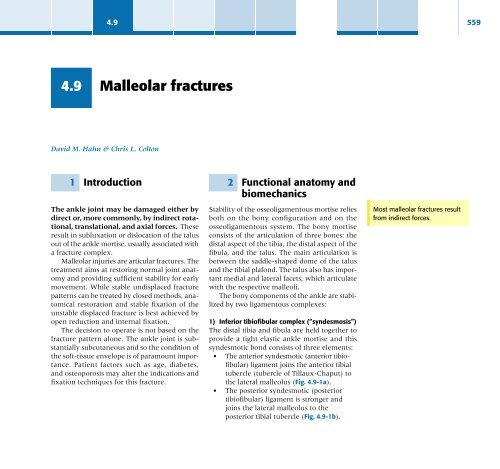
4.9 Malleolar fractures
4.9 Malleolar fractures
4.9 Malleolar fractures
- No tags were found...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
<strong>4.9</strong>5612.1 Mortise congruityThe talus remains in close contact with theentire articular surface of the mortise in allpositions of dorsiflexion and plantar flexion.This intimate contact is important for evendistribution of the load at the ankle [1] andmust be restored after injury. Biomechanicalstudies have shown that, rather than the anklesmoving as a hinge, this congruity is maintainedin all positions of dorsiflexion and plantar flexionby a combination of sliding and rotating ofthe talus, coupled with translational movementof the fibula [2, 3].Plantar flexion of the ankle is accompaniedby internal rotation of the talus; dorsiflexionresults in external rotation of the talus andcombined posterolateral translation and externalrotation of the fibula. This fibular motionat the syndesmosis is an essential part of thenormal ankle function.The total congruity of the articulation is themost important element in protecting the thinarticular cartilage of the ankle from high meanstress and secondary degeneration. Small disturbancesof this congruity reduce the contactarea and thereby overload the articularcartilage [4, 5].3 Pathogenesis/mechanism of injury:the basis of classificationThe position of the foot and the direction of thedeforming force dictate the pattern of failure ofthe osseoligamentous mortise. The position ofthe foot determines which structures are tightat the onset of the deformation, and thereforemost likely to fail first. If the foot is supinated(inverted), the lateral structures are tight andthe medial structures relaxed. By contrast, inpronation (everted), the medial structures aretight and fail first. The deforming force can berotational, usually external, or translational inabduction or adduction. The resulting specificfracture patterns of the lateral malleolus formthe basis for the classification (Fig. <strong>4.9</strong>-3).3.1 The infrasyndesmoticinjury (type A)(see Fig. <strong>4.9</strong>-9)With the foot supinated and an adduction deformingforce applied to the talus, the firstinjury will occur on the lateral side, which isunder tension. This may be either rupture of thelateral ligament, osseoligamentous avulsion ortransverse fracture of the lateral malleolus,at or just below the level of the tibial plafond(Fig. <strong>4.9</strong>-4a). If the deforming force thencontinues, the talus tilts and this causes ashearing compression fracture of the medialmalleolus (Fig. <strong>4.9</strong>-4b).3.2 The transsyndesmoticinjury (type B)(see Fig. <strong>4.9</strong>-10)The commonest pattern of injury occurswith axial loading of a supinated foot. Byvirtue of the obliquity of the axis, about whichsubtalar movement occurs, inversion results inexternal rotation of the talus (Fig. <strong>4.9</strong>-5). Firstly,the fibula fails producing an oblique fracture,The talus remains in contactthroughout the range of anklemovement.44-A1 44-B3 44-C2Fig. <strong>4.9</strong>-3: AO Müller ClassificationType A <strong>fractures</strong>:Transverse fracture of thelateral malleolus, at or justbelow the level of theankle joint.Small disturbances ofcongruity overload articularcartilage.Type B <strong>fractures</strong>:The commonest pattern ofinjury occurs with axial loadingof the supinated foot.
562 <strong>4.9</strong> <strong>Malleolar</strong> <strong>fractures</strong>—D.M. Hahn, C.L. Coltona)b)(i)(ii)(iii)Fig. <strong>4.9</strong>-4: Sequence of morphological changes givingrise to type A <strong>fractures</strong>.a) Failure in tension of the lateral side with the footsupinated and an adduction force applied:(i) rupture of the lateral ligament(ii) osseoligamentous avulsion(iii) transverse fibular fractureb) Medial injury resulting from forced talar adduction.With failure of the lateral side plus vertical axial load, thetalus tilts causing a shearing, compression fracture of themedial malleolus.a) b)Fig. <strong>4.9</strong>-5: a) The axis about which movement takesplace at the subtalar joint, is angled an average 42ºabove the horizontal and 16º medially.b) This causes the subtalar joint to act as a torqueconverter, similar to an angled hinge, so that as the oscalcis inverts, the talus is caused to rotate externally.
