Study of Blood Contact in Simulated Surgical Needlestick ... - CCIH
Study of Blood Contact in Simulated Surgical Needlestick ... - CCIH
Study of Blood Contact in Simulated Surgical Needlestick ... - CCIH
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
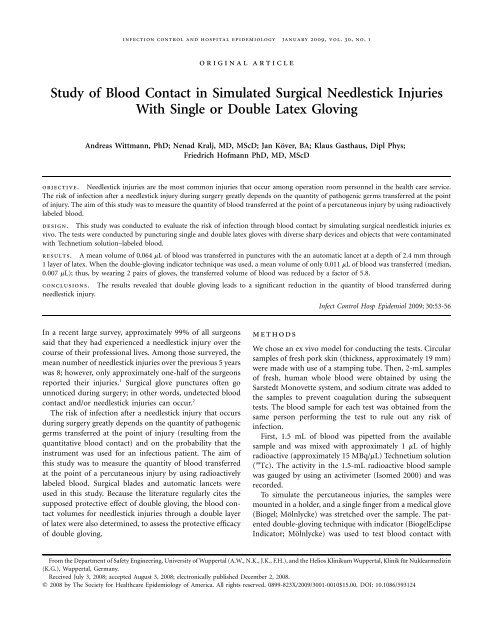
<strong>in</strong>fection control and hospital epidemiology january 2009, vol. 30, no. 1<br />
orig<strong>in</strong>al article<br />
<strong>Study</strong> <strong>of</strong> <strong>Blood</strong> <strong>Contact</strong> <strong>in</strong> <strong>Simulated</strong> <strong>Surgical</strong> <strong>Needlestick</strong> Injuries<br />
With S<strong>in</strong>gle or Double Latex Glov<strong>in</strong>g<br />
Andreas Wittmann, PhD; Nenad Kralj, MD, MScD; Jan Köver, BA; Klaus Gasthaus, Dipl Phys;<br />
Friedrich H<strong>of</strong>mann PhD, MD, MScD<br />
objective. <strong>Needlestick</strong> <strong>in</strong>juries are the most common <strong>in</strong>juries that occur among operation room personnel <strong>in</strong> the health care service.<br />
The risk <strong>of</strong> <strong>in</strong>fection after a needlestick <strong>in</strong>jury dur<strong>in</strong>g surgery greatly depends on the quantity <strong>of</strong> pathogenic germs transferred at the po<strong>in</strong>t<br />
<strong>of</strong> <strong>in</strong>jury. The aim <strong>of</strong> this study was to measure the quantity <strong>of</strong> blood transferred at the po<strong>in</strong>t <strong>of</strong> a percutaneous <strong>in</strong>jury by us<strong>in</strong>g radioactively<br />
labeled blood.<br />
design. This study was conducted to evaluate the risk <strong>of</strong> <strong>in</strong>fection through blood contact by simulat<strong>in</strong>g surgical needlestick <strong>in</strong>juries ex<br />
vivo. The tests were conducted by punctur<strong>in</strong>g s<strong>in</strong>gle and double latex gloves with diverse sharp devices and objects that were contam<strong>in</strong>ated<br />
with Technetium solution–labeled blood.<br />
results. A mean volume <strong>of</strong> 0.064 mL <strong>of</strong> blood was transferred <strong>in</strong> punctures with the an automatic lancet at a depth <strong>of</strong> 2.4 mm through<br />
1 layer <strong>of</strong> latex. When the double-glov<strong>in</strong>g <strong>in</strong>dicator technique was used, a mean volume <strong>of</strong> only 0.011 mL <strong>of</strong> blood was transferred (median,<br />
0.007 mL); thus, by wear<strong>in</strong>g 2 pairs <strong>of</strong> gloves, the transferred volume <strong>of</strong> blood was reduced by a factor <strong>of</strong> 5.8.<br />
conclusions. The results revealed that double glov<strong>in</strong>g leads to a significant reduction <strong>in</strong> the quantity <strong>of</strong> blood transferred dur<strong>in</strong>g<br />
needlestick <strong>in</strong>jury.<br />
Infect Control Hosp Epidemiol 2009; 30:53-56<br />
In a recent large survey, approximately 99% <strong>of</strong> all surgeons<br />
said that they had experienced a needlestick <strong>in</strong>jury over the<br />
course <strong>of</strong> their pr<strong>of</strong>essional lives. Among those surveyed, the<br />
mean number <strong>of</strong> needlestick <strong>in</strong>juries over the previous 5 years<br />
was 8; however, only approximately one-half <strong>of</strong> the surgeons<br />
reported their <strong>in</strong>juries. 1 <strong>Surgical</strong> glove punctures <strong>of</strong>ten go<br />
