Post coronary artery bypass graft surgery
Post coronary artery bypass graft surgery
Post coronary artery bypass graft surgery
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
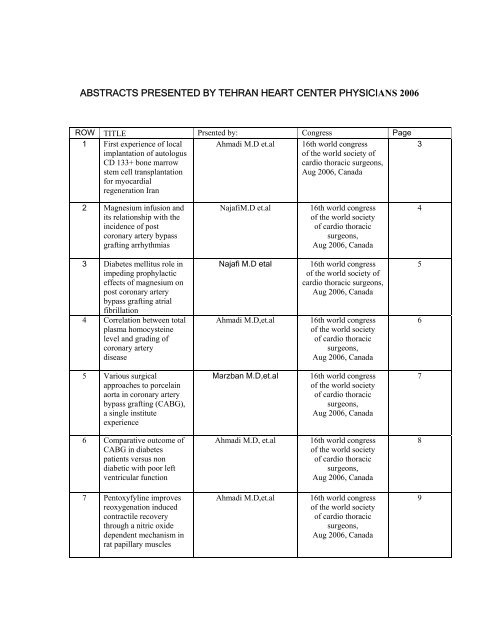
ABSTRACTS PRESENTED BY TEHRAN HEART CENTER PHYSICIANS 2006<br />
ROW<br />
1<br />
TITLE<br />
First experience of local<br />
implantation of autologus<br />
CD 133+ bone marrow<br />
stem cell transplantation<br />
for myocardial<br />
regeneration Iran<br />
Prsented by:<br />
Ahmadi M.D et.al<br />
Congress<br />
16th world congress<br />
of the world society of<br />
cardio thoracic surgeons,<br />
Aug 2006, Canada<br />
Page<br />
3<br />
2<br />
Magnesium infusion and<br />
its relationship with the<br />
incidence of post<br />
<strong>coronary</strong> <strong>artery</strong> <strong>bypass</strong><br />
<strong>graft</strong>ing arrhythmias<br />
NajafiM.D et.al<br />
16th world congress<br />
of the world society<br />
of cardio thoracic<br />
surgeons,<br />
Aug 2006, Canada<br />
4<br />
3<br />
4<br />
Diabetes mellitus role in<br />
impeding prophylactic<br />
effects of magnesium on<br />
post <strong>coronary</strong> <strong>artery</strong><br />
<strong>bypass</strong> <strong>graft</strong>ing atrial<br />
fibrillation<br />
Correlation between total<br />
plasma homocysteine<br />
level and grading of<br />
<strong>coronary</strong> <strong>artery</strong><br />
disease<br />
Najafi M.D etal<br />
Ahmadi M.D,et.al<br />
16th world congress<br />
of the world society of<br />
cardio thoracic surgeons,<br />
Aug 2006, Canada<br />
16th world congress<br />
of the world society<br />
of cardio thoracic<br />
surgeons,<br />
Aug 2006, Canada<br />
5<br />
6<br />
5<br />
Various surgical<br />
approaches to porcelain<br />
aorta in <strong>coronary</strong> <strong>artery</strong><br />
<strong>bypass</strong> <strong>graft</strong>ing (CABG),<br />
a single institute<br />
experience<br />
Marzban M.D,et.al<br />
16th world congress<br />
of the world society<br />
of cardio thoracic<br />
surgeons,<br />
Aug 2006, Canada<br />
7<br />
6<br />
Comparative outcome of<br />
CABG in diabetes<br />
patients versus non<br />
diabetic with poor left<br />
ventricular function<br />
Ahmadi M.D, et.al<br />
16th world congress<br />
of the world society<br />
of cardio thoracic<br />
surgeons,<br />
Aug 2006, Canada<br />
8<br />
7<br />
Pentoxyfyline improves<br />
reoxygenation induced<br />
contractile recovery<br />
through a nitric oxide<br />
dependent mechanism in<br />
rat papillary muscles<br />
Ahmadi M.D,et.al<br />
16th world congress<br />
of the world society<br />
of cardio thoracic<br />
surgeons,<br />
Aug 2006, Canada<br />
9
ROW<br />
8<br />
TITLE<br />
Experience with 36<br />
transvenous <strong>coronary</strong><br />
sinus lead implantation<br />
for cardiac<br />
resynchronization therapy<br />
Prsented by:<br />
Yamini sharif M.D , et.al<br />
Congress<br />
8th Asian pacific<br />
symposium<br />
on cardiac pacing and<br />
electrophysiology, Aug<br />
2006, Indonesia<br />
Page<br />
10<br />
9<br />
10<br />
Mid term follow up of<br />
sixty patients with<br />
implantable cardioverter<br />
defibrillator<br />
Induced myocardial<br />
infarction using ligation<br />
of the left anterior<br />
descending <strong>coronary</strong><br />
<strong>artery</strong> major diagonal<br />
branch: development of<br />
an ovine model<br />
Yamini sharif M.D, et.al<br />
Rabani M.D , et.al<br />
8th Asian pacific<br />
symposium<br />
on cardiac pacing and<br />
electrophysiology, Aug<br />
2006, Indonesia<br />
6th biennial international<br />
conference of Pakistan<br />
society of cardiovascular<br />
&<br />
thoracic surgeons, Dec<br />
2006, Karachi<br />
11<br />
12<br />
11<br />
First experience of local<br />
implantation of autologus<br />
CD 133+ bone marrow<br />
stem cell transplantation<br />
for myocardial<br />
regeneration Iran<br />
Ahmadi M.D, et.al<br />
Stem cell therapy for the<br />
failing heart, Dec 2006,<br />
Thailand<br />
13<br />
12<br />
PCL scaffold <strong>graft</strong>ed onto<br />
Infracted myocardium in<br />
sheep animal model: a<br />
vehicle for<br />
cardiomyocytes<br />
Soleymani M.D ,et.al<br />
Stem cell therapy for the<br />
failing heart, Dec<br />
2006,<br />
Thailand<br />
14<br />
13<br />
Improvement of cardiac<br />
function and tissue<br />
viability following<br />
expanded autologus<br />
marrow derived CD133<br />
stem cell transplantation<br />
in patients with ischemic<br />
cardiomyopathy<br />
undergoing <strong>coronary</strong><br />
<strong>bypass</strong> <strong>surgery</strong><br />
Ahmadi M.D,et.al<br />
Stem cell therapy for the<br />
failing heart, Dec 2006,<br />
Thailand<br />
15<br />
14<br />
Normal values for<br />
ventricular synchrony<br />
measured by tissue<br />
Doppler imaging and<br />
tissue Doppler<br />
synchronization imaging<br />
in structurally normal<br />
hearts<br />
Sadeghian H, M.D et.al<br />
10th anniversary Euro<br />
echo, Dec 2006<br />
17
ROW<br />
15<br />
TITLE<br />
Clinical characteristics of<br />
women with premature<br />
<strong>coronary</strong> <strong>artery</strong> disease<br />
requiring CABG<br />
compared with that of<br />
young men<br />
Prsented by:<br />
Daryani M.D , et.al<br />
Congress<br />
European heart congress,<br />
Barcelona , spanin ,2006<br />
Page<br />
19<br />
16<br />
Impact of risk factors for<br />
development of <strong>coronary</strong><br />
<strong>artery</strong> disease in patients<br />
undergoing CABG in<br />
Iran compared with that<br />
in USA<br />
Daryani M.D ,et.al<br />
European heart congress,<br />
Barcelona , spanin ,2006<br />
20<br />
17<br />
Association of<br />
lipoprotein(a) levels with<br />
the severity of <strong>coronary</strong><br />
<strong>artery</strong> stenosis in an<br />
Iranian population<br />
(according to Gensini<br />
score)<br />
Broumand M.D , et.al<br />
European heart congress,<br />
Barcelona , spanin ,2006<br />
22<br />
18<br />
19<br />
Fast track method in<br />
cardiac <strong>surgery</strong> :<br />
evaluation of risks<br />
and benefits<br />
Relationship between<br />
serum magnesium level<br />
and post <strong>coronary</strong> <strong>artery</strong><br />
<strong>bypass</strong> <strong>graft</strong> <strong>surgery</strong><br />
arrhythmias<br />
Najafi M.D ,et.al<br />
Najafi M.D, et.al<br />
European congress of<br />
anesthesiology Madrid ,<br />
spain ,2006<br />
European congress of<br />
anesthesiology Madrid ,<br />
spain ,2006<br />
23<br />
24<br />
20<br />
Carotid stenting in<br />
candidates for <strong>coronary</strong><br />
<strong>artery</strong> <strong>bypass</strong> <strong>surgery</strong>:<br />
Results of a heart hospital<br />
registry<br />
Kazemi saleh M.D,et.al<br />
Angioplasty Summit,<br />
2006,<br />
25<br />
21<br />
Predictors of the major<br />
adverse cardiac events<br />
(MACE) after<br />
percutaneous <strong>coronary</strong><br />
intervention- A single<br />
center registry<br />
Salari far M.D , et.al<br />
15th congress of the<br />
Iranian<br />
heart association, 2006,<br />
Iran<br />
27<br />
22<br />
Comparative study of<br />
success rate &<br />
complications frequency<br />
in two streptokinase trade<br />
forms: "A Randomized<br />
Double Blind Study”<br />
Salari far M.D, et.al<br />
15th congress of the<br />
Iranian<br />
heart association, 2006,<br />
Iran<br />
29
ROW<br />
23<br />
TITLE<br />
Study of factors affecting<br />
in- hospital mortality of<br />
patients with acute<br />
myocardial infarction<br />
Prsented by:<br />
Salari far M.D, et.al<br />
Congress<br />
15th congress of the<br />
Iranian<br />
heart association, 2006,<br />
Iran<br />
Page<br />
31<br />
24<br />
Risk factors for<br />
complications of delay in<br />
<strong>surgery</strong> in staged carotid<br />
stenting and <strong>coronary</strong><br />
<strong>bypass</strong> <strong>graft</strong> <strong>surgery</strong><br />
Kassaian M.D,et.al<br />
15th congress of the<br />
Iranian<br />
heart association, 2006,<br />
Iran<br />
33<br />
25<br />
26<br />
Angiographic profile and<br />
lesion characteristics in<br />
young patients with<br />
percutaneous <strong>coronary</strong><br />
intervention<br />
Short and long-term<br />
outcome of PCI in<br />
diabetic patients using<br />
drug eluting stents<br />
(DES)-A single center<br />
registry<br />
Kassaian M.D et.al<br />
Kassaian M.D, et.al<br />
15th congress of the<br />
Iranian<br />
heart association,<br />
2006,<br />
Iran<br />
15th congress of the<br />
Iranian<br />
heart association, 2006,<br />
Iran<br />
34<br />
35<br />
27<br />
Short and long-term<br />
outcome of PCI on the<br />
saphenous vein <strong>graft</strong>s a<br />
case series with 9 months<br />
follow up<br />
Kassaian M.D, et.al<br />
15th congress of the<br />
Iranian<br />
heart association, 2006,<br />
Iran<br />
36<br />
28<br />
Short and long-term<br />
outcomes following<br />
percutaneous <strong>coronary</strong><br />
intervention in young<br />
patient<br />
Kassaian M.D, et.al<br />
15th congress of the<br />
Iranian<br />
heart association, 2006,<br />
Iran<br />
37<br />
29<br />
Sensitivity and specificity<br />
of Q wave for diagnosis<br />
of wall motion<br />
abnormality in patients<br />
with <strong>coronary</strong> <strong>artery</strong><br />
disease<br />
sadeghian H. M.D, et.al<br />
15th congress of the<br />
Iranian<br />
heart association, 2006,<br />
Iran<br />
38<br />
30<br />
The prognosis of non-Qwave<br />
versus Q-wave<br />
myocardial infarction<br />
sadeghian H M.D, et.al<br />
15th congress of the<br />
Iranian<br />
heart association, 2006,<br />
Iran<br />
39<br />
31<br />
Normal values for<br />
ventricular synchrony<br />
measured by tissue<br />
Doppler synchronization<br />
imaging in structurally<br />
normal hearts<br />
sadeghian H M.D,et.al<br />
15th congress of the<br />
Iranian<br />
heart association, 2006,<br />
Iran<br />
40
ROW<br />
32<br />
TITLE<br />
Discrete subvalvular aortic<br />
stenosis: severity of aortic<br />
insufficiency and rate of<br />
recurrence after <strong>surgery</strong><br />
Prsented by:<br />
sadeghian H M.D , et.al<br />
Congress<br />
15th congress of the<br />
Iranian<br />
heart association, 2006,<br />
Iran<br />
Page<br />
42<br />
33<br />
Repositioning of dislodged<br />
atrial pacing lead with a<br />
specially designed<br />
urologic basket<br />
Yamini sharif M.D , et.al<br />
15th congress of the<br />
Iranian<br />
heart association, 2006,<br />
Iran<br />
̊ 43<br />
34<br />
Radiofrequency ablation<br />
of cardiac arrhythmia<br />
using a three-dimensional<br />
real-time position<br />
management and mapping<br />
system<br />
Yamini sharif M.D,et.al<br />
15th congress of the<br />
Iranian<br />
heart association, 2006,<br />
Iran<br />
45<br />
35<br />
Higher dose of heparin<br />
administration for<br />
prevention of catheterinduced<br />
thrombo -embolic<br />
events during cardiac<br />
catheterization & <strong>coronary</strong><br />
angiography<br />
Yamini sharif M.D , et.al<br />
15th congress of the<br />
Iranian<br />
heart association, 2006,<br />
Iran<br />
46<br />
36<br />
Early complications of<br />
permanent pacemaker<br />
implantation<br />
Yamini sharif M.D , et.al<br />
15th congress of the<br />
Iranian<br />
heart association, 2006,<br />
Iran<br />
47<br />
37<br />
Effect of completion of<br />
exercise training sessions<br />
in cardiac rehabilitation of<br />
physical functioning: A<br />
Historical Cohort Study<br />
Soleimani M.D, et.al<br />
15th congress of the<br />
Iranian<br />
heart association, 2006,<br />
Iran<br />
48<br />
38<br />
Coronary <strong>artery</strong> disease<br />
pattern in young adults<br />
compared with older<br />
patients<br />
Soleimani M.D, et.al<br />
15th congress of the<br />
Iranian<br />
heart association, 2006,<br />
Iran<br />
49<br />
39<br />
Physical functioning<br />
recovery following cardiac<br />
rehabilitation in post<br />
valvular <strong>surgery</strong> patients<br />
Soleimani M.D, et.al<br />
15th congress of the<br />
Iranian<br />
heart association, 2006,<br />
Iran<br />
50<br />
40<br />
Influence of complete<br />
cardiac rehabilitation on<br />
physical functioning after<br />
percutaneous transluminal<br />
<strong>coronary</strong> angioplasty<br />
Soleimani M.D, et.al<br />
15th congress of the<br />
Iranian<br />
heart association, 2006,<br />
Iran<br />
51
ROW<br />
41<br />
TITLE<br />
Correlation between 12-<br />
lead rest ECG and severe<br />
and very severe single<br />
<strong>coronary</strong> <strong>artery</strong> stenosis in<br />
patients with stable angina<br />
hospitalized in Tehran<br />
Heart Center<br />
Prsented by:<br />
Soleimani M.D, et.al<br />
Congress<br />
15th congress of the<br />
Iranian<br />
heart association, 2006,<br />
Iran<br />
Page<br />
52<br />
42<br />
The association between<br />
Hepatitis B surface<br />
antibody seropositivity<br />
and <strong>coronary</strong> <strong>artery</strong><br />
disease<br />
Amir zadegan M.D ,et.al<br />
15th congress of the<br />
Iranian<br />
heart association, 2006,<br />
Iran<br />
53<br />
43<br />
Frequency and prognosis<br />
of patients with segmental<br />
back flow of the contrast<br />
material in<br />
<strong>coronary</strong> arteries<br />
Amir zadegan M.D ,et.al<br />
15th congress of the<br />
Iranian<br />
heart association, 2006,<br />
Iran<br />
54<br />
44<br />
The relation between<br />
androgen levels in men<br />
and different stages of<br />
heart failure<br />
Davoodi M.D, et.al<br />
15th congress of the<br />
Iranian<br />
heart association, 2006,<br />
Iran<br />
55<br />
45<br />
Is there any gender<br />
difference in location of<br />
<strong>coronary</strong> involvement<br />
Davoodi M.D, et.al<br />
15th congress of the<br />
Iranian<br />
heart association,<br />
2006, Iran<br />
56<br />
46<br />
Influence of cigarette<br />
smoking on the risk of<br />
metabolic syndrome, body<br />
weight and waist<br />
circumferences in men<br />
with premature <strong>coronary</strong><br />
<strong>artery</strong> disease<br />
Davoodi M.D, et.al<br />
15th congress of the<br />
Iranian<br />
heart association, 2006,<br />
Iran<br />
57<br />
47<br />
The association between<br />
levels of male androgenic<br />
hormones and severity of<br />
<strong>coronary</strong> <strong>artery</strong> disease<br />
Davoodi M.D, et.al<br />
15th congress of the<br />
Iranian<br />
heart association, 2006,<br />
Iran<br />
58<br />
48<br />
Parental cardiovascular<br />
disease as a risk factor for<br />
acute <strong>coronary</strong> syndromes<br />
in adult offspring<br />
Hoseini M.D ,et.al<br />
15th congress of the<br />
Iranian<br />
heart association, 2006,<br />
Iran<br />
59
ROW<br />
49<br />
TITLE<br />
Is there any difference in<br />
EKG findings in responder<br />
and non- responder groups<br />
of CRT recipients<br />
Prsented by:<br />
Kazemi saied M.D,et.al<br />
Congress<br />
15th congress of the<br />
Iranian<br />
heart association, 2006,<br />
Iran<br />
Page<br />
60<br />
50<br />
Comparison between the<br />
effects of sedative drugs<br />
and placebo for <strong>coronary</strong><br />
angiography on<br />
patients'anxiety and<br />
hemodynamic status<br />
Kazemi saied M.D,et.al<br />
15th congress of the<br />
Iranian<br />
heart association, 2006,<br />
Iran<br />
61<br />
51<br />
Prevalence of CAD and<br />
related risk factors in first<br />
degree relatives of patients<br />
with premature CAD<br />
admitted in Tehran Heart<br />
Center in 2003-2004<br />
Kazemeni M.D,et.al<br />
15th congress of the<br />
Iranian<br />
heart association, 2006,<br />
Iran<br />
62<br />
52<br />
Left ventricular ejection<br />
fraction by left<br />
ventriculography before or<br />
after <strong>coronary</strong><br />
angiography correlation<br />
with left ventricular<br />
ejection fraction<br />
by echocardiography<br />
Kazemi saied M.D,et.al<br />
15th congress of the<br />
Iranian<br />
heart association, 2006,<br />
Iran<br />
63<br />
53<br />
Cardiovascular morbidity<br />
in relation to educational<br />
level in patients with chest<br />
pain presentation<br />
Yamini sharif M.D , et.al<br />
15th congress of the<br />
Iranian<br />
heart association, 2006,<br />
Iran<br />
64<br />
54<br />
Cardiopulmonary<br />
resuscitation; early results<br />
and success predictors- A<br />
single center registry<br />
Najafi M.D ,et.al<br />
15th congress of the<br />
Iranian<br />
heart association, 2006,<br />
Iran<br />
65<br />
55<br />
Early clinical result of<br />
double endarterectomy<br />
and reconstruction<br />
combined with multiple<br />
<strong>bypass</strong>es <strong>graft</strong>ing for<br />
severe <strong>coronary</strong> <strong>artery</strong><br />
disease: A single<br />
institute experience<br />
Marzban M.D , et.al<br />
15th congress of the<br />
Iranian<br />
heart association, 2006,<br />
Iran<br />
67<br />
56<br />
Non use of left internal<br />
mammary <strong>artery</strong>: It's a<br />
contributing factor<br />
Marzban M.D , et.al<br />
15th congress of the<br />
Iranian<br />
heart association, 2006,<br />
Iran<br />
68
ROW<br />
57<br />
TITLE<br />
Out come of <strong>coronary</strong><br />
<strong>artery</strong> <strong>bypass</strong> <strong>surgery</strong> in<br />
diabetic and non diabetic<br />
patients: A Comparative<br />
Study<br />
Prsented by:<br />
Ahmadi M.D , et.al<br />
Congress<br />
15th congress of the<br />
Iranian<br />
heart association, 2006,<br />
Iran<br />
Page<br />
69<br />
58<br />
Results of <strong>coronary</strong> <strong>artery</strong><br />
<strong>bypass</strong> <strong>graft</strong>ing in dialysis<br />
patients<br />
Ahmadi M.D , et.al<br />
15th congress of the<br />
Iranian<br />
heart association, 2006,<br />
Iran<br />
70<br />
59<br />
The impact of low serum<br />
triglyceride on LDLcholesterol<br />
estimation<br />
Ahmadi M.D , et.al<br />
15th congress of the<br />
Iranian<br />
heart association, 2006,<br />
Iran<br />
71<br />
60<br />
61<br />
Twenty four hours inhospital<br />
mortality<br />
predictions in <strong>coronary</strong><br />
<strong>artery</strong> <strong>bypass</strong> <strong>graft</strong>ing<br />
<strong>surgery</strong> patients<br />
Evidence for higher<br />
mortality in women after<br />
<strong>coronary</strong> <strong>artery</strong> <strong>bypass</strong><br />
<strong>graft</strong> <strong>surgery</strong><br />
Ahmadi M.D , et.al<br />
Sadeghian M.D ,et.al<br />
15th congress of the<br />
Iranian<br />
heart association, 2006,<br />
Iran<br />
15th congress of the<br />
Iranian<br />
heart association, 2006,<br />
Iran<br />
72<br />
73<br />
62<br />
A new risk factor for<br />
<strong>coronary</strong> <strong>artery</strong> disease<br />
Sadeghian M.D ,et.al<br />
15th congress of the<br />
Iranian<br />
heart association, 2006,<br />
Iran<br />
74<br />
63<br />
Direct costs of invasive<br />
cardiac procedures for<br />
heart diseases in the<br />
Islamic republic of Iran<br />
Sadeghian M.D ,et.al<br />
15th congress of the<br />
Iranian<br />
heart association, 2006,<br />
Iran<br />
75<br />
64<br />
Results on noninvasive<br />
tests compared with results<br />
of angiography in young<br />
patients<br />
Sadeghian M.D ,et.al<br />
15th congress of the<br />
Iranian<br />
heart association, 2006,<br />
Iran<br />
77<br />
65<br />
The association between<br />
left main <strong>coronary</strong> <strong>artery</strong><br />
disease and ischemic heart<br />
disease risk factors<br />
Darabian M.D , et.al<br />
15th congress of the<br />
Iranian<br />
heart association, 2006,<br />
Iran<br />
78<br />
66<br />
Evaluation of preoperative<br />
CRP serum level and<br />
CABG outcome in acute<br />
<strong>coronary</strong> syndrome<br />
patients<br />
Abbasi M.D ,et al<br />
15th congress of the<br />
Iranian<br />
heart association, 2006,<br />
Iran<br />
79<br />
67<br />
Developing a <strong>surgery</strong><br />
database: design and<br />
operation<br />
Abbasi M.D ,et al<br />
15th congress of the<br />
Iranian heart association,<br />
2006,<br />
80
ROW<br />
TITLE<br />
Prsented by:<br />
Congress<br />
Iran<br />
Page<br />
68<br />
Mediastinitis after<br />
<strong>coronary</strong> <strong>artery</strong> <strong>bypass</strong><br />
<strong>surgery</strong> (CABG), an<br />
evaluation of effect of<br />
different factors on<br />
developping ediastinitis<br />
after CABG in more than<br />
9000 cases<br />
Salehi Omran M.D , et.al<br />
15th congress of the<br />
Iranian heart association,<br />
2006,<br />
Iran<br />
81<br />
69<br />
Comparison of short and<br />
long-term outcomes<br />
between Sirolimus eluting<br />
stents and Paclitaxel<br />
eluting stents<br />
Ali doosti M.D , et.al<br />
15th congress of the<br />
Iranian heart association,<br />
2006, Iran<br />
82<br />
70<br />
Comparison of outcomes<br />
of percutaneous <strong>coronary</strong><br />
intervention on proximal<br />
versus non-proximal left<br />
anterior descending<br />
<strong>coronary</strong> <strong>artery</strong>, proximal<br />
left circumflex and<br />
proximal right <strong>coronary</strong><br />
<strong>artery</strong><br />
Alidoosti M.D,et.al<br />
15th congress of the<br />
Iranian heart association,<br />
2006,<br />
Iran<br />
83<br />
71<br />
Comparison of utcomes of<br />
direct stenting versus<br />
stenting with predilation<br />
Ali doosti M.D,et.al<br />
15 th congress of the<br />
Iranian heart association<br />
, 2006, Iran<br />
84<br />
72<br />
73<br />
Comparison of short and<br />
long-term outcomes and<br />
success rate of drugeluting<br />
stents with nondrug<br />
eluting stents<br />
Association of<br />
lipoprotein (a) levels with<br />
the severity of <strong>coronary</strong><br />
<strong>artery</strong> stenosis in an<br />
Iranian population<br />
(According to Gensini<br />
Score)<br />
Ali doosti M.D,et.al<br />
Broumand M.D, et.al<br />
15th congress of the<br />
Iranian heart association,<br />
2006,<br />
Iran<br />
15th congress of<br />
the Iranian heart<br />
association, 2006,<br />
Iran<br />
85<br />
́86<br />
74<br />
Interventional closure of<br />
patent foramen ovale with<br />
amplatzer PFO occluder in<br />
patients with paradoxical<br />
cerebral embolism<br />
Haje zeinali M.D, et.al<br />
15th congress of the<br />
Iranian heart association,<br />
2006,<br />
Iran<br />
87
ROW<br />
75<br />
TITLE<br />
Self-expandable stent<br />
implantation for severe<br />
native coarctation of aorta<br />
in adults<br />
Prsented by:<br />
Haje zeinali M.D, et.al<br />
Congress<br />
15th congress of the<br />
Iranian heart association,<br />
2006,<br />
Iran<br />
Page<br />
88<br />
76<br />
Echocardiographic<br />
predictors of left atrial<br />
appendage contraction<br />
velocity<br />
Saheb jam M.D ,et.al<br />
15th congress of the<br />
Iranian heart association,<br />
2006,<br />
Iran<br />
89<br />
77<br />
Magnesium infusion and<br />
its relationship with the<br />
incidence of post <strong>coronary</strong><br />
<strong>artery</strong> <strong>bypass</strong> <strong>graft</strong>ing<br />
arrhythmias<br />
Najafi M.D,et.al<br />
15th congress of the<br />
Iranian heart association,<br />
2006,<br />
Iran<br />
90<br />
78<br />
Results of <strong>coronary</strong> <strong>artery</strong><br />
<strong>bypass</strong> <strong>graft</strong>ing dialysis<br />
patients<br />
Ahmadi M.D, et.al<br />
15th congress of the<br />
Iranian heart association,<br />
2006,<br />
Iran<br />
91<br />
79<br />
80<br />
Late outcomes in patients<br />
with uncorrected moderate<br />
mitral regurgitation at the<br />
time of isolated <strong>coronary</strong><br />
<strong>artery</strong> <strong>bypass</strong><br />
The adverse effects of<br />
Milrinone in the elderly<br />
patients who underwent<br />
CABG<br />
Davoodi M.D, et.al<br />
Davoodi M.D, et.al<br />
15th congress of the<br />
Iranian heart association,<br />
2006,<br />
Iran<br />
15th congress of the<br />
Iranian heart association,<br />
2006,<br />
Iran<br />
92<br />
93<br />
81<br />
Correlation between net<br />
atrioventricular<br />
compliance and<br />
pulmonary <strong>artery</strong> pressure<br />
in mitral valve stenosis<br />
Saheb jam M.D , et.al<br />
15th congress of the<br />
Iranian heart association,<br />
2006,<br />
Iran<br />
94<br />
82<br />
Diabetes mellitus role in<br />
impeding prophylactic<br />
effects of magnesium on<br />
post atrial fibrillation<br />
Najafi M.D,et.al<br />
15th congress of the<br />
Iranian heart association,<br />
2006,<br />
Iran<br />
95<br />
83<br />
Beta-blocker<br />
administration<br />
for preventing post<br />
<strong>coronary</strong> <strong>artery</strong> <strong>bypass</strong><br />
<strong>graft</strong> arrhythmias" The<br />
role of diabetes mellitus<br />
Najafi M.D,et.al<br />
15th congress of the<br />
Iranian heart association,<br />
2006,<br />
Iran<br />
96
ABSTRAKT PRESENTED BY TEHRAN HEART CENTER PHYSICIANS<br />
2005<br />
ROW<br />
1<br />
2<br />
TITLE<br />
Coronary endartrectomy<br />
with off pump <strong>coronary</strong><br />
<strong>bypass</strong> <strong>surgery</strong><br />
(OPCAB): safe and<br />
feasible<br />
Prsented by:<br />
Marzban M.D ,et.al<br />
Davoodi M.D , et.al<br />
Congress<br />
3rd winter workshop,<br />
Shanghai, 2005<br />
Page<br />
99<br />
100<br />
3<br />
4<br />
Centrifugal pump as a<br />
temporary assist device<br />
for postcardiotomy heart<br />
failure<br />
Evaluation of correlation<br />
between serum level of<br />
lipoprotein (a) and<br />
cervical carotid <strong>artery</strong><br />
stenosis<br />
Evaluation of correlation<br />
between serum level of<br />
lipoprotein (a) and<br />
cervical carotid <strong>artery</strong><br />
stenosis<br />
Broumand M.D ,et.al<br />
Broumand M.D ,et.al<br />
58em congres de la<br />
societe francaise de<br />
chirurgie thoracique et<br />
cardiovasculaire, Parsi,<br />
2005<br />
ESC congress,<br />
Stockholm, 2005<br />
XXIII. World Congress<br />
of Pathology and<br />
Laboratory Medicine,<br />
Istanbul, 2005<br />
101<br />
102<br />
5<br />
Asymptomatic<br />
bacteriuria in type 2<br />
diabetic women in iran<br />
Broumand M.D ,et.al<br />
XXIII. World Congress<br />
of Pathology and<br />
Laboratory Medicine,<br />
Istanbul, 2005<br />
103<br />
6<br />
7<br />
Prognostic value of<br />
quantitative C-reactive<br />
protein in assessing intra<br />
– hospital MI in stable<br />
angina patients<br />
Predictive factors of the<br />
cardiopulmonary<br />
resuscitation results<br />
Broumand M.D et.al<br />
Najafi M.D ,et.al<br />
XXIII. World Congress<br />
of Pathology and<br />
Laboratory Medicine,<br />
Istanbul, 2005<br />
The 4th international<br />
congress of the Iranian<br />
society of cardiac<br />
surgeons, Tehran, 2005<br />
104<br />
105<br />
8<br />
<strong>Post</strong> <strong>coronary</strong> <strong>artery</strong><br />
<strong>bypass</strong> <strong>graft</strong> <strong>surgery</strong><br />
(CABG) atrial<br />
fibrillation : evaluating<br />
predisposing and<br />
preventive factors<br />
Najafi M.D , et.al<br />
The 4th international<br />
congress of the Iranian<br />
society of cardiac<br />
surgeons, Tehran, 2005<br />
106
ROW<br />
9<br />
TITLE<br />
Fast tract methods in<br />
carotid <strong>surgery</strong> :evaluation<br />
of risk and benefils<br />
Prsented by:<br />
Najafi M.D et.al<br />
Congress<br />
The 4th international<br />
congress of the Iranian<br />
society of cardiac<br />
surgeons, Tehran, 2005<br />
Page<br />
107<br />
10<br />
Effect of CABG on elderly<br />
patients: mortality,<br />
morbidity<br />
& mid term follow up<br />
Davoodi M.D,et.al<br />
The 4th international<br />
congress of the<br />
Iranian<br />
society of cardiac<br />
surgeons, Tehran, 2005<br />
108<br />
11<br />
Various surgical<br />
approaches to complex<br />
aortic arch<br />
aneurysim, a single<br />
institute experience<br />
Abbasi M.D,et.al<br />
The 4th international<br />
congress of the Iranian<br />
society of cardiac<br />
surgeons, Tehran, 2005<br />
109<br />
12<br />
Have diabetes worsen the<br />
outcome of CABG<br />
Ahmadi M.D ,et.al<br />
The 4th international<br />
congress of the Iranian<br />
society of cardiac<br />
surgeons, Tehran, 2005<br />
111<br />
13<br />
Comparison of eurologic<br />
and psychologic<br />
complications between<br />
conventional CABG and<br />
off-pump CABG<br />
Abbasi M.D , et.al<br />
The 4th international<br />
congress of the Iranian<br />
society of cardiac<br />
surgeons, Tehran, 2005<br />
112<br />
14<br />
In vitro effects of<br />
cardioplegia on<br />
saphenous<br />
vein <strong>graft</strong>s during CABG<br />
Ahmadi M.D, et.al<br />
The 4th international<br />
congress of the<br />
Iranian society of cardiac<br />
surgeons, Tehran, 2005<br />
113
ROW<br />
15<br />
TITLE<br />
Outcomes and long term<br />
survival for patients<br />
undergoing mitral valve<br />
repair versus replacement<br />
concomitant <strong>coronary</strong><br />
<strong>bypass</strong><br />
Prsented by:<br />
Sadeghian .h M.D ,et.al<br />
Congress<br />
The 4th international<br />
congress of the Iranian<br />
society of cardiac<br />
surgeons, Tehran, 2005<br />
Page<br />
114<br />
16<br />
Moderate nonorganic<br />
mitral regurgitation and<br />
<strong>coronary</strong> disease:<br />
treatment by<br />
<strong>coronary</strong> <strong>bypass</strong> alone<br />
Sadeghian .h M.D ,et.al<br />
The 4th international<br />
congress of the Iranian<br />
society of cardiac<br />
surgeons, Tehran, 2005<br />
115<br />
17<br />
Mid-term follow up of<br />
sixty patients with<br />
implantable cardiovertor<br />
defibrillator<br />
Yamini sharif<br />
M.D,et.al<br />
The 4th international<br />
congress of the Iranian<br />
society of cardiac<br />
surgeons, Tehran, 2005<br />
116<br />
18<br />
Evaluation of the effect of<br />
NMDA receptor inhibitors<br />
in<br />
controlling post <strong>coronary</strong><br />
<strong>artery</strong> <strong>bypass</strong> <strong>graft</strong> <strong>surgery</strong><br />
pain of addicted patients<br />
Najafi M.D, et.al<br />
The 4th international<br />
congress of the Iranian<br />
society of cardiac<br />
surgeons, Tehran, 2005<br />
117<br />
19<br />
Relationship between<br />
serum magnesium level<br />
and post <strong>coronary</strong> <strong>artery</strong><br />
<strong>bypass</strong> <strong>graft</strong> <strong>surgery</strong><br />
arrhythmias<br />
Najafi M.D,et.al<br />
The 4th international<br />
congress of the Iranian<br />
society of cardiac<br />
surgeons, Tehran, 2005<br />
118
ROW<br />
20<br />
TITLE<br />
First experience of local<br />
implantation of autologus<br />
AC133+ bone marrow<br />
stem cell transplantation<br />
for developing country<br />
Prsented by:<br />
Ahmadi M.D ,et.al<br />
Congress<br />
The 4th international<br />
congress of the Iranian<br />
society of cardiac<br />
surgeons, Tehran, 2005<br />
Page<br />
119
ROW<br />
1<br />
ABSTRAKT PRESENTED BY TEHRAN HEART CENTER PHYSICIANS<br />
2004<br />
TITLE<br />
Prsented by:<br />
Congress<br />
Comparison of two Marzban M.D,et.al meeting of the Asian<br />
surgical techniques for<br />
society for<br />
radial <strong>artery</strong> harvesting in<br />
cardiovascular <strong>surgery</strong>,<br />
<strong>coronary</strong> <strong>artery</strong> <strong>bypass</strong><br />
Istanbul, 2004<br />
<strong>surgery</strong><br />
Page<br />
123<br />
2<br />
Seven year follow-up of<br />
<strong>coronary</strong> <strong>artery</strong> <strong>surgery</strong> in<br />
young adults (
ROW<br />
6<br />
TITLE<br />
Long-term evaluation of<br />
laser-treated silicone(lts)<br />
membrane as a ericardial<br />
substitute an experimental<br />
study<br />
Prsented by:<br />
Ahmadi M.D, et.al<br />
Congress<br />
The 14th world congress<br />
of<br />
international society of<br />
cardio-thoracic<br />
surgeons,<br />
China, Oct 2004<br />
Page<br />
128<br />
7<br />
Preparation of chitosan<br />
derived from sherimp's shell<br />
of Persian gulf as a blood<br />
hemostasis agent<br />
Ahmadi M.D,et.al<br />
The 14th world congress<br />
of<br />
international society of<br />
cardio-thoracic<br />
surgeons,<br />
China, Oct 2004<br />
129<br />
8<br />
Evaluation of cardiac<br />
adhesions after pericardial<br />
substitution by laser-treated<br />
silicon (its)membrane<br />
Ahmadi M.D,et.al<br />
XXXI Annual<br />
ESAO Congress,<br />
Warsaw, 2004<br />
130<br />
9<br />
Steal phenomena from<br />
mammary side branches:<br />
real or imaginary<br />
Marzban M.D ,et.al<br />
The 14th congress of<br />
Iranian Heart<br />
Association<br />
in collaboration with<br />
British Cardiac Society,<br />
Tehran, 2004<br />
131
ROW<br />
10<br />
TITLE<br />
Treatment of mitral<br />
regurgitation and <strong>coronary</strong><br />
disease by <strong>coronary</strong> <strong>bypass</strong><br />
alone<br />
Prsented by:<br />
Sadeghian .H.<br />
M.D,et.al<br />
Congress<br />
The 14th congress of<br />
Iranian Heart<br />
Association<br />
in collaboration with<br />
British Cardiac ociety,<br />
Tehran, 2004<br />
Page<br />
132<br />
11<br />
Chronic total occlusion of<br />
left main <strong>coronary</strong> <strong>artery</strong>: a<br />
case series<br />
Marzban M.D ,et.al<br />
The 14th congress of<br />
Iranian Heart<br />
Association<br />
in collaboration<br />
with British Cardiac<br />
Society, Tehran, 2004<br />
133<br />
12<br />
Results of CABG<br />
concomitant with mitral<br />
valve replacement versus<br />
repair in patients with<br />
moderate to severe mitral<br />
regurgitation accompanying<br />
<strong>coronary</strong> <strong>artery</strong> disease<br />
Sadeghian .H. M.D<br />
,et.al<br />
The 14th congress of<br />
Iranian Heart<br />
Association<br />
in collaboration with<br />
British Cardiac Society,<br />
Tehran, 2004<br />
134<br />
13<br />
Effects of oral entoxifylline<br />
in cardiopulmonary <strong>bypass</strong><br />
surgeries<br />
Abbasi M.D ,et.al<br />
The 14th congress of<br />
Iranian Heart<br />
Association<br />
in collaboration with<br />
British Cardiac ociety,<br />
Tehran, 2004<br />
135
ROW<br />
14<br />
TITLE<br />
Evaluation of risk factors for<br />
CAD in young patients<br />
undergoing CABG<br />
Prsented by:<br />
Davoodi<br />
M.D,et.al<br />
Congress<br />
The 14th congress of<br />
Iranian Heart<br />
Association<br />
in collaboration with<br />
British Cardiac Society,<br />
Tehran, 2004<br />
Page<br />
136<br />
15<br />
Preoperative screening for<br />
carotid <strong>artery</strong> stenosis in<br />
patients who underwent<br />
cardiac <strong>surgery</strong><br />
Abbasi M.D ,et.al<br />
The 14th congress of<br />
Iranian Heart<br />
Association<br />
in collaboration with<br />
British Cardiac Society,<br />
Tehran, 2004<br />
137<br />
16<br />
Analysis of effective factors<br />
on mortality of CABG<br />
patients in hospital<br />
Sadeghian .H M.D,<br />
et.al<br />
The 14th congress of<br />
Iranian Heart<br />
Association<br />
in collaboration with<br />
British Cardiac Society,<br />
Tehran, 2004<br />
138<br />
17<br />
Long term evaluation of<br />
laser-treated silicone(lts)<br />
membrane as a ericardial<br />
substitute: An xperimental<br />
study<br />
Ahmadi M.D et.al<br />