<strong>4.9</strong>563a) b) c)Fig. <strong>4.9</strong>-6: Sequence of morphological changes givingrise to type B <strong>fractures</strong>. Failure of lateral side with footin supination, resulting in violent talar external rotation.a) The first injury is an oblique fracture of the fibulastarting at the level of the ankle joint and passingposteriorly. This may be a non-displaced crack fractureif the deforming force ceases at this point.b) Progressive talar rotation causes posterior displacementof the fibular fracture.starting at the level of the ankle joint andextending proximally from anterior to posterior(Fig.<strong>4.9</strong>-6a). Progressive talar external rotationcauses posterior displacement resulting in eitheran injury to the posterior syndesmotic ligamentor fracture of the posterior malleolus. Finally,as the talus subluxates posteriorly, the medialcomplex fails either by rupture of the deltoidligament or by a transverse fracture of themedial malleolus (Fig. <strong>4.9</strong>-6c).c) Further talar rotation results in a fracture of theposterior articular lip of the tibia (Volkmann’s fracture)and as the talus leaves the mortise posteriorly, medialfailure (malleolar fracture or deltoid ligament rupture)occurs as the final event of the sequence.3.3 The suprasyndesmoticinjury (type C)(see Fig. <strong>4.9</strong>-11)A third type of injury occurs when the foot isin pronation, the medial structures are undertension (Fig. <strong>4.9</strong>-7), and an external rotationforce is applied. The first injury will occur onthe tensioned medial side in the form of adeltoid ligament rupture or a medial malleolaravulsion fracture. This allows the medial side ofthe talus to translate anteriorly. As the talusrotates externally, it forces the fibula to twistabout its vertical axis. This results a rupture of
564 <strong>4.9</strong> <strong>Malleolar</strong> <strong>fractures</strong>—D.M. Hahn, C.L. ColtonFig. <strong>4.9</strong>-7: Sequence of morphologicalchanges giving rise to type C <strong>fractures</strong>.Mechanism of failure with the foot inpronation and external rotation force applied.a) The first injury is failure of themedial side with deltoid ligamentrupture or medial malleolar fracture.This allows the talus to moveanteriorly as it laterally rotates.b) Finally the fibula <strong>fractures</strong>proximal to the syndesmosis.a)b)Ligamentous injuries can beinferred from the fracturepattern.the anterior syndesmotic ligament and then ofthe interosseous ligament. At this point the tibiadislocates medially off the rotating talus, forcingseparation (diastasis) of the fibula fromthe tibia. This causes failure of the posteriorsyndesmotic ligament (or rarely, avulsion of theposterior malleolus), and finally an indirectfracture of the shaft of the fibula, the level ofwhich depends on how far proximally of theinterosseous membrane it ruptures (Fig. <strong>4.9</strong>-8).The AO Müller Classification is based onthe ability to recognize and describe the x-rayappearance of the fracture pattern. Obviously,ligament complexes are not seen on x-rays,and so to understand fully the anatomy of theinjury, one needs to be able to infer theligamentous injuries from the fracturepattern.Fig. <strong>4.9</strong>-8: The fibula is caused to rotateand to translate laterally, causing failureof the syndesmotic ligaments.
<strong>4.9</strong>565Fig. <strong>4.9</strong>-9: Type A (44-A1.3)Transverse avulsion fracture of the fibula at or below thelevel of the ankle joint can be associated with a shearfracture of the medial malleolus and impaction of tibialplafond medially.Fig. <strong>4.9</strong>-10: Type B (44-B1.3)Oblique fracture of the distal fibula passingupwards and backwards from the level ofthe tibial plafond. As the talus continues torotate, the fibular fracture displacesposteriorly. The posterolateral corner of thetibia may fracture (Volkmann's triangle).The medial side may be either intact or arupture of the deltoid ligament, or atransverse fracture of the medial malleolusis present.Fig. <strong>4.9</strong>-11: Type C (44-C1.3)Medial failure occurs first, either as adeltoid ligament rupture or an avulsionfracture of the medial malleolus.The inferior tibiofibular ligaments tearas the syndesmosis opens up fromanteriorly, due to the external rotationand lateral translation of the fibula.Indirect fibular fracture then occursabove the syndesmosis.a) The anterior syndesmotic ligamentmay fail by avulsion either of theanterior tibial tubercle (of Tillaux-Chaput), orb) of its fibular attachment .c) Rarely does a posterior tibial lipfracture accompany this injurycomplex.a) b) c)
566 <strong>4.9</strong> <strong>Malleolar</strong> <strong>fractures</strong>—D.M. Hahn, C.L. Colton<strong>Malleolar</strong> <strong>fractures</strong> have aspecial code in the AO MüllerClassification.Widening of the medial jointspace indicates instability ofthe mortise.A transverse fibular fracture below the levelof the ankle joint implies an adduction injurywith the syndesmotic ligament remaining intact.With foot supination and talar externalrotation, the fibular fracture is oblique andstarts anteriorly at the level of the ankle jointwith possible partial disruption of the anteriorsyndesmotic complex (Fig. <strong>4.9</strong>-10). The interosseousmembrane, as a rule, remains intact. Theposterior syndesmotic complex is either intactor detached in continuity with a fracture of theposterior tibial lip (Volkmann’s triangle).An indirect fibular shaft fracture, not extendingbelow the syndesmotic ligaments, impliesthat both the medial and syndesmoticcomplexes have been disrupted and there islikely to be major instability. The interosseousmembrane, from the ankle joint proximally toat least the level of the fibular fracture, and thesyndesmotic ligaments are ruptured throughtheir substance or avulsed with their bonyattachments. Although this is the common andpotentially more serious implication of thispattern, a suprasyndesmotic spiral fracture mayoccur from a purely external rotation ofthe fibula. This will disrupt only the anteriortibiofibular ligament, resulting in a more stablepattern as the fibula rotates externally on theintact interosseous membrane and posteriortibiofibular ligament.On this basis, the three main types of ankle<strong>fractures</strong> described may be classified accordingto the level of the fibular fracture as A, B, andC with increasing instability of the mortise. Thisis the basis of the AO Müller Classification ofmalleolar <strong>fractures</strong>.The unique nature of the complexity ofmalleolar <strong>fractures</strong> and their necessary distinctionfrom vertical compression injuriesof the tibial pilon require the allocation tothem of a special code. As an exception tothe rest of the AO Müller Classification, aregional code 4 is used. <strong>Malleolar</strong> <strong>fractures</strong>are therefore categorized as 44.For deeper levels of the malleolar classification,refer to “The Comprehensive Classificationof Fractures of Long Bones” [6] and/or “The AOElectronic Long Bone Fracture Classification”[7].4 Fracture assessmentand decision makingThree radiographic views of the ankle are required.These are the anterioposterior view, theAP view obtained in 20° of internal rotation tobring the transmalleolar axis parallel tothe plate (mortise view) and the lateral view.Shortening of the fibula is best appreciated bya step in the alignment of the subchondralplates of the tibial plafond and the lateralmalleolus (Fig. <strong>4.9</strong>-12a/a’). The talocrural angleis 83° ± 4° and if greater or lesser indicatesinstability or displacement of the mortise.The joint space between the talus and plafondshould equal the space between the medialmalleolus and medial talus. Widening of themedial space is indicative of mortise displacement.The lateral view demonstrates thepattern of fibular fracture and any anterior orposterior translation of the talus.CT scanning is rarely required for malleolar<strong>fractures</strong>.Stress films or views are only useful in thefully anesthetized patient and when comparedto the normal side (Fig. <strong>4.9</strong>-12b/c).
