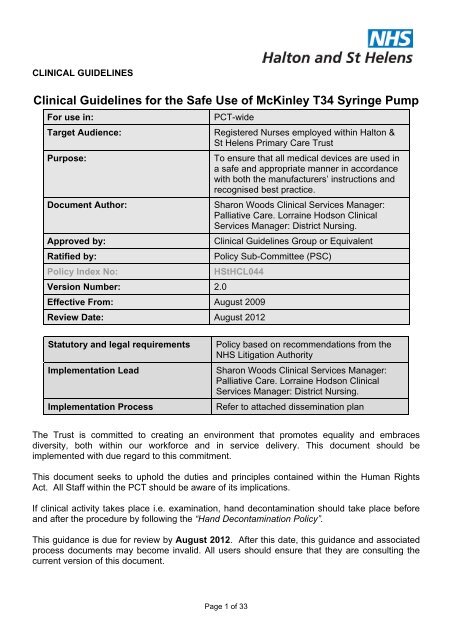
Clinical Guidelines for the Safe Use of McKinley T34 Syringe Pump
Clinical Guidelines for the Safe Use of McKinley T34 Syringe Pump
Clinical Guidelines for the Safe Use of McKinley T34 Syringe Pump
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
Table <strong>of</strong> ContentsIntroduction and Purpose.............................................................................................................5Definitions ....................................................................................................................................6Duties, Roles and Responsibilites................................................................................................6Scope...........................................................................................................................................8Indications <strong>for</strong> The <strong>Use</strong> <strong>of</strong> <strong>the</strong> Guideline ......................................................................................8Qualification and Training ............................................................................................................9Equipment..................................................................................................................................10Audit...........................................................................................................................................10Procedure ..................................................................................................................................10Register <strong>of</strong> medical devices .......................................................................................................10Decontamination <strong>of</strong> <strong>the</strong> <strong>McKinley</strong> <strong>T34</strong> <strong>Syringe</strong> <strong>Pump</strong> ................................................................10Incident reporting .......................................................................................................................11Obtaining in<strong>for</strong>med consent .......................................................................................................11Preparing <strong>the</strong> syringe.................................................................................................................11Labelling.....................................................................................................................................12Connecting infusion set to <strong>the</strong> syringe .......................................................................................12Preparing <strong>the</strong> <strong>McKinley</strong> <strong>T34</strong> <strong>Syringe</strong> <strong>Pump</strong> ...............................................................................13Fitting <strong>the</strong> syringe to <strong>the</strong> syringe pump ......................................................................................13Setting <strong>the</strong> infusion parameters .................................................................................................14Connecting <strong>the</strong> infusion to <strong>the</strong> patient........................................................................................14Starting <strong>the</strong> syringe pump ..........................................................................................................15Keypad lock ...............................................................................................................................15Stopping <strong>the</strong> infusion and removing <strong>the</strong> syringe pump ..............................................................16Resuming <strong>the</strong> infusion................................................................................................................16What to do if <strong>the</strong> patient dies whilst <strong>the</strong> syringe pump is running...............................................17Sites <strong>for</strong> placement <strong>of</strong> cannula <strong>for</strong> syringe pump infusion..........................................................17Page 3 <strong>of</strong> 33
INTRODUCTION AND PURPOSEIn accordance with <strong>the</strong> national policy and guidance outlined in <strong>the</strong> Medical Devices Directive93/42/EEC, NHS Halton & St Helens has a responsibility to ensure that all medical devices areused in a safe and appropriate manner in accordance with both <strong>the</strong> manufacturers’ instructionsand recognised best practice.In line with <strong>the</strong> first domain <strong>of</strong> <strong>the</strong> Standards <strong>for</strong> Better Health, <strong>the</strong> Primary Care Trust also hasa responsibility to take all necessary steps to ensure that patient safety is enhanced by <strong>the</strong> use<strong>of</strong> its health care processes, working Practice’s and systemic activities that prevent or reduce<strong>the</strong> risk <strong>of</strong> harm to its Patients. The development <strong>of</strong> this guideline will establish systems andprocedures that aim to protect patients and help to reduce <strong>the</strong> risks associated with <strong>the</strong>acquisition and use <strong>of</strong> medical devices. To this end, <strong>the</strong>se <strong>Guidelines</strong> will provide evidence tomeet <strong>the</strong> Standards <strong>for</strong> Better Health core Standards C4 (b), C5 (a) and <strong>the</strong> developmentstandards D1 and D2 (a).The syringe driver was originally developed in 1979 by Dr Martin Wright <strong>for</strong> <strong>Use</strong> in treatingthalassaemia with infusions <strong>of</strong> Desferrioxamine (Wright & Galland, 1979). The use <strong>of</strong> a portablebattery operated syringe driver <strong>for</strong> Subcutaneous medications is now a well establishedtechnique in palliative Care and its use is fully supported by Dickman et al (2005) who suggests"that It is particularly suited to palliative care".The benefits <strong>of</strong> employing <strong>the</strong> syringe driver is that it "allows <strong>for</strong> a minimally Invasive route <strong>of</strong>drug administration, which produces relatively constant Levels <strong>of</strong> medication which avoidspeaks that can result in reduced symptom Control" (Hunt 2002). Palliative care patients <strong>of</strong>tenpresent with multiple symptoms that can necessitate <strong>the</strong> need to use several drug treatments. If<strong>the</strong> patient’s condition deteriorates and <strong>the</strong> oral route cannot be used, Dickman et al (2005)fur<strong>the</strong>r suggests "that a continuous subcutaneous infusion via <strong>the</strong> syringe pump provides asimple and effective way to control symptoms".As a consequence <strong>of</strong> safety issues highlighted with <strong>the</strong> Graseby MS26 <strong>Syringe</strong> Driver, <strong>the</strong>syringe pump <strong>of</strong> choice within Halton & St Helens Primary Care Trust is now <strong>the</strong> <strong>McKinley</strong> <strong>T34</strong><strong>Syringe</strong> <strong>Pump</strong>.Parenteral administration <strong>of</strong> medicines carries a number <strong>of</strong> risks which have been welldocumented (Doyle et al, 1993). These can be attributed to a number <strong>of</strong> reasons, including usererror, maintenance, damage and contamination problems as well as device-related issues suchas per<strong>for</strong>mance, degradation, quality assurance and design and labelling (Medical DevicesAgency Device Bulletin 2003 (02)).Additionally, it is also recognised that syringe pumps may only be used intermittently andpr<strong>of</strong>essional competency can be difficult to maintain where its use is infrequent. Fur<strong>the</strong>rmore,<strong>the</strong> introduction <strong>of</strong> any new medical device brings with it <strong>the</strong> associated risks <strong>of</strong> unfamiliarity and<strong>the</strong> need to develop <strong>the</strong> required competences. The provision <strong>of</strong> local guidance on <strong>the</strong> use <strong>of</strong><strong>the</strong> <strong>McKinley</strong> <strong>T34</strong> <strong>Syringe</strong> <strong>Pump</strong> will introduce and establish robust procedures to promote aconsistent approach to its use across <strong>the</strong> Primary Care Trust.Page 5 <strong>of</strong> 33