The 14th congress of<br />
Iranian Heart<br />
Association<br />
in collaboration with<br />
British Cardiac<br />
Society,Tehran, 2004<br />
139
ROW<br />
18<br />
TITLE<br />
Autologus bone marrow<br />
stem cell transplantation for<br />
myocardial regeneration<br />
Prsented by:<br />
Ahmadi M.D, et.al<br />
Congress<br />
The 14th congress of<br />
Iranian Heart<br />
Association<br />
in collaboration with<br />
British Cardiac Society,<br />
Tehran, 2004<br />
Page<br />
140<br />
19<br />
Rest and stress<br />
echocardiography evaluation<br />
of patients with AVR for<br />
estimation of mismatch<br />
between effective orifice<br />
area<br />
and body surface area<br />
Sadeghian H M.D et.l<br />
The 14th congress of<br />
Iranian Heart<br />
Association<br />
in collaboration with<br />
British Cardiac Society,<br />
Tehran, 2004<br />
141<br />
20<br />
Relation between age<br />
and sex of CABG patients<br />
and kind and number of risk<br />
factors<br />
Sadeghian H M.D et.l<br />
The 14th congress<br />
Of Iranian Heart<br />
Association<br />
in collaboration with<br />
British Cardiac Society,<br />
Tehran, 2004<br />
142<br />
21<br />
Early results and 12 months<br />
follow-up of PTMC<br />
Salarifar M.D , et.al<br />
The 14th congress of<br />
Iranian Heart<br />
Association<br />
in collaboration with<br />
British Cardiac Society,<br />
Tehran, 2004<br />
143<br />
22<br />
Prevalence of left main<br />
<strong>coronary</strong> <strong>artery</strong> disease and<br />
the effective risk factors on<br />
its development<br />
Karimi M.D ,et.al<br />
The 14th congress of<br />
Iranian Heart<br />
Association<br />
in collaboration with<br />
British Cardiac Society,<br />
Tehran, 2004<br />
144
ROW<br />
23<br />
TITLE<br />
Effect of antioxidants on<br />
reducing the damaging effect<br />
of cardiopulmonary <strong>bypass</strong>:<br />
a clinical study<br />
Prsented by:<br />
Marzban M.D,et.al<br />
Congress<br />
The 14th congress of<br />
Iranian Heart<br />
Association<br />
in collaboration with<br />
British Cardiac Society,<br />
Tehran, 2004<br />
Page<br />
145<br />
24<br />
Cardiac resynchronization<br />
therapy (CRT) in patients<br />
with severe heart failure.<br />
Could MRI predict the<br />
results of CRT<br />
Yamini sharif M.D<br />
et.al<br />
The 14th congress of<br />
Iranian Heart<br />
Association<br />
in collaboration with<br />
British Cardiac Society,<br />
Tehran, 2004<br />
146<br />
25<br />
High-dose Heparin to<br />
prevent deep venous<br />
thrombosis in slow pathway<br />
ablation<br />
Yamini sharif M.D<br />
,et.al<br />
The 14th congress of<br />
Iranian Heart<br />
Association<br />
in collaboration with<br />
British Cardiac<br />
Society,Tehran, 2004<br />
147<br />
26<br />
How safe or feasible is post-<br />
CABG PCI<br />
Kazemi saleh M.D<br />
et.al<br />
The 14th congress of<br />
Iranian Heart<br />
Association<br />
in collaboration with<br />
British Cardiac<br />
Society,Tehran, 2004<br />
148<br />
27<br />
A report of first fractional<br />
flow reserve(FFR)<br />
measurements in Iran<br />
Kassaian M.D,et.al<br />
The 14th congress of<br />
Iranian Heart<br />
Association<br />
in collaboration with<br />
British Cardiac<br />
Society,Tehran, 2004<br />
149
ROW<br />
28<br />
TITLE<br />
Implication of small<br />
reference vessel diameter in<br />
patients undergoing<br />
percutaneous <strong>coronary</strong><br />
revascularization<br />
Prsented by:<br />
Ali doosti M.D,et.al<br />
Congress<br />
The 14th congress of<br />
Iranian Heart<br />
Association<br />
in collaboration with<br />
British Cardiac<br />
Society,Tehran, 2004<br />
Page<br />
150<br />
29<br />
Elevated serum<br />
lipoprotein(a) is a risk<br />
factor for left atrial thrombus<br />
in patients with chronic<br />
atrial fibrillation<br />
Kazemi saied M.D<br />
,et.al<br />
The 14th congress of<br />
Iranian Heart<br />
Association<br />
in collaboration with<br />
British Cardiac Society,<br />
Tehran, 2004<br />
151<br />
30<br />
Correlation between blood<br />
groups, <strong>coronary</strong> <strong>artery</strong><br />
disease risk factors and CAD<br />
Amir zadegan M.D<br />
et.al<br />
The 14th congress of<br />
Iranian Heart<br />
Association<br />
in collaboration with<br />
British Cardiac Society,<br />
Tehran, 2004<br />
152<br />
31<br />
Stem cell transplantation in<br />
patients with acute<br />
myocardial infarction; a<br />
single center registry<br />
Salarifar M.D ,et.al<br />
The 14th congress of<br />
Iranian Heart<br />
Association<br />
in collaboration with<br />
British Cardiac<br />
Society,Tehran, 2004<br />
153<br />
32<br />
Short-term results of renal<br />
<strong>artery</strong> ngioplasty(stenting)<br />
on blood pressure and serum<br />
creatinine<br />
Haji zeinali M.D et.al<br />
The 14th congress of<br />
Iranian Heart<br />
Association<br />
in collaboration with<br />
British Cardiac<br />
Society,Tehran, 2004<br />
154
ROW<br />
33<br />
TITLE<br />
Outcome of primary<br />
percutaneous <strong>coronary</strong><br />
intervention in acute<br />
myocardial infarction<br />
Prsented by:<br />
Ali doosti M.D ,et.al<br />
Congress<br />
The 14th congress of<br />
Iranian Heart<br />
Association<br />
in collaboration with<br />
British Cardiac<br />
Society,Tehran, 2004<br />
Page<br />
155<br />
34<br />
Comparing success rate,<br />
complications and late<br />
outcome in <strong>coronary</strong><br />
intervention for total and<br />
non-total occlusion<br />
Kazemi saleh M.D<br />
et.al<br />
The 14th congress of<br />
Iranian Heart<br />
Association<br />
in collaboration with<br />
British Cardiac<br />
Society,Tehran, 2004<br />
156<br />
35<br />
Slow pathway ablation with<br />
no <strong>coronary</strong> sinus and His<br />
bundle catheters-Is it safe<br />
Yamine sharif M.D<br />
et.al<br />
The 14th congress of<br />
Iranian Heart<br />
Association<br />
in collaboration with<br />
British Cardiac<br />
Society,Tehran, 2004<br />
157<br />
36<br />
37<br />
Relation between the<br />
number of involved <strong>coronary</strong><br />
arteries<br />
in patients and the kind and<br />
multiplicity of risk factors<br />
Angiographic findings in<br />
401 very premature CAD<br />
patients(age
ROW<br />
38<br />
TITLE<br />
Analysis of the patency of<br />
<strong>coronary</strong> arteries in<br />
Heberkinase treatment<br />
Prsented by:<br />
Sadeghian M.D ,et.al<br />
Congress<br />
The 14th congress of<br />
Iranian Heart<br />
Association<br />
in collaboration with<br />
British Cardiac Society,<br />
Tehran, 2004<br />
Page<br />
160<br />
39<br />
Short-term results of carotid<br />
<strong>artery</strong> stenting: A single<br />
center registry<br />
Kassaian M.D ,et.al<br />
The 14th congress of<br />
Iranian Heart<br />
Association<br />
in collaboration with<br />
British Cardiac<br />
Society,Tehran, 2004<br />
161<br />
40<br />
41<br />
Comparing background and<br />
confounding factors in the<br />
mace and non-mace patients;<br />
late outcome assessment of<br />
PCI<br />
Comparison of in-hospital<br />
and 9-month outcomes in<br />
patients with significant left<br />
ventricular dysfunction<br />
having percutaneous<br />
<strong>coronary</strong> intervention<br />
Salari far M.D, et.al<br />
Ali doosti M.D et.al<br />
The 14th congress of<br />
Iranian Heart<br />
Association<br />
in collaboration with<br />
British Cardiac Society,<br />
Tehran, 2004<br />
The 14th congress of<br />
Iranian Heart<br />
Association<br />
in collaboration with<br />
British Cardiac Society,<br />
Tehran, 2004<br />
162<br />
163<br />
42<br />
American or Europeanbased<br />
Bare stent: Which one<br />
is preferred<br />
Kassaian M.D, et.al<br />
The 14th congress of<br />
Iranian Heart<br />
Association<br />
in collaboration with<br />
British Cardiac Society,<br />
Tehran, 2004<br />
164
ROW<br />
43<br />
TITLE<br />
Short and long-term results<br />
after multi-vessel PCI<br />
Prsented by:<br />
Kassaian M.D, et.al<br />
Congress<br />
The 14th congress of<br />
Iranian Heart<br />
Association<br />
in collaboration with<br />
British Cardiac Society,<br />
Tehran, 2004<br />
Page<br />
165<br />
44<br />
45<br />
Short and long-term<br />
outcomes after PCI in<br />
patients with acute <strong>coronary</strong><br />
syndrome<br />
Are there any differences in<br />
mortality, complications,<br />
and late outcomes of PCI in<br />
patients with different<br />
educational levels<br />
Kassaian M.D, et.al<br />
Kazemi saleh M.D<br />
,et.al<br />
The 14th congress of<br />
Iranian Heart<br />
Association<br />
in collaboration with<br />
British Cardiac<br />
Society,Tehran, 2004<br />
The 14th congress of<br />
Iranian Heart<br />
Association in<br />
collaboration with<br />
British Cardiac Society,<br />
Tehran, 2004<br />
167<br />
166<br />
46<br />
Biopump as a temporary<br />
assist device for post<br />
cardiotomy heart failure<br />
Davoodi M.D, et.al<br />
The 14th congress of<br />
Iranian Heart<br />
Association<br />
in collaboration with<br />
British Cardiac<br />
Society,Tehran, 2004<br />
168<br />
47<br />
Effect of body mass index<br />
on in-hospital mortality in<br />
<strong>coronary</strong> <strong>artery</strong> <strong>bypass</strong><br />
<strong>surgery</strong><br />
Marzban M.D, et.al<br />
The 14th congress of<br />
Iranian Heart<br />
Association<br />
in collaboration with<br />
British Cardiac<br />
Society,Tehran, 2004<br />
169
ROW<br />
48<br />
TITLE<br />
Study of the rate of CAD<br />
patients without risk factors<br />
Prsented by:<br />
Sadeghian M.D, et.al<br />
Congress<br />
The 14th congress of<br />
Iranian Heart<br />
Association<br />
in collaboration with<br />
British Cardiac Society,<br />
Tehran, 2004<br />
Page<br />
170<br />
49<br />
Developmental ultrastructure<br />
of mouse emberyonic stem<br />
cell derived cardiomyocytes<br />
in vitro<br />
Baharvand M.D, et.al<br />
The 14th congress of<br />
Iranian Heart<br />
Association<br />
in collaboration with<br />
British Cardiac Society,<br />
Tehran, 2004<br />
171<br />
50<br />
Dose routine magnesium<br />
administration prevent<br />
preoperative <strong>coronary</strong> <strong>artery</strong><br />
<strong>bypass</strong> <strong>graft</strong> <strong>surgery</strong><br />
arrhythmias<br />
Najafi M.D ,et.al<br />
2nd international<br />
congress<br />
of anesthesiology&<br />
intensive care, Tehran,<br />
2005<br />
172<br />
51<br />
Furosmide administration in<br />
cardiac <strong>surgery</strong>: The best<br />
result with the least dosage<br />
Najafi M.D ,et.al<br />
2nd international<br />
congress of<br />
anesthesiology&<br />
intensive care, Tehran,<br />
2005<br />
173
First experience of local implantation of autologus CD 133+<br />
bone marrow stem cell transplantation for myocardial<br />
regeneration in a developing country<br />
Ahmadi H, Baharvand H, Kazemi Ashtiani S, Ardakani, Salehi Omran M,<br />
Sadeghian H, Madjd Ardakani J, Marzban M, Zareh N, Kohkan A, Madani-Civi<br />
M, Namiri M and Kamangari A<br />
Tehran Heart Center, Medical Sciences/University of Tehran, Tehran, Iran<br />
Abstract<br />
Background: Experimental studies suggest that autologous bone marrow stem cell<br />
transplantation (CD 133+) in patients with myocardial infarction (MI) may improve<br />
cardiac function. The aim of this study was to assess feasibility, safety of this therapy and<br />
cardiac performance as well.<br />
Methods: Between June 2004- June 2005, 21 patients with history of acute myocardial<br />
infarction within 3 months who were candidate for <strong>coronary</strong> <strong>artery</strong> <strong>bypass</strong> <strong>graft</strong>ing<br />
(CABG), were entered in our study. The patients randomly divided into two groups;<br />
control group (n=9, CABG alone) and BMC group (n=20, CABG with intramyocardial<br />
injection of autologus CD133+ bone marrow stem cell in the infracted border zone). For<br />
all patients, dobutamine stress echo (DSE) and thallium scan were performed before, 3<br />
and 9 months after CABG to determine perfusion and viability of the heart.<br />
Results: There were no significant differences between demographic factors of two<br />
groups. Left ventricular ejection fraction (LVEF) improved from 34.3r1.5 to 38r1.3 % in<br />
case group (p
Magnesium infusion and its relationship with the incidence of<br />
post <strong>coronary</strong> <strong>artery</strong> <strong>bypass</strong> <strong>graft</strong>ing arrhy thmias<br />
Najafi M, Haghighat B, Ahmadi H, Salehi Omran A, Soltaninia H, Ghiasi A,<br />
Boroomand MA, Fallah N, Fayazzadeh E, Ahmadi M and Mojtahed M<br />
Tehran Heart Center, Medical Sciences/University of Tehran, Tehran, Iran<br />
Abstract<br />
Background: Atrial and ventricular arrhythmias are among the most common<br />
complications following <strong>coronary</strong> <strong>artery</strong> <strong>bypass</strong> <strong>graft</strong>ing (CABG). Previous studies have<br />
demonstrated that serum magnesium (Mg) levels decreases following CABG, specially<br />
after cardiopulmonary <strong>bypass</strong> (CPB). In current study, we evaluated the prophylactic<br />
effect of Mg infusion on post-CABG arrhythmias.<br />
Methods: 345 patients (113 diabetic; 229 non-diabetic), candidates for isolated<br />
<strong>coronary</strong> <strong>artery</strong> <strong>bypass</strong> <strong>graft</strong>ing (CABG) with normal renal function, were randomly<br />
divided into two groups. Group A (case; 48.1%) received 2 g of Mg from induction of<br />
anesthesia to cardiopulmonary <strong>bypass</strong> (CPB) beginning and 8 g following CPB to 24 h<br />
there after. In group B (control; 51.9%), no supplemental Mg was administered. Mg<br />
serum levels were measured in all patients four times (at the onset of induction, and hours<br />
0, 24, and 48 after ICU admission). Patients were then followed for developing cardiac<br />
arrhythmias until their discharge from the hospital.<br />
Results: 79 patients (22.9%) developed post-operative arrhythmias (i.e. AF in 34<br />
[9.9%]; other supraventricular arrhythmias in 23 [6.7%]); and ventricular arrhythmias in<br />
47[13.6%] patients).Except for the first occasion (induction time), there were significant<br />
statistical differences in Mg serum levels in subsequent three measurements (p
Diabetes mellitus role in impeding prophylactic effects of<br />
magnesium on post<strong>coronary</strong> <strong>artery</strong> <strong>bypass</strong> <strong>graft</strong>ing atrial<br />
fibrillation<br />
Najafi M and Salehi Omran A<br />
Tehran Heart Center, Medical Sciences/University of Tehran, Tehran, Iran<br />
Abstract<br />
Background: Hypomagnesemia is a well known issue in diabetics. Recent studies have<br />
suggested the promising role of supplemental magnesium (Mg) administration in<br />
preventing post-surgical atrial fibrillation (AF); however, there is no evidence on<br />
differences between diabetic and non-diabetic patients in response to prophylactic<br />
administration of Mg supplements.<br />
Methods: Three hundred forty-five patients (115 diabetic; 230 non-diabetic), candidates<br />
for isolated <strong>coronary</strong> <strong>artery</strong> <strong>bypass</strong> <strong>graft</strong>ing (CABG) with normal renal function, were<br />
randomly divided into two groups. Group A (case; 48.1%) received 2 g of Mg after<br />
induction of anesthesia until cardiopulmonary <strong>bypass</strong> (CPB) onset and 8 g following CPB<br />
to 24 h thereafter. In group B (control; 51.9%), no supplemental Mg was administered.<br />
Mg serum levels was measured in all the patients four times (at the onset of induction,<br />
and hours 0, 24, and 48 after ICU admission).Patients were then followed for developing<br />
AF after the end of <strong>surgery</strong> until their discharge.<br />
Results: Thirty-four patients (9.9%) developed AF: 12 in group A and 22 in group B.<br />
Of 12 patients in group A, 8 (67%) were diabetic, whereas there were just 6 diabetic ones<br />
(27.3%) in group B (p=0.026). Serum Mg level were not statistically different between<br />
the groups. There was no significant difference statistically for the rate of DM in nonarrhythmic<br />
patients between the two groups (31% in group A vs. 34% in group B).<br />
Conclusions: DM has a major role in impeding prophylactic effects of Mg infusion on<br />
developing AF. This effect has no correlation with perioperative serum Mg levels.<br />
Keywords: magnesium, diabetes mellitus, atrial fibrillation<br />
5
Correlation between total plasma homocysteine level and<br />
grading of <strong>coronary</strong> <strong>artery</strong> disease<br />
Mirhoseini J, Radmehr H, Ahmadi H, Salehi M, Sattarzadeh R and Sanatkar M<br />
Tehran Heart Center, Medical Sciences/University of Tehran, Tehran, Iran<br />
Abstract<br />
Background: Elevated total plasma homocystein (tHcy) levels constitute a risk factor<br />
for <strong>coronary</strong> <strong>artery</strong> disease (CAD). A possible relationship was investigated between<br />
admission plasma homocystein level and the angiographic severity and extension of<br />
<strong>coronary</strong> <strong>artery</strong> disease in patients with CAD. This study looks at the relationship<br />
between total plasma homocystein and severity of <strong>coronary</strong> <strong>artery</strong> disease.<br />
Methods: From April 2004 to December 2004, 100 consecutive patients (65male 35<br />
female) that referred to our institution for <strong>coronary</strong> <strong>artery</strong> <strong>bypass</strong> <strong>graft</strong> <strong>surgery</strong> were<br />
enrolled. Fasting blood samples for homocystein were obtained on admission. Plasma<br />
homocystein concentration was measured with high performance liquid chromatography<br />
(HPLC). Our patients presented in Group with homocystein level >12 micromoles per<br />
liter and Group with total plasma homocystein =< 12 micromoles per liter. Vessel score<br />
assessed the number of vessels with significant stenosis … grading of atherosclerosis<br />
(Extent score) was intended to the atherosclerotic involvement of the entire arterial length<br />
circumscribe.<br />
Results: Our study was shown age > 60 years was correlated with tHcy, but gender,<br />
hypertension, history of smoking, hypercholesterolemia, family history and diabetes<br />
mellitus have not statistically difference between two groups. A poor correlation was<br />
found between abnormal homocystein level and vessel score ( r=0.35; p
Various surgical approaches to porcelain aorta in <strong>coronary</strong><br />
<strong>artery</strong> <strong>bypass</strong> <strong>graft</strong>ing (CABG), a single institute experience<br />
Marzban M, Abbasi K, Karimi A, Ahmadi H, Davoodi S, Movahedi N,<br />
Salehiomran A, Abbasi SH, Madani M and Rahnamayeazar A<br />
Tehran Heart Center, Medical Sciences/University of Tehran, Tehran, Iran<br />
Abstract<br />
Background: A heavily calcified aorta (the so called porceian aorta) is still a<br />
challenging dilemma for the surgeons with respect to <strong>bypass</strong> techniques, choice of<br />
conduit and handling of diseased aorta. In this article we present our experiences in<br />
management of eight patients.<br />
Methods: In 8 cases candidated for elective isolated CABG or in combined with aortic<br />
valve replacement we encountered porcelain aorta. Their management strategies include:<br />
1. off pump CABG as anastamosa of left internal mammary <strong>artery</strong> (LIMA) to the left<br />
anterior descending <strong>artery</strong> (LAD) and a jump SCG <strong>graft</strong> from proximal right <strong>coronary</strong><br />
<strong>artery</strong> (RCA) to the distal part.2. off pump CABG as Saphenus vein <strong>graft</strong> from proximal<br />
of innominate <strong>artery</strong> to LAD & from the SVG to OM, RCA and diagal branch.3. insertion<br />
of aortic valve in supra <strong>coronary</strong> position and anastomosis of LIMA to LAD and SVG to<br />
OM, RCA with proximal anastomosis to innaminate <strong>artery</strong>.4.and 5. aortic root<br />
replacement + CABG 6. hemiarch arch+root replacement + CABG.7. off pump CABG<br />
sequential LIMA to LAD and diagonal, RIMA to RCA radial to OM 1 and proximal of<br />
radial <strong>artery</strong> to the side of LIMA.8. off pump CABG as sequential LIMA to LAD and<br />
diagonal, RIMA to RCA.<br />
Results: The post operative course was uneventful in all patient no patient experienced<br />
a cerebrovascular accident or visceral organ injury as a result of atheroembolism.<br />
Conclusion: Although porcelin aorta is a difficult & cumbersome situation for CABG<br />
but with using different management strategies including offpump and no touch<br />
techniques of atherosclerotic aorta it can be managed <strong>graft</strong>ing results.<br />
7
Comparative outcome of CABG in diabetic patients versus<br />
non-diabetics with poor left ventricular function<br />
Ahmadi SH, Karimi AA, Davoodi S, Marzban M, Abbasi K, Movahedi N,<br />
Soleimani A, Abbasi SH, Alinejad B, Najafi M, Rahnemayeazar A and Fallah N<br />
Abstract<br />
Background: Although diabetes is commonly regarded as a risk factor for mortality<br />
and morbidity after CABG, the relationship between diabetes and mortality of CABG<br />
among patients with severe left ventricular dysfunction is less certain. This study was<br />
designed to assess this relationship.<br />
Methods: Between February 2002 and January 2006, 11197 CABG were done at our<br />
center, 1178 of those operations were isolated <strong>coronary</strong> <strong>artery</strong> <strong>bypass</strong> on patients with<br />
severe low ejection fraction. Of these 1178 patients, 434 patients had diabetes and 744<br />
patients were non-diabetics. We compared the diabetic and non-diabetic patients in this<br />
group in regard to gender, age, cerebrovascular accident, renal dysfunction, chronic<br />
pulmonary disease, significant left main <strong>coronary</strong> <strong>artery</strong> stenosis and postoperative inhospital<br />
mortality and morbidity. To analyze these data, univariate and multivariate<br />
analysis were done to compare the results.<br />
Results: Diabetic patients were older (59.55 y vs. 55.94 y), included more women<br />
(25.1% vs. 11.7%) and had more renal failure (4.1% vs. 2.2%), prolonged ventilation<br />
(2.6% vs. 0.9%), in-hospital mortality (4.6% vs. 1.9%) in comparison with non-diabetic<br />
patients (p
Pentoxifylline improves reoxygenation-induced contractile<br />
recovery through a nitric oxide dependent mechanism in rat<br />
papillary muscles<br />
Dehpour AR, Ebrahimi F, Hajrasouliha AR , S Tavakoli, Sadeghipour H, Ghasemi<br />
M, Ahmadi SH and Ziabakhsh Sh<br />
Mazandaran Heart Center, Sari, Iran.<br />
Tehran Heart Center, Medical Sciences/University of Tehran, Tehran, Iran<br />
Abstarct<br />
Background: In this study, the protective effect of pentoxifylline against hypoxiareoxygenation<br />
injury and the possible involvement of nitric oxide (NO)-mediated<br />
pathways in this protection were investigated in isolated rat papillary muscles.<br />
Methods: Papillary muscles were excised and isolated in Krebs-Henseleit solution<br />
aerated with 95% O2 and 5% CO2. Hypoxia was simulated by substituting O2 with<br />
argon. Three sets of experiments, testing 30, 60, and 90 min of hypoxia, were performed.<br />
The effects of different pentoxifylline concentrations on papillary muscle contractile<br />
parameters and responsiveness to isoproterenol were assessed. To investigate the role of<br />
NO, N(omega)-nitro-L-arginine methyl ester was added before pentoxifylline treatment.<br />
Results: Pentoxifylline did not show any inotropic effect on papillary muscles. Hypoxia<br />
caused a profound depression of contractile parameters, which was not affected by<br />
pentoxifylline treatment. Reoxygenation resulted in significant partial recovery of<br />
contractile parameters after 30 and 60 but not 90 min of hypoxia. In experiments with 30<br />
and 60 min of hypoxia, reoxygenation-induced contractile recovery and responsiveness to<br />
isoproterenol were improved by pentoxifylline in a concentration-dependent fashion.<br />
These functional improvements were completely blocked by N(omega)-nitro-L-arginine<br />
methyl ester pretreatment. No improvement was observed in 90-min hypoxia experiment.<br />
Conclusion: In conclusion, pentoxifylline improved contractile recovery during<br />
reoxygenation and postreoxygenation responsiveness to beta-adrenergic stimulation<br />
through the NO-dependent mechanism.<br />
9
Experience with 36 transvenous <strong>coronary</strong> sinus lead implantation for<br />
cardiac resynchronization therapy<br />
Yamini Sharif A, Kazemi Saeed A, Davoudi G, Sadegian S and Abbassi k<br />
Tehran Heart Center, Medical Sciences/University of Tehran, Tehran, Iran<br />
Abstract<br />
Background: Cardiac resynchronization therapy (CRT) using <strong>coronary</strong> sinus (CS)<br />
leads is a new method for the therapy of congestive heart failure (CHF) in case of inter<br />
and intraventricular conduction delay. Because the intervention is more complex than<br />
regular pacemaker implantation, more information on the feasibility of this intervention<br />
are of interest.<br />
Methods: From 09-08-2003 to 12-07-2005, 36 transvenous <strong>coronary</strong> sinus lead<br />
implantation was performed in 36 patients (mean age 57.53±11.33 years) (19-37 years<br />
spectrum) with EF 20.03±5.43%. The leads were preshaped and over the wire.<br />
Perioperative data were analyzed retrospectively. Twenty eight patients with LBBB (78<br />
%), 5 patients with RBBB (14%) and 2 patients with IVCD intraventricular conduction<br />
delay in ECG. All the patients had wide QRS in ECG•130 mmsec except one case with<br />
narrow QRS but intraventricular delay in TDI (tissue Doppler imaging). In 10 cases<br />
CRT+D were implanted in the others pure 3 chamber pace maker. Eleven patients (30%)<br />
had history of CABG. All the patients NYHA FC were 3 or 4. Seventy five percent were<br />
impalanted from right subclavian vein the others from left side. Coronary sinus leads<br />
were positioned according to variable vein anatomies 16x lateral 8x anterolateral 5x<br />
posterolateral 2x anterior.<br />
Results:In 5 patients CS lead implantation were unsuccessful transvenously. So<br />
epicardial LV leads were implanted because in 3 cases there were no suitable vein for CS<br />
lead implantation and in 2 cases <strong>coronary</strong> sinus perforation occurred. CS dissection<br />
occurred in 3 patients. In 7 casese phrenic nerve or diaphragmatic stimulation occurred<br />
during implantation, we solved this problem with repositoning of CS lead into other vein<br />
or by decreasing the threshold to minimum acceptable threshold. The mean operation<br />
time was 127±33 minutes (min) mean fluoroscopy time 35.5±19.3 min. Mean CS<br />
cannulation time 12.5±10.2 min and mean positioning time for lead 14±8 min in 29<br />
patients. Eighty percent showed an improvement in their NYHA class and could be<br />
classified as responder.<br />
Conclusion: Coronary sinus lead implantation is complex procedure with some hazard.<br />
Procedure time, fluoroscopy time and complication rate is noticeable therefore CRT<br />
should be offered to otherwise untreatable CHF patients NYHA class 3 or 4. At persent<br />
time, it is questionable to recommend CRT for CHF patient with mild symptom (NYHA<br />
class2). According to our experiences and reports from some other centers, it is not our<br />
policy to recommend CRT for patients with CHF and mild symptoms (NYHA class2).<br />
10
Mid term follow up of sixty patients with implantable<br />
cardioverter defibrillator<br />
Yamini Sharif A, Kazemi Saeed A, Davoudi Gh, Sadegian S and Moughaddam M<br />
Tehran Heart Center, Medical Sciences/University of Tehran, Tehran, Iran<br />
Abstract<br />
Background: This study assessed the results of ICD implantation in 60 patients with<br />
different etiology, age, ejection fraction and different venous access.<br />
Methods: From May 2002 to July 2005 60 ICDs were implanted in 60 patients who<br />
need to have ICD for secondary or primary prevention (except MADITII inclusion<br />
criteria). Their age were between (16 to 79years) mean 51±16 years (13% over 70 years).<br />
Follow up period was between (1 month to 38 months) mean 18±7 months. 75% of<br />
patients were male. EF in 22% of patients was 30-50% in 41%,
6 th biennial international conference of Pakistan society of cardiovascular & thoracic<br />
surgeons, Dec 2006, Karachi<br />
Induced myocardial infarction using ligation of the left<br />
anterior descending <strong>coronary</strong> <strong>artery</strong> major diagonal branch:<br />
development of an ovine model<br />
Rabbani Sh<br />
Tehran Heart Center, Medical Sciences/University of Tehran, Tehran, Iran<br />
Abstract<br />
Background: we report experimental myocardial infarction by occluding <strong>coronary</strong><br />
arteries in ovine models.<br />
Methods: Twelve ewes were included in the study. After the chest was opened by left<br />
lateral thoracotomy incision, the second diagonal branch of the left anterior descending<br />
<strong>coronary</strong> <strong>artery</strong> was ligted at a point approximately 40% distant from its base.<br />
Prophylactic antiarrhythmics were administered. Animals were mechanically ventilated<br />
during <strong>surgery</strong> and stayed at ICU for 24h afterwards. Experiments were then evaluated by<br />
echocardiographic, electrocardiographic, hemodynamic, serologic and morphologic<br />
investigations. Echocardiographic measurements were repeated after two months and<br />
animals were then sacrificed for postmortem cardiac examinations.<br />
Results: All animals survived the surgical procedure. Cyanotic discoloration and<br />
hypokinesia in the cardiac tissue in an area of 3*4 cm plus ST-segment elevations was<br />
detected immediately after vessel ligation. More over, there were pathologic Q-waves 2<br />
months later. Echocardiographic evaluations revealed an average of 30% relative<br />
decrease in cardiac ejection fraction. Wall motion analysis demonstrated anteroapical<br />
hypokinesia and akinesia in all animals one day and two months after operation. Thin<br />
walled infracted areas with tissue fibrosis were evident in pathologic investigations two<br />
months after <strong>surgery</strong>.<br />
Conclusion: In conclusion, we developed a practical and safe method of producing<br />
myocardial infarction in large animal models.<br />
12
First experience of local implantation of autologus CD 133+<br />
bone marrow stem cell transplantation for myocardial<br />
regeneration in Iran<br />
Ahmadi H, Baharvand H, Kazemi Ashtiani S, Soleimani M, Sadeghian H, Majd<br />
Ardekani J, Marzban M, Zareh N, Kouhkan A, Madani-Civi M, Namiri M and<br />
Kamangari A<br />
Tehran Heart Center, Medical Sciences/University of Tehran, Tehran, Iran Royan institute, stem cell<br />
department, tehran, Iran.<br />
Abstract<br />
Background: Experimental studies suggest that autologus bone marrow stem cell<br />
transplantation (CD 133+) in patients with myocardial infarction (MI) may improve<br />
cardiac function. The aim of this study was to assess feasibility, safety of this therapy and<br />
cardiac performance as well.<br />
Methods: Between June 2004 - June 2005, 29 patients with history of acute myocardial<br />
infarction within 3 months who were candidate for <strong>coronary</strong> <strong>artery</strong> <strong>bypass</strong> <strong>graft</strong>ing<br />
(CABG), were entered in our study. The patients randomly divided into groups: control<br />
group (n=9, CABG alone) and BMC group (n=20, CABG with intramyocardial injection<br />
of autologus CD 133+ bone marrow stem cell in the infracted border zone). For all<br />
patients, dobutamine stress echo and thallium scan was performed before, 3 and 9 months<br />
after CABG to determine improvement in regional viability and contractility of the heart.<br />
Results: There were no significant differences between demographic factors of two<br />
groups. Thallium scan and echocardiography reinvestigation showed improvement in<br />
global LV function, regional wall motion and perfusion of infracted area. Left ventricular<br />
ejection fraction (LVEF) improved from 34.3r1.5 to 38r1.3 in BMC group (p
PCL scaffold <strong>graft</strong>ed onto infarcted myocardium in sheep<br />
animal model: a vehicle for cardiomyocytes<br />
Soleimani M, Ahmadi SH, Rabbani Sh, Fayazzadeh E, Sahebjam M, Ahmadi ZH,<br />
Forozannia , Broumand MA, Sotudeh M, Karimi AA, Marzban M, Movahedi N,<br />
Abbasi K and Sadeghian S<br />
Experimental research lab, Tehran Heart Center, Medical Sciences/University of Tehran, Tehran, Iran<br />
Abstract<br />
Background: The emerging fields of tissue engineering and biomaterials have begun to<br />
provide potential treatment of cardiac infarcts. Tissue engineering approaches are<br />
designed to repair damaged cardiac tissue through the use of cellular transplantation, and<br />
biomaterial scaffolds.<br />
Methods: This study was designed to investigate the effectiveness of cardiomyocytesseeded<br />
patch <strong>graft</strong> on infracted area of the heart. MI in a sheep was induced by ligation of<br />
the distal portion of left <strong>coronary</strong> <strong>artery</strong>. A piece of left ventricular muscle and jugular<br />
vein were obtained. The samples were cultured and expanded. Expanded cardiomyocites<br />
and endothelial cells were seeded on 8 layers polycaprolactone material patches. After<br />
two months, the patch was sutured on the surface of infracted myocardium.<br />
Results: Eight weeks after patch transplantation, in echocardiography evaluation, there<br />
was no significant improvement in cardiac function; but in tissues evaluation by<br />
pathology and immunohistochemistry, a substantial amount of neovascularization and a<br />
tiny myogensis was seen in the infracted region and in the scaffold. There were no signs<br />
of acute inflammation.<br />
Conclusion: Our data demonstrate that <strong>graft</strong>ing of cell-seeded patch <strong>graft</strong> can induce<br />
angiogenesis and myogenesis in MI region. Such tissue engineered cell-sealed is the<br />
promising concept of tissue cardiomyoplasty to the field of regenerative medicine. This<br />
approach gives an overview of the current progress in the treatment of failing heart.<br />
14
Improvement of cardiac function and tissue viability following<br />
expanded autologus marrow derived CD133 stem cell<br />
transplantation in patients with ischemic cardiomyopathy<br />
undergoing <strong>coronary</strong> <strong>bypass</strong> <strong>surgery</strong><br />
Ahmadi SH, Soleimani M, Sahebjam M, Ahmadbeigi N, Madani-Civi M,<br />
Fayazzadeh E, Najafi M, Karimi AA, Abbasi K, Marzban M, Shirzad M and<br />
Forouzannian KH<br />
Tehran Heart Center, Medical Sciences/University of Tehran, Tehran, Iran<br />
Abstract<br />
Background: Ischemic cardiomyopathy comprises nearly two thirds of cases with<br />
heart failure. Coronary revascularization through surgical <strong>bypass</strong> <strong>graft</strong>ing is now a days<br />
