the egyptian society of cardiology board of ... - Cardioegypt.com
the egyptian society of cardiology board of ... - Cardioegypt.com
the egyptian society of cardiology board of ... - Cardioegypt.com
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
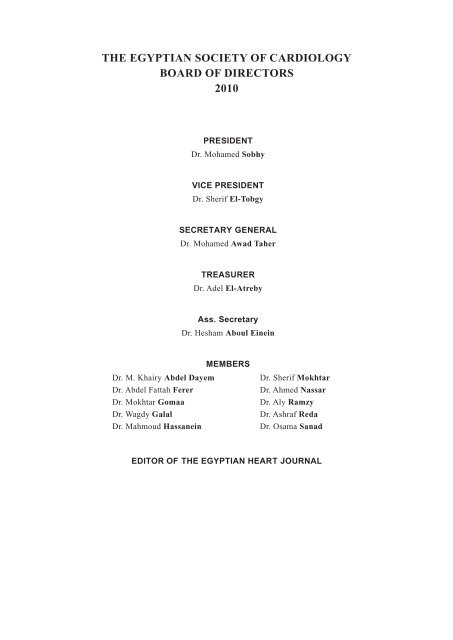
THE EGYPTIAN SOCIETY OF CARDIOLOGY<br />
BOARD OF DIRECTORS<br />
2010<br />
Dr. M. Khairy Abdel Dayem<br />
Dr. Abdel Fattah Ferer<br />
Dr. Mokhtar Gomaa<br />
Dr. Wagdy Galal<br />
Dr. Mahmoud Hassanein<br />
PRESIDENT<br />
Dr. Mohamed Sobhy<br />
VICE PRESIDENT<br />
Dr. Sherif El-Tobgy<br />
SECRETARY GENERAL<br />
Dr. Mohamed Awad Taher<br />
TREASURER<br />
Dr. Adel El-Atreby<br />
Ass. Secretary<br />
Dr. Hesham Aboul Einein<br />
MEMBERS<br />
Dr. Sherif Mokhtar<br />
Dr. Ahmed Nassar<br />
Dr. Aly Ramzy<br />
Dr. Ashraf Reda<br />
Dr. Osama Sanad<br />
EDITOR OF THE EGYPTIAN HEART JOURNAL
Osama Abd El-Aziz<br />
Khairy Abd El-Dayem<br />
Alia Abd El-Fattah<br />
Samir Abd El-Kader<br />
Wafaei Abou El-Einein<br />
Gamal Abou El-Nasr<br />
Sayed Akl<br />
Omar Awad<br />
Mohamed Taher Awad<br />
Wagdy Ayad<br />
Amal Ayoub<br />
Helmy Bakr<br />
Tarek El-Badawy<br />
Reda El-Eisawy<br />
Mohamed El-Gawady<br />
EGYPTIAN ADVISORY BOARD<br />
Ayman Abou El-Magd<br />
Ramzy Hamed El-Mawardy<br />
Galal El-Said<br />
Ezz El-Deen El-Sawy<br />
Hamdy El-Sayed<br />
Sherif El-Tobgy<br />
Hussien Gafaar<br />
Wagdy Galal<br />
Ramez Gendy<br />
Mokhtar Gomaa<br />
Magdy Gomaa<br />
Ebtihag Hamdy<br />
Mahmoud Hasanien<br />
Mesbah Taha Hassanien<br />
Mohamed Mohsen Ibrahim<br />
II<br />
Ayman Kaddah<br />
Hossam Kandil<br />
Fathy Maklady<br />
Moustafa Nawar<br />
Samier Rafla<br />
Hany Ragy<br />
Aly Ramzy<br />
Ashraf Reda<br />
Hussien Rizk<br />
Salwa Roshdy<br />
Ikram Sadek<br />
Mohamed Sobhy<br />
Khaled Sorour<br />
Nasser Taha<br />
Adel Zaki
Salah Abdel-Aleem<br />
Samir Alam<br />
Abel-Hahi AI-Awadi<br />
Zohair Al-Halees<br />
Saad AI-Kasab<br />
Fadel Al-Fadley<br />
Mohamed R. Al-Fagih<br />
Mansour Al-Nozha<br />
Gerd Assmann<br />
Salim Aziz<br />
A Bahnini<br />
L<strong>of</strong>ty Basta<br />
Eugene Braunwald<br />
Albert V.G. Bruschke<br />
Pat Commerford<br />
C. Richard Conti<br />
Alain Cripier<br />
Prakash C. Deedwania<br />
Naranjan S. Dhalla<br />
Nabil El-Sherif<br />
Mamdouh El-Gamal<br />
Ghanem Elias<br />
Mahfouz EI-Shahawy<br />
Fawzy G. Estafanous<br />
Hany Eteiba<br />
Jean Fajadet<br />
Harvey Feigenbaum<br />
Sayed Fighali<br />
Omar Galal<br />
Adolph M. Hutter<br />
INTERNATIONAL ADVISORY BOARD<br />
South Carolina, USA<br />
Beirut, Lebanon<br />
Manama, Bahrain<br />
Riyadh, Saudi Arabia<br />
Riyadh, Saudi Arabia<br />
Riyadh, Saudi Arabia<br />
Riyadh, Saudi Arabia<br />
Riyadh, Saudi Arabia<br />
Munster, Germany<br />
Colorado, USA<br />
Massy, France<br />
Florida, USA<br />
Boston, USA<br />
Rotterdam, Ne<strong>the</strong>rlands<br />
Cape Town, South Africa<br />
Florida, USA<br />
Paris, France<br />
San Francisco, USA<br />
Winnipeg, Canada<br />
New York, USA<br />
Eindhoven, Holand<br />
Beirut, Lebanon<br />
Florida, USA<br />
Cleveland, OH, USA<br />
Glagsgow, UK<br />
France, Paris<br />
Indianapolis, USA<br />
Houston, Txs, USA<br />
Riyadh, Saudi Arabia<br />
Massachusettes, USA<br />
III<br />
Ami E. Iskandrian<br />
Charles Jazra<br />
J. Ward. Kennedy<br />
Keneth Kent<br />
E.-Kieffer<br />
Petri Kovanen<br />
Zvonimir Krajcer<br />
Jules YT. Lam<br />
Joseph F. Malouf<br />
Antonis S. Manolis<br />
Athanasios Manolis<br />
Hamdy Masoud<br />
Navin C. Nanda<br />
Altan Onat<br />
Vasilios Papademeriou<br />
Wolf Rafflenbeul<br />
Shahbudin H. Rahimtoola<br />
Mehdi Razavi<br />
J.R.T.C. Roelandt<br />
Wilhelm Rutishauser<br />
David J. Sahn<br />
Ulrich Sigwart<br />
Jamil Tajik<br />
Eric Topol<br />
Christopher J. White<br />
James T. Willerson<br />
Bryn T. Will<br />
Magdi Yacoub<br />
James Young<br />
Philadiphia, USA<br />
Beirut, Lebanon<br />
Washington, USA<br />
Washington, USA<br />
Massy, France<br />
Helsinki, Finlanda<br />
Houston Txs, USA<br />
Montreal, Canada<br />
Florida, USA<br />
A<strong>the</strong>ns, Greece<br />
Patras, Greece<br />
Massy, France<br />
Alabama, USA<br />
Istambul, Turkev<br />
New York, USA<br />
Hannover; Gerrnariv<br />
Calitornia, USA<br />
Cleveland OH, USA<br />
Rotterdam, Hollarul<br />
Geneva, Swit: erland<br />
Portland, USA<br />
London, UK<br />
Minnesota, USA<br />
Cleveland OH, USA<br />
New Orleans, USA<br />
Houston. Txs. USA<br />
London, UK<br />
London, UK<br />
Cleveland OH, USA
NOTICE TO CONTRIBUTORS<br />
The Egyptian Heart Journal will be pleased to consider for publication articles by members <strong>of</strong> <strong>the</strong><br />
Egyptian Society <strong>of</strong> Cardiology, as well as non-members whose articles have a cardiological bearing.<br />
Articles submitted for publication will be published under <strong>the</strong> following subheadings: Editorials,<br />
Original Articles, Case reports, Letters to <strong>the</strong> Editor, Book Reviews and Editorial <strong>com</strong>ments.<br />
The Editor accepts no responsibility for <strong>the</strong> views and statements <strong>of</strong> authors as published in <strong>the</strong>ir<br />
original <strong>com</strong>munications. However articles are accepted on <strong>the</strong> understanding that <strong>the</strong>y-are subject to<br />
Editorial revision.<br />
All articles and manuscripts should be addressed to <strong>the</strong> Editor-in-chief, Egyptian Heart Journal, Pr<strong>of</strong>.<br />
Dr. Sherif Mokhtar, Egyptian Heart House, 9 El-Saraya Street, Dokki 12311, Giza, Egypt. Tel.: 202-<br />
33381308/9 Fax: 202-33381309.<br />
Original Articles:<br />
Articles are accepted for publication upon <strong>the</strong> understanding that <strong>the</strong>y are contributed solely to <strong>the</strong><br />
Egyptian Heart Journal and are not under consideration for publication elsewhere. In addition articles<br />
which have been published in <strong>the</strong> Journal be<strong>com</strong>e <strong>the</strong> property <strong>of</strong> <strong>the</strong> Journal and permission to republish<br />
<strong>the</strong>m must be obtained beforehand from <strong>the</strong> Editor.<br />
Manuscript preparation:<br />
Manuscripts should be submitted with a covering letter stating that 1) <strong>the</strong> paper is not under consideration<br />
elsewhere. 2) none <strong>of</strong> <strong>the</strong> paper's contents have been previously published and 3) all authors have read<br />
and approved <strong>the</strong> manuscript. The corresponding author (name, address, telephone, fax) should be<br />
specified in <strong>the</strong> covering letter. All editorial <strong>com</strong>munication will be sent to this author. Please include a<br />
<strong>com</strong>puter disk with word file (IBM <strong>com</strong>patible).<br />
Length <strong>of</strong> Article:<br />
Because <strong>of</strong> printed page limitations, <strong>the</strong> Editors prefer that <strong>the</strong> article should not exceed 5000 words<br />
including references and legends. Illustrations and tables should be limited to those necessary to highlight<br />
key data.<br />
Plan <strong>of</strong> Article Outlay:<br />
Articles sent for publication must be typewritten or word-processed on one side <strong>of</strong> <strong>the</strong> paper only<br />
with double spacing, on A4 white paper with 3-cm margin on all sides (8 cm at bottom <strong>of</strong> title page).<br />
Please use a standard laser printer 12 Font if possible. An original and 2 copies for <strong>the</strong> written manuscript,<br />
as well as figures, diagrams, tables and photographs will be required. Where half-tone reproduction <strong>of</strong><br />
radiographs is required, authors should satisfy <strong>the</strong>mselves that <strong>the</strong> appearances which <strong>the</strong>y desire to<br />
demonstrate are shown clearly on <strong>the</strong> prints.<br />
All articles must have within <strong>the</strong>m <strong>the</strong> following subheadings written in capital: Introduction, Materials<br />
(or Patients) and Methods, Results, Discussion, References. The manuscript should be arranged as follows:<br />
Title page, Abstract, Key words (3-6), Introduction, Materials and Methods, Results, Discussion,<br />
Acknowledgments, References, Tables, Figures and Figure legends.<br />
Title Page:<br />
The title <strong>of</strong> <strong>the</strong> article should be as concise as possible with no abbreviations and should be in capital<br />
letters. This should be followed by <strong>the</strong> surname <strong>of</strong> authors preceded by <strong>the</strong>ir full first name and middle<br />
initials and if possible followed by standard abbreviations <strong>of</strong> <strong>the</strong>ir degrees. At <strong>the</strong> footnote <strong>of</strong> <strong>the</strong> first<br />
page <strong>the</strong> department(s) or center(s) where <strong>the</strong> work was performed as well <strong>the</strong> name and address <strong>of</strong> <strong>the</strong><br />
corresponding author should be written. Under <strong>the</strong> heading "Address for correspondence", give <strong>the</strong> full<br />
name and <strong>com</strong>plete postal address <strong>of</strong> <strong>the</strong> author to whom <strong>com</strong>munications, printers pro<strong>of</strong>s or reprint<br />
requests should be sent. Also provide telephone and fax numbers and E-mail address, if possible.<br />
IV
Abstract:<br />
Articles should be preceded by an Abstract which should include problem statement, argument,<br />
findings as well conclusion. The Abstract must be not more than 250 words and should be more<br />
<strong>com</strong>prehensive than a summary which will not be required. If abbreviations are use <strong>the</strong>y should be<br />
preceded by <strong>the</strong> full word(s) when mentioned for <strong>the</strong> first time, this should be between brackets. e.g.<br />
Aortic Stenosis (AS).<br />
Key Words (3-6) at <strong>the</strong> end <strong>of</strong> <strong>the</strong> abstract are needed.<br />
References: (Important notice)<br />
Adequate references should be made to previous work on <strong>the</strong> subject <strong>of</strong> <strong>the</strong> paper. The references<br />
should he typed on separate pages from <strong>the</strong> text. Identify references in <strong>the</strong> text by Arabic numerals in<br />
paren<strong>the</strong>ses on <strong>the</strong> line. References must be numbered consecutively in <strong>the</strong> order in which <strong>the</strong>y are<br />
mentioned in <strong>the</strong> text.<br />
The reference itself should give <strong>the</strong> authors name, followed by his initials. In case <strong>of</strong> 2 or 3 au<strong>the</strong>rs<br />
<strong>the</strong>ir names should be written followed by <strong>the</strong>ir initials, with <strong>the</strong> "and" between <strong>the</strong> last author and <strong>the</strong><br />
one preceding. Where an article has more than 3 authors, <strong>the</strong> word "et al" should follow <strong>the</strong> third author's<br />
initials with no "and" preceding his name.<br />
Example:<br />
l- Paker M., Gheorghiade M., Young J.13, et al.: Withdrawal <strong>of</strong> digoxin from patients with chronic<br />
heart failure treaty with angiotensin-converting enzyme inhibitors. N Eng. J. Med., 1993, 329:1.<br />
The name <strong>of</strong> <strong>the</strong> authors are <strong>the</strong>n followed by <strong>the</strong> title <strong>of</strong> <strong>the</strong> article, <strong>the</strong>n <strong>the</strong> name <strong>of</strong> <strong>the</strong> Journal<br />
abbreviated' Index Medical style, year <strong>of</strong> publication <strong>the</strong> volume number, followed by <strong>the</strong> number <strong>of</strong> <strong>the</strong><br />
first page only.<br />
Chapter in Book:<br />
Start with author's name(s) followed by chapter title editors' name(s), followed by book title city,<br />
publishers, ai pages numbers.<br />
Example:<br />
Gersh B.J., Braunwald E. and Ru<strong>the</strong>rford J.D.: Chronic coronary artery disease. In: Braunwald E,<br />
(ed.) Heart Disease Philadelphia, W.B. Saunders Company, 1997, pp. 1289.<br />
Book (Personal author or authors):<br />
Example:<br />
Cohn PF. Silent Myocardial Ischemia and Infarction. (3 rd ed.) New York: Marcel Dekker, 1993, 33.<br />
Egyptian Thesis:<br />
Where a <strong>the</strong>sis is referenced, <strong>the</strong> name <strong>of</strong> <strong>the</strong> candidate who made <strong>the</strong> <strong>the</strong>sis followed by his initials,<br />
title <strong>of</strong> t, <strong>the</strong>sis, name <strong>of</strong> University where <strong>the</strong> <strong>the</strong>sis was presented followed by name <strong>of</strong> <strong>the</strong> city and<br />
country, e.g.: Ahdel A; M.K.; Prenatal Factors in <strong>the</strong> Aetiology <strong>of</strong> Congenital Heart Disease. MSc (or<br />
MD) Thesis, Al-Azhar Unviersity, 1986, Cairo, Egypt.<br />
Figure Legends:<br />
Figure legends should be typed on pages separate from <strong>the</strong> text, Figure numbers must correspond<br />
with <strong>the</strong> order in which <strong>the</strong>y are mentioned in <strong>the</strong> text.<br />
Figures:<br />
Photographs and photo-micrographs should be printed on glossy paper and should not be mounted,<br />
and letter when required, should be indicated on tracing paper fixed over <strong>the</strong> print. Drawings, diagrams,<br />
graphs and photographs should be typed and numbered on a separate sheet <strong>of</strong> paper.<br />
V
Submit three sets <strong>of</strong> laser prints or clean photocopies in three separate envelopes. Two sets <strong>of</strong> glossy<br />
prints should be provided for all half-toner color illustration. Figures particularly graphs, should be<br />
designed to take as lit space as possible. Lettering should be <strong>of</strong> sufficient size to be legible after reduction<br />
for publication. The optimal size after reduction is 9 points, <strong>the</strong> maximum width <strong>of</strong> one-column figures<br />
is 8.5cm, <strong>of</strong> two-column figures 17.5cm.<br />
All graphs and line drawings must be pr<strong>of</strong>essionally prepared or done on a <strong>com</strong>puter and reproduced<br />
as hi, quality laser prints.<br />
Tables:<br />
Tables should be typed double spaced on separate sheets, with <strong>the</strong> table number and title centered<br />
above <strong>the</strong> tat and explanatory notes below <strong>the</strong> tables. Abbreviations should be listed in a footnote under<br />
<strong>the</strong> table in alphabetical order.<br />
Reprints:<br />
Fifty reprints <strong>of</strong> articles are provided gratis to <strong>the</strong> authors. Additional reprints can be supplied if<br />
application is made at <strong>the</strong> time <strong>of</strong> printing. Colored photographs could be published at a rate <strong>of</strong> L.E. 100<br />
for each page.<br />
Fees:<br />
A fee <strong>of</strong> LE 300 for members <strong>of</strong> <strong>the</strong> Egyptian Society <strong>of</strong> Cardiology and L.E. 500 for non-members,<br />
against receipt, for consideration <strong>of</strong> articles for publication must ac<strong>com</strong>pany each article before it can<br />
be sent to <strong>the</strong> reference for acceptance.<br />
VI
General Cardiology:<br />
Myocardial Depression in Sepsis Syndrome Prognostic Value <strong>of</strong> Toll-Like Receptor 4<br />
Ahmed Mowafy, Gamal Hamed, Sanaa Abd El Shafee<br />
Cardiac Affection after Subarachnoid Hemorrhage, Correlation with Severity and Etiology<br />
Rania El Hoseiny, Ahmed Battah, Mohamed Ashraf<br />
Endo<strong>the</strong>lial Dysfunction and Insulin Resistance in Normoglycemic Offsprings <strong>of</strong> Patients with<br />
Type 2 Diabetes Mellitus<br />
Eman S Mohammad, Yasser Kamel, Hannan Taha, Essam Saad, Yasser Makram<br />
Comparative Study between Tissue Doppler Imaging and Radionuclide Scintigraphy in<br />
Evaluation <strong>of</strong> Right Ventricular Function in Patients with Chronic Obstructive Pulmonary<br />
Disease<br />
Sherine Elgangihi, Randa Aly, Sally Salah, Amr Elhadidy<br />
Metabolic Syndrome and its Impact on Vascular Damage Extent<br />
Ayman Sadek, Magdy Nouh Ain, Hany Fouad Hanaa, Ramzy Hamed El-Mawardy<br />
Cardiovascular Risk Factors in Patients with End Stage Renal Failure on Regular Hemodialysis<br />
Yaser AA El-Hendy, Mohamed Abdou<br />
Hypertension:<br />
White Coat Hypertension and Target Organ Damage<br />
Hamza Kabil, Metwally El-Emary, Ahmed Abdel-Moneim, Abdel-Rahman Samra<br />
Microalbuminuria and Subclinical Cardiac Structural Changes Relation to Isolated Systolic<br />
Hypertension in Elderly Patients<br />
Hamza Kabil, El-Metwally El-Shahawy, Amr Afifi, Hsassan Galal, Ashraf Talaat<br />
Urinary Albumin Excretion is Associated with Arterial Stiffness in Hypertensive Adults<br />
Mohammed A Abdel Wahab, Mohamed M Saad, Amr S Amin, Khalid A Baraka, Nasser M Taha<br />
Early Vascular Changes Preceding Morphological Cardiac Changes in Hypertensive Patients<br />
Mohammed A Abdel Wahab<br />
Metabolic Syndrome as A Predictor <strong>of</strong> Non Dipping Hypertension<br />
Islam Mohamed Mahdy El-Helaly, Mohamed Ayman Saleh, Ayman Sadek, Ahmed Onsy<br />
Echocardiography:<br />
THE EGYPTIAN HEART JOURNAL<br />
(EHJ)<br />
Volume 62 • Number 1 •<br />
March 2010<br />
TABLE OF CONTENTS<br />
Quantitative Power Doppler Technique <strong>of</strong> Myocardial Contrast Echocardiography: For <strong>the</strong><br />
Detection <strong>of</strong> Segmental Myocardial Perfusion Pr<strong>of</strong>ile<br />
Youssef FM Nosir, Ashraf A Ali, Ali A Abd-Elmagid, Mamdouh Altahan, Mansour Mostafa,<br />
Abdelmaksoud S Ahmed, Ayman Kholief, Hassan Chamsi Pasha, Ezz El-Ssawy<br />
The Carotid-Femoral Arterial Index and <strong>the</strong> Severity <strong>of</strong> Coronary A<strong>the</strong>rosclerosis<br />
Mahmoud Soliman, Hesham Hasan, Tamer Gazy, Walaa Fareed, Ashraf Reda, Said Shalaby<br />
Page<br />
1<br />
7<br />
19<br />
25<br />
39<br />
53<br />
63<br />
69<br />
77<br />
83<br />
89<br />
103<br />
111
Value <strong>of</strong> Contrast Echocardiography for <strong>the</strong> Diagnosis <strong>of</strong> Hepatopulmonary Syndrome in<br />
Patients with Chronic Liver Disease Due to Hepatitis C Virus<br />
Amal S Bakir, Ghada El-Shahed<br />
Cardiac Output Measurement by a New Transesophageal Doppler Probe in Circulatory Shock<br />
Nashwa Abed, Mohamed Afify<br />
Interventional:<br />
Comparison between Double Intravenous Bolus, Intracoronary Bolus, and Conventional<br />
Intravenous Bolus Dose <strong>of</strong> Tir<strong>of</strong>iban in Patients with Acute Anterior Myocardial Infarction<br />
Treated by Primary Coronary Intervention<br />
Ahmed Ibrahim Nassar, Nagwa Nagi El-Mahallawy, Bassem Wadei Habib, Adel Gamal Hassanin,<br />
Iman Esmat, Haytham Galal<br />
Safety and Feasibility <strong>of</strong> Transradial Versus Transfemoral Approach for Diagnostic Coronary<br />
Angiography During Early Phase <strong>of</strong> <strong>the</strong> Learning Curve<br />
Mahmoud M Sabbah, Mohamed A Oraby, Gamela M Nasr, Ahmed A El Hawary<br />
Correlation between Clinical Presentation, ECG and Echocardio-Graphic Findings and Those<br />
<strong>of</strong> Angiography in Patients Undergoing Coronary Angiography<br />
Fathi A Maklady, Hanan M Kamal, Azza Z El-Eraky, Omar M Saleh<br />
Measurement <strong>of</strong> Fractional Flow Reserve (FFR) for Guiding Percutaneous Coronary Intervention<br />
in Clinical Practice<br />
Hussein Shaalan<br />
Coronary Heart Disease:<br />
Angiographic Coronary Artery Disease in Women with Chest Pain and History <strong>of</strong> Anxiety<br />
Disorders<br />
Khaled E Darahim, Mona I Awaad<br />
Depression Post Acute Coronary Syndromes: Incidence and Predictors<br />
Mona I Awaad, Khaled E Darahim<br />
Coronary Ectasia: Risk Markers and Risk Factors<br />
Mahmoud A Soliman, Hosam M El Ezzawy<br />
Valvular Heart Disease:<br />
Usefulness <strong>of</strong> 2-Dimensional Mitral Valve Leaflets Separation Index as a New Technique for<br />
Assessment <strong>of</strong> Mitral Stenosis Severity: Comparison with Planimetry and PHT Methods<br />
Hany Younan<br />
Laboratory:<br />
(B)<br />
Thrombin-Activatable Fibrinolysis Inhibitor Thr325Ile Polymorphism as a Risk Factor <strong>of</strong><br />
Myocardial Infarction in Egyptians<br />
Hanan M Kamal, Amal S Ahmed, Manal S Fawzy, Faten A Mohamed, Amani A Elbaz<br />
Page<br />
117<br />
125<br />
135<br />
141<br />
147<br />
155<br />
165<br />
173<br />
181<br />
187<br />
197
Egypt Heart J 62 (1): 1-5, March 2010<br />
Myocardial Depression in Sepsis Syndrome Prognostic Value <strong>of</strong><br />
Toll-Like Receptor 4<br />
AHMED MOWAFY, MD; GAMAL HAMED, MD; SANAA ABD EL SHAFEE, MD<br />
Background: Myocardial dysfunction frequently ac<strong>com</strong>panies severe sepsis and septic shock. Whereas myocardial depression<br />
was previously considered a preterminal event, it is now clear that cardiac dysfunction as evidenced by biventricular dilatation<br />
and reduced ejection fraction is present in most patients with severe sepsis and septic shock. Myocardial depression exists<br />
despite a fluid resuscitation-dependent hyperdynamic state that typically persists in septic shock patients until death or recovery.<br />
Cardiac function usually recovers within 7–10 days in survivors. Myocardial dysfunction appears to be due to circulating<br />
depressant factors (e.g. tumor necrosis factor alpha and IL-1ß). It was hypo<strong>the</strong>sized that <strong>the</strong> Toll-like receptor 4 (TLR4) mediates<br />
myocardial dysfunction in sepsis through activation <strong>of</strong> cytokine production by monocytes/macrophages and through an increase<br />
in NO and TNF production by <strong>the</strong> myocytes <strong>the</strong>mselves.<br />
Objective: To study <strong>the</strong> relationship between <strong>the</strong> Toll-like receptor 4 concentrations and myocardial dysfunction, clinical<br />
course and out<strong>com</strong>e <strong>of</strong> septic patients.<br />
Methods: A total <strong>of</strong> 20 septic patients were enrolled into <strong>the</strong> study. Excluded from our study were <strong>the</strong> patients known to<br />
have cardiac problems and those on immunosuppressive <strong>the</strong>rapy. All included patients were subjected to <strong>the</strong> measurements <strong>of</strong><br />
TLR4. Blood samples were withdrawn at day 1 <strong>of</strong> ICU admission. Our end points were length <strong>of</strong> ICU stay, Need for organ<br />
supportive measures (Inotropic/Vasopressor support and/or Mechanical ventilation) and final out<strong>com</strong>e for all patients until ICU<br />
discharge or demise or up to a total <strong>of</strong> 28 days.<br />
Results: Toll-like receptor-4 concentrations were elevated in patients who were admitted to <strong>the</strong> ICU with septic criteria.<br />
TLR-4 concentrations were higher in patients who needed Inotropic/Vasopressor support during <strong>the</strong>ir ICU stay than those who<br />
did not require it (p value = 0.015). TLR-4 concentrations were higher in patients who developed impaired ventricular function<br />
during <strong>the</strong>ir ICU stay than those with preserved systolic cardiac function (p value = 0.006) and were significantly higher in<br />
patients who died in <strong>the</strong> ICU than those who survived (p value = 0.024).<br />
Conclusion: Estimation <strong>of</strong> Toll-like receptor-4 level may be a potentially useful prognostic test for <strong>the</strong> evaluation <strong>of</strong> septic<br />
patients when admitted to <strong>the</strong> ICU and for <strong>the</strong> prediction <strong>of</strong> <strong>the</strong>ir adverse out<strong>com</strong>es (e.g. impaired ventricular function,<br />
haemodynamic <strong>com</strong>promise with need for inotropic/vasopressor support and mortality).<br />
Key Words: Toll-like receptor-4 – Myocardial depression – Septic shock.<br />
Introduction<br />
Despite continuing advances in intensive care<br />
medicine, Sepsis represents a significant health<br />
problem. Severe sepsis and septic shock present<br />
high incidence <strong>of</strong> morbidity and mortality and are<br />
The Department <strong>of</strong> Critical Care, Cairo University.<br />
Manuscript received 11 Nov., 2009; revised 15 Dec., 2009;<br />
accepted 16 Dec., 2009.<br />
Address for Correspondence: Dr. Ahmed Mowafy, Critical<br />
Care Med. Department, Cairo University.<br />
1<br />
considered among <strong>the</strong> most important causes <strong>of</strong><br />
death in <strong>the</strong> intensive care units [1]. The overall<br />
mortality is approximately 30%, rising to 50% or<br />
more in patient with septic shock, despite recent<br />
progress in understanding its pathophysiology and<br />
improvements in supportive intensive care [2].<br />
Multiple organ systems are <strong>com</strong>promised during<br />
sepsis with several underlying mechanisms have<br />
been proposed. Myocardial dysfunction, a central<br />
<strong>com</strong>ponent in <strong>the</strong> <strong>com</strong>plex pathophysiology <strong>of</strong><br />
sepsis, contributes to <strong>the</strong> high mortality associated<br />
with this disorder. Cardiac dysfunction starts during
Myocardial Depression in Sepsis Syndrome Prognostic Value<br />
<strong>the</strong> first 24 hours <strong>of</strong> <strong>the</strong> development <strong>of</strong> sepsis,<br />
and it is reversible in survivors within 7 to 10 days<br />
[3].<br />
Sepsis develops when <strong>the</strong> initial immune response<br />
to an infection be<strong>com</strong>es amplified and <strong>the</strong>n<br />
dysregulated [4]. The pathogenesis <strong>of</strong> sepsis involves<br />
a <strong>com</strong>plex interaction between host and<br />
infecting microorganism, including bacterial recognition,<br />
cell activation, transmigration, phagocytosis<br />
and killing <strong>of</strong> <strong>the</strong> pathogens. Bacterial recognition<br />
and cellular activation are mainly driven by<br />
<strong>the</strong> interaction <strong>of</strong> <strong>the</strong> pathogens associated molecular<br />
pattern (PAMPs) and pattern recognition receptors<br />
(PRRs), among <strong>the</strong>m <strong>the</strong> Toll-like receptor<br />
[5].<br />
Toll-like receptors (TLRs) are a class <strong>of</strong> single<br />
membrane-spanning non-catalytic receptors that<br />
recognize structurally conserved molecules derived<br />
from microbes once <strong>the</strong>y have breached physical<br />
barriers such as <strong>the</strong> skin or intestinal tract mucosa,<br />
and activate immune cell responses. They play a<br />
key role in <strong>the</strong> innate immune system. This discovery<br />
fills an essential gap in our understanding <strong>of</strong><br />
<strong>the</strong> molecular events that follow microbial infection<br />
and <strong>the</strong> initial host defense to invasive pathogens.<br />
The TLRs are <strong>the</strong> critical pattern recognition molecules<br />
that alert <strong>the</strong> host to <strong>the</strong> presence <strong>of</strong> a<br />
microbial pathogen [6]. They receive <strong>the</strong>ir name<br />
from <strong>the</strong>ir similarity to <strong>the</strong> protein coded by <strong>the</strong><br />
Toll gene identified in Drosophila in 1985 by<br />
Christiane Nüsslein-Volhard [6].<br />
The presence <strong>of</strong> cardiovascular dysfunction in<br />
sepsis is associated with significantly increased<br />
mortality rate <strong>of</strong> 70% to 90% <strong>com</strong>pared with 20%<br />
in septic patients without cardiovascular impairment<br />
[7]. Numerous studies support <strong>the</strong> hypo<strong>the</strong>sis that<br />
endogenous mediators like tumour necrosis factor<br />
(TNF)-α, interleukin (IL)-1ß, as well as nitric<br />
oxide (NO) mediate myocardial dysfunction during<br />
septic shock [8]. Fur<strong>the</strong>rmore, cardiac myocytes<br />
<strong>the</strong>mselves syn<strong>the</strong>size significant amounts <strong>of</strong> TNF<br />
after LPS administration. Thus, cardiac syn<strong>the</strong>sis<br />
<strong>of</strong> proinflammatory mediators seems to play a<br />
major role in <strong>the</strong> pathogenesis <strong>of</strong> LPS-induced<br />
myocardial dysfunction. However, little is known<br />
about <strong>the</strong> cell types and <strong>the</strong> relevant signalling<br />
pathways that are involved in mediating myocardial<br />
dysfunction during gram-negative sepsis [9].<br />
In our study we tried to correlate <strong>the</strong> level <strong>of</strong><br />
TLR4 with <strong>the</strong> prognosis <strong>of</strong> septic patients.<br />
2<br />
Patients and Methods<br />
Out <strong>of</strong> 85 patients, with septic criteria, admitted<br />
to critical care department <strong>of</strong> Cairo University,<br />
twenty patients were eligible to this study. Inclusion<br />
criteria were age ≥17 yrs, with clinical signs <strong>of</strong><br />
sepsis syndrome. Sepsis was assessed according<br />
to American Colleague Of Chest Physicians/Society<br />
<strong>of</strong> Critical Care Medicine (ACCP/SCCM) criteria<br />
to have <strong>the</strong> following; clinically suspected infection<br />
with two or more <strong>of</strong> <strong>the</strong> following: temp > than<br />
38oC or less than 36oC, HR> 95/min, RR >20/min<br />
or PaCo2 12.000/mm 3 or
Ahmed Mowafy, et al<br />
Patients were divided according to <strong>the</strong> etiology <strong>of</strong><br />
sepsis into three groups medical, surgical or post<br />
traumatic patients, and according to <strong>the</strong> severity<br />
<strong>of</strong> sepsis into patients with severe sepsis or septic<br />
shock.<br />
Table 1: Demographic data <strong>of</strong> all patients.<br />
Parameter Range<br />
Age (years)<br />
Sex<br />
Admitting diagnosis<br />
Medical cases<br />
Surgical cases<br />
Trauma<br />
Severity <strong>of</strong> sepsis<br />
Severe sepsis<br />
Septic shock<br />
22-74<br />
Male (%) Female (%)<br />
13 (65%) 7 (35%)<br />
No. <strong>of</strong> patients (%)<br />
8 (40%)<br />
7 (35%)<br />
5 (25%)<br />
10 (50%)<br />
10 (50%)<br />
Mean age<br />
± SD<br />
45±17.21<br />
M:F ratio<br />
1.85<br />
The level <strong>of</strong> TLR-4 and its correlation to <strong>the</strong><br />
clinical status <strong>of</strong> <strong>the</strong> patients were thoroughly<br />
studied. TLR-4 value did not differ significantly<br />
between patients with severe sepsis and o<strong>the</strong>rs<br />
with septic shock (8.04 mg/100 mg blood vs. 11.56<br />
ug/100 uL blood respectively; p value: 0.906) Table<br />
(2).<br />
Table 2: TLR-4 in patients with severe sepsis versus septic<br />
shock.<br />
Group No.<br />
Severe sepsis<br />
Septic shock<br />
10<br />
10<br />
Mean TLR-4<br />
±SD<br />
8.04±5.95<br />
11.56±5.75<br />
p value<br />
0.906<br />
TLR4 level showed great variation in patient<br />
with heamodynamic <strong>com</strong>promise. Patients who<br />
needed vasopressor support showed higher levels<br />
<strong>of</strong> TLR4 than o<strong>the</strong>r stable patients (Table 3).<br />
Patients who needed mechanical ventilation showed<br />
higher levels <strong>of</strong> TLR4 than o<strong>the</strong>r patients (Table<br />
3).<br />
Table 3: TLR-4 value in relation to vasopressor support and<br />
need for MV.<br />
Mechanical<br />
ventilation (MV):<br />
No<br />
Yes<br />
Inotropic/vasopressor<br />
support:<br />
Yes<br />
No<br />
No.<br />
2<br />
18<br />
No.<br />
16<br />
4<br />
Mean TLR-4±SD<br />
7.28±6.47<br />
13.45±3.04<br />
Mean TLR-4±SD<br />
10.39±6.1<br />
2.43±1.56<br />
p value<br />
0.136<br />
p value<br />
0.015<br />
3<br />
There was remarkable difference in <strong>the</strong> level<br />
TLR4 in patients with myocardial dysfunction.<br />
Echocardiography was done on day 1 <strong>of</strong> <strong>the</strong> study<br />
& followed up weekly. Patients who showed early<br />
signs <strong>of</strong> myocardial dysfunction & reduction in<br />
ejection fraction had higher level <strong>of</strong> TLR4 than<br />
o<strong>the</strong>r stable patients (Table 4).<br />
Table 4: TLR-4 value and Echocardiographic findings.<br />
Reduction in EF% No. Mean TLR-4±SD p value<br />
Yes<br />
No<br />
9<br />
11<br />
12.8±4.9<br />
5.4±5.5<br />
0.006<br />
The overall mortality <strong>of</strong> all patients was very<br />
high. Fourteen out <strong>of</strong> twenty patients with severe<br />
sepsis and septic shock died during hospital stay.<br />
However, <strong>the</strong> mean TLR4 level was significantly<br />
lower in patients who survived Table (5).<br />
Table 5: TLR4 level and relation to mortality.<br />
TLR4 level<br />
no <strong>of</strong> pls<br />
Survivors Non survivors p value<br />
6 (30%)<br />
2.5<br />
Discussion<br />
14 (70%)<br />
10.6<br />
0.02<br />
Sepsis and septic shock have been recognized<br />
as an increasingly serious clinical problem, accounting<br />
for substantial morbidity and mortality.<br />
The past four decades have seen <strong>the</strong> age-adjusted<br />
mortality <strong>of</strong> sepsis increase from 0.5 to 7 per<br />
100,000 episodes despite major advances in <strong>the</strong><br />
understanding <strong>of</strong> its pathophysiology [10]. The<br />
incidence <strong>of</strong> severe sepsis in <strong>the</strong> United States<br />
today is estimated at 750,000 cases per year, resulting<br />
in 215,000 deaths annually [11]. The majority<br />
<strong>of</strong> <strong>the</strong>se sepsis patients die <strong>of</strong> refractory hypotension<br />
and cardiovascular collapse.<br />
Myocardial dysfunction frequently ac<strong>com</strong>panies<br />
severe sepsis and septic shock. Whereas myocardial<br />
depression was previously considered a preterminal<br />
event, it is now clear that cardiac dysfunction as<br />
evidenced by biventricular dilatation and reduced<br />
ejection fraction is present in most patients with<br />
severe sepsis and septic shock. Cardiac function<br />
usually recovers within 7-10 days in survivors.<br />
Myocardial dysfunction does not appear to be due<br />
to myocardial hypoperfusion but due to circulating<br />
depressant factors, including <strong>the</strong> cytokines tumor<br />
necrosis factor alpha and IL-1ß. At a cellular level,
Myocardial Depression in Sepsis Syndrome Prognostic Value<br />
reduced myocardial contractility seems to be induced<br />
by both nitric oxide-dependent and nitric<br />
oxide-independent mechanisms.<br />
Kumar et al. [12] were <strong>the</strong> first to report that<br />
<strong>the</strong> myocardial depressant activity <strong>of</strong> human serum<br />
from patients with septic shock could be eliminated<br />
by <strong>the</strong> immunoprecipitation <strong>of</strong> TNF-α and IL-1ß.<br />
Giroir et al. [13] reported that myocardial TNF-α<br />
mRNA expression increased after lipopolysaccharide<br />
(LPS) administration. Kapadia et al. [14] subsequently<br />
demonstrated that cardiac myocytes<br />
<strong>the</strong>mselves produce significant amounts <strong>of</strong> TNFα<br />
after endotoxemia. These findings suggested that<br />
<strong>the</strong> <strong>com</strong>partmentalized production <strong>of</strong> TNF-α and<br />
o<strong>the</strong>r cytokines might play an important role in<br />
<strong>the</strong> pathogenesis <strong>of</strong> LPS-induced myocardial depression<br />
in vivo. Supporting this hypo<strong>the</strong>sis is <strong>the</strong><br />
finding that <strong>the</strong> administration <strong>of</strong> TNF binding<br />
proteins preserves myocardial function in endotoxemic<br />
rats [15]. To date, however, <strong>the</strong> signaling<br />
pathways that lead to <strong>the</strong> expression <strong>of</strong> <strong>the</strong>se proinflammatory<br />
mediators in <strong>the</strong> heart during gramnegative<br />
sepsis remain undefined.<br />
A recent advance in unraveling <strong>the</strong> early events<br />
in LPS signaling has been <strong>the</strong> identification <strong>of</strong><br />
Toll-like receptors (TLRs). Toll is a transmembrane<br />
receptor in Drosophila species that is involved in<br />
dorsal-ventral patterning in <strong>the</strong> embryo and in <strong>the</strong><br />
induction <strong>of</strong> an antifungal response in <strong>the</strong> adult<br />
fly [16].<br />
It was hypo<strong>the</strong>sized that <strong>the</strong> Toll-like receptor<br />
4 (TLR-4) mediates myocardial dysfunction in<br />
sepsis through activation <strong>of</strong> cytokine production<br />
by monocytes/macrophages and through an increase<br />
in NO and TNF production by <strong>the</strong> myocytes <strong>the</strong>mselves<br />
[17].<br />
In our study we tried to correlate <strong>the</strong> relationship<br />
between level <strong>of</strong> TLR4 in serum <strong>of</strong> septic patients<br />
with <strong>the</strong>ir prognosis. The level <strong>of</strong> TLR4 was thoroughly<br />
studied in relation to <strong>the</strong> hospital course<br />
<strong>of</strong> <strong>the</strong> patients, <strong>the</strong>ir need for vasopressor support,<br />
mechanical ventilation, myocardial dysfunction<br />
and <strong>the</strong>ir final out<strong>com</strong>e.<br />
There was clear evidence that patients with<br />
septic shock had higher levels <strong>of</strong> TLR4 than patients<br />
with severe sepsis. TLR-4 concentrations were<br />
significantly higher in patients who needed inotropic/vasopressor<br />
support during <strong>the</strong>ir ICU stay.<br />
The TLR-4 levels were also significantly higher<br />
in patients with impaired left ventricular function.<br />
4<br />
Finally, <strong>the</strong> TLR-4 concentrations were also significantly<br />
higher in patients who died in <strong>the</strong> ICU<br />
than those who survived.<br />
The results reported here provide <strong>com</strong>pelling<br />
evidence for <strong>the</strong> presence <strong>of</strong> a direct relationship<br />
between TLR4 level with morbidity and mortality<br />
<strong>of</strong> septic patients. The level <strong>of</strong> TLR-4 was higher<br />
in heamodynamically unstable patients who needed<br />
vasopressor support or mechanical ventilation.<br />
Higher level <strong>of</strong> TLR-4 was usually related with<br />
adverse events.<br />
Although <strong>the</strong> above discussion focused attention<br />
on <strong>the</strong> potential deleterious effects <strong>of</strong> TLR-4 in<br />
<strong>the</strong> heart, <strong>the</strong>re may be questionable beneficial<br />
effect. Although <strong>the</strong> potential salutary effects <strong>of</strong><br />
<strong>the</strong> TLR-4 pathway in <strong>the</strong> heart remain largely<br />
unknown, it has been suggested recently that TLR-<br />
4, and perhaps o<strong>the</strong>r TLRs, may contribute to <strong>the</strong><br />
activation <strong>of</strong> an innate immune response in injured<br />
cardiac tissue [18,19]. Given <strong>the</strong> observation that<br />
TLR-4 is tightly coupled to TNF-kB activation<br />
and proinflammatory cytokine expression in <strong>the</strong><br />
heart, and that both TNF-kB and proinflammatory<br />
cytokines (physiologic levels) are cytoprotective<br />
in <strong>the</strong> heart [18,20,21], it will be important in future<br />
studies not only to delineate <strong>the</strong> full spectrum <strong>of</strong><br />
TLRs and ligands in <strong>the</strong> heart, but also to elucidate<br />
<strong>the</strong> adaptive and maladaptive signaling pathways<br />
that are downstream from TLR-mediated signaling<br />
in <strong>the</strong> adult heart.<br />
Concluding remarks:<br />
Patients with severe sepsis and septic shock<br />
represent real challenge in <strong>the</strong> ICU setting. Despite<br />
major advances in <strong>the</strong> diagnostic tools and <strong>the</strong>rapeutic<br />
options, <strong>the</strong>se entity <strong>of</strong> patient still represent<br />
a high mortality percentage. The human immune<br />
system is well endowed with potent detection and<br />
alarm systems to respond to <strong>the</strong> ever present threat<br />
<strong>of</strong> microbial pathogens. The recent discovery <strong>of</strong><br />
<strong>the</strong> TLR family now permits a detailed evaluation<br />
<strong>of</strong> <strong>the</strong> molecular pathogenesis <strong>of</strong> sepsis. The availability<br />
<strong>of</strong> human and microbial functional genomics<br />
should allow us to more fully understand <strong>the</strong> <strong>com</strong>plex<br />
interactions that exist between host and pathogen<br />
in septic patients in <strong>the</strong> future. The above<br />
findings indicate that <strong>the</strong> Toll-Like Receptor-4<br />
may be a potentially useful prognostic test for <strong>the</strong><br />
evaluation <strong>of</strong> septic patients when admitted to <strong>the</strong><br />
ICU and for <strong>the</strong> prediction <strong>of</strong> <strong>the</strong>ir adverse out<strong>com</strong>es<br />
(e.g. impaired ventricular function, haemodynamic<br />
<strong>com</strong>promise with need for inotropic/<br />
vasopressor support and mortality). Higher level
Ahmed Mowafy, et al<br />
<strong>of</strong> TLR4 is usually related to poor prognosis <strong>of</strong><br />
septic patients.<br />
References<br />
1- Angus DC, Wax RS: Epidemiology <strong>of</strong> sepsis: an update.<br />
Crit Care Med 2001; 29: 109-116.<br />
2- Martin GS, Mennino DM, Eaton S, Moss M: The epidemiology<br />
<strong>of</strong> sepsis in <strong>the</strong> United states from 1979 through<br />
2000. N Engl J Med 2003; 348: 1546-1554.<br />
3- Parker MM, Shelhamer JH. Bacharach SL, et al: Pr<strong>of</strong>ound<br />
but reversible myocardial depression in patients with<br />
septic shock. Ann Intern Med 1984; 100: 483-490.<br />
4- Alberti C, Brun-Buisson C, Burchardi H, Martin C,<br />
Goodman S, Artigas A, Sicignano A, Palazzo M, Moreno<br />
R, Boulmé R, Lepage E, et al: Epidemiology <strong>of</strong> sepsis<br />
and infection in ICU patients from an international multicentre<br />
cohort study. Intensive Care Med 2002; 28: 108-<br />
121.<br />
5- Medzhitov R, Janeway C Jr: Innate immunity. N Engl J<br />
Med 2000; 343: 338-344.<br />
6- Hansson GK, Edfeldt K: "Toll to be paid at <strong>the</strong> gateway<br />
to <strong>the</strong> vessel wall". Arterioscler. Thromb. Vasc. Biol.<br />
2005; 25 (6): 1085–7. doi:10.1161/01.ATV.0000168894.<br />
43759.47. PMID 15923538.<br />
7- Parrillo JE, Suffrendini AF, Danner RL, Cunnion: Septic<br />
shock in human advances in understanding <strong>of</strong> pathogenesis,<br />
cardiovascular dysfunction and <strong>the</strong>rapy 1990.<br />
8- Knaus WA, Draper EA, Wagner DP, et al: "APACHE II:<br />
a severity <strong>of</strong> disease classification system". Critical Care<br />
Medicine 1985; 13: 818-29.<br />
9- Horton JW, Maass D, White J, Sanders: Nitric oxide<br />
modulation <strong>of</strong> TNF-alpha induced cardiac contractility<br />
dysfunction in concentration dependent Am J Physical<br />
Heart Cir 2000.<br />
10- Center for Diseases Control and Prevention: National<br />
Center or Health Statistics: mortality patterns – United<br />
States, 1990. Monthly Vital Stat Rep 1993, 41: 5.<br />
11- Angus DC, Linde-Zwirble WT, Lidicker J, Clermont G,<br />
Carcillo J, Pinsky MR: Epidemiology <strong>of</strong> severe sepsis in<br />
5<br />
<strong>the</strong> United States: analysis <strong>of</strong> incidence, out<strong>com</strong>e and<br />
associated costs <strong>of</strong> care. Crit Care Med 2001; 29: 1303-<br />
1310.<br />
12- Kumar A, Thota V, Dee L, Olson J, Uretz E, Parrillo JE.<br />
Tumor necrosis factor α and interleukin 1ß are responsible<br />
for in vitro myocardial cell depression induced by human<br />
septic shock serum. J Exp Med 1996; 183: 949-58.<br />
13- Giroir BP, Johnson JH, Brown T, Allen GL, Beutler B:<br />
The tissue distribution <strong>of</strong> tumor necrosis factor biosyn<strong>the</strong>sis<br />
during endotoxemia. J Clin Invest 1992; 90: 693-<br />
8.<br />
14- Kapadia S, Lee J, Torre-Amione G, Birdsall HH, Ma TS,<br />
Mann DL: Tumor necrosis factor-α gene and protein<br />
expression in adult feline myocardium after endotoxin<br />
administration. J Clin Invest 1995; 96: 1042-52.<br />
15- Meng X, Ao L, Meldrum DR, et al: TNF-α and myocardial<br />
depression in endotoxemic rats: temporal discordance <strong>of</strong><br />
an obligatory relationship. Am J Physiol 1998; 275: R502-<br />
8.<br />
16- Kopp EB, Medzhitov R. The toll-receptor family and<br />
control <strong>of</strong> innate immunity. Curr Opin Immunol 1999;<br />
11: 13-8.<br />
17- Francis SE, Holden H, Holt CM, Duff GW: Interleukin-<br />
1 in myocardium and coronary arteries <strong>of</strong> patients with<br />
dilated cardiomyopathy. J Moll Cell Cardiol 1998; 30,<br />
215-243.<br />
18- Medzhitov RC, Janeway CA: Innate immunity: <strong>the</strong> virtues<br />
<strong>of</strong> a nonclonal system <strong>of</strong> recognition. Cell 1997; 91: 295-<br />
8.<br />
19- Frantz S, Kobzik L, Kim YD, et al: Toll4 (TLR4) expression<br />
in cardiac myocytes in normal and failing myocardium.<br />
J Clin Invest 1999; 104: 271-80.<br />
20- Xuan YT, Tang XL, Banerjee S, et al: Nuclear factor<br />
kappaÅ]B plays an essential role in <strong>the</strong> late phase <strong>of</strong><br />
ischemic preconditioning in conscious rabbits. Circ Res<br />
1999; 84: 1095-109.<br />
21- Kurrelmeyer K, Michael L, Baumgarten G, et al: Endogenous<br />
myocardial tumor necrosis factor protects <strong>the</strong> adult<br />
cardiac myocyte against ischemicÅ]induced apoptosis in<br />
a murine model <strong>of</strong> acute myocardial infarction. Proc Natl<br />
Acad Sci USA 2000; 97: 5456-61.
Egypt Heart J 62 (1): 7-17, March 2010<br />
Cardiac Affection after Subarachnoid Hemorrhage, Correlation with<br />
Severity and Etiology<br />
RANIA EL HOSEINY, MD; AHMED BATTAH, MD; MOHAMED ASHRAF, MD<br />
Introduction: Cardiac injury and dysfunction after subarachnoid hemorrhage (SAH) is a well-recognized phenomenon,<br />
ECG changes, arrhythmias, serum elevations <strong>of</strong> cardiac enzymes and left ventricular (LV) systolic dysfunction have been<br />
described in SAH patients. In recent years, considerable investigative interest has been directed at evaluation <strong>of</strong> frequency <strong>of</strong><br />
this cardiac injury, clinical implications, predictors and out<strong>com</strong>e, Despite <strong>the</strong> large body <strong>of</strong> evidence testifying <strong>the</strong> development<br />
<strong>of</strong> myocardial injury in SAH, <strong>the</strong> true incidence in this population remains unknown.<br />
Methodology: Thirty patients with acute subarachnoid hemorrhage were included in <strong>the</strong> study, <strong>of</strong> whome twenty patients<br />
had aneurysmal SAH (12 women, 8 men, with mean age 47.55±12.356 years) and ten patients had traumatic SAH (4 women,<br />
6 men, with mean age 42.10±14.75 years), patients with evidence <strong>of</strong> epidural, subdural or intracerebral hemorrhage, history<br />
<strong>of</strong> cardiac disease, renal impairement and systemic sepsis were excluded from <strong>the</strong> study, All patients were subjected to detailed<br />
medical history taken from <strong>the</strong> patient or a family member, daily clinical assessment <strong>of</strong> neurological status (graded according<br />
to Hess and Hunt score) and cardiac status, daily ECG, biochemical measurement <strong>of</strong> cardiac troponin I every o<strong>the</strong>r day for 7<br />
days using IMMULITE test (reference range for upper limit <strong>of</strong> normal 1ng/ml) and transthoracic echocardiographic examination<br />
on admission (day 1) <strong>of</strong> <strong>the</strong> patient and follow-up after one week (day 7) for assessment <strong>of</strong> both global and regional systolic<br />
functions <strong>of</strong> <strong>the</strong> left ventricle, it was reported as abnormal if <strong>the</strong>re was evidence <strong>of</strong> regional wall motion abnormality RWMA<br />
or EF
Cardiac Affection after Subarachnoid Hemorrhage<br />
Conclusions: Different types and frequencies <strong>of</strong> ECG changes were found in patients with SAH, most frequently were<br />
repolarization abnormalities, independent <strong>of</strong> previous history <strong>of</strong> ischemic heart disease.<br />
Elevated cardiac troponin I and Left ventricular systolic dysfunction both global and regional were frequently observed<br />
after SAH, aneurysmal exhibit more severe affection than traumatic.<br />
ECG abnormalities, elevated cardiac troponin I and left ventricular dysfunction were associated with more severe neurological<br />
injury.<br />
Key Words: ECG – Echocardiography – Cardiac troponin I – Subarachnoid hemorrhage.<br />
Introduction<br />
Subarachnoid hemorrhage (SAH) is a major<br />
clinical problem worldwide, it has a wide variety<br />
<strong>of</strong> neurological and extraneurological <strong>com</strong>plications,<br />
<strong>of</strong> which <strong>the</strong> most frequent were cardiovascular<br />
<strong>com</strong>plications [1,2].<br />
The association between central nervous system<br />
disease and cardiac affection is well known and<br />
has been described in intracerebral hemorrhage,<br />
intracranial tumors, meningitis, and stroke [3].<br />
However, this association is particularly strong in<br />
SAH, after which electrocardiogram (ECG) changes<br />
[4] arrhythmias, left ventricular (LV) dysfunction,<br />
and elevation <strong>of</strong> <strong>the</strong> creatine phosphokinase (CPK)-<br />
MB fraction and cardiac troponin I (cTnI) have<br />
been reported, <strong>of</strong> which, <strong>the</strong> most <strong>com</strong>mon is <strong>the</strong><br />
ECG changes.<br />
The pathophysiology <strong>of</strong> cardiac affection after<br />
SAH in humans remains unknown and controversial,<br />
although data from animal models indicates<br />
that catecholamine-mediated injury is <strong>the</strong> most<br />
likely cause <strong>of</strong> cardiac injury after SAH.<br />
Cardiac affection after SAH negatively influences<br />
mortality and, more specifically, <strong>the</strong> sequelae<br />
<strong>of</strong> heart failure affect out<strong>com</strong>e after SAH, as hypotension<br />
is <strong>the</strong> main cause <strong>of</strong> secondary brain<br />
injury, <strong>the</strong>refore, early identification and monitoring<br />
<strong>of</strong> cardiac dysfunction is a critical issue [5].<br />
Aim <strong>of</strong> <strong>the</strong> work:<br />
• To evaluate cardiac affection in patients with<br />
subarachnoid hemorrhage.<br />
• To correlate cardiac affection with <strong>the</strong> neurological<br />
status in <strong>the</strong>se patients.<br />
Methods<br />
The present study was carried out on 30 patients<br />
diagnosed to have acute subarachnoid hemorrhage<br />
8<br />
(confirmed by CT brain) and admitted within 24<br />
hours to Kasr El-Aini Hospital, Cairo University<br />
in <strong>the</strong> period between December 2008 to June<br />
2009, with <strong>the</strong> calendar day <strong>of</strong> SAH onset was<br />
referred to as day 1.<br />
Our patients were divided into two groups:<br />
• Group 1: Patients diagnosed to have aneurysmal<br />
SAH [20 patients] (with aneurysm identified with<br />
cerebral angiography).<br />
• Group 2: Patients diagnosed to have traumatic<br />
SAH [10 patients].<br />
Exclusion criteria:<br />
1- Patients with evidence <strong>of</strong> epidural, subdural or<br />
intracerebral hemorrhage.<br />
2- History <strong>of</strong> cardiac disease:<br />
• Coronary artery disease.<br />
• Impairement <strong>of</strong> left ventricular systolic function.<br />
3- Renal impairement defined as serum creatinine<br />
level more than 1.5mg/dl that causes a non<br />
specific elevation <strong>of</strong> <strong>the</strong> troponin.<br />
4- Systemic sepsis that also causes a non specific<br />
elevation <strong>of</strong> <strong>the</strong> troponin.<br />
All patients were subjected to:<br />
Detailed medical history taken from <strong>the</strong> patient<br />
or a family member including: Age, sex, history<br />
<strong>of</strong> smoking, history <strong>of</strong> diabetes mellitus, history<br />
<strong>of</strong> hypertension, history <strong>of</strong> neurological troubles<br />
and history <strong>of</strong> cardiac diseases.<br />
Daily clinical assessment <strong>of</strong>:<br />
a- Neurological status (graded according to Hess<br />
and Hunt score) [6].<br />
b- Cardiac status for evidence <strong>of</strong> cardiac dysfunction<br />
and/or arrhythmias.
Rania El Hoseiny, et al<br />
Daily ECG:<br />
Twelve lead ECG with consistent chest leads<br />
positioning performed daily for 7 days.<br />
ECG was considered abnormal if <strong>the</strong> following<br />
detected:<br />
• ST-T wave changes:<br />
º ST segment elevated or depressed greater than<br />
0.1mV in limb leads or 0.2mV in precordial<br />
leads.<br />
º T wave inversion, flattening or peaking, T wave<br />
was considered peaked if its amplitude exceeded<br />
0.5mV in any limb lead or 1.5mV in any<br />
precordial lead [11].<br />
• QTc interval prolongation (>460msec) measured<br />
with modified Bazett’s formula [QTc=QT+<br />
0.00175 (ventricular rate-60)] [12,13].<br />
• Arrhythmias.<br />
Biochemical measurement:<br />
Cardiac troponin I was measured every o<strong>the</strong>r<br />
day for 7 days using IMMULITE test, an immune<br />
assay method quantitatively measure cardiac troponin<br />
I in ng/ml (reference range for upper limit <strong>of</strong><br />
normal 1ng/ml).<br />
Transthoracic echocardiographic examination:<br />
All patients were subjected to transthoracic<br />
echocardiographic examination done upon admission<br />
(day 1) <strong>of</strong> <strong>the</strong> patient and follow-up done after<br />
one week (day 7).<br />
The study was conducted using an ATL HDI<br />
5000 colored echocardiographic machine using a<br />
transducer 3.5MHz.<br />
Both global and regional systolic functions <strong>of</strong><br />
<strong>the</strong> left ventricle were assessed. Echocardiogram<br />
was reported as abnormal if <strong>the</strong>re was evidence <strong>of</strong><br />
regional wall motion abnormality RWMA or EF<br />
Cardiac Affection after Subarachnoid Hemorrhage<br />
Correlation between hypertension and cardiac<br />
function: There was no statistically significant<br />
difference between both groups (hypertensive and<br />
non hypertensive) as regard:<br />
1- The frequency <strong>of</strong> abnormal ECG changes both<br />
on day 1 (p value=0.471) and on day 7 (p value=<br />
0.32).<br />
2- The frequency <strong>of</strong> elevated cardiac troponin I<br />
both on day 1 (p value=0.6) and day 7 (p value=<br />
0.556).<br />
3- The frequency <strong>of</strong> LV systolic dysfunction both<br />
on day 1 (p value=0.448) and day 7 (p value=<br />
0.464).<br />
Frequency and distribution <strong>of</strong> cardiac abnormalities<br />
in <strong>the</strong> aneurysmal SAH group:<br />
Out <strong>of</strong> twenty patients included in this group,<br />
fifteen patients (75%) had cardiac abnormalities,<br />
<strong>the</strong>ir distribution was as follow:<br />
a- Patients with ECG changes:<br />
All <strong>the</strong> fifteen patients had ECG changes, distributed<br />
as follow:<br />
1- ST-T wave changes were detected in thirteen<br />
patients since day 1, by day 7, <strong>the</strong>se ST-T wave<br />
changes were <strong>com</strong>pletely reversed in four patients<br />
and showed partial reversibility in six<br />
patients.<br />
2- Long QTc was detected in three patients, that<br />
normalized in two <strong>of</strong> <strong>the</strong>m by day 7.<br />
3- Arrhythmias were detected in six patients, <strong>of</strong><br />
whom, four had sinus tachycardia, one patient<br />
had sinus bradycardia and three patients had<br />
atrial premature beats (two <strong>of</strong> <strong>the</strong>m had sinus<br />
tachycardia), by day 5, three patients out <strong>of</strong> <strong>the</strong><br />
four patients with sinus tachycardia exhibited<br />
slowing which <strong>of</strong> this tachycardia was persistent<br />
in <strong>the</strong> fourth patient till day 7, all <strong>the</strong> patients<br />
with atrial extrasystoles, showed <strong>com</strong>plete recovery<br />
by day 7 and <strong>the</strong> patient with sinus<br />
bradycardia showed persistence <strong>of</strong> this rhythm<br />
till day 7.<br />
b- Patients with elevated cTnI:<br />
Six patients were detected to have elevated<br />
cardiac troponin (cTnI), <strong>of</strong> whom, three patients<br />
had cTnI normalized on day 7.<br />
c- Patients with echocardiographic abnormalities:<br />
There were two patients who had a low ejection<br />
fraction (EF=42% & 44%) on day 1, that improved<br />
on day 7 (EF =63% & 54% respectively).<br />
10<br />
Three patients were detected to have regional<br />
wall motion abnormalities on day 1, <strong>the</strong>n <strong>the</strong>se<br />
changes <strong>com</strong>pletely disappeared in two patients<br />
and partially disappeared in one patient on day 7.<br />
Table 1: Distribution <strong>of</strong> cardiac abnormalities in <strong>the</strong> aneurysmal<br />
SAH group.<br />
ECG changes<br />
ST-T wave changes<br />
Long QTc interval<br />
Arrhythmias:<br />
Sinus tachycardia<br />
Sinus bradycardia<br />
Atrial extrasystoles<br />
Positive cardiac<br />
troponin I<br />
Low EF<br />
RWMAs<br />
Number<br />
<strong>of</strong> affected<br />
patients<br />
13<br />
3<br />
6<br />
4<br />
1<br />
3<br />
6<br />
2<br />
3<br />
Complete<br />
reversibility<br />
on day 7<br />
4<br />
2<br />
3<br />
–<br />
3<br />
3<br />
2<br />
2<br />
Partial<br />
reversibility<br />
on day 7<br />
Frequency and distribution <strong>of</strong> cardiac abnormalities<br />
in <strong>the</strong> traumatic SAH group:<br />
a- Patients with ECG changes:<br />
Out <strong>of</strong> ten patients included in this group, only<br />
three had cardiac abnormalities represented by ST-<br />
T wave changes associated with sinus tachycardia,<br />
by day 7, two patients showed partial reversibility<br />
<strong>of</strong> <strong>the</strong>se changes and it was persistent in <strong>the</strong> third<br />
patient.<br />
There was no evidence <strong>of</strong> elevated cTnI nor<br />
echocardiographic abnormalities in any <strong>of</strong> <strong>the</strong><br />
Patients included in this group.<br />
Table 2: Distribution <strong>of</strong> cardiac abnormalities in <strong>the</strong> traumatic<br />
SAH group.<br />
ECG changes<br />
ST-T wave changes<br />
associated with sinus<br />
tachycardia<br />
Positive cardiac<br />
troponin I<br />
Low EF & RWMAs<br />
Number<br />
<strong>of</strong> affected<br />
patients<br />
3<br />
0<br />
0<br />
Complete<br />
reversibility<br />
on day 7<br />
–<br />
–<br />
–<br />
6<br />
–<br />
–<br />
–<br />
–<br />
–<br />
–<br />
1<br />
Partial<br />
reversibility<br />
on day 7<br />
2<br />
–<br />
–
Rania El Hoseiny, et al<br />
Correlation between neurological status and<br />
cardiac function in aneurysmal SAH group:<br />
a- Correlation between neurological status and<br />
ECG analysis:<br />
In <strong>the</strong> present study, we evaluated <strong>the</strong> neurological<br />
status <strong>of</strong> <strong>the</strong> studied patients by Hess &<br />
Hunt scoring system and divided <strong>the</strong>m into:<br />
Twelve patients exhibited mild affection (Hess<br />
& Hunt score 1&2) while severe affection (Hess<br />
& Hunt score 3-5) was exhibited by 8 patients.<br />
There was a statistically significant higher<br />
frequency <strong>of</strong> abnormal ECG on day 1 in those<br />
patients with severe aneurysmal SAH (H&H score<br />
3-5) when <strong>com</strong>pared to those with mild aneurysmal<br />
SAH (H&H score 1&2) (100% vs 58.3%) (p value=0.035),<br />
Fig. (1). On day 7 <strong>the</strong>re was no statistically<br />
significant difference between both groups<br />
(75% versus 41.7%, p value=0.142).<br />
100<br />
90<br />
80<br />
70<br />
60<br />
50<br />
40<br />
30<br />
20<br />
10<br />
0<br />
p value: 0.035<br />
58.3<br />
100<br />
Mild aneurysmal SAH Severe aneurysmal SAH<br />
Figure 1: Abnormal ECG in day 1.<br />
b- Correlation between neurological status and<br />
cardiac troponin I measurement:<br />
Out <strong>of</strong> twelve patients included in <strong>the</strong> mild<br />
aneurysmal SAH group, none showed positive<br />
cardiac troponin I on day 1 (0%), while six (out<br />
<strong>of</strong> eight patients) included in <strong>the</strong> severe aneurysmal<br />
SAH group (75%) had positive cardiac troponin I<br />
(p value=0.001) Fig. (2).<br />
80<br />
70<br />
60<br />
50<br />
40<br />
30<br />
20<br />
10<br />
0<br />
p value: 0.001<br />
0<br />
Mild aneurysmal SAH Severe aneurysmal SAH<br />
Figure 2: Frequency <strong>of</strong> positive troponin in day 1.<br />
75<br />
11<br />
Similarly, we found a statistically significant<br />
higher frequency <strong>of</strong> positive cardiac troponin I in<br />
day 7 in those patients with severe aneurysmal<br />
SAH (37.5%) when <strong>com</strong>pared to cases with mild<br />
aneurysmal SAH (0%) (p value=0.021) Fig. (3).<br />
40<br />
35<br />
30<br />
25<br />
20<br />
15<br />
10<br />
5<br />
0<br />
p value: 0.021<br />
0<br />
Mild aneurysmal<br />
SAH<br />
37.5<br />
Severe aneurysmal<br />
SAH<br />
Figure 3: Frequency <strong>of</strong> positive troponin in day 7.<br />
c- Correlation between neurological status and<br />
echocardigraphic findings:<br />
In <strong>the</strong> present work <strong>the</strong>re was a statistically<br />
significant higher incidence <strong>of</strong> systolic dysfunction<br />
(global & regional) in <strong>the</strong> cases with severe aneurysmal<br />
SAH (37.5%) when <strong>com</strong>pared to cases with<br />
mild aneurysmal SAH (0%) (p value=0.021) in<br />
day 1, with no statistically significant difference<br />
between both subgroups in day 7 (p value=0.4)<br />
Fig. (4).<br />
40<br />
35<br />
30<br />
25<br />
20<br />
15<br />
10<br />
5<br />
p value: 0.021<br />
0<br />
37.5<br />
0<br />
Mild aneurysmal Severe aneurysmal<br />
SAH<br />
SAH<br />
Figure 4: Frequency <strong>of</strong> systolic dysfunction in day 1.
Cardiac Affection after Subarachnoid Hemorrhage<br />
Table 3: Correlation between neurological status and cardiac<br />
function in aneurysmal SAH group on day 1.<br />
Frequency <strong>of</strong> ECG changes<br />
Frequency <strong>of</strong> positive<br />
cardiac troponin I<br />
Frequency <strong>of</strong> echocardiographic<br />
findings<br />
Mild<br />
affection<br />
subgroup<br />
58.3%<br />
0%<br />
0%<br />
Severe<br />
affection<br />
subgroup<br />
100%<br />
75%<br />
37.5%<br />
p<br />
value<br />
0.035<br />
0.001<br />
0.021<br />
Table 4: Correlation between neurological status and cardiac<br />
function in aneurysmal SAH group on day 7.<br />
Frequency <strong>of</strong> ECG changes<br />
Frequency <strong>of</strong> positive<br />
cardiac troponin I<br />
Frequency <strong>of</strong> echocardiographic<br />
findings<br />
Mild<br />
affection<br />
subgroup<br />
41.7%<br />
0%<br />
0%<br />
Severe<br />
affection<br />
subgroup<br />
75%<br />
37.5%<br />
12.5%<br />
p<br />
value<br />
0.14<br />
0.021<br />
0.4<br />
Comparison between aneurysmal and traumatic<br />
SAH groups as regards:<br />
a- Neurological status (assessed by Hess & Hunt<br />
score):<br />
We found a statistically significant higher frequency<br />
<strong>of</strong> poor neurological status in <strong>the</strong> traumatic<br />
SAH group when <strong>com</strong>pared to <strong>the</strong> aneurysmal<br />
SAH group On day 1 and day 7 (p value 0.002 &<br />
0.001 respectively).<br />
b- Electrocardiographic abnormalities:<br />
In <strong>the</strong> current study, <strong>the</strong>re was a statistically<br />
significant higher incidence <strong>of</strong> ECG abnormalities<br />
in <strong>the</strong> aneurysmal SAH group (75%) when <strong>com</strong>pared<br />
to <strong>the</strong> traumatic SAH group (30%) on day<br />
1 (p value=0.045), yet, we did not find any statistically<br />
significant difference between both groups<br />
as regard <strong>the</strong> incidence <strong>of</strong> ECG abnormalities on<br />
day 7 (p value=0.24).<br />
c- Cardiac troponin I (cTnI):<br />
On day 1, <strong>the</strong>re was a statistically significant<br />
higher frequency <strong>of</strong> positive cardiac troponin I in<br />
<strong>the</strong> aneurysmal SAH group (30%) <strong>com</strong>pared to<br />
traumatic SAH group (0%) (p value=0.05), yet, on<br />
day 7 <strong>the</strong>re was no statistically significant difference<br />
between both groups [aneurysmal (15%) versus<br />
traumatic (0%)] (p value=0.246).<br />
12<br />
d- Global and regional left ventricular systolic<br />
function:<br />
There was no statistically significant difference<br />
between both groups as regard <strong>the</strong> frequency <strong>of</strong><br />
LV systolic dysfunction both on day 1 and day 7,<br />
(p value=0.281 & 0.714 respectively).<br />
Table 5: Comparison between aneurysmal and traumatic SAH<br />
groups on day 1.<br />
Variable<br />
Frequency <strong>of</strong> poor<br />
neurological status<br />
Frequency <strong>of</strong> ECG changes<br />
Frequency <strong>of</strong> positive cTnI<br />
Frequency <strong>of</strong> LV systolic<br />
dysfunction<br />
Aneurysmal<br />
SAH<br />
40%<br />
75%<br />
30%<br />
15%<br />
Traumatic<br />
SAH<br />
100%<br />
30%<br />
0%<br />
0%<br />
p<br />
value<br />
0.004<br />
0.045<br />
0.05<br />
0.28<br />
Table 6: Comparison between aneurysmal and traumatic SAH<br />
groups on day 7.<br />
Variable<br />
Frequency <strong>of</strong> poor<br />
neurological status<br />
Frequency <strong>of</strong> ECG changes<br />
Frequency <strong>of</strong> positive CTAI<br />
Frequency <strong>of</strong> LV systolic<br />
dysfunction<br />
Aneurysmal<br />
SAH<br />
80%<br />
55%<br />
15%<br />
5%<br />
Discussion<br />
Traumatic<br />
SAH<br />
100%<br />
37.5%<br />
0%<br />
0%<br />
p<br />
value<br />
0.001<br />
0.24<br />
0.24<br />
0.71<br />
Primary findings <strong>of</strong> <strong>the</strong> study <strong>com</strong>pared with<br />
published literature revealed:<br />
1- Regarding <strong>the</strong> frequency <strong>of</strong> abnormal ECG<br />
findings in patients with aneurysmal subarachnoid<br />
hemorrhage:<br />
We detected abnormal ECG findings in 15 out<br />
<strong>of</strong> 20 patients (representing 75%), this frequency<br />
is consistent with most <strong>of</strong> <strong>the</strong> published data, <strong>the</strong><br />
distribution <strong>of</strong> <strong>the</strong>se findings was as follow: ST-<br />
T wave changes were detected in thirteen patients<br />
since day 1, long QTc was detected in three patients<br />
and arrhythmias detected in six patients, <strong>of</strong> whom,<br />
four patients had sinus tachycardia, one patient<br />
had sinus bradycardia and three patients had atrial<br />
premature beats.<br />
Penka, et al, in 2005; detected abnormal ECG<br />
findings in 45 out <strong>of</strong> 56 patients with aneurysmal
Rania El Hoseiny, et al<br />
SAH which represent 80.4%, out <strong>of</strong> <strong>the</strong> later 43.1%<br />
(n=22 cases) showed repolarization changes, 21.6%<br />
(n=11 cases) showed conductive disturbances,<br />
19.6% (n=10 cases) showed LVH, 15.6% (n=8<br />
cases) heart rhythm disturbances [7].<br />
Parekh, et al, in 2000; reported ECG changes<br />
in 23 out <strong>of</strong> 39 patients with aneurysmal SAH<br />
representing 59% with ST-T wave changes was<br />
detected in 17 patients, long QTc in six patients<br />
and supraventricular arrhythmias in four patients<br />
[14].<br />
Naidech, et al, in 2005; detected abnormal ECG<br />
findings in 174 out <strong>of</strong> 253 patients with aneurysmal<br />
SAH which represent 69% [10].<br />
Sugimoto, et al, in 2008; observed abnormal<br />
ECG findings-in <strong>the</strong> form <strong>of</strong> pathological Q wave,<br />
ST segment deviation, T wave inversion and QT<br />
prolongation-in 29 out <strong>of</strong> 47 patients with aneurysmal<br />
SAH which represent 62% [15].<br />
Sakr, et al, in 2004; reported ECG changes in<br />
106 out <strong>of</strong> 159 patients with aneurysmal SAH<br />
representing 66.7% [17].<br />
Contrary to our results were <strong>the</strong> data published<br />
by Frontera, et al, in 2008; studied <strong>the</strong> frequency<br />
<strong>of</strong> cardiac arrhythmias after SAH in 580 patients<br />
and <strong>the</strong>y detected a variety <strong>of</strong> arrhythmias in 4.3%<br />
(n=25) <strong>of</strong> <strong>the</strong>se patients, Atrial fibrillation and<br />
atrial flutter were <strong>the</strong> most <strong>com</strong>mon arrhythmias<br />
(19 patients). This frequency (4.3%) is much lower<br />
than detected in our study, as we detected arrhythmias<br />
in 30% (n=6 out <strong>of</strong> 20) <strong>of</strong> <strong>the</strong> patients but<br />
this can be related to <strong>the</strong> marked discrepancy in<br />
samples size [16].<br />
2- Regarding <strong>the</strong> frequency <strong>of</strong> abnormal ECG<br />
findings in patients with traumatic subarachnoid<br />
hemorrhage:<br />
We detected abnormal ECG findings in 3 out<br />
<strong>of</strong> 10 patients (representing 30%) represented by<br />
ST-T wave changes associated with sinus tachycardia<br />
detected in all <strong>of</strong> <strong>the</strong>m.<br />
Review <strong>of</strong> literature revealed that electrocardiographic<br />
abnormalities after head injury have<br />
so far been scarcely reported, no studies to date<br />
has been conducted evaluating cardiac <strong>com</strong>plications<br />
in traumatic SAH patients, most previous<br />
studies have dealt with ECG changes and o<strong>the</strong>r<br />
cardiac consequences <strong>of</strong> aneurysmal subarachnoid<br />
hemorrhage (SAH) [18].<br />
13<br />
Wittebole X, et al and Hemant, et al, published<br />
two case reports showed different patterns <strong>of</strong> ECG<br />
changes after closed head injury.<br />
Wittebole X, et al, in 2005 described different<br />
patterns <strong>of</strong> ECG changes-sinus tachycardia, a pattern<br />
<strong>of</strong> subepicardial injury with elevated ST segment<br />
in leads I, II, aVL, aVF, V5, V6 and a terminal<br />
T-wave negativity with prolonged QT interval and<br />
numerous self-terminating salvos <strong>of</strong> polymorphous<br />
ventricular tachycardia-in a 32 year old man admitted<br />
after a head trauma with a brain CT scan<br />
was normal, by 16 th day, <strong>the</strong> ECG only showed<br />
residual T-wave inversion in <strong>the</strong> inferior leads,<br />
four months later, <strong>the</strong> 12-lead ECG was normalized<br />
[19].<br />
Hemant, et al, 2008 reported ECG repolarization<br />
abnormalities (ST segment elevation in <strong>the</strong> inferolateral<br />
leads) and sinus tachycardia in a 31-year<br />
old male patient with head injury, within 48 hours,<br />
this patient was subjected to coronary angiography<br />
on <strong>the</strong> 9 th day that revealed normal coronaries [20].<br />
3- Regarding <strong>the</strong> frequency <strong>of</strong> elevated cardiac<br />
troponin I in patients with aneurysmal subarachnoid<br />
hemorrhage:<br />
In our study, 30% (n=6 cases) <strong>of</strong> patients had<br />
evidence <strong>of</strong> elevated cardiac troponin I, a result<br />
that is consistent with <strong>the</strong> published data.<br />
Similar to our results, Sommargren, et al, in<br />
2002; detected elevated cTnI in 21 out <strong>of</strong> 100<br />
patients (21%) included in <strong>the</strong>ir study [21].<br />
Parekh, et al, in 2000; studied <strong>the</strong> incidence <strong>of</strong><br />
myocardial injury in aneurysmal SAH using cTnI<br />
assay daily for 7 days, 39 patients were included<br />
in <strong>the</strong> study, <strong>of</strong> whom, 8 patients (representing<br />
20%) detected to have elevated cTnI [14].<br />
Tung, et al, in 2004; studied <strong>the</strong> neurocardiogenic<br />
injury after aneurysmal SAH in 223 patients,<br />
all <strong>of</strong> <strong>the</strong>m subjected to serial cTnI measurement<br />
on days 1, 3 and 6 after enrollement in <strong>the</strong> study,<br />
elevated cTnI was detected in 45 patients (representing<br />
20%) which is matched with our results<br />
[22].<br />
Ramappa, et al, in 2007, reported frequency <strong>of</strong><br />
elevated cTnI 37% in <strong>the</strong>ir retrospective study on<br />
incidence <strong>of</strong> elevated cTnI in patients with aneurysmal<br />
SAH, <strong>the</strong> study was conducted on 83 patients,<br />
<strong>of</strong> whom, 31 patients had elevated cTnI [24].
Cardiac Affection after Subarachnoid Hemorrhage<br />
Hravnak, et al, in 2009, conducted a prospective<br />
longitudinal study on 204 patients diagnosed to<br />
have aneurysmal SAH, elevated cTnI was detected<br />
in 65 patients (representing 31%) which is very<br />
close to our results [8].<br />
Naidech and colleagues in 2005; studied cTnI<br />
elevation in aneurysmal SAH and its relation to<br />
cardiovascular morbidity and out<strong>com</strong>e after <strong>the</strong><br />
hemorrhage, 253 patients were included in <strong>the</strong><br />
study, cTnI was measured in all patients on admission<br />
<strong>the</strong>n serial measurements were conducted for<br />
patients with elevated cTnI level on <strong>the</strong> first day,<br />
out <strong>of</strong> <strong>the</strong> 253 patients only 172 (representing 68%)<br />
detected to have elevated cTnI which is much<br />
higher than our results [10] also Tanabe, et al, in<br />
2008, studied frequency <strong>of</strong> cTnI elevation in patients<br />
with aneurysmal SAH, <strong>the</strong> study was conducted<br />
on 103 patients, elevated cTnI was reported<br />
in 54 patients (representing 52%) which is also<br />
higher than our results, this may be explained by<br />
marked discrepancy in samples size (253&103<br />
versus 20 patients) [23].<br />
4- Regarding <strong>the</strong> frequency <strong>of</strong> elevated cardiac<br />
troponin I in patients with traumatic subarachnoid<br />
hemorrhage:<br />
In our study <strong>the</strong>re was no evidence <strong>of</strong> elevated<br />
cardiac troponin I in patients with traumatic subarachnoid<br />
hemorrhage.<br />
Review <strong>of</strong> literature revealed that no studies to<br />
date has been conducted on evaluation <strong>of</strong> cardiac<br />
troponin I in traumatic SAH patients, only one<br />
study conducted by Salim, et al, in 2008 evaluated<br />
cardiac troponin I elevation in patients with traumatic<br />
brain injury, <strong>the</strong>y reported this elevation in<br />
125 out <strong>of</strong> 420 patients (representing 29.8%) [25].<br />
5- Regarding <strong>the</strong> prevelance <strong>of</strong> left ventricular<br />
systolic dysfunction, in patients with aneurysmal<br />
SAH:<br />
In our study, 15% (n=3 out <strong>of</strong> 20) <strong>of</strong> patients<br />
had evidence <strong>of</strong> left ventricular systolic dysfunction,<br />
all <strong>of</strong> <strong>the</strong>m had regional wall motion abnormalitiesthat<br />
were reversible on follow up on day 7, <strong>com</strong>peletely<br />
in 10% <strong>of</strong> patients and partially in 5% -<br />
and two patients had low ejection fraction (
Rania El Hoseiny, et al<br />
Review <strong>of</strong> literature revealed studies conducted<br />
only on evaluation <strong>of</strong> cardiac dysfunction due to<br />
traumatic brain injury.<br />
Bahloul, et al, in 2006, studied cardiac dysfunction<br />
due to traumatic brain injury in 202 patients,<br />
only two patients (representing about 1%) reported<br />
to have global hypokinesia with a decrease in<br />
LVEF to 0.40 that <strong>com</strong>pletely recovered during<br />
follow-up 7 days after <strong>the</strong> initial study [28].<br />
Wittebole, et al, in 2005, described-in <strong>the</strong> previously<br />
mentioned case report-hypokinesia <strong>of</strong> <strong>the</strong><br />
inferior wall <strong>of</strong> <strong>the</strong> left ventricle that normalized<br />
on day 6 after <strong>the</strong> trauma [19].<br />
7- Regarding <strong>the</strong> correlation between neurological<br />
status and ECG analysis:<br />
In <strong>the</strong> present study we found a statistically<br />
significant higher frequency <strong>of</strong> abnormal ECG in<br />
day 1 in those patients with severe aneurysmal<br />
SAH (100%) when <strong>com</strong>pared to those with mild<br />
aneurysmal SAH (58.3%) [p value=0.035], <strong>the</strong>n<br />
<strong>the</strong>re was a tendency toward higher frequency <strong>of</strong><br />
abnormal ECG in day 7 in those patients with<br />
severe SAH as <strong>com</strong>pared to those with mild SAH,<br />
yet this tendency lacked any statistical significance<br />
(75% versus 41.7%, p value=0.142).<br />
Similarly, Zar<strong>of</strong>f, et al, in 1999, who studied<br />
ECG abnormalities in aneurysmal SAH and <strong>the</strong>ir<br />
correlation with neurological status (assessed with<br />
Hess & Hunt score), <strong>the</strong>ir study was conducted on<br />
58 patients and <strong>the</strong>y concluded that ECG abnormalities<br />
are associated with more severe neurological<br />
injury [9].<br />
Contrary to our results <strong>the</strong> data published by<br />
Penka, et al, in 2005, who studied <strong>the</strong> correlation<br />
between ECG abnormalities in aneurysmal SAH<br />
patients and <strong>the</strong> degree <strong>of</strong> neurological impairment<br />
(assessed with Hess & Hunt score),<strong>the</strong>y concluded<br />
higher frequency <strong>of</strong> ECG changes (88.89%) in<br />
patients with lower grades <strong>of</strong> neurological impairement<br />
(patients with Hess & Hunt score 1&2)<br />
(p
Cardiac Affection after Subarachnoid Hemorrhage<br />
<strong>the</strong> incidence <strong>of</strong> systolic dysfunction (global &<br />
regional) in day 7 [p value=0.4].<br />
Similarly, Mayer, et al, in 1999, who studied<br />
left ventricular performance and its correlatin with<br />
neurological status in 72 patients with aneurysmal<br />
SAH, stated that RWMAs are more <strong>com</strong>mon in<br />
patients with poor neurological grades (p=0.002)<br />
[26].<br />
Kothavale, et al, in 2006, reported high prevelance<br />
<strong>of</strong> RWMAs in patients with high Hess &<br />
Hunt grades (3-5) (p=0.046) in <strong>the</strong> study conducted<br />
on three hundred patients with aneurysmal SAH,<br />
which goes in line with our results [27].<br />
Conclusions<br />
• Different types and frequencies <strong>of</strong> ECG changes<br />
were found in patients with SAH, most frequent<br />
were repolarization abnormalities, this supports<br />
<strong>the</strong> hypo<strong>the</strong>sis that neurogenic form <strong>of</strong> myocardial<br />
injury develops during and/or following SAH,<br />
more support <strong>com</strong>es from <strong>the</strong> observed elevation<br />
<strong>of</strong> cardiac troponin I and left ventricular systolic<br />
dysfunction.<br />
• The incidence <strong>of</strong> cardiac injury was positively<br />
correlated with <strong>the</strong> severity <strong>of</strong> SAH.<br />
• All <strong>the</strong>se findings were much less evident in <strong>the</strong><br />
traumatic SAH <strong>com</strong>pared with <strong>the</strong> aneurysmal<br />
SAH.<br />
• Cardiac injury and dysfunction following SAH<br />
is a potentially reversible phenomenon.<br />
References<br />
1- Kazzi AA, Ellis K: Subarachnoid Hemorrhage. eMedicine<br />
Journal 2001.<br />
2- Solenski NJ, Haley ECJ, Kassell NF et al: Medical <strong>com</strong>plications<br />
<strong>of</strong> aneurysmal subarachnoid hemorrhage: A<br />
report <strong>of</strong> <strong>the</strong> multicenter, cooperative aneurysm study.<br />
Participants <strong>of</strong> <strong>the</strong> Multicenter Cooperative Aneurysm<br />
Study. Crit Care Med 1995; 23: 1007-1017.<br />
3- Kantor HL, Krishnan SC: Cardiac problems in patients<br />
with neurologic disease. Cardiol Clin 1995; 13: 179-208.<br />
4- Davis TP, Alexander J, Lesch M, et al: Electrocardiographic<br />
changes associated with acute cerebrovascular disease:<br />
A clinical review. Prog Cardiovasc Dis 1993; 36: 245-<br />
260.<br />
5- Crago EA, Kerr ME, Kong Y et al: The impact <strong>of</strong> cardiac<br />
<strong>com</strong>plications on out<strong>com</strong>e in <strong>the</strong> SAH population. Acta<br />
Neurol Scand 2004; 110: 248-53.<br />
6- Hunt W, Hess R: "Surgical risk as related to time <strong>of</strong><br />
intervention in <strong>the</strong> repair <strong>of</strong> intracranial aneurysms".<br />
Journal <strong>of</strong> Neurosurgery 1968; 28 (1): 14-20. http://<br />
www.ncbi.nlm.nih.gov/pubmed/5635959<br />
16<br />
7- Penka A Atanassova, Maria P: Abnormal ECG patterns<br />
during <strong>the</strong> acute phase <strong>of</strong> subarachnoid hemorrhage in<br />
patients without previous heart disease CEJ Med 2006;<br />
1 (2): 148-157.<br />
8- Hravnak M, Crago EA, Frangiskakis JM, et al: Elevated<br />
Cardiac Troponin I and Relationship to Persistence <strong>of</strong><br />
Electrocardiographic and Echocardiographic Abnormalities<br />
After Aneurysmal Subarachnoid Hemorrhage. Stroke<br />
Nov. 2009.<br />
9- Zar<strong>of</strong>f JG, Rordorf GA, Newell JB, et al: Cardiac out<strong>com</strong>e<br />
in patients with subarachnoid hemorrhage and electrocardiographic<br />
abnormalities. Neurosurgery 1999; 44: 34-39.<br />
10- Naidech AM, Kurt T: Cardiac troponin elevation, cardiovascular<br />
morbidity, and out<strong>com</strong>e after subarachnoid<br />
hemorrhage. Circulaion 2005; 112 (18): 2851-6.<br />
11- Macfarlane PW, Lawrie TDV: Comprehensive Electro<strong>cardiology</strong>.<br />
Vol III. New York: Pergamon Press 1989; 1459.<br />
12- Macfarlane PW, Lawrie TDV: The normal electrocardiogram<br />
and vectorcardiogram. In: Macfarlane PW, Lawrie<br />
TDV, eds. Comprehensive Electro<strong>cardiology</strong>. Vol I. New<br />
York: Pergamon Press 1989; 451-452.<br />
13- Hodges M, Salemo D, Erlien D, et al: Bazett’s QT correction<br />
reviewed. Evidence that a linear QT correction for<br />
heart is better. J Am Coll Cardiol 1983; 1: 69.<br />
14- Nilesh Parekh, Bala Venkatesh: Cardiac troponin I predicts<br />
myocardial dysfunction in aneurysmal subarachnoid<br />
hemorrhage, J Am Coll Cardiol 2000; 36: 1328-1335.<br />
15- Sugimoto K, Watanabe E, Yamada A, et al: Prognostic<br />
implications <strong>of</strong> left ventricular wall motion abnormalities<br />
associated with subarachnoid hemorrhage. Int Heart J Jan<br />
2008; 49 (1): 75-85.<br />
16- Frontera JA, Parra A, Shimbo D, et al: Cardiac Arrhythmias<br />
after Subarachnoid Hemorrhage: Risk Factors and Impact<br />
on Out<strong>com</strong>e.Cerebrovasc Dis Jun 2008; 26 (1): 71-78.<br />
17- Sakr YL, Lim N, Amaral AC, et al: Relation <strong>of</strong> ECG<br />
changes to neurological out<strong>com</strong>e in patients with aneurysmal<br />
subarachnoid hemorrhage, Int J Cardiol 2004; 96<br />
(3): 369-73.<br />
18- Sakr YL, Ghosn I, Vincent JL, et al: Cardiac manifestations<br />
after subarachnoid hemorrhage: A systematic review <strong>of</strong><br />
<strong>the</strong> literature. Prog Cardiovasc Dis 2002; 45: 67.<br />
19- Xavier Wittebole MD, Philippe Hantson: Electrocardiographic<br />
changes after head trauma, Journal <strong>of</strong> Electro<strong>cardiology</strong><br />
2005; 38: 77-81.<br />
20- Hemant Bhagat, Rajiv Narang1, Deepak Sharma, et al:<br />
ST elevation - An indication <strong>of</strong> reversible neurogenic<br />
myocardial dysfunction in patients with head injury,<br />
Annals <strong>of</strong> Cardiac Anaes<strong>the</strong>sia Jul-Dec 2009; Vol. 12: 2.<br />
21- Sommargren CE, Zar<strong>of</strong>f JG, Banki N, et al: Electrocardiographic<br />
repolarization abnormalities in subarachnoid<br />
hemorrhage, J Electrocardiol 2002; 257-62.<br />
22- Tung P, Kopelnik A: Predictors <strong>of</strong> neurocardiogenic injury<br />
after subarachnoid hemorrhage. Stroke 2004; 35 (2): 548-<br />
51.