unnoticed dur<strong>in</strong>g surgery; <strong>in</strong> other words, undetected blood<br />
contact and/or needlestick <strong>in</strong>juries can occur. 2<br />
The risk <strong>of</strong> <strong>in</strong>fection after a needlestick <strong>in</strong>jury that occurs<br />
dur<strong>in</strong>g surgery greatly depends on the quantity <strong>of</strong> pathogenic<br />
germs transferred at the po<strong>in</strong>t <strong>of</strong> <strong>in</strong>jury (result<strong>in</strong>g from the<br />
quantitative blood contact) and on the probability that the<br />
<strong>in</strong>strument was used for an <strong>in</strong>fectious patient. The aim <strong>of</strong><br />
this study was to measure the quantity <strong>of</strong> blood transferred<br />
at the po<strong>in</strong>t <strong>of</strong> a percutaneous <strong>in</strong>jury by us<strong>in</strong>g radioactively<br />
labeled blood. <strong>Surgical</strong> blades and automatic lancets were<br />
used <strong>in</strong> this study. Because the literature regularly cites the<br />
supposed protective effect <strong>of</strong> double glov<strong>in</strong>g, the blood contact<br />
volumes for needlestick <strong>in</strong>juries through a double layer<br />
<strong>of</strong> latex were also determ<strong>in</strong>ed, to assess the protective efficacy<br />
<strong>of</strong> double glov<strong>in</strong>g.<br />
methods<br />
We chose an ex vivo model for conduct<strong>in</strong>g the tests. Circular<br />
samples <strong>of</strong> fresh pork sk<strong>in</strong> (thickness, approximately 19 mm)<br />
were made with use <strong>of</strong> a stamp<strong>in</strong>g tube. Then, 2-mL samples<br />
<strong>of</strong> fresh, human whole blood were obta<strong>in</strong>ed by us<strong>in</strong>g the<br />
Sarstedt Monovette system, and sodium citrate was added to<br />
the samples to prevent coagulation dur<strong>in</strong>g the subsequent<br />
tests. The blood sample for each test was obta<strong>in</strong>ed from the<br />
same person perform<strong>in</strong>g the test to rule out any risk <strong>of</strong><br />
<strong>in</strong>fection.<br />
First, 1.5 mL <strong>of</strong> blood was pipetted from the available<br />
sample and was mixed with approximately 1 mL <strong>of</strong> highly<br />
radioactive (approximately 15 MBq/mL) Technetium solution<br />
( 99 Tc). The activity <strong>in</strong> the 1.5-mL radioactive blood sample<br />
was gauged by us<strong>in</strong>g an activimeter (Isomed 2000) and was<br />
recorded.<br />
To simulate the percutaneous <strong>in</strong>juries, the samples were<br />
mounted <strong>in</strong> a holder, and a s<strong>in</strong>gle f<strong>in</strong>ger from a medical glove<br />
(Biogel; Mölnlycke) was stretched over the sample. The patented<br />
double-glov<strong>in</strong>g technique with <strong>in</strong>dicator (BiogelEclipse<br />
Indicator; Mölnlycke) was used to test blood contact with<br />
From the Department <strong>of</strong> Safety Eng<strong>in</strong>eer<strong>in</strong>g, University <strong>of</strong> Wuppertal (A.W., N.K., J.K., F.H.), and the Helios Kl<strong>in</strong>ikum Wuppertal, Kl<strong>in</strong>ik für Nuklearmediz<strong>in</strong><br />
(K.G.), Wuppertal, Germany.<br />
Received July 3, 2008; accepted August 3, 2008; electronically published December 2, 2008.<br />