As such, <strong>the</strong> main aim <strong>of</strong> <strong>the</strong>se guidelines is to assist health care pr<strong>of</strong>essionals administeringdrugs via <strong>the</strong> <strong>McKinley</strong> <strong>T34</strong> <strong>Syringe</strong> <strong>Pump</strong> and to promote a procedural uni<strong>for</strong>mity across Halton& St Helens Primary Care Trust.To this end, <strong>the</strong>se guidelines also aim to:I. Introduce and establish rigorous procedures to ensure a consistent approach to <strong>the</strong> use <strong>of</strong><strong>the</strong> <strong>McKinley</strong> <strong>T34</strong> <strong>Syringe</strong> <strong>Pump</strong>.II. Reduce <strong>the</strong> potential risk <strong>of</strong> adverse incidents (Medical Devices Agency Device Bulletin2003(02)).III. Improve patient safety and clinical outcomes.IV. Provide evidence <strong>for</strong> <strong>the</strong> organisation to meet <strong>the</strong> Standards <strong>for</strong> Better HealthV. Establish key per<strong>for</strong>mance indicators to monitor and evaluate <strong>the</strong> effectiveness <strong>of</strong> <strong>the</strong>guidanceThis document should be read in conjunction with <strong>the</strong> Policy <strong>for</strong> administration <strong>of</strong> ControlledDrugs, Decontamination Policy Infection Prevention and Control Policy and <strong>the</strong> End <strong>of</strong> Life CarePathway.DEFINITIONSThe <strong>McKinley</strong> <strong>T34</strong> syringe pump is a portable battery-operated infusion pump weighingapproximately 210g (excluding <strong>the</strong> battery) and measuring 169mm by 53mm by 23mm. It isused <strong>for</strong> <strong>the</strong> administration <strong>of</strong> medication subcutaneously over a 24 hour period.DUTIES, ROLES AND RESPONSIBILITESAuthor(s) are responsible <strong>for</strong> ensuring that:a) Once ratified, <strong>the</strong> clinical guideline is maintained in an editable electronic version (mastercopy).b) An Impact Assessment has been completed <strong>for</strong> <strong>the</strong> document and submitted to <strong>the</strong> Head<strong>of</strong> Corporate Services and Business.c) The responsible committee or <strong>of</strong>ficers are alerted <strong>of</strong> any necessary review to beundertaken.d) All amendments are completed subsequent to <strong>the</strong> findings <strong>of</strong> any review.Responsible Committee or Officers are responsible <strong>for</strong>:a) Undertaking any review <strong>of</strong> <strong>the</strong> document: In response to any recommendation(s) madefollowing an audit <strong>of</strong> <strong>the</strong> document. In line with <strong>the</strong> agreed review date (a maximum <strong>of</strong>Page 6 <strong>of</strong> 33
) Ensuring that if <strong>the</strong> author <strong>of</strong> <strong>the</strong> clinical guideline leaves, or <strong>the</strong>ir responsibilities changein relation to <strong>the</strong> guideline, that <strong>the</strong> Chair <strong>of</strong> <strong>the</strong> Multi-Disciplinary <strong>Clinical</strong> GuidelineRatification group is in<strong>for</strong>med to whom responsibility <strong>of</strong> being <strong>the</strong> author(s) is transferred<strong>for</strong> <strong>the</strong> relevant document.Multi-Disciplinary Guideline Ratification Group is responsible <strong>for</strong>:a) Ensuring that clinical guidelines are written in line with <strong>the</strong> Policy Standard.b) Ensuring that a master set <strong>of</strong> documents is maintained on behalf <strong>of</strong> <strong>the</strong> Primary CareTrust.c) Ensuring that <strong>the</strong> clinical guideline complies with all relevant legislation including Equality& Diversity.d) Monitoring and reviewing compliance against relevant Core and DevelopmentalStandards <strong>for</strong> Better Health and Risk Management Standards.e) Monitoring all clinical guidelines to ensure that <strong>the</strong>y are in date.f) Alerting <strong>the</strong> Primary Care Trust <strong>of</strong> all new clinical guidelines.The Head <strong>of</strong> Corporate Services and Business is responsible <strong>for</strong>:a) Maintaining copies <strong>of</strong> impact assessments and <strong>the</strong> action(s) necessary to ensuredocuments meet statutory requirements and o<strong>the</strong>r guidance.b) Publishing impact assessments on <strong>the</strong> Primary Care Trust’s public website and staffExtranet.The Governance Manager is responsible <strong>for</strong>:a) Notifying ‘receivers’ as identified on <strong>the</strong> Distribution Lists set up via <strong>the</strong> Policy CascadeSystem that a new document has been issued.b) Maintaining and updating distribution lists on <strong>the</strong> Policy Cascade System.The ‘receiver’, as identified by <strong>the</strong>ir Director, is responsible <strong>for</strong>:a) Updating <strong>the</strong> paper copy <strong>of</strong> <strong>the</strong> document in <strong>the</strong> paper files <strong>for</strong> which <strong>the</strong>y areresponsible.Page 7 <strong>of</strong> 33
) Responding to <strong>the</strong> Policy Cascade System Alert to ensure appropriate action is taken.c) In<strong>for</strong>ming relevant staff <strong>of</strong> an amended existing document or <strong>the</strong> introduction <strong>of</strong> a newone.Heads <strong>of</strong> Service and line managers are responsible <strong>for</strong>:a) Bringing <strong>the</strong> attention <strong>of</strong> <strong>the</strong>ir staff to <strong>the</strong> publication <strong>of</strong> a new document.b) Providing evidence that <strong>the</strong> document has been cascaded within <strong>the</strong>ir team ordepartment.c) Where appropriate, ensuring <strong>the</strong> new document is effectively implemented.d) Ensuring that <strong>the</strong>ir staff attend all training identified in respect <strong>of</strong> a new documents.The Employee is responsible <strong>for</strong>:All staff employed by NHS Halton & St Helens are responsible <strong>for</strong> adhering to this guideline,regardless <strong>of</strong> role, band, discipline or service area. All employees <strong>of</strong> Halton & St Helens PrimaryCare Trust have a contractual obligation to follow this document.SCOPEThis guidance is aimed at all qualified nursing staff working within NHS Halton & St Helens whoare currently registered with <strong>the</strong> Nursing and Midwifery Council and who have completed <strong>the</strong>relevant in-service training and are deemed competent in <strong>the</strong> use <strong>of</strong> <strong>the</strong> <strong>McKinley</strong> <strong>T34</strong> <strong>Syringe</strong><strong>Pump</strong>.INDICATIONS FOR THE USE OF THE GUIDELINEThe guidance contained in this document should be followed on all occasions when a <strong>McKinley</strong><strong>T34</strong> <strong>Syringe</strong> <strong>Pump</strong> is required to administer medication.The <strong>McKinley</strong> <strong>T34</strong> <strong>Syringe</strong> <strong>Pump</strong> is used to deliver drugs at a predetermined rate via <strong>the</strong>subcutaneous route over a 24 hour period. Typical applications include its use in pain andsymptom control. O<strong>the</strong>r indications <strong>for</strong> <strong>the</strong> use <strong>of</strong> <strong>the</strong> <strong>McKinley</strong> <strong>T34</strong> <strong>Syringe</strong> <strong>Pump</strong> are:Intractable nausea and vomitingIntestinal obstructionDysphagiaHead and neck lesions/surgerySemi or unconscious statePage 8 <strong>of</strong> 33
