hossein Ahmadi, MD, Arezoo<br />
Zoroufian, MD, Mohammad Sahebjam, MD, Naghmeh<br />
Moshtaghi, MD, Seyed Hessamedin Abbasi, MD *<br />
Tehran Heart Center, Tehran University of Medical Sciences,<br />
Tehran, Iran.<br />
*<br />
Seyed-Hesameddin Abbasi, Tehran University of<br />
Medical Sciences, Tehran Heart Center, North Kargar Street,<br />
Tehran, Iran. 1411713138. Tel: +98 21 88029720. Fax: +98 21<br />
88029702. E-mail: abbasi@tehranheartcenter.org.<br />
The two cases presented herein demonstrate<br />
that the rupture of the chordae tendineae of the<br />
tricuspid valve could be another cause of TR following<br />
blunt chest trauma. This is, however, a condition that<br />
can be repaired surgically without the need for valve<br />
replacement. Advances in echocardiography have<br />
enabled earlier diagnosis and ergo more effective<br />
treatment.<br />
We recommend that physicians working at<br />
emergency departments be on the alert for this<br />
potential complication of non-penetrating chest trauma<br />
and subject all patients admitted to the emergency<br />
department due to blunt chest trauma to TTE or TEE<br />
for accurate diagnosis.<br />
The LV pseudoaneurysm is an important<br />
complication that may occur late after MVR and<br />
thus necessitates due heed on the part of cardiologists<br />
and cardiac surgeons.<br />
LETTER TO <strong>THE</strong> EDITOR<br />
191 A Memorandum of "World Heart Day<br />
2012": Myocardial Infarction Mortality in<br />
Women in Birjand, 2008-2009<br />
Toba Kazemi, MD, Gholam Reza Sharifzadeh, MSc<br />
Valiassr Hospital, Birjand University of Medical Sciences<br />
(BUMS), Birjand, Iran.<br />
*<br />
Toba Kazemi, Associate Professor of Cardiology, Birjand<br />
University of Medical Sciences (BUMS), Valiassr Hospital, Ghafari<br />
Avenue, Birjand, Iran. 9717964151. Tel: +98 56 14443001-9. Fax:<br />
+98 56 14433004. E-mail: drtooba.kazemi@gmail.com.<br />
192 Ball in Chest<br />
PHOTO CLININC<br />
Mohammad Bagher Rahim, MD, Mohammad Hossein<br />
Mandegar, MD, Farideh Roshanali, MD *<br />
Shariati General Hospital, Tehran University of Medical<br />
Sciences, Tehran, Iran.<br />
188 Late Diagnosis of Large Left Ventricular<br />
Pseudoaneurysm after Mitral Valve<br />
Replacement and Coronary Artery Bypass<br />
Surgery by Real-Time Three-Dimensional<br />
Echocardiography<br />
*<br />
Farideh Roshanali, Shriati Hospital, North Kargar Street,<br />
Tehran, Iran. Tel: +98 912 3093151. Fax: +98 21 88797353. E-mail:<br />
farideh_roshanali@yahoo.com.<br />
Mohammad Sahebjam, MD * , Abbas Salehiomran, MD, Neda<br />
Ghaffari-Marandi, MD, Azam Safir, MD<br />
Tehran Heart Center, Tehran University of Medical Sciences,<br />
Tehran, Iran.<br />
*<br />
Mohammad Sahebjam, Assistant Professor of Cardiology,<br />
Echocardiography Department, Tehran Heart Center, Jalal Al Ahmad<br />
and North Kargar Intersection, Tehran, Iran. 1411713138. Tel: +98 21<br />
88029600. Fax: +98 21 88029731. E-mail: msahebjam@yahoo.com.
<strong>TEHRAN</strong> <strong>HEART</strong> <strong>CENTER</strong><br />
Review Article<br />
Prosthetic Tricuspid Valve Thrombosis: Three Case Reports<br />
and Literature Review<br />
Ahmad Yaminisharif, MD, Mohammad Javad Alemzadeh-Ansari, MD * ,<br />
Seyed Hossein Ahmadi, MD<br />
Tehran Heart Center, Tehran University of Medical Sciences, Tehran, Iran.<br />
Received 24 January 2012; Accepted 17 June 2012<br />
Abstract<br />
A common complication of prosthetic heart valves is thrombosis. Although the incidence of prosthetic valve thrombosis<br />
(PVT) in the tricuspid position is high, there are not enough data on the management of it, in contrast to left-sided PVT.<br />
Here, we describe three cases of tricuspid PVT with three different management approaches: thrombolytic therapy; close<br />
observation with oral anticoagulants; and surgery. The first case was a woman who suffered from recurrent PVT, for which<br />
we successfully used Tenecteplase for second and third episodes. We employed Tenecteplase in this case for the first time in<br />
the therapy of tricuspid PVT. The second case had fixed leaflets in open position while being symptomless. At six months'<br />
follow-up, with the patient having taken oral anticoagulants, the motion of the leaflets was restricted and she was symptomfree.<br />
The last case was a woman who had a large thrombus in the right atrium immediately after mitral and tricuspid valvular<br />
replacement. The patient underwent re-replacement surgery and a new biological valve was implanted in the tricuspid<br />
position. Also, we review the literature on the pathology, signs and symptoms, diagnosis, and management of tricuspid PVT.<br />
J Teh Univ Heart Ctr 2012;7(4):147-155<br />
This paper should be cited as: Yaminisharif A, Alemzadeh-Ansari MJ, Ahmadi SH. Prosthetic Tricuspid Valve Thrombosis: Three<br />
Case Reports and Literature Review. J Teh Univ Heart Ctr 2012;7(4):147-155.<br />
Keywords: Tricuspid valve • Thrombosis • Thrombolytic therapy • Anticoagulants • Surgical procedures, operative<br />
Introduction<br />
Since the 1950s, more than 80 models of the prosthetic<br />
heart valve have been developed and used. 1 Prosthetic valve<br />
thrombosis (PVT), however, remains a serious complication<br />
and can even prove lethal. Overall, the incidence of<br />
thrombosis is reported to be between 0.1% and 5.7% per<br />
patient-year. 2 The incidence is 0.5% to 6% in the aortic and/<br />
or mitral positions and up to 20% in the tricuspid position,<br />
whereas the risk of thrombosis in spite of adequate oral<br />
anticoagulation has been estimated at between 1% and<br />
4% per year. 3 Although inadequate anticoagulant therapy<br />
remains the main cause of this complication, it seems that<br />
lower pressures on the right side of the heart with a slower<br />
blood flow across the tricuspid valve is the most important<br />
cause of higher risk of thrombus formation in prosthetic<br />
tricuspid valves. 4, 5 In contrast to left-sided PVT, there is a<br />
paucity of data on the various aspects of tricuspid PVT. We<br />
herein present three cases of tricuspid PVT with different<br />
management approaches, namely thrombolytic therapy,<br />
conservative management, and re-replacement surgery, and<br />
then review the relevant literature.<br />
*<br />
Corresponding Author: Mohammad Javad Alemzadeh-Ansari, Department of Cardiology, Tehran University of Medical Sciences, Tehran Heart<br />
Center, Karegar Street, Tehran, Iran. 1411713138. Tel: +98 21 88029600. Fax: +98 21 88029731. Email: aansari@razi.tums.ac.ir.<br />
The Journal of Tehran University Heart Center 147
The Journal of Tehran University Heart Center<br />
Case Reports<br />
Case # 1<br />
A 32-year-old woman was admitted to our hospital with<br />
the complaint of dyspnea (The New York Heart Association<br />
[NYHA] factional class III) in January, 2004. Transthoracic<br />
echocardiography (TTE) showed left ventricular ejection<br />
fraction of 55%, severe mitral stenosis, mild mitral<br />
regurgitation, severe aortic regurgitation with moderate to<br />
severe aortic stenosis, and severe tricuspid regurgitation<br />
with moderate to severe tricuspid stenosis. In April 2004,<br />
the patient underwent three valves replacement surgery,<br />
during which she received a 24-mm St. Jude Valve (St. Jude<br />
Medical, Inc., St. Paul, MN, USA) in the mitral position,<br />
a 31-mm St. Jude Valve (St. Jude Medical, Inc., St. Paul,<br />
MN, USA) in the tricuspid position, and a 19-mm Regent<br />
Mechanical Prosthesis (St. Jude Medical, Inc., St. Paul, MN,<br />
USA) in the aortic position. Also, due to persistent atrial<br />
fibrillation with a slow ventricular response, she underwent<br />
permanent transvenous epicardial pacemaker placement<br />
during hospitalization. Twenty-one days after valvular<br />
surgery, TTE revealed that the function and gradients of the<br />
three prosthetic valves were within the acceptable range and<br />
the peak and mean gradients in the prosthetic tricuspid valve<br />
were 5 mm Hg and 3 mm Hg, respectively. At the time of<br />
discharge, the patient’s international normalized ratio (INR)<br />
was 3.9. She was discharged from the hospital with the<br />
recommendation to use Warfarin (with goal INR 2.5 - 3.5)<br />
plus 80 mg Aspirin daily.<br />
In February, 2006, the patient was re-admitted with the<br />
complaint of fatigue and palpitation. The pacemaker had a<br />
normal function. At the time of presentation, her INR was<br />
2.5. TTE revealed that the prosthetic aortic and mitral vales<br />
had normal functions and gradients, whereas the prosthetic<br />
tricuspid valve had malfunction with high gradients.<br />
Fluoroscopic evaluation revealed that there was no motion<br />
in both leaflets of the prosthetic tricuspid valve, while the<br />
motion of both other prosthetic valves was complete and<br />
within the normal range. With the diagnosis of tricuspid<br />
PVT, the patient was prescribed 250,000 U of Streptokinase<br />
via a peripheral vein over thirty minutes, followed by an<br />
intravenous infusion of 100,000 U per hour of Streptokinase<br />
for forty-eight hours. On the next day, fluoroscopic<br />
evaluation showed no evidence of prosthetic tricuspid valve<br />
malfunction, and the mobility of both leaflets was completely<br />
restored. At discharge, the patient’s INR was 2.6. She was<br />
discharged from the hospital with the recommendation to use<br />
Warfarin (with goal INR 3.0 - 3.5) plus 80 mg of Aspirin<br />
daily.<br />
In November, 2006, the patient was re-admitted to our<br />
hospital with the complaint of atypical chest pain. At<br />
presentation, her INR was 1.8 and her other laboratory<br />
data and also electrocardiogram were unremarkable. TTE<br />
Ahmad Yaminisharif et al.<br />
revealed that the prosthetic aortic and mitral vales had<br />
normal functions and gradients, whereas the prosthetic<br />
tricuspid valve had malfunction with high gradients.<br />
Fluoroscopic evaluation revealed that both leaflets of the<br />
prosthetic tricuspid valve were fixed without any motion,<br />
whereas the motion of both other prosthetic valves was<br />
complete and within the normal range. With the diagnosis<br />
of recurrent tricuspid PVT, the patient was administered a<br />
total of 35 mg of Tenecteplase: 15 mg bolus, followed by<br />
20 mg for four hours (the patient’s weight was 64 kg). On<br />
the next day, fluoroscopic evaluation showed no evidence<br />
of prosthetic tricuspid valve malfunction, and the mobility<br />
of both leaflets was completely restored. Twelve days after<br />
the administration of Tenecteplase, TTE demonstrated that<br />
a significant reduction had occurred in the gradient across<br />
the prosthetic tricuspid valve (9.5 mm Hg peak gradient,<br />
4.9 mm Hg mean gradient). At discharge, the patient’s INR<br />
was 3.5. She was discharged from the hospital with the<br />
recommendation to use Warfarin (with goal INR 3.0 - 3.5)<br />
plus 80 mg of Aspirin daily.<br />
Because of the battery depletion of the pacemaker, the<br />
patient was re-admitted for generator replacement on October<br />
30, 2011. She had discontinued Aspirin two years previously<br />
due to gastrointestinal problems. She complained of atypical<br />
chest pain of two months’ duration, but her myocardial<br />
perfusion scan was normal. TTE showed left ventricular<br />
ejection fraction of 55%, severe increased gradient in the<br />
prosthetic tricuspid valve with no paravalvular leakage, and<br />
normal function of the mitral and aortic prosthetic valves.<br />
Fluoroscopic evaluation of the prosthetic tricuspid valve<br />
revealed a severe drop in the motion of both leaflets. The<br />
patient was candidated for thrombolytic therapy with the<br />
diagnosis of recurrent tricuspid PVT. A single dose of 35<br />
mg of Tenecteplase was administrated via a peripheral vein,<br />
according to the dosing regimen used for acute myocardial<br />
infarction (the patient’s weight was 65 kg). Fluoroscopic<br />
evaluation exhibited no evidence of prosthetic tricuspid<br />
valve malfunction, and the mobility of both leaflets was<br />
completely restored. Seven days later, TTE demonstrated that<br />
a significant reduction had occurred in the gradients across<br />
the prosthetic tricuspid valve (9 mm Hg peak gradient, 4 mm<br />
Hg mean gradient). She was discharged from the hospital<br />
with the recommendation to use Warfarin (with goal INR<br />
3.0 - 3.5) plus 80 mg of Aspirin daily. Table 1 illustrates the<br />
three episodes of tricuspid PVT in our patient and the three<br />
successful methods for thrombolytic therapy.<br />
Case # 2<br />
A 49-year-old woman was admitted to our hospital for the<br />
replacement of the generator of a pacemaker in May 2011.<br />
Thirteen years previously in another center, because of severe<br />
aortic regurgitation and severe tricuspid regurgitation, she<br />
148
Prosthetic Tricuspid Valve Thrombosis: Three Case Reports and Literature Review<br />
<strong>TEHRAN</strong> <strong>HEART</strong> <strong>CENTER</strong><br />
Table 1. Three episodes of tricuspid PVT in case 1 and successful thrombolytic therapy<br />
Episode<br />
Time from valve<br />
replacement<br />
TTE findings in prosthetic tricuspid valve<br />
(before thrombolytic therapy) Thrombolytic drug Dosage<br />
Peak gradient<br />
Mean gradient<br />
1 22 months 14 mm Hg 11 mm Hg Streptokinase<br />
2 31 months 22 mm Hg 10 mm Hg Tenecteplase<br />
250,000 U loading dose followed<br />
by 100,000 U/h for 48 hours<br />
15 mg bolus, followed by 20 mg<br />
for 4 hours<br />
3 93 months 17 mm Hg 8.5 mm Hg Tenecteplase 35 mg bolus<br />
PVT, Prosthetic valve thrombosis; TTE, Transthoracic echocardiogram<br />
had undergone two valves replacement surgery, during which<br />
she received a 31-mm St. Jude Valve (St. Jude Medical, Inc.,<br />
St. Paul, MN, USA) in the tricuspid position and a 21-mm St.<br />
Jude Valve (St. Jude Medical, Inc., St. Paul, MN, USA) in the<br />
aortic position. After surgery, due to the presence of complete<br />
heart block, she underwent permanent epicardial pacemaker<br />
placement during hospitalization. But during this period, she<br />
was admitted frequently because of infection at the site of the<br />
pacemaker. At the time of recent presentation, her INR was<br />
1.9. TTE revealed that the prosthetic aortic valve had normal<br />
function and gradients, whereas the prosthetic tricuspid<br />
valve had malfunction with high gradients (15 mm Hg peak<br />
gradient, 10 mm Hg mean gradient). Fluoroscopic evaluation<br />
revealed that the motion of one leaflet of the prosthetic<br />
tricuspid valve was very restricted, while the other leaflet<br />
was fixed in an open position. The patient was symptomless.<br />
On physical examination, except for a holosystolic murmur<br />
at the left lower sternal border, there were no signs of heart<br />
failure. With the diagnosis of tricuspid PVT, the patient was<br />
administered 250,000 U of Streptokinase via a peripheral<br />
vein over thirty minutes, followed by an intravenous infusion<br />
of 100,000 U per hour of Streptokinase for forty-eight<br />
hours. Fluoroscopic evaluation showed no improvement<br />
in the motion of the leaflets. The patient was candidated<br />
for tricuspid valve replacement, but because of fungal<br />
infection in the pacemaker pocket and lead, replacement of<br />
the prosthetic valve or the generator was not performed. She<br />
was discharged from the hospital with the recommendation<br />
to use antibiotics with Warfarin (with goal INR 3.0 - 3.5)<br />
plus 80 mg of Aspirin daily. Six months later, she referred<br />
to our clinic; she had no signs or symptoms of heart failure.<br />
She was re-admitted for the replacement of the generator of<br />
the pacemaker. Before replacement, fluoroscopic evaluation<br />
showed no evidence of improvement in the motion of the<br />
prosthetic tricuspid valve leaflets. Because the patient was<br />
symptom-free, did not respond to thrombolytic therapy, and<br />
had a high risk for infection after valve replacement, surgery<br />
for valve replacement was not performed. After generator<br />
replacement, she was discharged with the recommendation<br />
to use Warfarin (with goal INR 3.0 - 3.5) plus 80 mg of<br />
Aspirin daily.<br />
Case # 3<br />
A 28-year-old woman was admitted to our hospital with the<br />
complaint of orthopnea and dyspnea (NYHA factional class<br />
III) in September, 2008. The electrocardiogram revealed<br />
atrial fibrillation. TTE showed left ventricular ejection<br />
fraction of 40%, severe mitral stenosis, severe tricuspid<br />
regurgitation, and a large mobile clot in the left atrium (2.7<br />
× 2.0 cm). She underwent two valves replacement surgery,<br />
during which she received a 31-mm St. Jude Valve (St.<br />
Jude Medical, Inc., St. Paul, MN, USA) in the tricuspid<br />
position and a 29-mm St. Jude Valve (St. Jude Medical,<br />
Inc., St. Paul, MN, USA) in the mitral position. Also in the<br />
same section of surgery, TEE revealed a large mobile clot<br />
in the left atrium without any lesion in the other chambers;<br />
the large clot was removed. After surgery, she received an<br />
intravenous bolus dose of 5000 U of heparin, followed by<br />
intravenous heparin (20000 U per day in divided doses).<br />
Because of persistent atrial fibrillation with a low ventricular<br />
response after surgery, eleven days later, she underwent<br />
permanent transvenous epicardial pacemaker placement.<br />
However, during implantation, fluoroscopy revealed that<br />
the motion of one leaflet of the prosthetic tricuspid valve<br />
was very restricted. With the diagnosis of the malfunction<br />
of the prosthetic tricuspid valve, she was transferred to the<br />
operating room again. During the removal of the previous<br />
prosthetic tricuspid valve, a large clot was seen in the<br />
right atrium which was attached to the leaflet. Thus, all of<br />
the thrombus was removed and a new 29-mm Hancock II<br />
bioprosthesis (Medtronic Inc., Minneapolis, Minn.) was<br />
placed in the tricuspid position. Because of the displacement<br />
of the transvenous epicardial lead during surgery, a new<br />
epicardial lead was placed. After surgery, TEE demonstrated<br />
an acceptable gradient across the tricuspid valve (5 mm Hg<br />
peak gradient, 2 mm Hg mean gradient). She was discharged<br />
with the recommendation to use Warfarin (with goal INR 3.0<br />
- 3.5) plus 80 mg of Aspirin daily.<br />
The Journal of Tehran University Heart Center149
The Journal of Tehran University Heart Center<br />
Discussion<br />
Pathogenesis<br />
Many studies have demonstrated that the leading cause<br />
of PVT is subtherapeutic anticoagulation, which chimes<br />
in with the findings in our two cases. 6-10 This is most often<br />
due to either patient noncompliance or iatrogenic cessation<br />
of anticoagulants in preparation for another procedure.<br />
Furthermore, valve design and materials influence the<br />
incidence of thrombotic complications. Some mechanisms<br />
have a role in PVT formation such as molecular interactions<br />
and influence of transprosthetic blood flow. Molecular<br />
interaction occurs between corpuscular blood components,<br />
plasma, and artificial surfaces. The initial adsorption of<br />
plasma proteins (fibrinogen, fibronectin, von Willebrand<br />
factor, vitronectin, and thrombospondin) on the artificial<br />
surface is generally followed by platelet adhesion. The<br />
passage of blood through the prosthetic valve creates a<br />
turbulent flow with shear stress, which gives rise to a<br />
structurally and metabolically damaged endocardium and<br />
thus reduces its resistance to thrombosis. Also, subclinical<br />
hemolysis with the release of adenosine diphosphatase,<br />
platelet factor 4, beta-thromboglobulin, and other proteins<br />
triggers the activation of the plasma coagulation system.<br />
Other intrinsic factors can progress to thrombus formation;<br />
these factors include loss of active atrial contractions (atrial<br />
fibrillation), presence of some systemic diseases (e.g.<br />
systemic lupus erythematosus) or malignant tumors, and<br />
incomplete endothelization of the sewing ring. Use of some<br />
drugs such as contraceptives leads to hypercoagulability<br />
state 3, 11-14 Recently, Ricome et al. reported two cases of PVT<br />
secondary to heparin-induced thrombocytopenia. 15<br />
Type and position of the prosthetic valve and time from<br />
1, 13, 16, 17<br />
surgery can influence thrombus formation (Table 2).<br />
Additionally, some studies have indicated that season can be<br />
correlated with an increased risk for thrombotic events. 18-20<br />
Piper et al. reported that PVT during winter months occurred<br />
more frequently than in the other seasons. 13<br />
Signs and Symptoms<br />
In contrast to the acute presentation of left-sided PVT, the<br />
onset of the symptoms of tricuspid PVT is usually insidious,<br />
and its diagnosis is often delayed. Sometimes symptoms<br />
are so slight that the patient is likely to have suffered from<br />
them for months or even a year without feeling the need for<br />
referral to the hospital. 4 Sometimes, the patient even may<br />
have no symptoms related to the tricuspid vale thrombosis,<br />
and the thrombosis is detected only during routine clinical<br />
examination. 4, 6 However, the involvement of both leaflets is<br />
usually required to produce symptoms. 6 The most frequent<br />
symptoms related to tricuspid valve malfunction include<br />
4, 6,<br />
dyspnea, ascites, peripheral edema, and systemic emboli.<br />
21, 22<br />
Also, sometimes the disappearance or attenuation of the<br />
prosthetic valve noise may be reported by the patient and/<br />
or relatives. Moreover, in some cases where an interatrial<br />
communication is present, a pulmonary embolus or a leftsided<br />
embolic event may be the presenting manifestation of<br />
23, 24<br />
tricuspid PVT.<br />
It seems that physical examination may provide important<br />
clues for the diagnosis of tricuspid PVT, compared to the<br />
thrombosis of the left side, which normally has more severe<br />
symptoms. 25 Absence or muffling of prosthetic sounds<br />
in the tricuspid position might be noted. Other findings<br />
include auscultation of a new holosystolic murmur located<br />
at the left lower sternal border or in the subxiphoid region<br />
that may increase with inspiration or maneuvers that<br />
increase venous return (denoting the presence of tricuspid<br />
regurgitation), auscultation of a new murmur that is low in<br />
frequency, diastolic, located at the lower left sternal border<br />
or infraxiphoid area, and increases with inspiration and other<br />
maneuvers that increase tricuspid flow velocity (denoting<br />
tricuspid stenosis), or auscultation of a combination<br />
of murmurs that characterize both of these conditions.<br />
Sometimes mid-diastolic and/or pan-systolic murmurs can<br />
be heard in the tricuspid area (Zhang DY, Lozier J, Chang R,<br />
Sachdev V, Chen MY, Audibert JL, Horvath KA, Rosing DR.<br />
Case study and review: Treatment of tricuspid prosthetic<br />
valve thrombosis. Int J Cardiol 2011 Oct 14. [Epub ahead<br />
of print]).<br />
Diagnosis<br />
Ahmad Yaminisharif et al.<br />
The onset of the symptoms of tricuspid PVT is usually<br />
insidious and sometimes the patient has nonspecific<br />
symptoms or is even symptomless; therefore, suspicion of<br />
tricuspid PVT may be raised by physical findings, symptoms<br />
of heart failure, or rarely the diagnosis of embolization,<br />
especially in patients with poor anticoagulation therapy 8,<br />
17, 25<br />
NYHA has classified PVT in functional classes I to<br />
IV. The non-obstructive forms of PVT (NYHA functional<br />
Table 2. Thrombogenicity of mechanical prosthetic valve based on type, position, and time from surgery<br />
Lower<br />
Higher<br />
Valve type Bileaflet-tilting-disk Caged-ball single-tilting-disk<br />
Position Mitral or aortic Tricuspid<br />
Time from replacement After 3 months First 3 months<br />
150
Prosthetic Tricuspid Valve Thrombosis: Three Case Reports and Literature Review<br />
<strong>TEHRAN</strong> <strong>HEART</strong> <strong>CENTER</strong><br />
classes I or II) are usually incidental echocardiographic<br />
findings in patients with symptomless, nonspecific<br />
symptoms, or thromboembolic events. The obstructive<br />
forms (NYHA functional classes III or IV) correspond to<br />
obvious hemodynamic repercussions, sometimes including<br />
cardiogenic shock, and are often associated with cerebral or<br />
3, 11, 26<br />
peripheral embolism.<br />
Imaging modalities in patients with suspected PVT are<br />
aimed to evaluate leaflet immobilization, cause of leaflet<br />
immobilization (thrombus versus pannus or both), and<br />
whether thrombolytic therapy attempt in the patient would<br />
be successful. Usually the first modality for detecting<br />
prosthetic tricuspid valve dysfunction is TTE. Montorsi<br />
et al. reported that sensitivity, specificity, and positive and<br />
negative predictive values for the diagnosis of PVT in the<br />
mitral or aortic position by TTE were 75%, 64%, 57%, and<br />
78%, respectively. TTE, especially in experienced hands, can<br />
detect increased transvalvular gradients (mean of 6 mm Hg<br />
or higher, and peak of 15 mm Hg or higher), pressure halftime<br />
of 230 msec or higher, transvalvular gradients of 50%<br />
or higher than that observed before, wide intravalvular jet of<br />
tricuspid regurgitation, lower orifice area, visible thrombus<br />
on the prosthetic valve, and inability to demonstrate two<br />
different mobile echoes representing the valve leaflets<br />
in a high quality image. Indirect, nonspecific signs are an<br />
3, 6, 27<br />
enlarged right atrium and engorged inferior vena cava.<br />
After performance of TTE, the diagnosis should be<br />
confirmed by more specific modalities, namely fluoroscopy<br />
or TEE. 28 Fluoroscopy is a non-invasive method for<br />
detecting PVT, especially in patients with bileaflet prosthetic<br />
valves, and have high clinical suspicious for PVT and<br />
normal Doppler study. 29 Sensitivity, specificity, and positive<br />
and negative predictive values for the diagnosis of PVT in<br />
the mitral or aortic position by fluoroscopy are 87%, 78%,<br />
80%, and 91%. 28 Also, fluoroscopy has an important role for<br />
detecting the response to thrombolytic therapy. Thrombolysis<br />
significantly reduces the mean pressure gradient and<br />
improves valve leaflet opening angle. But some patients<br />
whose pressure gradient normalizes after thrombolytic<br />
infusion tend to continue to have concomitant abnormal<br />
leaflet motion at fluoroscopy, suggesting incomplete<br />
resolution of valve obstruction (pseudo responders). If lytic<br />
infusion is stopped at this time, the remaining thrombus<br />
could be the trigger for a late rethrombotic process. Thus,<br />
fluoroscopy should be carried out at regular intervals during<br />
therapy to confirm Doppler changes. 29<br />
TEE can correctly identify opening and closing angles in<br />
all patients, regardless of the prosthetic type. 30 TEE should<br />
be performed in selected patients even if fluoroscopy is<br />
negative because TEE is an invasive modality. On the other<br />
hand, fluoroscopy and TTE can correctly identify PVT in<br />
85% of all cases. Thus, fluoroscopy and TTE are quick,<br />
effective, and complementary diagnostic tools for the<br />
diagnosis of PVT in most patients. 28 Despite the scarcity of<br />
data on the role of TEE in diagnosing tricuspid PVT, it seems<br />
that if there is high clinical suspicion and other diagnostic<br />
modalities are not helpful, TEE will be help. 27 Furthermore,<br />
TEE is a superior modality for detecting the etiology of the<br />
obstruction (thrombus versus pannus), size, and location of<br />
the thrombus compared with TTE and fluoroscopy. 31<br />
Magnetic Resonance Imaging (MRI) and cardiac<br />
catheterization have limited diagnostic roles, because TEE and<br />
fluoroscopy can provide adequate data for decision-making.<br />
Since MRI is more expensive and time-consuming than<br />
echocardiography, it should be used only when prostheticvalve<br />
regurgitation or paravalvular leakage is suspected but<br />
not adequately visualized by echocardiography. 1 In contrast,<br />
Cardiac Multi-Detector Computer Tomography can provide<br />
sharp images to characterize quantitatively the reduced<br />
mobility of prosthetic leaflets or even directly visualize and<br />
distinguish between thrombus and pannus. 32-34<br />
Treatment<br />
There are different therapeutic modalities available for<br />
PVT such as heparin treatment, thrombolysis, surgery, or<br />
even in some cases only watchful waiting. Selecting one<br />
of these modalities is largely influenced by the presence of<br />
valvular obstruction, valve location (left- or right-sided), and<br />
clinical status. 6, 35 Surgery is more frequently performed for<br />
the treatment of left-sided PVT, not least in patients with<br />
either NYHA functional class III–IV symptoms or a large<br />
clot burden 36 and thrombolytic therapy is more favorable for<br />
right-sided PVT, because the risk of systemic embolization<br />
and recurrence rate is high by thrombolytic therapy in left-<br />
37, 38<br />
sided PVT.<br />
The conservative continued anticoagulation approach<br />
in patients with tricuspid PVT would only be appropriate<br />
if there is no significant hemodynamic compromise or<br />
a contraindication to either surgery or pharmacologic<br />
intervention is present. Shapira et al. reported that<br />
asymptomatic patients with tricuspid PVT who did not<br />
respond to thrombolytic therapy might be discharged from<br />
the hospital with long-term intensified anticoagulant therapy<br />
and close follow-up. The leaflet motion can be fully restored<br />
later. 6 However, Montorsi et al. proposed that leaflet mobility<br />
and duration of prosthetic valve symptoms were important<br />
factors in determining successful thrombolytic therapy. It<br />
may be because the amount of the thrombus that led to the<br />
stuck valve was minimal, thereby improving the chance of<br />
successful thrombolytic therapy. 29<br />
According the guidelines of the American Heart Association<br />
/American College of Cardiology (AHA/ACC) and the<br />
American College of Chest physicians (ACCP), in contrast to<br />
left-sided PVT, thrombolytic therapy is reasonable for rightsided<br />
PVT with NYHA functional class III-IV symptoms or<br />
a large clot burden. 36, 39 It is due to the high success rate and<br />
The Journal of Tehran University Heart Center151
The Journal of Tehran University Heart Center<br />
Ahmad Yaminisharif et al.<br />
low incidence of embolism compared to left-sided PVT. The<br />
European Society of Cardiology guideline also recommends<br />
thrombolytic therapy for tricuspid PVT, but this guideline<br />
does not mention the NYHA functional class or clot burden. 40<br />
Long-standing symptoms even more than a month should<br />
not make one reluctant to use thrombolytic therapy. 6 If<br />
thrombolytic therapy fails, the presence of a large thrombus<br />
or pannus should be considered, which may require surgical<br />
intervention (thrombectomy or valve replacement).<br />
In contrast to left-sided PVT, there is limited information<br />
about thrombolytic therapy for tricuspid PVT. Various<br />
thrombolytic agents have been used for PVT, including<br />
streptokinase, urokinases, and tissue-type plasminogen<br />
activator (tPA). The choice of the thrombolytic agent depends<br />
on several factors, including cost, time to attain maximal<br />
pharmacologic effect, half-life of the thrombolytic agent,<br />
and hemorrhagic complications. Amongst the above agents,<br />
streptokinase is cheaper and has lower cerebral hemorrhage<br />
rates. In contrast, tPA has a faster effect reversion and<br />
faster reach to maximal pharmacologic effect. 3 Roudaut<br />
et al. indicated that patients treated by streptokinase had a<br />
significantly full success rate compared to patients treated<br />
by tPA or urokinases (86%, 68%, and 59%, respectively).<br />
Nonetheless, combined therapy improved the results of<br />
thrombolytic therapy in all the groups. 41 Also, they concluded<br />
that full success by thrombolytic therapy was higher in<br />
patients in NYHA functional classes I or II; nevertheless,<br />
they did not find a significant difference between patients<br />
with tilting-discs and bileaflet valves, or between patients<br />
with first episode of thrombosis and recurrent thrombotic<br />
episodes groups. 41 The dosage and route of the administration<br />
of thrombolytic therapy are different in various studies.<br />
Hering et al. recommended using streptokinase by starting<br />
a bolus dose of 250,000 IU over thirty minutes, followed<br />
by an intravenous infusion of 100,000 IU per hour (same<br />
as the therapy of our patient in the first episode of PVT),<br />
