Mastoidectomy and epitympanectomy - Vula - University of Cape Town
Mastoidectomy and epitympanectomy - Vula - University of Cape Town
Mastoidectomy and epitympanectomy - Vula - University of Cape Town
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
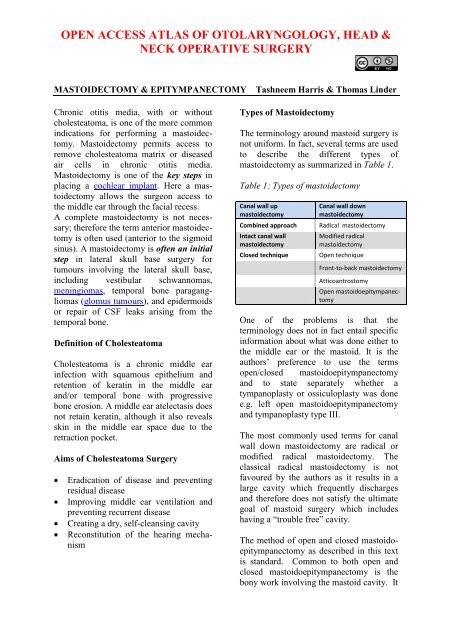
OPEN ACCESS ATLAS OF OTOLARYNGOLOGY, HEAD &NECK OPERATIVE SURGERYMASTOIDECTOMY & EPITYMPANECTOMY Tashneem Harris & Thomas LinderChronic otitis media, with or withoutcholesteatoma, is one <strong>of</strong> the more commonindications for performing a mastoidectomy.<strong>Mastoidectomy</strong> permits access toremove cholesteatoma matrix or diseasedair cells in chronic otitis media.<strong>Mastoidectomy</strong> is one <strong>of</strong> the key steps inplacing a cochlear implant. Here a mastoidectomyallows the surgeon access tothe middle ear through the facial recess.A complete mastoidectomy is not necessary;therefore the term anterior mastoidectomyis <strong>of</strong>ten used (anterior to the sigmoidsinus). A mastoidectomy is <strong>of</strong>ten an initialstep in lateral skull base surgery fortumours involving the lateral skull base,including vestibular schwannomas,meningiomas, temporal bone paragangliomas(glomus tumours), <strong>and</strong> epidermoidsor repair <strong>of</strong> CSF leaks arising from thetemporal bone.Definition <strong>of</strong> CholesteatomaCholesteatoma is a chronic middle earinfection with squamous epithelium <strong>and</strong>retention <strong>of</strong> keratin in the middle ear<strong>and</strong>/or temporal bone with progressivebone erosion. A middle ear atelectasis doesnot retain keratin, although it also revealsskin in the middle ear space due to theretraction pocket.Aims <strong>of</strong> Cholesteatoma SurgeryEradication <strong>of</strong> disease <strong>and</strong> preventingresidual diseaseImproving middle ear ventilation <strong>and</strong>preventing recurrent diseaseCreating a dry, self-cleansing cavityReconstitution <strong>of</strong> the hearing mechanismTypes <strong>of</strong> <strong>Mastoidectomy</strong>The terminology around mastoid surgery isnot uniform. In fact, several terms are usedto describe the different types <strong>of</strong>mastoidectomy as summarized in Table 1.Table 1: Types <strong>of</strong> mastoidectomyCanal wall upmastoidectomyCombined approachIntact canal wallmastoidectomyClosed techniqueCanal wall downmastoidectomyRadical mastoidectomyModified radicalmastoidectomyOpen techniqueFront-to-back mastoidectomyAtticoantrostomyOpen mastoido<strong>epitympanectomy</strong>One <strong>of</strong> the problems is that theterminology does not in fact entail specificinformation about what was done either tothe middle ear or the mastoid. It is theauthors’ preference to use the termsopen/closed mastoido<strong>epitympanectomy</strong><strong>and</strong> to state separately whether atympanoplasty or ossiculoplasty was donee.g. left open mastoido<strong>epitympanectomy</strong><strong>and</strong> tympanoplasty type III.The most commonly used terms for canalwall down mastoidectomy are radical ormodified radical mastoidectomy. Theclassical radical mastoidectomy is notfavoured by the authors as it results in alarge cavity which frequently discharges<strong>and</strong> therefore does not satisfy the ultimategoal <strong>of</strong> mastoid surgery which includeshaving a “trouble free” cavity.The method <strong>of</strong> open <strong>and</strong> closed mastoido<strong>epitympanectomy</strong>as described in this textis st<strong>and</strong>ard. Common to both open <strong>and</strong>closed mastoido<strong>epitympanectomy</strong> is thebony work involving the mastoid cavity. It
involves first identifying the importantl<strong>and</strong>marks (= skeletonization = leaving athin shelf <strong>of</strong> bone covering the importantstructure) before removing the disease <strong>and</strong>maximum exposure for completeexenteration <strong>of</strong> the disease.A closed technique, keeping the posteriorcanal wall in place <strong>and</strong> working transcanal(following a proper canalplasty) <strong>and</strong>transmastoid (with or without posteriortympanotomy) is suggested in moderatelypneumatized <strong>and</strong> ventilated ears withsufficient exposure to remove the disease.Open mastoidoepitymanectomy involvescomplete exenteration <strong>of</strong> the mastoid aircell system (e.g. retrosigmoid, retr<strong>of</strong>acial,perilabyrinthine) <strong>and</strong> the epitympanum(removal <strong>of</strong> incus <strong>and</strong> malleus head,exenteration <strong>of</strong> the supralabyrinthine <strong>and</strong>supratubal cells) <strong>and</strong> is indicated in poorlypneumatized <strong>and</strong> ventilated ears withlimited access <strong>and</strong> exposure. It requiresskeletonization <strong>of</strong> the facial nerve alongthe mastoid segment to lower the posteriorcanal wall to the facial nerve (still coveredby bone). The mastoid area behind thefacial nerve is later obliterated with amuscle flap to keep the volume <strong>of</strong> the finalcavity low <strong>and</strong> avoid discharging ears.The other method <strong>of</strong> “canal wall down”mastoidectomy is front-to-back mastoidectomy.Surgeons may elect this approachwhen it has been decided in advance thatthe canal wall will be taken down e.g. witha sclerotic mastoid. The principles <strong>of</strong> thismethod are that one follows the disease,i.e. the mastoid is only opened as far as theextent <strong>of</strong> the disease. The only problemwith this approach is that one has to becertain that