Rania El Hoseiny, et al<br />
23- Tanabe M, Crago EA, Suffoletto MS, et al: Relation <strong>of</strong><br />
elevation in cardiac troponin I to clinical severity, cardiac<br />
dysfunction, and pulmonary congestion in patients with<br />
subarachnoid hemorrhage. Am J Cardiol 2008; 1, 102<br />
(11): 1545-50.<br />
24- Ramappa P, Thatai D, Coplin W, et al: Cardiac Troponin-<br />
I: A Predictor <strong>of</strong> Prognosis in Subarachnoid Hemorrhage,<br />
Neurocrit Care Dec 2007; 18.<br />
25- Salim A, Hadjizacharia P, Brown C, et al: Significance<br />
<strong>of</strong> troponin elevation after severe traumatic brain injury,<br />
J Trauma Jan 2008; 64 (1): 46-52.<br />
26- Stephan A Mayer, MD, Julie Lin, MD: Myocardial Injury<br />
17<br />
and Left Ventricular performance After Subarachnoid<br />
Hemorrhage, Stroke 1999; 30: 780-786.<br />
27- Kothavale A, Banki NM, Kopelnik A, et al: Predictors <strong>of</strong><br />
left ventricular regional wall motion abnormalities after<br />
subarachnoid hemorrhage. Neurocrit Care 2006; 4 (3):<br />
199-205.<br />
28- Bahloul M, Chaari AN, Kallel H, et al: Neurogenic<br />
pulmonary edema due to traumatic brain injury: Evidence<br />
<strong>of</strong> cardiac dysfunction. Am J Crit Care 2006; 15: 462.<br />
29- Jeon IC, Chang CH, Choi BY, et al: Cardiac troponin I<br />
elevation in patients with aneurysmal subarachnoid hemorrhage,<br />
J Korean Neurosurg Soc 2009; 46 (2): 99-102.
Egypt Heart J 62 (1): 19-24, March 2010<br />
Endo<strong>the</strong>lial Dysfunction and Insulin Resistance in Normoglycemic<br />
Offsprings <strong>of</strong> Patients with Type 2 Diabetes Mellitus<br />
EMAN S MOHAMMAD, MD*; YASSER KAMEL, MD; HANNAN TAHA, MD**;<br />
ESSAM SAAD, MD; YASSER MAKRAM, MD***<br />
Background: Endo<strong>the</strong>lial dysfunction and insulin resistance are among <strong>the</strong> earliest detectable abnormalities in people at<br />
risk for a<strong>the</strong>rosclerosis. Similar genetic and environmental factors may contribute independently to both a<strong>the</strong>rosclerosis and<br />
type 2 diabetes mellitus. Whe<strong>the</strong>r family history for diabetes predispose to alteration in vascular function through an unknown<br />
''genetic susceptibility'' or through higher prevalence <strong>of</strong> insulin resistance has not yet been fully investigated.<br />
Objectives: To investigate endo<strong>the</strong>lial function in normotensive normoglycemic <strong>of</strong>fspring <strong>of</strong> diabetic subjects and to explore<br />
its relationship with <strong>the</strong> insulin resistance.<br />
Patients and Methods: We <strong>com</strong>pared normoglycemic <strong>of</strong>fspring <strong>of</strong> patients with type 2 diabetes mellitus (NOPD) (n=36)<br />
with matched healthy control subjects without family history <strong>of</strong> diabetes (n=21). Flow-mediated dilation (FMD) and nitroglycerinmediated<br />
dilation (GTN-MD) were assessed in brachial artery by colored Duplex ultrasound to evaluate endo<strong>the</strong>lium-dependent<br />
and independent vascular function. Homeostasis model assessment (HOMA) was performed to calculate insulin resistance.<br />
Results: FMD% was lower in NOPD than in control (7.31±2.73 Vs. 10.45±3.15, p
Endo<strong>the</strong>lial Dysfunction & Insulin Resistance in Normoglycemic Offsprings<br />
particularly in skeletal muscle [10]. Insulin stimulates<br />
bulk flow as an endo<strong>the</strong>lium-dependent vasodilator<br />
via nitric oxide production [11]. Impaired<br />
endo<strong>the</strong>lial function in type 2 diabetics is documented<br />
by reduced effect <strong>of</strong> endo<strong>the</strong>lial-dependent<br />
vasodilators such as acetylcholine (ACH) [12].<br />
Insulin resistance is defined as a state <strong>of</strong> reduced<br />
responsiveness to normal circulating levels <strong>of</strong><br />
insulin. This condition is a feature <strong>of</strong> various<br />
disorders, such as type 2 diabetes, is also implicated<br />
in impaired glucose tolerance (IGT) or impaired<br />
fasting glucose (IFG), both considered as ''prediabetes''<br />
by <strong>the</strong> Expert Committee on <strong>the</strong> Diagnosis<br />
and Classification <strong>of</strong> Diabetes Mellitus, as well as<br />
in obesity, hypertension, dyslipidaemia [13], <strong>the</strong><br />
possibility <strong>of</strong> existence <strong>of</strong> earlier in life metabolic<br />
effect in genetically predisposed persons as <strong>of</strong>fspring<br />
<strong>of</strong> type 2 diabetics was thought as ano<strong>the</strong>r<br />
face <strong>of</strong> <strong>the</strong> coin.<br />
Whe<strong>the</strong>r family history for diabetes predispose<br />
to alteration in vascular function through an unknown<br />
''genetic susceptibility'' or through higher<br />
prevalence <strong>of</strong> insulin resistance has not yet been<br />
fully investigated. The aim <strong>of</strong> <strong>the</strong> present study<br />
was to investigate endo<strong>the</strong>lial function in normotensive<br />
normoglycemic <strong>of</strong>fspring <strong>of</strong> diabetic subjects<br />
and to explore its relationship with <strong>the</strong> insulin<br />
resistance.<br />
Patients and Methods<br />
The study population consisted <strong>of</strong> 57 subjects:<br />
NOPD group: 36 healthy subjects, with one or<br />
both parents having type 2 diabetes mellitus.<br />
Control group: 21 healthy normotensive normoglycemic<br />
subjects with no family history <strong>of</strong><br />
type 2 diabetes mellitus.<br />
Exclusion criteria: Tobacco smoking, history<br />
or clinical evidence <strong>of</strong> cardiac diseases or systemic<br />
diseases, obesity [body mass index (BMI) ≥30kg/<br />
m 2 and/or Waist-to-hip ratio (WHR) >0.9m in<br />
males and >0.85m in females], hypertension, diabetes,<br />
or dyslipidemia. All women were premenopausal<br />
and <strong>the</strong>ir investigations were undertaken<br />
during <strong>the</strong> first week <strong>of</strong> <strong>the</strong>ir menstrual cycles.<br />
None <strong>of</strong> <strong>the</strong>m were taking oral contraceptives.<br />
Anthropometric, metabolic characteristics and<br />
laboratory measurements:<br />
Height, weight and waist circumference were<br />
determined for all participants. BMI was determined<br />
as body weight (kg)/height (m) 2. Total and<br />
20<br />
HDL cholesterol, triglycerides and routine chemistry<br />
were measured by standard laboratory techniques.<br />
Oral glucose tolerance test (OGTT):<br />
A standard OGTT was done after an overnight<br />
10- to 12-h fast. Blood samples were obtained<br />
before and 2h after 75g <strong>of</strong> glucose administration.<br />
Homeostasis model assessment (HOMA):<br />
Serum insulin was determined by an electrochemiluminescense<br />
assay. Insulin resistance [14]<br />
was calculated as follows:<br />
HOMA-IR=fasting glucose (mmol/L) x insulin (mIu/mL)<br />
––––––––––––––––––––––––––––––––––––––––––––––––<br />
22.5<br />
Endo<strong>the</strong>lial function:<br />
Endo<strong>the</strong>lial function was measured 1h before<br />
<strong>the</strong> OGTT was started. All studies were performed<br />
in <strong>the</strong> morning in a quiet room. Brachial artery<br />
reactivity was measured by colored Doppler ultrasound,<br />
using a 7.5MHz linear array transducer<br />
ultrasound system. The mean right brachial artery<br />
antero-posterior diameter was measured 3-5cm<br />
above <strong>the</strong> elbow, between media and adventitia<br />
from 4 cycles synchronized with <strong>the</strong> end-diastole<br />
at <strong>the</strong> R wave peaks [15]. The ECG was monitored<br />
continuously throughout <strong>the</strong> study.<br />
• A basic scan <strong>of</strong> <strong>the</strong> brachial artery diameter and<br />
flow was taken.<br />
• 2 nd scan was taken after applying a pneumatic<br />
tourniquet <strong>of</strong> 250-300mmHg. (Using mercurial<br />
sphygmomanometer) for about 5 minutes. The<br />
scan was taken to measure brachial artery diameter,<br />
60 seconds after releasing <strong>the</strong> tourniquet<br />
measuring <strong>the</strong> maximum FMD (index <strong>of</strong> endo<strong>the</strong>lium-dependent<br />
vasodilation).<br />
• 3 rd scan was taken after 15 minutes <strong>of</strong> rest to<br />
allow recovery <strong>of</strong> <strong>the</strong> artery after FMD and considered<br />
<strong>the</strong> basic scan <strong>of</strong> GTN-MD reading.<br />
• 4 th scan was taken 4 minutes after administration<br />
<strong>of</strong> 400mg <strong>of</strong> GTN spray sublingually to assess<br />
non-endo<strong>the</strong>lium dependent dilation. GTN serves<br />
as an exogenous source <strong>of</strong> Nitric Oxide (NO),<br />
bypassing <strong>the</strong> need for endogenous endo<strong>the</strong>lial<br />
NO production.<br />
o FMD percentage was calculated by <strong>the</strong> following<br />
equation:<br />
2 nd scan – 1 st scan<br />
FMD% = ––––––––––––––––– x 100<br />
1 st scan
Eman S Mohammad, et al<br />
o GTN-MD percentage was calculated by <strong>the</strong><br />
following equation:<br />
4 th scan – 3 rd scan<br />
GTN – MD% = ––––––––––––––––– x 100<br />
3 rd scan<br />
o Dilatation ratio was calculated by <strong>the</strong> following<br />
equation:<br />
FMD%<br />
DilRatio = –––––––––––––<br />
GTN – MD%<br />
Results<br />
The study included 57 subjects; 36 NOPD and<br />
21 controls. Table (1) shows <strong>the</strong> demographic and<br />
Table 1: Demographic and metabolic data for NOPD and<br />
controls.<br />
Gender:<br />
Male<br />
Female<br />
Age<br />
BMI<br />
WHR:<br />
Male<br />
Female<br />
Fasting Insulin<br />
Fasting Glucose<br />
HOMA-IR<br />
NOPD (n=36) Controls (n=21)<br />
Number<br />
10<br />
26<br />
Mean<br />
25.83<br />
23.98<br />
0.84<br />
0.78<br />
9.478<br />
5.02<br />
2.11<br />
%<br />
27.8<br />
72.2<br />
SD<br />
6.38<br />
2.95<br />
0.08<br />
0.07<br />
2.63<br />
0.59<br />
0.63<br />
Number<br />
6<br />
15<br />
Mean<br />
25.33<br />
22.89<br />
0.79<br />
0.82<br />
8.68<br />
4.76<br />
1.65<br />
%<br />
28.6<br />
71.4<br />
SD<br />
6.28<br />
2.71<br />
0.05<br />
0.03<br />
2.15<br />
0.67<br />
0.615<br />
p value<br />
0.759<br />
p value<br />
0.762<br />
0.160<br />
0.057<br />
0.06<br />
0.222<br />
0.194<br />
0.013<br />
Abbreviations:<br />
BMI : Body mass index.<br />
WHR: Waist to hip ratio.<br />
HOMA-IR: Homeostasis model assessment-Insulin resistance.<br />
25<br />
20<br />
15<br />
10<br />
5<br />
0<br />
p=0.24<br />
GTN% FMD%<br />
Endo<strong>the</strong>lial Dysfunction & Insulin Resistance in Normoglycemic Offsprings<br />
2.5<br />
2<br />
1.5<br />
1<br />
0.5<br />
0<br />
HOMA-IR<br />
HOMA-IR<br />
p=0.013<br />
Control NOPD<br />
Figure 3: HOMA-IR in NOPD and Controls.<br />
Discussion<br />
The present study showed that: (a) normotensive<br />
normoglycemic <strong>of</strong>fsprings <strong>of</strong> type 2 diabetic subjects<br />
present insulin resistance and early endo<strong>the</strong>lial<br />
dysfunction, as <strong>the</strong>y had impaired FMD, while <strong>the</strong><br />
direct vasodilator capacity induced by GTN was<br />
not impaired. (b) FMD was impaired more in<br />
<strong>of</strong>fsprings <strong>of</strong> diabetics with more insulin resistance.<br />
Our findings are in agreement with Caballero<br />
et al [16] who showed decreased FMD and decreased<br />
microvascular reactivity in first degree<br />
relatives <strong>of</strong> type 2 diabetic subjects as <strong>com</strong>pared<br />
to controls.<br />
Balletsh<strong>of</strong>er et al [17] found impaired FMD in<br />
normoglycemic <strong>of</strong>fspring <strong>of</strong> diabetic parents, but<br />
this was significant only in insulin resistant normoglycemic<br />
<strong>of</strong>fspring <strong>of</strong> diabetic parents <strong>com</strong>pared<br />
to controls. There was no significant difference in<br />
GTN-MD between all <strong>the</strong> studied groups. Of note,<br />
that study included only 10 control subjects to<br />
<strong>com</strong>pare with 53 subjects with diabetic parents<br />
and smokers were not excluded from study. This<br />
may attenuate <strong>the</strong> difference between <strong>of</strong>fspring <strong>of</strong><br />
diabetic parents and controls as regard FMD.<br />
Fur<strong>the</strong>rmore, Chen et al [18], McSorley et al<br />
[19] and Iellamo et al [20] found a significantly<br />
reduced forearm vasodilation, indicating endo<strong>the</strong>lial<br />
dysfunction in normoglycemic first degree relatives<br />
<strong>of</strong> type 2 diabetic subjects. However, McSorley et<br />
al [19] did not find significant difference in HOMA-<br />
IR, an index <strong>of</strong> insulin resistance, between NOPD<br />
and controls, none<strong>the</strong>less, several findings from<br />
that study suggested <strong>the</strong> presence <strong>of</strong> hyperinsulinemic<br />
state in <strong>the</strong> NOPD group. These include higher<br />
22<br />
values <strong>of</strong> HbA1c and higher values for blood glucose<br />
120 minutes after OGTT con<strong>com</strong>itant with<br />
higher insulin levels, reflecting a relative hyperinsulinemic<br />
state. In addition, <strong>the</strong> area under glucose<br />
curve (AUCs) for glucose and insulin during OGTT<br />
were inversely correlated with FMD.<br />
Goldfine et al [21] found that FMD was reduced<br />
in normoglycemic <strong>of</strong>fsprings <strong>of</strong> type 2 diabetic<br />
subjects (even <strong>the</strong> most insulin-sensitive), with no<br />
difference in GTN-MD. This significant attenuation<br />
<strong>of</strong> endo<strong>the</strong>lial dysfunction even in insulin sensitive<br />
<strong>of</strong>fsprings could be due to enriched familiar difference<br />
in that study as both parents were diabetic.<br />
Moreover, <strong>the</strong> studied subjects had non significantly<br />
higher BMI <strong>com</strong>pared to our subjects (23.98±2.95<br />
Vs 22.89±2.71).<br />
Tesauro et al [22] found that normoglycemic<br />
<strong>of</strong>fsprings <strong>of</strong> type 2 diabetic subjects were more<br />
insulin resistant on average than <strong>the</strong> control group,<br />
and had significantly lower both FMD and GTN-<br />
MD <strong>com</strong>pared with <strong>the</strong> control group. They suggested<br />
that in addition to decreased insulin sensitivity;<br />
o<strong>the</strong>rwise healthy subjects with a family<br />
history <strong>of</strong> type 2 diabetes mellitus have impairment<br />
in vascular responsiveness to NO that may be<br />
endo<strong>the</strong>lium dependent and/or independent.<br />
In concordance <strong>of</strong> our results, Amudha et al<br />
[23] found that NOPD had significantly impaired<br />
FMD and higher HOMA-IR, reflecting endo<strong>the</strong>lial<br />
dysfunction and insulin resistance.<br />
Frequent presence <strong>of</strong> vascular pathology at <strong>the</strong><br />
time <strong>of</strong> diagnosis <strong>of</strong> diabetes suggests importance<br />
for identification <strong>of</strong> prediabetic persons with diminished<br />
endo<strong>the</strong>lial function and early a<strong>the</strong>rosclerotic<br />
disease and family history <strong>of</strong> diabetes is a<br />
recognized risk for development <strong>of</strong> diabetes [21].<br />
In normoglycemic <strong>of</strong>fspring <strong>of</strong> patients with<br />
type 2 diabetes mellitus, significant endo<strong>the</strong>lial<br />
dysfunction and insulin resistance are detectable<br />
even in <strong>the</strong> absence <strong>of</strong> frank diabetes. This suggests<br />
that genetic factors contributing to insulin resistance<br />
and diabetes may also influence development <strong>of</strong><br />
cardiovascular diseases including a<strong>the</strong>rosclerosis<br />
and coronary heart disease that are related to endo<strong>the</strong>lial<br />
dysfunction [22].<br />
From data <strong>of</strong> our study and o<strong>the</strong>r studies, we<br />
can speculate that NOPD present a blunted endo<strong>the</strong>lial<br />
function in relation to a primary inherited<br />
genetic susceptibility yet to be identified, or in<br />
relation to <strong>the</strong> metabolic alteration detectable even
Eman S Mohammad, et al<br />
in normotensive and normoglycemic subjects.<br />
Certainly, <strong>the</strong> blunted endo<strong>the</strong>lial function observed<br />
in NOPD subjects may also be related to glycemic<br />
burden, even in <strong>the</strong> nondiabetic range, given that<br />
hyperglycemia has been shown to decrease NO<br />
bioavailability through activation <strong>of</strong> PKC (protein<br />
kinase C) via diacylglycerol, increased hexosamine<br />
pathway flux, increased advanced glycation end<br />
product formation, increased oxidative stress and<br />
increased polyol pathway flux [24,25]. It has been<br />
found that fasting hyperglycemia diminishes microvascular<br />
hyperemia and inversely correlates<br />
with endo<strong>the</strong>lial dependant vasodilataion [26].<br />
Indeed, our NOPD subjects had still normal but<br />
already higher glycemia as <strong>com</strong>pared to controls.<br />
In addition, reciprocal relationships between<br />
insulin resistance and endo<strong>the</strong>lial dysfunction may<br />
be secondary to impaired activation <strong>of</strong> endo<strong>the</strong>lial<br />
signalling pathways in <strong>the</strong> context <strong>of</strong> inherited<br />
insulin resistance [27]. It has been found that genetic<br />
mutations <strong>of</strong> insulin receptor genes and alteration<br />
<strong>of</strong> insulin signal transduction could contribute to<br />
<strong>the</strong> impairment <strong>of</strong> insulin secretory pr<strong>of</strong>ile and<br />
insulin resistance [28].<br />
Thus <strong>the</strong> endo<strong>the</strong>lial dysfunction and insulin<br />
resistance we found are inherited conditions, transmitted<br />
from <strong>the</strong> diabetic parents in whom endo<strong>the</strong>lial<br />
dysfunction and insulin resistance were previously<br />
proved [29,30].<br />
Conclusions<br />
We demonstrate that nondiabetic <strong>of</strong>fspring <strong>of</strong><br />
diabetic parents have impaired endo<strong>the</strong>lial dependant<br />
vasodilatation as well as insulin resistance.<br />
These data suggest bioavailability <strong>of</strong> nitric oxide<br />
is lower in <strong>of</strong>fspring <strong>of</strong> diabetic subjects and may<br />
contribute to cardiovascular risk in advance <strong>of</strong><br />
development <strong>of</strong> overt diabetes. Modest hyperglycemia,<br />
even within <strong>the</strong> normative range and insulin<br />
resistance may contribute to attenuated endo<strong>the</strong>lial<br />
function. Finally, as endo<strong>the</strong>lial dysfunction is<br />
present in nondiabetic <strong>of</strong>fspring <strong>of</strong> diabetic parents,<br />
strong family history <strong>of</strong> type 2 diabetes mellitus<br />
could be considered an additional cardiac risk<br />
factor.<br />
These results may have important implications<br />
for identifying populations that can derive substantial<br />
benefits from early lifestyle interventions<br />
including diet and exercise that are known to<br />
improve endo<strong>the</strong>lial function, increase insulin<br />
sensitivity and lower circulating markers <strong>of</strong> inflammation.<br />
23<br />
References<br />
1- Kannel WB, McGee DL: Diabetes and cardiovascular<br />
disease. The Framingham study. Jama 1979; 241: 2035-<br />
2038.<br />
2- Kawamori R, Yamasaki Y, Matsushima H, Nishizawa H,<br />
Nao K, Hougaku H, Maeda H, Handa N, Matsumoto M,<br />
Kamada T: Prevalence <strong>of</strong> carotid a<strong>the</strong>rosclerosis in diabetic<br />
patients. Ultrasound high-resolution B-mode imaging on<br />
carotid arteries. Diabetes Care 1992; 15: 1290-1294.<br />
3- Uusitupa M, Niskanen L, Siitonen O, Pyorala K: Hyperinsulinemia<br />
and hypertension in patients with newly<br />
diagnosed non-insulin-dependent diabetes. Diabete Metab<br />
1987; 13: 369-374.<br />
4- Ruotsalainen E, Vauhkonen I, Salmenniemi U, Pihlajamaki<br />
J, Punnonen K, Kainulainen S, Jalkanen S, Salmi M,<br />
Laakso M: Markers <strong>of</strong> endo<strong>the</strong>lial dysfunction and lowgrade<br />
inflammation are associated in <strong>the</strong> <strong>of</strong>fspring <strong>of</strong> type<br />
2 diabetic subjects. A<strong>the</strong>rosclerosis 2008; 197: 271-277.<br />
5- Blaschke F, Takata Y, Caglayan E, Law RE, Hsueh WA:<br />
Obesity, peroxisome proliferator-activated receptor and<br />
a<strong>the</strong>rosclerosis in type 2 diabetes. Arterioscler Thromb<br />
Vasc Biol 2006; 26: 28-40.<br />
6- Luscher TF: 1993 Mack Forster Award Lecture. Review.<br />
The endo<strong>the</strong>lium as a target and mediator <strong>of</strong> cardiovascular<br />
disease. Eur J Clin Invest 1993; 23: 670-685.<br />
7- Corretti MC, Anderson TJ, Benjamin EJ, Celermajer D,<br />
Charbonneau F, Creager MA, Deanfield J, Drexler H,<br />
Gerhard-Herman M, Herrington D, Vallance P, Vita J,<br />
Vogel R: Guidelines for <strong>the</strong> ultrasound assessment <strong>of</strong><br />
endo<strong>the</strong>lial-dependent flow-mediated vasodilation <strong>of</strong> <strong>the</strong><br />
brachial artery: A report <strong>of</strong> <strong>the</strong> International Brachial<br />
Artery Reactivity Task Force. J Am Coll Cardiol 2002;<br />
39: 257-265.<br />
8- Ross R: The pathogenesis <strong>of</strong> a<strong>the</strong>rosclerosis: A perspective<br />
for <strong>the</strong> 1990s. Nature 1993; 362: 801-809.<br />
9- Eskurza I, Seals DR, DeSouza CA, Tanaka H: Pharmacologic<br />
versus flow-mediated assessments <strong>of</strong> peripheral<br />
vascular endo<strong>the</strong>lial vasodilatory function in humans. Am<br />
J Cardiol 2001; 88: 1067-1069.<br />
10- Newman JM, Ross RM, Richards SM, Clark MG, Rattigan<br />
S: Insulin and contraction increase nutritive blood flow<br />
in rat muscle in vivo determined by microdialysis <strong>of</strong> L-<br />
[14C] glucose. J Physiol 2007; 585: 217-229.<br />
11- Scherrer U, Randin D, Vollenweider P, Vollenweider L,<br />
Nicod P: Nitric oxide release accounts for insulin's vascular<br />
effects in humans. J Clin Invest 1994; 94: 2511-2515.<br />
12- Rask-Madsen C, Ihlemann N, Krarup T, Christiansen E,<br />
Kober L, Nervil Kistorp C, Torp-Pedersen C: Insulin<br />
<strong>the</strong>rapy improves insulin-stimulated endo<strong>the</strong>lial function<br />
in patients with type 2 diabetes and ischemic heart disease.<br />
Diabetes 2001; 50: 2611-2618.<br />
13- Report <strong>of</strong> <strong>the</strong> expert <strong>com</strong>mittee on <strong>the</strong> diagnosis and<br />
classification <strong>of</strong> diabetes mellitus. Diabetes Care 2003;<br />
26 (Suppl 1): S5-20.<br />
14- Bonora E, Targher G, Alberiche M, Bonadonna RC,<br />
Saggiani F, Zenere MB, Monauni T, Muggeo M: Homeo-
Endo<strong>the</strong>lial Dysfunction & Insulin Resistance in Normoglycemic Offsprings<br />
stasis model assessment closely mirrors <strong>the</strong> glucose clamp<br />
technique in <strong>the</strong> assessment <strong>of</strong> insulin sensitivity: Studies<br />
in subjects with various degrees <strong>of</strong> glucose tolerance and<br />
insulin sensitivity. Diabetes Care 2000; 23: 57-63.<br />
15.- Hashimoto M, Miyamoto Y, Matsuda Y, Akita H: New<br />
methods to evaluate endo<strong>the</strong>lial function: Non-invasive<br />
method <strong>of</strong> evaluating endo<strong>the</strong>lial function in humans. J<br />
Pharmacol Sci 2003; 93: 405-408.<br />
16- Caballero AE, Arora S, Saouaf R, Lim SC, Smakowski<br />
P, Park JY, King GL, LoGerfo FW, Horton ES, Veves A:<br />
Microvascular and macrovascular reactivity is reduced<br />
in subjects at risk for type 2 diabetes. Diabetes 1999; 48:<br />
1856-1862.<br />
17- Balletsh<strong>of</strong>er BM, Rittig K, Enderle MD, Volk A, Maerker<br />
E, Jacob S, Matthaei S, Rett K, Haring HU: Endo<strong>the</strong>lial<br />
dysfunction is detectable in young normotensive firstdegree<br />
relatives <strong>of</strong> subjects with type 2 diabetes in association<br />
with insulin resistance. Circulation 2000; 101:<br />
1780-1784.<br />
18- Chen SC, Song GY, Wang SJ, Ye W, Ma BQ: [A study on<br />
endo<strong>the</strong>lial function and inflammation factors in <strong>the</strong> first<br />
degree relatives <strong>of</strong> type 2 diabetics with normal glucose<br />
tolerance]. Zhonghua Nei Ke Za Zhi 2005; 44: 165-168.<br />
19- McSorley PT, Bell PM, Young IS, Atkinson AB, Sheridan<br />
B, Fee JP, McCance DR: Endo<strong>the</strong>lial function, insulin<br />
action and cardiovascular risk factors in young healthy<br />
adult <strong>of</strong>fspring <strong>of</strong> parents with Type 2 diabetes: effect <strong>of</strong><br />
vitamin E in a randomized double-blind, controlled clinical<br />
trial. Diabet Med 2005; 22: 703-710.<br />
20- Iellamo F, Tesauro M, Rizza S, Aquilani S, Cardillo C,<br />
Iantorno M, Turriziani M, Lauro R: Con<strong>com</strong>itant impairment<br />
in endo<strong>the</strong>lial function and neural cardiovascular<br />
regulation in <strong>of</strong>fspring <strong>of</strong> type 2 diabetic subjects. Hypertension<br />
2006; 48: 418-423.<br />
21- Goldfine AB, Beckman JA, Betensky RA, Devlin H,<br />
Hurley S, Varo N, Schonbeck U, Patti ME, Creager MA:<br />
Family history <strong>of</strong> diabetes is a major determinant <strong>of</strong><br />
endo<strong>the</strong>lial function. J Am Coll Cardiol 2006; 47: 2456-<br />
2461.<br />
24<br />
22- Tesauro M, Rizza S, Iantorno M, Campia U, Cardillo C,<br />
Lauro D, Leo R, Turriziani M, Cocciolillo GC, Fusco A,<br />
Panza JA, Scuteri A, Federici M, Lauro R, Quon MJ:<br />
Vascular, metabolic and inflammatory abnormalities in<br />
normoglycemic <strong>of</strong>fspring <strong>of</strong> patients with type 2 diabetes<br />
mellitus. Metabolism 2007; 56: 413-419.<br />
23- Amudha K, Choy AM, Mustafa MR, Lang CC: Shortterm<br />
effect <strong>of</strong> atorvastatin on endo<strong>the</strong>lial function in<br />
healthy <strong>of</strong>fspring <strong>of</strong> parents with type 2 diabetes mellitus.<br />
Cardiovasc Ther 2008; 26: 253-261.<br />
24- Matsuoka H: Endo<strong>the</strong>lial dysfunction associated with<br />
oxidative stress in human. Diabetes Res Clin Pract 2001;<br />
54 (Suppl 2): S65-72.<br />
25- Zou MH, Shi C, Cohen RA: Oxidation <strong>of</strong> <strong>the</strong> zinc-thiolate<br />
<strong>com</strong>plex and uncoupling <strong>of</strong> endo<strong>the</strong>lial nitric oxide synthase<br />
by peroxynitrite. J Clin Invest 2002; 109: 817-826.<br />
26- Vita JA, Keaney JF, Jr., Larson MG, Keyes MJ, Massaro<br />
JM, Lipinska I, Lehman BT, Fan S, Osypiuk E, Wilson<br />
PW, Vasan RS, Mitchell GF, Benjamin EJ: Brachial artery<br />
vasodilator function and systemic inflammation in <strong>the</strong><br />
Framingham Offspring Study. Circulation 2004; 110:<br />
3604-3609.<br />
27- McEleavy OD, McCallum RW, Petrie JR, Small M, Connell<br />
JM, Sattar N, Cleland SJ: Higher carotid-radial pulse<br />
wave velocity in healthy <strong>of</strong>fspring <strong>of</strong> patients with Type<br />
2 diabetes. Diabet Med 2004; 21: 262-266.<br />
28- Montecucco F, Steffens S, Mach F: Insulin resistance: A<br />
proinflammatory state mediated by lipid-induced signaling<br />
dysfunction and involved in a<strong>the</strong>rosclerotic plaque instability.<br />
Mediators Inflamm 2008; 2008: 767623.<br />
29- Yu Y, Suo L, Yu H, Wang C, Tang H: Insulin resistance<br />
and endo<strong>the</strong>lial dysfunction in type 2 diabetes patients<br />
with or without microalbuminuria. Diabetes Res Clin<br />
Pract 2004; 65: 95-104.<br />
30- Nielsen MF, Nyholm B, Caumo A, Chandramouli V,<br />
Schumann WC, Cobelli C, Landau BR, Rizza RA, Schmitz<br />
O: Prandial glucose effectiveness and fasting gluconeogenesis<br />
in insulin-resistant first-degree relatives <strong>of</strong> patients<br />
with type 2 diabetes. Diabetes 2000; 49: 2135-2141.
Egypt Heart J 62 (1): 25-37, March 2010<br />
Comparative Study between Tissue Doppler Imaging and Radionuclide<br />
Scintigraphy in Evaluation <strong>of</strong> Right Ventricular Function in Patients<br />
with Chronic Obstructive Pulmonary Disease<br />
SHERINE ELGANGIHI, MD; RANDA ALY, MD; SALLY SALAH; AMR ELHADIDY, MD*<br />
Background: Cor-pulmonale <strong>com</strong>plicates 2-6/1000 <strong>of</strong> patients with chronic obstructive pulmonary disease (COPD). The<br />
early diagnosis <strong>of</strong> RV dysfunction 2 nd ry to pulmonary hypertension can reduce morbidity and mortality.<br />
Purpose: The objective <strong>of</strong> our study is to assess <strong>the</strong> usefulness <strong>of</strong> tissue Doppler imaging (TDI) in evaluation <strong>of</strong> RV function<br />
in patients with COPD in <strong>com</strong>parison <strong>of</strong> first pass radionuclide angiography (FPRNA) which is <strong>the</strong> gold standard method.<br />
Ano<strong>the</strong>r aim is to determine <strong>the</strong> relationship between lateral tricuspid annulus TDI parameters and PASP as estimated by<br />
continuous wave Doppler in patients with COPD.<br />
Methods: Thirty patients with COPD diagnosed by history, clinical examination, CXR, laboratory findings (ABG, CBC),<br />
12-lead ECG, TDI (to measure MPI, Sm, SmVTI, Em/Am), FPRNA (to measure RV EF).<br />
Results: Based on <strong>the</strong> nuclear study (FPRNA) our 30 pts divided to 17pts (56.7%) with RVEF >45% (55.2±1.4) and 13<br />
pts (43.3%) with RVEF
Comparative Study between Tissue Doppler Imaging & Radionuclide Scintigraphy<br />
ventricular after load and eventually lead to clinical<br />
syndrome <strong>of</strong> right heart failure with systemic<br />
congestion [3].<br />
Two dimensional echocardiography is not feasible<br />
in assessment <strong>of</strong> right ventricular (RV) function.<br />
In addition two dimensional echocardiography<br />
doesn't provide homodynamic information about<br />
right ventricular filling pressures, which can be<br />
derived from Doppler echocardiography studies<br />
[4].<br />
Tissue Doppler imaging TDI is an extension <strong>of</strong><br />
conventional Doppler flow echocardiography &<br />
has been proven to be useful & feasible clinical<br />
tool for assessing systolic & diastolic function<br />
since its introduction in early 1990s [5,6]. Also, it<br />
recently has emerged as a new method useful for<br />
predicting right atrial pressure and evaluation <strong>of</strong><br />
right ventricular systolic and diastolic function<br />
[7,8,9].<br />
Radionuclide ventriculography (RNV) is considered<br />
<strong>the</strong> gold standard for estimating <strong>the</strong> right<br />
ventricular ejection fraction (RVEF). Abnormal<br />
RV function in patients with COPD has been demonstrated<br />
by both first-pass & gated blood pool<br />
scanning [10].<br />
Aim <strong>of</strong> <strong>the</strong> work:<br />
to assess <strong>the</strong> usefulness <strong>of</strong> tissue Doppler imaging<br />
TDI in evaluation <strong>of</strong> RV function in patients<br />
with chronic obstructive pulmonary disease in<br />
<strong>com</strong>parison to first pass radionuclide angiography<br />
FPRNA which is <strong>the</strong> gold standard method.<br />
To describe <strong>the</strong> gastric mucosal morphologic<br />
abnormalities occurring in <strong>the</strong> septic settings, and<br />
whe<strong>the</strong>r or not, <strong>the</strong>se findings correlate with <strong>the</strong><br />
clinical course, prognosis and mortality <strong>of</strong> septic<br />
patients.<br />
Patients and Methods<br />
Patients: We prospectively enrolled Thirty<br />
patients (25 males, 5 females mean age 60.8±10.5<br />
yrs) were included in <strong>the</strong> study, admitted to Critical<br />
care department, Cairo university hospitals; from<br />
July 2007 to March 2009.<br />
Inclusion criteria: Any patient presented with<br />
COPD diagnosed by history, physical examination,<br />
laboratory analysis and imaging.<br />
Exclusion criteria: Rt. Ventricular infarction,<br />
Cardiomyopathies, Rheumatic heart diseases, Pri-<br />
26<br />
mary Pulmonary hypertension, Congenital heart<br />
disease, Pregnancy, Paced heart and Pulmonary<br />
embolism.<br />
Evaluation <strong>of</strong> Patients: All included patients were<br />
subjected to <strong>the</strong> following:<br />
1- Full clinical evaluation: Including history<br />
tacking including smoking index, physical examination<br />
and standard 12-leads electrocardiogram.<br />
2- Laboratory investigations: Including Arterial<br />
blood gases, Complete blood count (CBC) and<br />
O<strong>the</strong>r routine labs.<br />
Laboratory results indicative for <strong>the</strong> diagnosis <strong>of</strong><br />
COPD:<br />
• Secondary polycya<strong>the</strong>mia due to chronic hypoxemia.<br />
• Hematocrite <strong>of</strong> more than 52% in males and more<br />
than 47% in female indicates disease.<br />
• ABG on admission: Chronic hypoxia, hypercapnia<br />
& high level <strong>of</strong> HCO 3 as a <strong>com</strong>pensatory.<br />
• PCO 2 >45mmHg.<br />
• Hypoxia PaO 2 27mg/dl.<br />
3- Imaging studies:<br />
a- Chest radiograph: PA X-ray reveal signs <strong>of</strong><br />
hyperinflation, including a flattening <strong>of</strong> <strong>the</strong><br />
diaphragm, increased retrosternal air space, and<br />
a long narrow heart shadow. Hyperlucency <strong>of</strong><br />
<strong>the</strong> lungs are signs <strong>of</strong> emphysema.<br />
b- Echocardiographic examination: All patients<br />
underwent echocardiographic examination, including<br />
<strong>the</strong> routine transthoracic and tissue<br />
Doppler study. Each patient was examined in<br />
<strong>the</strong> left lateral decubitus position according to<br />
<strong>the</strong> re<strong>com</strong>mendations <strong>of</strong> <strong>the</strong> American Society<br />
<strong>of</strong> Echocardiography. The study was conducted<br />
using an ATL HDI 5000 colored echocardiographic<br />
machine with TDI s<strong>of</strong>tware incorporated<br />
in <strong>the</strong> device using a 3.5MHz. transducer.<br />
i- Routine echocardiographic study including<br />
LVEDD, VESD, EF and right ventricular<br />
dimensions to exclude cardiac myopathies<br />
and to give an idea about right ventricular<br />
size.<br />
ii- Tissue Doppler study: Tissue Doppler Imaging<br />
(TDI) was done in <strong>the</strong> pulsed modality<br />
from <strong>the</strong> apical 4 chamber view placing <strong>the</strong>
Sherine Elgangihi, et al<br />
sample volume <strong>of</strong> <strong>the</strong> Doppler cursor at <strong>the</strong><br />
lateral tricuspid annulus to determine <strong>the</strong><br />
following parameters (in a pt. with HR 70<br />
bpm):<br />
Isovolumic contraction time (IVCT): Measured<br />
in (msec) by Pulsed-Doppler from <strong>the</strong> end <strong>of</strong> A<br />
wave to <strong>the</strong> beginning <strong>of</strong> systolic wave (N: 50ms).<br />
Isovolumic relaxation time (IVRT): Measured<br />
in (msec) by Pulsed-Doppler from <strong>the</strong> end <strong>of</strong> systolic<br />
wave to <strong>the</strong> beginning <strong>of</strong> E wave (N: 60ms).<br />
Ejection time (ET): Measured in (msec) by<br />
Pulsed-Doppler as <strong>the</strong> period <strong>of</strong> aortic or pulmonary<br />
valve opening or <strong>the</strong> time <strong>of</strong> peak myocardial<br />
systolic velocity (N: 250ms).<br />
Myocardial performance index (MPI): Calculated<br />
by <strong>the</strong> following equation:<br />
IVRT + IVCT<br />
MPI = –––––––––––––– (N: 0.39)<br />
ET<br />
Peak myocardial systolic velocity (Sm): Measured<br />
in Cm/s by drawing a perpendicular line<br />
from <strong>the</strong> summit <strong>of</strong> <strong>the</strong> wave to <strong>the</strong> baseline (N:<br />
12-17cm/s).<br />
Velocity time integral (Sm VTI): It is area measured<br />
under <strong>the</strong> Doppler velocity envelope for<br />
systolic wave measured by tissue Doppler (N<br />
>2.7cm).<br />
Early diastolic wave (E): Corresponding rapid<br />
filling phase, measured in Cm/s by drawing a<br />
perpendicular line from baseline to summit <strong>of</strong><br />
wave.<br />
Late diastolic wave (Am): Corresponding to<br />
atrial contraction, measured in Cm/s by drawing<br />
a perpendicular line from baseline to summit <strong>of</strong><br />
wave.<br />
iii- Nuclear imaging: Myocardial nuclear imaging<br />
was done following stabilization <strong>of</strong> <strong>the</strong><br />
patient's medical condition.<br />
First pass radionuclide angiography (FPR-<br />
NA): First pass technique was used to assess <strong>the</strong><br />
RV ejection fraction by injecting 25-30mCi Tc-<br />
99m Sestamibi intravenously. Intravenous access<br />
should be obtained using a large-bore indwelling<br />
polyethylene ca<strong>the</strong>ter, ei<strong>the</strong>r a 18-or 20-gauge<br />
ca<strong>the</strong>ter in an external jugular vein or a 14- or 16-<br />
27<br />
gauge in a medial antecubital vein. The ca<strong>the</strong>ter<br />
should be connected to a saline-loaded 30 to 35ml<br />
syringe using tubing that has a 3 to 5ml capacity<br />
and a three-way stopcock. The tracer is <strong>the</strong>n loaded<br />
into <strong>the</strong> tubing and subsequently forced through<br />
this system using maximal hand pressure on <strong>the</strong><br />
syringe after starting <strong>the</strong> acquisition. The images<br />
are acquired in anterior view, (<strong>the</strong> acquisition<br />
duration should be set for at least 30 seconds in<br />
order to allow for <strong>com</strong>plete transition through <strong>the</strong><br />
central circulation <strong>the</strong>n processed and analyzed<br />
using <strong>the</strong> frame method for RV, which creates a<br />
representative ventricular volumes cycles by summing<br />
frames <strong>of</strong> several (usually 2 or 4 for RV)<br />
cardiac cycles, aligned by matching <strong>the</strong>ir ED to<br />
get <strong>the</strong> RV by semi-automated method.<br />
The statistics:<br />
• Data were collected on special format, verified<br />
and <strong>the</strong>n coded when needed prior to analysis.<br />
• All continuous data were expressed as mean ±<br />
SD, categorical data were expressed as frequency<br />
in tables.<br />
• Chi-square test and kappa for assessing agreement<br />
between two methods in categorical data.<br />
• Tools to assess <strong>the</strong> accuracy <strong>of</strong> diagnostic test<br />
have been calculated.<br />
• Sensitivity, specificity, positive and negative<br />
predictive values toge<strong>the</strong>r with Odds ratio.<br />
º Sensitivity = [True positive -– false negative]/<br />
True positive.<br />
º Specificity = [True negative – false positive]<br />
/ True negative.<br />
º Positive predictive value = [True positive –<br />
false positive] / True positive.<br />
º Negative predictive value = [True negative –<br />
false negative] / True negative.<br />
• p value
Comparative Study between Tissue Doppler Imaging & Radionuclide Scintigraphy<br />
Patients with COPD who have Rt ventricular impairment<br />
could be detected by <strong>the</strong> following:<br />
1- Pulsed wave tissue Doppler echocardiography<br />
at lateral tricuspid annulus that showed <strong>the</strong><br />
following parameters:<br />
• Peak myocardial systolic velocity (Sm)<br />
Sherine Elgangihi, et al<br />
Out <strong>of</strong> our 30 pts, Sm ≥12Cm/s and MPI
Comparative Study between Tissue Doppler Imaging & Radionuclide Scintigraphy<br />
%<br />
100<br />
90<br />
80<br />
70<br />
60<br />
50<br />
40<br />
30<br />
20<br />
10<br />
0<br />
11.1 61.9<br />
88.9 38.1<br />
RVD Normal RVD Dilated<br />
TDI Normal RV function<br />
TDI impaired RV function<br />
Figure 4: Shows <strong>the</strong> relation between (conventional echocardiograph)<br />
& TDI ± in assessment <strong>of</strong> RV function.<br />
A significant agreement between two methods<br />
RV diameter by measured by conventional echo<br />
TDI) in assessment <strong>of</strong> Rt ventricular function where<br />
sensitivity=62%, specificity=89%, +ve PV=92.9,<br />
–ve PV=50% & p value=0.011. But <strong>the</strong>re is no<br />
correlation between conventional echocardiograph<br />
& FPRNA in assessment <strong>of</strong> Rt ventricular function<br />
where p value 0.127.<br />
Table 6: Shows a <strong>com</strong>parison between TDI & clinical data<br />
in assessment <strong>of</strong> Rt ventricular functions.<br />
Normal RV function<br />
Impaired Rt<br />
ventricular function<br />
Total<br />
%<br />
100<br />
80<br />
60<br />
40<br />
20<br />
0<br />
TDI<br />
–ve signs<br />
cor-pulmonale<br />
Signs <strong>of</strong> Cor-pulmonale<br />
No.<br />
14<br />
1<br />
15<br />
–ve +ve<br />
6.7<br />
93.3<br />
Normal RV function<br />
Impaired RV function<br />
+ve signs<br />
cor-pulmonale<br />
86.7<br />
13.3<br />
Figure 5: Shows <strong>the</strong> relation between TDI & clinical data in<br />
evaluation <strong>of</strong> RV function.<br />
%<br />
93.3<br />
6.7<br />
100<br />
No.<br />
2<br />
13<br />
15<br />
%<br />
13.3<br />
86.7<br />
100<br />
p value<br />
Sherine Elgangihi, et al<br />
VI- The <strong>com</strong>parison between Rt ventricular systolic<br />
function (RVEF) detected by FPRNA &<br />
Rt ventricular dysfunction detected clinically<br />
(cor-palmonale):<br />
Our study group show 15 pt (50%) have no<br />
manifestation <strong>of</strong> cor-pulmonale & from which 13<br />
pt (86.7%) with normal Rt ventricular systolic<br />
function (RVEF >45%) detected by FPRNA & two<br />
Pts (13.3%) have Rt ventricular dysfunction by<br />
FPRNA.<br />
Also <strong>the</strong>re are 15 pts (50%) presented with<br />
manifestation <strong>of</strong> cor-pulmonale clinically from<br />
which only 11 pts (73.3%) have Rt ventricular<br />
impairment (RVEF 45%).<br />
There is a significant correlation between Rt<br />
ventricular function evaluated clinically & by<br />
FPRNA where p value is 0.01.<br />
VII- Correlation between PASP detect by continuous<br />
wave Doppler & lateral annulus velocities<br />
<strong>of</strong> tricuspid valve in patients with COPD:<br />
All patients <strong>of</strong> our study (30 pts) had elevated<br />
PASP as detected by pulsed wave Doppler echocardiography.<br />
Data <strong>of</strong> lateral annulus velocities <strong>of</strong><br />
tricuspid valve are shown in Table (8).<br />
Relationship between PASP and tricuspid lateral<br />
annulus systolic velocities are shown in Figs.<br />
(9,10,11).<br />
There were a significant negative correlation<br />
between PASP and Sm, SmVTI & Em/Am.<br />
Where: r=–0.61 p
Comparative Study between Tissue Doppler Imaging & Radionuclide Scintigraphy<br />
Figure 12: Tissue Doppler imaging = Sm 12.8 cm/s, IVRT = 33 ms, IVCT = 54 ms, MPI = 0.4,(EJ = 220), SmVTI = 2.2 cm,<br />
Em/Am = 0.8 (pt. No. 20).<br />
Figure 13: Tissue Doppler imaging = Sm 11.7 cm/s, IVCT = 75 ms, IVRT = 93 ms, ET = 177 ms, MPI = 0.9, SmVTI = 1.7,<br />
Em/Am = 0.3 (pt. No. 26).<br />
Discussion<br />
Evaluation <strong>of</strong> ventricular performance is <strong>of</strong>ten<br />
<strong>of</strong> paramount importance in ICU. Accurate and<br />
timely assessment <strong>of</strong> systolic ventricular function<br />
should be an integral part <strong>of</strong> medical management<br />
<strong>of</strong> <strong>the</strong> hemodynamically unstable critically ill<br />
patients [11].<br />
Right ventricular dysfunction is <strong>com</strong>mon, and<br />
its role in critically ill pts is underestimated [12].<br />
Additionally in <strong>the</strong> critical care setting, <strong>the</strong> RV<br />
function is also altered by increasing RV after load<br />
including high levels <strong>of</strong> positive end-expiratory<br />
pressure or increased pulmonary vascular resistance<br />
[13].<br />
For early diagnosis, electrocardiography and<br />
two dimensional echocardiography [159,160] are<br />
used. However, it is difficult to assess both RV<br />
anatomy and function with reliable conventional<br />
echocardiographic examination because <strong>of</strong> its <strong>com</strong>plex<br />
structure.<br />
32<br />
Tissue Doppler imaging (TDI) has been evolved<br />
as a new technique that enables myocardial velocities<br />
to be detected and makes <strong>the</strong> quantitative<br />
assessment <strong>of</strong> <strong>the</strong> systolic and diastolic movements<br />
<strong>of</strong> myocardial walls possible [16,17]. TDI has been<br />
considered to be a technique that leads to assessment<br />
<strong>of</strong> <strong>the</strong> RV function [18]. As determined from<br />
<strong>the</strong> position <strong>of</strong> <strong>the</strong> RV tricuspid annulus by TDI,<br />
myocardial velocities and <strong>the</strong> myocardial performance<br />
index (MPI), which are new parameters in<br />
assessing left ventricular function [19], can also<br />
give information about RV function.<br />
Despite RV function is less <strong>of</strong>ten measured than<br />
LV function it has been shown to hold clinical<br />
diagnostic and prognostic importance in many<br />
disorders [20-24]. Owing to its accuracy, First Pass<br />
Radionuclear Angiography has be<strong>com</strong>e a non invasive<br />
standard reference for RVEF, and has <strong>of</strong>ten<br />
been performed in concern with o<strong>the</strong>r measurements<br />
<strong>of</strong> RV function as a calibration method<br />
[25,26].
Sherine Elgangihi, et al<br />
Pulmonary artery pressure (PAP) is an important<br />
hemodynamic parameter that is used in <strong>the</strong> follow<br />
up <strong>of</strong> various cardiac & pulmonary disorder. It's<br />
<strong>the</strong> primary cause <strong>of</strong> right ventricular systolic and<br />
diastolic dysfunction and thus failure in COPD<br />
patients [27].<br />
In various studies <strong>the</strong> PASP could be determined<br />
by echocardiography in less than half <strong>of</strong> patients<br />
with COPD mostly due to absence <strong>of</strong> adequate TR<br />
velocity [28-31].<br />
Tissue Doppler imaging (TDI) is an extension<br />
<strong>of</strong> conventional Doppler flow echocardiography<br />
and has been established new method useful for<br />
predicting right atrial pressure, evaluation <strong>of</strong> right<br />
ventricular systolic and diastolic function also<br />
detecting <strong>the</strong> effect <strong>of</strong> PASP on <strong>the</strong> lateral tricuspid<br />
annulus velocities [7-9].<br />
The objective <strong>of</strong> present study is to assess <strong>the</strong><br />
usefulness <strong>of</strong> tissue Doppler imaging in evaluation<br />
<strong>of</strong> RV function in patients with COPD in <strong>com</strong>parison<br />
with FPRNA which is <strong>the</strong> gold standard method,<br />
also to determine <strong>the</strong> relationship between<br />
lateral tricuspid annulus velocities detected by TDI<br />
& PASP as estimated by continuous wave Doppler<br />
in patients with COPD.<br />
Previous studies using pulsed tissue Doppler<br />
in healthy adults have established normal reference<br />
values for adults at <strong>the</strong> level <strong>of</strong> <strong>the</strong> RV free wall<br />
and at <strong>the</strong> lateral tricuspid annulus and concluded<br />
that a peak systolic annular velocity
Comparative Study between Tissue Doppler Imaging & Radionuclide Scintigraphy<br />
motion indices and PASP where <strong>the</strong>re's a –ve correlation<br />
between PASP and Sm, SmVTI. (PASP<br />
Vs Sm r=–0.61, p value
Sherine Elgangihi, et al<br />
& lateral tricuspid annulus velocity where PASP<br />
vs Sm=–0.61, p
Comparative Study between Tissue Doppler Imaging & Radionuclide Scintigraphy<br />
19- (Copyright © 2009 Radiological Society <strong>of</strong> North America,<br />
Inc. (RSNA).<br />
20- Wencker D, Borer JS, Hochreiter C, et al: Preoperative<br />
predictors <strong>of</strong> late postoperative out<strong>com</strong>e among patients<br />
with non-ischemic mitral regurgitation with 'high-risk'<br />
descriptors and <strong>com</strong>parison with unoperated patients.<br />
Cardiology 2000; 93: 37.<br />
21- Di Salvo TG, Mathier M, Semigran MJ, et al: Preserved<br />
right ven-tricular ejection fraction predicts exercise capacity<br />
and survival in advanced heart failure. J Am Coll<br />
Cardiol 1995; 25: 1143.<br />
22- Hochreiter C, Niles N, Devereux RB, et al: Mitral regurgitation:<br />
Relationship <strong>of</strong> noninvasive descriptors <strong>of</strong> right and<br />
left ventricular performance to clinical and hemodynamic<br />
findings and to prognosis in medically and surgically<br />
treated patients. Criculation 1986; 73: 900.<br />
23- Sciurba FC, Rogers RM, Keenan RJ, et al: Improvement<br />
in pul-monary function and elastic recoil after lungreduction<br />
surgery for diffuse emphysema. N Engl J Med<br />
1996; 334: 1095.<br />
24- Bartlett MI, Seaton D, McEwan L, et al: Determination<br />
<strong>of</strong> right ventricular ejection fraction from reprojected<br />
gated pool SPECT. Comaprison with first-pass ventriuclargraphy.<br />
Eur J Nucl Med 2001; 28-608.<br />
25- Caplin JL, Flatman WD, Dymond DS: Effects <strong>of</strong> projection<br />
background correction method upon calculation <strong>of</strong> right<br />
ventricular ejection fraction using first-pass radionuclide<br />
angst phy. Int J Card Imaging 1985; 1: 171.<br />
26- Johnson LL, Lawson MA, Blackwell GG, et al: Optimizing<br />
<strong>the</strong> method to calculate right ventricular ejection fraction<br />
from first-pass data acquired with a multicrystal camera.<br />
J Nucl Cardiol 1995; 2: 372.<br />
27- Rich S, McLaughlin VV: Pulmonary hypertension. In:<br />
Zipes DP, Libby P, Bonow RO, Braunwald E (eds) Braunwald's<br />
Heart Disease. Elsevier Saunders, Philadelphia,<br />
PP 1807-1842.<br />
28- Arcasoy SM, Christie JD, Ferrari VA, et al: Echocardiographic<br />
assessment <strong>of</strong> pulmonary hypertension in patietns<br />
with advanced lung disease. Am J Respir Crit Care Med<br />
2003; 167: 735-740.<br />
29- Tramarin R, Torbicki A, Marchandise B, Laaban JP,<br />
Morpurgo M: Doppler echocardigoraphic evaluation <strong>of</strong><br />
pulmonary artery pressure in chronic obstructive pulmonary<br />
disese. A European multicentre study. Working Group<br />
on Noninvasive Evaluation <strong>of</strong> Pulmonary Artery Pressure.<br />
European Office <strong>of</strong> <strong>the</strong> world Health Organization, Copenhagen.<br />
Eur Heart J 1991; 12: 103-111.<br />
30- Spiropoulos K, Charokopos N, Petsas T, et al: Noninvasive<br />
estimation <strong>of</strong> pulmonary arterial hypertension<br />
in chronic obstructive pulmonary disease. Lung 1999;<br />
177: 65-75.<br />
31- Feigenbaum H, Armstrong WF, Ryan T: Evaluation <strong>of</strong><br />
systolic and diastolic function <strong>of</strong> <strong>the</strong> left ventricle. In:<br />
Feigenbaum H, Armstrong WF, Ryan T (eds) Feigenbaum's<br />
Echocardiography. Lippincott Williams, Philadelphia<br />
2005; pp 138-180.<br />
36<br />
32- Kukulski T, Voigt JU, Wilkensh<strong>of</strong>f UM, et al: A <strong>com</strong>parison<br />
<strong>of</strong> regional myocardial velocity information derived by<br />
pulsed and color Doppler techniques: An in vitro and in<br />
vivo study. Echocardiography 2000; 17: 639-51.<br />
33- Raizada V, Sahn DJ, Covell JW: Factors influencing late<br />
right ventricular ejection. Cardiovasc Res 1988; 22: 244-<br />
8.<br />
34- Myhre ES, Slinker BK, LeWinter MM: Absence <strong>of</strong> right<br />
ventricular isovolumic relaxation in open-chest anes<strong>the</strong>tized<br />
dogs. Am J Physiol 1992; 263: 587-90.<br />
35- Feneley MP, Olsen CO, Glower DD, et al.: Effect <strong>of</strong><br />
acutely increased right ventricular afterload on work<br />
output from <strong>the</strong> left ventricle in conscious dogs. Systolic<br />
ventricular interaction. Circ Res 1989; 65: 135-45.<br />
36- Caso P, Galderisi M, Cicala S, et al: Association between<br />
myocardial right ventricular relaxation time and pulmonary<br />
arterial pressure in chronic obstructive lung disease:<br />
Analysis by pulsed Doppler tissue imaging. J Am Soc<br />
Echocardiography 2001; 14: 970-7.<br />
37- Severino S, Caso P, Cicala S, et al: Involvement <strong>of</strong> right<br />
ventricle in left ventricular hypertrophic cardiomyopathy:<br />
Analysis by pulsed Doppler tissue imaging. Eur J Echocardiography<br />
2000; 1: 281-8.<br />
38- Cicala S, Galderisi M, Caso P, et al: Right ventricular<br />
diastolic dysfunction in arterial systemic hypertension:<br />
Analysis by pulsed tissue Doppler. Eur J Echocardiography<br />
2002, 39: 312-17.<br />
39- Galderisi M, Severino S, Caso P, et al: Right ventricular<br />
myocardial diastolic dysfunction in different kinds <strong>of</strong><br />
cardiac hypertrophy: Analysis by pulsed Doppler tissue<br />
imaging. Ital Heart J 2001; 2: 912-20.<br />
40- Sengupta PP, Mohan JC, Pandian NG: Tissue Doppler<br />
echocardiography: Principles and application. Indian<br />
Heart J 2002; 54: 368-78.<br />
41- OM Ueti, EE Camargo, A de A Ueti, E C de Lima-Filho,<br />
EA Nogueira: Assessment <strong>of</strong> right ventricular function<br />
with Doppler echocardiography indices derived from<br />
tricuspid annular motion: Comparison with radionuclide<br />
angiography. Heart 2002; 88 (3): 244-248.<br />
42- Meluzin J, Spiranova L, Bakala J, et al: Pulsed Doppler<br />
Tissue imaging <strong>of</strong> <strong>the</strong> velocity <strong>of</strong> tricuspid annular systolic<br />
motion. Eur Hert J 2001; 22: 340-48.<br />
43- Pavan K, Karnati, et al: Myocardial performance index<br />
correlates with right ventricular ejection fraction measured<br />
by nuclear ventriculography. Echocardiography 2006; 25:<br />
518-29.<br />
44- UM Ueti, EE Camargo, A de A Ueti, E C de Lima-Filho,<br />
EA Nogueira: Assessment <strong>of</strong> right ventricular function<br />
with Doppler echocardigoraphic indices derived from<br />
tricuspid annular motion: Comparison with radionuclide<br />
angiography. Heart 2002; 88: 244-248.<br />
45- W Macnee, Qf Xue, WJ Hannan, Dc Flenley, CJ Adie, Al<br />
Muir: Assessment by radionuclide angiography <strong>of</strong> right<br />
and left ventricular function in chronic bronchitis and<br />
emphysema. Thorax 1983; 38: 494-500.
Sherine Elgangihi, et al<br />
46- Bakry M, et al: Usefulness <strong>of</strong> Tissue Doppler Imaging<br />
versus Radionuclide Scintigraphy in Evaluation <strong>of</strong> Right<br />
Ventricular Myocardial Involvement In Acute Inferior<br />
Wall Myocardial Infarction. Master Thesis in Critical<br />
Care Medicine 2008.<br />
37<br />
47- Mehmet Mele, Ozlem Esen, Ali Metin Esen, Irfan Barutcu,<br />
Fatma Fidan, Ersel Onrat, Dayimi Kaya: Tissue Doppler<br />
evaluation <strong>of</strong> tricuspid annulus for estimation <strong>of</strong> pulmonary<br />
artery pressure in patients with COPD. Lung 2006; 184:<br />
121-131.
Egypt Heart J 62 (1): 39-52, March 2010<br />
Metabolic Syndrome and its Impact on Vascular Damage Extent<br />
AYMAN SADEK, MD; MAGDY NOUH AIN, MD; HANY FOUAD HANAA, MD;<br />
RAMZY HAMED EL-MAWARDY, MD<br />
Background: Metabolic syndrome is associated with increased risk <strong>of</strong> cardiovascular diseases in patients without a<br />
cardiovascular history, <strong>the</strong>re is nearly 3 fold increase cardiovascular related mortality <strong>com</strong>pared to subjects without metabolic<br />
syndrome.<br />
Aim <strong>of</strong> <strong>the</strong> Work: Was to investigate <strong>the</strong> relation between metabolic syndrome and extent <strong>of</strong> vascular damage.<br />
Methods and Results: We conducted a prospective observational study <strong>of</strong> 50 patients with history <strong>of</strong> coronary artery disease,<br />
history <strong>of</strong> stroke TIA or Peripheral arterial disease between January 2005 and March 2006 at Ain Shams University hospitals,<br />
Egypt. Patients having criteria <strong>of</strong> metabolic syndrome were identified. Echocardiography, carotid and femoral duplex, detection<br />
<strong>of</strong> microalbuminuria were done for <strong>the</strong> study population The study population was divided into three groups: Group I included<br />
12 patients with 3 metabolic risk factors, group II included 17 patients with 4 metabolic risk factors and group III included 21<br />
patients with 5 metabolic risk factors. Comparison between <strong>the</strong> study groups as regard intima media thickness (IMT) <strong>of</strong> <strong>the</strong><br />
carotid and femoral arteries revealed that right carotid IMT was 0.97mm ±0.17, 1.13mm ±0.14 and 1.18mm ±0.17 in group I,II<br />
and III respectively (p=0.002). Left carotid IMT was 0.97mm ±.19, 1.12mm ±0.12 and 1.19mm ±0.19 in group I,II and III<br />
respectively [p=0.003 right femoral IMT was 0.98 mm ±0.23, 1.11mm ± 0.18 and 1.09 mm ±0.20 in group I,II and III respectively<br />
(p=078)] left femoral IMT was 0.90mm ±.23, 1.10mm ±0.09 and 1.08 mm ±0.15 in group I,II and III respectively (p=0.003).<br />
Comparison between <strong>the</strong> study groups as regard presence <strong>of</strong> carotid or femoral plaques revealed that presence <strong>of</strong> carotid plaque<br />
was positive in 0.0 patient (0%) <strong>of</strong> group I and 5 patients (29.4%) <strong>of</strong> group II and 12 patient (57.1%) <strong>of</strong> group III (p=0.023).<br />
Presence <strong>of</strong> femoral plaque was positive in 3 patients (25%) <strong>of</strong> group I and 4 patients (23.5%) <strong>of</strong> group II and 8 patient (38.1%)<br />
<strong>of</strong> group III (p=0.56). Microalbuminuria was positive in 1 patient (8.3%) in group I, 4 patients (23.5%) <strong>of</strong> group II and 11<br />
patients (52.4%) <strong>of</strong> group III (p=0.022). When <strong>com</strong>paring between <strong>the</strong> study groups as regard number <strong>of</strong> vascular beds affected<br />
in each group (coronary, cerebral and peripheral vascular beds), we found that group I 10 patients (40%) was having one vascular<br />
bed affected, 2 patients (8.7%) having two vascular beds affected and 0.0 patient (0%) having three vascular beds affected, in<br />
group II we found that 10 patients 40% was having one vascular beds affected 7 patients (30.4%) having two vascular beds<br />
affected and 0.0 (0%) patient having three vascular beds affected. In group III we found that 5 patients (20%) was having one<br />
vascular beds affected 14 patients (60.5%) having two vascular beds affected and 2 (100%) patients having three vascular beds<br />
affected. Right femoral IMT was 1.06±0.19mm when one vascular bed affected, 1.13±0.22mm when two vascular beds affected<br />
and 1.12±0.17mm when three vascular beds affected (p=0.59). Left femoral IMT was 0.9±0.22mm when one vascular bed<br />
affected, 1.09±0.22mm when two vascular beds affected and 1.09±0.15mm when three vascular beds affected (p=0.003)<br />
Comparison between <strong>the</strong> presence <strong>of</strong> positive microalbuminuria and number <strong>of</strong> vascular beds affected revealed that it was<br />
positive in 2 patients (8.0%) when one vascular bed affected, 12 patients (52.2%) when two vascular beds affected and 2 patients<br />
(100%) when three vascular beds affected (p=0.001).<br />
Conclusions: Metabolic syndrome is constellation <strong>of</strong> risk factors for a<strong>the</strong>rosclerosis and increase in traits <strong>of</strong> metabolic<br />
syndrome is associated with increase in extent <strong>of</strong> vascular damage. The increase in traits <strong>of</strong> metabolic syndrome is associated<br />
with increase in carotid and femoral IMT and presence <strong>of</strong> microalbuminuria. The presence <strong>of</strong> thickened carotid and femoral<br />
IMT and presence <strong>of</strong> microalbuminuria is associated with increase in extent <strong>of</strong> vascular damage.<br />
Key Words: Metabolic syndrome – Vascular damage.<br />
Faculty <strong>of</strong> Medicine, Ain Shams University.<br />
Manuscript received 10 Sep., 2009; revised 20 Oct., 2009;<br />
accepted 21 Oct., 2009.<br />
Address for Correspondence: Dr. Ayman Sadek, Faculty <strong>of</strong><br />
Medicine, Ain Shams University.<br />
39
Metabolic Syndrome & its Impact on Vascular Damage Extent<br />
Introduction<br />
The metabolic syndrome is a constellation <strong>of</strong><br />
interrelated risk factors <strong>of</strong> metabolic origin (metabolic<br />
risk factors) that appear to directly promote<br />
<strong>the</strong> development <strong>of</strong> a<strong>the</strong>rosclerotic cardiovascular<br />
disease (ASCVD). According to Adult Treatment<br />
Panel III (ATP III) <strong>the</strong> metabolic syndrome is<br />
diagnosed when three or more metabolic abnormalities<br />
(impaired glucose metabolism, elevated<br />
blood pressure, hypertriglyceridemia, low HDL<br />
cholesterol and central obesity) cluster in <strong>the</strong> same<br />
person [1].<br />
This syndrome confers an increased risk for<br />
<strong>the</strong> development <strong>of</strong> diabetes mellitus and for cardiovascular<br />
morbidity and mortality [2-4].<br />
According to different investigators <strong>the</strong> increase<br />
<strong>of</strong> thickness <strong>of</strong> intima media <strong>com</strong>plex is said to be<br />
<strong>the</strong> earliest morphological alteration in pathogenesis<br />
<strong>of</strong> arteriosclerosis. Reitzschel and Associates<br />
(2001), were interested in <strong>the</strong> multivariate relation<br />
between most <strong>of</strong> cardiovascular risk factors and<br />
<strong>the</strong> carotid and femoral IMT. All <strong>the</strong> traditional<br />
risk factors were assessed for all candidates and<br />
cardiovascular risk was calculated using Framingham<br />
equation, which was directly related to CIMT<br />
and FIMT. Both <strong>the</strong> CIMT and FIMT were intercorrelated<br />
but <strong>the</strong> CIMT is easier and more suitable<br />
for risk stratification in low risk population [5].<br />
The appearance <strong>of</strong> trace amounts <strong>of</strong> albumin<br />
(microalbuminuria, 30 to 300mg/d) and larger<br />
amounts (frank proteinuria, ≥1g/d) are associated<br />
with an increased risk for renal failure, heart disease,<br />
stroke and cardiovascular mortality [6,7].<br />
Miettinen et al., (1996) found an association between<br />
amount <strong>of</strong> urinary protein excretion and risk<br />
<strong>of</strong> stroke and lower extremity amputation in a<br />
cohort <strong>of</strong> subjects that was independent <strong>of</strong> diabetes<br />
status and traditional risk factors [8].<br />
The syndrome is diagnosed when three or more<br />
metabolic abnormalities cluster in <strong>the</strong> same person:<br />
Impaired glucose metabolism (Fasting blood<br />
glucose >110mg/dl).<br />
Elevated blood pressure (≥130mmHg systolic<br />
or ≥85mmHg diastolic).<br />
Hypertriglyceridemia (serum triglycerides<br />
>150mg/dl).<br />
Low HDL-cholesterol (88cm in women) [1].<br />
This syndrome confers an increased risk for<br />
<strong>the</strong> development <strong>of</strong> diabetes mellitus and for cardiovascular<br />
morbidity and mortality [2].<br />
From several epidemiological studies it became<br />
clear that measurement <strong>of</strong> carotid intima media<br />
thickness (IMT) can be applied as a marker for<br />
generalized a<strong>the</strong>rosclerosis and as an indicator <strong>of</strong><br />
cardiovascular risk [9].<br />
Similarly albuminuria and decreased ankle<br />
brachial pressure index (ABPI) are markers <strong>of</strong><br />
a<strong>the</strong>rosclerosis and indicators <strong>of</strong> increased cardiovascular<br />
risk [10].<br />
The presence <strong>of</strong> <strong>the</strong> metabolic syndrome at<br />
baseline increased <strong>the</strong> risk for development <strong>of</strong><br />
diabetes mellitus almost 2-fold in American Indians<br />
and in Finnish men roughly 4-fold increase was<br />
shown [11].<br />
In a study by Lakka et al, men with metabolic<br />
syndrome had a nearly 3-fold increase in cardiovascular<br />
related mortality <strong>com</strong>pared to subjects<br />
without <strong>the</strong> metabolic syndrome [12].<br />
In addition, <strong>the</strong> risk for coronary heart disease<br />
and stroke tripled in metabolic syndrome subjects<br />
with a 10% increase in cardiovascular mortality<br />
during 6.9 years <strong>of</strong> follow-up [13].<br />
Aim <strong>of</strong> work:<br />
The aim <strong>of</strong> this study is to investigate whe<strong>the</strong>r<br />
<strong>the</strong> metabolic syndrome is related to <strong>the</strong> extent <strong>of</strong><br />
vascular damage in patients with various manifestations<br />
<strong>of</strong> vascular disease.<br />
Patients and Methods<br />
Patient selection:<br />
This study was conducted on 50 patients, in<br />
<strong>the</strong> period between July, 2005 and February, 2006<br />
who were referred to <strong>the</strong> <strong>cardiology</strong>, neurology,<br />
internal medicine and vascular departments in Ain<br />
Shams University Hospital. Patients who were<br />
newly presented with a manifest a<strong>the</strong>rosclerotic<br />
disease (coronary heart disease, stroke, peripheral<br />
arterial disease):<br />
Patients with coronary heart disease were patients<br />
with recent onset coronary heart disease<br />
whom were primarily referred for Coronary angiography,<br />
those with stroke had a TIA or cerebral<br />
infarction, those with PAD were symptomatic and
Ayman Sadek, et al<br />
had documented obstruction <strong>of</strong> distal arteries <strong>of</strong><br />
<strong>the</strong> leg (Peripheral angiography or lower limb<br />
arterial duplex).<br />
The following patients were be excluded from <strong>the</strong><br />
whole study:<br />
Previous neck or femoral irradiation, Previous<br />
neck or femoral surgery, or any neck or lower limb<br />
deformity interfering with carotid or femoral ultrasonography<br />
respectively.<br />
Methods:<br />
Every patient was subjected to <strong>the</strong> following:<br />
Proper history taking and examination:<br />
Full history for <strong>the</strong> presence <strong>of</strong> cardiovascular<br />
risk factors:<br />
Smoking, Hypertension, Diabetes mellitus,<br />
Dyslipidemia, Family history <strong>of</strong> ischemic heart<br />
disease, Symptoms suggestive <strong>of</strong> coronary artery<br />
diseases Peripheral vascular disease Cerebrovascular<br />
strokes or transient ischemic attacks:<br />
Complete general and local clinical examination<br />
with stress on <strong>the</strong> following points:<br />
Weight: Measured in kilograms.<br />
Height: Measured in meters.<br />
Body mass index = Weight in kilograms/(height<br />
in meters) 2<br />
Table 1: Criteria for clinical diagnosis <strong>of</strong> metabolic syndrome.<br />
Measure<br />
(any 3 <strong>of</strong> 5 constitute<br />
diagnosis <strong>of</strong> metabolic<br />
syndrome)<br />
Elevated waist circumference*<br />
Elevated triglycerides<br />
Reduced HDL-C<br />
Elevated blood pressure<br />
Elevated fasting glucose<br />
Categorical<br />
Cutpoints<br />
≥102 cm (≥40 inches) in<br />
men ≥88 cm (≥35 inches)<br />
in women<br />
≥150 mg/dL (1.7<br />
mmol/L)Or On drug<br />
treatment for elevated<br />
triglycerides<br />
≤40 mg/dL (1.03 mmol/L)<br />
in men≤50 mg/dL (1.3<br />
mmol/L) in women<br />
≥130 mm Hg systolic blood<br />
pressure or ≥85 mm Hg<br />
diastolic blood pressure<br />
or On antihypertensive<br />
drug treatment in a patient<br />
with a history <strong>of</strong><br />
hypertension<br />
≥100 mg/dL or On drug<br />
treatment for elevated<br />
glucose<br />
41<br />
Pulse: Radial, brachial with stress on pulse<br />
pressure and dorsalis pedis arteries were examined<br />
for rate, rhythm, volume, special character and<br />
equality <strong>of</strong> pulsations.<br />
Morning urine sample to measure microalbuminuria:<br />
Using HemoCue Urine albumin operator<br />
manuals instrument.<br />
1- We open <strong>the</strong> package and carefully remove <strong>the</strong><br />
cuvette <strong>the</strong>n we fill <strong>the</strong> cuvette by contact with<br />
<strong>the</strong> urine sample (a urine drop on a hydrophilic<br />
surface i.e a plastic film).<br />
2- Open <strong>the</strong> lid and push <strong>the</strong> filled cuvette into <strong>the</strong><br />
cuvette holder.<br />
3- Measuring should begin within 30 seconds after<br />
<strong>the</strong> cuvette has been filled with urine.<br />
4- Within 90 seconds <strong>the</strong> result will be displayed<br />
in mg/dl.<br />
12 lead surface ECG:<br />
Echocardiography:<br />
Echocardiography was done for measurement<br />
<strong>of</strong> (LVEDD), (LVEDD, (EF), (LVPWT) and<br />
(IVST).<br />
And assessment <strong>of</strong> RSWMA.<br />
Carotid and femoral arterial duplex:<br />
All patients underwent ultrasonography <strong>of</strong> <strong>the</strong><br />
right and left carotid and femoral arteries where<br />
<strong>the</strong> following measured:<br />
1- Carotid intima-media thickness (IMT):<br />
The characteristic B-scan pattern <strong>of</strong> <strong>the</strong> arterial<br />
walls shows two parallel echogenic lines separated<br />
by a relatively hypoechoic space "<strong>the</strong> double line<br />
pattern". This pattern is found in <strong>the</strong> posterior wall<br />
<strong>of</strong> <strong>the</strong> <strong>com</strong>mon carotid arteries; <strong>the</strong> inner line is<br />
generally more regular, smooth and thin than <strong>the</strong><br />
outer one and represents <strong>the</strong> lumen intima interface.<br />
The outer one is produced by <strong>the</strong> collagen containing<br />
upper layer <strong>of</strong> tunica adventitia, close to <strong>the</strong><br />
media-adventitia interface.<br />
The intima-media thickness (IMT) is measured<br />
from <strong>the</strong> leading edge <strong>of</strong> <strong>the</strong> inner line to <strong>the</strong><br />
leading edge <strong>of</strong> <strong>the</strong> outer one [14].<br />
An ultrasonographically determined increase<br />
in IMT may be regarded as an indicator <strong>of</strong> generalized<br />
a<strong>the</strong>rosclerosis [15].<br />
We measured <strong>the</strong> carotid IMT bilaterally by Bmode<br />
ultrasonography (7-8MHz linear array, gen-
Metabolic Syndrome & its Impact on Vascular Damage Extent<br />
eral electric vivid 5) in a linear segment <strong>of</strong> 10-<br />
12mm length <strong>of</strong> <strong>com</strong>mon carotid artery. The carotid<br />
IMT is measured as <strong>the</strong> distance between <strong>the</strong> bloodintima<br />
and media-adventitia interfaces as previously<br />
described by Pignoli et al. (1986)(16). In healthy<br />
adults, IMT ranges from 0.25 to 1.5mm and values<br />
>1.0mm are <strong>of</strong>ten regarded as abnormal [17].<br />
2- Carotid plaques:<br />
A plaque was defined as a localized intimal<br />
thickening
Ayman Sadek, et al<br />
with mean age <strong>of</strong> 51.2±9.21 years. There was no<br />
significance difference between <strong>the</strong> three subgroups<br />
as regard age and sex distribution (p>0.05). These<br />
data are presented in Table (2).<br />
I- Description and <strong>com</strong>parison between <strong>the</strong><br />
study groups:<br />
1- Age and sex:<br />
Fig. (1) demonstrates age and gender distribution<br />
among <strong>the</strong> study.<br />
14<br />
12<br />
10<br />
8<br />
6<br />
4<br />
2<br />
0<br />
Males<br />
Females<br />
Group I Group II Group III<br />
Figure 1: Sex distribution in <strong>the</strong> three studied groups.<br />
2- Risk factors:<br />
Every patient was asked about risk factors <strong>of</strong><br />
a<strong>the</strong>rosclerosis and special habits <strong>of</strong> medical importance<br />
and it was found that 25% <strong>of</strong> group I,<br />
41.7% among group II and 32% among group III<br />
were smokers or ex-smokers, whereas, positive<br />
family history <strong>of</strong> IHD, CVA or peripheral vascular<br />
disease was found to be 8.3% among group I, 5.9%<br />
among group II and 23% among group III. Past<br />
history <strong>of</strong> HTN, DM or past history <strong>of</strong> dyslipidemia<br />
by lipid pr<strong>of</strong>ile and regular intake <strong>of</strong> hypolipidemic<br />
drugs were considered among selection criteria for<br />
metabolic syndrome. These data and distribution<br />
<strong>of</strong> o<strong>the</strong>r metabolic risk factors are shown in Table<br />
(2).<br />
3- Clinical examination and laboratory investigations:<br />
All patients underwent clinical examination,<br />
where blood pressure, waist circumference in cm,<br />
height in meters, body weight in kg were measured<br />
and body mass index was calculated and LAB<br />
evaluation <strong>of</strong> blood sugar and lipid pr<strong>of</strong>ile. It was<br />
found that systolic and diastolic blood pressures<br />
were higher in group III, TG, female W.C, BMI<br />
and FBS were highest in group II while HDL-C<br />
was lowest in group III. Data are shown in Table<br />
(3).<br />
43<br />
Table 2: Distribution <strong>of</strong> risk factors within <strong>the</strong> study groups.<br />
Smoking<br />
FH<br />
HTN<br />
DM<br />
Dyslipidemia<br />
(+ve<br />
history)<br />
No (%)<br />
TG<br />
(increased)<br />
No (%)<br />
HDL-C<br />
(decreased)<br />
W.C<br />
(increased)<br />
Table 3: Quantitative analysis <strong>of</strong> risk factors <strong>of</strong> <strong>the</strong> study<br />
groups by using mean and SD.<br />
Systolic BP<br />
Diastolic BP<br />
DUR <strong>of</strong> HTN<br />
FBS<br />
DUR <strong>of</strong> DM<br />
TG<br />
HDL-C:<br />
Males<br />
Females<br />
W.C.:<br />
Males<br />
Females<br />
BMI<br />
Group I<br />
(no=12)<br />
3 (25%)<br />
1 (8.3%)<br />
10 (83.3%)<br />
5 (41/7%)<br />
1 (8.3%)<br />
8 (66.7%)<br />
10 (83.3%) 15 (88.2%) 21 (100%) 3.38<br />
5 (41.7%)<br />
Group I<br />
(no=12)<br />
Mean (SD)<br />
135.83+<br />
(20.54)<br />
83.33+<br />
(11.93)<br />
2.83+<br />
(3.49)<br />
147.5+<br />
(78.47)<br />
2.67+<br />
(4.47)<br />
170.42+<br />
(23.69)<br />
37.26+<br />
(5.6)<br />
44.2+<br />
(7.9)<br />
106+<br />
(9.41)<br />
95.21+<br />
(8.31)<br />
28.68+<br />
(3.12)<br />
Group II<br />
(no=17)<br />
7 (41.7%)<br />
1 (5.9%)<br />
15 (88.2%)<br />
8 (47.1%)<br />
4 (23.5%)<br />
17 (100%)<br />
FH = Family history.<br />
TG = Triglycerides.<br />
HDL-C = High density<br />
lipoprotein-cholesterol.<br />
BP = Blood pressure.<br />
FBS = Fang blood pressure.<br />
TG = Triglycerides.<br />
HDL-C = High density<br />
lipoprotein cholesterol.<br />
Group III<br />
(no=21)<br />
6 (32.0%)<br />
5 (23.8%)<br />
21 (100%)<br />
8 (38.0%)<br />
9 (42.9%)<br />
21 (100%) 13.77 0.001<br />
15 (88.2%) 21 (100%) 18.28 0.000<br />
Group II<br />
(no=17)<br />
Mean (SD)<br />
127.29+<br />
(22.45)<br />
81.17+<br />
(9.44)<br />
3.35+<br />
(5.80)<br />
152.47+<br />
(64.59)<br />
3.41+<br />
(4.03)<br />
191.35+<br />
(13.49)<br />
35.1<br />
(6.91)<br />
45.3+<br />
(8.3)<br />
108.36+<br />
(12.31)<br />
99.21+<br />
(7.81)<br />
31.83+<br />
(3.65)<br />
F<br />
1.04<br />
2.92<br />
3.38<br />
0.31<br />
4.77<br />
0.59<br />
0.23<br />
0.19<br />
0.86<br />
0.09<br />
0.19<br />
W.C = Waist circumference.<br />
HTN = Hypertension.<br />
DM = Diabetes mellitus.<br />
Group III<br />
(no=21)<br />
Mean (SD)<br />
150.0+<br />
(9.49)<br />
94.52+<br />
(9.73)<br />
6.47+<br />
(5.42)<br />
149.8+<br />
(48.83)<br />
2.33+<br />
(3.75)<br />
181.71+<br />
(16.55)<br />
33.3+<br />
(6.72)<br />
41.7+<br />
(8.31)<br />
112.38+<br />
(11.45)<br />
98.61+<br />
(10.81)<br />
31.31+<br />
(4.17)<br />
W.C = Waist circumference.<br />
BMI = Body mass index.<br />
DUR = Duration.<br />
p
Metabolic Syndrome & its Impact on Vascular Damage Extent<br />
4- Distribution <strong>of</strong> (IHD, PVD, CVA) within <strong>the</strong><br />
study groups:<br />
It was found that 11 patients <strong>of</strong> group I, 13 <strong>of</strong><br />
group II and 21 <strong>of</strong> group III had IHD,2 patients <strong>of</strong><br />
group I, 8 group II and 12 <strong>of</strong> group III had CVA,<br />
2 patients <strong>of</strong> group I, 3 <strong>of</strong> group II and 7 <strong>of</strong> group<br />
III had PVD, <strong>the</strong>se data are shown in Fig. (2).<br />
25<br />
20<br />
15<br />
10<br />
5<br />
0<br />
IHD<br />
CVA<br />
PVD<br />
Gr I Gr II Gr III<br />
Figure 2: Distribution <strong>of</strong> IHD, PVD and CVA in <strong>the</strong> three<br />
studied groups.<br />
5- Echocardiography:<br />
Echocardiography was done while <strong>the</strong> patient<br />
in left lateral position. M-mode was used for detection<br />
<strong>of</strong> left ventricular internal dimension measurements<br />
in end diastolic (LVEDD) and end systolic<br />
(LVEDD), ejection fraction (EF), left ventricle<br />
posterior wall thickness (LVPW) and interventricular<br />
septal thickness (IVS) were measured and<br />
resting segmental wall motion abnormality was<br />
assessed, <strong>the</strong>se data are shown in Table (4).<br />
Table 4: Comparing echocardiography parameters within <strong>the</strong><br />
study groups.<br />
Increased<br />
LV-IVS<br />
thickness<br />
Increased<br />
LV-PWT<br />
Diastolic<br />
dysfunction<br />
Resting<br />
SWMA<br />
Increased<br />
LVEDD<br />
Increased<br />
LVESD<br />
LV<br />
IVS<br />
PWT<br />
SWMA<br />
LVEDD<br />
LVESD<br />
Group I<br />
(no=12)<br />
7 (58.3%)<br />
7 (58.3%)<br />
10 (83.3%) 15 (88.2%) 20 (95.2%) 1.29 0.52<br />
2 (16.7$)<br />
0 (0.0%)<br />
0<br />
Group II<br />
(no=17)<br />
12 (70.6%) 18 (85.7%) 3.13 0.20<br />
12 (70.6%) 18 (85.7%) 3.13 0.20<br />
5 (29.4%)<br />
2 (11.8%)<br />
1 (5.9%)<br />
= Left ventricle.<br />
= Interventricular septum.<br />
= Posterior wall thickness.<br />
Group III<br />
(no=21)<br />
8 (38.1%)<br />
7 (33.3%)<br />
7 (33.3%)<br />
= Segmental wall motion abnormality.<br />
= Left ventricular end diastolic dimension.<br />
= Left ventricular end systolic dimension.<br />
F<br />
p<br />
1.67 0.43<br />
6.42 0.04<br />
8.27 0.016<br />
44<br />
6- Common Carotid and <strong>com</strong>mon femoral intima<br />
media thickness (CIMT and FIMT):<br />
All patients underwent carotid and femoral<br />
ultra-sonography where <strong>the</strong> <strong>com</strong>mon carotid and<br />
<strong>com</strong>mon femoral intima media thickness <strong>of</strong> both<br />
sides were measured and it was found that <strong>the</strong>re<br />
is a significant difference in RCIMT, LCIMT and<br />
LFIMT between <strong>the</strong> study groups (p0.05). These data are shown in Table<br />
(5).<br />
Table 5: Comparing R-CIMT, L-CIMT, R-FIMT and L-FIMT<br />
within <strong>the</strong> study groups.<br />
R-CIMT<br />
L-CIMT<br />
R-FIMT<br />
L-FIMT<br />
Group I<br />
(no=12)<br />
0.97+<br />
(0.17)<br />
0.97+<br />
(0.19)<br />
0.98+<br />
(0.23)<br />
0.90+<br />
(0.23)<br />
Group II<br />
(no=17)<br />
1.13+<br />
(0.14)<br />
1.12+<br />
(0.12)<br />
1.11+<br />
(0.18)<br />
1.1+<br />
(0.09)<br />
Group III<br />
(no=21)<br />
1.18+<br />
(0.17)<br />
1.19+<br />
(0.19)<br />
1.09+<br />
(0.20)<br />
1.08 +<br />
(0.15)<br />
R-CIMT = Right carotid intima-media thickness.<br />
L- CIMT = Left carotid intima-media thickness.<br />
R-FIMT = Right femoral intima-media thickness.<br />
L-FIMT = Left femoral intima-media thickness.<br />
6.87<br />
6.74<br />
2.60<br />
6.5<br />
7- Carotid plaques:<br />
There were no pathological carotid plaques in<br />
group (I). 29.4 % <strong>of</strong> group II had pathological<br />
carotid plaques, whereas 57.1% <strong>of</strong> group III had<br />
plaques (p0.05). These data are<br />
shown in Table (6).<br />
F<br />
p<br />
0.002<br />
0.003<br />
0.78<br />
0.003<br />
Table 6: Comparison between <strong>the</strong> study groups regarding<br />
presence or absence <strong>of</strong> carotid and femoral plaques.<br />
Positive<br />
carotid<br />
plaque<br />
Positive<br />
femoral<br />
plaque<br />
Group I<br />
(no=12)<br />
0 (0.0%)<br />
3 (25.0%)<br />
Group II<br />
(no=17)<br />
5 (29.4%)<br />
4 (23.5%)<br />
Group III<br />
(no=21)<br />
12 (57.1%)<br />
8 (38.1%)<br />
F<br />
11.36<br />
1.14<br />
p<br />
0.023<br />
0.56
Ayman Sadek, et al<br />
8- Micro albuminuria:<br />
There was a significant difference between <strong>the</strong><br />
study groups and it was found to be 52.4% in group<br />
III, 23.5% in group II and 8.3% in group I (p
Metabolic Syndrome & its Impact on Vascular Damage Extent<br />
4- Common carotid and <strong>com</strong>mon femoral IMT:<br />
There was a significant difference in L-CIMT,<br />
carotid plaque and L-FIMT (p0.05) between patients with one, two<br />
and three vascular beds affected, <strong>the</strong>se data are<br />
shown in Table (9).<br />
Table 9: Relation between carotid and femoral IMT and<br />
number <strong>of</strong> vascular beds affected in <strong>the</strong> form <strong>of</strong><br />
mean + SD.<br />
R-CIMT<br />
L-CIMT<br />
R-FIMT<br />
L-FIMT<br />
One<br />
(no=25)<br />
1.072 +<br />
(0.15)<br />
1.06 +<br />
(0.15)<br />
1.06 +<br />
(0.19)<br />
0.90 +<br />
(0.22)<br />
Number <strong>of</strong> vascular beds affected<br />
Two<br />
(no=23)<br />
1.13 +<br />
(0.19)<br />
1.15 +<br />
(0.21)<br />
1.13 +<br />
(0.22)<br />
1.09 +<br />
(0.08)<br />
Three<br />
(no=2)<br />
1.33 +<br />
(0.21)<br />
1.36 +<br />
(0.28)<br />
1.12 +<br />
(0.17)<br />
1.09 +<br />
(0.15)<br />
5- Microalbuminuria:<br />
There was a significant difference in presence<br />
<strong>of</strong> microalbuminuria between patients with one,<br />
two and three vascular beds affected, <strong>the</strong>se data<br />
are shown in Table (11).<br />
F<br />
2.47<br />
3.36<br />
0.53<br />
6.5<br />
p<br />
0.09<br />
0.043<br />
0.59<br />
0.003<br />
Table 10: Relation <strong>of</strong> carotid and femoral plaques to number<br />
<strong>of</strong> vascular beds affected.<br />
Positive<br />
carotid<br />
plaque<br />
Positive<br />
femoral<br />
plaque<br />
One<br />
(no=25)<br />
4 +<br />
(16.0%)<br />
4 +<br />
(16.0%)<br />
Number <strong>of</strong> vascular beds affected<br />
Two<br />
(no=23)<br />
11 +<br />
(47.8%)<br />
10 +<br />
(43.5%)<br />
Three<br />
(no=2)<br />
2 +<br />
(100%)<br />
1 +<br />
(50.0%)<br />
F<br />
9.84<br />
4.7<br />
p<br />
0.043<br />
0.095<br />
Table 11: Relation <strong>of</strong> microalbuminuria to number <strong>of</strong> vascular<br />
beds affected.<br />
Positive<br />
Microalbuminuria<br />
One<br />
(no=25)<br />
2 (8.0%)<br />
Number <strong>of</strong> vascular beds affected<br />
Two<br />
(no=23)<br />
12 (52.2%)<br />
Three<br />
(no=2)<br />
2 (100%)<br />
F p<br />
15.16<br />
0.001<br />
46<br />
Case number 11 Group II:<br />
Left carotid duplex:<br />
Figure 5: Show increased left carotid IMT (1.28mm) in female<br />
patient aged 55 with recent MI.<br />
Right carotid duplex:<br />
Figure 6: Show increased right carotid IMT (1.29mm) in<br />
female patient aged 55 with recent MI.<br />
Left femoral duplex:<br />
Figure 7: Show increased left femoral IMT (1.46mm) and<br />
femoral plaque in female patient aged 55 with<br />
recent MI.
