Resection of floor of mouth cancers - Vula - University of Cape Town
Resection of floor of mouth cancers - Vula - University of Cape Town
Resection of floor of mouth cancers - Vula - University of Cape Town
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
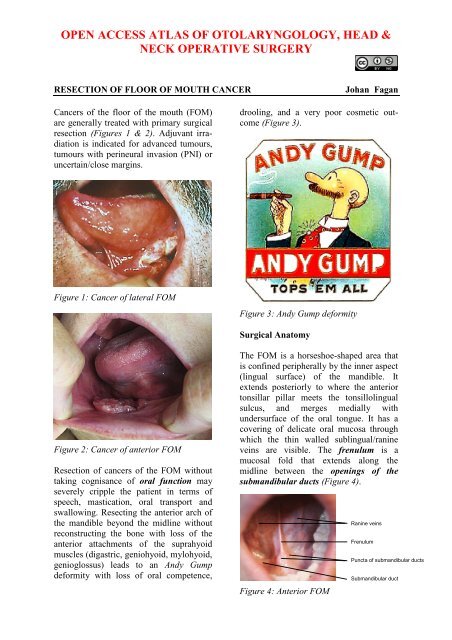
OPEN ACCESS ATLAS OF OTOLARYNGOLOGY, HEAD &NECK OPERATIVE SURGERYRESECTION OF FLOOR OF MOUTH CANCERJohan FaganCancers <strong>of</strong> the <strong>floor</strong> <strong>of</strong> the <strong>mouth</strong> (FOM)are generally treated with primary surgicalresection (Figures 1 & 2). Adjuvant irradiationis indicated for advanced tumours,tumours with perineural invasion (PNI) oruncertain/close margins.drooling, and a very poor cosmetic outcome(Figure 3).Figure 1: Cancer <strong>of</strong> lateral FOMFigure 3: Andy Gump deformitySurgical AnatomyFigure 2: Cancer <strong>of</strong> anterior FOM<strong>Resection</strong> <strong>of</strong> <strong>cancers</strong> <strong>of</strong> the FOM withouttaking cognisance <strong>of</strong> oral function mayseverely cripple the patient in terms <strong>of</strong>speech, mastication, oral transport andswallowing. Resecting the anterior arch <strong>of</strong>the mandible beyond the midline withoutreconstructing the bone with loss <strong>of</strong> theanterior attachments <strong>of</strong> the suprahyoidmuscles (digastric, geniohyoid, mylohyoid,genioglossus) leads to an Andy Gumpdeformity with loss <strong>of</strong> oral competence,The FOM is a horseshoe-shaped area thatis confined peripherally by the inner aspect(lingual surface) <strong>of</strong> the mandible. Itextends posteriorly to where the anteriortonsillar pillar meets the tonsillolingualsulcus, and merges medially withundersurface <strong>of</strong> the oral tongue. It has acovering <strong>of</strong> delicate oral mucosa throughwhich the thin walled sublingual/ranineveins are visible. The frenulum is amucosal fold that extends along themidline between the openings <strong>of</strong> thesubmandibular ducts (Figure 4).Figure 4: Anterior FOMRanine veinsFrenulumPuncta <strong>of</strong> submandibular ductsSubmandibular duct
The mylohoid muscle forms the diaphragm<strong>of</strong> the <strong>mouth</strong> and separates the FOM fromthe submental and submandibular triangles<strong>of</strong> the neck (Figures 5, 6, 7).Lingual nerveSublingual glandSubmandibular ductSubmandibular glandMylohyoid muscleGeniohyoid muscleFigure 5: Superior view <strong>of</strong> FOM andsubmandibular gland and duct, lingualnerve and mylohyoid and geniohyoidmusclesducts (Figures 5, 6), oral component <strong>of</strong>submandibular salivary glands (Figures 5,6, 7), genioglossus muscle (Figure 8), andthe lingual (Figures 5, 6, 7) and hypoglossalnerves (Figure 8).The paired sublingual salivary glands arelocated beneath the mucosa <strong>of</strong> the anterior<strong>floor</strong> <strong>of</strong> <strong>mouth</strong>, anterior to the submandibularducts and above the mylohyoid andgeniohyoid muscles (Figures 5, 6, 7). Theglands drain via 8-20 excretory ducts <strong>of</strong>Rivinus into the submandibular duct andalso directly into the <strong>mouth</strong> on an elevatedcrest <strong>of</strong> mucous membrane called the plicafimbriata which is formed by the gland andis located to either side <strong>of</strong> the frenulum <strong>of</strong>the tongue (Figures 6, 7).Lingual nerveSubmandibular ductSublingual glandSubmandibular glandMylohyoid muscleFigure 6: Intraoral view <strong>of</strong> left sublingualgland with ducts <strong>of</strong> Rivinus,submandibular gland and duct, lingualnerve and mylohyoid musclesFigure 7: Sagittal view <strong>floor</strong> <strong>of</strong> <strong>mouth</strong>Lingual nerveIntraoral SMGFloor <strong>of</strong> <strong>mouth</strong>Ducts <strong>of</strong> RivinusSublingual glandMylohyoidSubmental arteryCervical SMGThe following structures are locatedbetween the mucosa and the mylohyoidmuscle: