inTervieW - Green Cross Publishing
inTervieW - Green Cross Publishing
inTervieW - Green Cross Publishing
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
32<br />
case sTudy<br />
Cluster headache in a 24<br />
year old woman<br />
a<br />
24-year-old female patient<br />
presented with a four year history<br />
of daily headaches. She reported<br />
8-10 attacks per day and the<br />
duration of attacks lasted from 30-<br />
90 minutes. Most of these attacks<br />
would occur spontaneously but she always got<br />
an attack awakening her from sleep at around<br />
2am. When she awoke with this attack it would<br />
make her restless and agitated, forcing her to<br />
pace the bedroom floor until it subsided after<br />
approximately 30 minutes. The typical clinical<br />
characteristics of her headaches and associated<br />
symptoms were:<br />
• Abrupt in onset and occurred without warning<br />
• Always unilateral in location in the left<br />
periorbital/frontal region and extending to<br />
the temple<br />
• Duration 30-90 minutes<br />
• Sharp, piercing and burning in character<br />
• Very severe<br />
• Forehead sweating<br />
• Associated with restlessness, agitation and a<br />
feeling like ‘banging’ her head off a wall<br />
• Ipsilateral conjunctival tearing<br />
• Ipsilateral conjunctival reddening<br />
• Ipsilateral nasal congestion.<br />
• Ipsilateral nasal rhinorrhoea.<br />
• Ipsilateral ptosis of left upper eye lid.<br />
• Ipsilateral miosis of left pupil.<br />
Other symptoms associated with some<br />
attacks included intermittant photophobia,<br />
Prevalence Common: 10-12 per cent<br />
population<br />
phonophobia, nausea and occasional vomiting.<br />
The rest of the physical and neurological<br />
examination was normal.<br />
These headaches were having a major impact<br />
on her life. She was unable to get any relief from<br />
the attacks and as an acute therapy she was<br />
consuming up to 10 paracetamol daily without<br />
benefit. She was also on amitriptylline 25mg<br />
nocte as a preventive therapy, with no resultant<br />
change in the frequency of attacks. Over the<br />
years she had tried many other analgesics and<br />
preventive therapies without benefit. In addition<br />
she had been prescribed courses of antibiotics<br />
for a presumptive diagnosis of chronic sinusitis.<br />
Her life was being controlled by the headaches<br />
and she was unable to pursue a career or get a<br />
job. She previously had been working as a clerical<br />
officer but was forced to give up her job. Her<br />
social life had become non-existent. During this<br />
four-year period she had attended emergency<br />
departments and GP out-of-hours services on<br />
many occasions, all of whom either diagnosed<br />
‘severe migraine’ or ‘sinusitis’ and for immediate<br />
pain relief she was treated acutely with either<br />
parenteral courses of nSAIDs or narcotic agents,<br />
all of which were ineffective.<br />
Investigations carried out over the four-year<br />
period included a CTScan brain, CTScan sinuses,<br />
MRI scan brain and many blood tests, all of which<br />
were entirely normal.<br />
This patient has a diagnosis of chronic cluster<br />
headaches, a benign primary headache disorder.<br />
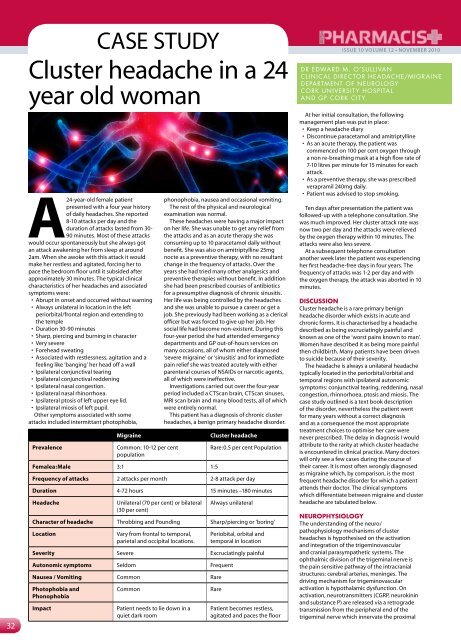
Migraine Cluster headache<br />
Femalea:Male 3:1 1:5<br />
Rare:0.5 per cent Population<br />
Frequency of attacks 2 attacks per month 2-8 attack per day<br />
Duration 4-72 hours 15 minutes –180 minutes<br />
Headache Unilateral (70 per cent) or bilateral<br />
(30 per cent)<br />
Always unilateral<br />
Character of headache Throbbing and Pounding Sharp/piercing or ‘boring’<br />
Location Vary from frontal to temporal,<br />
parietal and occipital locations.<br />
