Claims Submission Errors â February 2008 - Palmetto GBA
Claims Submission Errors â February 2008 - Palmetto GBA
Claims Submission Errors â February 2008 - Palmetto GBA
- No tags were found...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
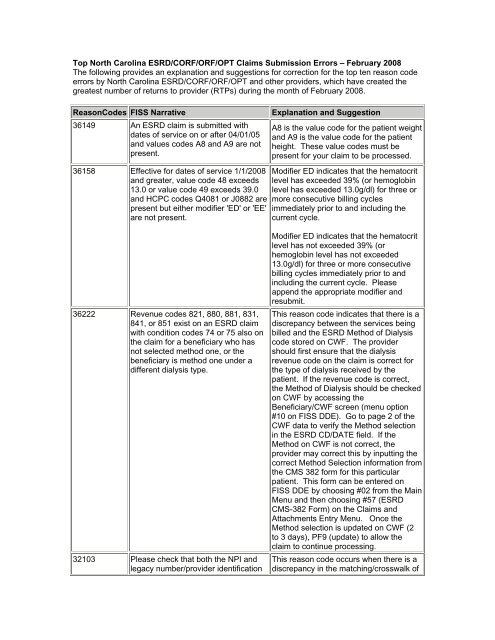
Top North Carolina ESRD/CORF/ORF/OPT <strong>Claims</strong> <strong>Submission</strong> <strong>Errors</strong> – <strong>February</strong> <strong>2008</strong>The following provides an explanation and suggestions for correction for the top ten reason codeerrors by North Carolina ESRD/CORF/ORF/OPT and other providers, which have created thegreatest number of returns to provider (RTPs) during the month of <strong>February</strong> <strong>2008</strong>.ReasonCodes FISS Narrative36149 An ESRD claim is submitted withdates of service on or after 04/01/05and values codes A8 and A9 are notpresent.36158 Effective for dates of service 1/1/<strong>2008</strong>and greater, value code 48 exceeds13.0 or value code 49 exceeds 39.0and HCPC codes Q4081 or J0882 arepresent but either modifier 'ED' or 'EE'are not present.Explanation and SuggestionA8 is the value code for the patient weightand A9 is the value code for the patientheight. These value codes must bepresent for your claim to be processed.Modifier ED indicates that the hematocritlevel has exceeded 39% (or hemoglobinlevel has exceeded 13.0g/dl) for three ormore consecutive billing cyclesimmediately prior to and including thecurrent cycle.36222 Revenue codes 821, 880, 881, 831,841, or 851 exist on an ESRD claimwith condition codes 74 or 75 also onthe claim for a beneficiary who hasnot selected method one, or thebeneficiary is method one under adifferent dialysis type.32103 Please check that both the NPI andlegacy number/provider identificationModifier ED indicates that the hematocritlevel has not exceeded 39% (orhemoglobin level has not exceeded13.0g/dl) for three or more consecutivebilling cycles immediately prior to andincluding the current cycle. Pleaseappend the appropriate modifier andresubmit.This reason code indicates that there is adiscrepancy between the services beingbilled and the ESRD Method of Dialysiscode stored on CWF. The providershould first ensure that the dialysisrevenue code on the claim is correct forthe type of dialysis received by thepatient. If the revenue code is correct,the Method of Dialysis should be checkedon CWF by accessing theBeneficiary/CWF screen (menu option#10 on FISS DDE). Go to page 2 of theCWF data to verify the Method selectionin the ESRD CD/DATE field. If theMethod on CWF is not correct, theprovider may correct this by inputting thecorrect Method Selection information fromthe CMS 382 form for this particularpatient. This form can be entered onFISS DDE by choosing #02 from the MainMenu and then choosing #57 (ESRDCMS-382 Form) on the <strong>Claims</strong> andAttachments Entry Menu. Once theMethod selection is updated on CWF (2to 3 days), PF9 (update) to allow theclaim to continue processing.This reason code occurs when there is adiscrepancy in the matching/crosswalk of
ReasonCodes FISS NarrativeNumber (pin)/OSCAR are correct andhave been entered on the claim.70045 Please verify the charges indicated onthis claim. If they are correct pleaseindicate in Remarks section of theclaim. If they are not correct pleasecorrect your charges and resubmit.32116 The receipt date of the claim is on orafter the NPI implementation date inThe system control file and the billingprovider NPI is not present on theclaim.31300 The Payer ID in UB-82 field 57 isinvalid. Valid entries are as follows:A = EGHP E = WC H = BLB = ESRD F = PHS I = VAC = COND G = LGHP Z =MedicareD = Auto32291 For dates of service on or after08/01/00:Hospital-based RHCs (3975-3999,3400-3499, 8500-8899) cannot billrevenue codes other than 52X and91X on 71X type of bill.Resubmit these services (rev codesnot equal to 52X or 91X) on a hospitalbill type 13X or 14X using the hospitalprovider number.