there are no more mastoid cellspresent as incomplete exenteration willcause a discharging cavity.Surgical TerminologyCanalplasty: Enlargement <strong>of</strong> the externalear canal while avoiding injury to thetemporom<strong>and</strong>ibular joint anteriorly <strong>and</strong> themastoid air cells posteriorly (Video)Epitympanotomy: Partial removal <strong>of</strong> thelateral wall <strong>of</strong> the attic to expose the head<strong>of</strong> the malleus <strong>and</strong> incus in order to removes<strong>of</strong>t tissue pathology in the epitympanum;the ossicles are left in placeEpitympanectomy: Removal <strong>of</strong> the lateralwall <strong>of</strong> the attic, with removal <strong>of</strong> the incus<strong>and</strong> head <strong>of</strong> malleus <strong>and</strong> with exenteration<strong>and</strong> exteriorisation <strong>of</strong> supralabyrinthinecellsCortical mastoidectomy: Also referred toas simple mastoidectomy, it entailsexenteration <strong>of</strong> the mastoid air cells <strong>and</strong> isperformed most commonly for acutemastoiditisPosterior tympanotomy: Drilling away <strong>of</strong>the bone between the pyramidal (mastoid)segment <strong>of</strong> the facial nerve, <strong>and</strong> the lateralbony canal <strong>and</strong> chorda tympani resulting inaccess to the middle ear from the mastoid.Posterior tympanotomy may be done forthe following reasons:As part <strong>of</strong> a closed mastoido<strong>epitympanectomy</strong>(combined approach)when removing cholesteatomaTo remove pus from the region <strong>of</strong> theround window in acute bacterial orviral otitis media with sensorineuralhearing lossTo provide access to the promontory orround window in cochlear implantsurgery <strong>and</strong> access to incus or roundwindow with insertion <strong>of</strong> the VibrantSoundbridgeClosed mastoido<strong>epitympanectomy</strong> withtympanoplasty: This includes acanalplasty, mastoidectomy, epitympanec-2
tomy, (posterior tympanotomy) <strong>and</strong>tympanoplasty. The external bony canal ispreserved. The drawback <strong>of</strong> this approachis the limited view into the anteriorepitympanum <strong>and</strong> the sinus tympani incases <strong>of</strong> limited pneumatisation <strong>and</strong>cholesteatoma formationOpen mastoido<strong>epitympanectomy</strong> (withobliteration): This involves the radicalexenteration <strong>of</strong> the tympanomastoid tractswith exteriorisation <strong>of</strong> the surgical cavity,<strong>and</strong> lowering <strong>of</strong> the posterior bony canalwall to the level <strong>of</strong> the skeletonised facialnerve. In order to reduce the size <strong>of</strong> thecavity, especially with moderately-wellpneumatised mastoids, the mastoid tip isremoved <strong>and</strong> a myosubcutaneous occipitalflap is created to reduce the size <strong>of</strong> thecavity. Meatoplasty is routinely performed.Open/Closed Mastoido<strong>epitympanectomy</strong>Age is not a limiting factor as childrenbehave equally well with open MET’s asdo adult patients!Deciding whether to do open or closedcavity mastoido<strong>epitympanectomy</strong> maydepend on the factors listed in Table 2.Applied AnatomyKnowledge <strong>of</strong> middle ear <strong>and</strong> temporalbone anatomy is vital to underst<strong>and</strong>ing theconcepts <strong>of</strong> surgical management. It isimperative to practise the surgery <strong>and</strong> learnthe 3-dimensional temporal bone anatomyin a temporal bone laboratory. Theimportant l<strong>and</strong>marks <strong>and</strong> structures will behighlighted with the surgical steps.Table 2: Indications for closed vs. opencavity mastoido<strong>epitympanectomy</strong> (MET)Factor Closed MET Open METExtent <strong>of</strong>diseasePneumatisationAerationFollow-upLimitedPrimary surgerywith sufficientspaceGoodpneumatisationAir in middleear <strong>and</strong> mastoidair cellsGood 5 yearfollow-upanticipatedPreoperative assessmentHistoryLargecholesteatomaLabyrinthinefistulaOthercomplicationsRecurrentcholesteatomaafter previousclosed METPoorpneumatisationGlue in middleearGranulation tissuein mastoid aircellsBleedingPoor 5 yearfollow-upanticipatedPatients with chronic ear diseasefrequently have a longst<strong>and</strong>ing history <strong>of</strong>hearing loss or chronic otorrhoea. It isimportant to establish whether there is ahistory <strong>of</strong> previous surgery. Foul smellingotorrhoea is a clear hint <strong>of</strong> cholesteatoma.OtomicroscopyThis is an important means to determinethe presence <strong>of</strong> cholesteatoma <strong>and</strong> it helpsto define the extent <strong>of</strong> disease. The earshould be thoroughly cleaned <strong>of</strong> secretions<strong>and</strong> debris. Findings may include a3