� 2008 by The Society for Healthcare Epidemiology <strong>of</strong> America. All rights reserved. 0899-823X/2009/3001-0010$15.00. DOI: 10.1086/593124
54 <strong>in</strong>fection control and hospital epidemiology january 2009, vol. 30, no. 1<br />
double-gloved hands. This double-glov<strong>in</strong>g technique <strong>in</strong>volves<br />
use <strong>of</strong> a green <strong>in</strong>ner glove that is an approximately half-size<br />
larger than necessary and that is worn with a straw-colored<br />
outer glove.<br />
We only conducted tests with at least 1 layer <strong>of</strong> latex, because<br />
it is no longer common to perform operations without<br />
sterile gloves. Each test configuration was repeated 40 times<br />
under identical conditions.<br />
To simulate punctures with surgical sutur<strong>in</strong>g needles, we<br />
first applied 3 mL <strong>of</strong> blood with a dos<strong>in</strong>g pipette (Brand<br />
Transferpette 20 mL; accuracy, 0.02%) to the outside <strong>of</strong> each<br />
test glove. Then, preloaded safety lancets (Owen Mumford<br />
Unistik3 Normal, 21G; depth <strong>of</strong> puncture, 2.4 mm ) were<br />
used to pierce the glove through the applied blood. By us<strong>in</strong>g<br />
preloaded safety lancets, we were able to ensure that each<br />
puncture took place under identical conditions (ie, the same<br />
duration and depth <strong>of</strong> puncture). Injuries caused by sharp<br />
objects such as bone fragments and scissor tips were also<br />
simulated with an automatic lancet (Owen Mumford Unistik2<br />
Neonatal, 18G; depth <strong>of</strong> puncture, 1.8 mm) equipped with<br />
a blade-shaped needle (Figure 1). These tests were also conducted<br />
by punctur<strong>in</strong>g a glove with 3 mL <strong>of</strong> preapplied blood.<br />
Punctures with scalpel blades (Otto Rüttgers KG M<strong>in</strong>i<br />
Blades [used for microsurgery]; material thickness, 0.6 mm)<br />
were made by us<strong>in</strong>g a specially constructed automated punctur<strong>in</strong>g<br />
device (Figure 2). The scalpel blades were immersed<br />
<strong>in</strong> blood at a depth <strong>of</strong> 10 mm for 30 seconds; then, the<br />
punctur<strong>in</strong>g device performed identical punctures (depth, 3<br />
mm). We orig<strong>in</strong>ally developed the punctur<strong>in</strong>g device for measur<strong>in</strong>g<br />
blood volume transfers with cannule punctures. The<br />
device reproducibly and constantly ma<strong>in</strong>ta<strong>in</strong>s the test<strong>in</strong>g parameters,<br />
such as puncture depth, duration, and speed.<br />
Each sample was then gauged by us<strong>in</strong>g a g well-counter<br />
connected to a computer (Maestro MCB 129). The transferred<br />
blood volume was calculated accord<strong>in</strong>g to the radioactive<br />
decay determ<strong>in</strong>ed 1 m<strong>in</strong>ute after blood contam<strong>in</strong>ation.<br />
figure 1. The 2 automated lancets used <strong>in</strong> the study: Unistik<br />
Normal (left) and Unistik Neonatal (right).<br />
figure 2. Automated punctur<strong>in</strong>g device with which scalpel<br />
blade <strong>in</strong>juries were simulated.<br />
Before tak<strong>in</strong>g measurements, the gauge was calibrated daily<br />
to the energy region <strong>of</strong> the Technetium activity with use <strong>of</strong><br />
2 different emitters ( 131 I and 99 Tc). The region <strong>of</strong> <strong>in</strong>terest was<br />
