Who Cares Wins - Royal College of Psychiatrists
Who Cares Wins - Royal College of Psychiatrists
Who Cares Wins - Royal College of Psychiatrists
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
2: Can Interventions<br />
Improve Outcome?<br />
2.1 The majority <strong>of</strong> mental disorder co-morbidity affecting older people in general hospitals is due to<br />
three disorders; dementia, depression and delirium (see Section 1) and these have been the<br />
focus <strong>of</strong> research. Older people with medical illnesses and hip fracture have particularly high<br />
levels <strong>of</strong> co-morbidity and form the populations for the majority <strong>of</strong> these studies. Recent years<br />
have seen the publication <strong>of</strong> important controlled trials involving older people demonstrating<br />
effective prevention and treatment. There is little information on the management <strong>of</strong> other mental<br />
disorders affecting older people.<br />
2.2 Also important are reports on the effect <strong>of</strong> providing different styles <strong>of</strong> consultation-liaison mental<br />
health services to general hospitals.<br />
2.3 A pre-requisite to instituting treatment or referral for a mental health assessment is the ability to<br />
identify the problem. Reported detection rates for mental disorder in older people in general<br />
hospitals indicate difficulties at this stage. Missed diagnosis rates for delirium <strong>of</strong> 32-67% (111) and<br />
for cognitive impairment <strong>of</strong> 55% (112,113) are typical examples. A meta-analysis <strong>of</strong> the prognosis<br />
<strong>of</strong> depression in older medical patients reported the detection rate for depression as “rare to<br />
26%”, with a median <strong>of</strong> 10% (114).<br />
2.4 Furthermore, there is an indication that general departments attempts to treat mental disorder are<br />
inconsistent. For example, depressed older medical patients may be as likely to receive<br />
benzodiazepines as antidepressants (115), as few as 25% <strong>of</strong> depressed older people with hip<br />
fracture receive antidepressants (106) and there seems to be an over reliance on psychotropic<br />
medication for the management <strong>of</strong> delirium (116). The use <strong>of</strong> psychological treatments is rare.<br />
There may be several explanations for these observations but poor knowledge, attitudes and skills<br />
combined with low confidence are likely to be significant factors.<br />
Delirium<br />
2.5 It is valuable to recognise the distinction between prevalent and incident delirium. Some older<br />
people arrive at the hospital with delirium (prevalent) while others develop delirium during their<br />
admission (incident). Studies aimed at prevention involve incident delirium and these have<br />
identified the most important characteristics that predict the risk <strong>of</strong> developing delirium (117).<br />
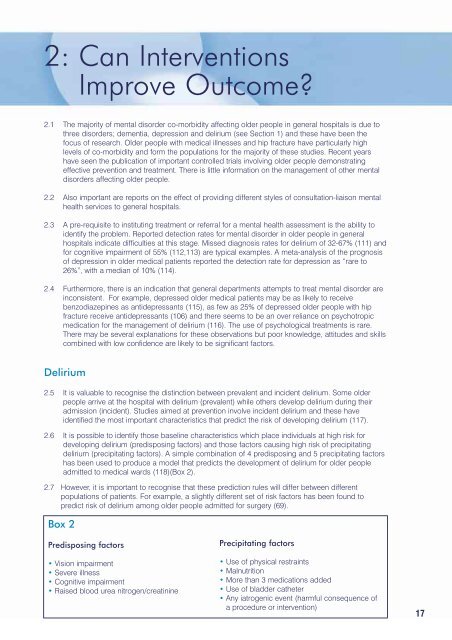
2.6 It is possible to identify those baseline characteristics which place individuals at high risk for<br />
developing delirium (predisposing factors) and those factors causing high risk <strong>of</strong> precipitating<br />
delirium (precipitating factors). A simple combination <strong>of</strong> 4 predisposing and 5 precipitating factors<br />
has been used to produce a model that predicts the development <strong>of</strong> delirium for older people<br />
admitted to medical wards (118)(Box 2).<br />
2.7 However, it is important to recognise that these prediction rules will differ between different<br />
populations <strong>of</strong> patients. For example, a slightly different set <strong>of</strong> risk factors has been found to<br />
predict risk <strong>of</strong> delirium among older people admitted for surgery (69).<br />
Box 2<br />
Predisposing factors<br />
• Vision impairment<br />
• Severe illness<br />
• Cognitive impairment<br />
• Raised blood urea nitrogen/creatinine<br />
Precipitating factors<br />
• Use <strong>of</strong> physical restraints<br />
• Malnutrition<br />
• More than 3 medications added<br />
• Use <strong>of</strong> bladder catheter<br />
• Any iatrogenic event (harmful consequence <strong>of</strong><br />
a procedure or intervention)<br />
17