MalabsorptionUnsatisfactory response to oral drugs (uncommon)StomatitisPatient compliancePatient not be well enough to take <strong>the</strong> oral medications <strong>the</strong>y requireThe advantages <strong>of</strong> using <strong>the</strong> <strong>McKinley</strong> <strong>T34</strong> <strong>Syringe</strong> <strong>Pump</strong> are:The ability to infuse a combination <strong>of</strong> drugs via one route negates <strong>the</strong> need <strong>for</strong> repeatedinjectionsPortable, lightweight and compact, allowing mobility and independenceSimple calculation <strong>of</strong> dosages over a 24 hour periodAvoids or reduces <strong>the</strong> need <strong>for</strong> oral medicationPlasma concentrations remain level, <strong>the</strong>re<strong>for</strong>e improved symptom controlInfusion timing accuracyThe standard delivery period <strong>for</strong> a continuous subcutaneous infusion is a 24 hour period inpalliative care. The <strong>McKinley</strong> <strong>T34</strong> pump may be used with most makes <strong>of</strong> syringes. The mostcommonly used syringes have been 10 ml and 20 ml. However, it has been more recentlyadvocated that a 20ml syringe is <strong>the</strong> recommended minimum (Dickman et al 2002) as thisallows a larger dilution to be used, which will reduce both <strong>the</strong> risks <strong>of</strong> an adverse site reactionand also any potential incompatibility. In addition, it will also accommodate larger doses <strong>of</strong>certain drugs (Merseyside and Cheshire Palliative Care Network 2006). It is <strong>the</strong>re<strong>for</strong>erecommended that 20ml and 30ml syringes should be used and that <strong>the</strong>y have a luer lockfacility in order to avoid leakage or accidental disconnection.NB: The 50 ml Luer lock syringe is <strong>the</strong> largest syringe that will fit <strong>the</strong> <strong>McKinley</strong> <strong>T34</strong> syringepump. The benefits are that it allows drugs to be diluted up to approximately 34 mls volume <strong>for</strong>Becton Dickinson (BD) syringes and 44 mls <strong>for</strong> Terumo syringes. This reduces <strong>the</strong> risk <strong>of</strong>reactions at <strong>the</strong> infusion site and also reduces <strong>the</strong> need <strong>for</strong> a fur<strong>the</strong>r syringe pump when givinglarger volume drugs.QUALIFICATION AND TRAININGMedical and non medical prescriber’s with V300 qualification are responsible <strong>for</strong> prescribing <strong>the</strong>drugs to be administered via a syringe pump.Medications can only be administered via a <strong>McKinley</strong> <strong>T34</strong> <strong>Syringe</strong> <strong>Pump</strong> by a competentRegistered General Nurse who has undertaken and completed <strong>the</strong> required training in thisprocedure.Competency based training is provided within Halton & St Helens Primary Care Trust throughDistrict Nurse Team Leader and Assistant Team Leaders.Page 9 <strong>of</strong> 33
EQUIPMENT <strong>McKinley</strong> <strong>T34</strong> syringe pump Battery: 6LR61 Duracell MN1604 alkaline or lithium. Plus spare new battery 20 ml, 30 ml or 50 ml luer lock syringe, e.g. Becton Dickinson (BD) <strong>McKinley</strong> infusion set Alcohol wipe Transparent adhesive dressing, e.g. TEGADERM Prescribed medicines I diluents <strong>Syringe</strong> pump prescription I recording sheet I drug labelAUDITAudit requirements and competencies in relation to nursing staff using <strong>the</strong> pumps is <strong>the</strong>responsibility <strong>of</strong> each individual Team Leader. The Team Leaders will evidence that <strong>the</strong>y areauditing <strong>the</strong>se requirements on an annual basis.PROCEDUREMaintenance schedule All syringe pumps must be serviced annually, whe<strong>the</strong>r <strong>the</strong>y have beenused or not. The responsibility <strong>for</strong> <strong>the</strong> annual service / maintenance contract lies with <strong>the</strong><strong>Clinical</strong> Services Manager; however it is <strong>the</strong> responsibility <strong>of</strong> individual Team Leaders(community) to ensure compliance with <strong>the</strong> contract.Additionally, syringe pumps should be sent <strong>for</strong> maintenance checks if <strong>the</strong>y have been droppedor submerged in fluid or if <strong>the</strong>re is any doubt as to <strong>the</strong>ir handling operation whilst out on loan.REGISTER OF MEDICAL DEVICESA register <strong>of</strong> all such devices within Halton & St Helens Primary Care Trust area is maintained.When new syringe pumps are introduced into <strong>the</strong> system or syringe pumps are removed fromservice, <strong>the</strong> Medical Devices Coordinator must be notified according to procedures outlined inHalton & St Helens Primary Care Trust Medical Devices Policy.DECONTAMINATION OF THE MCKINLEY <strong>T34</strong> SYRINGE PUMPDecontamination should be carried out with a damp disposable cloth (use warm water andgeneral-purpose detergent). Dry thoroughly. If any additional cleaning is needed, e.g. <strong>the</strong>threads <strong>of</strong> <strong>the</strong> screws <strong>the</strong> actuator moves along, contact <strong>the</strong> Infection Prevention and ControlTeam <strong>for</strong> advice. The pump must not be submerged in water: if it is accidentally dropped inwater, it must be withdrawn from use immediately and sent <strong>for</strong> repair (Decontamination Policy;Infection Prevention and Control Policy).Page 10 <strong>of</strong> 33
INCIDENT REPORTINGSystems are in place within Halton & St Helens Primary Care Trust to report and monitorincidents involving medical devices. Staff using <strong>the</strong> <strong>McKinley</strong> <strong>T34</strong> <strong>Syringe</strong> <strong>Pump</strong> should befamiliar with <strong>the</strong> Primary Care Trust’s Incident Reporting System.The following incidents should be reported and investigated:Administration <strong>of</strong> incorrect medication, dose and/or diluent selectionIncorrect rate setting on syringe pumps resulting in infusions completing ahead <strong>of</strong>intended time or carrying on beyond intended time <strong>of</strong> completionDevice not alarmingAny o<strong>the</strong>r incident or near miss which may compromise patient safety or com<strong>for</strong>t NB Anydevice involved in an adverse incident should be taken out <strong>of</strong> service and sent to <strong>the</strong><strong>Clinical</strong> Services manager.OBTAINING INFORMED CONSENTNo Action Rationale1 Ensure that in<strong>for</strong>med patient consent has already beenobtained by <strong>the</strong> prescribing pr<strong>of</strong>essional.To enable procedure tocommence2 Explain procedure to <strong>the</strong> patient To ensure that <strong>the</strong> patientunderstands <strong>the</strong> process andhas <strong>the</strong> opportunity to raiseany concerns.3 Provide <strong>the</strong> patient with relevant in<strong>for</strong>mation leaflet(Appendix C ) with completed contact telephonenumbersTo reiterate <strong>the</strong> in<strong>for</strong>mationgiven and to provide <strong>the</strong>patient / carer with fur<strong>the</strong>rin<strong>for</strong>mation and advice.(The Mental Capacity Act has been introduced to help people who are unable to makedecisions <strong>for</strong> <strong>the</strong>m selves).PREPARING THE SYRINGENo Action Rationale1 Draw up <strong>the</strong> medication and diluents into a luer locksyringe <strong>of</strong> at least 20ml (BD).It may not be possible to fill all sizes <strong>of</strong> syringe to fullcapacity, between 34-44 ml can be delivered from a50ml syringe and approximately 24ml from a 30mlsyringe.2 Complete <strong>the</strong> details on <strong>the</strong> drug additive label as perlabelling sectionTo Ensure <strong>the</strong> correctmedication is given within <strong>the</strong>appropriate volume <strong>of</strong> diluent.To ensure accurate recordkeeping.Page 11 <strong>of</strong> 33