Ayman Sadek, et al<br />
Discussion<br />
Although <strong>the</strong> metabolic syndrome unequivocally<br />
predisposes to type 2 diabetes mellitus. Many<br />
investigators <strong>of</strong> cardiovascular diseases consider<br />
this syndrome to be a multidimensional risk factor<br />
for ASCVD [21,22].<br />
Measurements <strong>of</strong> IMT are used in pathophysiological<br />
studies <strong>of</strong> <strong>the</strong> a<strong>the</strong>rosclerotic process, e.g.<br />
in studies <strong>of</strong> <strong>the</strong> factors regulating <strong>the</strong> early development<br />
<strong>of</strong> a<strong>the</strong>rosclerosis in <strong>the</strong> carotid and femoral<br />
arteries. An increase IMT is also used as a marker<br />
<strong>of</strong> generalized a<strong>the</strong>rosclerosis including coronary<br />
a<strong>the</strong>rosclerosis and carotid artery IMT has also<br />
been shown to be associated with coronary a<strong>the</strong>rosclerosis<br />
as measured by coronary angiography in<br />
several studies [23].<br />
The appearance <strong>of</strong> trace amounts <strong>of</strong> albumin<br />
(micro-albuminuria, 30 to 300mg/d) and larger<br />
amounts (frank proteinuria, ≥1g/d) are associated<br />
with an increased risk for renal failure, heart disease,<br />
stroke and cardiovascular mortality [6,8,10,24].<br />
The introduction <strong>of</strong> digital techniques for creating<br />
continuous loops, split-screen and quad screen<br />
presentations enhanced <strong>the</strong> utility <strong>of</strong> echocardiography<br />
for assessment <strong>of</strong> asymptomatic individuals<br />
[25].<br />
I- Relation <strong>of</strong> number <strong>of</strong> single <strong>com</strong>ponents <strong>of</strong><br />
metabolic syndrome and echocardiography:<br />
In this study it was found that <strong>the</strong>re is non<br />
significant difference with increase in <strong>the</strong> number<br />
<strong>of</strong> metabolic <strong>com</strong>ponents as regard presence <strong>of</strong><br />
DD and LVH in <strong>the</strong> form <strong>of</strong> increased LVPWT and<br />
IVST (p>0.05) this may be due to small number<br />
<strong>of</strong> <strong>the</strong> study population however <strong>the</strong> LVEDD and<br />
LVESD showed significant difference (p
Metabolic Syndrome & its Impact on Vascular Damage Extent<br />
<strong>of</strong> <strong>the</strong> metabolic syndrome is associated with an<br />
increase in mean CIMT, Patients who had all five<br />
criteria constituting <strong>the</strong> metabolic syndrome had<br />
<strong>the</strong> largest IMT (1.07mm) <strong>com</strong>pared to patients<br />
with less than five <strong>com</strong>ponents this was supported<br />
by <strong>the</strong> study <strong>of</strong> Wendy et al, which was done to<br />
investigate <strong>the</strong> association <strong>of</strong> metabolic syndrome<br />
with sub-clinical a<strong>the</strong>rosclerosis in young adults<br />
with metabolic syndrome according to NCEP and<br />
WHO criteria and was conducted on 507 non diabetic<br />
subjects and found that increasing numbers<br />
<strong>of</strong> metabolic syndrome <strong>com</strong>ponents were directly<br />
associated with higher <strong>com</strong>posite CIMT (p
Ayman Sadek, et al<br />
cantly across categories (14.3, 18.2, 31.6, 34.1,<br />
32.6%, respectively; p
Metabolic Syndrome & its Impact on Vascular Damage Extent<br />
proper conditions, carotid IMT could be used to<br />
identify person at higher risk than that revealed<br />
by <strong>the</strong> major risk factors alone [1].<br />
VI- Relation between microalbuminuria and extent<br />
<strong>of</strong> vasculopathy:<br />
In <strong>the</strong> present study it was found that <strong>the</strong>re is<br />
a significant difference (p=0.001) in <strong>the</strong> presence<br />
<strong>of</strong> micro-albuminuria and extent <strong>of</strong> vasculopathy<br />
in <strong>the</strong> form <strong>of</strong> number <strong>of</strong> vascular beds affected.<br />
The Monitoring Trends and Determinants <strong>of</strong><br />
Cardiovascular Diseases (MONICA) study investigators<br />
established in 2782 Danish participants<br />
that albuminuria was a potent predictor for <strong>the</strong><br />
development <strong>of</strong> ischemic heart disease, independent<br />
<strong>of</strong> o<strong>the</strong>r traditional risk factors such as male gender,<br />
hypertension, lipids, advancing age and obesity<br />
[10].<br />
Miettinen et al (1996) found an association<br />
between amount <strong>of</strong> urinary protein excretion and<br />
risk <strong>of</strong> stroke and lower extremity amputation in<br />
a cohort <strong>of</strong> subjects that was independent <strong>of</strong> diabetes<br />
status and traditional risk factors [8].<br />
Assessment <strong>of</strong> microalbuminuria in <strong>the</strong> first<br />
week after a myocardial infarction was a strong<br />
predictor for 1-year mortality [40].<br />
In <strong>the</strong> PREVEND Study <strong>the</strong> presence <strong>of</strong> microalbuminuria<br />
in patients with ST-T segment abnormalities<br />
on a resting ECG conferred an increased<br />
(cardiovascular) mortality risk [41].<br />
VII- Study limitations:<br />
It included a single medical center (Ain Shams<br />
University hospitals) with few patients referred<br />
from o<strong>the</strong>r centers all-over Egypt.<br />
The method <strong>of</strong> selecting patients included in<br />
<strong>the</strong> study does not ensure proper randomization.<br />
Limitations <strong>of</strong> duplex scanning: A number <strong>of</strong><br />
technical difficulties remain to be over<strong>com</strong>e in<br />
vascular ultrasound technology. The methodology<br />
is extremely operator and machine dependent and<br />
images can be varied by changing <strong>the</strong> gain settings<br />
on <strong>the</strong> machine. Tortuous and deep vessels may<br />
be difficult to visualize accurately. It is unable to<br />
penetrate areas <strong>of</strong> heavy calcification. This limits<br />
<strong>the</strong> effectiveness <strong>of</strong> vascular ultrasound in advanced<br />
lesions that are <strong>of</strong>ten heavily calcified.<br />
50<br />
Conclusions<br />
From <strong>the</strong> present sudy, <strong>the</strong> followings are concluded:<br />
Metabolic syndrome is a constellation <strong>of</strong> risk<br />
factors for a<strong>the</strong>rosclerosis and <strong>the</strong> increase in traits<br />
<strong>of</strong> metabolic syndrome is associated with increase<br />
in extent <strong>of</strong> vascular damage (CHD-CVA-PVD).<br />
The increase in number <strong>of</strong> metabolic syndrome<br />
traits is associated with increase in LV dimensions.<br />
The increase in number <strong>of</strong> metabolic syndrome<br />
traits is associated with increase in carotid and<br />
femoral IMT and microalbuminurea.<br />
The presence <strong>of</strong> thickened carotid and femoral<br />
IM and presence <strong>of</strong> carotid plaque is associated<br />
with significant increase in extent <strong>of</strong> vascular<br />
damage.<br />
The presence <strong>of</strong> microalbuminurea is associated<br />
with significant increase in extent <strong>of</strong> vascular<br />
damage.<br />
References<br />
1- Adults Treatment Panel III Program (NCEP): Expert Panel<br />
on Detection, Evaluation and Treatment <strong>of</strong> High Blood<br />
Cholesterol in adults. Executive Summary <strong>of</strong> <strong>the</strong> Third<br />
Report <strong>of</strong> <strong>the</strong> National Cholesterol Education. JAMA<br />
2001; 285-2497.<br />
2- Trevisan M, Liu J, Bahsas FB, et al: Syndrome X and<br />
mortality: A population-based study. Risk Factor and Life<br />
Expectancy Research Group. Am J Epidemiol 1998; 148<br />
(10): 958-96.<br />
3- Wilson PW: Estimating cardiovascular disease risk and<br />
<strong>the</strong> metabolic syndrome: A Framingham view. Endocrinol<br />
Metab Clin North Am 2004; 33: 467-481.<br />
4- Ridker PM, Buring JE, Cook NR, Rifai N: C-reactive<br />
protein, <strong>the</strong> metabolic syndrome and <strong>the</strong> risk <strong>of</strong> incident<br />
cardiovascular events: An 8-year follow-up <strong>of</strong> 14 719<br />
initially healthy American women. Circulation 2003; 107:<br />
391-397.<br />
5- Reitzschel ER, De-Buyzere ML, Duprez DA: Interchangeability<br />
<strong>of</strong> carotid and femoral intima media thickness<br />
in risk stratification. International Angiols 2001 Mar;<br />
20 (1): 38-46.<br />
6- Morgensen CE: Microalbuminuria predicts clinical proteinurea<br />
& early mortality maturity-onset dibetes. N Engl<br />
J Med 1984; 310: 356-360.<br />
7- Nelson RG, Pettit DJ, Viberti GC, et al: Effect <strong>of</strong> proteinurea<br />
on mortality in NIDDM. Diabetes 1988; 37:<br />
1499-1504.<br />
8- Miettinen H, Haffner SM, Lehto S, et al: Proteinurea<br />
predicts stroke and o<strong>the</strong>r a<strong>the</strong>rosclerotic vascular disease<br />
events in non-diabetic & noninsulin-dependent diabetic<br />
subjects. Stroke 1996; 27: 2033-2039.
Ayman Sadek, et al<br />
9- O'Leary DH, Polak JF, et al: Carotid-artery intima and<br />
media thickness as a risk factor for myocardial infarction<br />
and stroke in older adults. Cardiovascular Health Study<br />
Collaborative Research Group, New Engl J Met 1999;<br />
340: 14-22.<br />
10- Borch-Johnsen K, Feldt-Rasmussen B, Strandgaard S, et<br />
al: Urinary albumin excretion: An independent predictor<br />
<strong>of</strong> ischemic heart disease. Arterioscler Throm Vasc Biol<br />
1999; 19: 1992-1997.<br />
11- Resnick HE, Russel M, Howard BV: The metabolic<br />
syndrome in American indians: Strong heart study. J<br />
Cardio Metab Syndr Fall 2002; 2 (4): 283-7.<br />
12- Lakka HM, Kannen LK: The metabolic syndrome and<br />
total cardiovascular disease mortality in middle age men,<br />
JAMA 2002; Dec 4, 288 (21): 2709-16.<br />
13- Isomaa B, Almgren P, Tuomi T, et al: Cardiovascular<br />
morbidity and mortality associated with <strong>the</strong> metabolic<br />
syndrome. Diabetes Care 2001; 24: 683-689.<br />
14- Salonen R, Nyyssonen K, et al: Kuopio A<strong>the</strong>rosclerosis<br />
Prevention Study (KAPS)-a population-based primary<br />
preventive trial <strong>of</strong> <strong>the</strong> effect <strong>of</strong> LDL lowering on a<strong>the</strong>rosclerotic<br />
progression in carotid and femoral arteries.<br />
Circulation 1995; 92: 1758-1764.<br />
15- Heiss C, Sharrett AR, Barnes R: Carotid a<strong>the</strong>rosclerosis<br />
measured by B-mode ultrasound in populations associated<br />
with cardiovascular risk factors in <strong>the</strong> ARIC study. Am<br />
J Epidemiol 1991; 123: 250-256.<br />
16- Pignoli P, Tremoli E, Poli A, et al: Intimal plus medial<br />
thickness <strong>of</strong> <strong>the</strong> arterial wall: A direct measurement with<br />
ultrasonic imaging. Circulation 1986; 74: 1399-1406.<br />
17- Bots ML: Wall Thickness <strong>of</strong> <strong>the</strong> Carotid Artery as an<br />
Indicator <strong>of</strong> Generalized A<strong>the</strong>rosclerosis. Rotterdam,<br />
Ne<strong>the</strong>rlands: Erasmus University 1993.<br />
18- Ebrahim S, Papacosta O, Whincup P, et al: Carotid Plaque,<br />
Intima Media Thickness, Cardiovascular Risk Factors<br />
and Prevalent Cardiovascular Disease in Men and Women.<br />
The British Regional Heart Study. Stroke I999; 30: 84I-<br />
85.<br />
19- Eugene D Strandness JR: Duplex scanning in vascular<br />
disorders, edited by D.Eugene Strandness. Lippincott,<br />
Williams Wilkins 2002.<br />
20- De Groot E, Willem F, Terpstra, Albert Wiegman et al:<br />
B-mode ultrasound arterial wall thickness measurements<br />
<strong>of</strong> femoral arterial walls as an additional source <strong>of</strong> information<br />
on a<strong>the</strong>ro-sclerosis progression; In: IMT, Drug &<br />
Stroke 2002; 97-104, editor P.J. Touboul.<br />
21- Hanson RL, Imperatore G, Bennett PH, Knowler WC:<br />
Components <strong>of</strong> <strong>the</strong> ''metabolic syndrome'' and incidence<br />
<strong>of</strong> type 2 diabetes. Diabetes 2002; 51: 3120-3127.<br />
22- Laaksonen DE, Lakka HM, Niskanen LK, et al: Metabolic<br />
syndrome and development <strong>of</strong> diabetes mellitus: Application<br />
and validation <strong>of</strong> recently suggested definitions <strong>of</strong><br />
<strong>the</strong> metabolic syndrome in a prospective cohort study.<br />
Am J Epidemiol 2002; 156: 1070-1077.<br />
23- Chien KL, Liau CS, Chen MF, Lee YT, Jeng JS, Hwang<br />
BS, Su TC: Primary hypercholesterolemia, carotid ath-<br />
51<br />
erosclerosis and insulin resistance among Chinese. Lipids<br />
2008 Feb; 43 (2): 117-24. Epub 2007 Dec 15.<br />
24- Ballard DJ, Humphrey LL, Melton JIII, et al: Epidemiology<br />
<strong>of</strong> persistent proteinurea in type II diabetes mellitus:<br />
Population-based study in Rochester, Minnesota. Diabetes<br />
1988; 37: 405-412.<br />
25- Feigenbaum H: Coronary artery disease in echocardiography,<br />
fifth edition. Lea and Febiger (Malvm, Pennsylvania,<br />
USA) 1994; 447-490.<br />
26- Burchfiel CM, Skelton TN, Andrew ME, et al: Metabolic<br />
syndrome and echocardiographic left ventricular mass in<br />
blacks: The A<strong>the</strong>rosclerosis Risk in Communities (ARIC)<br />
Study. Circulation 2005 Aug 9; 112 (6): 819-27.<br />
27- Chinali M, Devereux RB, Howard BV, et al: Comparison<br />
<strong>of</strong> cardiac structure and function in American Indians<br />
with and without <strong>the</strong> metabolic syndrome (<strong>the</strong> Strong<br />
Heart Study). Am J Cardiol 2004 Jan 1; 93 (1): 40-4.<br />
28- Jobien K. Olijhoek, Yolanda van der Graaf, et al: The<br />
Metabolic Syndrome is associated with advanced vascular<br />
damage in patients with coronary heart disease, stroke,<br />
peripheral arterial disease or abdominal aortic aneurysm,<br />
for <strong>the</strong> SMART Study Group 1 December 2003.<br />
29- Erzen B, Sabovic M, Sebestjen M, Poredos P: Endo<strong>the</strong>lial<br />
dysfunction, intima-media thickness, ankle-brachial pressure<br />
index and pulse pressure in young post-myocardial<br />
infarction patients with various expressions <strong>of</strong> classical<br />
risk factors. Heart Vessels 2007 Jul; 22 (4): 215-22. Epub<br />
2007 Jul 20.<br />
30- Haffner SM, Agostino RD Jr, Saad MF, O'Leary DH,<br />
Savage PJ, Rewers M, Selby J, Bergman RN, Mykkänen<br />
L: Carotid artery a<strong>the</strong>rosclerosis in type-2 diabetic and<br />
nondiabetic subjects with and without symptomatic coronary<br />
artery disease (The Insulin Resistance A<strong>the</strong>rosclerosis<br />
Study). Am J Cardiol 2000 Jun 15; 85 (12): 1395-<br />
400.<br />
31- Nielsen S, Schmitz O, Orskov H, et al: Similar insulin<br />
sensitivity in NIDDM patients with normo-and microalbuminuria.<br />
Diabetes Care 1995; 18: 834-8.<br />
32- Stamler WS, Kazuya S, Yutaka HM: Diabetes, o<strong>the</strong>r risk<br />
factors and 12 year cardiovascular mortality for men<br />
screened in multiple risk factors intervention trial. Diabetes<br />
Care 1993; 3: 471.<br />
33- Zoppini G, Verlato G, Leuzinger C, Zamboni C, Brun E,<br />
Bonora E, Muggeo M: Body mass index and <strong>the</strong> risk <strong>of</strong><br />
mortality in type II diabetic patients from Verona. Int J<br />
Obes Relat Metab Disord 2003 Feb; 27 (2): 281-5.<br />
34- Linhart, Ales, Gariepy, Jerome, Massonneau, Mare, et al:<br />
Carotid intima-media thickness: The ultimate surrogate<br />
end-point <strong>of</strong> cardiovascular involvement in a<strong>the</strong>rosclerosis.<br />
Applied radiology (March) 2000; S.25-39.<br />
35- Barth J, Encino CA: IMT plaque tissue typing and its<br />
relationship to myocardial infarcion. Identifying subclinical<br />
a<strong>the</strong>rosclerotic disease: An evaluation <strong>of</strong> emerging<br />
techniques. International task force for prevention <strong>of</strong><br />
coronary heart disease, task force Symposium Scuol 2003;<br />
February 23.
Metabolic Syndrome & its Impact on Vascular Damage Extent<br />
36- Hollander M, Bots ML, Del Sol AI, et al: Carotid plaques<br />
increase <strong>the</strong> risk <strong>of</strong> stroke and subtypes <strong>of</strong> cerebral infarction<br />
in asymptomatic elderly: The Rotterdam Study.<br />
Circulation 2002; 105: 2872-2877.<br />
37- Chen TT: Essentials <strong>of</strong> cardiac roentgenology. Boston,<br />
Little Brown, 1987. In heart disease, edited by Eugen<br />
Braunwald et al, Vol. 1. W.B. Saunders 1992.<br />
38- Madis Suurkula, et al: A<strong>the</strong>rosclerotic disease in <strong>the</strong><br />
femoral artery in hypertensive patients at high cardiovascular<br />
risks; arteriosclerosis. Thrombosis and Vascular<br />
Biology 1996; 16: 971.<br />
52<br />
39-Antonio Iglesias del Sol, MD, Karel GM Moons, MD,<br />
PhD, et al: Is Carotid Intima-Media Thickness Useful in<br />
Cardiovascular Disease Risk Assessment? The Rotterdam<br />
Study. Stroke 2001; 32: 1532.<br />
40- Berton G, Cordiano R, Palmieri R, et al: Micro-albuminuria<br />
during acute myocardial infarction; a strong predictor for<br />
1-year mortality. Eur Heart J 2001; 22 (16): 1466-75.<br />
41- Diercks GF, Hillege HL, van Boven AJ, et al: Microalbuminuria<br />
modifies <strong>the</strong> mortality risk associated with<br />
electrocardiographic ST-T segment changes. J Am Coll<br />
Cardiol 2002; 40 (8): 1401.
Egypt Heart J 62 (1): 53-61, March 2010<br />
Cardiovascular Risk Factors in Patients with End Stage Renal Failure<br />
on Regular Hemodialysis<br />
YASER AA EL-HENDY, MD; MOHAMED ABDOU, MD*<br />
Aim <strong>of</strong> <strong>the</strong> Work: To investigate <strong>the</strong> relation between both fibrinogen, C-reactive protein (CRP), homocysteine (Hcy),<br />
lipoprotein a (Lpa), as a non traditional cardiovascular (CV) risk factors, plasma lipids, hypertension, smoking and <strong>the</strong> occurrence<br />
and severity <strong>of</strong> ischemic heart disease (IHD) in patients with end stage renal failure (ESRF) on regular hemodialysis (HD) and<br />
wea<strong>the</strong>r diabetic patients are a high risk than non diabetic.<br />
Patients and Methods: 50 ESRF patients on regular HD divided into 3 groups: Group 1 included 10 patients free from IHD<br />
as control.Group II: Included 20 non-diabetic patients. Group III: Included 20 type 2 diabetic patients. Both group II, III suffer<br />
from IHD. All patients were subjected to full history, clinical examination, routine investigations, evaluation <strong>of</strong> fibrinogen,<br />
quantitative CRP, serum Hcy, Lp(a), HDL, LDL cholesterol, triglycerides. 12-leads surface ECG, resting and dobutamine stress<br />
echocardiography (DSE) were also done.<br />
Results: Plasma fibrinogen was significantly higher in group III <strong>com</strong>pared to both group I, II and in group II <strong>com</strong>pared to<br />
group I (F=20.3, p
Cardiovascular Risk Factors in Patients with End Stage Renal Failure<br />
This study aimed to detect <strong>the</strong> relationship<br />
between cardiovascular risk factors as fibrinogen,<br />
CRP, homocysteine, Lp(a), lipid pr<strong>of</strong>ile, blood<br />
sugar, hypertension, smoking and occurrence and<br />
severity <strong>of</strong> ischemic heart disease in uraemic patients<br />
and whe<strong>the</strong>r diabetic patients on regular<br />
hemodialysis are at high risk <strong>of</strong> ischemic heart<br />
disease than non diabetic.<br />
Patients and Methods<br />
This study included 50 chronic renal failure<br />
patients on regular hemodialysis 12 hours per week<br />
divided into 3 sessions for variable periods <strong>of</strong> time<br />
from 3 years to 15 years using filter <strong>of</strong> polysulfone<br />
membrane with effective surface area 1.3m 2 during<br />
<strong>the</strong> study.<br />
They were divided into 3 groups:<br />
Control group (Group 1):<br />
Comprises 10 subjects (5 females and 5 males)<br />
with <strong>the</strong>ir ages ranged from 30 to 64 years. They<br />
were free from ischemic heart disease diagnosed<br />
by history, clinical examination, 12-leads surface<br />
ECG, resting echocardiography and dobutamine<br />
stress echocardiography.<br />
Ischemic heart disease group:<br />
This include a total number <strong>of</strong> 40 patients with<br />
chronic renal failure <strong>of</strong> variable etiologies <strong>com</strong>plaining<br />
<strong>of</strong> recurrent chest pain proved to be <strong>of</strong><br />
cardiac origin by character <strong>of</strong> pain clinically, 12leads<br />
surface ECG, resting echocardiography and<br />
dobutamine stress echocardiography.<br />
The patient group was classified according to<br />
<strong>the</strong> presence or absence <strong>of</strong> diabetes mellitus<br />
into:<br />
Non-diabetic patients (Group II):<br />
Include 20 subjects with chronic renal failure<br />
(14 males and 6 females) with ages ranged from<br />
40 to 65 years.<br />
Diabetic patients (Group III):<br />
Include 20 subjects with chronic renal failure<br />
(12 males and 8 females), with ages ranged from<br />
40 to 65 years. They were type 2 diabetes mellitus<br />
as diabetes started late in age, <strong>the</strong>y were diagnosed<br />
by history, fasting and two hours post-prandial<br />
blood glucose level and glycosylated hemoglobin;<br />
4 <strong>of</strong> <strong>the</strong>m were on oral hypoglycemic and 9 on<br />
insulin <strong>the</strong>rapy and 7 patients did not need treatment.<br />
54<br />
Methods:<br />
All patients were subjected to <strong>the</strong> followings:<br />
1- Thorough history and clinical examination:<br />
Assessment <strong>of</strong> mean arterial pressure:<br />
Mean arterial pressure =<br />
Systolic blood pressure + 2 (diastolic blood pressure)<br />
–––––––––––––––––––––––––––––––––––––––––––––<br />
3<br />
2- 12-Leads surface ECG.<br />
3- Routine laboratory investigations: Blood urea<br />
nitrogen, serum creatinine, serum albumin,<br />
<strong>com</strong>plete blood picture, fasting blood sugar,<br />
serum calcium and phosphorous.<br />
4- Special laboratory investigations: Blood samples<br />
were collected from all 12-hours fasting<br />
subjects and before starting <strong>the</strong> dialysis session;<br />
plasma and serum samples were collected for<br />
estimation <strong>of</strong>:<br />
• Serum total homocysteine with Chemiluminescent<br />
method using Immulite <strong>com</strong>petitive<br />
Immunoassay (DPC, New York, USA).<br />
• Quantitative Lipoprotein (Lpa) and C-reactive<br />
protein (CRP) determination with latex turbidimetry,<br />
Spinreact, S.A., Spain.<br />
• Total cholesterol, LDL cholesterol, HDL cholesterol,<br />
triglycerides.<br />
• Quantitative determination <strong>of</strong> fibrinogen in<br />
plasma by modification <strong>of</strong> <strong>the</strong> Clauss method.<br />
5- Resting echocardiography: The following data<br />
were assessed in each study:<br />
A- Measurement <strong>of</strong> LV dimensions and LV volumes:<br />
M-mode was used to measure septal (IVS) and<br />
posterior wall thickness (PWT) in diastole as well<br />
as LV end systolic diameter (LVSd) and LV end<br />
diastolic diameter (LVDd). We used <strong>the</strong> most <strong>com</strong>monly<br />
used algorithm to calculate LV volumes<br />
(Modified Simpson rule) which derives measurements<br />
by dividing <strong>the</strong> LV by parallel planes into<br />
a number <strong>of</strong> small segments (usually referred as<br />
disks) and summating <strong>the</strong> area <strong>of</strong> <strong>the</strong> individual<br />
disks. The approach has <strong>the</strong> advantage <strong>of</strong> making<br />
no assumption about <strong>the</strong> geometry <strong>of</strong> <strong>the</strong> left ventricle.<br />
B- Assessment <strong>of</strong> left ventricular regional systolic<br />
function as follow (Fig. 1):<br />
The left ventricular wall was divided into 16<br />
segments according to <strong>the</strong> re<strong>com</strong>mendations <strong>of</strong> <strong>the</strong><br />
American Society <strong>of</strong> Echocardiography to evaluate
Yaser AA El-Hendy & Mohamed Abdou<br />
regional LV function. The septal, lateral, anterior<br />
and inferior walls <strong>of</strong> <strong>the</strong> left ventricle were divided<br />
into basal, mid and apical thirds from apical 4chambers<br />
and apical 2-chambers views. The posterior<br />
and anteroseptal walls were divided into<br />
basal and mid segments only from <strong>the</strong> parasternal<br />
long axis view [6].<br />
Long-Axis<br />
Anteroseptal<br />
Mid Base<br />
Mid<br />
Base<br />
Posterior<br />
LAD<br />
LAD (PROX)<br />
A4C<br />
Short-Axis<br />
LAX<br />
A2C<br />
Four Chamber Two Chamber<br />
Apex<br />
Septal<br />
Apex<br />
Lateral<br />
Mid<br />
Apex<br />
Apex Anterior<br />
Mid<br />
Base<br />
Base<br />
Mid<br />
Base<br />
Base<br />
LCX<br />
RCA<br />
Figure 1: Shows 16-segments model <strong>of</strong> <strong>the</strong> left ventricle and<br />
its related blood supply.<br />
Wall motion for each segment was visually<br />
graded using both endocardial motion and wall<br />
thickness with a semiquantitative four-points scoring<br />
system as follow:<br />
Normal or hyperkinesis=1, hypokinetic, marked<br />
reduction <strong>of</strong> endocardial motion or thickening=2,<br />
a kinetic, absence <strong>of</strong> inward motion and thickening=<br />
3, dyskinetic, paradoxic wall motion away from<br />
<strong>the</strong> center <strong>of</strong> <strong>the</strong> left ventricle in systole=4.<br />
The sum <strong>of</strong> <strong>the</strong>se individual segmental scores<br />
is divided by <strong>the</strong> total number <strong>of</strong> <strong>the</strong> interpretable<br />
16 segments to obtain <strong>the</strong> total wall motion score<br />
index.<br />
6- Dobutamine Stress Echocardiography (DSE):<br />
• All studies were performed on a Hewlett-Packard<br />
Sonos 5500 ultrasound system equipped with a<br />
2.5-MHz transducer and were recorded on halfinch<br />
VHS tape.<br />
55<br />
The patients were instructed about <strong>the</strong> test (how<br />
to perform, risk and benefits <strong>of</strong> <strong>the</strong> test) and a<br />
written consent was taken.<br />
β-blockers and rate slowing calcium channel<br />
blockers were withdrawn 48-hours before performing<br />
<strong>the</strong> test.<br />
Blood pressure was recorded at <strong>the</strong> start <strong>of</strong> <strong>the</strong><br />
test and at <strong>the</strong> end <strong>of</strong> each stage with continuous<br />
ECG monitoring all through <strong>the</strong> test.<br />
After <strong>the</strong> test <strong>the</strong> patient was observed for 15<br />
min with continuous ECG monitoring.<br />
Echocardiographic protocol:<br />
• DSE was performed using a standard protocol.<br />
First, a resting echocardiogram was performed<br />
with <strong>the</strong> patient lying in left lateral recumbent<br />
position.<br />
• Echocardiographic imaging was <strong>the</strong>n performed<br />
during <strong>the</strong> intravenous infusion <strong>of</strong> dobutamine<br />
starting at a dose <strong>of</strong> 5μg/kg per minute, which<br />
was increased every 3 minutes to 10 (Low dose),<br />
20 (Intermediate dose), 30 and <strong>the</strong>n 40μg/kg per<br />
minutes (High Dose).<br />
• Images were obtained from <strong>the</strong> standard parasternal<br />
long-axis and short-axis views as well as <strong>the</strong><br />
apical four- and two-chamber views.<br />
DSE images were arranged in quad screen,<br />
continuous loop display, so that <strong>the</strong> baseline, low<br />
dose, peak dose and recovery images <strong>of</strong> each <strong>of</strong><br />
<strong>the</strong> four standard views were displayed simultaneously<br />
for analysis [7]. The test was terminated<br />
prematurely if <strong>the</strong>re was significant new wall<br />
motion abnormalities, significant ST segment depression<br />
or elevation, severe angina pectoris, significant<br />
reduction or elevation in blood pressure,<br />
significant tachyarrhythmia [8].<br />
Propranolol IV (1-3mg) and/or sublingual nitrate<br />
was given if <strong>the</strong>re was side effects.<br />
All studies were read by 2 experienced investigators,<br />
unaware to clinical information. A wall<br />
motion score was assigned to each <strong>of</strong> <strong>the</strong> 16 segments<br />
at every stage <strong>of</strong> <strong>the</strong> test.<br />
Results<br />
The results shown in <strong>the</strong> following Figs. (2-9)<br />
and Tables (1-5).
Cardiovascular Risk Factors in Patients with End Stage Renal Failure<br />
mg/dl<br />
400<br />
350<br />
300<br />
250<br />
200<br />
150<br />
100<br />
50<br />
0<br />
Fibrinogen FBG<br />
Groups<br />
Figure 2: Mean values <strong>of</strong> plasma fibrinogen and fasting blood<br />
glucose between <strong>the</strong> 3 studied groups.<br />
Fibrenogen (mg/dl)<br />
0<br />
1 1.1 1.2 1.3<br />
WMSI<br />
1.4 1.5 1.6 1.7<br />
Figure 4: Correlation between WMSI and plasma fibrinogen<br />
in group II + III.<br />
Serum tHCY (μmol/l)<br />
600<br />
500<br />
400<br />
300<br />
200<br />
100<br />
80<br />
70<br />
60<br />
50<br />
40<br />
30<br />
20<br />
10<br />
r=0.520, p=0.001<br />
r=0.320, p=0.04<br />
0<br />
1 1.1 1.2 1.3<br />
WMSI<br />
1.4 1.5 1.6 1.7<br />
Figure 6: Correlation between WMSI and serum total Hcy<br />
in group II + III.<br />
I<br />
II<br />
III<br />
56<br />
mg/dl<br />
200<br />
180<br />
160<br />
140<br />
120<br />
100<br />
80<br />
60<br />
40<br />
20<br />
0<br />
S.<br />
cholesterol S.HDL<br />
S.TG S.LDL S.Lp(a)<br />
Groups<br />
Figure 3: Mean values <strong>of</strong> lipid parameters between <strong>the</strong> 3<br />
studied groups. Application <strong>of</strong> LSD for <strong>com</strong>parison<br />
in between groups revealed non-significant differences<br />
in all studied lipid parameters in group II<br />
<strong>com</strong>pared to group III, but ANOVA test revealed<br />
significant difference between <strong>the</strong> three-studied<br />
groups.<br />
CRP (mg/dl)<br />
120<br />
100<br />
80<br />
60<br />
40<br />
20<br />
0<br />
1 1.1 1.2 1.3 1.4 1.5 1.6 1.7<br />
WMSI<br />
Figure 5: Correlation between WMSI and serum CRP in<br />
group II.<br />
Lp(a) (md/dl)<br />
80<br />
70<br />
60<br />
50<br />
40<br />
30<br />
20<br />
10<br />
r=0.695, p=0.001<br />
r=0.539, p=0.014<br />
0<br />
1 1.05 1.1 1.15 1.2 1.25 1.3 1.35 1.4<br />
WMSI<br />
Figure 7: Correlation between WMSI and Lp(a) in group III.<br />
I<br />
II<br />
III
Yaser AA El-Hendy & Mohamed Abdou<br />
Duration <strong>of</strong> DM/years<br />
25<br />
20<br />
15<br />
10<br />
5<br />
r=0.585, p=0.007<br />
0<br />
1 1.05 1.1 1.15 1.2<br />
WMSI<br />
1.25 1.3 1.35 1.4<br />
Figure 8: Correlation between WMSI and duration <strong>of</strong> DM in<br />
group III.<br />
57<br />
Figure 9: Factorial analysis for cardiovascular risk factors in<br />
hemodialysis patients.<br />
Table 1: Comparison <strong>of</strong> mean values ± SD <strong>of</strong> some studied parameters between <strong>the</strong><br />
three groups <strong>of</strong> <strong>the</strong> study.<br />
Sex:<br />
Male<br />
Female<br />
Age:<br />
± SD<br />
Range (years)<br />
MAP:<br />
± SD X<br />
Range (mmHg)<br />
Smoking:<br />
± SD X<br />
Range (Cigarette/day)<br />
Median<br />
5<br />
5<br />
I<br />
N=10<br />
48.7±10.8<br />
30-64<br />
93.8±13.8<br />
73-123<br />
0.8±2.5<br />
0-8<br />
0.0<br />
50<br />
50<br />
14<br />
6<br />
II<br />
N=20<br />
70<br />
30<br />
52.95±7.5<br />
40-65<br />
111.1±16.4<br />
83-140<br />
12.1±20.8<br />
0-90<br />
2<br />
12<br />
8<br />
III<br />
N=20<br />
54.1±7.4<br />
40-65<br />
110.1±15.8<br />
83-150<br />
13.1±18<br />
0-60<br />
10<br />
60<br />
40<br />
1.19<br />
F<br />
X 2<br />
1.46<br />
4.58<br />
K<br />
7.48<br />
p<br />
0.55<br />
0.23<br />
0.014<br />
Table 2: Comparison <strong>of</strong> mean Values ± SD <strong>of</strong> some studied laboratory parameters<br />
between <strong>the</strong> three groups <strong>of</strong> <strong>the</strong> study.<br />
CRP:<br />
± SD X<br />
Range (mg/l)<br />
Fibrinogen:<br />
± SD X<br />
Range (mg/dl)<br />
Homocysteine:<br />
± SD X<br />
Range (mmol/l)<br />
FBG:<br />
± SD X<br />
Range (mg/dl)<br />
S.Lp (a):<br />
± SD X<br />
Range (mg/dl)<br />
I<br />
N=10<br />
7.8±7.2<br />
3-26<br />
249.3±63.9<br />
180-398<br />
16.9±6.6<br />
6-28<br />
85.8±8.4<br />
75-100<br />
27.6±4.7<br />
22-36<br />
II<br />
N=20<br />
39.7±28<br />
5-96<br />
337.4±44.4<br />
245-410<br />
34±13.3<br />
15-72<br />
86.9±10.1<br />
70-105<br />
48.6±6.9<br />
40-65<br />
Lp(a)<br />
18.97<br />
III<br />
N=20<br />
22.15±22.1<br />
3-96<br />
377.8±52.9<br />
273-484<br />
35±10.8<br />
20-61<br />
130.5±36.4<br />
70-180<br />
49.75±8.1<br />
41-72<br />
Dyslipidemia<br />
11.58<br />
Fibrinogen<br />
20.014<br />
F<br />
19.57<br />
20. 3<br />
9.72<br />
19.2<br />
6.9<br />
0.02<br />
p<br />
0.001<br />
0.001<br />
0.001<br />
0.001<br />
0.001<br />
FBG<br />
49.436
Cardiovascular Risk Factors in Patients with End Stage Renal Failure<br />
Table 4: Comparison <strong>of</strong> mean values ± SD in dobutamine<br />
stress echocardiography between <strong>the</strong> three studied<br />
groups.<br />
WMAS:<br />
± SD X<br />
Range<br />
WMS:<br />
± SD X<br />
Range<br />
WMS1:<br />
± SD X<br />
Range<br />
I N=10<br />
0<br />
16±0.0<br />
1±0.0<br />
II N=20<br />
4.15±1.66<br />
2-7<br />
20.6±2.1<br />
18-25<br />
1.28±0.13<br />
1.11-1.6<br />
WMAS : Wall motion abnormal segments.<br />
WMS : Wall motion score.<br />
WMSI : Wall motion score index.<br />
Table 3: Comparison <strong>of</strong> mean values ± SD in resting echocardiography between <strong>the</strong><br />
three studied groups.<br />
IVS:<br />
± SD X<br />
Range (mm)<br />
LVPW:<br />
± SD X<br />
Range (mm)<br />
LVDd:<br />
± SD X<br />
Range (mm)<br />
LVSd:<br />
± SD X<br />
Range (mm)<br />
F.S:<br />
± SD X<br />
Range (%)<br />
Discussion<br />
III N=20<br />
3.65±1.26<br />
1-6<br />
19.8±1.3<br />
17-22<br />
1.23±0.08<br />
1.06-1.37<br />
I<br />
N=10<br />
10.1±1.97<br />
8-14<br />
10.2±2.1<br />
6-13<br />
50.8±6.1<br />
38-58<br />
29.5±4.4<br />
20-36<br />
41.3±4.8<br />
35-48<br />
1.6<br />
28.8<br />
27.4<br />
The traditional coronary risk factors are older<br />
age, diabetes, male gender, family history <strong>of</strong> coronary<br />
disease, hypertension, elevated LDL-C decreased<br />
HDL-C, history <strong>of</strong> smoking, physical inactivity,<br />
menopause and psychosocial stress. But<br />
uraemia-related risk factors are o<strong>the</strong>r cardiovascular<br />
disease (CVD) risk factors that increase in prevalence<br />
or severity as renal function declines. These<br />
include, among o<strong>the</strong>rs, albuminuria or proteinuria,<br />
extracellular fluid volume overload, electrolyte<br />
F<br />
p<br />
0.29<br />
0.001<br />
0.001<br />
II<br />
N=20<br />
12.3±2<br />
8-18<br />
12.25±2.1<br />
9-17<br />
52.7±10.2<br />
32-76<br />
31.2±7.96<br />
17-46<br />
41.2±7.2<br />
31-53<br />
IVS : Interventricular septal thickness.<br />
LVPW:<br />
Left ventricular posterior wall thickness.<br />
LVDd : Left ventricular diastolic diameter.<br />
58<br />
Table 5: Multiple regression analysis for cardiovascular risk<br />
factors in hemodialysis patients.<br />
Dyslipidemia<br />
Fibrinogen<br />
t Hcy<br />
Lp(a)<br />
CRP<br />
FBG<br />
III<br />
N=20<br />
11.3±1.3<br />
8-13<br />
10.95±1.96<br />
9-17<br />
52.6±7.2<br />
46-76<br />
31.75±7.5<br />
22-46<br />
39.3±9.3<br />
28-55<br />
β ± SE<br />
4.2±0.002<br />
4.54±0.001<br />
4.52±0.006<br />
2.22±0.008<br />
1.63±0.003<br />
7.4±0.002<br />
F<br />
5.2<br />
3.86<br />
0.19<br />
0.33<br />
0.36<br />
2.19<br />
3.26<br />
0.746<br />
2.76<br />
0.49<br />
3.527<br />
0.034<br />
0.002<br />
0.46<br />
0.008<br />
0.62<br />
0.001<br />
95% CI<br />
0.0-0.008<br />
0.002-0.007<br />
0.008-0.017<br />
0.006-0.039<br />
0.005-0.008<br />
0.003-0.012<br />
• It shows that fasting blood glucose, fibrinogen, Lpa and dyslipidemia<br />
are independent cardiovascular risk factors in CRF patients on<br />
hemodialysis treatment.<br />
imbalance, hypertriglyceridemia, elevated Lp (a),<br />
hyperhomocysteinaemia, markers <strong>of</strong> inflammation<br />
or infection; CRP, increased oxidant stress, thrombogenic<br />
factors, malnutrition, anaemia and o<strong>the</strong>r<br />
uraemic toxins [9].<br />
Hypertension appeared as a major risk factor<br />
for occurrence <strong>of</strong> ischemic heart disease as <strong>the</strong>re<br />
was significant increase in <strong>the</strong> mean arterial blood<br />
pressure in both group II and III <strong>com</strong>pared to <strong>the</strong><br />
control group. This was in consistent with Takeda<br />
et al (2004) [10] who found that hypertension is a<br />
t<br />
p<br />
0.009<br />
0.02<br />
0.82<br />
0.72<br />
0.7<br />
LVSd:<br />
Left ventricular systolic diameter.<br />
FS : Fractional shortening.<br />
p<br />
S<br />
S<br />
NS<br />
S<br />
NS<br />
S
Yaser AA El-Hendy & Mohamed Abdou<br />
potent risk factor for cardiovascular disease in<br />
hemodialysis patients, as in <strong>the</strong> general population,<br />
whereas <strong>the</strong>re is no association <strong>of</strong> hypertension<br />
with mortality. Conversely, a low incidence <strong>of</strong> CV<br />
death has been noted in dialysis patients with<br />
optimal blood pressure control [11].<br />
The obtained significant association between<br />
cigarette smoking and ischemic heart disease in<br />
group II and group III <strong>com</strong>pared to control group<br />
obviate <strong>the</strong> role <strong>of</strong> smoking in susceptibility to<br />
IHD as smoking may be especially a<strong>the</strong>rogenic in<br />
uraemic patients because it enhances free radical<br />
generation and subsequent lipid peroxidation [12],<br />
which is already increased in uraemic patients [13].<br />
There was significant increase in serum LDLcholesterol<br />
with significant decrease HDLcholesterol<br />
level in group II and group III in <strong>com</strong>parison<br />
to <strong>the</strong> control group. This result is in<br />
agreement with findings <strong>of</strong> Avram et al (1992) [14].<br />
Dyslipidemia, was an independent risk factor<br />
in multiple regression analysis for ischemic heart<br />
disease in hemodialysis patients in <strong>the</strong> present<br />
work.<br />
In uremia, <strong>the</strong> catabolism <strong>of</strong> Lp(a) is diminished<br />
[15]. The highly significant increase in serum Lp(a)<br />
in group II, III <strong>com</strong>pared to <strong>the</strong> control group may<br />
be due to decreased excretion <strong>of</strong> apolipoprotein(a)<br />
degradation products in patients with CRF as well<br />
as inflammation and <strong>the</strong> phenotype difference <strong>of</strong><br />
apolipoprotein(a) in <strong>the</strong> studied group. In our study<br />
Lp(a) concentration was an independent risk factor<br />
for ischemic heart disease in hemodialysis patients<br />
in multiple regression analysis and a significant<br />
positive correlation between wall motion score<br />
index and Lp(a) was present in group III. This was<br />
in agreement with findings <strong>of</strong> Longenecker et al<br />
(2004) [16] who found that both high Lp(a) concentration<br />
and low molecular weight (LMW) Apoa<br />
is<strong>of</strong>orms predicted a<strong>the</strong>rosclerotic cardiovascular<br />
disease events in dialysis patients.<br />
The obtained significant increase in plasma<br />
fibrinogen level and in IHD patients on hemodialysis<br />
in group II and group III <strong>com</strong>pared to<br />
control group could be partially related to inflammation<br />
as hemodialysis acts as a repeated stimulus<br />
for an inflammatory response. This was in agreement<br />
with findings <strong>of</strong> Zoccali et al (2003) [17] who<br />
found that fibrinogen is an independent risk factor<br />
for overall and cardiovascular mortality in patients<br />
with ESRD. Hyperfibrinogenaemia revealed a<br />
59<br />
strong independent a<strong>the</strong>rogenic risk factor in<br />
hemodialysis patients, as already observed in <strong>the</strong><br />
general population [18].<br />
An increased plasma fibrinogen level has been<br />
consistently reported in dialysis patients in association<br />
with evidence <strong>of</strong> endo<strong>the</strong>tial dysfunction<br />
characterized by con<strong>com</strong>itant high plasma concentrations<br />
<strong>of</strong> proconvertin and type 1 plasminogen<br />
activator inhibitor, (PAI-1); all factors that contribute<br />
to <strong>the</strong> initial steps <strong>of</strong> a<strong>the</strong>rogenesis [19]. Fibrinogen<br />
and PAI-1 are acute phase proteins which<br />
rise in response to various stimuli including cytokines,<br />
especially IL-1 and TNFα, which indeed are<br />
released following monocyte activation, a process<br />
which has recently be shown to be part <strong>of</strong> <strong>the</strong><br />
uraemia-associated immune dysregulation [20]. The<br />
obtained elevation <strong>of</strong> plasma fibrinogen level was<br />
an independent risk factor for ischemic heart disease<br />
in hemodialysis patients in multiple regression<br />
analysis and a significant positive correlation<br />
between wall motion score index and plasma fibrinogen<br />
was present in all ischemic patients (group<br />
II, III).<br />
In 2003 Lee BJ et al [21] demonstrated that<br />
hyperhomocysteinemia is a prominent risk factor<br />
<strong>of</strong> a<strong>the</strong>rosclerotic cardiovascular accidents. The<br />
elevated serum Hcy in ischemic patients (group<br />
II, III) could be due to accumulation <strong>of</strong> uraemic<br />
toxins that lead to impairment in <strong>the</strong> enzymes <strong>of</strong><br />
Hcy metabolism. These results go in harmony with<br />
<strong>the</strong> results obtained by Chauveau et al (1993) [22]<br />
who realized an increased serum total Hcy level<br />
in non-dialysed and in dialysis CRF patients and<br />
a relationship between elevated plasma homocysteine<br />
concentration and occurrence <strong>of</strong> a<strong>the</strong>rosclerotic<br />
cardiovascular accidents was evidenced in<br />
dialysis patients [23]. In <strong>the</strong> present study a significant<br />
positive correlation between WMSI and serum<br />
total Hcy was present in all ischemic patients<br />
(group II, III).<br />
Buccianti et al (2004) [24] found that Hcy is a<br />
strong independent mortality predictor in HD patients<br />
with a 3% increase in mortality for each<br />
1μmol/L increase in plasma Hcy concentration.<br />
The significant increase in serum CRP in<br />
hemodialysis patients with cardiac ischemia in<br />
group II and group III <strong>com</strong>pared to control group<br />
could be related to inflammation as hemodialysis<br />
acts as a repeated stimulus for an inflammatory<br />
response. This was in agreement with Zimmermann<br />
et al (1999) [25] who found that a considerable
Cardiovascular Risk Factors in Patients with End Stage Renal Failure<br />
number <strong>of</strong> hemodialysis patients exhibit an activated<br />
acute phase response (CRP), which is closely<br />
related to high levels <strong>of</strong> a<strong>the</strong>rogenic vascular risk<br />
factors and cardiovascular death.<br />
Genetic factors may significantly influence <strong>the</strong><br />
immune response, <strong>the</strong> levels <strong>of</strong> inflammatory markers,<br />
as well as <strong>the</strong> prevalence <strong>of</strong> vascular calcification<br />
in this patient group [26].<br />
The prognostic value <strong>of</strong> serum CRP on <strong>the</strong><br />
occurrence <strong>of</strong> myocardial infarction, sudden death,<br />
and stroke has been reported in <strong>the</strong> general population<br />
[27]. Consequently, CRP is a possible predictor<br />
<strong>of</strong> death in dialysis patients [28].<br />
The significant positive correlation between<br />
WMSI and serum CRP in group II clarify its role<br />
in <strong>the</strong> development <strong>of</strong> myocardial ischemia.<br />
Foley et al (1997) [29], found that diabetic<br />
dialysis patients had higher rates <strong>of</strong> do novo<br />
ischemic heart disease, overall mortality and cardiovascular<br />
mortality than non-diabetic dialysis<br />
patients. The 2-3 fold increase in CVD risk (attributable<br />
to diabetes) multiplied by <strong>the</strong> risk associated<br />
with ESRD results in an increased CVD risk <strong>of</strong><br />
around 50-fold in patients with ESRF caused by<br />
diabetic nephropathy [30]. In <strong>the</strong> present study,<br />
<strong>the</strong>re was significant increase in fasting blood<br />
glucose level in diabetic ischemic heart disease<br />
patients on hemodialysis <strong>com</strong>pared to <strong>the</strong> control<br />
group. Blood glucose level was an independent<br />
risk factor for ischemic heart disease in<br />
hemodialysis patients in multiple regression analysis<br />
and a significant positive correlation between<br />
WMSI and <strong>the</strong> duration <strong>of</strong> diabetes was present<br />
in group III.<br />
The significant increase in inter-ventricular<br />
septum dimension in hemodialysis patients with<br />
cardiac ischemia (group II, III) <strong>com</strong>pared to <strong>the</strong><br />
control group and in left ventricular posterior wall<br />
dimension in group II <strong>com</strong>pared to <strong>the</strong> control<br />
group may be due to uncontrolled hypertension.<br />
On <strong>the</strong> o<strong>the</strong>r hand left ventricular hypertrophy<br />
(LVH) predisposes to ischemic symptoms by reducing<br />
coronary reserve as reported by Yasuda et<br />
al [31].<br />
There was non significant difference in left<br />
ventricular end systolic and end diastolic dimensions<br />
in hemodialysis patients with cardiac ischemia<br />
<strong>com</strong>pared to <strong>the</strong> control group.<br />
Lastly, factorial analysis for CV risk factors in<br />
60<br />
hemodialysis patients concluded that diabetes<br />
mellitus was <strong>the</strong> most important cardiovascular<br />
risk factor for occurrence <strong>of</strong> cardiac ischemia in<br />
hemodialysis patients, fibrinogen is <strong>the</strong> second<br />
one, Lp(a) is <strong>the</strong> third and dyslipidemia is <strong>the</strong><br />
fourth one risk factor for occurrence <strong>of</strong> cardiac<br />
ischaemia in haemodialysis patients.<br />
In conclusion, a considerable number <strong>of</strong> traditional<br />
and non traditional risk factors for CV ischemia<br />
may be present in hemodialysis patients;<br />
usually one patient can be affected simultaneously<br />
by several risk factors leading to poor long term<br />
survival. Uncontrolled DM, elevated plasma fibrinogen,<br />
Lp(a), dyslipidemia are <strong>the</strong> most risk factors.<br />
So it can be re<strong>com</strong>mended that early evaluation<br />
and management <strong>of</strong> <strong>the</strong> specific cardiovascular<br />
risk pr<strong>of</strong>ile <strong>of</strong> each patient with ESRF may improve<br />
long term survival.<br />
References<br />
1- Parfrey PS: Cardiac disease in dialysis patients: Diagnosis,<br />
burden <strong>of</strong> disease, prognosis, risk factors and management.<br />
Nephrol Dial Transplant 2000; 15 (Suppl 5): 58.<br />
2- Levey AS, Beto JA, Coronado BE, et al: Controlling <strong>the</strong><br />
epidemic <strong>of</strong> cardiovascular disease in chronic renal disease:<br />
What do we know? What do we need to learn? Where do<br />
we go. Am J Kidney Dis 1998; 32 (5): 853-906.<br />
3- Parfrey PS, Foley RN: The clinical epidemiology <strong>of</strong><br />
cardiac disease in chronic renal failure. J Am Soc Nephrol<br />
1999; 10: 1606.<br />
4- Lawrence de Konig, Werstuck GH, Zhou J: Hyperhomocysteinemia<br />
and its role in <strong>the</strong> development <strong>of</strong> as<strong>the</strong>rosclerosis.<br />
Clin Biochem 2003; 36: 431-41.<br />
5- Luke RG: Chronic renal failure-a vasculopathic state.<br />
New Engl J Med 1998; 339: 841.<br />
6- Schiller NB, Shah PM, Crawford M, et al: Re<strong>com</strong>mendations<br />
for quantification <strong>of</strong> <strong>the</strong> left ventricle by twodimensional<br />
echocardiography. American Society <strong>of</strong><br />
Echocardiography Committee on Standards, Sub<strong>com</strong>mittee<br />
on Quantification <strong>of</strong> Two-Dimensional Echocardiograms.<br />
J Am Soc Echocardiogr 1989; 2: 358-67.<br />
7- Picano E, Mathias W Jr, Pingitore A, et al: Safety and<br />
tolerability <strong>of</strong> dobutamine-atropine stress<br />
echocardiography: A prospective, multicenter study: Echo<br />
Dobutamine International Cooperative Study Group.<br />
Lancet 1994; 344: 1190-1192.<br />
8- Sicari R, Picano E, Landi P, et al: Prognostic value <strong>of</strong><br />
dobutamine-atropine stress echocardiography early after<br />
acute MI. J Am Coll Cardiol 1997; 29: 254-60.<br />
9- Sarnak MJ, Levey AS: Cardiovascular disease and chronic<br />
renal disease: A new paradigm. Am J Kidney Dis 2000;<br />
35 (Suppl 1): S117.<br />
10- Takeda A, Toda T, Fujii T, et al: Discordance <strong>of</strong> influence<br />
<strong>of</strong> hypertension on mortality and cardiovascular risk in<br />
haemodialysis patients. Am J Kidney Dis 2004; 45 (1):<br />
112.
Yaser AA El-Hendy & Mohamed Abdou<br />
11- Charra B, Calemard E, Ruffet M, et al: Survival as an<br />
index <strong>of</strong> adequacy <strong>of</strong> dialysis. Kidney Int 1992; 41: 1286.<br />
12- Duthie GG, Arthur JR, Beattie JA, et al: Cigarette smoking,<br />
antioxidants, lipid peroxidation, and coronary heart disease.<br />
Ann N Y Acad Sci 1993; 686: 120.<br />
13- Maggi E, Bellazzi R, Falaschi F, et al: Enhanced LDL<br />
oxidation in uraemic patients: An additional mechanism<br />
for accelerated a<strong>the</strong>rosclerosis? Kidney Int 1994; 45: 876.<br />
14- Avram MM, Goldwasser P, Burrell DE, et al: The uraemic<br />
dyslipidemia: A cross-sectional and longitudinal study.<br />
Am J Kidney Dis 1992; 20: 324.<br />
15- Frischmann ME, Kronenberg F, Trenkwalder E, et al: In<br />
vivo turnover study demonstrates diminished clearance<br />
<strong>of</strong> lipoprotein(a) in hemodialysis patients. Kidney Int<br />
2007; 71: 1036-1043.<br />
16- Longenecker JC, Klag MJ, Marcovina SM, et al: High<br />
lipoprotein(a) levels and small apolipoprotein(a) size<br />
prospectively predict cardiovascular events in dialysis<br />
patients. J Am Soc Nephrol 2004; 16 (6): 1539.<br />
17- Zoccali C, Mallamaci F, TripepI G, et al: Fibrinogen,<br />
mortality and incident cardiovascular <strong>com</strong>plications in<br />
end-stage renal failure. Journal <strong>of</strong> Internal Medicine 2003;<br />
254: 132.<br />
18- Wilhelmsen L, Svardsudd K, Korsan-Bengtsen K, et al:<br />
Fibrinogen as a risk factor for stroke and myocardial<br />
infarction. N Engl J Med 1984; 311: 501.<br />
19- Tomura S, Nakamura Y, Doi M, et al: Fibrinogen, coagulation<br />
factor VII, tissue plasminogen activator, plasminogen<br />
activator inhibitor-1 and lipid as cardiovascular risk<br />
factors in chronic haemodialysis and continuous ambulatory<br />
peritoneal dialysis patients. Am J Kidney Dis 1996;<br />
27: 848.<br />
20- Descamps-Latscha B, Herbelin A, Nguyen AT, et al:<br />
Balance between IL-1 beta, TNF-alpha and <strong>the</strong>ir specific<br />
inhibitors in chronic renal failure and maintenance dialysis.<br />
Relationships with activation markers <strong>of</strong> T cells, B cells<br />
and monocytes. J Immunol 1995; 154: 882.<br />
61<br />
21- Lee BJ, Lin PT, Liaw YP, et al: Homocysteine and risk<br />
<strong>of</strong> coronary artery disease. Nutrition 2003; 19: 577-83.<br />
22- Chauveau P, Chadefaux B, Coudé M, et al: Hyperhomocysteinemia,<br />
a risk factor for a<strong>the</strong>rosclerosis in chronic<br />
uraemic patients. Kidney Int 1993; 43 (Suppl 41): S72.<br />
23- Bostom AG, Shemin D, Verhouf P, et al: Elevated fasting<br />
total plasma homocysteine levels and cardiovascular<br />
disease out<strong>com</strong>es in maintenance dialysis patients. Arterioscler<br />
Thromb Vasc Biol 1997; 17: 2554.<br />
24- Buccianti G, Baragetti I, Bamonti F, et al: Plasma homocysteine<br />
levels and cardiovascular mortality in patients<br />
with end-stage renal disease. J Nephrol 2004; 17: 405.<br />
25- Zimmermann J, Herrlinger S, Pruy A, et al: Inflammation<br />
enhances cardiovascular risk and mortality in haemodialysis<br />
patients. Kidney Int 1999; 55: 648.<br />
26- Stenvinkel P, Pecoits-Filho R, Lindholm B: For <strong>the</strong><br />
DialGene Consortium: Gene polymorphism association<br />
studies in dialysis: The nutrition-inflammation axis. Semin<br />
Dial 2005; 18: 322-330.<br />
27- Ridker PM, Glynn RJ, Henneken CH: C-reactive protein<br />
adds to <strong>the</strong> predictive value <strong>of</strong> total and HDL cholesterol<br />
in determining risk <strong>of</strong> first myocardial infarction. Circulation<br />
1998; 97: 2007.<br />
28- Bergstrom J, Heimburger O, Lindholm B, et al: Elevated<br />
serum C-reactive protein is a strong predictor <strong>of</strong> increased<br />
mortality and low serum albumin in haemodialysis (HD)<br />
patients. J Am Soc Nephrol 1995; 6: 573.<br />
29- Foley RN, Culleton BF, Parfrey PS, et al: Cardiac disease<br />
in diabetic end-stage renal disease. Diabetologia 1997;<br />
40: 1307.<br />
30- Jardine AG, McLaughlin K: Cardiovascular <strong>com</strong>plication<br />
<strong>of</strong> renal disease. Heart 2001; 86: 459.<br />
31- Yasuda K, Kasuga H, Aoyama T, et al: Comparison <strong>of</strong><br />
Percutaneous Coronary Intervention with Medication in<br />
<strong>the</strong> Treatment <strong>of</strong> Coronary Artery Disease in Hemodialysis<br />
Patients J Am Soc Nephrol 2006; 17: 2322-2332.
Egypt Heart J 62 (1): 63-68, March 2010<br />
White Coat Hypertension and Target Organ Damage<br />
HAMZA KABIL, MD; METWALLY EL-EMARY, MD; AHMED ABDEL-MONEIM, MD;<br />
ABDEL-RAHMAN SAMRA, MBCh<br />
Introduction: Twenty-four hour non-invasive ambulatory blood pressure monitoring (ABPM) has evolved as a research<br />
tool <strong>of</strong> limited clinical use into an important tool for stratifying cardiovascular risk and guiding <strong>the</strong>rapeutic decisions. Its clinical<br />
use focuses on identifying patients with white coat hypertension (WCH), but accumulated evidence now points to greater<br />
prognostic significance in detecting risk for target organ damage <strong>com</strong>pared with that <strong>of</strong> <strong>of</strong>fice blood pressure measurement.<br />
Aim: This study is planned to evaluate <strong>the</strong> impact <strong>of</strong> WCH on <strong>the</strong> target organs in order to determine if this type <strong>of</strong><br />
hypertension is really a benign condition or not.<br />
Patients and Methods: This study was conducted in <strong>the</strong> Cardiology department in Benha University Hospitals. It included<br />
20 patients with white coat hypertension diagnosed by both <strong>of</strong>fice and ambulatory blood pressure measurements, and ano<strong>the</strong>r<br />
20 patients with known sustained hypertension with blood pressure ≥140/90mmHg and not receiving any medical treatment.<br />
All patients underwent a history-taking, clinical examination taking into consideration <strong>of</strong>fice and home blood pressure<br />
measurement, ambulatory blood pressure monitoring for 24 hours, a 12-lead electrocardiogram, echocardiography, and laboratory<br />
investigations.<br />
Results: When taking <strong>the</strong> demographic data <strong>of</strong> <strong>the</strong> patients into consideration, <strong>the</strong> two groups were equally matched, with<br />
a significantly lower age prevalent in those with WCH (37±13.3 years Vs. 52.1±8.4, p
White Coat Hypertension & Target Organ Damage<br />
2- At least two measurements outside <strong>the</strong> physicians<br />
<strong>of</strong>fice with blood pressure lower than 140/<br />
90mmHg.<br />
3- Daytime ambulatory blood pressure lower than<br />
135/85mmHg (Verdecchia et al, 2003).<br />
Patients with white-coat hypertension may<br />
receive an incorrect diagnosis <strong>of</strong> sustained hypertension,<br />
this phenomenon has been reported in as<br />
many as 15-30% <strong>of</strong> patients labeled and treated as<br />
hypertensives, nearly one in every five patients,<br />
may receive antihypertensive drugs inappropriately<br />
(Pickering et al, 1988).<br />
Patients and Methods<br />
This study was conducted in <strong>the</strong> Cardiology<br />
Department in Benha University Hospital included<br />
20 patient with White Coat hypertension diagnosed<br />
by both clinic and ambulatory blood pressure<br />
measurements. This group was <strong>com</strong>pared with<br />
sustained hypertension (SH) group which included<br />
20 patients diagnosed as having S.H. equal or<br />
above 140/90mmHg and have not received any<br />
antihypertensive treatment before.<br />
All patients underwent: Full history-taking,<br />
thorough clinical examination with stress on <strong>of</strong>fice<br />
and home Blood pressure measurements, ambulatory<br />
Blood Pressure Monitoring using a non invasive<br />
recorder (SCHILIER Blood Pressure Recorder<br />
BR-102) for consecutive 24-h, resting 12-lead<br />
electrocardiogram (ECG), microalbuminuria and<br />
echo-doppler study.<br />
Results<br />
The present study included a group <strong>of</strong> 40 patients<br />
who presented to our out patient clinics <strong>of</strong><br />
Benha University Hospital by hypertension. By<br />
non-invasive ambulatory blood pressure monitoring<br />
<strong>the</strong>y were classified into white Coat Hypertension<br />
(WCH) including 20 patients (13 females and 7<br />
males) and Sustained Hypertension group, including<br />
20 patients (9 females and 11 males).<br />
There was a statistically significant difference<br />
between both groups regarding age distribution<br />
(p
Hamza Kabil, et al<br />
24-h heart rate: There was a statistically significant<br />
difference between both groups (p
White Coat Hypertension & Target Organ Damage<br />
Table 5: Complications <strong>of</strong> hypertension among <strong>the</strong> studied<br />
groups.<br />
Studied Groups<br />
Complications<br />
Retinopathy<br />
C.V. Stroke<br />
Ischemic Heart<br />
Disease<br />
Renal Impairment<br />
WCH<br />
(n=20)<br />
No.<br />
11<br />
1<br />
2<br />
0<br />
%<br />
55.0<br />
5.0<br />
10.0<br />
0.0<br />
Discussion<br />
SH<br />
(n=20)<br />
No.<br />
White-coat hypertension is a phenomenon<br />
whereby some patients who apparently have raised<br />
BP actually have normal BP when measurement<br />
is repeated away from medical environment<br />
(Michael et al, 2002). Those patients may receive<br />
an incorrect diagnosis <strong>of</strong> sustained hypertension.<br />
This phenomenon has been reported in as many as<br />
15-35% <strong>of</strong> patients labeled and treated as hypertensive<br />
(Pickering et al, 1988). Target organ damage<br />
was observed in a population with white-coat<br />
hypertension (Verdecchia et al, 1996).<br />
This study was planned to evaluate <strong>the</strong> impact<br />
<strong>of</strong> WCH on <strong>the</strong> target organs in order to determine<br />
if this type <strong>of</strong> hypertension is really benign or not?.<br />
This study showed that <strong>the</strong>re was a statistically<br />
significant difference between both WCH group<br />
and SH groups (p0.05), in relation to smoking among males as<br />
shown in Table (1), <strong>the</strong>se results were supported<br />
by <strong>the</strong> study carried out by Hernandez del Rey et<br />
al, 1997, who showed that <strong>the</strong>re was no difference<br />
between WCH and SH regarding prevalence <strong>of</strong><br />
smoking.<br />
13<br />
3<br />
6<br />
1<br />
%<br />
65.0<br />
15.0<br />
30.0<br />
5.0<br />
Z<br />
0.645<br />
1.054<br />
2.372<br />
1.013<br />
p<br />
>0.05<br />
>0.05<br />
>0.05<br />
>0.05<br />
66<br />
This study showed that <strong>the</strong>re was a statistically<br />
significant difference between both groups<br />
(p
Hamza Kabil, et al<br />
group and <strong>the</strong> SH group (p0.05), where <strong>the</strong> mean value <strong>of</strong> clinic<br />
HR in <strong>the</strong> WCH group was (90.9±6.4) and that in<br />
<strong>the</strong> SH group was (91.3±5.6), and <strong>the</strong> mean value<br />
<strong>of</strong> nighttime HR in <strong>the</strong> WCH group was (71.9±5.7)<br />
and that in <strong>the</strong> SH group was (72.1±6.4). Also,<br />
<strong>the</strong>re was a statistically significant difference<br />
between both <strong>the</strong> WCH group and <strong>the</strong> SH group<br />
regarding, 24-h and daytime ambulatory HR values<br />
(p
White Coat Hypertension & Target Organ Damage<br />
2- Bjorklund K, Lind L, Vessby B, et al: Different metabolic<br />
predictors <strong>of</strong> white-coat and sustained hypertension over<br />
a 20-year follow-up period: A population-based study <strong>of</strong><br />
elderly men, Circulation 2002; 106: 63-68.<br />
3- Cerasola G, Cottone S, Nardi E, D'Ignoto G, et al: Chair<br />
<strong>of</strong> Internal Medicine and Hypertension Center, University<br />
<strong>of</strong> Palermo, Italy 1995.<br />
4- Fondo de Investigation Sanitaria Ministerio de Sanidad<br />
Y Consumo: (Proyecto 95/26: 0-10); Beca VITA de Invetigacion<br />
en Atencion Primaria 1995.<br />
5- Greece: 1 st Cardiology Department <strong>of</strong> A<strong>the</strong>ns University,<br />
Hippokration Hospital, A<strong>the</strong>ns Greece.<br />
6- Hernandez R del Ray, Armario P, Cardenas G, et al: Red<br />
Cross Hospital Liobregat. Barcelona. Spain 1997.<br />
7- Jose A Alzpunja, Egle Silva, Glodys Masstre, et al: Cardiovasculares,<br />
Maracaibo, Venezuela, La Universidad del<br />
Zulla. Maracaibo, Venezuela 2002.<br />
8- Julius S, Mejia A, Jones K, et al: "White coat 'versus'<br />
sustained" borderline hypertension in Tecumseh Mi Hypertens<br />
1990; 16: 617-62.<br />
9- Karponou EA, Vyssoulis GP, Chrysohoou CA, et al: 1 st<br />
Cardiology Department, Onassis Cardiac Surgery Center,<br />
A<strong>the</strong>ns 2004.<br />
10- Kazue Eguchi, Kazuomi Kario, Satoshi Hoshide, Masato<br />
Morinari Joji Ishikawa, Kazuyuki Shimada, et al: Department<br />
<strong>of</strong> Cardiology. Jichi Medical School, Tochigi-Ken,<br />
Japan 2004.<br />
11- Khattar RS, Senior R, Lahiri A: Cardiovascular out<strong>com</strong>e<br />
68<br />
in white-coat versus sustained mild hypertension: A 10year<br />
follow-tip study, Circulation 1998; 89: 1892-1897.<br />
12- Michael E, Ernst, Pharm D, George R, Bergus: Non inasive<br />
24-hour Ambulatory Bp monitoring overview <strong>of</strong> Technology<br />
clinical application, Pharmaco<strong>the</strong>rapy 2002; 22 (5)<br />
© 2002 Pharmaco<strong>the</strong>rapy Publications.<br />
13- Mancia G, Parti G, Pomidossi G, et al: Altering reaction<br />
and rise in blood pressure during measurements by physician<br />
and nurse, Hypertension 1987; 9: 209-215.<br />
14- Opsahl JA, Abraham PA, Halstenson CE, Keane WF:<br />
Correlation <strong>of</strong> <strong>of</strong>fice and ambulatory blood pressure<br />
measurements with urinary albumin and N-acetyl-B-Dglucosaminidase<br />
excretions in essential hypertension ,<br />
Am J Hypertens 1988; 11: 7S-120S.<br />
15- Peckering TG, James GD, Boddie C, et al: How <strong>com</strong>mon<br />
is white coat hypertension? JAMA 1988; 259 (2): 225-<br />
228.<br />
16- Pierdomenico SD, Guglielmi MD, Lopenna D, et al:<br />
Hypertension Unit, chair <strong>of</strong> Internal Medicine, University<br />
<strong>of</strong> Chieti, Italy 1995.<br />
17- Verdecchia P, O'Brein E, Pickering, et al: When can <strong>the</strong><br />
practicing physician suspect white coat hypertension?<br />
Statement from <strong>the</strong> Working Group on Blood Pressure<br />
Monitoring <strong>of</strong> <strong>the</strong> European Society <strong>of</strong> Hypertension, Am<br />
J Hypertens 2003; 16: 87-91.<br />
17- Erdecchia P, Schillaci G, Borgioni C, Ciucci A, et al:<br />
White Coat hypertension. Lancet 1996; 348: 1444-5.<br />
18- Sasaki K, Kushiro T, Jin Inoue, Asgami T, Takahashi A,<br />
et al: Surugadai Nihon University Hospital, International<br />
Christian University Tokyo, Japan 1997.
Egypt Heart J 62 (1): 69-76, March 2010<br />
Microalbuminuria and Subclinical Cardiac Structural Changes<br />
Relation to Isolated Systolic Hypertension in Elderly Patients<br />
HAMZA KABIL, MD*; EL-METWALLY EL-SHAHAWY, MD; AMR AFIFI, MD;<br />
HSASSAN GALAL, MD; ASHRAF TALAAT, MD<br />
Isolated systolic hypertension is <strong>com</strong>mon in elderly people and accounts for more than 50% <strong>of</strong> all cases with hypertension<br />
above <strong>the</strong> age <strong>of</strong> 65 years. Microalbuminuria represents an early marker <strong>of</strong> cardiac structural damage.<br />
The Aim <strong>of</strong> this Work: Is to study <strong>the</strong> relationship between micro albuminuria and subclinical cardiac structural changes<br />
septal wall thickness (SWT), left ventricular mass (LVM) and left ventricular mass index (LVMI) in isolated systolic hypertension<br />
in elderly patients.<br />
Results: Showed significant positive correlation between microalbuminuria and cardiac structural changes (LVMI-p=0.01,<br />
SWT-p=0.01 and LVM-p=0.01). There was a significant positive correlation between <strong>the</strong> duration <strong>of</strong> hypertension and<br />
microalbuminuria, LVM (p=0.02) and LVH (p=0.01). Also, <strong>the</strong>re was a significant positive correlation between age <strong>of</strong> patients<br />
and LVM (p=0.01) and LVH (p=0.01).<br />
Conclusion: Taken toge<strong>the</strong>r this study showed that microalbuminuria represents an early marker <strong>of</strong> cardiac structural<br />
changes in isolated systolic hypertension in elderly patients. It is considered one <strong>of</strong> <strong>the</strong> new associated risk factors <strong>of</strong> hypertension.<br />
Cardiovascular prognosis depends not only on <strong>the</strong> blood pressure level but also on <strong>the</strong> presence <strong>of</strong> target organ damage. So we<br />
re<strong>com</strong>mend early detection <strong>of</strong> microalbuminuria in every hypertensive patient as it is an early sign <strong>of</strong> endo<strong>the</strong>lial dysfunction<br />
and damaged blood vessels.<br />
Key Words: Microalbuminuria – Subclinical cardiac structural changes – Isolated systolic hypertension – Elderly patients.<br />
Introduction<br />
Hypertension is a major public health problem<br />
all over <strong>the</strong> world. Its prevalence among Egyptians<br />
is 26.3% (Ibrahim, 2001). As <strong>the</strong> population ages,<br />
<strong>the</strong> prevalence <strong>of</strong> hypertension will increase. Isolated<br />
systolic hypertension is <strong>com</strong>mon in elderly<br />
people and probably accounts for more than 50%<br />
<strong>of</strong> all cases <strong>of</strong> hypertension above <strong>the</strong> age <strong>of</strong> 65<br />
years (Padfield, 2001). As arterial <strong>com</strong>pliance<br />
declines with age, systolic blood pressure increases,<br />
diastolic blood pressure declines and pulse pressure<br />
increases. This is a strong predictor <strong>of</strong> cardiovascular<br />
disease (Blacher et al, 2000).<br />
The Departments <strong>of</strong> Cardiology* and Internal Medicine,<br />
Benha Faculty <strong>of</strong> Medicine, Benha University, Egypt.<br />
Manuscript received 10 Sep., 2009; revised 12 Oct., 2009;<br />
accepted 13 Oct., 2009.<br />
Address for Correspondence: Dr. Hamza Kabil, 92 El-Sikka<br />
El-Kadima street, Mansoura, Dakahlia, Egypt.<br />
69<br />
Microalbuminuria represents a marker <strong>of</strong> vascular<br />
damage so, its presence is a signal from <strong>the</strong><br />
kidney that cardiovascular risk is increased and<br />
vascular responses are altered (Garg and Bakris,<br />
2002).<br />
Microalbuminuria is usually defined as a urinary<br />
albumin excretion rate <strong>of</strong> 30 to 300mg in a 24-h<br />
urine collection, or as a urinary albumin excretion<br />
rate <strong>of</strong> 20 to 200ug/min in a timed overnight urine<br />
collection. More than one consecutive urine collection<br />
is preferred given <strong>the</strong> high day to day<br />
variability <strong>of</strong> urinary albumin excretion (Diercks<br />
et al, 2002).<br />
The prevalence <strong>of</strong> microalburninuria is 5-8%<br />
in <strong>the</strong> general population and 6-24% in hypertensive<br />
patients (Hornych et al, 2000).<br />
In essential hypertension, microalbuminuria<br />
represents an early marker <strong>of</strong> cardiac structural<br />
damage e.g. left ventricular hypertrophy (Plavink<br />
et al., 2002).
Microalbuminuria & Subclinical Cardiac Structural Changes Relation<br />
Although microalbuminuria is useful and cost<br />
effective but is still too <strong>of</strong>ten neglected in clinical<br />
practice (Leoncini et al, 2002).<br />
Aim <strong>of</strong> <strong>the</strong> work:<br />
To study <strong>the</strong> relationship between microalbuminuria<br />
and subclinical cardiac structural changes<br />
(interventricular septum thickness, left ventricular<br />
wall thickness and left ventricular mass index) in<br />
isolated systolic hypertension in elderly patients.<br />
Patients and Methods<br />
The study was done in <strong>the</strong> Nephrology Unit-<br />
Benha Faculty <strong>of</strong> Medicine, where 100 patients<br />
were selected (61 females and 39 males) and 50<br />
apparently healthy persons aged 60 years or older<br />
(27 females and 23 males) as a control group.<br />
The inclusion criteria were:<br />
1- Patients aged 60 years or older.<br />
2- Isolated systolic hypertensive patients with<br />
systolic blood pressure ≥160mmHg and diastolic<br />
blood pressure ≥95mmHg (Amery et al, 1991).<br />
The exclusion criteria were:<br />
1- Renal failure or any renal disease, liver disease<br />
or collagen disease.<br />
2- Diabetes mellitus.<br />
3- Hypertensive patients with manifest heart failure.<br />
All subjects (patients-control group) have been<br />
subjected to <strong>the</strong> following:<br />
1- History taking with stress on: Age, sex, smoking,<br />
duration <strong>of</strong> hypertension, antihypertensive<br />
drugs, cardiovascular or cerebrovascular <strong>com</strong>plications<br />
and family history <strong>of</strong> hypertension,<br />
cardiovascular or cerebrovascular disease.<br />
2- Thorough clinical examination including:<br />
• Weight, height, body mass index.<br />
• Blood pressure measurement by <strong>the</strong> cuff method,<br />
using <strong>the</strong> 1 st and 5 th Korotk<strong>of</strong>f sounds for identification<br />
<strong>of</strong> systolic and diastolic blood pressures<br />
respectively. The average <strong>of</strong> three readings taken<br />
in different times <strong>of</strong> three consecutive days was<br />
recorded.<br />
• Pulse (rhythm-rate-special character-peripheral<br />
pulses-equality on both sides-vessel wall).<br />
• Complete heart, chest, abdomen and neurologic<br />
evaluation.<br />
70<br />
3- Laboratory investigations:<br />
a- Dipstick urine analysis:<br />
For rapid determination <strong>of</strong> urobilinogen, bilirubin,<br />
glucose, protein, blood, pH and gravity (<strong>com</strong>biscreen,<br />
analyticon Biotechnologies AG), only a<br />
fresh samples and <strong>com</strong>pare <strong>the</strong> reagent areas on<br />
<strong>the</strong> strip with <strong>the</strong> corresponding colour chart after<br />
60 seconds.<br />
b- Dipstick for microalbuminuria:<br />
For rapid detection <strong>of</strong> microalbuminuria by<br />
using an Accu-Check-Product-MICRAL-Test.<br />
Procedure:<br />
• Three urine samples were tested.<br />
• The first morning urine is collected.<br />
• Normal fluid intake prior testing is important<br />
(1.5-2 litre/day).<br />
• The screening result is positive when at least two<br />
<strong>of</strong> <strong>the</strong> three samples produce a reaction colour<br />
corresponding to 20mg/L albumin (threshold for<br />
microalbuminuria) or more as <strong>the</strong> dipstick is<br />
graded into 20, 50 and 100mg/L.<br />
N.B: If proteinuria was confirmed by dipstick<br />
for urine analysis, it was not necessary to screen<br />
for microalbuminuria.<br />
c- 24-hour urinary Protein:<br />
For all subjects with proteinuria and microalbuminuria<br />
(El-Khodary, 2000).<br />
d- Hematological parameters:<br />
Hemoglobin content, hematocrite value and<br />
<strong>com</strong>plete blood picture.<br />
e- Biochemical tests:<br />
1- Fasting and 2 hours-post-prandial blood sugar<br />
levels.<br />
2- Serum creatinine.<br />
3- Blood urea.<br />
4- Serum uric acid.<br />
5- Serum triglycerides and cholesterol.<br />
6- Serum calcium.<br />
7- Serum sodium and potassium.<br />
4- Electrocardiogram.<br />
5- Echocardiographic assessment.<br />
Two dimensional and M-mode echocardiography<br />
was performed with <strong>the</strong> patients in <strong>the</strong><br />
partial left lateral decubitus position using Hewled
Hamza Kabil, et al<br />
Packard (HP) Sonos 1000 system with 2.5MHz<br />
transducer. Left ventricular measurements were<br />
made at end-diastole and end-systole, according<br />
to <strong>the</strong> re<strong>com</strong>mendations <strong>of</strong> <strong>the</strong> American Society<br />
<strong>of</strong> Echocardiography (ASE).<br />
Left ventricular mass (LVM) was calculated by<br />
<strong>the</strong> equation:<br />
LVM (ASE) = 0.8 (1.04 (IVS + LVID + PWT)3 – LVID3) +<br />
0.6 gm (Devereux et al., 1986).<br />
IVS = Interventricular septum.<br />
LVID = Left ventricular internal dimension.<br />
PWT = Posterior wall thickness.<br />
Table 1:<br />
Variables<br />
Mi (Dipstick)/mg/L<br />
Protein in 24-hr urine (vol)/L<br />
Protin in 24-hr urine (amount)/gm<br />
HB (gm/dl)<br />
HT (%)<br />
WBCs/mm 3<br />
Platelets/mm 3 (x1000)<br />
Triglycerides mg/dl<br />
Cholestesterol mg/dl<br />
Creatinine mg/dl<br />
Urea mg/dl<br />
Uric acid mg/dl<br />
Serum Na mg/dl<br />
Serum K mg/dl<br />
Serum Ca++ mg/dl<br />
SBP = Systolic blood pressure.<br />
Mi = Microalbuminuria.<br />
WBCs = White blood cells.<br />
Compared to control group, patients with ISH<br />
tended to have significantly greater SWT (1.2±0.3<br />
Vs 0.9±0.08, p
Microalbuminuria & Subclinical Cardiac Structural Changes Relation<br />
There was significant positive correlation between<br />
<strong>the</strong> duration <strong>of</strong> hypertension and both microalbuminuria<br />
and cardiac structural changes as<br />
shown in Table (3).<br />
Table 3:<br />
Variables<br />
Mi mg/l<br />
SWT/cm<br />
PWT/cm<br />
LVM/gm<br />
LVMI gm/m 2<br />
LVH<br />
Mi<br />
PWT<br />
LVMI<br />
SWT<br />
LVM<br />
LVH<br />
There was a significant positive correlation<br />
between age and both microalbuminuria and cardiac<br />
structural changes.<br />
Table 4:<br />
Variables<br />
Mi mg/l<br />
SWT/cm<br />
PWT/cm<br />
LVM/gm<br />
LVMI gm/m 2<br />
LVH<br />
Mi<br />
PWT<br />
LVMI<br />
SWT<br />
LVM<br />
LVH<br />
Coefficient regression<br />
2.3<br />
0.009<br />
0.004<br />
2.3<br />
0.17<br />
0.21<br />
= Microalbuminuria.<br />
= Posterior wall thickness.<br />
= Left ventricular mass index.<br />
= Septal wall thickness.<br />
= Left ventricular mass.<br />
= Left ventricular hypertrophy.<br />
Coefficient regression<br />
–0.13<br />
0.003<br />
–0.0003<br />
0.08<br />
0.59<br />
0.08<br />
= Microalbuminuria.<br />
= Posterior wall thickness.<br />
= Left ventricular mass index.<br />
= Septal wall thickness.<br />
= Left ventricular mass.<br />
= Left ventricular hypertrophy.<br />
This table showed <strong>the</strong> relation between <strong>the</strong> level<br />
<strong>of</strong> albuminuria regarding dipstick for urine and<br />
microalbuminuria and cardiac structural changes<br />
regarding echocardiography and ECG.<br />
There was a significant difference between<br />
normoalbuminuric, microal buminuric and macroalbuminuric<br />
regarding cardiac structural changes<br />
(SWT - PWT - LVM - LVMI).<br />
Results <strong>of</strong> regression analysis between <strong>the</strong> level<br />
<strong>of</strong> microalbuminuria and cardiac structural changes<br />
as shown in Table (6).<br />
r 2<br />
0.05<br />
0.01<br />
0.005<br />
0.02<br />
0.0004<br />
0.09<br />
r 2<br />
0.0006<br />
0.008<br />
0.0001<br />
0.05<br />
0.02<br />
0.05<br />
p<br />
0.04<br />
0.2<br />
0.4<br />
0.02<br />
0.8<br />
0.01<br />
p<br />
0.8<br />
0.4<br />
0.9<br />
0.01<br />
0.2<br />
0.01<br />
72<br />
Table 5:<br />
Cardiac<br />
structural<br />
change<br />
SWT/cm<br />
PWT/cm<br />
LVM/g<br />
LV MI/gm/m 2<br />
* SWT<br />
* PWT<br />
* LVMI<br />
* LVM<br />
* S<br />
* MA<br />
* NA<br />
* Mi<br />
NA<br />
(N=22)<br />
Mean ± SD<br />
1.02±0.18<br />
0.95±0.15<br />
154.9±48.6<br />
83.8±23.2<br />
Albuminuria<br />
Mi<br />
(N=67)<br />
Mean ± SD<br />
1.25±0.25<br />
1.06±0.19<br />
223.9±54.2<br />
119.6±25.2<br />
= Septal wall thickness.<br />
= Posterior wall thickness.<br />
= Left ventricular mass index.<br />
= Left ventricular mass.<br />
= Standard deviation.<br />
= Macroalbuminuria.<br />
= Normoalburninuria.<br />
= Microalburninuria.<br />
Normal values:<br />
SWT = Up to 1.1 cm.<br />
PWT = Up to 1.1 cm.<br />
LVMI = Male: 136gm/m 2 female: 112 gm/m 2<br />
Table 6:<br />
Variables<br />
SWT/cm<br />
PWT/cm<br />
LVM/gm<br />
LVMI gm/m 2<br />
MA<br />
(N=11)<br />
Mean ± SD<br />
1.33±0.3<br />
1.2±0.28<br />
271.5±66.2<br />
148±37.7<br />
Hamza Kabil, et al<br />
There was a significant difference between<br />
normoalbuminuric, microalbuminuric and macroalbuminuric<br />
regarding cardiac structural changes.<br />
There was highly positive significant correlation<br />
between <strong>the</strong> level <strong>of</strong> microalbuminuria and both<br />
LVM and LVMI and significant with SWT and<br />
tendency to be significant with PWT.<br />
SWT<br />
There was a significant difference between<br />
normoalbuminuric, microalbuminuric and macroalbuminuric<br />
regarding SWT as shown in Table (7).<br />
LVMI<br />
100<br />
90<br />
80<br />
70<br />
60<br />
50<br />
40<br />
30<br />
20<br />
10<br />
0<br />
100<br />
90<br />
80<br />
70<br />
60<br />
50<br />
40<br />
30<br />
20<br />
10<br />
0<br />
95.5%<br />
4.5%<br />
NA (22%)<br />
* NA = Normoalbuminuria.<br />
* Mi = Microalbuminuria.<br />
Figure 1: Distribution <strong>of</strong> studied cases according to <strong>the</strong> level<br />
<strong>of</strong> albuminuria and SWT.<br />
95.5%<br />
4.5%<br />
NA (22%)<br />
* NA = Normoalbuminuria.<br />
* Mi = Microalbuminuria.<br />
55.2%<br />
55.2%<br />
44.8%<br />
44.8%<br />
36.4%<br />
38.4%<br />
Absent<br />
Present<br />
63.6%<br />
MI (67%) MA (11%)<br />
* MA = Macroalbuminuria<br />
* SWT = Septal wall thickness<br />
Absent<br />
Present<br />
63.6%<br />
MI (67%) MA (11%)<br />
* MA = Macroalbuminuria<br />
* LVMI = Left ventricular mass index<br />
Figure 2: Distribution <strong>of</strong> studied cases according to <strong>the</strong> level<br />
<strong>of</strong> albuminuria and LVMI.<br />
There was a significant difference between<br />
normoalbuminuric, microalbuminuric and macroalbuminuric<br />
regarding LVMI as shown in Table (7).<br />
73<br />
PWT<br />
100<br />
90<br />
80<br />
70<br />
60<br />
50<br />
40<br />
30<br />
20<br />
10<br />
0<br />
95.5%<br />
4.5%<br />
NA (22%)<br />
* NA = Normoalbuminuria.<br />
* Mi = Microalbuminuria.<br />
77.6%<br />
22.4%<br />
45.5%<br />
Absent<br />
Present<br />
54.5%<br />
MI (67%) MA (11%)<br />
* MA = Macroalbuminuria<br />
* LVMI = Left ventricular mass index<br />
Figure 3: Distribution <strong>of</strong> studied cases according to <strong>the</strong> level<br />
<strong>of</strong> albuminuria and PWT.<br />
There was a significant difference between<br />
normoalbuminuric, microalbuminuric and macroalbuminuric<br />
regarding PWT as shown in Table (7).<br />
LVH<br />
100<br />
90<br />
80<br />
70<br />
60<br />
50<br />
40<br />
30<br />
20<br />
10<br />
0<br />
81.8%<br />
18.2%<br />
NA (22%)<br />
* NA = Normoalbuminuria.<br />
* Mi = Microalbuminuria.<br />
58.2%<br />
41.8%<br />
45.5%<br />
Absent<br />
Present<br />
54.5%<br />
MI (67%) MA (11%)<br />
* MA = Macroalbuminuria.<br />
* LVH = Left ventricular hypertrophy.<br />
Figure 4: Distribution <strong>of</strong> studied cases according to <strong>the</strong> level<br />
albuminuria and LVH.<br />
There was a significant difference between<br />
normoalbuminuric, microalbuminuric and macroalbuminuric<br />
regarding LVH as shown in Table (7).<br />
Table (8) showed <strong>the</strong> relation between LVH,<br />
serum cholesterol level, serum triglycerides level<br />
and uric acid level regarding mean and standard<br />
deviation.<br />
There was a difference between patients having<br />
normal left ventricular wall and patients having<br />
LVH regarding (Cholesterol level-triglycerides<br />
level-uric acid level), however this difference was<br />
not statistically significant.