urokinase by the same protocol used in patients with acute<br />
pulmonary embolism, and t-PA at a dosage of 100 mg given<br />
over a period of two to five hours. 14 Caceres-Loriga et al.<br />
recommended using streptokinase by starting a bolus dose of<br />
250,000 IU over three minutes, followed by an intravenous<br />
infusion of 100,000 IU per hour (maximum duration of<br />
seventy-two hours), urokinase by starting a bolus dose of<br />
4500 U/kg, followed by an intravenous infusion of 4500<br />
U/kg/h (maximum duration of twenty-four to forty-eight<br />
hours), and tPA by starting a bolus dose of 15 mg over five<br />
minutes, followed by an intravenous infusion of 95 mg over<br />
ninety minutes. 3 Manteiga et al. used the short-course of<br />
thrombolytic therapy as a first line for PVT: streptokinase<br />
by starting a bolus dose of 250,000 IU over twenty minutes,<br />
followed by an intravenous infusion of 1,500,000 IU over<br />
ninety minutes, or tPA by starting a bolus dose of 10 mg,<br />
followed by an intravenous infusion of 90 mg over ninety<br />
minutes. They concluded that a successful rate by these<br />
regimes was 82%. 42 However, Alpert recommended another<br />
dose for streptokinase in right-sided PVT (starting a dose of<br />
500,000 IU over twenty minutes, followed by an intravenous<br />
infusion of 1,500,000 IU over ninety minutes). 43 Some<br />
other investigators have used direct intra-atrial infusion of<br />
thrombolytic for PVT. 44, 45 For the first time, Zhang et al.<br />
reported a case of tricuspid PVT, which was successfully<br />
treated by an intra-right atrium infusion of tPA.<br />
Recently, Tenecteplase (a genetically engineered variant<br />
of tPA which has a longer half-life than tPA and is resistant<br />
to inactivation by plasminogen activator inhibitor-1 46 ) has<br />
been utilized for PVT. Our literature search shows that<br />
Tenecteplase has been used in limited case repots for mitral<br />
or aortic PVT. 47-52 Although Tenecteplase has been prescribed<br />
in different doses and via different methods, we used this<br />
thrombolytic according to the dosing regimen employed<br />
for acute myocardial infarction. Data on Tenecteplase for<br />
the treatment of PVT are limited. Still, Melandri et al. in a<br />
review study about patients with acute myocardial infarction<br />
showed that this drug had some advantages compared with<br />
tPA. These advantages included being more fibrin-specific,<br />
usability in a single bolus dose, and having less non-cerebral<br />
bleeding. Be that as it may, mortality rates and intracranial<br />
hemorrhage rates were similar to those of tPA. 46 For the first<br />
time, we reported a successful use of Tenecteplase in our<br />
case 1 for the treatment of two episodes of recurrent tricuspid<br />
PVT. It seems that this drug might be a suitable alternative<br />
for the other types of tPA in the future.<br />
If thrombolytic therapy is successful, a continuous<br />
infusion of unfractionated heparin is indicated and should<br />
be initiated. Moreover, activated partial thromboplastin<br />
time should be maintained at twofold the baseline values,<br />
followed by conversion to oral anticoagulation combined<br />
with Aspirin (50 to 100 mg per day). 39 In contrast to leftsided<br />
PVT, guidelines do not provide a recommended INR<br />
for prostheses in the tricuspid position. 36, 39, 40 For bileaflet<br />
prosthetic valves in the mitral position, a range of 2.5 - 3.5<br />
is recommended, 2.0 - 3.0 in the aortic position for patients<br />
without additional risk factors for thromboembolism. 39<br />
However, Shapira et al. recommended target INR levels of<br />
3.5 - 4.0 for patients with tricuspid prostheses 6 and Zhang<br />
et al., in order to prevent future thrombotic complications<br />
of tricuspid PVT, considered target INR levels of 3.0 - 3.5.<br />
Recurrent tricuspid PVT<br />
A major disadvantage of thrombolytic therapy is the<br />
relatively high incidence of recurrent thrombosis during<br />
follow-up; however, data are limited about rethrombosis<br />
after thrombolytic therapy of tricuspid PVT. Recurrent<br />
rates after thrombolytic therapy vary from 11% to 31%. 3,<br />
53-58<br />
Overall, risk of recurrent thrombosis after thrombolytic<br />
therapy in left-sided prosthetic valves is higher than that in<br />
152
Prosthetic Tricuspid Valve Thrombosis: Three Case Reports and Literature Review<br />
<strong>TEHRAN</strong> <strong>HEART</strong> <strong>CENTER</strong><br />
the tricuspid position. A meta-analysis showed that while<br />
the incidence of recurrent thrombosis in left-sided prosthetic<br />
valves was 20%, it was 14% in the tricuspid position. 14 As<br />
was mentioned earlier, the etiology of recurrent thrombosis<br />
is the same as that of the first episode. Also, the coexistence<br />
of thrombus and pannus tissue on a prosthetic valve is<br />
another factor that can explain the recurrence of PVT after<br />
successful thrombolytic therapy in a subset of patients. 53,<br />
56<br />
However, some recurrences may be the result of an<br />
uncompleted resolution of the initial thrombotic process<br />
rather than the result of a new thrombosis. Thus, after<br />
successful thrombolytic therapy, it is very important to<br />
follow up patients with serial clinical and echocardiographic<br />
examinations. 27 The results of rethrombolysis after PVT<br />
recurrence are comparable to those obtained after the first<br />
thrombolytic therapy, which is concordant with our case 1. 38,<br />
41, 58-62<br />
Therefore, rethrombolysis is safe with a high successful<br />
rate and is recommended in patients with recurrent tricuspid<br />
PVT.<br />
Choose a prosthetic valve: mechanical or biological<br />
Tricuspid valve replacement is one of the most challenging<br />
operations of cardiac surgery. Most cardiac surgeons<br />
undertake tricuspid valve surgery infrequently and usually<br />
perform tricuspid valve repair. Incidence of tricuspid<br />
valve replacement is approximately 0.7% of all valve<br />
replacements. 63 Although many studies have been performed<br />
to determine the preference between mechanical or biological<br />
valves in the tricuspid position, they have not reached the<br />
same conclusion yet. 63-69 As was mentioned before, because<br />
the risk of thrombosis is high in the tricuspid position and<br />
thrombus formation is lower in biological valves, 65, 66, 70 we<br />
recommend the use of biological valves in the tricuspid<br />
position, which is similar to that in re-replacement valve<br />
surgery (the same as our case 3).<br />
Conclusion<br />
Thrombosis in tricuspid prosthetic valves is high and<br />
in some cases, patients are symptom-free or have a mild<br />
complaint. Thus, regular visits after vale replacement are<br />
reasonable and if there is suspicion of PVT, other modalities<br />
(first TTE) are recommended. Herein, we reported three cases<br />
of tricuspid PVT with different conditions. The main cause<br />
of PVT in our cases was subtherapeutic anticoagulation. The<br />
first case was a woman who suffered from recurrent PVT. In<br />
this case we successfully used for the first time Tenecteplase<br />
for second and third episodes. Given that this drug can be<br />
used in a single dose and has acceptable efficacy compared<br />
to the other conventional thrombolytic agents, we would<br />
recommend Tenecteplase as a good alternative for PVT<br />
treatment. Also, this case shows us that thrombolytic therapy<br />
is a good option for recurrent tricuspid PVT, in contrast to<br />
left-sided PVT. The second case had fixed leaflets in open<br />
position, while the patient was symptomless. Thrombolytic<br />
therapy failed in this case; however, due to the patient’s<br />
chronic infection, we could not replace her valve. At six<br />
months’ follow-up, the motion of the leaflets was restricted<br />
and she was symptom-free. Thus, if thrombolytic therapy<br />
fails, surgery is not possible, the patient is symptom-free,<br />
and hemodynamic is stable, close observation with oral<br />
anticoagulant would be a reasonable course of action. The<br />
last case was a woman who had a large thrombus in the<br />
right atrium immediately after mitral and tricuspid valve<br />
replacement. We think that the cause of thrombus formation<br />
in this case was inadequate anticoagulation therapy. The<br />
patient underwent re-replacement surgery and a new<br />
biological valve was implanted in the tricuspid position.<br />
References<br />
1. Butany J, Ahluwalia MS, Munroe C, Fayet C, Ahn C, Blit P, Kepron<br />
C, Cusimano RJ, Leask RL. Mechanical heart valve prostheses:<br />
identification and evaluation (erratum). Cardiovascular Pathology<br />
2003;12:322-344.<br />
2. Vongpatanasin W, Hillis LD, Lange RA. Prosthetic heart valves. N<br />
Engl J Med 1996;335:407-416.<br />
3. Caceres-Loriga FM, Perez-Lopez H, Santos-Gracia J, Morlans-<br />
Hernandez K. Prosthetic heart valve thrombosis: pathogenesis,<br />
diagnosis and management. Int J Cardiol 2006;110:1-6.<br />
4. Thorburn CW, Morgan JJ, Shanahan MX, Chang VP. Long-term<br />
results of tricuspid valve replacement and the problem of prosthetic<br />
valve thrombosis. Am J Cardiol 1983;51:1128-1132.<br />
5. Minami K, Horstkotte D, Schulte HD, Bircks W. Thrombosis of<br />
two St. Jude Medical prostheses in one patient after triple valve<br />
replacement. Case report and review of the literature. Eur J<br />
Cardiothorac Surg 1988;2:48-52.<br />
6. Shapira Y, Sagie A, Jortner R, Adler Y, Hirsch R. Thrombosis of<br />
bileaflet tricuspid valve prosthesis: clinical spectrum and the role<br />
of nonsurgical treatment. Am Heart J 1999;137:721-725.<br />
7. Buttard P, Bonnefoy E, Chevalier P, Marcaz PB, Robin J, Obadia<br />
JF, Kirkorian G, Touboul P. Mechanical cardiac valve thrombosis in<br />
patients in critical hemodynamic compromise. Eur J Cardiothorac<br />
Surg 1997;11:710-713.<br />
8. Lengyel M, Fuster V, Keltai M, Roudaut R, Schulte HD, Seward<br />
JB, Chesebro JH, Turpie AG. Guidelines for management of leftsided<br />
prosthetic valve thrombosis: a role for thrombolytic therapy.<br />
Consensus Conference on Prosthetic Valve Thrombosis. J Am Coll<br />
Cardiol 1997;30:1521-1526.<br />
9. Deviri E, Sareli P, Wisenbaugh T, Cronje SL. Obstruction of<br />
mechanical heart valve prostheses: clinical aspects and surgical<br />
management. J Am Coll Cardiol 1991;17:646-650.<br />
10. Kawano H, Oda T, Fukunaga S, Tayama E, Kawara T, Oryoji<br />
A, Aoyagi S. Tricuspid valve replacement with the St. Jude<br />
Medical valve: 19 years of experience. Eur J Cardiothorac Surg<br />
2000;18:565-569.<br />
11. Silber H, Khan SS, Matloff JM, Chaux A, DeRobertis M, Gray R.<br />
The St. Jude valve. Thrombolysis as the first line of therapy for<br />
cardiac valve thrombosis. Circulation 1993;87:30-37.<br />
12. Edmunds LH, Jr. Thrombotic and bleeding complications of<br />
prosthetic heart valves. Ann Thorac Surg 1987;44:430-445.<br />
13. Piper C, Hering D, Horstkotte D. Prosthetic valve thrombosis.<br />
predisposition and diagnosis. Eur Heart J Supplements 2001;3:Q16-21.<br />
The Journal of Tehran University Heart Center153
The Journal of Tehran University Heart Center<br />
Ahmad Yaminisharif et al.<br />
14. Hering D, Piper C, Horstkotte D. Management of prosthetic valve<br />
thrombosis. Eur Heart J Supplements 2001;3:Q22-26.<br />
15. Ricome S, Provenchere S, Aubier B, Ajzenberg N, Lepage L, Dilly<br />
MP, Dufour G, Montravers P, Longrois D. Two cases of valvular<br />
thrombosis secondary to heparin-induced thrombocytopenia<br />
managed without surgery. Circulation 2011;123:1355-1357.<br />
16. Cevik C, Izgi C, Dechyapirom W, Nugent K. Treatment of<br />
prosthetic valve thrombosis: rationale for a prospective randomized<br />
clinical trial. J Heart Valve Dis 2010;19:161-170.<br />
17. Pibarot P, Dumesnil JG. Prosthetic heart valves: selection of<br />
the optimal prosthesis and long-term management. Circulation<br />
2009;119:1034-1048.<br />
18. Wilhelmsen L, Svardsudd K, Korsan-Bengtsen K, Larsson B,<br />
Welin L, Tibblin G. Fibrinogen as a risk factor for stroke and<br />
myocardial infarction. N Engl J Med 1984;311:501-505.<br />
19. Kannel WB, Wolf PA, Castelli WP, D›Agostino RB. Fibrinogen<br />
and risk of cardiovascular disease. The Framingham Study. JAMA<br />
1987;258:1183-1186.<br />
20. Alderson M. Season and mortality. Health Trends 1985;17:87-96.<br />
21. Kao CL, Lu MS, Chang JP, Yang TY, Cheng HW. Thrombotic<br />
obstruction of a mechanical prosthetic valve in tricuspid position.<br />
Tex Heart Inst J 2009;36:261-263.<br />
22. Suwansirikul S, Glassman E, Raia F, Spencer FC. Late thrombosis<br />
of Starr-Edwards tricuspid ball valve prosthesis. Am J Cardiol<br />
1974;34:737-740.<br />
23. Oxenham H, Bloomfield P, Wheatley DJ, Lee RJ, Cunningham J,<br />
Prescott RJ. Twenty year comparison of a Bjork-Shiley mechanical<br />
heart valve with porcine bioprostheses. Heart 2003;89:715-721.<br />
24. Hammermeister K, Sethi GK, Henderson WG, Grover FL, Oprian<br />
C, Rahimtoola SH. Outcomes 15 years after valve replacement<br />
with a mechanical versus a bioprosthetic valve: final report<br />
of the Veterans Affairs randomized trial. J Am Coll Cardiol<br />
2000;36:1152-1158.<br />
25. Shapira Y, Vaturi M, Sagie A. Obstructive left-sided prosthetic<br />
valve thrombosis. Acute Card Care 2009;11:160-168.<br />
26. Reddy NK, Padmanabhan TN, Singh S, Kumar DN, Raju PR,<br />
Satyanarayana PV, Rao DP, Rajagopal P, Raju BS. Thrombolysis<br />
in left-sided prosthetic valve occlusion: immediate and follow-up<br />
results. Ann Thorac Surg 1994;58:462-470.<br />
27. Zoghbi WA, Chambers JB, Dumesnil JG, Foster E, Gottdiener<br />
JS, Grayburn PA, Khandheria BK, Levine RA, Marx GR, Miller<br />
FA, Jr, Nakatani S, Quiñones MA, Rakowski H, Rodriguez LL,<br />
Swaminathan M, Waggoner AD, Weissman NJ, Zabalgoitia<br />
M; American Society of Echocardiography›s Guidelines and<br />
Standards Committee; Task Force on Prosthetic Valves; American<br />
College of Cardiology Cardiovascular Imaging Committee;<br />
Cardiac Imaging Committee of the American Heart Association;<br />
European Association of Echocardiography; European Society<br />
of Cardiology; Japanese Society of Echocardiography; Canadian<br />
Society of Echocardiography; American College of Cardiology<br />
Foundation; American Heart Association; European Association<br />
of Echocardiography; European Society of Cardiology;<br />
Japanese Society of Echocardiography; Canadian Society of<br />
Echocardiography. Recommendations for evaluation of prosthetic<br />
valves with echocardiography and doppler ultrasound: a report<br />
From the American Society of Echocardiography›s Guidelines<br />
and Standards Committee and the Task Force on Prosthetic Valves,<br />
developed in conjunction with the American College of Cardiology<br />
Cardiovascular Imaging Committee, Cardiac Imaging Committee<br />
of the American Heart Association, the European Association of<br />
Echocardiography, a registered branch of the European Society<br />
of Cardiology, the Japanese Society of Echocardiography and the<br />
Canadian Society of Echocardiography, endorsed by the American<br />
College of Cardiology Foundation, American Heart Association,<br />
European Association of Echocardiography, a registered branch<br />
of the European Society of Cardiology, the Japanese Society of<br />
Echocardiography, and Canadian Society of Echocardiography. J<br />
Am Soc Echocardiogr 2009;22:975-1014.<br />
28. Montorsi P, De Bernardi F, Muratori M, Cavoretto D, Pepi M.<br />
Role of cine-fluoroscopy, transthoracic, and transesophageal<br />
echocardiography in patients with suspected prosthetic heart valve<br />
thrombosis. Am J Cardiol 2000;85:58-64.<br />
29. Montorsi P, Cavoretto D, Alimento M, Muratori M, Pepi M.<br />
Prosthetic mitral valve thrombosis: can fluoroscopy predict the<br />
efficacy of thrombolytic treatment Circulation 2003;108:II79-84.<br />
30. Muratori M, Montorsi P, Teruzzi G, Celeste F, Doria E, Alamanni<br />
F, Pepi M. Feasibility and diagnostic accuracy of quantitative<br />
assessment of mechanical prostheses leaflet motion by transthoracic<br />
and transesophageal echocardiography in suspected prosthetic<br />
valve dysfunction. Am J Cardiol 2006;97:94-100.<br />
31. Barbetseas J, Nagueh SF, Pitsavos C, Toutouzas PK, Quiñones MA,<br />
Zoghbi WA. Differentiating thrombus from pannus formation in<br />
obstructed mechanical prosthetic valves: an evaluation of clinical,<br />
transthoracic and transesophageal echocardiographic parameters. J<br />
Am Coll Cardiol 1998;32:1410-1417.<br />
32. Tsai IC, Lin YK, Chang Y, Fu YC, Wang CC, Hsieh SR, Wei HJ,<br />
Tsai HW, Jan SL, Wang KY, Chen MC, Chen CC. Correctness<br />
of multi-detector-row computed tomography for diagnosing<br />
mechanical prosthetic heart valve disorders using operative<br />
findings as a gold standard. Eur Radiol 2009;19:857-867.<br />
33. Teshima H, Hayashida N, Fukunaga S, Tayama E, Kawara T,<br />
Aoyagi S, Uchida M. Usefulness of a multidetector-row computed<br />
tomography scanner for detecting pannus formation. Ann Thorac<br />
Surg 2004;77:523-526.<br />
34. Habets J, Symersky P, van Herwerden LA, de Mol BA, Spijkerboer<br />
AM, Mali WP, Budde RP. Prosthetic heart valve assessment with<br />
multidetector-row CT: imaging characteristics of 91 valves in 83<br />
patients. Eur Radiol 2011;21:1390-1396.<br />
35. Roudaut R, Serri K, Lafitte S. Thrombosis of prosthetic heart valves:<br />
diagnosis and therapeutic considerations. Heart 2007;93:137-142.<br />
36. Bonow RO, Carabello BA, Chatterjee K, de Leon AC, Jr, Faxon<br />
DP, Freed MD, Gaasch WH, Lytle BW, Nishimura RA, O›Gara<br />
PT, O›Rourke RA, Otto CM, Shah PM, Shanewise JS; American<br />
College of Cardiology/American Heart Association Task Force<br />
on Practice Guidelines. 2008 focused update incorporated into<br />
the ACC/AHA 2006 guidelines for the management of patients<br />
with valvular heart disease: a report of the American College of<br />
Cardiology/American Heart Association Task Force on Practice<br />
Guidelines (Writing Committee to revise the 1998 guidelines for<br />
the management of patients with valvular heart disease). Endorsed<br />
by the Society of Cardiovascular Anesthesiologists, Society for<br />
Cardiovascular Angiography and Interventions, and Society of<br />
Thoracic Surgeons. J Am Coll Cardiol 2008;52:e1-142.<br />
37. Ozkan M, Kaymaz C, Kirma C, Sönmez K, Ozdemir N, Balkanay<br />
M, Yakut C, Deligönül U. Intravenous thrombolytic treatment<br />
of mechanical prosthetic valve thrombosis: a study using<br />
serial transesophageal echocardiography. J Am Coll Cardiol<br />
2000;35:1881-1819.<br />
38. Lengyel M, Horstkotte D, Völler H, Mistiaen WP; Working Group<br />
Infection, Thrombosis, Embolism and Bleeding of the Society for<br />
Heart Valve Disease. Recommendations for the management of<br />
prosthetic valve thrombosis. J Heart Valve Dis 2005;14:567-575.<br />
39. Salem DN, O›Gara PT, Madias C, Pauker SG; American College of<br />
Chest Physicians. Valvular and structural heart disease: American<br />
College of Chest Physicians Evidence-Based Clinical Practice<br />
Guidelines (8th Edition). Chest 2008;133:593S-629S.<br />
40. Vahanian A, Baumgartner H, Bax J, Butchart E, Dion R, Filippatos<br />
G, Flachskampf F, Hall R, Iung B, Kasprzak J, Nataf P, Tornos P,<br />
Torracca L, Wenink A; Task Force on the Management of Valvular<br />
Hearth Disease of the European Society of Cardiology; ESC<br />
Committee for Practice Guidelines. Guidelines on the management<br />
of valvular heart disease: The Task Force on the Management of<br />
Valvular Heart Disease of the European Society of Cardiology. Eur<br />
Heart J 2007;28:230-268.<br />
41. Roudaut R, Lafitte S, Roudaut MF, Courtault C, Perron JM, Jaïs<br />
C, Pillois X, Coste P, DeMaria A. Fibrinolysis of mechanical<br />
prosthetic valve thrombosis: a single-center study of 127 cases. J<br />
Am Coll Cardiol 2003;41:653-658.<br />
154
Prosthetic Tricuspid Valve Thrombosis: Three Case Reports and Literature Review<br />
42. Manteiga R, Carlos Souto J, Altès A, Mateo J, Arís A, Dominguez<br />
JM, Borrás X, Carreras F, Fontcuberta J. Short-course thrombolysis<br />
as the first line of therapy for cardiac valve thrombosis. J Thorac<br />
Cardiovasc Surg 1998;115:780-784.<br />
43. Alpert JS. The thrombosed prosthetic valve: current<br />
recommendations based on evidence from the literature. J Am Coll<br />
Cardiol 2003;41:659-660.<br />
44. Desai S, Kavinsky C. Localized left atrial administration of tPA<br />
for the treatment of mechanical mitral valve thrombosis. Catheter<br />
Cardiovasc Interv 2008;72:151-155.<br />
45. Seltzer SM, Reed MD, Siwik ES. Intra-atrial tissue plasminogen<br />
activator infusion for prosthetic valve thrombosis. Catheter<br />
Cardiovasc Interv 2006;67:139-141.<br />
46. Melandri G, Vagnarelli F, Calabrese D, Semprini F, Nanni S,<br />
Branzi A. Review of tenecteplase (TNKase) in the treatment of<br />
acute myocardial infarction. Vasc Health Risk Manag 2009;5:249-<br />
256.<br />
47. Maegdefessel L, Issa H, Scheler C, Thäle V, Schlitt A, Hartelt U,<br />
Grabitz R, Buerke M. 27-year old pregnant woman with syncope<br />
and dyspnea after aortic alloplastic heart valve replacement 15<br />
years ago. Internist (Berl) 2008;49:868-872.<br />
48. Charokopos N, Antonitsis P, Artemiou P, Rouska E, Foroulis<br />
C, Papakonstantinou C. Acute mechanical prosthetic valve<br />
thrombosis after initiating oral anticoagulation therapy. Is bridging<br />
anticoagulation with heparin required Interact Cardiovasc Thorac<br />
Surg 2009;9:685-687.<br />
49. Ferreiro-Gutierrez JL, riza-Sole A, Manas-Jimenez P, Ruiz-Majoral<br />
A. Repeated thrombolysis with tenecteplase as a bridge to valvular<br />
replacement in a case of preoclusive mitral prosthetic thrombosis.<br />
Med Clin (Barc) 2009;133:402-403.<br />
50. Al-Sarraf N, Al-Shammari F, Al-Fadhli J, Al-Shawaf E. Successful<br />
thrombolysis of a thrombosed prosthetic mitral valve using a<br />
synthetic tissue plasminogen activator: a case report. J Med Case<br />
Rep 2010;4:241.<br />
51. Slaoui M, Cherradi R, Ounzar M, Massou S, Srairi JE. Thrombosis<br />
valvular prosthesis of Starr treated successfully by tenecteplase<br />
during pregnancy. Ann Fr Anesth Reanim 2010;29:500-501.<br />
52. Ayyub Ghori M, Bakir S, Ellahham S, Al Nassir A, Al Zubaidi A,<br />
Augustin N, Ayman Abdelaziz M, Patrick Turrin N, Al Mahmeed<br />
WA. Tenecteplase in prosthetic mitral valve thrombosis. J Saudi<br />
Heart Assoc 2011;23:93-95.<br />
53. Keuleers S, Herijgers P, Herregods MC, Budts W, Dubois C,<br />
Meuris B, Verhamme P, Flameng W, Van de Werf F, Adriaenssens<br />
T. Comparison of thrombolysis versus surgery as a first line therapy<br />
for prosthetic heart valve thrombosis. Am J Cardiol 2011;107:275-<br />
279.<br />
54. Gupta D, Kothari SS, Bahl VK, Goswami KC, Talwar KK,<br />
Manchanda SC, Venugopal P. Thrombolytic therapy for prosthetic<br />
valve thrombosis: short- and long-term results. Am Heart J<br />
2000;140:906-916.<br />
55. Cáceres-Lóriga FM, Pérez-López H, Morlans-Hernández K,<br />
Facundo-Sánchez H, Santos-Gracia J, Valiente-Mustelier J,<br />
Rodiles-Aldana F, Marrero-Mirayaga MA, Betancourt BY, López-<br />
Saura P. Thrombolysis as first choice therapy in prosthetic heart<br />
valve thrombosis. A study of 68 patients. J Thromb Thrombolysis<br />
2006;21:185-190.<br />
56. Lengyel M, Vandor L. The role of thrombolysis in the management<br />
of left-sided prosthetic valve thrombosis: a study of 85 cases<br />
diagnosed by transesophageal echocardiography. J Heart Valve Dis<br />
2001;10:636-649.<br />
57. Ozkan M, Kaymaz C, Kirma C, Sönmez K, Ozdemir N, Balkanay<br />
M, Yakut C, Deligönül U. Intravenous thrombolytic treatment<br />
of mechanical prosthetic valve thrombosis: a study using<br />
serial transesophageal echocardiography. J Am Coll Cardiol<br />
2000;35:1881-1889.<br />
58. Shapira Y, Herz I, Vaturi M, Porter A, Adler Y, Birnbaum Y,<br />
Strasberg B, Sclarovsky S, Sagie A. Thrombolysis is an effective<br />
and safe therapy in stuck bileaflet mitral valves in the absence of<br />
high-risk thrombi. J Am Coll Cardiol 2000;35:1874-1880.<br />
<strong>TEHRAN</strong> <strong>HEART</strong> <strong>CENTER</strong><br />
59. Cáceres-Lóriga FM, Pérez-López H, Santos-Gracia J, Morlans-<br />
Hernández K, Marrero-Mirayaga MA. Thrombolytic treatment as<br />
first option in recurrent tricuspid prosthetic valve thrombosis and<br />
Ebstein›s anomaly. J Pharm Pharm Sci 2005;8:332-334.<br />
60. Torrado González E, Ferriz Martín JA, Prieto Palomino MA,<br />
Rodríguez García JJ, Alvarez Bueno JM, Vera Almazán A, Garrido<br />
Alcalde MR, González de Vega N. Thrombolysis of thrombosed<br />
heart valve prostheses: presentation of 2 cases and review of the<br />
literature. Rev Esp Cardiol 1990;43:345-351.<br />
61. Shapira Y, Herz I, Birnbaum Y, Snir E, Vidne B, Sagie A. Repeated<br />
thrombolysis in multiple episodes of obstructive thrombosis in<br />
prosthetic heart valves: a report of three cases and review of the<br />
literature. J Heart Valve Dis 2000;9:146-149.<br />
62. Shapira Y, Vaturi M, Hasdai D, Battler A, Sagie A. The safety and<br />
efficacy of repeated courses of tissue-type plasminogen activator in<br />
patients with stuck mitral valves who did not fully respond to the<br />
initial thrombolytic course. J Thromb Haemost 2003;1:725-728.<br />
63. Ratnatunga CP, Edwards MB, Dore CJ, Taylor KM. Tricuspid<br />
valve replacement: UK Heart Valve Registry mid-term results<br />
comparing mechanical and biological prostheses. Ann Thorac Surg<br />
1998;66:1940-1947.<br />
64. Rizzoli G, Vendramin I, Nesseris G, Bottio T, Guglielmi C,<br />
Schiavon L. Biological or mechanical prostheses in tricuspid<br />
position A meta-analysis of intra-institutional results. Ann Thorac<br />
Surg 2004;77:1607-1614.<br />
65. Rizzoli G, De Perini L, Bottio T, Minutolo G, Thiene G, Casarotto<br />
D. Prosthetic replacement of the tricuspid valve: biological or<br />
mechanical Ann Thorac Surg 1998;66:S62-67.<br />
66. Kaplan M, Kut MS, Demirtas MM, Cimen S, Ozler A. Prosthetic<br />
replacement of tricuspid valve: bioprosthetic or mechanical. Ann<br />
Thorac Surg 2002;73:467-473.<br />
67. Chang BC, Lim SH, Yi G, Hong YS, Lee S, Yoo KJ, Kang MS,<br />
Cho BK. Long-term clinical results of tricuspid valve replacement.<br />
Ann Thorac Surg 2006;81:1317-1323.<br />
68. Filsoufi F, Anyanwu AC, Salzberg SP, Frankel T, Cohn LH, Adams<br />
DH. Long-term outcomes of tricuspid valve replacement in the<br />
current era. Ann Thorac Surg 2005;80:845-850.<br />
69. Dalrymple-Hay MJ, Leung Y, Ohri SK, Haw MP, Ross JK, Livesey<br />
SA, Monro JL. Tricuspid valve replacement: bioprostheses are<br />
preferable. J Heart Valve Dis 1999;8:644-648.<br />
70. Carrier M, Hébert Y, Pellerin M, Bouchard D, Perrault LP, Cartier<br />
R, Basmajian A, Pagé P, Poirier NC. Tricuspid valve replacement:<br />
an analysis of 25 years of experience at a single center. Ann Thorac<br />
Surg 2003;75:47-50.<br />
The Journal of Tehran University Heart Center155
The Journal of Tehran University Heart Center<br />
Original Article<br />
Increased Carotid Artery Intima-Media Thickness in<br />
Pregnant Women with Gestational Diabetes Mellitus<br />
Gholamreza Yousefzadeh, MD 1 , Hashem Hojat, MD 1 , Ahmad Enhesari, MD 1 ,<br />
Mostafa Shokoohi, MSc 2* , Nahid Eftekhari, MD 1 , Mehrdad Sheikhvatan, MD 3<br />
1<br />
Physiology Research Center, Kerman University of Medical Sciences, Kerman, Iran.<br />
2<br />
Research Center for Modeling in Health, Kerman University of Medical Sciences, Kerman, Iran.<br />
3<br />
Tehran Heart Center, Tehran University of Medical Sciences, Tehran, Iran.<br />
Received 04 February 2012; Accepted 13 May 2012<br />
Abstract<br />
Background: Pregnant women with previous gestational diabetes mellitus are at increased risk of progressive carotid<br />
artery disorders. The current study evaluated carotid intima-media thickness (IMT) in pregnant women with gestational<br />
diabetes at two time points of mid-term and full-term pregnancy to determine whether gestational diabetes mellitus causes<br />
increased IMT.<br />
Methods: This cross-sectional study carried out at Afzalipour Hospital (Kerman, Iran) between 2009 and 2010, recruited<br />
50 women who were at high risk of gestational diabetes during pregnancy and had an oral glucose challenge test (OGCT)<br />
as screening for gestational diabetes. B-mode ultrasound scans were performed at baseline and at two time points of midterm<br />
pregnancy (20 to 24 weeks) and full-term pregnancy (36 to 38 weeks) on all the participants. The mean IMT of common<br />
carotids and internal carotid arteries from two walls (near and far walls) at four different angles was assessed.<br />
Results: An overall comparison between the impaired OGCT test group and the control group revealed significant<br />
differences in carotid IMT in the mid-term (0.65 ± 0.07 vs. 0.59 ± 0.06 mm; p value = 0.002) and full-term (0.65 ± 0.05<br />
vs. 0.59 ± 0.04 mm; p value < 0.001) pregnancy; however, the trend of the changes in carotid IMT during mid to full-term<br />
pregnancy was insignificant in each group (p value > 0.05).<br />
Conclusion: Carotid IMT was significantly higher in the women with gestational diabetes than that in the normoglycemic<br />
group in different trimesters. This finding denotes that atherosclerosis might start years before the diagnosis of gestational<br />
diabetes in vulnerable women.<br />
J Teh Univ Heart Ctr 2012;7(4):156-159<br />
This paper should be cited as: Yousefzadeh G, Hojat H, Enhesari A, Shokoohi M, Eftekhari N, Sheikhvatan M. Increased Carotid<br />
Artery Intima-Media Thickness in Pregnant Women with Gestational Diabetes Mellitus. J TehUniv Heart Ctr 2012;7(4):156-159.<br />
Keywords: Pregnancy • Diabetes mellitus • Carotid arteries<br />
Introduction<br />
Screening for gestational diabetes mellitus is routinely<br />
programmed to prevent complications caused by elevated<br />
blood glucose levels in pregnancy, including macrosomia,<br />
Cesarean delivery, shoulder dystocia, neonatal metabolic<br />
problems, perinatal mortality, and pre-eclampsia. 1 Diabetes<br />
mellitus during pregnancy also appears to be associated<br />
*<br />
Corresponding Author: Mostafa Shokoohi, Research Center for Modeling in Health, Kerman University of Medical Sciences, Jihad Blvd, Shariati<br />
Street, Azadi Square, Kerman, Iran. 7619813159. Tel: +98 341 2263983. Fax: +98 341 2264079. E-mail: shokouhi.mostafa@gmail.com.<br />
156
Increased Carotid Artery Intima-Media Thickness in Pregnant Women with ...<br />
with an increased risk of cardiovascular diseases even in<br />
later life. 2 Moreover, this underlying co-morbidity is an<br />
independent risk factor for subsequent coronary artery<br />
disease. In this context, diabetes mellitus during pregnancy<br />
has been identified as a major etiology for atherosclerosis in<br />
large elastic arteries. 3<br />
One of the main indicators for assessing atherosclerotic<br />
lesions during this period is the increased intima-media<br />
thickness (IMT) of carotid arteries. 4 It has been well known<br />
that, as opposed to the blood flow through the other arteries of<br />
the maternal organs, the blood flow through the carotid artery<br />
is decreased during pregnancy, which has been attributed to<br />
pregnancy-mediated increased responsiveness of the carotid<br />
artery to vasoconstrictors and decreased responsiveness<br />
to vasodilators. 5 Also, the endothelial hypertrophy of the<br />
carotid artery can be a common finding, leading to changes<br />
in the carotid blood flow and its complications. 6, 7 Thus,<br />
increased carotid IMT can be deemed a validated endothelial<br />
dysfunction surrogate endpoint during pregnancy.<br />
Some studies have recently shown that pregnant women<br />
with previous gestational diabetes mellitus are at increased<br />
risk of carotid artery disorders. 8, 9 Be that as it may, the scarcity<br />
of research into this hypothesis means that it is still unknown<br />
whether or not gestational diabetes mellitus causes increased<br />
IMT. The current study was performed to evaluate carotid<br />
IMT in diabetic pregnant women with gestational diabetes<br />
and to ascertain if an impaired oral glucose challenge test<br />
(OGCT) correlates with the development of increased IMT.<br />
Methods<br />
This cohort study included 50 women ranging from<br />
18 to 35 years of age at high risk of diabetes during<br />
pregnancy. Gestational diabetes mellitus was screened<br />
with a one-hour 50 g oral glucose challenge test (OGCT).<br />
Abnormal results were, thereafter, confirmed with a threehour<br />
100 g oral glucose tolerance test (OGTT). Eligible<br />
women were nulliparous with a singleton pregnancy, had<br />
a normal blood pressure at the time of recruitment, and<br />
gave informed consent. Women with any of the following<br />
were excluded: family history of cardiovascular disorders;<br />
history of hypertension; anti-hypertensive and cholesterol<br />