routinely performed to improve life quality of such patients. Simultaneous transplantation<br />
of stem cells in patients undergoing CABG has been described in some recent studies<br />
with promising results. In present randomized controlled trail, we investigated short term<br />
efficiency of stem cell transplantation on cardiac function as an adjuvant to conventional<br />
CABG technique in patients with congestive heart failure.<br />
Methods: After institutional review and university approval, 20 patients with ischemic<br />
cardiomyopathy (NYHA class III or IV) and low ejection fraction (
There was also a meaningful relative decrease in percentage of the nonviable area on<br />
echocardiography and scintigraphy in patients in the stem cell group comparing to those<br />
in the control group.<br />
Conclusion: Expanded autologous CD133 stem cell transplantation led to significant<br />
improvement in cardiac function and tissue viability in patients undergoing CABG for<br />
16
Normal values for ventricular synchrony measured by tissue<br />
Doppler imaging and tissue Doppler synchronization imaging<br />
in structurally normal hearts<br />
Sadeghian H, Saheb Jam M, Yamini Sharif A, Kazemisaied A, Fallah N, Goodarzynejad<br />
H and Raissi Dehkordi M<br />
Tehran Heart Center, Medical Sciences/University of Tehran, Tehran, Iran<br />
Abstract<br />
Background: We studied normal values for intraventricular and interventricular delay<br />
by tissue Doppler imaging (TDI) and tissue synchronization imaging (TSI).<br />
Methods: We evaluated 25 healthy adults volunteers (26.30±5.68 years, 16% male).<br />
Tissue Doppler Echocardiography was performed (system VIVID 7D, GE) using a 6-<br />
basal, 6 mid-segmental model to assess the time to peak systolic contraction (Ts). We<br />
also evaluated the right ventricle at basal and mid portion levels. We measured Ts both<br />
manually and with TSI.<br />
Results: Anterior basal and mid-portion had the shortest Ts and interventricular septum<br />
had the longest Ts with both methods. Correlation between manual and TSI method was<br />
significant (p
Table 1. Ts in anterior septal and RV free wall<br />
Std. Deviation<br />
Mean<br />
Maximum<br />
Minimum<br />
29.39<br />
88.40<br />
200<br />
TDI:60<br />
Anterior basal<br />
10.25<br />
79.08<br />
103<br />
TSI: 61<br />
29.25<br />
9.01<br />
88.40<br />
77.28<br />
200<br />
98<br />
TDI: 60<br />
TSI: 61<br />
Anterior<br />
midportion<br />
47.26<br />
153.60<br />
210<br />
TDI: 24<br />
Septal basal<br />
39.88<br />
141.56<br />
216<br />
TSI: 78<br />
40.89<br />
37.09<br />
161.60<br />
125.40<br />
210<br />
216<br />
TDI: 80<br />
TSI: 82<br />
Septal<br />
midportion<br />
38.10<br />
181.20<br />
230<br />
TDI: 40<br />
RV basal<br />
24.26<br />
176.04<br />
228<br />
TSI: 129<br />
52.56<br />
20.89<br />
173.60<br />
175.12<br />
260<br />
217<br />
TDI: 12<br />
TSI:129<br />
RV<br />
midportion<br />
18
Clinical characteristics of women with premature <strong>coronary</strong> <strong>artery</strong><br />
disease requiring CABG compared with that of young men<br />
Daryani YP and Daryani YP<br />
Tehran Heart Center, Medical Sciences/University of Tehran, Tehran, Iran London, United Kingdom<br />
Abstract<br />
Background: Significant atherosclerotic CAD requiring CABG is uncommon in young<br />
adults and it is even rarer in young females. Here we present and compare detail<br />
characteristics of young female patients with premature CAD undergoing CABG with<br />
that of young male patients in Iran.<br />
Methods: In this study data from consecutive patients undergoing CABG only <strong>surgery</strong><br />
in a university affiliated tertiary referral centre in Tehran during twelve moths period<br />
were obtained. Premature CAD was defined as development of atherosclerotic CAD<br />
requiring <strong>bypass</strong> <strong>surgery</strong> before the age of 45 in men and before the age of 50 in women.<br />
Their characteristics including main CAD risk factors (smoking, DM, hypertension,<br />
hyperlipidemia, and family history), gender, BMI, creatinine levels, history of previous<br />
MI, angina, heart failure, and prior cardio-vascular intervention were assessed and<br />
compared. Standard criteria similar to those used by ACC/AHA were used to define the<br />
patient's characteristics. However in this study a family history of CAD in first degree<br />
relatives (both males and females) before the age of 55 was considered as positive.<br />
Categorical data were compared using Chi-squared and continuous data were compared<br />
using Student t test. P value
Impact of risk factors for development of <strong>coronary</strong> <strong>artery</strong><br />
disease in patients undergoing CABG in Iran compared with<br />
that in USA<br />
Daryani YP and Daryani YP<br />
Tehran Heart Center, Medical Sciences/University of Tehran, Tehran, Iran London, United Kingdom<br />
Abstract<br />
Background: CAD is the leading cause of death in the US and in Iran. Although it is<br />
suggested that the known risk factors for development of CAD is similar throughout the<br />
world their impact may be different among nations with different social and cultural<br />
background. Therefore different strategies may be required to tackle and prevent CAD in<br />
different countries.<br />
Methods: Here we present and compare clinical profiles of patients with CABG in Iran<br />
with those in the USA. Data for the US were obtained from Society of Thoracic Surgery<br />
National Database website, 1997 CABG only patients. Data for Iran were obtained from<br />
Cardiac Surgery Database of Tehran Heart Center, a university affiliated hospital.<br />
Patients were referred from all over the country to the centre. All consecutive patients<br />
undergoing CABG for established CAD between Oct 03 and Sep 04 had their data<br />
collected on standardized forms by a qualified physician. They were then entered into a<br />
computerized database.<br />
Results: Pt population 2,213 (1yr) Iran 174,806 (8yr) USA: Mean (median) age 58.6<br />
(59) 64.8(65), Male 74.7% 70.8%, Smoking HX 39.9% 58.3%, Family HX 25.2%<br />
46.6%, DM 29.3% 30.5%, hyperchol 55.6% 52.8%, Hypertension 37.1% 65.9% .<br />
Morbid obesity 1.0% 11.8%, CVA 2.1% 6.4%, PVD 1.0% 14.3%, 1VD 5.1% 9.5%,<br />
2VD 21.7% 20%, 3VD 73.2% 70.5%, LMD 11.2% 20.6%. Age 61-65 vs
We conclude that major risk factors of CAD have different impacts on development of<br />
CAD in different countries. Therefore different approaches are required to tackle and<br />
prevent CAD.<br />
21
Association of lipoprtein (a) levels with the severity of <strong>coronary</strong><br />
<strong>artery</strong> stenosis in an Iranian population (according to Gensini<br />
score)<br />
Tehran Heart Center, Medical Sciences/University of Tehran, Tehran, Iran<br />
Absract<br />
Background: Lipoprotein (a) [LP (a)] is a known risk factor for developing <strong>coronary</strong><br />
<strong>artery</strong> disease. However, the pattern of LP (a) distribution in various racial and genetic<br />
groups has been found to be different. Furthermore, the association of LP (a) and the<br />
severity of <strong>coronary</strong> <strong>artery</strong> disease in different populations has not been clearly assessed.<br />
This study has been done to determine the relationship between LP (a) and the severity of<br />
<strong>coronary</strong> <strong>artery</strong> stenosis in an Iranian population.<br />
Methods: Between July 2004 and March 2005, 826 patients who had been candidates<br />
for angiography at Tehran Heart Center were included. The severity of their <strong>coronary</strong><br />
<strong>artery</strong> stenosis was assessed through Gensini score. At the first part of the study, to check<br />
interobserver reliability, 60 angiographies were reported and their Gensini scores were<br />
determined by two cardiologists. During hospitalization, LP (a), triglyceride, cholesterol,<br />
high density lipoprotein, low density lipoprotein and quantitative C reactive protein levels<br />
were measured and their correlation with <strong>coronary</strong> <strong>artery</strong> stenosis were assessed.<br />
Results: Among 826 participants, 510 (62%) patients were male and 316 (38%) were<br />
female. Coronary angiography was normal in 283 (34%), while 543 (66%) patients<br />
showed atherosclerosis. Mean LP (a) levels in both normal and atherosclerotic<br />
participants showed a significant difference (P
Fast track method in cardiac <strong>surgery</strong>: evaluation of risks and<br />
benefits<br />
Najafi M, Soleimanzadeh M and Haghighat B<br />
Tehran Heart Center, Medical Sciences/University of Tehran, Tehran, Iran<br />
Abstract<br />
Background: Fast Track (FT) method is recommended for accelerating the recovery<br />
phase, but it may not work because of some respiratory complications. This study<br />
compares the routine and FT method for managing post CABG patients in Intensive<br />
Care Unit (ICU).<br />
Methods: One hundred cases were divided into two groups. In FT group, fentanyl<br />
(0.05-0.15 Pg/kg/min) and Propofol (10-50 Pg/kg/min) infusions were started since<br />
induction time. Atracurium infusion started one hour later, no bolus drug was<br />
administered during operation. Muscle relaxants were neutralized at the end of <strong>surgery</strong>.<br />
Fentanyl infusion continued up to 12 hours post <strong>surgery</strong>. The above two groups were<br />
evaluated for time of alertness and extubation in ICU, total analgesic dosage<br />
administered during 24 hours post operation, ABG and SpO2 pre-and post-extubation.<br />
Inclusion and exclusion criteria for FT method as well as extubation criteria were<br />
explained to the ICU, staff.<br />
Results: Time period between ICU admition and alertness was significantly different in<br />
FT (1.3 hour) and control group (3.3 hours) (P
Relationship between serum magnesium level and post<br />
<strong>coronary</strong> <strong>artery</strong> <strong>bypass</strong> <strong>graft</strong> <strong>surgery</strong> arrhythmias<br />
Najafi M<br />
Tehran Heart Center, Medical Sciences/University of Tehran, Tehran, Iran<br />
Abstract<br />
Background: Atrial and ventricular arrhythmias are among the most common<br />
complications after <strong>coronary</strong> <strong>artery</strong> <strong>bypass</strong> <strong>graft</strong> (CABG) <strong>surgery</strong>. Previous studies<br />
demonstrated that cardiopulmonary <strong>bypass</strong> itself, results in reduced serum magnesium<br />
level. In this study, we wanted to evaluate the effect of total blood magnesium level<br />
(TMG) on preventing perioperative arrhythmias by routine regimens of 2-4 grams<br />
supplemental magnesium (SMG).<br />
Methods: TMG was measured in patients who were scheduled for CABG on 3<br />
occasions [just before anesthesia, just after entering intensive care unit (ICU)<br />
postoperatively and on the first morning after operation]. Patients were evaluated for<br />
primary cardiac rhythm and other variables that could have an influence on magnesium<br />
level (serum creatinine, urine output in operating room and diuretic therapy). SMG was<br />
also recorded in operating room and ICU.Then the patients were evaluated for the rate<br />
and kind of arrhythmia through next 3 days.<br />
Results: Mean TMG level in 174 cases was 2.2 (0.5), 2.6 (0.6) and 2.4 (0.6) mg/dl on<br />
three occasions respectively. Mean SMG was 2.5 (1.2) grams. 47 out of 157 patients<br />
developed post-operative arrhythmia (%30) [AF* (%6.4), Non-AF SVA** (%14.6) and<br />
Ventricular arrhythmia (%16.6)]. Mean serum creatinine level and urine output were 1.2<br />
mg/dl and 1800ml respectively. Although there was a significant difference between<br />
TMG on three occasions (P
Carotid stenting in candidates for <strong>coronary</strong> <strong>artery</strong> <strong>bypass</strong><br />
<strong>surgery</strong>: results of a heart hospital registry<br />
Kassaian SE, Kazemisaleh D, Alidoosti M, Salarifar M, Haji Zeinali AM, Hakki<br />
E, Sahraian AM, Gheini MR and Abbasi SH<br />
Abstract<br />
Background: In patients with severe coexisting <strong>coronary</strong> and carotid <strong>artery</strong> disease, 2<br />
treatment strategies may be used: simultaneous endarterectomy and <strong>coronary</strong> <strong>bypass</strong><br />
<strong>surgery</strong> or carotid stenting with delayed <strong>coronary</strong> <strong>bypass</strong> <strong>surgery</strong> after a few weeks. We<br />
sought to evaluate the safety and efficacy of carotid stenting with delayed <strong>coronary</strong><br />
<strong>bypass</strong> <strong>surgery</strong> after a few weeks in patients of Tehran Heart Center. Based on<br />
observations made in this study and previous lesion typing studies, we aimed to<br />
determine predictors that may be used to select the appropriate treatment plan for such<br />
patients.<br />
Methods: Between December 2003 and October 2004, thirty consecutive patients<br />
underwent carotid stenting. The mean age of the patients was 66.3 ± 8 years. All of the<br />
patients had significant <strong>coronary</strong> <strong>artery</strong> disease. Symptomatic patients with>60% stenosis<br />
and symptomatic patients with> 80% stenosis were included. A complete neurological<br />
history was taken and an examination performed on all patients by an experienced<br />
neourologist. The study protocol required that an independent neourologist not involved<br />
in the interventional procedure evaluate parients using the National Institute of Health<br />
Stroke Scale before the procedure and then 24 hours, 1 month, and 6 months after the<br />
procedure. Carotid duplex (based on the Washington criteria), magnetic resonance<br />
imaging, or computed tomographyof the head and complete diagnostic angiography,<br />
including intracranial views and assessment of the collateral circulation, were performed<br />
on all patients. Stenoses were crossed with a 0.014inch filter wire, which was placed at<br />
the site of internal carotid <strong>artery</strong> distal to the lesion. In most cases, predilation (low<br />
profile 3.5-4mm <strong>coronary</strong> balloon and low pressure) was performed before stent<br />
placement. Ballon inflations were routinely performed within the stents after placement.<br />
Continuous intravenous heparin was given during the night, and vascular sheats were<br />
removed the morning after the procedure. The clinical endpoints were major or minor<br />
stroke myocardial infarction, or death during follow up period.<br />
Results: The procedural success rate was 96.66%. For a mean follow up period of 5.6 ±<br />
3.2 months, 4 deaths occurred (17% of cases), none of which were attributed to a<br />
neurologic cause. Also 1(3%) case had a minor non fatal stroke (transient cognitive<br />
disorder). we designed a new evaluation system: anyone of the characteristics in class C<br />
is considered a predictor for events. Increased number of these predictors is associated<br />
with the risk of complications after the procedure. Also between these predictors; stenosis<br />
95%-99% and large crater ulceration of carotid lesions are more important than the<br />
others.<br />
25
Conclusion: To reduce carotid stenting complications in high risk cardiac patients and<br />
to optimize patient selection, we suggest a new evaluation system based on clinical and<br />
lesion characteristics of patients to determine the best treatment strategy.<br />
26
Predictors of the major adverse cardiac events (MACE) after<br />
percutaneous <strong>coronary</strong> intervention- a single center registry<br />
Salarifar M, Kassaian SE, Alidoosti M, Haji Zeinali AM, Paydari N and Sharafi<br />
Tehran Heart Center, Medical Sciences/University of Tehran, Tehran, Iran<br />
Abstract<br />
Objective: To propose a model for predicting the risk of MACE. MACE was defined as<br />
nonfatal MI, target vessel revascularization and cardiac death.<br />
Methods: The data of all patients undergoing PCI between March 2003 and March 2005,<br />
(n=2614) were analyzed in this prospective registry. The only exclusion criteria was dropout<br />
from the 9 month follow-up plan (n=434, 16.6%). All characteristics of the patients who had<br />
MACE (n=122, 4.7%) were compared with the others (NonMACE group). All significant<br />
factors entered in the model for multivariate analysis. Time of developing MACE (MACE<br />
time) and MACE hazard evaluated by the Cox regression.<br />
Results: Univariate ORs were revealed in the table 1. Although in univariate analysis Intraaortic<br />
balloon pump, cardiogenic shock and PCI on the left main, were strong predictors for<br />
the MACE they were not entered in the model (due to small sample size). Multivariate<br />
analysis reveals that EF lower than 40%, Unstable Angina or acute <strong>coronary</strong> syndrome and<br />
Dissection were predictors for the MACE.<br />
Median for MACE time was 5±0.49 month (SEM). Unsmoothed graph in Graph<br />
1(Hazard function) shows that the frequency of the MACE increased in the fourth and<br />
tenth month in the first year after PCI. Also It reveals that the frequency of the MACE<br />
increase in the 14 and 15 month.<br />
Conclusion: we propose that the follow up plan could cover the most dangerous time<br />
(4th, 10th, 15th month) after the PCI. So we recommend 18 month follow up plan (1, 4,<br />
9, 12, 18 and yearly after that). Our study reveals that in the current era of interventional<br />
cardiology, the best outcome achieve in the patients presenting by stable angina, having<br />
good EF and have been treated by experienced hands(to prevent dissection).<br />
27
Table 1: Univariate and multivariate analysis of the Major Adverse Cardiac Event<br />
Odds Ratio (95% Confidence Interval)<br />
Multivariate<br />
Univariate<br />
1.50(1.00-2.26)*<br />
Diabetes Mellitus
2.99(1.71-5.25) ‡<br />
0.51(0.34-0.76) †<br />
1.67(1.16-2.42) †<br />
2.01(1.07-376) *<br />
Stable Angina<br />
Unstable Angina<br />
Prior PCI<br />
1.76(0.99-3.14)<br />
3.14(1.14-8.60) *<br />
~<br />
1.80(1.15-2.83) *<br />
3.76(1.96-7.21) ‡<br />
2.77(1.46-5.24) †<br />
Multivessel Disease<br />
Primary PCI<br />
Dissection<br />
3.02(1.40-6.53) †<br />
Marked Increase in CPK 1<br />
0.61(0.38-0.97) *<br />
Right Coronary Artery Territory<br />
1.44(0.97-2.16)<br />
~<br />
Left Anterior Descending Territory<br />
~<br />
3.81(1.92-7.54) ‡<br />
1.93(0.89-4.21)<br />
1.74(1.02-2.96) *<br />
2.43(1.41-4.21) †<br />
8.56(1.56-47.19) †<br />
43.93(8.43-228.84) ‡<br />
43.93(8.43-228.84) ‡<br />
Bare Metal Stents (vs. Drug Eluting Stents)<br />
Reference Vessel Diameter ” 2.5mm<br />
Low Ejection Fraction(EF
Comparative study of success rate & complications frequency<br />
in two streptokinase trade forms:" A randomized double blind<br />
study"<br />
Salarifar M, Paydari N, Davoodi Gh, Amirzadegan AR and Biria A<br />
Tehran Heart Center, Medical Sciences/University of Tehran, Tehran, Iran<br />
Abstract<br />
Background: This study was to determine the efficacy and safety of the different trade<br />
forms of the streptokinase available in our country; Heberkinasa (heberbiotec, Havana, Cuba)<br />
and Streptase (Aventis Behring GmbH, Marburg, Germany).<br />
Methods: This study were conducted by grant of Undersecretary for Food and Drug<br />
Affairs, Ministry of Health & Medical Education. From the January 2005, the patient who<br />
met the inclusion criteria was enrolled in this randomized double blind clinical trial and<br />
allocated in one of the treatment arms; Heberkinasa(HBK) or Streptase(STP). Thrombolysis<br />
success was evaluated angiograpgically and TIMI 3 flow in the infarct-related epicardial<br />
<strong>artery</strong> was regarded as the successful <strong>coronary</strong> thrombolysis. Any complications or inhospital<br />
events (Safety) were documented on a detailed questionnaire. Clinical follow up<br />
(phone survey and mailed questionnaire) was done 30 days after thrombolysis. Successful<br />
thrombolysis and in-hospital mortality (Efficacy) were assessed in the primary end points.<br />
Secondary end point of the study (Reinfarction and cardiac death) was evaluated 1 month<br />
after thombolysis.<br />
Results: From January 2005 to January 2006, 221 patients (Age 56.9± 10.8, Men: 88.2%)<br />
were randomized, 119 were allocated in the HBK and 102 in the other group.<br />
Baseline clinical, risk factors and demographic characteristics were the same in both<br />
groups. Also there were no significant differences in the door to drug and pain to drug<br />
times. The rate of complications were the same (43.9% [HBK] vs. 45% [STP], p=NS).<br />
Angiography was done for 157(70.1 %) patients, in 9% in the first 24 hrs and in 39.8% in<br />
the first 72 Hrs after thrombolysis. Lesion morphology and<br />
Lesion / patient ratio were not significantly different (1.87[HBK] vs. 1.67[STP], p=NS).<br />
The rate of Successful thrombolysis were the same (67.5% [HBK] vs. 67.6% [STP], p=NS).<br />
Study endpoints were revealed in the table 1.<br />
Conclusion: So far, the Complication frequency and the success rate of the streptase and<br />
heberkinasa have been the same. The study will be ongoing to complete the sample size and<br />
increase the statistical power. Keywords: Streptokinase, Thrombolytic therapy,<br />
Complications, Success rate<br />
29
Study of factors affecting in-hospital mortality of patients with<br />
acute myocardial infarction<br />
Salarifar M, Darabian C, Solaymani A, Amirzadegan AR, Hamidian R and<br />
Mahmoudian M<br />
Tehran Heart Center, Medical Sciences/University of Tehran, Tehran, Iran<br />
Abstract<br />
Background: The objective of present study is to determine whether demographic,<br />
clinical and paraclinical risk factors can predict risk of In-hospital mortality of acute<br />
myocardial infarction (AMI).<br />
Methods: Using ischemic heart disease database, 1798 patients who were hospitalized<br />
for AMI were assigned to 2 groups in a retrospective cohort study: group one patients<br />
survived and group two patients died of AMI at hospitalization time.<br />
Results: Demographic findings show expired patients’ mean age was significantly<br />
higher and post- AMI mortality was significantly greater in female than male patients<br />
(p
Table1<br />
Group II Expired patients<br />
Group I Survived patients<br />
69.01 years old<br />
61.53% male ,38.46% female<br />
44.1%<br />
47.3%<br />
8%<br />
III & V<br />
51.8%<br />
29.62<br />
43.2%<br />
46.7%<br />
17.2%<br />
101.1<br />
11.7<br />
61.91 years old<br />
74.89% male ,24.61% female<br />
48.1%<br />
37.1%<br />
9.9%<br />
I & II<br />
43.3%<br />
46.1%<br />
44.8%<br />
52.5%<br />
4.3%<br />
80.67<br />
8.72<br />
Mean age<br />
Sex<br />
Dyslipidemia<br />
Diabetes mellitus<br />
Opium addiction<br />
Killip calss<br />
Hypertension<br />
LVEF<br />
Presence of Q wave<br />
ST elevation<br />
Bundle branch block<br />
mean CKMB serum<br />
concentration<br />
mean Troponin serum<br />
concentration<br />
Table 2<br />
other<br />
0,0<br />
Ant.<br />
lat<br />
15.4 %<br />
R<br />
V<br />
9.1<br />
%<br />
Ant.<br />
septal<br />
9.2%<br />
Affected region<br />
<strong>Post</strong><br />
11.1<br />
%<br />
Septal<br />
11.8%<br />
Apica<br />
l<br />
0.0<br />
La<br />
t<br />
9.1<br />
%<br />
In<br />
f<br />
6.9<br />
%<br />
Ant<br />
11.6<br />
%<br />
Female<br />
gender<br />
13.9%<br />
Male<br />
gende<br />
r<br />
7.8%<br />
Mortality (9.4%<br />
of all patients)<br />
32<br />
Risk factors for complications of delay in <strong>surgery</strong> in staged<br />
carotid stenting and <strong>coronary</strong> <strong>bypass</strong> <strong>graft</strong> <strong>surgery</strong>
Kassaian SE, Alidoosti M, Kazemi Saleh D, Haji Zeinali AM, Salarifar M, Shirani<br />
Sh, Hakki Kazazi E and Darvish S<br />
Tehran Heart Center, Medical Sciences/University of Tehran, Tehran, Iran<br />
Abstract<br />
Background: To answer the question whether the delay in <strong>coronary</strong> <strong>artery</strong> <strong>bypass</strong> <strong>graft</strong><br />
(CABG) results in adverse events, we describe our experience with planned staged carotid<br />
stenting followed by CABG in our patients.<br />
Methods: From December 2003 through February 2006, we performed 53carotid<br />
angioplasty procedures. Of these patients, 39 cases underwent carotid stenting followed by<br />
scheduled CABG but only 28 of them presented for CABG. In-hospital complications were<br />
evaluated by a neurologist .Long-term follow-up was then conducted by telephone interview<br />
for all of patients who were presented for CABG.<br />
Result: The procedural success rate was 97.4%. The mean interval from last carotid stent to<br />
CABG was 78.8±60 days (range, 8-254 days). In the interval between carotid stenting and<br />
CABG 4 deaths occurred (14.2% of cases), all of them in first week and none of which were<br />
attributed to a neurologic cause. Also 2(7.1%) case had a minor non fatal stroke. we designed<br />
a new evaluation system: anyone of the characteristics in class C, particularly stenosis 95%-<br />
99% and dense calcification is considered as a predictor for events. Increased number of<br />
these predictors in addition to age•75 and having valvular heart disease are associated with<br />
the risk of complications after the procedure.<br />
Conclusion: We suggest that if we decide for carotid intervention in patients with •4<br />
suggested predictors, especially stenosis •95% and dense calcification and/or patients who<br />
have valvular heart disease and/or age•75, the physician should closely observe the patient<br />
during the waiting period before CABG particularly in the first week after carotid stenting.<br />
Keywords: carotid stenting, CABG, complication<br />
33<br />
Angiographic profile and lesion characteristics in young<br />
patients with percutaneous <strong>coronary</strong> intervention<br />
Kassaian SE, Salarifar M, Alidoosti M, Haji Zeinali AM, Poorhosseini HR,
Pirzadeh L, Raissi Dehkordi M and Paydari N<br />
Tehran Heart Center, Medical Sciences/University of Tehran, Tehran, Iran<br />
Abstract<br />
Background: To find out the differences in baseline, angiographic, procedural and<br />
lesion characteristics in young patients ”40 years old versus old patients who underwent<br />
percutaneous <strong>coronary</strong> intervention (PCI).<br />
Methods: From April 2003 to March 2005, 138 PCI procedures were performed in 118<br />
patients aged ” 40 years and compared to 354 patients>40 years, who were randomly<br />
selected from a total of 2493 old patients as control group. Data was collected from our<br />
database.<br />
Results: 118 patients (4.5%) were 40 years old or under. Young patients were more<br />
often male (91.5% vs. 71.8%, P
Tehran Heart Center, Medical Sciences/University of Tehran, Tehran, Iran<br />
Abstract<br />
Background: PCI in diabetic patients had long been a dilemma due to high rate of<br />
restenosis. Multiple studies have shown the benefit of the use of drug eluting stents in this<br />
subgroup of patients. Our goal in the present study is to evaluate the results of PCI in<br />
diabetic patients using drug eluting stents in Iranian population.<br />
Methods: From April 2003 to March 2005, 268 patients (69 diabetic patient) underwent<br />
PCI with DES (220 Cypher and 71 Taxus) at our center. These patients made the study<br />
population. We undertook a thorough evaluation of baseline, clinical characteristics,<br />
angiographic and procedural properties. we also verified the clinical outcomes of PCI<br />
with DES in diabetic and non-diabetic subgroups.<br />
Result: There was no significant difference between the two groups regarding the<br />
baseline clinical characteristics except that the diabetics were significantly more<br />
hyperlipidemic (66.7% vs. 47% p=0.001). PCI on LAD territory was less frequent in<br />
diabetics (69% vs. 81.3% p=0.042), on the contrary PCIs on small-sized vessels<br />
(RVD
Background: Redo <strong>coronary</strong> <strong>artery</strong> <strong>bypass</strong> <strong>graft</strong> (CABG) is usually associated with high<br />
rate of complications including mortality. Many of these patients can be revascularized by<br />
PCI on their native vessels, Sapherous vein <strong>graft</strong>s (SVGS) or arterial <strong>graft</strong>s. PCI on SVG has<br />
been accompanied by high rate of procedural complications or long term restenosis. In this<br />
study we evaluated the success rate, complications and late outcomes of PCI on SVG in our<br />
patients.<br />
Methods: of 2614 consecutive patients, who underwent PCI during April 2003 to march<br />
2005, 70 (2.7%) patients had history of previous CABG and 20 of them (23 Lesion) had PCI<br />
on SVG. Based on our database we evaluated the baseline, procedural and outcomes<br />
characteristics in this group of patients.<br />
Result: They are all male. Mean age was 59.9±9.2 yrs and the period between CABG and<br />
PCI was 7.9±4.9 yrs. The most common <strong>graft</strong>s were SVG to OM (60.9%) and SVG to RCA<br />
(26.1%). 13(56.5%) patients were treated by direct stenting, 9 (39.1 %) by primary stenting<br />
and 1(4.3%) by pure only balloon angioplasty. Angiographic Success was achieved in all of<br />
them but 1 case had Non Q-wave MI after the PCI (Clinical Success Rate: 95.0%).There was<br />
not any in hospital mortality. Regarding the long-term outcome 4 patients had emergency<br />
room visit, 1 readmitted and angiography was done but no significant stenosis was revealed.<br />
Mean follow-up time was 9.5±3.1 months and of 80% patients complete their follow up plan.<br />
There was not any major adverse cardiac event in this group of patients.<br />
Conclusion: It seems that PCI on the Saphenous vein <strong>graft</strong> was safe and efficient using an<br />
appropriate patient selection and if indicated distal protecting devices.<br />
36<br />
Short- and long-term outcomes following percutaneous <strong>coronary</strong><br />
intervention in young patients<br />
Kassaian SE, Alidoosti M, Salarifar M, Haji Zeinali AM, Nematipour E, Pirzadeh L<br />
and Raissi Dehcordi M<br />
Tehran Heart Center, Medical Sciences/University of Tehran, Tehran, Iran
Abstract<br />
Background: We evaluated early and late outcomes of percutaneous <strong>coronary</strong> intervention<br />
(PCI) in patients”40 years.<br />
Methods: From April 2003 to March 2005, PCI outcomes in 118 patients ”40 years (group<br />
ǿ) was compared to 354 patients, who were randomly selected from 2493 patients >40 years<br />
(group ǿǿ) from our database.<br />
Result: Group ǿ was more often male (91.5% vs. 71.8%, P
Background: The conventional twelve-lead electrocardiogram (ECG) still is used for<br />
diagnosis of wall motion abnormality. The purpose of this study was to evaluate the<br />
relation between resting electrocardiographic abnormalities and wall motion (WM)<br />
abnormality in <strong>coronary</strong> <strong>artery</strong> disease (CAD).<br />
Methods: 6438 consecutive patients with CAD in angiography in our center over a<br />
period of two years included in this study. Electrocardiograms were reviewed for the<br />
presence of Q wave (• 2 contiguous ECG leads) and echocardiography were examined for<br />
various motion disorders (local hypokinesia, akinesia, dyskinesia and generalized<br />
hypokinesia) in patients with CAD in angiography.<br />
Result: Out of 6438 patients with CAD, 2407 had WM abnormality and 4031 patients<br />
had no WM abnormality. Among patients with CAD and wall-motion abnormality, 44%<br />
(1071) had Q waves and 66% (1336) did not have Q waves. From patients with CAD<br />
without WM abnormality, 19.5% (788) had Q waves and 80.5% (3243) did not have Q<br />
waves. So sensitivity and specificity of Q wave for the diagnosis of WM abnormality in<br />
CAD is 57% and 70%, respectively.<br />
Conclusion: Despite new methods for the diagnosis of wall-motion abnormality, the<br />
electrocardiogram is still a useful and simple method for the diagnosis of wall-motion<br />
disorders in CAD.<br />
Keywords: Wall motion abnormality, Q wave, Coronary <strong>artery</strong> disease<br />
38<br />
The prognosis of a non-Q-wave versus Q-wave myocardial<br />
infarction<br />
Sadeghian H, Sahebjam M and Mahmoodian M<br />
Tehran Heart Center, Medical Sciences/University of Tehran, Tehran, Iran<br />
Abstract
Background: Non-Q-wave myocardial infarction seems to have higher rates of<br />
complications. It is usually managed with an invasive strategy, Nevertheless, the clinical<br />
course and prognosis of this type of myocardial infarction and the best approach to its<br />
management remain controversial.<br />
Methods: From June 2003 to March 2005 data were collected from an ischemic heart<br />
disease registry enrolling 993 patients with acute non-Q-wave and 803 patients with Q-<br />
wave myocardial infarction. 49.04% of non-Q-wave and 54.4% of the patients with Q-<br />
wave myocardial infarction underwent <strong>coronary</strong> angiography within the first week after<br />
onset of a myocardial infarction.<br />
Results: The mean of patients with non-Q-wave myocardial infarction was higher<br />
(63.14±12.38 vs.61.87±12.1, P=0.029) and they were more likely to be female (P=0.013).<br />
The prevalence of single, two and three vessel disease in both group was similar<br />
(respectively P=0.65, P=0.97 and P=0.27), while the left main disease was more frequent<br />
in patients with non-Q-wave myocardial infarction (4.3% vs. 1.1, P=0.053). The<br />
prevalence of suggested treatments (percutaneous or surgical intervention and medical<br />
treatment) were similar in both groups (P=0.32). In-hospital Mortality was not<br />
statistically different between non-Q-wave and Q-wave myocardial infarction (10.3% vs.<br />
9.6%, P=0.59). Heart failure (P=0.036) and pulmonary edema were more frequent in Q-<br />
wave (P=0.043) and CVA was more frequent in non-Q-wave myocardial infarction<br />
(P=0.017).<br />
Conclusion: Patients with non-Q-wave myocardial infarction in comparison with Q-<br />
wave patients had similar angiographic features and in-hospital mortality rate and do not<br />
seem to have a worse prognosis<br />
39<br />
Normal values for ventricular synchrony measured by tissue<br />
Doppler imaging and tissue Doppler synchronization imaging<br />
in structurally normal hearts<br />
Sadeghian H, Saheb Jam M, Yamini Sharif A, Kazemisaied A, Fallah N,<br />
Goodarzynejad HR and Raissi Dehkordi M<br />
Tehran Heart Center, Medical Sciences/University of Tehran, Tehran, Iran
Abstract<br />
Background: We studied normal values for intraventricular and interventricular delay<br />
by tissue Doppler imaging (TDI) and tissue synchronization imaging (TSI).<br />
Methods: We evaluated 25 healthy adult volunteers (26.30±5.68 years, 16% male).<br />
Tissue Doppler Echocardiography was performed (system VIVID 7D, GE) using a 6-<br />
basal, 6 mid-segmental model to assess the time-to-peak systolic contraction (Ts). We<br />
also evaluated the right ventricle at basal and mid portion levels. We measured Ts both<br />
manually and with TSI.<br />
Results: Anterior basal and mid-portion had the shortest Ts and interventricular septum<br />