Microalbuminuria & Subclinical Cardiac Structural Changes Relation<br />
Table 8:<br />
Table (9) showed <strong>the</strong> relation between <strong>the</strong> level<br />
<strong>of</strong> albuminuria, cholesterol level, triglycerides<br />
level and uric acid level.<br />
There was a significant difference between<br />
normoalbuminuric, microalbuminuric and macroalbuminuric<br />
regarding uric acid level.<br />
Table 9:<br />
Variables<br />
Cholesterol<br />
mg/dl<br />
Triglycerides<br />
mg/dl<br />
Uric acid<br />
mg/dl<br />
Variables<br />
Cholesterol mg/dl<br />
Triglycerides mg/dl<br />
Uric acid mg/dl<br />
NA<br />
Mean ± SD<br />
196.1±49.6<br />
148.9±62.1<br />
4.9±1.8<br />
NA = Normoalbuminuria.<br />
MI = Microalbuminuria.<br />
No LVH<br />
Mean ± SD<br />
208.4±44.9<br />
151.5±36.7<br />
5.7±1.6<br />
Mi<br />
Mean ± SD<br />
2 16.7±39.4<br />
156.5±32.4<br />
6.1±1.6<br />
Discussion<br />
LVH<br />
Mean ± SD<br />
218.5±38.2<br />
154.1±48.5<br />
5.7±1.7<br />
MA<br />
Mean ± SD<br />
217.1±42.1<br />
136±43.7<br />
5.6±1.4<br />
MA = Macroalbuminuria.<br />
SD = Standard deviation.<br />
>0.05<br />
>0.05<br />
0.05<br />
>0.05<br />
>0.05<br />
p<br />
74<br />
sive increases in UAE may result in better protection<br />
against hypertension induced morbidity and<br />
mortality (Redon, 2006).<br />
This work was done to determine <strong>the</strong> relationship<br />
between microalbuminuria and subclinical<br />
cardiac structural changes (septal wall thickness,<br />
posterior wall thickness and left ventricular mass<br />
index) in elderly isolated systolic hypertensive<br />
patients.<br />
Table (1) showed highly significant differences<br />
(p
Hamza Kabil, et al<br />
microalbuminuria, LVM and LVH. Gerstein et al<br />
(2000) stated that <strong>the</strong> relation between microalbuminuria<br />
and <strong>the</strong> duration <strong>of</strong> hypertension was<br />
present. Hypertrophic growth <strong>of</strong> myocytes occur<br />
in response to pressure or volume overload especially<br />
with increased duration.<br />
There was a significant positive correlation<br />
between age <strong>of</strong> <strong>the</strong> patients and LVM and LVH as<br />
shown in Table (4). It can be explained by Dannenberg<br />
et al (1989) who mentioned that age-LVM<br />
relation is a function <strong>of</strong> multiple factors such as<br />
elevated blood pressure, obesity, valvular heart<br />
disease and occult coronary artery disease which<br />
tend to increase with age.<br />
There were insignificant positive correlations<br />
between age and microalbuminuria, SWT, and<br />
LVMI. These results are in agree with those reported<br />
by Lydakis and Lip (1998) but in contrast with<br />
those reported by Ritz et al (1994) who mentioned<br />
that urinary albumin excretion was positively correlated<br />
with age, possibly due to a degree <strong>of</strong> nephrosclerosis.<br />
Tables (5,6,7) and Figs. (1- 4) showed highly<br />
significant positive correlation between <strong>the</strong> albuminuria<br />
level and cardiac structural changes. It<br />
was confirmed between albuminuria (detected by<br />
urine analysis or dipstick) and PWT (p=0.004) and<br />
LVMI (p0.01)<br />
and LVMI (r=0.42, p
Microalbuminuria & Subclinical Cardiac Structural Changes Relation<br />
8- Fang J, Alderman MH: Serum uric and cardiovascular<br />
mortality, <strong>the</strong> NHANE-SI epidemiologic follow-up study<br />
1971-1992. JAMA 2000; 283: 2404-2410.<br />
9- Garg JP, Bakris GL: Microalbuminuria: marker <strong>of</strong> vascular<br />
dysfunction, risk factor for cardiovascular disease. Vascular<br />
Medicine 2002; 7: 35-43.<br />
10- Gerstein HS, Mann JF, Pogue J: Prevalence and determinants<br />
<strong>of</strong> microalbuminuria in high risk diabetic and nondiabetic<br />
patients (HOPE Study). Diabetes Care 2000; 23:<br />
Suppl. 2: 35-79.<br />
11- Hornych A Marre M, Mimran A: Microalbuminuria in<br />
arterial hypertension. Measurement, variables, interpretation,<br />
re<strong>com</strong>mendations. Arch Mal Coeur Viass 2000; 93<br />
(11): 1304-8.<br />
12- Ibrahim MM: Epidemiology <strong>of</strong> hypertension in Egyptains,<br />
In: Manual <strong>of</strong> hypertension 2001; Chapter 15, Page. 182.<br />
13- James MA, Fa<strong>the</strong>rby MD, Patter JF: Screening tests for<br />
microalbuminuria in nondiabetic elderly subjects and<br />
<strong>the</strong>ir relation to blood pressure. Clinical Science 1995;<br />
88: 185-140.<br />
14- Leoncini G, Sacchi G, Pontremoli R: Microalbuminuria<br />
is an integrated marker <strong>of</strong> subclinical organ damage in<br />
primary hypertension. J Hum Hyperten 2002; 16 (6): 344-<br />
404.<br />
15- Leoncini G, Sacchi G, Pontremoli R: Microalbuminuria<br />
identifies overall cardiovascular risk in essential hypertension:<br />
An artificial neural network-based approach. J<br />
Hypertension 2002; 20: 1315-1321.<br />
76<br />
16- Liebson PR, Grandits G, Prineas R: Echocardiographic<br />
correlates <strong>of</strong> left venmtricular structure among 844 mildly<br />
hypertensive men and women in <strong>the</strong> treatment <strong>of</strong> mild<br />
hypertensive study (TOMHS). Circulation 1993; 87: 476-<br />
486.<br />
17- Lydakis C, Lip GYH: Microalbuminuria and cardiovascular<br />
risk QJ Med 1998; 91: 381-391.<br />
18- Padfield PL: Fur<strong>the</strong>r reading on systolic blood pressure<br />
and isolated systolic hypertension: Epidemiology. The<br />
Hypertension Letter (41) 2001.<br />
19- Parving HH Anderson S, Jacobsen P, et al: Semin Nephrol<br />
2004; 24: 147-57.<br />
20- Pedrinelli R: Microalbuminuria in essential hypertension.<br />
A marker <strong>of</strong> systemic vascular damage. Nephrol Dial<br />
Transplant 1997; 12: 379-398.<br />
21- Pontremoli R, Dahl<strong>of</strong> B, Hansson L: Prevalence and<br />
clinical correlates <strong>of</strong> microalbuminuria in essential hypertension.<br />
The MAGIC study. Hypertension 1997; 30: 1135-<br />
1143.<br />
22- Redon J: Nephrol Dial Transplant 2006; 21: 573-6.<br />
23- Ritz E, Nowicki M, Klin HP: Proteinuria and hypertension.<br />
Kid Intern 1994; 46 (Suppl. 47): 576-580.<br />
24- Tsioufis C, Marinakis N, Toutouz A: Microalbuminuria<br />
is closely related to impaired arterial elasticity in untreated<br />
patients with essential hypertension. Nephron Exp Nephrol<br />
2003; 93 (3): 85-6.
Egypt Heart J 62 (1): 77-81, March 2010<br />
Urinary Albumin Excretion is Associated with Arterial Stiffness in<br />
Hypertensive Adults<br />
MOHAMMED A ABDEL WAHAB, MD; MOHAMED M SAAD, MD; AMR S AMIN, MD;<br />
KHALID A BARAKA, MD; NASSER M TAHA, MD<br />
Background: Microalbuminuria may represent <strong>the</strong> early renal manifestation <strong>of</strong> a widespread vascular dysfunction, and<br />
<strong>the</strong>refore it is an integrated marker <strong>of</strong> cardiovascular risk.<br />
Aim: To Verify whe<strong>the</strong>r <strong>the</strong> urinary albumin/creatinine ratio (UACR), a measure <strong>of</strong> albuminuria, is associated with arterial<br />
stiffness in hypertensive adults.<br />
Patients and Methods: 50 hypertensive patients (group 1) and 20 normo-tensive healthy subjects (group 2) (used as a<br />
control) were included in this study. Office and 24h systolic and diastolic blood pressure measurement was done for both groups<br />
and from it ambulatory arterial stiffness index (AASI) was calculated. Urinary albumin and creatinine concentrations were<br />
determined on a morning spot-urine sample. The urinary albumin-to-creatinine ratio (ACR) was <strong>the</strong>n calculated. Microalbuminuria<br />
was defined as an ACR <strong>of</strong> 30 to 299mg/g. Patients with macroalbuminuria (defined as ACR ≥300g/mg). We also assessed <strong>the</strong><br />
intima-media thickness (IMT) <strong>of</strong> <strong>the</strong> <strong>com</strong>mon carotid, and left ventricular mass index (LVMI) for correlation study.<br />
Results: The mean level <strong>of</strong> microalbuminuria was significantly increased in group 1 than in group 2 (35.91±43.95 versus<br />
8.25±2.544, p=0.007). There is significant correlation between AASI and microalbuminuria (r=0.312, p=0.009). Fur<strong>the</strong>rmore,<br />
significant correlation was found between microalbuminuria and left ventricular mass index (LVMI) (r=0.486, p
Urinary Albumin Excretion is Associated with Arterial Stiffness<br />
All <strong>the</strong> participant were subjected to: History<br />
taking, clinical examination, Office blood pressure<br />
measurement (Patients with blood pressure 140/90<br />
and above were considered hypertensive), measurement<br />
<strong>of</strong> body mass index and body surface area,<br />
Laboratory investigation (Fasting and post prandial<br />
blood sugar, lipogram, blood urea nitrogen, serum<br />
creatinine, and quantification <strong>of</strong> albumin in urine),<br />
and Ambulatory blood pressure monitoring<br />
(ABPM) using Space Labs TM 2430 device (Space<br />
Labs Inc., USA).<br />
Calculation <strong>of</strong> <strong>the</strong> ambulatory arterial stiffness<br />
index (AASI):<br />
From 24-hour recordings, for each participant<br />
<strong>the</strong> regression slope <strong>of</strong> diastolic on systolic blood<br />
pressure was calculated, <strong>the</strong> regression line was<br />
not forced through <strong>the</strong> origin (intercept 0), because<br />
during diastole when flow drops to 0, such a phenomenon<br />
does not occur for blood pressure [5].<br />
The rationale underlying this is that, for any<br />
given increase in distending arterial pressure,<br />
systolic and diastolic pressures tend to increase in<br />
a parallel fashion in a <strong>com</strong>pliant artery, whereas<br />
in a stiff artery, <strong>the</strong> increase in systolic pressure is<br />
Table 1: Classification <strong>of</strong> abnormal urinary albumin execration (UAE).<br />
Normal<br />
High Normal<br />
Microalbuminuria<br />
Macroalbuminuria<br />
24-H Urine<br />
Albumin<br />
(mg/24 h)<br />
Mohammed A Abdel Wahab, et al<br />
Statistical method:<br />
Data was analyzed by <strong>the</strong> Statistical Package<br />
for <strong>the</strong> Social Sciences (SPSS), version 16 for<br />
Window. All data were reported as mean ± SD. A<br />
Student t test was used to <strong>com</strong>pare variables for<br />
testing statistical significant difference between<br />
two groups and <strong>the</strong> differences were considered<br />
significant at a two-tailed p≤0.05 and Mann-<br />
Whitney Test used to study <strong>the</strong> correlations <strong>of</strong> <strong>the</strong><br />
non parametric variables.<br />
Results<br />
Table (2) show <strong>the</strong> mean level <strong>of</strong> microalbuminuria<br />
was 35.91±43.95 in group 1 whoever <strong>the</strong><br />
mean level <strong>of</strong> microalbuminuria was 8.25±2.54 in<br />
group 2, <strong>the</strong>re is statistically significant difference<br />
between both groups as regard <strong>the</strong> value <strong>of</strong> microalbuminuria<br />
(p=0.007).<br />
Table 2: Microalbuminuria among <strong>the</strong> study groups.<br />
Microalbuminuria<br />
Group 1<br />
(n=50)<br />
Mean<br />
35.91<br />
SD<br />
43.95<br />
Group 2<br />
(n=20)<br />
Mean<br />
8.25<br />
SD<br />
2.54<br />
p value<br />
0.007<br />
Fur<strong>the</strong>rmore, a significant correlation (r=0.312,<br />
p=0.009) between AASI and microalbuminuria was<br />
found as shown in Fig. (1).<br />
Microalbuminuria<br />
250<br />
200<br />
150<br />
100<br />
50<br />
0<br />
-50<br />
Microalbuminuria<br />
p=0.009<br />
0.00 .10 .20 .30 .40 .50 .60 .70 .80 .90 1.0<br />
AASI<br />
Figure 1: Shows significant positive correlation between<br />
AASI and <strong>the</strong> level <strong>of</strong> microalbuminuria.<br />
Also, <strong>the</strong>re is significant correlation between<br />
microalbuminuria and left ventricular mass index<br />
(LVMI) Table (3).<br />
Also, <strong>the</strong>re is significant correlation between <strong>the</strong><br />
microalbuminuria and <strong>the</strong> intima-media thickness <strong>of</strong><br />
right and left <strong>com</strong>mon carotid arteries. Moreover,<br />
<strong>the</strong>re is significant correlation between <strong>the</strong> microalbuminuria<br />
and mean <strong>com</strong>mon carotid arteries intimal<br />
thickness (Table 3).<br />
79<br />
Table 3: Correlations <strong>of</strong> <strong>the</strong> microalbuminuria.<br />
AASI<br />
LCCA<br />
RCCA<br />
MCCA<br />
LVMI<br />
LVMI<br />
LCCA IMT<br />
RCCA IMT<br />
MCCA IMT<br />
Pearson coefficient<br />
0.486<br />
0.210<br />
0.323<br />
0.311<br />
Discussion<br />
0.000<br />
0.081<br />
0.006<br />
0.009<br />
= Ambulatory Arterial Stiffness Index.<br />
= Left <strong>com</strong>mon carotid artery intima media thickness.<br />
= Right <strong>com</strong>mon carotid artery intima media thickness.<br />
= Mean <strong>com</strong>mon carotid artery intima media thickness.<br />
= Left ventricular mass index.<br />
Results <strong>of</strong> this study revealed that <strong>the</strong>re is<br />
significant increase in <strong>the</strong> level <strong>of</strong> microalbuminuria<br />
in hypertensive subjects <strong>com</strong>pared to controls.<br />
Similar results obtained in ano<strong>the</strong>r study which<br />
concluded that microalbuminuria is highly prevalent<br />
in hypertensive population, its prevalence varies<br />
from 10 to 40% [7]. This is also agree with <strong>the</strong><br />
result <strong>of</strong> ano<strong>the</strong>r trial which concluded that microalbuminuria<br />
prevalence is low in <strong>the</strong> absence<br />
<strong>of</strong> cardiovascular risk factors and progressively<br />
increases with <strong>the</strong> number cardiovascular risk<br />
factors and that <strong>the</strong> main correlate <strong>of</strong> microalbuminuria<br />
is blood pressure, ei<strong>the</strong>r systolic or diastolic<br />
pressure. The relation between blood pressure and<br />
microalbuminuria is continuous and graded because<br />
<strong>the</strong> microalbuminuria prevalence increases with<br />
<strong>the</strong> severity <strong>of</strong> hypertension [3].<br />
Results <strong>of</strong> this study revealed that microalbuminuria<br />
is significantly correlated with AASI as<br />
an index <strong>of</strong> arterial stiffness.<br />
The same result was obtained when <strong>com</strong>pared<br />
pulse wave velocity as a marker <strong>of</strong> arterial stiffness<br />
with microalbuminuria [8]. Fur<strong>the</strong>rmore, ano<strong>the</strong>r<br />
study detected that Albuminuria was significantly<br />
associated with lower small artery elasticity [9].<br />
In agreement with <strong>the</strong> current study Multe` et<br />
al, examined <strong>the</strong> correlation <strong>of</strong> <strong>the</strong> aortic pulse<br />
wave velocity (PWV) as a measure <strong>of</strong> arterial<br />
stiffness in <strong>com</strong>parison with <strong>the</strong> urinary albumin<br />
excretion in hypertensive patients, and found that<br />
<strong>the</strong> PWV found to be higher in hypertensive patients<br />
having albumin excretion rate higher than median,<br />
when <strong>com</strong>pared with those with those below <strong>the</strong><br />
median [10].<br />
Also Tsioufis et al, studied <strong>the</strong> relation <strong>of</strong> <strong>the</strong><br />
microalbuminuria and <strong>the</strong> augmentation index<br />
(AIx) as a measure <strong>of</strong> arterial stiffness, in a group<br />
p
Urinary Albumin Excretion is Associated with Arterial Stiffness<br />
<strong>of</strong> 130 untreated hypertensive subjects and <strong>the</strong>y<br />
found <strong>the</strong> higher <strong>the</strong> level <strong>of</strong> microalbuminuria <strong>the</strong><br />
more increased <strong>the</strong> augmentation index [11].<br />
Also Leoncini et al, studied <strong>the</strong> association <strong>of</strong><br />
<strong>the</strong> AASI and target organ damage in patients with<br />
primary hypertension, <strong>the</strong> results demonstrated<br />
significant correlation between <strong>the</strong> AASI and microalbuminuria<br />
[12].<br />
Moreover, Munakata et al, considered <strong>the</strong> brachial-ankle<br />
pulse wave velocity as a measure <strong>of</strong><br />
arterial stiffness. Thy examined <strong>the</strong> hypo<strong>the</strong>sis that<br />
higher brachial-ankle pulse wave velocity is associated<br />
with a much greater risk <strong>of</strong> albuminuria in<br />
718 never-treated hypertensive patients. The prevalence<br />
<strong>of</strong> microalbuminuria increased with a graded<br />
increase in brachial-ankle pulse wave velocity<br />
(p
Mohammed A Abdel Wahab, et al<br />
10- Multe G, Cottone S, Vadala A, Olope V, Mezzatesta V,<br />
Mongivoi R, Piazza G, Nardi E, Andronica G, Cerasola<br />
G: Relationship between albumin excretion rate and aortic<br />
stiffness in untreated essential hypertensive patients.<br />
Journal <strong>of</strong> Internal Medicine 2004; 256: 22-29.<br />
11- Tsioufis C, Tzioumis C, Marinakis N, Toutouzas K,<br />
Tousoulis D, Kallikazaros I, Stefanadis C, Toutouzas P:<br />
Microalbuminuria Is Closely Related to Impaired Arterial<br />
Elasticity in Untreated Patients with Essential Hypertension.<br />
Nephron Clin Pract 2003; 93: c106-c111.<br />
12- Leoncini G, Ratto E, Viazzi f, Vaccaro V, Parodi A, Falqui<br />
V, Conti N, Tomolillo Cinzia, Deferrari G, Pontremoli<br />
R: Increased Ambulatory Arterial Stiffness Index Is associated<br />
with Target Organ Damage in Primary Hypertension.<br />
Hypertension 2006; 48: 397-403.<br />
13- Munakata M, Nunokawa T, Yoshinaga K, Toyota T:<br />
Brachial ankle pulse wave velocity is an independent risk<br />
factor for microalbuminuria in patients with essential<br />
hypertension-a Japanese trial on <strong>the</strong> prognostic implication<br />
<strong>of</strong> pulse wave velocity. Hypertens Res 2006; 29 (7): 515-<br />
21.<br />
81<br />
14- Post WS, Blumenthal RS, Weiss JL, Levine DM, Thiemann<br />
DR, Gerstenblith G: Spot urinary albumin-creatinine ratio<br />
predicts left ventricular hypertrophy in young hypertensive<br />
African-American men. Am J Hypertens 2000; 13 (11):<br />
1168-72.<br />
15- Leoncini G, Sacchi G, Viazzi F, Ravera M, Parodi D,<br />
Ratto E, Vettoretti S, Tomolillo C, Deferrari G, Pontremoli<br />
R: Microalbuminuria identifies overall cardiovascular<br />
risk in essential hypertension: An artificial neural networkbased<br />
approach. J Hypertens 2002 Jul; 20 (7): 1315-21.<br />
16- Gatzka CD, Reid CM, Lux A, Dart AM, Jennings GL:<br />
Ventricular mass and microalbuminuria: Relation to ambulatory<br />
blood pressure. Hypertension Diagnostic Service<br />
Investigators", Clin Exp Pharmacol Physiol 1999; 26 (7):<br />
514-6.<br />
17- Ponteremoli R, Leoncini G, Ravera M, Viazzi F, Vettoretti<br />
S, Ratto E, Parodi D, Tomolillo C, Deferrari G: Microalbuminuria,<br />
Cardiovascular, and Renal Risk in Primary<br />
Hypertension. Journal <strong>of</strong> American Society <strong>of</strong> Nephrology<br />
2002; 13: S169-S172.
Egypt Heart J 62 (1): 83-88, March 2010<br />
Early Vascular Changes Preceding Morphological Cardiac Changes in<br />
Hypertensive Patients<br />
MOHAMMED A ABDEL WAHAB, MD<br />
Background: Left ventricular hypertrophy (LVH) has been identified as a powerful independent risk factor not only for<br />
total and cardiovascular mortality, but also for sudden cardiac death.<br />
Aim: To Verify <strong>the</strong> vascular changes occurring before morphological changes in LV geometry in hypertensive patients.<br />
Patients and Methods: 50 hypertensive patients and 20 normo-tensive subjects were divided into three groups as follows:<br />
normo-tensive subjects with normal LV geometry (Group I, n=20), hypertensive patients with normal LV geometry (Group II,<br />
n=18); hypertensive patients with abnormal LV geometry (Group III, n=32). 24h systolic and diastolic blood pressure was<br />
carried out for all groups to calculate <strong>the</strong> ambulatory arterial stiffness index (AASI).<br />
Endo<strong>the</strong>lial function was assessed by endo<strong>the</strong>lium-dependent flow-mediated dilatation (FMD) and -independent vasodilatation<br />
(after sublingual administration <strong>of</strong> nitroglycerin) <strong>of</strong> <strong>the</strong> brachial artery using high-resolution vascular ultrasound. We also<br />
assessed <strong>the</strong> intima-media thickness (IMT) <strong>of</strong> <strong>the</strong> <strong>com</strong>mon carotid, and left ventricular mass index (LVMI).<br />
Results: Compared to group I, Group II patients had a higher AASI and IMT and lower FMD (p≤0.001, 0.001 and 0.046<br />
respectively). Same changes were noticed when group II was <strong>com</strong>pared to group III (p≤0.011, 0.013 and 0.049 respectively.<br />
Conclusion: Increased IMT with reduced vasodilator capacity and increased arterial stiffness represent important vascular<br />
changes that precede changes in LV geometry in hypertensive patients that might be markers for early detection <strong>of</strong> high risk<br />
patients. These markers may also prove useful in <strong>the</strong> assessment <strong>of</strong> <strong>the</strong> efficacy <strong>of</strong> different <strong>the</strong>rapeutic modalities in prevention<br />
<strong>of</strong> structural and morphological cardiac changes.<br />
Key Words: Hypertension – Arterial stiffness – Endo<strong>the</strong>lial dysfunction.<br />
Introduction<br />
Left ventricular hypertrophy (LVH) and <strong>the</strong><br />
geometric shape <strong>of</strong> <strong>the</strong> left ventricle are wellestablished<br />
important risk factors for cardiovascular<br />
morbidity and mortality in <strong>the</strong> hypertensive population<br />
[1]. Four distinct geometric patterns were<br />
described [2]; normal geometry (normal LVMI with<br />
a relative wall thickness (RWT) 0.45),<br />
concentric hypertrophy (increased LVMI with RWT<br />
>0.45) and eccentric hypertrophy (increased LVMI<br />
associated with RWT
Early Vascular Changes Preceding Morphological Cardiac Changes<br />
• Group 3: Includes 32 hypertensive subjects with<br />
abnormal LV geometry.<br />
All <strong>the</strong> participant were subjected to: History<br />
taking, clinical examination, Office blood pressure<br />
measurement (Blood pressure 140/90 and above<br />
was considered hypertensive), Laboratory investigation<br />
(Fasting and post prandial blood sugar,<br />
lipogram, blood urea nitrogen, serum creatinine,<br />
and quantification <strong>of</strong> albumin in urine), and Ambulatory<br />
blood pressure monitoring (ABPM) using<br />
<strong>the</strong> ABPM device (model: TM 2430 Space Labs<br />
Inc).<br />
Calculation <strong>of</strong> <strong>the</strong> ambulatory arterial stiffness<br />
index (AASI):<br />
From 24-hour recordings, <strong>the</strong> regression slope<br />
<strong>of</strong> diastolic on systolic blood pressure for each<br />
participant was <strong>com</strong>puted according to <strong>the</strong> criteria<br />
described by Li and his co-workers [6]. AASI was<br />
defined as 1 minus <strong>the</strong> regression slope. The stiffer<br />
<strong>the</strong> arterial tree, <strong>the</strong> closer <strong>the</strong> regression slope and<br />
AASI are to 0 and 1, respectively.<br />
Colored duplex ultrasound to measure <strong>the</strong> Intimamedia<br />
thickness (IMT):<br />
The end-diastolic IMT <strong>of</strong> both <strong>com</strong>mon carotid<br />
artery was measured from <strong>the</strong> leading edge <strong>of</strong> <strong>the</strong><br />
1 st echogenic line to <strong>the</strong> leading edge <strong>of</strong> <strong>the</strong> 2 nd<br />
echogenic line 10mm caudal to <strong>the</strong> bulb using<br />
Hewlett Packard Sonos 1000 system, with 7.5Hz<br />
linear array transducer, with <strong>the</strong> patient in <strong>the</strong><br />
supine position and <strong>the</strong> neck in slight hyperextension.<br />
Plaques were sought in <strong>the</strong> entire extra-cranial<br />
carotid tree and were defined as presence <strong>of</strong> a focal<br />
thickening greater than 1.5mm.<br />
Colored duplex ultrasound to test <strong>the</strong> endo<strong>the</strong>lial<br />
function:<br />
Colored duplex ultrasound was done for all<br />
subjects. The mean right brachial artery anteroposterior<br />
diameter was measured 3-5cm above <strong>the</strong><br />
elbow, between media and adventitia from 4 cycles<br />
synchronized with <strong>the</strong> end-diastole at <strong>the</strong> R wave<br />
peaks [7].<br />
• A basic scan <strong>of</strong> <strong>the</strong> flow was taken.<br />
• 2 nd scan was taken after applying a pneumatic<br />
tourniquet <strong>of</strong> 250-300mmHg. (Using mercurial<br />
sphygmomanometer) for about 4.5sec. The scan<br />
was taken 60 seconds after releasing <strong>the</strong> tourniquet<br />
measuring <strong>the</strong> maximum FMD.<br />
• 3 rd scan was taken after 15 minutes <strong>of</strong> rest to<br />
allow recovery <strong>of</strong> <strong>the</strong> artery after FMD and that<br />
84<br />
was <strong>the</strong> basic <strong>of</strong> Glyceryl trinitrate (GTN)mediated<br />
dilatation (GTN-MD) reading.<br />
• 4 th scan was taken 4 minutes after administration<br />
<strong>of</strong> 400μg <strong>of</strong> GTN spray sublingually.<br />
o FMD percentage was calculating by <strong>the</strong> following<br />
equation:<br />
2 nd Scan – 1 st scan<br />
FMD % = –––––––––––––––––– x 100<br />
1 st scan<br />
o GTN percentage was calculating by <strong>the</strong> following<br />
equation:<br />
4 th Scan – 3 rd scan<br />
GTN – MD% = –––––––––––––––––– x 100<br />
3 rd scan<br />
o Dilatation percentage was calculating by <strong>the</strong><br />
following equation:<br />
FMD%<br />
DilRatio = –––––––––––––––––– x 100<br />
GTN – MD%<br />
Echocardiography evaluation <strong>of</strong> <strong>the</strong> LVMI<br />
and geometric pattern: Was done according to <strong>the</strong><br />
re<strong>com</strong>mendations <strong>of</strong> <strong>the</strong> American Society <strong>of</strong><br />
Echocardiography (ASE) as follows:<br />
LV mass in grams = 0.8 (1.04 ([LVIDD +<br />
PWTD + IVSTD]3 – [LVIDD]3)) + 0.6.<br />
And <strong>the</strong>n indexing <strong>the</strong> LVM to height 2.7 and<br />
BSA.<br />
Determining <strong>the</strong> geometric pattern from by<br />
calculating <strong>the</strong> relative wall thickness (RWT) as<br />
follows: RWT = 2 x PWTD/LVIDD.<br />
Statistical method:<br />
Data was analyzed by <strong>the</strong> Statistical Package<br />
for <strong>the</strong> Social Sciences (SPSS), version 16 for<br />
Window. All data were reported as mean ± SD. A<br />
Student’s t-test was used to <strong>com</strong>pare means <strong>of</strong> two<br />
groups. Mann-Whitney Test was used to <strong>com</strong>pare<br />
non parametric variables. Differences were considered<br />
significant at a two-tailed p≤0.05.<br />
Results<br />
As shown in Table (1), <strong>the</strong> study groups were<br />
all age matched.<br />
Table 1: Comparison <strong>of</strong> <strong>the</strong> age between in <strong>the</strong> study groups.<br />
Age (y)<br />
Group 1<br />
(n=20)<br />
Mean<br />
45.25<br />
SD<br />
7.88<br />
Group 2<br />
(n=18)<br />
Mean<br />
47.39<br />
SD<br />
8.22<br />
Group 3<br />
(n=32)<br />
Mean<br />
48.78<br />
SD<br />
5.19<br />
G1<br />
vrs<br />
G2<br />
0.419<br />
p<br />
G2<br />
vrs<br />
G3<br />
0.466
Mohammed A Abdel Wahab<br />
There is a statistically significant difference<br />
between group 1 and 2 as regards <strong>the</strong> <strong>of</strong>fice and<br />
mean 24 hours systolic and diastolic blood pressure,<br />
while <strong>the</strong>re is no significant difference between<br />
group 2 and 3 in <strong>the</strong>se parameters. Meanwhile<br />
<strong>the</strong>re is significant differences in AASI between<br />
both group 1&2 and group 2&3 (Table 2).<br />
There is significant increase in IMT <strong>of</strong> <strong>the</strong><br />
carotid arteries in group 2 <strong>com</strong>pared to group 1<br />
and in group 3 <strong>com</strong>pared to group 2 (Table 3).<br />
100<br />
75<br />
50<br />
LVMI 125<br />
25<br />
85<br />
There is significant decrease in FMD and dilatation<br />
ratio in group 2 <strong>com</strong>pared to group 1 while<br />
<strong>the</strong>re is tendency <strong>of</strong> FMD to decrease significantly<br />
in group 3 <strong>com</strong>pared to group 2 (Table 4).<br />
Fur<strong>the</strong>rmore, AASI was significantly correlated<br />
with LVM and LVMI (Fig. 1), as well as with <strong>the</strong><br />
right (Fig. 2) and left <strong>com</strong>mon carotid artery IMT<br />
(Fig. 3). AASI was negatively correlated with FMD<br />
(Fig. 4) and <strong>the</strong> dilatation ratio (Fig. 5).<br />
Table 2: Comparison if <strong>the</strong> blood pressure data and AASI in between <strong>the</strong> study groups.<br />
Office SBP<br />
Office DBP<br />
Mean 24h SBP<br />
Mean 24h DBP<br />
AASI<br />
Group 1<br />
(n=20)<br />
Mean<br />
127.35<br />
77.50<br />
123.05<br />
74.8<br />
0.52<br />
SBP = Systolic Blood Pressure.<br />
DBP = Diastolic Blood Pressure.<br />
SD<br />
5.32<br />
6.39<br />
6.65<br />
6.63<br />
.062<br />
Mean<br />
165.56<br />
97.78<br />
152.11<br />
94.33<br />
0.73<br />
Group 2<br />
(n=18)<br />
SD<br />
19.31<br />
10.03<br />
22.36<br />
10.63<br />
0.104<br />
Mean<br />
170.72<br />
97.67<br />
148.59<br />
92.03<br />
0.79<br />
Group 3<br />
(n=32)<br />
SD<br />
13.68<br />
11.57<br />
9.09<br />
7.1<br />
0.08<br />
G1 vrs G2<br />
Early Vascular Changes Preceding Morphological Cardiac Changes<br />
Left CCA-IMT<br />
Figure 3: Correlation between <strong>the</strong> AASI and <strong>the</strong> left CCA<br />
IMT.<br />
Dil Ratio<br />
0.35<br />
0.30<br />
0.25<br />
0.20<br />
0.15<br />
0.10<br />
0.05<br />
0.00<br />
0.00 .10 .20 .30 .40 .50 .60 .70 .80 .90 1.0<br />
250<br />
200<br />
150<br />
100<br />
50<br />
Left CCA-IMT<br />
p
Mohammed A Abdel Wahab<br />
decrease in FMD with progression <strong>of</strong> geometry to<br />
abnormal forms. This agrees with a previous study<br />
[15] that showed that <strong>the</strong> endo<strong>the</strong>lium-dependent<br />
vasodilatation is impaired progressively as LV<br />
hypertrophy advances. Also it was detected that<br />
FMD was considerably higher in <strong>the</strong> normo-tensive<br />
than in hypertensive patients with left ventricular<br />
hypertrophy [12].<br />
We also found that AASI is significantly correlated<br />
with LVMI. The same data obtained from<br />
[16] that concluded that as vascular resistance and<br />
left ventricular mass are also related. These findings<br />
could speak for a parallel development <strong>of</strong> total<br />
peripheral resistance and left ventricular hypertrophy<br />
in essential hypertension.<br />
Our results showed that AASI is negatively<br />
correlated with FMD, dilatation ratio and positively<br />
correlated with IMT <strong>of</strong> both carotid arteries. In<br />
agreement with result <strong>of</strong> <strong>the</strong> current study, previous<br />
study investigated <strong>the</strong> relationship between endo<strong>the</strong>lial<br />
damage/dysfunction, arterial stiffness (measured<br />
using digital volume photoplethysmography<br />
and expressed as <strong>the</strong> stiffness index) and found<br />
that significant correlation between circulating<br />
endo<strong>the</strong>lial cells and <strong>the</strong> stiffness index [17]. Meanwhile,<br />
endo<strong>the</strong>lial cell function and vascular smooth<br />
muscle cell tone do also have a strong influence<br />
on arterial stiffness. Arterial tone is affected by a<br />
number <strong>of</strong> factors like shear mechanical stress as<br />
well as paracrine mediators such as angiotensin II,<br />
endo<strong>the</strong>lin, and NO [18]. Fur<strong>the</strong>rmore, it was found<br />
that, aortic pulsed wave velocity (PWV) as a marker<br />
as arterial stiffness correlated inversely with FMD<br />
in a group <strong>of</strong> patients with isolated systolic hypertension<br />
[19].<br />
The magnitudes <strong>of</strong> carotid intima-medial thickness<br />
and lumen diameter parallel levels <strong>of</strong> LV mass<br />
and geometry, and are directly related to stroke<br />
volume and arterial stiffness [9].<br />
Evidence from both animal and human studies<br />
suggests that <strong>the</strong> endo<strong>the</strong>lium is an important<br />
regulator <strong>of</strong> arterial stiffness, both functionally<br />
and structurally. Inhibition <strong>of</strong> basal nitric oxide<br />
(NO) production in <strong>the</strong> endo<strong>the</strong>lium with Lmonomethyl-NG-arginine<br />
(L-NMMA) increases<br />
iliac PWV in sheep and, in humans, increases<br />
augmentation index and brachial artery stiffness<br />
[20].<br />
Nitric oxide (NO) may play a role in <strong>the</strong> pathogenesis<br />
<strong>of</strong> hypertension and its <strong>com</strong>plications.<br />
87<br />
Agents that inhibit NO through enzyme nitric oxide<br />
syn<strong>the</strong>tase (eNOS) cause endo<strong>the</strong>lium dependant<br />
contraction, and reduction in <strong>the</strong> blood flow. A<br />
continuous inhibition <strong>of</strong> NO-dependant vasodilatation<br />
results in hypertension and its related organ<br />
damage [20]. Also endo<strong>the</strong>lins have additional<br />
effects in vascular hypertrophy and increasing<br />
blood pressure, in addition to its systemic vasoconstrictor<br />
effect endo<strong>the</strong>lin-1 (E-1) is a growth factor<br />
in <strong>the</strong> cardiovascular system, in vitro studies demonstrated<br />
that endo<strong>the</strong>lins stimulates mitogenesis,<br />
hypertrophy including vascular and cardiac hypertrophy<br />
and protein syn<strong>the</strong>sis in vascular smooth<br />
muscle cells [20].<br />
From all <strong>the</strong> above data we can conclude that<br />
early vascular changes in <strong>the</strong> form <strong>of</strong> increased<br />
IMT, reduced vasodilator capacity and increased<br />
arterial stiffness precedes changes in LV geometry.<br />
The result that AASI is increased with <strong>the</strong> progression<br />
<strong>of</strong> LV geometry into abnormal geometry inspite<br />
<strong>of</strong> no significant change in blood pressure measurement<br />
may suggest that arterial stiffness (ra<strong>the</strong>r<br />
than increased blood pressure levels) is <strong>the</strong> cause<br />
<strong>of</strong> <strong>the</strong> progression <strong>of</strong> LV geometry and that endo<strong>the</strong>lial<br />
dysfunction may be <strong>the</strong> cornerstone in this<br />
story through its effect on arterial stiffness.<br />
References<br />
1- Di Bello VD, Pedrinelli R, Giorgi D, Bertini A, Talini E,<br />
Caputo MT, Dell'Omo G, Cioppi A, Moretti L, Paterni<br />
M, Giusti C: The potential prognostic value <strong>of</strong> ultrasonic<br />
characterization (videodensitometry) <strong>of</strong> myocardial tissue<br />
in essential arterial hypertension. Coron Artery Dis 2000<br />
Oct; 11 (7): 513-21.<br />
2- Ganau A, Devereux RB, Roman MJ, De Simone G, Pickering<br />
TG, Saba PS, Vargiu P, Simongini I, Laragh JH:<br />
Patterns <strong>of</strong> left ventricular hypertrophy and geometric<br />
remodeling in essential hypertension. J Am Coll Cardiol<br />
1992; 19: 1550-1558.<br />
3- Wolk R: Arrhythmogenic mechanisms in left ventricular<br />
hypertrophy. Europace 2000; 2: 216-223.<br />
4- Foppa M, Duncan B-B, Rohde L-E: "Echocardiographybased<br />
left ventricular mass estimation. How should we<br />
define hypertrophy?", Cardiovascular Ultrasound 2005;<br />
3: 17.<br />
5- De Luca N, Marchegiano R, Gisonni P, Iovino G, Fontana<br />
D, D'Auria F, Macciocchi B, Trimarco B, Pompeo F:<br />
Carotid vascular structural changes and left ventricular<br />
hypertrophy. Minerva Cardioangiol 1994 Dec; 42 (12):<br />
569-73.<br />
6- Li Y, Wang JG, Dolan E, Gao PJ, Guo HF, Nawrot T,<br />
Stanton AV, Zhu DL, O’Brien E, Staessen JA: "Ambulatory<br />
Arterial Stiffness Index Derived From 24-Hour Ambulatory<br />
Blood Pressure Monitoring", Hypertension 2006; 47:<br />
359-364.
Early Vascular Changes Preceding Morphological Cardiac Changes<br />
7- Hashimoto M, Miyamoto Y, Matsuda Y, Akita H: "New<br />
methods to evaluate endo<strong>the</strong>lial function: Non invasive<br />
methods <strong>of</strong> evaluating endo<strong>the</strong>lial function in humans",<br />
J Pharmacol Sci 2003; 93: 405.<br />
8- Pierdomenico SD, Lapenna D, Guglielmi MD, Porreca<br />
E, Antidormi T, Cuccurullo F, Mezzetti A.: Vascular<br />
changes in hypertensive patients with different left ventricular<br />
geometry. J Hypertens. 1995 Dec; 13 (12 Pt 2):<br />
1701-6.<br />
9- de Simone G, McClelland R, Gottdiener JS, Celentano<br />
A, Kronmal RA, Gardin JM: Relation <strong>of</strong> hemodynamics<br />
and risk factors to ventricular-vascular interactions in <strong>the</strong><br />
elderly: The Cardiovascular Health Study. J Hypertens<br />
2001 Oct; 19 (10): 1893-903.<br />
10- Guarini P, Tedeschi C, Giordano G, Messina V, Cicatiello<br />
AM, Strollo L Guarini, et al: Effects <strong>of</strong> hypertension on<br />
intimal-medial thickness, left ventricular mass and aortic<br />
distensibility. Int Angiol 1994 Dec; 13 (4): 317-22.<br />
11- Muiesan ML, Salvetti M, Zulli R, Pasini GF, Bettoni G,<br />
Monteduro C, Rizzoni D, Castellano M, Agabiti-Rosei<br />
E: Structural association between <strong>the</strong> carotid artery and<br />
<strong>the</strong> left ventricle in a general population in Nor<strong>the</strong>rn Italy:<br />
<strong>the</strong> Vobarno study. J Hypertens 1998 Dec; 16 (12 Pt 1):<br />
1805-12.<br />
12- Tsai WC, Lin CC, Huang YY, Chen JY, Chen JH: "Association<br />
<strong>of</strong> increased arterial stiffness and inflammation<br />
with proteinuria and left ventricular hypertrophy in nondiabetic<br />
hypertensive patients", Blood Press 2007; 5: 1-<br />
6.<br />
13- Libhaber E, Woodiwiss AJ, Libhaber C, Maseko M,<br />
Majane OH, Makaula S, Dessein P, Essop MR, Sareli P,<br />
Norton GR: Gender-specific brachial artery blood pressureindependent<br />
relationship between pulse wave velocity<br />
88<br />
and left ventricular mass index in a group <strong>of</strong> African<br />
ancestry. J Hypertens 2008 Aug; 26 (8): 1619-28.<br />
14- Palmieri V, Bella JN, Roman MJ, Gerdts E, Papademetriou<br />
V, Wachtell K, Nieminen MS, Dahlöf B, Devereux RB:<br />
Pulse pressure/stroke index and left ventricular geometry<br />
and function: The LIFE Study. J Hypertens 2003 Apr; 21<br />
(4): 781-7.<br />
15- Sekiya M, Funada J, Suzuki J, Watanabe K, Miyagawa<br />
M, Akutsu H: The influence <strong>of</strong> left ventricular geometry<br />
on coronary vasomotion in patients with essential hypertension.<br />
Am J Hypertens 2000 Jul; 13 (7): 789-95.<br />
16- Schulte KL, Liederwald K, Meyer-Sabellek W, van Gemmeren<br />
D, Lenz T, Gotzen R: Relationships between ambulatory<br />
blood pressure, forearm vascular resistance, and<br />
left ventricular mass in hypertensive and normotensive<br />
subjects. Am J Hypertens 1993 Sep; 6 (9): 786-93.<br />
17- Boos CJ, Lane DA, Karpha M, Beevers G, Haynes R, Lip<br />
GYH: "Circulating Endo<strong>the</strong>lial Cells, Arterial Stiffness,<br />
and Cardiovascular Risk Stratification in Hypertension",<br />
Chest 2007; 132: 1540-1547.<br />
18- Vane J, Anggard E, Botting R: "Regulatory function <strong>of</strong><br />
<strong>the</strong> vascular endo<strong>the</strong>lium". New England Journal <strong>of</strong><br />
Medicine 1990; 323: 27-36.<br />
19- Wallace SML, McEniery CM, Mäki-Petäjä KM, Booth<br />
AD, Cockcr<strong>of</strong>t JR, Wilkinson IB: "Isolated Systolic<br />
Hypertension Is Characterized by Increased Aortic Stiffness<br />
and Endo<strong>the</strong>lial Dysfunction", Hypertension 2007;<br />
50: 228.<br />
20- Oliver JJ, Webb DJ: "Noninvasive Assessment <strong>of</strong> Arterial<br />
Stiffness and Risk <strong>of</strong> A<strong>the</strong>rosclerotic Events", Arteriosclerosis<br />
and Thrombosis and Vascular Biology 2003; 23:<br />
554-566.
Egypt Heart J 62 (1): 89-101, March 2010<br />
Metabolic Syndrome as A Predictor <strong>of</strong> Non Dipping Hypertension<br />
ISLAM MOHAMED MAHDY EL-HELALY, MD; MOHAMED AYMAN SALEH, MD;<br />
AYMAN SADEK, MD; AHMED ONSY, MD<br />
Introduction: Metabolic syndrome (MS) and non-dipping hypertension both increase cardiovascular mortality. Although<br />
both clinical modalities share <strong>com</strong>mon pathophysiologic factors in <strong>the</strong>ir etiologies, previous studies did not find any association<br />
between <strong>the</strong>m [1]. Metabolic syndrome is a <strong>com</strong>plex disorder considered a "multiplex" cardiovascular risk factor, in that each<br />
<strong>com</strong>ponent <strong>of</strong> <strong>the</strong> cluster <strong>of</strong> abnormalities is a risk factor in its own right. Introduced as Syndrome X and also termed insulin<br />
resistance syndrome [2,3]. It is known that blood pressure varies markedly over 24-h period but <strong>the</strong> prognostic significance <strong>of</strong><br />
<strong>the</strong>se changes is still a matter for dispute. In particular, much attention has been paid to blood pressure changes associated with<br />
<strong>the</strong> sleep-wake cycle. Most individuals have a substantial fall in blood pressure when <strong>the</strong>y sleep ac<strong>com</strong>panied by a decrease<br />
in heart rate. It appeared that some individuals have little or no fall in blood pressure when <strong>the</strong>y sleep. This has led to classification<br />
<strong>of</strong> subjects into dippers and non-dippers [4]. Nocturnal non dipping refers to a 10% or lesser magnitude reduction in average<br />
systolic blood pressure SBP and/or diastolic blood pressure DBP at nighttime <strong>com</strong>pared to daytime SBP average values, The<br />
remainder defined as dipper [5]. Reduced nocturnal blood pressure fall is considered one <strong>of</strong> clinical traits associated with a<br />
greater cardiovascular risk and end organ damage [6,7].<br />
Aim <strong>of</strong> work: This work aimed at investigating <strong>the</strong> association between metabolic syndrome according to International<br />
Diabetes Federation criteria 2006 and non-dipping blood pressure as assessed by 24h ambulatory blood pressure.<br />
Patients and Methods: This study included 100 consecutive patients referred to <strong>the</strong> clinic in Mubarak Police Hospital with<br />
recently diagnosed essential hypertension for evaluation <strong>of</strong> blood pressure with ambulatory blood pressure monitoring (ABPM).<br />
These patients were subdivided into two groups according to <strong>the</strong> International Diabetes Federation 2006 (IDF 2006) criteria<br />
<strong>of</strong> metabolic syndrome. 1) 50 patients had metabolic syndrome. 2) 50 patients did not have metabolic syndrome.<br />
Exclusion criteria: Patients who had any <strong>of</strong> <strong>the</strong> following conditions are excluded from <strong>the</strong> study such as: Secondary<br />
hypertension, Congestive heart failure, Previous myocardial infarction, Cardiac valve disease, Chronic renal failure, Any<br />
conditions preventing technically adequate ABPM as atrial fibrillation.<br />
All <strong>of</strong> <strong>the</strong> Patients were Evaluated as Follow: I-A detailed history taking, II-A careful physical examination was done with<br />
search for evidence <strong>of</strong> organ damage and signs suggesting secondary hypertension, III-Laboratory investigations, IV-<br />
Electrocardiogram: 12 leads ECG was done under resting condition, V-All <strong>the</strong> patients with metabolic syndrome were evaluated<br />
according to Metabolic syndrome score (MS-Score) and VI-Ambulatory blood pressure monitoring (ABPM).<br />
Results: Study included 56 male representing 56% and 44 female, Dippers were 61 patients (61%) while non dippers were<br />
39 patients (39%) who showed a 10% or lesser magnitude reduction in average SBP and/or DBP at nighttime <strong>com</strong>pared to<br />
daytime SBP and/or DBP average value. The WC was above normal range in (17 subjects) 35.4% <strong>of</strong> dippers and (31 subjects)<br />
64.6% <strong>of</strong> non dippers (p
Metabolic Syndrome as A Predictor <strong>of</strong> Non Dipping Hypertension<br />
and male gender. The MS-score level was <strong>the</strong> most strong independent predictor <strong>of</strong> non dipping status with Odds ratio (OR)<br />
12.3, 95% Confidence Interval (CI) 4.371-29.245, (p
Islam M.M. El-Helaly, et al<br />
study such as: Secondary hypertension, Congestive<br />
heart failure, Previous myocardial infarction, Cardiac<br />
valve disease, Chronic renal failure, Any<br />
conditions preventing technically adequate ABPM<br />
as atrial fibrillation.<br />
All <strong>of</strong> <strong>the</strong> patients were evaluated as follow:<br />
I- A detailed history taking was done and provided<br />
information about:<br />
(A) Risk factors such as smoking, diabetes mellitus<br />
which is a group <strong>of</strong> metabolic diseases characterized<br />
by hyperglycemia due to defects in<br />
insulin secretion, action or both (ADA, 2008),<br />
hypertension, medical treatment, lifestyle factors<br />
such as dietary intake and physical activity.<br />
(B) Past history or current symptoms <strong>of</strong> coronary<br />
disease, heart failure, cerebrovascular or peripheral<br />
vascular disease, renal disease, gout,<br />
dyslipidemia, asthma or any o<strong>the</strong>r significant<br />
illnesses.<br />
(C) Symptoms suggestive <strong>of</strong> secondary causes <strong>of</strong><br />
hypertension and intake <strong>of</strong> drugs or substances<br />
that can raise blood pressure such as nasal<br />
drops.<br />
(D) Family and environmental factors that may<br />
influence blood pressure.<br />
II- A careful physical examination was done with<br />
search for evidence <strong>of</strong> organ damage and signs<br />
suggesting secondary hypertension:<br />
Office Arterial blood pressure was measured<br />
by a physician in <strong>the</strong> hospital clinic, using a mercury<br />
sphygmomanometer, after <strong>the</strong> subject sat for<br />
≥5 min and at least 30 minutes after caffeine, and<br />
smoking and without any stress. Measurements<br />
were done with appropriate Cuff size; <strong>the</strong> bladder<br />
encircled and covered two-thirds <strong>of</strong> <strong>the</strong> length <strong>of</strong><br />
<strong>the</strong> arm. A stethoscope placed lightly over <strong>the</strong><br />
brachial artery. The cuff was at <strong>the</strong> level <strong>of</strong> <strong>the</strong><br />
heart. Systolic pressure was defined as <strong>the</strong> pressure<br />
reading at <strong>the</strong> onset <strong>of</strong> <strong>the</strong> sounds described by<br />
Korotk<strong>of</strong>f (Phase one). Diastolic pressure was <strong>the</strong>n<br />
recorded as <strong>the</strong> pressure at which <strong>the</strong> sounds disappeared<br />
(K5). The average <strong>of</strong> six or more measurements<br />
for three sessions within a week was<br />
considered for <strong>the</strong> analysis with two measurements<br />
made at least 5 minutes apart each session, <strong>the</strong><br />
patients were not on any adrenergic stimulants,<br />
such as those found in many cold medications. An<br />
initial measurement included both arms. In elderly<br />
patients aged 60 years or more blood pressure was<br />
measured in <strong>the</strong> lying, sitting and standing position<br />
[1].<br />
91<br />
Waist circumference was measured at <strong>the</strong> midpoint<br />
between <strong>the</strong> bottom <strong>of</strong> <strong>the</strong> rib cage and above<br />
<strong>the</strong> top <strong>of</strong> <strong>the</strong> iliac crest from patient in standing<br />
position at breath hold after full expiration using<br />
a flexible tape measure and maintaining close<br />
contact with <strong>the</strong> skin without <strong>com</strong>pression <strong>of</strong> <strong>the</strong><br />
underlying tissue [1].<br />
III- Laboratory investigations were done as follow:<br />
Fasting blood sugar: blood sample was taken<br />
from <strong>the</strong> patient after fasting for 8 hours and analyzed<br />
with enzymatic ultraviolet test (N: 70-100<br />
mg/dl) (ADA, 2008).<br />
Fasting serum triglycerides: (N
Metabolic Syndrome as A Predictor <strong>of</strong> Non Dipping Hypertension<br />
V- All <strong>the</strong> patients with metabolic syndrome<br />
were evaluated according to Metabolic syndrome<br />
score (MS-Score) developed by [10] which was<br />
modified according to International Diabetes Federation<br />
2006 for Middle East (Arab) populations<br />
Waist circumference and <strong>the</strong>n all <strong>the</strong> points that<br />
were assigned for <strong>the</strong> different 6 risk factors are<br />
summed. These 6 risk factors were shown in <strong>the</strong><br />
Table (2) as <strong>the</strong> following: (I) Male gender, (II)<br />
Age >50 years, (III) Waist circumference, (IV)<br />
Fasting HDL-C, (V) Fasting Triglycerides, (VI)<br />
Fasting blood glucose.<br />
Table 2: Metabolic syndrome score.<br />
Risk factor<br />
Men<br />
Age >50 years<br />
Waist circumference:<br />
Islam M.M. El-Helaly, et al<br />
Table 3: Gender and smokers frequency in <strong>the</strong> whole study.<br />
Male/female<br />
Smokers/non-smokers<br />
Total<br />
Frequency<br />
56/44<br />
33/67<br />
100<br />
Percent<br />
Table (4) describes age, waist circumference,<br />
biochemical data and metabolic score in <strong>the</strong> whole<br />
study and showed that <strong>the</strong> mean age <strong>of</strong> <strong>the</strong> whole<br />
populations was 49.2±7.1 years and ranged between<br />
(28-68) years, <strong>the</strong> mean waist circumference was<br />
92±9.7 cm and ranged between (75-109) cm, <strong>the</strong><br />
mean fasting blood sugar was 122±59.4 mg/dl and<br />
ranged between (48-408) mg/dl, <strong>the</strong> mean fasting<br />
triglycerides was 199±124.3 mg/dl and ranged<br />
between (48-855) mg/dl, <strong>the</strong> mean fasting high<br />
density lipoproteins was 47.1±14.2 mg/dl and<br />
ranged between (13-99) mg/dl, <strong>the</strong> mean fasting<br />
low density lipoproteins was143±45.1 and ranged<br />
between (56-260) mg/dl.<br />
All <strong>the</strong> patients were evaluated according to<br />
metabolic syndrome score, <strong>the</strong> mean score was<br />
38.6±8.3 and ranged between (17-53).<br />
Table 4: Age, WC, biochemical data and MSscore<br />
in <strong>the</strong> whole study population.<br />
AGE (yrs)<br />
WC (cm)<br />
FBS (mg/dl)<br />
TG (mg/dl)<br />
HDL (mg/dl)<br />
LDL (mg/dl)<br />
MS-score<br />
Mean<br />
49.2±7.1<br />
92±9.7<br />
122.9±59.4<br />
199±124.3<br />
47.1±14.2<br />
143±45.1<br />
38.6±8.3<br />
Range<br />
28-68<br />
75-109<br />
84-408<br />
48-855<br />
13-99<br />
56-260<br />
17-53<br />
56-44<br />
33-67<br />
100<br />
The mean clinic systolic blood pressure was<br />
153±8.1 mmHg and ranged between (140-170)<br />
mmHg, <strong>the</strong> mean clinic diastolic blood pressure<br />
was95.1±6.4 mmHg and ranged between (80-115)<br />
mmHg, <strong>the</strong> mean average day systolic blood pressure<br />
was 141.7±6.1 mmHg and ranged between<br />
(135-161) mmHg, <strong>the</strong> mean average day diastolic<br />
blood pressure was 83.1±6.7 mmHg and ranged<br />
between (70-99) mmHg, <strong>the</strong> mean average night<br />
systolic blood pressure 128±13.5 mmHg and ranged<br />
between (111-174) mmHg, <strong>the</strong> mean average night<br />
diastolic blood pressure was 74.8±8.7 mmHg and<br />
ranged between (62-99) mmHg.<br />
93<br />
II- Analysis <strong>of</strong> dippers and non dippers data <strong>of</strong><br />
<strong>the</strong> whole study population:<br />
Dippers were 61 patients (61%) while non<br />
dippers were 39 patients (39%) who showed a 10%<br />
or lesser magnitude reduction in average SBP<br />
and/or DBP at nighttime <strong>com</strong>pared to daytime SBP<br />
and/or DBP average value as shown in Chart (1).<br />
Dippers %<br />
Table (5) describes <strong>the</strong> number and age in<br />
dippers and non dippers <strong>of</strong> <strong>the</strong> whole study population<br />
and showed that <strong>the</strong> mean age <strong>of</strong> dippers<br />
was 48.8±6.6 and that <strong>of</strong> non dippers was 49.6±7.8<br />
and <strong>the</strong>re was no significant difference between<br />
<strong>the</strong> two groups.<br />
Table 5: Number and mean age in dippers and non dippers<br />
<strong>of</strong> <strong>the</strong> study.<br />
Number<br />
Mean age (yrs)<br />
70<br />
60<br />
50<br />
40<br />
30<br />
20<br />
10<br />
0<br />
Non-dippers %<br />
Chart 1: Dippers and non dippers frequency in <strong>the</strong> whole<br />
study population.<br />
Dippers<br />
61<br />
48.8±6.6<br />
Frequency<br />
Non dippers<br />
39<br />
49.6±7.8<br />
p<br />
–<br />
0.597<br />
Table (6) describes Frequency and percentage<br />
<strong>of</strong> MS risk factors in dippers and non dippers <strong>of</strong><br />
<strong>the</strong> whole study and showed that:<br />
The WC was above normal range in (17 subjects)<br />
35.4% <strong>of</strong> dippers and (31 subjects) 64.6%<br />
<strong>of</strong> non dippers. There was a highly significant<br />
difference between <strong>the</strong> two groups.<br />
The HDL level was below normal range in (22<br />
subjects) 47.8% <strong>of</strong> dippers and (24 subjects) 52.2%<br />
<strong>of</strong> non dippers, <strong>the</strong>re was a significant difference<br />
between <strong>the</strong> two groups. The TG level was above<br />
normal range in (27 subjects) 47.4% <strong>of</strong> dippers<br />
and (30 subjects) 52.6% <strong>of</strong> non dippers, <strong>the</strong>re was<br />
a highly significant difference between <strong>the</strong> two<br />
groups.<br />
61<br />
61<br />
39<br />
39
Metabolic Syndrome as A Predictor <strong>of</strong> Non Dipping Hypertension<br />
The FBS was above normal range in (28 subjects)<br />
41.8% <strong>of</strong> dippers and (39 subjects) 58.2%<br />
<strong>of</strong> non dippers. There was a highly significant<br />
difference between <strong>the</strong> two groups.<br />
Table 6: Frequency and percentage <strong>of</strong> MS risk factors in<br />
dippers and non dippers <strong>of</strong> <strong>the</strong> whole study.<br />
WC ANR<br />
HDL BNR<br />
TG >150 mg/dl<br />
FBS >100 mg/dl<br />
Dippers<br />
17 (35.4%)<br />
22 (47.8%)<br />
27 (47.4%)<br />
28 (41.8%)<br />
Non dippers<br />
31 (64.6%)<br />
24 (52.2%)<br />
30 (52.6%)<br />
39 (58.2%)<br />
(ANR: Above normal range, BNR: Below normal range).<br />
Islam M.M. El-Helaly, et al<br />
Dippers %<br />
50<br />
40<br />
30<br />
20<br />
10<br />
0<br />
Non-dippers %<br />
17<br />
Chart 2: Number <strong>of</strong> dippers and non dippers with and without<br />
<strong>the</strong> metabolic syndrome.<br />
Table (9) describes <strong>the</strong> age, WC, biochemical<br />
data and MS-score in dippers and non dippers<br />
patients with metabolic syndrome and showed that:<br />
The mean age <strong>of</strong> dippers was 47.2±6.7 years<br />
and that <strong>of</strong> non dippers was 49.3±8.1 years. There<br />
was no significant difference between <strong>the</strong> two<br />
groups.<br />
The mean waist circumference <strong>of</strong> dippers was<br />
99.2±3.9 cm and that <strong>of</strong> non dippers was 99.5±6.5<br />
cm. There was no significant difference between<br />
<strong>the</strong>m.<br />
The mean fasting TG <strong>of</strong> dippers was 225.5±<br />
106.5 mg/dl and that <strong>of</strong> non dippers was 250.9±<br />
119.3 mg/dl. There was no significant difference<br />
between <strong>the</strong> two groups.<br />
The mean fasting HDL <strong>of</strong> dippers was 44.4±17.1<br />
mg/dl and that <strong>of</strong> non dippers was 41.4±11.4 mg/dl.<br />
There was no significant difference between <strong>the</strong><br />
two groups.<br />
The mean fasting LDL <strong>of</strong> dippers was 147.9±<br />
47.6 mg/dl and that <strong>of</strong> non dippers was 161.4±45.1<br />
mg/dl. There was no significant difference between<br />
<strong>the</strong> two groups.<br />
The mean fasting blood sugar <strong>of</strong> dippers was<br />
97.4±10.1 mg/dl and that <strong>of</strong> non dippers was<br />
170.1±85.3 mg/dl. There was a highly significant<br />
difference between <strong>the</strong> two groups.<br />
There was no subject with DM (0%) in dippers<br />
while 8 subjects (24%) <strong>of</strong> <strong>the</strong> non dippers had DM.<br />
There was a highly significant difference between<br />
<strong>the</strong> two groups.<br />
33<br />
44<br />
Metabolic Non<br />
17<br />
33<br />
44<br />
6<br />
6<br />
95<br />
The mean metabolic score <strong>of</strong> dippers was 28.9±<br />
5.1 and that <strong>of</strong> non dippers was 43.6±4.2 and <strong>the</strong>re<br />
was a highly significant difference between <strong>the</strong><br />
two groups.<br />
Table 9: Age, WC, biochemical data and MS-score in dippers<br />
and non dippers patients with metabolic syndrome.<br />
Age (yrs)<br />
WC (cm)<br />
TG (mg/dl)<br />
HDL (mg/dl)<br />
LDL (mg/dl)<br />
FBS (mg/dl)<br />
DM<br />
MS-score<br />
Dippers<br />
47.2±6.7<br />
99.2±3.9<br />
225.5±106.5<br />
44.4±17.1<br />
147.9±47.6<br />
97.4±10.1<br />
0 (0%)<br />
28.9±5.1<br />
Non dippers<br />
49.3±8.1<br />
99.5±6.5<br />
250.9±119.3<br />
41.4±11.4<br />
161.4±45.1<br />
170.1±85.3<br />
8 (24%)<br />
43.6±4.2<br />
p<br />
0.375<br />
0.830<br />
0.463<br />
0.463<br />
0.333<br />
Metabolic Syndrome as A Predictor <strong>of</strong> Non Dipping Hypertension<br />
Table 10: Age, WC, biochemical data and MS-score in dippers<br />
and non dippers <strong>of</strong> patients without metabolic syndrome.<br />
Age (yrs)<br />
WC (cm)<br />
TG (mg/dl)<br />
HDL (mg/dl)<br />
LDL (mg/dl)<br />
FBS (mg/dl)<br />
MS-score<br />
Dippers<br />
49.5±6.6<br />
84.7±6.7<br />
139.7±65.7<br />
50.5±11.7<br />
133.6±39.1<br />
98.1±6.8<br />
23.7±6.4<br />
Non dippers<br />
51.7±6.5<br />
83±7.5<br />
139.2±62.5<br />
60.3±21.9<br />
119.8±17.6<br />
117.8±12.7<br />
37.5±4.6<br />
0.451<br />
0.562<br />
0.984<br />
0.094<br />
0.403<br />
Islam M.M. El-Helaly, et al<br />
Table (13) describes <strong>the</strong> age, frequency and<br />
percent <strong>of</strong> gender and smokers in subjects with<br />
high score MS and that <strong>of</strong> low score MS <strong>of</strong> <strong>the</strong><br />
whole study population and showed that:<br />
The mean age was 49.2±7.8 cm in high MSscore<br />
and 49.1±6.7 cm in that <strong>of</strong> low MS-score.<br />
There was no significant difference between <strong>the</strong><br />
two groups.<br />
Males constituted 62% (23 patients) <strong>of</strong> subjects<br />
with high MS-score and 54% (34 patients) <strong>of</strong><br />
subjects with low MS-score. There was no significant<br />
difference between <strong>the</strong> two groups.<br />
Females constituted 38% (14 patients) <strong>of</strong> subjects<br />
with high MS-score and 46% (29 patients)<br />
<strong>of</strong> subjects with low MS-score. There was no<br />
significant difference between <strong>the</strong> two groups.<br />
Smokers constituted 32% (12 patients) <strong>of</strong> subjects<br />
with high MS-score and 33% (21 patients)<br />
<strong>of</strong> subjects with low MS-score (33%). There was<br />
no significant difference between <strong>the</strong> two groups.<br />
Table 13: Age, gender, smokers in high MS-score and low<br />
MS-score <strong>of</strong> <strong>the</strong> whole study.<br />
Age (yrs)<br />
Gender (M)<br />
Gender (F)<br />
Smokers<br />
70<br />
60<br />
50<br />
40<br />
30<br />
20<br />
10<br />
0<br />
High score<br />
Low score<br />
Chart 4: Percentage <strong>of</strong> high MS-score and low MS-score <strong>of</strong><br />
<strong>the</strong> whole study population.<br />
High score<br />
49.2±7.8<br />
23 (62%)<br />
14 (38%)<br />
12 (32%)<br />
37<br />
Number<br />
37<br />
63<br />
63<br />
Low score<br />
49.1±6.7<br />
34 (54%)<br />
29 (46%)<br />
21 (33%)<br />
p<br />
0.960<br />
0.104<br />
0.244<br />
0.171<br />
97<br />
Table (14) describes <strong>the</strong> WC, biochemical data<br />
and metabolic score in high MS-score and low<br />
MS-score <strong>of</strong> <strong>the</strong> whole study and showed that:<br />
The mean waist circumference was 98.1±7.6<br />
cm in subjects with high MS-score and 88.3±9 cm<br />
in that <strong>of</strong> low MS-score. There was a highly significant<br />
difference between <strong>the</strong> two groups.<br />
The mean fasting blood sugar in subjects with<br />
high MS-score was 164.5±82.1 mg/dl and in that<br />
<strong>of</strong> low MS-score was 98.5±8.5 mg/dl. There was<br />
a highly significant difference between <strong>the</strong> two<br />
groups.<br />
The mean fasting TG was 238.3±118.5 mg/dl<br />
in subjects with high MS-score and 163.3±87.6<br />
mg/dl in that <strong>of</strong> low MS-score. There was a highly<br />
significant difference between <strong>the</strong> two groups.<br />
The mean fasting HDL was 43.1±12 mg/dl in<br />
subjects with high MS-score and 49.4±14.9 mg/dl<br />
in that <strong>of</strong> low MS-score. There was a significant<br />
difference between <strong>the</strong> two groups.<br />
The mean fasting LDL was 157.2±44.7 mg/dl<br />
in subjects with high MS-score and 136.8±41.3<br />
mg/dl in that <strong>of</strong> low MS-score. There was a significant<br />
difference between <strong>the</strong> two groups.<br />
The mean metabolic score was 43.2±4.2 in<br />
subjects with high MS-score and 25.4±6.5 in that<br />
<strong>of</strong> low MS-score. There was a highly significant<br />
difference between <strong>the</strong> two groups.<br />
Table 14: WC, biochemical data and MS-score in high MSscore<br />
and low MS-score <strong>of</strong> <strong>the</strong> whole study population.<br />
Waist circumference<br />
(cm)<br />
LDL (mg/dl)<br />
HDL (mg/dl)<br />
TG (mg/dl)<br />
FBS (mg/dl)<br />
MS-score<br />
High score<br />
98.1±7.6<br />
157.2±44.7<br />
43.1±12<br />
238.3±118.5<br />
164.5±82.1<br />
43.2±4.2<br />
Low score<br />
88.3±9<br />
136.8±41.3<br />
49.4±14.9<br />
163.3±87.6<br />
98.5±8.5<br />
25.4±6.5<br />
p<br />
Metabolic Syndrome as A Predictor <strong>of</strong> Non Dipping Hypertension<br />
score. There was a significant difference between<br />
<strong>the</strong> two groups.<br />
The mean average day diastolic blood pressure<br />
was 84.1±6.3 mmHg in subjects with high MSscore<br />
and 82.6±6.9 mmHg in that <strong>of</strong> low MS-score.<br />
There was no significant difference between <strong>the</strong><br />
two groups.<br />
The mean average night systolic blood pressure<br />
was 141±12.8 mmHg in subjects with high MSscore<br />
and 121.4±6.8 mmHg in that <strong>of</strong> low MSscore.<br />
There was a highly significant difference<br />
between <strong>the</strong> two groups. The mean average night<br />
diastolic blood pressure was 80.4±9.7 mmHg in<br />
subjects with high MS-score and 71.5±6 mmHg<br />
in that <strong>of</strong> low MS-score. There was a highly significant<br />
difference between <strong>the</strong> two groups.<br />
Table 15: ABPM data in high MS-score and low MS-score<br />
<strong>of</strong> <strong>the</strong> whole study population.<br />
Daytime SBP<br />
Daytime DBP<br />
Nighttime SBP<br />
Nighttime DBP<br />
High score<br />
143.9±7.4<br />
84.1±6.3<br />
141.8±12.8<br />
80.4±9.7<br />
Low score<br />
140.3±4.4<br />
82.6±6.9<br />
121.4±6.8<br />
71.5±6<br />
0.002<br />
0.274<br />
Islam M.M. El-Helaly, et al<br />
that it can be precipitated by multiple underlying<br />
risk factors. The most important <strong>of</strong> <strong>the</strong>se underlying<br />
risk factors are abdominal obesity and insulin<br />
resistance. O<strong>the</strong>r associated conditions include<br />
physical inactivity, aging, hormonal imbalance,<br />
and genetic or ethnic predisposition [8].<br />
It is known that blood pressure varies markedly<br />
over 24-h period but <strong>the</strong> prognostic significance<br />
<strong>of</strong> <strong>the</strong>se changes is still a matter for dispute. In<br />
particular, much attention has been paid to blood<br />
pressure changes associated with <strong>the</strong> sleep-wake<br />
cycle. Most individuals have a substantial fall in<br />
blood pressure when <strong>the</strong>y sleep ac<strong>com</strong>panied by<br />
a decrease in heart rate. It appeared that some<br />
individuals have little or no fall in blood pressure<br />
when <strong>the</strong>y sleep. This has led to classification <strong>of</strong><br />
subjects into dippers and non-dippers [4].<br />
Nocturnal non dipping refers to a 10% or lesser<br />
magnitude reduction in average systolic blood<br />
pressure SBP and/or diastolic blood pressure DBP<br />
at nighttime <strong>com</strong>pared to daytime SBP and/or DBP<br />
average values, <strong>the</strong> remainder defined as dipper<br />
[5].<br />
Reduced nocturnal blood pressure fall is considered<br />
one <strong>of</strong> clinical traits associated with a<br />
greater cardiovascular risk and end organ damage<br />
[6,7].<br />
The present study aimed at investigating <strong>the</strong><br />
association between metabolic syndrome according<br />
to International Diabetes Federation criteria 2006<br />
and non-dipping blood pressure as assessed by 24<br />
h ambulatory blood pressure.<br />
This study included one hundred consecutive<br />
patients referred to our clinic in Mubarak Police<br />
Hospital with recently diagnosed essential hypertension<br />
for evaluation <strong>of</strong> blood pressure with ambulatory<br />
blood pressure monitoring (ABPM).<br />
These patients subdivided into two groups<br />
according to <strong>the</strong> International Diabetes Federation<br />
2006 (IDF 2006) criteria <strong>of</strong> metabolic syndrome.<br />
These groups are:<br />
1- 50 patients had metabolic syndrome.<br />
2- 50 patients did not have metabolic syndrome.<br />
All <strong>the</strong> patients had been evaluated with a<br />
detailed history taking and a physical examination,<br />
History taking provided information about risk<br />
factors such as smoking, past medical history,<br />
99<br />
diabetes mellitus, hypertension, its duration and<br />
medical treatment.<br />
Patients are excluded from <strong>the</strong> study if <strong>the</strong>y<br />
have Secondary hypertension, Congestive heart<br />
failure, previous myocardial infarction, Cardiac<br />
valve disease, chronic renal failure, any conditions<br />
preventing technically adequate ABPM as atrial<br />
fibrillation and o<strong>the</strong>r arrhythmia.<br />
All <strong>the</strong> patients underwent laboratory investigations<br />
for FBS, TG, HDL, and LDL. Waist circumference<br />
had been measured and Twenty-fourhour<br />
ABPM had been carried out for <strong>the</strong> entire<br />
patients and <strong>the</strong>n evaluated according to MS-score.<br />
Dippers constituted (61%) <strong>of</strong> <strong>the</strong> population<br />
studied while non dippers constituted (39%). There<br />
were more non-dippers with <strong>the</strong> metabolic syndrome<br />
(66%) than patients in those without <strong>the</strong><br />
metabolic syndrome (12%) and <strong>the</strong>se results are<br />
in agreement with [11].<br />
Hassan MO et al [11] examined <strong>the</strong> circadian<br />
changes in blood pressure and <strong>the</strong>ir relation to <strong>the</strong><br />
metabolic syndrome and its <strong>com</strong>ponents in 1124<br />
subjects in Omani Arabs. According to <strong>the</strong> International<br />
Diabetes Federation's definition, 264<br />
subjects had <strong>the</strong> metabolic syndrome, a prevalence<br />
<strong>of</strong> 23%. Non-dippers with <strong>the</strong> metabolic syndrome<br />
were 131 <strong>of</strong> 264 (50%), <strong>com</strong>pared with 265 <strong>of</strong> 860<br />
(31%) without <strong>the</strong> metabolic syndrome.<br />
There were no significant differences in age,<br />
sex, smoking, lipids pr<strong>of</strong>ile and FBS between<br />
dippers and non dippers and this goes with <strong>the</strong><br />
results <strong>of</strong> [1].<br />
Tartan et al [1] studied 132 patients with newly<br />
diagnosed essential hypertension in order to investigate<br />
<strong>the</strong> association between MS and non dipping<br />
blood pressure.<br />
There were highly significant differences<br />
(p
Metabolic Syndrome as A Predictor <strong>of</strong> Non Dipping Hypertension<br />
We hypo<strong>the</strong>size that <strong>the</strong> important determinants<br />
<strong>of</strong> a non dipping BP in this study were obesity,<br />
DM and high MS-score in addition to higher 24<br />
hour systolic blood pressure.<br />
In patients with metabolic syndrome <strong>the</strong>re were<br />
no significant differences in age, WC and lipids<br />
pr<strong>of</strong>ile between dippers and non dippers and this<br />
goes with <strong>the</strong> results <strong>of</strong> [11].<br />
In patients with metabolic syndrome <strong>the</strong>re were<br />
highly significant differences in FBS, DM and<br />
MS-score between dippers and non dippers and<br />
this goes with <strong>the</strong> results <strong>of</strong> [1].<br />
In patients with metabolic syndrome <strong>the</strong>re were<br />
significant differences in average day SBP and<br />
average night SBP and DBP and no significant<br />
difference in average day DBP between dippers<br />
and non dippers and it goes with <strong>the</strong> results <strong>of</strong> [11].<br />
In this study non dipping state in patients with<br />
metabolic syndrome is closely related to elevated<br />
FBS, DM and high MS-score in addition to higher<br />
24 hour systolic blood pressure.<br />
In <strong>the</strong> present study High MS-score was defined<br />
as a MS-score >34 which was <strong>the</strong> optimal cut-<strong>of</strong>f<br />
point to differentiate <strong>the</strong> patients having non dipping<br />
feature, based on <strong>the</strong> curve analysis as shown<br />
in chart 3, and thus, this study was able to show<br />
that a high MS-score, but not MS-IDF, predicts<br />
non dipping blood pressure.<br />
High MS-score subjects showed highly significant<br />
differences in WC, FBS, TG, HDL, and MSscore<br />
than those with low MS-score and this goes<br />
with <strong>the</strong> results <strong>of</strong> [1].<br />
A highly significant relationship was present<br />
between increasing MS-score and all systolic blood<br />
pressure particularly with night SBP and this goes<br />
with <strong>the</strong> results <strong>of</strong> [1].<br />
In this study multivariate logistic regression<br />
analysis was used to determine <strong>the</strong> independent<br />
factors related to <strong>the</strong> development <strong>of</strong> non dipping<br />
status and showed that <strong>the</strong> MS-score level was <strong>the</strong><br />
strongest independent predictor <strong>of</strong> non dipping<br />
status with Odds ratio (OR) 12.3, 95% Confidence<br />
Interval (CI) 4.371-29.245, (p
Islam M.M. El-Helaly, et al<br />
blood pressure reproducibility: results <strong>of</strong> <strong>the</strong> HARVEST<br />
trial. Hypertension 1994; 23: 211-216.<br />
5- Takakuwa H, Ise T, Kato T, Izumiya Y, Shimizu K, Yokoyama<br />
H, Kobayashi KI: Diurnal variation <strong>of</strong> hemodynamic<br />
indices in non-dipper hypertensive patients. Hypertens<br />
Res 2001; 24: 195-203.<br />
6- Bianchi S, Bigazzi R, Baldari G, Sgherri G, Campese<br />
VM: Diurnal variation <strong>of</strong> blood pressure and microalbuminuria<br />
in essential hypertension. Am J Hypertens 1994;<br />
7: 23-29.<br />
7- Cuspidi C, Amroioni E, Mancia G, Pessina AC, Trimarco<br />
B, Zanchetti A: Role <strong>of</strong> echocardiography and carotid<br />
ultrasonography in stratifying risk in patient with essential<br />
hypertension: <strong>the</strong> Assessment <strong>of</strong> prognostic Risk Observational<br />
Survey. J Hypertens 2002; 20: 1307-1314.<br />
8- Grundy SM: Metabolic Syndrome Scientific Statement<br />
by <strong>the</strong> American Heart Association and <strong>the</strong> National Heart,<br />
Lung, and Blood Institute Arterioscler. Thromb Vasc Biol<br />
November 2005; 1, 25 (11): 2243-2244.<br />
9- American Heart Association: New approaches to treating<br />
dyslipidemia, raising low high-density lipoprotein (HDL)<br />
2006.<br />
101<br />
10- Macchia A, Levantesi G, Borrelli G, Franzosi MG, Maggioni<br />
AP, Marfisi R, Scarano M, Tavazzi L, Tognoni G,<br />
Valagussa F, Marchioli R: A clinically practicable diagnostic<br />
score for metabolic syndrome improves its predictivity<br />
<strong>of</strong> diabetes mellitus: <strong>the</strong> Gruppo Italiano per lo<br />
Studio della Sopravvivenza nell'Infarto miocardico (GIS-<br />
SI)-Prevenzione scoring. Associazione Nazionale Medici<br />
Cardiologi Ospedalieri; Istituto di Ricerche Farmacologiche<br />
Mario Negri-Consorzio Mario Negri Sud, Santa<br />
Maria Imbaro; Gruppo Italiano per lo Studio della Sopravvivenza<br />
nell'Infarto miocardico (GISSI)-Prevenzione<br />
Investigators. Am Heart J Mar 2006; 151 (3): 754.e7-<br />
754.e17.<br />
11- Hassan MO, Jaju D, Albarwani S, Al-Yahyaee S, Al-<br />
Hadabi S, Lopez-Alvarenga JC, Rizvi SG, Comuzzie AG,<br />
Bayoumi RA: Non-dipping blood pressure in <strong>the</strong> metabolic<br />
syndrome among Arabs <strong>of</strong> <strong>the</strong> Oman family study. Obesity<br />
Silver Spring Oct 2007; 15 (10): 2445-53.<br />
12- Foss CH, Vestbo E, Frøland A, Gjessing HJ, Mogensen<br />
CE, Damsgaard EM: Normal blood pressure and preserved<br />
diurnal variation in <strong>of</strong>fspring <strong>of</strong> type 2 diabetic patients<br />
characterized by features <strong>of</strong> <strong>the</strong> metabolic syndrome: <strong>the</strong><br />
Fredericia Study.Diabetes Care Mar 2000; 23 (3): 283-<br />
9.
Egypt Heart J 62 (1): 103-110, March 2010<br />
Quantitative Power Doppler Technique <strong>of</strong> Myocardial Contrast<br />
Echocardiography: For <strong>the</strong> Detection <strong>of</strong> Segmental Myocardial<br />
Perfusion Pr<strong>of</strong>ile<br />
YOUSSEF FM NOSIR, MD* , **; ASHRAF A ALI, MD* , **; ALI A ABD-ELMAGID, MD**;<br />
MAMDOUH ALTAHAN, MD**; MANSOUR MOSTAFA, MD**;<br />
ABDELMAKSOUD S AHMED, MD**; AYMAN KHOLIEF, MD**;<br />
HASSAN CHAMSI PASHA, MD*; EZZ EL-SSAWY, MD**<br />
Background: Myocardial contrast echocardiography (MCE) is a relatively new method <strong>of</strong> visualizing <strong>the</strong> perfusion territory<br />
<strong>of</strong> a coronary artery using an intravenous (IV) injection <strong>of</strong> microbubbles. Harmonic power Doppler imaging (HPD) with IV<br />
contrast agents can qualitatively identify myocardial perfusion defects in patients with ischaemic heart disease (IHD), however,<br />
<strong>the</strong>re is still a need to study <strong>the</strong> ability <strong>of</strong> HPD imaging to detect perfusion defect areas quantitatively (Q).<br />
Objectives: The aim <strong>of</strong> <strong>the</strong> present study was to detect <strong>the</strong> feasibility <strong>of</strong> myocardial contrast echocardiography (MCE) using<br />
Q-HPD technique for <strong>the</strong> assessment <strong>of</strong> left ventricular (LV) myocardial perfusion pr<strong>of</strong>ile.<br />
Methods: Twenty-one patients with a recent LV myocardial infarction were recruited for this study. Patients underwent both<br />
MCE and coronary arteriography. MCE studies were performed using Phillips 75000 with IV infusion <strong>of</strong> sonicated diluted<br />
Definity. Images were acquired from <strong>the</strong> apical window with stepwise increase triggering intervals (1 to 9 beats) at end-systole.<br />
Images were scored for LV wall motion (WM) [16 segments model, (1=normal, 2=mild hypokinetic, 3=severe hypokinetic,<br />
4=akinetic and 5=dyskinetic)] as well as for subjective visual estimation (VS) <strong>of</strong> LV perfusion pr<strong>of</strong>ile (1=normal, 0.5=partial<br />
and 0.0=no perfusion).<br />
Results: Coronary arteriography showed that 18 out <strong>of</strong> <strong>the</strong> 21 patients had significant coronary artery stenosis (CAD), (5<br />
one vessel, 12 with 2 vessels and 1 with 3 vessels CAD). The mean ± SD <strong>of</strong> Q-HPD (db) with MCE were 32±7.8, 9.3±3.4 and<br />
3.5±1.6 for LV cavity, LV myocardial segments with normal and abnormal perfusion respectively. There was significant difference<br />
between Q-HPD <strong>of</strong> LV cavity and normal segments (p=0.00001), and between segments <strong>of</strong> normal and abnormal perfusion<br />
(p=0.0001). Significant difference was also found when Q-HPD measurements obtained from segments with abnormal perfusion<br />
score were <strong>com</strong>pared to measurements obtained from normal segments (p=0.003 and p=0.00001 for segments with VS score<br />
<strong>of</strong> 0.5 and 0.0 respectively). When segments were <strong>com</strong>pared according to WM score, <strong>the</strong> mean ± SD <strong>of</strong> Q-HPD (db) were<br />
8.1±3.5 and 3.5±2.1 (p=0.00001) for normal and abnormal segments respectively. Significant difference was also found when<br />
Q-HPD measurements obtained from abnormal segments were <strong>com</strong>pared with values obtained from normal segments (p=0.0002,<br />
p=0.0001 and p=0.004, for segments with WM score 2, 3 and 4, respectively. Q-HPD <strong>of</strong> MCE has very good sensitivity 100%<br />
(100-100), specificity 67% (47-87) and overall accuracy <strong>of</strong> 95% (86-104) for detecting CAD. WM score has good sensitivity<br />
88% (74-102), specificity 75% (56-94) and overall accuracy <strong>of</strong> 86% (71-101) for detecting CAD.<br />
Conclusion: Quantitative analysis <strong>of</strong> myocardial perfusion images obtained with HPD technique is feasible and could be<br />
performed in all patients recruited in this study with very good sensitivity, specificity and overall accuracy for detecting CAD.<br />
Therefore, Q-HPD analysis is re<strong>com</strong>mended for objective differentiation between normal and abnormal perfusion pr<strong>of</strong>ile <strong>of</strong><br />
LV myocardium.<br />
Key Words: Myocardial perfusion imaging – Harmonic power Doppler echocardiography – Myocardial infarction.<br />
From Cardiac Service, Kng Fahd Armed Force Hospital,<br />
Jeddah, KSA* and The Cardiology Department, Al-Hussein<br />
University Hospital, Al-Azhar University, Cairo, Egypt**.<br />
Manuscript received 2 Jan., 2010; revised 10 Feb., 2010;<br />
accepted 12 Feb., 2010.<br />
Address for Correspondence: Dr. Youssef FM Nosir,<br />
From Cardiac Service, Kng Fahd Armed Force Hospital,<br />
Jeddah, KSA* and The Cardiology Department, Al-Hussein<br />
University Hospital, Al-Azhar University, Cairo, Egypt**.<br />
103<br />
Appreviation list:<br />
MCE = Myocardial Contrast echocardiography.<br />
IV = Intravenous.<br />
HPD = Harmonic Power Doppler.<br />
ECG = Electrocardiogram.<br />
SD = Standard Deviation.<br />
WM = Wall Motion.<br />
SPECT = Single Photon Emission Computed Tomography.