<strong>4.9</strong>567a) a’)a’’)Fig. <strong>4.9</strong>-12: Evaluation of the x-rays.a) The normal ankle articulation with the foot in 20° of internal rotation: the joint space is of equal width throughout. The line of thesubchondral plate of the tibial plafond, projected over the gap, is continuous with that of the lateral malleolus without a step.a') Even the slightest shortening of the fibula can be recognized radiologically as a step in the alignment of the subchondral platesof the tibial plafond and the lateral malleolus. Lateral shift of the talus and consequent widening of the medial joint space are seen.a’’) Same case as a’) after lengthening osteotomy of the fibula, the joint congruency is re-established.b)c)b) AP stress x-ray of the ankle joint. Note the10° varus tilt of the talus. This denotes thatthe important calcaneofibular ligament isinjured, in addition to the anterior talofibularligament.c) Anterior subluxation of the talus seen on lateral viewwith anterior stress applied to the hindfoot. A differencebetween the injured and uninjured ankles of 3 mm ormore in the height of the joint space is pathognomonicof an injury of the anterior talofibular ligament.
568 <strong>4.9</strong> <strong>Malleolar</strong> <strong>fractures</strong>—D.M. Hahn, C.L. Colton4.1 Operative vs. nonoperativetreatmentAnkle mortise incongruity ispoorly tolerated and causesabnormal loads on cartilage.Timing of surgery is dictated bythe state of the soft tissues.The decision whether an ankle fracture requiresopen reduction and internal fixation should bebased on how best the normal anatomy can berestored and stability maintained. Ankle mortiseincongruity is poorly tolerated andleads to abnormal loads on the articularcartilage.Isolated infrasyndesmotic (type A) <strong>fractures</strong>of the distal fibula that do not involve the medialside may well be stable and capable of beingtreated non-operatively.Isolated non-displaced transsyndesmotic(type B) <strong>fractures</strong> of the lateral malleolus thatdo not involve the medial side can be treatednon-operatively, provided that the ankle mortiseremains congruent [8, 9]. The determination ofwhether the deltoid ligament has been disruptedrelies upon clinical findings of tenderness onthe medial side. If this is associated with evidenceof a displaced mortise, then treatmentshould be operative stabilization of the fibula.All displaced ankle injuries are likely to beunstable and accurate anatomical reductioncan usually only be secured by open reductionand stable internal fixation.4.2 Preoperative planningThe discipline of preoperative planning for anyfracture involves consideration of the timing ofsurgery, the choice of incision, and the selectionof implants. It may involve graphic planningwith the use of implant templates from a preoperativeplanning kit. The standard implantsrequired for the vast majority of malleolar <strong>fractures</strong>are in the small fragment set. A tensionband wiring set should also be available.Tracing out of fracture fragments and theirreduction, using the techniques illustrated inthe planning chapter, is often extremely usefulwhen dealing with malleolar <strong>fractures</strong>. Thelength of the fibular plate and placement of lagscrews can be planned preoperatively and theiravailability ensured before starting the operation.4.3 Timing of surgeryThe ideal time for surgery to the ankle is beforeany true swelling or fracture blisters have developed.The initial swelling is due to hematomaformation and not to edema. The techniques ofopen reduction and internal fixation often releasethis hematoma and allow primary closurewithout tension of the surgical wound. However,it is accepted that in many situations it isnot always possible to operate before soft tissuesbecome compromised. Timing of surgery isthen dictated by the state of the soft tissues.In the presence of intradermal edema (peaud’orange), marked subcutaneous edema, orfracture blisters it is strongly advisable thatsurgery be delayed until the soft-tissue conditionhas improved. In this event, the fractureis reduced by gentle manipulation and immobilizedin a well-padded plaster splint with the legthen elevated. Surgery is postponed until thesoft-tissue injury has resolved. This is evidencedby resolution of fracture blisters, epithelializationof abrasions, and the presence of thewrinkle sign at the operative site (skin wrinklesnormally if ankle is inverted or everted).