etraction pocket with accumulation <strong>of</strong>keratin in the attic or in the posterosuperiorquadrant <strong>of</strong> the tympanic membrane,granulation tissue or a polyp (Figures 1 &2). A polyp “signals” an underlyingcholesteatoma.Pneumatic otoscopyThis should be routinely performed todetermine the presence <strong>of</strong> a positive fistularesponse. A negative response, howeverdoes not exclude a fistula.AudiologyPure tone audiometry should be obtainedwith air <strong>and</strong> bone conduction, <strong>and</strong> alsospeech reception thresholds should bedetermined. These should be done within 3months <strong>of</strong> surgery.High resolution CT (HRCT) scanFigure 1: Right ear: Granulation tissue inthe attic <strong>and</strong> a retracted tympanicmembrane; bony erosion <strong>of</strong> the superiorcanal wall; lenticular <strong>and</strong> long process <strong>of</strong>the incus is present with retraction <strong>of</strong>posterosuperior quadrant <strong>of</strong> tympanicmembrane; tympanic membrane is indirect contact with the stapessuperstructure (myringostapediopexy)Figure 2. Right ear: Polyp obscuringposterosuperior retraction pocketAll patients undergoing surgery shouldideally have preoperative imaging asHRCT (0,5mm cuts) is invaluable for bothfor diagnosis <strong>and</strong> surgical planning.Preoperative counselling is m<strong>and</strong>atorywith any surgical procedure. Informationgained from the CT scan enables thesurgeon to discuss in detail with the patientwhat the surgical goals <strong>and</strong> risks <strong>of</strong> thesurgery are, as well as the possibility <strong>of</strong> astaged procedure <strong>and</strong> follow-up routine.Diagnostic value <strong>of</strong> HRCTSpecificity is poor with mass lesionswhich may include granulation tissue,secretions, cholesterol granuloma or aneoplasmIt therefore cannot be used todefinitively diagnose cholesteatoma,which remains a clinical diagnosisbased on otoscopic findingsFindings highly suggestive <strong>of</strong>cholesteatoma include the presence <strong>of</strong>an expansile s<strong>of</strong>t tissue mass; retraction<strong>of</strong> the tympanic membrane; erosion <strong>of</strong>the scutum; erosion <strong>of</strong> the ossicles;sharp erosion <strong>of</strong> bone; extension <strong>of</strong> thelesion medial to the otic capsule; <strong>and</strong>erosion <strong>of</strong> the tegmen tympani4
Surgical planning with HRCTHRCT <strong>of</strong> the temporal bone is theotologist’s road map <strong>and</strong> one should have asystematic approach when evaluating theCT scan. The decision whether to do anopen or closed cavity operation depends onthe degree <strong>of</strong> pneumatisation <strong>and</strong>ventilation <strong>of</strong> the temporal bone <strong>and</strong> extent<strong>of</strong> disease, all <strong>of</strong> which can be determinedon HRCT. Axial as well as coronal imagesare needed for preoperative evaluation <strong>and</strong>should always be in the operating theatre<strong>and</strong> visible to the surgeon as intraoperativereference (<strong>and</strong> not in the patient’s chart!)CT scan checklist1. Pneumatisation: The temporal bonemay be well-pneumatised, may havereduced pneumatisation, or besclerotic. This gives importantinformation about what the eustachiantube function during the first 4 years <strong>of</strong>the patient’s life was like. It isimportant to assess the pneumatisation<strong>of</strong> the petrous apex as well. Poorventilation favours an open cavityprocedure2. Ventilation: This is assessed by theaeration <strong>of</strong> the middle ear <strong>and</strong> mastoidair cells. Opacification <strong>of</strong> the middleear or mastoid cells suggests poorventilation <strong>of</strong> the middle ear cleft. Thisgives the best information abouteustachian function at the present time.Poor ventilation <strong>of</strong> already-impairedpneumatised cell tracts favours anopen cavity procedure3. Ear canal: Evaluate the thickness <strong>of</strong>the bone anteriorly <strong>and</strong> posteriorly.This is important when one needs to doa canalplasty as the anterior relation <strong>of</strong>the tympanic bone is the temporom<strong>and</strong>ibularjoint <strong>and</strong> posteriorly aremastoid air cells. These should not bebreached when doing a canalplasty4. Size <strong>and</strong> presence <strong>of</strong> emissary vein: Alarge emissary vein can causetroublesome bleeding if notanticipated!5. Sigmoid sinus <strong>and</strong> its relation in themastoid cavity: In children the sigmoidmay be very close to the lateral surface<strong>of</strong> the mastoid; in adults a sigmoidsinus malformation may only beappreciated on preoperative CT scan.When the sigmoid sinus lies veryanteriorly in the mastoid cavity it maybe difficult to perform a posteriortympanotomy due to very limitedexposure. In revision surgery, it isimportant to assess whether thesigmoid sinus has been exposed orwhether it is still covered by bone. Ifthe sigmoid sinus has been exposed atprevious surgery, it will be coveredwith scar tissue which becomesdifficult to elevate thus riskingbreaching the sinus when elevating theperiosteal flap6. Jugular bulb: Is it high-riding (up tothe level <strong>of</strong> annulus)? Is it dehiscent?7. Carotid artery: Is there dehiscence,especially at the level <strong>of</strong> the eustachiantube?8. Tegmen tympani: What is the shape <strong>of</strong>the tegmen? Is it flat or does it slopeupwards with cells lying medial to it?Is it low-lying? Is it dehiscent? A bonydefect <strong>of</strong> the tympanic tegmen oranterior wall <strong>of</strong> the epitympanumshould raise the suspicion <strong>of</strong> anencephalocoele or cholesteatomaextending into the middle cranial fossa.This requires further imaging in theform <strong>of</strong> an MRI9. Facial nerve: The tympanic segmentmay be dehiscent, especially inchildren or in the presence <strong>of</strong>cholesteatoma. In cases <strong>of</strong> revisionsurgery, it is important to knowwhether the facial nerve has been leftexposed in an open cavity whenelevating the tympanomeatal flap5