Quantitative Power Doppler Technique <strong>of</strong> Myocardial Contrast Echocardiography<br />
Introduction<br />
There is a growing interest in recent years in<br />
preserving acutely ischaemic myocardium which<br />
led to <strong>the</strong> development <strong>of</strong> thrombolitic and interventional<br />
techniques for restoring coronary perfusion<br />
to <strong>the</strong> jeopardized myocardium [1-3]. Coronary<br />
arteriography was used to evaluate <strong>the</strong> success <strong>of</strong><br />
<strong>the</strong>se techniques, however it does not provide an<br />
assessment <strong>of</strong> myocardial perfusion [4-6]. Thallium<br />
scintigraphy has been widely used as a method to<br />
study <strong>the</strong> myocardial perfusion [7-8], however, <strong>the</strong><br />
technique is ra<strong>the</strong>r expensive and necessitates <strong>the</strong><br />
exposure <strong>of</strong> <strong>the</strong> patient to ionized radiation.<br />
Myocardial contrast echocardiography (MCE)<br />
is a relatively new method <strong>of</strong> visualizing <strong>the</strong> perfusion<br />
territory <strong>of</strong> a coronary artery through an<br />
intravenous (IV) injection <strong>of</strong> microbubbles [9-14].<br />
Intermittent second harmonic and pulse inversion<br />
imaging can identify myocardial perfusion defect<br />
in gray scale [12-14]. Microbubbles are known to<br />
produce characteristic signals when exposed to<br />
high amplitude <strong>of</strong> ultrasound. Harmonic power<br />
Doppler (HPD) imaging had <strong>the</strong> potential to record<br />
<strong>the</strong> broad band signal during dissolution <strong>of</strong> <strong>the</strong><br />
microbubbles in <strong>the</strong> myocardial microcirculation.<br />
Preliminary results demonstrated that HPD imaging<br />
with transvenous contrast agents can qualitatively<br />
identify myocardial perfusion defects in patients<br />
with ischaemic heart disease [9-14]. However, <strong>the</strong>re<br />
is still a need to detect segmental perfusion defects<br />
quantitatively using MCE with HPD imaging.<br />
Therefore <strong>the</strong> aim <strong>of</strong> <strong>the</strong> present study was to<br />
detect <strong>the</strong> feasibility <strong>of</strong> <strong>the</strong> quantitative (Q) HPD<br />
technique with MCE for detecting myocardial<br />
perfusion pr<strong>of</strong>ile. Quantitative data were <strong>the</strong>n<br />
<strong>com</strong>pared with <strong>the</strong> results obtained from both<br />
segmental visual estimation <strong>of</strong> MCE and segmental<br />
wall motion score.<br />
Subjects<br />
Twenty one patients with a recent myocardial<br />
infarction, referred to <strong>the</strong> echocardiographic laboratory<br />
(King Fahd Hospital from September 2007<br />
till January 2009) for <strong>the</strong> assessment <strong>of</strong> left ventricular<br />
function. Patients were pre-selected for<br />
optimal apical echocardiographic image quality.<br />
Myocardial infarction was defined on <strong>the</strong> basis <strong>of</strong><br />
a classic history, ST elevation >2mm in two contiguous<br />
ECG leads and increase <strong>of</strong> creatinine phosphokinase<br />
<strong>of</strong> >2 SD units. Patients were 16 males<br />
and 5 females with a mean age <strong>of</strong> 57±12 years. All<br />
104<br />
patients were in sinus rhythm with a mean heart<br />
rate <strong>of</strong> 76±13b/m. Subjects included 12 patients<br />
with anterior wall and 9 patients with inferior wall<br />
myocardial infarction. Verbal consent was obtained<br />
from each patient after full explanation <strong>of</strong> <strong>the</strong><br />
procedure.<br />
Methods:<br />
Each patient underwent coronary arteriography<br />
and two-dimensional echocardiographic examination<br />
using Phillips 7500 with harmonic mode for<br />
<strong>the</strong> assessment <strong>of</strong> left ventricular function. Images<br />
were obtained from <strong>the</strong> apical window with <strong>the</strong><br />
patient in 45º left recumbent position. Apical 4chamber,<br />
2-chamber and long axis views were<br />
recorded for <strong>the</strong> assessment <strong>of</strong> left ventricular wall<br />
motion using <strong>the</strong> 16-segments model (Fig. 1). Each<br />
segment was scored using <strong>the</strong> 5 score index model<br />
(1=normal wall motion, 2=mild hypokinesia,<br />
3=severe hypokinesia, 4=akinesia & 5=dyskinesia).<br />
Myocardial contrast echocardiography:<br />
Myocardial contrast echocardiography was<br />
performed with Phillips 7500 during continuous<br />
IV infusion <strong>of</strong> Sonicated diluted Definity (Schering<br />
AG, Duitsland) using <strong>the</strong> HPD mode.<br />
Echocardiographic settings for contrast: The<br />
gain setting <strong>of</strong> <strong>the</strong> echo machine should be adjusted<br />
for grey scale myocardial visualization prior to IV<br />
infusion <strong>of</strong> <strong>the</strong> contrast. The focus should be at <strong>the</strong><br />
level or just above <strong>the</strong> mitral annulus. Second<br />
harmonic mode and power Doppler mode for image<br />
acquisition were selected. Triggering mode is<br />
adjusted at end-systole (peak <strong>of</strong> T wave). To avoid<br />
colour artifact <strong>the</strong> gain setting is adjusted for HPD,<br />
so that no colour artifact appears in <strong>the</strong> myocardium<br />
at baseline before <strong>the</strong> contrast injection.<br />
Image acquisition: Images were acquired from<br />
<strong>the</strong> apical window using harmonic mode for both<br />
grey scale and power Doppler with stepwise increase<br />
triggering intervals from 1 to 9 beats at endsystole.<br />
Apical 4-chamber, 2-chamber and apical<br />
long axis views were obtained, recorded and stored<br />
digitally for fur<strong>the</strong>r <strong>of</strong>f line qualitative and quantitative<br />
analysis with <strong>the</strong> Phillips <strong>of</strong>f-line quantitative<br />
workstation (Q-laboratory).<br />
Image analysis: HPD images were subjected<br />
into qualitative and quantitative analysis using <strong>the</strong><br />
16 segments model.<br />
Visual analysis: The recorded HPD images<br />
were analyzed using <strong>the</strong> 3 score index (0=no per-
Youssef FM Nosir, et al<br />
fusion, 0.5=delayed/partial perfusion & 1=<strong>com</strong>plete<br />
normal perfusion).<br />
Quantitative analysis: Quantitative analysis <strong>of</strong><br />
<strong>the</strong> HPD images was performed <strong>of</strong>f-line. For each<br />
apical view and for each segment <strong>of</strong> <strong>the</strong> 16-segment<br />
model, an area <strong>of</strong> interest (5mm X 5mm) was<br />
selected within <strong>the</strong> myocardium for quantitative<br />
analysis. In addition, quantitative HPD analysis<br />
was also obtained from <strong>the</strong> left ventricular cavity<br />
<strong>of</strong> <strong>the</strong> three apical views and <strong>the</strong>n averaged (Fig.<br />
2). Quantitative data were obtained from 5 successive<br />
frames without echo dropouts, at peak triggering<br />
intervals and data averaged.<br />
Coronary arteriography:<br />
Coronary arteriography for <strong>the</strong> identification<br />
<strong>of</strong> <strong>the</strong> infarct-related coronary artery was performed,<br />
for each patient after myocardial contrast<br />
echocardiographic study, on <strong>the</strong> same day in 15<br />
patients and within 48 hours in 6 patients. Clinical<br />
condition and medications remained stable between<br />
<strong>the</strong> two tests. The infarct related coronary artery<br />
was identified as <strong>the</strong> one with reduced TIMI flow<br />
and/or <strong>the</strong> artery with <strong>the</strong> more severe stenosis, if<br />
<strong>the</strong> patient had more than one artery affected.<br />
Mid post<br />
sept<br />
(10)<br />
Basal post<br />
sept<br />
(5)<br />
Apical<br />
sept<br />
(11)<br />
4-chamber<br />
Apical<br />
lat<br />
(13)<br />
Mid<br />
lat<br />
(8)<br />
Basal<br />
lat<br />
(3)<br />
Apical<br />
inf<br />
(14)<br />
Mid inf<br />
(9)<br />
Basal inf<br />
(4)<br />
105<br />
Statistical analysis:<br />
For each patient, analysis <strong>of</strong> wall motion score,<br />
visual estimation <strong>of</strong> myocardial contrast echocardiographic<br />
data and quantitative analysis was performed<br />
blindly to all o<strong>the</strong>r technique results with<br />
one week interval and without knowing <strong>the</strong> coronary<br />
arteriographic results. Quantitative data were<br />
presented as <strong>the</strong> mean ± standard deviation <strong>of</strong> each<br />
segment in 5 successive frames without echo dropout.<br />
Results obtained from <strong>the</strong> quantitative analysis<br />
<strong>of</strong> HPD were <strong>the</strong>n classified and <strong>com</strong>pared according<br />
to both <strong>the</strong> wall motion score index and according<br />
to visual scoring <strong>of</strong> <strong>the</strong> myocardial perfusion<br />
images. Paired student T-test was performed to<br />
<strong>com</strong>pare quantitative data obtained from <strong>the</strong> left<br />
ventricular cavity to <strong>the</strong> normal perfused segments<br />
and normal to total number <strong>of</strong> abnormal perfused<br />
segments. In addition, T-test was used to <strong>com</strong>pare<br />
normal segments to abnormal segments when classified<br />
according to both abnormal wall motion<br />
score and abnormal visual estimation score. Significance<br />
was stated at
Quantitative Power Doppler Technique <strong>of</strong> Myocardial Contrast Echocardiography<br />
Results<br />
Myocardial contrast echocardiographic study<br />
was performed successfully in all patients recruited<br />
in this study. There were no adverse events.<br />
Coronary arteriography:<br />
Coronary arteriographic data revealed that 18<br />
out <strong>of</strong> <strong>the</strong> 21 patients had significant coronary<br />
(A) (B)<br />
Figure 2: Myocardial perfusion image <strong>of</strong> apical 2-chamber view obtained from a patient having anterior wall myocardial<br />
infarction. Displays are in gray scale (panel A) and power Doppler (panel B). There is a perfusion defect involving<br />
<strong>the</strong> anterior wall and part <strong>of</strong> <strong>the</strong> apex while <strong>the</strong> inferior wall shows normal perfusion. This figure demonstrated that<br />
power Doppler image could reflect <strong>the</strong> myocardial segments with normal and abnormal perfusion.<br />
(A) (B)<br />
Figure 3: Myocardial perfusion image <strong>of</strong> a patient with anterior wall myocardial infarction, using harmonic power Doppler<br />
mode is demonstrated. Panel A shows <strong>the</strong> apical 2-chamber view with perfusion defect involving <strong>the</strong> posterior septum<br />
and septal part <strong>of</strong> <strong>the</strong> apex. while lateral wall shows normal perfusion pr<strong>of</strong>ile. The number in <strong>the</strong> rectangles represents<br />
<strong>the</strong> MCE power reflected from each selected area <strong>of</strong> interest in db. Panel B shows <strong>the</strong> coronary arteiography (left<br />
system) <strong>of</strong> this patient revealing significant proximal left anterior descending (LAD) and distal circumflex (CX)<br />
coronary artery stenosis.<br />
106<br />
artery stenosis. Five patients had one vessel, 12<br />
patients had two vessels and 1 patient had 3 vessels<br />
coronary artery disease.<br />
Wall motion score:<br />
Wall motion analysis with <strong>the</strong> 16 segments<br />
score index <strong>of</strong> <strong>the</strong> echocardiographic examination,<br />
revealed <strong>the</strong> presence <strong>of</strong> abnormal wall motion in<br />
16 out <strong>of</strong> <strong>the</strong> 21 patients. Among <strong>the</strong>se 16 patients,
Youssef FM Nosir, et al<br />
15 had significant coronary artery disease by coronary<br />
arteriography. Out <strong>of</strong> <strong>the</strong> 5 patients with no<br />
wall motion abnormality 3 had significant coronary<br />
artery disease by coronary arteriography.<br />
Myocardial perfusion imaging:<br />
Analysis <strong>of</strong> <strong>the</strong> myocardial perfusion echocardiographic<br />
images with HPD after intravenous<br />
injection <strong>of</strong> contrast agent revealed that 19 out <strong>of</strong><br />
<strong>the</strong> 21 patients had segmental myocardial perfusion<br />
defects. Eighteen out <strong>of</strong> <strong>the</strong>se 19 patients had<br />
significant coronary artery disease by coronary<br />
arteriography. The angiographic data from <strong>the</strong> two<br />
patients with normal myocardial perfusion pr<strong>of</strong>ile<br />
revealed no significant coronary artery lesion.<br />
The mean ± SD <strong>of</strong> Q-HPD (db) with MCE were<br />
32±7.8, 9.3±3.4 and 3.5±1.6 for left ventricular<br />
cavity, left ventricular myocardial segments with<br />
normal and abnormal perfusion respectively. There<br />
107<br />
was significant difference between Q-HPD <strong>of</strong> left<br />
ventricular cavity and segments with normal perfusion<br />
(p=0.00001), and between segments <strong>of</strong><br />
normal and abnormal perfusion (p=0.0001).<br />
Quantitative HPD data <strong>of</strong> myocardial perfusion<br />
echocardiography were classified and studied according<br />
to both segmental wall motion score and<br />
visual estimation <strong>of</strong> segmental myocardial perfusion<br />
pr<strong>of</strong>ile (Table 1).<br />
Comparison between echocardiographic and coronary<br />
arteriographic data:<br />
Data obtained from wall motion score and<br />
myocardial perfusion analysis were <strong>com</strong>pared with<br />
coronary arteriographic data. Sensitivity, specificity<br />
and accuracy <strong>of</strong> both wall motion and myocardial<br />
perfusion analysis to detect coronary artery disease<br />
were calculated and presented in Table (2).<br />
Table 1: Comparison between QHPD measurements <strong>of</strong> normal segments and measurements obtained<br />
from abnormal segments when LV myocardial segments classified according both WMS<br />
index and visual estimation <strong>of</strong> perfusion pr<strong>of</strong>ile.<br />
Mean ± SD<br />
p<br />
1<br />
8.1±3.5<br />
HPD according to WM<br />
QHPD = Quantitative harmonic power Doppler.<br />
LV = Left ventricle.<br />
2<br />
3.9±2.2<br />
0.0002<br />
3<br />
3.4±1.1<br />
0.0001<br />
4<br />
2.9±2.1<br />
0.004<br />
5<br />
–<br />
–<br />
9.3±3.4<br />
WMS = Wall motion score.<br />
VS = Visual estimation.<br />
1<br />
HPD according to VS<br />
0.5<br />
4.3±2.1<br />
0.003<br />
0.0<br />
2.3±1.1<br />
0.00001<br />
SD = Standard deviation.<br />
p = p value.<br />
Table 2: Comparison between QHPD and WMS in predicting CAD as <strong>com</strong>pared to coronary<br />
arteriography.<br />
QHPD<br />
WMS<br />
Sensitivity<br />
100 (100-100)<br />
88 (74-102)<br />
Specificity<br />
67 (47-87)<br />
75 (56-94)<br />
Negative PA<br />
100 (100-100)<br />
60 (39-81)<br />
Positive PA<br />
95 (85-104)<br />
94 (83-104)<br />
CAD = Coronary artery disease. PA = Predictive accuracy, all o<strong>the</strong>r abbreviations as in table.<br />
Discussion<br />
In patients with acute myocardial infarction<br />
who have undergone attempted reperfusion, <strong>the</strong><br />
cardiologist needs to know whe<strong>the</strong>r <strong>the</strong> myocardium<br />
has been successfully reperfused, how much <strong>of</strong> <strong>the</strong><br />
myocardium has been salvaged and how much can<br />
still potentially be salvaged. The current methods<br />
<strong>of</strong> evaluating infarct size are indirect and do not<br />
provide a <strong>com</strong>plete assessment <strong>of</strong> both <strong>the</strong> infarct<br />
size and area at risk [15]. Cardiac enzymes [16] and<br />
electrocardiogram [17,18] are useful clinical tools<br />
in <strong>the</strong> diagnosis <strong>of</strong> acute ischaemic syndromes.<br />
Electrocardiogram is less valuable in determining<br />
Overall Accuracy<br />
95 (86-104<br />
86 (71-101)<br />
<strong>the</strong> success <strong>of</strong> reperfusion or <strong>the</strong> extent <strong>of</strong> myocardial<br />
salvage. Cardiac enzymes do provide an accurate<br />
estimate <strong>of</strong> infarct size, however <strong>the</strong>y do so<br />
without reference to <strong>the</strong> risk area that can expand<br />
and result in left ventricular dilation and heart<br />
failure [16].<br />
Wall motion abnormality is a valuable tool for<br />
<strong>the</strong> diagnosis <strong>of</strong> prior infarction and resting or<br />
inducible ischemia. However, in patients with acute<br />
myocardial infarction who have recently undergone<br />
reperfusion <strong>the</strong>rapy wall motion abnormality is<br />
likely to be present with or without successful<br />
reperfusion. Regional function will be normal if
Quantitative Power Doppler Technique <strong>of</strong> Myocardial Contrast Echocardiography<br />
<strong>the</strong> period <strong>of</strong> ischaemia was very brief, which is<br />
un<strong>com</strong>mon in <strong>the</strong> clinical practice [19].<br />
Coronary arteriography can be used to indicate<br />
restoring <strong>the</strong> patency <strong>of</strong> <strong>the</strong> coronary arteries [4].<br />
However recent studies demonstrated that coronary<br />
arteriography has very limited value in determining<br />
<strong>the</strong> success <strong>of</strong> myocardial reperfusion as one sixth<br />
to one fourth <strong>of</strong> all patients with Timi grade 3 flow<br />
have poor tissue perfusion due to loss <strong>of</strong> microvascular<br />
integrity. This has recently been defined as<br />
no-reflow phenomenon [20]. Therefore, in order to<br />
study myocardial perfusion and/or reperfusion one<br />
has to assess myocardial capillary blood flow [5,21].<br />
Of <strong>the</strong> currently available and developing techniques<br />
capable <strong>of</strong> assessing capillary blood flow<br />
are single-photon emission <strong>com</strong>puted tomography<br />
(SPECT) and MCE [22-23].<br />
SPECT technique has been used for detection<br />
<strong>of</strong> CAD and risk stratification [7,8]. It has also<br />
provided valuable data <strong>of</strong> coronary physiology and<br />
pathophsiology. However <strong>the</strong> technique is limited<br />
because <strong>of</strong> <strong>the</strong> need to inject radioisotopes, exposure<br />
to radiation, time consuming and expense [12].<br />
MCE proved to be <strong>the</strong> most promising technique<br />
since it uses microbubbles, which are pure intravascular<br />
tracers [9-14,22,23].<br />
The results <strong>of</strong> this study demonstrated that HPD<br />
<strong>of</strong> MCE is a feasible technique for detection <strong>of</strong><br />
segmental myocardial perfusion pr<strong>of</strong>ile. Segment<br />
to segment concordance between MCE scoring<br />
and WMA scoring was excellent and both showed<br />
concordance with <strong>the</strong> infarct related artery. However,<br />
HPD <strong>of</strong> MCE showed higher sensitivity,<br />
specificity and predictive accuracy for detection<br />
<strong>of</strong> coronary artery disease, than that obtained from<br />
WMA score when <strong>com</strong>pared with coronary arteriography.<br />
One out <strong>of</strong> <strong>the</strong> 19 patients with myocardial<br />
perfusion defects had normal coronary arteriogram,<br />
this could be explained by <strong>the</strong> no-reflow phenomena<br />
with <strong>the</strong> possible loss <strong>of</strong> microvascular integrity.<br />
Segmental quantitative analysis <strong>of</strong> HPD images<br />
with MCE is feasible. Significant difference was<br />
found between quantitative HPD <strong>of</strong> left ventricular<br />
cavity and segments with normal perfusion<br />
(p=0.00001), and between segments with normal<br />
and abnormal perfusion (p=0.0001). Significant<br />
difference was also found when HPD measurements<br />
obtained from segments with partial and segments<br />
with no perfusion were <strong>com</strong>pared to measurements<br />
obtained from segments with normal perfusion<br />
108<br />
(Table 1). In addition, significant difference was<br />
found when HPD measurements obtained from<br />
segments with abnormal wall motion were <strong>com</strong>pared<br />
with values obtained from segments with<br />
normal wall motion (p=0.0002, p=0.0001 and<br />
p=0.004, for segments with WM score 2, 3 and 4,<br />
respectively.<br />
Our results demonstrated that <strong>the</strong> assessment<br />
<strong>of</strong> myocardial perfusion pr<strong>of</strong>ile <strong>of</strong> HPD images<br />
with MCE could be performed quantitatively. Quantitative<br />
HPD data reflected from <strong>the</strong> left ventricular<br />
cavity was around (= ~ 30db), normal perfused myocardial<br />
segment (= ~ 9db), myocardial segments<br />
with partial perfusion (= ~ 4db) and myocardial<br />
segment with no perfusion (≤2.3db).<br />
Study limitations, clinical implications and future<br />
directions:<br />
Echocardiographic examination with intravenous<br />
infusion <strong>of</strong> contrast agents can be used with<br />
harmonic mode for left ventricular opacification<br />
and HPD mode for <strong>the</strong> assessment <strong>of</strong> myocardial<br />
perfusion.<br />
Left ventricular opacification is used for endocardial<br />
border delineation for calculation <strong>of</strong> left<br />
ventricular volume and mass, as well as for <strong>the</strong><br />
assessment <strong>of</strong> wall motion abnormality at rest and<br />
during stress echocardiography.<br />
Myocardial perfusion imaging with contrast<br />
echocardiography can be used in-patients with<br />
myocardial infarction to determine <strong>the</strong> infarct size<br />
and area at risk. In-patients who underwent coronary<br />
revascularization, myocardial contrast echocardiography<br />
can be used to assess reperfusion efficacy<br />
and to diagnose <strong>the</strong> no-reflow phenomena.<br />
Myocardial contrast echocardiography can be<br />
used in conjunction with stress echocardiography<br />
to study myocardial viability at low dose dobutamine,<br />
myocardial ischaemia at peak stress and/or<br />
with IV administration <strong>of</strong> vasodilators to determine<br />
<strong>the</strong> coronary flow reserve. In addition, myocardial<br />
contrast echocardiography can assess <strong>the</strong> collateral<br />
flow.<br />
The present study was designed to study <strong>the</strong><br />
feasibility <strong>of</strong> quantitative HPD <strong>of</strong> myocardial contrast<br />
echocardiography for detection <strong>of</strong> myocardial<br />
perfusion pr<strong>of</strong>ile as <strong>com</strong>pared to both visual estimation<br />
<strong>of</strong> MCE and wall motion score index. It<br />
shoes its superiority over wall motion score using<br />
coronary arteriographic data as <strong>the</strong> anatomical
Youssef FM Nosir, et al<br />
reference. However <strong>the</strong>re is still a need to <strong>com</strong>pare<br />
quantitative HPD echocardiographic data to data<br />
obtained from o<strong>the</strong>r imaging technique like SPECT.<br />
Patients were pre-selected for good apical image<br />
quality, <strong>the</strong>re is still a need to study MCE independent<br />
from image quality or by using transeosophageal<br />
echocardiographic technique.<br />
Moreover, myocardial contrast echocardiography<br />
with HPD technique is at its infancy and<br />
<strong>the</strong>re is still a need to reach an optimal clinical<br />
protocol. There is still a need to optimize <strong>the</strong> dose<br />
required for each available contrast agent in order<br />
to visualize <strong>the</strong> myocardial perfusion. Recent advances<br />
in ultrasound technology such as flash<br />
imaging allows continuous myocardial perfusion<br />
imaging. The optimal technique for detection <strong>of</strong><br />
segmental perfusion defect is not well established<br />
yet. Disagreement concerning <strong>the</strong> mode <strong>of</strong> administration<br />
<strong>of</strong> <strong>the</strong> contrast agents at different scenarios<br />
is still present. Is it better to use continuous intravenous<br />
infusion or bolus injection, particularly<br />
during stress echocardiography.<br />
In addition, controversy still exists whe<strong>the</strong>r<br />
image analysis using harmonic grey scale or HPD<br />
should be used. Data presented in this study shows<br />
that if HPD imaging is used, analysis should be<br />
performed quantitatively.<br />
Conclusion<br />
Quantitative analysis <strong>of</strong> myocardial perfusion<br />
images obtained by HPD technique could be performed<br />
in all patients with myocardial infarction<br />
recruited in this study. Therefore, quantitative HPD<br />
analysis is re<strong>com</strong>mended for objective differentiation<br />
between normal and abnormal perfusion<br />
pr<strong>of</strong>ile <strong>of</strong> LV myocardium.<br />
References<br />
1- Braunwald E: The aggressive treatment <strong>of</strong> acute myocardial<br />
infarction. Circulation 1985; 71: 1087-1092.<br />
2- Przyklenk K, Vivalidi MT, Scoen FJ, Arnold JMO, Kloner<br />
RA: Salvage <strong>of</strong> ischemic myocardium by reperfusion:<br />
Importance <strong>of</strong> collateral blood flow and myocardial oxygen<br />
demand during occlusion. Cardiovas Res 1986; 20: 403-<br />
414.<br />
3- Patel B, Kloner RA: Analysis <strong>of</strong> reported randomized<br />
trials for streptokinase <strong>the</strong>rapy for acute myocardial<br />
infarction in <strong>the</strong> 1980s. Am J Cardiol 1987; 59: 501-504.<br />
4- Cheseboro JH, Knatterud G, Rob R, et al: Thrombolysis<br />
in Myocardial Infarction (TIMI) trial, phase I: Comparison<br />
between intravenous plasminogen activator and intravenous<br />
streptokinase: Clinical findings through hospital<br />
discharge. Circulation 1987: 76: 142-154.<br />
109<br />
5- Ito H, Okamura A, Lwakura K, et al: Myocardial perfusion<br />
patterns related to thrombolysis in myocardial infarction<br />
grades after coronary angioplasty in patients with acute<br />
anterior wall myocardial infarction. Circulation 1996; 93:<br />
1993-99.<br />
6- Porter TR, Li S, Kilzer K, Deligonul U: Effect <strong>of</strong> significant<br />
two-vessel versus one-vessel coronary artery stenosis<br />
on myocardial contrast defects observed with intermittent<br />
harmonic imaging after intravenous contrast injection<br />
during dobutamine stress echocardiography. J Am Coll<br />
Cardiol 1997; 30: 1399-406.<br />
7- Wackers FJ, Russo DJ, Russo D, Clements JP: Prognostic<br />
significance <strong>of</strong> normal quantitative planar Thallium-201<br />
stress scintigraphy in patients with chest pain. J Am Coll<br />
Cardiol 1985; 6: 27-30.<br />
8- Brown KA: Prognostic value <strong>of</strong> thallium-201 myocardial<br />
perfusion in imaging: A diagnostic tool <strong>com</strong>es <strong>of</strong> age.<br />
Circulation 1991; 83: 363-381.<br />
9- Moore CA, Smucker ML, Kaul S: Myocardial contrast<br />
echocardiography in humans: Safety: A <strong>com</strong>parison with<br />
routine coronary arteriography. J Am Coll Cardiol 1986;<br />
8: 1066-1072.<br />
10- Lang RM, Borow KM, Neumann A, Al-Sadir J, Feinstein<br />
SB: Effects <strong>of</strong> intracoronary injection <strong>of</strong> sonicated microbubbles<br />
on left ventricular contractility. Am J Cardiol<br />
1987; 60: 166-171.<br />
11- Reisner SA, Ong LS, Lichtenberg GS, et al: Myocardial<br />
perfusion imaging by contrast echocardiography with use<br />
<strong>of</strong> intracoronary sonicated albumin in humans. J Am Coll<br />
Cardiol 1989; 14: 660-665.<br />
12- Kaul S, Senior R, Dittrich H, Raval U, Khattar R, Lahiri<br />
A: Detection <strong>of</strong> Coronary Artery Disease With Myocardial<br />
Contrast Echocardiography Comparison With 99m TC<br />
Sestamibi Single-Photon Emission Computed Tomography.<br />
Circulation 1997; 96: 785-792.<br />
13- Porter TR, Xie F, Kricsfield A, Kilzer K: Noninvasive<br />
identification <strong>of</strong> acute myocardial infarction and reperfusion<br />
with contrast ultrasound using intravenous perfluoropropane<br />
exposed sonicated dextrose albumin. J Am<br />
Coll Cardiol 1995; 26: 33-40.<br />
14- Rocchi G, Kasprzak JD, Galema TW, de Jong N, Ten Cate<br />
FJ: Usefulness <strong>of</strong> power Doppler contrast echocardiography<br />
to identify reperfusion after acute myocardial<br />
infarction. Am J Cardiol 2001; 87 (3): 278.<br />
15- Kaul S, MD: Assessing <strong>the</strong> myocardium after attempted<br />
reperfusion: Should we bo<strong>the</strong>r. Circulation 1998; 98: 625-<br />
627.<br />
16- Tanasijevic MJ, Cannon CP, Wybenga DR, et al: Myoglobin,<br />
creatine kinase MB, and cardiac troponin-I to assess<br />
reperfusion after thrombolysis for acute myocardial infarction:<br />
Results from TIMI 10A. Am Heart J 1997; 134:<br />
622-630.<br />
17- Califf RM, O'Neil W, Stack RS, et al: Failure <strong>of</strong> simple<br />
clinical measurements to predict perfusion status after<br />
intravenous thrombolysis. Ann Intern Med 1988; 108:<br />
658-662.
Quantitative Power Doppler Technique <strong>of</strong> Myocardial Contrast Echocardiography<br />
18- Kruc<strong>of</strong>f MW, Croll MA, Pope JE, et al: Continuous 12lead<br />
ST-segment recovery analysis in <strong>the</strong> TAMI 7 Study:<br />
Performance <strong>of</strong> a noninvasive method for real-time detection<br />
<strong>of</strong> failed myocardial perfusion. Circulation 1993;<br />
88: 437-446.<br />
19- Kaul S: Echocardiography in coronary artery diease. Curr<br />
Probl Cardiol 1990; 15: 233-298.<br />
20- Krug A, Du Mesnil de Rochemont W, Korb G: Blood<br />
supply to <strong>the</strong> myocardium after temporary coronary<br />
occlusion. Circ Res 1966; 19: 57-62.<br />
21- Regosta M, Camarano GP, Kaul S, Powers E, Sarembock<br />
IJ, Gimple LW: Microvascular integrity indicates myo-<br />
110<br />
cellular viability in patients with recent myocardial infarction:<br />
New insights using myocardial contrast echocardiography.<br />
Circulation 1994; 89: 2562-2569.<br />
22- Sanjiv Kaul: Myocardial Contrast Echocardiography: A<br />
25 Year Retrospective. Circulation 2008; 118: 291-308.<br />
23- Miszalski-Jmka T, Kuntz Hehner S, Schmidt H, Hamerstingl<br />
C, Tiemann K, Ghanem A, Troatz C, Luderitz B,<br />
Omran H: Real time myocardial contrast echocardiography<br />
during supine bicycle stress and continuous infusion <strong>of</strong><br />
contrast agent: Cut<strong>of</strong>f values for myocardial contrast<br />
replenishment discriminating abnormal myocardial perfusion.<br />
Echocardiography 2007; 24: 638-648.
Egypt Heart J 62 (1): 111-116, March 2010<br />
The Carotid-Femoral Arterial Index and <strong>the</strong> Severity <strong>of</strong><br />
Coronary A<strong>the</strong>rosclerosis<br />
MAHMOUD SOLIMAN, MD*; HESHAM HASAN, MD*; TAMER GAZY, MSc*;<br />
WALAA FAREED, MD*; ASHRAF REDA, MD*; SAID SHALABY, MD*<br />
Although extensively investigated, <strong>the</strong> value <strong>of</strong> carotid intima media thickness as surrogate marker <strong>of</strong> coronary a<strong>the</strong>rosclerosis<br />
is still a matter <strong>of</strong> debate. Examination <strong>of</strong> o<strong>the</strong>r vascular beds and hence more a<strong>the</strong>rosclerotic burden may have more impact<br />
than examination <strong>of</strong> carotids alone.<br />
Aim: Detection <strong>of</strong> coronary a<strong>the</strong>rosclerosis and assessment <strong>of</strong> its severity non-invasively by examination <strong>of</strong> <strong>the</strong> <strong>com</strong>mon<br />
carotid and superficial femoral arteries.<br />
Subjects and Methods: This study included 120 patients; (30 with normal coronary arteries, group 1, 30 patients with single<br />
vessel disease group 2, 30 with two vessel disease group 3, 30 with three vessel disease group 4). The severity <strong>of</strong> coronary<br />
a<strong>the</strong>rosclerosis calculated according to Gensini score.<br />
All patients underwent a vascular duplex scan <strong>of</strong> <strong>the</strong> right and left carotid arteries and <strong>the</strong> right and left femoral superficial<br />
arteries by means <strong>of</strong> transcutaneous high axial resolution B-mode ultrasound imaging, <strong>the</strong> Carotid femoral index (CARFEM)<br />
in mm was determined as follows: (Intima media thickness <strong>of</strong> right <strong>com</strong>mon carotid + IMT left <strong>com</strong>mon carotid + Total width<br />
<strong>of</strong> right femoral + Total Width left femoral)/4.<br />
Results: The CARFEM index was: 0.54±0.06 in group 1, 0.87±0.04 in group 2, 1.22±0.08 in group 3 and 1.54±0.1 in group<br />
4 and <strong>the</strong> difference was highly significant, p value
The Carotid-Femoral Arterial Index & <strong>the</strong> Severity <strong>of</strong> Coronary A<strong>the</strong>rosclerosis<br />
Whe<strong>the</strong>r examination <strong>of</strong> more vascular beds<br />
(like femoral arteries) and hence more a<strong>the</strong>rosclerotic<br />
burden could affect this correlation is still<br />
unclear.<br />
Aim <strong>of</strong> <strong>the</strong> work: Detection <strong>of</strong> coronary a<strong>the</strong>rosclerosis<br />
and assessment <strong>of</strong> its severity noninvasively<br />
by examination <strong>of</strong> <strong>the</strong> <strong>com</strong>mon carotid<br />
and superficial femoral arteries.<br />
Subjects and Methods<br />
The present study included 120 patients; 90<br />
with coronary a<strong>the</strong>rosclerosis; (30 with single<br />
vessel disease, 30 with two vessel disease, 30 with<br />
three vessel disease), 30 with normal coronary<br />
angiography; (10 preoperative assessment, 12 with<br />
typical chest pain and highly suggestion <strong>of</strong> angina<br />
pectoris, <strong>com</strong>bined with electrocardiographic aberrations<br />
during an exercise test, 8 with positive<br />
ei<strong>the</strong>r stress ECG test or dobutamine Echocardiography),<br />
63 males (52.5%) and 57 females (47.5%)<br />
with age ranged from (35-68) years. All subjects<br />
underwent coronary arteriography by <strong>the</strong> Judkins<br />
method.<br />
According to <strong>the</strong> findings from coronary angiographic<br />
exploration we divided our patients into<br />
four groups: Group 1 with normal coronary arteries;<br />
Group 2 with one-vessel coronary artery disease;<br />
Group 3 with two-vessel coronary artery disease;<br />
and Group 4 with three-vessel coronary artery<br />
disease.<br />
The severity <strong>of</strong> coronary a<strong>the</strong>rosclerosis calculated<br />
according to (Gensini score) [6]. The Gensini<br />
score was <strong>com</strong>puted by assigning a severity score<br />
to each coronary stenosis according to <strong>the</strong> degree<br />
<strong>of</strong> luminal narrowing and its geographic importance.<br />
Reduction in <strong>the</strong> lumen diameter were evaluated;<br />
(reductions <strong>of</strong> 25%, 50%, 75%, 90%, 99%, and<br />
<strong>com</strong>plete occlusion were given scores <strong>of</strong> 1, 2, 4,<br />
8, 16, and 32, respectively). Each principal vascular<br />
segment was assigned a multiplier in accordance<br />
with <strong>the</strong> functional significance <strong>of</strong> <strong>the</strong> myocardial<br />
area supplied by that segment: The left main coronary<br />
artery, x 5; <strong>the</strong> proximal segment <strong>of</strong> left<br />
anterior descending coronary artery (LAD), x 2.5;<br />
<strong>the</strong> proximal segment <strong>of</strong> <strong>the</strong> circumflex artery, x<br />
2.5; <strong>the</strong> mid-segment <strong>of</strong> <strong>the</strong> LAD, x 1.5; <strong>the</strong> right<br />
coronary artery, <strong>the</strong> distal segment <strong>of</strong> <strong>the</strong> LAD,<br />
<strong>the</strong> posterolateral artery, and <strong>the</strong> obtuse marginal<br />
artery, x 1; and o<strong>the</strong>rs, x 0.5.<br />
112<br />
Gensini score <strong>of</strong> each lesion = (score <strong>of</strong> reduction<br />
x score <strong>of</strong> vascular segment).<br />
All patients included in <strong>the</strong> study underwent a<br />
vascular duplex scan <strong>of</strong> <strong>the</strong> right and left carotid<br />
arteries and <strong>the</strong> right and left femoral superficial<br />
arteries by means <strong>of</strong> transcutaneous high axial<br />
resolution B-mode ultrasound imaging.<br />
The Carfem index in mm was determined as<br />
follows [7]:<br />
(IMThCR + IMThCL + TWThFR + TWThFL)/4.<br />
Where: IMThCR denotes intima media thickness<br />
<strong>of</strong> Rt. Common carotid artery, IMThCL denotes<br />
intima media thickness <strong>of</strong> Lt. Common carotid<br />
artery, TWThFR denotes <strong>the</strong> total wall<br />
thickness <strong>of</strong> <strong>the</strong> right femoral superficial artery<br />
and TWThFL denotes <strong>the</strong> total wall thickness <strong>of</strong><br />
<strong>the</strong> left femoral superficial artery.<br />
Statistical methodology:<br />
The data collected were tabulated and analyzed<br />
by SPSS statistical package version 13 on IBM<br />
<strong>com</strong>patible <strong>com</strong>puter.<br />
Quantitative data were expressed as mean and<br />
standard deviation (X ± SD) analyzed by applying<br />
ANOVA test (f-test) for <strong>com</strong>parison <strong>of</strong> more than<br />
two groups <strong>of</strong> normally distributed variables; and<br />
krauskal wallis test for non normally distributed<br />
variables.<br />
Qualitative data were expressed as number and<br />
percentage (No & %) and analyzed by applying<br />
chi-square (X 2) test.<br />
Pearson correlation (r) was used to detect association<br />
between quantitative variables.<br />
All <strong>the</strong>se tests were used as tests <strong>of</strong> significance<br />
at p0.05, but <strong>the</strong>re was significant difference for <strong>the</strong><br />
systolic blood pressure & diastolic blood pressure<br />
p value
Mahmoud Soliman, et al<br />
Table 1: Clinical characteristics and basic data in studied groups.<br />
Variable<br />
Age (years)<br />
Sex:<br />
Male<br />
Female<br />
SBP (mmHg)<br />
DBP (mmHg)<br />
DM:<br />
+Ve<br />
–Ve<br />
WM:<br />
+Ve<br />
–Ve<br />
Total Chol: mg/dl<br />
HDL: mg/dl<br />
LDL: mg/dl<br />
TG: mg/dl<br />
Group 1<br />
(No. 30)<br />
53.3±6.89<br />
14 (46.7%)<br />
16 (53.3%)<br />
138.3±17.2<br />
86.3±10.3<br />
13 (43.3%)<br />
17 (56.7%)<br />
7 (23.3%)<br />
23 (76.7%)<br />
171±20.7<br />
37.6±3.5<br />
94.7±11.9<br />
158±19.9<br />
SBP : Systolic blood pressure.<br />
DBP : Diastolic blood pressure.<br />
DM : Diabetes Mellitus.<br />
WM : Wall motion abnormalities.<br />
Comparison between all studied group as regards<br />
CARFEM index & Gensini score (Table<br />
2):<br />
CARFEM index showed highly significant<br />
difference between all groups, p value
The Carotid-Femoral Arterial Index & <strong>the</strong> Severity <strong>of</strong> Coronary A<strong>the</strong>rosclerosis<br />
CARFEM<br />
CARFEM<br />
1.9<br />
1.8<br />
1.7<br />
1.6<br />
1.5<br />
1.4<br />
Group: 4.00<br />
Table 2: Comparison between all studied groups as regard to CARFEM index & Gensini score.<br />
Variable<br />
CARFEM mm.<br />
Gensini score<br />
Group 1<br />
(No. 30)<br />
0.54±0.06<br />
0<br />
CARFEM: Carotid-Femoral vascular index.<br />
Group 2<br />
(No. 30)<br />
0.87±0.04<br />
17.6±10.92<br />
114<br />
Group 3<br />
(No. 30)<br />
1.22±0.08<br />
66±25.13<br />
Group 4<br />
(No. 30)<br />
1.54±0.1<br />
181.33±37.11<br />
p. value<br />
Mahmoud Soliman, et al<br />
Figure 5: Lfeft <strong>com</strong>mon croatid, supper femoral arteries and<br />
coronary angio <strong>of</strong> <strong>the</strong> same Patient.<br />
Discussion<br />
The value <strong>of</strong> Carotid intima media thickness<br />
as surroguate <strong>of</strong> coronary a<strong>the</strong>rosclerosis is still a<br />
matter <strong>of</strong> debate. Many studies and even postmortem<br />
studies documented high correlation between<br />
carotid and coronary a<strong>the</strong>rosclerosis [8-11]. However<br />
o<strong>the</strong>r studies showed that <strong>the</strong> correlation between<br />
carotid intima media thickness and severity <strong>of</strong><br />
coronary a<strong>the</strong>rosclerosis is relatively weak [12].<br />
115<br />
Examination <strong>of</strong> more vascular beds (like femoral<br />
arteries) and hence more a<strong>the</strong>rosclerotic burden<br />
may have more impact than examination <strong>of</strong> carotids<br />
alone. In this study, <strong>the</strong> carotid femoral index<br />
(CARFEM) was measured and correlated with<br />
severity <strong>of</strong> coronary a<strong>the</strong>rosclerosis detected by<br />
quantitative coronary angiography according to<br />
GENSINI score. In this study, all patients were<br />
matched for age and sex to avoid possible effects<br />
on a<strong>the</strong>rosclerosis process.<br />
There was significant difference between <strong>the</strong><br />
studied groups as regards: SBP, DBP, HDL, and<br />
LDL which considered risk factors for a<strong>the</strong>rosclerosis.<br />
As regards CARFEM vascular index; <strong>the</strong>re was<br />
highly significant difference between all studied<br />
groups, even group 3 & 4 p value 0.05.
The Carotid-Femoral Arterial Index & <strong>the</strong> Severity <strong>of</strong> Coronary A<strong>the</strong>rosclerosis<br />
But, among patients with three vessels disease<br />
<strong>the</strong>re was significant positive correlation between<br />
CARFEM index and Gensini score r: 0.4 & p value<br />
Egypt Heart J 62 (1): 117-124, March 2010<br />
Value <strong>of</strong> Contrast Echocardiography for <strong>the</strong> Diagnosis <strong>of</strong><br />
Hepatopulmonary Syndrome in Patients with Chronic Liver<br />
Disease Due to Hepatitis C Virus<br />
AMAL SHAWKY BAKIR, MD; GHADA EL-SHAHED, MD*<br />
Background: Hepatopulmonary syndrome (HPS), a triad <strong>of</strong> liver disease, pulmonary gas exchange abnormalities and<br />
widespread pulmonary vascular dilatation, is most <strong>com</strong>monly seen in patients with liver cirrhosis. Contrast-enhanced twodimensional<br />
echocardiography (CEE) using agitated saline can be used to detect <strong>the</strong> presence and degree <strong>of</strong> intra or extracardiac<br />
right-to-left shunting.<br />
Aim: The aim <strong>of</strong> this work was to evaluate HPS in patients with chronic liver disease due to hepatitis C virus (HCV) using<br />
CEE and to determine its relation to <strong>the</strong>ir clinical and laboratory pr<strong>of</strong>ile.<br />
Methods: Sixty patients with chronic liver disease due to hepatitis C virus underwent thorough clinical and laboratory<br />
assessment for evaluation and Child classification <strong>of</strong> liver disease, and to confirm HCV virus infection. Arterial blood gas<br />
analysis, abdominal ultrasonography, pulmonary function testing and upper GI endoscopy were done for all patients. CEE was<br />
performed by injecting agitated saline into an antecubital vein. An intrapulmonary shunt (IPS) was considered present if<br />
microbubbles appeared in <strong>the</strong> left atrium (LA) at least four heart beats after <strong>the</strong>ir appearance in <strong>the</strong> right side <strong>of</strong> <strong>the</strong> heart. It<br />
was graded semi- quantitatively (grades I-IV) according to <strong>the</strong> relative opacification <strong>of</strong> <strong>the</strong> LA.<br />
Results: The mean age <strong>of</strong> <strong>the</strong> patients was 48.28±5.3 years, and 90% were males. Thirty-one patients (51.67%) showed<br />
positive echo findings, reflecting <strong>the</strong> presence <strong>of</strong> IPS. Twelve patients (20%) had grade II echo findings, 7 (11.67%) had grade<br />
III, and 12 (20%) had grade IV echo findings. Sixteen patients (26.67%) showed <strong>the</strong> clinical picture and criteria <strong>of</strong> HPS, while<br />
15 patients (25%) had positive echo findings without <strong>the</strong> clinical picture. There was a highly significant correlation between<br />
echo grading and each <strong>of</strong> Child's score, shrunken liver, splenomegaly, collaterals, dyspnea, platypnea, cyanosis, clubbing,<br />
orthodeoxia, impaired FEV 1 and esophageal varices (p0.05). The most sensitive predictors for HPS were increase portal vein diameter,<br />
clubbing and cyanosis p25mmHg with a normal pulmonary capillary<br />
wedge pressure in <strong>the</strong> setting <strong>of</strong> portal hypertension.<br />
(Ioachimescu et al, 2007).<br />
HPS is defined as <strong>the</strong> triad <strong>of</strong> liver disease,<br />
pulmonary gas exchange abnormalities leading to
Value <strong>of</strong> Contrast Echocardiography for <strong>the</strong> Diagnosis <strong>of</strong> Hepatopulmonary Syndrome<br />
arterial deoxygenation (PO 2
Amal S Bakir & Ghada El-Shahed<br />
Pulmonary function test. Simple spirometeric<br />
function test including FEV 1 (forced expiratory<br />
volume in <strong>the</strong> 1 st second) was done to assess <strong>the</strong><br />
airway function. The respirometer used was (spirometrics<br />
1986, Model 2500, version 3.1. USA).<br />
Upper GIT endoscopy was done for all patients,<br />
using pentax EG-2940 endoscope (videoscope),<br />
with <strong>the</strong> patient fasting for at least 6 hrs.<br />
Transthoracic contrast enhanced echocardiography<br />
(CEE) was performed using a 2.5MHz<br />
transducer attached to a <strong>com</strong>mercially available<br />
VINGMED VIVID V machine equipped with a<br />
harmonic imaging capability.<br />
CEE was performed by injecting 8mL agitated<br />
saline solution through an antecubital 18-gauge<br />
cannula and two 10-mL syringes connected by a<br />
three-way stopcock. In <strong>the</strong> apical 4-chamber view,<br />
<strong>the</strong> appearance <strong>of</strong> microbubbles in <strong>the</strong> right cardiac<br />
chambers was noted. An intrapulmonary shunt<br />
(IPS) was considered present if microbubbles<br />
appeared in <strong>the</strong> LA at least four heart beats after<br />
<strong>the</strong> initial appearance <strong>of</strong> contrast in <strong>the</strong> right side<br />
<strong>of</strong> <strong>the</strong> heart (Rodriguez-Roision et al, 2004).<br />
The relative opacification <strong>of</strong> <strong>the</strong> LA was assessed<br />
semiquantitatively as follows: Grade 0, no<br />
microbubble in LA; grade I, a few bubbles in LA<br />
indicating small IPS; grade II, moderate bubbles<br />
without <strong>com</strong>plete filling <strong>of</strong> <strong>the</strong> LA (moderate IPS);<br />
grade III, many bubbles filling <strong>the</strong> LA <strong>com</strong>pletely<br />
(large IPS); and grade IV, extensive bubbles as<br />
dense as in <strong>the</strong> right atrium (extensive IPS). Three<br />
repeated contrast injections were performed. The<br />
next injection was started after <strong>com</strong>plete removal<br />
<strong>of</strong> microbubbles from RA and LA cavities. An IPS<br />
was considered present if any <strong>of</strong> <strong>the</strong> three injections<br />
119<br />
was positive (Vedrinne et al, 1997). Studies performed<br />
during involuntary Valsalva maneuver or<br />
coughing were excluded to avoid an increase <strong>of</strong><br />
RA pressure which may cause shunting across a<br />
patent foremen ovale after three or more cardiac<br />
cycles, <strong>the</strong>refore giving a false-positive result.<br />
All patients had a chest X-ray to exclude <strong>the</strong><br />
presence <strong>of</strong> pulmonary disease, and high resolution<br />
CT chest was done in cases with abnormal X-ray<br />
findings. Pateints with any lung abnormalities were<br />
excluded from <strong>the</strong> study.<br />
A rectal snip was taken from all patients to<br />
exclude Bilharziasis. Liver biopsy was done in<br />
cases suitable for biopsy to exclude any o<strong>the</strong>r<br />
etiology than HCV for chronic liver disease.<br />
Results<br />
Sixty patients were included in <strong>the</strong> study, with<br />
a mean age <strong>of</strong> 48.28±5.3 years. Fifty-four patients<br />
(90%) were males.<br />
Tweny-nine patients (48.33%) showed negative<br />
echo findings (grade 0) indicating absence <strong>of</strong><br />
intrapulmonary vascular dilatation (IPVD), while<br />
31 patients (51.67%) showed positive echo findings,<br />
which reflected presence <strong>of</strong> IPVD.<br />
Sixteen patients (26.67%) showed <strong>the</strong> clinical<br />
picture and criteria <strong>of</strong> HPS (IPVD and hypoxia),<br />
while 15 patients (25%) had positive echo findings<br />
but were lacking <strong>the</strong> clinical picture i.e. subclincal<br />
HPS. None <strong>of</strong> <strong>the</strong> patients showed grade I echo<br />
findings, while 12 (20%) had grade II, 7 patients<br />
(11.67%) had grade III, and 12 patients (20%) had<br />
grade IV echo findings, with presence <strong>of</strong> extensive<br />
bubbles in <strong>the</strong> left side <strong>of</strong> <strong>the</strong> heart equivalent to<br />
that <strong>of</strong> <strong>the</strong> right side (Fig. 1).<br />
Figure 1: Transthoracic 2-dimensional echocardiogram, apical 4 chamber view. Left: Presence <strong>of</strong> contrast in <strong>the</strong> right chambers;<br />
Right: Presence <strong>of</strong> contrast in <strong>the</strong> left chambers after 5 cardiac cycles, <strong>com</strong>patible with intrapulmonary vascular<br />
dilatations.
Value <strong>of</strong> Contrast Echocardiography for <strong>the</strong> Diagnosis <strong>of</strong> Hepatopulmonary Syndrome<br />
As regards <strong>the</strong> correlation between Child's<br />
scoring and echo findings (Table 1), <strong>the</strong>re was a<br />
highly significant correlation between echo grading<br />
and Child's score, showing that <strong>the</strong> more progressed<br />
<strong>the</strong> stage <strong>of</strong> liver disease is, <strong>the</strong> more <strong>the</strong> number<br />
<strong>of</strong> cases with positive echo findings, and <strong>the</strong> grade<br />
<strong>of</strong> echo findings is higher (p
Amal S Bakir & Ghada El-Shahed<br />
Table 5: Correlation between platypnea, cyanosis, clubbing,<br />
and echo grading.<br />
Platypnea,<br />
cyanosis &<br />
clubbing<br />
–ve<br />
+ve<br />
Total<br />
Zero<br />
28<br />
(65.12%)<br />
1<br />
(5.88%)<br />
29<br />
Echo grading<br />
CHI-SQUARE = 23.527 PROB.
Value <strong>of</strong> Contrast Echocardiography for <strong>the</strong> Diagnosis <strong>of</strong> Hepatopulmonary Syndrome<br />
feasible parameter to detect HPS in cirrhotic patients<br />
(Zamirian et al, 2007). Also, Karabulut et al<br />
(2006) showed that right ventricular diastolic dysfunction<br />
was notably more <strong>com</strong>mon in cirrhotic<br />
patients with HPS than those without HPS. We did<br />
not use any <strong>of</strong> <strong>the</strong>se measurements, as we think<br />
<strong>the</strong>y can be non-specific (e.g. LA dilatation can<br />
be caused by systemic hypertension, and RV diastolic<br />
dysfunction can be part <strong>of</strong> <strong>the</strong> normal aging<br />
process). More recently, Lenci et al (2009) showed<br />
that standard echocardiographic parameters did<br />
not distinguish between patients with and those<br />
without HPS.<br />
Transesophageal echocardiography was proposed<br />
for better visualization <strong>of</strong> bubbles in <strong>the</strong><br />
left-sided cardiac chambers, as it allows <strong>the</strong> contrast<br />
to be seen entering from <strong>the</strong> pulmonary veins<br />
(Vedrinne et al, 1997). However, TTE is diagnostic<br />
in <strong>the</strong> majority <strong>of</strong> cases. In addition, <strong>the</strong> presence<br />
<strong>of</strong> esophageal varices, which is considered a relative<br />
contraindication to <strong>the</strong> performance <strong>of</strong> TEE, is<br />
relatively <strong>com</strong>mon in <strong>the</strong>se patients (Rollan et al,<br />
2007). Moreover, we did not wish to expose patients<br />
with de<strong>com</strong>pensated liver to <strong>the</strong> sedation needed<br />
for TEE.<br />
There are, however, some limitations <strong>of</strong> contrast-enhanced<br />
echocardiography. Most notably it<br />
does not accurately quantify <strong>the</strong> degree <strong>of</strong> intrapulmonary<br />
shunting, allowing only a semiquantitative<br />
grading (Wang and Lin 2005). Although<br />
99Technetium macroaggregated albumin<br />
perfusion lung scanning over<strong>com</strong>es this limitation<br />
and permits quantification <strong>of</strong> <strong>the</strong> degree <strong>of</strong> shunting<br />
(Abrams et al, 1998), contrast enhanced ecardiography<br />
has been shown to be more sensitive<br />
than lung perfusion scanning for <strong>the</strong> detection <strong>of</strong><br />
IPVD (Abrams et al, 1995). It has <strong>the</strong> additional<br />
advantage that it can be performed as part <strong>of</strong> routine<br />
echocardiographic screening for pulmonary hypertension.<br />
The European Respiratory Society Task<br />
Force on Pulmonary-Hepatic vascular disorders<br />
has re<strong>com</strong>mended contrast-enhanced echocardiography<br />
as <strong>the</strong> first line screening modality for HPS<br />
(Rodriguez-Roision et al, 2004).<br />
The prevalence <strong>of</strong> HPS varies widely between<br />
different reports (4-47%) (Colle et al, 2007) and<br />
a definitive diagnosis <strong>of</strong> HPS varies between 4%<br />
and 19% in cirrhotic patients. This shows <strong>the</strong><br />
presence <strong>of</strong> intrapulmonary vascular dilatations<br />
(IPVD) in cirrhotic patients without HPS (Lima et<br />
al, 2004). In our study 31 patients (51.67%) showed<br />
positive echo findings <strong>of</strong> IPVD. Sixteen patients<br />
122<br />
(26.67%) showed <strong>the</strong> clinical picture and criteria<br />
<strong>of</strong> HPS, and 15 (25%) had positive echo findings<br />
but not <strong>the</strong> clinical picture i.e. subclincal HPS.<br />
Our study agrees with <strong>the</strong> results <strong>of</strong> Vedrinne et al<br />
(1997), who studied 37 cirrhotic patients and found<br />
that 51% had positive echocardiographic findings.<br />
The prevalence found in our study was lower<br />
than that <strong>of</strong> Byung et al (2004) who studied 130<br />
cirrhotic patients, and found that 61% had positive<br />
echocardiographic findings and 47% had HPS.<br />
On <strong>the</strong> o<strong>the</strong>r hand, Lenci et al (2009) showed<br />
late right-to-left shunting in 26% <strong>of</strong> patients, while<br />
only 16% had a definite diagnosis <strong>of</strong> HPS i.e. CEE<br />
detected intrapulmonary shunting before a change<br />
in arterial blood gases.<br />
The present study clearly showed a significant<br />
correlation between <strong>the</strong> severity <strong>of</strong> hepatopulmonary<br />
syndrome and <strong>the</strong> Child-pugh classification<br />
and score. This is in agreement with Abrams et al<br />
(1995), who showed greater shunt fractions in<br />
Child Pugh A cirrhosis <strong>com</strong>pared with Child Pugh<br />
B and C classes, and Vardereli et al (2001), who<br />
found that hypoxemic cirrhotic patients had a<br />
significantly higher Child-pugh score than those<br />
without hypoxemia. In addition, Ferreira et al<br />
(2008) showed that more advanced liver disease<br />
was associated with HPS. This study also agrees<br />
with that <strong>of</strong> Byung et al (2004) and Amir et al<br />
(2006), who suggested that <strong>the</strong> hepato-pulmonary<br />
syndrome is related to <strong>the</strong> development <strong>of</strong> cirrhosis.<br />
The present study found a direct correlation<br />
between orthodeoxia and hepatopulmonary syndrome<br />
with high statistical significance. We found<br />
that orthodeoxia was present in 51.67% <strong>of</strong> patients,<br />
while Amir et al (2006) found it in 66% with no<br />
significant statistical relation. This may be due to<br />
<strong>the</strong>ir cut <strong>of</strong>f value for hypoxia, which was PO 2<br />
Amal S Bakir & Ghada El-Shahed<br />
This study found a significant correlation between<br />
portal hypertension detected by abdominal<br />
ultrasound and HPS. This agrees with Amir et al<br />
(2006), who found a relation between portal hypertension<br />
and HPS. We also found a direct correlation<br />
between <strong>the</strong> presence <strong>of</strong> esophageal varices<br />
detected by UGIT endoscopy and hepatopulmonary<br />
syndrome. Schenk et al (2002) agreed with our<br />
study. They found esophageal varices more <strong>of</strong>ten<br />
in <strong>the</strong> groups with positive contrast echocardiography,<br />
but <strong>the</strong> difference did not reach statistical<br />
significance. This may be due to <strong>the</strong> small number<br />
<strong>of</strong> patients with HPS found in <strong>the</strong>ir study (9 patients).<br />
Our results agree with Lima et al (2004), who<br />
found no significant difference between HPS and<br />
abnormal pulmonary function.<br />
We used PaO 2 as a measure <strong>of</strong> hypoxia for<br />
prediction <strong>of</strong> HPS. Amir et al (2006) used both<br />
PaO 2
Value <strong>of</strong> Contrast Echocardiography for <strong>the</strong> Diagnosis <strong>of</strong> Hepatopulmonary Syndrome<br />
sepatopulmonary syndrome. Mayo Clin Proc 2004; 79:<br />
42-50.<br />
23- Lucey MR, Brown KA, Everson GT, et al: Minimal criteria<br />
for placement <strong>of</strong> adults on <strong>the</strong> liver transplant waiting<br />
list: A report <strong>of</strong> a national conference organized by <strong>the</strong><br />
American Society <strong>of</strong> Transplant Physicians and <strong>the</strong> American<br />
Association for <strong>the</strong> Study <strong>of</strong> Liver Diseases. Liver<br />
Transpl Surg 1997; 3 (6): 628-637.<br />
24- Martinez G, Barbera J, Visa J, et al: Hepato-pulmonary<br />
syndrome in candidates for liver trans-plantation. J Hepatol<br />
2001; 34: 756-758.<br />
25- Miguel RA, Britt B, Ashwani K, et al: Carboxyhemoglobin<br />
levels in cirrhotic patients with and without HPS.<br />
Gastroenterology 2005; 128: 328-333.<br />
26- Moller S, Henriksen JH: Cardiopulmonary <strong>com</strong>plications<br />
in chronic liver disease. World J Gastroenterol 2006; 12<br />
(4): 526-538.<br />
27- Moorman JP, Joo M, Hahn YS: Evasion <strong>of</strong> host immune<br />
surveillance by hepatitis C virus: Potentian roles in viral<br />
persistence. Arch Immunol Ther Exp (Warsz) 2001; 49:<br />
189-194.<br />
28- Regev A, Yeshurun M, Rodriguez M, et al: Transient<br />
hepatopulmonary syndrome in a patient with acute hepatitis<br />
A. J Viral Hepat 2001; 8: 83-86.<br />
29- Rodriguez-Roision R, Krowka MJ, Herve P, et al: Pulmonary<br />
Hepatic vascular disorders (PHD). Eur Respir J 2004;<br />
24: 861-880.<br />
30- Rodriguez-Roisin R, Krowka MJ: Hepatopulmonary<br />
Syndrome-A Liver-Induced Lung Vascular Disorder.<br />
NEJM 2008; 358: 2378-2387.<br />
124<br />
31- Rollan MJ, Munoz AC, Perez T, et al: Value <strong>of</strong> contrast<br />
echocardiography for <strong>the</strong> diagnosis <strong>of</strong> hepatopulmonary<br />
syndrome. European Journal <strong>of</strong> Echocardiography 2007;<br />
8 (5): 408-410.<br />
32- Schenk P, Fuhrman V, Madl C, et al: Hepatopulmonary<br />
syndrome: Prevalence and predictive value if various cut<br />
<strong>of</strong>fs for arterial oxygenation and <strong>the</strong>ir clinical consequences.<br />
Gut 2002; 51: 853-859.<br />
33- Taille C, Cadranel J, Bellocq A, et al: Liver trans-plantation<br />
for hepatopulmonary syndrome. A ten-year experience in<br />
paris, France Trans-Plantation 2003; 75: 1482-1489.<br />
34- Umeda A, Tagawa M, Kohsaka T, et al: HPS can show<br />
spontaneous resolution: Possible mechanism <strong>of</strong> POPH<br />
overlap? Respirology 2006; 11: 120-123.<br />
35- Vardereli E, Saricam T, Nesrin Aslan N, et al: Hepatopulmonary<br />
syndrome. The Turkish Journal <strong>of</strong> Gastroenterology<br />
2001; 12 (3): 179-184.<br />
36- Vedrinne, Duperret S, Bizollon T, et al: Comparison <strong>of</strong><br />
transesophageal and transthoracic contrast echocardiography<br />
for detection <strong>of</strong> an intrapulmonary shunt in liver<br />
disease. Chest 1997; 111: 1236-1240.<br />
37- Waggoner A, Davila-Roman V, Barzilai B, et al: Contrast<br />
two-dimensional echocardiography provides clinical<br />
information not available with color flow imaging. Journal<br />
<strong>of</strong> Diagnostic Medical Sonography 1992; 8 (1): 2-13.<br />
38- Wang YW, Lin HC: Recent advances in hepatopulmonary<br />
syndrome. J Chin Med Assoc 2005; 68: 500-505.<br />
39- Zamirian M, Aslani A, Shahrzad S: Left atrial volume: A<br />
novel predictor <strong>of</strong> hepatopulmonary syndrome. Am J<br />
Gastroenterol 2007; 102: 1392-1396.
Egypt Heart J 62 (1): 125-133, March 2010<br />
Cardiac Output Measurement by a New Transesophageal Doppler Probe<br />
in Circulatory Shock<br />
NASHWA ABED, MD; MOHAMED AFIFY<br />
Introduction: We conducted a prospective observational study from August 2007 to August 2008 to evaluate efficacy <strong>of</strong><br />
esophageal Doppler monitoring (EDM) in monitoring cardiac output (CO) and tailoring <strong>of</strong> vasoactive drugs doses in patients<br />
with septic shock.<br />
Methods: EDM used in 18 patients with septic shock in which CO measured using cardio Q doltex monitor every 48 hours<br />
and values <strong>com</strong>pared to those taken by pulmonary artery ca<strong>the</strong>ter (PAC) and transthoracic echo (TTE). Also safety <strong>of</strong> EDM<br />
and its value in tailoring doses <strong>of</strong> IV fluids and vasoactive drugs were assessed.<br />
Reuslts: A good correlation was present between CO measured by EDM & TTE and that by PAC. No significant <strong>com</strong>plications<br />
with <strong>the</strong> use <strong>of</strong> EDM in contrast to that <strong>of</strong> PAC; 2 cases <strong>of</strong> pneumothorax no mortality related to <strong>the</strong> procdures in both PAC or<br />
EDM.<br />
Conclusion: The EDM showed an excellent correlation to TTE & PAC, <strong>the</strong> bedside simplicity 3-8min for insertion and<br />
interpretaion safety and continous real time on screen monitoring make it a promising technique for critically ill patients.<br />
Key Words: PAC – EDM – TTE – CO.<br />
Introduction<br />
The transesophaseal Doppelr is currently <strong>the</strong><br />
most promising non invasive technique for monitoring<br />
cardiac output (CO) in ICU patients.<br />
The esophageal Doppler first described in 1971<br />
and subsequently refined by Singer provides a<br />
minimally invasive means <strong>of</strong> continuously monitoring<br />
cardiac function in <strong>the</strong> ICU [1].<br />
Doppler signals can be obtained by an ultrasound<br />
probe placed externally at <strong>the</strong> suprasternal<br />
notch and directed at ascending aorta. However,<br />
esophageal Doppler monitoring has a number <strong>of</strong><br />
advantages over <strong>the</strong> transcutaenous noute. The<br />
close proximity <strong>of</strong> descending aorta to <strong>the</strong> esophagus<br />
probe is an excellent window for obtaining<br />
Doppler signals. Fur<strong>the</strong>rmore, once positioned <strong>the</strong><br />
The Department <strong>of</strong> Critical Care Medicine, Cairo University.<br />
Manuscript received 10 Dec., 2009; revised 15 Jan., 2010;<br />
accepted 16 Jan., 2010.<br />
Address for Correspondence: Dr. Nashwa Abed,<br />
The Department <strong>of</strong> Critical Care Medicine, Cairo University<br />
125<br />
transeophageal probe is stabilized by <strong>the</strong> esophagus,<br />
<strong>the</strong>reby permitting continuous monitoring.<br />
A good correlation has been demonstrated between<br />
<strong>the</strong> CO measured by esophageal doppelr<br />
and simultaneously by <strong>the</strong>rmodilution and fick<br />
methods [2].<br />
Esophageal Doppler monitoring (EDM) would<br />
be <strong>of</strong> limited clinical utility if it only provided an<br />
estimate <strong>of</strong> CO. However, <strong>the</strong> characteristics <strong>of</strong><br />
<strong>the</strong> Doppler flow velocity waveform provides<br />
information on both cardiac preload and contractility.<br />
The peak velocity that's identified as <strong>the</strong> apex<br />
<strong>of</strong> <strong>the</strong> wave form is a good indicator <strong>of</strong> myocardial<br />
contractility and <strong>the</strong> base <strong>of</strong> wave form which is<br />
<strong>the</strong> flow time is indictor for <strong>the</strong> volume status and<br />
preload <strong>of</strong> <strong>the</strong> heart [3].<br />
Aim <strong>of</strong> <strong>the</strong> study:<br />
• The aim <strong>of</strong> this study is to evaluate <strong>the</strong> efficacy<br />
<strong>of</strong> EDM to evaluate CO monitoring <strong>com</strong>pared to<br />
CO measured by transthroacic echocardiography<br />
(TTE).
Cardiac Output Measurement by a New Transesophageal Doppler Probe<br />
• To evaluate <strong>the</strong> efficacy <strong>of</strong> EDM for tailoring <strong>the</strong><br />
doses <strong>of</strong> vasoactive drugs and monitoring <strong>of</strong><br />
hemdoynamics in patients with septic shock.<br />
• To assess <strong>the</strong> overall safety <strong>of</strong> EDM as applied<br />
to critical care patients.<br />
Methods and Material<br />
The study was done at Critical Care Medicine<br />
Department Cairo University in one year period<br />
(2007-2008), all critically ill patients with septic<br />
shock.<br />
Eighteen patients were included in <strong>the</strong> study<br />
10 males and 8 females.<br />
Exclusion criteria:<br />
• Patients with esophageal pathology as cancer,<br />
achalsia, varices.<br />
• Patients with hematemesis if upper endoscopy<br />
not done to exclude varices or cancer.<br />
• Patients with severe coagulopathy.<br />
• Also cardiac patients with ejection fraction less<br />
than 45% or severe valve dysfunction.<br />
Study design and data collection:<br />
• A prospective observational cohart study design<br />
was used.<br />
• For all patients <strong>the</strong> following characteristics were<br />
prospectively recorded.<br />
• Full consent taken by patients relatives.<br />
• Age, weight, height, body surface area.<br />
• PO2/FiO2 ratio.<br />
• Coagulation pr<strong>of</strong>ile.<br />
• Complete blood count.<br />
• Liver function tests.<br />
• Severity <strong>of</strong> illness as indicated by Acute Physiology<br />
and Chronic Health evaluation (APACHE)<br />
II as well as sequential organ failure assessment<br />
(SOFA) score.<br />
• Hemdoynamic variables as heart rate central<br />
venous pressure (CVP), arterial blood pressure.<br />
• Cardiac output and systemic vascular resistance<br />
by EDM and TTE.<br />
• Also monitoring <strong>of</strong> possible <strong>com</strong>plications as<br />
esophageal perforations or O 2 desaturation less<br />
than 90% by oximetry, atrial or ventricular ar-<br />
126<br />
rhythmias, gastrointestinal bleeding and unintentional<br />
tracheal extubation or accidental tracheal<br />
insertion or accidental removal <strong>of</strong> nasogastric<br />
tube.<br />
Measurement <strong>of</strong> CO:<br />
EDM probe consists <strong>of</strong> continuous wave Doppler<br />
transducer (4MHz) mounted at 45º at <strong>the</strong> tip<br />
<strong>of</strong> <strong>the</strong> probe (diameter 8mm). The probe is connected<br />
to a monitor (Deltex medical Ltd, England)<br />
that display <strong>the</strong> blood flow velocity wave form<br />
after spectral analysis <strong>of</strong> <strong>the</strong> reflected doppelr shift<br />
signal [4]. After oral introduction <strong>the</strong> probe is<br />
advanced gently until 35cm from <strong>the</strong> incisors is<br />
reached, and a good wave form is obtained. Gain<br />
& Filler settings were optimized to eliminate <strong>the</strong><br />
noise related to low frequency motion <strong>of</strong> <strong>the</strong> vessels<br />
wall.<br />
The monitor was preset to calculate CO (Litters<br />
per minutes) by averaging stroke volume over 12<br />
beats and multiplying <strong>the</strong> value obtained by <strong>the</strong><br />
HR.<br />
The left ventricular flow time (i.e. ejection<br />
time) corrected for heart rate provide an index <strong>of</strong><br />
left ventricular preload [4].<br />
Cardiac output normally 3-7 litres/min [5] below<br />
3 considered low CO and above 7 considered high<br />
CO.<br />
Corrected flow time (FTc) less than 300 m.sec<br />
were considered low i.e. preload and values greater<br />
than 360 msec were considered high [8].<br />
CO & FTc as well as o<strong>the</strong>r hemodynamic variable<br />
were measured every 12 hours for 48 hours.<br />
CO measured by EDM <strong>com</strong>pared to that measured<br />
by TTE using transaortic flow and left ventricular<br />
outflow diameter and getting velocity time<br />
integral (VTI) across <strong>the</strong> left ventricular outflow<br />
using <strong>the</strong> velocity equation:<br />
SV = VTI x BSA<br />
SV = VTI x πr 2<br />
CO = SV x HR<br />
Were r is radius <strong>of</strong> LV outflow.<br />
π = 3.14<br />
Statistical analysis:<br />
All <strong>com</strong>parisons between EDM measures and<br />
by TTE correlation determined by using simple<br />
linear regression analysis.
Nashwa Abed & Mohamed Afify<br />
Results<br />
A total <strong>of</strong> 18 patients with septic shock underwent<br />
hemdoynamic variables monitoring via EDM<br />
& TTE <strong>the</strong> patients characteristics were shown in<br />
<strong>the</strong> above table.<br />
EDM was successfully applied to all patients<br />
with average time for interpretation about 8 minute<br />
ranging from 7 to 15 minutes.<br />
Safety <strong>of</strong> <strong>the</strong> EDM: Accidental removal <strong>of</strong><br />
nasogastric tube in two patients and <strong>the</strong> need for<br />
sedation with intermittent doses <strong>of</strong> prop<strong>of</strong>ol caused<br />
reversible hypotension with fluid boluses in two<br />
Table 1: Characteristic <strong>of</strong> <strong>the</strong> simple.<br />
No.<br />
1<br />
2<br />
3<br />
4<br />
5<br />
6<br />
7<br />
8<br />
9<br />
10<br />
11<br />
12<br />
13<br />
14<br />
15<br />
16<br />
17<br />
18<br />
CO-EDM<br />
12.00<br />
10.00<br />
8.00<br />
6.00<br />
4.00<br />
Age<br />
28<br />
60<br />
68<br />
75<br />
80<br />
50<br />
38<br />
58<br />
99<br />
65<br />
45<br />
29<br />
60<br />
52<br />
60<br />
65<br />
63<br />
60<br />
Sex<br />
M<br />
M<br />
M<br />
M<br />
M<br />
F<br />
M<br />
F<br />
F<br />
F<br />
F<br />
F<br />
M<br />
M<br />
M<br />
F<br />
F<br />
M<br />
SOFA<br />
score<br />
11<br />
11<br />
8<br />
10<br />
10<br />
7<br />
12<br />
8<br />
10<br />
11<br />
8<br />
19<br />
10<br />
10<br />
18<br />
16<br />
12<br />
12<br />
APACHE II<br />
25<br />
27<br />
24<br />
25<br />
27<br />
24<br />
39<br />
25<br />
27<br />
35<br />
25<br />
30<br />
19<br />
17<br />
40<br />
30<br />
36<br />
36<br />
CVP<br />
CmH 2 O<br />
5<br />
10<br />
14<br />
13<br />
8<br />
10<br />
18<br />
10<br />
16<br />
8<br />
3<br />
13<br />
3<br />
16<br />
9<br />
9<br />
7<br />
6<br />
CO<br />
EDM<br />
7.7<br />
6.4<br />
11<br />
8<br />
7.2<br />
8.9<br />
7.9<br />
9<br />
4.8<br />
4<br />
10.8<br />
5.7<br />
4.6<br />
6.2<br />
11.4<br />
6.1<br />
9.5<br />
10<br />
4.00 6.00 8.00 10.00 12.00 14.00<br />
CO-ECHO<br />
Figure 1: Show correlation between CO measured by TTE<br />
and esophageal Doppler probe.<br />
127<br />
patients no accidental endotracheal tube extubation<br />
nor false insertion <strong>of</strong> <strong>the</strong> probe into trachea, desaturation,<br />
GIT bleeding nor arrhythmias.<br />
Comparison between Co measured by EDM &<br />
TTE: EDM measurement <strong>of</strong> CO were <strong>com</strong>pared<br />
with TTE in all patients <strong>the</strong> correlation between<br />
<strong>the</strong> 2 types <strong>of</strong> measurement was significant (p:<br />
0.0005).<br />
Comparison between Co measured by EDM &<br />
CO by PAC: EDM measurement <strong>of</strong> CO were <strong>com</strong>pared<br />
with PAC in all patients <strong>the</strong> correlation<br />
between <strong>the</strong> 2 types <strong>of</strong> measurement was significant<br />
(p: 0.0005).<br />
CO<br />
Echo<br />
7.8<br />
6<br />
10<br />
7.9<br />
8<br />
8.3<br />
7.5<br />
9.5<br />
4.5<br />
4.8<br />
9.5<br />
6<br />
4.5<br />
6.4<br />
12.5<br />
5.8<br />
8.4<br />
9.4<br />
CO-EDM<br />
12.00<br />
10.00<br />
8.00<br />
6.00<br />
4.00<br />
FTc<br />
m.sec<br />
372<br />
272<br />
360<br />
329<br />
275<br />
270<br />
361<br />
329<br />
320<br />
497<br />
330<br />
270<br />
359<br />
280<br />
280<br />
360<br />
395<br />
335<br />
Complications<br />
Nasogastric tube<br />
Nasogastric<br />
No<br />
No<br />
No<br />
Hypotension<br />
Hypotension<br />
No<br />
No<br />
No<br />
No<br />
No<br />
No<br />
No<br />
No<br />
No<br />
No<br />
No<br />
Need for<br />
sedation<br />
Yes<br />
Yes<br />
Yes<br />
No<br />
No<br />
Yes<br />
Yes<br />
Yes<br />
Yes<br />
Yes<br />
Yes<br />
No<br />
No<br />
Yes<br />
Yes<br />
Yes<br />
Yes<br />
Yes<br />
CO by PAC<br />
8.5<br />
6.5<br />
11<br />
8<br />
8.2<br />
8.5<br />
7.8<br />
9.2<br />
5<br />
9.5<br />
10<br />
6<br />
4.5<br />
6.9<br />
11.2<br />
6<br />
9.8<br />
11.2<br />
4.00 6.00 8.00 10.00 12.00<br />
CO-PAC<br />
Figure 2: Correlation between CO measured by pulmonary<br />
artery ca<strong>the</strong>ter and esophageal Doppler probe.
Cardiac Output Measurement by a New Transesophageal Doppler Probe<br />
Table 2: Summary Studies <strong>com</strong>paring hemodynamics measured by EDM and conventional protocols.<br />
Author/Year<br />
Noblett, et al,<br />
2006 [15]<br />
NR: Not reported.<br />
Table 3.<br />
Author/Year<br />
Wakeling, et al,<br />
2005 [16]<br />
Study<br />
Design/Purpose<br />
Design: RCT<br />
Purpose: to assess <strong>the</strong><br />
effect <strong>of</strong> optimizing<br />
hemodynamic status,<br />
using a protocoldriven<br />
intraoperative<br />
fluid regimen, on<br />
out<strong>com</strong>e following<br />
elective colorectal<br />
resection.<br />
ECRI Quality Score<br />
(Rating): 9.1 (High)<br />
Study<br />
Design/Purpose<br />
Design: RCT<br />
Purpose: to determine<br />
whe<strong>the</strong>r using<br />
intraoperative<br />
esophageal Doppler<br />
guided fluid<br />
management to<br />
minimize<br />
hypovolemia<br />
would reduce<br />
postoperative hospital<br />
stay and <strong>the</strong> time<br />
before<br />
return to gut function<br />
after colorectal<br />
surgery.<br />
ECRI Quality Score<br />
(Rating): 9.0 (High)<br />
Intervention/<br />
Out<strong>com</strong>es<br />
Treatment group<br />
Intervention:<br />
EDM (CardioQ) +<br />
CVP + conventional<br />
protocol<br />
Control Group<br />
Intervention:<br />
CVP + conventional<br />
protocol<br />
Intervention/<br />
Out<strong>com</strong>es<br />
Treatment Intervention:<br />
EDM (CardioQ) +<br />
CVP + conventional<br />
protocol<br />
Control Intervention:<br />
CVP + conventional<br />
protocol<br />
128<br />
Demographics<br />
54 in treatment group<br />
54 in control group<br />
Age (median ± IQR)<br />
Treatment: 62.3±14.0<br />
Control: 67.6±15.<br />
% female: Treatment:<br />
NR Control: NR Type <strong>of</strong><br />
surgery: Elective bowel<br />
surgery<br />
Inclusion Criteria:<br />
Patients requiring<br />
elective bowel surgery<br />
Exclusion Criteria:<br />
Severe esophageal<br />
disease, recent<br />
esophageal or upper<br />
airway surgery,<br />
systemic steroid<br />
medication, moderate<br />
or severe aortic valve<br />
disease, bleeding<br />
dia<strong>the</strong>sis and patient<br />
choice<br />
Demographics<br />
Total Enrolled:<br />
128 (64) in treatment<br />
group (64) in control<br />
group Age (median ±<br />
IQR) Treatment:<br />
69.1±12.3 Control:<br />
69.6±10.2% female:<br />
Treatment: 40.6<br />
Control: 46.9 Type <strong>of</strong><br />
surgery: Elective or<br />
semi-elective bowel<br />
surgery<br />
Inclusion Criteria:<br />
Patients requiring<br />
elective or semi-elective<br />
bowel surgery<br />
Exclusion Criteria:<br />
Patients with age
Nashwa Abed & Mohamed Afify<br />
Table 4.<br />
Author/Year<br />
Conway, et al,<br />
2002 [17]<br />
Table 5.<br />
Author/Year<br />
Gan, et al,<br />
2002 [18]<br />
Study<br />
Design/Purpose<br />
Design: RCT<br />
Purpose: to examine<br />
<strong>the</strong> effect <strong>of</strong> esophageal<br />
Doppler guided fluid<br />
administration during<br />
colorectal resection on<br />
hemodynamic<br />
performance, hospital<br />
stay, and post-operative<br />
<strong>com</strong>plications ECRI<br />
Quality Score (Rating):<br />
8.5 (High)<br />
Study<br />
Design/Purpose<br />
Design: RCT<br />
Purpose: to investigate<br />
whe<strong>the</strong>r goal-directed<br />
intraoperative plasma<br />
volume expansion<br />
guided by <strong>the</strong> EDM<br />
would shorten <strong>the</strong><br />
length <strong>of</strong> hospital stay<br />
and improve<br />
postoperative out<strong>com</strong>es<br />
in patients undergoing<br />
moderate risk surgery<br />
ECRI Quality Score<br />
(Rating): 8.1 (Moderate)<br />
Intervention/<br />
Out<strong>com</strong>es<br />
Treatment Intervention:<br />
EDM (TECO 2) + CVP<br />
+ conventional protocol<br />
Control Intervention:<br />
CVP + conventional<br />
protocol<br />
Intervention/<br />
Out<strong>com</strong>es<br />
Treatment Intervention:<br />
EDM (EDMTM) + CVP<br />
+ conventional protocol<br />
Control Intervention:<br />
CVP + conventional<br />
protocol<br />
129<br />
Demographics<br />
Total Enrolled:<br />
57 29 in treatment group<br />
28 in control group Age<br />
(mean ± SD) Treatment:<br />
66.5±12.5 Control:<br />
67.5±10.1 % female:<br />
Treatment: NR Control: NR<br />
Type <strong>of</strong> surgery: Major<br />
non-emergent bowel<br />
surgery<br />
Inclusion Criteria:<br />
Patients undergoing major<br />
bowel resections<br />
Exclusion Criteria:<br />
Patients undergoing<br />
emergency, intrathoracic,<br />
or esophageal surgery,<br />
patients with known<br />
sensitivity to starch-based<br />
colloid or history <strong>of</strong><br />
esophageal disease<br />
Demographics<br />
Total Enrolled:<br />
100 50 in treatment group<br />
50 in control group Age<br />
(mean ± SD) Treatment:<br />
56±13 Control: 59±12<br />
% female: Treatment: 38<br />
Control: 48 Type <strong>of</strong> surgery:<br />
Major elective general,<br />
urologic, or gynecologic<br />
surgery<br />
Inclusion Criteria:<br />
Patients with American<br />
Society <strong>of</strong> Anes<strong>the</strong>siologists<br />
(ASA) physical status I, II,<br />
and III who were to undergo<br />
major elective general,<br />
urologic, or gynecologic<br />
surgery with an anticipated<br />
blood loss <strong>of</strong> >500ml.<br />
Exclusion Criteria:<br />
Patients with age 50% or liver enzymes<br />
>50% upper limit <strong>of</strong> normal<br />
values), congestive heart<br />
failure, and esophageal<br />
pathology (avoid potential<br />
<strong>com</strong>plications <strong>of</strong> <strong>the</strong><br />
esophageal probe), and<br />
those undergoing gastric or<br />
esophageal surgery or who<br />
were on antiemetic<br />
medication within 3 days <strong>of</strong><br />
surgery<br />
Results<br />
Mortality Treatment:<br />
0% (0/29) Control: 3.6%<br />
(1/28) p-value: 0.49<br />
Major <strong>com</strong>plications:<br />
Treatment: 0% (0/30)<br />
Control: 17.9% (5/30)<br />
p-value: 0.02<br />
Total <strong>com</strong>plications:<br />
Treatment: 17.2% (5/29)<br />
Control: 32.1% (9/28)<br />
p-value: 0.23a<br />
Length <strong>of</strong> hospital stay:<br />
Mean ± SD in days<br />
Treatment: 18.7±20.2<br />
Control: 12.7±6.0<br />
Median (range):<br />
Treatment: 12<br />
(7-103) Control:<br />
11 (7-30)<br />
p-value: NR<br />
Results<br />
Mortality:<br />
Treatment: 0% (0/50)<br />
Control: 0% (0/50)<br />
p-value: 1.0<br />
Major <strong>com</strong>plications:<br />
Not reported separate<br />
from total <strong>com</strong>plications<br />
Total <strong>com</strong>plications:<br />
Treatment: 42% (21/50)<br />
Control: 76% (38/50)<br />
p-value: 0.001a<br />
Length <strong>of</strong> hospital stay:<br />
Mean ± SD in days<br />
Treatment: 5±3 Control:<br />
7±3 Median Treatment: 6<br />
Control: 7 p-value: 0.03
Cardiac Output Measurement by a New Transesophageal Doppler Probe<br />
Table 6.<br />
Author/<br />
Year<br />
Venn et al,<br />
2002 [19]<br />
Table 7.<br />
Author/<br />
Year<br />
Sinclair,<br />
et al,<br />
1997 [20]<br />
Study<br />
Design/Purpose<br />
Design: RCT<br />
Purpose: to investigate<br />
whe<strong>the</strong>r repeated colloid<br />
fluid challenges to<br />
optimize <strong>the</strong> circulation<br />
intraoperatively, guided<br />
by CVP or esophageal<br />
Doppler ultrasonography,<br />
would benefit high-risk<br />
patients admitted with<br />
fractured hips to a<br />
London teaching hospital<br />
ECRI Quality Score<br />
(Rating): 9.0 (High)<br />
Study<br />
Design/Purpose<br />
Design: RCT<br />
Purpose: to examine <strong>the</strong><br />
possible benefits <strong>of</strong><br />
intraoperative circulatory<br />
optimization using EDM in<br />
patients with fractured neck<br />
<strong>of</strong> femur ECRI Quality<br />
Score (Rating): 8.9 (High)<br />
Intervention/<br />
Out<strong>com</strong>es<br />
Treatment Intervention:<br />
EDM (CardioQ) +<br />
conventional protocol<br />
Control Intervention:<br />
CVP + conventional<br />
protocol<br />
O<strong>the</strong>r Intervention:<br />
Conventional protocol<br />
alone<br />
Intervention/<br />
Out<strong>com</strong>es<br />
Treatment Intervention:<br />
EDM (ODM 2) +<br />
conventional protocol<br />
Control Intervention:<br />
Conventional protocol<br />
130<br />
Demographics<br />
Total Enrolled:<br />
90 30 in treatment group 31<br />
in control group 29 in o<strong>the</strong>r<br />
group Age (mean ± SD)<br />
Treatment: 82±8.7 Control:<br />
85±6.2 O<strong>the</strong>r: 84.5±9.3 %<br />
female: Treatment: 80<br />
Control: 87.1 O<strong>the</strong>r: 79.3<br />
Type <strong>of</strong> surgery: Proximal<br />
femoral fracture repair<br />
Inclusion Criteria:<br />
Patients admitted with<br />
fractured hips<br />
Exclusion Criteria:<br />
Patients with age
Nashwa Abed & Mohamed Afify<br />
Table 8.<br />
Author/<br />
Year<br />
My<strong>the</strong>n and<br />
Webb 1995<br />
[20]<br />
Table 9.<br />
Author/<br />
Year<br />
McKendry,<br />
et al, [22]<br />
Study<br />
Design/Purpose<br />
Design: RCT<br />
Purpose: to test <strong>the</strong><br />
hypo<strong>the</strong>sis that<br />
perioperative plasma<br />
volume expansion with<br />
colloid (guided by EDM+<br />
CVP) would maintain pHi<br />
during elective cardiac<br />
surgery ECRI Quality<br />
Score (Rating): 8.9 (High)<br />
Study<br />
Design/Purpose<br />
Design: RCT<br />
Purpose: to assess whe<strong>the</strong>r<br />
a nurse led, flow<br />
monitored<br />
protocol for optimizing<br />
circulatory status in<br />
patients after cardiac<br />
surgery reduces<br />
<strong>com</strong>plications and<br />
shortens stay in intensive<br />
care and hospital ECRI<br />
Quality Score (Rating):<br />
8.5 (High)<br />
Intervention/<br />
Out<strong>com</strong>es<br />
Treatment Intervention:<br />
EDM (ODM 1) + CVP<br />
+ conventional protocol<br />
Control Intervention:<br />
CVP + conventional<br />
protocol<br />
Intervention/<br />
Out<strong>com</strong>es<br />
Treatment Intervention:<br />
EDM (CardioQ) +<br />
conventional protocol<br />
Control Intervention:<br />
Conventional protocol<br />
131<br />
Demographics<br />
Total Enrolled:<br />
60 30 in treatment group 30<br />
in control group Age (mean<br />
and range) Treatment: 63<br />
(42-89) Control: 64 (44-86)<br />
% female: Treatment: NR<br />
Control: NR Type <strong>of</strong><br />
surgery: Elective cardiac<br />
surgery (CABG or single<br />
valve replacement)<br />
Inclusion Criteria:<br />
Patients scheduled for<br />
elective coronary artery<br />
bypass grafts (CABG) or<br />
single heart valve<br />
replacement) who had a<br />
preoperative left ventricular<br />
ejection fraction (LVEF)<br />
estimated to be ≥50% and<br />
graded by <strong>the</strong> anes<strong>the</strong>siologist<br />
in charge as ASA grade III.<br />
Exclusion Criteria:<br />
Patients with age
Cardiac Output Measurement by a New Transesophageal Doppler Probe<br />
Discussion<br />
Transesophageal Doppler is minimally invasive<br />
method for continuous monitoring <strong>of</strong> cardiac output<br />
in critically ill patients.<br />
In this study it was used for monitoring <strong>of</strong><br />
cardiac output and SVR in patients with severe<br />
septic shock that's refractory to catecholomines<br />
<strong>the</strong>rapy.<br />
The probe was successfully introduced in all<br />
patients without any significant <strong>com</strong>plication and<br />
was used to follow hemodynamics at bedside along<br />
all <strong>the</strong> hospital stay <strong>of</strong> <strong>the</strong> patient without need for<br />
transfer to <strong>the</strong> echocardiography lab for optimizing<br />
CO nor systemic vascular resistance.<br />
The cardiac output value was correlated well<br />
with measures taken by pulmonary artery ca<strong>the</strong>ter<br />
and transthoracic echocardiography at bed side.<br />
The average insertion time to interpretation<br />
was about 7-8min for EDM and 10-12min for PAC<br />
and about 8.5 minutes for TTE.<br />
Clinical assessment <strong>of</strong> CO at bed side by physician<br />
can be problematic especially patients with<br />
underlying cardiac disease. These previous studies<br />
indicated that physician could estimate CO correctly<br />
only in 50% <strong>of</strong> patients [4].<br />
Ano<strong>the</strong>r study done at Barnes Jewish hospital<br />
2 decade before showed that PCWP was correctly<br />
predicted 30% <strong>of</strong> <strong>the</strong> time, and CO, SVR and right<br />
atrial pressure were correctly predicted approximately<br />
50% <strong>of</strong> <strong>the</strong> time [5].<br />
The limitations <strong>of</strong> <strong>the</strong> currently available techniques<br />
as PAC, dye dilation and transthroacic<br />
electrical impedance for measuring CO suggest a<br />
need for tansesophageal Doppler monitoring.<br />
Thermodilution is affected by variety <strong>of</strong> external<br />
factors and patients related conditions (e.g., tricuspid<br />
regurgitation intracardiac shunts and low cardiac<br />
output state) [6,7].<br />
Similarly, estimation <strong>of</strong> CO obtained by using<br />
fick methods e.g. dye dilution can be adversely<br />
affected by <strong>the</strong> lack <strong>of</strong> hemdoynamic instability<br />
<strong>of</strong>ten encountered in patients on mechanical ventilation<br />
[8,9]. Which is <strong>com</strong>mon situation in critically<br />
ill patients.<br />
More important patient out<strong>com</strong>e may be adversely<br />
affected by <strong>the</strong>se techniques to assess <strong>the</strong><br />
132<br />
hemdonamic status as shown by <strong>the</strong> Study to Understand<br />
Prognosis and Preference for Out<strong>com</strong>es<br />
and Risk <strong>of</strong> Treatment (SUPPORT) that examined<br />
more than 5000 patients and found by case matching<br />
analysis that patients with right sided heart<br />
ca<strong>the</strong>terization had an increased 30 day mortality<br />
(odds ratio, 1.24; 95% CI, 1.03-1.99) [10,11]. These<br />
investigator also found that <strong>the</strong> mean cost per<br />
hospital study was higher in patients received PAC<br />
for monitoring <strong>of</strong> hemodynamcis. This view was<br />
supported by a recent consensus panel.<br />
Also, <strong>the</strong> need for multiple steps in obtaining<br />
hemdoynamic data including ca<strong>the</strong>ter placement,<br />
calibration <strong>of</strong> transducers, interpretation <strong>of</strong> wave<br />
form, increase <strong>the</strong> likelihood for error in interpretation<br />
[12,13]. On <strong>the</strong> o<strong>the</strong>r hand EDM provided an<br />
easy and rapid time for interpretation without all<br />
<strong>the</strong>se steps in addition to provide a continuous real<br />
time monitoring <strong>of</strong> CO [11].<br />
Our study may be a leading one in using EDM<br />
in monitoring <strong>of</strong> CO and SVR in patients with<br />
septic shock receiving hemodynamic supportive<br />
drugs in addition to fluid replacement <strong>the</strong>rapy. The<br />
o<strong>the</strong>r studies used EDM intra-operative and postoperatiave<br />
purpose for monitoring volume status<br />
<strong>of</strong> patient underwent hip replacement, bowel resection<br />
or proximal femoral fracture [15-18].<br />
Compared to our study <strong>the</strong>se studies <strong>com</strong>pared<br />
volume status and fluid replacement <strong>the</strong>rapy in<br />
two groups in one using EDM +CVP. To monitoring<br />
<strong>the</strong>rapy and ano<strong>the</strong>r group using only CVP monitoring<br />
yet in our study we used EDM & CVP to<br />
monitor CO, SVR to optimize filling pressure and<br />
doses <strong>of</strong> noraderaline and terlipressin in those<br />
patients with severe septic shock.<br />
In <strong>the</strong> study <strong>of</strong> Noblette, et al [15] EDM was<br />
used to asses effect <strong>of</strong> optimizing hemodynamic<br />
status using a protocol driven intra-operative fluid<br />
regimen on out<strong>com</strong>e following elective colorectal<br />
resection.<br />
In which EDM caused significant decrease in<br />
length <strong>of</strong> hospital stay and less major <strong>com</strong>plications<br />
yet no effect on mortality.<br />
Compared to our study <strong>the</strong> aim was to use EDM<br />
as bed side technique for measuring CO & SVR<br />
and by which we could wean noradrenaline and<br />
adjust doses <strong>of</strong> dobutamien and terlipressin. EDM<br />
could help in weaning <strong>of</strong> vasoactive drugs in 7 out<br />
18 patients with severe catecholamine dependency.
Nashwa Abed & Mohamed Afify<br />
In our study no reported significant <strong>com</strong>plications<br />
only accidental removal <strong>of</strong> nasogastric tube<br />
in one case.<br />
We can conclude that EDM can be a good and<br />
cost effective alternative to PAC for obtaining<br />
hemdoynamic data.<br />
The EDM showed an excellent correlation to<br />
echocardiography & PAC. The bed side simplicity<br />
3-8min for insertion and interpretation safety and<br />
continuous real time monitoring <strong>of</strong> CO make EDM<br />
show a promises as a reliable method for critically<br />
ill patients need continuous monitoring and support.<br />
References<br />
1- Side CD, Gosling RJ: Non-surgical assessment <strong>of</strong> cardiac<br />
function. Nature 1971; 232: 335-336.<br />
2- Singer M, Clarke J, Bennett ED: Continuous hemodynamic<br />
monitoring by esophageal Doppler. Crit Care Med 1989;<br />
17: 447-452.<br />
3- Cuschien J, Rivers E, Caruso J, et al: A <strong>com</strong>parison <strong>of</strong><br />
transesophageal Doppler, <strong>the</strong>rmodilution and Fick cardiac<br />
output measurements in critically ill patients [abstract].<br />
Crit Care Med 1998; 26 (Suppl), A62.<br />
4- Connors AF Jr, McCaffree DR, Gray BA: Evaluation <strong>of</strong><br />
right-heart ca<strong>the</strong>terization in <strong>the</strong> critically ill patient<br />
without acute myocardial infarction. N Engl J Med 1983;<br />
308: 263-267. [Medline].<br />
5- Eisenberg PR, Jaffe AS, Schuster DP: Clinical evaluation<br />
<strong>com</strong>pared to pulmonary artery ca<strong>the</strong>terization in <strong>the</strong><br />
hemodynamic assessment <strong>of</strong> critically ill patients. Crit<br />
Care Med 1984; 12: 549-553. [Medline].<br />
6- Levett JM, Replogle RL: Thermodilution cardiac output:<br />
A critical analysis and review <strong>of</strong> <strong>the</strong> literature. J Surg Res<br />
1979; 27: 392-404. [Medline].<br />
7- Wessel HU, Paul MH, James GW, Grahn AR: Limitations<br />
<strong>of</strong> <strong>the</strong>rmal dilution curves for cardiac output determinations.<br />
J Appl Physiol 1971; 30: 643-652. [Free Full Text].<br />
8- Taylor SH: Measurement <strong>of</strong> <strong>the</strong> cardiac output in man.<br />
Proc R Soc Med 1966; 59 (Suppl): 35-53.<br />
9- Taylor SH, Silke B: Is <strong>the</strong> measurement <strong>of</strong> cardiac output<br />
useful in clinical practice? Br J Anaesth 1988; 60 (8 Suppl<br />
1): 90S-98S. [Medline].<br />
10- Connors AF Jr, Sper<strong>of</strong>f T, Dawson NV, et al: The effectiveness<br />
<strong>of</strong> right heart ca<strong>the</strong>terization in <strong>the</strong> initial care<br />
<strong>of</strong> critically ill patients. SUPPORT Investigators. JAMA<br />
1996; 276: 889-897. [Abstract].<br />
11- Bernard GR, Sopko G, Cerra F, et al: Pulmonary artery<br />
133<br />
ca<strong>the</strong>terization and clinical out<strong>com</strong>es: National Heart,<br />
Lung, and Blood Institute and Food and Drug Administration<br />
Workshop Report. Consensus statement. JAMA<br />
2000; 283: 2568-2572. [Abstract/Free Full Text].<br />
12- Gnaegi A, Feihl F, Perret C: Intensive care physicians’<br />
insufficient knowledge <strong>of</strong> right-heart ca<strong>the</strong>terization at<br />
<strong>the</strong> bedside: Time to act? Crit Care Med 1997; 25: 213-<br />
220. [Medline].<br />
13- Marini JJ: Obtaining meaningful data from <strong>the</strong> Swan Ganz<br />
ca<strong>the</strong>ter. Respir Care 1985; 30: 572-585.<br />
14- Marik PE: Pulmonary artery ca<strong>the</strong>terization and esophageal<br />
Doppler monitoring in <strong>the</strong> ICU. Chest 1999; 116: 1085-<br />
1091. [Abstract/Free Full Text].<br />
15- Noblett SE, Snowden CP, Shenton BK, Horgan AF:<br />
Randomized clinical trial assessing <strong>the</strong> effect <strong>of</strong> Doppleroptimized<br />
fluid management on out<strong>com</strong>e after elective<br />
colorectal resection. The British Journal <strong>of</strong> Surgery 2006;<br />
93 (9): 1069-76.<br />
16- Wakeling HG, McFall MR, Jenkins CS, Woods WG, Miles<br />
WF, Barclay GR, Fleming SC: Intraoperative oesophageal<br />
Doppler guided fluid management shortens postoperative<br />
hospital stay after major bowel surgery Br J Anaesth<br />
2005; 95 (5): 634-42.<br />
17- Conway DH, Mayall R, Abdul-Latif MS, Gilligan S,<br />
Tackaberry C: Randomised controlled trial investigating<br />
<strong>the</strong> influence <strong>of</strong> intravenous fluid titration using oesophageal<br />
Doppler monitoring during bowel surgery. Anaes<strong>the</strong>sia<br />
2002 Sep; 57 (9): 845-9.<br />
18- Gan TJ, Soppitt A, Maro<strong>of</strong> M, El-Moalem H, Robertson<br />
KM, Moretti E, Dwane P, Glass PS: Goal-directed intraoperative<br />
fluid administration reduces length <strong>of</strong> hospital<br />
stay after major surgery. Anes<strong>the</strong>siology 2002; 97: 820-<br />
6.<br />
19- Venn R, Steele A, Richardson P, Poloniecki J, Grounds<br />
M, Newman P: Randomized controlled trial to investigate<br />
influence <strong>of</strong> <strong>the</strong> fluid challenge on duration <strong>of</strong> hospital<br />
stay and perioperative morbidity in patients with hip<br />
fractures. Br J Anaesth 2002 Jan; 88 (1): 65-71.<br />
20- Sinclair S, James S, Singer M: Intraoperative intravascular<br />
volume optimisation and length <strong>of</strong> hospital stay after<br />
repair <strong>of</strong> proximal femoral fracture: Randomized controlled<br />
trial. BMJ 1997; Oct 11, 315 (7113): 909-12.<br />
21- My<strong>the</strong>n MG, Webb AR: Perioperative plasma volume<br />
expansion reduces <strong>the</strong> incidence <strong>of</strong> gut mucosal hypoperfusion<br />
during cardiac surgery. Arch Surg 1995 Apr; 130<br />
(4): 423-9.<br />
22- McKendry M, McGloin H, Saberi D, Caudwell L, Brady<br />
AR, Singer M: Randomised controlled trial assessing <strong>the</strong><br />
impact <strong>of</strong> a nurse delivered, flow monitored protocol for<br />
optimisation <strong>of</strong> circulatory status after cardiac surgery.<br />
BMJ 2004; Jul 31, 329 (7460): 258.