<strong>4.9</strong>5695 Surgical techniques5.1 Patient positionThe patient is positioned supine with a sandbagunderneath the buttock of the affected side.This allows the foot to lie in neutral position andprevents the normal external rotation of the legin the anesthetized patient. The lower leg canthen be placed on a foam block with the kneeflexed to 30°. This allows ease of simultaneousaccess to both the medial and lateral sides. Theuse of a tourniquet is advised, unless otherwisecontra-indicated.For ease of access to the posteromedial aspectof the distal tibia it is sometimes helpful to placea sandbag beneath the opposite buttock andto rest the injured ankle on the oppositeshin (with appropriate padding) in the figure-4position.Occasionally the prone position on bolsterswill allow access by the posterior approach tothe posterior malleolus, particularly if it is alarge fragment or comminuted and requiringbuttressing. The approach to the medial malleolusis more difficult in this position but can bedone safely.5.2 Posterior approachThe incision is between the Achilles tendon andthe peroneal tendons. The sural nerve must beavoided. Dissection is continued through theposterior fat pad and on to the posterior aspectof the tibia. Flexor hallucis longus is medial andprotects the posterior tibial artery and nerve. Thefracture is easily identified and reduced. Byinternally rotating the leg and using a posteriomedialincision, the medial malleolus is exposed.5.3 Choice of incision(Fig. <strong>4.9</strong>-13)5.3.1 Lateral sideThe skin incision on the lateral side is placed sothat the minimum of soft-tissue dissection needsto be carried out to obtain reduction and fixation.If a lateral plate is required for the fibula,then the incision may be placed slightly anteriorlyso that on skin closure the plate does notlie immediately beneath the surgical incision.Care should be taken not to damage the superficialfibular nerve that runs anteriorly to thefibula (Fig. <strong>4.9</strong>-13a). A more posterior incisioncan be used either if a posterior plate is to beplaced on the fibula or if access is required tothe posterolateral corner of the tibia. Such anincision must avoid damage to the sural nerve.5.3.2 Medial sideThe standard medial incision runs either posterioror anterior to the malleolus. The saphenousvein and nerve should be protected (Fig. <strong>4.9</strong>-13b).6 Steps in open reductionand internal fixationIn most instances the first step in fixation isreconstruction of the fibula. Soft-tissue dissectionshould be kept to a minimum, but in simple<strong>fractures</strong> minimal exposure of the fracture linesis necessary to allow anatomical reduction andprovisional stabilization with pointed reductionforceps or K-wires. Occasionally the medial sidemust be exposed prior to definitive stabilizationbecause the deltoid ligament or an osteochon-
570 <strong>4.9</strong> <strong>Malleolar</strong> <strong>fractures</strong>—D.M. Hahn, C.L. Coltondral fragment may be interposed, preventingfull reduction. Inability to reduce the fibula isa clue to the need to open the medial side.If fixation has been delayed for reasons ofsoft-tissue recovery, the fracture planes must bemeticulously cleared of organized blood clotprior to reduction.6.1 Infrasyndesmotic fibular<strong>fractures</strong>: type 44-A1.3malleolar <strong>fractures</strong>Where the whole lateral malleolus is avulsedwith a transverse fracture line, it is reduced anda)b)Fig. <strong>4.9</strong>-13: Incisions:a) Medial side: The incision runs slightlyposterior to the medial malleolus in line withthe tibia, curving anteriorly distally to form a“J” incision. Care is to be taken to avoid thesaphenous vein and saphenous nerve.b) Lateral side: Incision is placedslightly posterior to the fibula, takingcare not to damage either thesuperficial fibular nerve or the suralnerve. An anteromedial incision maybe used, especially in type A injuries.
<strong>4.9</strong>571may be stabilized by a one-third tubular platefunctioning as a tension band (Fig. <strong>4.9</strong>-14a). Atension band wiring technique or a retrogradescrew, inserted up the fibular medullary canal,may also be used when the lateral failure is ofthe osseoligamentous type. With avulsion ofonly the tip of the lateral malleolus, tensionband wiring is used (Video AO00068a), supplementedby ligamentous suture where appropriate(Fig. <strong>4.9</strong>-14b).If the lateral injury is a rupture of the lateralligament complex, this should be sutured onlyif the ankle is unstable and a reduction cannotbe maintained (Fig. <strong>4.9</strong>-14c).The next step is to expose the medialmalleolus from anteromedially and clearVideo AO00068aa) b)c) d)44-A2Fig. <strong>4.9</strong>-14: Type A fracture—typical internal fixation:a) Where the bone is of good quality, a large lateralmalleolar fragment may be fixed with a well-contouredone-third tubular plate under slight compression,functioning as a tension band.b) An avulsion fragment of the lateral malleolus is firststabilized with two K-wires and then fixed undercompression by means of a tension band wire loop.c) A rupture of the lateral collateral ligament complexmay be sutured.d) Posteromedial fragments associated with type A3<strong>fractures</strong> are rare. They always lie next to the medialmalleolar fragment. Such fragments may be exposed,reduced, and fixed with small cancellous bone screwsfrom a posteromedial direction.