10. Is there a fistula <strong>of</strong> the lateralsemicircular canal?11. Extent <strong>of</strong> disease: Does it only involvethe mesotympanum or does it extendfurther into the mastoid cavity? Is thepetrous apex involved?12. Status <strong>of</strong> ossicular chain: Are theossicles present or have they beeneroded?When approaching the mastoid tip theskin incision follows the skin tensionlines which run directly inferiorly (notcurved) towards the neckPreoperative preparationDrugs: A single intravenous dose <strong>of</strong>amoxicillin with clavulanic acid <strong>and</strong> ananti-emetic is given preoperatively.However antibiotics are unnecessary witha dry ear, even in presence <strong>of</strong> acholesteatoma. Low dose subcutaneousheparin is recommended to prevent deepvein thrombosis with prolonged surgery.Positioning: The patient lies supine withthe head rotated away from the surgeon.Avoid overextension in children; Down’ssyndrome is associated with atlantoaxialsubluxation.Facial nerve monitoring: Avoid longactingmuscle relaxants so that the facialnerve can be monitored.Figure 3. Postauricular skin incision(left ear)Elevate the skin flap towards theexternal ear canal. Cut through thepostauricular muscle to reach thecorrect plane just superficial totemporalis fascia. A large rake can beused to retract the pinna forward(Figure 4)For adequate exposure the superiorincision has to be made at the 12o’clock position relative to the bony earcanal (Figure 4)Closed Mastoido<strong>epitympanectomy</strong>Skin Incision <strong>and</strong> flapInfiltrate the area <strong>of</strong> the postauricularskin incision as with local anaesthetic(lidocaine 1% <strong>and</strong> adrenaline diluted to1:200 000)Make a curved skin incision about1,5cm behind the postauricular sulcuswith a #10 blade extending from justabove linea temporalis to the mastoidtip. Do not place the incision in thepostauricular sulcus (Figure 3)Figure 4: Flap elevated in plane justsuperficial to temporalis fascia6
Periosteal flapAn anteriorly based periosteal flap isdeveloped, about 1,5cm in length(Figure 5)CanalplastyIf there are any bony overhangs acanalplasty is performedA canalplasty should always be donefirst as it defines the anterior limit <strong>of</strong>your mastoidectomyFor a detailed description <strong>of</strong> thesurgical technique readers arereferred to the canalplasty chapter orcanalplasty videoThe entire annulus should be visiblewith one view <strong>of</strong> the microscopefollowing canalplasty (Figure 7)Figure 5: Periosteal flapA periosteal raspatory is used toelevate the flap from the bone until thespine <strong>of</strong> Henlé <strong>and</strong> the entrance tobony canal come into view (Figure 6)Figure 7: Completed canalplasty withentire annulus visibleElevation <strong>of</strong> tympanomeatal flapFigure 6: Raspatory used to elevateflap until spine <strong>of</strong> Henlé <strong>and</strong> theentrance to bony canal come into viewA sharp towel clip can be placed on theperiosteal flap at the level <strong>of</strong> the earcanal to retract the pinna forwardIn an adult two self-retaining retractorsare placed between the skin edges <strong>and</strong>s<strong>of</strong>t tissue for exposure; one selfretainingretractor is usually sufficientin a childThe posterior meatal skin flap iselevated towards the annulus using amicroraspatory in one h<strong>and</strong> <strong>and</strong> a piece<strong>of</strong> ribbon gauze which has been soakedin adrenalineThe microsuction is never placeddirectly onto the meatal skin for risk <strong>of</strong>injury <strong>of</strong> the skin flapElevate the annulus from its sulcusaway from the pathological area e.g. aposterior retraction pocket wouldpreclude entering the middle ear at thelevel <strong>of</strong> the posterior tympanic spine asthis would breach the cholesteatomasac (Figure 8)7
eflect periosteum posteriorly whereyou may encounter an emissary vein,<strong>and</strong> inferiorly to the mastoid tip12345Figure 8: Tympanomeatal flap <strong>and</strong>annulus have been elevated <strong>and</strong> middleear is entered below the pathologicalareaInspection <strong>of</strong> middle earThe middle ear in Figure 8 has beenentered at 6 o’clock after excluding adehiscent jugular bulb on CT scanDefine the extent <strong>of</strong> the disease in themiddle ear <strong>and</strong> around the ossicularchainFigure 9: Surface markings <strong>of</strong> left ear:Temporom<strong>and</strong>ibular joint (1); root <strong>of</strong>zygoma (2); external ear canal (3);suprameatal spine (4); mastoid tip (5);Macewen’s triangle (6); opening <strong>of</strong>emissary vein (7)67Division <strong>of</strong> incudostapedial jointTo avoid causing a sensorineuralhearing loss when working in theepitympanum, the incudostapedial jointis divided using a small joint knifeAntrotomy <strong>and</strong> <strong>Mastoidectomy</strong>Note: Always perform antrotomy <strong>and</strong>/ormastoidectomy after the canalplasty hasbeen doneThe principal surgical l<strong>and</strong>marks arelinea temporalis superiorly, the bonyear canal <strong>and</strong> spine <strong>of</strong> Henlé anteriorly<strong>and</strong> the mastoid tip inferiorlyIdentify <strong>and</strong> expose the surgicall<strong>and</strong>marks (Figures 9, 10)Using the mastoid raspatory, reflect theperiosteal tissue superiorly in order toexpose the linea temporalis; thenFigure 10: Completed bony exposureIdentify Macewen’s triangle which issituated posterosuperiorly to theexternal auditory canal. It is boundedanteriorly by the Spine <strong>of</strong> Henlé <strong>and</strong>approximates the position <strong>of</strong> theantrum medially (Figure 10, 11)AntrotomyA common mistake is to search for theantrum very low, thus endangering thefacial nerveThe safest way to finding the antrum isto follow dura8