Egypt Heart J 62 (1): 135-140, March 2010<br />
Comparison between Double Intravenous Bolus, Intracoronary Bolus,<br />
and Conventional Intravenous Bolus Dose <strong>of</strong> Tir<strong>of</strong>iban in Patients with<br />
Acute Anterior Myocardial Infarction Treated by Primary<br />
Coronary Intervention<br />
AHMED IBRAHIM NASSAR, MD; NAGWA NAGI EL-MAHALLAWY, MD;<br />
BASSEM WADEI HABIB, MD; ADEL GAMAL HASSANIN, MD;<br />
IMAN ESMAT, MD; HAYTHAM GALAL, MSc<br />
Primary percutaneous coronary intervention (PCI) in patients with AMI has been shown to be preferable to thrombolytic<br />
<strong>the</strong>rapy in terms <strong>of</strong> patient survival, higher rates <strong>of</strong> patency in <strong>the</strong> infarcted arteries, and lower rates <strong>of</strong> reinfarction and stroke<br />
(Zijlstra et al, 1999). Tir<strong>of</strong>iban stands out as a potentially useful adjunct to PCI because it is a small non-peptide molecule,<br />
somewhat similar to eptifibatide, and does not elicit an adverse immune reaction. Compared with abciximab, its advantages<br />
as an adjunct <strong>the</strong>rapy for PCI are lower cost and no overt bleeding <strong>com</strong>plications (Gunasekara et al, 2005).<br />
Aim <strong>of</strong> <strong>the</strong> Study: To <strong>com</strong>pare <strong>the</strong> efficacy <strong>of</strong> different ways <strong>of</strong> bolus dose administration <strong>of</strong> Tir<strong>of</strong>iban in patients with acute<br />
anterior ST segment elevation MI treated with primary percutaneous coronary intervention (1ry PCI) by <strong>com</strong>paring <strong>the</strong><br />
angiographic results, and <strong>the</strong> size <strong>of</strong> infarction in <strong>the</strong> three regimen groups.<br />
Patients and Methods: The study was conducted on 60 patients who presented to <strong>the</strong> emergency room at Ain Shams<br />
University Hospitals, in <strong>the</strong> period between April 2007 and April 2009, <strong>com</strong>plaining <strong>of</strong> acute chest pain and were diagnosed<br />
as having acute anterior ST segment elevation myocardial infarction. All patients were treated by primary percutaneous coronary<br />
intervention. The patients divided randomly into three groups according to <strong>the</strong> bolus dose <strong>of</strong> Tir<strong>of</strong>iban:<br />
• Group (I): It included 20 patients who received <strong>the</strong> conventional single intravenous bolus dose <strong>of</strong> Tir<strong>of</strong>iban upstream in <strong>the</strong><br />
CCU prior to primary PCI (0.4μg/kg/min for 30min).<br />
• Group (II): It included 20 patients who received a high (double) intravenous bolus dose <strong>of</strong> Tir<strong>of</strong>iban upstream in <strong>the</strong> CCU<br />
prior to primary PCI (25μg/kg).<br />
• Group (III): It included 20 patients who received 0.4μg/kg bolus dose Tir<strong>of</strong>iban intracoronary downstream in <strong>the</strong> ca<strong>the</strong>terization<br />
laboratory in addition to <strong>the</strong> upstream intravenous bolus dose.<br />
The bolus dose was given randomly to <strong>the</strong> patients according to <strong>the</strong> group and all patients continued on Tir<strong>of</strong>iban in <strong>the</strong><br />
dose <strong>of</strong> 0.15μ/kg/min continuous infusion for 48 hours, in addition to half dose unfractionated heparin or low molecular weight<br />
heparin.<br />
Echocardiographic examination was done for all patients during <strong>the</strong>ir hospital stay to evaluate:<br />
1- Ejection fraction (EF).<br />
2- LV dimensions.<br />
3- Segmental wall motion abnormalities.<br />
Complications <strong>of</strong> acute MI such as ventricular septal rupture (VSR), acute mitral regurgitation (MR), aneurysms, LV<br />
thrombus etc.<br />
The Department <strong>of</strong> Cardiology, Ain Shams University,<br />
Cairo, Egypt.<br />
Manuscript received 10 Oct., 2009; revised 5 Nov., 2009;<br />
accepted 6 Nov., 2009.<br />
Address for Correspondence: Dr. Ahmed Ibrahim Nassar,<br />
The Department <strong>of</strong> Cardiology, Ain Shams University, Cairo,<br />
Egypt.<br />
Iman Esmat, Ain Shams University, Cairo, Egypt,<br />
E-mail: i_esmat@yahoo.<strong>com</strong><br />
135
Comparison between Double Intravenous Bolus, Intracoronary Bolus<br />
Statistics: Data were collected, revised and <strong>the</strong>n edited on <strong>the</strong> P.C. The data were analyzed statistically by using SPSS<br />
statistical package version (12).<br />
Results: Our results Showed that two vessel disease was present in 35% <strong>of</strong> group I, 25% <strong>of</strong> group II and 10% <strong>of</strong> group III.<br />
Three vessel disease was present in 10% <strong>of</strong> group II and 15% <strong>of</strong> group III and no 3 vessel disease was present in group I. This<br />
was statistically non-significant among <strong>the</strong> three groups (p>0.05). No reflow phenomenon was present in 25% <strong>of</strong> patients in<br />
group I, 15% <strong>of</strong> patients in group III and although <strong>the</strong>re was not any patient who developed no reflow in group II. LV systolic<br />
function; ejection fraction (EF); was estimated by using <strong>the</strong> Simpson method. The mean and SD <strong>of</strong> EF in group I was 41.65±7.82,<br />
in group II was 48.95±8.69 and in group III was 41.20±8.21. This was statistically highly significant in between groups (p0.05).<br />
Conclusion: In patients presented with acute anterior STEMI and treated with primary PCI, <strong>the</strong> high bolus dose tir<strong>of</strong>iban<br />
given intravenously upstream prior to PCI seems to be a safe and effective regimen to improve <strong>the</strong> angiographic and clinical<br />
out<strong>com</strong>es in <strong>com</strong>parison to <strong>the</strong> conventional bolus dose regimen and <strong>the</strong> intracoronary bolus dose regimen, without increasing<br />
<strong>the</strong> risk <strong>of</strong> bleeding.<br />
Key Words: Acute MI – Primary PCI – Tir<strong>of</strong>iban.<br />
Introduction<br />
Primary percutaneous coronary intervention<br />
(PCI) in patients with AMI has been shown to be<br />
preferable to thrombolytic <strong>the</strong>rapy in terms <strong>of</strong><br />
patient survival, higher rates <strong>of</strong> patency in <strong>the</strong><br />
infarcted arteries, and lower rates <strong>of</strong> reinfarction<br />
and stroke (Zijlstra et al, 1999).<br />
These benefits <strong>of</strong> PCI can be fur<strong>the</strong>r enhanced<br />
by administration <strong>of</strong> platelet glycoprotein IIb/IIIa<br />
inhibitors abciximab (Antoniucci et al, 2003). The<br />
conventional dose <strong>of</strong> Tir<strong>of</strong>iban may not achieve<br />
adequate platelet aggregation inhibition <strong>com</strong>pared<br />
with abciximab (Goto et al, 2003). Timing <strong>of</strong> <strong>the</strong><br />
administration <strong>of</strong> Tir<strong>of</strong>iban before PCI also varied,<br />
and patients with different clinical scenarios <strong>of</strong><br />
acute coronary syndrome were studied (De Luca<br />
et al, 2005).<br />
Aim <strong>of</strong> <strong>the</strong> work:<br />
To <strong>com</strong>pare <strong>the</strong> efficacy <strong>of</strong> different ways <strong>of</strong><br />
bolus dose administration <strong>of</strong> Tir<strong>of</strong>iban in patients<br />
with acute anterior ST segment elevation MI treated<br />
with primary percutaneous coronary intervention<br />
(1ry PCI) by <strong>com</strong>paring <strong>the</strong> angiographic results<br />
and <strong>the</strong> size <strong>of</strong> infarction as assessed by echocardiography.<br />
Patients and Methods<br />
The study was conducted on 60 patients who<br />
came to <strong>the</strong> emergency room at Ain Shams University<br />
Hospitals, in <strong>the</strong> period between April 2007<br />
and April 2009, <strong>com</strong>plaining <strong>of</strong> acute chest pain<br />
and were diagnosed as having acute anterior ST<br />
segment elevation myocardial infarction. All patients<br />
were treated by primary percutaneous coronary<br />
intervention.<br />
136<br />
Inclusion criteria:<br />
1- Males and females with age between 20-70<br />
years presenting with acute chest pain and ST<br />
elevation indicative <strong>of</strong> myocardial infarction,<br />
as proposed by <strong>the</strong> Joint Committee <strong>of</strong> <strong>the</strong><br />
European Society <strong>of</strong> Cardiology (ESC) and<br />
American College <strong>of</strong> Cardiology (ACC), is a<br />
new ST segment elevation in 2 or more contiguous<br />
leads <strong>of</strong> at least 1mm at <strong>the</strong> J point in <strong>the</strong><br />
anterior leads (V1-V6, I, aVL) (Alpert et al,<br />
2000).<br />
2- Feasibility to perform PCI within 6 hours from<br />
onset <strong>of</strong> symptoms.<br />
Exclusion criteria:<br />
Patients who have one or more <strong>of</strong> <strong>the</strong> following<br />
were excluded from <strong>the</strong> study:<br />
1- Contraindications for antiplatelets such as bleeding<br />
disorder including gastrointestinal bleeding,<br />
hematuria, or known presence <strong>of</strong> occult blood<br />
in <strong>the</strong> stool prior to randomization.<br />
2- Thrombocytopenia (Platelet count
Ahmed I Nassar, et al<br />
The patients were divided randomly into three<br />
groups according to <strong>the</strong> bolus dose <strong>of</strong> Tir<strong>of</strong>iban:<br />
• Group (I): It included 20 patients who received<br />
<strong>the</strong> conventional single intravenous bolus dose<br />
<strong>of</strong> Tir<strong>of</strong>iban upstream in <strong>the</strong> CCU prior to primary<br />
PCI (0.4μg/kg/min for 30min).<br />
• Group (II): It included 20 patients who received<br />
a high (double) intravenous bolus dose <strong>of</strong><br />
Tir<strong>of</strong>iban upstream in <strong>the</strong> CCU prior to primary<br />
PCI (25μg/kg).<br />
• Group (III): It included 20 patients who received<br />
0.4μg/kg bolus dose Tir<strong>of</strong>iban intracoronary<br />
downstream in <strong>the</strong> ca<strong>the</strong>terization laboratory in<br />
addition to <strong>the</strong> upstream intravenous bolus dose.<br />
All patients were subjected to <strong>the</strong> following:<br />
1- Thorough history taking and <strong>com</strong>plete physical<br />
examination.<br />
2- 12 leads surface ECG.<br />
3- Laboratory investigations, including lipid pr<strong>of</strong>ile,<br />
fasting and post prandial blood sugar, serial<br />
evaluation <strong>of</strong> cardiac enzymes including CK,<br />
CKMB, Troponin levels.<br />
4- Patient preparation by antiplatelets and heparin.<br />
5- Tir<strong>of</strong>iban (R/Aggrastat): Bolus dose according<br />
to <strong>the</strong> patient group.<br />
6- Emergency coronary angiography and coronary<br />
angioplasty <strong>of</strong> <strong>the</strong> infarct related artery (1ry<br />
PCI) to <strong>the</strong> culprit lesion <strong>of</strong> <strong>the</strong> infracted artery<br />
(LAD). TIMI flow and myocardial blush grade<br />
(MBG) will be evaluated.<br />
7- Transthoracic Echocardiography.<br />
8- In-hospital clinical follow-up for MACE.<br />
Patient preparation by antiplatelets:<br />
All patients received 300mg aspirin, 8 tablets<br />
<strong>of</strong> clopidogrel (600mg) and 10.000 iu unfractionated<br />
heparin intravenously in <strong>the</strong> ca<strong>the</strong>terization<br />
laboratory.<br />
Time to treatment:<br />
The door to needle time (time from admission<br />
till administration <strong>of</strong> <strong>the</strong> Tir<strong>of</strong>iban) and <strong>the</strong> door<br />
to balloon time (time from admission till opening<br />
<strong>of</strong> <strong>the</strong> occluded artery by balloon angioplasty) were<br />
calculated.<br />
Tir<strong>of</strong>iban (R/Aggrastat):<br />
The bolus dose was given randomly to <strong>the</strong><br />
patients according to <strong>the</strong> group and all patients<br />
continued on Tir<strong>of</strong>iban in <strong>the</strong> dose <strong>of</strong> 0.15μ/kg/min<br />
137<br />
continuous infusion for 48 hours, in addition to<br />
half dose unfractionated heparin or low molecular<br />
weight heparin.<br />
Primary percutaneous coronary intervention:<br />
By using <strong>the</strong> modified Seldinger technique,<br />
coronary angiography was done by using femoral<br />
artery puncture, and Target Vessel Revascularization<br />
(TVR) was performed by using balloon dilatation<br />
and stenting.<br />
(TIMI) flow grades were observed (TFGs):<br />
Grade 0, no perfusion (no antegrade flow beyond<br />
<strong>the</strong> point <strong>of</strong> occlusion); grade 1, penetration without<br />
perfusion (contrast material passes beyond <strong>the</strong> area<br />
<strong>of</strong> obstruction but fails to opacify <strong>the</strong> entire coronary<br />
bed distal to <strong>the</strong> obstruction for <strong>the</strong> duration<br />
<strong>of</strong> <strong>the</strong> cineangiographic filming sequence); grade<br />
2, partial perfusion (contrast material passes across<br />
<strong>the</strong> obstruction and opacifies <strong>the</strong> coronary artery<br />
distal to <strong>the</strong> obstruction-however, <strong>the</strong> rate <strong>of</strong> entry<br />
<strong>of</strong> contrast material into <strong>the</strong> vessel distal to <strong>the</strong><br />
obstruction or its rate <strong>of</strong> clearance from <strong>the</strong> distal<br />
bed (or both) is slower than its flow into or clearance<br />
from <strong>com</strong>parable areas not perfused by <strong>the</strong><br />
occluded vessel (for example, <strong>the</strong> opposite coronary<br />
artery or <strong>the</strong> coronary bed proximal to <strong>the</strong> obstruction);<br />
and grade 3, <strong>com</strong>plete perfusion (antegrade<br />
flow into <strong>the</strong> bed distal to <strong>the</strong> obstruction occurs<br />
as promptly as antegrade flow into <strong>the</strong> bed proximal<br />
to <strong>the</strong> obstruction, and clearance <strong>of</strong> contrast material<br />
from <strong>the</strong> involved bed is as rapid as clearance from<br />
an uninvolved bed in <strong>the</strong> same vessel or <strong>the</strong> opposite<br />
artery) Successful reperfusion is defined as <strong>the</strong><br />
establishment <strong>of</strong> TIMI grade 3 flow in <strong>the</strong> infarctrelated<br />
artery on <strong>the</strong> final coronary arteriogram<br />
(The TIMI Study Group, 1985).<br />
MBG myocardial blush grade was evaluated<br />
as follows on <strong>the</strong> final left coronary angiogram in<br />
<strong>the</strong> lateral view after reperfusion: 0=no myocardial<br />
blush or contrast density; 1=minimal myocardial<br />
blush or contrast density; 2=moderate myocardial<br />
blush or contrast density, but less than that obtained<br />
during angiography <strong>of</strong> <strong>the</strong> contra-lateral or ipsilateral<br />
non-infarct-related coronary artery; and<br />
3=normal myocardial blush or contrast density,<br />
<strong>com</strong>parable to that obtained during angiography<br />
<strong>of</strong> a contra-lateral or ipsilateral non-infarct-related<br />
coronary artery. When myocardial blush persisted,<br />
this finding will be graded as 0. MBG 2 or 3 will<br />
be defined as good myocardial tissue-level perfusion<br />
(Van’t H<strong>of</strong> et al, 1998).
Comparison between Double Intravenous Bolus, Intracoronary Bolus<br />
No reflow defined as reduction <strong>of</strong> 1 or more in<br />
<strong>the</strong> TIMI grade in <strong>the</strong> final angiogram <strong>com</strong>pared<br />
to <strong>the</strong> post PTCA angiogram or patients with TIMI<br />
3 flow and low TIMI myocardial perfusion grade<br />
(0-1) was observed (Piana et al, 1994).<br />
Transthoracic echocardiography:<br />
Echocardiographic examination was done for<br />
all patients using a 2.5MHz mechanical transducer<br />
mounted in a Vingmed CFM-800 machine (HP in<br />
specialized hospital) with <strong>the</strong> patient in <strong>the</strong> left<br />
lateral position from multiple windows. The followings<br />
were measured:<br />
1- Ejection fraction (EF).<br />
2- LV dimensions.<br />
3- Segmental wall motion abnormalities.<br />
4- Complications <strong>of</strong> acute MI such as ventricular<br />
septal rupture (VSR), acute mitral regurgitation<br />
(MR), aneurysms, LV thrombus….etc.<br />
In-hospital course:<br />
All patients were followed-up during <strong>the</strong>ir<br />
hospital stay for development <strong>of</strong> any major adverse<br />
cardiovascular event (MACE) such as death, recurrent<br />
ischemia, and target vessel revascularization<br />
(TVR). Also <strong>the</strong>y were followed-up for development<br />
major bleeding, minor bleeding and puncture<br />
site bleeding.<br />
Data management:<br />
Data were collected, revised and <strong>the</strong>n edited<br />
on <strong>the</strong> P.C. The data were <strong>the</strong>n analyzed statistically<br />
by using SPSS statistical package version (12).<br />
The following tests were used:<br />
• X = Mean.<br />
• SD = Standard deviation.<br />
• t test for independent samples.<br />
• ANOVA= Analysis <strong>of</strong> variance.<br />
• X 2 = Chi square test.<br />
• Post Hoc test.<br />
• p value >0.05 = Non-significant (NS). p value<br />
0.05).
Ahmed I Nassar, et al<br />
Time to treatment:<br />
The mean and SD <strong>of</strong> door to needle time in<br />
group I was 26.35±4.81, in group II was 27.25min<br />
±8.34 and in group III was 28.25min ±7.99 and it<br />
was statistically not significant between <strong>the</strong> study<br />
groups (p>0.05). The mean and SD <strong>of</strong> door to<br />
balloon time in group I was 84.20min ±8.44, in<br />
group II was 86.65min ±21.34 and in group III<br />
was 86.85min ±15.61, and it was statistically not<br />
significant between <strong>the</strong> study groups (p>0.05).<br />
Coronary angiographic data: Post PCI TIMI<br />
flow assessment revealed achievement <strong>of</strong> TIMI III<br />
flow in 90% <strong>of</strong> group II, and 70% <strong>of</strong> patients in<br />
group I and group III. TIMI II was present in 20%<br />
<strong>of</strong> group I, 10% <strong>of</strong> group II, and 15% <strong>of</strong> group III.<br />
TIMI I was present in 10% <strong>of</strong> patients in group I<br />
and group III, while TIMI 0 was present in only<br />
5% <strong>of</strong> group III patients.<br />
PTCA and stenting: PTCA and stenting was<br />
done for all patients in group I, and all patients in<br />
group II except one patient who had recanalized<br />
LAD. Whereas in group III, PTCA was done for<br />
all patients but only 18 patients underwent stenting<br />
as PTCA only was angiographically satisfactory<br />
in <strong>the</strong> remaining 2 patients. All stents were bare<br />
metal stents. PTCA and stenting were statistically<br />
non-significant among <strong>the</strong> study groups (p>0.05).<br />
No reflow phenomenon: No reflow phenomenon<br />
was present in 25% <strong>of</strong> patients in group I, 15%<br />
<strong>of</strong> patients in group III and although <strong>the</strong>re was not<br />
any patient who developed no reflow in group II<br />
but it was non-significant statistically (p>0.05).<br />
Myocardial perfursion: Myocardial perfusion<br />
was assessed by using myocardial blush grading<br />
(MBG) and it revealed that MBG 0 was present in<br />
20% <strong>of</strong> group I patients and 30% <strong>of</strong> group III<br />
patients while <strong>the</strong>re was no MBG 0 among group<br />
II. MBG I was present in 30% <strong>of</strong> group I patients,<br />
15% <strong>of</strong> group II patients and 20% <strong>of</strong> group III<br />
patients. MBG II was present in 30% <strong>of</strong> group I<br />
patients, 15% <strong>of</strong> group II patients and 20% <strong>of</strong><br />
group III patients. MBG III was present in 20% <strong>of</strong><br />
group I patients, 70% and 30% <strong>of</strong> group III patients<br />
while most <strong>of</strong> patients in group II had MBG III<br />
(70%). There was significant difference value<br />
between <strong>the</strong> study groups regarding <strong>the</strong> MBG<br />
(p0.05).<br />
Minor bleeding: Three patients (15%) in group<br />
I developed minor bleeding, two patients (10%)<br />
in group III developed minor bleeding and no any<br />
patient in group II developed minor bleeding.<br />
Minor bleeding was statistically non-significant<br />
in-between groups (p>0.05).<br />
Post PCI TIMI flow: Assessment revealed<br />
achievement <strong>of</strong> TIMI III flow in 90% <strong>of</strong> group II,<br />
and 70% <strong>of</strong> patients in group I and group III. TIMI<br />
II was present in 20% <strong>of</strong> group I, 10% <strong>of</strong> group II,<br />
and 15% <strong>of</strong> group III. TIMI I was present in 10%<br />
<strong>of</strong> patients in group I and group III, while TIMI 0<br />
was present in only 5% <strong>of</strong> group III patients.<br />
Although TIMI III flow post PCI was more prevalent<br />
in group II in <strong>com</strong>parison to groups I and III<br />
but it was statistically non-significant (p>0.05).<br />
No reflow phenomenon:<br />
No reflow phenomenon was present in 25% <strong>of</strong><br />
patients in group I, 15% <strong>of</strong> patients in group III<br />
and although <strong>the</strong>re was not any patient who developed<br />
no reflow in group II.<br />
Conclusion<br />
In patients presented with acute anterior STEMI<br />
and treated with primary PCI, <strong>the</strong> high bolus dose<br />
tir<strong>of</strong>iban given intravenously upstream prior to
Comparison between Double Intravenous Bolus, Intracoronary Bolus<br />
PCI seems to be a safe and effective regimen to<br />
improve <strong>the</strong> angiographic and clinical out<strong>com</strong>es<br />
in <strong>com</strong>parison to <strong>the</strong> conventional bolus dose<br />
regimen and <strong>the</strong> intracoronary bolus dose regimen,<br />
without increasing <strong>the</strong> risk <strong>of</strong> bleeding.<br />
This effect could be explained by <strong>the</strong> early<br />
reach <strong>of</strong> high drug concentration in <strong>the</strong> blood and<br />
subsequently early higher degree <strong>of</strong> inhibition <strong>of</strong><br />
platelet aggregation.<br />
References<br />
1- Alpert JS, Thygesen K, Antman E, et al: Myocardial<br />
infarction redefined a consensus document <strong>of</strong> <strong>the</strong> Joint<br />
European Society <strong>of</strong> Cardiology/American College <strong>of</strong><br />
Cardiology Committee for <strong>the</strong> redefinition <strong>of</strong> myocardial<br />
infarction. J Am Coll Cardiol 2000; 36: 959-969.<br />
2- Antoniucci D, Rodriguez A, Hempel A, et al: A randomized<br />
trial <strong>com</strong>paring primary infarct artery stenting with or<br />
without abciximab in acute myocardial infarction. J Am<br />
Coll Cardiol 2003; 42: 1879-1885.<br />
3- De Luca G, Smit JJ, Ernst N, et al: Impact <strong>of</strong> adjunctive<br />
tir<strong>of</strong>iban administration on myocardial perfusion and<br />
mortality in patients undergoing primary angioplasty for<br />
140<br />
ST-segment elevation myocardial infarction. Thromb<br />
Haemost 2005; 93: 820-823.<br />
4- Goto S, Tamura N, Li M, et al: Different effects <strong>of</strong> various<br />
anti-GPIIb-IIIa agents on shear-induced platelet activation<br />
and expression <strong>of</strong> procoagulant activity. J Thrombosis<br />
Haemostasis 2003; 1: 2022-2030.<br />
5- Gunasekara AP, Walters DL, Aroney CN: Comparison <strong>of</strong><br />
abciximab with "high-dose" tir<strong>of</strong>iban in patients undergoing<br />
percutaneous coronary intervention. Int J Cardiol<br />
2006; Apr 28, 109 (1): 16-20.<br />
6- Piana RN, Paik GY, Moscucci M, et al: Incidence and<br />
treatment <strong>of</strong> ''no-reflow'' after percutaneous coronary<br />
intervention. Circulation 1994; 89: 2514-8.<br />
7- The TIMI Study Group: Thrombolysis in myocardial<br />
infarction (TIMI) trial. N Engl J Med 1985; 312: 932-6.<br />
8- van’t H<strong>of</strong> AW, Ernst NM, de Boer MJ, et al: On-TIME<br />
study group: Facilitaiton <strong>of</strong> primary 2480 Editorial coronary<br />
angioplasty by early start <strong>of</strong> a glycoprotein 2b/3a<br />
inhibitor: Results <strong>of</strong> <strong>the</strong> ongoing tir<strong>of</strong>iban in myocardial<br />
infarction evaluation (On-TIME) trial. Eur Heart J 2004;<br />
25: 837-846.<br />
9- Zijlstra F, Hoorntje JCA, de Boer M-J, et al: Long-term<br />
benefit <strong>of</strong> primary angioplasty as <strong>com</strong>pared with thrombolytic<br />
<strong>the</strong>rapy for acute myocardial infarction. N Engl<br />
J Med 1999; 341: 1413-1419.
Egypt Heart J 62 (1): 141-145, March 2010<br />
Safety and Feasibility <strong>of</strong> Transradial Versus Transfemoral Approach for<br />
Diagnostic Coronary Angiography During Early Phase <strong>of</strong><br />
<strong>the</strong> Learning Curve<br />
MAHMOUD M SABBAH, MBBCh; MOHAMED A ORABY, MD;<br />
GAMELA M NASR, MD; AHMED A EL HAWARY, MD<br />
Background: The radial approach has been increasingly used as an alternative to femoral access as it improves patients’<br />
<strong>com</strong>fort and permits earlier ambulation and discharge. Our aim was to assess <strong>the</strong> feasibility, and safety <strong>of</strong> transradial approach<br />
(TRA) versus transfemoral approach (TFA) for diagnostic coronary angiography, during early phase <strong>of</strong> <strong>the</strong> learning curve.<br />
Methods: This is a prospective single-centre <strong>com</strong>parative study carried out at <strong>the</strong> ca<strong>the</strong>terization laboratory at Suez Canal<br />
University hospital. We enrolled 203 consecutive patients referred to our centre for diagnostic coronary angiography. Patients<br />
were divided into TRA or TFA groups. We <strong>com</strong>pared <strong>the</strong> two groups regarding access/procedure success and time, fluoroscopy<br />
time, contrast volume, length <strong>of</strong> hospital stay and <strong>com</strong>plications. All studies were performed by only 3 angiographers.<br />
Results: There was no significant difference in access success between <strong>the</strong> two groups. However, TFA was associated with<br />
significantly higher procedure success than TRA (96.7% versus 76.7% respectively, p-value=0.002). TRA was more time<br />
consuming than transfemoral one (23.2±8.4min. versus 19.4±5.9min. respectively, p-value=0.007). Compared with TFA group,<br />
TRA had a significantly longer X-ray exposure time (8.9±2.27min. versus 7.1±1.6min. respectively, p-value=0.002) and associated<br />
with larger amount <strong>of</strong> contrast (148.04±23.1ml. versus 132.4±22.7ml. respectively, p-value=0.001). Total length <strong>of</strong> hospital<br />
stay was significantly shorter in <strong>the</strong> TRA group than in TFA (5.1±1.2 hour Vs 8.9±1.5 hour respectively. p=0.0001). TFA had<br />
higher access site haematoma while arterial spasm was encountered only with TRA.<br />
Conclusions: Compared with transfemoral approach, transradial approach for coronary angiography is a safe and feasible<br />
alternative that is associated with lower local vascular <strong>com</strong>plication rates and shorter hospital stay. However, transradial approach<br />
is associated with some technical difficulties at <strong>the</strong> early phase <strong>of</strong> <strong>the</strong> learning curve that may improve with accumulating<br />
experience.<br />
Key Words: Transradial access – Transfemoral access – Coronary angiography.<br />
Introduction<br />
For <strong>the</strong> last 2 decades, femoral access has been<br />
<strong>the</strong> dominant access site for coronary angiography<br />
[1]. Then transradial access emerged as an excellent<br />
alternative to femoral access as this artery has a<br />
superficial course with no nerves or veins <strong>of</strong> significant<br />
size near <strong>the</strong> usual site <strong>of</strong> puncture [2].<br />
Moreover transradial access is associated with less<br />
The Department <strong>of</strong> Cardiology, Faculty <strong>of</strong> Medicine,<br />
Suez Canal University.<br />
Manuscript received 28 Nov., 2009; revised 20 Dec., 2009;<br />
accepted 21 Dec., 2009.<br />
Address for Correspondence: Dr. Mohamed A Oraby,<br />
Cardiology Department, Suez Canal University Hospital,<br />
Ismailia, Egypt, Email: maoraby@yahoo.<strong>com</strong><br />
141<br />
access site <strong>com</strong>plications (local ischemia, large<br />
haematoma, minor or major hemorrhagic <strong>com</strong>plications)<br />
[3]. Also in transradial access, post procedural<br />
bed rest is not required, permitting immediate<br />
ambulation, more <strong>com</strong>fort and early discharge [2,3].<br />
This last advantage has shown to improve quality<br />
<strong>of</strong> life for patients 4 and to reduce <strong>the</strong> costs <strong>of</strong><br />
hospitalization in <strong>com</strong>parison to transfemoral access<br />
[4,5]. Many interventional cardiologists perceive<br />
that <strong>the</strong> decrease in minor vascular <strong>com</strong>plications<br />
with radial access3 is balanced by technical difficulties<br />
and increased radiation exposure required<br />
for radial access [5,6].<br />
So, our study was designed to <strong>com</strong>pare <strong>the</strong><br />
feasibility and safety <strong>of</strong> transradial versus transfemoral<br />
approaches for diagnostic coronary angiog-
Safety & Feasibility <strong>of</strong> Transradial Versus Transfemoral Approach<br />
raphy and to describe <strong>the</strong> <strong>com</strong>plications and difficulties<br />
associated with <strong>the</strong> transradial approach<br />
during <strong>the</strong> early phase <strong>of</strong> learning curve.<br />
Subjects and Methods<br />
This was a <strong>com</strong>parative study between <strong>the</strong> TRA<br />
and TFA approaches in patients undergoing first<br />
time diagnostic coronary angiography in Suez<br />
Canal University hospital cardiac ca<strong>the</strong>terization<br />
laboratory during <strong>the</strong> period from January 2008,<br />
to January 2009.<br />
Allen's test 7 was performed in all patients and<br />
patients with abnormal test were excluded from<br />
<strong>the</strong> study. Patients were <strong>the</strong>n sequentially randomized<br />
to ei<strong>the</strong>r TRA or TFA and all patients had <strong>the</strong><br />
same probability to be included in ei<strong>the</strong>r group.<br />
Five minutes before each procedure, <strong>the</strong> patients<br />
were premedicated with intravenous 2-4mg midazolam<br />
for sedation.<br />
Angiographic procedures:<br />
TRA was started with <strong>the</strong> patient lying down<br />
with <strong>the</strong> right wrist placed in a hyperextended<br />
position. After local anes<strong>the</strong>sia with 1ml lidocaine,<br />
<strong>the</strong> radial artery was punctured using a 3.8cm<br />
arterial needle. Then, a 6Fr (8.5cm in length)<br />
introducer sheath was advanced over a 0.025 inch<br />
straight guidewire. To reduce spasm and dis<strong>com</strong>fort,<br />
a drug ''cocktail'' containing 200μg <strong>of</strong> nitroglycerine,<br />
and 2.5mg <strong>of</strong> verapamil (unless <strong>the</strong> patient<br />
had bradycardia or heart failure) and 5000 IU <strong>of</strong><br />
heparin were administered through <strong>the</strong> sheath side<br />
arm. Standard left and right Judkins ca<strong>the</strong>ters were<br />
introduced over a 0.035 inch (150cm) guidewire.<br />
The sheath was removed immediately after <strong>the</strong><br />
procedure and an elastic band was used to secure<br />
bleeding. The patients were asked to stay for two<br />
hours, during which access site was frequently<br />
checked and patients were discharged if <strong>the</strong>re was<br />
no <strong>com</strong>plications [1,5,8].<br />
Transfemoral ca<strong>the</strong>terization using standard<br />
Seldinger technique was performed and coronary<br />
arterial cannulation was performed using 6Fr diagnostic<br />
Judkins ca<strong>the</strong>ters. After <strong>the</strong> procedure,<br />
<strong>the</strong> 6Fr sheath was removed immediately and homeostasis<br />
was achieved by digital pressure on <strong>the</strong><br />
access site for 10 minutes. Patients were asked to<br />
stay for six hours after <strong>the</strong> procedure and <strong>the</strong> access<br />
site was checked frequently. Patients were discharged<br />
if no <strong>com</strong>plication occurred [1,5,8].<br />
All <strong>the</strong> studies had been performed by 3 interventional<br />
cardiologists who had a limited experi-<br />
142<br />
ence in performing transradial procedures and<br />
under <strong>the</strong> supervision <strong>of</strong> a highly experienced<br />
interventional cardiologist in doing this procedure.<br />
Study endpoints:<br />
Both approaches were <strong>com</strong>pared for <strong>the</strong> following<br />
endpoints: Access and procedure success rates,<br />
access and procedure times, fluoroscopy time,<br />
contrast volume, procedure-related <strong>com</strong>plications,<br />
and post-procedural hospital stay. Access time<br />
was defined as <strong>the</strong> interval between local anes<strong>the</strong>tic<br />
injection and sheath introduction, and procedural<br />
time was defined as <strong>the</strong> interval between local<br />
anes<strong>the</strong>tic injection and <strong>com</strong>pletion <strong>of</strong> coronary<br />
angiography.<br />
Statistics:<br />
Analysis <strong>of</strong> <strong>the</strong> results was performed using<br />
<strong>the</strong> Statistical Package for Social Sciences, version<br />
15.0 s<strong>of</strong>tware for Windows. Continuous variables<br />
were expressed as mean ± standard deviation, and<br />
categorical variables as percentages. Continuous<br />
variables <strong>of</strong> normal and non-normal distribution<br />
were <strong>com</strong>pared with an independent t-test. Categorical<br />
variables were assessed using <strong>the</strong> chisquare<br />
test. Statistical significance was defined as<br />
a p value <strong>of</strong> less than 0.05.<br />
Results<br />
Our study included 203 patients, 57.5% <strong>of</strong> <strong>the</strong>m<br />
were males with mean age 53.5±9.7 years (Table<br />
1), 101 patients had coronary angiography through<br />
<strong>the</strong> radial approach (TRA group) and <strong>the</strong> o<strong>the</strong>r 102<br />
had angiography performed through <strong>the</strong> femoral<br />
approach (TFA group). Hypertension was <strong>the</strong> most<br />
prevalent risk factor (68.3%) and 50% <strong>of</strong> our<br />
patients were currently smokers (Fig. 1). Access<br />
success was achieved in 98.34% <strong>of</strong> <strong>the</strong> patients in<br />
<strong>the</strong> femoral group versus 93.3% in radial group<br />
(p-value=0.1). Procedure success was significantly<br />
higher In TFA than in TRA (96.7% versus 76.7%<br />
respectively, p-value=0.002) (Fig. 2).<br />
Procedure time was significantly shorter with<br />
femoral access than with radial access (19.4±<br />
5.9min. versus 23.2±8.4min., p-value=0.007). Patients<br />
with transradial approach had also longer<br />
X-ray exposure time than patients in TFA (8.9±<br />
2.27min. versus 7.1±1.6min., p-value=0.002) and<br />
received larger amount <strong>of</strong> contrast material (148.04<br />
±23.1ml. versus 132.4±22.7ml. p-value=0.001)<br />
(Table 2). Regarding procedure related <strong>com</strong>plications,<br />
arterial spasm was encountered only in patients<br />
with transradial approach (26.1%). There
Mahmoud M Sabbah, et al<br />
was a higher rate <strong>of</strong> access site haematoma in TFA<br />
group (32.8% Versus 2.2%, p=0.002) (Table 4).<br />
TRA was associated with significantly shorter post<br />
procedural hospital than TFA (5.1±1.2 versus<br />
8.9±1.5 hours. p=0.0001).<br />
The number <strong>of</strong> ca<strong>the</strong>ters used for engagement<br />
<strong>of</strong> <strong>the</strong> right and left coronary arteries did not vary<br />
significantly between <strong>the</strong> two groups. The most<br />
frequently used ca<strong>the</strong>ter for cannulation <strong>of</strong> RCA<br />
in TRA group was JR 3.5 (71.7%) while <strong>the</strong> most<br />
<strong>com</strong>monly used ca<strong>the</strong>ter for cannulation <strong>of</strong> RCA<br />
in TFA group was JR 4 (86.2%). For <strong>the</strong> left coronary<br />
system, JL 3.5 ca<strong>the</strong>ter was <strong>the</strong> most frequently<br />
used in TRA group (67.4%) while JL 4 was <strong>the</strong><br />
most frequently used in TFA group (87.9%).<br />
Regarding <strong>com</strong>parison between both Lt and Rt<br />
radial approaches, left radial artery was accessed<br />
more frequently than <strong>the</strong> right one according to<br />
<strong>the</strong> operator preference. There was no significant<br />
difference between <strong>the</strong> two sides regarding procedure<br />
success (92.9% versus 93.5% in Rt and Lt<br />
radial artery respectively). Despite a smaller number<br />
patients in <strong>the</strong> Rt radial group; access time, procedure<br />
time, fluoroscopy time and contrast volume<br />
were similar between <strong>the</strong> two sides (Table 5).<br />
Table 1: Baseline characteristics <strong>of</strong> <strong>the</strong> study population.<br />
Sex:<br />
Male<br />
Female<br />
Age:<br />
Mean ± SD<br />
Range<br />
Height (cm):<br />
Mean ± SD<br />
Weight (Kg):<br />
Mean ± SD<br />
BMI (Kg/m 2 ):<br />
Mean ± SD<br />
Radial access<br />
(n=60)<br />
51.7%<br />
48.3%<br />
51.9±8.1<br />
[30-74]<br />
171.2±11.3<br />
85.3±9.8<br />
27.5± 2.8<br />
Femoral access<br />
(n=60)<br />
63.3%<br />
36.7%<br />
54.7±10.3<br />
[31-76]<br />
168.9±6.1<br />
86.9±12.3<br />
28.6±3.9<br />
*Statistically significant difference (p-value
Safety & Feasibility <strong>of</strong> Transradial Versus Transfemoral Approach<br />
%<br />
100<br />
90<br />
80<br />
70<br />
60<br />
50<br />
40<br />
30<br />
20<br />
10<br />
0<br />
p-value=0.1 p-value=0.002<br />
93.3 100<br />
Access success<br />
Figure 2: Procedure and access success/failure among <strong>the</strong><br />
studied Population.<br />
Discussion<br />
This study was designed to assess feasibility<br />
and safety <strong>of</strong> transradial versus transfemoral approaches<br />
to diagnostic coronary angiography in<br />
our center during <strong>the</strong> early phase <strong>of</strong> <strong>the</strong> learning<br />
curve. We showed no significant difference in <strong>the</strong><br />
access success between ei<strong>the</strong>r groups (i.e. TRA<br />
and TFA), and this was matched with <strong>the</strong> results<br />
<strong>of</strong> Fernández et al [9] and Labrunie et al [5]. We<br />
found also that TRA was associated with more<br />
procedure failure (23.3%) than TFA (3.3%).<br />
A systemic review (including 14 randomized<br />
studies published up to 2004) by Agostoni et al<br />
[1], reported a failure rate with TRA <strong>of</strong> 7.2%, and<br />
<strong>the</strong>y refer to <strong>the</strong> lack <strong>of</strong> adequate previous learning<br />
curve as <strong>the</strong> major cause <strong>of</strong> <strong>the</strong> failure <strong>of</strong> this<br />
procedure. More recent studies reported success<br />
rates higher than 97%, <strong>com</strong>parable to those<br />
achieved with TFA [6,9,10]. The lower TRA success<br />
rate in our study <strong>com</strong>pared with o<strong>the</strong>rs could be<br />
attributed to <strong>the</strong> lower experience and familiarity<br />
<strong>of</strong> our operators with this technique as <strong>the</strong>y were<br />
still in <strong>the</strong> early phase <strong>of</strong> <strong>the</strong> learning curve, also<br />
deficiency <strong>of</strong> well settled transradial programme<br />
and dedicated materials could play a role in increasing<br />
failure rate. Labrunie et al [5] showed that<br />
<strong>the</strong> most important improvement in TRA was related<br />
to operator skill. In fact, <strong>the</strong>re is clear evidence<br />
in all <strong>the</strong> examined trials that a learning curve is<br />
essential for this technique [11].<br />
The causes <strong>of</strong> procedure failure in TRA group<br />
in our study included: Access failure, severe radial<br />
77<br />
96.7<br />
Procedure success<br />
Radial access Femoral access<br />
144<br />
arterial spasm (that occurs before or during coronary<br />
procedures) and failed cannulation <strong>of</strong> <strong>the</strong><br />
coronary arteries. Both Hildick-Smith et al [12]<br />
and Amoroso et al [13] reported similar causes for<br />
<strong>the</strong> failure <strong>of</strong> TRA. In our study <strong>the</strong> failed transradial<br />
cases were crossed over to alternate arterial<br />
access according to operator preference.<br />
In our study TRA was more time consuming<br />
and associated with longer X-ray exposure than<br />
TFA. Similarly, larger amount <strong>of</strong> contrast material<br />
was used in TRA than in TFA. Similar findings<br />
were reported by, Louvard et al [14], Lange et al<br />
[15] and Hildick-Smith et al [16]. They attributed<br />
<strong>the</strong>se findings to <strong>the</strong> technical difficulties related<br />
to this technique during <strong>the</strong> early phase <strong>of</strong> <strong>the</strong><br />
learning curve and assured that when <strong>the</strong> right<br />
skills are grasped, <strong>the</strong> technique be<strong>com</strong>e much<br />
easier and reliable and take less time and dye.<br />
We showed also that patients with TRA had<br />
significantly shorter post-procedural hospital stay<br />
<strong>com</strong>pared to patients with TFA. O<strong>the</strong>r investigators<br />
[4,10,13] reported <strong>the</strong> same observation and concluded<br />
that TRA leads to favorable post-procedural<br />
quality <strong>of</strong> life, presumably due to <strong>the</strong> near absence<br />
<strong>of</strong> required bed rest and <strong>the</strong> rapid return to a normal<br />
level <strong>of</strong> functioning.<br />
Arterial spasm was <strong>the</strong> most <strong>com</strong>monly encountered<br />
<strong>com</strong>plication with TRA as it occurred in one<br />
every four procedures and attributed to procedure<br />
failure in <strong>the</strong> majority <strong>of</strong> cases. This was supported<br />
by <strong>the</strong> findings <strong>of</strong> Coppola et al [17] and Saito et<br />
al [18], both showed that, even in centers having<br />
an extensive experience with <strong>the</strong> radial access,<br />
radial spasm occurs in 15% to 30% <strong>of</strong> <strong>the</strong> procedures<br />
and suggested more effective sedation, intraarterial<br />
vasodilator cocktails and smaller ca<strong>the</strong>ters,<br />
as means to over<strong>com</strong>e this phenomenon. On <strong>the</strong><br />
o<strong>the</strong>r hand, access site haematoma was <strong>the</strong> main<br />
<strong>com</strong>plication <strong>of</strong> TFA as it occurred in more than<br />
one fourth <strong>of</strong> <strong>the</strong> procedures and more <strong>com</strong>monly<br />
encountered in obese and female patients.<br />
Comparing Rt. and Lt. Radial approaches, <strong>the</strong>re<br />
was no significant difference regarding procedure<br />
success, access time, procedure time, and fluoroscopy<br />
time and contrast volume. There was also no<br />
significant difference in procedure related <strong>com</strong>plications<br />
or in length <strong>of</strong> hospital stay between <strong>the</strong><br />
two sides. Bodi et al [19] reported similar findings,<br />
while Wu et al [20] pointed out that passage through<br />
<strong>the</strong> right <strong>com</strong>mon brachiocephalic trunk, primarily<br />
in elderly patients, could generate difficulties for
Mahmoud M Sabbah, et al<br />
right transradial ca<strong>the</strong>terization. So <strong>the</strong> Left transradial<br />
ca<strong>the</strong>terization <strong>of</strong>fers <strong>the</strong> <strong>the</strong>oretical advantage<br />
<strong>of</strong> avoiding this passage and permitting a more<br />
direct access to ascending aorta [20]. These differences<br />
have been reflected in clinical terms in certain<br />
studies such as those <strong>of</strong> Kawashima et al [21] in<br />
which <strong>the</strong> left transradial ca<strong>the</strong>terization shortened<br />
<strong>the</strong> procedure and <strong>the</strong> examination time. Fernández<br />
et al [22] reported that <strong>the</strong> right transradial ca<strong>the</strong>terization<br />
was associated with a higher failure rate<br />
due to problems with <strong>the</strong> tortuosity and a<strong>the</strong>rosclerosis<br />
<strong>of</strong> <strong>the</strong> right <strong>com</strong>mon brachiocephalic trunk.<br />
Conclusion<br />
Compared with transfemoral approach, transradial<br />
approach for coronary angiography is a safe<br />
and feasible alternative that is associated with<br />
lower local vascular <strong>com</strong>plication rates and shorter<br />
hospital stay. However, TRA is associated with<br />
some technical difficulties at <strong>the</strong> early phase <strong>of</strong><br />
<strong>the</strong> learning curve that may improve with accumulating<br />
experience.<br />
References<br />
1- Agostoni P, Biondi-Zoccai GG, Benedictis ML, et al:<br />
Radial versus femoral approach for percutaneous diagnostic<br />
and interventional procedures: Systemic overview<br />
and meta-analysis <strong>of</strong> randomized trials. J Am Coll Cardiol<br />
2004; 44: 349-356.<br />
2- Campeau L: Percutaneous radial artery approach for<br />
coronary angiography. Ca<strong>the</strong>t Cardiovasc Diagn 1989;<br />
16: 3-72.<br />
3- Jolly S, Amlani S, Hamon, M, et al: Radial versus femoral<br />
access for coronary angiography or intervention and <strong>the</strong><br />
impact on major bleeding and ischemic events: A systematic<br />
review and meta-analysis <strong>of</strong> randomized trials. American<br />
Heart Journal 2008; 12: 2-9.<br />
4- Cooper CJ, El-Shiekh RA, Cohen DJ: Effect <strong>of</strong> transradial<br />
access on quality <strong>of</strong> life and cost <strong>of</strong> cardiac ca<strong>the</strong>terization:<br />
A randomized <strong>com</strong>parison. Am Heart J 1999; 138: 430-<br />
436.<br />
5- Labrunie A, Silveira W, Contero L: Transradial approach<br />
to coronary angiography: The reality <strong>of</strong> <strong>the</strong> learning curve<br />
evaluated in a <strong>com</strong>parative, randomized, multicenter<br />
study. Am J Cardiol 2001; 88 (Suppl 5A): 111G.<br />
6- Yoo BS, Lee SH, Ko JY, et al: Procedural out<strong>com</strong>es <strong>of</strong><br />
repeated transradial coronary procedure. Ca<strong>the</strong>ter Cardiovasc<br />
Interv 2003; 58: 301-4.<br />
7- Barbeau GR, Arsenault F, Dugas L, Simard S, Lariviere<br />
MM: Evaluation <strong>of</strong> <strong>the</strong> ulnopalmar arterial arches with<br />
pulse oximetry and plethysmography: Comparison with<br />
<strong>the</strong> Allen’s test in 1010 patients; American Heart Journal<br />
March 2004; 147: 489-93.<br />
8- Louvard Y, Pezzano M, Scheers L: Coronary angiography<br />
by a radial artery approach: Feasability, learning curves:<br />
145<br />
One operator’s experience. Arch Mal Coeur Vaiss 1998;<br />
91: 209-215.<br />
9- Fernández JS, Santos RC, Rodríguez JMV, et al: Transradial<br />
Approach to Coronary Angiography and Angioplasty:<br />
Initial Experience and Learning Curve. Rev Esp Cardiol<br />
2003; 56 (2): 152-9.<br />
10- Veli Vefalı, Uˇ gur Arslan: Our experience with transradial<br />
approaches for coronary angiography. Arch Turk Soc<br />
Cardiol 2008; 36 (3): 163-167.<br />
11- Kiemeneij F, Vajifdar BU, Eccleshall SC, et al: Evaluation<br />
<strong>of</strong> a spasmolytic cocktail to prevent radial artery spasm<br />
during coro-nary procedures. Ca<strong>the</strong>ter Cardi-Ovasc Interv<br />
2003; 58 (3): 281-4.<br />
12- Hildick-Smith DJR, Lowe MD, Walsh JT, et al: Coronary<br />
angiography from <strong>the</strong> radial artery-experience, <strong>com</strong>plications<br />
and limitations. Int J Cardiol 1998 May 15; 64 (3):<br />
231-9.<br />
13- Amoroso G, Sarti M, Bellucci R, et al: Clinical and<br />
procedural predictors <strong>of</strong> nurse workload during and after<br />
invasive coronary procedures: The potential benefit <strong>of</strong> a<br />
systematic radial access. Eur J Cardiovasc Nurs 2005; 4:<br />
234-241.<br />
14- Louvard Y, Lefevre T, Allain A, Morice MC: Coronary<br />
angiography through <strong>the</strong> radial or <strong>the</strong> femoral approach:<br />
The CARAFE study. Ca<strong>the</strong>t Cardiovasc Intervent 2001;<br />
52: 181-7.<br />
15- Lange HW, von Boetticher H: Randomized <strong>com</strong>parison<br />
<strong>of</strong> operator radiation exposure during coronary angiography<br />
and intervention by radial or femoral approach.<br />
Ca<strong>the</strong>ter Cardiovasc Interv 2006; 67 (1): 12-6.<br />
16- Hildick-Smith DJ, Walsh JT, Lowe MD, Shapiro LM,<br />
Petch MC: Transradial coronary angiography in patients<br />
with contraindications to <strong>the</strong> femoral approach. Ca<strong>the</strong>ter<br />
Cardiovasc Interv 2004; 61: 60-6.<br />
17- Coppola J, Patel T, Kwan T, et al: Nitroglycerin, nitroprusside,<br />
or both, in preventing radial artery spasm during<br />
transradial artery ca<strong>the</strong>terization. J Invasive Cardiol 2006<br />
Apr; 18 (4): 155-8.<br />
18- Saito S, Tanaka S, Hiroe Y, et al: Usefulness <strong>of</strong> hydrophilic<br />
coating on arterial sheath introducer in trans-radial coronary<br />
intervention. Ca<strong>the</strong>ter Cardiovasc Interv 2002 Jul;<br />
56 (3): 328-32.<br />
19- Bodi V, Sanchis J, Nunez J, et al: Left radial approach in<br />
daily practice. Results <strong>of</strong> a randomized study <strong>com</strong>paring<br />
femoral, right and left radial approaches. JACC Cardiovasc<br />
Intervent 2008; 1 [2 (Supplement B)]: B94.<br />
20- Wu Ch-J, Lo P-H, Chang K-Ch, Fu M, Lau K-W, Hung<br />
J-S: Transradial coronary angiography and angioplasty<br />
in Chinese patients. Ca<strong>the</strong>ter Cardiovasc Diagn 1997, 40:<br />
159-63.<br />
21- Kawashima O, Endoh N, Terashima M, Ito Y, Abe S,<br />
Ootomo T, et al: Effectiveness <strong>of</strong> right or left radial<br />
approach for coronary angiography. Ca<strong>the</strong>ter Cardiovasc<br />
Interv 2004; 61: 333-7.<br />
22- Fernández-Portales J, Valdesuso R, Carreras R, Jiménez-<br />
Candil J, Serrador A, Romaní S: Vía radial derecha o<br />
izquierda en la coronariografía. Importancia en la curva<br />
de aprendizaje. Rev Esp Cardiol 2006; 59: 1071-4.
Egypt Heart J 62 (1): 147-154, March 2010<br />
Correlation between Clinical Presentation, ECG and<br />
Echocardio-Graphic Findings and Those <strong>of</strong> Angiography in Patients<br />
Undergoing Coronary Angiography<br />
FATHI A MAKLADY, MD,FRCP; HANAN M KAMAL, MD; AZZA Z EL-ERAKY, MD;<br />
OMAR M SALEH, MBBCh<br />
Background: Coronary artery disease (CAD) is <strong>the</strong> most important among cardiovascu-lar diseases, both CAD mortality<br />
and <strong>the</strong> prevalence <strong>of</strong> risk factors continue to rise rap-idly in developing countries. The cardinal symptom <strong>of</strong> patients with CAD<br />
is chest pain that initiates clinical evaluation. The 12-lead ECG and <strong>the</strong> echocardiography are <strong>the</strong> core to <strong>the</strong> diagnostic and<br />
triage pathway for ACS and provides important prognostic infor-mation. Coronary angiography (CA) remains <strong>the</strong> standard for<br />
identifying <strong>the</strong> presence or absence <strong>of</strong> a<strong>the</strong>rosclerotic CAD it helps to delineate coronary anatomy for determining <strong>the</strong> appropriate<br />
<strong>the</strong>rapy in patients with ischemic CAD.<br />
Aim <strong>of</strong> <strong>the</strong> Work: To correlate <strong>the</strong> risk factors, <strong>the</strong> <strong>com</strong>plaint, <strong>the</strong> ECG and <strong>the</strong> echocar-diographic findings with those <strong>of</strong><br />
<strong>the</strong> coronary angiography.<br />
Subjects and Methods: A total <strong>of</strong> 150 patients who were referred electively to <strong>the</strong> CA procedure. All <strong>of</strong> <strong>the</strong>m were subjected<br />
to a thorough clinical assessment using Rose questionnaire and Framingham risk score, ECG and echocardiography.<br />
Results: The results showed that <strong>the</strong> proportion <strong>of</strong> males was found to be more than fe-males (66% and 44% respectively.<br />
(The ECG findings showed that 40% <strong>of</strong> patients with normal coronaries had ECG changes indicative <strong>of</strong> ischemia and 63% <strong>of</strong><br />
patients with dis-eased coronaries had no resting ECG changes. The echocardiography findings showed that 44% <strong>of</strong> those with<br />
CAD had SWMA and 9.5% had SWMA with normal coronaries. Various sensitivities and specificities were calculated and<br />
revealed that chest pain has a good sensitivity and positive predictive value, <strong>the</strong> ECG had an equal sensitivity and specificity<br />
and echocardiography had <strong>the</strong> highest specificity and positive predictive value in diagnosing CAD.<br />
Conclusion: The overall correlation between <strong>the</strong> studied parameters showed that <strong>the</strong> Framingham risk score came in first<br />
place followed by <strong>the</strong> echocardiography. The chest pain character came in third place and finally <strong>the</strong> ECG findings.<br />
Key Words: Chest pain – Echocardiography – ECG – Coronary angiography.<br />
Introduction<br />
Coronary artery disease (CAD) is <strong>the</strong> most<br />
important among cardiovascular diseases, it kills<br />
more than 7 million people each year worldwide.<br />
Both CAD mortality and <strong>the</strong> prevalence <strong>of</strong> risk<br />
factors continue to rise rapidly in developing countries<br />
partly as a result <strong>of</strong> in-creasing longevity,<br />
The Department <strong>of</strong> Cardiology, Faculty <strong>of</strong> Medicine,<br />
Suez Canal University.<br />
Manuscript received 5 Jan., 2010; revised 14 Feb., 2010;<br />
accepted 15 Feb., 2010.<br />
Address for Correspondence: Dr. Hanan Mohamed Kamal,<br />
The Department <strong>of</strong> Cardiology, Faculty <strong>of</strong> Medicine, Suez<br />
Canal University, Ismailia, Email: hananmkamal@yahoo.<strong>com</strong><br />
147<br />
urbanization, and lifestyle changes [1,2]. Survivors<br />
<strong>of</strong> myocardial infarction (MI) continue to have a<br />
poor prognosis, and <strong>the</strong>ir risk <strong>of</strong> mortality and<br />
morbidity is 1.5-15 times greater than that <strong>of</strong> <strong>the</strong><br />
rest <strong>of</strong> <strong>the</strong> population. This fact remains true despite<br />
a 30% reduction in mortality from coronary artery<br />
disease over <strong>the</strong> past 3 decades in <strong>the</strong> western<br />
<strong>com</strong>munities [3].<br />
The cardinal symptom <strong>of</strong> patients with CAD is<br />
chest pain that initiates clinical evaluation. It is<br />
<strong>com</strong>mon among <strong>the</strong> general population [4]. The<br />
(ACC/AHA) guidelines (2007) empha-size that<br />
<strong>the</strong> patient with symptoms consistent with acute<br />
coronary syndrome (ACS) should be referred to<br />
facilities that allow rapid evaluation by a physician<br />
and <strong>the</strong> recording <strong>of</strong> a 12 lead electrocardiogram
Correlation between Clinical Presentation, ECG & Echocardio-Graphic Findings<br />
(ECG). The 12-lead ECG is central to <strong>the</strong> diagnostic<br />
and triage pathway for ACS and provides important<br />
prognostic information [5]. In a number <strong>of</strong> studies,<br />
<strong>the</strong> presence <strong>of</strong> ischemic changes in <strong>the</strong> resting<br />
ECG, that is, ST-segment depression and T-wave<br />
inversion, has been reported to be a strong predictor<br />
<strong>of</strong> fatal ischemic heart disease (IHD) in men without<br />
clinical evidence <strong>of</strong> IHD, independent <strong>of</strong> major<br />
conventional risk factors <strong>of</strong> IHD [6,7].<br />
Echocardiography is <strong>the</strong> most frequently used<br />
imaging test to evaluate all cardiovascular diseases.<br />
Evaluation <strong>of</strong> CAD is <strong>the</strong> most <strong>com</strong>mon use <strong>of</strong><br />
echocardiography. Its strength is <strong>the</strong> assessment<br />
<strong>of</strong> myocardial thickness, thickening, and motion<br />
at rest. Its usage ranges from <strong>the</strong> diagnosis with<br />
resting or stress echo to <strong>the</strong> detection <strong>of</strong> a <strong>com</strong>plication<br />
and prognosis using wall motion score [8].<br />
CA remains <strong>the</strong> standard for identifying <strong>the</strong><br />
presence or absence <strong>of</strong> a<strong>the</strong>rosclerotic CAD it<br />
helps to delineate coronary anatomy for determining<br />
<strong>the</strong> appropriate <strong>the</strong>rapy in patients with ischemic<br />
CAD [9]. In addition to defining <strong>the</strong> site, severity,<br />
and morphology <strong>of</strong> lesions, it helps provide a<br />
qualitative assessment <strong>of</strong> coronary blood flow and<br />
helps identify collateral vessels [10].<br />
The aim <strong>of</strong> this study was to correlate <strong>the</strong> risk<br />
factors, clinical presentation, electrocardiography<br />
and echocardiographic findings with <strong>the</strong> angiographic<br />
findings in patients undergoing coronary<br />
angiography.<br />
Subjects and Methods<br />
The study was a descriptive cross sectional<br />
study conducted in Suez Canal University Hospital,<br />
cardiac ca<strong>the</strong>terization laboratory, Cardiology<br />
department. The target population are patients<br />
attending <strong>the</strong> hospital, who were referred for elective<br />
coronary angiography.<br />
The inclusion criteria include, history <strong>of</strong> chest<br />
pain prior to procedure which was due to suspected<br />
ischemic heart disease, history <strong>of</strong> angina equivalent<br />
symptoms (e.g.: Dyspnea, fatigue), and patients<br />
who were referred for coronary angiography for<br />
<strong>the</strong> first time. The study excluded patients undergoing<br />
percutanous coronary intervention (PCI).<br />
patients with valvular heart disease due to any<br />
cause o<strong>the</strong>r than ischemic one, patients in clinical<br />
heart failure, and patients with history <strong>of</strong> coronary<br />
artery bypass graft (CABG).<br />
148<br />
Each individual was subjected to <strong>the</strong> following:<br />
1- Personal information about <strong>the</strong> patient, including:<br />
Age, sex, occupation, marital status, special<br />
habits (e.g.: Smoking, alcohol intake), waist<br />
circumference and body mass index (BMI). The<br />
latter is calculated as: Weight (in kg)/(height<br />
[in meters]) 2.<br />
2- History and clinical examination <strong>of</strong> <strong>the</strong> patient,<br />
including: Past history <strong>of</strong> any chronic illness,<br />
clinical presentation <strong>of</strong> <strong>the</strong> present <strong>com</strong>plaint.<br />
The chest pain was analyzed by using <strong>the</strong> WHO<br />
Rose questionnaire [11] and was subdivided into<br />
four categories: No chest pain, non-exertional<br />
chest pain, possible angina, and definite angina.<br />
Complete clinical examination was done.<br />
3- Laboratory findings <strong>of</strong> <strong>the</strong> following investigations:<br />
Random blood sugar, total cholesterol,<br />
triglycerides, LDL level, and HDL level.<br />
4- Risk score classification: All <strong>the</strong> patients’ data<br />
was grouped by <strong>the</strong> Framingham risk score [12]<br />
and assigned to ei<strong>the</strong>r had very low, low, intermediate<br />
or high risk score.<br />
5- Twelve-leads ECG (using Fukuda Denshi, Cardimax<br />
FX 2111 device): Preprocedural ECG was<br />
analyzed for ST-T abnormalities that correlate<br />
to coronary artery disease including: ST depression<br />
more than 0.1mV, or ele-vation and symmetrical<br />
T-wave inversion >0.2mV. Changes<br />
were grouped according to relevant territories<br />
supplied by native coronary ar-teries [13].<br />
6- Echocardiography: 2D and Doppler echocardiogaphy<br />
were performed prior to <strong>the</strong> procedure in<br />
<strong>the</strong> standard views. Regional function assessment<br />
according to <strong>the</strong> 16 segment model <strong>of</strong> <strong>the</strong><br />
American Society <strong>of</strong> Echocar-diography: Grade<br />
1=normal, grade 2=hypokinesia, grade 3=akinesia,<br />
grade 4=dyskinesia. LVEF was determined<br />
with Teich method in <strong>the</strong> short axis view at <strong>the</strong><br />
level <strong>of</strong> <strong>the</strong> papillary muscles. It was <strong>the</strong>n classified<br />
into: Normal: ≥55%, mildly de-pressed:<br />
45%-54%, moderately de-pressed: 30%-44%,<br />
severely de-pressed: 50% in LM artery and >70% in all o<strong>the</strong>r
Fathi A Maklady, et al<br />
vessels, patients were categorized into four<br />
groups: Group 1: Normal coronaries, Group 2:<br />
Single vessel disease, Group 3: Two vessel<br />
disease, Group 4: Multivessel disease.<br />
Statistical analysis:<br />
Data was tabulated and analyzed using SPSS<br />
ver. 16 s<strong>of</strong>tware to determine <strong>the</strong> statistical inference<br />
<strong>of</strong> <strong>the</strong> variables in question. Discrete variables<br />
were presented in <strong>the</strong> form <strong>of</strong> frequency and percentage<br />
tables. Inferences were done using Pearson’s<br />
chi-square test <strong>of</strong> significance and Yates’<br />
correction for 2x2 tables to determine <strong>the</strong> statistical<br />
significance among <strong>the</strong>m. Continuous variables<br />
were presented in <strong>the</strong> form <strong>of</strong> mean and standard<br />
deviation. t-test <strong>of</strong> independence was used to analyze<br />
inferences about <strong>the</strong>m. ANOVA tables were<br />
used to determine <strong>the</strong> level <strong>of</strong> significance between<br />
multiple variables. Spearman's correlation coefficient<br />
was used to estimate different correlations<br />
between variables. p-value less than 0.05 was<br />
considered significant. The sensitivity, specificity,<br />
positive predictive value and negative predictive<br />
value <strong>of</strong> different variables in relation to <strong>the</strong> gold<br />
standard coronary angiography for diagnosing<br />
CAD were calculated.<br />
Results<br />
A random sample <strong>of</strong> 150 participants was enrolled<br />
in <strong>the</strong> study after fulfilling <strong>the</strong> inclusion<br />
criteria. The majority <strong>of</strong> <strong>the</strong>m were males (66%).<br />
Table (1) shows <strong>the</strong> data <strong>of</strong> <strong>the</strong> studied population<br />
distributed among <strong>the</strong> CA findings. Most <strong>of</strong> <strong>the</strong><br />
studied group lies within <strong>the</strong> age range <strong>of</strong> 40-69<br />
years with mean age <strong>of</strong> 55.5±10. Twenty seven<br />
percent <strong>of</strong> <strong>the</strong> study group were smokers and all<br />
<strong>of</strong> <strong>the</strong>m are males. Hypertension was more prevalent<br />
than diabetes among <strong>the</strong> studied population<br />
(60% vs. 43% respectively). Most <strong>of</strong> <strong>the</strong> study<br />
group were dyslipidemic (77%) and obese (46%).<br />
Using <strong>the</strong> Framingham risk score <strong>the</strong> studied population<br />
was categorized most.<br />
Considering <strong>the</strong> clinical presentation <strong>of</strong> patients,<br />
chest pain was <strong>the</strong> most <strong>com</strong>mon presenting <strong>com</strong>plaint<br />
(62%) ra<strong>the</strong>r than angina equivalent (10.7%).<br />
Fur<strong>the</strong>r evaluation by using Rose questionnaire<br />
revealed that 35% <strong>of</strong> <strong>the</strong> population presented by<br />
definite anginal pain. The ECG findings shows<br />
that 55% <strong>of</strong> <strong>the</strong> studied population had changes<br />
suggestive <strong>of</strong> ischemia. Thirty four percent had<br />
segmental wall motion abnormalities by<br />
echocardiography and most <strong>of</strong> <strong>the</strong> population (77%)<br />
had normal ejection fraction (Table 1).<br />
149<br />
Fig. (1) shows <strong>the</strong> distribution <strong>of</strong> <strong>the</strong> studied<br />
population among <strong>the</strong> findings <strong>of</strong> <strong>the</strong> coronary<br />
angiography procedure. The majority <strong>of</strong> <strong>the</strong> patients<br />
(29%) lies in <strong>the</strong> multivessel disease group and<br />
only 16% lies in <strong>the</strong> two vessel disease group.<br />
Analysis <strong>of</strong> <strong>the</strong> risk factors in conjunction with<br />
<strong>the</strong>se findings (Table 1) showed that male gender<br />
had higher proportion <strong>of</strong> CAD ra<strong>the</strong>r than females<br />
(75% vs. 25%) and <strong>the</strong> relation was significant<br />
(p
Correlation between Clinical Presentation, ECG & Echocardio-Graphic Findings<br />
Figure 1: Coronary angiography diagnosis among <strong>the</strong> studied<br />
population <strong>of</strong> <strong>the</strong>m (34%) lie within <strong>the</strong> intermediate<br />
risk score.<br />
Table 1: Characteristics <strong>of</strong> <strong>the</strong> studied population.<br />
Item<br />
Gender:*<br />
Male<br />
Female<br />
Age groups:*<br />
30-39<br />
40-49<br />
50-59<br />
60-69<br />
> 70<br />
Smoker*<br />
Ex-smoker*<br />
Hypertensive<br />
Diabetic<br />
Dyslipidemic<br />
FRS:*<br />
Very low<br />
Low<br />
Intermediate<br />
High<br />
Presenting <strong>com</strong>plaint:*<br />
Chest pain<br />
Angina equivalent<br />
Both<br />
Rose questionnaire:<br />
No chest pain<br />
Non-exertion pain<br />
Possible angina<br />
Definite angina<br />
ECG changes*<br />
SWMA*<br />
28%<br />
27%<br />
No CAD<br />
Two vessel<br />
EF: Normal<br />
Mildly depressed<br />
Moderately depressed<br />
Severely depressed<br />
CAD<br />
No (%)<br />
81 (75)<br />
27 (25)<br />
9 (8)<br />
16 (15)<br />
35 (32)<br />
38 (35)<br />
10 (9)<br />
34 (32)<br />
30 (28)<br />
62 (46)<br />
50 (46)<br />
89 (82)<br />
13 (12)<br />
21 (19)<br />
42 (39)<br />
32 (30)<br />
72 (67)<br />
8 (7)<br />
14 (13)<br />
22 (20)<br />
16 (15)<br />
25 (23)<br />
45 (42)<br />
65 (60)<br />
47 (44)<br />
78 (72)<br />
18 (17)<br />
10 (9)<br />
2 (2)<br />
* Significant at p
Fathi A Maklady, et al<br />
Table 2: The overall correlation between coronary angiography<br />
and o<strong>the</strong>r parameters.<br />
Item<br />
Risk score<br />
Echocardiography<br />
Chest pain<br />
ECG<br />
* Significant at p0.05). Valenzuela LF et al [20] and<br />
Kato et al [21], found also in <strong>the</strong>ir study that diabetes<br />
had an insignificant relation with <strong>the</strong> coronary<br />
artery diagnosis in patients with ACS. Kalantzi et<br />
al [22] found hypertension to have a significant<br />
relation with CA diagnosis in patients with ACS.<br />
The difference may be attributed to <strong>the</strong> selection<br />
r<br />
Coronary angiography<br />
0.343<br />
0.3<br />
0.262<br />
0.224<br />
p-value<br />
0.000*<br />
0.000*<br />
0.001*<br />
0.006*<br />
151<br />
<strong>of</strong> patients, as <strong>the</strong> studied population in <strong>the</strong>ir study<br />
was young; below <strong>the</strong> age <strong>of</strong> 50 years, whereas we<br />
studied all <strong>the</strong> age groups and so <strong>the</strong> prevalence<br />
<strong>of</strong> hypertension in our study was more. The<br />
Framingham risk score was used extensively before<br />
for assessing <strong>the</strong> risk for coronary heart disease<br />
and prediction <strong>of</strong> cardiovascular risk. The higher<br />
proportion <strong>of</strong> patients with normal CA (64%) lies<br />
in <strong>the</strong> very low and low risk categories while only<br />
14% lies in <strong>the</strong> high risk category. By increasing<br />
<strong>the</strong> extent <strong>of</strong> <strong>the</strong> disease, <strong>the</strong> number <strong>of</strong> patients<br />
in <strong>the</strong> very low and low categories falls down and<br />
most <strong>of</strong> <strong>the</strong> patients are grouped between <strong>the</strong> intermediate<br />
and <strong>the</strong> high risk categories.<br />
The clinical presentation:<br />
The relation between <strong>the</strong> presenting <strong>com</strong>plaint<br />
and <strong>the</strong> CA diagnoses showed that <strong>the</strong> majority <strong>of</strong><br />
patients were <strong>com</strong>plaining <strong>of</strong> chest pain that was<br />
variable among gender and showed different distribution<br />
among <strong>the</strong> chest pain character with Rose<br />
questionnaire. In normal subjects, 50% had chest<br />
pain only and 26% had <strong>the</strong> chest pain <strong>com</strong>bined<br />
with angina equivalent symptoms. The majority<br />
<strong>of</strong> <strong>the</strong>m were females (66%). Normal angiography<br />
in patients with chest pain was found to be five<br />
times more <strong>com</strong>mon in women than in men, this<br />
may be attributed to abnormalities <strong>of</strong> <strong>the</strong> microcirculatory<br />
vessels [23], abnormality <strong>of</strong> both endo<strong>the</strong>liumdependent<br />
and independent vasodilatation [24],<br />
occult a<strong>the</strong>rosclerosis [25], or peripheral coronary<br />
microembolization [26]. On <strong>the</strong> o<strong>the</strong>r hand, <strong>the</strong><br />
percentage <strong>of</strong> patients with CAD diagnosed by CA<br />
and were presented without symptoms was 13%,<br />
<strong>the</strong> majority <strong>of</strong> <strong>the</strong>m had single vessel disease<br />
(50%). The concept <strong>of</strong> silent myocardial ischemia,<br />
has emerged long years ago, several studies have<br />
proposed that patients with diabetes mellitus are<br />
subgroup, estimating <strong>the</strong> prevalence <strong>of</strong> silent ischemia<br />
in <strong>the</strong>m to be 29-69% <strong>com</strong>pared with 5-<br />
35% for non-diabetic patients [27-29]. The overall<br />
value <strong>of</strong> <strong>the</strong> chest pain as a diagnostic tool for<br />
CAD in our study was 80% sensitive and 24%<br />
specific. It has a low ability to role out CAD<br />
between both sexes but much more less in females<br />
than males (13% vs. 39% respectively).<br />
The ECG:<br />
The results <strong>of</strong> <strong>the</strong> coronary angiography pose<br />
a significant relation with ischemic ECG changes<br />
found in <strong>the</strong> patients before undergoing <strong>the</strong> procedure.<br />
It was found that 63% with abnormal coronary<br />
arteries had no ECG changes. Also, 40% <strong>of</strong> <strong>the</strong><br />
patients with normal CA had ECG changes indic-
Correlation between Clinical Presentation, ECG & Echocardio-Graphic Findings<br />
ative <strong>of</strong> ischemia. Welch RD et al [30] stated that<br />
8% <strong>of</strong> patients with confirmed transmural myocardial<br />
infarction will have an entirely normal ECG.<br />
In patients with diagnosis <strong>of</strong> CAD by CA, more<br />
than 50% had normal or non-diagnostic ECGs.<br />
O<strong>the</strong>r studies also found <strong>the</strong> same results as ours.<br />
[20,31] The value <strong>of</strong> <strong>the</strong> ECG in predicting <strong>the</strong> CAD<br />
in <strong>the</strong> present study was variable. It shows an<br />
overall equal sensitivity and specificity with low<br />
negative predictor value than a positive predictor<br />
value. Among gender, <strong>the</strong> values are almost <strong>the</strong><br />
same for males with higher positive predictive<br />
value. In females <strong>the</strong> values were less than males<br />
but with higher negative predictor value.<br />
The echocardiogram:<br />
Two-Dimensional echocardiography is well<br />
accepted for evaluation <strong>of</strong> cardiac function [32].<br />
The association <strong>of</strong> echo features with underlying<br />
CAD is less well established [33]. In this study we<br />
studied <strong>the</strong> relation <strong>of</strong> <strong>the</strong> ejection fraction (EF)<br />
assessed by M-mode and <strong>the</strong> segmental wall motion<br />
abnormalities (SWMA) assessed by 2-D with <strong>the</strong><br />
extend <strong>of</strong> CAD. The extent <strong>of</strong> CAD influence <strong>the</strong><br />
ejection fraction <strong>of</strong> <strong>the</strong> studied population. The<br />
mean EF was found to be higher in patients with<br />
normal coronaries than those with multivessel<br />
disease. The presence <strong>of</strong> SWMA in our study was<br />
significantly associated with <strong>the</strong> extend <strong>of</strong> CAD<br />
and with individual coronary artery. It was mentioned<br />
in previous studies that regional wall motion<br />
abnormalities may also occur without history or<br />
clinical and ECG signs <strong>of</strong> coronary artery disease<br />
[34]. In our study, <strong>the</strong>re was a percentage <strong>of</strong> patients<br />
(9.56%) with normal coronary arteries and had<br />
SWMA by 2-D echocardiography. This could be<br />
explained by <strong>the</strong> presence <strong>of</strong> microvascular and<br />
endo<strong>the</strong>lial dysfunction that could cause ischemia<br />
to <strong>the</strong> myocardium without detected major occlusions<br />
[35], also post-ischemic dysfunction, or myocardial<br />
stunning, which is <strong>the</strong> mechanical dysfunction<br />
that persists after reperfusion despite <strong>the</strong><br />
absence <strong>of</strong> irreversible damage and despite restoration<br />
<strong>of</strong> normal or near-normal coronary flow.<br />
Implicit in this definition is that post-ischemic<br />
dysfunction is a fully reversible abnormality, provided<br />
<strong>of</strong> course that sufficient time is allowed for<br />
<strong>the</strong> myocardium to recover [36]. It has been mentioned<br />
by o<strong>the</strong>rs that SWMA could occur with<br />
normal coronaries due to ei<strong>the</strong>r transient ischemic<br />
dysfunction, myocardial scar, stunning/hibernation,<br />
cardiomyopathy, or different <strong>com</strong>binations <strong>of</strong> <strong>the</strong>se<br />
conditions [34].<br />
152<br />
The overall correlation:<br />
In <strong>the</strong> overall correlation <strong>of</strong> <strong>the</strong> studied parameter,<br />
<strong>the</strong> risk score assessment was <strong>the</strong> mostly<br />
correlated parameter with coronary angiographic<br />
findings. Recent studies mentioned that global risk<br />
assessment has be<strong>com</strong>e an important tool in <strong>the</strong><br />
primary prevention <strong>of</strong> CVD and has led to a paradigm<br />
shift in <strong>the</strong> clinical management <strong>of</strong> risk factors<br />
[37,38]. Most authors agreed that <strong>the</strong> first and internationally<br />
most widely used risk prediction tools<br />
were developed with data from <strong>the</strong> Framingham<br />
Heart Study [39,40] which was used in our study.<br />
The echocardiography is <strong>the</strong> second parameter<br />
in order significantly correlated with coronary<br />
angiography. Previous studies have shown that<br />
some isolated echo features are associated with<br />
underlying CAD ei<strong>the</strong>r using marker <strong>of</strong> CAD like<br />
SPECT, stress Echo or angiography [41,42].<br />
The chest pain character was found to be in <strong>the</strong><br />
third order <strong>of</strong> correlation with coronary angiography.<br />
Several cardiac or non-cardiac diseases may<br />
cause chest pain, which makes <strong>the</strong> differential<br />
diagnosis <strong>of</strong> <strong>the</strong>se diseases a great challenge. However,<br />
Diamond and Forrester [43] demonstrated that<br />
<strong>the</strong> type <strong>of</strong> chest pain is <strong>the</strong> best determination<br />
indicative <strong>of</strong> pre-test probability <strong>of</strong> coronary disease<br />
in <strong>the</strong>se patients, more predictive than <strong>the</strong> basic or<br />
stress electrocardiogram.<br />
The ECG was <strong>the</strong> least correlated parameter<br />
with coronary angiography. Miranda CP et al [44]<br />
found that <strong>the</strong> occurrence <strong>of</strong> ST-segment depression<br />
and T-wave inversion in <strong>the</strong> resting ECG appears<br />
to correlate with <strong>the</strong> severity <strong>of</strong> <strong>the</strong> underlying<br />
heart disease, including <strong>the</strong> number <strong>of</strong> vessels<br />
involved and <strong>the</strong> presence <strong>of</strong> left ventricular dysfunction.<br />
However, Ischemic changes in <strong>the</strong> ECG<br />
(ST changes, T wave changes and new arrhythmias<br />
or bundle branch block) are seen in only half <strong>of</strong><br />
<strong>the</strong> patient population presenting with suspected<br />
ACS. Hence <strong>the</strong> ECG is non-diagnostic in at least<br />
half <strong>of</strong> <strong>the</strong> patients [45,46].<br />
Conclusion<br />
• The constellation <strong>of</strong> risk factors pose a strong<br />
correlation with <strong>the</strong> extent <strong>of</strong> CAD.<br />
• The echocardiography is a mainstay in diagnosing<br />
CAD, it has a good specificity and positive predictive<br />
value.<br />
• The chest pain has a reliable sensitivity and a<br />
positive predictive value.
Fathi A Maklady, et al<br />
• The ECG has a poor sensitivity and specificity<br />
in diagnosing CAD hence it is useful for exclusion<br />
<strong>of</strong> high risk patients.<br />
Re<strong>com</strong>mendations<br />
The following measures are re<strong>com</strong>mended:<br />
Using a risk score system in all patients under risk<br />
<strong>of</strong> developing CAD for early detection and management.<br />
• Applying a chest pain questionnaire for patients<br />
presenting by chest pain.<br />
• Training <strong>of</strong> all physicians dealing with chest pain<br />
patients in ECG interpretation.<br />
• Echocardiography should be used for all patients<br />
routinely ei<strong>the</strong>r for detection or for follow-up.<br />
• Carry on a nation-wide study for determining<br />
<strong>the</strong> exact prevalence <strong>of</strong> <strong>the</strong> disease in our country<br />
and <strong>the</strong> ways <strong>of</strong> diagnosis.<br />
References<br />
1- Mackay Judith, Mensah George: The atlas <strong>of</strong> heart diseases<br />
and stroke, Global burden <strong>of</strong> coronary heart disease, WHO<br />
publicans 2007; ch 13: 18-47.<br />
2- Sniderman A, Michel C, Racine N: Heart disease in<br />
patients with diabetes mellitus. Journal <strong>of</strong> Clinical Epidemiology<br />
1999; 45: 1357-1370.<br />
3- Michel E Zevitz, Vibhuti N Singh: Myocardial ischemi,<br />
apublished on www.emedicine\med\<strong>cardiology</strong>.htm, 2006.<br />
4- Lee TH, Cannon CP: Approach to <strong>the</strong> patient with chest<br />
pain, Braunwald's Heart Diseases, 7 th ed. 2005; ch 45,<br />
1129: 31.<br />
5- Fleet RP, Dupuis G, Marchand A, et al: ACC/AHA 2007<br />
guidelines update for <strong>the</strong> management <strong>of</strong> patients with<br />
unstable angina and non-ST elevation myocardial infarction:<br />
Summary article: A report <strong>of</strong> <strong>the</strong> American College<br />
<strong>of</strong> Cardiology/American Heart Association Task Force<br />
on Practice Guidelines (Committee on <strong>the</strong> management<br />
<strong>of</strong> patients with unstable angina). Circulation 2002; 106:<br />
1893.<br />
6- Sigurdsson E, Sigfusson N, Sigvaldason H, et al: Silent<br />
ST-T changes in an epidemiologic cohort study: A marker<br />
<strong>of</strong> hypertension or coronary heart disease, or both: <strong>the</strong><br />
Reykjavik Study. J Am Coll Cardiol 1996; 27: 1140-7.<br />
7- De Bacquer D, De Backer G, Kornitzer M, et al: Prognostic<br />
value <strong>of</strong> ECG findings for total, cardiovascular disease,<br />
and coronary heart disease death in men and women.<br />
Heart 1998; 80: 570-7.<br />
8- Oh JK, Seward JB, Tajik AJ: How to obtain a good<br />
echocardiography examination: Ultrasound physics, Technique<br />
and medical knowledge. In: The Echo Manual,<br />
3 rd ed. Philadelphia, Lippincott Williams and Wilkins, p.<br />
2006; 1-6.<br />
9- Grossman W: Historical prospective and present practice<br />
<strong>of</strong> cardiac ca<strong>the</strong>terization. In: Grossman's Cardiac Cath-<br />
153<br />
eterization, Angiography, and Intervention. 6 th ed. Philadelphia,<br />
Pa: Lippincott Williams and Wilkins 2000.<br />
10- Olade R, Safi A, Kesari S: Cardiac Ca<strong>the</strong>terization (Left<br />
Heart), published on http://www.emedicine.<strong>com</strong>/med/<br />
topic 2958. htm 2006.<br />
11- Rose GA: The diagnosis <strong>of</strong> ischaemic heart pain and<br />
intermittent claudication in field surveys. Bull World<br />
Health Organ 1962; 27: 645-38.<br />
12- Wilson PWF, Castelli WP, Kannel WB: Coronary risk<br />
prediction in adults: The Framingham Heart Study. Am<br />
J Cardiol 1987; 59: 91-94.<br />
13- Christ<strong>of</strong>ferson RD: Manual <strong>of</strong> cardiovascular medicine,<br />
ch. 1: Acute myocardial infarction. Edited by Griffin BP,<br />
Topol EJ; Lippincott Williams and Wilkins. 3 rd edition,<br />
p 2004; 5.<br />
14- Lang RM, Beirig M, Devereaux RB, et al: Chamber<br />
Quantification Writing group, American Society <strong>of</strong><br />
Echocardiography’s Guidelines and Standards Committee,<br />
European Association <strong>of</strong> Echocardiography. Re<strong>com</strong>mendations<br />
for chamber Quantification: A report from <strong>the</strong><br />
American Society <strong>of</strong> Echocardiography’s Guidelines and<br />
Standards Committee and <strong>the</strong> Chamber Quantification<br />
Writing Group, developed in conjunction with <strong>the</strong> European<br />
Association <strong>of</strong> Echocardiography, a branch <strong>of</strong> <strong>the</strong><br />
European Society <strong>of</strong> Cardiology. Journal <strong>of</strong> <strong>the</strong> American<br />
Society <strong>of</strong> Echocardiography 2005; 18: 1440-1463.<br />
15- Lopez AD, Murray C: The global burden <strong>of</strong> disease 1990-<br />
2020. Nat Med 1998; 4: 1241-1243.<br />
16- Goodacre SW, Angelini K, Arnold J, et al: Clinical predictors<br />
<strong>of</strong> acute coronary syndromes in patients with<br />
undifferentiated chest pain. Q J Med 2003; 96: 893-898.<br />
17- Larson DM, Menssen KM, Sharkey SW, et al: "False-<br />
Positive" Cardiac Ca<strong>the</strong>terization Laboratory Activation<br />
Among Patients With Suspected ST-Segment Elevation<br />
Myocardial Infarction. JAMA 2007; 298 (23): 2754-2760.<br />
18- O’Donoghue M, Boden WE, Braunwald E, et al: Early<br />
nvasive vs conservative treatment strategies in women<br />
and men with unstable angina and non ST-segment elevation<br />
myocardial Infarction: A meta-analysis. JAMA 2008;<br />
300 (1): 71-80.<br />
19- The National Board <strong>of</strong> Health and Welfare. Myocardial<br />
infarctions in Sweden 2007; 1987-2004. 64 p 4.<br />
20- Valenzuela LF, Vázquez R, Fournier JA, et al: Prediction<br />
<strong>of</strong> infarction-related artery occlusion and multivessel<br />
disease in postinfarction angina. International Journal <strong>of</strong><br />
Cardiology 2007; 115: 381-385.<br />
21- Kato J, Aihara A, Kikuya M, et al: Risk factors and<br />
predictors <strong>of</strong> coronary arterial lesions in Japanese hypertensive<br />
patients. Hypertens Res 2001; 24 (1): 3-11.<br />
22- Kalantzi K, Korantzopoulos P, Tzimas P, et al: The relative<br />
value <strong>of</strong> metabolic syndrome and cardiovascular risk<br />
score estimates in premature acute coronary syndromes.<br />
Am Heart J 2008; 155: 534-40.<br />
23- Bugiardini R, Manfrini O, Pizzi C, et al: Endo<strong>the</strong>lial<br />
function predicts future development <strong>of</strong> coronary artery<br />
disease. A study on women with chest pain and normal<br />
angiograms. Circulation 2004; 109: 2518-2523.