LABELLINGNo Action Rationale1 All syringes containing drug additives must be labelled To ensure accurate recordkeeping2 If <strong>the</strong>re is any doubt as to <strong>the</strong> contents <strong>of</strong> a syringe, <strong>the</strong>contents should be discarded into denaturing kit.3 Complete <strong>the</strong> label details in black ink or o<strong>the</strong>r indelibleprint. The label requires to state: The name <strong>of</strong> <strong>the</strong> patient <strong>for</strong> whom it is intended; The date and time <strong>of</strong> preparation; The full name <strong>of</strong> <strong>the</strong> person preparing <strong>the</strong>contents; The name and quantity <strong>of</strong> all drugs; The name <strong>of</strong> <strong>the</strong> diluent; The total volume <strong>of</strong> <strong>the</strong> contents; The time period over which <strong>the</strong> contents are tobe infused; The intended route <strong>of</strong> infusion; The date and time <strong>the</strong> infusion started4 Ensure <strong>the</strong> label does not interfere with <strong>the</strong> mechanism<strong>of</strong> <strong>the</strong> infusion device, i.e. where <strong>the</strong>re is contact with<strong>the</strong> barrel clamp arm.5 Attach <strong>the</strong> label to <strong>the</strong> syringe. Ensure that <strong>the</strong> labeldoes not obscure any visuals scales.To ensure that any risks to <strong>the</strong>patient are minimised and tocomply with Halton & StHelens Primary Care TrustPolicy <strong>for</strong> <strong>the</strong> Disposal <strong>of</strong>Controlled Drugs.To ensure accurate recordkeeping.Ensuring safe practice and toprevent malfunctioning <strong>of</strong>pumpTo ensure <strong>the</strong> visual scalescan be viewed during <strong>the</strong>infusionCONNECTING INFUSION SET TO THE SYRINGENo Action Rationale1 <strong>McKinley</strong> infusion sets must be used To ensure <strong>the</strong> correct infusion<strong>for</strong> <strong>the</strong> administration <strong>of</strong>medication via a syringepump.2 Connect it securely to <strong>the</strong> syringe To prevent leakage andwastage <strong>of</strong> medications anddisconnection3 If it is a new infusion set, prime <strong>the</strong> line Prevents time delay in patientreceiving medicationPage 12 <strong>of</strong> 33
PREPARING THE MCKINLEY <strong>T34</strong> SYRINGE PUMPNo Action Rationale1 Install <strong>the</strong> battery. 6LR61 Duracell MN1604 alkaline orlithium to be used. Ensure that any battery with a lifeless than 40% is replaced.2 Be<strong>for</strong>e placing <strong>the</strong> syringe into <strong>the</strong> <strong>Pump</strong> ensure lift andturn <strong>the</strong> barrel clamp arm. Turn and lower <strong>the</strong> barrelarm. Press and hold <strong>the</strong> "ON/OFF" key until <strong>the</strong> "SELFTEST" screen appears3 The LCD display will show "PRELOADING" and <strong>the</strong>actuator will start to move. Wait until it stops movingand <strong>the</strong> syringe sensor detection screen (syringegraphic) appears. NOTE: During Pre-Loading, <strong>the</strong>actuator always returns to <strong>the</strong> start position <strong>of</strong> <strong>the</strong> lastinfusion programmed.4 If <strong>the</strong> actuator is not in <strong>the</strong> correct position toaccommodate <strong>the</strong> syringe, leave <strong>the</strong> barrel clamp armdown and use <strong>the</strong> "FF" or "BACK" buttons on <strong>the</strong>keypad to move <strong>the</strong> actuator. Forward movement <strong>of</strong> <strong>the</strong>actuator is limited, <strong>for</strong> safety; <strong>the</strong>re<strong>for</strong>e repeatedpresses <strong>of</strong> <strong>the</strong> "FF" key may be required when moving<strong>the</strong> actuator <strong>for</strong>ward. Backwards movement is notrestricted5 Check <strong>the</strong> battery Press "INFO" key repeatedly until <strong>the</strong>battery level appears on <strong>the</strong> screen and <strong>the</strong>n press"YES" to confirmIn order to power <strong>the</strong> pumpTo ensure <strong>the</strong> pump isworking correctly.To ensure LCD display isworking properly.The barrel clamp arm needsto be in <strong>the</strong> down position toenable <strong>the</strong> “FF” and “BACK”buttons to work.In order to verify <strong>the</strong>re issufficient battery power <strong>for</strong> <strong>the</strong>programme. (The averagebattery life, starting at 100%,is approx 3 -4 days dependingon use.) Discard <strong>the</strong> battery ifless than 40% life remaining.FITTING THE SYRINGE TO THE SYRINGE PUMPNo Action RationaleENSURE THE LINE IS NOT CONNECTED TO THE PATIENT (unless repriming only)1 Lift and turn <strong>the</strong> barrel clamp arm This will enable syringe to beplaced on <strong>the</strong> pump2 Seat <strong>the</strong> filled syringe collar/ear and plunger so <strong>the</strong>back <strong>of</strong> <strong>the</strong> collar/ear sits against <strong>the</strong> back <strong>of</strong> <strong>the</strong> centralslot (ensure correct placement with <strong>the</strong> syringe scalefacing <strong>the</strong> front). The syringe collar/ears should bevertical3 Turn and lower <strong>the</strong> barrel clamp arm to secure <strong>the</strong>syringeTo ensure <strong>the</strong> safe delivery <strong>of</strong>medication.To ensure <strong>the</strong> safe delivery <strong>of</strong>medication.Page 13 <strong>of</strong> 33
NOTE: The syringe graphic on <strong>the</strong> screen ceases to flash at each point as <strong>the</strong> syringe iscorrectly seated.Confirm that <strong>the</strong> syringe size and brand match <strong>the</strong> screen message. Press "YES" to confirm orscroll up + down - arrows to view o<strong>the</strong>r syringe manufacture choices, select press “YES” toconfirm.SETTING THE INFUSION PARAMETERSNew PatientAfter <strong>the</strong> syringe confirmation, <strong>the</strong> firstscreen that appears is displayedSame PatientAfter <strong>the</strong> syringe confirmation, <strong>the</strong> first screenthat appears will showVol. 15.73 (<strong>of</strong>) 15.7mlDuration: 24.00Rate: 0.66/hConfirm. Press YesThe pump calculates and displays<strong>the</strong> deliverable volume, duration <strong>of</strong> infusion(24hrs) and rate <strong>of</strong> infusion (millilitres per hour)Press Yes to confirm.PressYES to RESUMENO <strong>for</strong> New ProgramN.B. If <strong>the</strong> original syringe is still inplace, pressing "No <strong>for</strong> New programwill reset <strong>the</strong> 24 hour clock, this means that<strong>the</strong> remaining contents <strong>of</strong> <strong>the</strong> syringe will bedelivered over <strong>the</strong> next 24 hoursfrom confirming "start infusion".<strong>Pump</strong> screen prompts “ START INFUSION”Check <strong>the</strong> line is connected to <strong>the</strong> pumpCONNECTING THE INFUSION TO THE PATIENTNo Action Rationale1 Shave or clip excess hair from <strong>the</strong>selected site2 Insert <strong>the</strong> needle inverted (bevel up) at an angle<strong>of</strong> 30-45 degrees into <strong>the</strong> subcutaneous tissue at<strong>the</strong> selected site.To enable site to be viewedand to ensure that anydressing used will adhereproperly.To ensure needle is placedcorrectly.3 Secure <strong>the</strong> needle with a transparent dressing To ensure that <strong>the</strong> site can beviewed at all times.4 Include a loop <strong>of</strong> <strong>the</strong> infusionset under <strong>the</strong> dressing.To avoid any direct pull on <strong>the</strong>needle.Page 14 <strong>of</strong> 33
5 Ensure <strong>the</strong> patient and carers know that <strong>the</strong>syringe pump must NOT be placed at a levelhigher than <strong>the</strong> infusion site.6 Record in <strong>the</strong> appropriate documents, <strong>the</strong>drugs/diluent administered and <strong>the</strong> time <strong>the</strong>infusion commenced.7 Never take a syringe that is not empty <strong>of</strong>f <strong>the</strong>pump if it is still connected to <strong>the</strong> patient.To ensure that <strong>the</strong> contents do notsiphon out.To ensure accurate recordkeeping.To prevent <strong>the</strong> patient fromreceiving an accidentaladministration <strong>of</strong> medication.N.B. It takes 4-6 hours <strong>for</strong> drugs to reach <strong>the</strong>rapeutic blood plasma levels via <strong>the</strong> syringe pump,<strong>the</strong>re<strong>for</strong>e, an additional stat dose <strong>of</strong> <strong>the</strong>medication may require to be administered when <strong>the</strong> syringe pump is set up if <strong>the</strong> patient hasunrelieved symptoms.STARTING THE SYRINGE PUMPIn order to start <strong>the</strong> infusion, press “YES” on <strong>the</strong> syringe pump. When <strong>the</strong> pump is running, <strong>the</strong>screen displays <strong>the</strong> following:• Top line -infusion duration time remaining;• Main line -infusion rate in ml/hour;• Bottom line -alternates between syringe size/brand and <strong>the</strong> message"«« <strong>Pump</strong> delivering". The green LED indicator will also flash.KEYPAD LOCKThe <strong>T34</strong> allows all users to lock <strong>the</strong> operation <strong>of</strong> <strong>the</strong> Keypad during infusion. This functionshould be routinely used to prevent tampering with <strong>the</strong> device.I. Activating <strong>the</strong> keypad lockWith <strong>the</strong> pump infusing press and hold <strong>the</strong> "INFO" key until a chart is displayed showing a'progress' bar moving from left to right. Hold <strong>the</strong> key until <strong>the</strong> bar has moved completelyacross <strong>the</strong> screen and a beep is heard to confirm <strong>the</strong> lock has been activated. NB Thefollowing buttons are still active Stop / No, Start / Yes, In<strong>for</strong>mation.II. Deactivating <strong>the</strong> keypad lockTo turn <strong>the</strong> lock <strong>of</strong>f, repeat <strong>the</strong> above procedure. The bar will now move from right (lock) toleft (unlock) and a beep will be heard.Page 15 <strong>of</strong> 33