Periobital, orbital and<br />
temporal in location<br />
severity Severe Excruciatingly painful<br />
autonomic symptoms Seldom Frequent<br />
nausea / vomiting Common Rare<br />
Photophobia and<br />
Phonophobia<br />
Common Rare<br />
impact Patient needs to lie down in a<br />
quiet dark room<br />
Patient becomes restless,<br />
agitated and paces the floor<br />
issue 10 volume 12 • novemBeR 2010<br />
dr edwArd M. o’sullIvAN<br />
ClINICAl dIreCtor HeAdACHe/MIGr AINe<br />
dePArtMeNt of NeuroloGy<br />
Cork uNIversIt y HosPItAl<br />
ANd GP Cork CIt y.<br />
At her initial consultation, the following<br />
management plan was put in place:<br />
• Keep a headache diary<br />
• Discontinue paracetamol and amitriptylline<br />
• As an acute therapy, the patient was<br />
commenced on 100 per cent oxygen through<br />
a non re-breathing mask at a high flow rate of<br />
7-10 litres per minute for 15 minutes for each<br />
attack.<br />
• As a preventive therapy, she was prescribed<br />
verapramil 240mg daily.<br />
• Patient was advised to stop smoking.<br />
Ten days after presentation the patient was<br />
followed-up with a telephone consultation. She<br />
was much improved. Her cluster attack rate was<br />
now two per day and the attacks were relieved<br />
by the oxygen therapy within 10 minutes. The<br />
attacks were also less severe.<br />
At a subsequent telephone consultation<br />
another week later the patient was experiencing<br />
her first headache-free days in four years. The<br />
frequency of attacks was 1-2 per day and with<br />
the oxygen therapy, the attack was aborted in 10<br />
minutes.<br />
discussion<br />
Cluster headache is a rare primary benign<br />
headache disorder which exists in acute and<br />
chronic forms. It is characterised by a headache<br />
described as being excruciatingly painful and<br />
known as one of the ‘worst pains known to man’.<br />
Women have described it as being more painful<br />
then childbirth. Many patients have been driven<br />
to suicide because of their severity.<br />
The headache is always a unilateral headache<br />
typically located in the periorbital/orbital and<br />
temporal regions with ipsilateral autonomic<br />
symptoms: conjunctival tearing, reddening, nasal<br />
congestion, rhinnorhoea, ptosis and miosis. The<br />
case study outlined is a text book description<br />
of the disorder, nevertheless the patient went<br />
for many years without a correct diagnosis<br />
and as a consequence the most appropriate<br />
treatment choices to optimise her care were<br />
never prescribed. The delay in diagnosis I would<br />
attribute to the rarity at which cluster headache<br />
is encountered in clinical practice. Many doctors<br />
will only see a few cases during the course of<br />
their career. It is most often wrongly diagnosed<br />
as migraine which, by comparison, is the most<br />
frequent headache disorder for which a patient<br />
attends their doctor. The clinical symptoms<br />
which differentiate between migraine and cluster<br />
headache are tabulated below.<br />
neurophysiology<br />
The understanding of the neuro/<br />
pathophysiology mechanisms of cluster<br />
headaches is hypothesised on the activation<br />
and integration of the trigeminovascular<br />
and cranial parasympathetic systems. The<br />
ophthalmic division of the trigeminal nerve is<br />
the pain sensitive pathway of the intracranial<br />
structures: cerebral arteries, meninges. The<br />
driving mechanism for trigeminovascular<br />
activation is hypothalamic dysfunction. On<br />
activation, neurotransmitters (CGRP, neurokinin<br />
and substance P) are released via a retrograde<br />
transmission from the peripheral end of the<br />
trigeminal nerve which innervate the proximal