paired geniohyoid muscles in themidline (Figure 5); sublingual salivaryglands (Figures 5, 6, 7), submandibularFigure 8: XIIn accompanied by ranineveinsThe submandibular duct is locatedimmediately deep to the mucosa <strong>of</strong> theanterior and lateral FOM, and opens intothe oral cavity to either side <strong>of</strong> thefrenulum (Figures 4, 5, 6).The lingual nerve provides sensation tothe <strong>floor</strong> <strong>of</strong> the <strong>mouth</strong>. It crosses deep tothe submandibular duct in the lateral <strong>floor</strong><strong>of</strong> <strong>mouth</strong> (Figures 5, 6, 7). In the anteriorFOM it is located posterior to the duct(Figure 5).2
Ranine veins are visible on the ventralsurface <strong>of</strong> the tongue, and accompany thehypoglossal nerve (Figures 4, 8).Arterial supply to the tongue and FOM isderived from the lingual artery and itsbranches (ranine artery, dorsalis linguae,and sublingual arteries) (Figures 8, 9);and the mylohyoid and submentalbranches <strong>of</strong> the facial artery.The lingual artery arises from the externalcarotid artery between the superior thyroidand facial arteries and courses obliquelyforwards and medial to the greater cornu <strong>of</strong>the hyoid (Figures 8, 9).genioglossus and mylohyoid and suppliesthe sublingual salivary gland and mucousmembrane <strong>of</strong> the FOM and gingiva(Figures 8, 9). A branch <strong>of</strong> the sublingualartery pierces the mylohyoid muscle andanastomoses with the submental branch <strong>of</strong>the facial artery.The submental branch <strong>of</strong> the facial arterycourses along the inferior, inner margin <strong>of</strong>the mandible (Figures 10). The mylohyoidartery and vein are encountered when thesurgeon elevates the submandibular glandfrom the lateral surface <strong>of</strong> the mylohyoid(Figures 10 & 11). It branches from theinferior alveolar artery just before it entersthe mandibular foramen, crosses themylohyoid, and disappears anteriorlybehind the digastric. It has connectionswith the submental artery, and via a defectin the mylohyoid with the sublingual arteryin the <strong>floor</strong> <strong>of</strong> the <strong>mouth</strong>.Ranine arteryFigure 9: Lingual arterySublingual arteryLingual arteryDorsalis linguae arterySubmental arteryMylohyoid muscleMylohyoid arteryFacial arteryIt then loops downward and anteriorly andcrosses medial to XIIn and the stylohyoidmuscle. It then courses directly anteriorlybelow hyoglossus and finally ascends asthe ranine artery (pr<strong>of</strong>unda linguae)submucosally on the undersurface <strong>of</strong> thetongue as far as its tip; it lies to either side<strong>of</strong> the genioglossus, and is accompanied bythe lingual nerve. Two or three smalldorsales linguæ arteries arise beneath thehyoglossus and ascend to the posterior part<strong>of</strong> the dorsum <strong>of</strong> the tongue and alsosupply the mucous membrane <strong>of</strong> theposterior FOM, and oropharynx. Thesublingual artery arises from the lingualartery at the anterior edge <strong>of</strong> thehyoglossus and runs forward between theFigure 10: Facial artery emerges frombehind posterior belly <strong>of</strong> digastric(removed), and gives rise to a fewbranches including submental arteryFigure 11: Mylohyoid artery is a branch <strong>of</strong>the inferior alveolar artery3
