open access atlas of otolaryngology, head & neck operative surgery
open access atlas of otolaryngology, head & neck operative surgery
open access atlas of otolaryngology, head & neck operative surgery
- No tags were found...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
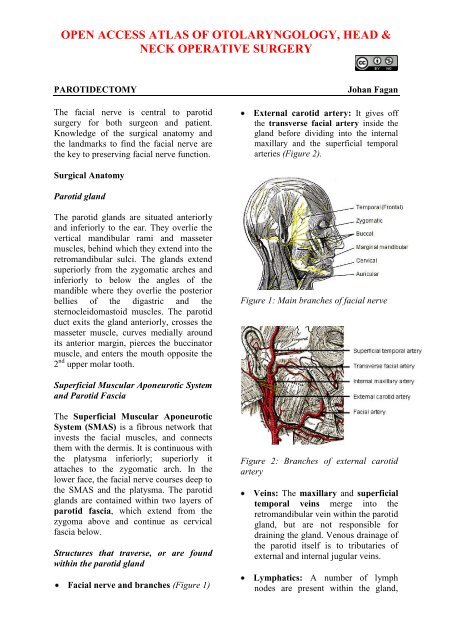
OPEN ACCESS ATLAS OF OTOLARYNGOLOGY, HEAD &NECK OPERATIVE SURGERYPAROTIDECTOMYThe facial nerve is central to parotid<strong>surgery</strong> for both surgeon and patient.Knowledge <strong>of</strong> the surgical anatomy andthe landmarks to find the facial nerve arethe key to preserving facial nerve function.Johan FaganExternal carotid artery: It gives <strong>of</strong>fthe transverse facial artery inside thegland before dividing into the internalmaxillary and the superficial temporalarteries (Figure 2).Surgical AnatomyParotid glandThe parotid glands are situated anteriorlyand inferiorly to the ear. They overlie thevertical mandibular rami and massetermuscles, behind which they extend into theretromandibular sulci. The glands extendsuperiorly from the zygomatic arches andinferiorly to below the angles <strong>of</strong> themandible where they overlie the posteriorbellies <strong>of</strong> the digastric and thesternocleidomastoid muscles. The parotidduct exits the gland anteriorly, crosses themasseter muscle, curves medially aroundits anterior margin, pierces the buccinatormuscle, and enters the mouth opposite the2 nd upper molar tooth.Figure 1: Main branches <strong>of</strong> facial nerveSuperficial Muscular Aponeurotic Systemand Parotid FasciaThe Superficial Muscular AponeuroticSystem (SMAS) is a fibrous network thatinvests the facial muscles, and connectsthem with the dermis. It is continuous withthe platysma inferiorly; superiorly itattaches to the zygomatic arch. In thelower face, the facial nerve courses deep tothe SMAS and the platysma. The parotidglands are contained within two layers <strong>of</strong>parotid fascia, which extend from thezygoma above and continue as cervicalfascia below.Structures that traverse, or are foundwithin the parotid glandFacial nerve and branches (Figure 1)Figure 2: Branches <strong>of</strong> external carotidarteryVeins: The maxillary and superficialtemporal veins merge into theretromandibular vein within the parotidgland, but are not responsible fordraining the gland. Venous drainage <strong>of</strong>the parotid itself is to tributaries <strong>of</strong>external and internal jugular veins.Lymphatics: A number <strong>of</strong> lymphnodes are present within the gland,
principally in the superficial lobe, anddrain to Level 2 <strong>of</strong> the <strong>neck</strong>.Relevant surgical relationsPosterior: Cartilage <strong>of</strong> external auditorymeatus; tympanic bone, mastoid process,sternocleidomastoid muscleDeep: Styloid process, stylomandibulartunnel, parapharyngeal space, posteriorbelly <strong>of</strong> digastric, sternocleidomastoidmuscleSuperior: Zygomatic arch, temporomandibularjointFacial nerveThe facial nerve exits the stylomastoidforamen, and enters the parotid gland.Although the branching pattern does varyfrom patient to patient, the trunk generallydivides at the pes anserinus into upper andlower divisions that subsequently branchinto temporal (frontal), zygomatic, buccal,marginal mandibular and cervical branchesthat innervate the muscles <strong>of</strong> facialexpression. Small branches to the posteriorbelly <strong>of</strong> digastric, stylohyoid, and auricularmuscles also arise from the trunk (Figure3).The nerve traverses the parotid gland, withabout 2/3 <strong>of</strong> the gland substance beingsuperficial to the nerve. As parotiddissection generally is directed along thefacial nerve, the nerve in effect divides theparotid from a surgical perspective intosuperficial and deep lobes, although thereis no natural s<strong>of</strong>t tissue dissection planethat separates the two lobes.The midfacial nerve branches havemultiple