572 <strong>4.9</strong> <strong>Malleolar</strong> <strong>fractures</strong>—D.M. Hahn, C.L. Coltonany entrapped periosteum from between thefracture surfaces. The anterior capsule is oftentorn and this permits an excellent view of theintra-articular portion of the fracture. Smallbone fragments can be removed, but largerfragments should be preserved. The surface ofthe tibial plafond at the medial corner shouldbe inspected by hinging open the fracture planeanteriorly. Any impaction fracture is reducedand bone grafted.In an adduction fracture the main fractureline of the medial malleolus is often vertical oroblique and is on the compression side of theinjury (the tension being on the lateral side).Tension band wiring techniques are not suitablefor these compression <strong>fractures</strong>.Once reduction is complete and held provisionallywith K-wires, definitive fixation isachieved by lag screws placed perpendicular tothe main fracture plane. Application of a buttressingwasher or a short (two or three holes)one-third tubular plate at the apex of this fracturewill improve the stability of the construct.Video AO00069a6.2 Transsyndesmotic fibular<strong>fractures</strong>: type 44-B1.3malleolar <strong>fractures</strong>The fibular fracture is usually oblique, runningfrom distal anterior to proximal posterior. Thelateral malleolus is usually shifted proximally,displaced posteriorly, and externally rotated.Inspection of the dome of the talus may bepossible through the fracture itself and any loosechondral flakes can be removed manually or byirrigation. Dissection of the distal lateral malleolusis kept to a minimum. Reduction of thesimple, short oblique fracture of the lateral malleolusis best achieved with gentle traction andinternal rotation of the foot. Pointed reductionforceps can then be applied across the fracturefor temporary stabilization.If reduction is difficult, it may occasionallybe because the tip of the proximal fibular fragmentcan fracture and swing, on a pedicle offibers of the anterior tibiofibular ligament, intothe fracture gap. This is not always obviousand must be sought and extracted before thereduction is completed.The accuracy of reduction can be assessed byinspecting the anterior edge of the fibula at thelevel of the anterior syndesmosis. To achievedefinitive fixation, 3.5 mm cortex lag screws areplaced from anterior to posterior. A one-thirdtubular plate contoured to the lateral aspect ofthe fibula acts as a neutralization plate (VideoAO00069a). Care must be taken when placingthe screws in the distal lateral malleolus to ensurethat the articular surface is not penetrated. Themetaphyseal bone of the lateral malleolus isoften quite soft and better purchase of the screwscan be achieved either by inserting cortex screwswithout tapping or by the use of untapped fullythreaded cancellous bone screws (Fig. <strong>4.9</strong>-15a).
<strong>4.9</strong>5736.3 Posterior “anti-glide”plate(Fig. <strong>4.9</strong>-15b)The main deformity of the lateral malleoluswith a type B fracture is of external rotation,posterior displacement, and proximal shift.Reduction of this fragment is often maintainedby pushing the distal fragment from posteriorly,while at the same time reducing the externalrotation deformity. If the fracture of the lateralmalleolus is not simple and does not lend itselfto stabilization with lag screws, a one-thirdtubular plate can be placed posteriorly on thefibula as a buttress, resisting the posterior displacement[10]. Occasionally, a lag screw canbe incorporated through the plate. If this techniqueis to be used, the incision should beplaced more posteriorly to allow access to theposterior edge of the fibula. Usually a 5-hole or6-hole one-third tubular plate is applied to theposterior aspect of the fibular so that it coversthe proximal apex of the fracture. The plate isstraight and either clamped to the fibula proximallyor attached with a screw through themost proximal hole. The screw just proximal tothe fracture is now inserted and this forces thestraight plate to push the distal fragment alongthe oblique fracture surface, effecting a reductionand stability. A reduction forceps on thetip of the fibula is helpful in controlling rotationduring plate application. The remaining screwsare then inserted and a lag screw can be insertedthrough the plate (Video AO00069b).6.4 Medial sideInjuries of the deltoid ligament do not requireroutine exploration. However, if after reductionof the fibular fracture the intraoperative filmsor x-rays show that the medial joint spaceremains widened, or if there are difficulties withaccurate reduction of the fibular fracture, themedial side should be explored. On occasions,the medial ligament or an osteochondral fragmentwill have tucked into the medial jointspace and must be lifted out. The deltoid ligamentcan then be repaired, largely in order toprevent its reinterposition postoperatively duringjoint mobilization (Fig. <strong>4.9</strong>-15g).Very rarely, a block to reduction can arisefrom the entrapment of the tibialis posteriortendon within the ankle joint after a severelydisplaced fracture-dislocation.Injuries of the medial malleolus in type B<strong>fractures</strong> are usually avulsion <strong>fractures</strong> causedwhen the talus displaces posteriorly out of themortise. They may extend posteromedially andare of variable size. Exposure of the fracture isVideo AO00069b