The mandible forms the peripheral border<strong>of</strong> the FOM, and may be involved by FOMtumours or may have to be divided(mandibulotomy) or resected (alveolectomy/ marginal mandibulectomy / segmentalmandibulectomy / hemimandibulectomy).Important surgical featuresare the position <strong>of</strong> the mental foraminathrough which the mental nerves exit toinnervate the lower lip, the mylohyoid lineto which the mylohyoid muscle attaches,and when planning a marginalmandibulectomy, the height <strong>of</strong> the body <strong>of</strong>the mandible and the depth <strong>of</strong> the dentalroots (Figures 12a, b).The mental foramen and inferior alveolarnerve may be very close to the superiorsurface <strong>of</strong> a resorbed mandible such as isseen in older, edentulous patients (Figure13). A marginal mandibulectomy may alsonot be possible in such a resorbedmandible due to the lack <strong>of</strong> residual bone.Mental foramenFigure 13: Position <strong>of</strong> mental foramen in aresorbed mandibleSurgical ObjectivesFigure 12a: Attachments <strong>of</strong> mylohyoid,geniohyoid, genioglossus and digastricmuscles to inner aspect <strong>of</strong> mandibleFigure 12b: Attachments <strong>of</strong> muscles toouter aspect <strong>of</strong> mandible and location <strong>of</strong>mental foramenClear resection marginsAvoid postoperative orocervicalfistulaeOptimise cosmesis and functiono Maintain length and mobility <strong>of</strong>the tongueo Avoid pooling <strong>of</strong> secretions andfood in the reconstructed FOMo Avoid obstruction <strong>of</strong> thesubmandibular ductso Avoid injury to lingual andhypoglossal nerveso Maintain mandibular continuityand strengtho Restore dentitionThe author advocates elective neckdissection (END) levels I-IV for squamouscell carcinomas that are >4mm thick and/or >T2 stage. A useful rule <strong>of</strong> thumb is that4
a palpable tumour is likely to have atumour thickness that warrants END.Tumours <strong>of</strong> the anterior FOM thatapproach the midline require bilateralEND.The remainder <strong>of</strong> this chapter will focus onthe surgical treatment <strong>of</strong> the primarytumour.Preoperative evaluationseen on Panorex may be removed atthe time <strong>of</strong> the surgery5. Mandible: Tumour may involveperiosteum, invade only the innercortex, or involve medullary bone.Panorex shows gross involvement <strong>of</strong>bone (Figure 14). Invasion <strong>of</strong> corticalbone is better assessed with CT scan(Figure 15); MRI is superior forassessing invasion <strong>of</strong> medullary bone.1. Are there synchronous primaries,cervical or distant metastases?2. Is the tumour resectable? Other thantumours that extend posteriorly toinvolve the carotid sheath, very fewFOM tumours are irresectable. The keyconsideration is surgical morbidity; thisin turn is dependent on the range andreliability <strong>of</strong> reconstructive surgery thatare available e.g. resection <strong>of</strong> themandible beyond the midline can onlybe done if it is possible to reconstructthe bone with a free fibula flap so as toavoid an Andy Gump deformity(Figure 3).3. Is there clinical evidence <strong>of</strong>perineural invasion (PNI)? Examinethe patient for neurological deficits <strong>of</strong>the hypoglossal, mental, inferioralveolar and lingual nerves. Widening<strong>of</strong> the alveolar canal on mandibularorthopantomography (Panorex) may beseen. MRI can demonstrate PNI.Should there be evidence <strong>of</strong> PNI thenthe affected nerve should be dissectedproximally until a clear tumour marginis obtained on frozen section. In thecase <strong>of</strong> the inferior alveolar nerve, thiswould require a hemi- or segmentalmandibulectomy that encompasses theentire inferior alveolar canal.4. Status <strong>of</strong> dentition? Carious teeth maycause osteoradionecrosis. Carious teethFigure 14: Panorex view <strong>of</strong> erosion andpathological fractureFigure 15: Cortical erosion visible on CTIn the absence <strong>of</strong> CT scanning, thesurgeon may elect to strip tumour <strong>of</strong>fbone at the time <strong>of</strong> resection to inspectthe bone for evidence <strong>of</strong> tumourinfiltration and to decide how toproceed. If only the periosteum isinvolved then a marginalmandibulectomy (removal <strong>of</strong> cortical5