had the longest Ts with both methods. Correlation between manual and TSI methods was<br />
significant (p
29.25<br />
88.40<br />
200<br />
TDI: 60<br />
Anterior<br />
9.01<br />
77.28<br />
98<br />
TSI: 61<br />
midportion<br />
47.26<br />
153.60<br />
210<br />
TDI: 24<br />
Septal basal<br />
39.88<br />
141.56<br />
216<br />
TSI: 78<br />
40.89<br />
37.09<br />
161.60<br />
125.40<br />
210<br />
216<br />
TDI: 80<br />
TSI: 82<br />
Septal<br />
midportion<br />
38.10<br />
181.20<br />
230<br />
TDI: 40<br />
RV basal<br />
24.26<br />
176.04<br />
228<br />
TSI: 129<br />
52.56<br />
20.89<br />
173.60<br />
175.12<br />
260<br />
217<br />
TDI: 12<br />
TSI:129<br />
RV<br />
midportion<br />
41<br />
Discrete subvalvular aortic stenosis: severity of aortic<br />
insufficiency and rate of recurrence after <strong>surgery</strong><br />
Tehran Heart Center, Medical Sciences/University of Tehran, Tehran, Iran<br />
Abstract<br />
Background: Discrete subaortic stenosis (DSS) is a progressive condition, and it is<br />
debatable whether <strong>surgery</strong> reduces the severity of aortic insufficiency (AI). The aim of
this study was to determine the changes in the severity of aortic regurgitation and the<br />
recurrence rate of obstruction after <strong>surgery</strong> in patients with discrete subaortic stenosis.<br />
Methods: Between March 2002 and January 2006, 28 patients with a mean age of (28.9<br />
± 15.4) years were evaluated before and after <strong>surgery</strong> for DSS. Mean follow-up time was<br />
14.6 ± 10.2 months. Peak systolic gradients across the left ventricular outflow tract and<br />
severity of aortic regurgitation were evaluated by Doppler Echocardiography.<br />
Results: preoperative left ventricular outflow tract gradient of our patients were •30<br />
mmHg which decreased from a mean of 89.46 ± 41.67 to 25.23 ± 17.26 mmHg<br />
postoperatively and reached to 27.38 ± 19.02 mmHg at follow-up. The gradient remained<br />
•30 mmHg in 42.9% of patients at follow up. AI was identified in 22 (78.5%) patients<br />
preoperatively: 1+ in 13 (59.1%) patients and 2+ in 9(40.1%) patients. From 9 patients<br />
with grade 2 of AI, 2 (22.2%) remained unchanged, 4 (44.5%) had 1+, 1 (11.1%) had 4+<br />
AI (bicuspid aortic valve) and 2 (22.2%) were lost to follow-up. We had 2 recurrences of<br />
membrane after operation and 2 of our patients underwent <strong>surgery</strong> because of recurrence.<br />
Conclusion: Our results suggest that although subaortic resection may reduces the<br />
severity of AI in some patients, future studies with more cases are needed to determine<br />
whether the severity of AI decreases after membrane resection.<br />
Keywords: Subvalvular aortic stenosis, valvular heart <strong>surgery</strong><br />
42<br />
Repositioning of dislodged atrial pacing lead with a specially<br />
designed urologic basket<br />
Yamini Sharif A, Davoodi Gh and Kazemi Saeed A<br />
Tehran Heart Center, Medical Sciences/University of Tehran, Tehran, Iran<br />
Abstract<br />
Background: Lead dislodgement requiring reoperation is a complication that raises the<br />
costs of pacemaker implantation <strong>surgery</strong> while adding to patient discomfort. Migration of
a dislodged lead can cause complication such as under sensing, loss of atrial capture and<br />
loss of atrial kick in patients who need AV synchrony. Once detected, the dislodged lead<br />
should be immediately repositioned. In recent years, percutaneous transcatheter<br />
repositioning of displaced permanent pacemaker leads has been advocated before<br />
consideration of surgical repositioning. The procedure is easy and safe, allowing a<br />
reduction of the need for surgical lead revision and the associated morbidity and cost. In<br />
this report we introduce a method with specially designed urologic basket (figure 1) to<br />
solve this problem in 2 patients<br />
Methods : To perform repositioning of passive fixation atrial pacing leads , patients<br />
were brought to cath. lab in the post absorptive non-sedated state .Mullins sheath was<br />
placed around the atrial lead of pacemaker and by using the deflectable ablating<br />
catheter,the Mullins sheath was positioned over the loop of the atrial pacing lead. After<br />
the removal of the ablation catheter, the specially designed urologic basket was sent over<br />
the loop of passive fixation j-shaped atrial lead. The deflectable part of this basket was<br />
passed through the tip of Mullins sheath which had been positioned over the loop of the<br />
dislodged pacemaker lead. By deflecting the tip of basket, we made a hook around the<br />
lead. Then by pulling back the basket and Mullins sheath and some traction, the atrial<br />
lead was sent to a new position in the atrium. Immediately pacing analysis was<br />
performed, atrial pacing and sensing parameters were acceptable. By decreasing the<br />
curve and pulling back of the basket into the Mullins sheath, all devices were taken out.<br />
Results: During follow up, in one patient the lead was stable and did not move again,<br />
and in a second patient the repositioned lead dislodged again (one day after the<br />
procedure) and migrated to the previous position (SVC). Therefore, this pacemaker<br />
problem was corrected in a second operation session by the replacement of an active<br />
fixation lead.<br />
Conclusion: Percutaneous techniques could also allow us to reposition leads in a less<br />
aggressive way, maintaining adequate success and reducing the number of complications.<br />
Repositioning of displaced passive fixation atrial pacing leads with this basket could be<br />
another solution when the lead is tightly fixed to the atrial wall or SVC. When this is not<br />
feasible, surgical approach is necessary to manage the problem.<br />
43
Figure .1These figures show the specially designed urologic basket and how it makes a<br />
hook.<br />
44<br />
Radiofrequency ablation of cardiac arrhythmia using a threedimensional<br />
real-time position management and mapping<br />
system<br />
Yamini Sharif A, Kazemi Saeed A and Davoudi Gh<br />
Tehran Heart Center, Medical Sciences/University of Tehran, Tehran, Iran<br />
Abstract
Background: A recently developed three- dimensional real-time position management<br />
system (RPM) uses an ultrasound ranging technique that enables multiple distance<br />
measurements between two reference catheters and a mapping catheter each equipped<br />
with ultrasound transducers. In addition to three-dimensional representation of the<br />
catheters and ablation sites, it displays real- time movement of catheters (including the<br />
tip and shaft) .A recently released version of the system enables additional geometry<br />
reconstruction of the heart chamber and activation mapping. This study included four<br />
patients referred for radiofrequency ablation of arrhythmia.<br />
Methods: Geometry was reconstructed by tracing the endocardial contour of the<br />
respective heart chambers. Global and color coded activation maps were constructed to<br />
confirm the nature of arrhythmia and to guide ablation. Spontaneous or induced<br />
arrhythmia were AVNRT common type (n=2) and atrial tachycardia (n=2). Geometry<br />
reconstruction and mapping of arrhythmia were possible in all of them.<br />
Results: RPM-guided radiofrequency ablation was successful in 3 of 4 patients. In the<br />
patient who had atrial tachycardia very close to AV node, this system was very useful to<br />
show the location of arrhythmia. This patient was successfully ablated with no damage to<br />
AV nodal system. .Ablation procedures were successful in both patients with AVNRT,<br />
but it took a long time to insert the reference catheter into the <strong>coronary</strong> sinus and to map<br />
the arrhythmia. During follow-up, in one patient the lead was stable and did not move<br />
again, n a second patient the repositioned lead dislodged again( one day after the<br />
procedure) and migrated to the previous position(SVC), so this pacemaker problem was<br />
corrected in the second operation session by the placement of an active fixation lead.<br />
Conclusion: The new RPM system enables geometry reconstruction, and threedimensional<br />
positioning of the ablation catheters, reconstruction of the activation maps,<br />
marking of anatomic structures and reproducible tracking of multiple ablation sites. The<br />
system could be used to guide radiofrequency ablation of atrial and ventricular<br />
arrhythmia, and it is not logical and economical to use this system for arrhythmias that<br />
are easily ablated with conventional methods. In the future, we hope to solve the<br />
technical and administrative problems leading to some difficulties in using this new<br />
system.<br />
45<br />
Higher dose of heparin administration for prevention of<br />
catheter - induced thromboembolic events during cardiac<br />
catheterization & <strong>coronary</strong> angiography<br />
Yamini Sharif A, Khoshgoftar Z, Mohamadhossaini M,Sheikhrezaii F, Ghazanchai F,<br />
Nayebhosaaini M, Arab M and Ghayeghvar F<br />
Tehran Heart Center, Medical Sciences/University of Tehran, Tehran, Iran<br />
Abstract
Background: Prophylactic heparin during cardiac catheterization is recommended by<br />
some authors, but there are controversies about the recommended doses. After occurrence of<br />
a case of stroke in one of our patients during <strong>coronary</strong> angiography, we decided to evaluate<br />
the safety and efficacy of higher dose of heparin in prevention of thromboembolic events<br />
during cardiac catheterization& <strong>coronary</strong> angiography.<br />
Methods: From February 2002 to May 2005, seven hundred consecutive patients who<br />
underwent cardiac catheterization entered the study in prospective manner. Exclusion criteria<br />
were systolic blood pressure •200 mm Hg, coagulopathy, end stage renal disease, and<br />
multiple attempts to gain arterial access (> 1 arterial puncture).The intervention consisted of<br />
altering the routine dose of heparin (1000IU) to a higher dose (5000IU), in the above<br />
mentioned patients 1500IU intra introducer, the remaining in to the galipot and it was used<br />
during the procedure. Protamin sulfate was not used to neutralize heparin. All of the study<br />
population was assessed for thromboembolic as well as hemorrhagic events. Additionally in<br />
100 randomly selected subjects who received higher dose of heparin, "Compression time"<br />
was calculated and compared with a matched control group with previous dose (1000IU).<br />
Results: No hemorrhagic complication such as massive hematoma, intracranial<br />
hemorrhage, gastrointestinal or urinary tract bleeding occurred in our patients. We also did<br />
not find any thromboembolic events including stroke, renal or mesenteric emboli in our<br />
patients. More over, "compression time" was similar in both groups (6.5 ± 2 versus 6.7±2<br />
minutes).<br />
Conclusion: Higher prophylactic dose of heparin during cardiac catheterization appears to<br />
be free from the increased risk of major hemorrhagic events. More studies with larger study<br />
population are required to investigate the efficacy of this protocol in preventing<br />
thromboembolic events during cardiac catheterization & <strong>coronary</strong> angiography.<br />
46<br />
Early complications of permanent pacemaker implantation<br />
Yamini Sharif A, Kazeme Saeed A, Davoodi Gh, Abolbaghaei SM, Paydari N and<br />
Goodarzynejad HR<br />
Tehran Heart Center, Medical Sciences/University of Tehran, Tehran, Iran<br />
Abstract<br />
Background: This study was done to evaluate the incidence of intra operative and early<br />
postoperation complication (up to two months after implantation) of permanent pacemaker<br />
insertion in all patients undergoing a first implant at our center.<br />
Methods: Retrospective evaluation of all pacemaker implantation procedures performed<br />
from May 2002 to March 2006 was carried out by completion of our database form. Patients`
demographic data, medical history, details of pacemaker hardware used, and major<br />
complications were noted. Five hundred eighty-one consecutive patients underwent<br />
implantation of their first permanent pacemaker. The mean age was 68±14 years (range: 15-<br />
95) and 48.7% were male. Dual chamber units were implanted in 136 patients (23.4%) and<br />
single chamber pacemakers (VVIR) were implanted in 257 patients (44.2%).<br />
One hundred thirty-six patients received (VDDR) pacemakers (23.4%) and (VVI)<br />
pacemakers were implanted in two patients. Most implants (82.4%) were performed via right<br />
subclavian vein. The most common cause of PPM insertion was complete heart<br />
block(79.7%), followed by sick sinus syndrome in 9.3%, two to one AV Block (5.2%) and<br />
4.1% Tachy-brady syndrome.<br />
Results: Twenty four patients (4.13%) required reoperation. Ventricular or atrial lead<br />
displacement (n=19) was the most common reason for reoperation, and pacemaker pocket<br />
infection led to reoperation in 2 patients (0.34%). Pneumothorax occurred in 3 patients and<br />
was treated successfully with chest tube insertion.<br />
Conclusion: In our center, the incidence of complications following pacemaker<br />
implantation was low and compares favorably with complication rates in other centers. Lead<br />
dislodgement was the most common reason for second operation. Infection rates were low,<br />
(
<strong>surgery</strong>, and post percutaneous transvenous mitral commissurotomy (PTMC) underwent an<br />
outpatient cardiac rehabilitation (CR) program (three exercise sessions per week of 1 hour)<br />
from July 2004 to January 2006. We comprised them in three groups before and after CR:<br />
group ǿ completed <br />
10, group ǿǿ: 11 to 20, and group ǿǿǿ: 21 to 30 sessions. Also, each<br />
group was assessed in two subgroups in terms of gender. Data were collected from CR<br />
database.<br />
Results: The three groups were similar in mean age, gender, and the frequency of risk<br />
factors. There were 64.1% patients in group ǿ, 15.4% in group ǿǿ, and 18.8% in group ǿǿǿ.<br />
At baseline, consumptive calorie, and treadmill velocity were similar between all the groups,<br />
and subgroups that after CR, significantly accelerated in each group, and subgroup, but<br />
among the groups, group ǿǿǿ was the most (P
groups: Group I (n = 342) included patients < 40 years, group II (n = 765) included<br />
patients > 60 years.<br />
Results: Most of patients were male in both groups (82 Vs 60.5%). Family history of<br />
<strong>coronary</strong> <strong>artery</strong> disease, current smoking and opium addiction were more prevalent in<br />
younger patients (p < 0.001). Dyslipidemia, hypertension and diabetes mellitus were<br />
more prevalent in older patients (p < 0.001). Excluding normal angiogram, presentation<br />
of <strong>coronary</strong> <strong>artery</strong> disease in two groups was: 36% in group I and 14% in group II with<br />
ST elevation MI (p < 0.001), 8% in group I and 7% in group II with non ST elevation MI<br />
(p = 0.71), 23% in group I and 31% in group II with unstable angina (p = 0.029), 34% in<br />
group I and 48% in group II with stable angina (p < 0.001). Coronary angiography<br />
revealed more number of multivessel in older patients (62 Vs 31%; p
Results: There were no differences in mean age, gender, the frequency of risk factors<br />
between the groups. At baseline; consumptive calorie and treadmill velocity were similar in<br />
all groups (mean: 31.9, and 2.8, respectively). But after CR, calorie increased by 50.2±12.4 in<br />
group ǿ vs. 67.3±18.7 in group ǿǿ vs. 71.3±11.3 cal⁄h in group ǿǿǿ. Also, velocity improved<br />
in each group: 3.8±1 vs. 4.8±1 vs. 6.2±1.8 km⁄h, respectively, but these accelerations in<br />
calorie, and velocity were the greatest in group ǿǿǿ (P
efore and after CR.<br />
Results: Mean age, gender, and the frequency of risk factors were similar between the three<br />
groups. Before CR, these groups were similar in consumptive calorie, and treadmill velocity.<br />
After CR, consumptive calorie in group ǿ increased from 34.9±6.7 to 51±9.4 cal⁄h (P
involvement and stenosis greater than 70% were selected. Thereafter, patients were<br />
assigned to two groups: severe (70-90%) and very severe (>90%) stenosis and then<br />
correlation of ECG abnormalities with severity of <strong>coronary</strong> <strong>artery</strong> stenosis were assessed.<br />
Results: Participants include 90 female (40.7%) and 131male (59.3%) patients<br />
between25-79 at a mean age 55.05 years old. The <strong>coronary</strong> arteries that showed<br />
correlation with ECG abnormalities were left anterior descending (LAD) and left<br />
circumflex (LCX). LAD very severe stenosis (119 patients, 53.84 %) correlated<br />
significantly with inverted T in V1-V4 and AVL leads. Existence of inverted T in V1-V4<br />
and AVL leads was 53.8% and 31.1% respectively. Inverted T wave in V5-V6, inferior<br />
(II, III and AVF) and AVR was 40.3%, 6.7% and 0.0% respectively. There were 49<br />
patients (22.17%) with LAD severe stenosis which 25 patients (51%) of them presented<br />
inverted T in V1-V4 leads, but it was insignificant. There were 4 LCX severe stenosis<br />
cases (< 2%) associated with ST depression in V1-V6 leads.<br />
Conclusions: This study shows that existence of inverted T wave in V1-V6<br />
(precordial) ECG leads certainly correlates with the site of <strong>coronary</strong> <strong>artery</strong> stenosis in<br />
very severe LAD stenosis.<br />
52<br />
The association between hepatitis B surface antibody<br />
seropositivity and <strong>coronary</strong> <strong>artery</strong> disease<br />
Amirzadegan A, Davoodi Gh, Borumand MA, Raissi Dehkordi M, Goodarzynejad HR,<br />
Darabian S and Fallah N<br />
Tehran Heart Center, Medical Sciences/University of Tehran, Tehran, Iran<br />
Abstract<br />
Background: Specific infectious agents have been found to be related to the<br />
pathogenesis of <strong>coronary</strong> atherosclerosis. In this study, we assessed the possible<br />
association between angiographically-proven <strong>coronary</strong> <strong>artery</strong> disease (CAD) and<br />
Hepatitis B surface antibody (HBsAb) seropositivity.<br />
Methods: HBsAb and C - Reactive protein (CRP) were checked with Enzyme-linked<br />
immunosorbent assay and immunoturbidometry in 703 patients with no history of<br />
Hepatitis B vaccination prior to <strong>coronary</strong> angiography. Angiographic results were
eported by two cardiologists for inter-observer reliability and interpreted as significant<br />
CAD in case of •50% stenosis in •1 major <strong>coronary</strong> <strong>artery</strong> (group 1) versus normal<br />
<strong>coronary</strong> or
Results: We found 15 patients (0.35%) with segmental backflow phenomenon with a mean<br />
age of 46 years (Range: 29-61).The male to female ratio was 1.5. At 1-year's follow up, no<br />
patients presented with acute myocardial infarction and there was no mortality. But as a<br />
result of angina like chest pain, six patients were admitted to CCU in this period of time.<br />
Conclusion: Pure Segmental backflow indicates an abnormal flow in <strong>coronary</strong> arteries and<br />
can be considered as a cause of myocardial ischemia. At present the data is not sufficient to<br />
delineate the borders of this phenomenon. It should be clarified if this finding is a separate<br />
entity or sign of other pathologies such as atherosclerosis or ectasia. In addition, more time is<br />
required for better determining the prognosis of the patients with this angiographic finding.<br />
54<br />
The relationship between androgen levels in men and different<br />
stages of heart failure<br />
Davoodi Gh, Borumand MA, Amirzadegan A, Raissi Dehkordi M, Salarifar M,<br />
Haji Zeinali AM and Paydari N<br />
Abstract<br />
Background: Previous studies have shown that Congestive Heart Failure (CHF) may<br />
have correlation with low androgen levels in men. Some experts have even proposed to<br />
treat CHF with exogenous androgens. This study was conducted to compare androgen<br />
levels in patients with and without heart failure scheduled for <strong>coronary</strong> angiography.<br />
Methods: Three pooled blood samples were taken from 515 consecutive male patients<br />
before angiography. Blood samples were checked for free testosterone (fT) with Enzymelinked<br />
immunosorbent assay and total testosterone (tT) and Dehydroepiandrosterone
sulfate (DHEA-S) with Radio immunoassay. Ejection Fraction (EF) was assessed<br />
according to echocardiographic and angiographic findings. Androgen levels were<br />
compared in patients with an EF
Results: Male and female patients' mean age was 60.06 & 60.68 years, respectively.<br />
Prevalence of single vessel disease (SVD), 2VD, 3VD and Left main (LMS) lesion in<br />
males was16.7%, 21.2%, 56.7% and 5.5%, respectively. Prevalence of these lesions in<br />
females was 23.3%, 25.1%, 48.2% and 3.4%, respectively. Involvement of major<br />
diagonal (MD) (p
circumferences and the risk of metabolic syndrome in 302 men aged
dehydroepiandrosterone sulfate(DHEA-S) with radioimmunoassay, lipid profile,<br />
lipoprotein a (Lpa), and CRP were taken from 529 consecutive patients before SCA.<br />
Angiographic results were reported by two cardiologists and checked for intra- and interobserver<br />
reliability, before they were interpreted as Gensini Score , and on the base of the<br />
number of involved segments. The relations were assessed with independent sample t-<br />
tests and Chi-square.<br />
Results: 16% of the patients had single, 22% had two, and 38% had three-vessel<br />
disease. 22% had normal angiograms or minimal lesions. Significant lesions in right<br />
<strong>coronary</strong> <strong>artery</strong>, left anterior descending, and left circumflex were seen in 53%, 69% and<br />
53% of the patients, respectively. fT, tT, and DHEA-S in patients with significant CAD<br />
vs. normal individuals were 6.70±3.21pg/mL, 16.80±6.94nm/L, and 113.55±72.73µg/dL<br />
vs. 7.10±3.57pg/mL, 15.83±7.23nm/L, and 111.86±74.32µg/dL, respectively,<br />
p>0.05).There was no correlation between Gensini Score or the number of involved<br />
segments and androgen levels. However, a significant negative correlation was found<br />
between fT, and Lpa and CRP(p=0.014 and p=0.017, respectively).<br />
Conclusion: There is no significant correlation between fT, tT, DHEA-S and presence<br />
or severity of CAD. Also, no correlation was found between androgen levels and lipid<br />
profile. However, CRP and Lpa levels negatively correlate with fT concentration.<br />
Hoseini K, SadeghianS and Mahmoodian M<br />
58<br />
Parental cardiovascular disease as a risk factor for acute<br />
<strong>coronary</strong> syndromes in adult offspring<br />
Tehran Heart Center, Medical Sciences/University of Tehran, Tehran, Iran<br />
Abstract<br />
Background: Whether parental cardiovascular disease confers increased event risk<br />
independent of other risk factors remains controversial. We investigate influence of<br />
parental cardiovascular disease as an independent predictor for acute <strong>coronary</strong><br />
syndromes in offspring and importance of maternal or paternal induced risk.<br />
Methods: Data originated from single center ischemic heart disease registry and<br />
consisted of 6399 patients with established ischemic heart disease, admitted between<br />
June 2004 to March 2006.<br />
Results: 1352(21.1%) patients had a positive family history of <strong>coronary</strong> <strong>artery</strong> disease.
Among 953 patients with verified family history, father had <strong>coronary</strong> <strong>artery</strong> disease in<br />
193(17.4%), mother in 215(19.4%), brother in 257(23.1%) and sister in 118(10.6%)<br />
patients. The mean age of clinical onset of ischemic heart disease in patients with only<br />
positive family history as a risk factor was significantly lower compare with that in the<br />
others (59.21±13.21 vs. 64.58±32.84, P
positioned in lateral vein of <strong>coronary</strong> sinus, RV lead in RV apex and RA lead in the<br />
appendage of RA inserted. The patients were followed for up to 6 months; and<br />
echocardiography, 6-min walking test, EKG analysis and clinical functional class were<br />
assessed. The patients were categorized into two groups of responders and nonresponders<br />
according to their clinical and paraclinical findings. The EKGs were taken<br />
immediately, one month and 3 months after CRT.<br />
Results: In responder group 50% of LBBB patterns were switched to RBBB patterns,<br />
while this percentage was 60% in non-responders. The percentage of R>S in lead V1 was<br />
53% in responders and 28% in non-responders, respectively. There was 25% of R>S in<br />
lead aVR in the responders and 0% in non-responders. These differences were<br />
statistically significant (P
Methods: 150 patients who had referred for <strong>coronary</strong> angiography were randomized into<br />
three groups with equal populations. The first group (DP) received intramuscular injection of<br />
5 mg diazepam + 25 mg promethazine. The second (M) received 0.2 mg/kg intravenous<br />
midazolam, and the third group (P) received 2cc intravenous distilled water. Vital signs and<br />
arterial blood O2 saturation were recorded in specifically-designed questionnaires.<br />
Results: There was no significant difference in pulse rate, respiratory rate, and mean<br />
systolic blood pressure between these groups. Diastolic blood pressure decreased in all<br />
groups after angiography, which was more significant in group M (p
TG, Cholesterol, LDL and HDL were measured. Noninvasive studies for CAD performed<br />
with resting ECG, exercise stress test and echocardiography. If these tests were positive<br />
myocardial perfusion scan performed and if it was positive we proceeded to <strong>coronary</strong><br />
angiography.<br />
Results: DM was found in 5.3 %, smoking in 14.7%, hypertension in 20.6%, cholesterol<br />
> 200 mg/dl in 39.9%, TG > 200 mg/dl in 18%, LDL > 160 mg/dl in 24.6% and HDL <<br />
40 mg/dl in 32.6%. 6.4% had ECG changes and 3% echocardiographic abnormalities in<br />
favor of ischemia. ETT was positive in 7.3% (51 individuals ,36 females and 15<br />
males)and myocardial perfusion scan was positive in 2.1 % of the total study<br />
population(15 individuals ,10 males and 5 females).Coronary angiography showed<br />
stenosis of <strong>coronary</strong> lumen(50-70 % ) in 8 patients (1.1%) and stenosis of >70 % in 4<br />
patient (0.6%).Only 1 patient had severe 3VD and none had left main disease. Others<br />
had SVD (5 patients) and 2VD (6 patients).<br />
Conclusion: We found a high rate of cardiovascular risk factors in sibling and<br />
offspring of patients with premature CAD. Determination of these risk factors and proper<br />
management may be beneficial. Noninvasive tests for CAD yield low true positive results<br />
and is not recommended in this population<br />
Keywords: premature <strong>coronary</strong> <strong>artery</strong> disease, Non-invasive tests, cardiovascular risk<br />
factors<br />
62<br />
Left ventricular ejection fraction by left ventriculography<br />
before or after <strong>coronary</strong> angiography: Correlation with<br />
echocardiography<br />
Kazemi Saeed A, Salarifar M, Haji Zeinali AM, Davoodi Gh, Amirzadegan A,<br />
Yamini Sharif A and Hakki Kazazi E<br />
Tehran Heart Center, Medical Sciences/University of Tehran, Tehran, Iran<br />
Abstract<br />
Background: Measurement of global left ventricular function is important in the<br />
follow-up of cardiovascular disease and is a good prognostic indicator in cardiac<br />
situation. Detection of ejection fraction made with ventriculography after <strong>coronary</strong><br />
angiography maybe decrease ejection fraction falsely because of cardio-depressant
effects of contrast media. The purpose of this study was to evaluate the effect of the<br />
angiographic contrast medium on left ventricular ejection fraction in patients undergoing<br />
<strong>coronary</strong> angiography.<br />
Methods: We categorized the patient population in two groups: group I (n = 1027)<br />
included patients whose ejection fraction was evaluated with ventriculography before<br />
<strong>coronary</strong> angiography and group II (n = 5612) was compromised of patients whose<br />
ejection fraction was evaluated with ventriculography after <strong>coronary</strong> angiography. We<br />
calculated the difference between ejection fraction in echocardiography and<br />
ventriculography in the two groups and then compared the mean of this difference<br />
between the two groups with independent T-test.<br />
Results: Mean difference between ejection fraction in echocardiography and<br />
ventriculography was 1.06 ± 9.83% in group I and 0.8 ± 10.47% in group II (p = 0.45).<br />
Conclusion: The injection of moderate amounts of contrast in <strong>coronary</strong> angiography<br />
does not cause significant changes in ejection fraction immediately after <strong>coronary</strong><br />
angiography compared with before left ventriculography. Keywords: Left ventricular<br />
ejection fraction, Ventriculography, Echocardiography<br />
63<br />
Cardiovascular morbidity in relation to educational level in<br />
patients with chest pain presentation<br />
Yamini Sharif A, Kazemi Saeed A, Sadeghian H, Alidoosti M,. Darabian C,<br />
Sahebjam M and Mahmoodian M<br />
Abstract<br />
Background: In many industrialized countries inverse associations have been reported<br />
between socioeconomic and educational status and the prevalence of morbidity and<br />
mortality from cardiovascular disease. The aim of this study was to investigate, in a<br />
developing country, the influence of educational level on the prevalence of <strong>coronary</strong><br />
<strong>artery</strong> disease and related risk factors in patients with chest pain at the time of admission.<br />
Methods: Data originated from single center ischemic heart disease registry and<br />
consisted of 7041 patients who presented with chest pain, carried out from June 2004 to
March 2006.<br />
Results: 515(8.1%) patients had high levels of academic education as high educational<br />
level. Males were found to have a higher educational level than females (P
ooms was excluded. Successful CPR was defined as a complete improvement of the<br />
patient’s condition without any residual sequel or complication. Early results were calculated<br />
immediately after CPR, after 24 hours and at discharge and were revealed as percentage of all<br />
resuscitated patients. Regarding CPR results patients were stratified into two groups:<br />
successful and unsuccessful CPR. All factors in these groups were compared.<br />
Results: Between January 2005 and March 2006, 577 patients (320 male and 257 female,<br />
Mean age: 65.24±13.66) were resuscitated. The most important etiology of the CPR were<br />
arrhythmia (36.7%), respiratory failure (30.3%), and homodynamic instability (25.0%).<br />
Overall, success rates after resuscitation, at 24 hours and at discharge were 51.0%, 40.0% and<br />
28.3%, respectively. CPR by various etiologies had significantly different success rates<br />
which are presented in table 1. The lowest success rates were seen in the homodynamic<br />
instability [after resuscitation] and asystol or bradicardia [at 24 hours and at discharge]. Age,<br />
sex, concurrent disease and serum pH were similar between groups. As it is shown in the<br />
table 2 upper GCS levels (>8), cardiac massage duration lower than 15 minutes and CPR<br />
duration
2.78<br />
4.87<br />
1.23<br />
1.27<br />
1.85<br />
2.49<br />
0.003<br />
0.007<br />
Atropine dose < 2 mg<br />
Serum potassium lower than 6 mEq/L<br />
resuscitation (Univariate Analysis) OR: Odds Ratio ; CI: Confidence Interval<br />
Table 1: Success rates in CPR by different etiology<br />
At<br />
Discharge<br />
13.5<br />
25.6<br />
43.1<br />
12.4<br />
30.4<br />
Success Rates (%)<br />
At 24 hours After Resuscitation<br />
20.4<br />
38.2<br />
34.7<br />
52.5<br />
61.5<br />
73.1<br />
18.5<br />
40.5<br />
43.8<br />
61.0<br />
Etiology<br />
Homodynamic instability<br />
Arrhythmia<br />
VF-VT<br />
Asystol or bradycardia<br />
Respiratory failure<br />
66<br />
Early clinical result of double endarterectomy and<br />
reconstruction combined with multiple <strong>bypass</strong> <strong>graft</strong>ing for<br />
severe <strong>coronary</strong> <strong>artery</strong> disease: A single institute experience<br />
Marzban M, Karimi AA, Ahmadi SH, Movahedi N, Abbasi K, SalehiOmran A,<br />
Davoodi S and Yazdanifard P<br />
Tehran Heart Center, Medical Sciences/University of Tehran, Tehran, Iran<br />
Abstract
Background: Coronary <strong>artery</strong> endarterectomy is a valuable adjunct to conventional <strong>bypass</strong><br />
<strong>surgery</strong> when attempting to revascularize “diffuse <strong>coronary</strong> <strong>artery</strong> disease “disease <strong>coronary</strong><br />
arteries. In this study we examined the early clinical outcome of double <strong>coronary</strong><br />
endarterectomy.<br />
Methods: Between January 2002 and 2006, 10136 patients underwent <strong>coronary</strong> <strong>artery</strong><br />
<strong>bypass</strong> that 221 of whom (2.1%) required endarterectomy and 20 cases (0.2%) required<br />
double endarterectomy. There were16 men (80%), ranging in age from 44 to 80 (average 58).<br />
All of 20 patients (100%) had angina preoperatively, which was Canadian cardiovascular<br />
society (ccs) class III or IV in13 patients. The average EF was42% and 4 patients (5%) had<br />
low EF (24 h) and cardiac arrest in one patient (5%). 15 patients of 19 (78%)<br />
were followed up for a mean of 21 months. There were 2 death (13%) five months post<br />
operatively both in cardiac cause. In left 13 patients, four (30%) were in angina class I by ccs<br />
and 8 patients (61.5%) were in class II and one patient was in class III. There was no post<br />
myocardial infarction.<br />
Conclusion: Although diffuse CAD is an important risk factor of CABG, but even in these<br />
patients, CABG adjunct to <strong>coronary</strong> endarterectomy is feasible and successful in symptom<br />
relief.<br />
67<br />
Non use of left internal mammary <strong>artery</strong>: It's contributing<br />
factors<br />
Tehran Heart Center, Medical Sciences/University of Tehran, Tehran, Iran<br />
Abstract<br />
Background: In our institute, as in most centers, the left internal mammary <strong>artery</strong><br />
(LIMA) is the first choice conduit for <strong>coronary</strong> <strong>artery</strong> <strong>bypass</strong> <strong>graft</strong>ing. The purpose of this<br />
study was to investigate the frequency of non-use of lima as a <strong>bypass</strong> conduit and it’s<br />
contributing factors.<br />
Methods: A total of 11000 consecutive patients who underwent CABG (isolated or<br />
combined) from February 2002 up to 2006 were reviewed. The demographic and<br />
contributing factors to non-use of LIMA identified from the data base and operation notes<br />
of patients.