The tegmen tympani marks the superiorlimit <strong>of</strong> the dissectionStart drilling above linea temporalisFigures 11, 12)to avoid touching the ossicles whichwould induce sensorineural hearinglossLSSCDural plateFigure 11: Yellow lines indicate whereto drill along; red star indicates whereto commence drillingFigure 13. Dural plate <strong>and</strong> lateralsemicircular canalThe body <strong>and</strong> short process <strong>of</strong> incusare the next l<strong>and</strong>marks one encounters;the incus is <strong>of</strong>ten first identified by itsrefraction in the irrigation fluid (Figure14)Medial to the incus the tympanicsegment <strong>of</strong> the facial nerve (VIIn) isidentified (Figure 14)Figure 12: Drilling along lineatemporalisExpose tegmen tympani (middlecranial fossa dural plate); it isidentified by a change in colour <strong>of</strong> thebone <strong>and</strong> change in the pitch <strong>of</strong> theburr (Figure 13)Always skeletonize the dura <strong>of</strong> themiddle cranial fossa (dura seen shiningthrough thin layer <strong>of</strong> bone) <strong>and</strong> followthe dural plate <strong>of</strong> the middle cranialfossa in an anteromedial directionThe lateral semicircular canal isencountered next (Figure 13)The direction <strong>of</strong> the drilling now has tobe changed to a medial-to-lateral actionFigure 14. Postero-anterior viewthrough antrotomy <strong>and</strong> aditus adantrum into epitympanumIncusBodyShort processVIInDural plateLSCC9
Drilling tipsAvoid keyhole surgery; work through awide spaceThe tip <strong>of</strong> the drill should always bevisibleNever drill behind edges <strong>of</strong> boneDrilling should always be parallel toany structure you are trying topreserve e.g. facial nerve, sigmoidsinusWhen drilling deeper in the mastoidcavity the burr needs to be lengthenedOne cannot lengthen a cutting burr asthis will cause the drill to jump withthe risk <strong>of</strong> injuring structures (Figure15)<strong>Mastoidectomy</strong>Follow the sinodural plate posteriorlyup to the sinodural angle, which is thearea between the sigmoid sinus <strong>and</strong>duraLike the dural plate, the sinus plate isidentified by the change in colour <strong>of</strong>the bone <strong>and</strong> a change in the pitch <strong>of</strong>the burrSkeletonise the sigmoid sinus; do notexpose the sigmoid sinus, but leave acovering <strong>of</strong> bone over the sinus.(Figure 17)Figure 17: Sigmoid sinus, sinoduralangle <strong>and</strong> dural plateDural plateSinoduralangleSigmoidsinusFigure 15: Correct length <strong>of</strong> a cuttingburr in the drillTherefore if it is necessary to lengthenthe burr, then change to a roughdiamond or diamond burr (Figure 16)Figure 16: A diamond burr can belengthened in order to safely drilldeeper in the mastoidThe lateral <strong>and</strong> posterior semicircularcanals are identified <strong>and</strong> theretrolabyrinthine air cells areexenteratedNext identify the facial nerveThe superior l<strong>and</strong>marks for the mastoidsegment <strong>of</strong> the facial nerve are thelateral semicircular canal, to which thefacial nerve runs anteroinferiorly, <strong>and</strong>the posterior semicircular canal, towhich the nerve runs 2,5mm anteriorto. The figure below is a cadaverdissection which demonstrates therelationship between the lateralsemicircular canal, posterior semicircularcanal <strong>and</strong> facial nerve (Figure18)10
DuraSCCSigmoid sinusIncusLSCVIInPSCCFigure 18: Relations <strong>of</strong> VIIn to shortprocess <strong>of</strong> incus; superior semicircularcanal (SCC); lateral semicircularcanal (LSC); posterior semicircularcanal (PSC); dura; <strong>and</strong> sigmoid sinusFinding the facial nerve along digastricridge <strong>and</strong> the stylomastoid fibers is avery safe way <strong>of</strong> identifying the facialnerve away from any mastoidpathologyIt requires proper drilling technique<strong>and</strong> can easily be learned in thetemporal bone laboratoryWhen searching for the mastoidsegment <strong>of</strong> facial the nerve, a large (4-5mm) diamond burr is usedUse ample irrigation to prevent thermalinjury to the nerveThe digastric ridge is the distall<strong>and</strong>mark for the mastoid segment <strong>of</strong>the facial nerve. It is a smooth convexbone found close to the mastoid tip.The digastric ridge can be difficult t<strong>of</strong>ind in poorly pneumatised temporalbones. Once the sigmoid sinus hasbeen skeletonised the digastric ridge isfound by drilling inferiorly to the sinus,close to the mastoid tip, from laterallyto medially, in a horizontal direction.Periosteal fibres run anteriorly from thedigastric ridge in a plane perpendicularto the ridge. The facial nerve can belocated proximal to the stylomastoidforamen by drilling the last <strong>of</strong> theseperiosteal fibres. One <strong>of</strong>ten encountersthe sensory branch <strong>of</strong> facial nerve(which innervates the posterior wall <strong>of</strong>the external auditory canal <strong>and</strong> aportion <strong>of</strong> the tympanic membrane)just above the stylomastoid foramen.Skeletonise the nerve by drilling in awide plane between the lateralsemicircular canal proximally <strong>and</strong> thestylomastoid foramen distally, workingfrom anteriorly to posteriorly (Figure19)Figure 19: Distal portion <strong>of</strong> mastoidsegment <strong>of</strong> facial nerve (arrow) isidentified close to digastric ridgeAlways drill parallel to the course <strong>of</strong>the facial nerve <strong>and</strong> use lots <strong>of</strong> waterfor irrigation. Drill along the lateralaspect <strong>of</strong> the nerve; do not drill behind<strong>and</strong> medial to the fallopian canalWatch out for an early take-<strong>of</strong>f <strong>of</strong> thechorda tympani close to thestylomastoid foramenOnce the facial nerve has beenidentified, the retr<strong>of</strong>acial cells can beexenteratedPosterior tympanotomyThe facial nerve is skeletonised leavinga thin shelf <strong>of</strong> bone covering the nerveIt is followed proximally towards itspyramidal segment, just inferior to thelateral semicircular canalThe facial recess is approached bydrilling away the bone situated11