medication use; hyperlipidemia; overt diabetes or fasting<br />
plasma glucose (FPG) > 125 mg/dl according to the<br />
American Diabetes Association (ADA) definition; 10 chronic<br />
renal or hepatic diseases; malignancies; recent hormonal<br />
medications; cigarette smoking; severe obesity (body<br />
mass index [BMI] > 35 kg/m 2 ); and history of infertility<br />
or polycystic ovarian disease. Those with the status of<br />
plaques/shadowing ( > 1.0 mm) at any carotid site were also<br />
excluded. The study protocol was approved by the Research<br />
and Ethics Committees at Kerman University of Medical<br />
Sciences.<br />
<strong>TEHRAN</strong> <strong>HEART</strong> <strong>CENTER</strong><br />
Baseline demographic variables were collected either<br />
from the women’s medical records or self-completed<br />
questionnaires at trial entry and comprised maternal age,<br />
height, weight, BMI, smoking status, and blood pressure<br />
at trial entry. Complete baseline data were available for<br />
all the women. All lipid and lipoprotein measurements<br />
were made at a central laboratory. Total cholesterol was<br />
measured enzymatically with standard methods and total<br />
triglyceride was measured via standard spectrophotometric<br />
techniques. After the precipitation of low-density lipoprotein<br />
(LDL) particle with phosphotungstic acid, high-density<br />
lipoprotein (HDL) cholesterol was measured enzymatically<br />
in the supernatant by a modification of the method for total<br />
cholesterol.<br />
B-mode ultrasound scans were performed at baseline<br />
and at two time points of mid-term pregnancy (20 to 24<br />
weeks) and full-term pregnancy (36 to 38 weeks) on all the<br />
participants. Carotid ultrasound scans were carried out by a<br />
single trained sonographer unaware of the study protocols<br />
and methodology. B-mode ultrasound images were equipped<br />
with a 7.5-MHz linear array transducer and captured with<br />
a GE log 200 ultrasound machine. The ultrasonic variable<br />
used in the statistical analysis was the mean of the IMT of<br />
common carotids and internal carotid arteries from two walls<br />
(near and far walls) at four different angles.<br />
The mean of carotid IMT was compared between the<br />
women with impaired OGCT and those who screened<br />
normal on OGCT at the two study time points. For the<br />
statistical analyses, the statistical software SPSS version<br />
19.0 for Windows (SPSS Inc., Chicago, IL) was used. The<br />
continuous variables, if normally distributed, were analyzed<br />
using the Student-test and presented as mean differences,<br />
while the Mann-Whitney test was employed for skewed<br />
data. A p value of 0.05 or less was considered to indicate<br />
statistical significance.<br />
Results<br />
The baseline characteristics of the pregnant women with<br />
impaired and normal OGCT tests are presented in Table 1.<br />
The two groups were similar in terms of pregnancy age,<br />
height, weight, BMI, and baseline laboratory parameters.<br />
There were no significant associations between carotid<br />
IMT and maternal indices, including the demographic<br />
variables and laboratory parameters.<br />
An overall comparison between the impaired OGCT test<br />
group and the control group via the Mann-Whitney U test<br />
revealed significant differences in carotid IMT in the midterm<br />
and full-term pregnancy (Table 2). The trend of the<br />
changes in carotid IMT during the mid-term to full-term<br />
pregnancy was, however, insignificant in each group.<br />
The Journal of Tehran University Heart Center157
The Journal of Tehran University Heart Center<br />
Gholamreza Yousefzadeh et al.<br />
Table 1. Demographic characteristics and clinical data of GDM versus non-GDM women *<br />
Characteristics<br />
GDM group<br />
(n=25)<br />
Non-GDM group<br />
(n=25)<br />
Age (y) 24.4±3.6 25.1±4.2 0.259<br />
Height (cm) 159.4±5.5 161.5±7.3 0.276<br />
Weight (kg) 72.8±11.5 68.7±10.9 0.225<br />
Body mass index (kg/m 2 ) 28.7±4.5 26.5±4.5 0.109<br />
Systolic BP (mm Hg) 110.0±9.4 107.6±8.0 0.369<br />
Diastolic BP (mm Hg) 69.0±10.4 65.2±8.5 0.192<br />
Serum HDL (mg/dL) 49.0±8.7 49.0±10.5 0.987<br />
Serum LDL (mg/dL) 140.7±37.4 137.7±36.0 0.780<br />
Fasting blood sugar (mg/dL) 85.3±13.7 83.2±19.8 0.680<br />
Serum triglyceride (mg/dL) 183.5±67.0 178.0±61.0 0.775<br />
Serum cholesterol (mg/dL) 219.0±54.7 223.8±43.8 0.746<br />
*<br />
Data are presented as mean±SD<br />
GDM, Gestational diabetes mellitus; BP, Blood pressure; HDL, High-density lipoprotein; LDL, Low-density lipoprotein<br />
P value<br />
Table 2. Differences in carotid IMT in GDM versus non-GDM women *<br />
CIMT<br />
Mid-term pregnancy<br />
(mm)<br />
Full-term<br />
pregnancy(mm)<br />
GDM group<br />
(n=25)<br />
Non-GDM group<br />
(n=25)<br />
P value **<br />
0.65±0.07 0.59±0.06 0.002<br />
0.65±0.05 0.59±0.04 < 0.001<br />
P value *** 0.989 0.992<br />
*<br />
Data are presented as mean±SD<br />
**<br />
Between groups comparison<br />
***<br />
Within groups comparison<br />
IMI, Intima-media thickness; GDM, Gestational diabetes mellitus; CIMT,<br />
Carotid intima-media thickness<br />
Discussion<br />
An increased carotid IMT can be observed not only in<br />
long-standing type II diabetic but also in newly detected type<br />
II diabetic patients. Especially in pregnant women, carotid<br />
IMT gradually increases from the first to the third trimester<br />
of normal pregnancy and regresses in the postpartum period.<br />
Nevertheless, the trend of the increase in pregnant women<br />
with gestational diabetes is still unclear. In our study, with the<br />
aid of carotid ultrasound, arterial examination was performed<br />
at mid-term and full-term pregnancy and both controls and<br />
the women with an impaired OGCT test were assessed<br />
and compared with regard to the changes in carotid IMT.<br />
We showed that although carotid IMT was more increased<br />
in those with impaired OGCT, the trend of this change was<br />
similar between the impaired and normal OGCT groups.<br />
Furthermore, we observed that carotid IMT was significantly<br />
higher in the diabetic group than in the normoglycemic<br />
group in different trimesters, but the trend of these gradual<br />
changes from the first to the third trimester was similar in<br />
both groups. Totally, effective glycemic control seems to be<br />
helpful for the prevention of increased carotid IMT.<br />
During the pregnancy period, peripheral vascular<br />
resistance is physiologically paralleled by improved<br />
macrovascular compliance. 11, 12 Some researchers have<br />
shown that 2-4 years after previous gestational diabetes<br />
mellitus, a significantly higher arterial stiffness can be<br />
found compared with reference women without a history of<br />
diabetes. 13 Pregnancies complicated by diabetes not only are<br />
associated with increased carotid IMT but also can lead to<br />
increased maternal arterial stiffness. 9<br />
This study demonstrates increased IMT of the carotid artery<br />
in a group of women who had a pregnancy complicated by<br />
impaired OGCT. This finding is in line with the literature<br />
confirming that women with a history of gestational diabetes<br />
have a higher risk of developing increased carotid IMT. This<br />
change can potentially lead to cardiovascular diseases in<br />
later life. There are some explanations for this phenomenon.<br />
One of the first steps in the development of atherosclerosis is<br />
endothelial activation, followed by endothelial dysfunction.<br />
Thus, in diabetes mellitus, vascular endothelial activation<br />
or dysfunction is considered to play a key role in the<br />
development of many of the clinical manifestations related<br />
to carotid artery disease, several years after delivery.<br />
Association between parity and carotid artery disease<br />
can be affected by some underlying factors. Some<br />
epidemiological studies have found positive associations<br />
between parity and risk of carotid artery plaques in elderly<br />
women and, therefore, age of pregnancy can be a trigger<br />
for this phenomenon. 14 Also, multi-gravidity and previous<br />
history of coronary diseases have been also identified to be<br />
related to the appearance of carotid artery plaques. 15 Folate<br />
deficiency during pregnancy is another probable triggering<br />
factor for progressing carotid IMT. Folate deficiency is<br />
linked with hyperhomocystinemia, 16 which is associated with<br />
accelerated progression of atherosclerosis 17 and, thereby,<br />
158
Increased Carotid Artery Intima-Media Thickness in Pregnant Women with ...<br />
carotid artery IMT. Pregnancy is potentially a cause of folate<br />
deficiency. 18 Consequently, it is possible that multiparous<br />
women are at risk of prolonged folate deficiency; this may<br />
explain their susceptibility to the development of carotid<br />
artery IMT.<br />
In the present study, the main limitation was blood glucose<br />
controlled by insulin; we could not hold treatment because<br />
of ethical issues. Also, we did not assess the confounding<br />
effects of the triggering variables such as age of pregnancy,<br />
multi-parity, or medication during this period on increasing<br />
carotid IMT; that should be considered in further studies.<br />
Another weakness of this study would be the relatively small<br />
sample size. The study was designed to enroll 50women.<br />
Despite this, we feel that it provides valuable information.<br />
Prospective follow-up studies will also be needed and have<br />
meanwhile been started to determine whether diabetes during<br />
pregnancy itself is responsible for the increase in IMT.<br />
Conclusion<br />
In conclusion, an impaired OGCT test is proven to be<br />
an independent risk factor for increased carotid IMT and<br />
subsequent coronary artery disease. Even with this small<br />
study, we were able to find an increased IMT after diabetes<br />
appearance, which might be used as an indicator of a potential<br />
increased vascular risk. Furthermore, IMT measurements<br />
in diabetic pregnant women could offer an opportunity to<br />
identify a high-risk group of women who might benefit from<br />
early screening and preventive measures. These measures<br />
could include lifestyle interventions such as improving diet<br />
and physical activity as well as increased surveillance of<br />
blood pressure, serum lipids, and particularly blood glucose.<br />
Acknowledgment<br />
This study was a resident’s thesis and was financially<br />
supported by Kerman University of Medical Sciences.<br />
<strong>TEHRAN</strong> <strong>HEART</strong> <strong>CENTER</strong><br />
artery intima-media thickness in cardiovascular risk assessment by<br />
Framingham risk-score in type 2 diabetes: a retrospective cohort<br />
study. J Diabetes 2009;1:188-193.<br />
5. Akinci B, Demir T, Celtik A, Baris M, Yener S, Ozcan MA, Yuksel<br />
F, Secil M, Yesil S. Serum osteoprotegerin is associated with<br />
carotid intima media thickness in women with previous gestational<br />
diabetes. Diabetes Res Clin Pract 2008;82:172-178.<br />
6. Blaauw J, van Pampus MG, Van Doormaal JJ, Fokkema MR, Fidler<br />
V, Smit AJ, Aarnoudse JG. Increased intima-media thickness after<br />
early-onset preeclampsia. Obstet Gynecol 2006;107:1345-1351.<br />
7. Jovanović S, Jovanović A. Pregnancy is associated with hypotrophy<br />
of carotid artery endothelial and smooth muscle cells. Hum Reprod<br />
1998;13:1074-1078.<br />
8. Tarim E, Yigit F, Kilicdag E, Bagis T, Demircan S, Simsek<br />
E, Haydardedeoglu B, Yanik F. Early onset of subclinical<br />
atherosclerosis in women with gestational diabetes mellitus.<br />
Ultrasound Obstet Gynecol 2006;27:177-182.<br />
9. Savvidou MD, Anderson JM, Kaihura C, Nicolaides KH. Maternal<br />
arterial stiffness in pregnancies complicated by gestational and<br />
type 2 diabetes mellitus. Am J Obstet Gynecol 2010;203:274.e1-7.<br />
10. American Diabetes Association. Standards of medical care in<br />
diabetes-2011. Diabetes Care2011;34:11-61.<br />
11. Visontai Z, Lenard Z, Studinger P, Rigo J, Jr, Kollai M. Impaired<br />
baroreflex function during pregnancy is associated with stiffening<br />
of the carotid artery. Ultrasound Obstet Gynecol 2002;20:364-369.<br />
12. Mersich B, Rigó J, Jr, Besenyei C, Lénárd Z, Studinger P, Kollai M.<br />
Opposite changes in carotid versus aortic stiffness during healthy<br />
human pregnancy. Clin Sci 2005;109:103-107.<br />
13. Hu J, Norman M, Wallensteen M, Gennser G. Increased large<br />
arterial stiffness and impaired acetylcholine induced skin<br />
vasodilatation in women with previous gestational diabetes<br />
mellitus. Br J Obstet Gynaecol 1998;105:1279-1287.<br />
14. Humphries KH, Westendorp IC, Bots ML, Spinelli JJ, Carere<br />
RG, Hofman A. Parity and carotid artery atherosclerosis inelderly<br />
women: the Rotterdam Study. Stroke2001;32:2259-2264.<br />
15. Ness RB, Harris T, Cobb J, Flegal KM, Kelsey JL, Balanger A.<br />
Number of pregnancies and the subsequent risk of cardiovascular<br />
disease. N Engl J Med 1993;328:1528-1533.<br />
16. Boushey CJ, Beresford SA, Omenn GS, Motulsky AG. A<br />
quantitative assessment of plasma homocysteine as a risk factor for<br />
vascular disease. Probable benefits of increasing folic acid intakes.<br />
JAMA 1995;274:1049-1057.<br />
17. Selhub J, Jacques PF, Bostom AG, D’Agostino RB, Wilson PW,<br />
Belanger AJ, O’Leary DH, Wolf PA, Schaefer EJ, Rosenberg IH.<br />
Association between plasma homocysteine concentrations and<br />
extracranial carotid-artery stenosis. N Engl J Med1995;332:286-<br />
291.<br />
18. Mc Partlin J, Halligan A, Scott JM, Darling M, Weir DG. Accelerated<br />
folate breakdown in pregnancy. Lancet 1993;341:148-149.<br />
References<br />
1. Bo S, Valpreda S, Menato G, Bardelli C, Botto C, Gambino R,<br />
Rabbia C, Durazzo M, Cassader M, Massobrio M, Pagano G.<br />
Should we consider gestational diabetes a vascular risk factor<br />
Atherosclerosis 2007;194:72-79.<br />
2. Ben-Haroush A, Yogev Y, Hod M. Epidemiology of gestational<br />
diabetes mellitus and its association with type 2 diabetes. Diabet<br />
Med 2004;21:103-113.<br />
3. Vastagh I, Horváth T, Garamvölgyi Z, Rosta K, Folyovich A, Rigó<br />
J, Kollai M, Bereczki D, Somogyi A. Preserved structural and<br />
functional characteristics of common carotid artery in properly<br />
treated normoglycemic women with gestational diabetes mellitus.<br />
Acta Physiol Hung 2011;98:294-304.<br />
4. Ataoglu HE, Saler T, Uzunhasan I, Yenigun M, Yigit Z, Temiz LU,<br />
Saglam Z, Cetin F, Kumbasar B, Sar F. Additional value of carotid<br />
The Journal of Tehran University Heart Center159
The Journal of Tehran University Heart Center<br />
Original Article<br />
Right Ventricular Myocardial Tissue Velocities,<br />
Myocardial Performance Index, and Tricuspid Annular<br />
Plane Systolic Excursion in Totally Corrected Tetralogy<br />
of Fallot Patients<br />
Asadolah Tanasan, MD 1 , Keyhan Sayadpour Zanjani, MD 2* , Armen<br />
Kocharian, MD 2 , Abdolrazagh Kiani, MD 2 , Mohammad Ali Navabi, MD 2<br />
1<br />
Besat Hospital, Hamadan University of Medical Sciences, Hamadan, Iran.<br />
2<br />
Children’s Medical Center, Tehran University of Medical Sciences, Tehran, Iran.<br />
Received 03 November 2011; Accepted 16 May 2012<br />
Abstract<br />
Background: Longer survival after the total repair of the Tetralogy of Fallot increases the importance of late complications<br />
such as right ventricular dysfunction. This is a prospective study of the right ventricular function in totally corrected Tetralogy<br />
of Fallot patients versus healthy children.<br />
Methods: Thirty-two healthy children were prospectively compared with 30 totally corrected Tetralogy of Fallot patients.<br />
Right ventricular myocardial tissue velocities, right ventricular myocardial performance index, and tricuspid annular plane<br />
systolic excursion were investigated as well as the presence and severity of pulmonary regurgitation.<br />
Results: The two groups were age-and sex-matched. Mean systolic peak velocity (Sa) and tricuspid annular plane systolic<br />
excursion were significantly decreased, while myocardial performance index and early to late diastolic velocity (Ea/Aa)<br />
were significantly increased in the Tetralogy of Fallot patients. Early diastolic velocity (Ea) showed no significant difference<br />
between the two groups. Sa correlated significantly with tricuspid annular plane systolic excursion in both the normal children<br />
and totally corrected Tetralogy of Fallot patients. Myocardial performance index was significantly higher in the patients<br />
with moderate to severe pulmonary regurgitation than in those with mild regurgitation. However, there was no significant<br />
correlation between this index and right ventricular myocardial tissue velocities.<br />
Conclusion: In this study, systolic right ventricular function indices (Sa and tricuspid annular plane systolic excursion)<br />
were impaired in the totally corrected Tetralogy of Fallot patients. Myocardial performance index was affected by the severity<br />
of pulmonary regurgitation.<br />
J Teh Univ Heart Ctr 2012;7(4):160-163<br />
This paper should be cited as: Tanasan A, Sayadpour Zanjani K, Kocharian A, Kiani A, Navabi MA. Right Ventricular Myocardial<br />
Tissue Velocities, Myocardial Performance Index, and Tricuspid Annular Plane Systolic Excursion in Totally Corrected Tetralogy of Fallot<br />
Patients. J Teh Univ Heart Ctr 2012;7(4):160-163.<br />
Keywords: Tetralogy of Fallot • Tricuspid valve • Elasticity imaging technique • Child • Heart ventricles<br />
*<br />
Corresponding Author: Keyhan Sayadpour Zanjani, Assistant Professor of Pediatric Cardiology, Tehran University of Medical Sciences, Children’s<br />
Medical Center, No.62, Dr Gharib Street, Tehran, Iran. 1419733151. Tel: +98 21 66911029. Fax: +98 21 66930024. E-mail: sayadpour@tums.ac.ir.<br />
160
Right Ventricular Myocardial Tissue Velocities, Myocardial Performance Index ...<br />
<strong>TEHRAN</strong> <strong>HEART</strong> <strong>CENTER</strong><br />
Introduction<br />
Although excellent outcomes have been achieved long<br />
after the total correction of the Tetralogy of Fallot (T<strong>OF</strong>) in<br />
the developed countries, right ventricular (RV) dysfunction<br />
may still cause mortality and morbidity. 1, 2 Pulmonary<br />
regurgitation (PR) has a detrimental effect on the RV<br />
diastolic function. 3 Late systolic RV dysfunction has been<br />
reported after the correction of the T<strong>OF</strong> in the developed<br />
countries. 4 The long-term survival after the T<strong>OF</strong> repair in the<br />
developing countries is unknown; 5, 6 we, therefore, sought to<br />
focus on the earlier RV function in these patients. We used<br />
the right ventricular myocardial performance index (RVMPI<br />
or Tei index), tricuspid annular plane systolic excursion<br />
(TAPSE), and myocardial tissue velocities for the evaluation<br />
of the RV systolic and diastolic functions in totally corrected<br />
T<strong>OF</strong> patients. 7<br />
Methods<br />
Thirty consecutive totally corrected T<strong>OF</strong> patients, who<br />
referred to our Outpatient Clinic between July 2008 and<br />
July 2009, were enrolled in the study and written informed<br />
consent was obtained from all of them. The study population<br />
underwent surgery using valved trans-annular patches, nonvalved<br />
trans-annular patches, or sub-annular patches at<br />
a mean age of 3.6 ± 3.2 years. Thirty-two normal healthy<br />
children with innocent murmur were selected as the control<br />
group.<br />
The inclusion criteria for this study included classic T<strong>OF</strong><br />
with pulmonary stenosis. The exclusion criteria were other<br />
variants of the T<strong>OF</strong> (pulmonary atresia with ventricular septal<br />
defect [VSD], absent pulmonary valve, and double-outlet<br />
RV) and the presence of a significant residual abnormality<br />
(VSD, valvular or peripheral pulmonary stenosis, or tricuspid<br />
regurgitation) other than PR.<br />
Echocardiography was performed using a single<br />
echocardiographic scanner (MicroMaxx Ultrasound System,<br />
Sonosite Inc., USA). RVMPI was measured using continuous<br />
pulse wave Doppler of the pulmonary and tricuspid valves.<br />
The formula a-b/b was used, where a was the time interval<br />
between cessation and onset of tricuspid inflow and b was<br />
pulmonary ejection time. 7<br />
The systolic displacement of the lateral portion of the<br />
tricuspid annular plan (TAPSE) was measured on the<br />
M-mode tracing under a two-dimensional echocardiogram<br />
in the four-chamber view. 8<br />
The averages of the RV systolic (Sa), early diastolic (Ea),<br />
and late diastolic velocities (Aa) in three cardiac cycles were<br />
measured using tissue Doppler echocardiography. 4 Threemillimeter<br />
Doppler sample volume was applied parallel<br />
to the RV free wall at the tricuspid valvular level to avoid<br />
sampling the right-heart cavities due to normal cardiac<br />
movement.<br />
Severity of PR was assessed by color and continues<br />
Doppler studies in the parasternal short-axis view. Duration<br />
of the PR flow to total diastolic time (PR index and PRi)<br />
was measured. PRi ≥ 70% was defined as mild PR, while<br />
9, 10<br />
the lower values were defined as moderate to severe PR.<br />
The severity of PR was also assessed on the color Doppler<br />
imaging. The presence of persistent retrograde color flow<br />
from the distal main pulmonary artery or branches that<br />
extend into the RV was defined as moderate to severe PR. 3<br />
The study was approved by the local Ethics Committee and<br />
it was conducted in accordance with good clinical practice<br />
and the Declaration of Helsinki.<br />
For the statistical analyses, the statistical software<br />
SPSS version 13.0 for Windows (SPSS Inc., Chicago, IL)<br />
was used. An independent samples t-test was performed<br />
to compare the RV function indices between the normal<br />
children and T<strong>OF</strong> patients. A bivariate correlation was<br />
performed using the Pearson correlation coefficient<br />
between the RV function indices. Statistical significance<br />
was inferred at a p value < 0.05.<br />
Results<br />
The 32 normal healthy children (17 males and 15 females<br />
at a mean age of 5.6 ± 3.8 years) and the 30 totally corrected<br />
T<strong>OF</strong> patients (17 males and 13 females at a mean age of<br />
6.4 ± 4.1 years) were age- and sex-matched. PR severity<br />
was evaluated in all of the totally corrected T<strong>OF</strong> patients,<br />
of whom 15 had valved trans-annular, 8 non-valved transannular,<br />
and 7 sub-annular patches.<br />
There were statistically significant differences in RVMPI,<br />
TAPSE, and myocardial tissue velocities (Sa, Aa, and Ea/<br />
Aa) between the healthy children and totally corrected T<strong>OF</strong><br />
patients. There was no significant difference in Ea (Table 1).<br />
Table 1. Indices of the RV function in the totally corrected T<strong>OF</strong> patients and<br />
normal healthy children *<br />
Variable T<strong>OF</strong> group Normal group P value<br />
RVMPI 0.3±0.1 0.2±0.1 0.001<br />
TAPSE (mm) 13.6±2.9 16.3±3.3 0.001<br />
Sa (cm/s) 8.6±8.9 11.4±2.2 < 0.001<br />
Ea (cm/s) 10.9±3.3 11.9±2.1 > 0.05<br />
Aa (cm/s) 5.9±1.8 8.2±2.1 < 0.001<br />
Ea/Aa 2.0±0.8 1.5±0.4 0.015<br />
*<br />
Data are presented as mean±SD<br />
RV, Right ventricle; T<strong>OF</strong>, Tetralogy of Fallot; RVMPI, Right ventricular<br />
myocardial performance index; TAPSE, Tricuspid annular plain systolic<br />
excursion; Sa, RV systolic velocity; Ea, Early diastolic velocity; Aa, Late<br />
diastolic velocity<br />
The Pearson analysis showed a strong correlation between<br />
The Journal of Tehran University Heart Center161
The Journal of Tehran University Heart Center<br />
TAPSE and Sa both in the control (r = 0.755, p value < 0.001)<br />
and patient (r = 0.662, p value = 0.002) groups. There was<br />
a significant inverse correlation between Sa and RVMPI (p<br />
value = 0.001) in the control group but not in the patient<br />
group (p value = 0.054). There was no significant correlation<br />
between RVMPI and Ea/Aa in either group.<br />
PRi was measured in all the totally corrected T<strong>OF</strong> patients,<br />
of whom 13 had a value ≥ 70% (mild PR) and 17 had a value<br />
< 70% (moderate to severe PR). PRi < 50% was found in 2<br />
patients. There was a significant correlation between RVMPI<br />
and PRi (p value < 0.001) in the patient group. The RVMPI<br />
in patients with PRi < 70% was 0.42 ± 0.13, which differed<br />
significantly from the RVMPI (0.24 ± 0.1) in the patients<br />
with PRi ≥ 70% (p value < 0.05). In the 2 patients with PRi <<br />
50%, RVMPI was 0.62 and 0.47, respectively. There was no<br />
significant difference in the Ea/Aa ratio between the patients<br />
who had PRi ≥ 70% and those who had PRi < 70% (p value<br />
= 0.38). The Ea/Aa ratio was insignificantly higher in PRi<br />
< 70% (2.1 ± 9.4 vs. 1.85 ± 7.4; p value = 0.405). In the 2<br />
patients who had PRi < 50%, the Ea/Aa ratio was 4.57/1 and<br />
2.92/1, respectively (restrictive pattern).<br />
In the color flow Doppler assessment of PR, 11 patients<br />
had mild PR and 19 had moderate to severe PR. There was a<br />
significant correlation between PR severity in the retrograde<br />
color flow mapping and RVMPI (p value = 0.023), but there<br />
was no correlation between PR severity and Ea/Aa ratio (p<br />
value = 0.38).<br />
Discussion<br />
Advances in cardiac surgery and postoperative<br />
management in the developed countries have contributed<br />
to the excellent long-term outcome of the totally corrected<br />
T<strong>OF</strong> patients; 1 nevertheless, the long-term outcome of<br />
the corrected T<strong>OF</strong> surgery in developing countries is<br />
unknown. 5, 6 In the developed countries, PR and RV<br />
diastolic dysfunction is the most important outcome factor<br />
following the T<strong>OF</strong> repair. 2, 3 There are reports of the usage<br />
of pulmonary valve sparing surgery to decrease the severity<br />
of PR in the T<strong>OF</strong> patients. 11, 12 Intra- and postoperative<br />
management problems, delay in corrective surgery, and<br />
palliative surgery (aorto-pulmonary shunts) are probably<br />
additional contributory factors to the poor long-term<br />
outcome in developing countries. 5, 6 At follow-ups of the<br />
repaired T<strong>OF</strong> patients, simple and fast evaluation of the<br />
systolic and diastolic RV functions is of great importance.<br />
In our study, the RV systolic and diastolic function indices<br />
were clearly impaired in the T<strong>OF</strong> patients in comparison with<br />
the normal children at mid-term follow-ups (Table 1). A few<br />
studies have focused on the RV function at mid-term followup<br />
after the T<strong>OF</strong> repair. Pilla et al. evaluated the presence<br />
of mid-term RV dysfunction and health-related quality of<br />
life after the T<strong>OF</strong> repair in Brazil. 13 In their investigation,<br />
Asadolah Tanasan et al.<br />
35 patients at a median age of 6.1 years and 4.9 years of<br />
follow-up after surgery were compared with 36 sex- and<br />
age-matched healthy controls and RVMPI (0.34 vs. 0.2)<br />
demonstrated RV dysfunction in the patients compared with<br />
the controls. In adult patients late after the repair of the T<strong>OF</strong>,<br />
D’Andrea et al. detected a correlation between myocardial<br />
performance assessed at rest via tissue Doppler (TD) and<br />
cardiac performance during physical effort in adult patients<br />
(21.4 ± 3.8 years). 4 In their study, TD analysis showed lower<br />
Sa, Ea, Ea/Aa ratios in the corrected T<strong>OF</strong> patients compared<br />
to the normal group. In contrast to our study, the corrected<br />
T<strong>OF</strong> patients of their study had no significant PR, the mean<br />
age of the T<strong>OF</strong> patients was higher than that in our study<br />
(21.4 ± 3.8 vs. 6.3 ± 3.3 years), and the mean age of the<br />
corrected T<strong>OF</strong> patients was lower than that in our study (1.4<br />
± 0.5 vs. 3.6 ± 3.2 years). 4 In the Puranik et al. study, Sa<br />
and Ea were significantly lower in asymptomatic corrected<br />
adult T<strong>OF</strong> patients compared with their normal group. 14<br />
Similar to our study, there was significant PR but the age at<br />
corrective surgery was higher (6.6 vs. 3.6 years). Although<br />
the increased Ea/Aa ratio in our study, in contrast to the<br />
D’Andrea’s, may suggest the role of combined prolonged<br />
cyanosis and post-correction PR, a comparison with the<br />
Puranik study emphasizes the importance of other factors in<br />
4, 14<br />
the restrictive diastolic RV dysfunction in our patients.<br />
On the other hand, while our study demonstrates combined<br />
systolic dysfunction (decrease in both Sa and TAPSE) and<br />
restrictive RV dysfunction (increase in Ea/Aa ratio), the two<br />
other studies 4, 14 showed mild systolic dysfunction (decrease<br />
in Sa) associated with a significant decrease in Ea/Aa in adult<br />
corrected T<strong>OF</strong> patients. Frigola et al. reported that PR was an<br />
important factor of RV contractile dysfunction after the T<strong>OF</strong><br />
repair. 15 These observations may suggest that the systolic and<br />
restrictive diastolic RV dysfunctions in our study probably<br />
originated through others mechanisms and they were present<br />
since the early postoperative period. In a study by Cullen<br />
et al, 16 patients with early restrictive physiology after the<br />
T<strong>OF</strong> repair had a clinical picture of low cardiac output and<br />
slow postoperative recovery but a study by Gatzoulis et al.<br />
suggested that late restrictive physiology predicted a superior<br />
exercise performance. 17 Further studies are clearly warranted<br />
about how the RV systolic and diastolic functions correlate<br />
with intra- and early postoperative management and PR.<br />
In addition to significant PR and prolonged preoperative<br />
cyanosis, intra- or early postoperative management may<br />
have been affected by systolic and restrictive diastolic RV<br />
functions in our study. 6 Although RVMPI was significantly<br />
correlated with PR severity (retrograde color flow and PRi),<br />
there was no significant correlation between RVMPI and<br />
Ea/Aa ratio. In our 2 patients with severe PR (PRi < 50%),<br />
the Ea/Aa ratio was significantly elevated. As RVMPI was<br />
not correlated with systolic and diastolic function indices<br />
(Sa, TAPSE, Ea, and Ea/Aa) but was allied to PR severity,<br />
RVMPI may have been affected more by PR severity than<br />
162
Right Ventricular Myocardial Tissue Velocities, Myocardial Performance Index ...<br />
by the RV function in the totally corrected T<strong>OF</strong> patients with<br />
restrictive physiology. In accordance with our study, Abd<br />
El Rahman et al. suggested that MPI was affected by the<br />
severity of PR in the presence of RV diastolic dysfunction. 18<br />
Yasuoka et al. showed that MPI obtained by pulsed wave<br />
Doppler was not different in patients with the T<strong>OF</strong> repair<br />
compared with normal children but RVMPI measured by<br />
tissue Doppler was significantly higher in patients with the<br />
T<strong>OF</strong> than in normal children. 19<br />
The current study had some limitations. The sample<br />
size was inadequate to compare the totally corrected T<strong>OF</strong><br />
subgroups. Furthermore, half of the corrected T<strong>OF</strong> patients<br />
underwent valved trans-annular patch repair, which is a new<br />
technique for right ventricular outflow tract reconstruction.<br />
Conclusion<br />
RVMPI was significantly correlated with PR severity<br />
without the presence of a significant correlation between<br />
RVMPI (obtained by pulsed wave Doppler) and the RV<br />
function indices obtained by tissue Doppler imaging<br />
(EA, Aa, Ea/Aa, and Sa). We suggest that these indices,<br />
RVMPI by tissue Doppler and PRi, be measured basically<br />
at postoperative and follow-up evaluations. In addition, as<br />
TAPSE was significantly decreased in the totally corrected<br />
T<strong>OF</strong> patients and there was a significant correlation between<br />
TAPSE and Sa, we suggest that TAPSE be also measured as<br />
the global RV systolic function index.<br />
Acknowledgment<br />
This study was approved and supported by Tehran<br />
University of Medical Sciences.<br />
References<br />
1. Bacha EA, Scheule AM, Zurakowski D, Erickson LC, Hung J, Lang<br />
P, Mayer JE, Jr, del Nido PJ, Jonas RA. Long-term results after<br />
early primary repair of tetralogy of Fallot. J Thorac Cardiovasc<br />
Surg 2001;122:154-161.<br />
2. Knauth AL, Gauvreau K, Powell AJ, Landzberg MJ, Walsh<br />
EP, Lock JE, del Nido PJ, Geva T. Ventricular size and function<br />
assessed by cardiac MRI predict major adverse clinical outcomes<br />