Results: 351 patients of 11000(3.2%) didn’t receive Lima for CABG, 48.7%were in the<br />
first year of hospital practice, 27.1% in second year, 14.5% in 3 year,9.4% in the last year.<br />
The mortality rate of 11000(isolated and combined CABG) was 1.2%, but in study group was<br />
10.6%. 175 patients of 351(49.9%) were women while 26% of 11000 patients were<br />
women.114 patients of 351(32.5%) had diabetes, 4.8% had urgency CABG, 9.4% had normal<br />
LAD and 8.5% had low flow and unsuitable LIMA.0.6 % had left sided arteriovenous fistula,<br />
2.3% had previous CABG, 2.6% had left ventricle anurysm, 2.8% had copd, 4.6%had<br />
osteoprotic sternum and 4.3%had poor <strong>coronary</strong> vessels.<br />
Conclusion: In comparison with most centers the frequency of LIMA usage is acceptable,<br />
as the experience increases so does use of LIMA is increasing. In some groups of patients,<br />
such as those with huge left ventricular aneurysm with LAD involvement or patients with left<br />
sided AVF or when there is unrepairable damage to LIMA, non-use of LIMA is<br />
inevitable. Nevertheless, some patients still deprive of LIMA unreasonably.<br />
68<br />
nondiabetic patients: A comparative study<br />
Ahmadi SH, Alinejad B, Karimi AA, Marzban M, Abbasi , Salehi Omran A,<br />
Davoodi Gh and Abbasi SH<br />
Tehran Heart Center, Medical Sciences/University of Tehran, Tehran, Iran<br />
Abstract<br />
Background: We evaluated the impact of diabetes mellitus on in-hospital mortality and<br />
morbidity after CABG.<br />
Methods: From February 2002 through January 2006, 9163 patients (3094 diabetic and<br />
6069 non-diabetic) underwent isolated CABG at our center. Demographic and
preoperative data and postoperative in-hospital mortality and morbidity were compared in<br />
both diabetic and non diabetic groups. Univariate and multivariate analysis were<br />
performed to compare the results.<br />
Results: Diabetic patients in comparison with non-diabetics were older (mean age 59.6y<br />
vs. 57.9y), included more women (37.6 %vs. 19.4%), had more postoperative<br />
mediastinitis (0.7%vs. 0.2 %) , renal failure (0.8% vs. 0.3%), cardiac arrest (1.1% vs.<br />
0.7%), and in-hospital mortality (1.5%vs 0.5%) (p< 0.05). We found no significant<br />
differences in left main <strong>coronary</strong> <strong>artery</strong> disease (9.8% vs. 9.6%), postoperative prolonged<br />
ventilation (1.2% vs. 0.8%), and atrial fibrillation (6.3% vs. 5.6%) between two groups<br />
(p>0.05).There were also significant differences in hospital stay (mean 8.0 vs. 7.2 days),<br />
ICU stay (mean 40.8 vs. 38.5 hours), and mean aortic cross clamp and cardiopulmonary<br />
<strong>bypass</strong> times between diabetics and non-diabetics (44.38vs 42.95 min and 74.28 vs. 71.85<br />
min respectively) (p
Results: All patients were men with a mean age of 50.2± 9 years. The major causes of<br />
renal failure were primary hypertension in 25%, diabetes mellitus in 18%, and combined<br />
of these causes in 34%. The qualities of <strong>graft</strong>s were poor in 5 patients, moderate in 2<br />
patients and good in 2. Mean preoperative ejection fraction was 40.5%±15% (range 25%<br />
to 50 %). Cardiopulmonary <strong>bypass</strong> and aortic cross-clamp times were 80.2 ± 15 and 43.8<br />
± 10 minutes respectively. Intra aortic balloon pump was used for one patient. The<br />
complications were prolonged ventilation in one patient and pricardial effusion in another<br />
one. There was not early mortality. In long-term fallow up (mean time: 2.8 years) the late<br />
mortality rate was 33.3% (3 patients). The causes were infection and renal failure in 2<br />
patients, and end stage renal failure in one.<br />
Conclusion: Coronary <strong>artery</strong> <strong>bypass</strong> <strong>graft</strong>ing could be performed in dialysis –<br />
dependent patients with acceptable perioperative morbidity and mortality risks if there is<br />
a well-organized dialysis program.<br />
70<br />
The impact of low serum triglyceride on LDL-cholesterol<br />
estimation<br />
Ahmadi SH, Boroumand MA, Dibaj SM, Tajik P and Abbasi SH<br />
Tehran Heart Center, Medical Sciences/University of Tehran, Tehran, Iran<br />
Abstract<br />
Background: Most clinical laboratories directly measure serum triglyceride, total<br />
cholesterol and HDL and indirectly calculate LDL value using the Friedewald equation. This<br />
study was done assess the effects of low serum triglyceride on LDL estimation.<br />
Methods: Between October 2002 and October 2003, in a case-control study, 115 serum
samples (group A-case) were selected from patients with triglyceride level below 100mg/dl.<br />
Another group of 115, sex and age-matched cases were also selected for comparison (group<br />
B-control) who had triglyceride levels between 150-350 mg/dl. On each sample total<br />
cholesterol, triglyceride, HDL and LDL were directly measured in duplicate by enzymatic<br />
methods. LDL-C assay was based on 2-step (homogenous) selective degradation of non-LDL<br />
lipoproteins. LDL was also calculated using Friedewald equation.<br />
Results: In group A, calculated LDL was on average 12.17 mg/dl higher than measured<br />
LDL (CI 95% = 10.34 to 14mg/dl), while in group B, calculated LDL was about 1.48 mg/dl<br />
lower than measured LDL (CI 95% = -4.21to 1.25mg/dl). Comparing the calculated and<br />
measured LDL-C levels by paired t-test in group B showed no significant difference (P =<br />
0.285), but in group A the difference was statistically significant (P < 0.001). Using this<br />
modified equation the Pearson’s correlation coefficient between the two methods approaches<br />
0.976 and the average calculated LDL is only about 0.67 mg/dl less than measured LDL (CI<br />
95% = -0.72 to 0.85mg/dl) with no significant difference between the two methods<br />
(P=0.867).<br />
Conclusion: In patients with low triglyceride and undesirably high serum cholesterol<br />
levels, LDL-C should be either directly assayed or be calculated by a modified Friedewald<br />
formula. By using linear regression modeling we proposed a modified formula. Keywords:<br />
Triglyceride, Cholesterol, LDL, HDL, Friedewald equation<br />
71<br />
Twenty –four hours in-hospital mortality predictions in<br />
<strong>coronary</strong> <strong>artery</strong> <strong>bypass</strong> <strong>graft</strong>ing <strong>surgery</strong> patients<br />
Ahmadi SH, Karimi AA, Marzban M, Movahedi N, Abbasi K, Salehi Omran A,<br />
Soleymanzadeh Ardabili M and Yazdanifard P<br />
Abstract<br />
Background: The purpose of this study was to determine the factors which can help to<br />
predict risk of mortality in the first 24 hours of <strong>coronary</strong> <strong>artery</strong> <strong>bypass</strong> <strong>graft</strong>ing (CABG)<br />
because mortality in few hours of <strong>surgery</strong> is a disastrous event for surgeon and patients<br />
family.<br />
Methods: The study population consisted of 122 in-hospital mortality case (1.2%) from
9862 patients who underwent CABG, from February 2002 to February 2006 by the same<br />
group of surgeons in a referral center. one group, 36 patients of 122(about 29.5%) who<br />
passed away during 24 hours after <strong>surgery</strong> were compared to 86 patient (70.4%) who<br />
expired after the second day up to 30 days postoperatively. A set of data was gathered<br />
from <strong>surgery</strong> database of hospital and analyzed in univariate model. In- hospital mortality<br />
was considered all expired cases during first 30 days after <strong>surgery</strong>.<br />
Results: Among studied variables, only following factors proved to be significant<br />
previous PTCA, emergent and urgent status, intra aortic balloon pump use, perfusion<br />
time, postoperative stroke and comatous state. In addition, poor <strong>coronary</strong> vessels proved<br />
to be significant in 24 hour mortality.<br />
Conclusion: It seems that influencing factors in global in-hospital mortality such as<br />
BMI, diabetes mellitus, COPD, preoperative arrhythmia , ejection fraction, history of<br />
previous CABG and resuscitation, were not significant in our study regarding the<br />
comparison of 24 hours postoperative and in-hospital mortality, although poor quality of<br />
<strong>coronary</strong> vessels was an important factor in this period of time .<br />
72<br />
Evidence for a higher mortality in women after <strong>coronary</strong><br />
<strong>artery</strong> <strong>bypass</strong> <strong>graft</strong> <strong>surgery</strong><br />
Sadeghian S, Karimi AA, Nemateepoor E, Lotfi-Tokaldany M, Soleymanzadeh<br />
Ardabili M, Sasanpoor P and Rahimi-Dehkordi N<br />
Abstract<br />
Background: Surgical outcomes have shown higher operative mortality in younger<br />
women compare with men at a similar age after Coronary Artery Bypass Graft <strong>surgery</strong><br />
(CABG). We compared multiple causes of procedural and early postoperative mortality<br />
between different age groups of men and women.<br />
Methods: 9857 patients who underwent CABG were studied between 2001 and 2006.<br />
All data were collected from the heart center data base. The mortality rate of male and
female patients was compared for a variety of risk factors. Risk-adjusted mortality rate<br />
were obtained by stepwise logistic regression.<br />
Results: There were 7304 men (mean age: 57.74±10.43 years) and 2553 women (mean<br />
age: 60.28±9.61years) in this study. The mortality rate of CABG in our center was 1.2%.<br />
Compared with men, more women had comorbidities and risk factors. In hospital<br />
mortality rate was higher in women and sex differences in mortality rate were remarkable<br />
among younger and older patients. Women 70 years of age were<br />
respectively 4.1 and 3.7 times more likely to die than men and in the other age groups<br />
women were 2.3 to 2.6 times more likely to die than men. A sex difference in diabetes<br />
was more marked among younger patients (women Vs men: OR=3.1, P
Results: The mean age of total population was 57.5r10.3 years and 64.1% of these patients<br />
were male. The prevalence of <strong>coronary</strong> <strong>artery</strong> disease (CAD) in them was 84.2%. Besides,<br />
Frequency of opium consumption was 13.4% in all patients and 19.7% in males.<br />
Notably,93.4% of opium users were male and 5.7% were female .The mean duration of<br />
opium consumption was 138.7 months and daily amounts via smoking and/or oral route<br />
varied from 0.03gram/year to 60gram/year. According to the angiographic findings,<br />
prevalence of CAD was higher in opium users (93.4% versus 82.7%, p
costs were calculated as mean direct costs multiplied by the number of patients tested.<br />
Results: Tables 1and 2 present the number of important invasive cardiac procedures and<br />
their mean charge per year in Iran and United States, respectively.<br />
Conclusion: This study is the first to estimate the costs of invasive cardiac procedures in<br />
Iran. Tables 1 and 2 show that despite the higher prevalence of <strong>coronary</strong> <strong>artery</strong> disease<br />
(CAD) in Iran as compared to that in United States, the mean amount of costs of cardiac<br />
catheterization, CABG and PTCA are 30, 16 and 10 times higher in the United States. So<br />
even after adjustment of the prevalence of CAD in these two countries, the rate of cardiac<br />
catheterization, CABG and PTCA may increase by at least 3, 4 and 9 times in the future in<br />
Iran, which could lead to at least a 60–fold increase in treatment costs. This emphasizes the<br />
need for insurance organizations to formulate the budget that<br />
must be allocated for this purpose.<br />
75<br />
Table1.Estimated direct costs of some invasive cardiac procedures per year, Iran
*Including temporary, permanent and 3 chamber<br />
**Including AICD and ICD 3 chamber ***Openheart<br />
valvuloplasty with replacement<br />
Table2.Estimated direct costs of some invasive cardiac procedures per year, USA<br />
*Including temporary, permanent and 3 chamber<br />
** Including AICD and ICD 3 chamber ***Open-heart valvuloplasty without<br />
replacement<br />
76<br />
Results of noninvasive test compared with results of<br />
angiography in young patients<br />
Sadeghian S, Hakki Kazazi E, Poorhosseini HR, Zoroofian A and Roozkari M<br />
Tehran Heart Center, Medical Sciences/University of Tehran, Tehran, Iran<br />
Abstract<br />
Background: On the basis of previous studies cardiac perfusion scan, compared with<br />
standard exercise testing, has more sensitivity and specificity especially in young women.
The purpose of present study was to compare results of these two tests with results of<br />
angiography in young adults.<br />
Methods: 1120 Consecutive patients with positive exercise test (ETT) or myocardial<br />
perfusion scan (MPS) and age < 50 years who had undergone <strong>coronary</strong> angiography over<br />
a period of two years were included in the study. We categorized these patients in two<br />
groups on the basis of sex.<br />
Results: From 204 women with positive ETT, 46% (94) and from 158 women with<br />
positive MPS 46% (73) had <strong>coronary</strong> <strong>artery</strong> disease (CAD) in angiography. Also from<br />
450 men with positive ETT, 74% (335) and from 298 men < 50 years with positive MPS<br />
74.5% (222) had CAD on angiography. After the exclusion of stenosis < 50% in <strong>coronary</strong><br />
arteries, 30% (62) of women with positive ETT, 37% (59) of women with positive MPS,<br />
65% (292) men with positive ETT and 60% (180) of men with positive MPS had CAD in<br />
angiography.<br />
Conclusion: Based on studies, previous MPS has a higher sensitivity than exercise test.<br />
However, for the diagnosis of <strong>coronary</strong> <strong>artery</strong> disease in this study, MPS led to the same<br />
results as exercise test; this may be due to an error in the accomplishment or in the report<br />
of the results.<br />
77<br />
The association between left main <strong>coronary</strong> <strong>artery</strong> disease and<br />
ischemic heart disease risk factors<br />
Darabyan C, Amirzadegan AR, Davoodi Gh, Sadeghian H, Kazemisaeid A ,<br />
Raissi Dehkordi M and Fallah N<br />
Tehran Heart Center, Medical Sciences/University of Tehran, Tehran, Iran<br />
Abstract
Background: Left main trunk disease (LMTD) is an important factor contributing to<br />
the severity of <strong>coronary</strong> <strong>artery</strong> disease (CAD) and negatively affects patients' survival.<br />
Previous studies have shown no obvious risk factor for this type of involvement. In this<br />
study, we aimed to find any association between established risk factors and LMTD.<br />
Methods: 8230 patients who had undergone selective <strong>coronary</strong> angiography (CAG)<br />
were enrolled in this study. Lipid profile, lipoprotein (a), and homocyteine were<br />
measured before <strong>coronary</strong> angiogram Risk factors for ischemic heart disease were also<br />
recorded from our angiography database. Patients were divided into three groups based<br />
on their CAG results: 1) CAD plus significant LMTD, 2) CAD without significant<br />
LMTD, and 3) normal coronaries. ANOVA and multivariate logistic regression tests<br />
were used for statistical analysis between CAD plus significant LMTD vs. the two other<br />
groups<br />
Results: Total cholesterol (P=0.03), HDL (P=0.01), LDL (P=0.04), LP (a) (P=0.01)<br />
were significantly higher in patients with LMTD versus normal <strong>coronary</strong>. Also, cigarette<br />
smoking, hypertension, diabetes mellitus, male gender and higher age (P
Background: CRP is a sensitive reactant released during tissue injury and<br />
inflammation such as ischemic events in acute <strong>coronary</strong> syndrome. We tried to evaluate<br />
the predictive value of CRP for outcome after CABG and introduce it as a risk factor for<br />
<strong>surgery</strong>.<br />
Methods: Pre-operative CRP serum level was measured in a series of 145 acute<br />
<strong>coronary</strong> syndrome Patients who underwent CABG for the first time and without any<br />
other thoracic procedure.<br />
Results: Our study consisted of 92 males and 53 females. During the in - hospital stay, 2<br />
patients ( 1.4% ) died, 3 patients ( 2.1% ) suffered bleeding while perioperative MI,<br />
mediastinitis and cerebrovascular events did not take place. Preoperative CRP correlation<br />
was statistically significant with age ( P: 0.049 ), hypercholesterolemia ( P: 0.007 ), preoperative<br />
EF ( P: 0.027 ) and parsonnet score<br />
( P: 0.000 ).<br />
Conclusion: Increased pre-operative CRP in association with other risk factors, can<br />
predict CABG outcome and operation risk in acute <strong>coronary</strong> syndrome patients.<br />
79<br />
Developing a <strong>surgery</strong> database: design and operation<br />
Abbasi K, Marzban M, Ahmadi SH,Karimi AA, Davoodi S, Salehi Omran A,<br />
Movahedi N and Soleymanzadeh M<br />
Tehran Heart Center, Medical Sciences/University of Tehran, Tehran, Iran<br />
Abstract<br />
Background: The great number of patients referring to our center leads to a great amount<br />
of data, while its classification and categorization seems to be the first priority for research<br />
and management purposes.<br />
Methods: The <strong>surgery</strong> databank in our center first developed in June 2003, and the basic
data collection form was prepared by Iranian cardiac surgeons' society. This procedure is<br />
conducted by two trained physician and a computer operator. Data collection forms are first<br />
filled up at patient’s bedside (defining risk factors and Canadian score) and then after<br />
discharge to determine their postoperative variables. This information set is then transferred<br />
to SPSS software program by the operator. 10% Of the surveyed surgical files are checked<br />
randomly to determine the probable source of fault. Cleaning of raw date is done bimonthly<br />
and a final report of <strong>surgery</strong> data bank is reported to research committee every 6 month.<br />
Conclusion: An appropriate method of transforming and computerizing data will be a<br />
great help to shorten research period and make the researcher work much easier. It is also<br />
suggested that all people involving databank (surgeons, managers and planners,<br />
Epidemiologists and statisticians) can access via an intrahospital network.<br />
80<br />
Mediastinitis after <strong>coronary</strong> <strong>artery</strong> <strong>bypass</strong> <strong>surgery</strong> (CABG),<br />
an evaluation of effect of different factors on developing<br />
mediastinitis after CABG in more than 9000 cases<br />
Tehran Heart Center, Medical Sciences/University of Tehran, Tehran, Iran<br />
Abstract<br />
Background: We aimed to evaluate the impact of different factors on developing post-<br />
CABG mediasinitis.<br />
Methods: A retrospective study was done on 9201 cases of CABG between January<br />
2002 and February 2006. The total number of the cases of sternal wound infection
(mediastinitis) was 44(about 0.5%) with mean age of 60.1 years. All the cases of<br />
mediastinitis divided into 2 parts: superficial sternal wound infection (group A-23 case)<br />
and deep sternal wound infection (group B-21 case).<br />
Results: In group 1, 74.5% were male and 25.5% female versus 47.7%male and<br />
52.3%female in group 2(mediastinitis), and this difference was significant (P=0.0001).<br />
Different factors such as BMI (Body Mass Index) and cigarette smoking and type of<br />
antibiotic prophylaxis had no significant impact on the incidence of mediastinitis as well<br />
as hypercholesterolemia, preoperative ejection fraction and peripheral vascular disease,<br />
but diabetes(59.1% versus 40.9%)and hypertension(90.9% versus 49.7%)were two<br />
significant factors in group 2 and 1 respectively. In-hospital mortality rate in CABG<br />
group 1 was 1.1% and 9.1% for mediastinitis group. There was a significant difference in<br />
rate of bleeding and reexploration in mediastinitis group in comparison with group<br />
1(13.6% vs. 1.1%).Positive sternal culture with S. aureus as a most common cause was<br />
seen in 72.1% in mediastinitis group.<br />
Conclusion: Rate of mediastinitis was about 0.5% that 0.23% were deep sternal wound<br />
infection. Mortality was high in mediastinitis group. It was shown that the risk of<br />
mediastinitis was higher in females. Furthermore, diabetes and hypertension had a<br />
significant role (P=0.0001) in the incidence of mediastinitis. It seems that there was an<br />
association between mediastinitis and reoperation for bleeding.<br />
81<br />
Comparison of short- and long-term outcomes between<br />
sirolimus eluting stents and paclitaxel eluting stents<br />
Alidoosti M, Salarifar M, Haji Zeinali AM, Kassaian E, Atashpar S and Raissi<br />
Dehkordi M<br />
Tehran Heart Center, Medical Sciences/University of Tehran, Tehran, Iran<br />
Abstract<br />
Background: Both sirolimus- and paclitaxel-eluting stents have demonstrated superior
efficacy over bare-metal stents, but recently published trials have not shown one drugeluting<br />
stent to be superior to the other. The aim of this study is to compare short- and<br />
long-term outcomes between these two groups.<br />
Methods: The data were collected from our registry for interventional cardiology. From<br />
April 2003 to September 2005, a total of 2971 patients underwent percutaneous <strong>coronary</strong><br />
intervention (PCI). Patients with primary and multivessel PCI were excluded Finally,<br />
Cypher and Taxus were used in 471 and 109 patients, respectively, but their usage has<br />
been regularly increased thereafter.<br />
Results: Patients in Cypher vs. Taxus group had more frequently presented with stable<br />
angina (50.3% vs. 34.3%, p=0.02), and less with myocardial infarction (20.3% vs.<br />
32.8%,p=0.037). Baseline characteristics such as diabetes were similar between these<br />
groups. Total occlusions and type B2/C lesions were more frequently treated with Taxus<br />
compared to Cypher(9% vs. 3%, p=0.04, 78.8% vs. 74.2%, p=0.04). The effect of<br />
confounders was fixed using stratified statistical method. Procedural and clinical success<br />
rates were not significantly different between Cypher and Taxus(100% vs. 98%, p=0.08<br />
and 97% vs. 94%, p=0.2). Intra-hospital complications were similar between these<br />
groups, too. At 9 month follow-up, cardiac mortality occurred in 2 patients (3.7%) in<br />
Taxus, but none of patients in Cypher group (p=0.056). Rate of major adverse cardiac<br />
events (MACE) at nine month follow-up was 2.9% in Cypher and 3.7% in Taxus group<br />
(p=0.7).<br />
Conclusion: There is no significant difference in procedural success rate, intra-hospital<br />
and late outcomes and major adverse cardiac events between Cypher and Taxus stenting.<br />
82<br />
Comparison of outcomes of percutaneous <strong>coronary</strong><br />
intervention on proximal versus non-proximal left anterior<br />
descending <strong>coronary</strong> <strong>artery</strong>, proximal left circumflex and<br />
proximal right <strong>coronary</strong> <strong>artery</strong><br />
Tehran Heart Center, Medical Sciences/University of Tehran, Tehran, Iran<br />
Abstract<br />
Background: Lesions in proximal left anterior descending <strong>coronary</strong> <strong>artery</strong> (LAD) may
develop more restenosis after angioplasty than stenoses in other <strong>coronary</strong> segments.<br />
Thus, we compared outcomes of percutaneous <strong>coronary</strong> intervention (PCI) on proximal<br />
LAD vs. proximal left circumflex (LCX) or right <strong>coronary</strong> <strong>artery</strong> (RCA) (study 1) and<br />
proximal versus non-proximal LAD (study 2).<br />
Methods: From 1737 patients in our database who had undergone PCI, those with<br />
multivessel and primary PCI, and total occlusion were excluded. Study 1 and 2 were<br />
conducted on 515 and 652 patients, respectively and baseline characteristics and shortand<br />
long-term outcomes were compared within groups.<br />
Results: In patients with PCI on proximal LAD vs. proximal RCA or LCX, diabetes<br />
mellitus, smoking, multivessel disease and prior PCI were less frequent(p
Mehtods: This study was conducted on 2023 patients, who had undergone 2296<br />
procedures of direct stenting or stenting with predilation between April 2003 and March<br />
2005. Patients with multivessel percutaneous <strong>coronary</strong> intervention (PCI) were included<br />
only if the procedures on attempted lesions were entirely direct or predilation type. Then,<br />
PCI outcomes were compared between Direct and Predilation groups.<br />
Results: Direct stenting was conducted on 961 patients (47.5%).Patients in Direct<br />
versus Predilation group had more frequently presented with stable angina (p
cardiac death, myocardial infarction, revascularization) of drug-eluting stents (DES) with<br />
Bare metal stents (BMS).<br />
Methods: Using our angioplasty database, 267 DES and 535 BMS patients who<br />
underwent angioplastic procedure were selected. Thereafter, success rate and adverse<br />
outcomes after 12-months follow-up were assessed.<br />
Results:Procedural success rate was significantly higher in DES group (p=0.015), while<br />
procedural complication was significantly greater in BMS group (p=0.003). In-hospital<br />
complications and mortality rate were equal in two groups. Number of patients with<br />
previous PCI procedure was significantly greater in DES group (12.3% versus 7.1%)<br />
(p=0.014) due to occurrence of more restenotic lesion. Involvement of RCA and LCX<br />
territory was more prevalent in BMS, while involvement of LAD territory was<br />
significantly more frequent in DES group (p
<strong>artery</strong> disease. However, the pattern of Lp (a) distribution in various racial and genetic<br />
groups has been found to be different. Furthermore, the association of Lp (a) and the<br />
severity of <strong>coronary</strong> <strong>artery</strong> disease in different population has not been clearly assessed.<br />
This study has been done to determine the relationship between Lp (a) and the severity of<br />
<strong>coronary</strong> <strong>artery</strong> stenosis in an Iranian population.<br />
Methods: Between July 2004 and March 2005, in Tehran Heart Center, 826 patients<br />
who had been candidates for angiography, were included. The severity of their <strong>coronary</strong><br />
<strong>artery</strong> stenosis was assessed through Gensini score. At the first part of the study, for<br />
checking interobserver reliability, 60 angiographies were reported and their Gensini<br />
scores were determined by two cardiologists. During hospitalization, Lp (a), triglyceride,<br />
cholesterol, high density lipoprotein, low density lipoprotein and quantitative C reactive<br />
protein levels were measured and their correlation with <strong>coronary</strong> <strong>artery</strong> stenosis were<br />
assessed.<br />
Results: Among 826 participants, 510(62%) patients were male and 316 (38%) were<br />
female. Coronary angiography was normal in 283(34%), while showed atherosclerosis in<br />
543(66%) patients. Mean Lp (a) levels in both normal and atherosclerotic participants<br />
showed a significant difference (P
embolism and patent foramen ovale (PFO).<br />
Methods: There were two symptomatic patients (29 and 47 years old) who underwent<br />
percutaneous transcatheter closure of PFO after at least two events of cerebral ischemia;<br />
one embolic event had occurred under antiplatelet therapy. For both patients Amplatzer<br />
PFO occluder measuring 25 mm in diameter were used. Complete occlusion by color<br />
Doppler and transesophageal contrast echocardiography investigation were achieved in<br />
both after the procedure and at 3 months follow-up after implantation. Mean fluoroscopy<br />
time was 16.7 minutes.<br />
Results: Percutaneous transcatheter closure was technically successful in both patients<br />
(100%). No residual shunt was seen in the end of procedure and at follow-up. In-hospital<br />
follow-up was uneventful. At a mean follow-up of 3 months no recurrent embolic<br />
neurological events was observed.<br />
Conclusion: Transcatheter closure of PFO with Amplatzer PFO occluder devices is a<br />
safe and effective therapy for patients with previous paradoxical embolism PFO.<br />
Percutaneous closure is associated with a high success rate, low incidence of hospital<br />
complications, and freedom of cerebral ischemic events.<br />
15 congress of the Iranian heart association, 2006, Iran<br />
87<br />
Interventional closure of patient foramen ovale with amplatzer<br />
PFO occluder in patients with paradoxical cerebral embolism<br />
Haji Zeinali AM and Ghasemi M<br />
Tehran Heart Center, Medical Sciences/University of Tehran, Tehran, Iran<br />
Abstract<br />
Background: Balloon angioplasty for coarctation of the aorta (CoA) in adults, though<br />
promising, is sometimes limited by significant residual gradient (>20 mm Hg). Few<br />
studies available have reported on use of balloon-expandable stents in such a situation.
We evaluated the use of self-expandable stents in patients with native coarctation.<br />
Methods: 5 hypertensive patients (age 16 to 27 years) with native CoA and peak<br />
systolic gradient [PSG]>40 mmHg underwent stent implantation. Balloon predilation was<br />
done and self-expandable nitinol aortic stents (optimed) were implanted in all patients.<br />
Results: Peak systolic gradient decreased from 55r15 (40 to 75) mmHg to 5r2 (3 to 7)<br />
mmHg after angioplasty. Nitinol stents were easier to deploy and conformed better to<br />
aortic anatomy compared with balloon-expandable stents. The diameter of the coarcted<br />
segment increased from 3r1 mm to 16r2 mm. There was no any complication in our<br />
series. On 3 to 6 months follow up all the implanted stents remained in their original<br />
position and none showed evidence of fracture. Significant improvement in hypertension<br />
was seen in 4 of 5 of the patients.<br />
Conclusion: Stent implantation is safe and effective in improving for CoA. Selfexpandable<br />
stents were easier to implant, adapted better to the wall of the aorta, and in<br />
most patients had similar efficacy in reducing coarctation as surgical repair.<br />
88<br />
Echocardiographic predictors of left atrial appendage<br />
contraction flow velocity<br />
Sahebjam M, Salarifar M, Davoodi Gh, Amir Zadegan A and Sadeghian H<br />
Tehran Heart Center, Medical Sciences/University of Tehran, Tehran, Iran<br />
Abstract<br />
Background: Low left atrial appendage (LAA) contraction velocity is a known<br />
important predictor of LAA thrombus formation in mitral valve stenosis (MS), but its<br />
echocardiographic predictors, especially in patients with normal sinus rhythm (NSR), are<br />
not completely established. We, therefore, designed this study to assess the
echocardiographic predictors of LAA velocity.<br />
Methods: We studied 52 (35 F, 17 M, mean age 46 yrs) consecutive patients with MS<br />
and NSR who had been referred to our echocardiography lab for transesophageal<br />
echocardiography. The patients with more than moderate Mitral regurgitation and aortic<br />
valve disease were excluded. Transthoracic and transesophageal echocardiography were<br />
performed on all cases, and we measured LAA velocity , left atrial size , mitral valve<br />
peak and mean diastolic gradient, mitral valve area(MVA) , mitral valve Wilkins score,<br />
and left ventricular ejection fraction(LVEF) .<br />
Results :The mean LAA contraction velocity ( ±SD ) was 23.3 cm/s (±10.8 ), ranging<br />
from 9.0 cm/s to 54 cm/s .The mean LA size ( ±SD) was 47.3 mm (± 7.8 ). Mean<br />
MVA (±SD) was 1.07± 0.30 cm2, and mean LVEF was 50.3. The mean mitral valve peak<br />
and mean gradient (mmHg) were 9.7 and 16.9 respectively. In our study, the most<br />
important correlation was that between LAA velocity and MVA (r = 0.56 , P value =<br />
0.000), and there was also significant negative correlation between LAA velocity and LA<br />
size (r = - 0.458 , P value = 0.01) . MVA ” 1.0 cm2 and LA size > 40 mm had sensitivity<br />
equal to 71%, 89% and specificity of 64% and 52% respectively, for determination of<br />
LAA velocity ” 30 cm/s .There was no significant correlation between the other evaluated<br />
parameters and LAA velocity.<br />
Conclusion: MVA and LA size which are measurable by transthoracic<br />
echocardiography, can be used as predictors of LAA contraction velocity in patients with<br />
MS and NSR.<br />
Keywords: Left atrial appendage, Mitral valve stenosis, Transesophageal<br />
echocardiograph<br />
Magnesium infusion and its relationship with the incidence of<br />
post <strong>coronary</strong> <strong>artery</strong> <strong>bypass</strong> <strong>graft</strong>ing arrhythmias<br />
89<br />
Najafi M, Haghighat B, Ahmadi H, Soltaninia H, Ghiasi A, Mohammadali B,<br />
Fallah N and Fayazzadeh E<br />
Tehran Heart Center, Medical Sciences/University of Tehran, Tehran, Iran<br />
Abstract
Background: Atrial and ventricular arrhythmias are among the most common<br />
complications following <strong>coronary</strong> <strong>artery</strong> <strong>bypass</strong> <strong>graft</strong>ing (CABG). Previous studies have<br />
demonstrated that serum magnesium (Mg) levels decrease following CABG, especially<br />
after cardiopulmonary <strong>bypass</strong> (CPB). In the current study, we evaluated the prophylactic<br />
effect of Mg infusion on post-CABG arrhythmias.<br />
Method: Three hundred forty five patients, candidates for isolated <strong>coronary</strong> <strong>artery</strong><br />
<strong>bypass</strong> <strong>graft</strong>ing (CABG) with normal renal function, were randomly divided into two<br />
groups. Group A (case; 48.1%) received 2 g of Mg from induction of anesthesia to<br />
cardiopulmonary <strong>bypass</strong> (CPB) at the beginning and 8 g following CPB to 24h thereafter.<br />
In group B (control; 51.9%), no supplemental Mg was administered. Mg serum levels<br />
were measured in all the patients four times (at the onset of induction, and hours 0, 24,<br />
and 48 after ICU admission). Patients were then followed for developing cardiac<br />
arrhythmias until their discharge from the hospital.<br />
Result: Seventy-nine patients (22.9%) developed post-operative arrhythmia (i.e. AF in<br />
34 [9.9%]; other supraventricular arrhythmia in 23 [6.7%]); and ventricular arrhythmias<br />
in 47 [13.6%] patients). Except for the first occasion (induction time), there were<br />
significant statistical differences in Mg serum levels in the subsequent three<br />
measurements (p
underwent isolated <strong>coronary</strong> <strong>artery</strong> <strong>bypass</strong> <strong>graft</strong>ing at our center. The patients'<br />
preoperative, operative and postoperative data were reviewed respectively. The duration<br />
of dialysis ranged from 1 to 75 months (mean 18.4 ± 12.5 months). All of the patients<br />
were on hemodialysis which was scheduled on the day before <strong>surgery</strong>, and<br />
their usual hemodialysis was carried out on the 2 nd postoperative day.<br />
Results: All the patients were men with a mean age of 50.2 ± 9 years. The major causes<br />
of renal failure were primary hypertension in 25%, diabetes mellitus in 18%, and a<br />
combination of these causes in 34%. The qualities of the <strong>graft</strong>s were poor in 5 patients,<br />
moderate in 2 patients and good in 2. Mean preoperative ejection fraction was<br />
40.5%±15% (range 25% to 50%). Cardiopulmonary <strong>bypass</strong> and aortic cross-clamp times<br />
were 80.2±15 and 43.8±10 minutes, respectively. Intra-aortic balloon pump was used for<br />
one patient. The complications were prolonged ventilation in one patient and pericardial<br />
effusion in another one. There was no early mortality. Long-term follow up (mean time:<br />
2.8 years) the late mortality rate was 33.3% (3 patients). The cases were infection and<br />
renal failure in 2 patients, and end stage renal failure in one.<br />
Conclusion: Coronary <strong>artery</strong> <strong>bypass</strong> <strong>graft</strong>ing could be performed in dialysis-dependent<br />
patients with acceptable preoperative morbidity and mortality risks if there is a wellorganized<br />
dialysis program.<br />
Keywords: Hemodialysis, <strong>coronary</strong> <strong>artery</strong> <strong>bypass</strong> <strong>graft</strong><br />
91<br />
Late outcomes in patients with uncorrected moderate mitral<br />
regurgitation at the time of isolated <strong>coronary</strong> <strong>artery</strong> <strong>bypass</strong><br />
Davoodi S, Gholami MH, Dadashi Y, Mirhosseini M, Jalalmanesh F, Javadpour J<br />
and Madani Civi M<br />
Tehran Heart Center, Medical Sciences/University of Tehran, Tehran, Iran<br />
Abstract<br />
Background: Mitral valve intervention combined with <strong>coronary</strong> <strong>artery</strong> <strong>bypass</strong> <strong>surgery</strong><br />
is inevitable in the case of severe mitral regurgitation in patients with <strong>coronary</strong> <strong>artery</strong>
disease, but the best treatment protocol for patients with a moderate degree of mitral<br />
regurgitation is under debate. We evaluated the progress of mitral regurgitation after<br />
isolated <strong>coronary</strong> <strong>artery</strong> <strong>bypass</strong> <strong>surgery</strong> in cases of ischemic mitral regurgitation.<br />
Method: The study was conducted between June 1998 and Oct 2004. Fourteen patients<br />
(85% men, with a mean age of 56 years, a mean ejection fraction of 39.3%, and a mean<br />
New York Heart Association class of 2.53) with preoperative diagnoses of moderate<br />
degree ischemic mitral regurgitation (Grade 2 mitral regurgitation on a scale of 0 to 4)<br />
and <strong>coronary</strong> <strong>artery</strong> disease underwent isolated <strong>coronary</strong> <strong>artery</strong> <strong>bypass</strong> <strong>surgery</strong>. Patients<br />
were followed up at a mean of 48 months and an echocardiographic evaluation was done<br />
to determine the progress of the mitral disease.<br />
Result: In the postoperative period the mean ejection fraction was 44.6% and the mean<br />
functional capacity of the patients was 1.31. Mitral regurgitation regressed to a mild<br />
degree in 57.1% of the patients. Grade of MR was unchanged after CABG in 5 (35.7%)<br />
patients with grade 2 ischemic MR. <strong>Post</strong> CABG-MR progression was present in 1 (7.2%)<br />
patient. No patient required subsequent mitral valve operation or other procedures in long<br />
term follow up. The 30-day operative mortality rate was 0%.<br />
Conclusion: We conclude that in patients with moderate MR isolated CABG (without<br />
mitral valve replacement or repair) suffices as it produces dramatic improvement in<br />
ejection fraction and in degree of MR with good long-term survival.<br />
Keywords: Ischemic mitral regurgitation, <strong>coronary</strong> <strong>artery</strong> <strong>bypass</strong> <strong>graft</strong>, late outcome<br />
92<br />
The adverse effects of milrinone in the elderly patients who<br />
underwent CABG<br />
Davoodi S, Mirhosseini SM, Gholami MH, Dadashi Y, Jalalmanesh F, Mehraein<br />
A, Javadpour J and Akbarnejad M<br />
Abstract<br />
Background:The phosphodiesterase inhibitors are currently available to produce both<br />
positive inotropic effects and vasodilation. Milrinone, as one of the major forms of this<br />
group of agents, increases cardiac output, while it decreases pulmonary <strong>artery</strong> pressure,<br />
pulmonary vascular resistance and systemic vascular resistance. Although milrinone is<br />
generally accepted and used to treat young patients with high pulmonary <strong>artery</strong> pressure,
using this drug in elderly patients is still under debate.<br />
Method: We studied the effect of milrinone in a group of old patients with high<br />
pulmonary <strong>artery</strong> pressure. In 5 cases who underwent CABG, intravenous milrinone was<br />
administered to overcome the raised pulmonary <strong>artery</strong> pressure. All the patients were<br />
above 65 yrs of age; they comprised 3 males and 2 females with an ejection fraction of<br />
35-65%. None of the patients had renal failure. Milrinone was started after weaning off<br />
CPB. The initial loading dose was 50 micrograms/kg given over 20 minutes, followed by<br />
a maintenance dose of 0.50 micrograms/kg/min. Hemodynamic data were recorded<br />
before and after the drug injection.<br />
Results: In response to the therapy, pulmonary <strong>artery</strong> pressure decreased, heart rate<br />
increased while severe hypotension occurred in all the cases with a mean systolic<br />
pressure of less than 65 mmHg. To increase blood pressure, electrolyte imbalances, blood<br />
gas disequilibrium and hypokalemia were assessed and corrected properly. Several<br />
medical manipulations were performed, but none of them was effective. At the last step,<br />
we discontinued milrinone, which raised the blood pressure to the normal level in all the<br />
patients, while it did not have any adverse effect on pulmonary <strong>artery</strong> pressure.<br />
Conclusion: Our data showed that although milrinone is useful in decreasing<br />
pulmonary <strong>artery</strong> pressure, hypotension induced by this drug is common, especially in the<br />
elderly group. One should keep this in mind and treat the probably observed hypotension<br />
after milrinone therapy with discontinuation of the drug. Further studies are needed to<br />
confirm these findings. Keywords: CABG, milrinone, elderly patients<br />
93<br />
Correlation between net atrioventricular compliance and<br />
pulmonary <strong>artery</strong> pressure in mitral stenosis<br />
Sahebjam M, Salarifar M, Sadeghian H and Sadeghian S<br />
Tehran Heart Center, Medical Sciences/University of Tehran, Tehran, Iran<br />
Abstract<br />
Background: There are diverse data about the impact of net atrioventricular<br />
compliance (Cn) measured by Doppler echocardiography on systolic pulmonary <strong>artery</strong><br />
pressure (PAP) in patients with mitral valve stenosis. We, therefore, planned this study to
assess the relation between Cn and PAP.<br />
Method: Thirty-six patients (24 F, 12 M, mean age: 47.8y) with mitral valve stenosis<br />
were examined by Doppler echocardiography. Our exclusion criteria were more than<br />
mild mitral regurgitation, aortic valve disease, and atrial fibrillation rhythm. Cn was<br />
calculated from the ratio of effective mitral valve area (Continuity equation) and E wave<br />
downslope (Flachskampf formula). PAP was derived from the tricuspid regurgitant jet<br />
velocity with the modified Bernoulli equation and assuming right atrial pressure base on<br />
inferior vena cava diameter and its respiratory variation.<br />
Results: Mean (±SD) mitral valve area by pressure half-time was 1.48 (±0.36) cm2, and<br />
mean gradient was 7.8±4.0 mmhg. Cn ranged from 1.8 to 12.2 (mean±SD=5.28±2.55),<br />
and PAP ranged from 27 to 80mmhg (mean±SD=43±10.7). There was a statistically<br />
important negative correlation between Cn and PAP (r=-0.367, p=0.03), but the most<br />
significant correlation in our study was that between the mean mitral valve gradient and<br />
PAP (r=784, p=0.00).<br />
Conclusion: Atrioventricular compliance, which can be non-invasively assessed, has<br />
an important correlation with PAP in mitral valve stenosis and can be useful in daily<br />
practice.<br />
Keywords: Mitral valve stenisis, Atriovantricular compliance, Pulmanary <strong>artery</strong><br />
pressure<br />
94<br />
Diabetes Mellitus Role in Impeding Prophylactic Effects of<br />
Magnesium on <strong>Post</strong>-Coronary Artery Bypass Grafting Atrial<br />
Fibrillation<br />
Najafi M and Salehi Omran A<br />
Tehran Heart Center, Medical Sciences/University of Tehran, Tehran, Iran<br />
Abstract<br />
Background: Hypomagnesaemia is a well known issue in diabetics. Recent studies have<br />
suggested promising role of supplemental magnesium (Mg) administration in preventing post<br />
surgical atrial fibrillation (AF); however, there is no evidence on differences between<br />
diabetic and non-diabetic patients in response to prophylactic administration of Mg
supplements.<br />
Methods: Thirty hundred foty-five patients (115 diabetic; 230 non-diabetic), elective<br />
candidates for isolated <strong>coronary</strong> <strong>artery</strong> <strong>bypass</strong> <strong>graft</strong>ing (CABG) with normal renal function,<br />
were randomly divided into two groups. Group A (case; 48.1%) received 2g of Mg after<br />
induction of anesthesia until cardiopulmonary <strong>bypass</strong> (CPB) onset and 8 g following CPB to<br />
24 h there after. In group B (control; 51.9%), no supplemental Mg was administered. Mg<br />
serum levels were measured in all patients four times (at the onset of induction, and hours 0,<br />
24, and 48 after ICU admission).Patients were then followed for developing AF after the end<br />
of <strong>surgery</strong> until their discharge.<br />
Results: Thirty-four patients (9.9%) developed AF of which 12 ones were in group A, and<br />
22 in group B. Of 12 patients in group A, 8 (67%) were diabetic, whereas there were just 6<br />
diabetic ones (27.3%) in group B (p=0.026). Serum Mg levels were not statistically different<br />
among groups. There was no significant difference statistically for the rate of DM in nonarrhythmic<br />
patients between the two groups (31% in group A vs. 34% in group B).<br />
Conclusions: DM has a major role in impeding prophylactic effects of Mg infusion on<br />
developing AF. This effect has no correlation with perioperative serum Mg levels. Keywords:<br />
magnesium, diabetes mellitus, <strong>coronary</strong> <strong>artery</strong> <strong>bypass</strong>, atrial fibrillation<br />
95<br />
Beta-blocker administration for preventing post-<strong>coronary</strong><br />
<strong>artery</strong> <strong>bypass</strong> <strong>graft</strong> arrhythmias: The role of diabetes mellitus<br />
Najafi M, Karimi A and Hamidian R<br />
Tehran Heart Center, Medical Sciences/University of Tehran, Tehran, Iran<br />
Abstract<br />
Background: Prophylactic effect of supplemental magnesium (Mg) and ȕ-blocker<br />
administration on atrial fibrillation (AF) is a well-known issue in <strong>coronary</strong> <strong>artery</strong><br />
<strong>bypass</strong> <strong>graft</strong> (CABG). However, there is no evidence of differences between diabetic<br />
and non-diabetic patients in response to prophylactic administration of ȕ-blocker<br />
especially in preventing ventricular arrhythmia (VA).