calibrated to 10 MeV greater than and 10 MeV less than the<br />
mean b-decay energy (141 MeV) <strong>of</strong> the 99 Tc isotope. The data<br />
were analyzed us<strong>in</strong>g SPSS, version 14 (SPSS).<br />
results<br />
A mean volume <strong>of</strong> 0.064 mL <strong>of</strong> blood (median, 0.037 mL;<br />
standard error <strong>of</strong> the mean [SEM], 0.012 mL) was transferred<br />
<strong>in</strong> punctures with the Unistik3 Normal automatic lancet at<br />
a depth <strong>of</strong> 2.4 mm through 1 layer <strong>of</strong> latex. With the doubleglov<strong>in</strong>g<br />
<strong>in</strong>dicator technique, a mean volume <strong>of</strong> only 0.011<br />
mL <strong>of</strong> blood (median, 0.007 mL; SEM, 0.003 mL; P ! .05)<br />
was<br />
transferred; thus, use <strong>of</strong> 2 pairs <strong>of</strong> gloves, the transferred<br />
volume <strong>of</strong> blood was reduced by a factor <strong>of</strong> 5.8.<br />
Punctures with the blade-shaped Unistik2 Neonatal lancet<br />
through a s<strong>in</strong>gle layer <strong>of</strong> latex transferred a mean volume<br />
(�SD) <strong>of</strong> 0.133 � 0.069 mL <strong>of</strong> blood (median, 0.113 mL;<br />
SEM, 0.011 mL), which was considerably more than the<br />
amount transferred when punctures were made with the needle-shaped<br />
Unistik3 Normal lancet, even though the puncture<br />
depth <strong>of</strong> the Unistik2 Neonatal lancet was only 1.8 mm. When<br />
punctures were made through a double layer <strong>of</strong> latex, the<br />
transferred mean volume (�SD) decreased to 0.035 �<br />
0.033 mL (median, 0.027 mL; SEM, 0.005 mL; P ! .05),<br />
which<br />
resulted <strong>in</strong> a factor <strong>of</strong> protection <strong>of</strong> 3.8.<br />
<strong>Needlestick</strong> <strong>in</strong>juries through a s<strong>in</strong>gle layer <strong>of</strong> latex simulated<br />
with blood-contam<strong>in</strong>ated m<strong>in</strong>i-blades resulted <strong>in</strong> a<br />
mean transferred volume <strong>of</strong> blood (�SD) <strong>of</strong> 0.168 � 0.102<br />
mL (median, 0.141 mL; SEM, 0.016 mL); through a double<br />
layer <strong>of</strong> latex, the mean transferred volume <strong>of</strong> blood (�SD)<br />
was 0.036 � 0.031 mL (median, 0.028 mL; SEM, 0.005 mL;<br />
P ! .05).<br />
Double glov<strong>in</strong>g resulted <strong>in</strong> a factor <strong>of</strong> protection <strong>of</strong><br />
4.6 (Figure 3).<br />
All punctures <strong>of</strong> the double layer <strong>of</strong> latex were clearly identifiable<br />
by the green color<strong>in</strong>g <strong>of</strong> the puncture site. This col-
figure 3. Box plot show<strong>in</strong>g the transferred blood volume <strong>in</strong> ex<br />
vivo tests with 3 different automated puncture devices and with<br />
s<strong>in</strong>gle and double glov<strong>in</strong>g. Grey boxes, <strong>in</strong>terquartile range (IQR);<br />
black l<strong>in</strong>es with<strong>in</strong> the boxes, median values; horizontal l<strong>in</strong>es outside<br />
boxes, range exclud<strong>in</strong>g outliers and extreme values; black circles, outliers<br />
(values 11.5 and !3 times the IQR from the 75th percentile);<br />
stars, extreme values (values 13 times the IQR from either the 25th<br />
or the 75th percentiles).<br />
or<strong>in</strong>g is the result <strong>of</strong> fluids enter<strong>in</strong>g the space between the<br />