STOPPING THE INFUSION AND REMOVING THE SYRINGE PUMPEach practitioner will be issued with a key and will be responsible <strong>for</strong> its safe keeping. NB. IR1must be completed if a key is lost. Any member <strong>of</strong> staff leaving <strong>the</strong> PCT must return <strong>the</strong> key to<strong>the</strong> <strong>Clinical</strong> Services Manager.No Action Rationale1 Removal <strong>of</strong> <strong>the</strong> Cannula and/ordiscontinuation <strong>of</strong> infusion must only becarried out by an appropriately trained healthpr<strong>of</strong>essional.2 When <strong>the</strong> infusion is complete and <strong>the</strong>syringe is empty, it will stop automatically and<strong>the</strong> alarm will sound. If <strong>the</strong> syringe pump isno longer required <strong>for</strong> <strong>the</strong> patient, press"OFF" and <strong>the</strong>n remove <strong>the</strong> battery from <strong>the</strong>syringe pump.3 If <strong>the</strong> infusion is to be stopped be<strong>for</strong>e <strong>the</strong>syringe is empty, it should also bedisconnected at <strong>the</strong> syringe end from <strong>the</strong>patient <strong>for</strong> safety reasons be<strong>for</strong>e <strong>the</strong> syringeis taken <strong>of</strong>f <strong>the</strong> pump. A syringe that is notempty must NEVER be taken <strong>of</strong>f <strong>the</strong> pumpwhile connected to <strong>the</strong> patient.4 Clean <strong>the</strong> pump and <strong>the</strong> cover (do notimmerse pump in water). Dry and replace inpackaging if no longer required <strong>for</strong> use.5 Temporary Interruption <strong>of</strong> Infusion,e.g. bathing: Press STOP6 Press and hold "OFF" button untila beep is heard; <strong>the</strong> screen willgo blank.To ensure patient safety and maintainpr<strong>of</strong>essionalresponsibilityTo ensure <strong>the</strong> pump is <strong>of</strong>f and <strong>the</strong>remaining battery life is saved.To ensure <strong>the</strong>re is no accidentaladministration <strong>of</strong> drugs to <strong>the</strong> patient.To comply with infection controlguidelines.To ensure pump is <strong>of</strong>f while bathing.To ensure pump is switched <strong>of</strong>f7 Do not remove syringe from pump. To ensure pump can reset to originalregime.8 Disconnect <strong>the</strong> line from <strong>the</strong> syringe and cap<strong>the</strong> end <strong>of</strong> <strong>the</strong> line and syringe tip.To avoid contamination <strong>of</strong> line andsyringe.RESUMING THE INFUSIONNo Action Rationale1 Check that <strong>the</strong> prescription, syringe label andpatient details match.2 Reconnect <strong>the</strong> line to <strong>the</strong> syringe on <strong>the</strong>pump.To ensure that this is <strong>the</strong> correctsyringe <strong>for</strong> this patient.To ensure pump can reset to originalregime.Page 16 <strong>of</strong> 33
3 Press and hold <strong>the</strong> "ON" button until a beepis heard.To ensure pump is switched on.4 The screen will request confirmation <strong>of</strong>syringe size and syringe brand.5 The screen will display <strong>the</strong> remaining volume,duration and rate <strong>of</strong> infusion.To ensure <strong>the</strong> correct rate <strong>of</strong> infusionis calculated.To confirm <strong>the</strong> correct amount andduration <strong>of</strong> infusion remaining.6 Press "YES" to confirm If you press "NO" <strong>the</strong> pumpinterprets this as a completely new24hr period. In this case, you wouldrequire setting up a completely newprescription from <strong>the</strong> start.7 The screen will display "StartInfusion".To confirm that <strong>the</strong> infusion is to berecommenced.8 "YES" to confirm Press. To start infusion.WHAT TO DO IF THE PATIENT DIES WHILST THE SYRINGE PUMPIS RUNNINGNo Action Rationale1 Stop <strong>the</strong> pump To discontinue <strong>the</strong> infusion.2 Press <strong>the</strong> "INFO" button and record <strong>the</strong> date,time and amount <strong>of</strong> solution remaining to beinfused in <strong>the</strong> syringe (ml).3 If <strong>the</strong>re are doubts about <strong>the</strong> circumstances<strong>of</strong> <strong>the</strong> death, leave <strong>the</strong> pump in place andcontact <strong>the</strong> Line Manager <strong>for</strong> advice.4 In a straight<strong>for</strong>ward situation, followingidentification <strong>of</strong> death, remove <strong>the</strong> needleand line from <strong>the</strong> patient and discardcontents into denaturing kitTo ensure accurate record keeping.To ascertain any legal requirements.To ensure compliance with NHSHalton & St Helens policy <strong>for</strong> Disposal<strong>of</strong> Controlled Drugs5 Remove <strong>the</strong> battery. To protect battery life and pump.6 Record <strong>the</strong> signature(s) <strong>of</strong> person(s)destroying <strong>the</strong> remaining solution.To ensure compliance with <strong>the</strong> HealthRecords Policy.SITES FOR PLACEMENT OF CANNULA FOR SYRINGE PUMPINFUSIONI. Appropriate sites <strong>for</strong> continuous infusion <strong>of</strong> subcutaneous drugs are as follows: Anterior chest wall AbdomenPage 17 <strong>of</strong> 33
Lateral aspects <strong>of</strong> upper arms and thighsBack (scapula) -particularly suitable <strong>for</strong> confused patientsII. Areas which should not be used <strong>for</strong> syringe pump infusion Lymph oedematous limbs or trunk Sites over bony prominences Sites near a joint Previously irradiated skin Infected skin/skin lesionsCARE OF INFUSION SITENo Action Rationale1 A transparent dressing must be used. To permit visible monitoring <strong>of</strong>site.2 If <strong>the</strong>re is evidence <strong>of</strong> inflammation or poorabsorption (hard subcutaneous swelling), <strong>the</strong>infusion site should be renewed.3 The needle site should be changed at leastevery 3 days.4 Inspect <strong>for</strong> leakage at <strong>the</strong> cannula site and at<strong>the</strong> connection sites.This may effect absorption <strong>of</strong>medication and patient com<strong>for</strong>tTo reduce <strong>the</strong> risk <strong>of</strong> irritation /inflammation / cannula displacement.In order to minimise <strong>the</strong> risk <strong>of</strong> anymalfunction or administrationproblems.SITE BREAKDOWNNo Action Rationale1 Fur<strong>the</strong>r dilute drug if possible To reduce any site irritation2 Change infusion device, e.g. Thalus set ifpatient has allergy to metal (Unomedical -available through NHS Logistics).To reduce any site reaction andprevent absorption problems.3 Change type <strong>of</strong> site dressing To reduce any site irritation4 Change site more <strong>of</strong>ten To reduce any site reaction.5 Check diluent To ensure <strong>the</strong> appropriate diluentis used.6 Check compatibility <strong>of</strong> drugs. (Seek advicefrom a pharmacist on whe<strong>the</strong>r an alternativediluent would be appropriate).To reduce <strong>the</strong> possibility <strong>of</strong> druginteractions.7 Consider <strong>the</strong> use <strong>of</strong> an additional pump. To reduce any possible druginteractions.Page 18 <strong>of</strong> 33
