Most Frequent RTP Reason Codes - Palmetto GBA
Most Frequent RTP Reason Codes - Palmetto GBA
Most Frequent RTP Reason Codes - Palmetto GBA
- No tags were found...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
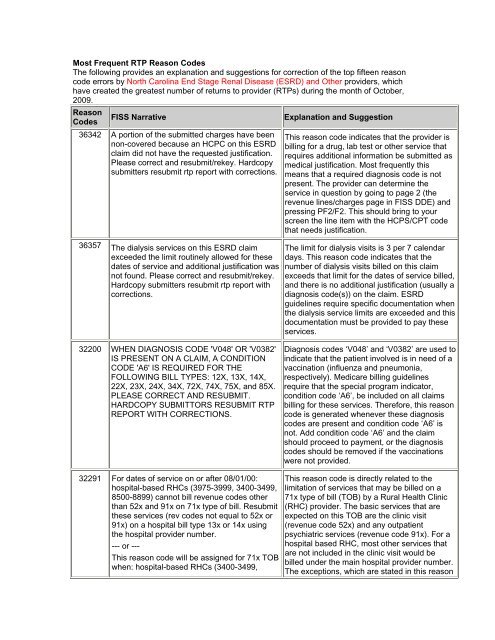
<strong>Most</strong> <strong>Frequent</strong> <strong>RTP</strong> <strong>Reason</strong> <strong>Codes</strong>The following provides an explanation and suggestions for correction of the top fifteen reasoncode errors by North Carolina End Stage Renal Disease (ESRD) and Other providers, whichhave created the greatest number of returns to provider (<strong>RTP</strong>s) during the month of October,2009.<strong>Reason</strong>FISS NarrativeExplanation and Suggestion<strong>Codes</strong>36342 A portion of the submitted charges have beennon-covered because an HCPC on this ESRDclaim did not have the requested justification.Please correct and resubmit/rekey. Hardcopysubmitters resubmit rtp report with corrections.36357 The dialysis services on this ESRD claimexceeded the limit routinely allowed for thesedates of service and additional justification wasnot found. Please correct and resubmit/rekey.Hardcopy submitters resubmit rtp report withcorrections.This reason code indicates that the provider isbilling for a drug, lab test or other service thatrequires additional information be submitted asmedical justification. <strong>Most</strong> frequently thismeans that a required diagnosis code is notpresent. The provider can determine theservice in question by going to page 2 (therevenue lines/charges page in FISS DDE) andpressing PF2/F2. This should bring to yourscreen the line item with the HCPS/CPT codethat needs justification.The limit for dialysis visits is 3 per 7 calendardays. This reason code indicates that thenumber of dialysis visits billed on this claimexceeds that limit for the dates of service billed,and there is no additional justification (usually adiagnosis code(s)) on the claim. ESRDguidelines require specific documentation whenthe dialysis service limits are exceeded and thisdocumentation must be provided to pay theseservices.32200 WHEN DIAGNOSIS CODE 'V048' OR 'V0382'IS PRESENT ON A CLAIM, A CONDITIONCODE 'A6' IS REQUIRED FOR THEFOLLOWING BILL TYPES: 12X, 13X, 14X,22X, 23X, 24X, 34X, 72X, 74X, 75X, and 85X.PLEASE CORRECT AND RESUBMIT.HARDCOPY SUBMITTORS RESUBMIT <strong>RTP</strong>REPORT WITH CORRECTIONS.Diagnosis codes ‘V048’ and ‘V0382’ are used toindicate that the patient involved is in need of avaccination (influenza and pneumonia,respectively). Medicare billing guidelinesrequire that the special program indicator,condition code ‘A6’, be included on all claimsbilling for these services. Therefore, this reasoncode is generated whenever these diagnosiscodes are present and condition code ‘A6’ isnot. Add condition code ‘A6’ and the claimshould proceed to payment, or the diagnosiscodes should be removed if the vaccinationswere not provided.32291 For dates of service on or after 08/01/00:hospital-based RHCs (3975-3999, 3400-3499,8500-8899) cannot bill revenue codes otherthan 52x and 91x on 71x type of bill. Resubmitthese services (rev codes not equal to 52x or91x) on a hospital bill type 13x or 14x usingthe hospital provider number.--- or ---This reason code will be assigned for 71x TOBwhen: hospital-based RHCs (3400-3499,This reason code is directly related to thelimitation of services that may be billed on a71x type of bill (TOB) by a Rural Health Clinic(RHC) provider. The basic services that areexpected on this TOB are the clinic visit(revenue code 52x) and any outpatientpsychiatric services (revenue code 91x). For ahospital based RHC, most other services thatare not included in the clinic visit would bebilled under the main hospital provider number.The exceptions, which are stated in this reason
<strong>Reason</strong><strong>Codes</strong>FISS Narrativebeing billed is valid for the dates of service onthe claim.32005 The statement covers from date is less thanthe provider's effective date on the providerfile. Note: for the following type bills, use theeffective date in the inpatient Provider Filerecord: 11x, 18x, 21x, 28x, 32x, 33x, 34x, 41x,51x, 75x. For all other type bills, use theeffective date in the outpatient Provider Filerecord.32011 The statement covers from date is before theprovider's fiscal start date, and the statementcovers to date is after the provider's fiscal startdate. Verify the information billed. Pleasecorrect and resubmit/rekey.Hardcopy submitters resubmit rtp report withcorrections.Explanation and SuggestionThis error usually occurs as a result of aprovider billing for a date of service that is priorto its official effective date under the submittedprovider number. <strong>Frequent</strong>ly this will occurwhen a provider is changing its billing statusand provider number, such as changing from anacute care PPS hospital to a critical accesshospital (CAH). The “from” date on the claimmust be changed to a date equal to or after theProvider File effective date.This reason code is usually secondary toreason code 32005 (which see above). The“from” date on the claim must be changed to adate equal to or after the provider’s fiscal startdate contained in the Provider File.32063 The statement covers from and through dateon this claim is before your fiscal year startdate on the Provider File. Please verify that thedates on the claim are correct; if the dates arenot correct, make changes and re-sendThe claim for processing. If dates on the claimare correct and the date on the date on theprovider is incorrect, pleaseContact our service center staff.This reason code is frequently received inconjunction with reason code 32005 (which seeabove). However, this error can also occurwhen a provider is billing for very old dates ofservice which may be before the fiscal periodsbeing maintained on the Provider File. If this isthe case, the provider should contact the<strong>Palmetto</strong> <strong>GBA</strong> provider contact center (PCC) toreport this problem.If you encounter some other reason code that you are unable to decipher, please submit it to ususing the “I Have a Question” form included in the Medicare Advisory.