Methods: Three hundred forty-five patients (115 diabetic and 230 non-diabetic)<br />
candidates for isolated CABG with normal renal function sinus rhythm and positive<br />
(group A) or negative history of at least three days of ȕ-blocker consumption (group B),<br />
were randomly divided into two groups to receive 10 gr. supplemental Mg in 24 hours<br />
(case, 48.1%) or no supplementary Mg (control, 51.9%). Mg serum levels were measured<br />
in all patients 4 times (at onset of induction, hours 0, 24 and 48 after ICU admission).<br />
Then the patients were followed for developing AF and VA.<br />
Results: Forty-five patients (13.6%) (15 diabetic and 30 non-diabetic patients)<br />
developed VA. Out of 15 diabetic patients, 5 patients were in group A and 10 patients<br />
were in group B. The incidence of VA was significantly higher in group B (p
performed in our institution. The indication for off-pump <strong>surgery</strong> was renal dysfunction,<br />
in three patient advances COPD in three patient, age>80 year in one patient, sever<br />
atherosclerotic aorta in two patient. The endartrectomized vessel was left anterior<br />
descending in three patients, right <strong>coronary</strong> <strong>artery</strong> in five patients and diagonal in two<br />
patient.<br />
Results: There was no operative mortality, perioperative myocardial infarction occurred<br />
in one patient with LAD endarterectomy requiring ionotrope and intra-aortic balloon<br />
pump to recover. The mean ejection fraction before operation was 36r4. The mean<br />
ejection fraction post-op 45±8 which was significantly higher than the pre-operative<br />
value (p
from cardiopulmonary machine that were refractory to inotropic and IABP support.<br />
Methods: Between Oct 1998 and June 2004, 1450 patients underwent CABG in our<br />
center. We used Centrifugal pump in six patients (52±12 years) with acute left sided heart<br />
failure following CABG. The patients' characteristics and their risk factors for developing<br />
CAD were recorded.<br />
Results: The success rate was 30% (2 cases from 6 pt.). Four cases were not weaned<br />
from Centrifugal pump after 17±8 hours. Two patients were weaned after 21±5 hours and<br />
with good outcome. The mean preoperative left ventricular EF was 50%±10. The mean<br />
vessel involvement in these patients was 2.66 (1VD-3VD). The <strong>coronary</strong> <strong>artery</strong> Gensini<br />
score was 89±6 (p value
independent risk factor for atherosclerosis. LP (a) level in serum is genetically<br />
determined with an autosomal dominant pattern. The aim of this study was to assess the<br />
association between LP (a) and cervical carotid <strong>artery</strong> stenosis in Iranian population.<br />
Methods: Between May 2004 and January 2005, at Tehran Heart Center, 920 patients<br />
who were candidate for open heart <strong>surgery</strong> for any reason, were selected. Carotid<br />
Doppler Sonography was performed for all of these patients. Serum levels of LP (a), total<br />
cholesterol, triglyceride, High Density Lipoprotein (HDL), Low Density Lipoprotein<br />
(LDL) and LDL/HDL ratio of these patients were measured and their correlation with<br />
carotid atherosclerosis were assessed.<br />
Results: No correlation was found between high levels of LP (a) (>30 mg/dl) and<br />
carotid atherosclerosis (P>0.93). Serum levels of cholesterol (P
independent risk factor for atherosclerosis. LP (a) level in serum is genetically<br />
determined with an autosomal dominant pattern. The aim of this study was to assess the<br />
association between LP (a) and cervical carotid <strong>artery</strong> stenosis in Iraninan population.<br />
Methods: Between May 2004 and January 2005, at Tehran Heart Center, 920 patients<br />
who were candidate for open heart <strong>surgery</strong> for any reason, were selected. Carotid<br />
Doppler Sonography was performed for all of these patients. Serum levels of LP(a), total<br />
cholesterol, triglyceride, High Density Lipoprotein (HDL), Low Density Lipoprotein<br />
(LDL) and LDL/HDL ratio of these patients were measured and their correlation with<br />
carotid atherosclerosis were assessed.<br />
Results: No correlation was found between high levels of LP (a) (>30 mg/dl) and<br />
carotid atherosclerosis (P>0.93). Serum levels of cholesterol (P
type 2 who were between 31 to 78 years old and had no abnormalities of the urinary tract<br />
system were included. We defined ASB as the presence of at least 105 colony-forming<br />
units/ml of 1 or 2 bacterial species, in two separated cultures of clean voided midstream<br />
urine. All the patients were free from any symptoms of urinary tract infection(UTI). Risk<br />
factors for developing bacteriuria were assessed and compared in participants with and<br />
without bacteriuria.<br />
Results: In this study, the prevalence of ASB was 10.9% among diabetic women. E-coli<br />
was the most prevalent microorganism responsible for positive urine cultures. Most of the<br />
isolated microorganisms had resistant to Co-trimoxazole, Nalidixic acid and<br />
Ciprofloxacin. Pyuria (p
infarction. The aim of this study was to assess the prognostic value of quantitative CRP<br />
(Q-CRP) for predicting intra-hospital MI in patients with unstable angina.<br />
Methods: This cohort study was done between December 2003 & June 2004 in Tehran<br />
Heart Center. 121 patients with unstable angina were studied. The exclusion criteria for<br />
this study were: cases with acute MI of less than 1 month duration, finding of left<br />
Bundle Branch Block on EKG and cases with any kind of inflammation, infection,<br />
trauma or acute rheumatic fever. Q-CRP of these patients was measured, and 10 mg/l<br />
considered as a cut off point value for Q-CRP. Patients were divided into two groups<br />
according to their Q-CRP values. One group with Q-CRP >= 10 mg/l (n=68) and the<br />
other group with Q-CRP 10 mg/l and in 1 (1.8%) case of patients with<br />
CRP 0.38).<br />
Conclusion: Considering analyzed results in this study, although there is no<br />
significant correlation between Q-CRP level and MI development, in places in which<br />
there are no facilities to assess the specific laboratory tests for MI, Q-CRP can be used<br />
as a risk stratification module in unstable angina patients.<br />
104<br />
Predictive factors of the cardiopulmonary resuscitation results<br />
Najafi M<br />
Tehran Heart Center, Medical Sciences/University of Tehran, Tehran, Iran<br />
Abstract<br />
Background: Cardiopulmonary resuscitation (CPR) is one of the most important,<br />
lifesaving and unfortunately disappointing components of the standard hospital cares. Former<br />
studies reveal that the CPR success rate (at discharge) was nearly 14%.This study was<br />
designed to evaluate the predictive factors of the CPR results.<br />
Methods: This study was performed on Tehran Heart Center Registry–CPR database
(THCR-CPR) which contains demographical, clinical, procedural and in hospital data for<br />
each resuscitated patient in Tehran Heart Center. CPR in the operating rooms or<br />
postoperative intensive care units was excluded. Successful CPR was defined as a complete<br />
improvement of the patient’s condition without any residual sequel or complication.<br />
Regarding CPR results patients were stratified in two groups: successful and unsuccessful<br />
CPR. All factors in these two groups were compared.<br />
Results: Between January 21, 2004 and June 22, 2004 193 patients (107 male and 86<br />
female, Mean age: 65.11±13.34) were resuscitated. The most important causes of the CPR<br />
were arrhythmia (35.2%), respiratory failure (34.1%), and homodynamic instability (26.7%).<br />
Success rate after resuscitation, at 24 hours and at discharge were 48.7%, 33.8% and 25.5%,<br />
respectively. CABG candidates, patients with unstable angina, patients who had serum<br />
potassium lower than 6 mEq/dl, ventricular fibrillation as starting arrhythmia, CPR or cardiac<br />
massage duration lower than 15 minutes, epinephrine dose lower than 3 mg and higher GCS<br />
levels had significantly better results. On the contrary, cerebrovascular accident, asystol and<br />
need for epinephrine usage in the CPR were significantly higher in the unsuccessful group.<br />
Age, sex, concurrent disease, CPR reason, and serum pH were similar between groups. CPR<br />
and shock delay although were lower in the successful group, were not significantly different.<br />
Conclusion: Our results are comparable with the former studies. Further studies and more<br />
sample size required to determine other predictive factors of the successful CPR.<br />
105<br />
<strong>Post</strong> <strong>coronary</strong> <strong>artery</strong> <strong>bypass</strong> <strong>graft</strong> <strong>surgery</strong> (CABG) atrial<br />
fibrillation: evaluating predisposing and preventive factors<br />
Najafi M, Kamangari A, Haghighat B and Fallah N<br />
Tehran Heart Center, Medical Sciences/University of Tehran, Tehran, Iran<br />
Abstract<br />
Background: <strong>Post</strong> operative arrhythmia are among common complications of CABG<br />
<strong>surgery</strong> and Atrial Fibrillation (AF) is the most important of them. Studies show variable<br />
and different predisposing factors and different studies are evaluating preventive factors.
This study evaluates the role of amiodarone and Magnesium (Mg) administration in<br />
preventing AF.<br />
Methods: CABG candidates with normal sinus rhythm were divided into 4 groups:<br />
1. 1. No Mg. administration<br />
2. 2. With Mg. administration<br />
3. 3. Only amiodarone (300 mg) administration.<br />
4. 4. Mg and amiodarone administration. Other interfering factors were also<br />
evaluated including: sex, age, preoperative Mg blood level, serum creatinine level,<br />
congestive heart failure (CHF), obstructive lung disease, right <strong>coronary</strong> <strong>artery</strong><br />
obstruction, pericarditis, duration of aortic cross clamp and total dosage of Mg<br />
administration.<br />
Results: 822 cases (581 male , 241 female) with a mean age of 60.9 (9.5), mean<br />
creatinine of 1.2 mg/dl, mean aortic cross clamp duration of 49.8 minutes and mean<br />
blood Mg level of 2.3 were evaluated. 107 out of 727 (14.7%) cases developed AF. AF<br />
was statistically related to age (P
Methods: One hundred cases were divided into two groups. In FT group, fentanyl<br />
(0.05-0.15 Pg/kg/min) and Propofol (10-50 Pg/kg/min) infusions were started since<br />
induction time. Atracurium infusion started one hour later, no bolus drug was<br />
administered during operation. Muscle relaxants were neutralized at the end of <strong>surgery</strong>.<br />
Fentanyl infusion continued up to 12 hours post <strong>surgery</strong>. The above two groups were<br />
evaluated for time of alertness and extubation in ICU, total analgesic dosage administered<br />
during 24 hours post operation, ABG and SpO2 pre-and post-extubation. Inclusion and<br />
exclusion criteria for FT method as well as extubation criteria were explained to the ICU,<br />
staff.<br />
Results: Time period between ICU admition and alertness was significantly different in<br />
FT (1.3 hour) and control group (3.3 hours) (P
2002-2005, of which 209 elderly patients were selected. We reviewed their records to<br />
evaluate the effectiveness of CABG and assess their outcomes after <strong>surgery</strong>.<br />
Results: 72.4% of patients were male and 25.8% were female. Left main lesions were<br />
markedly higher than younger patients (18.5% vs. 16%). The rate of postoperative<br />
complications was 15.7% vs. 10%, which showed significant difference [cardiac: AF<br />
rhythm (11.4% vs. 6.5%) & cardiac arrest (3.3% vs. 0.9%), non cardiac: pneumonia (1%<br />
vs. 0.1%), renal failure multisystem failure (1% vs. 0.1%)]. Elderly people also had<br />
considerable longer stay in ICU hospital (49 hrs vs. 33 & 8.9 days vs. 7.4). <strong>Post</strong>operative<br />
ventilation time between two group was noticeably different (13 hr vs. 9 hr). The use of<br />
intra aortic balloon pump was more common in the elderly (4.8% vs 2.1%). In hospital<br />
mortality was 4.8% in old group and readmission was more common in older patients.<br />
Conclusion: Regarding to high rate of complications, trace changes in quality of life in<br />
elderly group limited financial sources and prolonged waiting list for CABG it is wise to<br />
select old patients properly to achieve acceptable outcomes after CABG.<br />
108<br />
Various surgical approaches to complex aortic arch aneurysim,<br />
a single institute experience<br />
Abbasi K, Marzban M, Ahmadi SH, Davoodi S, Movahedi N, Salehi Omran<br />
A, Madani Civi M and Rahnama Azar A<br />
Abstract<br />
Background: Aneurysms of the aortic arch are usually a manifestation of more<br />
diffuse aortic disease involving either the ascending or descending aorta or both. These<br />
aneurysms are a dillence for a surgeon because deciding whether or not to resect an arch<br />
aneurysm involves careful assessment of both the liked hood of rupture and the
operative risk in each individual, balancing one against another.<br />
Methods: In 120 cases with ascending aortic aneurysms (acute or chronic) referred to<br />
our institute; 15 patients had involvement of arch, 8 ones with a complex disorder;<br />
following procedures were scheduled:<br />
1) A-54-year-old man presented with acute limb ischemia underwent a femmo- femoral<br />
<strong>bypass</strong> in another center and then referred to our institute as a case of acute aortic<br />
dissection and managed by aortic hemiarch replacement but about 24h after operation<br />
develops cerebral ischemia; CVA (re dissection) and expired. 2) A-62y-old man<br />
presented with sub-acute aortic dissection (12 days before)<br />
underwent total arch replacement with insertion of innominate <strong>artery</strong><br />
on tube <strong>graft</strong>s separate buttons 3) A-32y-old marfan patient with acute<br />
aortic dissection and acute AI underwent hemiarch replacement<br />
(uneventful recovery)<br />
4) A 68 y old women a case of aortic archaneurysm underwent supra <strong>coronary</strong> root<br />
and total arch replacement complicated by prolonged ventilatory support (72hr) but<br />
uneventful recovery<br />
5) A-22y-old man with chronic dissection underwent Bental operation with arch vessel<br />
implantation and left carotid to left subclavin <strong>bypass</strong> had uneventful recovery (type of<br />
cerebral perfusion: retrograde)<br />
6) A-65y-old man case of acute type dissection underwent Bentall operation and<br />
arch vessel implantationassending aorta to brachiocephalic <strong>bypass</strong>; patient expired due<br />
to ATN<br />
7) A-64y-old man case of choronic dissection and 3 vesel disease underwent aortic valve<br />
preservation, supra<strong>coronary</strong> <strong>graft</strong>s, excision of arch bifurcated <strong>graft</strong>s of brachiocephalic<br />
and carotid <strong>artery</strong> and CABG (antegrade cerebral perfusion) complicated by prolonged<br />
ventilatory support (72h) but uneventful recovery. 8) A-32-y old man a case of acute<br />
dissection underwent bental procedure and <strong>graft</strong><br />
of brachiocephalic <strong>artery</strong> and uneventful recovery.<br />
Results:The postoperative course was uneventful in 4 patients, two patients had a<br />
prolonged ventilation time and two patients of our study group were expired, one (case2)<br />
109<br />
because of re dissection and cerebrovascular accident and other (case6) because of<br />
developing acute tubular necrosis. Hypothermic circulatory arrest in all of patients was<br />
below 45 minute.<br />
Conclusion: Aortic arch aneurysm is a cumbersome and difficult situation needs to a<br />
good decision making and expert hands. Results of this experience could be comparable<br />
with other institute results; this may be due to using deep hypothermia (15c) good<br />
myocardial protection and individualized techniques. One of the major postoperative<br />
morbidities is cerebrovascular accident should be managed with good preservation of<br />
cerebral perfusion and fortunately none of our patients experience these type s of<br />
complications. At last to have better results we recommend to limit the time of<br />
hypothermic circulatory arrest and using deep hypothermi and individualized every<br />
patient in different aspects as methods of cerebral perfusion and operative techniques.
110<br />
Have diabetes worson the outcome of CABG<br />
Tehran Heart Center, Medical Sciences/University of Tehran, Tehran, Iran<br />
Abstract<br />
Background: Diabetes is commonly regarded as a risk factor for mortality and<br />
morbidity after <strong>coronary</strong> <strong>artery</strong> <strong>bypass</strong> <strong>graft</strong>ing.<br />
Methods: In 5795 consecutive patients underwent isolated <strong>coronary</strong> <strong>artery</strong> <strong>bypass</strong><br />
<strong>surgery</strong> in our institute, impact of diabetes on mortality and morbidity was investigated.<br />
Two thousands and seventy four (2071) patients of these had diabetes (mean<br />
age=58.9±9.08). In this article we study the impact of many factors such as age, sex,
BMI, unstable angina, smoking, previous MI cerebral vascular disease, renal dysfunction,<br />
respiratory disease, significant left main stenosis, ejection fraction, emergent <strong>surgery</strong><br />
along with diabetes on in hospital mortality and post operative morbidity and to control<br />
for differences in patient characteristics we used a multivariate logistic regression model<br />
(SPSS ver. 11.0)<br />
Results: In this study there was a significant difference in age (diabetic mean<br />
age=58.9±9.08, non diabetic mean age=57.9±9.95), number of diseased vessels (in<br />
diabetic=3.7±0.51, in non diabetic= 3.6 ±0.58), aortic cross clamp time (in diabetic=<br />
42.3±16.63 min, non diabetic= 67.2±25.94) and number of vein <strong>graft</strong>s but not arterial<br />
ones (diabetic=2.6±0.89, non diabetic= 2.4± 0.94). In hospital mortality was significantly<br />
higher for diabetic patients (in diabetic=2.4%, in non diabetic=1.1% with p value
patients after <strong>coronary</strong> <strong>artery</strong> <strong>bypass</strong> <strong>surgery</strong> and in USA annually more than 70000<br />
patients,underwent <strong>coronary</strong> <strong>artery</strong> <strong>bypass</strong> <strong>graft</strong>ing (CABG) experience such a problems<br />
during their postoperative period. Mild moderate depression is another complication<br />
affects 1/3 of patients after CABG.<br />
Methods: 45 patients with conventional <strong>bypass</strong> and 45 patients with off pump <strong>bypass</strong><br />
were included in this study and we assessed the incidence of depression 5 days before<br />
and 4 days after CABG in both groups (with standard beck depression inventory test). To<br />
control for differences in patient characteristics we try to select patients with higher<br />
matched risk factors (age, sex, smoking…).<br />
Results: There was not any significant difference in time of <strong>surgery</strong>; time of extubation<br />
and history of depression. But the number of <strong>graft</strong>s had significant difference between<br />
two groups. Coma, seizure and cerebrovascular accident were not seen in our patients<br />
after <strong>surgery</strong>. The incidence of depression in conventional group was meaningfully<br />
higher than off pump group (p value=0.04) and also incidence of memory deficit was<br />
higher in conventional group but no significant difference was seen (p value= 0.3).<br />
Conclusion: Although non of the patients of this study experience neurologic<br />
complications but it seems that neurologic morbidities be lower in off pump CABG.<br />
Based on the founding of this study we can conclude that depression was lower in off<br />
pump method than conventional one.<br />
112<br />
In vitro effects of cardioplegia on saphenous vein <strong>graft</strong>s<br />
during CABG<br />
Ahmadi SH, Soleimani M, Daliri M, Dehpour HR, Sanatkar, Karimi AA, Abbasi<br />
K, Kaviani S, Piryaee A, Fayaz-Zadeh and Madani-Civi M<br />
Abstract<br />
Background: Administration of cardioplegia into vein <strong>graft</strong> is an establish method to<br />
ensure cardioplegia distribution beyond <strong>coronary</strong> <strong>artery</strong> stenosis. The aim of this study<br />
was to examine the influence of potassium concentration in cardioplegia on structure and
function of saphenous vein.<br />
Methods: 10 specimens of saphenous vein <strong>graft</strong> from 10 patients during CABG were<br />
used. A part of each specimen served as control: the others were assigned to test groups.<br />
All test groups of specimens exposed to solution supplemented with 5, 20, mmol/1 KCL<br />
for at least 1 hour. A part of each specimen was sent to laboratory for tissue culture.<br />
Endothelial cell viability, calcium mobilization and NO generation were determined by<br />
using specific florescence marker. Another part of each specimen of vein <strong>graft</strong>s was<br />
studied by scanning electron microscopy. The last part of each specimen was evaluated<br />
for function and vasomotor responses.<br />
Results: Structural disorder and dysfunction of vein <strong>graft</strong> due to expose to cardioplegia<br />
will be discussed in the future.<br />
Conclusion: Intravenous cardioplegic administration can contribute to early and late<br />
thrombosis. So, complete evaluation of vein <strong>graft</strong> after exposure to cardioplegia can<br />
provide new insights into cardioprotection during aorto-<strong>coronary</strong> <strong>bypass</strong> <strong>surgery</strong>.<br />
113<br />
Outcomes and long term survival for patients undergoing<br />
mitral valve repair versus replacement concomitant <strong>coronary</strong><br />
<strong>bypass</strong><br />
Tehran Heart Center, Medical Sciences/University of Tehran, Tehran, Iran<br />
Abstract<br />
Background: In moderate to severe mitral regurgitation (MR) and <strong>coronary</strong> <strong>artery</strong><br />
disease (CAD), use of mitral valve repair (MV repair) vs replacement (MVR) in the time<br />
of CABG is controversial. To determine success rate and durability of mitral valve repair<br />
vs replacement concomitant with CABG in this group of patients.
Methods: From March 2002 to February 2005, 88 consecutive patients (mean age<br />
63.00±8.08 years, mean ejection fraction 44.80±10.89%parsonnet score 20.70±8.82) with<br />
CAD and moderate to severe MR (2 to4+) and CAD underwent CABG plus MVR or MV<br />
repair, 78.4% had post operative echocardiography, 47.7% had follow up<br />
echocardiography and 93.2% had post operative or follow up echocardiography, intra<br />
operative TEE was performed for 19(21%) patients, mean time of follow up was 8±4<br />
months.<br />
Results: 48.9% of patients underwent CABG plus MVR and 51.1% CABG plus MV<br />
repair, early mortality was (8%) 7 patients, all in MV repair group, but difference of<br />
mortality between MVR and MV repair group was not statistically significant p=0.114,<br />
late mortality was 3.4% (3 patients). MR was ischemic in 61% (with persistent wall<br />
motion abnormality) and ischemic in 23. Mortality was not related to preoperative<br />
ejection fraction, severity and mechanism of MR, or post operative MR, p=0.59, 0.49,<br />
0.41, 0.18, but mortality was higher in patients with more severe LV systolic dysfunction<br />
after CABG (EF 33% vs 40% p=0.04). in MV repair group, 39.8% had no MR, 33% mild<br />
MR, 13.6% moderate MR, 5.7% moderately severe and 1.1% severe MR (2 patients<br />
underwent reopration one because of severe MS and another because of severe MR.<br />
overall 72.8% had no or mild MR and 27.2% had moderate to severe MR, success of<br />
repair was not related to preoperative ejection fraction, severity and mechanism of MR<br />
and mechanism of mitral valve repair. 44.9±10.6 vs 41 25±12.9% p=0.38 p=0.6 p=0.9,<br />
p=0.59). We performed intraoperative TEE for 12 patients in MV repair group, severity<br />
of MR in intraoperative TEE had exact correlation with postoperative and follow up<br />
echocardiography. 20% had both follow up and postoperative echocardiography, MR<br />
severity was unchanged in follow up p=0.5.<br />
Conclusion: Early and late mortality was not difference between MVR vs MV repair<br />
group concomitant CABG. Durability of MV repair in MR and CAD in mid term is<br />
acceptable and repair is successful in most patients, so mitral valve repair may be<br />
preferred if technically possible.<br />
114<br />
Moderate nonorganic mitral regurgitataion and <strong>coronary</strong><br />
disease: treatment by <strong>coronary</strong> <strong>bypass</strong> alone<br />
Tehran Heart Center, Medical Sciences/University of Tehran, Tehran, Iran<br />
Abstract<br />
Background: In cases of moderate (2+ or 3+ on a scale of 0 to 4+) mitral regurgitation<br />
(MR) and <strong>coronary</strong> <strong>artery</strong> disease operative strategy continues to be debated between<br />
<strong>coronary</strong> <strong>artery</strong> <strong>bypass</strong> <strong>graft</strong>ing alone (CABG) or concomitant valve repair. To clarify the<br />
optimal management of these patients we evaluated the mid term result of isolated CABG
on moderate MR without organic mitral valve disease.<br />
Methods: From March 2002 to February 2005, 40 consecutive patients (57.5% male,<br />
mean age 62.45 years, mean ejection fraction 43.81%, mean Parsonnet score 19.58) with<br />
<strong>coronary</strong> <strong>artery</strong> disease and moderate MR without leaflet prolapse or rheumatism or other<br />
organic mitral valve disease underwent CABG alone 31 (77.5%) patients had either post<br />
operative or follow up transthoracic echocardiography with mean time of follow up<br />
10.82±8.12 months.<br />
Results: MR was ischemic in 25 (62.5%) patients (with persistent wall motion<br />
abnormality) and without significant etiology in 15 (37.5%) patients. Overall mortality<br />
was 7 (25.9%), 2(5)% early or in hospital and 5/30 (16.6%)late, mortality was not<br />
different between ischemic and non ischemic MR group, p=0.99. Also it was not related<br />
preoperative ejection fraction and severity of MR, 0.48, 0.62. considering postoperative<br />
and follow up transthorasic echocardiography, 16.1% had moderately severe MR , 29%<br />
had moderate MR, 29% mild MR and 25.8% no MR. p=0.000. Overall 54.8% had no or<br />
mild MR and 45.2% had moderate to severe MR. Ischemic MR, preoperative ejection<br />
fraction and LV systolic and diastolic dimensions had no significant effect on resolution<br />
of MR, p=0.46, 0.09, 0.79, 0.70.<br />
Conclusion: Although CABG alone for <strong>coronary</strong> <strong>artery</strong> disease accompanying<br />
moderate nonorganic MR reduces MR severity significantly, but many patients left with<br />
moderate or moderately severe MR. So a pre operative diagnosis of moderate nonorganic<br />
MR may warrant concomitant mitral repair.<br />
Mid-Term follow up of sixty patients with implantable<br />
cardiovertor defibrillator<br />
YaminisharifA, Kazemisaeid.A, Davoudi.G, Sadegian.S, Moughaddam.M ,<br />
Goodarzynejad H and Paydari.N<br />
115<br />
Tehran Heart Center, Medical Sciences/University of Tehran, Tehran, Iran<br />
Abstract<br />
Background: This study assessed the results of ICD implantation in 60 patients with<br />
different etiology, age, ejection fraction and different venous access.