cross-innervations; however thefrontal and marginal mandibular branchesdo not have cross-innervations and injuryto these branches is followed by paralysis<strong>of</strong> the fore<strong>head</strong> and depressors <strong>of</strong> the lowerlip (Figure 4). Therefore unlike thetemporal and marginal mandibular nerves,selected midfacial branches may besacrificed without loss <strong>of</strong> facial function.Figure 4: Midfacial branches (yellow)interconnect whereas temporal andmarginal mandibular (black) do notLocating the Facial NerveFigure 3: The facial nerve trunk dividinginto superior and inferior division at thepes anserinusIt is useful to know pre<strong>operative</strong>ly whethera parotid tumour is situated deep orsuperficial to the facial nerve. Thisfacilitates surgical planning and facilitatespre<strong>operative</strong> consent relating to thelikelihood <strong>of</strong> a temporary post<strong>operative</strong>facial nerve weakness.2
Surface markingsFacial nerve trunk: The trunk exits theskull at the stylomastoid foramen. This issituated at the deep end <strong>of</strong> thetympanomastoid suture line, which can belocated at the junction between the mastoidprocess and the tympanic ring <strong>of</strong> theexternal ear canalTemporal (frontal) branch <strong>of</strong> facialnerve: The nerve crosses the zygomaticarch; it runs within the SMAS and liessuperficial to the deep temporalis fascia. Itcourses more or less along a line drawnbetween the attachment <strong>of</strong> the lobule <strong>of</strong> theear to a point 1.5 cm above the lateralaspect <strong>of</strong> the eyebrow. To avoid injury tothe temporal branch dissect either in asubcutaneous plane or deep to the SMAS(Figure 1).Figure 5: Facial nerve running superficialto retromandibular veinRadiologyRadiological investigation is not routinelyrequired with parotid tumours. It isrecommended for surgical planning withtumours that are large, fixed, and areassociated with facial nerve involvement,trismus, and parapharyngeal spaceinvolvement. MRI is a valuableinvestigation with recurrence <strong>of</strong>pleomorphic adenoma as it is <strong>of</strong>tenmultifocal.The extratemporal facial nerve is notvisible with ultrasound, CT or MRI. Theretromandibular vein is however intimatelyassociated with the facial nerve. The veincourses through the parotid glandimmediately deep to the facial nerve, butrarely runs immediately superficial to thenerve (Figures 5 & 6). Reliance istherefore placed on the juxtaposition <strong>of</strong> theretromandibular vein and the nerve topredict whether a tumour is likely to bedeep or superficial to the nerve.Figure 6: Facial nerve running deep, butclose, to retromandibular veinFigure 7: Red arrows indicateretromandibular veins, and yellow arrowthe course <strong>of</strong> the facial nerve in asuperficial lobe pleomorphic adenomaThe retromandibular vein can be clearlyvisualized on a CT with contrast, or anMRI (Figures 7, 8).3
Figure 8: Red arrows indicate retromandibularveins, and yellow arrow thecourse <strong>of</strong> the facial nerve in a deep lobepleomorphic adenomaanserinus and the divisions and nervebranches. Occasionally this is not possiblee.g. with a large fixed mass centered at thestylomastoid foramen. In such cases aretrograde dissection may be required afterlocating the temporal branch where itcrosses the zygoma, the buccal brancheswhich lie parallel to the parotid duct(Figure 10), or the marginal mandibularbranch where is crosses the facial arteryand vein just below or at the inferiormargin <strong>of</strong> the mandible, where it is justdeep to platysma (Figure 11).Radiology may also alert the surgeon toextension <strong>of</strong> a deep lobe parotid tumourthrough the stylomandibular tunnel into theparapharyngeal space (Figure 9).Figure 10: Buccal branches adjacent tothe parotid ductMarginal mandibularnerveFacial artery and veinFigure 9: Tumour passing through stylomandibulartunnel to parapharyngealspace (Arrow indicates styloid process)Intra<strong>operative</strong> location <strong>of</strong> facial nerveThe facial nerve is usually explored byprograde dissection i.e. by locating thenerve trunk where it exits from thestylomastoid foramen, and then dissectinganteriorly along the trunk, the pesFigure 11: Marginal mandibular nervecrossing facial artery and veinThe surgical landmarks for finding thefacial nerve trunk at the stylomastoidforamen are remarkably constant, and allthe landmarks should be identified at everySubmandibular salivarygland4