gloves through the puncture site, which causes the green <strong>in</strong>ner<br />
glove to show through the straw-colored outer glove.<br />
discussion<br />
A series <strong>of</strong> studies has been conducted worldwide on the risk<br />
<strong>of</strong> surgical personnel be<strong>in</strong>g exposed to blood-borne pathogens.<br />
3 In those studies, blood contact and/or <strong>in</strong>jury was usually<br />
detected by <strong>in</strong>spect<strong>in</strong>g the latex gloves worn dur<strong>in</strong>g surgical<br />
procedures. The glove puncture rate was most frequently<br />
determ<strong>in</strong>ed by fill<strong>in</strong>g the gloves with water or by us<strong>in</strong>g electrical<br />
measur<strong>in</strong>g methods similar to those used for condom<br />
test<strong>in</strong>g. 4 In every study, the glove puncture rate depended on<br />
the type <strong>of</strong> surgical procedure (ie, there is an <strong>in</strong>creased the<br />
risk <strong>of</strong> blood contact dur<strong>in</strong>g longer procedures 5 ); operations<br />
that required great effort and <strong>in</strong>volved bones6,7or deep locations<br />
8 resulted <strong>in</strong> glove puncture rates <strong>of</strong> up to 70%. The<br />
risk <strong>of</strong> blood contact dur<strong>in</strong>g endoscopic procedures was significantly<br />
lower, with a puncture rate <strong>of</strong> approximately 9%. 9–<br />
11<br />
The lead surgeon and the assist<strong>in</strong>g personnel have the highest<br />
risk <strong>of</strong> <strong>in</strong>jury. 12,13<br />
Improved protection aga<strong>in</strong>st <strong>in</strong>fection can be achieved by<br />
wear<strong>in</strong>g 2 pairs <strong>of</strong> gloves. Many studies have proven the ben-<br />
surgical needlestick <strong>in</strong>juries 55<br />
efits <strong>of</strong> double glov<strong>in</strong>g <strong>in</strong> prevent<strong>in</strong>g blood contact. Studies<br />
from the United States 14,15 determ<strong>in</strong>ed that double glov<strong>in</strong>g<br />
can reduce the risk <strong>of</strong> blood contact by a factor <strong>of</strong> 10. Two<br />
other studies found that use <strong>of</strong> doubled surgical gloves reduced<br />
the rate <strong>of</strong> blood contam<strong>in</strong>ation among surgeons from<br />
70% (<strong>in</strong> both studies) to 13% (<strong>in</strong> one study) and 2% (<strong>in</strong> the<br />
other study). 16,17 The rate <strong>of</strong> blood contam<strong>in</strong>ation was m<strong>in</strong>imized<br />
despite a puncture <strong>in</strong> the outer glove, because the<br />
<strong>in</strong>ner glove rema<strong>in</strong>ed <strong>in</strong>tact <strong>in</strong> up to 82% <strong>of</strong> cases. 18–20<br />
Protection aga<strong>in</strong>st <strong>in</strong>fection can be <strong>in</strong>creased even more<br />
by double glov<strong>in</strong>g with an <strong>in</strong>dicator glove. This glov<strong>in</strong>g technique<br />
<strong>in</strong>cludes a colored <strong>in</strong>ner glove and an outer glove that<br />
is neutral <strong>in</strong> color. If the outer glove is punctured dur<strong>in</strong>g the<br />
operation, the fluids present <strong>in</strong> all procedures will appear as<br />
a clearly visible spot at the site <strong>of</strong> the puncture. Once such<br />
a spot is noticed by any member <strong>of</strong> the surgical team, the<br />