one) will suffice. Should marginalmandibulectomy be considered, thenthe vertical height <strong>of</strong> the mandibleshould be assessed clinically or byPanorex so as to predict whether a freebony composite flap would be requiredto bolster the remaining mandible.Once the cortex is invaded, then eithera marginal or segmental mandibulectomyis required. Once the medullais invaded, then a segmental orhemimandibulectomy is done thatincludes at least a 2cm length <strong>of</strong>mandible on either side <strong>of</strong> the tumour.6. Is a tracheostomy required? Patientswith small tumours <strong>of</strong> the anteriorFOM may not require temporarytracheostomy. However whenever thelaryngeal support <strong>of</strong> the mylohyoid,geniohyoid and genioglossus musclesis lost, and especially when a flap isused to reconstruct a FOM defect, thepatient is at risk <strong>of</strong> airway obstructionand should have a temporarytracheostomy inserted.7. Submandibular salivary glands: Atumour <strong>of</strong> the FOM may invade thesubmandibular duct and cause a hard,fibrotic submandibular salivary glandthat can be confused with a lymphnode metastasis. In a small T1 anteriorFOM tumour that involves the duct inwhich an END is not planned theremaining duct may have to betranslocated so as preserve salivaryflow. This is simply done by tunnellingover the duct with a haemostat justbelow the mucosa <strong>of</strong> the lateral FOM.The end <strong>of</strong> the transected duct is thengrasped with the haemostat and passedposteriorly along the tunnel anddelivered through a stab incision. It issecured to the mucosa with anabsorbable suture (Figure 16).8. What type <strong>of</strong> reconstruction isrequired?Figure 16: Submandibular ducttranslocated to right lateral <strong>floor</strong> <strong>of</strong> <strong>mouth</strong>and sutured to mucosa with a vicryl sutureAnaesthesiaNasal intubation is followed bytracheostomy. Perioperative antibiotics areadministered.Surgical accessTransoral: Smaller tumours (T 1 -T 2 ) areusually easily excised though the open<strong>mouth</strong> in an edentulous patient. The <strong>mouth</strong>is kept widely open either with a dentalbite bock (Figure 17) or with a selfretainingretractor taking care to protect theteeth (Figure 18).Figure 17: Dental bite block is interposedbetween lateral teeth to keep <strong>mouth</strong> open6
Sublingual glandMidline lip-split: The lip is split in themidline after scoring/marking thevermillion border so as to ensure anaccurate repair. The s<strong>of</strong>t tissues arestripped <strong>of</strong>f the front <strong>of</strong> the mandible(Figure 20).Submandibular ductFigure 18: Self-retaining retractor inplace; sublingual salivary gland andsubmandibular ductHowever, resecting an anterior FOMtumour may be quite challenging in apatient with a full set <strong>of</strong> lower teeth as theteeth may obstruct access to the anteriorFOM. In such cases lower teeth may needto be extracted and a marginal mandibulectomy(Figure 19) or a mandibulotomymay be required for access.When a FOM tumour abuts the anteriormandible then doing a marginalmandibulectomy in continuity with thetumour resection greatly facilitatesresection by freeing up the tumour.Figure 19: This marginal mandibulectomydefect was covered by advancinggingivolabial mucosa over the bone andsuturing it to the edge <strong>of</strong> the FOM defectFigure 20: Midline lip-split incision andpreplating <strong>of</strong> mandible before performingsegmental mandibulectomy and resectingtumourVisor flap: This is achieved by cuttingalong the gingivolabial and gingivobuccalsulci about 1cm from the bone so as topermit placement <strong>of</strong> sutures when closingthe wound, and then stripping the s<strong>of</strong>ttissues from the outer aspect <strong>of</strong> themandible. Take care not to transect themental nerves if they can be saved. Theskin flap is then retracted superiorly toexpose the mandible (Figure 21).Pull-through: This may be employedwhen the tumour stops some distance fromthe inner aspect <strong>of</strong> the mandible.Following bilateral neck dissections <strong>of</strong>Levels 1a and 1b, the mandibularattachments <strong>of</strong> the anterior bellies <strong>of</strong>digastric, mylohyoid, geniohyoids andgenioglossus are divided withelectrocautery working from inferiorly(Figure 12a). The mucosa <strong>of</strong> the anteriorFOM is then divided 1cm from the inner7