operation to facilitate finding the nerve(Figures 12, 13).Figure 12: Schematic surgical landmarksfor the facial nerve trunkFigure 13: Intra<strong>operative</strong> surgicallandmarks for the facial nerve trunkPosterior belly <strong>of</strong> digastric muscle: Thenerve runs at the same depth below theskin surface, and bisects the angle betweenthe muscle and the styloid processCartilage pointer: This refers to themedial-most, pointed end <strong>of</strong> the cartilage<strong>of</strong> the external auditory meatus. The nerveexits the foramen approximately 1cm deepand 1cm inferior to this pointTympanic ring, mastoid process andtympanomastoid suture line: Thetympanomastoid suture line is the mostprecise landmark for the facial nerve as itleads medially, directly to the stylomastoidforamenStyloid process: The facial nerve crossesthe styloid process. Palpating the styloidprocess is therefore a useful means todetermine the depth and position <strong>of</strong> thefacial nerveBranch <strong>of</strong> occipital artery: A smallbranch <strong>of</strong> the occipital artery is commonlyencountered just lateral to the facial nerveclose to the stylomastoid foramen. Briskarterial bleeding should therefore alert thesurgeon to the proximity <strong>of</strong> the facialnerve; it is easily controlled with bipolarcautery.Electrical stimulation and monitoringThese need not be routinely employed, butmay be useful adjuncts to a soundknowledge <strong>of</strong> facial nerve anatomy inselected cases such as revision <strong>surgery</strong> andwith large tumours. It may however notrecord facial stimulation with faultyequipment, and nerve fatigue followingexcessive mechanical or electricalstimulation, and use <strong>of</strong> a muscle relaxant.Electrophysiological monitoring: AnEMG monitor may be used to detectcontraction <strong>of</strong> the facial muscles when thefacial nerve is mechanically orelectrically stimulated.Facial nerve electrical stimulation:Battery operated or more sophisticatednerve stimulators may be employedintra<strong>operative</strong>ly to assist with finding thenerve, or to differentiate between nerveand blood vessels. Stimulating the nerveproduces visible contraction <strong>of</strong> the facialmusculature or an EMG signal.Types <strong>of</strong> ParotidectomyPartial parotidectomy: Resection <strong>of</strong>parotid pathology with a margin <strong>of</strong> normalparotid tissue. This is the standard5
operation for benign pathology andfavourable malignanciesSuperficial parotidectomy: Resection <strong>of</strong>the entire superficial lobe <strong>of</strong> parotid(Figure 3) and is generally used formetastases to parotid lymph nodes e.g.from skin cancers, and for high grademalignant parotid tumours.Total parotidectomy: This involvesresection <strong>of</strong> the entire parotid gland,usually with preservation <strong>of</strong> the facialnervePre<strong>operative</strong> consentScar: usually very good healing exceptover the mastoid where some scarring maybe occurAnaesthesia in the greater auriculardistribution: Skin <strong>of</strong> inferior part <strong>of</strong>auricle, and overlying the angle <strong>of</strong> themandibleFacial nerve weakness: Temporaryweakness common (