CARE DURING INFUSIONNo Action Rationale1 Explain care <strong>of</strong> <strong>the</strong> pump to carers e.g. avoidspillage <strong>of</strong> liquids on it or avoid dropping.Report if light stops flashing or if alarmshould sound.Good communication enables betterpatient/family experience and ensuresearly intervention <strong>of</strong> health carepr<strong>of</strong>essionals if pump malfunctions.2 Check battery daily To ensure sufficient battery life.3 Avoid using mobile telephone nearer than 1metre to <strong>the</strong> syringe pump (<strong>McKinley</strong> MedicalUK Ltd).To ensure <strong>the</strong>re is no interference with<strong>the</strong> operation <strong>of</strong> <strong>the</strong> syringe pump.4 When <strong>the</strong> patient is mobile, ensure syringepump is well supported.To ensure <strong>the</strong> com<strong>for</strong>t <strong>of</strong> <strong>the</strong> patientand also to prevent pump malfunction.CHECKS TO BE MADE WHILST SYRINGE PUMP IS IN USENo Action Rationale1 Assess symptom control regularly Individualised care/ good practice.2 Check site <strong>for</strong> redness, inflammation,infection or needle displacement.3 Check syringe and infusion line <strong>for</strong>crystallisation, precipitation, cloudiness orcolour change <strong>of</strong> contents or leakage.Re-prime pump if this is <strong>the</strong> case.4 Check <strong>the</strong> display -pump is delivering andinfusion rate is as programmed.To ensure early detection <strong>of</strong> siteproblems.To ensure early detection <strong>of</strong> drug /diluent incompatibility.To ensure <strong>the</strong> pump is delivering <strong>the</strong>correct infusion rate as required.5 Record rate setting To ensure accurate record Keeping6 Press <strong>the</strong> "INFO" key to check: Single press -VTBI (Volume to beInfused) and volume infused andrecord. Double press -battery life remaining.7 Visually check fluid remaining in syringe ateach check and compare with pump readingkeeping a record <strong>of</strong> measurement at eachvisit.To verify infusion rate and batterylife.To verify that contents <strong>of</strong> <strong>the</strong>syringe reflect pump reading.Page 19 <strong>of</strong> 33
TROUBLESHOOTINGNo Action RationaleIf fast (running more than 1 hour ahead <strong>of</strong> expected time)1 Check <strong>the</strong> rate setting is correct. To ensure pump rate is not set too fast.2 Check <strong>the</strong> correct syringe brand or sizehas been selected.3 Change <strong>the</strong> entire syringe pump <strong>for</strong> a newone and send <strong>for</strong> servicing.To ensure exact calculation by syringepump <strong>of</strong> rate.In order to maintain patient safety and incompliance with NHS Halton & StHelens Medical Devices Policy.4 In<strong>for</strong>m <strong>the</strong> patient’s medical practitioner if<strong>the</strong> patient's clinical condition gives cause<strong>for</strong> concern.5 Report <strong>the</strong> incident through <strong>the</strong> PrimaryCare Trust’s incident reporting system.To obtain expert medical adviceTo ensure compliance with Halton & StHelens Primary Care Trust IncidentReporting Policy.No Action RationaleIf slow (running more than 1 hour behind expected time).1 Check <strong>the</strong> syringe pump light is on. To ensure that <strong>the</strong> pump has power.2 Check <strong>the</strong> battery level. (If battery leveldisplays 40% or below, change battery.)To ensure <strong>the</strong> power level is sufficient tocomplete <strong>the</strong> safe delivery <strong>of</strong> drugs overa 24 hour period.3 Check <strong>the</strong> rate setting is correct. To ensure <strong>the</strong> appropriate dose isdelivered.4 Check <strong>the</strong> correct syringe brand or sizehas been selected.5 Check that syringe is inserted correctly intosyringe pump.6 Ascertain if syringe pump has beenstopped and restarted <strong>for</strong> any reason.7 Check contents <strong>of</strong> syringe and line -is <strong>the</strong>reany evidence <strong>of</strong> crystallisation/kinking <strong>of</strong>tubing8 Check needle site -is this red / hard /lumpy/sore?To ensure exact calculation by pump <strong>of</strong>rate <strong>of</strong> administration.The pump will not work if <strong>the</strong> syringeinserted incorrectly.This will affect <strong>the</strong> functioning <strong>of</strong> <strong>the</strong>pump.This may slow delivery <strong>of</strong> contents.This may affect absorption9 Change needle site if necessary To improve absorption.10 Consider fur<strong>the</strong>r dilution <strong>of</strong> drugs tominimise irritation by setting up a freshTo prevent irritation.Page 20 <strong>of</strong> 33
syringe.11 Consider metal allergy from needle. Patient may have an allergy to <strong>the</strong> metalin <strong>the</strong> needle.If a patient is assessed as having anallergy to <strong>the</strong> <strong>McKinley</strong> giving sets, <strong>the</strong>secan be substituted with Teflon coatedgiving set to ensure that <strong>the</strong> patient’shypoallergenic issue is addressed.12 If <strong>the</strong> syringe pump continues to runthrough too slowly, change <strong>the</strong> entire pumpand send <strong>for</strong> servicing.13 Check <strong>the</strong> rate <strong>of</strong> infusion at regularintervals.To ensure that any problems with<strong>the</strong> syringe pump are investigated andrepaired if necessary. To ensure <strong>the</strong>patient receives correct medication overcorrect timeCheck <strong>the</strong> rate <strong>of</strong> infusion at regularintervals.IF THE PUMP ALARM ACTIVATESWhen <strong>the</strong> pump detects a problem four things occur:The infusion stops;An audible alarm is activated;A message appears on <strong>the</strong> display screen indicating <strong>the</strong> cause <strong>of</strong> <strong>the</strong> alarm;The LED indicator turns RED.The following table indicates <strong>the</strong> appropriate actions should <strong>the</strong> pump alarm.Actions to be taken by <strong>the</strong> patient / carer in <strong>the</strong> event that <strong>the</strong> pump alarms are also outlined in<strong>the</strong> Patient In<strong>for</strong>mation Leaflet (Refer to Appendix 2)Alarm Possible Cause ActionOcclusion or <strong>Syringe</strong>Empty.Patient access deviceblocked, kinked, clamped.Release clamp. Flush orreplace access device.<strong>Syringe</strong> Displaced<strong>Pump</strong> UnattendedOcclusion.Actuator has reachedminimum travel position.<strong>Syringe</strong> has been removed ordisplaced.<strong>Pump</strong> left or no key pressesdetected <strong>for</strong> 2 minutes.Remove occlusion and restart.End <strong>of</strong> program, switch pump<strong>of</strong>f.Check and confirm syringeseated correctly and resume.Start infusion, continueprogramming or switch<strong>of</strong>f.Page 21 <strong>of</strong> 33
Near End15 minutes from end <strong>of</strong>infusion.Prepare to change syringe orswitch <strong>of</strong>f.End Program Infusion complete The pump will ei<strong>the</strong>r default toKVO, (keep vein open) awaitnurse, or it will alarm in whichcase switch pump <strong>of</strong>f.DRUG ADMINISTRATION USING SYRINGE PUMPI. Prescribing <strong>for</strong> <strong>Syringe</strong> <strong>Pump</strong>sAnticipation <strong>of</strong> symptoms and corresponding patient requirements is advocated <strong>for</strong>at least 24 hours. Appropriate quantities <strong>of</strong> supplies require to be obtained <strong>for</strong>patients' <strong>for</strong>eseeable needs. (For fur<strong>the</strong>r in<strong>for</strong>mation, please refer to NHS Halton &St Helens End <strong>of</strong> Life Care Pathway).The prescription should contain: Patient demographic details Drug name Drug dose Diluent Route <strong>of</strong> administration Duration <strong>of</strong> infusionAdditional 'as required' stat doses <strong>of</strong> analgesia should always be prescribed on <strong>the</strong>appropriate prescription sheet and be available <strong>for</strong> administration by nursing staff asrequired.II. Prescribed medications:Four groups <strong>of</strong> drugs are commonly prescribed:Analgesics (usually Diamorphine or Morphine Sulphate or Oxycodone)Anti-emetics (Cyclizine, Haloperidol, Levomepromazine, Metoclopramide)Sedatives (Midazolam)Anti-secretory drugs (Glycopyrronium, Hyoscine hydro bromide) <strong>for</strong> fur<strong>the</strong>r guidanceabout drug prescriptions and conversions please contact <strong>the</strong> Macmillan SpecialistPalliative Care Team or GP.Page 22 <strong>of</strong> 33