late after tetralogy of Fallot repair. Heart 2008;94:211-216.<br />
3. Bouzas B, Kilner PJ, Gatzoulis MA. Pulmonary regurgitation: not<br />
a benign lesion. Eur Heart J 2005;26:433-439.<br />
4. D‘Andrea A, Caso P, Sarubbi B, Russo MG, Ascione L, Scherillo M,<br />
Cobrufo M, Calabrò R. Right ventricular myocardial dysfunction<br />
in adult patients late after repair of tetralogy of fallot. Int J Cardiol<br />
2004;94:213-220.<br />
5. Ho KW, Tan RS, Wong KY, Tan TH, Shankar S, Tan JL. Late<br />
complications following tetralogy of Fallot repair: the need for<br />
long-term follow-up. Ann Acad Med Singapore 2007;36:947-953.<br />
6. Rao SG. Pediatric cardiac surgery in developing countries. Pediatr<br />
Cardiol 2007;28:144-148.<br />
<strong>TEHRAN</strong> <strong>HEART</strong> <strong>CENTER</strong><br />
7. Haddad F, Hunt SA, Rosenthal DN, Murphy DJ. Right ventricular<br />
function in cardiovascular disease. Part I: anatomy, physiology,<br />
aging, and functional assessment of the right ventricle. Circulation<br />
2008;117:1436-1448.<br />
8. Miller D, Farah MG, Liner A, Fox K, Schluchter M, Hoit BD. The<br />
relation between quantitative right ventricular ejection fraction and<br />
indices of tricuspid annular motion and myocardial performance. J<br />
Am Soc Echocardiogr 2004;17:443-447.<br />
9. Festa P, Ait-Ali L, Minichilli F, Kristo I, Deiana M, Picano E.<br />
A new simple method to estimate pulmonary regurgitation by<br />
echocardiography in operated fallot: comparison with magnetic<br />
resonance imaging and performance test evaluation. J Am Soc<br />
Echocardiogr 2010;23:496-503.<br />
10. Li W, Davlouros PA, Kilner PJ, Pennell DJ, Gibson D, Henein<br />
MY, Gatzoulis MA. Doppler-echocardiographic assessment of<br />
pulmonary regurgitation in adults with repaired tetralogy of Fallot:<br />
comparison with cardiovascular magnetic resonance imaging. Am<br />
Heart J 2004;147:165-172.<br />
11. Boni L, García E, Galletti L, Pérez A, Herrera D, Ramos V,<br />
Marianeschi SM, Comas JV. Current strategies in tetralogy of<br />
Fallot repair: pulmonary valve sparing and evolution of right<br />
ventricle/left ventricle pressures ratio. Eur J Cardiothorac Surg<br />
2009;35:885-889.<br />
12. Singh S, Pratap H, Agarwal S, Singh A, Satsangi DK. Pulmonary<br />
valve preservation in tetralogy of Fallot with a mildly hypoplastic<br />
annulus-should we do it Indian J Thorac Cardiovasc Surg<br />
2011;27:76-82.<br />
13. Pilla CB, Pereira CA, Fin AV, Aquino FV, Botta A, DalleMulle L,<br />
Ricachinevsky CP, Nogueira AJ, Lucchese FA, Rohde LE. Healthrelated<br />
quality of life and right ventricular function in the midterm<br />
follow-up assessment after tetralogy of Fallot repair. Pediatr<br />
Cardiol 2008;29:409-415.<br />
14. Puranik R, Greaves K, Hawker RE, Pressley LA, Robinson PJ,<br />
Celermajer DS. Abnormal right ventricular tissue velocities after<br />
repair of congenital heart disease-implications for late outcomes.<br />
Heart Lung Circ 2007;16:295-299.<br />
15. Frigiola A, Redington AN, Cullen S, Vogel M. Pulmonary<br />
regurgitation is an important determinant of right ventricular<br />
contractile dysfunction in patients with surgically repaired<br />
tetralogy of Fallot. Circulation 2004;110:II153-157.<br />
16. Cullen S, Shore D, Redington A. Characterization of right<br />
ventricular diastolic performance after complete repair of tetralogy<br />
of Fallot. Restrictive physiology predicts slow postoperative<br />
recovery. Circulation 1995;91:1782-1789.<br />
17. Gatzoulis MA, Clark AL, Cullen S, Newman CG, Redington AN.<br />
Right ventricular diastolic function 15 to 35 years after repair<br />
of tetralogy of Fallot. Restrictive physiology predicts superior<br />
exercise performance. Circulation 1995;91:1775-1781.<br />
18. Abd El Rahman MY, Abdul-Khaliq H, Vogel M, Alexi-Meskischvili<br />
V, Gutberlet M, Hetzer R, Lange PE. Value of the new Dopplerderived<br />
myocardial performance index for the evaluation of right<br />
and left ventricular function following repair of tetralogy of Fallot.<br />
Pediatr Cardiol 2002;23:502-507.<br />
19. Yasuoka K, Harada K, Toyono M, Tamura M, Yamamoto F. Tei<br />
index determined by tissue Doppler imaging in patients with<br />
pulmonary regurgitation after repair of tetralogy of Fallot. Pediatr<br />
Cardiol 2004;25:131-136.<br />
The Journal of Tehran University Heart Center163
The Journal of Tehran University Heart Center<br />
Original Article<br />
Anatomy of Atrioventricular Node Artery and Pattern of<br />
Dominancy in Normal Coronary Subjects: A Comparison<br />
between Individuals with and without Isolated Right<br />
Bundle Branch Block<br />
Ali Kazemisaeid, MD, Marziyeh Pakbaz, MD * , Ahmad Yaminisharif, MD,<br />
Gholamreza Davoodi, MD, Masoumeh Lotfi Tokaldany, MD, Elham Hakki<br />
Kazazi, MD<br />
Tehran Heart Center, Tehran University of Medical Sciences, Tehran, Iran.<br />
Received 24 December 2011; Accepted 20 May 2012<br />
Abstract<br />
Background: Isolated right bundle branch block (RBBB) is a common finding in the general population. The atrioventricular<br />
node (AVN) artery contributes to the blood supply of the right bundle branch. Our hypothesis was that the anatomy of the<br />
AVN artery and the pattern of dominancy differ between subjects with and without RBBB.<br />
Methods: We retrospectively studied the coronary angiography of 92 patients with RBBB and 184 age- and gendermatched<br />
controls without RBBB. All the subjects had angiographically proven normal coronary arteries. The dominant<br />
circulation and precise origin of the AVN artery were determined in each subject. Obtained data were compared between the<br />
two study groups.<br />
Results: There was no significant difference between the two groups in terms of dominancy (p value = 0.200). Origination<br />
of the AVN artery from the right circulatory system was more common in both groups, but this pattern was more prevalent<br />
in the cases than in the controls (p value = 0.021). There was a great variation of the AVN artery origin. In the total study<br />
population, the AVN artery was more commonly separated from a non crux origin than from the crux area. The prevalence of<br />
the non-crux origination of the AVN artery was significantly higher in the cases than in the controls (p value < 0.001). While<br />
the origination of the AVN artery from the right circulatory system was more common in both groups, the prevalence of the<br />
right origin of the AVN artery was significantly higher in the cases than in the controls. We observed that the AVN artery most<br />
commonly originated from the dominant artery but not necessarily from the crux.<br />
Conclusion: The anatomy of the AVN artery but not the pattern of dominancy is somewhat different in subjects with RBBB<br />
compared with normal individuals.<br />
J Teh Univ Heart Ctr 2012;7(4):164-169<br />
This paper should be cited as: Kazemisaeid A, Pakbaz M, Yaminisharif A, Davoodi G, Lotfi Tokaldany M, Hakki Kazazi E. Anatomy<br />
of Atrioventricular Node Artery and Pattern of Dominancy in Normal Coronary Subjects; A Comparison Between Individuals With and<br />
Without Isolated Right Bundle Branch Block. J TehUniv Heart Ctr 2012;7(4):164-169.<br />
Keywords: Anatomy • Coronary vessels • Bundle-branch block<br />
*<br />
Corresponding Author: Marziyeh Pakbaz, Department of Cardiology, Tehran University of Medical Sciences, Tehran Heart Center, North Kargar<br />
Street, Tehran, Iran.1411713138. Tel: +98 21 88029256. Fax: +98 21 88029256. E-Mail: marzi.pakbaz@gmail.com.<br />
164
Anatomy of Atrioventricular Node Artery and Pattern of Dominancy in Normal ...<br />
<strong>TEHRAN</strong> <strong>HEART</strong> <strong>CENTER</strong><br />
Introduction<br />
The atrioventricular node (AVN) is an area of specialized<br />
tissue between the atria and the ventricles of the heart and<br />
specifically acts as an electrical relay station for electrical<br />
impulses, passing from the atria to the ventricles. The arterial<br />
blood supply of the AVN, which is quite variable, was the<br />
topic of anatomic, histologic, and radiologic research for<br />
many years. The origin of the blood supply to the conduction<br />
system is highly relevant to the clinical symptoms and<br />
surgical procedures. 1 Recognition of the anatomical variants<br />
of the arterial blood supply to the AVN may help overcome<br />
potential complications following ablation procedures or in<br />
mitral valve surgery.<br />
Isolated right bundle branch block (RBBB) is a common<br />
finding in the general population. RBBB may be associated<br />
with structural heart disease but many subjects with this<br />
conduction abnormality have no evidence of underlying<br />
heart disease. 2, 3 The blood supply to the proximal part of<br />
the right bundle branch is provided by the left anterior<br />
descending artery (LAD) or the AVN artery, and the distal<br />
part is mainly supplied by branches from the LAD. 4<br />
With regard to the contribution of the AVN artery to the<br />
blood supply of the right bundle branch, we postulated that<br />
RBBB may be associated with anatomical variations in the<br />
AVN artery. The aim of this study was to investigate the<br />
origin of the AVN artery in patients with isolated RBBB and<br />
to compare it with normal electrocardiogram individuals.<br />
Methods<br />
This case control study was conducted enrolling patients<br />
with normal coronary arteries or mild coronary artery<br />
disease who underwent coronary angiography between 2001<br />
and 2010 in Tehran Heart Center. Demographic features,<br />
coronary risk factors, drug history, history of cardiac events,<br />
electrocardiographic interpretation, echocardiographic<br />
findings, past history of coronary or any other type of<br />
intervention and open heart surgery, and the result of<br />
coronary angiography were drawn out of the computerized<br />
angiography database of Tehran Heart Center. Patients eligible<br />
for inclusion were men and women at least 20 years of age<br />
with documented RBBB on the surface electrocardiogram,<br />
mild or normal coronary arteries proven by angiography, and<br />
a normal ejection fraction (more than 50%). Major exclusion<br />
criteria included the presence of conduction abnormalities<br />
other than RBBB, history of using drugs affecting the heart<br />
conduction system such as beta adrenergic receptor blockers<br />
and antiarrhythmic agents, significant valvular heart disease<br />
(more than mild regurgitation or stenosis of any valve) on<br />
echocardiography study, and congenital or acquired structural<br />
heart disease that could be an etiology for developing RBBB<br />
such as atrial septal defect, ventricular septal defect, and<br />
pulmonary thromboembolism. Case selection was done<br />
with convenience non-probability sampling. Initially, 141<br />
patients were selected from the angiography database.<br />
Subsequently, the hospital records of these patients,<br />
including the history of symptoms, further evaluation of<br />
the electrocardiogram, echocardiographic findings, and<br />
coronary angiography report sheets, were reviewed in detail.<br />
First, the electrocardiogram and records were selected for<br />
further study if the electrocardiogram satisfied the criteria<br />
previously defined for typical RBBB by the World Health<br />
Organization and the International Society and Federation<br />
for Cardiology in 1985, as follows: 1) prolongation of QRS<br />
to 0.12 second or more; 2) an rsr’, rsR’, or rSR’ pattern and<br />
occasionally a wide and notched R pattern in lead V 1<br />
or V 2<br />
;<br />
3) an S wave duration longer than the R wave duration or<br />
greater than 40 ms in leads V 6<br />
and I; and 4) an R peak time<br />
greater than 0.05 second in lead V 1<br />
but normal in leads V 5<br />
and V 6<br />
. 5<br />
Of these criteria, the first three should be present for the<br />
diagnosis to be made. When a notched dominant R pattern is<br />
present in V 1<br />
, criterion 4 should be satisfied as well.<br />
Of the initial 141 patients selected, 49 subjects who did<br />
not meet the inclusion criteria were excluded. Finally, a<br />
total of 92 subjects were entered for final analysis. Control<br />
subjects, who underwent coronary angiography during the<br />
same period, were randomly extracted from the angiography<br />
database. The controls were matched by age and sex to<br />
the cases with a 2:1 ratio. Inclusion criteria other than<br />
electrocardiography findings were the same as those of the<br />
cases. For each group, the coronary angiography recorded on<br />
CDs was studied to determine the pattern and characteristics<br />
of the coronary anatomy and the origination of the AVN<br />
artery. The dominant circulation was also determined.<br />
The classification described by Popma JJ was used in the<br />
present study to define the dominant coronary circulation 6 :<br />
a) in a right dominant circulation, the posterior descending<br />
artery (PDA) and at least one posterolateral branch (PLB)<br />
originate from the right coronary artery (RCA); b) in a left<br />
dominant circulation, the PDA and all of the PLBs originate<br />
from the left coronary artery; and c) In a co-dominant<br />
circulation, the PDA originates from the RCA and all of the<br />
PLBs originate from the left coronary artery.<br />
In order to determine the origin of the AVN artery, the<br />
dominant artery was ascertained. Based on the knowledge<br />
that the AVN artery most commonly originates from the<br />
crux, 7 if a branch to the AVN region originated from the<br />
dominant artery at the area of the crux, it was considered<br />
the AVN artery. If such a branch was not detected, other<br />
segments of the dominant artery and thereafter the nondominant<br />
artery were evaluated in multiple views. At the<br />
end, the origin of the AVN artery was classified to be from<br />
the right, left, or dual circulation (if both circulatory systems<br />
gave rise to the AVN blood supply). If the AVN artery was<br />
not originated from the crux, we determined the specific<br />
The Journal of Tehran University Heart Center165
The Journal of Tehran University Heart Center<br />
Ali Kazemisaeid et al.<br />
artery giving rise to it.<br />
Statistical analysis was performed using SPSS version<br />
15.0 software. Results for the quantitative variables were<br />
reported as mean ± standard deviation and as frequencies for<br />
the qualitative variables. The mean values of the quantitative<br />
variables of the two study groups were compared using the<br />
Student t-test. The frequency distributions of the qualitative<br />
variables, obtained from the two study groups, were<br />
compared using the chi-square test. A p value ≤ 0.05 was<br />
considered a statistically significant difference.<br />
Results<br />
A total of 276 patients were involved, and 92 (33.3%) and<br />
184 (66.7%) subjects were grouped as cases and controls,<br />
respectively. The mean age for the case group (59.8% male)<br />
was 59.19 ± 10.93 years and for the controls (62.5% male)<br />
59.29 ± 10.94 years. In terms of dominancy, there was no<br />
significant difference between the study groups (p value = 0.<br />
200). Also, 75.0% of the cases versus 76.6% of the controls<br />
had right dominant, 12.0% of the cases versus 16.3% of the<br />
controls had left dominant, and 13.0% of the cases versus<br />
7.1% of the controls had co-dominant circulations (Figure<br />
1). By comparison, in terms of dominancy, there was no<br />
significant difference between the study groups.<br />
Figure 1. Comparison between the cases (individuals with right bundle<br />
branch block) and controls (individuals without right bundle branch block),<br />
showing the frequency of the distribution of the types of dominancy<br />
In the evaluation of the AVN artery origin, we determined<br />
whether it was originated from the right or left or whether<br />
it had a dual origin, whether or not it was from the crux.<br />
Furthermore, we determined the specific artery, from which<br />
the AVN artery branched (Tables 1 and 2). The crux was<br />
defined as the U-turn segment of the dominant artery.<br />
Of the total study population, the AVN origin was from<br />
the crux in 106 (38.4%) and from a non-crux origin in 169<br />
(61.2%) subjects (Table 1).<br />
Table 1. Variations of the AVN origin artery in the total study population<br />
Origin of AVN artery<br />
Number of subjects<br />
Undetermined 1<br />
Crux 106<br />
Non-crux origins 169<br />
Dual origin<br />
PLB and distal of LCX 2<br />
OM and distal of RCA 1<br />
Origin from LCX<br />
Distal of LCX 3<br />
Mid-part of LCX 1<br />
Origin from OM 40<br />
Origin from RCA<br />
Conus 3<br />
Proximal of RCA 7<br />
Distal of RCA 24<br />
Posterior descending artery 2<br />
Posterolateral branch 85<br />
Origin from Ramus 1<br />
Total 276<br />
AVN, Atrioventricular node; LCX, Left circumflex artery; RCA, Right<br />
coronary artery; OM, Obtuse marginal artery<br />
In one patient, the AVN origin was undetermined, probably<br />
because it was too small to be visualized. Only a minority of<br />
the patients had an AVN artery with a dual origin (2 of the<br />
cases and one of the controls), as is shown in Table 1.<br />
These special cases were omitted from the subsequent<br />
analysis of the AVN origin because of the very small number<br />
of such cases. The results after such an adjustment are<br />
depicted in Table 2.<br />
Table 2 illustrates that origination of the AVN artery from<br />
a non-crux origin was more common than origination from<br />
the crux in both groups. The prevalence of the non-crux<br />
origination of the AVN artery was significantly higher in the<br />
cases than in the controls (79.8% vs. 51.4%, respectively; p<br />
value < 0.001).<br />
Although origination from the right circulatory system<br />
was more common in both groups (82.0% of the cases and<br />
68.9% of the controls), the prevalence of the right origin of<br />
the AVN artery was significantly higher in the cases than in<br />
the controls (p value = 0.021) (Table 2).<br />
A more detailed comparison of the AVN artery origin<br />
between the cases and controls is illustrated in Figure 2.<br />
The most common origin of the AVN artery was the crux<br />
in the controls and the PLB in the cases when considering<br />
the frequency of the different non-crux origin variations of<br />
the AVN artery separately. Nevertheless, by integrating these<br />
166
Anatomy of Atrioventricular Node Artery and Pattern of Dominancy in Normal ...<br />
<strong>TEHRAN</strong> <strong>HEART</strong> <strong>CENTER</strong><br />
subtypes and considering the single variant of the “non-crux<br />
origin of the AVN artery”, it became more common than the<br />
crux origin even slightly in the controls.<br />
We analyzed the association between the origin of the<br />
AVN artery and the type of dominancy in the whole study<br />
population and observed that the AVN artery most commonly<br />
originated from the dominant artery. In the case of the codominant<br />
circulation, it most commonly originated from the<br />
right circulation (Table 3).<br />
Table 2. Comparison of the AVN artery origin in individuals with right<br />
bundle branch block (cases) and individuals without right bundle branch<br />
block )controls) *<br />
AVN artery<br />
origin<br />
Total<br />
n=272<br />
Case<br />
n=89<br />
Control<br />
n=183<br />
Left 73 (26.8) 16 (18.0) 57 (31.1)<br />
Right 199 (73.2) 73 (82.0) 126 (68.9)<br />
Crux 107 (39.3) 18 (20.2) 89 (48.6)<br />
Non-crux 165 (60.7) 71 (79.8) 94 (51.4)<br />
*<br />
Data are presented as n )%(<br />
**<br />
Case vs. Control<br />
AVN, Atrioventricular node<br />
P value **<br />
0.021<br />
< 0.001<br />
Figure 2. Frequency of the AVN artery origin in cases (individuals with<br />
right bundle branch block) and controls (individuals without right bundle<br />
branch block)<br />
AVN, Atrioventricular node; CX, Left circumflex artery; OM, Obtuse<br />
marginal artery; PDA, Posterior descending artery; PLB, Posterolateral<br />
branch artery; RCA, Right coronary artery<br />
Table 3. Association of the AVN artery origin with dominancy<br />
Dominancy<br />
Origin of the AVN artery<br />
from right circulation from left circulation<br />
Right dominant 87.9% 12.1%<br />
Left dominant 7.5% 92.5%<br />
Co-dominant 60.0% 40.0%<br />
AVN, Atrioventricular node<br />
Discussion<br />
The findings of the present study suggest that there is no<br />
relationship between the dominancy of the epicardial arteries<br />
and the presence of RBBB in subjects with normal coronary<br />
arteries. There was a great variation of the AVN artery origin<br />
among all the study subjects. In the total study population<br />
and also in each group, the AVN artery was more commonly<br />
separated from a non-crux origin than from the crux (61.2%<br />
versus 38.4%); this is in contrast to the conventional<br />
wisdom. 7 The prevalence of the non-crux origination of<br />
the AVN artery was significantly higher in the cases than<br />
in the controls. A dual artery supply of the AVN was a rare<br />
variation, only observed in 0.01% of the subjects. While<br />
the origination of the AVN artery from the right circulatory<br />
system was more common in both groups, the prevalence of<br />
the right origin of the AVN artery was significantly higher in<br />
the cases than in the controls. Finally, we observed that the<br />
AVN artery most commonly originated from the dominant<br />
artery but not necessarily from the crux.<br />
To this date, there has been no previous study aiming to<br />
specifically compare anatomic variations in the AVN artery<br />
in subjects with RBBB versus subjects with normal surface<br />
electrocardiograms.<br />
Table 4 represents the results of the previous studies that<br />
investigated the AVN artery origin. 8-14 All the studies showed<br />
that the AVN artery originated most commonly from the<br />
RCA, which was the most common dominant system. This<br />
led to the conclusion that the AVN artery usually branched<br />
from the dominant artery. However, this was not always the<br />
case as we observed some cases of the origination of the<br />
AVN artery from the non-dominant artery. These out-ofthe-rule<br />
variants were more commonly seen in the control<br />
group (15% of the controls versus 1% of the cases and 10%<br />
of the total study population). The results of the current<br />
study with regard to this variable were very close to the<br />
results of Ramanathan and his colleagues’ angiographybased<br />
study on an Indian population and somewhat different<br />
from other studies, suggesting that race might be a potential<br />
factor influencing the anatomic variables of the coronary<br />
artery. 14 Three per cent of the total population investigated<br />
by Ramanathan et al., showed origination of the AVN artery<br />
from the non-dominant artery.<br />
Pejković B et al., in an anatomic study of 150 human hearts,<br />
found that the artery supplying the AVN arose most frequently<br />
from the U- or V-shaped segment of the right (90%) or left<br />
(10%) coronary artery termed the ‘U-turn’ at the level of the<br />
crux. 15 Differently in our study, the AVN artery was more<br />
commonly separated from a non-crux origin than from the<br />
crux (61.2% versus 38.4%). In 72.1% of the subjects, it was<br />
a branch from the right circulation and in 26.4% from the left<br />
circulation. In line with our observation, Pejkovic B et al., also<br />
showed that the AVN artery origin depended on topographic<br />
The Journal of Tehran University Heart Center167
The Journal of Tehran University Heart Center<br />
Ali Kazemisaeid et al.<br />
arterial dominance: in cases with right or balanced arterial<br />
coronary vascularization, the AVN artery was a branch of the<br />
RCA, and in cases of left dominance the left coronary artery<br />
gave a branch to the AVN. 15<br />
Dual supply of the AVN was a rare variation in the present<br />
sample of individuals. Such a dual supply has been described<br />
in the literature previously. 8, 10, 12-14, 16, 17 The co-dominant<br />
circulation seems not to be related to the dual arterial blood<br />
supply of the AVN insofar as in our study none of the 3<br />
patients with dual supply were co-dominant (one was leftdominant<br />
and the other 2 were right-dominant).<br />
Rusu MC et al., in an anatomic study of 50 human hearts,<br />
described five morphological types (each with distinctive<br />
subtypes) of the AVN artery: 1) type I (22%, the AVN artery<br />
from the U-turn of the RCA); 2) type II (18%, the AVN artery<br />
from the PDA); 3) type III (34%, the AVN artery from the<br />
PLB); 4) type IV (8%, the AVN artery from the bifurcation of<br />
the RCA into the PDA and the PLB-trifurcated RCA); and 5)<br />
type V (18%, the AVN artery from the circumflex artery). 18<br />
According to this type of classification, in our total study<br />
population the prevalence of each subtype was as follows:<br />
38.4% type I; 0.7% type II; 30.8% type III; 8.6% type IV;<br />
and 1.4% type V. We also observed additional subtypes such<br />
as origination from the OM, conus, proximal part of the RCA<br />
and ramus in 14.5%, 1.1%, 2.5%, and 0.3% of the subjects,<br />
respectively. Similar to the Russu study, the separation of the<br />
AVN artery from a non-crux origin was more common than<br />
that from the crux. Also in both studies, the most common<br />
non-crux origin of the AVN artery was from the PLB. The<br />
least common subtype in our study was origination from<br />
the PDA (and also ramus), in contrast to the Russu study, in<br />
which origination from the PDA was a common variation.<br />
By comparing the two study groups in our investigation, as<br />
is shown in Figure 2, this conclusion could be readily made<br />
that the origin of the AVN artery differed in the subjects with<br />
RBBB and those without RBBB.<br />
Conclusion<br />
According to our observations, there was no relationship<br />
between the dominancy of the epicardial arteries and the<br />
presence of RBBB in subjects with normal coronary arteries.<br />
There was a great variation of the AVN artery origin. Noncrux<br />
origination of the AVN artery was more common than<br />
the crux origination in both groups, and the prevalence of<br />
non-crux origination of the AVN artery was significantly<br />
higher in the cases than in the controls. Origination of the<br />
AVN artery from the right circulatory system was more<br />
common in both groups and the prevalence of the right origin<br />
of the AVN artery was significantly higher in the cases than<br />
in the controls. The AVN artery most commonly originated<br />
from the dominant artery but not necessarily from the crux.<br />
Acknowledgment<br />
This study was approved and supported by Tehran<br />
University of Medical Sciences.<br />
References<br />
1. Abuin G, Nieponice A. New findings on the origin of the<br />
blood supply to the atrioventricular node. Clinical and surgical<br />
significance. Tex Heart Inst J 1998;25:113-117.<br />
2. Knilans TK. Right bundle branch block. In: Surawicz B, ed. Chou’s<br />
Electrocardiography In Clinical Practice. 6th ed. Philadelphia:<br />
Saunders; 2008. p. 99-100.<br />
3. Mirvis DM, Goldberger AL. Electrocardiography. In: Bonow RO,<br />
Mann DL, Zipes DP, Libby P, Braunwald E, eds. Braunwald’s<br />
Heart Disease, A Textbook of Cardiovascular Medicine. 9th ed.<br />
Philadelphia: Saunders; 2011. p. 146-147.<br />
4. Stambler BS, Rahimtoola SH, Ellenbogen KA. Pacing for<br />
atrioventricular conduction system disease. In: Ellenbogen<br />
KA, Kay GN, eds. Clinical Cardiac Pacing, Defibrillation, and<br />
Resynchronization Therapy. 3rd ed. Philadelphia: Saunders; 2007.<br />
p. 429-430.<br />
5. Willems JL, Robles de Medina EO, Bernard R, Coumel P, Fisch<br />
C, Krikler D, Mazur NA, Meijler FL, Mogensen L, Moret P.<br />
Criteria for intraventricular conduction disturbances and preexcitation.<br />
World Health Organizational/International Society and<br />
Federation for Cardiology Task Force Ad Hoc. J Am Coll Cardiol<br />
1985;5:1261-1275.<br />
6. Pompa JJ. Coronary arteriography. In: Bonow RO, Mann DL,<br />
Table 4. Origin of the AVN artery reported by various authors<br />
Author Study date Sample size<br />
Origin of AVN artery (%)<br />
RCA LCX Dual<br />
Vieweg et al. 1975 118 84 8 8<br />
Hutchison 1978 40 80 20 -<br />
Hadziselimović 1978 200 85 13 2<br />
Krupa 1993 120 90 10 -<br />
Futami et al. 2003 30 80 10 10<br />
Saremietal 2008 102 87 11 2<br />
Ramanathan et al. 2009 300 72 28 0<br />
The present study 2011 276 72.1 26.4 1.1<br />
AVN, Atrioventricular node; RCA, Right coronary artery; LCX, Left circumflex artery<br />
168
Anatomy of Atrioventricular Node Artery and Pattern of Dominancy in Normal ...<br />
<strong>TEHRAN</strong> <strong>HEART</strong> <strong>CENTER</strong><br />
Zipes DP, Libby P, Braunwald E, eds. Braunwald’s Heart Disease,<br />
A Textbook of Cardiovascular Medicine. 9th ed. Philadelphia:<br />
Saunders; 2011. p. 406-440.<br />
7. Rubart M, Zipes DP. Genesis of cardiac arrhythmias:<br />
electrophysiologic considerations. In: Bonow RO, Mann DL,<br />
Zipes DP, Libby P, Braunwald E, eds. Braunwald’s Heart Disease,<br />
A Textbook of Cardiovascular Medicine. 9th ed. Philadelphia:<br />
Saunders; 2011. p. 653-686.<br />
8. Vieweg WV, Alpert JS, Hagan AD. Origin of the sinoatrial node<br />
and atrioventricular node arteries in right, mixed, and left inferior<br />
emphasis systems. Cathet Cardiovasc Diagn 1975;1:361-373.<br />
9. Hutchinson MC. A study of the artrial arteries in man. J Anat<br />
1978;125:39-54.<br />
10. Hadziselimović H. Vascularization of the conducting system in the<br />
human heart. Acta Anat (Basel) 1978;102:105-110.<br />
11. Krupa U. The atrioventricular nodal artery in the human heart.<br />
Folia Morphol (Warsz) 1993;52:G1-9.<br />
12. Futami C, Tanuma K, Tanuma Y, Saito T. The arterial blood supply<br />
of the conducting system in normal human hearts. Surg Radiol<br />
Anat 2003;25:42-49.<br />
13. Saremi F, Abolhoda A, Ashikyan O, Milliken JC, Narula J,<br />
Gurudevan SV, Kaushal K, Raney A. Arterial supply to sinuatrial<br />
and atrioventricular nodes: imaging with multidetector CT.<br />
Radiology 2008;246:99-107.<br />
14. Ramanathan L, Shetty P, Nayak SR, Krishnamurthy A, Chettiar<br />
GK, Chockalingam A. Origin of the sinoatrial and atrioventricular<br />
nodal arteries in South Indians: an angiographic study. Arq Bras<br />
Cardiol 2009;92:314-319.<br />
15. Pejković B, Krajnc I, Anderhuber F, Kosutić D. Anatomical aspects<br />
of the arterial blood supply to the sinoatrial and atrioventricular<br />
nodes of the human heart. J Int Med Res 2008;36:691-698.<br />
16. Krauss D, Carter JE, Jr, Feldman T. Anomalous connection between<br />
the sinus node artery and the A-V node artery. Cathet Cardiovasc<br />
Diagn 1993;29:236-239.<br />
17. James TN, Burch GE. The atrial coronary arteries in man.<br />
Circulation 1958;17:90-98.<br />
18. Rusu MC, Ferechide D, Curca GC, Dermengiu D. Morph functional<br />
considerations on the atrioventricular node arterial vascularization.<br />
Rom J Leg Med 2009;17:101-110.<br />
The Journal of Tehran University Heart Center169
The Journal of Tehran University Heart Center<br />
Original Article<br />
Determinants of Length of Stay in Surgical Ward after<br />
Coronary Bypass Surgery: Glycosylated Hemoglobin as a<br />
Predictor in All Patients, Diabetic or Non-Diabetic<br />
Mahdi Najafi, MD * , Hamidreza Goodarzynejad, MD<br />
Tehran Heart Center, Tehran University of Medical Sciences, Tehran, Iran.<br />
Received 03 March 2012; Accepted 23 July 2012<br />
Abstract<br />
Background: Reports on the determinants of morbidity in coronary artery bypass graft surgery (CABG) have focused on<br />
outcome measures such as length of postoperative stay in the Intensive Care Unit (ICU). We proposed that major comorbidities<br />
in the ICU hampered the prognostic effect of other weaker but important preventable risk factors with effect on patients’<br />
length of hospitalization. So we aimed at evaluating postoperative length of stay in the ICU and surgical ward separately.<br />
Methods: We studied isolated CABG candidates who were not dialysis dependent. Preoperative, operative, and<br />
postoperative variables as well as all classic risk factors of coronary artery disease were recorded. Using multivariate<br />
analysis, we determined the independent predictors of length of stay in the ICU and in the surgical ward.<br />
Results: Independent predictors of extended length of stay in the surgical ward ( > 3 days) were a history of peripheral<br />
vascular disease, total administered insulin during a 24-hour period after surgery, glycosylated hemoglobin (HbA1c), last<br />
fasting blood sugar of the patients before surgery, and inotropic usage after cardiopulmonary bypass. The area under the<br />
Receiver Operating Characteristic Curve (AUC) was found to be 0.71 and Hosmer-Lemeshow (HL) goodness of fit statistic p<br />