Divide the greater auricular nerve as itcrosses sternocleidomastoid muscle,posteriorly to the external jugular veino Tragal pointer (nerve 1 cm deep andinferior)o Tympanic ringo Anterior aspect <strong>of</strong> mastoid boneo Tympanomastoid suture line (leadsdirectly to stylomastoid foramen)o Posterior belly <strong>of</strong> digastric muscle(Facial nerve at same depth, justabove muscle)o Palpate the styloid process (facialnerve in angle between styloid anddigastric, and crosses styloid moreanteriorly)Cartilage pointerTympanic ringFigure 15: Exposure <strong>of</strong> parotid mass orglandIdentify and skeletonise the posteriorbelly <strong>of</strong> the digastric muscle. Do notdissect cephalad <strong>of</strong> the muscle as onemay injure the facial nerve (Figure 16).Digastric muscleVIInDigastricSternomastoidFigure 17: Identify facial nerve landmarksLocate the facial nerve trunk by bluntdissection with a fine haemostat(Figure 18)Tympanomastoid sutureMastoid processExternal jugular vein(ligated)Greater auricular nerveSternomastoid muscleFigure 16: Expose the sternomastoid andposterior belly <strong>of</strong> digastric muscleSkeletonise the cartilage <strong>of</strong> the externalauditory canal up to the tragal pointer.This can be done quite quickly withelectrocautery dissection as the facialnerve exits the stylomastoid foramen1cm deep to the tragal pointerSkeletonise the mastoid tip to the depth<strong>of</strong> the tragal pointerIdentify all the following landmarks forthe facial nerve (Figures 12, 13 & 17)Figure 18: Location <strong>of</strong> facial nerve trunk,and superior and inferior release <strong>of</strong>capsule and parotid tissues (yellowarrows)Use fine curved blunt tipped scissorsfor the remainder <strong>of</strong> the nerve7VIIn
dissection. Tunnel and spread thetissues overlying the facial nerve andits branches, and divide the parotidtissue overlying the nerve. It isimportant to dissect directly on thenerve so as not to lose sight <strong>of</strong> it.Never divide parotid tissue beyondexposed facial nerve. Wearing loupese.g. with 2.5x magnification assistswith the dissection, and enables one tobetter distinguish between bloodvessels and nerves. Employ bipolardiathermy and fine silk ties forhaemostasis.Dissect along the trunk to the pesanserinusDissect back towards the stylomastoidforamen to exclude early branchingfrom the trunkDivide the parotid fascia and parotidtissue superiorly and inferiorly torelease the parotid posteriorly and topermit anterior mobilisation <strong>of</strong> thegland/tumour (Figure 17)Dissect along, and strip the superficiallobe <strong>of</strong>f the branches <strong>of</strong> facial nerve.Unless a complete superficialparotidectomy is done, only thebranches close the mass are dissectedand exposed.Identify the retromandibular vein as itcrosses the medial to the facial nerve(Figures 5 & 6)If removing the superior part <strong>of</strong> thegland, identify/ligate the superficialtemporal artery superiorly, just anteriorto auricleIf dissecting to the anterior border <strong>of</strong>the gland, identify and transect theparotid ductRemove the tumour with a cuff <strong>of</strong> thesuperficial parotid lobe (Figure 3)Parotid dissection for deep lobe tumoursThe principles <strong>of</strong> resecting deep lobetumours are to:Identify, dissect and free up the facialnerve from the underlying deep lobe ortumour, to provide <strong>access</strong> to the deeplobe. This may involve either asuperficial parotidectomy, or simplyreflecting the superficial lobeanteriorly, keeping the parotid ductintact, and replacing it at theconclusion <strong>of</strong> <strong>surgery</strong> (Figure 19)Figure 19: Reflecting superficial lobe for<strong>access</strong> to facial nerve and to deep lobetumourDeliver the tumour either between, orinferior to the facial nerve or itsbranches, identifying the branches <strong>of</strong>the facial nerve branches around thetumour, and removing tumour betweensplayed facial nerve branches (Figure20)The deep lobe <strong>of</strong> the parotid/tumour isbordered medially by the fat <strong>of</strong> theparapharyngeal space, and can bedelivered from the parapharyngealspace by blunt dissectionBe prepared to divide the externalcarotid, deep transverse facial andsuperficial temporal arteries and theretromandibular and superficialtemporal veins if and when they areencountered during dissection8