aspect <strong>of</strong> the mandible (so as to facilitatelater repair). This permits the surgeon todeliver the anterior FOM and anteriortongue into the neck and then to proceedwith the resection.height <strong>of</strong> the outer cortex for mandibularstrength, but to remove the inner cortexthat abuts the tumour. With segmentalmandibulectomy the bone is cut at least2cm from visible tumour (Figure 21).Tumour: Once the mandibulectomy hasbeen completed, keep the bone attached tothe tumour specimen and divide thegingival mucosa on the inside <strong>of</strong> bone cuts;this will release the tumour from bone andfacilitate delivery <strong>of</strong> the tumour into thesurgical field. Identify and preserve thesubmandibular duct(s), and the lingual andhypoglossal nerve(s) if possible. Thesublingual gland may be encountered inanterior FOM cancer resections (Figure18).Figure 21: Visor approach with anteriorsegmental mandibulectomy for cancer <strong>of</strong>anterior FOM and gingivaTumour <strong>Resection</strong>First complete Levels 1a and b <strong>of</strong> the neckdissection(s) before proceeding to theresection. This permits the surgeon to cutthrough the muscles in the FOM andtongue knowing the location <strong>of</strong> the XIIn,lingual nerve and lingual artery.Mandibulectomy: If a marginal orsegmental mandibulectomy is plannedthen it should be done before resecting theFOM tumour as it improves surgicalexposure (Figure 21). If a segmentalmandibulectomy is to be done, then preplatethe mandible with a reconstructionplate so as to ensure alignment <strong>of</strong> the teethand a good bony contour (Figure 20).Marginal mandibulectomy is done withsmall sharp osteotomes so as to avoidinadvertent fracture <strong>of</strong> the mandible, orwith a powered oscillating or reciprocatingsaw. With marginal mandibulectomy thecut is made obliquely so as to preserve theUse diathermy to resect the tumour with atleast 1cm margins. Cauterise the raninevessels during the resection. Largerbranches <strong>of</strong> the lingual artery are ligated asthey are encountered. Obtain frozensection confirmation <strong>of</strong> clear tumourmargins if available.RepairFollowing resection the surgeon carefullyassesses the defect to determine how bestto restore form and function i.e.mandibular integrity and contour, and oralcompetence, mastication, oral transport,swallowing and speech.Reconstruction pointersMobility <strong>of</strong> the tongue is key to oralfunctionIt is imperative that reconstructivesurgeons follow patients long-term tolearn how best to optimise functionalflap designTongue length is more important thanwidth8
Never suture the edge <strong>of</strong> the tongue tothe gingiva; in such cases alwaysmaintain tongue mobility with a flapAvoid tethering the tip <strong>of</strong> the tongueSome defects are best left open to healby secondary intention so as to retainmobilitySimply shaping a flap to match theresected tissue may well restore formbut may have poor functional resultToo broad a flap in the FOM will causepooling <strong>of</strong> saliva and adversely affectoral transportA marginal mandibulectomy may bedone as part <strong>of</strong> the reconstructiveprocedure to enable the surgeon tosuture the gingivobuccal orgingivolabial mucosa to the FOMmucosa or flap (Figure 19)Reduce the risk <strong>of</strong> orocervical fistulaby approximating the mylohyoid to thedigastric muscle in the neck, andensuring that the suction drain is notplaced in the upper neckNo repair: Small and/or superficialresections above the mylohyoid that do notcommunicate with the neck dissection maybe left open to heal like a tonsillectomywound. Resist the temptation to suturesuch