Correlation between Clinical Presentation, ECG & Echocardio-Graphic Findings<br />
24- Nabel EG, Ganz P, Gordon JB, et al: Dilation <strong>of</strong> normal<br />
and constriction <strong>of</strong> a<strong>the</strong>rosclerotic coronary arteries caused<br />
by <strong>the</strong> cold pres sor test. Circulation 1988; 77: 43-52.<br />
25- Tuzcu EM, Kapadia SR, Tutar E, et al: High prevalence<br />
<strong>of</strong> coronary a<strong>the</strong>rosclerosis in asymptomatic teenagers<br />
and young adults: Evidence from intravascular ultrasound.<br />
Circulation 2001; 103: 2705-2710.<br />
26- Erbel R, Heusch G: Coronary microembolization. J Am<br />
Coll Cardiol 2000; 36: 22-24.<br />
27- Ahluwalia G, Jain P, Chugh SK, et al: Silent myocardial<br />
ischaemia in diabetics with normal autonomic function.<br />
Int J Cardiol 1995; 48: 147-53.<br />
28- Parmley WW: Prevalence and clinical significance <strong>of</strong><br />
silent myocardial ischaemia. Circulation, 80 (6 suppl IV)<br />
1989; 68-73.<br />
29- Sharma SN, Bajaj R, Kaul U, et al: Silent myocardial<br />
ischemia in patients with angiographically proven coronary<br />
artery disease. Indian Heart J 1989; 41: 158-61.<br />
30- Welch RD, Zalenski RJ, Frederick PD, et al: for <strong>the</strong><br />
National Registry <strong>of</strong> Myocardial Infarction 2 and 3 Investigators.<br />
Prognostic value <strong>of</strong> a normal or nonspecific<br />
initial electrocardiogram in acute myocardial infarction.<br />
JAMA 2001; 286: 1977-84.<br />
31- Cannon CP, McCabe CH, Stone BH, et al: The electrocardiogram<br />
predicts one-year out<strong>com</strong>e <strong>of</strong> patients with<br />
unstable angina and non-Q wave myocardial infarction:<br />
Results <strong>of</strong> <strong>the</strong> TIMI III registry ECG ancillary study. J<br />
Am Coll Cardiol 1997; 30: 133-40.<br />
32- Cheitlin MD, et al: ACC/AHA/ASE 2003 Guidelines<br />
update for <strong>the</strong> Clinical application <strong>of</strong> Echocardiography:<br />
Summary article. A report <strong>of</strong> <strong>the</strong> American College <strong>of</strong><br />
Cardiology/American Heart Association Task Force on<br />
practice Guidelines. J Am Soc Echocardiography 2003;<br />
16: 1091-1110.<br />
33- Levy D, Garrison RJ, Savage DD, et al: Left ventricular<br />
mass and incidence <strong>of</strong> coronary heart disease in an elderly<br />
cohort. The Framingham Heart Study. Ann Intern Med<br />
1989; 110 (2): 101-7.<br />
34- Cicala S, de Simone G, Roman MJ, et al: Prevalence and<br />
prognostic significance <strong>of</strong> wall-motion abnormalities in<br />
adults without clinically recognized cardiovascular disease:<br />
The Strong Heart study. Circulation 2007; 116, 143-150.<br />
35- Bugiardini R, Badimon L, Collins P, et al: Angina, "Nor-<br />
154<br />
mal" Coronary Angiography, and Vascular Dysfunction:<br />
Risk Assessment Strategies. PLoS Med 2007; 4 (2): e12.<br />
36- Bolli R: Myocardial stunning in man. Circulation 1992;<br />
86: 1671-91.<br />
37- Hense HW: Observations, predictions and decisionsassessing<br />
cardiovascular risk assessment. Int J Epidemiol<br />
2004; 33: 235-9.<br />
38- Jackson R: Guidelines on preventing cardiovascular<br />
disease in clinical practice. BMJ 2000; 320: 659-61.<br />
39- Adult Treatment Panel III. Executive summary <strong>of</strong> <strong>the</strong><br />
third report <strong>of</strong> <strong>the</strong> National Cholesterol Education Program<br />
(NCEP) Expert Panel on Detection, Evaluation, and<br />
Treatment <strong>of</strong> High Blood Cholesterol in Adults (Adult<br />
Treatment Panel III). JAMA 2001; 285: 2486-97.<br />
40- Wilson PW, D'Agostino RB, Levy D, et al: Prediction <strong>of</strong><br />
Coronary Heart Disease Using Risk Factor Categories.<br />
Circulation 1998; 97, 1837-1847.<br />
41- Elhendy A, van Domburg RT, Bax JJ, Roelandt JR:<br />
Significance <strong>of</strong> resting wall motion abnormalities in 2dimensional<br />
echocardiography in patients without previous<br />
myocardial infarction referred for pharmacologic stress<br />
testing. J Am Soc Echocardiogr 2000; 13 (1): 1-8.<br />
42- Jeon DS, Atar S, Brasch AV, et al: Association <strong>of</strong> mitral<br />
annulus calcification, aortic valve sclerosis and aortic<br />
root calcification with abnormal myocardial perfusion<br />
single photon emission tomography in subjects age
Egypt Heart J 62 (1): 155-164, March 2010<br />
Measurement <strong>of</strong> Fractional Flow Reserve (FFR) for Guiding Percutaneous<br />
Coronary Intervention in Clinical Practice<br />
HUSSEIN SHAALAN, MD<br />
Background: FFR, calculated from coronary pressure measurement, is a reliable invasive index to indicate if a stenosis is<br />
ischemia-related and can be determined in <strong>the</strong> ca<strong>the</strong>terization laboratory in a simple and rapid way.<br />
Aim <strong>of</strong> <strong>the</strong> Work: Study <strong>the</strong> role <strong>of</strong> measurement <strong>of</strong> FFR before PCI in daily practice with regards to decision making and<br />
procedure out<strong>com</strong>e.<br />
Patients and Methods: 80 patients with CAD referred for coronary angiography with possible PCI were included. Patients<br />
were divided into two equal groups: FFR guided group in whom coronary pressure wire was part <strong>of</strong> <strong>the</strong> procedure and FFR<br />
had an impact on decision making, and angiographic guided group or <strong>the</strong> standard (control) group. The cut-<strong>of</strong>f point for FFR<br />
group was 0.75 above which no PCI was done; while diameter stenosis <strong>of</strong> 70% was <strong>the</strong> cut-<strong>of</strong>f point in <strong>the</strong> control group below<br />
which <strong>the</strong> decision for PCI was left for <strong>the</strong> operator discretion. Accordingly, each group was fur<strong>the</strong>r divided into 3 subgroups;<br />
PCI, medically treated, and mixed subgroups (relevant lesions underwent PCI, and irrelevant ones were managed medically).<br />
All patients were followed-up both in-hospital and for at least one month after discharge. Both groups were <strong>com</strong>pared with<br />
regards to; MACE (<strong>com</strong>posite <strong>of</strong> death, MI, and repeat revascularizations), as <strong>the</strong> primary end points, and procedure time,<br />
fluoroscopic time, contrast volume, functional status (angina or dyspnea), and total procedure cost as secondary end points.<br />
Results: Both groups were matched with regards to demographic data and clinical presentations. PCI was performed in 55<br />
(68.8%) patients in both groups (25 in FFR group and 30 in angiograph group); <strong>the</strong> rest <strong>of</strong> patients were managed medically.<br />
All patients received DES. FFR was measured successfully in 60 vessels <strong>of</strong> FFR guided group. FFR significantly increased in<br />
PCI patients from 0.70 to 0.88 (p0.05). However, procedure time and contrast consumption were significantly higher in FFR guided group Vs. <strong>the</strong> control<br />
group (p
Measurement <strong>of</strong> Fractional Flow Reserve (FFR)<br />
[3]; FFR can reliably interrogate any individual<br />
stenosis, and <strong>the</strong>refore, can be used for immediate<br />
decision-making in <strong>the</strong> ca<strong>the</strong>terization laboratory<br />
whe<strong>the</strong>r to stent or not [4,5,6].<br />
Compared with intravascular ultrasound<br />
(IVUS), which shows anatomical lesion characteristics,<br />
FFR localizes <strong>the</strong> ischemia producing lesion<br />
among different morphologic lesions seen by<br />
IVUS.Similarly, not all angiographic ally relevant<br />
lesions as decided visually by experienced interventional<br />
cardiologist or even by quantitative<br />
coronary angiography (QCA) are ischemia producing<br />
lesions (especially those <strong>of</strong> moderate severity)<br />
and need to be treated.<br />
It is to be noted that, some previous studies<br />
suggested that acute ischemic events not frequently<br />
occur at <strong>the</strong> site <strong>of</strong> previously insignificant or mild<br />
stenosis [7,8]. This has been extended into <strong>the</strong><br />
general belief that a mild stenosis could have a<br />
worse prognosis and that use <strong>of</strong> PCI in such a<br />
lesion might be beneficial [9]. However, in <strong>the</strong><br />
defer study [1] it was shown that PCI <strong>of</strong> such lesions<br />
without functional significance did not improve<br />
out<strong>com</strong>e or anginal status and did not reduce <strong>the</strong><br />
use <strong>of</strong> antianginal medications.<br />
Coronary artery disease patients with nonischemia<br />
producing lesions have total event rate<br />
<strong>of</strong> 21% for <strong>the</strong> next 5 years which is still higher<br />
than normal people. Risk factor modification and<br />
adequate medical treatment are probably <strong>of</strong> greater<br />
prognostic value than mechanical coronary intervention.<br />
According to <strong>the</strong> current guidelines, PCI<br />
should be performed after having documented<br />
inducible ischemia [10,11]. Never<strong>the</strong>less, a prior<br />
non-invasive evidence <strong>of</strong> ischemia is present in a<br />
minority <strong>of</strong> patients underlying PCI [12].<br />
In <strong>the</strong> era <strong>of</strong> drug eluting stent (DES), FFR<br />
measurement holds its value for guiding PCI as<br />
stenting non-ischemia-related lesion with bare<br />
metal stent (BMS) has worse out<strong>com</strong>e than <strong>the</strong><br />
defer approach but better than stenting ischemic<br />
lesion. DES does reduce target vessel revascularization<br />
(TVR), but not mortality or myocardial<br />
infarction (MI).<br />
Compared with BMS, treatment <strong>of</strong> intermediate<br />
lesions with DES ra<strong>the</strong>r than BMS appears safe<br />
and results in a marked reduction in clinical and<br />
angiographic re-stenosis. The efficacy <strong>of</strong> DES may<br />
require re-evaluation <strong>of</strong> current treatment paradigm<br />
for intermediate lesions.<br />
156<br />
Aim <strong>of</strong> <strong>the</strong> study:<br />
Study <strong>the</strong> role <strong>of</strong> measurement <strong>of</strong> fractional<br />
flow reserve (FFR) using coronary pressure wire<br />
for guiding PCI in daily practice with regards to<br />
decision making (to stent or not) and its impact on<br />
procedure out<strong>com</strong>e.<br />
Patients and Methods<br />
The present study included 80 patients with<br />
CAD referred for coronary angiography with possible<br />
PCI. Patients were divided into two equal<br />
groups: Group I (FFR or study group) in whom<br />
coronary pressure wire was part <strong>of</strong> <strong>the</strong> cardiac<br />
ca<strong>the</strong>terization procedure to estimate lesion severity<br />
by FFR, and group II (control or angiography<br />
group) in whom <strong>the</strong> whole procedure was guided<br />
angiographically.<br />
According to <strong>the</strong> coronary anatomy seen during<br />
diagnostic coronary angiography and fractional<br />
flow reserve measurement results, patients were<br />
fur<strong>the</strong>r subdivided into 3 subgroups: Subgroup A<br />
(PCI group guided by ei<strong>the</strong>r FFR if ≤0.75 or angiography<br />
if ≥70% diameter stenosis), subgroup<br />
B (medical treatment group when FFR is >0.75 or<br />
Hussein Shaalan<br />
Ca<strong>the</strong>ter findings: Standard coronary angiography<br />
was done for all patients using <strong>the</strong> standard<br />
technique with ad hoc PCI after reviewing <strong>the</strong><br />
angiographic findings.<br />
Clearly significant lesions (≥70%) as seen in<br />
all projections were tackled immediately whenever<br />
suitable for PCI without fur<strong>the</strong>r evaluating <strong>the</strong><br />
lesion severity by FFR. while intermediate coronary<br />
lesions (between 50-70%), ei<strong>the</strong>r <strong>the</strong>y were left<br />
for medical treatment or stented according to FFR<br />
result in <strong>the</strong> study group or as decided by <strong>the</strong><br />
operator in <strong>the</strong> angiography control group).<br />
In case coronary pressure wire was not available,<br />
<strong>the</strong> decision to do PCI is left for <strong>the</strong> operator<br />
after correlating patient symptoms to ca<strong>the</strong>ter<br />
findings or whenever non-invasive test is available.<br />
This study is a single centre, single operator randomized,<br />
controlled study. The overall Coronary<br />
morphology and lesion <strong>com</strong>plexity were described<br />
according to <strong>the</strong> SYNTAX score.<br />
Fractional flow reserve measurement: FFR is<br />
defined as <strong>the</strong> ratio <strong>of</strong> <strong>the</strong> maximal blood flow<br />
achievable in a stenotic vessel to <strong>the</strong> <strong>the</strong>oretical<br />
maximal flow in <strong>the</strong> same vessel if no stenosis was<br />
present. In a normal coronary artery <strong>the</strong>re should<br />
be no pressure gradient between <strong>the</strong> aorta and <strong>the</strong><br />
distal artery resulting in a FFR value <strong>of</strong> 1. These<br />
simultaneous measurements can be made in a<br />
stenosed coronary artery using a pressure tipped<br />
coronary guide wire to record distal pressure and<br />
a guide ca<strong>the</strong>ter to record pressure in <strong>the</strong> aorta.<br />
The cut-<strong>of</strong>f value <strong>of</strong> FFR is ≤0.75 (ischemic<br />
zone); and value between 0.75 and 0.8 (<strong>the</strong> grey<br />
zone) was also considered for PCI whenever <strong>the</strong>re<br />
is ano<strong>the</strong>r lesion with FFR ≤0.075 in need <strong>of</strong> PCI<br />
in <strong>the</strong> same patient [13]. Coronary pressure guide<br />
wire (RadiMedical system) was used at maximal<br />
hyperemia induced by IC (in most cases) adenosine<br />
or IV infusion (140ug/kg/min) in a central vein.<br />
However, big doses <strong>of</strong> adenosine (70-90ug at<br />
least and up to 150ug) should be given for each<br />
lesion to get a reliable result. The effect starts to<br />
appear within 10sec and remains only for 20sec.<br />
The effect <strong>of</strong> IV adenosine starts within 1min and<br />
disappear in 1min after cessation <strong>of</strong> infusion.<br />
Calculation <strong>of</strong> FFR: Unfractionated heparin (5000<br />
units) is given initially; <strong>the</strong> transducer <strong>of</strong> <strong>the</strong> coronary<br />
pressure should be in <strong>the</strong> left main stem or<br />
in a healthy area proximal to <strong>the</strong> lesion. The piezoelectric<br />
crystal is located 30mm from <strong>the</strong> wire tip<br />
157<br />
i.e. at <strong>the</strong> beginning <strong>of</strong> <strong>the</strong> radio-opaque distal<br />
segment. Nitroglycerine IC (200ug) is injected<br />
first followed by IC adenosine to achieve maximal<br />
hyperemia. Caffeine intake prior to <strong>the</strong> procedure<br />
is not yet proved to alter FFR measurements [14].<br />
If <strong>the</strong> recorded aortic pressure is damping (ventricularized)<br />
upon ca<strong>the</strong>ter engagement smaller sized<br />
ca<strong>the</strong>ter is preferred [15].<br />
FFR=mean distal coronary pressure (measured<br />
with <strong>the</strong> pressure wire)/mean aortic pressure (measured<br />
simultaneously with <strong>the</strong> guiding ca<strong>the</strong>ter)<br />
using maximal hyperemia. FFR is checked before<br />
and after PCI to ensure adequate stent deployment<br />
(if FFR >0.90). The higher <strong>the</strong> post stenting FFR<br />
value <strong>the</strong> lower <strong>the</strong> event rate [16].<br />
PCI: PCI was performed using <strong>the</strong> standard<br />
technique, and usually via <strong>the</strong> femoral approach.<br />
PCI patients received only DES. However, PCI<br />
with DES was not planned for more than 2-vessels<br />
in one session. All consumables during PCI were<br />
collected at <strong>the</strong> end <strong>of</strong> <strong>the</strong> procedure and each item<br />
price is included to get <strong>the</strong> total procedure cost<br />
(namely; guide wires, guiding ca<strong>the</strong>ters, balloons,<br />
stents, coronary pressure wires, adenosine, and 1year<br />
clopidogrel <strong>the</strong>rapy). The mean procedure<br />
time (defined as <strong>the</strong> total time starting from puncture<br />
site till removal <strong>of</strong> <strong>the</strong> guiding ca<strong>the</strong>ter),<br />
fluoroscopic time, and contrast volume were reported<br />
and <strong>com</strong>pared between <strong>the</strong> two groups.<br />
Repeat cardiac markers were rechecked after PCI.<br />
Follow-up: All patients were given appointment<br />
in <strong>the</strong> outpatient clinic within 1 month post procedure,<br />
3 months, and lastly 6 months. Patients should<br />
attend at least once in <strong>the</strong> outpatient clinic to be<br />
included in this study.<br />
End points: All patients will be followed-up<br />
post procedure both in-hospital and during followup<br />
period in outpatient clinic for major adverse<br />
cardiac events (MACE); death (all cause mortality),<br />
MI (diagnosed by ≥3 folds rise <strong>of</strong> cardiac markers<br />
or new Q-waves in 2 contiguous leads), and repeat<br />
revascularization (PCI or CABG). Functional status<br />
(angina and/or shortness <strong>of</strong> breath), procedure<br />
time, contrast volume, and total cost were also<br />
<strong>com</strong>pared between groups.<br />
Statistical analysis:<br />
Data was analyzed on an IBM personal <strong>com</strong>puter,<br />
using Statistical Package for Special Science<br />
(SPSS) s<strong>of</strong>tware <strong>com</strong>puter program version 15.
Measurement <strong>of</strong> Fractional Flow Reserve (FFR)<br />
• Data were described as mean ± standard deviation<br />
(SD) for quantitative (Numerical) variables and<br />
as frequency and percentage for qualitative (Categorical)<br />
variables.<br />
• Independent Student t test was used for <strong>com</strong>parison<br />
<strong>of</strong> quantitative variables among two independent<br />
groups.<br />
• Paired t test was used for <strong>com</strong>parison <strong>of</strong> quantitative<br />
variables among two dependent groups.<br />
• One-way ANOVA test was used for <strong>com</strong>parison<br />
<strong>of</strong> quantitative variables among more than two<br />
independent groups. Least significant difference<br />
test (LSD) test was used as post-hoc test.<br />
• Chi-square test (or Fisher’s exact test when<br />
appropriate) was used for <strong>com</strong>parison <strong>of</strong> distribution<br />
<strong>of</strong> qualitative variables among different<br />
group.<br />
• Correlation between continuous variables was<br />
performed using person correlation coefficient.<br />
• Kaplan–Meier estimate and logrank test was<br />
used for assessment <strong>of</strong> survival <strong>of</strong> different out<strong>com</strong>es.<br />
Table 1: Patient’s demographic data between both groups.<br />
Parameter<br />
Age (mean ±SD) (range:27-85)<br />
M: F ratio<br />
Smoking<br />
DM<br />
(on insulin)<br />
Hypertension<br />
Hyperlipidemia<br />
Family history<br />
BMI (mean ± SD)<br />
FFR guided<br />
58.50±11.99<br />
24 (60%):16 (40%)<br />
19 (47.5%)<br />
27 (67.5%)<br />
9 (22.5%)<br />
26 (65%)<br />
18 (45%)<br />
2 (5%)<br />
29.16±5.74<br />
Table 2: The clinical presentations <strong>of</strong> <strong>the</strong> studied groups.<br />
Parameter<br />
Stable CAD<br />
Unstable CAD<br />
NSTEMI<br />
Old MI (>3 months)<br />
Recent MI (>5 days)<br />
Renal impairment<br />
Previous PCI<br />
EF (mean ± SD)<br />
FFR guided<br />
18 (45%)<br />
7 (17.5%)<br />
11 (27.5%)<br />
11 (27.5%)<br />
10 (25%)<br />
4 (10%)<br />
16 (40%)<br />
45.62±9.94<br />
158<br />
• Significance level (p) value: p>0.05 is insignificant<br />
(NS). p≤0.05 is significant (S).<br />
Results<br />
A total <strong>of</strong> 80 patients were enrolled in this<br />
study. Of <strong>the</strong> total 55 (68.8%) PCI patients, 25<br />
(45.5%) patients were assigned for FFR guided<br />
strategy and 30 (54.5%) patients were assigned for<br />
<strong>the</strong> standard angiographic strategy. The rest <strong>of</strong> <strong>the</strong><br />
patients were followed-up medically. Each group<br />
was divided into 3-subgroups: (A) PCI was performed<br />
in 7 (17.5%) patients guided by FFR measurement<br />
versus 14 (35%) patients guided by angiography,<br />
(B) medically treated patients in 15<br />
(37.5%) patients guided by FFR measurement<br />
versus 10 (25%) patients guided by angiography,<br />
and (C) mixed group with PCI performed in relevant<br />
lesions while <strong>the</strong> non relevant ones were left<br />
untreated in 18 (45%) patients in FFR group versus<br />
16 (40%) in angiography group (p value=0.17).<br />
Both groups were matched with regards to<br />
demographic data and clinical presentations (except<br />
patients with previous PCI) with no statistical<br />
differences among main groups or <strong>the</strong> three subgroups,<br />
as shown in Tables (1,2).<br />
Angiographic guided<br />
56.67±13.88<br />
30 (75%):10 (25%)<br />
16 (40%)<br />
22 (55%)<br />
8 (20%)<br />
24 (60%)<br />
17 (42.5%)<br />
3 (7.5%)<br />
29.86±5.84<br />
Angiographic guided<br />
19 (47.5%)<br />
7 (17.5%)<br />
9 (22.5%)<br />
6 (15%)<br />
13 (32.5%)<br />
2 (5%)<br />
4 (10%)<br />
45.37±9.63<br />
0.05<br />
0.00<br />
0.26<br />
1.86<br />
0.54<br />
0.72<br />
9.6<br />
Chi-square<br />
0.62 (t-test)<br />
2.05<br />
0.45<br />
1.31<br />
0.07<br />
0.21<br />
0.05<br />
0.21<br />
–0.54 (t-test)<br />
Chi-square<br />
0.11 (t-test)<br />
p value<br />
0.53<br />
0.15<br />
0.45<br />
0.25<br />
0.78<br />
0.64<br />
0.82<br />
0.64<br />
0.58<br />
p value<br />
0.82<br />
1.0<br />
0.60<br />
0.17<br />
0.45<br />
0.39<br />
0.002<br />
0.90
Hussein Shaalan<br />
Non-invasive tests were not frequently requested<br />
in <strong>the</strong> present study, 14 (17.5%) patients; in<br />
o<strong>the</strong>r words, <strong>the</strong> decision to send <strong>the</strong> patient to <strong>the</strong><br />
invasive service was made mainly on clinical basis.<br />
Out <strong>of</strong> total FFR guided procedure (>80 patients)<br />
done in our centre (from January 2007 till June<br />
Table 3: Shows <strong>the</strong> ca<strong>the</strong>ter findings among both groups.<br />
Parameter<br />
(mean ± SD)<br />
Lesion: Patient ratio<br />
Vessel: Patient ratio<br />
Rx vessel: Patient ratio<br />
(50% to 0.75<br />
Vessel (2) ≤0.75<br />
Total<br />
Vessel<br />
Vesse 1&2 >0.75<br />
Vessel 1&2 ≤0.75<br />
0.93<br />
0.71±0.07<br />
0.89<br />
0.70±0.1<br />
0.88<br />
0.70<br />
N=40 (100%)<br />
N=20 (50%)<br />
FFR<br />
guided<br />
FFR pre PCI<br />
3.0±1.4<br />
In <strong>the</strong> FFR guided group, 8 vessels out <strong>of</strong> 60<br />
measured had <strong>the</strong>ir value in <strong>the</strong> grey zone (>0.75-<br />
≤0.80); half <strong>of</strong> <strong>the</strong>m were followed-up medically,<br />
and <strong>the</strong> o<strong>the</strong>r half underwent PCI because <strong>of</strong> con<strong>com</strong>itant<br />
PCI planned for ano<strong>the</strong>r vessel.<br />
Cardiac biomarkers were measured before and<br />
after PCI, <strong>the</strong> results are shown in Table (5) which<br />
illustrates <strong>the</strong> PCI out<strong>com</strong>es between both groups.<br />
There was no difference between both groups with<br />
2.37±1.0<br />
1.28±0.45<br />
1.72±1.1<br />
1.3±1.0<br />
1.1±0.90<br />
1.37±1.1<br />
11.23±5.9<br />
38.45±21.25<br />
n=29 (72.5%)<br />
n=11 (27.5%)<br />
n=14 (35%)<br />
n=6 (15%)<br />
n=43 vessels<br />
n=17 vessels<br />
159<br />
2009), only 40 patients were included, <strong>the</strong> o<strong>the</strong>r<br />
patients were excluded because <strong>of</strong> exclusion criteria.<br />
There were more patients with borderline<br />
lesions (50%-
Measurement <strong>of</strong> Fractional Flow Reserve (FFR)<br />
Table 5: PCI out<strong>com</strong>es between both groups.<br />
Parameter<br />
Ck-MB pre PCI<br />
Ck-MB post PCI (3-5X N)<br />
TNT (I) pre PCI<br />
TNT (I) post PCI (3-5X N)<br />
DES: Patient ratio<br />
DES size ≥2.75<br />
DES size
Hussein Shaalan<br />
Table 8: Comparison <strong>of</strong> total cost (a) and hospital stay (b) between 3 subgroups.<br />
Parameter<br />
FFR group (a)<br />
(b)<br />
Angiographic group (a)<br />
(b)<br />
t-test (a) (b)<br />
p value (a) (b)<br />
PCI sub G<br />
7208±1873<br />
6.2±4.2<br />
4843±2048<br />
3.8±2.38<br />
2.5 1.6<br />
0.01 0.1<br />
Rx sub G<br />
On follow-up, coronary angiography was performed<br />
in 4 (10%) patients <strong>of</strong> FFR guided group<br />
(two <strong>of</strong> <strong>the</strong>m had PCI, and <strong>the</strong> o<strong>the</strong>r two were<br />
followed up medically) versus 3 (8%) patients <strong>of</strong><br />
angiographic guided group (none <strong>of</strong> <strong>the</strong>m was in<br />
need <strong>of</strong> PCI or CABG, (p=0.69). The follow-up<br />
duration was significantly longer in FFR-guided<br />
group, 7.59±8.3 months <strong>com</strong>pared with <strong>the</strong> angiography<br />
guided group, 3.83±2.0 months (p=0.008).<br />
Since <strong>the</strong> present study enrolled patients with<br />
multiple lesions and diseased vessels, although<br />
with low SYNTAX score (as shown in Table 3),<br />
some patients continue to have chest pain and/or<br />
shortness <strong>of</strong> breath; 7 (17.5%) and 10 (25%) patients<br />
in FFR guided group versus 9 (22.5%) and<br />
6 (15%) patients in angiographic guided group<br />
respectively (p=0.24). Kaplan-Meier survival functional<br />
curves addressing <strong>the</strong> results <strong>of</strong> <strong>the</strong> functional<br />
status between both groups are shown below toge<strong>the</strong>r<br />
with <strong>the</strong> patients who had follow up coronary<br />
angiography (CAG) ± PCI. The number <strong>of</strong> patients<br />
reached <strong>the</strong> hard end points was too little to plot<br />
<strong>the</strong> curves for <strong>the</strong>m.<br />
The cost <strong>of</strong> procedures and <strong>the</strong> duration <strong>of</strong><br />
hospital stay are shown in Tables (7,8). Although<br />
2140±414<br />
2.4±0.9<br />
1000±0.0<br />
2.9±1.5<br />
10.66 –0.8<br />
Measurement <strong>of</strong> Fractional Flow Reserve (FFR)<br />
Decision making only on anatomic finding<br />
(including IVUS) is more likely to waist resources<br />
and make <strong>the</strong> role <strong>of</strong> PCI in stable patients only<br />
for cosmetic purpose [18]. Interventional cardiologist<br />
is not only responsible for mechanical revascularization<br />
by PCI, but also optimization <strong>of</strong> medical<br />
<strong>the</strong>rapy and life style modifications. According<br />
to <strong>the</strong> Courage trial [19], PCI benefits <strong>the</strong> subsets<br />
<strong>of</strong> patients who demonstrated ischemia reduction<br />
by ≥5% as documented by non-invasive tests; while<br />
<strong>the</strong> 5 years follow-up failed to demonstrate any<br />
benefit <strong>of</strong> PCI over optimum medical <strong>the</strong>rapy in<br />
reducing all cause mortality or MI.<br />
Why would we need FFR and/or IVUS if <strong>the</strong><br />
lesion is clearly significant? The probability <strong>of</strong><br />
having non ischemic lesion when <strong>the</strong> lesion looks<br />
significant angiographically (≥90%) is nil if FFR<br />
measurements is applied, and it rises when <strong>the</strong><br />
diameter stenosis gets less (≥70-
Hussein Shaalan<br />
FAME trial versus 81% in FFR guided group with<br />
no statistical difference, (p=0.20). The same findings<br />
were documented in <strong>the</strong> present study (77.5%<br />
<strong>of</strong> patients free from angina in angiographic guided<br />
group versus 82.5% in FFR guided group, p=0.24).<br />
Procedure time (but not fluoroscopic time) and<br />
contrast volume were higher-in <strong>the</strong> present studyin<br />
FFR guided group <strong>com</strong>pared with angiographic<br />
guided group; this is in contrast to <strong>the</strong> FAME<br />
results which showed less cost and less consumption<br />
<strong>of</strong> contrast material in FFR guided group<br />
<strong>com</strong>pared with angiographic guided group.<br />
In FAME trial <strong>the</strong> mean number <strong>of</strong> stent deployment<br />
per patient was 2.7±1.2 in angiographic<br />
guided group versus 1.9±1.3 in FFR guided group,<br />
p
Measurement <strong>of</strong> Fractional Flow Reserve (FFR)<br />
7- Falk E, Shah PK, Fuster V: Coronary plaque disruption<br />
Circulation 1996; 92: 657-671.<br />
8- Ambrose JA, Tannenbaum MA, Alexopoulos D, et al:<br />
Angiographic progression <strong>of</strong> coronary artery disease and<br />
<strong>the</strong> development <strong>of</strong> myocardial infarction. J AM Coll<br />
Cardiol 1988; 12: 56-62.<br />
9- Teirstein PS: Dueling hazards <strong>of</strong> in<strong>com</strong>plete revascularization<br />
and in<strong>com</strong>plete data Circulation 2006; 113: 2380-<br />
2382.<br />
10- Smith Jr SC, Feldman TE, Hirshfeld Jr JW, et al:<br />
ACC/AHA/SCAI 2005 guideline update for percutaneous<br />
coronary intervention-summary article: A report <strong>of</strong> <strong>the</strong><br />
American College <strong>of</strong> Cardiology/American Heart Association<br />
Task Force on Practice Guidelines (ACC/AHA/<br />
SCAI Writing Committee to Update <strong>the</strong> 2001 Guidelines<br />
for Percutaneous Coronary Intervention) Circulation 2006;<br />
113: 156-175.<br />
11- Silber S, Albertsson P, Aviles FF, et al: Guidelines for<br />
percutaneous coronary interventions Eur Heart J 2005;<br />
26: 804-847.<br />
12- Moses JW, Stone GW, Martin B Leon, Eberhard Grube,<br />
Alexandra J Lansky, Nikolsky E, et al: Drug-eluting stents<br />
in <strong>the</strong> treatment <strong>of</strong> intermediate lesions. J Am Coll Cardiol<br />
2006; 47: 2164-2171.<br />
13- Ross J, McGeoch, MB/chB, MRCP, Keith G Oldroyd,<br />
MB/chB, MRCP: Pharmacological options for inducing<br />
maximal hyperemia during studies <strong>of</strong> coronary physiology:<br />
In core curriculum ca<strong>the</strong>terization and cardiovascular<br />
interventions 2008; 71: 198-204.<br />
14- Raed AA, Gilbert JZ, Trimm JR, Baldwin SA, Iskandrian<br />
AE: Effect <strong>of</strong> caffeine administered intravenously on<br />
intrcaronary administered adenosine-induced coronary<br />
hemodynamics in patients with coronary artery disease.<br />
Am J Cardiol 2004; 93: 343-346.<br />
15- Hau WK: Routine pressure-derived fractional flow reserve<br />
guidance: From diagnostic to everyday practice. J Invasive<br />
Cardiol 2006; 18: 240-24.<br />
16- Pijls NHJ, Klauss V, Siebert U, et al: Coronary pressure<br />
measurement after stenting predicts adverse events at<br />
follow-up: A multicenter registry Circulation 2002; 105:<br />
2950-2954.<br />
17- EJ Topol, SG Ellis, DM Cosgrove, ER Bates, DW Muller,<br />
NJ Schork, MA Schork, FD Loop: Analysis <strong>of</strong> coronary<br />
angioplasty practice in <strong>the</strong> United States with an insuranceclaims<br />
data base Circulation 1993; 87: 1489-1497.<br />
164<br />
18- William Wijns: Stable angina, any change after Courage?<br />
In: The 3 rd European EAPCI Fellows Course; Royal<br />
College <strong>of</strong> physicians, London November 21, 2008;<br />
available in http://www. europcronline.<strong>com</strong> /key_topics/<br />
0901_FFR<br />
19- William E Boden, Robert A O'Rourke, Koon K Teo, et al:<br />
(For <strong>the</strong> COURAGE Trial Research Group). Optimal<br />
Medical Therapy with or without PCI for Stable Coronary<br />
Disease N Engl J Med 2007; 356: 1503-1516.<br />
20- Atsushi Takagi, Yukio Tsurumi, Yasuhiro Ishii, Kazuhito<br />
Suzuki, et al: Clinical Potential <strong>of</strong> Intravascular Ultrasound<br />
for Physiological Assessment <strong>of</strong> Coronary Stenosis: Relationship<br />
Between Quantitative Ultrasound Tomography<br />
and Pressure-Derived Fractional Flow Reserve Circulation<br />
1999; 100: 250-255.<br />
21- François Schiele. Routine Use <strong>of</strong> FFR In: euroPCR 2005;<br />
available in http://www. europcronline.<strong>com</strong> /key_topics/<br />
0901_FFR<br />
22- Pierre Legalery, Francois Schiele, Marie-France Seronde,<br />
Nicolas Meneveau, Hu Wei, Katy Didier, Marie-Cecile<br />
Blonde, Fiona Caulfield, Jean-Pierre Bassand: One-year<br />
out<strong>com</strong>e <strong>of</strong> patients submitted to routine fractional flow<br />
reserve assessment to determine <strong>the</strong> need for angioplasty<br />
Eur Heart J 2005; 10: 1093.<br />
23- Pim AL Tonino, Bernard De Bruyne, Nico HJ Pijls, Uwe<br />
Siebert, Fumiaki Ikeno, Volker Klauss, et al: (For <strong>the</strong><br />
FAME Study Investigators). Fractional Flow Reserve<br />
versus Angiography for Guiding Percutaneous Coronary<br />
Intervention N Engl J Med 2009; 360: 213-224.<br />
24- Amit Segev, Lorne E Goldman, Warren J Cantor, Aiala<br />
Barr, Bradley H Strauss, Luke D Winegard, Kim A Bowman,<br />
Robert J Chisholm: Elevated troponin-I after percutaneous<br />
coronary interventions: Incidence and risk factors<br />
Cardiovascular Radiation Medicine 2004; 5: 59-63.<br />
25- MB Nienhuis, JP Ottervanger, J-HE Dambrink, LD Dikkeschei,<br />
H Suryapranata, AWJ van‘t H<strong>of</strong>, JCA Hoorntje,<br />
MJ de Boer, ATM Gosselink, F Zijlstra: Troponin T<br />
elevation and prognosis after multivessel <strong>com</strong>pared with<br />
single-vessel elective percutaneous coronary intervention<br />
Neth Heart J 2007; May 15 (5): 178-183.<br />
26- Howard C Herrmann: Isolated cTnT Elevation after PCI<br />
(Post-PCI cTnT elevation <strong>of</strong> 0.03ng/mL or greater had<br />
prognostic value in a single-center study patients without<br />
post procedural CK-MB elevation Journal Watches (specialities)<br />
<strong>cardiology</strong> 2006 December 6; and J Am Coll<br />
Cardiol 2006; Nov 7 (48): 1765-70.
Egypt Heart J 62 (1): 165-171, March 2010<br />
Angiographic Coronary Artery Disease in Women with Chest Pain and<br />
History <strong>of</strong> Anxiety Disorders<br />
KHALED E DARAHIM, MD, MRCP*; MONA IBRAHIM AWAAD, MD**<br />
Background: Among women, <strong>the</strong> presentation <strong>of</strong> angina symptoms is nei<strong>the</strong>r a sensitive nor a specific marker for coronary<br />
artery disease.<br />
Objective: This study aimed to evaluate <strong>the</strong> ability <strong>of</strong> psychiatric anxiety-disorder history to discriminate between women<br />
with and without angiographic coronary artery disease (CAD) in a population with chest pain.<br />
Methods: We included 50 women who were referred for coronary angiogram to evaluate chest pain or suspected myocardial<br />
ischemia. Participants <strong>com</strong>pleted <strong>the</strong> Hamilton Rating Scale for Anxiety (HAM-A), a five-item behavioral avoidance scale, and<br />
<strong>the</strong> Beck Depression Inventory (BDI). Coronary artery disease covariate measures included analysis <strong>of</strong> chest pain, coronary<br />
artery disease risk factors, quantitative coronary angiography analysis including modified Gensini score.<br />
Results: Women with a history <strong>of</strong> anxiety disorders [9 <strong>of</strong> 50 (18%) participants] were younger (48.0 Vs. 60.7 years <strong>of</strong> age;<br />
p
History <strong>of</strong> Anxiety & Coronary Angiography<br />
Chest pain symptoms may also be related to<br />
noncardiac causes, including psychological disorders<br />
(Freedland et al, 1996; Smith et al, 1996;<br />
Freedland et al, 1991 and Freeman et al, 1987).<br />
Although some studies showed that anxiety is more<br />
<strong>com</strong>mon in patients with normal anatomy than<br />
those with coronary disease, <strong>the</strong>re is <strong>of</strong>ten considerable<br />
overlap (Chambers and Bass, 1998). Crosssectional<br />
studies have demonstrated relationships<br />
between psychological factors such as high anxiety<br />
and life stress with chest pain symptoms in women<br />
(Stansfeld et al, 1993; Fisher et al, 1996 and Costa,<br />
1987). These associations, however, may be interpreted<br />
to suggest that stress and anxiety contribute<br />
to increased CAD risk (Rozanski et al, 1999 and<br />
Musselman et al, 1998), or that chest pain promotes<br />
increased stress and anxiety resulting from symptom-related<br />
concerns <strong>of</strong> illness or death.<br />
Studies showed that generalized anxiety disorder<br />
and major depression were more <strong>com</strong>mon in<br />
cardiac patients than in <strong>the</strong> general <strong>com</strong>munity<br />
(Frasure-Smith, 2006). Fur<strong>the</strong>rmore, some studies<br />
showed that Generalized Anxiety Disorder appeared<br />
to be associated with elevated coronary heart disease<br />
risk relative to major depressive disorder<br />
(Barger and Sydeman, 2005). Evidence pertaining<br />
to <strong>the</strong> relationship between psychological factors<br />
and an objective measure <strong>of</strong> CAD among women<br />
with chest pain symptoms would aid in <strong>the</strong> interpretation<br />
<strong>of</strong> <strong>the</strong>se data, but we are unaware <strong>of</strong> such<br />
findings to date.<br />
In this study, we hypo<strong>the</strong>size that women with<br />
chest pain and a psychiatric history <strong>of</strong> anxiety<br />
disorders are less likely to have angiographic CAD<br />
than are those women with chest pain symptoms<br />
and no anxiety history.<br />
Objective:<br />
This study aimed to evaluate <strong>the</strong> ability <strong>of</strong><br />
psychiatric anxiety-disorder history to discriminate<br />
between women with and without angiographic<br />
coronary artery disease (CAD) in a population with<br />
chest pain.<br />
Methodology<br />
Study population:<br />
The study included 50 women who were referred<br />
for coronary angiogram to evaluate chest<br />
pain or suspected myocardial ischemia. Participants<br />
<strong>com</strong>pleted a battery <strong>of</strong> symptom and psychological<br />
questionnaires at baseline testing, along with quantitative<br />
coronary angiography.<br />
166<br />
The inclusion criteria were:<br />
1- Women older than 18 year <strong>of</strong> age.<br />
2- Referred for a coronary angiogram.<br />
Exclusion criteria included patients with:<br />
1- Current pregnancy.<br />
2- Recent myocardial infarction, cardiomyopathy.<br />
3- Revascularization procedure (percutaneous transluminal<br />
coronary angioplasty or coronary artery<br />
bypass graft).<br />
4- Congenital heart disease.<br />
5- Language barrier preventing questionnaire <strong>com</strong>pletion.<br />
The study protocol was approved by <strong>the</strong> research<br />
<strong>com</strong>mittee <strong>of</strong> our institution and informed<br />
consent <strong>of</strong> all subjects was obtained.<br />
Methods:<br />
Coronary artery disease assessment:<br />
Coronary artery disease covariate measures<br />
included age, body mass index, obesity (BMI<br />
>30kg/m 2), menopausal status, family history <strong>of</strong><br />
coronary artery disease, diabetes status, smoking<br />
status, hypertension status, and hypercholesterolemia<br />
status (positive/negative history). Risk<br />
factors (when not previously known) were defined<br />
according to <strong>the</strong> European Society <strong>of</strong> Cardiology<br />
guidelines as follows: Hypertension as blood pressure<br />
>140/90mmHg in three consecutive readings,<br />
at rest; hypercholesterolemia as total and low LDL<br />
cholesterol level >5mmol/L (>190mg/dL) and<br />
3mmol/L (>114mg/dl), respectively; diabetes as<br />
fasting glucose level >7.0mmol/L (>125mg/dl);<br />
obesity as body mass index (BMI) >30kg/m 2; and<br />
family history <strong>of</strong> CAD as parents with CAD at age<br />
Khaled E Darahim & Mona I Awaad<br />
multiple projections, and reference vessel diameter,<br />
minimal lumen diameter, and percent diameter<br />
stenosis were measured from <strong>the</strong> 'worst' angiographic<br />
view.<br />
Coronary disease severity was judged by three<br />
criteria. First, using <strong>the</strong> quantitative angiogram<br />
results, we assigned each participant to a group:<br />
"no CAD" (20mm <strong>of</strong> normal artery segment was<br />
classified as 2-VD.<br />
In addition, a total <strong>of</strong> 10 (16.7% <strong>of</strong> <strong>the</strong> noanxiety-history<br />
participants and 37.5% <strong>of</strong> <strong>the</strong> positive-anxiety-history<br />
group) participants also <strong>com</strong>pleted<br />
noninvasive tests for myocardial ischemia<br />
(exercise stress testing).<br />
Left CA Right CA<br />
Figure 1: Schematic drawing <strong>of</strong> <strong>the</strong> GENSINI score (left). The method assigned a different severity score depending on <strong>the</strong><br />
degree <strong>of</strong> stenosis, its location (proximal, middle or distal tract) along <strong>the</strong> target vessel and <strong>the</strong> type <strong>of</strong> coronary<br />
vessel involved (left anterior descending, left circumflex, or right coronary artery). An example <strong>of</strong> Gensini score<br />
calculation is shown on <strong>the</strong> right part <strong>of</strong> <strong>the</strong> figure. MLCA, main left coronary artery; LAD, left anterior descending;<br />
CFx, left circumflex; RCA, right coronary artery.<br />
Psychiatric and covariate measures: Participants<br />
<strong>com</strong>pleted <strong>the</strong> Hamilton Rating Scale for<br />
Anxiety, a five-item behavioral avoidance scale,<br />
and <strong>the</strong> Beck Depression Inventory.<br />
Prox<br />
X1<br />
lurnen diameter Severity score<br />
PD<br />
x1<br />
LAD: Patent<br />
Score: 0<br />
CFx: 99% concentric (16), proximal (2)<br />
Score: 2 X 16=32<br />
RCA: 90% eccentric (8), proximal (1)<br />
Score: 8 X 1=8<br />
Final Gensini score: 0 + 32 + 8 = 40<br />
The Hamilton Rating Scale for Anxiety (HAM-<br />
A) was developed in <strong>the</strong> late 1950s to assess anxiety<br />
symptoms, both somatic and cognitive. Because<br />
conceptualization <strong>of</strong> anxiety has changed consid-
History <strong>of</strong> Anxiety & Coronary Angiography<br />
erably, <strong>the</strong> HAM-A provides limited coverage <strong>of</strong><br />
"worry" required for DSM-IV diagnosis <strong>of</strong> generalized<br />
anxiety disorder and does not include <strong>the</strong><br />
episodic anxiety found in panic disorder. There<br />
are 14 items, each <strong>of</strong> which is rated 0 to 4 on an<br />
unanchored severity scale, with <strong>the</strong> total score<br />
ranging from 0 to 56. A score <strong>of</strong> 14 has been<br />
suggested as <strong>the</strong> threshold for clinically significant<br />
anxiety, but scores <strong>of</strong> 5 or less are typical in individuals<br />
in <strong>the</strong> <strong>com</strong>munity.<br />
The avoidance scale contained five questions<br />
(scores range from 5 to 50; higher scores equal<br />
greater avoidance) assessing <strong>the</strong> avoidance <strong>of</strong><br />
<strong>com</strong>mon situations (traveling by bus, walking alone<br />
on busy streets, going into crowded shops, going<br />
alone far from home, and large open spaces) because<br />
<strong>of</strong> fear.<br />
Finally, <strong>the</strong> Beck Depression Inventory (BDI)<br />
(Beck et al, 1996): Created by Dr. Aaron T. Beck,<br />
is a 21-question multiple-choice (scores range from<br />
0 to 63) self-report inventory that is one <strong>of</strong> <strong>the</strong><br />
most widely used instruments for measuring <strong>the</strong><br />
severity <strong>of</strong> depression. The most current version<br />
<strong>of</strong> <strong>the</strong> questionnaire is designed for individuals<br />
aged 13 and over and is <strong>com</strong>posed <strong>of</strong> items relating<br />
to depression symptoms such as hopelessness and<br />
irritability, cognitions such as guilt or feelings <strong>of</strong><br />
being punished, as well as physical symptoms such<br />
as fatigue, weight loss, and lack <strong>of</strong> interest in sex.<br />
There are three versions <strong>of</strong> <strong>the</strong> BDI-<strong>the</strong> original<br />
BDI, first published in 1961 and later revised in<br />
1971 as <strong>the</strong> BDI-1A, and <strong>the</strong> BDI-II, published in<br />
1996. The BDI is widely used as an assessment<br />
tool by healthcare pr<strong>of</strong>essionals and researchers<br />
in a variety <strong>of</strong> settings. Scores <strong>of</strong> 0 to 9 are considered<br />
minimal; 10 to 16 mild; 17 10 29 moderate;<br />
and 30 to 48 severe. A BDI score <strong>of</strong> 17 is frequently<br />
used to mark <strong>the</strong> presence <strong>of</strong> "subclinical" (i.e.,<br />
not Diagnostic and Statistical Manual <strong>of</strong> Mental<br />
Disorders [DSM-IV] (American Psychiatric Association,<br />
1994) diagnostic for a mood disorder)<br />
depression.<br />
Additional questions assessed whe<strong>the</strong>r participants<br />
had ever received treatment from a psychologist<br />
or psychiatrist for an anxiety disorder (we<br />
did not collect data regarding <strong>the</strong> length, type,<br />
precipitating factors or success <strong>of</strong> <strong>the</strong> treatment).<br />
Statistical analysis:<br />
The data were analyzed statistically using <strong>the</strong><br />
s<strong>of</strong>tware Statistical Package for Social Science<br />
168<br />
(SPSS) version (9). Chi square test for categorical<br />
variables. Using independent sample t tests, we<br />
<strong>com</strong>pared participants with and without a history<br />
<strong>of</strong> anxiety disorders on measured CAD risk factors,<br />
angina symptoms and o<strong>the</strong>r pain indices (e.g.,<br />
headaches, back pain, etc.) and anxiety symptoms<br />
experienced at baseline testing (i.e., scores on <strong>the</strong><br />
above HAM-A, avoidance and depression scales).<br />
p value ≤0.05 (2 tailed) is considered significant<br />
and ≤0.01 is highly significant.<br />
Results<br />
The study included 50 women who were referred<br />
for coronary angiogram to evaluate chest<br />
pain or suspected myocardial ischemia.<br />
Clinical characteristics <strong>of</strong> <strong>the</strong> study group:<br />
Table (1) <strong>com</strong>pares women with and without a<br />
history <strong>of</strong> anxiety disorders across measured CAD<br />
risk factors, angina and o<strong>the</strong>r physical symptoms.<br />
Women with a history <strong>of</strong> anxiety disorders [9 <strong>of</strong><br />
50 (18%) participants] were younger (48.0 Vs.<br />
60.7 years <strong>of</strong> age), more likely to smoke and had<br />
lower cholesterol blood levels. Symptom pr<strong>of</strong>iles<br />
also differed between groups. Women with a positive<br />
anxiety history more frequently endorsed<br />
sensations <strong>of</strong> "sharp, knife-like pain" in describing<br />
<strong>the</strong>ir chest pain.<br />
Table 1: A Comparison <strong>of</strong> patients with and without an anxiety<br />
disorder history on angina and o<strong>the</strong>r physical symptoms,<br />
CAD risk factors.<br />
Age (years)<br />
% Current smokers<br />
% Hypertensive<br />
% Diabetic<br />
% Hypercholesterolemic<br />
% FH <strong>of</strong> CAD<br />
Body mass index<br />
% Obesity<br />
% Angina from exertion<br />
% Sharp, knife-like pain<br />
% Tightness<br />
% Left arm pain<br />
% rest pain<br />
% Using nitroglycerin<br />
% Headaches<br />
% Positive exercise test<br />
With<br />
anxiety<br />
history<br />
(n=9)<br />
48.0±12.2<br />
33.3<br />
44.4<br />
33.3<br />
33.3<br />
33.3<br />
32.99±7.46<br />
55.6<br />
33.3<br />
33.3<br />
55.6<br />
22.2<br />
66.7<br />
11.1<br />
44.4<br />
33.3<br />
Without<br />
anxiety<br />
history<br />
(n=41)<br />
60.7±10.4<br />
2.4<br />
65.9<br />
41.5<br />
70.7<br />
14.6<br />
32.19±5.87<br />
48.8<br />
43.9<br />
4.9<br />
87.8<br />
14.6<br />
51.2<br />
12.2<br />
29.3<br />
34.1<br />
p<br />
value<br />
0.002<br />
0.006<br />
NS<br />
NS<br />
0.034<br />
NS<br />
NS<br />
NS<br />
NS<br />
0.01<br />
0.023<br />
NS<br />
NS<br />
NS<br />
NS<br />
NS<br />
Data are expressed as a mean ± standard deviation or percent (%).<br />
CAD = Coronary artery disease.<br />
FH = Family history <strong>of</strong> CAD.<br />
NS = Non-significant.
Khaled E Darahim & Mona I Awaad<br />
A positive anxiety-disorder history was not<br />
associated with a lower likelihood <strong>of</strong> having inducible<br />
ischemia on noninvasive stress testing (33%<br />
Vs. 34%, p=NS).<br />
Table (2) showed that women with a past history<br />
<strong>of</strong> anxiety history still experience higher anxiety<br />
symptoms, both somatic and cognitive. The positive<br />
anxiety group expressed significantly greater distress<br />
levels at baseline, as indicated by higher<br />
behavioral avoidance scores and more depressive<br />
symptoms.<br />
Table 2: A <strong>com</strong>parison <strong>of</strong> patients with and without an anxiety<br />
disorder history on psychological characteristics.<br />
HAM-A<br />
BDI<br />
Avoidance scale<br />
Table 3: A <strong>com</strong>parison <strong>of</strong> women with and without a history<br />
<strong>of</strong> anxiety disorders on three indices <strong>of</strong> CAD.<br />
CAD<br />
CAD groups:<br />
%Normal<br />
%Non-obstructive<br />
%Obstructive<br />
VD Number:<br />
%Normal<br />
%Single<br />
%Double<br />
%Triple<br />
Gensini score<br />
With anxiety<br />
history (n=9)<br />
29.4±9.8<br />
11.7±7.1<br />
13.6±7.4<br />
With anxiety<br />
history (n=9)<br />
22.2<br />
66.7<br />
11.1<br />
22.2<br />
77.8<br />
0<br />
11.1<br />
11.1<br />
4.4±8.5<br />
Without anxiety<br />
history (n=41)<br />
5.8±4.3<br />
2.9±2.6<br />
5.6±2.4<br />
Data are expressed as a mean ± standard deviation.<br />
HAM-A = Hamilton Rating Scale for Anxiety.<br />
BDI = Beck Depression Inventory.<br />
NS = Non-significant.<br />
Without anxiety<br />
history (n=41)<br />
41.5<br />
53.7<br />
4.9<br />
41.5<br />
58.5<br />
22<br />
9.8<br />
9.8<br />
13.3±20.6<br />
p<br />
value<br />
0.000<br />
0.006<br />
0.013<br />
p<br />
value<br />
NS<br />
NS<br />
NS<br />
0.047<br />
Data are expressed as a mean ± standard deviation or percent (%).<br />
CAD = Coronary artery disease.<br />
CAD groups: Normal = Maximum stenosis
History <strong>of</strong> Anxiety & Coronary Angiography<br />
Fur<strong>the</strong>rmore, <strong>the</strong> symptom pr<strong>of</strong>iles also differed<br />
between <strong>the</strong> two groups. Women with a positive<br />
anxiety history more frequently endorsed sensations<br />
<strong>of</strong> tightness and sharp, knife-like pain in describing<br />
<strong>the</strong>ir chest pain. Rutledge et al, also demonstrated<br />
that women with past history <strong>of</strong> anxiety described<br />
<strong>the</strong>ir pain more frequently as sharp knife-like chest<br />
pain, besides <strong>the</strong>y demonstrated that <strong>the</strong>ir pains<br />
last longer and had a greater chance <strong>of</strong> experiencing<br />
angina while at rest. (Rutledge et al, 2001).<br />
Although previous studies have explored relationships<br />
between psychological factors and endpoints<br />
such as angina during exercise testing (Freedland<br />
et al, 1996), <strong>the</strong> prevalence <strong>of</strong> psychological<br />
distress among patients with angina (Smith et al,<br />
1996) and <strong>the</strong> role <strong>of</strong> psychological factors in silent<br />
myocardial ischemia (Freedland et al, 1991), few<br />
reports investigated <strong>the</strong> association between a<br />
history <strong>of</strong> anxiety disorders and angiographic CAD<br />
in women with chest pain.<br />
Our findings suggest that a history <strong>of</strong> anxiety<br />
disorders is associated with a less severe angiographic<br />
CAD among women presenting with chest<br />
pain symptoms. Rutledge et al, demonstrated that<br />
<strong>the</strong> presence <strong>of</strong> an anxiety-disorder history was<br />
associated with a significantly lower likelihood <strong>of</strong><br />
significant angiographic CAD among women with<br />
angina, also <strong>the</strong>y demonstrated that women with<br />
a history <strong>of</strong> anxiety disorders evidenced significantly<br />
less severe disease (Rutledge et al, 2001).<br />
Our study did not show significant difference<br />
as regard <strong>the</strong> presence <strong>of</strong> coronary artery disease,<br />
or number <strong>of</strong> diseased vessels. Although not statistically<br />
significant, based on CAD groupings,<br />
women in <strong>the</strong> positive-anxiety-history group were<br />
less than twice as likely (22.2% Vs. 41.5%) to<br />
show obstructive CAD. Failure to show statistical<br />
significance may reflect that <strong>the</strong> study is underpowered<br />
to show this difference.<br />
Although we observed a low prevalence <strong>of</strong><br />
obstructive CAD among women with chest pain<br />
who reported a history <strong>of</strong> anxiety disorders, it is<br />
notable that a 22.2% <strong>of</strong> this group never<strong>the</strong>less did<br />
show angiographic evidence <strong>of</strong> obstructive CAD<br />
(i.e., >50% stenosis). Therefore, this result reinforces<br />
<strong>the</strong> need to carefully evaluate symptoms in<br />
women irrespective <strong>of</strong> psychological history and<br />
to consider anxiety-history variables as a topic in<br />
future investigations.<br />
Fur<strong>the</strong>rmore, our results do not suggest that<br />
women as a group are immune to have severe CAD<br />
170<br />
(which is <strong>the</strong> leading cause <strong>of</strong> death among both<br />
women and men), or even that an anxious female<br />
patient is less likely to show evidence <strong>of</strong> severe<br />
CAD (i.e., our results reflect a known anxietydisorder<br />
history, not current symptoms).<br />
Limitations <strong>of</strong> <strong>the</strong> study:<br />
Our observation <strong>of</strong> an association between a<br />
previous anxiety disorder and current angiogram<br />
results also raises questions concerning <strong>the</strong> temporal<br />
nature <strong>of</strong> this relationship. However, we believed<br />
that concurrent anxiety symptoms assessed at<br />
baseline testing before or after angiogram may<br />
reflect more transient factors (e.g., concern about<br />
health or potential test results or current life difficulties)<br />
and may <strong>the</strong>refore <strong>of</strong>fer less insight into<br />
<strong>the</strong> long-term symptom reporting style we have<br />
shown to be linked to a less severe disease.<br />
Our measure <strong>of</strong> anxiety history was also ra<strong>the</strong>r<br />
global and did not allow us to examine relationships<br />
with specific anxiety conditions. Although <strong>the</strong><br />
sample size and prevalence rate <strong>of</strong> anxiety disorders<br />
found in our population would have limited such<br />
an examination, most <strong>of</strong> <strong>the</strong> cases included in <strong>the</strong><br />
study were diagnosed according to <strong>the</strong> Diagnostic<br />
and Statistical Manual <strong>of</strong> Mental Disorders, Fourth<br />
Edition (DSM-IV) as generalized anxiety disorder,<br />
two cases have panic disorder and one case has<br />
mixed anxiety and depression.<br />
There is a possibility <strong>of</strong> a referral bias (i.e.,<br />
participants may not represent a random sample<br />
<strong>of</strong> women with angina, and anxiety characteristics<br />
may affect treatment-seeking behavior) that may<br />
constrain <strong>the</strong> generalizability <strong>of</strong> <strong>the</strong>se results.<br />
Conclusion<br />
Our study demonstrates that <strong>the</strong> presence <strong>of</strong> an<br />
anxiety-disorder history was associated with a<br />
significantly less severe angiographic CAD among<br />
women with chest pain. Determining a patient’s<br />
anxiety-disorder history may assist <strong>the</strong> clinician<br />
in identifying women with chest pain having less<br />
severe CAD.<br />
References<br />
1- American Psychiatric Association: Diagnostic and Statistical<br />
Manual <strong>of</strong> Mental Disorders: Fourth Edition. Washington<br />
DC: American Psychological Association 1994.<br />
2- Bankier B, Litman AB: Psychitric Disorders and Coronary<br />
Heart Disease in Women-A still Neglected Topic: Review<br />
<strong>of</strong> <strong>the</strong> Literature from 1971 to 2000. Psycho<strong>the</strong>r Psychosom<br />
2002; 71: 133-140.
Khaled E Darahim & Mona I Awaad<br />
3- Barger SD, Sydeman SJ: Does generalized anxiety disorder<br />
predict coronary heart disease risk factors independently<br />
<strong>of</strong> major depressive disorder? Journal <strong>of</strong> Affective Disorders,<br />
(1): 87-91.<br />
4- Beck AT: Depression Inventory. Philadelphia: Center for<br />
Cognitive Therapy 1978.<br />
5- Buchthal SD, den Hollander, JA, Merz CNB, et al: Abnormal<br />
myocardial phosphorus-31 nuclear magnetic resonance<br />
spectroscopy in women with chest pain but normal coronary<br />
angiograms. N Engl J Med 1999; 342: 829-35.<br />
6- Chambers J, Bass C: Atypical chest pain: Looking beyond<br />
<strong>the</strong> heart. Q J Med 1998; 91: 239-244<br />
7- Costa PT, Jr: Influence <strong>of</strong> <strong>the</strong> normal personality dimension<br />
<strong>of</strong> neuroticism on chest pain symptoms and coronary<br />
artery disease. Am J Cardiol 1987; 60: 20J-26J.<br />
8- Fisher SG, Cooper R, Weber L, Liao Y: Psychosocial<br />
correlates <strong>of</strong> chest pain among African-American women.<br />
Women Health 1996; 24: 19-35.<br />
9- Frasure-Smith N: Major anxiety ups heart risk. Archives<br />
<strong>of</strong> General Psychiatry 2006; 75: 1.<br />
10- Freedland KE, Carney RM, Krone RJ, Case NB, Case<br />
RB: Psychological determinants <strong>of</strong> anginal pain perception<br />
during exercise testing <strong>of</strong> stable patients after recovery<br />
from acute myocardial infarction or unstable angina<br />
pectoris. Am J Cardiol 1996; 77: 1-4.<br />
11- Freedland KE, Carney RM, Krone RJ, et al: Psychological<br />
factors in silent myocardial ischemia. Psychosom Med<br />
1991; 53: 13-24.<br />
12- Freeman LJ, Nixon PG, Sallabank P, Reaveley D: Psychological<br />
stress and silent myocardial ischemia. Am Heart<br />
J 1987; 114: 477-82.<br />
13- Gensini G: A more meaningful scoring system for determining<br />
<strong>the</strong> severity <strong>of</strong> coronary artery disease. Am J<br />
Cardiol 1983; 51: 606.<br />
14- Kennedy JW, Killip R, Fisher LD, et al: The clinical<br />
spectrum <strong>of</strong> coronary artery disease and its surgical and<br />
medical management, 1974-1979. The Coronary Artery<br />
Surgery Study. Circulation 1982; 66 (Suppl 3): 16.<br />
15- King KB, Clark PC, Hicks GL, Jr: Patterns <strong>of</strong> referral<br />
and recovery in women and men undergoing coronary<br />
artery bypass grafting. Am J Cardiol 1992; 69: 179-82.<br />
171<br />
16- Krumolz HM, Douglas PS, Lauer MS, Pasternak RC:<br />
Selection <strong>of</strong> patients for coronary angiography and coronary<br />
revascularization early after myocardial infarction:<br />
Is <strong>the</strong>re evidence for a gender bias? Ann Intern Med 1992;<br />
116: 785-90.<br />
17- Kuhn FE, Rackley CE: Coronary artery disease in women.<br />
Risk factors, evaluation, treatment, and prevention. Arch<br />
Intern Med 1993; 153: 2626-36.<br />
18- Musselman DL, Evans DL, Nemer<strong>of</strong>f CB: The relationship<br />
<strong>of</strong> depression to cardiovascular disease: Epidemiology,<br />
biology & treatment. Arch Gen Psych 1998; 55: 580-92.<br />
19- Petticrew M, McKee M, Jones J: Coronary artery surgery:<br />
Are women discriminated against? BMJ 1993; 306: 1164-<br />
6.<br />
20- Principal Investigators <strong>of</strong> CASS and Their Associates:<br />
The National Heart, Lung, and Blood Institute Coronary<br />
Artery Surgery Study (CASS). Circulation 1981; 63 (Suppl<br />
1): 1-81.<br />
21- Reis SE, Holubkov R, Lee JS, et al: Coronary flow velocity<br />
response to adenosine characterizes coronary microvascular<br />
function in women with chest pain and no obstructive<br />
coronary disease. J Am Coll Cardiol 1999; 33: 1469-75.<br />
22- Rozanski A, Blumenthal JA, Kaplan J: Impact <strong>of</strong> psychological<br />
factors on <strong>the</strong> pathogenesis <strong>of</strong> cardiovascular<br />
disease and implications for <strong>the</strong>rapy. Circulation 1999;<br />
99: 2192-217.<br />
23- Rutledge T, Reis SE, Olson M, Owens J, Kelsey SF, et<br />
al: History <strong>of</strong> anxiety disorders is associated with a<br />
decreased likelihood <strong>of</strong> angiographic coronary artery<br />
disease in women with chest pain: The WISE study. J Am<br />
Coll Cardiol March 1, 2001; 37 (3): 780-785.<br />
24- Shaw LJ, Miller DD, Romeis JC, et al: Gender differences<br />
in <strong>the</strong> noninvasive evaluation and management <strong>of</strong> patients<br />
with suspected coronary artery disease. Ann Intern Med<br />
1994; 120: 559-66.<br />
25- Smith DF, Sterndorff B, Ropcke G, Gustavsen EM, Hansen<br />
JK: Prevalence and severity <strong>of</strong> anxiety, depression, and<br />
Type A behaviors in angina pectoris. Scand J Psychol<br />
1996; 37: 249-58.<br />
26- Stansfeld SA, Smith GD, Marmot M: Association between<br />
physical and psychological morbidity in <strong>the</strong> Whitehall II<br />
Study. J Psychosom Res 1993; 37: 227-38.
Egypt Heart J 62 (1): 173-179, March 2010<br />
Depression Post Acute Coronary Syndromes: Incidence and Predictors<br />
MONA IBRAHIM AWAAD, MD; KHALED E DARAHIM, MD, MRCP<br />
Depression occurs <strong>com</strong>orbidly in patients hospitalized for a range <strong>of</strong> cardiac conditions and procedures. To date, few<br />
predictors <strong>of</strong> persistent depression in cardiac patients have been identified, apart from a past history <strong>of</strong> depression. This study<br />
assess <strong>the</strong> incidence <strong>of</strong> depressive symptoms and predictors <strong>of</strong> depression within 3 months post acute coronary syndromes. This<br />
study included 72 patients with acute coronary syndromes; 25 patients diagnosed with MI and 47 patients diagnosed with<br />
unstable angina. Depression was measured using <strong>the</strong> Beck Depression Inventory (BDI). Predictor variables were assessed and<br />
included demographic details and clinical cardiac and depression risk factors. The incidence <strong>of</strong> depressive symptoms was 41.7%,<br />
while <strong>the</strong> severity <strong>of</strong> depression according to <strong>the</strong> BDI score was; 16.7% for mild depression, 20.8% for moderate depression<br />
and 4.2% for severe depression. The independent predictors for depression (moderate and severe) within 3 months after acute<br />
coronary syndromes were; having a past history <strong>of</strong> depression (OR 20.4), female gender (OR 17), marital separation (OR 4.6),<br />
and having past history <strong>of</strong> cardiac condition (OR 3.5). In conclusion, <strong>the</strong>se predictors in this study may assist physicians in<br />
identification <strong>of</strong> cardiac patients who are at risk <strong>of</strong> depression and who may require active intervention.<br />
Key Words: Depression – Acute coronary syndromes.<br />
Introduction<br />
Depression occurs <strong>com</strong>orbidly in patients hospitalized<br />
for a range <strong>of</strong> cardiac conditions and<br />
procedures. Most <strong>com</strong>monly, research has focused<br />
on <strong>the</strong> relationship between depression and myocardial<br />
infarction (MI); previous studies showed<br />
that post-MI patients have an incidence <strong>of</strong> 18%<br />
for meeting <strong>the</strong> criteria for major depressive disorder<br />
and an incidence <strong>of</strong> 27% for having significant<br />
depressive symptoms (Roose, 2001). However,<br />
similar high prevalence rates <strong>of</strong> depression have<br />
been reported in patients experiencing unstable<br />
angina and congestive heart failure (Friedman and<br />
Griffin, 2001) and in patients undergoing cardiac<br />
procedures such as coronary artery bypass graft<br />
(CABG) and angioplasty (Blumenthal et al, 2003).<br />
In <strong>the</strong> last decade many large-scale, wellcontrolled<br />
studies, in which initially healthy subjects<br />
were followed-up prospectively, have identified<br />
depression as a significant independent risk<br />
The Departments <strong>of</strong> Psychiatry and Cardiology, Ain Shams<br />
University.<br />
Manuscript received 30 Sep., 2009; revised 3 Nov., 2009;<br />
accepted 4 Nov., 2009.<br />
Address for Correspondence: Dr. Mona Ibrahim Awaad,<br />
The Department <strong>of</strong> Psychiatry, Ain Shams University.<br />
173<br />
factor for both first myocardial infarction (MI) and<br />
cardiovascular mortality, with an adjusted relative<br />
risk in <strong>the</strong> range <strong>of</strong> 1.5 to 2. Similarly, among<br />
individuals with established ischemic heart disease,<br />
depression has been found to be associated with<br />
an approximately 3- to 4-fold increase in <strong>the</strong> risk<br />
<strong>of</strong> subsequent cardiovascular morbidity and mortality<br />
(Glassman et al, 2002).<br />
Moreover, hospitalization for cardiac disease<br />
is associated with an increased risk for depression,<br />
which itself confers a poorer prognosis (Mayou et<br />
al, 2000). Few prospective studies have examined<br />
<strong>the</strong> determinants <strong>of</strong> depression after hospitalization<br />
in cardiac patients, and even fewer have examined<br />
depression within weeks after hospital discharge<br />
(Kaptien et al, 2006).<br />
Previous studies have reported that depression<br />
is associated with an increased risk <strong>of</strong> cardiac<br />
events in cardiovascular disease (CVD) patients<br />
and is known to increase <strong>the</strong> cost <strong>of</strong> patient care<br />
and decrease <strong>the</strong> quality <strong>of</strong> life. Even at low levels<br />
<strong>of</strong> severity, depressive symptoms are associated<br />
with increased risk for <strong>the</strong> incidence and recurrence<br />
<strong>of</strong> acute coronary syndromes (Bush et al, 2001),<br />
as well as all-cause mortality risk in patients with<br />
known heart disease increased by 60% (Roose,<br />
2003). Moreover, prospective epidemiologic studies<br />
have shown that depression is associated with an
Depression Post Acute Coronary Syndromes<br />
increase in risk independent <strong>of</strong> o<strong>the</strong>r known medical<br />
prognostic markers in this population (Davidson<br />
et al, 2006).<br />
The pathways to such negative out<strong>com</strong>es for<br />
depressed cardiac patients are unclear. Both biological<br />
and psychological explanations have been<br />
advanced, including serotonin-mediated platelet<br />
disturbances, sympa<strong>the</strong>tic nervous system dysfunction,<br />
poor treatment <strong>com</strong>pliance, and low motivation<br />
to change smoking habits or lifestyle (Lane<br />
et al, 2001). Findings indicative <strong>of</strong> hyperactivity<br />
<strong>of</strong> <strong>the</strong> hypothalamic-pituitary-adrenocortical axis,<br />
including elevated cerebrospinal fluid corticotropinreleasing<br />
factor levels, elevated plasma cortisol<br />
concentrations, and nonsuppression <strong>of</strong> cortisol<br />
secretion in response to dexamethasone administration,<br />
have been repeatedly reported in patients<br />
with major depression. In addition to elevated<br />
cortisol, many patients with depression also have<br />
elevated plasma and urinary catecholamine levels,<br />
indicating dysregulation <strong>of</strong> <strong>the</strong> autonomic nervous<br />
system. Imbalance between sympa<strong>the</strong>tic and parasympa<strong>the</strong>tic<br />
tone that results in sympa<strong>the</strong>tic overdrive<br />
predisposes patients with IHD to arrhythmia,<br />
ventricular fibrillation, and sudden cardiac death.<br />
Increased catecholamine activity may also increase<br />
platelet activation and aggregation, contributing<br />
to thrombus formation and may trigger an ischemic<br />
event (Carney et al, 2002).<br />
To date, few predictors <strong>of</strong> persistent depression<br />
in cardiac patients have been identified, apart from<br />
a past history <strong>of</strong> depression (Schrader et al, 2004).<br />
The recognition <strong>of</strong> factors connected with post<br />
infarct depressive symptoms has a significant role<br />
for rehabilitation in coronary heart disease (Krzyzkowiak,<br />
2007). Moreover, this will lead to identifying<br />
better treatments for depression in this population<br />
which could lead to improved medical,<br />
financial, and psychosocial out<strong>com</strong>es for those<br />
patients (Taylor et al, 2005).<br />
This study aimed to assess <strong>the</strong> incidence and<br />
predictors <strong>of</strong> depression after hospitalization for<br />
acute coronary syndromes (myocardial infarction<br />
and unstable angina) and to <strong>com</strong>pare <strong>the</strong> incidence<br />
<strong>of</strong> depression in patients with acute myocardial<br />
infarction (MI) and patients with unstable angina.<br />
Methodology<br />
Study population:<br />
The inclusion criteria included Patients older<br />
than 18 years <strong>of</strong> age, hospitalized for acute coronary<br />
174<br />
syndromes (including acute myocardial infarction<br />
or unstable angina).<br />
Exclusion criteria included patients with alcohol<br />
or substance abuse or dependence; psychotic symptoms,<br />
history <strong>of</strong> psychosis, organic brain syndrome.<br />
The study protocol was approved by <strong>the</strong> research<br />
<strong>com</strong>mittee <strong>of</strong> Alzhra Hospital, Almadina<br />
Almunawara, Kingdom Saudi Arabia, and informed<br />
consent <strong>of</strong> all subjects was obtained.<br />
Methods:<br />
For a diagnosis <strong>of</strong> acute MI, a patient must<br />
have met at least 1 criterion from each <strong>of</strong> <strong>the</strong><br />
following 2 categories. Category 1 criteria were:<br />
(a) creatine kinase isoenzyme MB (CK-MB) level<br />
greater than <strong>the</strong> upper limit <strong>of</strong> normal; (b) CK or<br />
troponin T or troponin I level more than 2 times<br />
<strong>the</strong> upper limit <strong>of</strong> normal; or (c) a total lactate<br />
dehydrogenase (LDH) level more than 1.5 times<br />
<strong>the</strong> upper limit <strong>of</strong> normal (with LDH 1 greater than<br />
LDH 2). Category 2 criteria were: (a) typical<br />
ischemic symptoms (chest pain or shortness <strong>of</strong><br />
breath) lasting for more than 10 minutes; or (b)<br />
electrocardiographic (ECG) evidence <strong>of</strong> ischemic<br />
ST-segment depression, ST-segment elevation, or<br />
new pathological Q waves.<br />
Alternatively, patients could enter <strong>the</strong> study if<br />
<strong>the</strong>y met <strong>the</strong> following criteria for unstable angina:<br />
(a) experienced angina or anginal equivalent symptoms<br />
at rest, with episodes lasting for at least 10<br />
minutes and leading to hospitalization, and had<br />
ECG documentation <strong>of</strong> transient ST-segment elevation<br />
or depression <strong>of</strong> more than 0.5mm, or had<br />
T-wave inversion <strong>of</strong> greater than 1mm within 12<br />
hours <strong>of</strong> an episode <strong>of</strong> chest pain; or (b) were<br />
hospitalized for symptoms <strong>of</strong> unstable angina and<br />
had known coronary artery disease with a documented<br />
history <strong>of</strong> a prior MI, had undergone a<br />
prior revascularization procedure, or had documented<br />
coronary artery stenosis greater than 75% in<br />
one <strong>of</strong> <strong>the</strong> major epicardial vessels.<br />
Psychiatric and covariate measures:<br />
Depression was measured using <strong>the</strong> Beck Depression<br />
Inventory (BDI) within 3 months after<br />
hospitalization for acute coronary syndromes. The<br />
Beck Depression Inventory (BDI) (Beck et al,<br />
1996): Created by Dr. Aaron T. Beck, is a 21question<br />
multiple-choice (scores range from 0 to<br />
63) self-report inventory that is one <strong>of</strong> <strong>the</strong> most<br />
widely used instruments for measuring <strong>the</strong> severity<br />
<strong>of</strong> depression. The most current version <strong>of</strong> <strong>the</strong>
Mona I Awaad & Khaled E Darahim<br />
questionnaire is designed for individuals aged 13<br />
and over and is <strong>com</strong>posed <strong>of</strong> items relating to<br />
depression symptoms such as hopelessness and<br />
irritability, cognitions such as guilt or feelings <strong>of</strong><br />
being punished, as well as physical symptoms such<br />
as fatigue, weight loss, and lack <strong>of</strong> interest in sex.<br />
There are three versions <strong>of</strong> <strong>the</strong> BDI-<strong>the</strong> original<br />
BDI, first published in 1961 and later revised in<br />
1971 as <strong>the</strong> BDI-1A, and <strong>the</strong> BDI-II, published in<br />
1996. The BDI is widely used as an assessment<br />
tool by healthcare pr<strong>of</strong>essionals and researchers<br />
in a variety <strong>of</strong> settings. Scores <strong>of</strong> 0 to 9 are considered<br />
minimal; 10 to 16 mild; 17 10 29 moderate;<br />
and 30 to 63 severe. A BDI score <strong>of</strong> 17 is frequently<br />
used to mark <strong>the</strong> presence <strong>of</strong> "subclinical" depression.<br />
Predictor variables, chosen with regard to evidence<br />
from previous research on <strong>com</strong>orbid depression,<br />
included demographic details (e.g. age, gender,<br />
marital status, employment, education) and<br />
cardiac and depression risk factors (e.g. selfreported<br />
smoking status, medical history "including;<br />
hypertension, diabetes, dyslipidymia, thyroid disorders,<br />
renal failure, and liver failure", past history<br />
<strong>of</strong> "including; myocardial infarction, angina, cardiac<br />
procedures, depression, anxiety or o<strong>the</strong>r psychiatric<br />
disorders") from <strong>the</strong> baseline questionnaire administered<br />
during hospitalization, as well as information<br />
from hospital administrative records on <strong>the</strong> index<br />
admission and o<strong>the</strong>r hospital admissions in <strong>the</strong><br />
previous 2 years.<br />
Patients are also interviewed for <strong>the</strong> social<br />
readjustment rating scale (SRRS), this scale is<br />
based on <strong>the</strong> premise that good and bad events in<br />
one's life can increase stress levels and make one<br />
more susceptible to illness and mental health problems.<br />
Each event should be considered if it has<br />
taken place in <strong>the</strong> last 12 months, <strong>the</strong>n add values<br />
to <strong>the</strong> right <strong>of</strong> each item to obtain <strong>the</strong> total score,<br />
scores
Depression Post Acute Coronary Syndromes<br />
Table 2: Comparison <strong>of</strong> <strong>the</strong> demographic, cardiac and psychiatric<br />
risk factors for depression.<br />
Age (years)<br />
Age category:<br />
18-54 years<br />
55-64 years<br />
>65 years<br />
Gender:<br />
Males<br />
Females<br />
Marital status:<br />
Not married<br />
Married<br />
Marital separation<br />
Education:<br />
Not educated<br />
Low education<br />
High education<br />
Occupation:<br />
Employed<br />
Unemployed<br />
Retired<br />
Smokers:<br />
Current smoker<br />
Ex smoker<br />
Never smoked<br />
Obesity (BMI >30)<br />
Hypertensive<br />
Diabetic<br />
Hypercholesterolemic<br />
PH <strong>of</strong> cardiac condition<br />
PH <strong>of</strong> cardiac procedure<br />
O<strong>the</strong>r medical condition<br />
PH <strong>of</strong> depression<br />
FH <strong>of</strong> Cardiac condition<br />
FH <strong>of</strong> depression<br />
Cardiac diagnosis:<br />
MI<br />
Unstable angina<br />
Depression<br />
(n=30)<br />
54.7±11.87<br />
18 (39.1%)<br />
8 (44.4%)<br />
4 (50%)<br />
21 (35%)<br />
9 (75%)<br />
1 (100%)<br />
19 (33.9%)<br />
10 (66.7%)<br />
19 (57.6%)<br />
2 (25%)<br />
9 (29%)<br />
15 (31.3%)<br />
9 (75%)<br />
6 (50%)<br />
10 (34.5%)<br />
7 (50%)<br />
13 (44.8%)<br />
13 (46.4%)<br />
11 (37.9%)<br />
13 (48.1%)<br />
25 (44.6%)<br />
10 (55.6%)<br />
16 (45.7%)<br />
1 (50%)<br />
5 (83.3%)<br />
7 (50%)<br />
1 (50%)<br />
11 (44%)<br />
19 (40.4%)<br />
No depression<br />
(n=42)<br />
50.6±8.92<br />
28 (60.9%)<br />
10 (55.6%)<br />
4 (50%)<br />
39 (65%)<br />
3 (25%)<br />
0 (0%)<br />
37 (66.1%)<br />
5 (33.3%)<br />
14 (42.4%)<br />
6 (75%)<br />
22 (71%)<br />
33 (68.7%)<br />
3 (25%)<br />
6 (50%)<br />
19 (65.5%)<br />
7 (50%)<br />
16 (56.2%)<br />
15 (53.6%)<br />
18 (62.1%)<br />
14 (51.9%)<br />
31 (55.4%)<br />
8 (44.4%)<br />
19 (54.3%)<br />
1 (50%)<br />
1 (16.7%)<br />
7 (50%)<br />
1 (50%)<br />
14 (56%)<br />
28 (59.6%)<br />
p<br />
value<br />
NS<br />
NS<br />
0.022<br />
0.036<br />
0.041<br />
0.019<br />
NS<br />
NS<br />
NS<br />
NS<br />
NS<br />
0.1<br />
NS<br />
NS<br />
0.042<br />
NS<br />
NS<br />
NS<br />
Data are expressed as a mean ± standard deviation or percent (%).<br />
FH = Family history.<br />
BMI = Body mass index.<br />
PH = Past history.<br />
NS = Non-significant.<br />
Table (3) presents <strong>the</strong> variables found to be<br />
statistically significant in <strong>the</strong> multivariate analysis;<br />
it showed that <strong>the</strong> independent predictors <strong>of</strong> depression<br />
post acute coronary syndrome were; having<br />
a past history <strong>of</strong> depression (OR 8.2), female<br />
gender (OR 5.6), and marital separation (OR 4.3).<br />
176<br />
Table 3: Multivariate predictors <strong>of</strong> depression post acute<br />
coronary syndrome.<br />
Predictors<br />
PH <strong>of</strong> Depression<br />
Gender (female)<br />
Marital status<br />
(unmarried/marital separation)<br />
Odds<br />
Ratio<br />
8.2<br />
5.57<br />
4.28<br />
Confidence<br />
interval<br />
0.91-74.29<br />
1.36-22.82<br />
1.29-14.13<br />
p<br />
value<br />
0.026<br />
0.037<br />
0.039<br />
However <strong>the</strong> independent predictors <strong>of</strong> moderate<br />
to severe depression post acute coronary syndrome<br />
were; having a past history <strong>of</strong> depression<br />
(OR 20.4), female gender (OR 17), marital separation<br />
(OR 4.6), and having past history <strong>of</strong> cardiac<br />
condition (OR 3.5) as shown in Table (4).<br />
Table 4: Multivariate predictors <strong>of</strong> moderate to severe depression<br />
post acute coronary syndrome.<br />
Predictors<br />
PH <strong>of</strong> Depression<br />
Gender (female)<br />
Marital status<br />
(unmarried/marital separation)<br />
Past history <strong>of</strong> cardiac condition<br />
Susceptibility to illness and mental health problems<br />
assessed by <strong>the</strong> social readjustment rating<br />
scale showed that in <strong>the</strong> group <strong>of</strong> patients with<br />
depression; low susceptibility was 40%, mild susceptibility<br />
was 56.7% and moderate susceptibility<br />
was 3.3%. While <strong>the</strong> group <strong>of</strong> patients without<br />
depression showed only low susceptibility (100%)<br />
as shown in Table (5).<br />
Table 5: Social readjustment rating scale <strong>of</strong> depressed patients<br />
post acute coronary syndrome.<br />
Social readjustment<br />
rating scale<br />
Low<br />
Mild<br />
Moderate<br />
Depression<br />
(n=30)<br />
12 (40%)<br />
17 (56.7%)<br />
1 (3.3%)<br />
Odds<br />
Ratio<br />
20.38<br />
17<br />
4.6<br />
3.5<br />
Data are expressed as a number (percent <strong>of</strong> <strong>the</strong> groups with or<br />
without depression)<br />
Discussion<br />
Confidence<br />
interval<br />
2.19-189.79<br />
3.84-75.16<br />
1.39-15.19<br />
1.11-11.18<br />
No depression<br />
(n=42)<br />
42 (100%)<br />
0 (0%)<br />
0 (0%)<br />
p<br />
value<br />
0.001<br />
0.000<br />
0.020<br />
0.056<br />
p<br />
value<br />
0.0001<br />
Depression in cardiac patients is well documented<br />
in <strong>the</strong> literature, studies have reported a low<br />
level <strong>of</strong> identification by physicians and very low<br />
levels <strong>of</strong> psychiatric intervention for this group<br />
(Graham and Hogg, 2002). Findings from recent<br />
intervention studies <strong>of</strong> depressed cardiac patients<br />
have underlined <strong>the</strong> need to identify cardiac patients
Mona I Awaad & Khaled E Darahim<br />
whose depression persists and who may be at risk<br />
<strong>of</strong> adverse health out<strong>com</strong>es (Schrader et al, 2004).<br />
Moreover, depression in patients with cardiovascular<br />
disease is a significant risk factor for developing<br />
symptomatic and fatal ischemic heart disease<br />
(van Melle, et al, 2004) and <strong>the</strong>y have higher than<br />
expected rate <strong>of</strong> sudden death (Roose, 2001). Few<br />
prospective studies have examined <strong>the</strong> determinants<br />
<strong>of</strong> depression after hospitalization in cardiac patients,<br />
and even fewer have examined depression<br />
within <strong>the</strong> weeks after hospital discharge (Davidson<br />
et al, 2006).<br />
Our results illustrate considerable fluidity in<br />
<strong>the</strong> level <strong>of</strong> depressive symptoms during <strong>the</strong> first<br />
3 months after hospitalization for acute coronary<br />
syndromes, where 41.7% had depressive symptoms<br />
and 25% <strong>of</strong> <strong>the</strong>m had moderate to severe depression<br />
according to <strong>the</strong> BDI score. These results matched<br />
<strong>the</strong> results <strong>of</strong> Ellis et al (2005), as <strong>the</strong>y found<br />
depressive symptoms in 40.2%<strong>of</strong> patients diagnosed<br />
with acute coronary syndrome, and with Schrader<br />
et al (2004), who found that 40% <strong>of</strong> patients experienced<br />
moderate to severe depression at 3 months<br />
after cardiac hospitalization, and were in consistent<br />
with Kaptein et al (2006), who found that 22.7%<br />
<strong>of</strong> patients had severe depressive symptoms post<br />
MI and <strong>the</strong> presence <strong>of</strong> <strong>the</strong>se depressive symptoms<br />
was relatively stable at 3 months and 12 months<br />
post MI. However, our study showed no statistical<br />
significance as regard <strong>the</strong> incidence <strong>of</strong> depression<br />
in patients with MI and those with unstable angina,<br />
and <strong>the</strong>y did not contribute to <strong>the</strong> prediction <strong>of</strong><br />
depression. This result was in agreement with a<br />
previous study reported that patients with unstable<br />
angina had similar prevalence rates <strong>of</strong> depression<br />
as patients with MI (Lesperance et al, 2000).<br />
Analysis <strong>of</strong> <strong>the</strong> social readjustment scale<br />
showed that patients with mild to moderate susceptibility<br />
to mental health problems were all<br />
having depressive symptoms, while only 22% <strong>of</strong><br />
those with low susceptibility showed depressive<br />
symptoms. It should be noted that marital separation,<br />
personal illness (including acute coronary<br />
syndromes), and unemployment (which we noted<br />
as predictors for depression in our study) are strong<br />
stressors in this scale with <strong>the</strong> highest point score.<br />
In our study <strong>the</strong> predictors <strong>of</strong> depression at 3<br />
months (for both mild and moderate to severe<br />
depression) were; female gender, marital separation<br />
(ei<strong>the</strong>r unmarried, divorced or widowed), not educated,<br />
unemployment and having past history <strong>of</strong><br />
177<br />
depression. However, our multinomial regression<br />
model showed that <strong>the</strong> independent predictors for<br />
both mild and moderate to severe depression were;<br />
female gender, marital separation and having past<br />
history <strong>of</strong> depression. The finding that female<br />
gender was a predictor <strong>of</strong> depression at 3 months<br />
post acute coronary syndrome was confirmed by<br />
a previous study that showed that female gender<br />
predicted depression in <strong>the</strong> early recovery period<br />
after hospitalization for acute coronary syndrome<br />
(Dunn et al, 2006).<br />
The finding that past history <strong>of</strong> depression was<br />
a strong predictor <strong>of</strong> depression at 3 months was<br />
in agreement with Lesperance et al (1996), who<br />
found that people with a history <strong>of</strong> previous major<br />
depression were more likely to be depressed after<br />
infarction both in hospital and after discharge.<br />
They argued that most efforts in settings with<br />
limited psychiatric resources should be directed<br />
toward post-MI patients with a history <strong>of</strong> depression.<br />
Fur<strong>the</strong>rmore, Glassman et al (2002), reported<br />
in <strong>the</strong> SADHART study that sertraline was found<br />
to be robustly superior to placebo only in cardiac<br />
patients who had a history <strong>of</strong> at least two prior<br />
episodes <strong>of</strong> depression.<br />
However, <strong>the</strong> independent predictors <strong>of</strong> mild<br />
depression post acute coronary syndrome were less<br />
clear, <strong>the</strong>refore, we analyzed <strong>the</strong> independent predictors<br />
for patients with moderate to severe depression<br />
which showed that <strong>the</strong> significant predictors<br />
were female gender, marital separation, having<br />
past history <strong>of</strong> depression, and having past history<br />
<strong>of</strong> cardiac condition. These results were in consistent<br />
with a previous study which found that significant<br />
variables associated with prevalence <strong>of</strong> depression<br />
post acute coronary syndrome were;<br />
female gender, past history <strong>of</strong> MI, and smoking<br />
(Nagvi et al, 2007).<br />
However, as regard <strong>the</strong> o<strong>the</strong>r variables we<br />
assessed (age, smoking status, obesity, hypertension,<br />
diabetes, past history <strong>of</strong> cardiac procedure,<br />
past history <strong>of</strong> anxiety or o<strong>the</strong>r psychiatric conditions,<br />
and family history <strong>of</strong> cardiac condition or<br />
psychiatric condition), we did not find significant<br />
correlations between <strong>the</strong>m and <strong>the</strong> incidence <strong>of</strong><br />
depression after acute coronary syndromes. These<br />
results were not in agreement with, The Identifying<br />
Depression as a Comorbid Condition IDACC)<br />
study (2003) prospectively examined depression<br />
in patients with a range <strong>of</strong> cardiac conditions,<br />
young age, female, divorced or separated, not
Depression Post Acute Coronary Syndromes<br />
employed, living alone, having a lower level <strong>of</strong><br />
education, and having poor health and quality <strong>of</strong><br />
life were risk factors for depression after admission<br />
for a cardiac condition. But most <strong>of</strong> <strong>the</strong> risk factors<br />
identified by <strong>the</strong> IDACC study have individually<br />
been associated with depression in o<strong>the</strong>r studies,<br />
and <strong>the</strong>y have not been reported as a group.<br />
Moreover, Schrader et al (2004), who found in<br />
<strong>the</strong>ir study that younger age, smoking status and<br />
past history <strong>of</strong> a cardiac condition were also significant<br />
predictors for depression after cardiac<br />
hospitalization. The association between smoking<br />
and an increased risk <strong>of</strong> depression at 3 months<br />
was consistent with evidence <strong>of</strong> increased risk <strong>of</strong><br />
major depression being associated with smoking<br />
(Ziegelstien et al, 2000). Such disagreement between<br />
our study and previous studies is perhaps<br />
attributable to <strong>the</strong> small sample size.<br />
In conclusion, our study demonstrated that <strong>the</strong><br />
independent predictors for depression (moderate<br />
to severe) within 3 months after acute coronary<br />
syndromes were; female gender, marital separation,<br />
having a past history <strong>of</strong> depression and having a<br />
past history <strong>of</strong> cardiac condition. It is noteworthy<br />
that <strong>the</strong>se 4 variables are routinely sought during<br />
patient history taking and <strong>the</strong>refore are readily<br />
accessible to clinicians. Screening hospitalized<br />
cardiac patients using a short checklist <strong>of</strong> risk<br />
factors in conjunction with a measure <strong>of</strong> depression<br />
severity may be a more efficacious method <strong>of</strong><br />
identifying those at risk <strong>of</strong> persistent depression<br />
than mass screening using a measure <strong>of</strong> depression<br />
severity alone. Targeting this group for close monitoring<br />
and management <strong>of</strong> depression may provide<br />
most benefits to patients and may represent a costefficient<br />
means <strong>of</strong> preventing adverse out<strong>com</strong>es<br />
associated with depression in cardiac patients.<br />
Therefore, <strong>the</strong>re is a need to develop practical ways<br />
to identify this substantial segment <strong>of</strong> population<br />
and provide pragmatic general-practitioner-based<br />
interventions for managing depression as a <strong>com</strong>orbid<br />
condition.<br />
References<br />
1- Beck AT, Steer RA, Brown GK: Manual for <strong>the</strong> BDI-II.<br />
San Antonio, TX, The Psychological Corporation 1996.<br />
2- Blumenthal JA, Lett HS, Babyak MA, White W, Smith<br />
PK, Mark DB, Jones R, Ma<strong>the</strong>w JP, Newman MF, for <strong>the</strong><br />
NORG investigators: Depression as a risk factor for<br />
mortality after coronary artery bypass surgery. Lancet<br />
2003; 362: 604-9.<br />
3- Bush DE, Ziegelstein RC, Tayback M, Richter D, Stevens<br />
S, Zahalsky H, Fauerbach JA: Even minimal symptoms<br />
178<br />
<strong>of</strong> depression increase mortality risk after acute myocardial<br />
infarction. Am J Cardiol 2001; 88: 337-41.<br />
4- Carney RM, Freedland KE, Miller GE, et al: Depression<br />
as a risk factor for cardiac mortality and morbidity: A<br />
review <strong>of</strong> potential mechanisms. J Psychosom Res 2002;<br />
53: 897-902.<br />
5- Cheok F, Schrader G, Banham D, Marker J, Hordacre A-<br />
L: Identification, course and treatment <strong>of</strong> depression<br />
following admission for a cardiac condition: Rationale<br />
and patient characteristics for <strong>the</strong> IDACC (Identifying<br />
Depression as a Comorbid Condition) project. Am Heart<br />
J 2003; 146: 978-84.<br />
6- Chew-Graham CA, Hogg T: Patients with chronic physical<br />
illness and co-existing psychological <strong>com</strong>orbidity: GPs’<br />
views on <strong>the</strong>ir role in detection and management. Prim<br />
Care Psychiatry 2002; 8: 35-9.<br />
7- Davidson KW, Kupfer DJ, Bigger JT, Califf RM, et al:<br />
Assessment and Treatment <strong>of</strong> Depression in Patients With<br />
Cardiovascular Disease: National Heart, Lung, and Blood<br />
Institute Working Group Report Psychosomatic Medicine<br />
2006; 68: 645-650.<br />
8- Dunn SL, Corser W, Stommel M, Holmes-Rovner M:<br />
Hopelessness and depression in <strong>the</strong> early recovery period<br />
after hospitalization for acute coronary syndrome. J<br />
Cardiopulm Rehabil 2006; May-Jun 26 (3): 152-9.<br />
9- Ellis JJ, Eagle KA, Kline-Rogers EM, Erickson SR:<br />
Depressive symptoms and treatment after acute coronary<br />
syndrome. Int J Cardiol 2005; Mar 30 (3): 443-7.<br />
10- Friedman MM, Griffin JA: Relationship <strong>of</strong> physical<br />
symptoms and physical functioning to depression in<br />
patients with heart failure. Heart Lung 2001; 30: 98-104.<br />
11- Glassman AH, O'Connor CM, Califf RM, Swedberg K,<br />
Schwartz P, J Thomas Bigger JT, Krishnan KRR, Zyl LT,<br />
Swenson JR, Finkel MS, Landau C, Shapiro PA, Pepine<br />
CJ, Mardekian J, and Harrison WM, for <strong>the</strong> Sertraline<br />
Antidepressant Heart Attack Randomized Trial<br />
(SADHART) Group: Sertraline Treatment <strong>of</strong> Major Depression<br />
in Patients With Acute MI or Unstable Angina;<br />
JAMA 2002; 288: 701-709.<br />
12- Holmes TH, Rahe RH: The social readjustment rating<br />
scale. Journal <strong>of</strong> Psychosomatic Research 1967; 11: 213-<br />
218.<br />
13- Hosmer DW, Lemeshow S: Applied logistic regression.<br />
New York: John Wiley & Sons, Inc 2000.<br />
14- Kaptein KI, Jonge P, Brink RHS, Korf J: Course <strong>of</strong><br />
Depressive Symptoms After Myocardial Infarction and<br />
Cardiac Prognosis: A Latent Class Analysis Psychosomatic<br />
Medicine 2006; 68: 662-668.<br />
15- Krzyzkowiak W: Depression after myocardial infarction<br />
and its psychosocial conditions. Psychiatr Pol 2007; 41<br />
(5): 679-91.<br />
16- Lane D, Carroll D, Ring C, Beevers DG, Lip GY: Predictors<br />
<strong>of</strong> attendance at cardiac rehabilitation after myocardial<br />
infarction. J Psychosom Res 2001; 51: 497-501.<br />
17- Lespérance F, Rieckmann N, Sheps DS, MSPH, Suls JM:<br />
Assessment and Treatment <strong>of</strong> Depression in Patients With
Mona I Awaad & Khaled E Darahim<br />
Cardiovascular Disease: National Heart, Lung, and Blood<br />
Institute Working Psychosomatic Medicine 2006; 68:<br />
645-650.<br />
18- Lesperance F, Frasure-Smith N, Juneau M, Theroux P:<br />
Depression and 1-year prognosis in unstable angina. Arch<br />
Intern Med 2000; 160: 1354-60.<br />
19- Lesperance F, Frasure-Smith N, Talajic M: Major depression<br />
before and after myocardial infarction: Its<br />
nature and consequences. Psychosom Med 1996; 58:<br />
99-110.<br />
20- Mayou RA, Gill D, Thompson DR, Nicolas Hicks AD,<br />
Volmink J, Neil A: Depression and anxiety as predictors<br />
<strong>of</strong> out<strong>com</strong>e after myocardial infarction. Psychosom Med<br />
2000; 62: 212-9.<br />
21- Naqvi TZ, Rafique AM, Andreas V, Rahban M, Mirocha<br />
J, Naqvi SS: Predictors <strong>of</strong> depressive symptoms postacute<br />
coronary syndrome. Gend Med 2007; Dec 4 (4):<br />
339-51.<br />
22- Roose SP: Depression, anxiety and cardiovascular system:<br />
The psychiatrist 's perspective. J Clin Psychiatry 2001;<br />
62 (Suppl 8): 19-22.<br />
179<br />
23- Rosse SP: Depression: Links With Ischemic Heart Disease<br />
and Erectile Dysfunction. J Clin Psychiatry 2003; 64<br />
(Suppl 10): 26-30.<br />
24- Schrader G, Cheok F, Hordacre A, Guiver N: Predictors<br />
<strong>of</strong> Depression Three Months After Cardiac Hospitalization<br />
Psychosomatic Medicine 2004; 66: 514-520.<br />
25- Taylor CB, Youngblood ME, Catellier D, Veith RC, Carney<br />
RM, et al, for <strong>the</strong> ENRICHD Investigators: Effects <strong>of</strong><br />
antidepressant medication on morbidity and mortality in<br />
depressed post-MI patients. Arch Gen Psychiatry 2005;<br />
62: 792-8.<br />
26- van Melle JP, de Jonge P, Spijkerman TA, Gijssen JGP,<br />
Ormel J, van Veldhuisen DJ, van den Brink RHS, van<br />
den Berg MP: Prognostic association <strong>of</strong> depression following<br />
myocardial infarction with mortality and cardiovascular<br />
events: A meta-analysis. Psychosom Med 2004;<br />
66: 814-22.<br />
27- Ziegelstein RC, Fauerbach JA, Stevens SS, Romanelli J,<br />
Richter DP, Bush DE: Patients with depression are less<br />
likely to follow re<strong>com</strong>mendations to reduce cardiac risk<br />
during recovery from a myocardial infarction. Arch Intern<br />
Med 2000; 160: 1818-23.