etween the pyramidal segment <strong>of</strong> thefacial nerve posteriorly, the chordatympani, <strong>and</strong> the fossa incudissuperiorly (Figure 20)IncusChordaPTympanotomyVIInFigure 21: Direction <strong>of</strong> drilling withepitympanotomy or <strong>epitympanectomy</strong>Figure 20: L<strong>and</strong>marks for posteriortympanotomy are VIIn, chorda tympani<strong>and</strong> short process <strong>of</strong> incusIn the absence <strong>of</strong> disease in the facialrecess, the stapes superstructure isvisible through the tympanotomyFor removal <strong>of</strong> cholesteatoma in facialrecess one has to work from both sides<strong>of</strong> the intact posterior external auditorycanal wallEpitympanotomyIf the cholesteatoma does not extendsignificantly into the epitympanum, anepitympanotomy (atticotomy) isperformedThis involves exposure <strong>of</strong> the head <strong>of</strong>the malleus <strong>and</strong> the incus to removes<strong>of</strong>t tissue from the epitympanumThe lateral wall <strong>of</strong> the epitympanumor attic is removed with a diamondburr; drilling is commenced at 12o’clock relative to the ear canal, takingcare not to make drill contact with themalleus or incus which is immediatelymedial to the outer attic wall, or tobreach the dural plate above (Figure21)EpitympanectomyThis is indicated when cholesteatomaextends medial to the ossicles oroverlies the lateral semicircular canal;in cases <strong>of</strong> bony erosion <strong>of</strong> the ossiclesdue to cholesteatoma, the ossicles needto be removedOnly recently, KTP laser evaporation<strong>of</strong> cholesteatoma matrix has beendiscussedThe incus is removed by mobilising itwith a 2,5mm. 45° hook <strong>and</strong> rotating itlaterally, taking care not to injure theunderlying facial nerveThe malleus head is severed with amalleus nipper applied across its neck.The malleus nipper is held anteriorlybetween the thumb <strong>and</strong> index finger tostabilise it when the malleus head isdividedThe head <strong>of</strong> the malleus is removedleaving the tensor tympani tendonintactClear cholesteatoma from theepitympanumDetailed knowledge <strong>of</strong> facial nerveanatomy is crucial to avoid injury tothe nerve when drilling or removingcholesteatoma in the epitympanumThe tympanic <strong>and</strong> labyrinthinesegments <strong>and</strong> geniculum all lie in this12
very confined space <strong>and</strong> may bedehiscentThe tympanic segment lies in the floor<strong>of</strong> the anterior epitympanic recess (Fig22)TTVIInCogStRCPTTympETFigure 22: Anatomy <strong>of</strong> anteriorepitympanic recess: Facial nerve(VIIn); Tegmen tympani (TT); Cog;Supratubal recess StR; Cochleariformprocess (CP); Eustachian tube (ET)The cochleariform process is a fairlyconsistent l<strong>and</strong>mark <strong>and</strong> the nerve liesdirectly superior to it; the semicanal <strong>of</strong>the tensor tympani is sometimesmistaken for the facial nerve; howeverthis canal ends at the cochleariformprocess (Figure 22)The cog is a bony process in theanterior epitympanum which extendsfrom the tegmen tympani <strong>and</strong> points tothe facial nerve (Figure 22)Figure 23 above shows the geniculateganglion <strong>and</strong> greater superficialpetrosal nerve once the Cog <strong>and</strong>cochleariform process have beendrilled awayfenestrating the posterior wall <strong>of</strong> theexternal auditory canalAvoid fenestrating the posterosuperiorcanal wallIdentifying the facial nerve along itscourse in the mastoid is the best way <strong>of</strong>avoiding injury to the nerveMost injuries occur when the facialnerve has not been adequatelyvisualisedDuraVII.LSSCGSPTeTGGVII.TLSCFigure 23: View <strong>of</strong> epitympanum withcog <strong>and</strong> cochleariform process drilledaway: Tympanic (VII.T) <strong>and</strong>Labyrinthine (VII.L) segments <strong>of</strong> facialnerve <strong>and</strong> Geniculate Ganglion (GG)<strong>and</strong> Greater Superficial Petrosal nerve(GSP); Superior Semicircular Canal(SSC); Lateral Semicircular Canal(LSC); Dura; Tensor Tympani tendon(cut) (TeT)Key points: Completed closed mastoido<strong>epitympanectomy</strong>(Figure 24)The posterior canal wall should not betoo thinAvoid drilling too far anteriorly whileexposing the facial nerve <strong>and</strong>Figure 24: Completed closedmastoido<strong>epitympanectomy</strong>13