CARE OF MEDICATIONSNo Action Rationale1 Protect <strong>the</strong> syringe from directlight whenever possible.2 Visual inspection <strong>of</strong> drug solutionsshould be made at eachmonitoring check (at least daily)and discarded if evidence <strong>of</strong>crystallisation, precipitation,cloudiness or discolouration.3 Avoid high concentrations <strong>of</strong> drugsused singly or in combination.4 Do not infuse contents <strong>of</strong> syringepump over a period longer than 24hoursSome drugs may be lightsensitive.To enable early detection <strong>of</strong> drug interactions.This will minimise <strong>the</strong> risk <strong>of</strong> site irritation.Prescriptions are only issued withinHalton & St Helens Primary CareTrust <strong>for</strong> 24 hour delivery.It remains <strong>the</strong> responsibility <strong>of</strong> each individual practitioner to ensure that <strong>the</strong> drug(s) prescribedare suitable <strong>for</strong> continuous subcutaneous infusion, and are stable under <strong>the</strong>se conditions. If inany doubt, seek advice from an appropriate Pharmacist or o<strong>the</strong>r appropriate pr<strong>of</strong>essional.DILUENTSA greater dilution <strong>of</strong> syringe pump contents reduces:The risk <strong>of</strong> incompatibilityThe impact <strong>of</strong> priming a lineInjection site skin reactionsKEY PERFORMANCE INDICATORSI.The number <strong>of</strong> untoward incidents reported relating to drug errors whilst using <strong>the</strong><strong>McKinley</strong> <strong>T34</strong> <strong>Syringe</strong> <strong>Pump</strong>.II.The number <strong>of</strong> untoward incidents reported relating to <strong>the</strong> per<strong>for</strong>mance <strong>of</strong> <strong>the</strong><strong>McKinley</strong> <strong>T34</strong> <strong>Syringe</strong> <strong>Pump</strong>.III.The number <strong>of</strong> staff attending <strong>Syringe</strong> <strong>Pump</strong> training annually.AUDIT PLAN<strong>McKinley</strong> <strong>T34</strong> <strong>Syringe</strong> <strong>Pump</strong> Audit will be carried out on an annual basis which will be based on<strong>the</strong> above key per<strong>for</strong>mance indicators.Page 23 <strong>of</strong> 33
ACKNOWLEDGEMENTSWe extend our thanks and appreciation to Western Cheshire <strong>for</strong> allowing us to utilise <strong>the</strong>ir ownguidelines as a basis <strong>for</strong> this document.Page 24 <strong>of</strong> 33
REFERENCESReferenceRelevance (wholedocument orsection, pleasestate)British Medical Journal, 2(6190): 582 Section ReportDickman, A. Littlewood, C. Varga, J (2005) The<strong>Syringe</strong> Driver. University Press, Ox<strong>for</strong>d.Doyle, D. Hanks, G. Cherry, N. Calman, K. (1993)Ox<strong>for</strong>d Textbook <strong>of</strong> Palliative Medicine, 3rd Edition,Ox<strong>for</strong>d University Press, Ox<strong>for</strong>d.Hunt, T. (2002) in: Pension, J. Fisher, R. (eds)Palliative care <strong>for</strong> people with Cancer. London: Arnold.<strong>McKinley</strong> Medical UK Limited. Ambulatory <strong>Syringe</strong><strong>Pump</strong> Instruction Manual. <strong>McKinley</strong> <strong>T34</strong>, June 2005.Medical Devices Agency (2003). Devices Bulletin:Infusion Systems. Medical. Devices Agency, March2003.Merseyside and Cheshire Palliative Care NetworkAudit Group, 3rd edition (2006).Western Cheshire Primary Care Trust (2008). End <strong>of</strong>Life Care Pathway. (<strong>Guidelines</strong> <strong>for</strong> Strong OpioidSubstitution in Palliative Care.)Wright, B.M. & Callan K. (1979) Slow drug infusionsusing a portable syringe driver.NHS Halton and St Helens, Records ManagementPolicy 2007WholeEvidenceGradePolicyNHS Halton and St Helens, Consent Policy 2009 Whole PolicyPage 25 <strong>of</strong> 33
APPENDIX 1Glossary <strong>of</strong> TermsThe following terms are used in this document;Stat: The injection <strong>of</strong> a drug (or drugs) in a high quantity at once, <strong>the</strong> opposite <strong>of</strong> gradualadministration (as in intravenous infusion).Cannula: A tube which can be inserted into <strong>the</strong> body, <strong>of</strong>ten <strong>for</strong> <strong>the</strong> delivery or removal <strong>of</strong> fluid.Diluent: An agent used <strong>for</strong> effecting dilution.Infusion set: An implantable device consisting <strong>of</strong> a fine needle and tubing which is attached toa syringe to enable <strong>the</strong> delivery <strong>of</strong> drugs via a syringe pump.Page 26 <strong>of</strong> 33
APPENDIX 2<strong>McKinley</strong> <strong>Syringe</strong> <strong>Pump</strong>sPatient In<strong>for</strong>mation LeafletWhat is a <strong>Syringe</strong> <strong>Pump</strong>?This is a small, portable battery controlled pump. It can be carried about in a pouch attached toa belt, on a shoulder holster, or in your pocket. The pump is fitted with a syringe, which givesyour medicines through a needle just under <strong>the</strong> skin. The medicines are absorbed directly intoyour bloodstream. The pump runs 24 hours a day, avoiding <strong>the</strong> need <strong>for</strong> repeated injections.Why do I need one?Sometimes it is easier <strong>for</strong> you to have some <strong>of</strong> your medicines this way.This may be because: You have been vomiting, and find it difficult to keep your medicines down. Medicines tohelp stop vomiting are given in <strong>the</strong> syringe pump, along with medicines to help o<strong>the</strong>rsymptoms such as pain. Once <strong>the</strong> vomiting has settled you may go back to having yourmedicines by mouth. You have so many medicines to take that you are finding it difficult to manage <strong>the</strong>m all.Putting some <strong>of</strong> <strong>the</strong> medicines in <strong>the</strong> syringe pump can reduce <strong>the</strong> number <strong>of</strong> medicinesyou need to take by mouth. You are unable to swallow medicines. Medicines to help your symptoms can be put into<strong>the</strong> syringe pump. Starting a syringe pump doesn’t mean that your medicines havestopped working or aren’t strong enough, only that this is a more effective way <strong>of</strong> getting<strong>the</strong>m into your body, if you cannot take <strong>the</strong>m by mouth.Page 27 <strong>of</strong> 33
Who will look after my syringe pump?If you are at home, your community nurse will come in each day to replace <strong>the</strong> syringe, checkthat <strong>the</strong> needle is com<strong>for</strong>table and that <strong>the</strong>re are no problems with <strong>the</strong> medicines.If you are staying in <strong>the</strong> hospital, hospice or care home <strong>the</strong> staff <strong>the</strong>re will check your syringepump regularly to make sure it is working well. The syringe will be changed each day by <strong>the</strong>staff. They will check that <strong>the</strong> needle is com<strong>for</strong>table and that you are not having any problemswith <strong>the</strong> medicines.The medicines in your syringe pump have been prescribed by your doctor to help yoursymptoms; you do not need to do anything to <strong>the</strong> syringe pump. The medicines will continue tobe absorbed over 24 hours, helping your symptoms round <strong>the</strong> clock.What does a syringe pump look like?The syringe pump currently in use in Halton & St Helens Primary Care Trust is <strong>the</strong> <strong>McKinley</strong><strong>T34</strong> syringe pump. The pump (actuator) pushes <strong>the</strong> medicine into <strong>the</strong> giving set, through <strong>the</strong>needle and into <strong>the</strong> tissues under <strong>the</strong> skin where it is absorbed into your bloodstream. While <strong>the</strong>pump is running <strong>the</strong> indicator light will flash to let you know that it is working.The pump is lightweight and about 15cm long by 5cm tall. It may have a clear plastic cover toprotect it and may be in a fabric bag, to protect <strong>the</strong> syringe from light. Your nurse or doctor willbe able to show you <strong>the</strong> syringe pump.Some dos and don’tsThe