value was 0.88. Independent predictors of extended length of stay in the ICU ( > 48 hours) were surgeon category, New York<br />
Heart Association functional class, intra-aortic balloon pump, postoperative arrhythmias, total administered insulin during<br />
a 24-hour period after surgery, and mean base excess of the first 6 postoperative hours (AUC = 0.70, HL p value = 0.94 ).<br />
Conclusion: This study revealed that the indices of glycemic control were the most important predictors of length of stay in<br />
the ward after cardiac surgery in all patients, diabetic or non-diabetic. However, because HbA1c level did not change under<br />
the influence of perioperative events, it could be deemed a valuable measure in predicting outcome in CABG candidates.<br />
J Teh Univ Heart Ctr 2012;7(4):170-176<br />
This paper should be cited as: Najafi M, Goodarzynejad H. Determinants of Length of Stay in Surgical Ward after Coronary Bypass<br />
Surgery: Glycosylated Hemoglobin as a Predictor in All Patients, Diabetic or Non-Diabetic. J Teh Univ Heart Ctr 2012;7(4):170-176.<br />
Keywords: Coronary artery bypass • Treatment outcome • Hemoglobin A, glycosylated • Length of stay<br />
Introduction<br />
In a world of limited medical care resources, despite<br />
increasing demand for medical services, clinicians often<br />
need to identify patients that are likely to require a longer<br />
period of high dependency care after cardiac surgery.<br />
Coronary artery bypass graft surgery (CABG) has received<br />
particular attention as it is an expensive and commonly<br />
*<br />
Corresponding Author: Mahdi Najafi, Assistant Professor of Anesthesiology, Tehran Heart Center, Tehran University of Medical Sciences, Tehran<br />
Heart Center, North Karegar Street, Tehran, Iran. 1411713138. Tel: +98 21 88029600. Fax: +98 21 88029731. E-mail: najafik@sina.tums.ac.ir.<br />
170
Determinants of Length of Stay in Surgical Ward after Coronary Bypass Surgery ...<br />
<strong>TEHRAN</strong> <strong>HEART</strong> <strong>CENTER</strong><br />
performed procedure. 1, 2 Indeed, detection of patients who<br />
are likely to need a longer postoperative length of stay (LOS)<br />
for CABG would allow operations on these patients to be<br />
spread over the operating week. This would maximize the<br />
chance of the availability of the Intensive Care Unit (ICU)<br />
beds for other sick patients and also prevent the cancellations<br />
of operations. Moreover, prolonged ICU and ward stay in<br />
patients undergoing CABG increases overall hospital costs. 3<br />
LOS in hospital after cardiac surgery is among the most<br />
important determinants of outcome to have been studied<br />
so far. Many studies have reported the factors affecting the<br />
length of postoperative ICU stay. 4-12 A few investigators have<br />
evaluated total hospital LOS, 13-16 but to our knowledge, no<br />
study has assessed such predictors at cardiac surgical wards.<br />
Although the total time of hospital stay contains the time<br />
of stay in the ward, prolonged stay in the surgical ward is<br />
important itself inasmuch as it limits the number of available<br />
ICU beds because of a reduced throughput in the surgical<br />
ward, and as a consequence in the ICU unit. We proposed<br />
that the predictors of a prolonged ICU stay might be different<br />
from the predictors of a long postoperative stay in the<br />
hospital ward.<br />
Methods<br />
We prospectively studied a total of 570 consecutive patients<br />
undergoing elective CABG at Tehran Heart Center during<br />
a period of five months. Patients who underwent CABG<br />
combined with a heart valve repair or replacement, resection<br />
of a ventricular aneurysm, or other surgical procedures<br />
were excluded. The study was approved by the division of<br />
cardiothoracic surgery and by the research department of the<br />
hospital.<br />
Data were collected prospectively during the patients’<br />
admission by interviews and physical examinations on the<br />
following variables: age; gender; body mass index (BMI);<br />
educational level; New York Heart Association (NYHA)<br />
functional class; number of diseased vessels; and left<br />
ventricular ejection fraction (LVEF). A history of myocardial<br />
infarction, smoking, alcohol abuse, opiate dependency,<br />
diabetes, hypercholesterolemia, hypertension, peripheral<br />
vascular disease, cerebrovascular disease, respiratory failure,<br />
and renal failure were also noted.<br />
Laboratory data included measured blood sugar in<br />
perioperative and glycated or glycosylated hemoglobin<br />
(HbA1c) at operation day.<br />
The patients’ data, risk factors, operation, and outcome<br />
data were recorded in a structured form. Perioperative<br />
medical characteristics were collected by research general<br />
practitioners. The data were transcribed onto the SPSS<br />
software by a data entry operator at a later date.<br />
Regarding educational level, three levels of education<br />
were categorized: 1 = primary school or lower; 2 =<br />
secondary school; and 3 = university/college or equivalents.<br />
Current smoker was defined as anybody who had smoked<br />
within one month of surgery. Alcohol abuse was defined<br />
as the consumption of alcohol despite recurrent adverse<br />
consequences. Daily regular use of opium products was<br />
defined as opium dependency according to the DSM-IV<br />
criteria. (American Psychiatric Association. Diagnostic<br />
and statistical manual of mental disorders: DSM-IV-TR.<br />
American Psychiatric Publishing, Inc.; 2000) Any cerebral<br />
neurological deficit induced by both cerebrovascular<br />
accident and transient ischemic attacks or previous cerebral<br />
surgery was defined as cerebrovascular disease. Peripheral<br />
vascular disease was defined as a history or any evidence<br />
of aneurysm or occlusive peripheral vascular disease on<br />
physical examination. After surgery, the patients who stayed<br />
in the ward for more than 2 consecutive days on the initial<br />
admission were classified as having a prolonged ward stay.<br />
A long cardiac surgical ICU stay was defined as > 2 days.<br />
The patients within the first 24 hours after bypass surgery<br />
were categorized into three groups according to the average<br />
amount of insulin intake: group 0 = zero U; group 1 = 1 to<br />
9 U; and group 2 = 10 or more U of insulin. The operations<br />
were performed by seven surgeons. The surgeons, in terms<br />
of mean total in-hospital duration of stay for the patients of<br />
each individual surgeon, were classified into 3 groups, as<br />
follows: 1 = total LOS < 8 days; 2 = 8 ≤ total LOS < 10<br />
days; and 3 = total LOS ≥ 10 days. 17 Central and peripheral<br />
circulations were measured by the amount of inotropic<br />
support and arterial blood gas parameters (base excess and pH<br />
in plasma), respectively. A wound infection was any wound<br />
infection in the sternum or leg incision following surgery.<br />
Postoperative arrhythmias were all observed rhythms that<br />
needed treatment rather than normal sinus rhythm.<br />
The numerical variables are presented as mean ± SD,<br />
while the categorized variables are summarized by absolute<br />
frequencies and percentages. The continuous variables<br />
were compared using the Student t-test, and the categorical<br />
variables were compared using the chi-square (or the<br />
Fisher exact test, as required) and the Mantel-Haenszel<br />
chi-square test for trend. A multivariate forward stepwise<br />
logistic regression model for risk factors predicting LOS<br />
in the ICU and the surgical ward was constructed. Through<br />
the multivariate forward stepwise analysis, the variables<br />
were entered into the logistic regression model according<br />
to their statistical significance (entering criterion p value ≤<br />
0.15). The associations between the independent predictors<br />
and LOS in the ICU or the surgical ward in the final model<br />
were expressed as odds ratios (OR) with 95% CIs. Model<br />
discrimination was measured using the c statistic, which<br />
is equal to the area under the ROC (Receiver Operating<br />
Characteristic) curve. Model calibration was estimated<br />
using the Hosmer-Lemeshow (HL) goodness-of-fit statistic<br />
(higher p values imply that the model fits the observed data<br />
better). For the statistical analyses, the statistical software<br />
The Journal of Tehran University Heart Center171
The Journal of Tehran University Heart Center<br />
Mahdi Najafi et al.<br />
SPSS version 13.0 for Windows (SPSS Inc., Chicago, IL)<br />
and the statistical package SAS version 9.1 for Windows<br />
(SAS Institute Inc., Cary, NC, USA) were used. All the p<br />
values were two-tailed, with statistical significance defined<br />
by p value ≤ 0.05.<br />
Results<br />
The baseline characteristics, preoperative data, and<br />
outcome variables of the CABG patients according to LOS in<br />
the ICU are presented in Table 1. Overall, 380/570 (66.7%)<br />
patients were discharged from the ICU in ≤ 48 hours, and 190<br />
(33.3%) patients spent > 48 hours in the ICU. Table 2 shows<br />
the predictors of LOS in the ICU in the patients, undergoing<br />
bypass surgery. Three most important variables were intraaortic<br />
balloon pump support, mean 24 hours’ insulin intake<br />
of ≥ 10 units, and NYHA functional class, with odds ratios<br />
of 25.5, 2.3, and 2.2, respectively.<br />
The relationship between the LOS in the ICU and the<br />
Table 1. Baseline characteristics of the coronary artery bypass graft patients according to length of stay in the Intensive Care Unit<br />
ICU stay ≤ 48 hours (n=380) ICU stay > 48 hours (n=190) P value<br />
Age (y) 58.44±8.80 60.21±9.20 0.026<br />
Male sex 290 (76.3) 139 (73.2) 0.410<br />
Body mass index (kg/m 2 ) 27.14±4.09 27.84±4.01 0.055<br />
Surgeon category 0.017<br />
1 218 (57.4) 102 (53.7)<br />
2 104 (27.4) 41 (21.6)<br />
3 58 (15.3) 47 (24.7)<br />
Cardiac risk factors<br />
Diabetes mellitus 159 (41.8) 74 (38.9) 0.508<br />
Hypertension 178 (46.8) 104 (54.7) 0.076<br />
Hyperlipidemia 264 (69.5) 136 (71.6) 0.605<br />
Cigarette smoking 138 (36.3) 68 (35.8) 0.902<br />
Family history of CAD 186 (48.9) 84 (44.2) 0.286<br />
Prior MI 187 (49.5) 100 (52.9) 0.440<br />
Prior CVA 10 (2.6) 12 (6.3) 0.031<br />
History of PVD 100 (26.3) 58 (30.5) 0.290<br />
NYHA functional class 0.032<br />
1 141 (37.1) 60 (31.6)<br />
2 193 (50.8) 93 (48.9)<br />
3 46 (12.1) 37 (19.5)<br />
LVEF (%) 48.88±9.80 47.78±11.38 0.253<br />
Number of diseased vessels 0.607<br />
1 12 (3.2) 9 (4.7)<br />
2 73 (19.2) 35 (18.4)<br />
3 295 (77.6) 146 (76.8)<br />
Operative details and complications<br />
Pump time (min) 68.45±20.36 73.19±25.24 0.025<br />
Number of grafts 3.70±0.94 3.79±0.99 0.265<br />
Intraoperative IABP-support 1 (0.3) 11 (5.8) < 0.001<br />
Endarterectomy 27 (7.1) 12 (6.3) 0.725<br />
Pacemaker dependents 33 (8.7) 20 (10.5) 0.475<br />
Inotropic drug use 148 (38.9) 90 (47.4) 0.055<br />
Arrhythmia 123 (32.4) 101 (53.2) < 0.001<br />
Perioperative MI 1 (0.3) 3 (1.6) 0.110<br />
Respiratory failure 56 (14.7) 48 (25.3) 0.002<br />
Wound infection 0 3 (1.6) 0.037<br />
Arterial blood gas parameters<br />
Mean BE within 6 hours after surgery (mmol/l) -5.42±2.55 -6.19±2.57 0.001<br />
pH < 7.34 within 6 hours after surgery 74 (19.5) 59 (31.1) 0.002<br />
Mean insulin intake within 24 hours after surgery < 0.001<br />
Zero U 193 (50.8) 69 (36.3)<br />
1 - 9 U 99 (26.1) 48 (25.3)<br />
≥ 10 U 88 (23.2) 73 (38.4)<br />
*<br />
Data are presented as mean±SD or n (%)<br />
ICU, Intensive Care Unit; CAD, Coronary artery disease; MI, Myocardial infarction; CVA, Cerebrovascular accident; PVD, Peripheral vascular disease;<br />
NYHA, New York Heart Association; LVEF, Left ventricular ejection fraction; IABP, Intra-aortic balloon pump; BE, Base excess<br />
172
Determinants of Length of Stay in Surgical Ward after Coronary Bypass Surgery ...<br />
<strong>TEHRAN</strong> <strong>HEART</strong> <strong>CENTER</strong><br />
Table 2. Predictors of length of stay in the Intensive Care Unit in patients undergoing bypass surgery<br />
Predictors<br />
Univariate analysis<br />
Multivariate analysis<br />
OR<br />
95% CI<br />
P value<br />
OR<br />
95% CI<br />
P value<br />
NYHA classification<br />
0.05<br />
0.02<br />
2 vs. 1<br />
1.13<br />
0.76-1.67<br />
1.17 0.77-1.79<br />
3 vs. 1<br />
1.89<br />
1.11-3.20<br />
2.15 1.22-3.79<br />
Surgeon category<br />
0.02<br />
0.04<br />
Group 2 vs. 1<br />
0.84<br />
0.54-1.29<br />
0.69 0.43-1.12<br />
Group 3 vs. 1<br />
1.73<br />
1.10-2.71<br />
1.47 0.91-2.38<br />
Intra-aortic balloon pump<br />
support<br />
23.29<br />
2.98-181.79 < 0.01 25.22 3.14-202.43 < 0.01<br />
Postoperative arrhythmia<br />
2.37<br />
1.65-3.38<br />
< 0.01<br />
1.95 1.33-2.86<br />
< 0.01<br />
Mean BE within 6 hours<br />
after surgery<br />
0.88<br />
0.82-0.95<br />
< 0.01<br />
0.90 0.83-0.97<br />
< 0.01<br />
Mean insulin intake within<br />
24 hours after surgery *<br />
1 vs. 0<br />
1.35<br />
0.87-2.10<br />
< 0.01<br />
1.31 0.82-2.09<br />
< 0.01<br />
2 vs. 0<br />
*<br />
Group 0 = Zero U<br />
Group 1 = 1 to 9 U<br />
Group 2 = ≥ 10 U<br />
2.32<br />
1.53-3.51<br />
2.27 1.45-3.55<br />
OR, Odds ratio; CI, Confidence interval; NYHA, New York Heart Association; BE, Base excess; AUC, Area under the Receiver Operating Characteristic<br />
Curve (c = 0.70)<br />
Table 3. Durations of Intensive Care Unit, surgical ward and total hospital stay as well as in-hospital mortality rate for both study groups *<br />
Group A<br />
Group B<br />
Patients with ICU stay ≤ 48h (n=380)<br />
Patients with ICU stay > 48h (n=190)<br />
P value<br />
ICU stay (hr) 27.38±9.30 85.79±34.87<br />
Surgical ward stay (d) 2.78±1.79 2.63±2.35 0.43<br />
Total hospital stay (d) 7.21±2.84 9.85±7.36 < 0.01<br />
In-hospital mortality 0 3 (1.6) 0.04<br />
*<br />
Data are presented as mean±SD or n (%)<br />
Table 4. Comparison of patients with regard to LOS in ward after CABG *<br />
Ward stay ≤ 3 days (n=426) Ward stay > 3 days (n=144) P value<br />
Male sex<br />
336 (78.9) 93 (64.6) < 0.01<br />
Body mass index (kg/m 2 ) 27.13±3.96 28.12±4.31 0.01<br />
Education class ** < 0.01<br />
1 218 (51.2) 94 (65.3)<br />
2 133 (31.2) 36 (25.0)<br />
3 75 (17.6) 14 (9.7)<br />
Diabetes mellitus 153 (35.9) 80 (55.6) < 0.01<br />
Family history of CAD 191 (44.8) 79 (54.9) 0.04<br />
History of PVD 104 (24.4) 54 (37.5) < 0.01<br />
Inotropic drug use 166 (39.0) 72 (50.0) 0.02<br />
Postoperative arrhythmia 179 (42.0) 45 (31.3) 0.02<br />
HbA1C at operation day 5.83±1.58 6.55±1.90 < 0.01<br />
Last fasting blood sugar 103.58±30.41 119.45±46.88 < 0.01<br />
Mean insulin intake within 24 hours after surgery *** < 0.01<br />
0 220 (51.6) 42 (29.2)<br />
1 100 (23.5) 47 (32.6)<br />
2 106 (24.9) 55 (38.2)<br />
Mean BG within the first 24 hours after surgery (mg/dl) 167.41±26.28 176.49±28.10 < 0.01<br />
Blood urea nitrogen (mg/dl) 38.86±11.56 42.19±12.92 < 0.01<br />
Total cholesterol (mg/dl) 157.97±43.89 169.19±47.32 < 0.01<br />
*<br />
Data are presented as mean±SD or n (%)<br />
**<br />
1 = primary school or lower; 2 = secondary school; 3 = university/college or equivalents<br />
***<br />
Group 0 = Zero U; Group 1 = 1 to 9 U; Group 2 ≥ 10 U<br />
LOS, Length of stay; CABG, Coronary artery bypass surgery; CAD, Coronary artery disease; PVD, Peripheral vascular disease; HbA1C, Glycosylated<br />
hemoglobin; BG, Blood glucose<br />
The Journal of Tehran University Heart Center173
The Journal of Tehran University Heart Center<br />
Mahdi Najafi et al.<br />
Table 5. Predictors of length of stay at surgical ward in patients undergoing bypass surgery<br />
Univariate analysis<br />
Multivariate analysis<br />
OR 95% CI P value OR 95% CI P value<br />
Peripheral vascular disease 1.858 1.241-2.781 < 0.01 1.568 1.013-2.426 0.04<br />
HbA1c 1.268 1.133-1.419 < 0.01 1.210 1.074-1.362 < 0.01<br />
Last fasting blood sugar 1.011 1.006-1.016 < 0.01 1.009 1.003-1.014 < 0.01<br />
Inotropic drug use 1.566 1.071-2.291 0.02 1.638 1.088-2.465 0.02<br />
Postoperative arrhythmia 0.627 0.420-0.937 0.02 0.531 0.343-0.822 0.01<br />
Mean insulin intake within 24 hours after surgery * < 0.01 < 0.01<br />
1 vs. 0 2.462 1.525-3.973 2.455 1.487-4.054<br />
2 vs. 0 2.718 1.709-4.321 2.708 1.648-4.450<br />
*<br />
Group 0 = Zero U<br />
Group 1 = 1 to 9 U<br />
Group 2 ≥ 10 U<br />
OR, Odds ratio; CI, Confidence interval; NYHA, New York Heart Association; HbA1c, Glycosylated hemoglobin<br />
surgical ward was investigated through a comparison of the<br />
average ICU, surgical ward, and total hospital stay as well<br />
as in-hospital mortality rate between two groups of ICU stay<br />
( ≤ 48 and > 48 hours) as listed in Table 3. The overall inhospital<br />
mortality rate was 0.5%.<br />
In all the patients studied, the LOS at the cardiac surgical<br />
ward ranged from 1 to 14 days (mean ± SD, 2.73 ± 1.99<br />
days) with a median of 2 days. Patients with a prolonged<br />
surgical ward stay (144/570, 25.3%) were more likely to be<br />
women and have diabetes, family history of coronary artery<br />
disease, history of peripheral disease, and lower educational<br />
level.<br />
Table 4 compares the patients’ characteristics by taking<br />
into consideration the LOS in the ward after cardiac surgery.<br />
Among the important factors that were significantly different<br />
between the two groups, i.e. LOS > 3 days and LOS ≤ 3 days,<br />
five factors were independent predictors. Three predictors<br />
were indices of glycemic control (Table 5). The area under<br />
the Receiver Operating Characteristic Curve (AUC) was<br />
found to be 0.71, which showed a good predictive accuracy<br />
in the variables included in the model. The model was also<br />
found to fit the data well since the Hosmer-Lemeshow p<br />
value was 0.88 (p < 0.05 indicated a poor fit).<br />
Discussion<br />
In the current study, we included preoperative,<br />
intraoperative, and immediate postoperative variables to<br />
find LOS determinants in 570 CABG patients after bypass<br />
surgery. The six variables of intra-aortic balloon pump<br />
(IABP), NYHA functional class, postoperative arrhythmia,<br />
24-hour average insulin intake, mean 6-hour BE, and surgeon<br />
category were found to be the independent predictors of<br />
an ICU LOS greater than 48 hours. We also found five<br />
predictors to be the independent risk factors for an increased<br />
cardiac surgical ward LOS. Considerable reports have been<br />
published on the predictors of LOS in the ICU following<br />
CABG 4-12 and some studies have investigated factors<br />
increasing postoperative hospital stay. 13-16 To our knowledge,<br />
however, no study has focused on the determinants of the<br />
LOS of cardiac surgical wards. Thus, we think that our study<br />
may contribute to the literature in this regard.<br />
Over the past two decades, attempts have been made to find<br />
the determinants of postoperative LOS in CABG patients.<br />
Be that as it may, a great disparity in type and number of<br />
independent variables analyzed has been reported. Although<br />
most of outcome studies with the focus on LOS have<br />
investigated only preoperative and intraoperative variables,<br />
there are some outcome research reports with immediate<br />
6, 13<br />
postoperative variables included.<br />
Poor cardiac output states, as reflected by the need for<br />
an IABP and inotropic therapy, have been identified as a<br />
predictor of a prolonged ICU stay in several studies. 6, 8, 9 In<br />
the present study, use of IABP was an ICU stay predictor,<br />
whereas inotropic support was a surgical ward stay predictor.<br />
Additionally, both reflected cardiac output.<br />
Need for an IABP was identified as an independent<br />
risk factor for ICU stay longer than 48 hours in three<br />
studies. 18-20 In contrast, Doering et al. showed that only early<br />
hemodynamic instability was indicative of an ICU stay<br />
longer than 24 hours, whereas postoperative IABP and use<br />
of inotropic drugs were not. 9 Michalopoulos et al. also noted<br />
that the number of inotropes, rather than inotrope use itself,<br />
was the significant factor. 6<br />
These differences may result from different treatment<br />
protocols or the way in which variables such as the use of<br />
inotropes were defined. Michaloupolous et al. used a 6- hour<br />
window for starting inotropic support after surgery and did<br />
not consider vasodilators. 6 By contrast, in the Doering et al.<br />
study, a 3-hour period was adopted and after-load reducers<br />
such as nitroprusside were considered in the definition of<br />
inotropic support. 9 Christakis et al. did not consider inotropic<br />
support alone, adding to IABP support in defining low output<br />
state. 7<br />
Some disparities in study results may be due to various<br />
study populations and treatment protocols, different cut-offs<br />
used to define a prolonged stay in the ICU (from ≥ 2 to 10<br />
174
Determinants of Length of Stay in Surgical Ward after Coronary Bypass Surgery ...<br />
<strong>TEHRAN</strong> <strong>HEART</strong> <strong>CENTER</strong><br />
days), 5, 14, 21-23 differences in variables definitions, and the<br />
large number of variables that could be considered. 4<br />
The main difference between our study and those described<br />
above is that we took into account surgeon category and<br />
amount of insulin administered during a 24-hour period after<br />
CABG. We found that a patient’s surgeon could potentially<br />
influence the duration of ICU stay and that there were<br />
differences in the average length of ICU stay between the<br />
surgeons at our hospital. 17 It may indicate the necessity of<br />
using a unique protocol for discharging the patients from<br />
the ICU and hospital after surgery. We also found that the<br />
LOS in the ICU and ward depended predominantly on the<br />
amount of insulin received by the patients during the first 24-<br />
hour postoperative period. In addition, we could not show<br />
any association between the LOS in the ICU and that in the<br />
surgical ward (Table 3). As a result, a prolonged stay in the<br />
ICU probably is not an independent predictor of surgical<br />
ward stay.<br />
We found that the blood glucose control indices, including<br />
HbA1c and last fasting blood sugar (FBS) before surgery,<br />
were the risk factors for an extended LOS in surgical wards<br />
in patients undergoing CABG, diabetic or non-diabetic.<br />
Finding both HbA1c and FBS as the determinants of<br />
the LOS in the surgical ward suggests that HbA1c is an<br />
independent predictor of hospital stay regardless of the level<br />
of blood sugar. However, as HbA1c is an index of glycemic<br />
control during previous months, its level is independent of<br />
perioperative events. It may, therefore, be a more stable<br />
and reliable perioperative marker. HbA1c has been used<br />
as a marker of short-term glycemic control in diabetic<br />
patients for many years. Recently, the American Diabetes<br />
Association included HbA1c in diabetes mellitus diagnosis<br />
criteria. 24 The role of HbA1c in predicting morbidity and<br />
mortality in non-diabetic healthy people has been suggested<br />
by some population-based studies. 25, 26 However, there is<br />
limited knowledge about the prognostic role of HbA1c for<br />
perioperative outcome, and the relationship between HbA1c<br />
and postoperative outcome in cardiovascular surgery is<br />
controversial. 27-30<br />
Our study revealed that HbA1c could predict postoperative<br />
LOS in the surgical ward and not in the ICU. This may be<br />
explained by the hampering effect of more important strong<br />
cofactors such as IABP and NYHA functional class.<br />
Conclusion<br />
Among the five predictors of the LOS in the surgical<br />
ward, three were the indices of glycemic control. HbA1c is<br />
the most reliable marker of outcome because its level is not<br />
influenced by perioperative events. Taking these findings<br />
into consideration, the prognostic role of HbA1c for the<br />
LOS following CABG is promising. We would, therefore,<br />
recommend its use as a simple predictor of outcome after<br />
cardiac surgery in daily practice.<br />
Acknowledgments<br />
This study was approved and supported by Tehran<br />
University of Medical Sciences.<br />
References<br />
1. Nilsson J, Algotsson L, Höglund P, Lührs C, Brandt J. EuroSCORE<br />
predicts intensive care unit stay and costs of open heart surgery.<br />
Ann Thorac Surg 2004;78:1528-1534.<br />
2. Riordan CJ, Engoren M, Zacharias A, Schwann TA, Parenteau GL,<br />
Durham SJ, Habib RH. Resource utilization in coronary artery<br />
bypass operation: does surgical risk predict cost Ann Thorac Surg<br />
2000;69:1092-1097.<br />
3. Doering LV, Esmailian F, Laks H. Perioperative predictors of ICU<br />
and hospital costs in coronary artery bypass graft surgery. Chest<br />
2000;118:736-743.<br />
4. Tuman KJ, McCarthy RJ, March RJ, Najafi H, Ivankovich AD.<br />
Morbidity and duration of ICU stay after cardiac surgery. A model<br />
for preoperative risk assessment. Chest 1992;102:36-44.<br />
5. Tu JV, Mazer CD, Levinton C, Armstrong PW, Naylor CD. A<br />
predictive index for length of stay in the intensive care unit<br />
following cardiac surgery. CMAJ 1994;151:177-185.<br />
6. Michalopoulos A, Tzelepis G, Pavlides G, Kriaras J, Dafni U,<br />
Geroulanos S. Determinants of duration of ICU stay after coronary<br />
artery bypass graft surgery. Br J Anaesth 1996;77:208-212.<br />
7. Christakis GT, Fremes SE, Naylor CD, Chen E, Rao V, Goldman<br />
BS. Impact of preoperative risk and perioperative morbidity on<br />
ICU stay following coronary bypass surgery. Cardiovasc Surg<br />
1996;4:29-35.<br />
8. Ryan TA, Rady MY, Bashour CA, Leventhal M, Lytle B, Starr NJ.<br />
Predictors of outcome in cardiac surgical patients with prolonged<br />
intensive care stay. Chest 1997;112:1035-1042.<br />
9. Doering LV, Esmailian F, Imperial-Perez F, Monsein S.<br />
Determinants of intensive care unit length of stay after coronary<br />
artery bypass graft surgery. Heart Lung 2001;30:9-17.<br />
10. Janssen DP, Noyez L, Wouters C, Brouwer RM. Preoperative<br />
prediction of prolonged stay in the intensive care unit for coronary<br />
bypass surgery. Eur J Cardiothorac Surg 2004;25:203-207.<br />
11. Ghotkar SV, Grayson AD, Fabri BM, Dihmis WC, Pullan DM.<br />
Preoperative calculation of risk for prolonged intensive care unit<br />
stay following coronary artery bypass grafting. J Cardiothorac<br />
Surg 2006;1:14.<br />
12. Rosenfeld R, Smith JM, Woods SE, Engel AM. Predictors and<br />
outcomes of extended intensive care unit length of stay in patients<br />
undergoing coronary artery bypass graft surgery. J Card Surg<br />
2006;21:146-150.<br />
13. Weintraub WS, Jones EL, Craver J, Guyton R, Cohen C.<br />
Determinants of prolonged length of hospital stay after coronary<br />
bypass surgery. Circulation 1989;80:276-284.<br />
14. Mounsey JP, Griffith MJ, Heaviside DW, Brown AH, Reid DS.<br />
Determinants of the length of stay in intensive care and in hospital<br />
after coronary artery surgery. Br Heart J 1995;73:92-98.<br />
15. Lazar HL, Fitzgerald C, Gross S, Heeren T, Aldea GS, Shemin RJ.<br />
Determinants of length of stay after coronary artery bypass graft<br />
surgery. Circulation 1995;92:II20-24.<br />
16. Jensen L, Yang L. Risk factors for postoperative pulmonary<br />
complications in coronary artery bypass graft surgery patients. Eur<br />
J Cardiovasc Nurs 2007;6:241-246.<br />
17. Najafi M, Goodarzinejad H, Sheikhfathollahi M, Adibi H. Role of<br />
surgeon in length of stay in ICU after cardiac bypass surgery. J Teh<br />
Univ Heart Ctr 2010;1:9-13.<br />
18. Wong DT, Cheng DC, Kustra R, Tibshirani R, Karski J, Carroll-<br />
The Journal of Tehran University Heart Center175
The Journal of Tehran University Heart Center<br />
Mahdi Najafi et al.<br />
Munro J, Sandler A. Risk factors of delayed extubation, prolonged<br />
length of stay in the intensive care unit, and mortality in patients<br />
undergoing coronary artery bypass graft with fast-track cardiac<br />
anesthesia: a new cardiac risk score. Anesthesiology 1999;91:936-<br />
944.<br />
19. Bucerius J, Gummert JF, Walther T, Doll N, Falk V, Schmitt DV,<br />
Mohr FW. Predictors of prolonged ICU stay after on-pump versus<br />
off-pump coronary artery bypass grafting. Intensive Care Med<br />
2004;30:88-95.<br />
20. Hein OV, Birnbaum J, Wernecke K, England M, Konertz W, Spies<br />
C. Prolonged intensive care unit stay in cardiac surgery: risk factors<br />
and long-term-survival. Ann Thorac Surg 2006;81:880-885.<br />
21. Staat P, Cucherat M, George M, Lehot JJ, Jegaden O, André-Fouët<br />
X, Beaune J. Severe morbidity after coronary artery surgery:<br />
development and validation of a simple predictive clinical score.<br />
Eur Heart J 1999;20:960-966.<br />
22. Kurki TS, Kataja M. Preoperative prediction of postoperative<br />
morbidity in coronary artery bypass grafting. Ann Thorac Surg<br />
1996;61:1740-1745.<br />
23. Miller KH. Factors influencing selected lengths of ICU stay for<br />
coronary artery bypass patients. J Cardiovasc Nurs 1998;12:52-61.<br />
24. American Diabetes Association. Diagnosis and classification of<br />
diabetes mellitus. Diabetes Care 2010;33:S62-69.<br />
25. Silbernagel G, Grammer TB, Winkelmann BR, Boehm BO, März<br />
W. Glycated hemoglobin predicts all-cause, cardiovascular, and<br />
cancer mortality in people without a history of diabetes undergoing<br />
coronary angiography. Diabetes Care 2011;34:1355-1361.<br />
26. Selvin E, Steffes MW, Zhu H, Matsushita K, Wagenknecht L,<br />
Pankow J, Coresh J, Brancati FL. Glycated hemoglobin, diabetes,<br />
and cardiovascular risk in nondiabetic adults. N Engl J Med<br />
2010;362:800-811.<br />
27. Liu Y, Yang YM, Zhu J, Tan HQ, Liang Y, Li JD. Prognostic<br />
significance of hemoglobin A1c level in patients hospitalized with<br />
coronary artery disease. A systematic review and meta-analysis.<br />
Cardiovasc Diabetol 2011;10:98.<br />
28. Medhi M, Marshall MC, Jr, Burke HB, Hasan R, Nayak D, Reed G,<br />
LaFaro R, Southren AL. HbA1c predicts length of stay in patients<br />
admitted for coronary artery bypass surgery. Heart Dis 2001;3:77-<br />
79.<br />
29. O’Sullivan CJ, Hynes N, Mahendran B, Andrews EJ, Avalos G,<br />
Tawfik S, Lowery A, Sultan S. Haemoglobin A1c (HbA1C) in nondiabetic<br />
and diabetic vascular patients. Is HbA1C an independent<br />
risk factor and predictor of adverse outcome Eur J Vasc Endovasc<br />
Surg 2006;32:188-197.<br />
30. Goode KM, John J, Rigby AS, Kilpatrick ES, Atkin SL, Bragadeesh<br />
T, Clark AL, Cleland JG. Elevated glycated haemoglobin is a<br />
strong predictor of mortality in patients with left ventricular<br />
systolic dysfunction who are not receiving treatment for diabetes<br />
mellitus. Heart 2009;95:917-923.<br />
176
<strong>TEHRAN</strong> <strong>HEART</strong> <strong>CENTER</strong><br />
Original Article<br />
Obvious or Subclinical Right Ventricular Dysfunction in<br />
Diabetes Mellitus (Type II): An Echocardiographic Tissue<br />
Deformation Study<br />
Mozhgan Parsaee, MD * , Parvaneh Bahmanziari, MD, Maryam Ardeshiri, MD,<br />
Maryam Esmaeilzadeh, MD<br />
Rajaei Cardiovascular, Medical and Research Center, Tehran University of Medical Sciences, Tehran,<br />
Iran.<br />
Received 20 May 2011; Accepted 07 March 2012<br />
Abstract<br />
Background: Diabetes mellitus is capable of impairing the myocardial function. Several studies have documented the<br />
influential impact of diabetes mellitus on the left ventricular function. The right ventricular function plays a significant role<br />
in the overall myocardial contractility; hence, this study was undertaken to evaluate the effect of diabetes mellitus type II on<br />
the right ventricular function.<br />
Methods: Twenty-two diabetic patients without any coronary artery disease, hypertension, or left ventricular dysfunction<br />
were studied. The right ventricular end diastolic diameter, tricuspid plane systolic excursion, right ventricular inflow Doppler<br />
parameters, longitudinal myocardial velocities, and deformation indices from the basal and apical segments of the right<br />
ventricular free wall of the case group were measured. The control group consisted of 22 healthy individuals.<br />
Results: The tricuspid annular plane systolic excursion (TAPSE) and tricuspid peak early to peak late diastolic flow<br />
velocities ratio (E/A) in the diabetic patients were significantly lower than those of the control group patients (18.9 vs. 23.2,<br />
p value < 0.001 and 0.96 vs. 1.21, p value = 0.012), but there were no significant differences in the right ventricular end<br />
diastolic diameter and the right ventricular Tei index between the two groups (p value = 0.72). The right ventricular basal<br />
peak myocardial systolic velocity (SM) (12 cm/sec vs. 13.4 cm/sec; p value = 0.03), basal and apical right ventricular free<br />
wall systolic strain (-13.3% and -18.7% vs. -20.2% and -25.7%; p value = 0.001), and apical strain rate (-1.2 1/s vs. -1.6 1/s;<br />