OssiculoplastyRefer to the chapter on ossiculoplasty <strong>and</strong>incus interposition for detailed surgicalsteps.The following conditions should be presentin order to proceed to an incusinterposition at the time <strong>of</strong> the primarysurgery (Figure 25)Malleus h<strong>and</strong>le presentStapes superstructure intactFootplate mobileCholeasteatoma limited <strong>and</strong> could beremoved entirelyIncus free <strong>of</strong> cholesteatomaAnterior third or half <strong>of</strong> the eardrum ispreserved <strong>and</strong> defines the proper planeSecond-stage surgery is done at 6-12months to ensure stabilisation <strong>of</strong> the graftin cases <strong>of</strong> perforation; to verifyeradication <strong>of</strong> cholesteatoma; <strong>and</strong> to assesswhether there is good middle earventilation <strong>and</strong> whether eustachian tubedysfunction is presentFigure 25: Incus interpositionThe cartilage is cut into 2-3 thin pieces(use a new 10 or 20 #blade)These pieces are aligned so as toslightly overlap each otherTympanic membrane reconstructionRefer to chapter on Myringoplasty <strong>and</strong>tympanoplasty for detailed surgical stepsTemporalis fascia or cartilage isharvestedIf there is diseased middle ear mucosaor retraction <strong>of</strong> the pars tensa, thensilastic sheeting (1mm thickness) isintroduced into the tympanic cavity<strong>and</strong> protympanum to prevent adhesionsbetween the graft <strong>and</strong> the promontoryThe graft always lies medial to theh<strong>and</strong>le <strong>of</strong> malleus (if present);therefore a slit has to be made toaccommodate the tensor tendonWound closure <strong>and</strong> packingThe meatal skin flap is replaced <strong>and</strong>gelfoam pledgets are placedstrategically over the meatal skin flap<strong>and</strong> fascia to secure it over thetympanic sulcusThe external canal is packed with astrip <strong>of</strong> gauze impregnated withantibiotic ointmentAn easyflow drain or tube <strong>of</strong> a suctiondrain (without suction!) is placed in themastoid cavity through a separate skinincision <strong>and</strong> the wound is closed inlayersA mastoid pressure b<strong>and</strong>age is appliedfor 1 dayPosterior canal wall reconstructionConchal or tragal cartilage is used toreconstruct the posterosuperior canalwall14
Open Mastoido<strong>epitympanectomy</strong> (MET)Skin incision: As for Closed METPeriosteal flap: A small periosteal flap ismade in order to preserve the s<strong>of</strong>t tissue formyosubcutaneous occipital flapCanalplasty: As for Closed METInspection <strong>of</strong> middle ear <strong>and</strong> division <strong>of</strong>incudostapedial joint: As for Closed METAntrotomyAs for Closed METWith Open MET you may already havelowered the posterosuperior canal wall<strong>Mastoidectomy</strong> <strong>and</strong> <strong>epitympanectomy</strong>Radical exenteration <strong>and</strong> exteriorisation<strong>of</strong> all cell tracts, includingretr<strong>of</strong>acial, retrolabyrinthine, supralabyrinthine,<strong>and</strong> supratubal cell tractsA common error is not to saucerise thecavity; this limits exposure <strong>and</strong> createsa larger cavityThe more bone one removes, thesmaller the cavityIncomplete exenteration will result in adischarging cavityNever leave bony overhangsLower the facial ridge over the mastoidsegment <strong>of</strong> facial nerveA high facial ridge may cause adischarging mastoid cavityTherefore it is important to skeletonisethe facial nerve in order to lower thefacial ridge sufficientlyLower the facial ridge with a largediamond burr <strong>and</strong> continuous suctionirrigationSkeletonize the facial nerve, keepingthe nerve intact within the bonyfallopian canal, but lowering the boneto the level <strong>of</strong> the facial nerveThe course <strong>of</strong> the nerve can clearly beidentified inferior to the lateralsemicircular canal, anterior to theposterior canal, <strong>and</strong> along thestylomastoid periosteal fibres at thelevel <strong>of</strong> the digastric ridgeRemoval <strong>of</strong> mastoid tipRemoval <strong>of</strong> the mastoid tip will helpreduce the size <strong>of</strong> the cavity byallowing s<strong>of</strong>t tissue to collapse into thecavityThe stylomastoid foramen is medial tothe digastric ridgeAnteriorly where it extends into theexternal ear canal, the drill thereforeremains lateral to the digastric ridgeThe mastoid tip is weakened when onedrills with a diamond drill lateral to thedigastric ridge to expose the muscle atits attachment along the mastoid tip<strong>and</strong> will develop a fracture lineA rongeur is used to remove themobilised mastoid tip by rotating itoutwardsThe remaining s<strong>of</strong>t tissue attachmentcan be cut with scissors pointing to theboneTympanoplastySee chapter on Myringoplasty <strong>and</strong> tympanoplastyfor detailed technique. Notethat if the tympanic membrane <strong>and</strong> annulusare deficient then a tympanic sulcus isdrilled out with a small diamond burr inorder to support the fascial graftObliteration <strong>of</strong> mastoid cavityThe mastoid cavity is small afterexteriorisation <strong>of</strong> a poorly pneumatisedmastoid <strong>and</strong> does not require obliteration.However following exenteration <strong>of</strong> alltracts in a highly pneumatised mastoid, one15