Method: From May 2002 to July 2005, 60 ICDs were implanted in 60 patients who<br />
need to have ICD for secondary or primary prevention (Except MADITII inclusion<br />
criteria). Their age were between (16 to 79y) mean 51±16y (13% over 70 years). Follow<br />
up period was between (1 month to 38 months) mean 18±7m. 75% of patients were<br />
male.EF in 22% of patients was t %50 ,30-50% in 41%,
not respond to conventional analgesics. This study evaluates the effect of low dose<br />
ketamine (NMDA receptor inhibitor) infusion in controlling post CABG pain of opium<br />
addicts.<br />
Methods: We administered 100g/kg ketamine to 25 opium addicted CABG candidates<br />
after induction of anesthesia and before surgical incision. We continued ketamine<br />
infusion (2g/kg/min) for 48 hours after extubation. 25 controlled cases received placebo<br />
with the same pattern as ketamine. We recorded pain severity at rest and deep inspiration<br />
by VAS score in 6 equal intervals up to 48 hours after extubation. Besides, we recorded<br />
analgesic dosage during and after <strong>surgery</strong> up to 48 hours.<br />
Results: Sedation score was not high in either group. Although total analgesic dosage<br />
during <strong>surgery</strong> was lower in ketamine group (14.6 vs 20 mg), there was no significant<br />
difference between two groups. Although total dosage and number of analgesic and<br />
opium consumption in ICU was not different significantly, VAS score both in rest and<br />
deep inspiration in all intervals except 6 hour after extubation was higher in control group<br />
compared to ketamine group (p
demonstrated that cardiopulmonary <strong>bypass</strong> itself, results in reduced serum magnesium<br />
level. In this study, we wanted to evaluate the effect of total blood magnesium level<br />
(TMG) on preventing perioperative arrhythmias by routine regimens of 2-4 grams<br />
supplemental magnesium (SMG).<br />
Methods: TMG was measured in patients who were scheduled for CABG on 3<br />
occasions [just before anesthesia, just after entering intensive care unit (ICU)<br />
postoperatively and on the first morning after operation]. Patients were evaluated for<br />
primary cardiac rhythm and other variables that could have an influence on magnesium<br />
level (serum creatinine, urine output in operating room and diuretic therapy). SMG was<br />
also recorded in operating room and ICU. Then the patients were evaluated for the rate<br />
and kind of arrhythmia through next 3 days.<br />
Results: Mean TMG level in 174 cases was 2.2 (0.5), 2.6 (0.6) and 2.4 (0.6) mg/dl on<br />
three occasions respectively. Mean SMG was 2.5 (1.2) grams. 47 out of 157 patients<br />
developed post-operative arrhythmia (%30) [AF* (%6.4), Non-AF SVA** (%14.6) and<br />
Ventricular arrhythmia (%16.6)]. Mean serum creatinine level and urine output were 1.2<br />
mg/dl and 1800ml respectively. Although there was a significant difference between<br />
TMG on three occasions (P
Abstract<br />
Background: Experimental studies suggest that autologous bone marrow stem cell<br />
transplantation (AC 133+) in patients with myocardial infarction (MI) may improve<br />
cardiac function. The aim of this study was to assess feasibility, safety of this therapy and<br />
cardiac performance as well.<br />
Methods:Between June 2004- June 2005, 21 patients with history of acute myocardial<br />
infarction within 3 months who were candidate for <strong>coronary</strong> <strong>artery</strong> <strong>bypass</strong> <strong>graft</strong>ing<br />
(CABG), were entered in our study. The patients randomly divided to two groups: control<br />
group (n=8, CABG alone) and case group (n=13, CABG with intramyocardial injection<br />
of autologus AC133+ bone marrow stem cell in the infracted border zone). For all<br />
patients we have done dobutamine stress echo (DSE) and thallium scan before CABG<br />
and 3 months after CABG to determine perfusion and viability of the heart.<br />
Results:There were no significant differences between demographic factors of two<br />
groups. Left ventricular ejection fraction (LVEF) improved from 31.25% to 46.25% in<br />
case group (EF improvement in control group less than 10%, P
<strong>artery</strong> harvesting regarding arterial flow, vessel wall operative time, economic aspects<br />
and complications.<br />
Methods: Forty four consecutive patients undergoing <strong>coronary</strong> <strong>artery</strong> <strong>bypass</strong> and<br />
candidate for radial <strong>artery</strong> harvesting were randomized to two groups. In the first group,<br />
harvesting was done by sharp dissection (n=22) and in the second group by<br />
electrocautery as a vascular pedicle.<br />
Radial <strong>artery</strong> flow was measured before and after papaverin injection to its lumen.<br />
Specimens were examined by two special staining and immunohistochemistry to assess<br />
the vessel wall integrity.<br />
Results: Arterial flow was higher in group two (p=0.033) morphologic analysis showed<br />
full integrity of endothelium and no major arterial damage. Immunohistochemical<br />
staining demonstrated an extremely high degree of endothelial integrity in both groups.<br />
Operative time was shorter in group two (P=0.0001) The number of used clips was lesser<br />
in group two No special major complication was noted from radial <strong>artery</strong> harvesting in<br />
two groups.<br />
Conclusion: Elecrrocautery dissection for radial <strong>artery</strong> harvesting is a fact, safe and<br />
reliable technique compared with sharp dissection.<br />
123<br />
Seven-year follow-up of <strong>coronary</strong> <strong>artery</strong> <strong>surgery</strong> in young<br />
adults (
the 40 years old and evaluated mid-term results of CABGs in this group of patients, this<br />
study was done.<br />
Methods: Between July 1997 and March 2003, a total of 54 patients under the age of 40<br />
years at the time of <strong>surgery</strong>, operated for <strong>coronary</strong> <strong>artery</strong> disease. Gender, family history,<br />
cigarette smoking, opium addiction, diabetes, hypertension, hyperlipidemia, angina class,<br />
number of diseased vessels, ejection fraction (EF), prior MI and cardiac arrest were<br />
studied. The mean age was 35. The average EF was 36.8% (20-55%). Patients were<br />
followed for seven years.<br />
Results: Ninety three percent of these patients were male. Smoking (92%), positive<br />
family history for CAD (83%), hyperlipidemia (70%) opium addiction (39%) and<br />
diabetes (31%) were more prevalent in this study compared with patients older than 40<br />
years whereas the occurrence of hypertension (9%) was lower (P
Background: The aim of this study is to evaluate the appropriation between the size of<br />
prosthetic Aortic valve and body surface area in patients with AVR because of AS.<br />
Prosthetic Aortic valve replacement in a small aortic root raises concern about its<br />
hemodynamic effect.<br />
Methods: 12 AVR patients were evaluated with exercise stress echocardiography, peak<br />
gradient, effective orifice area and valve index were evaluated at rest and peak exercise.<br />
Results: Two patients had ideal hemodynamic results (peak gradient, Mean gradient 22<br />
appropriate, valve index > 1 cm/m at rest and exercise) (group AI).<br />
Five patients had intermediate hemodynamic results (good peak and mean gradient and<br />
valve index > 1 cm/m at rest but peak gradient, MG and or VI < 1 cm/m at peak exercise)<br />
(group A II).Five patients had inappropriate hemodynamic results at rest (PG, MG<br />
elevated and / or valve index < 1 cm2/m2).prosthetic Aortic valve size / BSA = 14/48 AI,<br />
12/53 AII, 12/22 B. The difference between group AI and AII was significant, but not<br />
meaningful statistically, (P = 0.08). The difference between group AI and B was<br />
meaningful statistically, (P = 0.05).<br />
Conclusion: For ideal hemodynamic results, we can consider Aortic root enlargement<br />
in small aortic roots with large BSA. BSA: body surface area PG: peak gradient MG:<br />
mean gradient :Valve Indexeffective orifice area BSA<br />
Absence of beneficial effect of autotransfusion combined with<br />
tranexamic acid on post cardiopulmonary <strong>bypass</strong> bleeding<br />
125<br />
Mehr-Aein A, Davoodi S and Madani-Civi M<br />
Department of anesthesiology , shariati hospital, Tehran University, Tehran Heart Center, Iran Tehran<br />
University of Medical Sciences. National Iranian oil company central hospital, Tehran, Iran<br />
Abstract
Background: The aim of this study was to assess the effects of intraoperative<br />
autotransfusion combined with tranexamic acid on post-operative bleeding and need for<br />
allogeneic transfusion.<br />
Methods: In a prospective, double blinded, randomized trial, 350 patients undergoing<br />
conventional CABG allocated into two groups:<br />
.Group1= 175 patients received tranexamic acid, 15mg/kg before the injection of<br />
heparin and 15mg/kg after protamin injection. .<br />
Group2= 175 patients received 30 mg/kg tranexamic acid and 2 units autologous blood.<br />
<strong>Post</strong>operative bleeding allogenic transfusions and complications were recorded.<br />
Results: The intraoperative and postoperative bleeding was 600±125 ml in group1 and<br />
620±150 ml in group2 (p=0.7). The rates of transfused patients in group 1&2 were 67%<br />
and 72% (P
Background: Several studies showed that elevated plasma homocysteine level is a risk<br />
factor for <strong>coronary</strong> <strong>artery</strong> disease. A common mutation C677T of<br />
methylenetetrahydrofolate reductase (MTHFR) gene is reported to be associated with<br />
decreased enzyme activity and increased blood homocysteine level.<br />
Methods: This study was to analyze the frequency of this mutation in relation to blood<br />
homocysteine level in 100 patients with CAD compared to the 100 normal controls.<br />
Results: Higher prevalence of the C677T mutation as well as elevated level in blood<br />
homocysteine were observed in Iranian CAD cases compared to the normal control. The<br />
C677T MTHFR common mutation was significantly linked to the CAD, supported by a P<br />
value
Abstract<br />
Background: Retrosternal and pericardial adhesions formation after cardiac <strong>surgery</strong><br />
make a repeat sternotomy, time consuming and dangerous, with high risk of iatrogenic<br />
trauma to heart, aorta, innominate vessels and <strong>graft</strong>s. So we decided to find another<br />
substitute for pericard other than the ordinary ones in use, with the advantage of lower<br />
cost but good results.<br />
Methods: Thirty sheep, 35-45 kg were used in this study and categorized into two<br />
groups including test group and control group. In group one (n=18) pericardium was<br />
excised and the LTS (laser treated silicone) membrane implanted as a pericardial<br />
substitute. In control group (n=12) the pericardium was excised without LTS membrane<br />
implantation. During follow up ranging from 3-24 months, sheep were observed for any<br />
clinical sign of post operation problems. Reoperation was done in all animals of test and<br />
control groups to evaluate adhesions formation.<br />
Results: In the control group dense adhesions were observed, while in the study group<br />
adhesions formation were reduced at all sites covered by LTS membrane and no infection<br />
or other complications were observed.<br />
Conclusion: The LTS membrane is safe and efficacious in the reduction of pericardial<br />
adhesions formation and might be used in patients undergoing cardiac <strong>surgery</strong> and may<br />
need reoperation, and due to it's lower costs it may replace other substitute such as PTFE.<br />
128<br />
Preparation of chistosan derived from shrimp’s shell of<br />
Persian gulf as a blood hemostasis agent<br />
Mirzadeh H, Yaghobi N, Amanpour S, Ahmadi SH, Ziabakhsh Tabary Sh,<br />
Mohagheghi MA and Hormozi F<br />
Iran Polymer Institute Cancer Institute, Tehran University of medical sciences Mazandaran University of<br />
medical sciences<br />
Abstract
Background: Hemostasis especially in heparinized patients has always been a problem<br />
and a large number of products has been introduced to make it easier. The purpose of this<br />
experiment was to evaluate the effectiveness and safety of PGC (Percian Gulf Chistosan)<br />
as a hemostasis agent with surgical application.<br />
Methods: Chitin used in this experiment was extracted from Persian Gulf shrimp' s<br />
shell according to Kifune et al. Method. Eighteen adult female mixed breed sheep<br />
(weight range: 40-50kg) were used in this study, an oblique incision was made at the<br />
anterior border of sternocleidomastoid muscle, carried directly down to the carotid sheat,<br />
three holes were punctured in carotid <strong>artery</strong> and led to jet bleeding. Bleeding time from<br />
the holes was assessed in different conditions: after manual compression with or without<br />
using PGC (and in heparinized and non heparinized animals).<br />
Results: Using PGC had significant reduction in manual compression time of the<br />
carotid <strong>artery</strong> in comparison with the control. It's mechanism of hemostasis seems to be<br />
independent from classic coagulation cascade because it works also in heparinized<br />
animals.<br />
Conclusion: There is significant reduction in manual compression time form bleeding<br />
site when PGC is used. It has a good hemostatic effect that is independent from classic<br />
coagulation cascade. The optimization and a better formulation of PGC for hemostatic<br />
purpose require further studies.<br />
129<br />
Evaluation of cardiac adhesions after pericardial substitution<br />
by laser treated silicone (LTS) membrane.<br />
Amanpour S, Mirzadeh H, Ahmadi SH and Mirkhani SH<br />
Tehran Heart Center, Medical Sciences/University of Tehran, Tehran, Iran Iran polymer and petrochemical<br />
institute, Tehran, Iran<br />
Abstract
Background: Reoperative median sternotomy may result in cardiac rupture due to<br />
severe adhesion between heart and surrounding tissues. To avoid this type of adhesion<br />
LTS membrane was developed and evaluated in animal models as a pericardial substitute.<br />
Methods: In this study 24 sheep were used. After general anesthesia chest was opened<br />
as in human, pencardium was excised and LTS membranes implanted in 14 sheep. 10<br />
sheep were used as a control group and the same surgical procedure was carried out<br />
without LTS membrane. According to a defined timetable between 1-27 months, the<br />
chest reopened and adhesion formation was evaluated both for LTS membranes and<br />
control groups.<br />
Results: As a substitute LTS membrane showed no adhesion to the posterior surface of<br />
the chest wall. Total adhesion scores were also statistically significant (P
Background: The clinical significance of mammary side branches is still controversial.<br />
This study was designed to show the potential phenomena in two different situations of<br />
distal resistance to mammary flow.<br />
Methods: Mammary <strong>artery</strong> flow measurement was done in four different situations<br />
(with and without distal resistance producing by partial occlusion of it's lumen by clip<br />
with patent or occluded side branch) in 31 patients undergoing elective CABG at end of<br />
harvesting by ejection of blood to a syringe.<br />
Results: There was significant difference (p
Abstract<br />
Background: In cases of moderate mitral regurgitation and <strong>coronary</strong> <strong>artery</strong> disease<br />
operative strategy continues to be debated between <strong>coronary</strong> <strong>artery</strong> <strong>bypass</strong> <strong>graft</strong>ing alone<br />
and concomitant valve replacement or repair.<br />
Method: From March 2002 to June 2004 20 consecutive patients mean age 63.30 ± 8.16<br />
years were treated for moderate mitral regurgitation and <strong>coronary</strong> <strong>artery</strong> disease with<br />
CABG alone, mean EF was 47.22± 14.16 and Parsonet score was 12.55± 9.40 Follow up<br />
ranged from<br />
Results: MR reduced from 1.61± 0.92 but difference was not statistically significant.<br />
(PV=0.12) EF reached from 47.22±14.16 to 48.61±9.6 post operatively difference was<br />
not statistically significant also. In hospital mortality was a and late mortality was 10% (2<br />
patients)<br />
Conclusion: Severity of MR in most patients with moderate ischemic MR reduce with<br />
CABG alone, but even moderate ischemic MR include high risk patients with high late<br />
mortality for CABG alone.<br />
132<br />
Chronic total occlusion of left main <strong>coronary</strong> <strong>artery</strong>: a case<br />
series<br />
Marzban M, Mandegar MH, Karimi A, Salarifar M, Amirzadegan A, Ahmadi H,<br />
Abbasi K, Movahedi N, Davoodi S and Abbasi SH<br />
Tehran Heart Center, Medical Sciences/University of Tehran, Tehran, Iran
Abstract<br />
Background: Acute occlusion of left main <strong>coronary</strong> <strong>artery</strong> as a complication of cardiac<br />
catheterization is a well-known clinical entity; but few reports exist about chronic total<br />
occlusion, its incidence and management.<br />
Methods: From 2000 to 2003, 10 patients with chronic total occlusion of left main<br />
<strong>coronary</strong> <strong>artery</strong> underwent <strong>coronary</strong> revascularization with conventional technique<br />
(cardiopulmonary <strong>bypass</strong> and combined antegrade with retrograde cardioplegia delivery<br />
technique). Patients were followed regularly.<br />
Results: No mortality, no major morbidity except one episode of postoperative bleeding<br />
requiring re-exploration were seen. At mean follow up of 30 months, all patients were in<br />
NYHA class I.<br />
Conclusion: Total occlusion of left main <strong>coronary</strong> <strong>artery</strong> is not as rare as literature<br />
review suggests and can be managed as other patients with left main stenosis.<br />
133<br />
Results of CABG concomitant with mitral valve replacement<br />
versus repair in patients with moderate to severe mitral<br />
regurgitation accompanying <strong>coronary</strong> <strong>artery</strong> disease<br />
Sadeghian H, Karimi AA, Ahmadi H, Salarifar M, Darabian C, Davoodi S, Abbasi K,<br />
Haji Zeinali A, Amirzadeghan A and Majd M<br />
Tehran Heart Center, Medical Sciences/University of Tehran, Tehran, Iran
Abstract<br />
Background: We studied outcome of <strong>surgery</strong> in patients with moderate to severe mitral<br />
regurgitation (MR) suffering from <strong>coronary</strong> <strong>artery</strong> disease (CAD), undergone mitral valve<br />
replacement (MVR) vs. mitral valve (MV repair) accompanying <strong>coronary</strong> <strong>artery</strong> <strong>bypass</strong><br />
<strong>graft</strong>ing(CABG).<br />
Methods: From March 2002 to January 2004, 40 consecutive patients (mean age:<br />
59/7±8/9years) undergone CABG plus MVR or MV repair. From 40 patients, 18(45%) were<br />
in NYHA functional class lll or IV, 36(90%) of them had MR grade III. The mean follow-up<br />
time was 7/7±5/9 months.<br />
Results: The mitral valve was replaced in 16 (group A) and repaired in 24 (group B)<br />
concomitant with CABG. Risk for CABG was similar in both groups according to Parsonnet<br />
scorer. 1) Early mortality was similar in both groups (0 in group A, 3 in group B, 7/5%,<br />
p=0.26), late mortality also had no significant difference between two groups(1 in group A, 0<br />
in group B , p=0.9). Multivariate analysis identified poor coronaries as a risk factor for early<br />
death (p=0.004). Pulmonary hypertension had a trend for increased mortality (p=0.12), but<br />
recent unstable angina, low ejection fraction (EF) and history of pulmonary edema had no<br />
influence. 2) In group A, EF decreased from mean 51.87±10.14 to 44.37± 8.3% after <strong>surgery</strong><br />
(p=0.002), in group B no significant change in EF occurred (from 43.42± 11 to 43.7± 13%,<br />
p=0.86).<br />
Conclusion: in patients with moderate to severe MR accompanying CAD, mortality was<br />
similar in MVR vs. MV repair plus CABG, but EF significantly decreased after MVR, thus<br />
according to this study there is a trend for MV repair concomitant with CABG in patients<br />
with significant MR accompanying CAD, but we need more studies for definite conclusion.<br />
134<br />
Effects of oral Pentoxifylline in cardiopulmonary <strong>bypass</strong><br />
surgeries<br />
Abbasi K, Karimi A, Ahmadi H, Davoodi S, Movahedi N, Marzban M and<br />
Khamne'ian S<br />
Tehran Heart Center, Medical Sciences/University of Tehran, Tehran, Iran
Abstract<br />
Background: The aim of the presented study was to evaluate the preservation effect of<br />
the Pentoxifylline on enzymatic raise after the cardiopulmonary <strong>bypass</strong> <strong>surgery</strong>.<br />
Methods: 60 patients undergoing cardiopulmonary <strong>bypass</strong> surgeries in Tehran Heart<br />
Center in1381-82 were entered in a prospective placebo controlled clinical trial and<br />
randomly divided to control (placebo) and case (oral Pentoxifyliin 400mg tds<br />
preoperative and 400mg bd in early postoperative period) groups. Plasma concentration<br />
of creatine phosphokinase (CK), creatine phosphokinase MB (CK-MB) and lactate<br />
dehydrogenase (LDH) were recorded immediately, 4, 6 and 24 hours after the<br />
cardiopulmonary <strong>bypass</strong> and preoperative ejection fraction were measured.<br />
Results: There were no significant difference between demographic factors (age and<br />
gender) and operation duration and ejection fraction in control and case groups (51.50 vs.<br />
54.80 yr; 63.64 vs. 70% male and 192.23 vs. 176.38 min. and 40.50% vs. 48.80<br />
respectively. CK means in immediately, 4, 6 and 24 hours after operation were<br />
significantly higher in control group (156.6 vs. 131.02 and 921.10 vs. 343.43 and 316.70<br />
vs. 287.30 IU/L; respectively p
Abstract<br />
Background: This study was undertaken to evaluate of risk factors for CAD in patients<br />
< 40 years old<br />
Method: Among 2269 patients undergoing CABG operation. A total of 86 patients were<br />
40 years old. (group<br />
2) gender, family history, smoking, diabetes, hypertension, hyperlipidemia, functional<br />
class, number of disease vessels, Ejection fraction, prior MI were studied and we<br />
compared CAD risk factors between 2 groups.<br />
Results: From 86 patients who were
Abstract<br />
Background: The role of preoperative screening for carotid <strong>artery</strong> stenosis in patients<br />
who underwent cardiac surgical procedures is not clearly established. This retrospective<br />
study was designed to determine the prevalence of carotid disease in this population and<br />
to identify preoperative risk factors for carotid <strong>artery</strong> stenosis.<br />
Methods: During a 13-month interval 2677 patients of a consecutive series of patients<br />
55 years of age and older who underwent carotid <strong>artery</strong> <strong>bypass</strong> <strong>graft</strong>ing were evaluated<br />
before operation with carotid duplex ultrasonography.<br />
Results: The prevalence of disease was 2.6% for significant stenosis (significant<br />
stenosis was defined as 60% or greater narrowing of intraluminal diameter due to<br />
Washington University criteria). The major risk factors were male gender (61.4%),<br />
hypercholesterolemia (50%), HTN (61.4%), familial history of CAD and smoking did not<br />
show significant relation with carotid <strong>artery</strong> stenosis. Carotid endarterectomy combined<br />
with CABG was performed on 16 patients; all operative and postoperative variables were<br />
collected and analyzed. For 33 patients did not been performed any carotid intervention<br />
in combination with CABG and in short-term follow-up we didn’t detect any major<br />
complication such as stroke and 30-day mortality in these 33 cases.<br />
Conclusion: This study showed that prevalence of carotid stenosis in CAD patients of<br />
our society is less than western studies (2.6% vs. 5.9%): so we can organize a specific<br />
scoring for preoperative carotid evaluation.<br />
137<br />
Analysis of effective factors on mortality of CABG patients in<br />
hospital<br />
Sadeghian S, Salarifar M, Karimi A, Marzban M, Abbasi K, Ahmadi H, Movahed<br />
N, Davoodi S, Paydari N and Padeghan M.
Tehran Heart Center, Medical Sciences/University of Tehran, Tehran, Iran<br />
Abstract<br />
Background: More than 30.000 CABG surgeries are performed in Iran annually. The<br />
main goal of performing CABG <strong>surgery</strong> is to control disease symptoms and to increase<br />
the patients' life expectancy; therefore, analyzing the rate of mortality and the effective<br />
factors can affect the decision we make about performing CABG.<br />
Methods: In order to analyze these factors in Iranian patients the files of all the patients<br />
from March 2002 to March 2004 from the viewpoint of their personal data disease and<br />
the risk factors were analyzed.<br />
Results: During this period the total number of patients who underwent CABG <strong>surgery</strong><br />
was 5475 patients with an average age of 58 years old of whom 24% were 65-75 years<br />
old and 76% were male. Seventy patients have passed away during this period which<br />
shows a mortality of 1.3%. The mortality in emergency surgeries was 2.4% and in<br />
elective surgeries was 1.2%. The risk of this <strong>surgery</strong> in both sexes increases after the age<br />
of 65, but this increase is higher in men (1.8 times against 1.4). After the age of 75 this<br />
risk in men multiplies by<br />
4.3. in general, the risk of the <strong>surgery</strong> in women was twice as much as men (p=0.001).<br />
Emergency <strong>surgery</strong> multiplies the risk by 1.9 (p=0.001). Carotid arterial stenosis and<br />
heart valve <strong>surgery</strong> multiply the risk by 3 and 8, respectively (p=0.001). there is a relation<br />
between EF and mortality rate of the <strong>surgery</strong> (p=0.001), so that for an EF of less<br />
than30%, the risk of the <strong>surgery</strong> multiplies by 2.4 and for an EF range of 30-50% the risk<br />
multiplies by 1.9. Among atherosclerotic risk factors only a relation between the risk of<br />
this <strong>surgery</strong> and diabetes mellitus (p=0.02) and hypertension (p=0.07) has been proved<br />
which multiply the mortality rate of the <strong>surgery</strong> by 1.6 and 1.5, respectively. For those<br />
patients who are addicted to smoking cigarettes, the age of disease appearance and the<br />
life expectancy are five years less than that of other patients.<br />
Conclusion: The results indicate that the age of CAD appearance in Iran is eight years<br />
less than that of America and the increase in risk of the <strong>surgery</strong> except left main <strong>coronary</strong><br />
<strong>artery</strong> <strong>surgery</strong> is similar to other studies but the rate of this increase is different.<br />
138<br />
Long term evaluation of laser-treated silicone (LTC)<br />
membrane as a pericardial substitute: An experimental study<br />
Ahmadi H, Mirzadeh H, Amanpour S, Rabbani Sh, Mohagheghi MA and<br />
Mirkhani H<br />
Tehran Heart Center, Medical Sciences/University of Tehran, Tehran, Iran
Abstract<br />
Background: Evaluation of efficacy and safety of LTC membrane as a new<br />
pericardial substitute in sheep model.<br />
Methods: 30 ewes (35-45 kg) were used and categorized into two groups including test<br />
group and control group. In group one (n=18) pericardium was excised and the LTC<br />
membrane implanted as a pericardial substitute. In control group (n=12) the pericardium<br />
was excised without LTC membrane implantation. During follow up ranging from 3-24<br />
months, sheep were observed for any clinical sign of post operation problems.<br />
Reoperations were done in all animals of test and control group to evaluate adhesions<br />
formation.<br />
Results: In the control group dense adhesions were observed, while in the study group<br />
adhesions formation was reduced at all sites covered by LTC membrane and no infection<br />
or other complications were observed.<br />
Conclusions: The LTC membranes were safe and efficacious in the reduction of<br />
pericardial adhesions formation and might be used in patient undergoing cardiac <strong>surgery</strong><br />
and may need re-operation. Key words: cardiac <strong>surgery</strong>, pericardial adhesions, sheep,<br />
silicone.<br />
139<br />
Autologus bone marrow stem cell transplantation for<br />
myocardial regeneration<br />
Ahmadi H, Baharvand H, Soleymani A, Kamangari A, Ashtiani K, Salarifar M,<br />
Sadeghian H, Emami, Ardekani JM and Madani Civi M<br />
Tehran Heart Center, Medical Sciences/University of Tehran, Tehran, Iran
Abstract<br />
Background: To assess the therapeutic effect safety and feasibility of this method in<br />
patients with myocardial infarction.<br />
Method: 4 patients with history of acute myocardial infarction within 3 months<br />
underwent <strong>coronary</strong> <strong>artery</strong> <strong>bypass</strong> <strong>graft</strong>ing. Autologus AC 133+ bone marrow stem cells<br />
were injected intra-myocardially in the infracted border zone at the time of <strong>surgery</strong>. In<br />
nest four weeks we are going to schedule cell transplantation in six cases.<br />
Results: Global and regional left ventricular function would be evaluated by stress<br />
echocardiography. Ischemia and viability of target area of myocardium were evaluated by<br />
thallium scan. Final results would be reported after 3-4 months.<br />
Conclusion: We believe that implantation of AC133+ bone marrow stem cell into the<br />
heart is safe and might induce cell regeneration with angiogenesis in infracted areas thus<br />
improving function and perfusion of the myocardium.<br />
140<br />
Rest and Stress echocardiographic evaluation of patients with<br />
AVR for estimation of mismatch between effective area and<br />
body surface area<br />
Sadeghian H, Kamangari A, Marzban M, Mandegar MH, Karimi AA, Davoodi S ,<br />
Salarifar M, Ahmadi SH, Abbasi SH and Madani Civi M
Tehran Heart Center, Medical Sciences/University of Tehran, Tehran, Iran<br />
Abstract<br />
Background: The aim of this study is to evaluate the appropriation between the size of<br />
prosthetic Aortic valve and body surface area in patients with AVR because of AS.<br />
Prosthetic Aortic valve replacement in a small aortic root raises concern about its<br />
hemodynamic effect.<br />
Methods: 12 AVR patients were evaluated with exercise stress echocardiography, peak<br />
gradient, effective orifice area and valve index were evaluated at rest and peak exercise.<br />
Results: Two patients had ideal hemodynamic results (peak gradient, Mean gradient<br />
appropriate, valve index > 1 cm 2 /m 2 at rest and exercise) (group AI).<br />
Five patients had intermediate hemodynamic results (good peak and mean gradient and<br />
valve index > 1 cm 2 /m 2 at rest but peak gradient, MG and or VI < 1 cm/m at peak<br />
exercise) (group A II).Five patients had inappropriate hemodynamic results at rest (PG,<br />
MG elevated and / or valve index < 1 cm 2 /m 2 ).prosthetic Aortic valve size / BSA = 14/48<br />
AI, 12/53 AII, 12/22 B. The difference between group AI and AII was significant, but not<br />
meaningful statistically, (P = 0.08). The difference between group AI and B was<br />
meaningful statistically, (P = 0.05).<br />
Conclusion: For ideal hemodynamic results, we can consider Aortic root enlargement in<br />
small aortic roots with large BSA. BSA: body surface area PG: peak gradient MG: mean<br />
gradient :Valve Indexe ffective orifice area<br />
BSA<br />
141<br />
Relation between age and sex of CABG patients and kind and<br />
number of risk factors<br />
Sadeghian S, Darabian C, Haji Zeinali AM, Karimi A, Amirzadegan A, Marzban<br />
M, Abbasi K and Hanafizadeh B<br />
Tehran Heart Center, Medical Sciences/University of Tehran, Tehran, Iran
Abstract<br />
Background: Regarding the importance of knowledge of the risk factors (RF) in<br />
preventing atherosclerosis the rate of risk factors was studied in CABG patients at<br />
different ages based on their sex.<br />
Methods: A questionnaire including the age, sex, and risk factors of the disease was<br />
designed for all CABG patients who have been hospitalized in the past 11 months (from<br />
23 Aug 2003 to 19 may 2004).these questionnaires were filled out after bedside<br />
interviews and lab tests. Meanwhile, the same questionnaire was filled out for the patients<br />
who had normal angiographies as the control group.<br />
Results: Out of 2734 CABG patients, 79% were men and 21% were women. The<br />
women had an average age of 60 years and the men had an average of 57.9 years. The<br />
highest rate of RF in the men under 45 years old was cigarette smoking (63.5% control<br />
group: 17.4%), hypercholesterolemia (49.6% control group: 7%) and positive FH (49.4%,<br />
control group: 26.1%). The highest rate of RF in the women under 45 years old was<br />
hypercholesterolemia (55.6%, control group: 11.1), diabetes mellitus (48.9%, control<br />
group: 3.4%), and positive FH (48.9%, control group: 37.9%). In comparison with the<br />
control group, the highest increase in the rate of RF in this group was seen in women with<br />
diabetes mellitus which can indicate the importance of diabetes mellitus in this age group.<br />
The highest rate of RF in the men 45-55 age group was cigarette smoking (58.3%, control<br />
group: 27.7%), in 55-56 age group was cigarette smoking (45.3%, control group: 43.5%),<br />
and in 65-75 age group was diabetes mellitus (35.2%, control group: 16.7%). The highest<br />
rate of RF in the women of 45-55age group was hypercholesterolemia (62.3%, control<br />
group: 28%), in 55-56 age group was hypercholesterolemia (63.6%, control group:<br />
56.3%), and in 65-75 age group was hypercholesterolemia (596%, control group: 44.4%).<br />
The largest number of risk factors was 2 for men under 65 years old and 1 for men over<br />
65 years old. In women the largest number of risk factors was 2 in all age groups.<br />
Conclusion: In general in men the rate of risk factors of cigarette smoking, positive<br />
FH, and hypercholesterolemia decrease as their age increases, but the rate of diabetes<br />
mellitus increases as their age increases. The rate of HTN in men increases till the age of<br />
65 and then decreases. In women the rate of positive FH decreases till the age of 75, but<br />
there was no meaningful statistical relation between "cigarette, DM,<br />
hypercholesterolemia, and HTN risk factors" and different age groups.<br />
142<br />
Early results and 12 months follow up of PTMC<br />
Salarifar M, Sadeghian H, Kazemi Saleh D, Kassaian E, Haji Zeinali A, Alidoosti<br />
M, Sobh Bidarai and Paydari N<br />
Tehran Heart Center, Medical Sciences/University of Tehran, Tehran, Iran
Abstract<br />
Background: Percutaneous transvenous mitral commissurotomy (PTMC) is now the<br />
treatment of choice for selected patients with symptomatic mitral stenosis (MS) with<br />
mitral valve area (MVA)
Abstract<br />
Background: Regarding the higher danger of left main <strong>coronary</strong> arterial disease<br />
(LMD) in comparison with other kinds of <strong>coronary</strong> <strong>artery</strong> disease (CAD), the study of the<br />
rate of this disease in the total CAD patients and their ages and sex may probably help us<br />
to diagnose these patients earlier.<br />
Methods: A questionnaire was filled out for all patients who were candidates for CABG<br />
during a period of six months (from 23 Sep 2003 to 19 Apr 2004) after bedside<br />
interviews, lab tests, and angiography.<br />
Results: Out of 1465 CAD patients, 136 patients (7.2%) had more than 50% left main<br />
<strong>coronary</strong> stenosis (79.7% male and 20.3% female). This shows no statistically<br />
meaningful difference between both sexes in comparison with the total number of each<br />
sex. From the view point of the patients' ages, the most common age for development of<br />
this disease was 55-65 which is the same as CAD. In four age groups, classified from<br />
under 45 to 75 years, the rate of the disease in men was 8.3%, 24%, 34% and 28%<br />
respectively, while in women the rate was 0%, 21%, 39% and 32%. Regarding the age of<br />
CAD development, there was no meaningful difference. From the viewpoint of the<br />
number of risk factors (RF), 14.2% of men had no risk factors, 26.4% had one risk factor,<br />
43.4% two risk factors, 9.4% three risk factors, 4.7% four risk factors and 1.9% five risk<br />
factors, which shows a meaningful difference in comparison with the number of risk<br />
factors in CAD patients of 45-55 age group. 7.1% of the women had no risk factors, 25%<br />
had one risk factor, 49.5% two risk factors, 17.9 % three risk factors, 3.6% four risk<br />
factors, and 0% five risk factors, which shows no meaningful difference in comparison<br />
with the number of risk factors in CAD patients. There was a meaningful difference, from<br />
the viewpoint of the rate of RF, between LMD patients and the total number of the<br />
patients.<br />
Conclusion: The prevalence of LMD in our patients is almost similar to that of other<br />
communities and some factors such as having two risk factors, age group of 55-65,<br />
cigarette smoking for men, and DM for women, increases the probability of LMD<br />
development.<br />
144<br />
Effect of antioxidants on reducing the damaging effect of<br />
cardiopulmonary <strong>bypass</strong>: a clinical study<br />
Marzban M, Mandegar MH, Abbasi K and Hanafizadeh B<br />
Tehran Heart Center, Medical Sciences/University of Tehran, Tehran, Iran
Abstract<br />
Background: Damaging effects of CPB on different organs is a well-known clinical<br />
entity. To reduce these effects some antioxidant agents have introduced, such as<br />
allopurinol, vitamin E and vitamin C. This study was designed to show the potential<br />
benefit of these agents on heart and lung <strong>bypass</strong> patients.<br />
Method: 96 consecutive candidates for elective CABG were divided into two groups.<br />
The study group received allopurinol (1500mg orally in 3 divided doses), vitamin C (3g<br />
in two divided doses) and vitamin E (600mg) on the day before operation. Control group<br />
received placebo. Following indices were recorded: demographic data, EF, CPB time,<br />
cross-clamp time, ICU stay, hospital stay, IABP use, inotrope use, serial EKG, serum<br />
cardiac enzymes, PaO2, PAO2, alveoloatrial O2 difference and intubation time.<br />
Results: There was a significant difference in indices of myocardial damage (EKG and<br />
serum enzymes) between the two groups ( p
Abstract<br />
Background: Previous studies have suggested that cardiac resynchronization achived<br />
through atrial-synchronized pacing produces clinical benefits in patients with heart failure<br />
who have an intraventricualr and interventricular conduction delay. We performed CRT<br />
in patients with severe heart failure in our center.<br />
Methods: Between July 2003 and May 2004 twelve patients (11males and 1 female<br />
with average age of 58±13.2 years) with severe symptoms of heart failure associated with<br />
ejection fraction of 30% or less and QRS interval 136 msec or more underwent CRT. To<br />
evaluate progress in our patient conditions we used ECG, echocardiography and<br />
exertional test, before and after the procedure. Mean follow up period was 169±108 days.<br />
MRI was performed for nine patients before CRT implantation.<br />
Results: 10 patients experienced an improvement in functional class and exertion time<br />
in exertional test. Echocardiography showed decreased LV size and (MR grading). One<br />
patient had no clinical progress and is a candidate for cardiac transplantation. In nine<br />
patients MRI showed asynchron wall and septal movement. Among 3 patients without<br />
MRI report, one case died shortly after cardiac transplantation due to transplant rejection.<br />
Conclusion: Cardiac Resynchronization results in significant clinical improvement in<br />
patients who have severe heart failure with an intraventricular and interventricular<br />
conduction delay. In addition; MRI guided patient selection could help to achieve more<br />
benefactions for the patients.<br />
146<br />
High-dose heparin to prevent deep venous thrombosis in slow<br />
pathway ablation<br />
Yamini Sharif A, Moghddam M, Kazemi-Saeed A and Lotfi-Tokaldany M
Tehran Heart Center, Medical Sciences/University of Tehran, Tehran, Iran Dr. Shariati Hospital, Medical<br />
Sciences/University of Tehran, Tehran, Iran<br />
Abstract<br />
Background: Deep Venous Thrombosis (DVT) is a rare complication of slow pathway<br />
ablation (SPA). We decided to increase the dosage and duration of heparin administration<br />
to prevent complication.<br />
Methods: Between 1995 and 2002, we recorded 2 cases of DVT in 148 patients who<br />
underwent SPA for atrioventricular nodal reentrant tachycardia (AVNRT).<br />
Anticoagulation consisted of 5000 units of heparin IV bolus, followed by 1000 units/hour<br />
up to the end of the procedure. Mean patient age was 46.9±13.4 years. Average procedure<br />
time was 2.8±1.4. After the 2 cases of DVT, we decided to increase the initial IV heparin<br />
dosage to 10,000 units in adults and continue heparin at 1000 units/hour for 24 hours. 92<br />
patients (mean age of 48.8±13.4 years) underwent SPA with the new anticoagulation<br />
regimen. Average procedure and fluoroscopy times were 60±10 and 10±3 minuets,<br />
respectively. Mean hospitalization period was 3.3±0.8 days and duration of follow up<br />
was 265±128 days.<br />
Results: No bleeding events or DVT occurred in the patients who received high-dose<br />
heparin.<br />
Conclusion: Increasing the dosage and the duration of heparin prevented DVT in out<br />
patients, without any additional risk of bleeding.<br />
147<br />
How Safe or Feasible is <strong>Post</strong> CABG PCI<br />
Kazemi Saleh D, Haji Zeinali A, Kassaian E, Salarifar M, Alidoosti M, Paydari<br />
N and Madani Civi M<br />
Tehran Heart Center, Medical Sciences/University of Tehran, Tehran, Iran
Abstract<br />
Background: Redo-CABG is usually associated with more complications and<br />
mortality so, feasibility and safety of PCI in this group of patients is important.<br />
This study was performed to evaluate success rate, complications and late outcomes of<br />
PCI in patients with history of previous CABG and comparing the results with patients<br />
with no history of previous CABG.<br />
Methods: Analysis of data of 1376 consecutive patients who underwent PCI from April<br />
2003 to March 2004 revealed that38 of these patients had history of previous CABG.<br />
We analyzed and compared the rate of mortality, early complications, success rate and<br />
MACE during follow up between these two groups (group A=Previous history of<br />
CABG, group B= No history of CABG).<br />
Results: Success rate in two group was (97.2% in group A and 98.6 % group in B,<br />
P = NS). The rate of mortality was also similar (0 % in group A, 1.2 % in group B,<br />
P = NS). The rate of re-PCI or redo CABGs was also the same in two groups (7.7 %<br />
group A vs. 2 % group B, P= NS) and (0 % group A vs. 2.5 % group B, p = NS),<br />
respectively. The rate of MACE during follow up (9.64 mo ± 2.4) was 8.3 % in group A<br />
vs.6.6 % in group B (P = NS).<br />