p value = 0.008 ) were significantly lower in the study group. There was a weak correlation between the right ventricular<br />
function and HbA1c as well as the duration of diabetes mellitus and C-reactive protein.<br />
Conclusion: Our results suggest that diabetes mellitus type II can influence the right ventricular function in the absence of<br />
coronary artery disease, diastolic dysfunction, and pulmonary hypertension.<br />
J Teh Univ Heart Ctr 2012;7(4):177-181<br />
This paper should be cited as: Parsaee M, Bahmanziari P, Ardeshiri M, Esmaeilzadeh M. Obvious or Subclinical Right Ventricular<br />
Dysfunction in Diabetes Mellitus (Type II): An Echocardiographic Tissue Deformation Study. J Teh Univ Heart Ctr 2012;7(4):177-181.<br />
Keywords: Echocardiography • Diabetes mellitus • Ventricular function, right<br />
*<br />
Corresponding Author: Mozhgan Parsaee, Assistant Professor of Cardiology, Department of Echocardiography, Rajaei Cardiovascular, Medical<br />
and Research Center, Vali-Asr Ave. Adjacent to Mellat Park, Tehran, Iran. 1996911151. Tel: +98 21 23922930. Fax: +98 21 2055594. E-mail:<br />
parsaeemozhgan@yahoo.com.<br />
The Journal of Tehran University Heart Center 177
The Journal of Tehran University Heart Center<br />
Introduction<br />
Diabetes mellitus (DM) increases the risk of heart failure<br />
development even in the absence of coronary artery disease,<br />
hypertension, or other comorbidities 1, 2 and could result in<br />
a two to fourfold greater mortality in heart failure patients.<br />
Indeed, DM is capable of impairing the myocardial function:<br />
this is initially a clinically silent condition; nevertheless, if<br />
left unrecognized and insufficiently managed, it could beget<br />
overt diabetic cardiomyopathy.<br />
The right ventricular (RV) function plays a significant<br />
role in the overall myocardial contractility. 3 Nevertheless,<br />
most of the previous studies regarding diabetes-induced<br />
changes in myocardial dysfunction were dedicated to the left<br />
ventricle (LV) at the cost of ignoring the role of the right<br />
heart chambers. The existing literature of course does contain<br />
a limited number of studies on the RV cardiomyopathies of<br />
patients with DM type I; however, to our knowledge, there<br />
is only one recent study probing into DM type II drawing up<br />
on three-dimensional strain and strain rate.<br />
The objectives of the present study were to evaluate the<br />
RV systolic and diastolic functions using conventional<br />
echocardiography, tissue Doppler imaging (TDI), and<br />
deformation indices (strain and strain rate) in patients with<br />
DM type II and without coronary artery disease or LV<br />
dysfunction.<br />
Methods<br />
The study group was comprised of 22 diabetic patients (9<br />
men and 13 women) aged 55.6 ± 6.0 years. These patients<br />
either referred to the DM Clinic of Rajaei Cardiovascular,<br />
Medical and Research Center or were amongst the hospital<br />
stuff. The control group consisted of 22 healthy individuals<br />
(9 men and 13 women). All the diabetic patients enrolled<br />
in this study were asymptomatic, without any clinical<br />
evidence of either systolic or diastolic heart failure. The<br />
control subjects were considered to have a low probability<br />
of coronary disease or heart failure based on clinical data.<br />
Coronary artery disease was excluded if there was a<br />
negative Dobutamine stress echocardiographic examination<br />
or a negative treadmill exercise electrocardiographic test.<br />
In a few cases, coronary artery disease was excluded on the<br />
evidence of equivocal non-invasive stress tests and normal<br />
coronary angiograms. The other exclusion criteria included<br />
valvular or congenital heart disease, left ventricular ejection<br />
fraction (LVEF) less than 50%, rhythms other than normal<br />
sinus rhythm, documented pulmonary diseases or pulmonary<br />
hypertension, and tricuspid regurgitation more than a mild<br />
degree.<br />
All the diabetic patients were on a diet and treatment with<br />
oral hypoglycemic drugs. Plasma glucose and HbA1c were<br />
observed periodically and controlled by the endocrinologist<br />
Mozhgan Parsaee et al.<br />
in the aforementioned clinic. None of the patients had such<br />
diabetic complications as progressive and complex diabetic<br />
retinopathy, neuropathy, and nephropathy.<br />
The study participants in the two groups underwent<br />
echocardiographic examinations (Vivid 7, GE Vingmed).<br />
The variables measured are presented as follows:<br />
1. The RV dimension and tricuspid annular plane systolic<br />
excursion (TAPSE) were measured from the apical fourchamber<br />
view.<br />
2. The RV Doppler parameters of the diastolic function<br />
(peak early [A] and peak late diastolic flow velocity [E],<br />
together with their ratio [E/A] and deceleration time [DT])<br />
were recorded. The trans-tricuspid flow was measured in the<br />
apical four-chamber view using pulsed Doppler, with the<br />
sample volume positioned at the tips of the tricuspid leaflets.<br />
The measurements were averaged from three end-expiratory<br />
cycles.<br />
3. TDI was conducted to assess the RV longitudinal<br />
myocardial function in the apical four-chamber view. Color<br />
TDI was used in addition to two-dimensional images,<br />
with adjustment of the depth and sector angle to obtain an<br />
acceptable frame rate. The TDI variables of peak systolic<br />
velocity (Sm), peak early diastolic velocity (Em), peak late<br />
diastolic velocity (Am), myocardial performance index<br />
(MPI), and acceleration time of the isovolumetric contraction<br />
time (IVCT) were analyzed online.<br />
4. The deformation indices were measured by adjusting the<br />
imaging angle to achieve a parallel alignment of the beam<br />
with the myocardial segment of interest. The images were<br />
stored on a remote archive of the echocardiography machine<br />
so that they could be analyzed offline. The myocardial<br />
deformation curves were investigated from the basal segment<br />
of the RV free wall, which belongs to the inflow part of the<br />
RV, and also from the apical segment, which belongs to the<br />
trabecular portion of the RV.<br />
5. The strain rate and stain were measured based on the<br />
standard deformation measurement, and the peak of the R<br />
on the electrocardiography (ECG) was utilized to define<br />
end diastole. End systole was determined using the pulsed<br />
Doppler velocity profile of the left ventricular outflow tract<br />
(LVOT) as the aortic valve closure, and the RV end systole<br />
was determined using the pulsed wave profile of the right<br />
ventricular outflow tract (RVOT) at end expiration. The<br />
analysis of the myocardial strain and strain rate data included<br />
the assessment of the systolic strain (є), peak systolic strain<br />
rate (SRs), and peak early diastolic strain rate (SRe).<br />
The data are expressed as Mean ± SD and percentages. The<br />
Student unpaired t-test was used to evaluate the differences<br />
between the groups, and the chi-square test was employed to<br />
compare the categorical variables. The Pearson correlation<br />
coefficients were utilized to pair the continuous variables.<br />
A two-tailed p value < 0.05 was considered significant. For<br />
the statistical analyses, the statistical software SPSS version<br />
17.0 for Windows (SPSS Inc., Chicago, IL) was used.<br />
178
Table 1. Demographic characteristics of the studied groups * Diabetic group Control subjects P value<br />
Table 2. Echocardiographic and Doppler data of the studied groups * Diabetic group Control subjects P value<br />
Obvious or Subclinical Right Ventricular Dysfunction in Diabetes Mellitus (Type II): ...<br />
<strong>TEHRAN</strong> <strong>HEART</strong> <strong>CENTER</strong><br />
Results<br />
The demographic characteristics and clinical parameters<br />
of the participants are depicted in Tables 1. There were no<br />
significant differences between the two groups in terms<br />
of sex, age, body mass index, creatinine, total cholesterol<br />
level, low-density lipoprotein cholesterol (LDL), highdensity<br />
lipoprotein cholesterol (HDL), and being a smoker.<br />
The diabetic group, however, showed a higher level of<br />
triglyceride (p value = 0.049), but this was statistically, and<br />
not clinically, significant.<br />
The echocardiographic and Doppler data of the studied<br />
groups are illustrated in Table 2. There were no significant<br />
differences between the two groups as regards the right<br />
ventricular end diastolic diameter (RVEDD) (mm), and<br />
tricuspid E velocity, whereas the tricuspid annular plane<br />
systolic excursion (TAPSE), and tricuspid E/A ratio of the<br />
diabetic patients (18.9 ± 2.1 vs. 23.2 ± 2.9 and 0.96 ± 0.2<br />
vs. 1.21 ± 0.3, respectively) were significantly lower. The<br />
tricuspid A velocity and E wave deceleration time of the<br />
diabetic patients (0.5 ± 0.1 m/s vs. 0.4 ± 0.1 m/s and 289.2<br />
± 67 msec vs. 250.9 ± 57.1 msec) were significantly higher.<br />
Age (y) 54.5±7.0 49.8±8.4 0.05<br />
Male 9 (40.9) 9 (40.9) 0.69<br />
Hypertension 9 (40.9) 4 (18.2) 0.07<br />
Smoking 2 (9.1) 3 (13.6) 0.82<br />
Body mass index (Kg/m 2 ) 28.7±3.1 26.4±3.8 0.05<br />
Systolic blood pressure (mm Hg) 125.6±15.4 120.5±13.4 0.28<br />
Diastolic blood pressure (mm Hg) 79.5±11.6 76.1±10.5 0.32<br />
Creatinine (mg/dl) 1.0±0.2 1.1±0.1 0.47<br />
Total cholesterol (mg/dl) 178.4±40.0 166.0 ±37.0 0.39<br />
Duration of diabetes (y) 7.0±3.0 - -<br />
Triglyceride (mg/dl) 186.0±82.0 130.0±67.0 0.04<br />
Low-density lipoprotein cholesterol (mg/dl) 90.0±26.0 89.0±27.0 0.96<br />
*<br />
Data are presented as mean±SD or n (%)<br />
Right ventricular end diastolic diameter (mm) 28.0±2.9 28.0±3.7 0.56<br />
Tricuspid annular plane systolic excursion (mm) 18.9±2.1 23.2±2.9 < 0.01<br />
Tricuspid E velocity (m/s) 0.47±0.05 0.46±0.08 0.52<br />
Tricuspid A velocity (m/s) 0.5±0.1 0.4±0.1 0.04<br />
Tricuspid deceleration time (msec) 289.2±67.0 250.9±57.1 0.04<br />
E/A ratio 0.9±0.2 1.2±0.3 0.01<br />
*<br />
Data are presented as mean±SD<br />
E/A, Tricuspid peak early to peak late diastolic flow velocities ratio<br />
Table 3. Tissue Doppler imaging data of the studied groups * Diabetic group Control subjects P value<br />
Right ventricular basal segment Sm (cm/s) 12.0±1.9 13.4±2.1 0.03<br />
Right ventricular basal segment Em (cm/s) 8.5±2.1 11.6±2.4 < 0.01<br />
Right ventricular basal segment Am (cm/s) 12.6±2.7 14.7±3.3 0.03<br />
Myocardial performance index 0.42±0.11 0.40±0.09 0.72<br />
Acceleration time of the isovolumetric contraction time (ms) 37.8±8.4 35.4±8.4 0.45<br />
E/Em ratio 0.05±0.01 0.04±0.01 < 0.01<br />
*<br />
Data are presented as mean±SD<br />
Sm, Peak myocardial systolic velocity; Em, Peak early diastolic velocity; Am, Peak late diastolic velocity; E, Peak late diastolic flow velocity<br />
The Journal of Tehran University Heart Center179
The Journal of Tehran University Heart Center<br />
Mozhgan Parsaee et al.<br />
Table 4. Deformation indices data of the studied groups * Diabetic group Control subjects P value<br />
Right ventricular basal Є (%)<br />
Right ventricular basal SRs (1/s)<br />
Right ventricular basal SRe (1/s)<br />
Right ventricular apical Є (%)<br />
Right ventricular apical SRs (1/s)<br />
Right ventricular apical SRe (1/s)<br />
*<br />
Data are presented as mean±SD<br />
Є, Systolic stain; SRs, Peak systolic strain rate; SRe, Early diastolic strain rate<br />
-13.3±4.3 -20.2±7.3 < 0.01<br />
-1.0±0.5 -1.37±0.9 0.18<br />
0.9±0.3 1.2±0.5 0.05<br />
-18.7±4.3 -25.7±8.2 < 0.01<br />
-1.2±0.3 -1.6±0.6 < 0.01<br />
1.2±0.4 1.9±0.7 < 0.01<br />
The TDI data of the study population are shown in Table<br />
3, according to which the RV basal segment Sm, Em, Am,<br />
and E/Em (12 ± 1.9 cm/sec vs. 13.4 ± 2.1 cm/sec, 8.5 ± 2.1<br />
cm/sec vs. 11.6 ± 2.4 cm/sec, 12.6 ± 2.7 cm/sec vs. 14.7 ±<br />
3.3 cm/sec, and 0.05 ± 0.01 vs. 0.04 ± 0.01, respectively)<br />
were significantly lower in the case group than in the control<br />
group. There were no significant differences between the two<br />
groups with respect to the MPI of the RV and the acceleration<br />
time of the IVCT.<br />
The data on the deformation indices of the two study<br />
groups are demonstrated in Table 4, according to which the<br />
RV basal segment systolic strain (Є) and RV apical segment<br />
(Є, SRs, and SRe) of the case group were significantly lower<br />
than those in the control group (p value < 0.01). There were,<br />
however, no significant differences in regard to the RV basal<br />
segment SRs and SRe between the two groups.<br />
There were no significant correlations between HBA1c,<br />
duration of diabetes, C-reactive protein (CRP), and measures<br />
of the RV systolic or diastolic dysfunction (based on<br />
conventional Doppler, TDI data, or deformation indices).<br />
Discussion<br />
The present study shows that both systolic and diastolic<br />
RV functions are impaired in patients with DM type II and<br />
without coronary artery disease or ejection fractions of less<br />
than 50%. This finding was demonstrated by significantly<br />
lower RV systolic parameters (TAPSE, RV basal Sm, basal<br />
and apical RV free wall systolic strains, and apical SRs) and<br />
lower RV diastolic parameters (E/A ratios, Em, Am, E/Em<br />
ratios, and apical early diastolic strain rate [SRe]) in our case<br />
group than those in a normal, sex- and age-matched control<br />
group. There were no statistically significant differences in<br />
the RV basal segment SRs and SRe between the diabetic and<br />
control subjects, which may be due to difficulties in drawing<br />
basal RV strain rate curves.<br />
Our results chime in with those of the Kosmala et al., 4<br />
study, which reported the impairment of both basal and apical<br />
segments of the RV free wall performance. In that study,<br />
however, the apical segments exhibited more pronounced<br />
systolic impairment than did the basal segments and it<br />
was concluded that the RV might be divided into the three<br />
components of the inflow or sinus, the trabecular, and the<br />
outflow portions. Geva et al., 5 stated that the inflow region,<br />
compared with the other parts of the RV, had significant<br />
predominance in fiber shortening and contribution to the<br />
global RV systolic function. As the basal segment of the RV<br />
free wall is a part of the inflow component, and the apical<br />
segment refers to the trabecular portion of the RV, they<br />
suggested that the differences seen in their cohort might be<br />
related to the regional inhomogeneity of the RV in patients<br />
with DM.<br />
The Kosmala et al., study 4 reported RV diastolic<br />
dysfunction in a non-uniform type I and type II diabetic<br />
cohort using TDI and demonstrated significantly lower<br />
values of Em and Em-to-Am ratio in the basal and midsegments<br />
and longer isovolumic relaxation time (IRTm) in<br />
the mid-segment. Nonetheless, that study failed to show<br />
any difference in the E/A ratio, Em, and systolic parameters<br />
(Sm and TAPSE) between the diabetic patients and normal<br />
subjects. Furthermore, the said study found no significant<br />
correlations between the estimated echocardiographic<br />
parameters and indices of diabetic control (plasma glucose<br />
and HbA1c) as well as the duration of diabetes.<br />
In another study, Kosmala et al., 4 evaluated non-uniform<br />
type I and type II diabetic groups and showed impairment<br />
of the RV systolic function according to deformation studies<br />
(RV systolic stain and SRs in the basal and apical segments<br />
of the RV free wall) and impairment of the RV diastolic<br />
function (decreased SRe in both RV segments). In a study by<br />
Karamitsos et al., 6 type I diabetic patients were found to have<br />
an impaired RV diastolic function (trans-tricuspid E velocity,<br />
A velocity, E/A ratio, Em, and Am). Nevertheless, the RV<br />
systolic function was preserved in the authors’ diabetic<br />
population.<br />
Consistent with the findings of the present study, Gaber<br />
et al., 7 assessed patients with DM type II and demonstrated<br />
impairment of the RV systolic and diastolic functions<br />
according to deformation studies via three-dimensional<br />
echocardiography (systolic strain, SRs, and SRe in both RV<br />
basal and apical segments).<br />
The present study, in agreement with some other similar<br />
studies, 4, 8, 9 found no importance for the impact of the<br />
180
Obvious or Subclinical Right Ventricular Dysfunction in Diabetes Mellitus (Type II): ...<br />
<strong>TEHRAN</strong> <strong>HEART</strong> <strong>CENTER</strong><br />
duration of diabetes on the RV function. This finding could<br />
suggest that controlling diabetes mellitus is more important<br />
than its duration.<br />
Med J 2008;11:65-74.<br />
9. Rowland TW, Martha PM, Jr, Reiter EO, Cunningham LN. The<br />
influence diabetes mellitus on cardiovascular function in children<br />
and adolescents. Int J Sports Med 1992;13:431-435.<br />
Conclusion<br />
Whether the RV diastolic abnormalities have prognostic<br />
implications in the clinical course of patients with DM<br />
type II remains to be investigated. We believe that serial<br />
echocardiography measurements are warranted in this<br />
diabetic population if the progression from subclinical<br />
RV involvement to symptomatic RV dysfunction is to be<br />
followed. In addition, subclinical RV systolic and diastolic<br />
abnormalities should be considered when planning<br />
pharmacotherapy to prevent the development of symptomatic<br />
RV dysfunction.<br />
Acknowledgments<br />
This research project was supported by Rajaei<br />
Cardiovascular, Medical and Research Center. Special<br />
thanks are due to the above-mentioned hospital’s personnel<br />
and nurses who enrolled in our control group.<br />
References<br />
1. Kosmala W, Colonna P, Przewlocka-Kosmala M, Mazurek W.<br />
Right ventricular dysfunction in asymptomatic diabetic patients. J<br />
Diabetes Care 2004;27:2736-2738.<br />
2. Dounis V, Siegmund T, Hansen A, Jensen J, Schumm-Draeger PM,<br />
von Bibra H. Global myocardial perfusion and diastolic function<br />
are impaired to a similar extent in patients with type 2 diabetes<br />
mellitus and in patients with coronary artery disease-evaluation by<br />
contrast echocardiography and pulsed tissue Doppler. Diabetologia<br />
2006;49:2729-2740.<br />
3. Van den Brom CE, Bosmans JW, Vlasblom R, Handoko LM,<br />
Huisman MC, Lubberink M, Molthoff CF, Lammertsma AA,<br />
Ouwens MD, Diamant M, Boer C. Diabetic cardiomyopathy in<br />
Zucker diabetic fatty rats: the forgotten right ventricle. J Cardiovasc<br />
Diabetologia 2010;9:25-32.<br />
4. Kosmala W, Przewlocka-Kosmala M, Mazurek W. Subclinical<br />
right ventricular dysfunction in diabetes mellitus-an ultrasonic<br />
strain/strain rate study. Diabet Med 2007;24:656-663.<br />
5. Geva T, Powell AJ, Crawford EC, Chung T, Colan SD. Evaluation<br />
of regional differences in right ventricular systolic function by<br />
acoustic quantification by echocardiography and cine magnetic<br />
resonance imaging. Circulation 1998;98:339-345.<br />
6. Karamitsos TD, Karvounis HI, Dalamanga EG, Papadopoulos<br />
CE, Didangellos TP, Karamitsos DT, Parharidis GE, Louridas GE.<br />
Early diastolic impairment of diabetic heart: the significance of<br />
right ventricle. Int J Cardiol 2007;114:218-223.<br />
7. Gaber R, Kotb NA. Early diagnosis of right ventricular dysfunction<br />
in type II diabetes mellitus: value of 3 dimensional strain/strain<br />
rate. Heart mirror J 2010;4:80-85.<br />
8. Elshahed GS, Ahmed MI, El-Beblawy NS, Kamal HM, lsmaiel<br />
MF, Bin Zheidan OAS. Evaluation of right and left ventricular<br />
systolic and diastolic function in patients with type I diabetes using<br />
echocardiography and tissue Doppler imaging. Suez Canal Univ<br />
The Journal of Tehran University Heart Center181
The Journal of Tehran University Heart Center<br />
Case Report<br />
Surgical Treatment of Amplatzer Embolus in a Secundum<br />
Atrial Septal Defect Patient<br />
Ahmet Baris Durukan, MD 1* , Hasan Alper Gurbuz, MD 1 , Murat Tavlasoglu,<br />
MD 2 , Nevriye Salman, MD 1 , Halil Ibrahim Ucar, MD 1 , Cem Yorgancioglu,<br />
MD 1<br />
1<br />
Medicana International Ankara Hospital, Ankara, Turkey.<br />
2<br />
Diyarbakir Military Hospital, Diyarbakir, Turkey.<br />
Received 18 August 2011; Accepted 23 January 2012<br />
Abstract<br />
A secundum atrial septal defect is the most common congenital heart defect. Transcatheter treatment of secundum atrial<br />
septal defects is a popular and less invasive alternative to surgery. Procedural complications may occur in a wide spectrum,<br />
particularly device embolus as the most emergent one, but luckily they do not commonly occur in the clinical setting. Mortality<br />
from adverse events related to transcatheter treatment strategies is twentyfold higher than that of primary elective surgical<br />
closure. Here, we report an Amplatzer device embolus in a secundum atrial septal defect patient. The device was successfully<br />
removed with surgery, postoperative course was uneventful, and the patient was discharged from the hospital on the 5 th<br />
postoperative day.<br />
J Teh Univ Heart Ctr 2012;7(4):182-184<br />
This paper should be cited as: Durukan AB, Gurbuz HA, Tavlasoglu M, Salman N, Ucar HI, Yorgancioglu C. Surgical Treatment of<br />
Amplatzer Embolus in a Secundum Atrial Septal Defect Patient. J Teh Univ Heart Ctr 2012;7(4):182-184.<br />
Keywords: Heart septal defects, atrial • Septal occluder device • Surgical procedures, operative<br />
Introduction<br />
A secundum atrial septal defect (ASD) is the most<br />
common congenital heart defect, making up 10% of all<br />
congenital heart defects. Five to ten percent of children and<br />
30% of adults with congenital heart disease have the ostium<br />
secundum ASD. 1 ASD closure is indicated to prevent right<br />
ventricular volume overload due to left-to-right shunting<br />
over four years of age and to prevent arrhythmias and right<br />
heart failure in later decades. 2<br />
Transcatheter treatment of the secundum ASD is a popular<br />
and less invasive alternative to surgery. By 2008, 30000<br />
devices had been implanted. 2 Procedural complications<br />
do exist, luckily very rarely in the clinical setting. These<br />
complications increase morbidity and mortality rates<br />
compared to conventional surgical closure. 3<br />
Here, we report a case with the secundum ASD in which<br />
the atrial septal occluder device was embolized during the<br />
transcatheter procedure and was successfully treated with<br />
surgery.<br />
Case Report<br />
A 38-year-old, 160 cm tall, 65 kg woman was referred to<br />
our hospital with the diagnosis of the secundum ASD. She<br />
*<br />
Corresponding Author: Ahmet Baris Durukan, Medicana International Ankara Hospital, Umit Mahallesi 2463.sokak 4/18, 06810, Yenimahalle,<br />
Ankara, Turkey. Tel: +90 532 2273814. Fax: +90 312 2203170. E-mail: barisdurukan@yahoo.com.<br />
182
Surgical Treatment of Amplatzer Embolus in a Secundum Atrial Septal Defect Patient<br />
<strong>TEHRAN</strong> <strong>HEART</strong> <strong>CENTER</strong><br />
had initially referred to another hospital with the complaints<br />
of palpitation and shortness of breath. During cardiologic<br />
evaluation, echocardiography was performed and a secundum<br />
type ASD (pulmonary to systemic blood flow ratio [Qp/Qs]:<br />
2.0), first to second degree mitral regurgitation, and first<br />
to second degree tricuspid regurgitation were noted. There<br />
was a mild increase in the right ventricular dimensions.<br />
Pulmonary artery pressure was measured as 45 mm Hg. In<br />
our hospital, echocardiography was performed again and<br />
the anatomy was found suitable for the implantation of an<br />
ASD occluder device. During catheter closure, the occluder<br />
device was embolized. The patient was heparinized for<br />
systemic anticoagulation. It was not possible to retrieve<br />
the embolized device via catheterization procedures, and<br />
the patient was referred for emergency surgical removal.<br />
Surgical intervention was performed within forty-five<br />
minutes of embolization. The electrocardiogram was normal<br />
sinus rhythm. On chest X-ray, the ‘Amplatzer occluder<br />
Device’ was seen in the right pulmonary artery localization<br />
(Figure 1).<br />
was closed with a Teflon patch. Right pulmonary arteriotomy<br />
was performed proximal to the superior vena cava and the<br />
device was removed (Figures 2 and 3). Arteriotomy was<br />
closed primarily. The postoperative course was uneventful,<br />
and the patient was discharged on the 5 th postoperative day.<br />
Figure 2. Intraoperative image. The right pulmonary artery is opened and<br />
the septal occluder device (arrow) is being removed through the arteriotomy<br />
Figure 3. Removed "Amplatzer Occluder Device"<br />
Figure 1. Preoperative chest X-ray of the patient, performed following device<br />
embolization. The arrow points very clearly to the septal occluder device<br />
in the right pulmonary artery<br />
The patient underwent surgery under general anesthesia<br />
and with standard median sternotomy incision. There were<br />
pericardial adhesions. Once the pericardium had been<br />
opened, the ‘Amplatzer Occluder Device’ was easily palpated<br />
in the right pulmonary artery proximal to the superior vena<br />
cava. Cardiopulmonary bypass (CPB) under moderate<br />
hypothermia was established with aorto-bicaval cannulation<br />
(selective superior vena cava cannulation was performed).<br />
Myocardial management was provided by antegrade cold<br />
and terminal warm blood cardioplegia. Right atriotomy was<br />
performed. A 2.5 × 1.5 cm secundum type ASD was seen. It<br />
Discussion<br />
The approach has shifted from surgical closure to<br />
transcatheter procedures in the treatment of the secundum<br />
ASD, which is definitely a less invasive approach. Hospital<br />
stay is shorter with transcatheter treatment and cosmetic<br />
results are better. Return to work for adults and return to<br />
school for children are earlier than those with cardiac surgery.<br />
Developmental outcome has been reported to be better in<br />
cases treated with transcatheter procedures. Adverse events<br />
related with CPB are avoided. 4 Right ventricular functions<br />
are preserved better. 5 And most importantly, the incidence<br />
of minor or major complications is lower with transcatheter<br />
closure. 6<br />
Procedural complications like device malposition or<br />
embolization, atrial wall erosion, mitral regurgitation,<br />
The Journal of Tehran University Heart Center183
The Journal of Tehran University Heart Center<br />
Ahmet Baris Durukan et al.<br />
cardiac arrhythmia requiring treatment, sciatic nerve<br />
compression due to retroperitoneal hematoma, prolonged<br />
time for femoral vein hemostasis, access site hematoma,<br />
arteriovenous fistula formation, pericardial/pleural<br />
effusions, and transient ischemic attacks have been<br />
previously reported. 1, 2 Butera et al. 1 reported 0.7%<br />
malposition/embolization. Wilson et al. 2 reported device<br />
embolization in 2 out of 227 patients and one was again<br />
treated via the transcatheter route. Sarris et al. 7 reviewed<br />
data from 19 well-known European institutes; and in a 10-<br />
year period, 56 cases undergoing emergency surgery after<br />
catheter intervention were reported. Among the 56 cases,<br />
there were 22 embolization cases and 7 cases were due<br />
to the pulmonary artery. Surgical removal of the device,<br />
closure of the defect, and repair/replacement of the damaged<br />
cardiac structure were performed. Operative mortality was<br />
5.4%. Based on the EACTS reports, operative mortality<br />
for primary surgical ASD closure was 0.36% in the same<br />
time period. 7 Based on the FDA reports, in a 7-year period,<br />
mortality rates for transcatheter closure were similar to<br />
those of primary surgical closure (0.13%), but the mortality<br />
for the surgical management of a device adverse event<br />
(2.6%) was twentyfold higher than that for primary elective<br />
ASD closure. 3<br />
We managed to remove the device in a very short time, and<br />
the patient was discharged without any further complications.<br />
of the US Food and Drug Administration Manufacturer and User<br />
Facility Device Experience database for adverse events involving<br />
Amplatzer septal occluder devices and comparison with the<br />
Society of Thoracic Surgery congenital cardiac surgery database.<br />
J Thorac Cardiovasc Surg 2009;137:1334-1341.<br />
4. Visconti KJ, Bichell DP, Jonas RA, Newburger JW, Bellinger<br />
DC. Developmental outcome after surgical versus interventional<br />
closure of secundum atrial septal defect in children. Circulation<br />
1999;100:II145-150.<br />
5. Dhillon R, Josen M, Henein M, Redington A. Transcatheter closure<br />
of atrial septal defect preserves right ventricular function. Heart<br />
2002;87:461-465.<br />
6. Berger F, Vogel M, Alexi-Meskishvili V, Lange PE. Comparison of<br />
results and complications of surgical and Amplatzer device closure<br />
of atrial septal defects. J Thorac Cardiovasc Surg 1999;118:674-<br />
678.<br />
7. Sarris G, Kirvassilis G, Zavaropoulos P, Belli E, Berggren H, Carrel<br />
T, Comas JV, Corno AF, Daenen W, Di Carlo D, Ebels T, Fragat J,<br />
Hamilton L, Hraska V, Jacobs J, Lazarov S, Mavroudis C, Metras<br />
D, Rubay J, Schreiber C, Stellin G. Surgery for complications of<br />
transcatheter closure of atrial septal defects: a multi-institutional<br />
study from the European Congenital Heart Surgeons Association.<br />
Eur J Cardiothorac Surg 2010;37:1285-1290.<br />
Conclusion<br />
Transcatheter device closure of the ASD can lead to serious<br />
complications despite its advantages over surgical closure.<br />
But it should be kept in mind that even if most cases are<br />
successful, not only early, but also late complications may<br />
occur regardless of the size or type of the current devices.<br />
Surgical treatment of the complications may be mandatory<br />
and should be performed immediately, especially in cases<br />
of embolization. Surgery is quite effective in treatment,<br />
but it is a fact that operative mortality rises when surgery<br />
is performed for the treatment of complications. Operative<br />
mortality is much lower for primary surgical repair.<br />
References<br />
1. Butera G, Romagnoli E, Carminati M, Chessa M, Piazza L, Negura<br />
D, Giamberti A, Abella R, Pome G, Condoluci C, Frigiola A.<br />
Treatment of isolated secundum atrial septal defects: impact of age<br />
and defect morphology in 1,013 consecutive patients. Am Heart J<br />
2008;156:706-712.<br />
2. Wilson N, Smith J, Prommete B, O’Donnell C, Gentles TL,<br />
Ruygrok PN. Transcatheter closure of secundum atrial septal<br />
defects with the Amplatzer septal occluder in adults and childrenfollow-up<br />
closure rates, degree of mitral regurgitation and<br />
evolution of arrhythmias. Heart Lung Circ 2008;17:318-324.<br />
3. DiBardino DJ, McElhinney DB, Kaza AK, Mayer JE, Jr. Analysis<br />
184
<strong>TEHRAN</strong> <strong>HEART</strong> <strong>CENTER</strong><br />
Case Report<br />
Post-Traumatic Chordae Rupture of Tricuspid Valve<br />
Kyomars Abbasi, MD, Hossein Ahmadi, MD, Arezoo Zoroufian, MD,<br />
Mohammad Sahebjam, MD, Naghmeh Moshtaghi, MD, Seyed Hessamedin<br />
Abbasi, MD *<br />
Tehran Heart Center, Tehran University of Medical Sciences, Tehran, Iran.<br />
Received 26 October 2011; Accepted 07 January 2012<br />
Abstract<br />
Blunt injury to the chest can affect any one or all components of the chest wall and thoracic cavity. The clinical presentation<br />
of patients with blunt chest trauma varies widely and ranges from minor reports of pain to florid shock. Traumatic tricuspid<br />
valve regurgitation is a rare cardiovascular complication of blunt chest trauma. Tricuspid valve regurgitation is usually<br />
begotten by disorders that cause the right ventricle to enlarge. Diagnosis is made by physical examination findings and is<br />
confirmed by echocardiography. We report two cases of severe tricuspid regurgitation secondary to the rupture of the chordae<br />
tendineae of the anterior leaflet following non-penetrating chest trauma. Both patients had uneventful postoperative courses.<br />
J Teh Univ Heart Ctr 2012;7(4):185-187<br />
This paper should be cited as: Abbasi K, Ahmadi H, Zoroufian A, Sahebjam M, Moshtaghi N, Abbasi SH. Post-Traumatic Chordae<br />
Rupture of Tricuspid Valve. J Teh Univ Heart Ctr 2012;7(4):185-187.<br />
Keywords: Heart rapture • Tricuspid valve • Wounds and injuries<br />
Introduction<br />
Blunt thoracic trauma has become a regular occurrence<br />
courtesy of high-speed motor vehicle accidents, 1 especially<br />
in the last decade. 2 Such accidents are the principal cause of<br />
isolated tricuspid valve regurgitation (TR). 3 Traumatic TR<br />
is a rare cardiovascular complication of blunt chest trauma.<br />