Egypt Heart J 62 (1): 181-186, March 2010<br />
Coronary Ectasia: Risk Markers and Risk Factors<br />
MAHMOUD ALI SOLIMAN, MD*; HOSAM M EL EZZAWY, MD**<br />
Introduction: Coronary artery ectasia represents a not un<strong>com</strong>mon entity <strong>of</strong> coronary artery disease. However, many<br />
unanswered questions remain regarding its aetiology, clinical sequalae and management.<br />
Aim <strong>of</strong> <strong>the</strong> Work: To assess risk markers namely high sensitivity CRP (HsCRP) and risk factors in patients with coronary<br />
ectasia and to <strong>com</strong>pare <strong>the</strong>m with those in patients with a<strong>the</strong>rosclerotic coronary artery disease.<br />
Subjects and Methods: The present study included 49 patients with coronary ectasia constituted <strong>the</strong> first group. Ano<strong>the</strong>r<br />
49 patients with a<strong>the</strong>rosclerotic coronary artery disease were randomly selected and constituted <strong>the</strong> second group.<br />
All patients underwent:<br />
• History taking, through clinical examination, ECG, Echocardiography.<br />
• Lab. Investigations: FBs & PPS, S. creatinine anti HCV & HBs antigen Lipidpr<strong>of</strong>ile, high sensitivity CRP, Coronary angiography<br />
by judkins's technique.<br />
Patients with acute coronary syndromes, peripheral arterial disease, valvular heart disease, local or systemic infectious,<br />
malignancies were excluded from <strong>the</strong> study.<br />
Results: There was no significant difference as regards age and sex between patients with coronary ectasia (group I) and<br />
patients with a<strong>the</strong>rosclerotic heart disease (group II) (p value >0.05).<br />
Patients with coronary ectasia have higher levels <strong>of</strong> Hs CRP (2.94±2.33 Vs 1.86±1.27, p
Coronary Ectasia: Risk Markers & Risk Factors<br />
Introduction<br />
Coronary artery ectasia was first described by<br />
Morgani many years ago [1]. Coronary artery ectasia<br />
has been defined as localized or diffuse non obstructive<br />
lesions <strong>of</strong> <strong>the</strong> epicardial coronary arteries,<br />
with a luminal dilation ≥1.5 times normal <strong>of</strong> <strong>the</strong><br />
adjacent segments or vessel diameter [2]. Coronary<br />
artery ectasia has been found in 1-5% during coronary<br />
angiography.<br />
In <strong>the</strong> largest series from <strong>the</strong> CASS registry,<br />
Swaye et al [2] found CAE in 4.9% <strong>of</strong> more than<br />
20000 coronary angiograms <strong>the</strong>y reviewed. The<br />
incidence <strong>of</strong> CAE in an Indian patients cohort with<br />
ischaemic heart disease has been reported to exceed<br />
10% [3]. The incidence <strong>of</strong> coronary ectasia among<br />
Egyptian patients is unknown and only a limited<br />
number <strong>of</strong> studies addressed this issue [4].<br />
The exact mechanism <strong>of</strong> coronary ecdtasia is<br />
still unknown and evidences suggest a <strong>com</strong>bination<br />
<strong>of</strong> genetic predisposition, <strong>com</strong>mon risk factors for<br />
coronary artery disease and abnormal vessel wall<br />
metabolism [5].<br />
Aim <strong>of</strong> <strong>the</strong> Work:<br />
To assess risk markers namely high sensitivity<br />
CRP (HsCRP) and risk factors in patients with<br />
coronary ectasia and to <strong>com</strong>pare <strong>the</strong>m with those<br />
in patients with a<strong>the</strong>rosclerotic coronary artery<br />
disease.<br />
Subjects and Methods<br />
The present study included 49 patients with<br />
coronary ectasia (group I) and 49 patients with<br />
a<strong>the</strong>rosclerotic coronary artery disease (group II)<br />
randomly selected from patients who underwent<br />
coronary angiography in our hospital.<br />
All patients underwent:<br />
History taking through clinical examination<br />
ECG. Echo cardiography.<br />
Lab. Investigations:<br />
FBs & PPS S. creatinine anti HCV & HBs<br />
antigen.<br />
Lipid pr<strong>of</strong>ile (total cholesterol, TG, HDL, LDL)<br />
was performed in Beckman Colter Synchron system<br />
CX9 ALX manufacture by Beckman Coulter Inc.<br />
California (UAS).<br />
High sensitivity CRP was performed in Turbi<br />
Quick manufacture by Vital Diagnostics S.r.l.<br />
(ITALY).<br />
182<br />
Coronary angiography was done by judkins's<br />
technique in multiple projections.<br />
Exclusion criteria:<br />
Patients with acute coronary syndromes, peripheral<br />
artery disease, valvular heart disease, local<br />
or systemic infections, malignancies were excluded<br />
from <strong>the</strong> study.<br />
Statistical analysis:<br />
The data collected were tabulated and analyzed<br />
by SPSS (statistical pakage for <strong>the</strong> social science<br />
s<strong>of</strong>t ware) version II on IBM <strong>com</strong>patible <strong>com</strong>puter.<br />
Quantitative data were expressed as mean &<br />
standard deriation (X±SD) and analyzed by applying<br />
t-test for <strong>com</strong>parison <strong>of</strong> two groups <strong>of</strong> normally<br />
distributed variables and mann whiteny U test for<br />
non normally distributed ones.<br />
Quatitative data were expressed as number &<br />
percentage and analyzed by applying chi-square<br />
test.<br />
Results<br />
There was no significant difference between<br />
patients coronary ectasia (group I) and patients<br />
with a<strong>the</strong>rosclerotic coronary artery disease (group<br />
II) as regards age and sex p value >0.05) Table<br />
(1).<br />
In patients with coronary ectasia (group I)<br />
hypertension and dyslipidaemia were more prevalent<br />
than in group II (79.6% Vs 59.2%, 59.1% Vs<br />
38.8% respectively, p value
Mahmoud Ali Soliman & Hosam M El Ezzawy<br />
When we <strong>com</strong>pare patients with single vessel<br />
ectasia with those with single vessel disease <strong>the</strong><br />
former have more triglyceride levels (p0.05) Tables (7,9).<br />
When we <strong>com</strong>pare patients with two or more<br />
vessel ectasia with those with two or more vessel<br />
disease, <strong>the</strong> former were older, more hypertensive<br />
& have significantly higher HsCRP p0.05<br />
>0.05<br />
0.05<br />
>0.05<br />
0.05<br />
p<br />
value<br />
0.05<br />
>0.05<br />
>0.05<br />
0.05<br />
0.05<br />
>0.05<br />
>0.05<br />
>0.05<br />
p<br />
value<br />
>0.05<br />
0.05<br />
>0.05<br />
>0.05<br />
0.05<br />
Odds<br />
ratio<br />
(95%CI)<br />
1.35<br />
0.42<br />
1.02<br />
1.28<br />
Odds<br />
ratio<br />
(95%CI)<br />
0.37<br />
5.0<br />
1.15<br />
0.28<br />
0.95<br />
2.17
Coronary Ectasia: Risk Markers & Risk Factors<br />
Table 5: Single vessel & two or more vessel affected among<br />
stable angia group regarding lipid pr<strong>of</strong>ile & CRP.<br />
Lipid<br />
pr<strong>of</strong>ile<br />
Age<br />
Chol<br />
TG<br />
HDL<br />
LDL<br />
Hs CRP<br />
* Mann whitey test.<br />
Single vessel<br />
(n=15)<br />
No. %<br />
52±5.55<br />
186.31±48.25<br />
111.46±26.53<br />
38.77±7.56<br />
123.77±51.03<br />
2.62±1.42<br />
Two or more<br />
(n=34)<br />
No. %<br />
54.44±8.03<br />
199.92±41.36<br />
152.42±57.43<br />
35.56±9.21<br />
131.56±44.06<br />
1.59±1.12<br />
t-test<br />
1.01<br />
0.97<br />
2.59*<br />
1.13<br />
0.37*<br />
2.36*<br />
p<br />
value<br />
>0.05<br />
>0.05<br />
0.05<br />
>0.05<br />
0.05<br />
>0.05<br />
>0.05<br />
>0.05<br />
>0.05<br />
>0.05<br />
p<br />
value<br />
0.05<br />
0.05<br />
>0.05<br />
>0.05<br />
Odds<br />
ratio<br />
(95%CI)<br />
1.29<br />
0.54<br />
2.4<br />
2.4<br />
184<br />
Table 8: Comparison between two or more vessel affected<br />
among group 1 & 2 regarding risk factors.<br />
Risk<br />
factors<br />
HTN:<br />
No<br />
Yes<br />
DM:<br />
No<br />
Yes<br />
Smoking:<br />
No<br />
Yes<br />
Lipid:<br />
No<br />
Yes<br />
FH:<br />
No<br />
Yes<br />
Statin use:<br />
No<br />
Yes<br />
Table 9: Single vessel among G1 & G2 regarding lipid pr<strong>of</strong>ile<br />
& CRP.<br />
Lipid<br />
pr<strong>of</strong>ile<br />
Age<br />
Chol<br />
TG<br />
HDL<br />
LDL<br />
Hs CRP<br />
* Mann whitey test.<br />
Single vessel<br />
in group I<br />
(n=15)<br />
53.67±7.14<br />
213.93±42.79<br />
158.33±45.69<br />
35.8±6.28<br />
150.8±39.33<br />
3.67±3.39<br />
Single vessel<br />
in group II<br />
(n=13)<br />
52±5.55<br />
186.31±48.25<br />
111.46±26.53<br />
38.77±7.56<br />
123.77±51.03<br />
2.62±1.42<br />
t-test<br />
0.68<br />
1.61<br />
3.25<br />
1.14<br />
0.13*<br />
0.75*<br />
p<br />
value<br />
>0.05<br />
>0.05<br />
0.05<br />
>0.05<br />
>0.05<br />
Table 10: Two or more vessel affected among G1 & G2<br />
regarding lipid pr<strong>of</strong>ile & CRP.<br />
Lipid<br />
pr<strong>of</strong>ile<br />
Age<br />
Chol<br />
TG<br />
HDL<br />
LDL<br />
Hs CRP<br />
Two or<br />
more<br />
vessels in<br />
group I<br />
(n=34)<br />
No. %<br />
4<br />
30<br />
30<br />
4<br />
12<br />
22<br />
14<br />
20<br />
34<br />
0<br />
26<br />
8<br />
11.8<br />
88.2<br />
88.2<br />
11.8<br />
35.3<br />
64.7<br />
41.2<br />
58.8<br />
100<br />
00<br />
76.5<br />
23.5<br />
2 or more VS in<br />
Group I<br />
(n=34) X±SD<br />
58.65±6.3<br />
215.47±49.59<br />
122.53±35.55<br />
40.0±9.18<br />
146.88±41.79<br />
2.62±1.62<br />
Two or<br />
more<br />
vessels in<br />
group II<br />
(n=36)<br />
No.<br />
14<br />
22<br />
27<br />
9<br />
6<br />
30<br />
22<br />
14<br />
31<br />
5<br />
16<br />
20<br />
%<br />
38.9<br />
61.1<br />
75<br />
25<br />
16.7<br />
83.3<br />
61.1<br />
38.9<br />
86.1<br />
13.9<br />
44.4<br />
55.6<br />
X 2<br />
6.74<br />
2.03<br />
3.18<br />
2.78<br />
5.09<br />
7.47<br />
2 or more VS in<br />
Group II<br />
(n=36) X±SD<br />
54.44±8.03<br />
199.92±41.36<br />
152.42±57.43<br />
35.56±9.21<br />
131.56±44.06<br />
1.59±1.12<br />
p<br />
value<br />
0.05<br />
>0.05<br />
>0.05<br />
Mahmoud Ali Soliman & Hosam M El Ezzawy<br />
Figure 1: Ecstatic LCX.<br />
Discussion<br />
Coronary artery ectasia has been defined as<br />
dilatation <strong>of</strong> a part or whole <strong>of</strong> <strong>the</strong> coronary artery<br />
1.5 times ore more <strong>the</strong> normal adjacent segment<br />
or <strong>the</strong> normal corresponding artery.<br />
Coronary ectasia has been found in 1-5% <strong>of</strong><br />
patients undergoing coronary angiography. It is<br />
<strong>com</strong>monly associated with a<strong>the</strong>rosclerotic artery<br />
disease, <strong>the</strong>refore it is considered as a variant <strong>of</strong><br />
coronary a<strong>the</strong>rosclerosis.<br />
Also, many studies have documented <strong>the</strong> association<br />
<strong>of</strong> coronary ectasia with <strong>the</strong> presence <strong>of</strong><br />
aneurysm in o<strong>the</strong>r vascular beds like <strong>the</strong> abdomenal<br />
aorta and popliteal arteries, probably owing to a<br />
<strong>com</strong>mon underlying pathogenetic mechanisms [6].<br />
However, many questions remain unanswered<br />
regarding its aetiology, pathogenesis, clinical sequala<br />
and management. In <strong>the</strong> present study, 49<br />
patients with coronary ectasia and 49 patients with<br />
a<strong>the</strong>rosclerotic coronary artery disease were enrolled.<br />
We assess risk markers namely HsCRP and<br />
o<strong>the</strong>r risk factors in both groups. There was no<br />
difference between both groups as regards age &<br />
sex so, any possible effect <strong>of</strong> age and gender could<br />
be excluded. The main finding is that patient with<br />
coronary ectasia have significantly higher levels<br />
<strong>of</strong> HsCRP than patients with a<strong>the</strong>rosclerotic artery<br />
disease in agreement with <strong>the</strong> results <strong>of</strong> Turbon H<br />
et al [7] in a series <strong>of</strong> 32 patients with isolated<br />
coronary ectasia and 32 patients with obstructive<br />
coronary artery disease.<br />
This finding support <strong>the</strong> potential role <strong>of</strong> inflammation<br />
in <strong>the</strong> pathogenesis <strong>of</strong> ectasia and may<br />
185<br />
open <strong>the</strong> door to anti-inflammatory agents and/or<br />
statins to be used in its management.<br />
Previous studies have reported inflammation<br />
to be an important <strong>com</strong>ponent <strong>of</strong> abdominal aneurysm<br />
formation as illustrated by extensive medial<br />
and advential inflammatory cell infiltrations [8,9].<br />
Also, Powell et al, showed that patients with<br />
abdominal aortic aneurysms had increased CRP<br />
[10]. Analysis <strong>of</strong> <strong>the</strong>se findings suggest a potential<br />
role <strong>of</strong> inflammation in <strong>the</strong> pathogenesis <strong>of</strong> both<br />
coronary ectasia & abdominal aortic aneorysms.<br />
Ano<strong>the</strong>r important findings in <strong>the</strong> present study<br />
is that in patients with coronary ectasia, hypertension<br />
<strong>the</strong>n dyslipidaemia were more prevalent than<br />
in patients with a<strong>the</strong>rosclerotic coronary artery<br />
disease.<br />
These findings agree with those reported by<br />
Nyamup et al [11] who studies 134 patients with<br />
coronary ectasia and reported hypertension in 54%<br />
and dyslipidaemia in 48% but, in <strong>the</strong>re study hypertnglycerdemia<br />
was <strong>the</strong> most <strong>com</strong>mon lipid<br />
abnormality (65% <strong>of</strong> patients). In our study, hypercholesterolemia<br />
was <strong>the</strong> most <strong>com</strong>mon abnormality<br />
and hypertriglyceridemia was only in those with<br />
signle vessel ectasia.<br />
These findings may point to <strong>the</strong> role <strong>of</strong> lipid<br />
abnormalities in <strong>the</strong> genesis <strong>of</strong> ectasia which <strong>com</strong>e<br />
in agreement with Sudhirk et al [12] who reported<br />
increased prevalence <strong>of</strong> coronary ectasia in patients<br />
with familial hypercholesterolemia.<br />
Limitations <strong>of</strong> <strong>the</strong> study:<br />
First, matching for Statin use was not optimal<br />
because patients in a<strong>the</strong>rosclerotic disease group<br />
were more on statin <strong>the</strong>rapy than ectasia group.<br />
Second, exclusion <strong>of</strong> peripheral artery disease was<br />
done on clinical basis only, but this was for both<br />
groups.<br />
In conclusion patients with coronary ectasia<br />
have higher levels <strong>of</strong> HsCRP, also hypertension<br />
and dyslipidaemia are more prevalent than in patients<br />
with a<strong>the</strong>rosclerotic coronary artery disease,<br />
whe<strong>the</strong>r this higher inflammatory state affect <strong>the</strong><br />
total risk and/or can be modulated by anti inflammatory<br />
agents, statins and ACE inhibitors, needed<br />
to be investigated.<br />
References<br />
1- Morgagni JB DE Sedbus, et al: Causis Morborum Per<br />
Anatomen Indaytis. Tomus Primus, Liber II, Epist 27,<br />
Article 28, Venetlis, 1761.
Coronary Ectasia: Risk Markers & Risk Factors<br />
2- Swaye PS, Fisher LD, Litwin P, Vignola PA, et al: Aneurysmal<br />
Coronary Artery Disease. Circulation 1983; 67:<br />
134-138.<br />
3- Sharmo SN, Kaul U, Wasiv HS, Rajani M, et al: Coronary<br />
Angiographic Pr<strong>of</strong>ile in Yaing and Old Indian Patients<br />
with Ischaemic Heart Disease: A Xomparative Study.<br />
Indion Theart J 1990; 42: 365-369.<br />
4- Waly HM, Elyda, MA, Lee VV, El Said G, Reul, GJ, Hall<br />
RJ: Coronary Artery Ectasia in Patients with Coronary<br />
Artery Disease. Tex Heart Ins J 1997; 24 (4).<br />
5- Athana Ssios M, Dennis V: Coronary Artery Ectasia:<br />
Imaging, Functional and Clinical Implications. Eur Heart<br />
J 2006; 27: 1026-1031.<br />
6- Befeler B, Aronda JM, Embi A, et al: Coronary Artery<br />
Aneusysms: Study <strong>of</strong> Their Aetiology Clinical Course,<br />
and Effect on Left Ventricular Function and Prognosis.<br />
Am J Med 1977; 62: 597-607.<br />
7- Turban H, Eraby A, Yasar A, et al: Comparison <strong>of</strong> C-<br />
186<br />
Reacdive Protein Levels In Patients Arith Coronary Artery<br />
Ectasia Versus Patients With Obstructive Coronary Artery<br />
Disease. Am J Cardial 2004; 94: 1303-1306.<br />
8- Brophy CM, Reilly JM, et al: The Role <strong>of</strong> Inflammation<br />
in Non Specific Abdominal Aortic Aneurysm Disease.<br />
Ann Vasc Surg 1991; 5: 229-233.<br />
9- Patel MI, Hardman DT, et al: Current Views <strong>of</strong> <strong>the</strong> Pathogenesis<br />
<strong>of</strong> Abdominal Aortic Aneurysm. J Am Collsury<br />
1995; 181: 371-382.<br />
10- Powell T, Muller BR, et al: Acute Phase Porticos in<br />
Patients with Abdominal Aortic Aneuryms. J Cardiovasc<br />
Surg 1987; 28: 528-530.<br />
11- Myamu P, Mullasori S, Joseph P, et al: The Prevalence<br />
and Clinical Pr<strong>of</strong>ile <strong>of</strong> Angiographic Coronary Ectasia.<br />
Asian Cardiovasc Thorac Ann 2003; 11: 122-126.<br />
12- Sudhir K, Ports TA, Amidon TM, et al: Increased Prevalence<br />
<strong>of</strong> Coronary Ectasia in hetrozygous Familial Hypercholesterolemia.<br />
Circulation 1995; 19: 1375-80.
Egypt Heart J 62 (1): 187-195, March 2010<br />
Usefulness <strong>of</strong> 2-Dimensional Mitral Valve Leaflets Separation Index<br />
as a New Technique for Assessment <strong>of</strong> Mitral Stenosis Severity:<br />
Comparison with Planimetry and PHT Methods<br />
HANY YOUNAN, MD<br />
Objective: To determine <strong>the</strong> usefulness <strong>of</strong> 2-Dimensional mitral valve leaflets separation index as a new technique for<br />
assessment <strong>of</strong> mitral stenosis severity.<br />
Patients and Methods: Our study included 55 patients with mitral stenosis who had undergone echocardiographic examination<br />
from July 2008 to March 2009 at Fayoum University hospital. Maximum separation <strong>of</strong> mitral leaflet tips in diastole in parasternal<br />
long-axis and apical 4-chamber views was measured and averaged to yield <strong>the</strong> mitral leaflet separation index. The index<br />
was <strong>com</strong>pared with mitral valve area determined by planimetry and pressures half-time methods.<br />
Results: Of <strong>the</strong> 55 study subjects, Eighteen patients had mild mitral stenosis (MVA 2.26±0.42cm 2 by PHT and 2.19±0.43cm 2<br />
by planimetry), 20 patients had moderate mitral stenosis (MVA 1.30±0.12cm 2 by PHT and 1.20±0.09cm 2 by planimetry) and<br />
17 patients had severe mitral stenosis (MVA 0.90±0.09cm 2 by PHT and 0.84±0.10cm 2 by planimetry). A MLS index <strong>of</strong> 0.975cm<br />
or more identified mild MS with 94.4% sensitivity, 78.4% specificity, 68% PPV, 96.7% NPV and 83.6% total accuracy, MLS<br />
index <strong>of</strong> 1.025cm or more identified mild MS with 88.9% sensitivity, 94.6% specificity, 88.9% PPV, 94.6% NPV and 92.7%<br />
total accuracy, and MLS index <strong>of</strong> 1.225cm or more identified mild MS with 83.3% sensitivity, 97.3% specificity, 93.8% PPV,<br />
92.3% NPV and 92.7% total accuracy. On <strong>the</strong> o<strong>the</strong>r hand, MLS index <strong>of</strong> 0.775cm or less identified severe MS with 88.2%<br />
sensitivity, 100% specificity, 100% PPV, 95% NPV and 96.4% total accuracy, and MLS index <strong>of</strong> 0.925cm or less identified<br />
severe MS with 94.1% sensitivity ,76.3% specificity, 64% PPV, 96.7% NPV and 81.8% total accuracy.<br />
Conclusions: The MLS index is an easy, accurate and reliable measure to estimate severity <strong>of</strong> MS, it provides a quick<br />
estimate <strong>of</strong> MS severity from standard 2D echocardiographic views without having to resort to tedious measurements.<br />
Key Words: Mitral leaflet separation index and mitral stenosis severity.<br />
Introduction<br />
In nearly all patients, valvular mitral stenosis<br />
(MS) is caused by rheumatic involvement <strong>of</strong> mitral<br />
valve. Echocardiography is <strong>the</strong> gold standard method<br />
for evaluating MS, obviating cardiac ca<strong>the</strong>terization<br />
(Jorge Solis et al, 2009 and Vimal Raj BS<br />
et al, 2008). Two-dimensional echocardiographic<br />
(2D) planimetry <strong>of</strong> <strong>the</strong> mitral valve orifice and<br />
pressure half-time (PHT) are <strong>the</strong> two most <strong>com</strong>monly<br />
used methods to estimate mitral valve orifice<br />
The Department <strong>of</strong> Cardiology, Faculty <strong>of</strong> Medicine,<br />
Fayoum University.<br />
Manuscript received 5 Nov., 2009; revised 10 Dec., 2009;<br />
accepted 12 Dec., 2009.<br />
Address for Correspondence: Dr. Hany Younan,<br />
Department <strong>of</strong> Cardiology Faculty <strong>of</strong> Medicine,<br />
Fayoum University, Email: azerhany@yahoo.<strong>com</strong>.<br />
187<br />
area. These two methods have an excellent concordance<br />
and, in most cases, can be used interchangeably<br />
(Jagdish C Mohan et al, 2004).<br />
Several studies have demonstrated that current<br />
echocardiographic techniques for estimating valve<br />
area in mitral stenosis have important limitations.<br />
In particular, <strong>the</strong> reliability <strong>of</strong> <strong>the</strong> pressure halftime<br />
method is reduced by conditions that alter<br />
left preload, Fur<strong>the</strong>rmore, because <strong>of</strong> <strong>the</strong> acute<br />
atrio-ventricular <strong>com</strong>pliance changes, <strong>the</strong> PHT<br />
method is reputed invalid immediately after percutaneous<br />
mitral <strong>com</strong>misurotomy (PMC) (Messika-<br />
Zeitouna D et al, 2005; Nishimura R et al, 1994;<br />
Abascal VM et al, 1988; Loyd D et al, 1988 and<br />
Grayburn PA et al, 1987).<br />
Similarly, leaflet calcification and poor parasternal<br />
windows impair <strong>the</strong> accuracy and feasibility
Usefulness <strong>of</strong> 2-Dimensional Mitral Valve Leaflets Separation Index<br />
<strong>of</strong> orifice planimetry (Martin RP et al, 1979 and<br />
Smith MD et al, 1986).<br />
Therefore, a simple and accurate method for<br />
<strong>the</strong> assessment <strong>of</strong> MS severity is desirable. The<br />
mitral leaflet separation (MLS) index, measuring<br />
<strong>the</strong> distance between <strong>the</strong> tips <strong>of</strong> <strong>the</strong> mitral leaflets<br />
in para-sternal long-axis and four-chamber views<br />
was recently presented as a reliable measure <strong>of</strong><br />
MS severity and as a surrogate for MVA (Caroline<br />
Holmin et al, 2007).<br />
Aim <strong>of</strong> <strong>the</strong> work:<br />
Our study aimed to determine <strong>the</strong> usefulness<br />
<strong>of</strong> 2-Dimensional mitral valve leaflets separation<br />
index as a new technique for assessment <strong>of</strong> mitral<br />
stenosis severity.<br />
Patients and Methods<br />
The study sample included 55 consecutive<br />
consenting patients with various grades <strong>of</strong> mitral<br />
stenosis undergoing echo Doppler study at Fayoum<br />
university hospital between July 2008 and March<br />
2009.<br />
Exclusion criteria:<br />
Patients were excluded:<br />
• If <strong>the</strong>y were not in sinus rhythm.<br />
• Heavily calcified mitral valve.<br />
• Associated moderate or severe mitral regurgitation.<br />
• Associated moderate or severe aortic valve disease.<br />
• Prior mitral <strong>com</strong>misurotomy in <strong>the</strong> preceding 6<br />
months.<br />
• Estimated right ventricular systolic pressure<br />
>75mmHg with right ventricular dilatation.<br />
• A suboptimal acoustic window.<br />
Each patient included in <strong>the</strong> study was subjected<br />
to:<br />
1- Careful history taking and thorough physical<br />
examination.<br />
2- Echo Doppler study.<br />
• Echocardiograms were recorded at rest, using<br />
General Electric-Vivid 3 expert and ACUSON<br />
CV70 Echo-Doppler machines equipped with<br />
a 2.5/3.25-MHz annular array transducer.<br />
188<br />
• Patients underwent a <strong>com</strong>plete echocardigraphic<br />
examination including 2-D transthoracic<br />
imaging, pulsed wave Doppler, continuous<br />
wave Doppler, and color flow mapping.<br />
• Two-dimensional echocardiographic planimetry<br />
<strong>of</strong> <strong>the</strong> mitral valve orifice area was carefully<br />
performed in para-sternal short-axis view<br />
at <strong>the</strong> leaflets tips with adjustment <strong>of</strong> <strong>the</strong><br />
probe for optimal mitral valve orifice.<br />
• Doppler examination <strong>of</strong> <strong>the</strong> mitral valve in<br />
<strong>the</strong> apical 4-chamber view to obtain diastolic<br />
trans-mitral velocity-time integral, peak and<br />
mean trans-mitral pressure gradients, and<br />
MVA by PHT.<br />
• Doppler interrogation <strong>of</strong> <strong>the</strong> regurgitant jet in<br />
2 orthogonal views (mild MR: mean color<br />
flow jet area in <strong>the</strong> left atrium 8cm 2 (Jagdish Mohan et al, 2004 and Zoghbi<br />
et al, 2003).<br />
• MS severity was determined using a <strong>com</strong>bination<br />
<strong>of</strong> planimetry and PHT methods. Severe<br />
MS was defined as a MVA <strong>of</strong> 1cm 2 or less by<br />
planimetry or pressure half-time method<br />
and/or a mean trans-mitral gradient <strong>of</strong> greater<br />
than 10mmHg. Moderate MS was defined as<br />
a MVA between 1cm 2 and 1.5cm 2 by planimetry<br />
or pressure half-time method, with a mean<br />
trans-mitral gradient <strong>of</strong> 5 to 10mmHg. Mild<br />
MS was defined as a MVA <strong>of</strong> greater than<br />
1.5cm 2 by planimetry or pressure half-time<br />
and/or a trans-mitral gradient <strong>of</strong> less than<br />
5mmHg (Seow et al, 2006).<br />
• The MLS index was estimated by measuring<br />
<strong>the</strong> maximal separation <strong>of</strong> tip <strong>of</strong> <strong>the</strong> mitral<br />
leaflets in end diastole in para-sternal long<br />
axis (PLAX) view and in apical 4-chamber<br />
view (A4C view). 3 measurements were obtained<br />
in PLAX view and three in A4C view.<br />
A mean <strong>of</strong> this was taken as MLS index. MLS<br />
index was <strong>com</strong>pared with MVA assessed by<br />
planimetry and PHT.<br />
Statistical analysis:<br />
Statistical analyses were performed using <strong>the</strong><br />
Statistical Program for Social Sciences (SPSS Inc,<br />
version 12.0).
Hany Younan<br />
Quantitative data were expressed as mean ±<br />
standard deviation.<br />
Qualitative data were expressed as absolute<br />
number (percentage).<br />
The MLS index was correlated using linear<br />
regression analysis against MVA by planimetry<br />
and <strong>the</strong> pressure half-time methods.<br />
Receiver operating characteristic (ROC) curves<br />
were used to determine <strong>the</strong> values <strong>of</strong> MLS index<br />
that predicted mild and severe MS with <strong>the</strong> best<br />
sensitivity and specificity. The diagnostic values<br />
<strong>of</strong> various thresholds <strong>of</strong> MLS index were expressed<br />
as sensitivity, specificity, positive predictive value<br />
(PPV), and negative predictive value (NPV).<br />
Results<br />
In this study 55 patients were enrolled. The<br />
mean age <strong>of</strong> <strong>the</strong> patients was 32.7±8.9 years, and<br />
60% were female. All <strong>the</strong> patients were in sinus<br />
rhythm, 20% <strong>of</strong> patients were in New York Heart<br />
Association functional class II, 40% in class III<br />
and 20% in class IV; four patients were pregnant<br />
at <strong>the</strong> time <strong>of</strong> echocardiographic examination.<br />
Eighteen patients had mild mitral stenosis (MVA<br />
2.26±0.42cm 2 by PHT and 2.19±0.43cm 2 by<br />
planimetry), 20 had moderate mitral stenosis (MVA<br />
1.30±0.12cm 2 by PHT and 1.20±0.09cm 2 by<br />
planimetry) and 17 had severe mitral stenosis<br />
(MVA 0.90±0.09cm 2 by PHT and 0.84±0.10cm 2<br />
by planimetry) (Figs. 3,4).<br />
The PG was significantly different for patients<br />
with mild (9.38±1.75mmHg), moderate (15.15±<br />
2.18mmHg), and severe MS (22.52±3.42mmHg<br />
cm) and was significantly higher in patients with<br />
severe MS <strong>com</strong>pared with mild MS (p
Usefulness <strong>of</strong> 2-Dimensional Mitral Valve Leaflets Separation Index<br />
4.1<br />
3.1<br />
2.1<br />
1.1<br />
0.1<br />
Mild stenosis Moderate stenosis Severe stenosis<br />
Figure 4: Comparison <strong>of</strong> MVA by planimetry in <strong>the</strong> study<br />
group.<br />
MSI index (cm)<br />
MSI index (cm)<br />
1.50<br />
1.00<br />
0.50<br />
0.00<br />
1.50<br />
1.25<br />
1.00<br />
0.75<br />
0.50<br />
Mild MS Moderate MS Severe MS<br />
MS severity<br />
Figure 5: Correlation between MLS index and MS severity.<br />
p-value
Hany Younan<br />
Image 1-A: MVA by PHT in a patient with mild MS. Image 1-B: MVA by Planimetry in <strong>the</strong> same patient with mild<br />
MS.<br />
Image 1-C: MLS in PLX in <strong>the</strong> same patient with mild MS. Image 1-D: MLS in apical 4-C view in <strong>the</strong> same patient with<br />
mild MS.<br />
Image 2-A: MVA by PHT in a patient with moderate MS. Image 2-B: MVA by Planimetry in <strong>the</strong> same patient with<br />
moderate MS.<br />
191
Usefulness <strong>of</strong> 2-Dimensional Mitral Valve Leaflets Separation Index<br />
Image 2-C: MLS in PLX in <strong>the</strong> same patient with moderate<br />
MS.<br />
A MLS index <strong>of</strong> 0.975cm or more identified<br />
mild MS with 94.4 % sensitivity, 78.4% specificity,<br />
68% PPV, 96.7% NPV and 83.6% total accuracy,<br />
MLS index <strong>of</strong> 1.025cm or more identified mild<br />
MS with 88.9% sensitivity, 94.6% specificity,<br />
88.9% PPV, 94.6% NPV and 92.7% total accuracy,<br />
and MLS index <strong>of</strong> 1.225cm or more identified mild<br />
192<br />
Image 2-D: MLS in apical 4-C view in <strong>the</strong> same patient with<br />
moderate MS.<br />
Image 3-A: MVA by PHT in a patient with severe MS. Image 3-B: MVA by Planimetry in <strong>the</strong> same patient with<br />
severe MS.<br />
Image 3-C: MLS in PLX in <strong>the</strong> same patient with severe MS. Image 3-D: MLS in apical 4-C view in <strong>the</strong> same patient with<br />
severe MS.<br />
MS with 83.3% sensitivity, 97.3% specificity,<br />
93.8% PPV, 92.3% NPV and 92.7% total accuracy<br />
(Table 1).<br />
On <strong>the</strong> o<strong>the</strong>r hand, MLS index <strong>of</strong> 0.775cm or<br />
less identified severe MS with 88.2% sensitivity,<br />
100% specificity, 100% PPV, 95% NPV and 96.4%
Hany Younan<br />
total accuracy, and MLS index <strong>of</strong> 0.925cm or less<br />
identified severe MS with 94.1% sensitivity, 76.3%<br />
Table 1: MLS index cut <strong>of</strong>f points for detection <strong>of</strong> mild M.<br />
MLS index<br />
Cut-<strong>of</strong>f<br />
points<br />
0.975 cm<br />
1.025 cm<br />
1.225 cm<br />
Sensitivity Specificity PPV<br />
0.944<br />
0.889<br />
0.833<br />
0.784<br />
0.946<br />
0.973<br />
Discussion<br />
68%<br />
88.9%<br />
93.8%<br />
NPV<br />
96.7%<br />
94.6%<br />
92.3%<br />
Total<br />
accuracy<br />
83.6%<br />
92.7%<br />
92.7%<br />
MVA is most <strong>of</strong>ten measured non-invasively<br />
by Doppler echocardiography. Four different methods<br />
can be used: Planimetry, PHT, continuity equation<br />
and <strong>the</strong> proximal iso-velocity surface area<br />
method (PISA), each method has its specific limitations<br />
(Messika-Zeitouna D et al, 2008).<br />
Planimetry provides an anatomical measurement<br />
<strong>of</strong> <strong>the</strong> mitral valve orifice; it is considered to be<br />
<strong>the</strong> reference method and correlates closely with<br />
anatomical findings (Faletra F et al, 1996 and<br />
Palacios IF, 1994). The procedure requires an<br />
experienced operator because minor changes to<br />
<strong>the</strong> depth or angle <strong>of</strong> <strong>the</strong> ultrasound beam may<br />
lead to significant MVA overestimation (Binder<br />
TM et al, 2000). Planimetry may not be feasible<br />
in approximately 5% <strong>of</strong> patients because <strong>of</strong> a poor<br />
echocardiographic window or massive calcifications<br />
(Lung B et al, 1994).<br />
The PHT is <strong>the</strong> time interval between <strong>the</strong> maximum<br />
early diastolic gradient and <strong>the</strong> point at<br />
which <strong>the</strong> gradient is half this maximum value.<br />
The main advantage <strong>of</strong> PHT is its simplicity (MVA=<br />
220/PHT); However tachycardia and non-linear<br />
Doppler velocity curves affect <strong>the</strong> accuracy and<br />
reliability <strong>of</strong> PHT measurements (Voelker W et al,<br />
1992 and Gonzalez MA et al, 1987). In addition,<br />
a major assumption <strong>of</strong> <strong>the</strong> PHT method is that <strong>the</strong><br />
rate <strong>of</strong> pressure decline is only determined by <strong>the</strong><br />
valve area (and not by <strong>the</strong> left atrial and ventricular<br />
<strong>com</strong>pliance) consequently, <strong>the</strong> PHT method is<br />
reputed invalid immediately after percutaneous<br />
mitral <strong>com</strong>misurotomy (PMC) (Thomas JD et al,<br />
1988).<br />
In clinical practice, correlation between planimetry<br />
and PHT is only fair, with discrepancies greater<br />
than or equal to 0.3cm 2 observed in 20% <strong>of</strong> patients.<br />
Fisher et al, in 1979 had first suggested that<br />
<strong>the</strong> separation <strong>of</strong> mitral leaflets could be used to<br />
193<br />
specificity, 64% PPV, 96.7% NPV and 81.8% total<br />
accuracy (Table 2).<br />
Table 2: MLS index cut <strong>of</strong>f points for detection <strong>of</strong> severe<br />
MS.<br />
MLS index<br />
Cut-<strong>of</strong>f<br />
points<br />
0.775 cm<br />
0.925 cm<br />
Sensitivity Specificity<br />
0.882<br />
0.941<br />
1.000<br />
0.763<br />
PPV<br />
100%<br />
64%<br />
NPV<br />
95%<br />
96.7%<br />
Total<br />
accuracy<br />
96.4%<br />
81.8%<br />
measure severity <strong>of</strong> MS, He measured <strong>the</strong> maximum<br />
diastolic separation <strong>of</strong> <strong>the</strong> mitral valve leaflets<br />
by M-mode echocardiography in 44 patients and<br />
found a good correlation with MVA obtained invasively<br />
using Gorlin formula. As <strong>the</strong> mitral valve<br />
is a 3-dimensional structure, measuring leaflet<br />
separation using 2D echocardiography would be<br />
more accurate.<br />
In our study we found that MLS index measured<br />
by 2-D echocardiography is an easy, accurate and<br />
reliable measure to estimate <strong>the</strong> severity <strong>of</strong> MS<br />
and correlated well with MVA by planimetry and<br />
pressure half-time method. The MLS index was<br />
significantly different for patients with mild MS<br />
(1.34±0.19cm), moderate MS (0.96±0.11cm), and<br />
severe MS (0.68±0.12cm), significantly lower in<br />
patients with severe MS <strong>com</strong>pared with mild MS<br />
(p.001) and demonstrated excellent correlation<br />
with MVA by pressure half-time and planimetry<br />
(r=0.809 and p
Usefulness <strong>of</strong> 2-Dimensional Mitral Valve Leaflets Separation Index<br />
planimetry (r=0.93, p
Hany Younan<br />
16- Palacios IF: What is <strong>the</strong> gold standard to measure mitral<br />
valve area post-mitral balloon valvuloplasty? Ca<strong>the</strong>ter<br />
Cardiovascular Diagnosis 1994; 33 (4): 315-6.<br />
17- Smith MD, Handshoc R, Handshoe S, Kwan OL De-Maria<br />
AN: Comparative accuracy <strong>of</strong> two dimensional echocardiography<br />
and Doppler pressure halftime methods in<br />
assessing <strong>the</strong> severity <strong>of</strong> mitral stenosis in patients with<br />
and without prior <strong>com</strong>misurotomy. Circulation 1986; 73:<br />
100-7.<br />
18- Seow SC, Koh LP, Yeo TC: Hemodynamic significance<br />
<strong>of</strong> mitral stenosis: Use <strong>of</strong> a simple, novel index by 2dimensional<br />
echocardiography. J Am Soc Echocardiography<br />
2006 Jan; 19 (1): 102-6.<br />
19- Thomas JD, Wilkins GT, Choong CY: Inaccuracy <strong>of</strong> mitral<br />
pressure half-time immediately after percutaneous mitral<br />
195<br />
valvotomy. Dependence on trans-mitral gradient and left<br />
atrial and ventricular <strong>com</strong>pliance. Circulation 1988; 78<br />
(4): 980-93.<br />
20- Vimal Raj BS, Paul George, Jacob Jose V: Mitral Leaflet<br />
Separation Index-A Simple Novel Index to Assess <strong>the</strong><br />
Severity <strong>of</strong> Mitral Stenosis. Indian Heart J 2008; 60: 563-<br />
566.<br />
21- Voelker W, Regele B, Dittmann H: Effect <strong>of</strong> heart rate on<br />
trans-mitral flow velocity pr<strong>of</strong>ile and Doppler measurements<br />
<strong>of</strong> mitral valve area in patients with mitral stenosis.<br />
Eur Heart J 1992; 13 (2): 152-9.<br />
22- Zoghbi WA, Enriquez-Sarano M, Foster E: Re<strong>com</strong>mendations<br />
for evaluation <strong>of</strong> <strong>the</strong> severity <strong>of</strong> native valvular<br />
regurgitation with two-dimensional and Doppler echocardiography.<br />
Am Soc Echocardiography 2003; 16 (7): 77.
Egypt Heart J 62 (1): 197-204, March 2010<br />
Thrombin-Activatable Fibrinolysis Inhibitor Thr325Ile Polymorphism<br />
as a Risk Factor <strong>of</strong> Myocardial Infarction in Egyptians<br />
HANAN M KAMAL, MD; AMAL S AHMED, MD*; MANAL S FAWZY, MD**;<br />
FATEN A MOHAMED, MD***; AMANI A ELBAZ, MD***<br />
Thrombin activatable fibrinolysis inhibitor (TAFI) is an important inhibitor <strong>of</strong> fibrinolysis that decreases plasminogen<br />
binding to <strong>the</strong> fibrin surface. The plasma TAFI concentration is almost entirely genetically determined. We investigated whe<strong>the</strong>r<br />
TAFI Thr325Ile polymorphisms could constitute a risk marker <strong>of</strong> myocardial infarction (MI) in Egyptian patients.<br />
Patients and Methods: Forty six unrelated patients with acute myocardial infarction (MI) aged 37-67 years, (mean age<br />
55.7±8.1 years, male: female 33:13) and age, sex-matched unrelated healthy volunteers (n=54) as a control group were included<br />
in this study. All study groups subjected to thorough clinical and laboratory investigation, electrocardiographic examination<br />
and/or echocardiography. TAFI Thr325Ile (reference sequence: rs1926447) polymorphism was genotyped in both studied groups<br />
using TaqMan SNP (single nucleotide polymorphism) genotyping assay. We also examined <strong>the</strong> impact <strong>of</strong> this variant on <strong>the</strong><br />
studied clinical and laboratory traits.<br />
Results: TAFI Ile325Ile (TT) genotype was significantly more frequent in patients with acute MI <strong>com</strong>pared to control group<br />
[OR: 4.95; (95% CI: 1.80-13.63); p=0.0001]. Also high risk T allele frequency was significantly higher in MI patients <strong>com</strong>pared<br />
to controls, [OR: 3.26 (95% CI: 1.82-5.83); p=0.001]. No statistically significant relation was found between TAFI Thr325Ile<br />
polymorphism and ei<strong>the</strong>r <strong>the</strong> type nor <strong>the</strong> site <strong>of</strong> MI. In MI patients high risk T allele frequency was significantly higher in<br />
diabetics <strong>com</strong>pared to non-diabetics (p=0.04). O<strong>the</strong>r risk factors showed no relation with <strong>the</strong> genotyping in studied patients.<br />
Conclusions: This study indicated that TAFI Thr325Ile (rs1926447) could have a contribution to MI risk in Egyptian<br />
population. Fur<strong>the</strong>r investigation <strong>of</strong> <strong>the</strong> interaction between this gene and o<strong>the</strong>r susceptibility genes in large scale association<br />
studies in this region, will provide useful information for better understanding <strong>of</strong> <strong>the</strong> impact <strong>of</strong> this gene in <strong>the</strong> development<br />
<strong>of</strong> acute coronary syndrome (ACS).<br />
Key Words: Thrombin activatable fibrinolytic inhibitor – Myocardial infarction – Genetic polymorphism – Egyptians.<br />
Introduction<br />
Discovering <strong>the</strong> mechanisms that determine <strong>the</strong><br />
grade or persistence <strong>of</strong> coronary thrombosis in<br />
acute coronary syndrome (ACS) would have implications<br />
for <strong>the</strong> prevention and treatment <strong>of</strong><br />
coronary a<strong>the</strong>rosclerosis. The hemostatic system<br />
plays a central role in <strong>the</strong> pathogenesis <strong>of</strong> ACS<br />
and many studies suggest that vulnerability to<br />
The Departments <strong>of</strong> Cardiology, Clinical Pathology*,<br />
Biochemistry** and Physiology***, Faculty <strong>of</strong> Medicine,<br />
Suez Canal University, Ismailia, Egypt.<br />
Manuscript received 2 Jan., 2010; revised 30 Jan., 2010; accpted<br />
2 Feb., 2010.<br />
Address for Correspondence: Dr. Hanan Mohamed Kamal,<br />
Department <strong>of</strong> Cardiology, Faculty <strong>of</strong> Medicine, Suez Canal<br />
University, Ismailia, Egypt,<br />
E-mail: hananmkamal@yahoo.<strong>com</strong>.<br />
197<br />
a<strong>the</strong>rothrombosis may be modulated by individual<br />
variations in <strong>the</strong> balance between coagulation and<br />
fibrinolysis [1].<br />
Impaired fibrinolysis might be a risk factor for<br />
arterial thrombotic events [2] and a <strong>com</strong>mon feature<br />
<strong>of</strong> ACS in <strong>com</strong>parison with stable angina [3]. The<br />
main inhibitors <strong>of</strong> fibrinolysis are PAI-1 (type-1<br />
plasminogen activator inhibitor) and TAFI (thrombin-activatable<br />
fibrinolysis inhibitor). TAFI is a<br />
procarboxypeptidase that attenuates fibrinolysis<br />
by removing carboxy-terminal lysine residues from<br />
partially degraded fibrin, inhibiting <strong>the</strong> assembly<br />
<strong>of</strong> fibrinolytic factors on <strong>the</strong> fibrin surface [4].<br />
The plasma TAFI concentration is almost entirely<br />
genetically determined. Non-modifiable<br />
factors such as polymorphisms in <strong>the</strong> genes encoding<br />
<strong>the</strong>se proteins that may affect <strong>the</strong>ir structure,
Thrombin-Activatable Fibrinolysis Inhibitor Thr325Ile Polymorphism<br />
concentration, or function, might have an influence<br />
in <strong>the</strong> balance between coagulation and fibrinolysis<br />
and should be investigated to help identify a subset<br />
<strong>of</strong> patients at higher risk.<br />
Several single nucleotide polymorphisms<br />
(SNPs) <strong>of</strong> <strong>the</strong> TAFI gene have been identified [5].<br />
Plasma TAFI levels or function have been related<br />
to <strong>the</strong>se polymorphisms, <strong>of</strong> which <strong>the</strong> mostthoroughly-studied<br />
are two polymorphisms in <strong>the</strong><br />
coding region that result in amino acid substitutions,<br />
Ala147Thr (505A/G), and Thr325Ile (1040C/T)<br />
[6,7].<br />
The genotype, 1040C/T SNP, which results in<br />
<strong>the</strong> conversion <strong>of</strong> a threonine codon (ACU) to an<br />
Isolucine codon (AUU) at a position 325<br />
(Thr325Ile) is <strong>of</strong> particular interest since it is<br />
associated with increased antifibrinolytic activity<br />
[7-9]. Pharmacological inhibition <strong>of</strong> <strong>the</strong> TAFI pathway<br />
may constitute a novel strategy to prevent<br />
thrombosis or to increase <strong>the</strong> efficacy <strong>of</strong> thrombolytic<br />
<strong>the</strong>rapy [10].<br />
Recently, biological functions <strong>of</strong> TAFI distinct<br />
from fibrinolysis regulation have been described,<br />
including regulation <strong>of</strong> inflammation, blood pressure,<br />
cell migration, and wound healing [10]. These<br />
functions may depend on substrates <strong>of</strong> TAFI o<strong>the</strong>r<br />
than fibrin, for instance bradykinin, <strong>the</strong> anaphylatoxins<br />
C3a and C5a, annexin II, and osteopontin<br />
[11,12].<br />
As <strong>the</strong>re are a limited number <strong>of</strong> studies on <strong>the</strong><br />
genetic basis <strong>of</strong> ACS in Egyptian population, this<br />
study aimed to determine <strong>the</strong> frequency <strong>of</strong> allelic<br />
variant in <strong>the</strong> TAFI Thr325Ile (rs1926447) gene<br />
in Suez Canal region. In <strong>com</strong>bination with o<strong>the</strong>r<br />
genetic and non-genetic data, this could be helpful<br />
in refining a risk pr<strong>of</strong>ile for coronary heart disease<br />
patients in order to determine <strong>the</strong> need for and <strong>the</strong><br />
intensity <strong>of</strong> follow-up or to influence decisions<br />
about staged implementation <strong>of</strong> preventive interventions<br />
with behavioral or drug <strong>the</strong>rapy.<br />
Subjects and Methods<br />
Patient group: We prospectively recruited forty<br />
six unrelated Egyptian patients with acute myocardial<br />
infarction [33 (72%) male, 13 (28%) female,<br />
aged 37-67 years, mean age 55.7±8.1 years] from<br />
<strong>the</strong> Cardiology Department <strong>of</strong> Suez Canal University<br />
Hospital (Egypt). Diagnosis <strong>of</strong> patients with<br />
acute MI was based on full history taking, clinical<br />
examination, resting ECG, cardiac enzymes and<br />
echocardiography. Myocardial infarction (MI) was<br />
198<br />
defined ei<strong>the</strong>r by presence <strong>of</strong> ST-segment elevation<br />
(STE) or depression (non-STE) ≥1mm in two or<br />
more contiguous leads. In leads V 2 and V 3, 2mm<br />
<strong>of</strong> ST elevation in men and 1.5mm in women was<br />
required, and troponin I levels >0.1ng/mL. In <strong>the</strong><br />
acute setting all <strong>the</strong> patients received aspirin,<br />
nitroglycerin, morphine and thrombolytic <strong>the</strong>rapy<br />
as indicated [4,13].<br />
Control group: Fifty four unrelated healthy<br />
blood donors were included as control (38 males,<br />
16 females) <strong>the</strong>y had no history <strong>of</strong> coronary heart<br />
disease and had normal resting ECG. Their ages<br />
range from 38 to 64 years (mean 50.2±6.2 years).<br />
The following variables were recorded: Diabetes<br />
(defined as patients receiving insulin or oral<br />
hypoglycemic drugs or with fasting glycemia<br />
>200mg/dL at admission or >126mg/dl in two<br />
determinations); hypertension (defined as repeated<br />
blood pressure ≥140/90mmHg or previous treatment<br />
with antihypertensive drugs); dyslipidemia<br />
(defined as total cholesterol >220mg/dl, triglycerides<br />
>150mg/dl or treatment with lipid lowering<br />
drugs), smoking and family history <strong>of</strong> cardiovascular<br />
disease. The study was approved by <strong>the</strong><br />
institutional review <strong>board</strong> (IRB) <strong>of</strong> Suez Canal<br />
University. Written informed consent was obtained<br />
from all participants.<br />
Echocardiography was performed in <strong>the</strong><br />
echocardiography laboratory <strong>of</strong> Suez Canal University<br />
Hospital using Vivid-7 Dimension echocardiographic<br />
unite (GE Vingmend Ultrasound,<br />
Horten, Norway) with a multi-frequency probe<br />
ranging between 1.7 and 3.4 MHz. M-mode, Two-<br />
Dimensional and Doppler echocardiographic measurements<br />
with color flow imaging were made. All<br />
cardiac dimensions and functions were calculated<br />
[14].<br />
Laboratory methods: Fasting blood glucose<br />
(FBG) was determined by glucose oxidase method<br />
[15] (Trinder, 1969). Fasting serum total cholesterol<br />
(TC), high density lipoprotein (HDL)-cholesterol<br />
and serum triglycerides (TG) were determined by<br />
<strong>the</strong> enzymatic method using Hitachi 912 system.<br />
Low density lipoprotein cholesterol (LDL-C) value<br />
was calculated with <strong>the</strong> Friedewald's equation [16]<br />
(Onaka, 1993).<br />
Genotyping: Genomic DNA was extracted from<br />
peripheral blood leukocytes using <strong>the</strong> Wizard®<br />
Genomic DNA Purification Kit (Promega Co.),<br />
quantified by absorbance at 260nm using Nano-
Hanan M Kamal, et al<br />
drop-1000 spectrophotometer (NanoDrop Tech.,<br />
Wilmington, USA) and stored at –20°C. TAFI<br />
Thr325Ile SNP, rs1926447 was genotyped using a<br />
real-time PCR allelic discrimination TaqMan assay<br />
(Applied Biosystems, California, USA) [17] (Livak,<br />
et al, 1999). The primer sequences were AGCT-<br />
CAAAGTTCTCTAA-GATCATAAGAAGA (forward)<br />
and AGTCTCTAGTAGCCAGTGAAG-<br />
CAGTTC (reverse) and <strong>the</strong> TaqMan probe<br />
sequences were Thr-probe: (VIC)-TTTACTA<br />
GTTT-TCTCAATAGCA-(MGB) and Ile-probe:<br />
(FAM)-TTTTACTAATTTTCTCAATAG-CA-<br />
(MGB) (polymorphism in bold) [18]. PCR reaction<br />
was carried out in a 25ml containing 20ng <strong>of</strong> sample<br />
DNA, 12.5ml <strong>of</strong> TaqMan Universal PCR Master<br />
Mix, and 1.25ml <strong>of</strong> TaqMan SNP genotyping assay<br />
Mix. Appropriate negative controls were also run.<br />
Real-time PCR was performed on Rotor-Gene 6000<br />
(Corbett Research, Australia) using <strong>the</strong> following<br />
conditions: two initial holds (50°C for 2min and<br />
95°C for 10min) followed by a 40-cycle two-step<br />
PCR (95°C denaturation for 15 s and annealing/extension<br />
60°C for 1min) [18]. Genotyping was<br />
performed blinded to case/control status. Ten per<br />
cent <strong>of</strong> <strong>the</strong> randomly selected samples were regenotyped<br />
in separate runs to exclude <strong>the</strong> possibility<br />
<strong>of</strong> false genotype calls.<br />
Statistical analysis: The genotypes and alleles<br />
frequencies <strong>of</strong> <strong>the</strong> studied polymorphism in TAFI<br />
gene were calculated by counting. Consistency <strong>of</strong><br />
genotype frequencies at TAFI (C1040T) Polymorphism<br />
with Hardy-Weinberg equilibrium was tested<br />
on a contingency table <strong>of</strong> observed and expected<br />
genotype frequencies using <strong>the</strong> Markov simulationbased<br />
goodness <strong>of</strong> fit. Continuous trait data are<br />
shown as mean ± SD unless o<strong>the</strong>rwise specified.<br />
Comparison <strong>of</strong> allelic and genotypes frequencies<br />
between groups, and association <strong>of</strong> polymorphism<br />
with quantitative traits were examined for statistical<br />
significance using standard Pearson chi-square test<br />
(χ 2) or Fisher’s exact test where appropriate. The<br />
odds ratio (OR) was calculated by means <strong>of</strong> logistic<br />
regression and <strong>the</strong> confidence interval (CI) was<br />
calculated at <strong>the</strong> 95% level. Data were analyzed<br />
by Texas<strong>of</strong>t WINKS, 4.651 s<strong>of</strong>tware (Texas<strong>of</strong>t,<br />
Texas, USA). Statistical significance was assumed<br />
for P values less than 0.05.<br />
Results<br />
Study population characteristics: Table (1)<br />
showed <strong>the</strong> demographic details and basic laboratory<br />
parameters <strong>of</strong> <strong>the</strong> MI patients and controls.<br />
Patients were insignificantly different from controls<br />
199<br />
as regards age and sex. However, as <strong>com</strong>pared<br />
with normal subjects, MI patients had significant<br />
higher levels <strong>of</strong> FBG, total cholesterol, TG and<br />
LDL-C. Also, BMI was significantly increased in<br />
MI patients.<br />
Forty (87%) patients had STEMI, and only 6<br />
(13%) had non-STEMI. Seventeen (36%) had anterior<br />
MI, 21 (45%) had inferior MI and 2 (4%)<br />
has lateral MI. All patients with STE developed a<br />
Q-wave MI. Twenty three (50%) patients were<br />
smokers, 22 (48%) had diabetes, 34 (74%) had<br />
dyslipidemia, 26 (56%) had hypertension, and 15<br />
(32%) had a recorded family history <strong>of</strong> cardiovascular<br />
disease.<br />
The Echocardiographic characteristics <strong>of</strong> <strong>the</strong><br />
study population was shown in Table (2). Left<br />
ventricular systolic function was estimated to be<br />
normal in 23 (50%) patients, mildly depressed in<br />
9 (20%) patients, moderately depressed in 12 (26%)<br />
and severely depressed in only 2 (4%) patients.<br />
Diastolic dysfunction was diagnosed in 44 (95%)<br />
patients, 24 (52%) had grade I diastolic dysfunction,<br />
12 (26%) had grade II dysfunction and 3 (7%)<br />
patients had grade III dysfunction. Left ventricular<br />
dilatation was reported in 20 (43%) <strong>of</strong> patients.<br />
Genotype and Allele Frequencies among MI patients<br />
and controls:<br />
Table (3) Summarized <strong>the</strong> genotype and allele<br />
frequencies among MI patients and controls and<br />
<strong>the</strong> results <strong>of</strong> genotypic association analysis for<br />
<strong>the</strong> studied SNP. In MI patient group, <strong>the</strong> distribution<br />
<strong>of</strong> three genotypes CC, CT, and TT were 13%,<br />
54.4%, and 32.6%, respectively, and <strong>the</strong> frequency<br />
<strong>of</strong> high risk allele T was 60%. In healthy control<br />
group, <strong>the</strong> genotype distribution <strong>of</strong> CC, CT, and<br />
TT were 42.6%, 51.8%, and 5.6% respectively,<br />
and <strong>the</strong> T allele frequency was 31.5%. It was<br />
confirmed that <strong>the</strong> genotype proportions <strong>of</strong> both<br />
studied groups fit <strong>the</strong> Hardy-Weinberg equilibrium<br />
estimated with a χ 2 test (p>0.05). The genotype<br />
carrying <strong>the</strong> risk allele [Thr/Ile (CT) and Ile/Ile<br />
(TT)] was significantly more frequent in patients<br />
with acute MI <strong>com</strong>pared to control group (OR:<br />
4.95; [95% CI: 1.80-13.63]; p=0.0001). High risk<br />
T allele frequency was higher in CHD patients<br />
<strong>com</strong>pared to controls, [OR=3.26, 95% (CI=1.82-<br />
5.83), p=0.001].<br />
Genotype and MI patients: No significant<br />
relation was found between TAFI polymorphism<br />
and both type or site <strong>of</strong> MI (p>0.05).
Thrombin-Activatable Fibrinolysis Inhibitor Thr325Ile Polymorphism<br />
Genotype and risk factors: High risk T allele<br />
frequency was significantly higher in diabetic<br />
<strong>com</strong>pared to non-diabetic in MI patients (p=0.04).<br />
However o<strong>the</strong>r risk factors showed no significant<br />
relation regarding <strong>the</strong> patients' genotyping.<br />
Table 1: Clinical and laboratory characteristics <strong>of</strong> study<br />
population.<br />
Sex (male/female)<br />
Age at study (years)<br />
Systolic blood pressure*<br />
Diastolic blood pressure<br />
BMI (kg/m 2 )*<br />
FBG (mg/dl)*<br />
Cholesterol (mg/dl)*<br />
TG (mg/dl)*<br />
HDL-C (mg/dl)<br />
LDL-C (mg/dl)*<br />
Patient (n=46)<br />
(mean ± SD)<br />
33/13<br />
55.7±8.1<br />
(37.0-67.0)<br />
136.7±17.8<br />
(100-180)<br />
89.1±10.9<br />
(65-110)<br />
28.1±3.7<br />
(22.0-38.0)<br />
173.3±74.6<br />
(78.0-340.0)<br />
211.1± 52.8<br />
(120.0-424.0)<br />
142.4±73.5<br />
(47.0-473.0)<br />
42.1±13.4<br />
(20.0-77.0)<br />
137.1±46.9<br />
(65.0-339.0)<br />
Control (n=54)<br />
(mean ± SD)<br />
38/16<br />
50.2±6.2<br />
(38.0-64.0)<br />
123±1.7<br />
(95-150)<br />
81.2±8.3<br />
(61-100)<br />
25.1±1.6<br />
(21.6-27.1)<br />
100.3±14.6<br />
(53.0-130.0)<br />
202.1±16.7<br />
(179.0-241.0)<br />
100.2±30.2<br />
(61.0-182.0)<br />
78. 6±13.6<br />
(54.0-123.0)<br />
103.2±19.6<br />
(63.0-155.0)<br />
Abbreviations: BMI Body mass index, FBG fasting blood glucose,<br />
TG triglycerides, HDL high density lipoprotein cholesterol, LDL low<br />
density lipoprotein cholesterol. * p
Hanan M Kamal, et al<br />
centrations were more frequent in cases in France,<br />
but more frequent in controls in Nor<strong>the</strong>rn Ireland<br />
[20].<br />
This polymorphism is <strong>of</strong> particular interest<br />
because, besides its association with TAFI plasma<br />
levels, studies using re<strong>com</strong>binant proteins have<br />
demonstrated a functional effect <strong>of</strong> <strong>the</strong> Thr325Ile<br />
substitution on <strong>the</strong> stability <strong>of</strong> activated TAFI<br />
(TAFIa species with a prolonged half-life at 37°C),<br />
resulting in altered antifibrinolytic activity [9]. The<br />
presence <strong>of</strong> <strong>the</strong> Ile at position 325 results in a 30-<br />
60% greater antifibrinolytic effect for TAFIa than<br />
<strong>the</strong> Thr at this position [9]. Many studies showed<br />
that The TT (Ile/Ile) genotype <strong>of</strong> <strong>the</strong> Thr325Ile<br />
polymorphism showed lower TAFI Ag and TAFI<br />
activity levels.<br />
The increased antifibrinolytic potential <strong>of</strong> Ile-<br />
325-containing TAFIa variants reflects <strong>the</strong> fact that<br />
<strong>the</strong>se variants have an increased ability to suppress<br />
<strong>the</strong> up-regulation in plasminogen activation that<br />
normally occurs during fibrinolysis. In turn, differences<br />
in plasminogen activation are explained<br />
by TAFIa mediated lysine release. Thus, TAFIa<br />
variants containing Ile at position 325 release twice<br />
as much lysine during fibrinolysis as variants<br />
containing Thr at this position. It is possible in<br />
vivo that if <strong>the</strong> ability to suppress plasminogen<br />
activation and <strong>the</strong> antifibrinolytic potential <strong>of</strong> TAFI<br />
were to be increased, <strong>the</strong> dynamic balance between<br />
accretion and lysis <strong>of</strong> a clot could be shifted toward<br />
accretion and <strong>the</strong>refore thrombosis [9].<br />
In <strong>the</strong> case <strong>of</strong> <strong>the</strong> Ile-325 variant <strong>of</strong> TAFI,<br />
changing <strong>the</strong> hydrophilic Thr residue to a hydrophobic<br />
Ile residue may diminish <strong>the</strong> effect <strong>of</strong> <strong>the</strong><br />
favorable entropic change that ac<strong>com</strong>panies <strong>the</strong><br />
inactivation process, <strong>the</strong>reby stabilizing TAFIa.<br />
Possibly, this increased stability <strong>of</strong> TAFIa <strong>com</strong>pensates<br />
for <strong>the</strong> decreased levels <strong>of</strong> <strong>the</strong> protein.<br />
Discrepant findings have also been reported<br />
with respect to <strong>the</strong> association <strong>of</strong> TAFI concentrations<br />
or genotype and arterial vascular disease.<br />
Early studies found slight elevations in plasma<br />
TAFI concentrations (measured as total potential<br />
TAFIa by an activity assay) in patients with stable<br />
angina pectoris [21]. In some studies, high TAFI<br />
levels were found to be protective against MI [22],<br />
while in o<strong>the</strong>rs <strong>the</strong>y were associated with increased<br />
risk <strong>of</strong> coronary disease [20,23] or no association<br />
with arterial thrombosis has been found [24,25].<br />
In Egypt El-Shafie, et al (2008), <strong>com</strong>pared <strong>the</strong><br />
effect <strong>of</strong> TAFI gene polymorphism (Ala 147Thr)<br />
201<br />
with <strong>the</strong> severity <strong>of</strong> coronary artery disease in<br />
patients with IHD, <strong>the</strong>y concluded that polymorphism<br />
<strong>of</strong> TAFI gene had influence on plasma TAFI<br />
level but was not associated with <strong>the</strong> risk <strong>of</strong> CHD<br />
or with coronary events [26].<br />
Two studies have examined <strong>the</strong> TAFI pathway<br />
as a risk factor for restenosis after coronary angioplasty<br />
or stenting: Both lower plasma TAFI antigen<br />
concentrations and <strong>the</strong> more stable Ile/Ile genotype<br />
at position 325 were associated with a lower rate<br />
<strong>of</strong> restenosis [27,28].<br />
A partial explanation for <strong>the</strong>se discrepancies<br />
could be differences in <strong>the</strong> type <strong>of</strong> patient included<br />
(young survivors <strong>of</strong> a MI [22], patients with ACS<br />
[23,25], or angina [20], <strong>the</strong> time <strong>of</strong> sampling (baseline<br />
[20,25] or acute phase [23,25] or in <strong>the</strong> methods<br />
used to measure TAFI antigenic [20] or functional<br />
[23]. The effect <strong>of</strong> TAFI polymorphisms on TAFI<br />
antigen levels is unclear, since variable antibody<br />
reactivity to TAFI is<strong>of</strong>orms in some TAFI antigen<br />
ELISA techniques underestimates real plasma TAFI<br />
levels when an Ile is located at position 325 [29-<br />
31].<br />
Since we have no TAFI levels in this study to<br />
show <strong>the</strong> association between its levels and MI,<br />
<strong>the</strong> interpretation for our results is limited. We<br />
explored only <strong>the</strong> associations between <strong>the</strong> polymorphism<br />
and MI by genotype analysis.<br />
Importantly, underestimation <strong>of</strong> <strong>the</strong> Ile/Ile in<br />
<strong>the</strong> <strong>com</strong>mercially available antigen assays will<br />
result in erroneous conclusions with regard to TAFI<br />
levels in patients samples. Obviously, this has to<br />
be taken into account for any analysis on <strong>the</strong> association<br />
between TAFI levels and cardiovascular<br />
pathologies [29].<br />
The importance <strong>of</strong> this phenomenon is even<br />
more stressed because <strong>the</strong> most stable variant,<br />
exhibiting a more pronounced antifibrinolytic effect<br />
is being underestimated [9].<br />
Meltzer, et al proposed that a dose response<br />
association was found between TAFI levels and<br />
myocardial infarction. In o<strong>the</strong>r words, <strong>the</strong>re might<br />
be a threshold, above which levels <strong>of</strong> TAFI protect<br />
against myocardial infarction [19].<br />
In <strong>the</strong> present study no statistically significant<br />
relation was found between TAFI Thr325Ile polymorphism<br />
and ei<strong>the</strong>r <strong>the</strong> type nor <strong>the</strong> site <strong>of</strong> MI.<br />
Tàssies, et al, 2009, found that TAFI allele<br />
325Ile, associated with lower TAFI levels, were
Thrombin-Activatable Fibrinolysis Inhibitor Thr325Ile Polymorphism<br />
associated with non-STE ACS (non Q wave MI<br />
and unstable angina) in <strong>com</strong>parison with STE ACS.<br />
This study showed that in patients with MI high<br />
risk T allele frequency was significantly higher in<br />
diabetics <strong>com</strong>pared to non-diabetics. However<br />
o<strong>the</strong>r risk factors showed no significant relation<br />
regarding <strong>the</strong> patients' genotyping.<br />
The contradictory results from epidemiological<br />
studies may be explained by two opposite effects<br />
<strong>of</strong> TAFI on <strong>the</strong> development <strong>of</strong> arterial thrombosis.<br />
While <strong>the</strong> association between high levels <strong>of</strong> TAFI<br />
and arterial thrombosis may be <strong>the</strong> result <strong>of</strong> a<br />
hyp<strong>of</strong>ibrinolytic state, <strong>the</strong> association between low<br />
TAFI levels and arterial thrombosis may be explained<br />
by a defective regulation <strong>of</strong> inflammation.<br />
Ano<strong>the</strong>r explanation <strong>of</strong> <strong>the</strong> contradictory results<br />
could be <strong>the</strong> use <strong>of</strong> different methods for measuring<br />
TAFI. Several different antigen assays as well as<br />
distinct activity assays have been used in epidemiological<br />
studies.<br />
With <strong>the</strong> discovery that some enzyme linked<br />
immunosorbent assays <strong>of</strong> TAFI antigen are dependent<br />
on <strong>the</strong> 1040C/T polymorphism, revealing a<br />
lack <strong>of</strong> reactivity with <strong>the</strong> 1040T variant [19], even<br />
more caution is required in <strong>the</strong> interpretation <strong>of</strong><br />
results.<br />
Although TAFI has been shown to inhibit fibrinolysis<br />
in vivo, recent studies suggest that TAFI<br />
plays an important role in regulating <strong>com</strong>plementmediated<br />
vascular inflammation in vivo. TAFI<br />
inhibits inflammation in vivo by inactivating <strong>the</strong><br />
inflammatory mediators bradykinin and <strong>the</strong> anaphylatoxins<br />
C3a and C5a [11]. Fur<strong>the</strong>rmore,<br />
TAFI–/– plasminogen+/– mice expressed increased<br />
leukocyte migration <strong>com</strong>pared with <strong>the</strong>ir wild-type<br />
counterparts in a model <strong>of</strong> peritoneal inflammation<br />
[32]. In ano<strong>the</strong>r study, TAFI-deficient mice, primed<br />
by lipopolysaccharide, showed increased mortality<br />
after infusion <strong>of</strong> cobra venom factor, which is a<br />
potent non-specific activator <strong>of</strong> <strong>com</strong>plement proteins<br />
[33]. Based on <strong>the</strong>se results, one might expect<br />
that TAFI-deficient mice would have a more rapid<br />
progression <strong>of</strong> a<strong>the</strong>rosclerosis, in which inflammation<br />
plays a pivotal role. However, no data on<br />
a<strong>the</strong>rosclerosis progression in TAFI knockout mice<br />
are available. As inflammation plays an important<br />
role in <strong>the</strong> development <strong>of</strong> a<strong>the</strong>rosclerosis and<br />
arterial thrombosis [34] it is not implausible that<br />
increased TAFI levels decrease <strong>the</strong> risk <strong>of</strong> myocardial<br />
infarction by decreasing <strong>the</strong> inflammatory<br />
response. These two counteracting effects may<br />
202<br />
also explain <strong>the</strong> conflicting study results on TAFI<br />
and arterial thrombosis, and, because inflammation<br />
is less important in venous disease, <strong>the</strong> consistent<br />
relation between high TAFI levels and venous<br />
thrombosis risk.<br />
There is also evidence that TAFI binds to collagen<br />
resulting in reduced platelet adhesion to<br />
collagen under flow conditions, [35] which could<br />
also contribute to <strong>the</strong> protective effect <strong>of</strong> TAFI.<br />
With <strong>the</strong> advent <strong>of</strong> more accurate assays for<br />
measurement <strong>of</strong> plasma TAFI concentrations, <strong>the</strong><br />
stage is set for major advances in our understanding<br />
<strong>of</strong> <strong>the</strong> contribution <strong>of</strong> <strong>the</strong> TAFI pathway to vascular<br />
disease, and <strong>of</strong> <strong>the</strong> molecular genetics <strong>of</strong> CPB2,<br />
<strong>the</strong> gene encoding TAFI. This will form <strong>the</strong> basis<br />
for <strong>the</strong> development <strong>of</strong> <strong>the</strong>rapeutic strategies to<br />
manipulate <strong>the</strong> TAFI pathway in order to ameliorate<br />
or prevent vascular disease. Moreover, CPB2 genotype,<br />
plasma TAFI concentrations, and functional<br />
TAFI levels may be able to be used to identify<br />
individuals at high risk for developing vascular<br />
disease.<br />
Conclusion<br />
These data provide evidence that TAFI<br />
Thr325Ile SNP, (rs1926447) could be one <strong>of</strong> <strong>the</strong><br />
genetic factors that increase <strong>the</strong> risk for MI in<br />
Egyptian population. However, to assess <strong>the</strong> applicability<br />
<strong>of</strong> <strong>the</strong>se findings to <strong>the</strong> general population,<br />
fur<strong>the</strong>r extensive large scale and prospective cohort<br />
studies with functional analysis in several localities<br />
are re<strong>com</strong>mended in Egyptians. In addition, many<br />
fur<strong>the</strong>r studies will be required to examine <strong>the</strong><br />
efficacy <strong>of</strong> preventive measures in groups with<br />
high-risk genotypes before any immediate rush to<br />
use this information to give individual predictions<br />
<strong>of</strong> disease risk.<br />
Acknowledgements: We thank all <strong>the</strong> patients<br />
and control subjects for agreeing to join this work.<br />
References<br />
1- Libby P, Theroux P: Pathophysiology <strong>of</strong> coronary artery<br />
disease. Circulation 2005; 111: 3481-8.<br />
2- Hamsten A, Wiman B, de Faire U, Blombäck M: Increased<br />
plasma levels <strong>of</strong> a rapid inhibitor <strong>of</strong> tissue plasminogen<br />
activator inhibitor in young survivors <strong>of</strong> myocardial<br />
infarction. N Eng J Med 1985; 313: 1557-63.<br />
3- Undas A, Szuldrzynski K, Stepien E, Zalewski J, Godlewski<br />
J, Tracz W, et al: Reduced clot permeability and susceptibility<br />
to lysis in patients with acute coronary syndrome:<br />
Effects <strong>of</strong> inflammation and oxidative stress. A<strong>the</strong>rosclerosis<br />
2008; 196: 551-7.
Hanan M Kamal, et al<br />
4- Tàssies D, Merce Roqué M, Monteagudo J , Martorell T,<br />
Sionis A, Arzamendi D, Heras M, Reverter JC: Thrombinactivatable<br />
fibrinolysis inhibitor genetic polymorphisms<br />
as markers <strong>of</strong> <strong>the</strong> type <strong>of</strong> acute coronary syndrome.<br />
Thrombosis Research 2009; 124: 614-618.<br />
5- Wang W, B<strong>of</strong>fa PB, Bajzar L, Walker JB, Nesheim ME:<br />
A study <strong>of</strong> <strong>the</strong> mechanism <strong>of</strong> inhibition <strong>of</strong> fibrinolysis by<br />
activated thrombin-activatable fibrinolysis inhibitor. J<br />
Biol Chem 1998; 273: 27176-81.<br />
6- Zhao L, Morser J, Bajzar L, Nesheim M, Nagashima M:<br />
Identification and characterization <strong>of</strong> two thrombinactivatable<br />
fibrinolysis inhibitor is<strong>of</strong>orms. Thromb Haemost<br />
1998; 80: 949-55.<br />
7- Brouwers GJ, Vos HL, Leebeek FW, Bulk S, Schneider<br />
M, B<strong>of</strong>fa M, et al: A novel, possibly functional, single<br />
nucleotide polymorphism in <strong>the</strong> coding region <strong>of</strong> <strong>the</strong><br />
thrombin activatable fibrinolysis inhibitor (TAFI) gene<br />
is also associated with TAFI levels. Blood 2001; 98: 1992-<br />
3.<br />
8- Henry M, Aubert H, Morange PE, Nanni I, Alessi MC,<br />
Tiret L, et al: Identification <strong>of</strong> polymorphisms in <strong>the</strong><br />
promoter and <strong>the</strong> 3 Vregion <strong>of</strong> <strong>the</strong> TAFI gene: Evidence<br />
that plasma TAFI antigen levels are strongly genetically<br />
controlled. Blood 2001; 97: 2053-8.<br />
9- Schneider M, B<strong>of</strong>fa M, Stewart R, Rahman M, Koschinsky<br />
M, Nesheim M: Two naturally occurring variants <strong>of</strong> TAFI<br />
(Thr-325 and Ile-325) differ substantially with respect to<br />
<strong>the</strong>rmal stability and antifibrinolytic activity <strong>of</strong> <strong>the</strong> enzyme.<br />
J Biol Chem 2002; 277: 1021-30.<br />
10- B<strong>of</strong>fa MB, Koschinsky ML: Curiouser and curiouser:<br />
Recent advances in measurement <strong>of</strong> thrombin-activatable<br />
fibrinolysis inhibitor (TAFI) and in understanding its<br />
molecular genetics, gene regulation, and biological roles.<br />
Clin Biochem 2007; 40: 431-42.<br />
11- Myles T, Nishimura T, Yun TH, Nagashima M, Morser J,<br />
Patterson AJ, et al: Thrombin activatable fibrinolysis<br />
inhibitor, a potential regulator <strong>of</strong> vascular inflammation.<br />
J Biol Chem 2003; 278: 51059-67.<br />
12- Fogg DK, Bridges DE, Cheung KK, Kassam G, Filipenko<br />
NR, Choi KS, et al: The p11 subunit <strong>of</strong> annexin II heterotetramer<br />
is regulated by basic carboxypeptidase. Biochemistry<br />
2002; 41: 4953-61.<br />
13- Christ<strong>of</strong>ferson RD: Manual <strong>of</strong> cardiovascular medicine;<br />
ch.1: Acute myocardial infarction. Edited by Griffin BP,<br />
Topol EJ; Lippincott Williams & Wilkins. 3 rd edition,<br />
2009; p. 1-28.<br />
14- Connolly HM, Oh JK. Ch 14-Echocardiography, in<br />
Braunwald's Heart Disease: A Textbook <strong>of</strong> Cardiovascular<br />
Medicine, 8 th ed. Eidited by Libby P, Bonow RO, Mann<br />
DL, Zipes DP. Saunders Elsevier 2008; 227-314.<br />
15- Trinder P: Enzymatic colorimetric test. Ann Clin Biochem<br />
1969; 6: 24.<br />
16- Onaka L: Lipids. In Clinical Chemistry Concepts and<br />
Applications. Anderson SC, Cockayne S (eds.). London:<br />
W.B. Saunders 1993.<br />
17- Livak KJ: Allelic discrimination using fluorogenic probes<br />
and <strong>the</strong> 5` nuclease assay. Genet Anal 1999; 14: 143.<br />
203<br />
18- Ladenvall C: Genetic Association Studies in Stroke.<br />
Doctoral <strong>the</strong>sis from <strong>the</strong> Institute <strong>of</strong> Neuroscience and<br />
Physiology, <strong>the</strong> Sahlgrenska Academy at Göteborg University,<br />
Göteborg, Sweden 2008.<br />
19- Meltzer ME, Doggen CJM, de Groot PG, Meijers JCM,<br />
Rosendaal FR, Lisman T: Low thrombin activatable<br />
fibrinolysis inhibitor activity levels are associated with<br />
an increased risk <strong>of</strong> a first myocardial infarction in men.<br />
Haematologica 2009; 94: 811-818.<br />
20- Morange PE, Tregouet DA, Frere C, Luc G, Arveiler D,<br />
Ferrieres J, et al: TAFI gene haplotypes, TAFI plasma<br />
levels and future risk <strong>of</strong> coronary heart disease: The<br />
PRIME study. J Thromb Haemost 2005; 3: 1503-10.<br />
21- Silveira A, Schatteman K, Goossens F, et al: Plasma<br />
procarboxypeptidase U in men with symptomatic coronary<br />
artery disease. Thromb Haemost 2000; 84: 364-8.<br />
22- Juhan-Vague I, Morange PE, Aubert H, Henry M, Aillaud<br />
MF, Alessi MC, et al: Plasma Thrombin-activatable fibrinolysis<br />
inhibitor antigen concentration and genotype<br />
in relation to myocardial infarction in <strong>the</strong> north and south<br />
<strong>of</strong> Europe. Arterioscler Thromb Vasc Biol 2002; 22: 867-<br />
73.<br />
23- Santamaría A, Martínez-Rubio A, Borrell M, Mateo J,<br />
Ortín R, Fontcuberta J: Risk <strong>of</strong> acute coronary artery<br />
disease associated with functional thrombin activatable<br />
fibrinolysis inhibitor plasma level. Haematologica 2004;<br />
89: 880-1.<br />
24- Folkeringa N, Coppens M, Veeger NJ, Bom VJ, Middeldorp<br />
S, Hamulyak K, et al: Absolute risk <strong>of</strong> venous and arterial<br />
thromboembolism in thrombophilic families is not increased<br />
by high thrombin-activatable fibrinolysis inhibitor<br />
(TAFI) levels. Thromb Haemost 2008; 100: 38-44.<br />
25- Cellai AP, Antonucci E, Liotta AA, Fedi S, Marcucci R,<br />
Falciani M, et al: TAFI activity and antigen plasma levels<br />
are not increased in acute coronary artery disease patients<br />
admitted to a coronary care unit. Thromb Res 2006; 118:<br />
495-500.<br />
26- El-Shafie M, Risk A, Saad M, Ragab D, Abed N, Saber<br />
H, et al: Thrombin-activatable fibrinolysis inhibitor gene<br />
polymorphism in IHD, diagnostic and prognostic correlation.<br />
Egypt Heart J 2008; 60 (3): 309-318.<br />
27- Lau HK, Segev A, Hegele RA, et al: Thrombin-activatable<br />
fibrinolysis inhibitor (TAFI): A novel predictor <strong>of</strong> angiographic<br />
coronary restenosis. Thromb Haemost 2003; 90:<br />
1187-91.<br />
28- Segev A, Hegele RA, Lau HK, et al: Thr325Ile polymorphism<br />
<strong>of</strong> <strong>the</strong> TAFI gene is related to TAFI antigen plasma<br />
levels and angiographic restenosis after percutaneous<br />
coronary interventions. Thromb Res 2004; 114: 137-41.<br />
29- Gils A, Alessi MC, Browers E, Peeters M, Marx P, Leurs<br />
J, et al: Development <strong>of</strong> a genotipe 325-specific proCPU/<br />
TAFI ELISA. Arterioscler Thromb Vasc Biol 2003; 23:<br />
1122-7.<br />
30- Guimarães AHC, van Tilburg NH, Vos HL, Bertina RM,<br />
Rijken DC: Association between thrombin activatable<br />
fibrinolysis inhibitor genotype and levels in plasma:<br />
Comparison <strong>of</strong> different assays. Br J Haematol 2004; 124:<br />
659-65.
Thrombin-Activatable Fibrinolysis Inhibitor Thr325Ile Polymorphism<br />
31- Tregouet D, Schnabel R, Alessi M, Godefroy T, Declerck<br />
P, Nicaudv, Munzel T, Bickel C, et al: Activated thrombin<br />
activatable fibrinolysis inhibitor levels are associated<br />
with <strong>the</strong> risk <strong>of</strong> cardiovascular death in patients with<br />
coronary artery disease: The A<strong>the</strong>roGene study. Journal<br />
<strong>of</strong> Thrombosis and Haemostasis 2008; 7: 49-57.<br />
32- Swaisgood CM, Schmitt D, Eaton D, Plow EF: In vivo<br />
regulation <strong>of</strong> plasminogen function by plasma carboxypeptidase.<br />
B J Clin Invest 2002; 110: 1275-82.<br />
33- Asai S, Sato T, Tada T, Miyamoto T, Kimbara N, Motoyama<br />
204<br />
N, et al: Absence <strong>of</strong> procarboxypeptidase R induces<br />
<strong>com</strong>plement-mediated lethal inflammation in lipopolysaccharide-primed<br />
mice. J Immunol 2004; 173: 4669-74.<br />
34- Libby P: Inflammation in a<strong>the</strong>rosclerosis. Nature 2002;<br />
420: 868-74.<br />
35- Marx PF, Lisman T, Adelmeijer J, Marquart J, Meijers<br />
JCM: Binding <strong>of</strong> TAFI to collagen: A role for TAFI in<br />
<strong>the</strong> regulation <strong>of</strong> platelet adhesion? J Thromb Haemost<br />
2006; 4 (Suppl 1): 208.