Conclusion: There are no significant differences regarding mortality, early<br />
complications, success rate and MACE rate during follow up between PCI patients with<br />
or without history of previous CABGs.<br />
148<br />
A report of first fractional flow reserve (FFR) measurements<br />
in Iran<br />
Kassaian E, Salarifar M, Alidoosti M, Haji zeinali AM, Kazemi Saleh D, Majd<br />
Ardakani J, Abbasi H and Padegan M<br />
Tehran Heart Center, Medical Sciences/University of Tehran, Tehran, Iran
Abstract<br />
Background: Coronary <strong>artery</strong> stenosis of moderate severity is often a challenge for<br />
decision making and planning an appropriate management. Furthermore waiting for non<br />
invasive testing such as SPECT in patients admitted for acute chest pain is often time<br />
consuming and prolongs hospital stay. FFR which can be derived easily from the ratio of<br />
the mean distal <strong>coronary</strong> <strong>artery</strong> pressure to the aortic pressure during maximal<br />
vasodilation is useful for making clinical decisions concerning patients with ambiguous<br />
clinical symptoms and moderate <strong>coronary</strong> stenosis as determined angiographically.<br />
Methods: According to a specific protocol during the year 2004 we are going to<br />
measure FFR in patients with moderate stenosis. In this study we want to compare the<br />
results of FFR with SPECT and to know if measuring FFR can change the therapeutic<br />
plans of these patients.<br />
Results: For the first 5 patients (mean age 57.8) for whom FFR has been measured 7<br />
<strong>coronary</strong> arteries were evaluated. Of these patients 2 of them had FFR
diameter of the culprit <strong>coronary</strong> <strong>artery</strong> influences the outcome of an attempted<br />
percutaneous <strong>coronary</strong> intervention (PCI) in the current era of interventional cardiology.<br />
Methods: A total of 1344 patients undergoing PCI were divided into groups with<br />
reference diameter”2.5 mm (n=305) and>2.5 (n=1039). Success and in-hospital and 9-<br />
month major adverse cardiac events (death, myocardial infarction and target vessel<br />
revascularization) rates between both groups were compared.<br />
Results: Patients with lesions in small vessel were more frequency female (36% vs.<br />
27%; p= 0.006), diabetic (30% vs. 21%; p=0.005), had multi-vessel involvement (45%<br />
vs. 15%; p
Background: Atrial fibrillation (AF) is a frequent arrhythmia among the cardiac<br />
patients and because of increased risk of thromboembolism in this arrhythmia<br />
discrimination of effective risk factors in producing left atrial (LA) thrombosis is<br />
clinically important. Lipoprotein (a) [LP (a)] has similar structure as plasminogen, so<br />
when it is high can be a risk for prevention of fibrinolysis (thrombogenesis).<br />
Methods: This study is a case control among the chronic AF patients mostly with mitral<br />
stenosis. LA thrombus had been confirmed by transthoracic and transesophageal<br />
echocardiography.<br />
Results: 50 patients mostly with mitral stenosis had been studied half of them had LA<br />
thrombosis (patient group) and half of them had no LA thrombosis (control group). All of<br />
them had chronic AF. Between sex and LA gradient and existence of LA thrombus was<br />
no significant correlation. In the control group © age was 45±11y in contrast to patient<br />
group (p) where it was 57±9y. LA size was 49±5mm ( c ) and 56±9mm (p) La blood<br />
velocity was 12±2 cm/sec ( c) and 5±3 cm/sec (p) LP(a) concentration was 30±6.7 mg/dl<br />
( c) and 55±2.75 mg/dl (p). Significant correlation (p
Back ground: Coronary <strong>artery</strong> disease is the treating cause of mortality at present.<br />
So, understanding the different factors while affect this disease can help for better<br />
prevention of CAD.<br />
Methods: From February 2003 to December 2003, the blood group and Rh of 2026<br />
patients with documented <strong>coronary</strong> <strong>artery</strong> disease who underwent <strong>coronary</strong> <strong>artery</strong><br />
<strong>bypass</strong> <strong>surgery</strong>, was preoperatively determined in a routine laboratory test.<br />
The frequency of each blood group and Rh in the study group was compared with<br />
frequency of blood groups and Rh in Iranian general population that has been already<br />
published by Blood Transfusion Organization of Iran. Also in each group of patients with<br />
different blood group the frequency of main risk factor for CAD, (HIP, HTN, NIDDM,<br />
smoking) was assessed to evaluate any correlation between blood group and known risk<br />
factor with CAD.<br />
Result: The frequency of blood groups( A,B,AB, O)of these patients were as follow:<br />
A=650(32.1%), B=503(24.8%), AB=153(7.5%), O=720(35.6%) and 1830(90.5%) of<br />
them were Rh positive while 193(9.5%) were Rh negative. In evaluation of the frequency<br />
each blood group and Rh in the study group versus Iranian general population no<br />
significant difference was detected. In CAD patient with different blood groups, no<br />
significant difference was detected. In CAD patient with different blood groups, no<br />
significant difference was detected in frequency of risk factors.<br />
With considering of age the frequency of each blood group was similar in patients under<br />
and above 45 years old.<br />
Conclusion: There is no correlation between different blood groups and Rh and<br />
development of CAD. Also the frequency of main risk factors is equal in patients with<br />
different blood groups. Blood groups have no effect in development of premature CAD.<br />
152<br />
Stem cell transplantation in patients with acute myocardial<br />
infarction; a single center registry<br />
Salarifar M, Kassaian E, Kazemi Saleh D, Alidoosti M, Haji Zeinali A,<br />
Sadeghian H, Ghavamzadeh A, Ali Moghadam K, Majd Ardakani J and Hakki<br />
kazazi E<br />
Tehran Heart Center, Medical Sciences/University of Tehran, Tehran, Iran
Abstract<br />
Background: Many clinical and experimental studies reveal that blood derived or bone<br />
marrow derived progenitor cells could beneficially affect post infarction remodeling. We<br />
have designed a study protocol to evaluate the effects of these cells in conjunction with<br />
TUMS hematologic research center. The main purpose of this study is to examine if<br />
intra<strong>coronary</strong> transplantation of autologous hematopoietic bone marrow derived<br />
progenitor cells could improve patients ejection fraction and extent of viable tissue.<br />
Methods: from July to October 2004; 12 patients with reperfused recent (within 30<br />
days) AMI will be included in the study to received intra<strong>coronary</strong> infusion of bone<br />
marrow derived autologus hematopoeitic stem cells into the infracted related <strong>artery</strong>.<br />
Ventricular EF, regional wall motion and extent of non viable tissue are measured at base<br />
line and 3 months after the procedure using stress echocardioghraphy, myocardial<br />
perfusion scan and dobutamine stress echocardioghraphy. Also the procedure and in<br />
hospital reactions and complications will be measured.<br />
Results: primary stenting was done in our first 35 years old patient with recent<br />
anteroseptal MI with 95% stenosis of the proximal LAD and EF=30%. 8x 10 16<br />
hematopoeitic stem cells were injected with over the wire balloon technique. We are<br />
going to present the results of the short term follow up of these patients in December<br />
2004.<br />
153<br />
Short term results of renal <strong>artery</strong> angioplasty (stenting) on<br />
blood pressure and serum creatinine<br />
Haji Zeinali A, Kazemi Saleh D, Salarifar M, Kassaian E, Alidoosti M, and Hakki<br />
kazazi E<br />
Tehran Heart Center, Medical Sciences/University of Tehran, Tehran, Iran<br />
Abstract<br />
Back ground: Angioplasty and stenting are a good alternative treatment for renal<br />
<strong>artery</strong> stenosis (RAS), which have the advantage of avoiding general anesthesia and the
discomforts of <strong>surgery</strong>. Prevalence of atherosclerotic RAS in old hypertensive CAD<br />
patients in high and angioplasty of significant RAS helps in the management of both<br />
HTN and CAD symptoms. This report is a summary of the primary results of our cases<br />
from 2002.<br />
Methods:21 renal angioplasties (18 patients) were done (mean age 58±14 years old) in<br />
11 males and 7 females.17 of them were hypertensive, 6 diabetic, 9 had renal dysfunction<br />
(Cr>1.5) and associated CAD were seen in 12 patients. All of them had stenosis•70%<br />
with 9 right RAS, 6 leftand 3 bilateral RAS. Five stenoses were ostial, 3 had 99%<br />
stenosis and 2 were total occlusions. 17 angioplasties were done from the right or left<br />
femoral <strong>artery</strong> and one brachial approach. The stents were 14 Herculink, 3 Bridge, 3<br />
express vascular and 1 S7. Predilation was done in 7 and direct stenting in 11 cases. <strong>Post</strong>dilation<br />
was done in 7 cases.<br />
Results: In 12 renal stenting procedures with mean stenosis 85%±15, success rate was<br />
100%. Major procedural complications (death, MI, emergency <strong>surgery</strong>) were zero. Minor<br />
femoral <strong>artery</strong> complications were seen in two cases. Elevation of serum creatinine was<br />
seen in the first day because of dye in all patients and decreasing serum Cr in 6 of 9<br />
uremic patients took place from the third day. One patient needed dialysis because of<br />
symptomatic uremia. A decrease in BP took place from the first day in 12 of 17 patients.<br />
In 4 months of follow up, there was one mortality because of underlying CHF and CRF.<br />
No case of MI, CVA and repeat admission was seen. From 17 hypertensive patients, 2<br />
had no HTN and 10 had mild HTN with minimal drug treatment and 5 had no change in<br />
drug consumption. From 9 uremic patients, serum Cr was increased in one, unchanged in<br />
2, and decreased in 6 patients (60%).<br />
Conclusion: renal <strong>artery</strong> angioplasty (stenting) is a safe alternative for <strong>surgery</strong>.<br />
Primary success rate without major complications was near 100% and the effect on BP<br />
and serum Cr in follow up is significant.<br />
Outcome of primary percutaneous <strong>coronary</strong> intervention in<br />
acute my cordial infarction.<br />
Alidoosti M, Salarifar M, Haji Zeinali A, Kassaian E, Kojouri J, Kazemi Saleh<br />
D, Soleimani A, Hakki Kazazi E and Dariyani Saeed K.<br />
154<br />
Tehran Heart Center, Medical Sciences/University of Tehran, Tehran, Iran<br />
Abstract<br />
Background: There is increasing evidence that primary PCI, when carried out by
experienced interventional cardiologist in high volume angiography laboratory is superior<br />
to thrombolytic therapy especially in high risk patients (hemodynamic instability, large<br />
anterior myocardial infarction, elderly & diabetics).<br />
Method: we established the protocol of primary PCI in patients with ST segment<br />
elevation MI (especially high risk cases) admitted within 12 hours of onset of symptoms,<br />
if balloon dilatation could be performed within 90 minutes of admission (day time).<br />
Results: 33 cases (21-80 year old, mean age 53±12) of primary PCI were performed<br />
between April 2003 and March 2004. Two thirds were accomplished within 4 hours of<br />
symptoms onset. Six (18%) of patients were in cardiogenic shock (two were transferred<br />
to cath lab under CPR). Target vessels were; LAD (n=21), RCA (n=9), LCX (n=2) & left<br />
main (n=1). In seven patients, a second critically stenotic vessel was also approached<br />
additionally (five diagonals, one LAD, one LCX ). Our procedural strategy was: primary<br />
stenting (n=22), provisional stenting (n=6), direct stenting (n=1) &pure only balloon<br />
angioplasty (n=3). Intra-aortic balloon was inserted in six patients. protection device was<br />
used in two. Angiographic success was achieved in all patients. Major complications in<br />
follow up period {3-14 months; mean :7 months} were; death (n=5) mostly in shock<br />
group (80%), but in non shock group mortality was 4% (1/25), non fatal MI (n=1) &<br />
target lesion revascularization (n=1) due to subacute thrombus also occurred. Patients<br />
with adverse outcome had significantly (p=0.006) lower systolic pressures (90±20mmHg)<br />
relative to those with favorite outcomes (129±28 mmHg). Moreover, patients with<br />
adverse outcomes had significantly lower ejection fraction<br />
(22.5 % vs. 53%).<br />
Conclusion: These encouraging results particularly in non-shock group are<br />
comparable with the other reports and persuade us to perform more primary PCI in high<br />
risk patients.<br />
Comparing success rate complications and late outcome in<br />
<strong>coronary</strong> intervention for total and non total occlusion<br />
Kazemi Saleh D, Kassaian E, Haji Zeinali A, Salarifar M, Alidoosti M, Sobh<br />
bidari P and Fallah N<br />
155<br />
Tehran Heart Center, Medical Sciences/University of Tehran, Tehran, Iran<br />
Abstract
Background: PCI in <strong>coronary</strong> total occlusion is a complex procedure with lower<br />
success rate and more complications compared to non total occlusion. In this study, we<br />
compared success rate complications and late outcomes in <strong>coronary</strong> intervention for total<br />
and non total occlusion.<br />
Methods: The data of 1344 consecutive patients who underwent <strong>coronary</strong> intervention<br />
during April 2003 to March 2004 were analyzed. 175 cases were total occlusion<br />
interventions (TOI) comparing to 1169 cases of non total occlusion interventions (NTOI).<br />
All the confounding variables were adjusted.<br />
Results: Success rate was (94.3% in TOI vs. 99.1% NTOI p
Background: To perform slow pathway ablation, multiple catheters (usually 4-5) are<br />
often inserted percutaneously. In this study it is hypothesized that it is safe and feasible to<br />
perform both diagnostic and therapeutic treatment for AV Nodal re-entrant Tachycardia<br />
(AVNRT) using 2-catheter inserted via the right femoral vein alone.<br />
Methods: Eighty consecutive patients (14 males and 66 females, mean age of 49.4±11<br />
years) with AVNRT underwent Radiofrequency (RF) ablation with the minimally<br />
invasive strategy as the initial approach. Both the diagnostic electrophysiologic study and<br />
catheters ablation were performed as a combined procedure in all patients. A mean of<br />
3±3 (Rang 1-10) RF applications were required for successful ablation. Procedure and<br />
fluoroscopy times were 60±10 minutes and 10±3 minutes, respectively.<br />
Results: For all patients (except one patient with dextrocardia and corrected<br />
transposition) undergoing the procedure, the 2 catheters approach could be employed<br />
successfully. Two patients had Wenkebach AV block which after a few days was<br />
changed to first degree AV block.<br />
Recurrence occurred in 3 patients. Two patients were treated in the second and the<br />
third underwent a third ablation session. The success rate and recurrence rate was<br />
similar to conventional methods.<br />
Conclusion: Two-catheter approach could be considered as initial strategy for patient<br />
undergoing ablation for AVNRT.<br />
Relation between the number of involved <strong>coronary</strong> arteries in<br />
patients and the kind and multiplicity of risk factors<br />
157<br />
Sadeghian S, Haji Zeinali AM, Salarifar M, Kazemi Saeed A, Yamini Sharif A,<br />
Sadeghian H and Hanafizadeh B<br />
Tehran Heart Center, Medical Sciences/University of Tehran, Tehran, Iran<br />
Abstract
Background: Regarding the proved effect of risk factors (RF) in development of CAD<br />
the relations between each of them singly and along with other risk factors and the<br />
patients involved <strong>coronary</strong> <strong>artery</strong> were analyzed in order to determine whether the effects<br />
of risk factors in development of multi vessel disease are similar or different.<br />
Methods: All the patients who were recognized as CAD patients through angiographies<br />
during a period of six months (from 23 September 2003 to 19 April 2004) were studied<br />
from the view point of the anatomy of their <strong>coronary</strong> arteries and the prevalence of risk<br />
factors.<br />
Results: Out of 1645 CAD patients 4% had MVD and 74% 3VD. The most common<br />
age group for this disease in all the three kinds in both sexes was 55-65 and the average<br />
for the disease was 58 years. In men there were meaningful relation between the patients<br />
involved <strong>coronary</strong> arteries and cigarette smoking (p=0.001) diabetes mellitus (p=0.001)<br />
positive family history (p=0.002) and risk factors multiplicity (p=0.001) and in women<br />
there were meaningful relations between the patients involved <strong>coronary</strong> arteries and<br />
hypercholesterolemia (p=0.002) diabetes mellitus (p=0.001) risk factors multiplicity<br />
(p=0.014) but for other risk factors there was no meaningful relation.<br />
Conclusion: This study indicates that different kinds of risk factors have different<br />
effects on the number of the patients involved <strong>coronary</strong> arteries in both sexes. Risk<br />
factors multiplicity and diabetes mellitus in both sexes were effective on development of<br />
multi vessel <strong>coronary</strong> <strong>artery</strong> disease. In men cigarette smoking and family history were<br />
effective in this regard and in women hypercholesterolemia was effective; but in other<br />
risk factors this effect was not proved.<br />
158<br />
Angiographic findings in 401 very premture CADpatients<br />
(age
in very premature patients (age
Abstract<br />
Background: Injection of thrombolytics is still the most common treatment of acute<br />
myocardial infarction. Regarding the consumption of specific kinds of them in our<br />
country and inadequacy of these effective substances in some reports, this study has been<br />
designed.<br />
Methods: 110 acute MI patients who received thrombolytic treatment in first 12 hours<br />
and their angiography was done till 20 days after receiving treatment were selected, and<br />
the highest "TIMI 2 flow" was regarded as patency. For 49% of the patients, the drug was<br />
injected in the first two hours and in 39% of them it was injected in the first 2-6 hours.<br />
Results: 73 patients underwent angiography during the first ten days and had a patency<br />
of 61% in the involved <strong>artery</strong>, and the remaining 37 ones underwent angiography during<br />
the second 10 days and had a patency of 50%. The average of patency in 20 days was<br />
55%. The rate of patency had no relations with the period of drug injection up to 6 hours<br />
(P=0.09), the location of MI, or the involved arteries (P=0.09). Comparing two groups of<br />
the patients with patent and occluded arteries, there was no obvious difference between<br />
ST elevation changes, but enzymatic changes in 12 hours and 24 hours had obvious<br />
difference (P=0.02). EF of both groups had obvious difference and it was 5% higher for<br />
the patent group (P=0.03).<br />
Conclusion: Comparing the results with five similar studies indicates that the patency<br />
rate in the first 10 days was 9% less than that of the similar treated patients and 5% more<br />
than that of non-treated patients. Patency rate for all the patients in the first 20 days<br />
was16% less than that of the similar treated patients and was not different from that of the<br />
patients who did not receive thrombolytic treatment. With regard to EF and enzymes, we<br />
can conclude that this drug is effective but not as much as those in other studies.<br />
160<br />
Short term results of carotid <strong>artery</strong> stenting: A single center<br />
registry<br />
Kassaian E, Kazemi Saleh D, Alidoosti M, Haji Zeinali A, Salarifar M, Kojoori J,<br />
Gheini M, Shirani Sh, Hakki kazazi E and Abbasi E.<br />
Tehran Heart Center, Medical Sciences/University of Tehran, Tehran, Iran
Abstract<br />
Back ground: Angioplasty and stenting are alternative treatments for carotid <strong>artery</strong><br />
stenosis which have the advantage of avoiding general anaesthesia, cranial never injury<br />
and the discomforts of <strong>surgery</strong>. Although there are several years of experience in western<br />
countries, it is still a new therapeutic modality in Iran. Therefore we started a carotid<br />
stenting program in our center since December 2003. This is a summary of the<br />
preliminary report of our first 18 patients.<br />
Methods: From December 2003 to July 2004, 18 consecutive patients were treated by<br />
angioplasty and stenting (12 males and 6 females with mean age of 64.88± 8.53 years):<br />
two patients were symptomatic with more than 60% stenosis; 16 patients were<br />
asymptomatic with more than 80% stenosis who had high risk <strong>coronary</strong> anatomies (6 left<br />
main and all multi-vessel <strong>coronary</strong> lesions) and were CABG candidates. All patients were<br />
evaluated by a neurologist pre- and post-procedure and had at least a baseline brain MRI<br />
or CT scan prior to the procedure. In all cases self-expandable stents (Acculink in 12 and<br />
wall stent in 6) and distal protective devices (Accunet in 12 and filter wire EZ in 6) were<br />
used in the left (n=7) or right (n=11) internal carotid <strong>artery</strong>. Follow-up period ranged<br />
from 1 to 6 months (mean 3.1± 2 months).<br />
Results: The procedural success rate was 100%. Mean carotid <strong>artery</strong> stenosis was<br />
85.18% ± 9.37% before and 10.2%± 3.5% after the procedure. After stent deployment,<br />
control cerebral angiogram was normal in all patients. Neurologic assessment showed no<br />
transient neurological deficit, minor or major stroke during the procedure, predischarge<br />
and during the follow-up. Three cases died of unrelated causes during the first month of<br />
follow-up. One of them died in the CCU after three days with pulmonary edema and<br />
cardiogenic shock, another death was one day after CABG (8 days after the procedure)<br />
with bradycardia and electromechanical dissociation, and the third was 5 days after<br />
discharge with hypoglycemia and MI.<br />
Conclusion: Carotid stenting is a safe and feasible method in patients who are high risk<br />
for surgical carotid endarterectomy.<br />
161<br />
Comparing background and confounding factors in the<br />
MACE and non-MACE patients; late outcome assessment of<br />
PCI<br />
Salarifar M, Alidoosti M, Kazemi Saleh D, Haji Zeinali A, Kassaian E, Dariyani<br />
Saeed K, Fallah N and Paydari N<br />
Tehran Heart Center, Medical Sciences/University of Tehran, Tehran, Iran
Abstract<br />
Background: PCI is a common choice for revascularization of CAD patients. But still<br />
there is debate about long-term results of PCI. Forty percent restenosis in angioplasty and<br />
25-30% restenosis in stenting with bare stents has been reported. However by using the<br />
new generation of stents, the restenosis rate has decreased significantly.<br />
Methods: So far 534 consecutive patients, who underwent PCI from April 2003 to<br />
September 2003, were followed based on the follow-up clinic data, filing room data and<br />
phone survey. Based on the late outcome data, patients were divided into 2 groups. Group<br />
A; MACE group and group B; non MACE group. We compared the early rates including<br />
risk factors, procedural and device success, complications and procedural details in these<br />
groups. All confounding variables were adjusted.<br />
Results: The MACE rate in the patients who completed the follow up period (mean,<br />
10.2± 1.6) was 6.3%. MACE group consisted of 7 MI (29.2%), 9 CABG (37.5%), 8 Re-<br />
PCI (33.3%), 7 TVR , 5 TLR and 4 mortalities. Age and gender distribution of patients in<br />
A and B groups was the same. Also there was no statistically meaningful difference in the<br />
frequency of risk factors. Success rate in the two groups was significantly different<br />
(91.7% group A vs. 98.5% group B; p value
Abstract<br />
Background: Outcome studies of conventional balloon angioplasty have established<br />
increased in-hospital and 1-year mortality in patients with left ventricular dysfunction. It<br />
is unclear whether recent practice innovation, including stents and adjunctive<br />
pharmacotherapy, have made percutaneous <strong>coronary</strong> intervention (PCI) safer and more<br />
effective in patients with LV dysfunction.<br />
Methods: We evaluated the influence of LV ejection fraction (EF) on in-hospital and 9<br />
months outcomes in 1,344 patients within our dynamic registry. Patients with acute<br />
myocardial infarction were excluded. The remaining were divided into two categories:<br />
group 1, EF”40% (n=193), group 2, EF>40% (n=1151). We determined success rate and<br />
the frequency of individual and composite adverse events (death/ myocardial infarction<br />
(MI)/ target vessel revascularization) at discharge and 9 months.<br />
Results: Mean EF in the groups with EF40 was 35±6% and 56±6 %(<br />
success rate 97% vs. 98%) and in-hospital adverse events did not differ between groups<br />
(zero vs. 1%). The composite end point of death /MI/ target vessel revascularization after<br />
9 months was not significantly different, although it occurred more frequently in group 1<br />
patients (8.8% vs. 4.6%).<br />
Conclusion: It seems recent improvement in devices (especially stents) and adjunctive<br />
pharmacotherapy in peri-procedural and follow-up periods results in more successful<br />
complete revascularization in patients with LV dysfunction and clinical outcomes are<br />
almost similar with other patients undergoing PCI.<br />
163<br />
American or European based bare stent: which one is<br />
preferred<br />
Kassaian E, Haji Zeinali A, Salarifar M, Kazemi Saleh D, Alidoosti M, Abbasi<br />
SH and Paydari N<br />
Tehran Heart Center, Medical Sciences/University of Tehran, Tehran, Iran
Abstarct<br />
Background: The role of <strong>coronary</strong> stents in reducing early and long term<br />
complications of percutaneaus <strong>coronary</strong> intervention has been evaluated in multiple<br />
studies. Different types of stents with several brand names are frequently used in our<br />
country. We compared the effects of expensive drug-eluting stents, relatively expensive<br />
FDA-approved American bare stents and cheaper European products (with CE mark of<br />
approval).<br />
Methods: The data of 1197 consecutive patients with 1542 stents who underwent PCI<br />
from April 2003 to march 2004 were analyzed (drug-eluting stents (DES) [Cypher,<br />
Taxus], 5.6% , American-based bare stents [Driver, S660, S7, Biodivysio, Cordis,<br />
Express, Penta, Tetra, Zeta, Jomed], 75.9% and European-based bare stents<br />
[AMG,Coroflex, Genius, Occam, Phytis, Sorin, Tron], 18.5% of all cases). All the<br />
confounding variables were adjusted.<br />
Results: Successful deployment was equal for the groups (99%). There were more<br />
patients with NQWMI in DES patients (3% vs. 1.1% and 0.5% in DES, American-based<br />
and European-based stents consecutively; p=0.05). Regarding long-term results<br />
(including MACE, TVR and TLR), there were significantly less complications in DES<br />
group. Importantly there was no significant difference between American and European<br />
stents regarding all short and long-term outcomes. Conclusion: Although there are some<br />
technical problems with their use, European-based stents have equal efficacy and<br />
complication rate compared to American-based bare stents.<br />
164<br />
Short and long-term results after multivessel PCI<br />
Kassaian E, Kazemi Saleh D, Alidoosti M, Salarifar M, Haji Zeinali A, Paydari N<br />
and Hakki Kazzazi E<br />
Tehran Heart Center, Medical Sciences/University of Tehran, Tehran, Iran<br />
Abstract
Background: The present study evaluated clinical outcomes in patients after multivessel<br />
PCI.<br />
Methods: Of 1374 consecutive patients who had undergone PCI from April 2003 to<br />
March 2004; 796 patients (58%) had angiographic evidence of multi-vessel CAD and 211<br />
patients (21%) underwent multi-vessel PCI. All of these patients underwent PCI in at<br />
least 2 vessels at the same session. In 61% of the vessels, at least one stent was deployed<br />
(in contrast to 89% in single-vessel PCI).<br />
After considering the effects of confounding factors; short and long term results of<br />
patients with multi-vessel PCI were compared to those of single vessel PCI.<br />
Results: Procedural success was high (98.6%); there were no significant differences in<br />
short-term complications( NQMI, CABG, death) between patients with multi- and single<br />
vessel PCI. Multi-vessel PCI patients had higher rate of 9 months MI (4.2% vs. 1.4%<br />
p=0.05). Mace (death, MI and repeat revascularization), TVR and TLR rates were 8.6%.<br />
3% and 2.8% consecutively in multi-vessel PCI patients (no difference with data of<br />
single-vessel PCI cases).<br />
Conclusion: In patients undergoing multi-vessel PCI, short and long term results are<br />
favorable in carefully selected patients.<br />
Short and long term outcome after PCI in patients with acute<br />
165<br />
<strong>coronary</strong> syndrome<br />
Kassaian E, Haji Zeinali A, Salarifar M, Kazemi Saleh D, Alidoosti M, Paydari N<br />
and Padegan M<br />
Tehran Heart Center, Medical Sciences/University of Tehran, Tehran, Iran
Abstract<br />
Background: PCI has been successfully applied in patients with acute <strong>coronary</strong><br />
syndrome (ACS) to carefully selected patients. This is a report of acute (in hospital)<br />
results and 9 months follow up data in patients with acute <strong>coronary</strong> syndrome (recentwithin<br />
the last 2 weeks-ST elevation myocardial infarction (MI), non-ST elevation MI or<br />
unstable angina) who underwent PCI at our center from April 2003 till March 2004.<br />
Methods: Success rate; early (in hospital) complications and 9 months MACE (death,<br />
MI and repeat revascularization), TVR and TLR were analyzed in 200 cases with ACS<br />
(14.6% of all PCI cases) and were compared to data of other patients. Primary PCI cases<br />
were excluded from the study.<br />
Results: Success rate was about 98.5% in both groups. The rate of in-hospital NQMI<br />
amounted to 3% in ACS and 0.9% in other patients (p=0.01). There was only 1 predischarge<br />
death in ACS group. Other acute complications were rare (0.5%) and equal.<br />
During a 9-month follow-up period, there was more MACE rate in acute <strong>coronary</strong><br />
syndrome group (10% vs. 6%, p=0.05) which was mostly due to more death rate (3.4%<br />
vs. 0.7%, p=0.02), and there was a trend towards more cases with repeat<br />
revascularization, TVR and TLR in the ACS group.<br />
Conclusion: Although the short and long-term results after PCI of ACS patients are<br />
within safe limits, there are still more complications in this high-risk group.<br />
Are there any differences in mortality, complications and late<br />
outcomes of PCI in patients with different educational levels<br />
Kazemi Saleh D, salarifar M, Kassaian E, Haji zeinali A, Alidoosti M, Abbasi<br />
SH and Jalali Roodsary M<br />
166<br />
Tehran Heart Center, Medical Sciences/University of Tehran, Tehran, Iran
Abstract<br />
Background: The knowledge of patients about their disease and its necessary care is<br />
dependent on their level of education and this knowledge may affect outcomes of PCI.<br />
This study was performed to compare the incidence of risk factors, early complications,<br />
mortality, success rate and late outcomes in PCI patients with different educational levels.<br />
Methods: The data of 1029 consecutive patients who underwent PCI during April 2003<br />
to March 2004 period were analyzed regarding their educational level in three groups.<br />
Group A with educational level zero, group B with educational level under high school<br />
diploma and group C with educational level above diploma.<br />
Results: 25% of our patients (n=257) were in group A, 60.5% (n=623) in group B and<br />
14.5% (n=149) in group C. The rate of cigarette smoking was significantly different in<br />
the three groups (7.8% group A, 21.2% group B, 16.1% group C, p=0.000). Incidence of<br />
HTN was significantly higher in group A vs. group C (43% vs. 21.5%, p=0.000). Positive<br />
family history of CAD was significantly higher in group C vs. group A (30.9% vs.<br />
16.35%). There were no significant differences regarding success rate and early<br />
complications between all three groups. There was no mortality during hospitalization.<br />
Although the rate of MACE was highest in group A and B (6.8% group A, 5.5% group B,<br />
2% group C, p=ns) but statistically these differences were not significant.<br />
Conclusion: There is no differences regarding mortality, success rate, complication and<br />
MACE during follow up between patients with different educational levels who<br />
underwent PCI.<br />
167<br />
Biopump as a temporary assist device for postcardiotomy<br />
heart failure<br />
Davoodi S, Madani Civi M and Abbasi SH<br />
Tehran Heart Center, Medical Sciences/University of Tehran, Tehran, Iran
Abstract<br />
Background: Ventricular assist devices (VAD) have become an important therapeutic<br />
tool to manage the patients with post-cardiotomy heart failure. We evaluated biopump as<br />
a circulatory support for bridge to recovery in the setting of difficult weaning from<br />
cardiopulmonary machine that were refractory to inotropic and IABP support.<br />
Methods: Between Oct 1998 and June 2004, 1450 patients underwent CABG in our<br />
center. There were 24 cases that required high dose inotropes or IABP for weaning from<br />
CPB machine in the operating room. We used biopump in six patients (52±12 years) with<br />
acute left-sided heart failure following CABG. The patients' characteristics and their risk<br />
factors for developing CAD were recorded.<br />
Results: The success rate was 30% (2 cases from 6pts). Four cases were not weaned<br />
from the biopump after 17±8 hours. Two patients were weaned after 21± 5 hours and<br />
with good outcome. The mean preoperative left ventricular EF was 50%±10. The mean<br />
vessel involvement in these patients was 2.66 (IVD-3VD). The <strong>coronary</strong> <strong>artery</strong> Gensini<br />
score was 89±6 (P value
Background: The number of CABGs is increasing in our country. In spite of this, little<br />
data exists about the risk factors influencing the in-hospital mortality in Iranian patients;<br />
in addition, the effect of body mass index (BMI) on mortality is still in controversial<br />
issue.<br />
Methods: This is a cross-sectional study on 1258 patients who underwent isolated<br />
CABG in our center between 2002 and 2004. The patients were divided in 3 groups: nonobese<br />
(BMI
cigarette smoking). The rate of the patients without the risk factors in our CAD patients<br />
was not known; therefore, this study has been done in order to analyze the percentage of<br />
CAD patients without risk factors out of the whole CAD patients.<br />
Methods: The risk factors in the patients, who were hospitalized to undergo CABG<br />
since July 2003, were studied after interviews and lab tests, and the following results<br />
have been concluded.<br />
Results: Out of 2734 patients, 256 patients (9.3%) had none of the atherosclerosis risk<br />
factors. 81.2% of these patients were men and 18.8% were women, which shows no<br />
meaningful difference between them and the patients who had risk factors. The most<br />
common age of the patients who did not have the risk factors was 65-75 which is 10<br />
years higher than that of the patients who had risk factors (55-65). The prevalence of<br />
the disease in the patients without risk factors and the patients who had risk factors,<br />
based on their age group, were as follows:<br />
Age groups Patients without RF Patients having RF<br />
There were no meaningful differences between the patients who had risk factors and the<br />
ones who did not have the risk factors from the viewpoint of the rate of SVD, 2VD, 3VD,<br />
and even LMD.<br />
Conclusion: In comparison with other studies, the rate of our patients who did not<br />
have risk factors (9.3%) was lower. These patients were distributed in all the age groups,<br />
but the rate increased as their age increased. The rate of patients, with various kinds of<br />
<strong>coronary</strong> <strong>artery</strong> disease, including SVD, 2VD, 3VD, and even left main <strong>coronary</strong> <strong>artery</strong>,<br />
who did not have risk factors, was similar to the rate of the diseases itself.<br />
170<br />
Developmental ultrastructure of mouse embryonic stem cell<br />
derived cardiomyocytes in vitro<br />
Baharvand H, Rohani R, Pyriaie A and Taei A<br />
Tehran Heart Center, Medical Sciences/University of Tehran, Tehran, Iran<br />
Abstract
Background: Stem cell biology has been the subject of much recent discussion.<br />
Embryonic stem cells, derived from the inner cell mass of the blastocyst-stage early<br />
mammalian embryos are expected to become a powerful tool for future regenerative<br />
medicine and developmental biology due to their capacity of self-renewal and<br />
pluripotency. In the present study, developmental ultrastructure of mouse embryonic stem<br />
cells-derived cardiomyocyte was assessed.<br />
Methods: Cardiomyocytes were derived from a newly established murine ES line<br />
derived from a C57B1/6 strain mouse embryo. Cardiomyocytes of 3, 7, 14 and 21 days<br />
after plating (day 7) were processed for immunhistochemistry and transmission electron<br />
microscopy (TEM).<br />
Results: While in 7+21d cardiomyocytes showed all sarcomeric components such as A-<br />
and I-band, Z line, H-band and also M-band, T-Tubule, endoplasmic reticulum and<br />
intercalated discs were present, in early stages (7+3d, 7+7d and 7+14) a few primary<br />
characteristics of subcellular structures found.<br />
Conclusion: Embryonic stem cell provide a good model for cardiomyocyte<br />
development and may use for cell therapy in future.<br />
171<br />
Dose routine magnesium administration prevent perioperative<br />
<strong>coronary</strong> <strong>artery</strong> <strong>bypass</strong> <strong>graft</strong> <strong>surgery</strong> arrhythimas<br />
Najafi M and Haghighat B<br />
Tehran Heart Center, Medical Sciences/University of Tehran, Tehran, Iran<br />
Abstract
Background: Atrial and ventricular arrhythmias are among the most common<br />
complication after <strong>coronary</strong> <strong>artery</strong> <strong>bypass</strong> <strong>graft</strong> (CABG) <strong>surgery</strong>. Previous studies<br />
demonstrated that cardiopulmonary <strong>bypass</strong> itself, results in reduced serum magnesium<br />
level. In this study, we wanted to evaluate the effect of total blood magnesium level<br />
(TMG) on preventing peri-operative arrhythmias by routine regimens of 2-4 gram<br />
supplemental mangnesium (SMG).<br />
Methods: TMG was measured in patients who were scheduled for CABG on 3<br />
occasions [just before anesthesia, just after entering to intensive care unit (ICU)<br />
postoperatively and on the first morning after operation]. Patients were evaluated for<br />
primary cardiac rhythm (97cases) and other variables that could have an influence on<br />
magnesium level (serum creatinine, urine output in operating room and diuretic therapy).<br />
SMG was also recorded in operating room and ICU. Then the patients were evaluated for<br />
the rate of arrhythmia.<br />
Results: Mean TMG level in 160 cases was 2.2, 2.6 and 2 mg/dl on three occasions<br />
respectively. Mean SMG was 2.5 grams. 27 of 97 patients developed post-operative<br />
arrhythmia [AF* (7cases), PAC** (12cases) and PVC*** (16cases)]. Mean serum<br />
creatinine level and urine output were 1.2 mg/dl and 1800 ml respectively. Although<br />
there was a significant difference between TMG on the first and second occasion which<br />
were both in the normal range (P
cardiopulmonary <strong>bypass</strong> (CPB) during <strong>coronary</strong> <strong>artery</strong> <strong>bypass</strong> <strong>graft</strong> (CABG) <strong>surgery</strong>.<br />
Furosemide therapy is regarded as a way of preventing renal compromise due to CPB.<br />
Previous studies have variable results. This study is to determine whether it is necessary<br />
to administer furosemide and if it is what are the best timing and the least amount that<br />
work best.<br />
Methods: Candidates for CABG were divided into 4 groups. 51 patients were oliguric<br />
(U/O*0.2). Group3, had clearly the least U/O before CPB (P
POUR HOSEINI 34-75-77<br />
HAJI ZEINALI 25-27-33-34-35-36-37-38-54-55-61-63-82-83-84-85-87-88-134-<br />
142-143-148-149-150-153-154-155-156-158-159-160-161-162-<br />
163-164-165-166-167-170-174<br />
HOSEINI 59-75<br />
HAGHIGHAT 4-23-24-65-90-105-106-107-117-118-172-173<br />
KHATAMI 70-91<br />
DARABIAN 31-53-56-64-134-142-152-160<br />
DARIANI 19-20<br />
DAVOODI ,S 7-8-67-68-79-80-81-92-93-99-100-101-102-105-108-109-111-112-<br />
115-124-125-126-127-131-132-133-134-135-136-137-138-141-<br />
144-168<br />
DAVOODI .GH 10-11-17-22-29-36-38-43-45-47-49-53-54-55-56-57-58-60-61-63-<br />
69-74-76-86-89-116-164-152-157-159-160-170-174<br />
RABBANI 12-14-128-139<br />
SALARIFAR 25-27-29-31-33-34-35-36-37-54-55-56-62-63-74-82-83-84-85-89-<br />
94-103-104-114-115-131-132-133-134-138-140-143-144-148-149-<br />
150-152-153-154-155-156-158-160-161-162-163-164-165-166-<br />
167-170-174<br />
SOTUDEH<br />
14<br />
SOLEMANI 8-13-14-15-31-48-49-50-51-52-56-65-113-140-155<br />
SHIRANI 33-101-102-137-146-161<br />
SHIRZAD 15<br />
SAHEB JAM 14-15-17-38-39-40-57-64-89-94<br />
SADEGHIAN .H 3-13-17-38-39-40-42-58-64-76-87-89-94-114-115-119-125-132-<br />
134-140-141-143-144-153-158-175<br />
SADEGHIAN .S 10-11-14-17-59-65-73-74-75-77-94-105-114-115-116-132-138-<br />
142-144-152-157-158-159-160-170<br />
SALEHI 3-4-5-7-67-68-69-72-79-0 -81-95-99-109-111-112-119-175<br />
OMRAN<br />
ZOROFIAN 75-77-89<br />
ABBASI .H 7-8-22-25-35-38-42-69-70-71-86-91-99-100-101-102-103-104-<br />
108-124-127-131-133-136-137-149-164-167-168<br />
ABBASI .K 7-8-10-14-15-67-68-69-72-79-80-81-99-109-111-112-113-123-<br />
131-132-133-134-135-136-137-138-142-145<br />
KAZEMISAEID 10-11-17-40-43-45-47-54-56-58-60-61-63-64-76-116-147-151-<br />
157-158<br />
KAZEMI<br />
SALEH<br />
25-33-36-143-148-149-150-153-154-155-156-161-162-163-164-<br />
165-166-167-<br />
KAZEMEINI 62<br />
KASSAEIAN 25-27-33-34-36-37-57-82-83-84-85-103-143-148-149-150-153-<br />
154-155-156-161-162-163-164-165-166-167<br />
KARIMI 7-8-14-15-42-65-67-68-69-70-72-73-74-79-80-81-91-96-99-101-<br />
102-105-108-111-112-113-114-115-123-125-131-132-133-134-
135-136-137-138-141-142-144-175<br />
ALIDOOSTI 25-27-33-34-35-36-37-57-64-82-83-84-85-143-148-149-150-153-<br />
154-155-156-159-161-162-163-164-165-166-167<br />
MARZBAN 3-7-8-13-14-15-36-67-68-69-70-72-79-80-81-91-99-101-102-108-<br />
109-111-112-114-119-123-125-131-132-133-135-136-138-141-<br />
142-144-145-169<br />
MAJD<br />
3-13-42-119-134-140-149-153<br />
ARDAKANI<br />
MOVAHEDI 7-8-14-67-68-70-72-79-80-81-91-99-109-111- 112-123-131-132-<br />
133-135-136-137-138<br />
MIRHOSENI 6-92-93<br />
NEJATIAN 48-50-51<br />
NAJAFI 4-5-8-15-23-24-65-90-95-96-105-106-107-117-118-172-173-176<br />
NEMATI POOR 37-73-74-75<br />
YAMINI 10-11-17-40-43-45-47-54-56-58-60-60-63-64-76-116-146-147-<br />
SHARIF<br />
151-157-158