The most frequently involved valve in blunt chest trauma is<br />
the aortic valve, followed by the mitral and tricuspid valves. 4<br />
Traumatic TR is usually well tolerated; 5 however, as far as<br />
treatment is concerned, the tricuspid valve replacement has<br />
been the conventional procedure, especially in cases with<br />
delayed presentation. 6 We herein report two cases of severe<br />
TR secondary to the rupture of the chordae tendineae of the<br />
anterior leaflet following non-penetrating chest trauma.<br />
Case Reports<br />
Case # 1<br />
A 28-year-old man was admitted to our hospital suffering<br />
from exertional dyspnea and palpitation. One year previously,<br />
he had sustained blunt chest trauma in a car accident, but<br />
no cardiac abnormality had been noticed at the time. His<br />
symptoms started about two months before his referral to us.<br />
At presentation, the patient had a blood pressure of 120/90<br />
mmHg and pulse of 70 beats/min. The electrocardiogram<br />
revealed sinus rhythm and right bundle branch block with<br />
left-axis deviation. Transthoracic echocardiography (TTE)<br />
demonstrated a normal left ventricle (LV) size, mild LV<br />
systolic dysfunction, septal motion abnormality due to the<br />
right ventricle (RV) volume overload, severe RV and right<br />
*<br />
Corresponding Author: Seyed-Hesameddin Abbasi, Tehran University of Medical Sciences, Tehran Heart Center, North Kargar Street, Tehran, Iran.<br />
1411713138. Tel: +98 21 88029720. Fax: +98 21 88029702. E-mail: abbasi@tehranheartcenter.org.<br />
The Journal of Tehran University Heart Center 185
The Journal of Tehran University Heart Center<br />
atrium (RA) enlargement, and finally, severe low pressure<br />
TR due to the flail anterior leaflet of the tricuspid valve.<br />
Transesophageal echocardiography (TEE) was conducted<br />
as a complementary study and confirmed the flail leaflet<br />
secondary to the ruptured chordae. The patient was, therefore,<br />
scheduled for tricuspid valve repair.<br />
The operation was performed through median sternotomy.<br />
Following the institution of cardiopulmonary bypass (CPB),<br />
the heart was arrested via cardioplegia and the RA was<br />
explored: there was chordae rupture of the anterior leaflet.<br />
The rupture was repaired by first constructing two near<br />
chordae with 5/0 Gortex suture and then placing edge-toedge<br />
stitches on the edge of the three leaflets. Additionally,<br />
ring annuloplasty using a Carpenter (31mm) was performed.<br />
Postoperative TEE demonstrated mild to moderate TR and<br />
no significant tricuspid valve stenosis (TS) (tricuspid valve<br />
mean gradient = 2.5 mm Hg). The patient’s postoperative<br />
course was uneventful.<br />
Case # 2<br />
A 53-year-old man was referred to our hospital because of<br />
exertional dyspnea. One year previously, he had sustained<br />
multiple traumas in a bus accident. The accident left him in<br />
a deep coma for 17 days, after which he suffered a stroke,<br />
right hemi-paresis, and aphasia due to infarction in the left<br />
temporal lobe. Also, he had fractures in the left femoral<br />
bone, left tibia bone, right hand, and two ribs on the superior<br />
right side. At the time, no cardiac symptoms were detected<br />
but the patient was subjected to splenectomy.<br />
On admission, the electrocardiogram showed sinus rhythm,<br />
right bundle branch block with left-axis deviation. TTE<br />
revealed a normal LV size with mildly reduced LV systolic<br />
function, abnormal septal motion due to the RV volume<br />
overload, severe RV and RA enlargement with mild RV<br />
systolic dysfunction, and flail anterior tricuspid valve leaflet<br />
with severe low pressure TR. In addition, a large, mobile<br />
filamentous mass was detected on the tip of the flail leaflet, in<br />
favor of ruptured chordae. These findings were all confirmed<br />
by preoperative TEE, which also demonstrated an aneurismal<br />
inter-atrial septum with a small secondary type of atrial septal<br />
defect (ASD). Cardiac catheterization showed a small left-toright<br />
shunt with no evidence of coronary artery disease.<br />
Intraoperatively, the chest was explored via median<br />
sternotomy. CPB was instituted, the heart was arrested by<br />
cardioplegia, and the RA was explored. The anterior papillary<br />
muscle was ruptured, resulting in the prolapse of the anterior<br />
tricuspid leaflet. The De Vega technique was applied to the<br />
tricuspid annulus. Pledgeted 4/0 Prolene suture was used for<br />
the reconstruction of the anterior tricuspid valve papillary<br />
muscle to scar tissue in the base of the papillary muscle.<br />
Linear repair was thereafter performed for the closure of<br />
the ASD. Saline test was carried out next and the result was<br />
Kyomars Abbasi et al.<br />
so optimal that it obviated the need for TEE. Postoperative<br />
TTE revealed mild RV enlargement with mild systolic<br />
dysfunction. Doppler and contras study showed mild TR and<br />
no residual shunt flow.<br />
The patient made an uneventful recovery. One year after<br />
surgery now, the patient is well and asymptomatic with<br />
trivial TR on echocardiography.<br />
Discussion<br />
Traumatic TR is a rare sequela in the wake of blunt thoracic<br />
trauma. The most likely cause is compression, decompression,<br />
or deceleration of the thorax. These mechanisms give rise to<br />
intraventricular pressure peaks, which in combination with a<br />
closed valve and the systolic pressure in the RV most often<br />
affect the chordae tendineae and the papillary muscles. 1<br />
TR frequently goes undiagnosed at blunt chest trauma<br />
because of its asymptomatic nature; sometimes several<br />
or even more than ten years elapse before a diagnosis is<br />
made. 7-10 Nevertheless, severe TR eventually leads to right<br />
ventricular dilatation and progressive right heart failure,<br />
even if it is associated with no pulmonary hypertension. 6 The<br />
clinical course of TR following blunt chest trauma varies<br />
largely. Little is known about the clinical course of isolated<br />
ruptured chordae tendineae. Indeed, the only detailed case to<br />
have been reported thus far is that by Kleikamp et al., whose<br />
patient developed TR due to ruptured chordae tendineae of<br />
the anterior leaflet seven years after a blunt chest trauma,<br />
which was surgically corrected. 1 It is deserving of note<br />
that the rupture of the chordae tendineae is believed to be<br />
the consequence of an acute increase in the RV pressure<br />
associated with a closed tricuspid valve. 11<br />
Conclusions<br />
The two cases presented herein demonstrate that the<br />
rupture of the chordae tendineae of the tricuspid valve could<br />
be another cause of TR following blunt chest trauma. This<br />
is, however, a condition that can be repaired surgically<br />
without the need for valve replacement. Advances in<br />
echocardiography have enabled earlier diagnosis and ergo<br />
more effective treatment.<br />
We recommend that physicians working at emergency<br />
departments be on the alert for this potential complication<br />
of non-penetrating chest trauma and subject all patients<br />
admitted to the emergency department due to blunt chest<br />
trauma to TTE or TEE for accurate diagnosis.<br />
References<br />
1. Kleikamp G, Schnepper U, Körtke H, Breymann T, Körfer R.<br />
186
Post-Traumatic Chordae Rupture of Tricuspid Valve<br />
<strong>TEHRAN</strong> <strong>HEART</strong> <strong>CENTER</strong><br />
Tricuspid valve regurgitation following blunt thoracic trauma.<br />
Chest 1992;102:1294-1296.<br />
2. Lin SJ, Chen CW, Chou CJ, Liu KT, Su HM, Lin TH, Voon WC,<br />
Lai WT, Sheu SH. Traumatic tricuspid insufficiency with chordae<br />
tendinae rupture: a case report and literature review. Kaohsiung J<br />
Med Sci 2006;22:626-629.<br />
3. Nelson M, Wells G. A case of traumatic tricuspid valve<br />
regurgitation caused by blunt chest trauma. J Am Soc Echocardiogr<br />
2007;20:198.e4-5.<br />
4. Colombo T, Russo C, Ciliberto GR, Lanfranconi M, Bruschi G,<br />
Agati S, Vitali E. Tricuspid regurgitation secondary to mitral valve<br />
disease: tricuspid annulus function as guide to tricuspid valve<br />
repair. Cardiovasc Surg 2001;9:369-377.<br />
5. Noera G, Sanguinetti M, Pensa P, Biagi B, Cremonesi A, Lodi R,<br />
Lessana A, Carbone C. Tricuspid valve incompetence caused by<br />
nonpenetrating thoracic trauma. Ann Thorac Surg 1991;51:320-<br />
322.<br />
6. Fujiwara K, Hisaoka T, Komai H, Nishimura Y, Yamamoto<br />
Sh, Okamura Y. Successful repair of traumatic tricuspid valve<br />
regurgitation. Jpn J Thorac Cardiovasc Surg 2005;53:259-262.<br />
7. Gayet C, Pierre B, Delahaye JP, Champsaur G, Andre-Fouet X,<br />
Rueff P. Traumatic tricuspid insufficiency. An underdiagnosed<br />
disease. Chest 1987;92:429-432.<br />
8. van Son JA, Danielson GK, Schaff HV, Miller FA, Jr. Traumatic<br />
tricuspid valve insufficiency. Experience in thirteen patients. J<br />
Thorac Cardiovasc Surg 1994;108:893-898.<br />
9. Holper K, Hahnel C, Augustin N, Meisner H. Operative correction<br />
of traumatic tricuspid insufficiency. Herz 1996;21:172-178.<br />
10. Maisano F, Lorusso R, Sandrelli L, Torracca L, Coletti G, La Canna<br />
G, Alfieri O. Valve repair for traumatic tricuspid regurgitation. Eur<br />
J Cardiothorac Surg 1996;10:867-873.<br />
11. dos Santos J, Jr, de Marchi CH, Bestetti RB, Corbucci HA,<br />
Pavarino PR. Ruptured chordae tendineae of the posterior leaflet of<br />
the tricuspid valve as a cause of tricuspid regurgitation following<br />
blunt chest trauma. Cardiovasc Pathol 2001;10:97-98.<br />
The Journal of Tehran University Heart Center187
The Journal of Tehran University Heart Center<br />
Case Report<br />
Late Diagnosis of Large Left Ventricular Pseudoaneurysm<br />
after Mitral Valve Replacement and Coronary Artery<br />
Bypass Surgery by Real-Time Three-Dimensional<br />
Echocardiography<br />
Mohammad Sahebjam, MD * , Abbas Salehiomran, MD, Neda Ghaffari-Marandi,<br />
MD, Azam Safir, MD<br />
Tehran Heart Center, Tehran University of Medical Sciences, Tehran, Iran.<br />
Abstract<br />
One of the most serious complications of mitral valve replacement is left ventricular rupture and pseudoaneurysm<br />
formation, which is rare but potentially lethal. We herein present a late type of post mitral valve replacement and coronary<br />
artery bypass surgery pseudoaneurysm in a 74-year-old female, who was admitted to our hospital with a recent history of<br />
exertional dyspnea. She had the above-mentioned operation 10 months before. The diagnosis was made via two-dimensional<br />
and real-time three-dimensional transthoracic echocardiography. The prosthetic mitral valve was removed, and the large<br />
orifice of the pseudoaneurysm was closed by surgery. At one year's follow-up, the patient was in good condition.<br />
J Teh Univ Heart Ctr 2012;7(4):188-190<br />
Received 17 August 2011; Accepted 04 February 2012<br />
This paper should be cited as: Sahebjam M, Salehiomran A, Ghaffari-Marandi N, Safir A. Late diagnosis of Large Left Ventricular<br />
Pseudoaneurysm after Mitral valve Replacement and Coronary Artery Bypass Surgery by Real-Time Three-Dimensional Echocardiography.<br />
J Teh Univ Heart Ctr 2012;7(4):188-190.<br />
Keywords: Echocardiography, three-dimensional • Mitral valve • Aneurysm, false<br />
Introduction<br />
One of the most serious complications of mitral valve<br />
replacement (MVR) is the left ventricular (LV) rupture and<br />
pseudoaneurysm formation, which is rare but potentially<br />
lethal. 1-4 According to the time of the LV rupture, it is<br />
classified into three categories: early; delayed; and late<br />
ruptures. Early types are those that happen in the operating<br />
room after cardiopulmonary bypass discontinuation,<br />
delayed types are events which occur several hours or days<br />
after surgery, and late ruptures are cases that happen days<br />
to years after MVR. 1, 2 Because of the high propensity of<br />
the pseudoaneurysm to enlargement and rupture, immediate<br />
surgical management is inevitable. 3-5 We report a case<br />
with a late diagnosis of the LV pseudoaneurysm following<br />
previous MVR and coronary artery bypass graft surgery<br />
(CABG), which was diagnosed via two-dimensional and<br />
real-time three-dimensional transthoracic echocardiography<br />
(RT 3D TTE).<br />
Case Report<br />
A 74-year-old female with a history of coronary artery<br />
*<br />
Corresponding Author: Mohammad Sahebjam, Assistant Professor of Cardiology, Echocardiography Department, Tehran Heart Center, Jalal Al<br />
Ahmad and North Kargar Intersection, Tehran, Iran. 1411713138. Tel: +98 21 88029600. Fax: +98 21 88029731. E-mail: msahebjam@yahoo.com.<br />
188
Late Diagnosis of Large Left Ventricular Pseudoaneurysm after Mitral Valve ...<br />
disease was admitted to our hospital with a history of<br />
exertional dyspnea (function class II) during recent<br />
months. She had a past history of CABG and MVR surgery<br />
approximately 10 months prior to her admission.<br />
The postoperative echocardiography, performed one<br />
week after surgery, showed mild LV hypertrophy with an<br />
ejection fraction of 50%, a prosthetic MV with an acceptable<br />
gradient, and a normal right ventricle size with a good<br />
systolic function.<br />
On present admission, the patient’s pulse rate was 90 per<br />
minute and regular, and her blood pressure was 130/70 mm<br />
Hg. The patient had 1+ edema in her lower limbs. Auscultation<br />
revealed fine crackles in both lung bases and III/VI systolic<br />
murmur. An electrocardiogram (ECG) showed left bundle<br />
branch block and inverted T wave in V5-V6 leads.<br />
TTE showed a large echolucent space with a narrow neck<br />
(about 1.8 - 2 cm in diameter) on the basal posterolateral portion<br />
of the LV (near the prosthetic MV) and the diameter of the<br />
cavity was about 70 mm, suggestive of a large pseudoaneurysm<br />
in the basal posterolateral portion of the LV with a to-and-fro<br />
flow on color Doppler (Figures 1 and 2). RT 3D TTE (Vivid 7<br />
/ GE / RT 3D probe) was performed in order to better reveal<br />
the spatial relations between the pseudoaneurysm and the<br />
adjacent cardiovascular and thoracic structures and to better<br />
delineate the pseudoaneurysm borders before surgery. RT 3D<br />
TTE showed a large pseudoaneurysm (80 × 52 mm), parallel<br />
to the free wall of the LV (Figure 3). Its orifice was about 20<br />
mm and was very close to the MV annulus.<br />
<strong>TEHRAN</strong> <strong>HEART</strong> <strong>CENTER</strong><br />
prosthetic MV was removed. In the posterolateral aspect of<br />
the LV just below the annulus of the MV, the large orifice<br />
of the pseudoaneurysm (about 20 mm in diameter) was<br />
found, which was closed with a pericardial patch (Figure<br />
4). After the closure of the defect, MVR with a bileaflet<br />
mechanical valve (St. Jude # 27) was performed and the<br />
patient was weaned from CPB without problems. Post-pump<br />
intraoperative transesophageal echocardiography confirmed<br />
the complete closure of the orifice of the pseudoaneurysm<br />
without a flow. The postoperative course was acceptable and<br />
the patient was discharged on 10 th postoperative day. TTE<br />
was performed before discharge and showed the prosthetic<br />
MV with an acceptable gradient, without paravalvular leak<br />
and a large echomixed cavity (7 × 3.8 cm) due to a previous<br />
pseudoaneurysm posterolateral to the LV, which was filled<br />
by a clot. At one year's follow-up, the patient was in good<br />
condition and was taking oral medications.<br />
Figure 2. Two-dimensional color Doppler echocardiography, showing<br />
a turbulent flow on the orifice of the pseudoaneurysm (arrow) and the<br />
pseudoaneurysm (asterisk)<br />
Figure 1. Two-dimensional echocardiography, showing the orifice of<br />
the pseudoaneurysm near the mitral valve sewing ring (arrow) and the<br />
pseudoaneurysm (asterisk)<br />
The patient underwent urgent surgery through median<br />
sternotomy using cardiopulmonary bypass. After mid<br />
sternotomy and moderate hypothermia (28 °C), the left<br />
atrium was opened. The prosthetic MV (St Jude # 27)<br />
remained intact, but the orifice of the LV pseudoaneurysm<br />
was unclear when visualized through the St Jude valve. The<br />
Figure 3. Three-dimensional echocardiography, showing the orifice of the<br />
pseudoaneurysm (arrow) and the pseudoaneurysm (asterisk)<br />
The Journal of Tehran University Heart Center189
The Journal of Tehran University Heart Center<br />
Mohammad Sahebjam et al.<br />
important for the operative approach plan.<br />
Conclusion<br />
The LV pseudoaneurysm is an important complication that<br />
may occur late after MVR and thus necessitates due heed on<br />
the part of cardiologists and cardiac surgeons.<br />
References<br />
Figure 4. The operation site. The black arrow points to the pseudoaneurysm<br />
orifice (PS) and the white arrow to the prosthetic mitral valve (MV)<br />
Discussion<br />
Rupture of the LV wall after MVR, albeit infrequent,<br />
is a fatal complication, especially in the delayed class. 4,<br />
6, 7<br />
The most frequent cause of the LV pseudoaneurysm is<br />
myocardial infarction secondary to atherosclerotic coronary<br />
artery disease, but many other causes may be responsible<br />
for the LV pseudoaneurysm such as trauma, infective<br />
endocarditis, inflammation, and cardiac surgery. 8 Congestive<br />
heart failure is the most common clinical presentation of the<br />
LV pseudoaneurysm but the rate of asymptomatic patients is<br />
more than 10%. 9 For the first time, Spellberg and O’Reilly<br />
reported post-MVR pseudoaneurysm, which was diagnosed<br />
via left ventriculography. 10 Two third of the LV ruptures are<br />
the early type, and the mortality rate of this category reaches<br />
near 50% despite early management. 10 Classification of<br />
the post-MVR pseudoaneurysm may be based on the time<br />
and location of the rupture. 1 Miller and co-workers also<br />
classified the LV pseudoaneurysm based on the location of<br />
the LV rupture and its relative location to the MV annulus. 10<br />
In patients with congestive heart failure symptoms, the<br />
mortality rate is high, particularly without surgery. One<br />
of the previous case series study reported 11 deaths in 35<br />
patients in non-operated cases with pseudoaneurysms. 9<br />
The initial technique for the diagnosis of postoperative<br />
complications is TTE. 1 Proper anatomic delineation is<br />
essential in order to plan appropriate therapy. Contrary<br />
to the post-myocardial infarction cases, these aneurysms<br />
following MVR tend to be sub-annular in location. 11<br />
Previously, pseudoaneurysm diagnosis was made by left<br />
ventriculography, while echocardiography and Cardiac<br />
Computed Tomography (CT) can be the other diagnostic<br />
approaches for these cases. 11<br />
The usage of RT 3D TTE in this case conferred better<br />
delineation of the pseudoaneurysm territory, which is<br />
1. Biyikoglu SF, Guray Y, Turkvatan A, Boyaci A, Katircioglu F.<br />
A serious complication late after mitral valve replacement: left<br />
ventricular rupture with pseudoaneurysm. J Am Soc Echocardiogr<br />
2008;21:1178.e1-3.<br />
2. Ono M, Wolf RK. Left ventricular pseudoaneurysm late after<br />
mitral valve replacement. Ann Thorac Surg 2002;73:1303-1305.<br />
3. Suda H, Ikeda K, Doi K, Shiraishi R, Furukawa K, Ito T. Successful<br />
repair of left ventricular pseudoaneurysm after mitral reoperation<br />
under hypothermic circulatory arrest. Jpn J Thorac Cardiovasc<br />
Surg 2003;51:18-20.<br />
4. Choi JB, Choi SH, Oh SK, Kim NH. Left ventricular<br />
pseudoaneurysm after coronary artery bypass and valve<br />
replacement for post-infarction mitral regurgitation. Tex Heart Inst<br />
J 2006;33:505-507.<br />
5. Nekkanti R, Nanda NC, Ansingkar KG, McGiffin DC.<br />
Transesophageal three-dimensional echocardiographic<br />
assessment of left ventricular pseudoaneurysm. Echocardiography<br />
2002;19:169-172.<br />
6. Kupari M, Verkkala K, Maamies T, Härtel G. Value of combined<br />
cross sectional and Doppler echocardiography in the detection of<br />
left ventricular pseudoaneurysm after mitral valve replacement. Br<br />
Heart J 1987;58:52-56.<br />
7. Honda K, Okamura Y, Nishiharu Y, Hayashi H. Patch repair<br />
of a giant left ventricular pseudoaneurysm after mitral valve<br />
replacement. Ann Thorac Surg 2011;91:1596-1597.<br />
8. Mahilmaran A, Nayar PG, Sheshadri M, Sudarsana G, Abraham<br />
KA. Left ventricular pseudoaneurysm caused by coronary spasm,<br />
myocardial infarction, and myocardial rupture. Tex Heart Inst J<br />
2002;29:122-125.<br />
9. Leitman M, Shmueli R, Stamler A, Krakover R, Hendler A,<br />
Vered Z. An unusual presentation of a large left ventricular<br />
pseudoaneurysm. Echocardiography 2006;23:403-404.<br />
10. Lanjewar C, Thakkar B, Kerkar P, Khandeparkar J. Submitral left<br />
ventricular Pseudoaneurysm after mitral valve replacement: early<br />
diagnosis and successful repair. Interact Cardiovasc Thorac Surg<br />
2007;6:505-507.<br />
11. Yeo TC, Malouf JF, Oh JK, Seward JB. Clinical profile and<br />
outcomein 52 patients with cardiac pseudoaneurysm. Ann Intern<br />
Med 1998;128:299-305.<br />
190
<strong>TEHRAN</strong> <strong>HEART</strong> <strong>CENTER</strong><br />
Letter to the Editor<br />
A Memorandum of "World<br />
Heart Day 2012": Myocardial<br />
Infarction Mortality in Women<br />
in Birjand, 2008-2009<br />
September 29th, 2012 is entitled "World Heart Day" and<br />
the theme of the current year is "One World, One Heart, One<br />
Home, and Focus on Women and Children".<br />
Cardiovascular diseases are the most common causes of<br />
mortality in women and men. 1 Various studies have probed<br />
into the differences in the clinical symptoms, risk factors,<br />
and prognoses between male and female patients with acute<br />
myocardial infarction (AMI). 2<br />
One study on AMI patients in Birjand, Iran (2008-2009)<br />
reported the following results:<br />
Out of 471 patients, 136 (28.9%) cases were women<br />
and 335 (71.1%) were men. The mean age of the females<br />
and males was 64.6 ± 13.6 years and 61.4 ± 13.95 years,<br />
respectively; p value = 0.001.The most prevalent cardiac risk<br />
factors in the women and men were hypertension (54.4%<br />
in women, 32.2% in men; p value < 0.001), dyslipidemia<br />
(30.1% in women, 18.5% in men; p value = 0.006), diabetes<br />
mellitus (18.4% in women, 14.9% in men; p value = 0.35),<br />
and smoking (3.7% in women, 22.7% in men; p value =<br />
0.04).<br />
Table 1 shows that the consumption of Aspirin and beta<br />
blockers was lower in the women than in the men, but<br />
there was no other difference between the two genders with<br />
respect to other treatments. In-hospital mortality was 11.5%:<br />
8.4% in the men and 19.1% in the women (p value = 0.001).<br />
One-month mortality was 12.9%; it was significantly higher<br />
in the women than in the men (22.1% in women, 9.2% in<br />
men; p value ≤ 0.001). Finally, in-hospital mortality and<br />
one-month mortality after AMI were significantly higher in<br />
the women.<br />
Factors such as old age, higher prevalence of diabetes<br />
mellitus and hypertension, delayed referral of women to<br />
physicians, and difference in clinical symptoms can be play<br />
a decisive role in this regard. 3 Indeed, women do not tend to<br />
deem cardiovascular diseases as their most fatal disease and<br />
thus fail to take their risk factors into consideration; that is<br />
why cardiovascular diseases are diagnosed later in women<br />
and are more acute. It is, therefore, necessary that educational<br />
programs be devised to raise women's knowledge about<br />
these fatal diseases.<br />
Table 1. Comparison of drug therapy in patient with acute myocardial<br />
infarction (AMI) according to sex<br />
Drug<br />
Female<br />
n (%)<br />
Male<br />
n (%)<br />
P value<br />
Beta-blocker 77 (56.6) 222 (66.3) 0.04<br />
ASA 107 (78.7) 302 (90.1) 0.01<br />
Statins 74 (54.4) 213 (63.6) 0.06<br />
ACE-I 40 (29.4) 105 (31.3) 0.68<br />
Streptokinase 12 (8.8) 46 (13.7) 0.14<br />
Clopidogrel 27 (19.9) 90 (26.9) 0.11<br />
Nitrate 104 (76.5) 280 (83.6) 0.07<br />
ASA, Acetylsalicylic acid; ACE-I, Angiotensin-converting enzyme<br />
inhibitors<br />
References<br />
1. Kazemi T, Sharifzadeh GR, Zarban A, Fesharakinia A, Rezvani<br />
MR, Moezy SA. Risk factors for premature myocardial infarction:<br />
a matched case-control study. J Res Health Sci 201;11:77-82.<br />
2. Abbasi SH, Kassaian SE. Women and coronary artery disease. Part<br />
I: basic considerations. J Teh Univ Heart Ctr 2011;6:109-116.<br />
3. Hosseini SK, Soleimani A, Karimi AA, Sadeghian S, Darabian S,<br />
Abbasi SH, Ahmadi SH, Zoroufian A, Mahmoodian M, Abbasi<br />
A. Clinical features, management and in-hospital outcome of ST<br />
elevation myocardial infarction (STEMI) in young adults under 40<br />
years of age. Monaldi Arch Chest Dis 2009;72:71-76.<br />
Toba Kazemi, MD<br />
Associate Professor of Cardiology,<br />
Birjand Atherosclerosis and Coronary Artery Research Center,<br />
Department of Cardiology,<br />
Birjand University of Medical Sciences (BUMS),<br />
Valiassr Hospital, Ghafari Avenue,<br />
Birjand, Iran.<br />
9717964151.<br />
Tel: +98 56 14443001-9.<br />
Fax: +98 56 14433004.<br />
E-mail: drtooba.kazemi@gmail.com.<br />
Gholam Reza Sharifzadeh, MSc<br />
Epidemiologist,<br />
Birjand University of Medical Sciences (BUMS),<br />
Pasdaran Avenue,<br />
Birjand, Iran.<br />
9717964151.<br />
Tel: +98 56 14443001-9.<br />
Fax: +98 56 14433004.<br />
E-mail: rezamood@yahoo.com.<br />
The Journal of Tehran University Heart Center191
The Journal of Tehran University Heart Center<br />
Photo Clinic<br />
Ball in Chest<br />
Mohammad Bagher Rahim, MD, Mohammad Hossein Mandegar, MD,<br />
Farideh Roshanali, MD *<br />
Shariati General Hospital, Tehran University of Medical Sciences, Tehran, Iran.<br />
A 50-year-old male underwent a check-up for an insurance company. Chest X-ray revealed a large ball-like lesion in the<br />
posterior mediastinum. The finding was confirmed by computed tomography (CT) scan (Figure 1). The patient was referred<br />
to our center, where he had a successful mass removal surgery (Figure 2). Pathology identified the mass as neurinoma.<br />
A<br />
B<br />
Figure 1. Chest X-ray (A) and computed tomography (CT)<br />
scan (B), revealing a large ball-like lesion in the chest (arrows)<br />
Figure 2. The removed mass<br />
J Teh Univ Heart Ctr 2012;7(4):192<br />
This paper should be cited as: Rahim MB, Mandegar MH, Roshanali F. Ball in Chest. J Teh Univ Heart Ctr 2012;7(4):192.<br />
Keywords: Mass chest X-Ray • Thorax • Neoplasms<br />
*<br />
Corresponding Author: Farideh Roshanali, Shriati Hospital, North Kargar Street, Tehran, Iran. Tel: +98 912 3093151. Fax: +98 21 88797353.<br />
E-mail: farideh_roshanali@yahoo.com.<br />
192
<strong>TEHRAN</strong> <strong>HEART</strong> <strong>CENTER</strong><br />
INTERNATIONAL CARDIOVASCULAR SURGERY<br />
MEETINGS CALENDER (2012)<br />
Congress Time - Location Address<br />
Intermediate Skills in Cardiac Surgery<br />
2nd Leadership Course for Cardiovascular and<br />
Thoracic Surgeons<br />
31st Annual Winter Meeting of the Association of<br />
Physician Assistants in Cardiovascular Surgery<br />
(APACVS)<br />
STS/AATS Tech-Con 2012<br />
48th Annual Meeting of The Society of Thoracic<br />
Surgeons<br />
STS 48th Annual Meeting: Late-Breaking Clinical<br />
Trial Abstract Presentations<br />
ESAO Winter School 2012 "New Emerging<br />
Technology In Organ Failure" - Artificial Organs vs.<br />
Transplantation<br />
SCMR 15th Annual Scientific Sessions<br />
15th Comprehensive Review & Update of<br />
Perioperative Echo<br />
10-11 January 2012<br />
Birmingham<br />
United Kingdom<br />
16-20 January 2012<br />
Windsor<br />
United Kingdom<br />
26-29 January 2012<br />
Ft. Lauderdale, FL<br />
United States<br />
28-29 January 2012<br />
Fort Lauderdale, FL<br />
United States<br />
28 January-01 February 2012<br />
Fort Lauderdale, FL<br />
United States<br />
28 January-01 February 2012<br />
Fort Lauderdale, FL<br />
United States<br />
02-04 February 2012<br />
Catania, Sicily<br />
Italy<br />
02-05 February 2012<br />
Orlando, FL<br />
United States<br />
06-11 February 2012<br />
San Diego, CA<br />
United States<br />
http://ubis.rcsed.ac.uk/courses/<br />
coursedetails.aspxdiaryId=923<br />
http://www.eacts.org<br />
http://www.apacvs.org/<br />
http://www.sts.org/education-meetings/<br />
sts-annual-meeting/sts/aats-techcon-2011<br />
http://www.sts.org/education-meetings/stsannual-meeting<br />
http://www.sts.org/education-meetings/<br />
sts-annual-meeting/abstract-submission<br />
http://www.esaowinterschool2012.it<br />
http://www.scmr.org/meetings.html<br />
http://www.scahq.org/sca3/events/2012/<br />
echo/<br />
The Journal of Tehran University Heart Center
The Journal of Tehran University Heart Center<br />
Congress Time - Location Address<br />
1st IACTS-EACTS Joint Worksop<br />
The 22nd Annual Scientific Meeting SSRCTS<br />
58th Annual Meeting of Indian Association of<br />
Cardiovascular & Thoracic Surgeons (IACTS)<br />
41th Annual Meeting of the German Society for<br />
Thoracic - Cardiovascular Surgery GSTCVS<br />
ESTS School of Thoracic Surgery (Practical Course<br />
in the Laboratory)<br />
Course of Minimal Invasive Techniques in Adult<br />
Cardiac Surgery<br />
12th Annual International Symposium on Congenital<br />
Heart Disease<br />
The 32nd Annual Cardiothoracic Surgery<br />
Symposium (CREF 2012)<br />
8th International Congress of Update In Cardiology<br />
And Cardiovascular Surgery<br />
30th Cardiovascular Surgical Symposium<br />
Re-Evolution Summit III: Minimally Invasive<br />
Cardiac Surgery (MICS) and Hybrid Strategies<br />
Mitral Conclave Course: AATS Postgraduate Course<br />
17th Annual Update on Cardiopulmonary Bypass<br />
ESTS School of Thoracic Surgery (Theoretical<br />
Course)<br />
Florida Valve 2012 "Cardiovascular Practice<br />
Transformation"<br />
Houston Aortic Symposium: Frontiers in<br />
Cardiovascular Diseases, The Fifth in the Series<br />
08-09 February 2012<br />
Kolkata, West Bengal<br />
India<br />
09-11 February 2012<br />
Geilo<br />
Norway<br />
10-12 February 2012<br />
Kolkata, West Bengal<br />
India<br />
12-15 February 2012<br />
Freiburg<br />
Germany<br />
13-14 February 2012<br />
Paris<br />
France<br />
13-15 February 2012<br />
Nieuwegein<br />
Netherlands<br />
18-21 February 2012<br />
St. Petersburg, FL<br />
United States<br />
29 February-04 March 2012<br />
San Diego, CA<br />
United States<br />
01-04 March 2012<br />
Antalya<br />
Turkey<br />
03-10 March 2012<br />
Zuers/Arlberg<br />
Austria<br />
08-10 March 2012<br />
Houston, TX<br />
United States<br />
09-11 March 2012<br />
Bali<br />
Indonesia<br />
11-16 March 2012<br />
Snowmass Village, CO<br />
United States<br />
14-18 March 2012<br />
Antalya<br />
Turkey<br />
21-23 March 2012<br />
Orlando, FL<br />
United States<br />
22-24 March 2012<br />
Houston, TX<br />
United States<br />
http://www.iacts2012.com<br />
http://www.ssrcts.org/<br />
http://www.iacts2012.com<br />
http://www.dgthg-jahrestagung.de/en<br />
http://www.estsschool.org<br />
http://www.eacts.org<br />
http://www.allkids.org/conferences<br />
http://www.amainc.com/cref_<br />
cardiothoracic.html<br />
http://www.uccs2012.org<br />
http://www.surgery-zurs.at<br />
http://www.methodisthealth.com/basic.<br />
cfmid=37173<br />
http://www.ascvtsbali2012.org/program.<br />
html<br />
http://www.scahq.org/sca3/events/2012/<br />
cpb/<br />
http://www.estsschool.org<br />
http://www.floridavalvesymposium.com<br />
http://www.promedicacme.com/meeting/<br />
Houston-Aortic-Symposium-Frontiersin-73.html
<strong>TEHRAN</strong> <strong>HEART</strong> <strong>CENTER</strong><br />
Congress Time - Location Address<br />
AmSECT's 50th International Conference Meeting<br />
The 10th Annual International Nuss Pectus<br />
Excavatum and Carinatum Lecture Series<br />
Minimally Invasive Robotic Association (MIRA):<br />
7th International Congress<br />
Valves in the Heart of the Big Apple VII:<br />
Evaluation & Management of Valvular Heart<br />
Disease 2012<br />
34th International Symposium CX Charing Cross<br />
Controversies Challenge Consensus - Vascular &<br />
Endovascular Controviersies Update<br />
Association of Cardiothoracic Anesthetists & Society for<br />
Cardiothoracic Surgery in Great Britain and Ireland -<br />
2012 Annual Meeting and Cardiothoracic Forum<br />
Arteriosclerosis, Thrombosis and Vascular Biology<br />
(ATVB) 2012 Scientific Sessions<br />
32nd Annual Meeting & Scientific Sessions of<br />
The International Society of Heart and Lung<br />
Transplantation (ISHLT)<br />
SNM's 3rd Multimodality Cardiovascular Molecular<br />
Imaging Symposium<br />
61st Annual Meeting of the European Society for<br />
Cardiovascular Surgery (ESCVS)<br />
Aortic Symposium 2012<br />
Annual Thoracic Anesthesia Symposium<br />