glove can be replaced, thus m<strong>in</strong>imiz<strong>in</strong>g the risk <strong>of</strong> an <strong>in</strong>fection<br />
that results from cont<strong>in</strong>u<strong>in</strong>g with the operation.<br />
To date, the studies conducted on early detection <strong>of</strong> glove<br />
punctures dur<strong>in</strong>g surgical procedures have revealed that <strong>in</strong>dicator<br />
gloves are very effective. Compared with complicated<br />
electronic <strong>in</strong>dicator systems that <strong>of</strong>ten tend to sound the<br />
alarm because <strong>of</strong> changes <strong>in</strong> the conductivity <strong>of</strong> the latex<br />
gloves, 21,22 <strong>in</strong>dicator gloves enable the detection <strong>of</strong> up to 100%<br />
<strong>of</strong> punctures immediately after they occur. 23,24<br />
A meta-analysis <strong>of</strong> the 18 studies conducted on glove safety<br />
worldwide found that double glov<strong>in</strong>g led to 3 times fewer<br />
contacts with blood, compared with us<strong>in</strong>g a s<strong>in</strong>gle pair <strong>of</strong><br />
gloves. No concentrations <strong>of</strong> punctures on the outer glove<br />
were found that could <strong>in</strong>dicate a reduction <strong>in</strong> hand sensitivity<br />
or dexterity. 3<br />
Although the protective effect <strong>of</strong> double glov<strong>in</strong>g is very<br />
evident, it is not yet rout<strong>in</strong>e practice. This is ma<strong>in</strong>ly attributable<br />
to the alleged reduction <strong>in</strong> dexterity and sense <strong>of</strong> touch<br />
through the double layer <strong>of</strong> latex. A study conducted at the<br />
University <strong>of</strong> Wuppertal (Wuppertal, Germany), <strong>in</strong> which<br />
participants underwent a standard neurological 2-po<strong>in</strong>t discrim<strong>in</strong>ation<br />
test and a “dice test” (<strong>in</strong> which the bl<strong>in</strong>dfolded<br />
participant had to determ<strong>in</strong>e the number <strong>of</strong> pips on dice <strong>of</strong><br />
various sizes), found no significant reductions <strong>in</strong> the sense<br />
<strong>of</strong> touch <strong>in</strong> those wear<strong>in</strong>g 2 pairs <strong>of</strong> gloves. 25 A US study that<br />
tested both sense <strong>of</strong> touch and dexterity found that 2 pairs<br />
<strong>of</strong> gloves had an adverse effect only on the surgeons who<br />
normally operated with a s<strong>in</strong>gle pair <strong>of</strong> gloves; with<strong>in</strong> a short<br />
period, however, even these surgeons became accustomed to<br />
us<strong>in</strong>g 2 pairs <strong>of</strong> gloves. 26<br />
Our tests prove that double glov<strong>in</strong>g also has a positive effect<br />
on the blood volumes transferred by surgical needlestick <strong>in</strong>juries.<br />
Use <strong>of</strong> 2 pairs <strong>of</strong> gloves led to a significant reduction<br />
<strong>in</strong> transferred blood volume <strong>in</strong> all <strong>of</strong> the tests.<br />
Therefore, it has been established that double glov<strong>in</strong>g provides<br />
a significant reduction <strong>in</strong> the risk <strong>of</strong> blood exposure to<br />
surgical personnel. Indicator systems have the added advantage<br />
<strong>of</strong> prevent<strong>in</strong>g the <strong>in</strong>fection <strong>of</strong> unnoticed <strong>in</strong>juries, which