574 <strong>4.9</strong> <strong>Malleolar</strong> <strong>fractures</strong>—D.M. Hahn, C.L. Coltona) b) c) d)43-B1ventralviewe) e’)43-B3medial viewFig. <strong>4.9</strong>-15: Type B fracture. Typical internal fixation:a) The short oblique fracture of the fibula is fixed with a 3.5 mmcortex lag screw. This fixation is supplemented with a one-thirdtubular plate functioning as a neutralization plate.b) Posterior placement of one-third tubular “anti-glide” plate.c/d) The different types of internal fixation of the medialmalleolus, with a lag screw or a tension band.e) A large posterolateral Volkmann’s fragment of the tibia iscarefully reduced and then fixed with a 4.0 mm cancellous bonelag screw inserted in an AP direction.e’) If the size of the Volkmann’s fragment cannot accommodatethe thread of the cancellous bone screw, a 3.5 mm cortex screwcan be used as a lag screw.f) Alternative fixation with a lag screw inserted from posteriorly.g) If exposure of the deltoid ligament becomes necessarybecause of soft-tissue interposition, it should be sutured.dorsal viewf) g)
<strong>4.9</strong>575achieved by a standard medial incision and anyinterposed periosteum is removed from thefracture gap to allow accurate reduction. Asmall pointed reduction forceps to grasp themedial malleolus and hold it reduced is helpful.Temporary stabilization with K-wires is followedby definitive stabilization, achieved with a 4.00 mmpartially threaded cancellous bone lag screw(Fig. <strong>4.9</strong>-15c). If the fragment is large enough, twoparallel screws can be used (Video AO00068b).With smaller fragments, one screw can be combinedwith a K-wire (Video AO00070a). Thescrews should only be long enough to allow thethread to pass fully beyond the fracture plane.Screws of excessive length in the distal tibia gainpoor purchase in the often sparse cancellousbone of the metaphysis, especially in the olderpatient or if fixation is delayed.An alternative technique is to use two parallelK-wires and a tension band wire (Fig. <strong>4.9</strong>-15d).6.5 Posterolateralfragments or posteriormalleolar <strong>fractures</strong>Video AO00068bThe posterolateral corner (Volkmann’s) fragmentin type B or rarely C <strong>fractures</strong> is oftendisplaced along with the lateral malleolus,being bound to it by the posterior syndesmoticligament. Accurate reduction of the fibularfracture will have reduced some of the upwarddisplacement of the posterior fragment, but thefracture gap may still remain open. Fragmentsof less than 25% of the articular surface on thelateral view need not be stabilized unless thereis a tendency for the talus to sublux posteriorly.Larger fragments can be fixed either by theplacement of a lag screw through a stab incisionfrom anterior to posterior (Fig. <strong>4.9</strong>-15e)(Video AO00070b) or by direct exposure of theposterior fragment through the posterolateralincision and insertion of a lag screw fromposterior to anterior (Fig. <strong>4.9</strong>-15f). The lattertechnique requires more dissection but oftengives a more accurate placement of the screw.When using the percutaneous anterior toposterior technique, it should be rememberedVideo AO00070a
576 <strong>4.9</strong> <strong>Malleolar</strong> <strong>fractures</strong>—D.M. Hahn, C.L. ColtonVideo AO00070bVideo AO00070cthat the fragment in a type B fracture will lieat the posterolateral corner of the tibia andtherefore the screw must be directed appropriately(Fig. <strong>4.9</strong>-15e).6.6 Suprasyndesmotic fibularfracture: type 44-C1.3malleolar <strong>fractures</strong>(Fig. <strong>4.9</strong>-16)As in the case of the type A and B <strong>fractures</strong>, thefirst step in dealing with type C <strong>fractures</strong> isto approach the fibula. The key to successfulfixation is to restore the length and rotation ofthe fibula. If the fibular fracture is short oblique,or spiral, then the fracture can be exposed,accurately reduced with the use of reductionforceps, and fixed using lag screws and a onethirdtubular plate (Video AO00070c). If thefibular fracture, however, is multifragmentary,then techniques of indirect reduction should beused. There, the best technique is to use theplate as a reduction tool. The lateral malleolusand fibular shaft distal to the fracture, and theproximal fibula above the fracture zone, areexposed, but no dissection is carried out aroundthe area of comminution. A one-third tubularplate is then contoured, remembering that onreduction the fibula will effectively be lengthenedand therefore a long enough plate mustbe chosen. It is advisable to plan this graphicallybefore operation. The plate is anchored to thedistal fibula, spanning the comminuted area. Ascrew is then placed in the fibular shaft proximalto the upper end of the plate and the proximalend of the plate is secured lightly to thefibula with a plate-holding clamp. Using alaminar spreader against the screw, the plate ispushed distally, thereby lengthening the fibula.X-rays are taken to check the accuracy of thereduction determined by the correspondence ofthe subchondral plateau of the tibial plafondand the lateral malleolus. A preoperative planof the uninjured ankle serves as an intraoperativereference.