defects as it may alter the shape <strong>of</strong> thetongue or fix the tongue to the anteriorFOM.Split skin graft: This may be used to covera defect that could otherwise be left openbut for concern about a through-andthroughcommunication to the neck, orover a marginal mandibulectomy defect(Figure 22). The skin is sutured to themargins <strong>of</strong> the defect with absorbablesutures, the ends <strong>of</strong> which are left a fewcentimetres long. A bolster <strong>of</strong> antisepticimpregnatedgauze is placed over the skingraft and tied down with the long sutures.The bolster is removed after about 5 days.Figure 22: Healed split skin graft overmarginal mandibulectomy defect 1Buccinator myomucosal flap: (Figures23a,b,c) This is an excellent flap for bothanterior and lateral FOM defects as it hasthe same physical qualities as tissues <strong>of</strong> theFOM. The pedicle however has to crossthe mandible and is therefore best suitedfor edentulous patients, patients withmissing teeth, or who have undergonemarginal mandibulectomy. (See chapter:Buccinator myomucosal flap)Primary closure: Avoid tethering ordistorting the tongue. Note the commentabout marginal mandibulectomy above(Figure 19).Figure 23a: FOM defect with marginalmandibulectomy9
Figure 23b: Buccinator flap based onfacial arteryFigure 24a: Marginal mandibulectomydefectFigure 23 c: Buccinator flap for FOMresection with marginal mandibulectomyFigure 24b: Onlay radial osseocutaneousflapPectoralis major flap: This flap is onlyused if other flaps listed are not available.(See chapter: Pectoralis major flap)Radial free forearm flap: This is a popularchoice for FOM repair as the flap is thinand pliable. An osseocutaneous flap can beused as an onlay graft with marginalmandibulectomy defects (Figure 24a, b)Anterolateral free thigh flap: Muscleharvested with the flap can be tailoredaccording to the volume <strong>of</strong> the defect to befilled. However it is less pliable than theradial free forearm flap and is only suitablefor oral reconstruction in patients with thinthighs.Figure 25: Anterolateral free thigh flapused for lateral FOM and tongue defectFree fibula flap: This is the workhorse <strong>of</strong>mandible reconstruction followingsegmental mandibulectomy, but can alsobe used as an onlay flap. It is suitable fordental implants (Figure 27 a, b).10
Figure 26a: Resected FOM minor salivarygland tumourFigure 26c: Mandible reconstructed withfree fibula flapFigure 27a: Dental implants following freefibula flap for segmental mandibulectomyFigure 26b: Note absent mandibular bodyand FOMFigure 27b: Denture being slipped intoplace over implantsTitanium reconstruction plate: Althoughit can be used to replace mandible, it isprone to extrusion both to the inside <strong>of</strong> the<strong>mouth</strong> and through skin (Figure 28).11
THE OPEN ACCESS ATLAS OFOTOLARYNGOLOGY, HEAD &NECK OPERATIVE SURGERYwww.entdev.uct.ac.zaFigure 28: Titanium plateThe Open Access Atlas <strong>of</strong> Otolaryngology, Head &Neck Operative Surgery by Johan Fagan (Editor)johannes.fagan@uct.ac.za is licensed under a CreativeCommons Attribution - Non-Commercial 3.0 UnportedLicenseFinal commentsResecting tumours <strong>of</strong> the FOM ischallenging particularly in terms <strong>of</strong>optimising oral function. The surgical teamhas to master a wide array <strong>of</strong> reconstructivetechniques so as to secure the bestfunctional and cosmetic outcomes.Reference1. Deleyiannis F, Dunklebarger J, Lee E,Gastman B, Lai S, Ferris R, Myers EN,Johnson J. Reconstruction <strong>of</strong> themarginal mandibulectomy defect: anupdate. Am J Otolaryngol Head NeckMed Surg. 2007; 28 (6): 363-6Author & EditorJohan Fagan MBChB, FCORL, MMedPr<strong>of</strong>essor and ChairmanDivision <strong>of</strong> Otolaryngology<strong>University</strong> <strong>of</strong> <strong>Cape</strong> <strong>Town</strong><strong>Cape</strong> <strong>Town</strong>South Africajohannes.fagan@uct.ac.za12