medicines in <strong>the</strong> syringe pump will flow into your blood stream throughout <strong>the</strong> 24-hourperiod, controlling your symptoms. Any adjustments required will be made by your GP orCommunity Nurse or by <strong>the</strong> hospital or hospice staff. Do not interfere with <strong>the</strong> syringe or <strong>the</strong>pump.You must keep <strong>the</strong> syringe pump and <strong>the</strong> infusion site dry. Take care when washing or bathingto keep <strong>the</strong> syringe pump dry. If you drop it into water contact your nurse, a new syringe pumpwill be needed to be sure that your medicines are being given at <strong>the</strong> right rate.The syringe in <strong>the</strong> pump should not be exposed to direct sunlight– you should keep it in <strong>the</strong>fabric pouch to protect it from light.The syringe pump should not be exposed to extremes <strong>of</strong> heat. Avoid placing <strong>the</strong> syringe pumpnext to a heat pad, electric blanket or hot water bottle.Avoid <strong>the</strong> use <strong>of</strong> mobile phones within a metre <strong>of</strong> <strong>the</strong> pump if at all possible as <strong>the</strong>y mayinterfere with <strong>the</strong> way <strong>the</strong> pump works. If a call is unavoidable, keep <strong>the</strong> length <strong>of</strong> <strong>the</strong> calls asshort as possible.If you notice any <strong>of</strong> <strong>the</strong> following contact your nurse/GP:Page 28 <strong>of</strong> 33
The colour <strong>of</strong> <strong>the</strong> medicines in <strong>the</strong> giving set has changed.There is a cloudiness or sediment in <strong>the</strong> giving set.The skin around <strong>the</strong> needle is red, swollen or painful.The alarm on <strong>the</strong> pump sounds.How will I know <strong>the</strong> syringe pump is working?The green light on <strong>the</strong> case will flash so long as <strong>the</strong>re is power in <strong>the</strong> battery. If <strong>the</strong> light goesout while <strong>the</strong> syringe pump is running, <strong>the</strong> battery will need to be replaced when <strong>the</strong> nextsyringe is put in. There is no need to change <strong>the</strong> battery be<strong>for</strong>e <strong>the</strong>n <strong>the</strong> rest <strong>of</strong> <strong>the</strong> medicine inyour syringe will be given. A new battery will last <strong>for</strong> three to four days.If <strong>the</strong> alarm sounds it may mean your infusion is complete, or that <strong>the</strong>re is a blockage in <strong>the</strong>syringe or giving set. Contact your nurse who will check <strong>the</strong> pump.If I have any worries who should I contact?District Nurse: TelOut <strong>of</strong> Hours contact: TelVersion No: 1.0Date <strong>of</strong> Issue: October 2009Page 29 <strong>of</strong> 33
APPENDIX 3ChecklistThe <strong>McKinley</strong> <strong>T34</strong> <strong>Syringe</strong> <strong>Pump</strong> Monitoring Checklist needs to be completed <strong>for</strong> every patientwho has a pump in operation. The trained member <strong>of</strong> staff undertaking <strong>the</strong> visit needs to ensurethat this <strong>for</strong>m is complete at every visit.Following completion, if <strong>the</strong> staff member has any concerns <strong>the</strong> syringe pump needs to bediscontinued and <strong>the</strong> Team Leader in<strong>for</strong>med immediately.Click here to download <strong>the</strong> checklistName:NHS Number:D.O.B.Date commenced:<strong>Syringe</strong> pump number:All syringe pumps should be checked. At Every Visit. Checkcorrect delivery rate, site condition and <strong>for</strong> signs <strong>of</strong>crystallisation or precipitation. Nurses must sign and date when<strong>the</strong> driver is commenced and checked. Document <strong>the</strong> siteposition in <strong>the</strong> patients’ care plan and any subsequent sitechange. Any problems should be recorded in <strong>the</strong> commentsbox, patients’ health records and acted upon. Contact TeamLeader or on-call clinician.DrugsTimecheckedRemainingvolume tobe infusedVTBIVolumeinfusedVIBatteryLiferemainingas %<strong>Pump</strong>deliveringY/NTimeRemainingSitepositionandconditionDesignationPrintSignatureStartTimeDateAStartVolumeBatteryLife %RateTimeRemainingBCDDiluentStartTimeDateAStartVolumeBBatteryLife %RateTimeRemainingCDDiluentPage 30 <strong>of</strong> 33
StartTimeDateAStartVolumeBBatteryLife %RateTimeRemainingCDDiluentPage 31 <strong>of</strong> 33
APPENDIX 4EQUALITY IMPACT ASSESSMENT TOOLTo be completed with <strong>the</strong> policy document when submitted to <strong>the</strong> appropriate committee <strong>for</strong>consideration, approval and ratification.1. Does <strong>the</strong> policy/guidance affect one group less ormore favourably than ano<strong>the</strong>r on <strong>the</strong> basis <strong>of</strong>:Yes/No Race No Ethnic origins (including gypsies and travellers) No Nationality No Gender No Culture No Religion or belief NoSexual orientation including lesbian, gay andbisexual people Age NoDisability - learning disabilities, physical disability,sensory impairment and mental health problems2. Is <strong>the</strong>re any evidence that some groups areaffected differently?3. If you have identified potential discrimination, are<strong>the</strong>re any exceptions valid, legal and/orjustifiable?4. Is <strong>the</strong> impact <strong>of</strong> <strong>the</strong> policy/guidance likely to benegative?5. If so can <strong>the</strong> impact be avoided? No6. What alternative are <strong>the</strong>re to achieving <strong>the</strong>policy/guidance without <strong>the</strong> impact?7. Can we reduce <strong>the</strong> impact by taking differentaction?NoNoNoNoNoNoNoCommentsIf you have identified a potential discriminatory impact <strong>of</strong> this policy document, please refer it to[insert name <strong>of</strong> appropriate person], toge<strong>the</strong>r with any suggestions as to <strong>the</strong> action required toavoid/reduce this impact. For advice in respect <strong>of</strong> answering <strong>the</strong> above questions, pleasecontact [insert name <strong>of</strong> appropriate person and contact details].Page 32 <strong>of</strong> 33
APPENDIX 5DISSEMINATION AND TRAINING PLANTo be completed with <strong>the</strong> policy document when submitted to <strong>the</strong> appropriate committee <strong>for</strong>consideration, approval and ratification.The status column must be given a Red, Amber or Green rating with evidence to demonstratean action has been completed.DISSEMINATION PLANTitle <strong>of</strong> document: <strong>Clinical</strong> <strong>Guidelines</strong> <strong>for</strong><strong>the</strong> <strong>Safe</strong> <strong>Use</strong> <strong>of</strong> <strong>McKinley</strong> <strong>T34</strong> <strong>Syringe</strong><strong>Pump</strong>Dissemination Lead: (Print name andcontact details) Sharon Woods, LorraineHodsonProposed action to retrieve out-<strong>of</strong>-datecopies <strong>of</strong> <strong>the</strong> document: N/ATo be disseminated to:All District NursesTRAINING PLANDate finalised: September 2009Previous document already being used? No (Please delete asappropriate)Disseminatedby whom?Event (Please provide details <strong>of</strong> available training venues/dates toeducate staff about this policy document)Timescale(Date)StatusR A GPaperorElectronicCommentsTimescale Owner StatusR A GE-Learning cascaded to all District Nurses4 weeksandOngoingTeamLeadersG2 x 2 day Training courses delivers to all District Nurses. Including Train<strong>the</strong> Trainer4 weeksandOngoingTeamLeadersGTraining Plan Lead (Please provide details <strong>of</strong> staff who will beresponsible <strong>for</strong> overseeing this training)AnnualupdateSr LorraineDowney/SrJean MorrisDistrict Nurse Team LeadersAdditional in<strong>for</strong>mation (Please provide details <strong>of</strong> any processes in placeto support implementation)Ongoing training will be supplied and coordinated by <strong>the</strong> Team leaders <strong>for</strong>new staffDenotes: Action not yet taken or deadline <strong>for</strong> action not met. Action plan to address this must be provided.Denotes: Action partially implemented.Denotes: Action complete.Page 33 <strong>of</strong> 33