<strong>4.9</strong>577The plate can then be anchored proximally,with fibular length and orientation restored andwith the multiple intermediate fragments indirectlyreduced.Proximal <strong>fractures</strong>, occurring through thefibular neck, need not as a rule be exposed, butthe fibula must be reduced down into its normalposition in the incisura fibularis by traction,using a towel clip or pointed reduction forceps.Reduction can then be temporarily held withone or two K-wires passed through the fibulainto the tibia, later to be replaced by definitivepositioning screw fixation (see below).The medial malleolar <strong>fractures</strong> are reducedand fixed using the techniques described abovefor type B <strong>fractures</strong>.6.7 Fibulotibial “syndesmotic”positioning screwThe decision as to whether any further fixationis necessary depends on the stability ofthe syndesmosis once the fibular length hasbeen restored, the fibula fixed, and the medialside reconstructed. The anterior syndesmosiscan be exposed via the lateral incision. Ifavulsed with the anterior tibial tubercle (Tillaux-Chaput) or from the fibula, it can be reducedand fixed with a small lag screw. If the anteriorsyndesmotic ligament is torn within its substanceit may be repaired with sutures.Whether any further fibular stabilization isthen necessary can be determined by the use ofthe hooktest, in which the fibula is grasped withbone forceps, or a bone hook, and pulled gentlylaterally to reveal any significant residual fibulotibialinstability. In addition, stress views inexternal rotation must be taken intraoperatively.Widening of the medial joint space by more than2 mm suggests syndesmotic instability.If the syndesmosis is unstable, a positioningscrew should be placed from the fibula into thetibia. This screw is introduced obliquely fromposterior to anterior at an angle of 25–30° andparallel to the tibial plafond. It is placed justproximal to the fibulotibial joint. As this screwis not intended to act as a compressive lag screw,the fibula and tibia should both be fully tappedand a 3.5 mm cortex screw inserted, while thefibula is held, without compression, in its anatomicalrelationship to the tibia.During the procedure, the foot should bemaintained in slight dorsiflexion. In this positionthe wider anterior part of the talar body isengaged in the mortise to prevent narrowing,which can often lead to permanent loss of dorsiflexion,even after screw removal (see below).There is no clear agreement on whether oneor both tibial cortices should be engaged by thepositioning screw threads. Certainly, if thefibular fracture is so high that its direct fixationis not possible (as in the Maisonneuve injury),then both tibial cortices should be used. Occasionally,two positioning screws may be neededin these circumstances. A further advantage ofengaging both tibial cortices is that, should apositioning screw break in a non-compliantpatient, the thread fragment can easily beremoved via a small window in the medial tibialcortex.Intraoperative check x-rays or image intensificationto confirm the position of the screware advised.Stability of the syndesmosisdetermines whether apositioning screw is used.
578 <strong>4.9</strong> <strong>Malleolar</strong> <strong>fractures</strong>—D.M. Hahn, C.L. Coltona) b)43-C1.3Fig. <strong>4.9</strong>-16: Typical internalfixation for type C fracture.a) The fibular shaft fracture isreduced and stabilized with aone-third tubular plate. Thesmall avulsion fracture of themedial malleolus is fixed withtwo K-wires and a tension bandwire loop. The torn anteriorsyndesmotic ligament is thentested with a small hook.b’)43-C2b/b') A fracture of the midshaft of the fibula isfixed with a plate. The anterior syndesmosis hasbeen avulsed from its attachment to the lateralmalleolus. This is reduced and fixed with either asmall cancellous bone screw or a transosseouswire suture. The ruptured deltoid ligament may besutured. A large posterolateral fragment is rare inthis injury, but if present is carefully reduced andthen fixed with a cancellous bone lag screw. Thisrestores stability of the ankle mortise.c)43-C3c/c’) Not infrequently, a very proximal fibular fracture is not shortened and does not needopen reduction. It is most important, however, to check very carefully for any shorteningon an AP of the ankle. Look for any step in the alignment of the subchondral plates of thetibial plafond and the lateral malleolus. Any shortening must be corrected. A smallavulsion fracture of the anterior syndesmotic ligament from the tibia is reduced and fixedwith a small cancellous bone lag screw.Since this injury involves almost the full extent of the interosseous membrane, the fixationof the anterior syndesmotic origin may not provide sufficient stability to the ankle mortiseand a positioning screw is necessary. This will be revealed by the hook test. Two screwsshould be introduced obliquely from back to front at an angle of 25–30°, the thread beingtapped into both the fibula and the tibia. The avulsion fracture of the medial malleolus isfixed under compression, using one or two 4 mm cancellous bone lag screws. Positioningscrews should be removed at 6–8 weeks.c’)
<strong>4.9</strong>5797 Postoperativemanagementd)Fig. <strong>4.9</strong>-16: Type C fracture (cont.)d) Exact anatomical reduction of the fibula into thefibular notch of the tibia (incisura fibularis) guaranteesa normal ankle mortise. Imperfect reduction withshortening or rotation of the fibula leads to wideningof the ankle mortise and valgus tilt of the talus. Evensmall degrees of malreduction are likely to lead toposttraumatic degenerative arthritis (see Fig. <strong>4.9</strong>-12).On the left the fibula is shortened and externallyrotated, resulting in syndesmotic incongruity andsecondary ankle instability. On the right afteranatomical reduction of the fibula the fibulotibialrelationship is again normal.Both medial and lateral wounds are closedusing fine sutures without tension. The use ofsuction drainage on the lateral side is recommended.The ankle is rested in a plaster of Parisback slab with the foot at 90° to prevent anequinus deformity. Where an anatomical reductionof the fibular fracture may not havebeen possible, it is wise to obtain a CT scanof the syndesmosis in the early postoperativeperiod to exclude malrotation of the fibula [11].The patient is encouraged to start early activemovement of the toes and, if the woundsare satisfactory at 24–48 hours, then activemobilization of the ankle can be started underskilled supervision. The decision as to whether,once active dorsiflexion has been achieved, thepatient can be left free, or protected in a cast,depends on a number of factors. These includethe stability of fixation achieved by the surgeon,the general mobility of the patient, andthe prospect of compliance with the chosenpostoperative regime. Studies [12, 13] haveshown that the long-term outcome is similar,whether the ankle is immobilized or free during6 postoperative weeks. A decision regardingweight bearing, either in or out of a cast, alsolargely depends on the stability of fixationachieved and the cooperation of the patient. Noproblems have been experienced by the authorsusing a regime of progressive, light weightbearing in a cast for 6 weeks, although thereturn to full activity is more rapid in the earlymobilization-group. At the end of this period,active mobilization and full weight bearing canbe allowed.If a syndesmotic screw has been used and thepatient left free, then it is recommended thatweight bearing be protected for the first 6–8 weeks.