34th Annual Meeting of the Society of Cardiovascular<br />
Anesthesiologists & Workshops<br />
92nd Annual Meeting - American Association for<br />
Thoracic Surgery<br />
5th Biennial Meeting on Heart Valve Biology and<br />
Tissue Engineering<br />
International Society for Minimally Invasive Cardiac<br />
Surgery 2012 ISMICS Annual Meeting<br />
28-31 March 2012<br />
Orlando, Florida<br />
United States<br />
29-30 March 2012<br />
Norfolk, VA<br />
United States<br />
11-13 April 2012<br />
Baltimore, MD<br />
United States<br />
12-14 April 2012<br />
New York City, NY<br />
United States<br />
14-17 April 2012<br />
London<br />
United Kingdom<br />
18-20 April 2012<br />
Manchester<br />
United Kingdom<br />
18-20 April 2012<br />
Chicago, IL<br />
United States<br />
18-21April 2012<br />
Prague<br />
Czech Republic<br />
19-21 April 2012,<br />
Bethesda, Maryland<br />
United States<br />
25-28 April 2012<br />
Dubrovnik<br />
Croatia<br />
26-27 April 2012<br />
New York, NY<br />
United States<br />
27-28 April 2012<br />
Boston, MA<br />
United States<br />
28 April-02 May 2012<br />
Boston, MA<br />
United States<br />
28 April-02 May 2012<br />
San Francisco, CA<br />
United States<br />
18-20 May 2012<br />
Mykonos<br />
Greece<br />
30 May-02 June 2012<br />
Los Angeles, CA<br />
United States<br />
http://amsect.societyhq.com/meetings/<br />
international/2012/abstracts/<br />
http://www.chkd.org/pectus<br />
http://www.mirasurgery.org/events.php<br />
http://www.heartvalveconference.com/<br />
http://www.cxvascular.com/<br />
cxsymposium<br />
http://www.scts.org/<br />
http://my.americanheart.org/professional/<br />
Sessions/ATVB/ATVB_UCM_316902_<br />
SubHomePage.jsp<br />
http://www.ishlt.org/meetings/<br />
annualMeeting.asp<br />
www.snm.org/cvmi2012<br />
http://www.escvs.com<br />
http://www.aats.org/aortic/<br />
http://www.scahq.org/sca3/events/2012/<br />
thoracic/<br />
http://www.scahq.org/sca3/events/2012/<br />
annual/<br />
http://www.aats.org/annualmeeting<br />
http://greeceheartvalve.com/home.asp<br />
http://www.ismics.org/<br />
The Journal of Tehran University Heart Center
The Journal of Tehran University Heart Center<br />
Congress Time - Location Address<br />
47th Congress of the European Society for Surgical<br />
Research ESSR 2012<br />
6th Congress of the Asian Society of Cardiovascular<br />
Imaging (ASCI)<br />
22nd congress of the world society of cardiothoracic<br />
surgeons<br />
20th European Conference on General Thoracic<br />
Surgery<br />
8th International Conference Pediatric Mechanical<br />
Circulatory Support Systems and Pediatric<br />
Cardiopulmonary Perfusion<br />
American Society of Arificial Internal Organs -<br />
ASAIO 58th Annual Conference<br />
6th Annual The New Orleans Conference: Practices<br />
in Cardiac Surgery and Extracorporeal Technologies<br />
The 3rd Beijing International Symposium and<br />
Workshop on Robotic Cardiac Surgery (BISROCS<br />
2012)<br />
4th Joint Conference of Scandinavian Association<br />
for Thoracic Surgery<br />
Georgia Health Sciences University Cardiac<br />
Conference<br />
ESTS School of Thoracic Surgery (Practical Course<br />
in the Laboratory)<br />
26th EACTS Annual Meeting<br />
National Meeting of Turkish Society of<br />
Cardiovascular Surgery<br />
Second International Joint Meeting on Thoracic<br />
Surgery, Barcelona 2012<br />
06-09 June 2012<br />
Lille<br />
France<br />
07-09 June 2012<br />
Bangkok<br />
Thailand<br />
09-13 June 2012<br />
Vancouver<br />
Canada<br />
10-13 June 2012<br />
Essen<br />
Germany<br />
13-16 June 2012<br />
Istanbul<br />
Turkey<br />
14-16 June 2012<br />
San Francisco, CA<br />
United States<br />
27-30 June 2012<br />
New Orleans, LA<br />
United States<br />
14-16 July 2012<br />
Beijing<br />
China<br />
16-18 August 2012<br />
Vilnius<br />
Lithuania<br />
21-23 September 2012<br />
Braselton, GA<br />
United States<br />
24-25 September 2012<br />
Paris<br />
France<br />
27-31 October 2012<br />
Barcelona<br />
Spain<br />
8-11 November 2012<br />
Antalya<br />
Turkey<br />
14-16 November 2012<br />
Barcelona<br />
Spain<br />
http://www.essr2012.com/<br />
http://www.asci2012.org<br />
www.wscts.org<br />
www.ests.org<br />
http://pennstatehershey.org/web/pedscpb/<br />
home<br />
http://www.asaio.com<br />
http://www.TheNewOrleansConference.<br />
com<br />
http://www.roboticsurg301.net<br />
http://www.scandinavian-ats.org/<br />
http://www.<br />
georgiahealthcardiacconference.com/<br />
http://www.estsschool.org<br />
http://www.eacts.org<br />
http://www.tkdcd.org<br />
http://thoracicsurgery2012.org/
<strong>TEHRAN</strong> <strong>HEART</strong> <strong>CENTER</strong><br />
INTERNATIONAL CARDIOVASCULAR MEETING<br />
AND CONGRESSES CALENDER (2012)<br />
Title Location Start Date End Date<br />
3rd Asia PCR/ SingLive 2012<br />
Singapore<br />
Republic of Singapore<br />
12 January 2012<br />
14 January 2012<br />
ISET 2012: International Symposium on Endovascular<br />
Therapy<br />
Miami Beach, Florida<br />
United States<br />
15 January 2012<br />
19 January 2012<br />
44th Ten-Day International Teaching Seminar on<br />
Cardiovascular Disease Epidemiology and Prevention<br />
Cape Town<br />
South Africa<br />
15 January 2012<br />
27 January 2012<br />
Ninth Gulf Heart Association Conference<br />
Muscat<br />
Oman<br />
18 January 2012<br />
21 January 2012<br />
22nd Annual Echo Hawaii 2012<br />
Big Island, HI<br />
United States<br />
23 January 2012<br />
27 January 2012<br />
6th Middle East Cardiovascular Congress & IVth<br />
International Congress of Cardiovascular Imaging<br />
Dubai<br />
UAE<br />
24 January 2012<br />
27 January 2012<br />
33rd Annual Seminar of The American Academy of<br />
Cardiovascular Perfusion<br />
New Orleans, Louisiana<br />
United States<br />
26 January 2012<br />
29 January 2012<br />
19th Annual Arrhythmias & the Heart: A Cardiovascular<br />
Update<br />
Kauai<br />
Hawaii<br />
30 January 2012<br />
03 February 2012<br />
31st Annual Scientific Meeting of the Belgian Society of<br />
Cardiology<br />
Brussels<br />
Belgium<br />
02 February 2012<br />
03 February 2012<br />
International Congress on Personalized Medicine: Up<br />
Close and Personalized (UPCP 2012)<br />
Florence<br />
Italy<br />
02 February 2012<br />
05 February 2012<br />
APCHF 2012<br />
6th Asian Pacific Congress of Heart Failure<br />
Chiang Mai<br />
Thailand<br />
03 February 2012<br />
05 February 2012<br />
Cardiovascular Research Technologies (CRT) 2012<br />
Washington DC<br />
United States<br />
04 February 2012<br />
07 February 2012<br />
The Journal of Tehran University Heart Center
The Journal of Tehran University Heart Center<br />
Title Location Start Date End Date<br />
Vascular Care 2012: New Technologies and Emerging<br />
Therapies<br />
Truckee, CA<br />
United States<br />
05 February 2012<br />
08 February 2012<br />
37th Annual Cardiovascular Conference at Snowbird<br />
Snowbird, UT<br />
United States<br />
05 February 2012<br />
08 February 2012<br />
Gulf Heart Association & Saudi Heart Association Annual<br />
Conference<br />
Riyadh<br />
Saudi Arabia<br />
06 February 2012<br />
09 February 2012<br />
10th International Kawasaki Disease Symposium<br />
Kyoto<br />
Japan<br />
07 February 2012<br />
10 February 2012<br />
13th International Forum for the Evaluation of<br />
Cardiovascular Care<br />
Nice<br />
France<br />
09 February 2012<br />
11 February 2012<br />
Icon 2012- International Congress for Endovascular<br />
Specialists<br />
Scottsdale, Arizona<br />
United States<br />
12 February 2012<br />
16 February 2012<br />
12th Annual International Symposium on Congenital Heart<br />
Disease (CHD)<br />
Florida<br />
United States<br />
18 February 2012<br />
18 February 2012<br />
11th Genoa Meeting on Hypertension, Diabetes and Renal<br />
Disease<br />
Genoa<br />
Italy<br />
23 February 2012<br />
25 February 2012<br />
2nd Annual Case Based Approach to Controversies in<br />
Cardiovascular Disease<br />
Dubai<br />
UAE<br />
23 February 2012<br />
25 February 2012<br />
Cardiovascular Disease Prevention 2012: Tenth Annual<br />
Comprehensive Symposium<br />
Miami Beach, Florida<br />
United States<br />
23 February 2012<br />
26 February 2012<br />
17th Annual Cardiology at Cancun: Topics in Clinical<br />
Cardiology: Focus on Heart Failure<br />
Cancun<br />
Mexico<br />
27 February 2012<br />
02 March 2012<br />
NCVH Latin America<br />
An International Approach to Lower Limb Interventions<br />
San Jose<br />
Costa Rica<br />
28 February 2012<br />
01 March 2012<br />
The Future of Genomic Medicine V<br />
La Jolla, California<br />
United States<br />
01 March 2012<br />
02 March 2012<br />
International Conference on Heart & Brain<br />
Paris<br />
France<br />
01 March 2012<br />
03 March 2012<br />
8th International Congress of Update in Cardiology and<br />
Cardiovascular Surgery<br />
Antalya<br />
Turkey<br />
01 March 2012<br />
04 March 2012<br />
2012 Hypertension Congress<br />
Cape Town<br />
South Africa<br />
03 March 2012<br />
05 March 2012<br />
Interventional Cardiology 2012: 27th Annual International<br />
Symposium<br />
Snowmass Village, CO<br />
United States<br />
04 March 2012<br />
09 March 2012<br />
10th National Congress of the Italian Society for<br />
Cardiovascular Prevention SIPREC<br />
Napoli<br />
Italy<br />
08 March 2012<br />
10 March 2012<br />
9th Mediterranean Meeting on Hypertension and<br />
Atherosclerosis<br />
Antalya<br />
Turkey<br />
14 March 2012<br />
18 March 2012<br />
12th Annual Spring Meeting on Cardiovascular Nursing<br />
Copenhagen<br />
Denmark<br />
16 March 2012<br />
17 March 2012<br />
76th Annual Scientific Meeting of the Japanese Circulation<br />
Society<br />
Fukuoka<br />
Japan<br />
16 March 2012<br />
18 March 2012<br />
The Houston Aortic Symposium - Frontiers in Cardiovascular<br />
Diseases: The Fifth in the Series<br />
Houston, TX<br />
United States<br />
22 March 2012<br />
24 March 2012
<strong>TEHRAN</strong> <strong>HEART</strong> <strong>CENTER</strong><br />
Title Location Start Date End Date<br />
61st Annual American College of Cardiology Scientific<br />
Sessions<br />
Chicago<br />
United States<br />
24 March 2012<br />
27 March 2012<br />
Frontiers in CardioVascular Biology 2012<br />
London<br />
United Kingdom<br />
30 March 2012<br />
01 April 2012<br />
Cardiology in the Young 2012<br />
London<br />
United Kingdom<br />
02 April 2012<br />
04 April 2012<br />
German Society of Cardiology 78th Annual Meeting 2012<br />
(DGK 2012)<br />
Manheim<br />
Germany<br />
11 April 2012<br />
14 April 2012<br />
34th Charing Cross International Symposium<br />
London<br />
United Kingdom<br />
14 April 2012<br />
17 April 2012<br />
Arteriosclerosis, Thrombosis and Vascular Biology 2012<br />
Scientific Sessions<br />
Chicago, IL<br />
United States<br />
18 April 2012<br />
20 April 2012<br />
World Congress of Cardiology Scientific Sessions<br />
Dubai<br />
UAE<br />
18 April 2012<br />
21 April 2012<br />
18th Annual Interventional Cardiology Fellows Course<br />
Miami, FL<br />
United States<br />
19 April 2012<br />
22 April 2012<br />
7th Clinical Update on Cardiac MRI & CT<br />
Cannes<br />
France<br />
20 April 2012<br />
22 April 2012<br />
Portuguese Society of Cardiology 33rd Congress 2012 (SPC<br />
2012)<br />
Vilamoura<br />
Portugal<br />
22 April 2012<br />
24 April 2012<br />
Angioplasty Summit Transcatheter Cardiovascular<br />
Therapeutics Asia Pacific 2012<br />
Seoul<br />
Korea<br />
25 April 2012<br />
27 April 2012<br />
22nd European Meeting On Hypertension and<br />
Cardiovascular Protection<br />
London<br />
United Kingdom<br />
26 April 2012<br />
29 April 2012<br />
Concepts in Contemporary Cardiovascular Medicine 2012<br />
Houston, TX<br />
United States<br />
01 May 2012<br />
04 May 2012<br />
EuroPRevent 2012<br />
Dublin<br />
Ireland<br />
03 May 2012<br />
05 May 2012<br />
APSC Intervention and Imaging 2012 Subspecialty Congress<br />
Taipei<br />
Taiwan<br />
04 May 2012<br />
06 May 2012<br />
Taiwan Society of Cardiology<br />
Annual Convention & Scientific Sessions<br />
Taipei<br />
Taiwan<br />
05 May 2012<br />
06 May 2012<br />
Quality of Care and Outcomes Research in Cardiovascular<br />
Disease and Stroke 2012 Scientific Sessions<br />
Atlanta, GA<br />
United States<br />
9 May 2012<br />
9 May 2012<br />
SCAI 2012 Scientific Sessions<br />
Las Vegas<br />
United States<br />
09 May 2012<br />
12 May 2012<br />
Heart Rythm 2012<br />
Boston<br />
United States<br />
09 May 2012<br />
12 May 2012<br />
EuroPCR 2012<br />
Paris<br />
France<br />
15 May 2012<br />
18 May 2012<br />
Metabolic Syndrome, Type II Diabetes and Atherosclerosis<br />
Marrakesh<br />
Morocco<br />
16 May 2012<br />
20 May 2012<br />
2nd International Congress on Cardiac Problems in<br />
Pregnancy (CPP 2012)<br />
Berlin<br />
Germany<br />
17 May 2012<br />
20 May 2012<br />
The Journal of Tehran University Heart Center
The Journal of Tehran University Heart Center<br />
Title Location Start Date End Date<br />
Heart Failure Congress 2012<br />
Belgrade<br />
Serbia<br />
19 May 2012<br />
22 May 2012<br />
EAS 2012, the 80th European Atherosclerosis Society<br />
Congress<br />
Milan<br />
Italy<br />
25 May 2012<br />
28 May 2012<br />
New Cardiovascular Horizons 13th Annual Conference<br />
New Orleans<br />
United States<br />
06 June 2012<br />
09 June 2012<br />
6th Congress of the Asian Society of Cardiovascular<br />
Imaging<br />
Bangkok<br />
Thailand<br />
07 June 2012<br />
09 June 2012<br />
15th Annual 2011 Live Symposium of Complex Coronary<br />
and Vascular Cases<br />
C3 Complex Cardiovascular Catheter Therapeutics-<br />
Advanced Endovascular and Coronary Intervention<br />
Global Summit 2012<br />
New York, NY<br />
United States<br />
Orlando, FL<br />
United States<br />
13 June 2012<br />
19 June 2012<br />
16 June 2012<br />
23 June 2012<br />
The iCi 2012 - imaging in cardiovascular interventions<br />
Frankfurt<br />
Germany<br />
27 June 2012<br />
27 June 2012<br />
CSI 2012- European congress on congenital and structural<br />
interventions<br />
Frankfurt<br />
Germany<br />
28 June 2012<br />
30 June 2012<br />
The 9th Tunisian European Days of cardiology practice<br />
Hammam Sousse<br />
Tunisia<br />
28 June 2012<br />
30 June 2012<br />
25th World Congress of the International Union of<br />
Angiology<br />
Prague<br />
Czech Republic<br />
01 July 2012<br />
05 July 2012<br />
15th Annual Cardiothoracic Update and TEE Board<br />
Review<br />
South Carolina<br />
United States<br />
05 July 2012<br />
08 July 2012<br />
International Society for the Study of Hypertension in<br />
Pregnancy 18th World Congress 2012 (ISSHP 2012)<br />
Geneva<br />
Switzerland<br />
09 July 2012<br />
12 July 2012<br />
19th ASEAN Federation of Cardiology Congress 2012<br />
Singapore<br />
Republic of Singapore<br />
13 July 2012<br />
15 July 2012<br />
Basic Cardiovascular Sciences 2012 Scientific Sessions<br />
New Orleans, LA<br />
United States<br />
23 July 2012<br />
26 July 2012<br />
Ten-Day Seminar on the Epidemiology and Prevention<br />
of Cardiovascular Disease<br />
Tahoe City, CA<br />
United States<br />
22 July 2012<br />
03 August 2012<br />
6th Annual Australian and New Zealand Endovascular<br />
Therapies Meeting 2012 (Anzet 2012)<br />
Brisbane<br />
Australia<br />
15 August 2012<br />
16 August 2012<br />
60th Annual Scientific Meeting of the Cardiac Society of<br />
Australia and New Zealand (CSANZ 2012)<br />
Brisbane<br />
Australia<br />
16 August 2012<br />
19 August 2012<br />
European Society of Cardiology Congress 2012<br />
Munich<br />
Germany<br />
25 August 2012<br />
29 August 2012<br />
CIRSE 2012 /Cardiovascular and Interventional<br />
Radiological Society of Europe<br />
Lisbon<br />
Portugal<br />
15 September 2012<br />
19 September 2012<br />
High Blood Pressure Research 2012 Scientific Sessions<br />
Washington DC<br />
United States<br />
19 September 2012<br />
22 September 2012<br />
Hypertension Sydney 2012<br />
Sydney<br />
Australia<br />
29 September 2012<br />
04 October 2012<br />
28th Annual Echocardiography in Pediatric and Adult<br />
Congenital Heart Disease<br />
Rochester, MN<br />
United States<br />
07 October 2012<br />
10 October 2012
<strong>TEHRAN</strong> <strong>HEART</strong> <strong>CENTER</strong><br />
Information for Authors<br />
The first three consecutive issues of "The Journal of Tehran University Heart Center" were published under the title of<br />
"The Journal of Tehran Heart Center" with ISSN: 1735-5370. From the fourth issue onward, however, the journal has been<br />
entitled ‘’The Journal of Tehran University Heart Center" with ISSN:1735-8620.<br />
Scope of the journal<br />
"The Journal of Tehran University Heart Center" aims to publish the highest quality material, both clinical and scientific,<br />
on all aspects of Cardiovascular Medicine. It includes articles related to research findings, technical evaluations, and reviews.<br />
In addition, it provides a forum for the exchange of information on all aspects of Cardiovascular Medicine, including<br />
educational issues. "The journal of Tehran University Heart Center" is an international, English language, peer reviewed<br />
journal concerned with Cardiovascular Medicine. It is an official journal of the Cardiovascular Research Center of the Tehran<br />
University of Medical Sciences (in collaboration with the Iranian Society of Cardiac Surgeons) and is published quarterly.<br />
Papers submitted to this journal which do not adhere to the Instructions for Authors will be returned for appropriate revision<br />
to be in line with the Instructions for Authors. They may then be resubmitted. Submission of an article implies that the work<br />
described has not been published previously (except in the form of an abstract or as part of a published lecture or academic<br />
thesis), that it is not under consideration for publication elsewhere, that its publication is approved by all Authors and tacitly<br />
or explicitly by the responsible authorities where the work was carried out, and that, if accepted, it will not be published<br />
elsewhere in the same form, in English or in any other language, without the written consent of the publisher.<br />
Article Categories<br />
The Journal of Tehran University Heart Center” accepts the following categories of articles:”<br />
Guest Editorial<br />
Original Article<br />
Clinical and pre-clinical papers based on either normal subjects or patients and the result of cardiovascular pre-clinical<br />
research will be Considered for publication provided they have an obvious clinical relevance.<br />
Brief communication<br />
Case report<br />
Review Article<br />
"The Journal of Tehran University Heart Center" publishes a limited number of scholarly, comprehensive reviews whose<br />
aims are to summarize and critically evaluate research in the field addressed and identify future implications. Reviews should<br />
not exceed 5000 words.<br />
Letter to editor<br />
Letters to the editor must not exceed 500 words and should focus on a specific article published in "The Journal of<br />
Tehran University Heart Center" within the preceding 12 weeks. No original data may be included. Authors will receive prepublication<br />
proofs, and the authors of the article cited invited to reply.<br />
Submission of manuscripts<br />
Four double spaced copies on 8 1/2 × 11 in. paper should be sent to:<br />
Dr. A. Karimi,<br />
Editor in Chief,<br />
"The Journal of Tehran University Heart Center",<br />
Tehran Heart Center,<br />
North Kargar Street,<br />
The Journal of Tehran University Heart Center
The Journal of Tehran University Heart Center<br />
Tehran, Iran.<br />
1411713138.<br />
Photocopies or good reproductions of illustrations are acceptable only on the spare copies. Included also should be a set<br />
of the electronic files of the manuscript on floppy - disk or CD-ROM. For preparation of electronic files, see the instructions<br />
herein below.<br />
Also, manuscripts can be submitted electronically via the journal’s website: http://jthc.tums.ac.ir. On-line submission<br />
allows the manuscript to be handled in electronic forms throughout the review process.<br />
Review of manuscripts<br />
All manuscripts correctly submitted to will first be reviewed by the Editors. Some manuscripts will be returned to authors<br />
at this stage if the paper is deemed inappropriate for publication in “The Journal of Tehran University Heart Center”, if the<br />
paper does not meet submission requirements, or if the paper is not deemed to have a sufficiently high priority. All papers<br />
considered suitable by the Editors to progress further in the review process will undergo appropriate peer review and all<br />
papers provisionally accepted for publication will undergo a detailed statistical review.<br />
Preparation of manuscripts<br />
All submitted manuscripts must not exceed 5000 words, including References, Figure Legends and Tables. The number of<br />
Tables, Figures and References should be appropriate to the manuscript content and should not be excessive. Authors should<br />
comply with the manuscript formatting and the ethical conventions of the “Uniform Requirements for Manuscripts Submitted<br />
to Biomedical Journals” issued by the International Committee of Medical Journal Editors ( http://www.icmje.org ).<br />
Style and spelling<br />
Authors whose first language is not English are requested to have their manuscripts checked carefully before submission.<br />
This will help expedite the review process and avoid confusion. Abbreviations of standard SI units of measurement only<br />
should be used.<br />
Declaration of Helsinki<br />
The Authors should state that their study complies with the Declaration of Helsinki that the locally appointed ethics<br />
committee has approved the research protocol and that informed consent has been obtained from the subjects (or their<br />
guardians).<br />
Clinical trials<br />
Authors should comply with the clinical trial registration statement from the ICMJE. More information can be found at<br />
www.icmje.org. Clinical trial reports should also comply with the Consolidated Standards of Reporting Trials (CONSORT)<br />
and include a flow diagram presenting the enrollment, intervention allocation, follow-up, and data analysis with number of<br />
subjects for each (www.consort-statement.org). Please also refer specifically to the CONSORT Checklist of items to include<br />
when reporting a randomized clinical trial.<br />
Section of the manuscripts<br />
Original articles should be divided into the following sections: (1) Title page, (2) Abstract and Keywords, (3) Introduction,<br />
(4) Methods, (5) Results, (6) Discussion, (7) Conclusion, (8) Acknowledgements, (9) References, (10) Figure legends,<br />
(11) Tables, (12) Figures.<br />
General format<br />
Prepare your manuscript text using a word processing package. Submissions of text in the form of PDF files are not
<strong>TEHRAN</strong> <strong>HEART</strong> <strong>CENTER</strong><br />
permitted. Manuscripts should be double-spaced, including text, tables, legends and references. Number each page. Please<br />
avoid footnotes; use instead, and as sparingly as possible, parenthesis within brackets. Enter text in the style and order of<br />
the Journal. Type references in the correct order and style of the journal. Type unjustified, without hyphenation, except for<br />
compound words. Type headings in the style of the journal. Use the TAB key once for paragraph indents. Where possible use<br />
Times New Roman for the text font and Symbol for the Greek and special characters. Use the word processing formatting<br />
features to indicate Bold, Italic, Greek, Maths, Superscript and subscript characters. Clearly identify unusual symbols and<br />
Greek letters. Differentiate between the letter o and zero, and the letters I and i and the number 1. Mark the approximate<br />
position of each figure and table. Check the final copy of your paper carefully, as any spelling mistakes and errors may be<br />
translated into the typeset version.<br />
Title page<br />
The title page should include the following: (1) the title, (2) the name (s) of authors and their highest degree ( no more<br />
than 12 authors are acceptable), (3) the institution (s) where work was performed, (4) institution, and location of all authors,<br />
(5) the address, telephone number, fax number and e-mail address of the corresponding author.<br />
Abstract<br />
All abstracts may not contain more than 250 words and should also be submitted as a separate file. The abstract should be<br />
formatted with the following heading: (1) Background, (2) Methods, (3) Results, (4) Conclusion.<br />
A maximum of six Keywords may be submitted.<br />
Figures<br />
The review process will not begin until all figures are received. Figures should be limited to the number necessary for<br />
clarity and must not duplicate data given in tables or in the text. They must be suitable for high quality reproduction and<br />
should be submitted in the desired final printed size so that reduction can be avoided. Figures should be no larger than 125<br />
(height)×180 (width) mm (5×7 inches) and should be submitted in a separate file from that of the manuscript.<br />
Electronic submission of figures<br />
Figures should be saved in TIFF format at a resolution of at least 300 pixels per inch at the final printed size for colour<br />
figures and photographs, and 1200 pixels per inch for black and white line drawings. Although some other formats can be<br />
translated into TIFF format by the publisher, the conversion may alter the tones, resolution and contrast of the image. Digital<br />
colour art should be submitted in CMYK rather than RGB format, as the printing process requires colours to be separated<br />
into CMYK and this conversion can alter the intensity and brightness of colours. Therefore authors should be satisfied with<br />
the colours in CMYK (both on screen and when printed) before submission. Please also keep in mind that colours can appear<br />
differently on different screens and printers. Failure to follow these guides could result in complications and delays.<br />
Photographs: Photographs should be of sufficiently high quality with respect to detail, contrast and fineness of grain to<br />
withstand the inevitable loss of contrast and detail inherent in the printing process. Please indicate the magnification by a rule<br />
on the photograph. Colour figures: There is a special charge for the inclusion of colour figures. Figure legends: These should<br />
be on a separate, numbered manuscript sheet grouped under the heading “Legends” on a separate sheet of the manuscript<br />
after the References. Define all symbols and abbreviations used in the figure. All abbreviations and should be redefined in<br />
the legend.<br />
Tables<br />
Tables should be typed with double spacing, but minimizing redundant space and each should be placed on a separate<br />
sheet. Tables should be submitted, wherever possible, in portraits, as opposed to landscape, layout. Each Table should be<br />
numbered in sequence using Arabic numerals. Tables should also have a title above and an explanatory footnote below. All<br />
abbreviations and should be redefined in the Footnote.<br />
The Journal of Tehran University Heart Center
The Journal of Tehran University Heart Center<br />
Acknowledgements<br />
All sources of funding and support, and substantive contributions of individuals, should be noted in the Acknowledgements,<br />
positioned before the list of references.<br />
Reference format<br />
Number references sequentially and use Arabic number in superscript to cite the reference in the text. All references<br />
should be compiled at the end of the article in the Vancouver style. Complete information should be given for each reference<br />
including the title of the article, abbreviated journal title and page numbers. All authors should be listed. Personal communications;<br />
manuscripts in preparation and other unpublished data should not be cited in the reference list but may be mentioned<br />
in parentheses in the text. Authors should get permission from the source to cite unpublished data.<br />
Titles of journals should be abbreviated in accordance with Index Medicus (see list printed annually in the January issue<br />
of Index Medicus). If a journal is not listed in Index Medicus then its name should be written out in full.<br />
Article citation example:<br />
Journal citation example: 1. Schroeder S, Baumbach A, Mahrholdt H. The impact of untreated coronary dissections on the<br />
acute and long-term outcome after intravascular ultrasound guided PTCA. Eur Heart J 2000;21:137-145.<br />
Chapter citation example: 2. Nichols WW, O’Rourke MF. Aging, high blood pressure and disease in humans. In: Arnold<br />
E, ed. McDonald’s Blood Flow in Arteries: Theoretical, Experimental and Clinical Principles. 3rd ed. London/Melbourne/<br />
Auckland: Lea and Febiger; 1990. p. 398-420.<br />
Webpage citation example: 3. Panteghini M. Recommendations on use of biochemical markers in acute coronary syndrome:<br />
IFCC proposals. eJIFCC 14. http://www.ifcc.org/ejifcc/vol14no2/1402062003014n.htm (28 May 2004). Where the<br />
date in parenthesis refers to the access date.<br />
Statistics<br />
All manuscripts selected for publication will be reviewed for the appropriateness and accuracy of the statistical methods<br />
used and the interpretation of statistical results. All papers submitted should provide in their Methods section a subsection<br />
detailing the statistical methods, including the specific method used to summarize the data, the methods used to test their<br />
hypothesis testing and (if any) the level of significance used for hypothesis testing.<br />
Conflict of interest<br />
At submission, the editors require authors to disclose any financial association that might pose a conflict of interest in<br />
connection with the submitted article. All sources of funding for the work should be acknowledged in a footnote on the title<br />
page and in the Acknowledgements within the manuscript, as should all the institutional affiliations of the authors (including<br />
corporate appointments). Other kinds of associations, such as consultancies, stock ownership or other equity interest<br />
or patent-licensing arrangements should be disclosed to the editors in the cover letter at the time of the of submission. If no<br />
conflict of interest exists, please state this in the cover letter.<br />
Proofs<br />
Page proofs will be sent to the corresponding author. Please provide an e-mail address to enable page proofs to be sent<br />
as PDF files via e-mail. These should be checked thoroughly for any possible changes or typographic errors. Significant<br />
alterations instigated at this stage by the author will be charged to the author. It is the intention of the Editor to review,<br />
correct and publish your article as quickly as possible. To achieve this it is important that all of your corrections are returned<br />
to us in one all- inclusive mail or fax. Subsequent additional corrections will not be possible, so please ensure that your first<br />
communication is complete.
<strong>TEHRAN</strong> <strong>HEART</strong> <strong>CENTER</strong><br />
New Subscription:<br />
Surname:<br />
First Name:<br />
Hospital or Organization:<br />
Date of subscription:<br />
Full mail address:<br />
Subscription Form<br />
The Journal of Tehran University Heart Center<br />
P.O.BOX: Tell: Fax:<br />
E-mail:<br />
Continuation of Subscription:<br />
The annual Subscription and postage rate: 100/000 Rials for Iran and US $ 100 including postage for other countries.<br />
Please liquidate the total amount of Subscription and postal charges into:<br />
Bank: Refah Branch Code: 1232 Account: Tehran Heart Center Account Number: 200001.28<br />
and send the original Bank slip along with Duly completed form of Subscription to the following addre<br />
ss:<br />
Tehran Heart Center,<br />
North Karegar Street,<br />
Tehran, Iran: 1411713138<br />
Tel: +98 21 88029720<br />
Fax: +98 21 88029702<br />
E-mail: jthc@tums.ac.ir<br />
<strong>TEHRAN</strong> <strong>HEART</strong> <strong>CENTER</strong><br />
New Subscription:<br />
Surname:<br />
First Name:<br />
Hospital or Organization:<br />
Date of subscription:<br />
Full mail address:<br />
Subscription Form<br />
The Journal of Tehran University Heart Center<br />
P.O.BOX: Tell: Fax:<br />
E-mail:<br />
Continuation of Subscription:<br />
The annual Subscription and postage rate: 100/000 Rials for Iran and US $ 100 including postage for other countries.<br />
Please liquidate the total amount of Subscription and postal charges into:<br />
Bank: Refah Branch Code: 1232 Account: Tehran Heart Center Account Number: 200001.28<br />
and send the original Bank slip along with Duly completed form of Subscription to the following addre<br />
ss:<br />
Tehran Heart Center,<br />
North Karegar Street,<br />
Tehran, Iran: 1411713138<br />
Tel: +98 21 88029720<br />
Fax: +98 21 88029702<br />
E-mail: jthc@tums.ac.ir<br />
<strong>TEHRAN</strong> <strong>HEART</strong> <strong>CENTER</strong><br />
The Journal of Tehran University Heart Center