56 <strong>in</strong>fection control and hospital epidemiology january 2009, vol. 30, no. 1<br />
can occur with glove punctures that are difficult to detect.<br />
The aforementioned double-glov<strong>in</strong>g techniques already exist,<br />
and their benefits, compared with s<strong>in</strong>gle glov<strong>in</strong>g, are known<br />
<strong>in</strong> the field <strong>of</strong> surgery. In conclusion, double glov<strong>in</strong>g should<br />
be recommended for all surgical procedures and should be<br />
required for procedures for patients with known <strong>in</strong>fections<br />
or for patients who have not yet been tested for <strong>in</strong>fections.<br />
acknowledgments<br />
F<strong>in</strong>ancial support. Regent Medical Overseas, Mölnlycke Healthcare.<br />
Potential conflicts <strong>of</strong> <strong>in</strong>terest. All authors report no conflicts <strong>of</strong> <strong>in</strong>terest<br />
relevant to this article.<br />
Address repr<strong>in</strong>t requests to Andreas Wittmann, PhD, University <strong>of</strong> Wuppertal,<br />
Dept. <strong>of</strong> Safety Eng<strong>in</strong>eer<strong>in</strong>g, Gauss Str. 20, D-42097 Wuppertal, Germany<br />
(andwitt@uni-wuppertal.de).<br />
references<br />
1. Makary MA, Al-Attar A, Holzmueller ChG, et al. <strong>Needlestick</strong> <strong>in</strong>juries<br />
among surgeons <strong>in</strong> tra<strong>in</strong><strong>in</strong>g. NEnglJMed2007; 356:2693-2699.<br />
2. Kralj N, Beie M, H<strong>of</strong>mann F. <strong>Surgical</strong> gloves–how well do the protect<br />
aga<strong>in</strong>st <strong>in</strong>fections? [<strong>in</strong> German]. Gesundheitswesen 1999; 61:398-403.<br />
3. Tanner J, Park<strong>in</strong>son H. Double glov<strong>in</strong>g to reduce surgical cross-<strong>in</strong>fection.<br />
Cochrane Database Syst Rev 2006;(3):CD003087.<br />
4. Kralj N. Handschuhe—<strong>in</strong>fektionsschutz für beschäftigte und patienten.<br />
In: H<strong>of</strong>mann F, Reschauer G, Stößel U. Arbeitsmediz<strong>in</strong> im Gesundheitsdienst<br />
XIV. Freiburg: FFAS; 2001:100-105.<br />
5. Zimmermann CH, Junghanns K. Die verwendung e<strong>in</strong>es neuen perforations<strong>in</strong>dikatorsystems<br />
<strong>in</strong> der chirurgischen rout<strong>in</strong>e. Hyg Med 1996; 21:<br />
486-492.<br />
6. Eckersley JR, Williamson DM. Glove punctures <strong>in</strong> an orthopaedic trauma<br />
unit. Injury 1990; 21:177-178.<br />
7. Wright KU, Moran CG, Briggs PJ. Glove perforation dur<strong>in</strong>g hip arthroplasty:<br />
a randomised prospective study <strong>of</strong> a new taperpo<strong>in</strong>t needle. J<br />
Bone Jo<strong>in</strong>t Surg 1993;75:918-920.<br />
8. Hollaus PH, Lax F, Janakiev D, Wurnig PN, Pridu NS. Glove perforation<br />
rate <strong>in</strong> open lung surgery. Eur J Cardiothorac Surg 1999; 15:461-464.<br />
9. Eklund AM, Ojajärvi J, Lait<strong>in</strong>en K, Valtonen M, Werkkala KA. Glove<br />
punctures and postoperative sk<strong>in</strong> flora <strong>of</strong> hands <strong>in</strong> cardiac surgery. Ann<br />
Thorac Surg 2002; 74:149-153.<br />
10. Beie M, Kralj N, H<strong>of</strong>mann F. Gefährdungsanalysen <strong>in</strong> krankenhäusern.<br />
In: H<strong>of</strong>mann F, Reschauer G, Stößel U. Arbeitsmediz<strong>in</strong> im Gesundheitsdienst<br />
XII. Freiburg: FFAS; 1999:347-364.<br />