Figure 20: Tumour resected by removingtumour between splayed facial nervebranchesAdditional <strong>access</strong> may be provided tothe deep aspect <strong>of</strong> a tumour by dividingthe styloid process and/or via atranscervical approach (Figure 21)Figure 21: Access to parapharyngealspace tumour extension by reflecting thesuperficial lobe and division <strong>of</strong> styloidprocessTumour spillageGreat care should be taken to avoid ruptureand spillage <strong>of</strong> pleomorphic adenomatissue into the <strong>operative</strong> site as it may leadto multifocal tumour recurrence, <strong>of</strong>tenmore than 20yrs following <strong>surgery</strong> (Figure22).Figure 22: Multifocal recurrence <strong>of</strong>pleomorphic adenomaA minor controlled capsular rupture maybe simply managed by copiously irrigatingthe wound. With more extensive ruptures,especially <strong>of</strong> pleomorphic adenoma in theparapharyngeal space, some wouldadvocate post<strong>operative</strong> radiation therapy.Due to the multifocal nature <strong>of</strong> therecurrence, MRI is an importantpre<strong>operative</strong> investigation for recurrence.Having to operate in a previously dissectedfield, the facial nerve is at greater risk <strong>of</strong>injury, and should be monitored during<strong>surgery</strong>.Wound closureConfirm nerve continuity: Carefullyinspect the nerve. One may stimulate thenerve with a nerve stimulator. Neuropraxiadue to mechanical trauma may howevercause failure <strong>of</strong> muscle contraction.Obtain meticulous haemostasis. Use tiesand bipolar diathermy. Employ a Valsalvamanoeuvre to identify venous bleeding.Sealed suction drain: Until drainage
Facial nerve repairUnlike with malignant tumours, the facialnerve and its branches can virtually alwaysbe dissected free from benign neoplasms.Isolated midfacial branches may besacrificed without causing visible facialdysfunction. Transection <strong>of</strong> the temporal(frontal) and marginal mandibular nerveshowever results in disfiguring facialasymmetry; these nerves should berepaired with 8/0 nylon/proline epineuralsutures. When primary nerve repair is notpossible due to undue tension or nerveresection, then the nerve can be graftedwith greater auricular nerve, or sural nerve.The greater auricular nerve isapproximately the same diameter as thefacial nerve trunk, and has a few branchesthat can be used to graft more than onefacial nerve branch. The sural nerveprovides greater length and more branchesand is better suited to bridging longerdefects and for grafting to more peripheralbranches (Figure 22).hypoglossal nerve to expose the nerveaxons (Figure 23).Figure 23: Hypoglossal/facial nerve graftAuthor & EditorJohan Fagan MBChB, FCORL, MMedPr<strong>of</strong>essor and ChairmanDivision <strong>of</strong> OtolaryngologyUniversity <strong>of</strong> Cape TownCape TownSouth Africajohannes.fagan@uct.ac.zaAnastomosis toVIIn trunkGreater auricular ninterposition graftAnastomosis to XIInFigure 22: Sural nerve graftThe Open Access Atlas <strong>of</strong> Otolaryngology, Head &Neck Operative Surgery by Johan Fagan (Editor)johannes.fagan@uct.ac.za is licensed under a CreativeCommons Attribution - Non-Commercial 3.0 UnportedLicenseWhen the proximal end <strong>of</strong> the facial nerveis not available, e.g. with extensiveproximal perineural tumour extension, thena hypoglossal-facial nerve interpositiongraft can be used to restore facial tone andmovement. The nerve graft is sutured endto-endto the distal facial nerve(s), andend-to-side to the hypoglossal nerve aftercutting about 25% into the side <strong>of</strong> the10