--- or ---This reason code will be assigned for71X TOB when:Hospital-based RHCs (3400-3499,3975-3999, 8500-8899) bill claimsWith dates of service on or after01/01/02 and revenue code 0401 ispresent without HCPCS 76090,76091, or G0236 or revenue code0403 is present without HCPCSExplanation and Suggestionyour NPI to your legacy (34-xxxx)provider number. Please verify that yourlegacy number has been includedcorrectly in NPPES and that your NPI hasbeen included on any CMS-855submission.*Also note that these errors may havebeen caused by recent FISS processingproblems.This edit for high-dollar claims has beenrescinded.Resubmit your claim after entering theappropriate NPI.First of all, this reason code incorrectlyidentifies the field in error as form locator(FL) 57 on the UB-92. The Payer ID is FL50. This reason code is produced whenother insurance is primary. FISS requiresthat the Payer ID code correspond to thetype of other insurance coverageprovided by the primary payer. Check thePayer ID codes included in the narrativefor this reason code, and/or refer to page7 of the FISS DDE Help Sheets for thecorrect code for the coverage being billedfor this patient.This reason code is directly related to thelimitation of services that may be billed ona 71x type of bill (TOB) by a Rural HealthClinic (RHC) provider. The basic servicesthat are expected on this TOB are theclinic visit (revenue code 52x) and anyoutpatient psychiatric services (revenuecode 91x). For a hospital based RHC,most other services that are not includedin the clinic visit would be billed under themain hospital provider number. Theexceptions, which are stated in thisreason code narrative, aremammography services (revenue codes401 and 403), glaucoma screening(revenue code 770 with HCPCS codeG0117 or G0118), and the treatment ofdiabetic patients with diabetic sensoryneuropathy and/or LOPS (loss ofprotective sensation) (revenue code 940
ReasonCodes FISS Narrative76092 or 76085. Revenue code 52Xmust also be present on the claim.*Effective 01/01/04, CAD code G0236is replaced by HCPCS 76082 andCAD code 76085 is replaced byHCPCS 76083.--- Or ---This reason code will be assigned for71X TOB when:Hospital-based RHCs (3400-3499,3975-3999, 8500-8899) and freestandingRHCs (8900-8999) billclaims with dates of service on or after01/01/02 and revenue code 770 ispresent without HCPCS G0117 orG0118. Revenue code 52X must alsobe present on the claim.--- Or ---This reason code will be assigned for71X TOB when:Hospital-based RHCs (3400-3499,3975-3999, 8500-8899) and freestandingRHCs (8900-8999) billclaims with dates of service on or after07/01/02 and revenue code 940 ispresent without HCPCS G0245,G0246, or G0247. Revenue code 52Xmust also be present on the claim.19202 The first 3 positions of the attendingphysician's UPIN (Fld 82) must bealpha or numeric. Spaces are notallowed in the first 3 positions. Thephysician's last name and first initialare also required.31202 For the second occurrence code, thedate exceeds the through date.Correct the invalid occurrence codedate.Explanation and Suggestionwith HCPCS code G0245, G0246 orG0247). Any services other than thoseindicated here being billed on a 71x TOBwill be returned to provider (RTP) withthis reason code.This reason code means FISS hasdetected an unacceptable character inthe first three positions of the AttendingPhysician UPIN field. Use the TAB key tomove to the UPIN field; erase the fieldcompletely using END or CTRL + END;retype the correct UPIN data; ENTER tosee that the data is formatted correctly;then resubmit (F9/PF9). This reasoncode may indicate a problem in yourelectronic (ANSI 837) claim record beingsubmitted to EDI.Self-explanatory. Occurrence code datemust fall with the span dates of yourclaim.