580 <strong>4.9</strong> <strong>Malleolar</strong> <strong>fractures</strong>—D.M. Hahn, C.L. ColtonLight weight bearing in a protective cast ispermissible.Controversy exists over syndesmotic screwremoval. The syndesmotic screw may beremoved at 6–8 weeks, before return to fullnormal activity. In cases where both the medialand syndesmotic failures have been exclusivelyligamentous, it is advisable to retain thepositioning screw and restrict full activity for10–12 weeks.If the positioning screw is not removed, itwill either erode a wider track through thefibula as normal fibulotibial motion occurs, orit will break. These possibilities are explained tothe patients so that they are well aware of thepostoperative course.8 Pitfalls andcomplications8.1 Soft-tissue problemsAnkle <strong>fractures</strong> can swell dramatically withinhours of injury. If surgery can be performedwithin 6–8 hours, the swelling is almost alwayshematoma and not edema within the tissues.Primary closure of the surgical wounds canusually be achieved in these instances. If, however,this can only be achieved with tension, thewound should be left open, absorbent steriledressings applied, and the foot elevated. Carefulpreoperative planning of the placement of theincisions should take this possibility into accountand avoid leaving the implants exposed. At 48hours the wounds can be reinspected and veryoften can be closed at that time.If edema and blisters have developed, it ishighly recommended that surgery be delayed forup to 4–6 days until the soft tissues are recovering.8.2 Open <strong>fractures</strong>The soft-tissue wounds in open <strong>fractures</strong> of theankle should be dealt with according to thesurgical principles outlined for all open <strong>fractures</strong>[14] (chapter 5.1). The most common wound inopen ankle fracture-dislocations is a medialtransverse laceration. Anatomical reduction andstable fixation of the ankle mortise should stillbe achieved in most cases once débridement ofall open wounds has taken place. Soft-tissuewounds should then be left open, although thesurgical extensions of the débridement may beclosed primarily, provided all tension is avoided.A well-padded, non-adherent, and absorbentdressing is applied, followed by limb elevationand then a “second look” at 48–72 hours. Definitivewound closure decisions will take accountof the principles referred to above.8.3 Osteoporotic boneWhere the bone is osteoporotic, techniquesalready described for the lateral side include theuse of the anti-glide plate and indirect reductiontechniques for restoration of the fibular length.The use of closed reduction and intramedullaryfibular fixation in fracture patterns that areaxially stable may be another alternative forosteoporotic bone, in particular if there arecompromised soft-tissue conditions. On themedial side the medial fragment cannot withstandthe use of a cancellous bone lag screw andtherefore K-wire stabilization and tension bandwiring may be more useful in the B and Cinjuries.
<strong>4.9</strong>5819 Bibliography1. Calhoun JH, Li F, Ledbetter BR, et al.(1994) A comprehensive study ofpressure distribution in the ankle jointwith inversion and eversion. Foot AnkleInt; 15 (3):125–133.2. Lundberg A, Goldie I, Kalin B, et al.(1989) Kinematics of the ankle/footcomplex: plantarflexion and dorsiflexion.Foot Ankle; 9 (4):194–200.3. Michelson JD (1995) Fractures aboutthe ankle. J Bone Joint Surg [Am];77 (1):142–152.4. Ramsey PL, Hamilton W (1976)Changes in tibiotalar area of contactcaused by lateral talar shift. J Bone JointSurg [Am]; 58 (3):356–357.5. Riede UN, Schenk RK, Willenegger H(1971) [Joint mechanical studies on posttraumaticarthrosas in the ankle joint. I.The intra-articular model fracture].Langenbecks Arch Chir; 328 (3):258–271.6. Müller ME, Nazarian S, Koch P, et al.(1990) The Comprehensive Classification ofFractures of Long Bones. Berlin HeidelbergNew York: Springer-Verlag.7. AO Müller Electronic Long Bone FractureClassification. (2000) AO Publishing/Thieme. (in preparation).8. Bauer M, Bergstrom B, Hemborg A,et al. (1985) <strong>Malleolar</strong> <strong>fractures</strong>:nonoperative versus operative treatment.A controlled study. Clin Orthop; (199):17–27.9. Kristensen KD, Hansen T (1985)Closed treatment of ankle <strong>fractures</strong>. StageII supination-eversion <strong>fractures</strong> followedfor 20 years. Acta Orthop Scand;56 (2):107–109.10. Brunner CF, Weber BG (1982) SpecialTechniques in Internal Fixation. BerlinHeidelberg New York: Springer-Verlag.11. Wanders L, Oliver CW (1998) Fibularmalreduction in AO/Weber type C ankle<strong>fractures</strong>. Injury; 29 (2):144–146.12. Stuart PR, Brumby C, Smith SR(1989) Comparative study of functionalbracing and plaster cast treatment ofstable lateral malleolar <strong>fractures</strong>. Injury;20 (6):323–326.13. Hedstrom M, Ahl T, Dalen N (1994)Early postoperative ankle exercise. Astudy of postoperative lateral malleolar<strong>fractures</strong>. Clin Orthop; (300):193–196.14. Wiss DA, Gilbert P, Merritt PO, et al.(1988) Immediate internal fixation ofopen ankle <strong>fractures</strong>. J Orthop Trauma;2 (4):265–271.10 UpdatesUpdates and additional references for this chapterare available online at:http://www.aopublishing.org/PFxM/49.htm