may be left with a large cavity; in suchcases obliteration is necessary to create adry cavityMastoid obliteration with myosubcutaneousoccipital flapThis is an inferiorly-based flap basedon the occipital artery which is rotatedinto the mastoid cavity (Figure 26)Vicryl 2/0 sutures are used to suturethe flap to the exposed digastric muscleto hold the flap in place in the mastoidcavityMeatoplastyFailure to do a meatoplasty with an opencavity can lead to a chronic draining ear. Ameatoplasty is therefore routinelyperformed because for exteriorization <strong>and</strong>self-cleansingA # 11 blade is inserted into theexternal ear canal <strong>and</strong> is directedposterosuperiorly toward the sinoduralangle; the concha is incised throughboth skin <strong>and</strong> cartilage (Figure 27)Figure 26: Inferiorly-based myosubcutaneousoccipital flapThe flap comprises subcutaneous fascia<strong>and</strong> muscleIt extends superiorly behind themastoidectomy cavity from the mastoidtip where it is pedicled; the pedicle hasto be kept wide (3.5cm) enough so thatblood supply is adequateThe tip <strong>of</strong> the flap is just below thelevel <strong>of</strong> the temporalis muscle; thelength is approximately 7.5cmElevate the retroauricular skin from thesubcutaneous fascia using electrocauteryUse a mastoid raspatory to elevate theflap from the boneMastoid emissary veins may beencountered; bleeding is stopped withbipolar coagulation <strong>and</strong>/or diamonddrilling <strong>of</strong> the bony foramen with alarge diamond burr without irrigationFigure 27: Initial incisionHold the skin with forceps <strong>and</strong> usingcurved scissors, separate the skin fromthe conchal cartilage; it is important todirect the curvature <strong>of</strong> the scissorstowards the cartilage <strong>and</strong> not upwardstowards the skin as this may injure theskinOnce sufficient cartilage has beenexposed, excise cartilage circumferentiallywith tympanoplastyscissors; this results in 2 crescentshapedpieces <strong>of</strong> cartilage (Figure 28)The opening is approximately the size<strong>of</strong> the surgeon’s finger16
Gelfoam is placed medially in the earcanalGauze impregnated with Terracortrilointment is used to fill the lateralportion <strong>of</strong> the mastoid cavity <strong>and</strong> earA mastoid pressure dressing is appliedPostoperative care (Figure 30)Figure 28: Exposing cartilage, <strong>and</strong>illustrating cartilage to be removedThe conchal skin flaps are inverted byplacing 2/0 Vicryl sutures through theskin flaps <strong>and</strong> suturing them to thetemporal muscle superiorly <strong>and</strong> to themastoid s<strong>of</strong>t tissues inferiorly. It maybe necessary to place more sutures toimprove the shape <strong>of</strong> the meatalopening (Figure 29)Mastoid drain removed after 24hoursMastoid pressure b<strong>and</strong>age removedafter 24hoursSutures/clips removed after 7-10 daysRibbon gauze with Terracortil ischanged every 2 weeks for 2 monthsAfter the ribbon gauze has beenremoved, topical eardrops (e.g.Otosporin) are applied for 2-4weeksFigure 30: Epithelialised mastoidcavity <strong>and</strong> meatoplasty 4 weeks aftersurgeryFigure 29: Completed meatoplastyIt is important that there are noexposed edges <strong>of</strong> the cartilage as thiscan lead to perichondritisWound closure <strong>and</strong> packingThe retroauricular wound is closed intwo layers using 2/0 Vicryl forsubcutaneous tissue <strong>and</strong> skin clips or3/0 Nylon for the skin. An easy-flowdrain may be insertedPostoperative ImagingCT cannot accurately definecholesteatoma postoperatively, becausethe CT attenuation <strong>of</strong> cholesteatoma isnot specific enough to differentiate itfrom granulation tissue or effusionNon-EPI MRI has better tissuedifferentiation for cholesteatoma <strong>and</strong>has a high sensitivity <strong>and</strong> specificityfor cholesteatomas measuring >5mmThe senior author (T.L) recommendsroutine imaging, ideally with non- EPIdiffusion weighted MRI, at 1 & 3 yearsfollowing closed mastoidoepitympa-17
nectomy when there is concern aboutrecurrent or residual cholesteatomaReferencesFisch U, May J. Tympanoplasty, <strong>Mastoidectomy</strong>,<strong>and</strong> Stapes Surgery. New York:Thieme; 1994Jindal M, Riskalla A, Jiang D, Connor S,O'Connor AF. A systematic review <strong>of</strong>diffusion-weighted magnetic resonanceimaging in the assessment <strong>of</strong> postoperativecholesteatoma. Otol Neurotol 2011; 32(8):1243-9AcknowledgementsThis guide is based on the text by Pr<strong>of</strong>Fisch (Tympanoplasty, <strong>Mastoidectomy</strong>,<strong>and</strong> Stapes Surgery) <strong>and</strong> personalexperience <strong>of</strong> Pr<strong>of</strong> Linder, as well ascourse material for the temporal <strong>and</strong>advanced temporal bone courses conductedannually by Pr<strong>of</strong> Fisch <strong>and</strong> Pr<strong>of</strong> Linder atthe Department <strong>of</strong> Anatomy, <strong>University</strong> <strong>of</strong>Zurich, Switzerl<strong>and</strong>AuthorTashneem Harris MBChB, FCORL,MMED (Otol), Fisch InstrumentMicrosurgical FellowENT SpecialistDivision <strong>of</strong> Otolaryngology<strong>University</strong> <strong>of</strong> <strong>Cape</strong> <strong>Town</strong><strong>Cape</strong> <strong>Town</strong>, South Africaharristasneem@yahoo.comSenior AuthorThomas Linder, M.D.Pr<strong>of</strong>essor, Chairman <strong>and</strong> Head <strong>of</strong>Department <strong>of</strong> Otorhinolaryngology,Head, Neck <strong>and</strong> Facial Plastic SurgeryLucerne Canton Hospital, Switzerl<strong>and</strong>thomas.linder@ksl.chEditorJohan Fagan MBChB, FCORL, MMedPr<strong>of</strong>essor <strong>and</strong> ChairmanDivision <strong>of</strong> Otolaryngology<strong>University</strong> <strong>of</strong> <strong>Cape</strong> <strong>Town</strong><strong>Cape</strong> <strong>Town</strong>South Africajohannes.fagan@uct.ac.zaTHE OPEN ACCESS ATLAS OFOTOLARYNGOLOGY, HEAD &NECK OPERATIVE SURGERYwww.entdev.uct.ac.zaThe Open Access Atlas <strong>of</strong> Otolaryngology, Head &Neck Operative Surgery by Johan Fagan (Editor)johannes.fagan@uct.ac.za is licensed under a CreativeCommons Attribution - Non-Commercial 3.0 UnportedLicense18