11. Popejoy SL, Fry DE. <strong>Blood</strong> contact and exposure <strong>in</strong> the operat<strong>in</strong>g room.<br />
Surg Gynec Obstet 1991; 172:480-483.<br />
12. Rieger MA, Hasselhorn HM, Beie M, Kralj N, Vetter HD, H<strong>of</strong>mann F.<br />
Personnel-to-patient transmission <strong>of</strong> hepatitis C virus: underestimation<br />
<strong>of</strong> exposure. Arch Int Med 2000; 161:2313-2316.<br />
13. Heeg P. Sicherheitsaspekte bei operationshandschuhen. Operat Orthop<br />
Traumatol 1993; 5:291-293.<br />
14. Bennett B, Duff P. The effect <strong>of</strong> double glov<strong>in</strong>g on frequency <strong>of</strong> glove<br />
perforations. Obstet Gynecol 1991; 78:1019-1022.<br />
15. Bebb<strong>in</strong>gton MW, Treissman MJ. The use <strong>of</strong> a surgical assist device to<br />
reduce glove perforation <strong>in</strong> post vag<strong>in</strong>al repair: a randomised control<br />
trial. Am J Obst Gynecol 1996; 175:862-866.<br />
16. Greco RJ, Garza JR. Use <strong>of</strong> double gloves to protect the surgeon from<br />
blood contact dur<strong>in</strong>g aesthetic procedures. Aesthetic Plast Surg 1995; 19:<br />
265-267.<br />
17. Naver LPS, Gottrup F. Incidence <strong>of</strong> glove perforations <strong>in</strong> gastro<strong>in</strong>test<strong>in</strong>al<br />
surgery and the protective effect <strong>of</strong> double gloves: a prospective, randomised<br />
controlled study. Europ J Surg 2003; 166:293-295.<br />
18. Cole RP, Gault CT. Glove perforation dur<strong>in</strong>g plastic surgery. Br J Plast<br />
Surg 1989; 42:481-483.<br />
19. Thomas S, Agarwal M, Mehta G. Intraoperative glove perforation—s<strong>in</strong>gle<br />
versus double glov<strong>in</strong>g <strong>in</strong> protection aga<strong>in</strong>st sk<strong>in</strong> contam<strong>in</strong>ation. Postgrad<br />
Med J 2001; 77:458-60.<br />
20. König M, Bruha M, Hirsch HA. Perforation <strong>of</strong> surgical gloves <strong>in</strong> gynecologic<br />
operations and abdom<strong>in</strong>al Cesarean section [In German]. Geburtsh<br />
Frauenheilk 1992; 52:109-112.<br />
21. Caillot JL, Cote C, Abidi H, Fabry J. Electronic evaluation <strong>of</strong> the value<br />
<strong>of</strong> double glov<strong>in</strong>g. Br J Surg 1999; 86:1387-1390.<br />
22. Fisher MD, Reddy VR, Williams VM, L<strong>in</strong> KY, Thacker JG, Redlich RF.<br />
Biomechanical performance <strong>of</strong> latex and non-latex double-glove systems.<br />
J Biomed Mater Res 1999; 48:797-806.<br />
23. Manson TT, Bromberg WG, Thacker JG, McGregor W, Morgan RF,<br />
Redlich RF. A new glove puncture detection system. J Emerg Med<br />
1995; 13:357-364.<br />
24. Duron JJ, Keilani K, Elian NG. Efficacy <strong>of</strong> double glov<strong>in</strong>g with coloured<br />
<strong>in</strong>ner pair for immediate detection <strong>of</strong> operative glove perforations. Eur<br />
J Surg 1996; 162:941-944.<br />
25. Beie M, Kralj N, Sieker S, H<strong>of</strong>mann F. Infektionsschutz im arbeitslebenstudien<br />
zum tasts<strong>in</strong>n bei e<strong>in</strong>facher bzw. doppelter behandschuhung. In<br />
Schäcke G, Lüth P. Dokumentationsband über 40. Jahrestagung der<br />
DGAUM. R<strong>in</strong>dt Druck: Fulda; 2000:310-312.<br />
26. Novak CB, Patterson MM, Mack<strong>in</strong>non SE. Evaluation <strong>of</strong> hand sensibility<br />
with s<strong>in</strong>gle and double latex gloves. Plast Reconstr Surg 1999; 1:128-131.